From Biol557
Contents
- 1 The urinary system
- 1.1 An introduction to the urinary system
- 1.2 Consisting of the kidneys, ureters, urinary bladder, and urethra, the urinary system has three primary functions
- 1.3 Kidneys are highly vascular structures containing functional units called nephrons, which perform filtration, reabsorption, and secretion
- 1.4 Different segments of the nephron form urine by filtration, reabsorption, and secretion
- 1.5 An Overview of Renal Function
- 1.6 Hydrostatic and colloid osmotic pressures influence glomerular filtration pressure, which in turn affects the glomerular filtration rate
- 1.7 Countercurrent multiplication and the influence of antidiuretic hormone and aldosterone affect reabsorption and secretion
|
[edit] The urinary system
[edit] An introduction to the urinary system
- The urinary system removes most of the physiological waste from the body.
- We'll talk about the organization of the kidney and how it removes waste.
- We'll talk about how urine concentration and volume is controlled.
[edit] Consisting of the kidneys, ureters, urinary bladder, and urethra, the urinary system has three primary functions
- There are three major functions of the urinary system:
- Excretion: the removal of organic waste products from the body fluids; performed by the kidneys.
- Elimination: the discharge (urination, micturition) of wastes from the body; performed by the ureters, bladder, and urethra.
- Homeostatic regulation of the volume and solute concentration of the blood plasma: performed by the kidneys in conjunction with endocrine (and nervous system?) control.
- The urinary system has several other functions:
- Regulating blood volume and blood pressure.
- Regulating plasma concentrations of sodium, potassium, chloride, calcium, and other ions.
- Helping to stabilize blood pH by controlling the loss of hydrogen ions and bicarbonate ions in urine.
- Conserving valuable nutrients, by preventing their excretion in urine.
- Assisting the liver in detoxifying poisons and deaminating amino acids for metabolism by other tissues.
- All of these processes are tightly regulated and if neglected can be deadly.
[edit] Kidneys are highly vascular structures containing functional units called nephrons, which perform filtration, reabsorption, and secretion
- The kidneys lie on either side of the vertebral column.
- There are three mechanisms that stabilize the kidneys in their location:
- the overlying peritoneum,
- contact with neighboring visceral organs, and
- supporting connective tissues.
- The connective tissues that support and protect the kidneys can be broken down into three layers:
- The fibrous capsule lies closest to the kidney and covers the whole organ.
- The perinephric fat capsule is a thick layer of adipose tissue that surrounds the fibrous capsule.
- The renal fascia is a layer of connective tissue that connects to the fibrous capsule of the kidney, to the muscular wall of the thoracic cavity to the posterior, and to the peritoneum to the anterior, thus anchoring the kidney in position.
- Detachment of the kidney from its anchored position can place the kidney at risk for easy injury upon bumping or jarring.
- Adult kidneys are about 10cm by 5.5cm.
- The hillum is the indentation where the renal artery and renal nerves enter the kidney and where the renal vein and ureter exit the kidney.
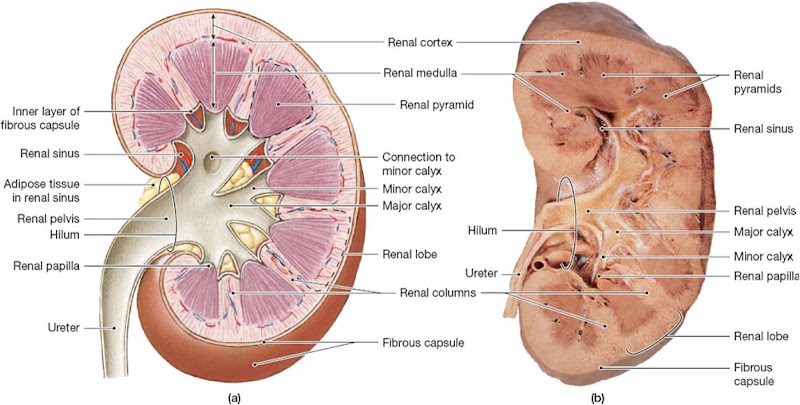
[edit] Sectional anatomy of the kidney
- The fibrous capsule that covers the outside of the kidney also attaches to the outer-most structures just inside the kidney.
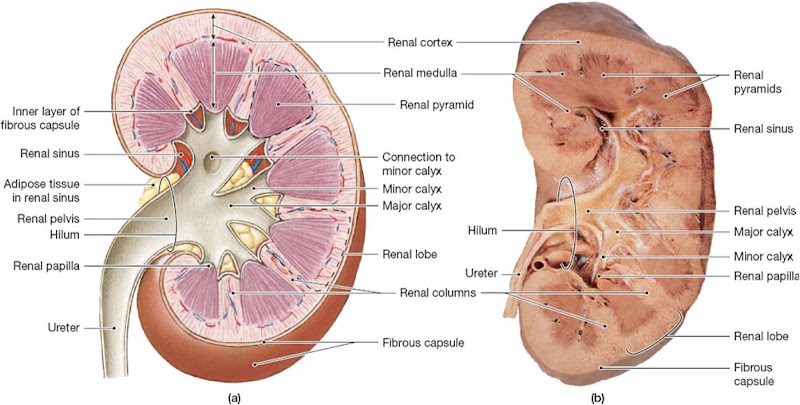
- Urine drains from the papilla into minor calyces which make up major calyces which make up the renal pelvis which drains into the ureter.
- Urine production begins at the nephrons which are located in the cortex of each renal lobe and number about 1.25 million.
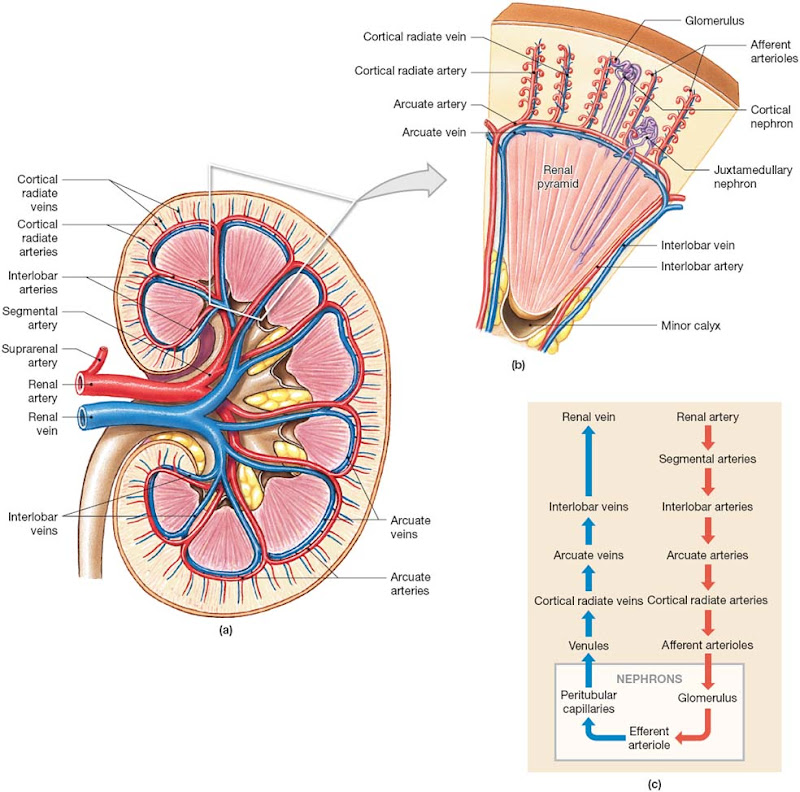
[edit] Blood Supply and Innervation of the Kidneys
- Tons of blood flows through the kidneys: 20-25% of one's cardiac output, about 1.2 liters per minute!
- The renal artery enters the kidney and the divides into smaller and smaller segments which ultimately provide nutrients to the individual nephrons before they join back together to form the renal vein.
- Renal invervation consists of a nerve that enters at the hillum and follows the pathways of the renal artery.
- The nerves of the kidney are primarily sympathetic.
- The nerves of the kidney:
- Adjusts rates of urine production by changing the blood pressure at the kidney and the amount of blood flow.
- Stimulates the release of renin which ultimately retains water and salt from the urine by stimulating enhanced reabsorption.
[edit] Clinical note: Analysis of renal blood flow
- Because PAH (para-aminohippuretic acid) is nearly completely removed from the blood at the kidney, one can measure the renal blood flow by administering it into the blood and comparing concentrations of PAH in the blood plasma and the urine.
- However, it is usually easier to just measure the glomerular filtration rate.
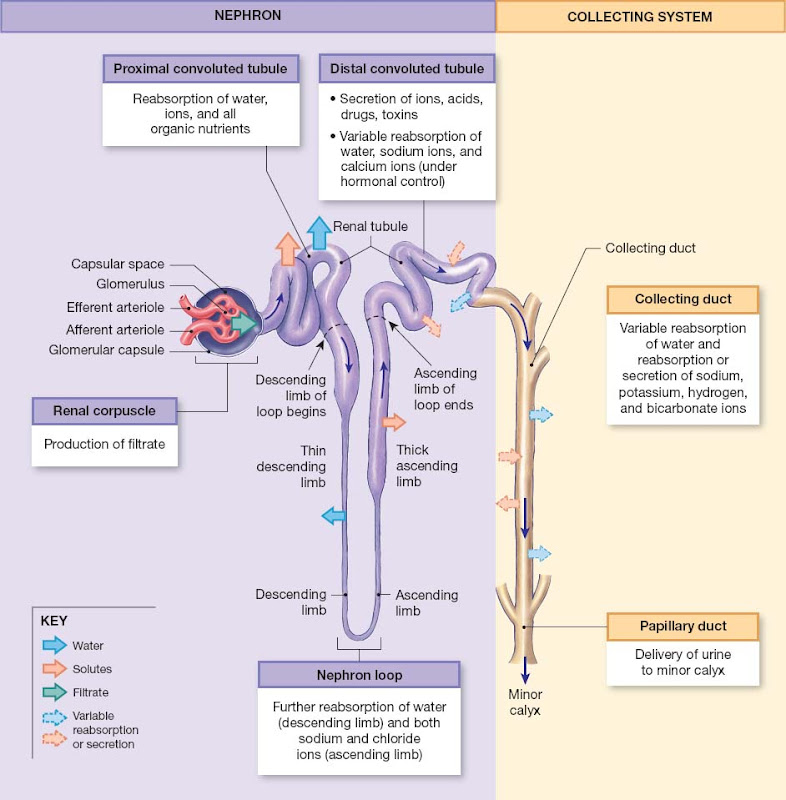
[edit] The Nephron
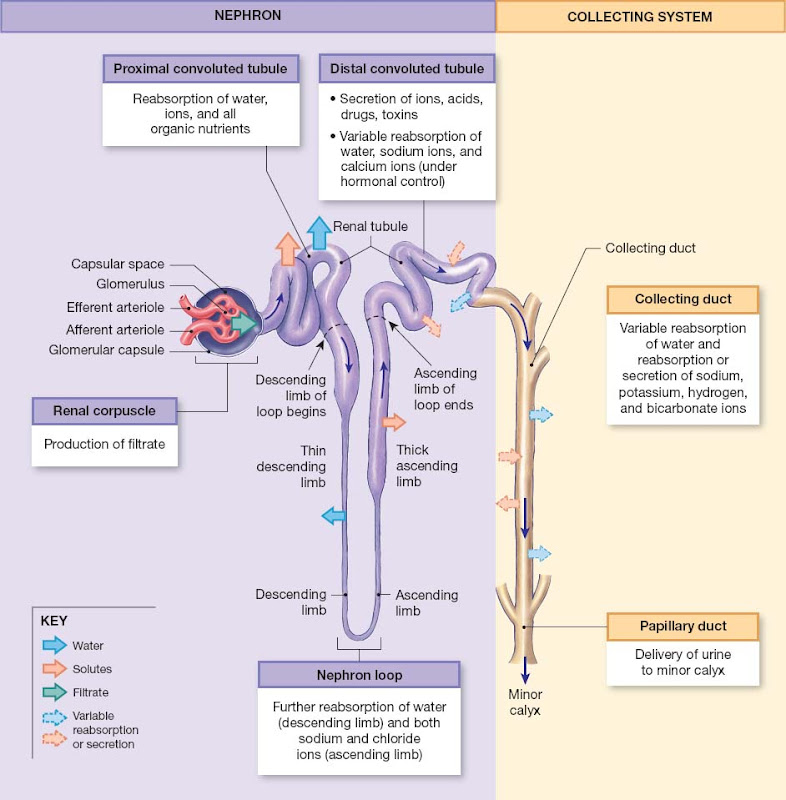
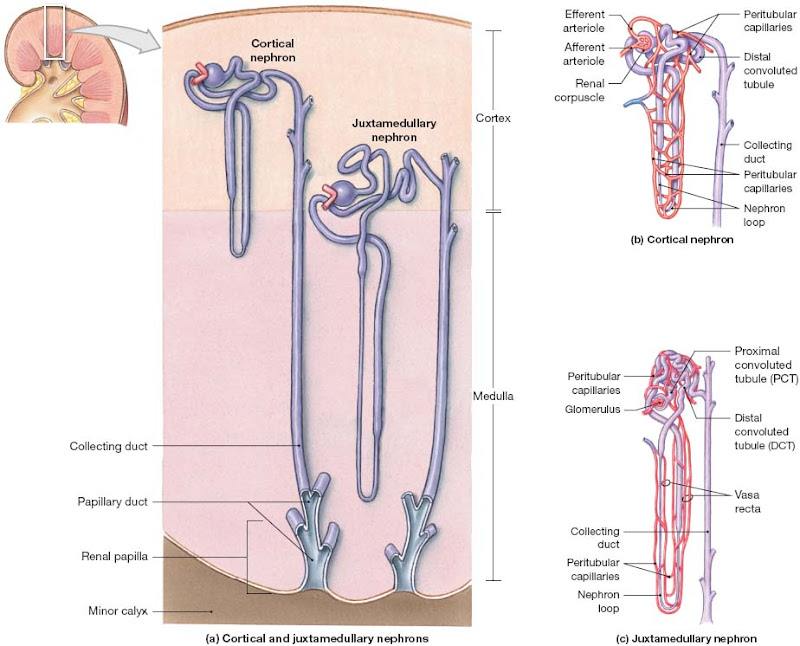
- Blood comes through the afferent arteriole to the renal corpuscle, then continues through the glomerulus and the capillaries there. Blood then leaves the glomerulus through the efferent arteriole, to the peritubular capillaries, and on to the venous system.
- The filtrate that leaves the blood into the nephron at the renal corpuscle is essentially protein-free.
- Filtrate enters the renal tubules where three things occur:
- Reabsorption of 90% of the water in the filtrate,
- Reabsorption of all the useful organic nutrients,
- Secretion of any remaining waste products that weren't filtered at the glomerulus.
- Once filtrate has entered the renal tubules it is also called tubular fluid.
- Remember that the tubular fluid is going to become urine, so when we say that some part of the nephron reabsorbs something we mean that the entity comes out of the tubular fluid (that is, urine) back into the body. Therefore, reabsorbed stuff will not be excreted.
- There are subregions to the renal tubules, each with a particular function:
- The proximal convoluted tubules: serve to reabsorb ions, organic molecules, vitamins and water while secreting drugs, toxins, and acids.
- The loop of Henle (nephron loop):
- The descending loop reabsorbs water.
- The ascending loop reabsorbs ions and helps form a concentration gradient in the medulla.
- The distal convoluted tubules: reabsorb sodium and calcium and secrete drugs, ammonia, toxins, and acids.
- Nephrons empty their tubular fluid into collecting ducts, which begin in the cortex, travel to the medulla, and empty into papillary ducts which drain into the minor calyx (which form major calyces, etc.).
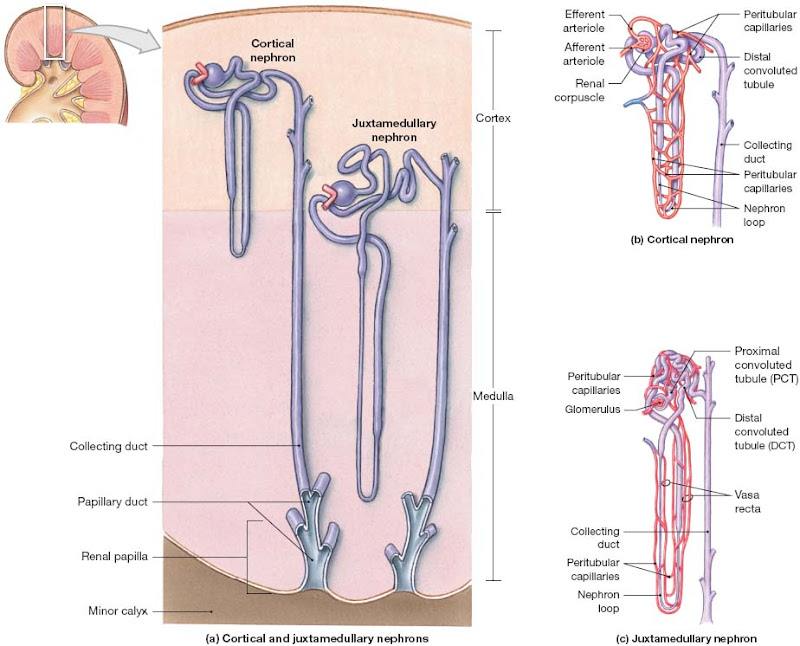
- There are two types of nephrons: cortical nephrons and juxtamedullary nephrons.
- Though the cortical nephrons outnumber the juxtamedullary nephrons and therefore are responsible for most the fitration of the blood, it is the juxtamedullary nephrons that are responsible for generating concentrated urine.
- These two types of nephrons differ in the length of the nephron loop (juxtamedullary nephrons have much longer loops that extend into the medulla) and in the vasculature that follow the renal tubules.
[edit] The renal corpuscle
- The glomerular capsule surrounds the capillaries of the corpuscle and connects the fluid to the opening of the renal tubules.
- The outerwall of the corpuscle is made of a simple squamous cell wall.
- Podocytes are specialized cells of the visceral wall of the corpuscle that extend their foot-like processes onto the areas of the capillaries where filtrate passes through. Podocytes serve as a mesh through which filtrate must be small enough to pass.
- Mesangial cells sit between the capillaries and can respond to angiotensin II, vasopressin, and histamine in order to change the diameter of the capillaries, thus changing the rate of capillary blood flow.
- Fenestrated: "Having windows" per wiktionary.
- The capillaries at the glomerulus are fenestrated to allow lots of stuff to flow out.
- The filtration membrane is made up of the podocyte processes, the fenestrated endothelium of the capillaries, and the dense layer of the capillaries.
- While filtration is passive and effective, many useful molecules that we'd like to keep pass into the tubular fluid along with the many waste molecules that we don't want to keep.
[edit] Clinical note: Glomerulonephritis
- Glomerulonephritis is an inflammation of the glomerulus.
- Any condition that causes a massive immune response can cause this condition which leads to decreased filtration at the glomerulus.
- This disorder is caused by the clogging of the glomerulus by antibodies, which are small enough to get through the dense layer but too large to get through the podocyte processes.
[edit] The proximal convoluted tubule
- The peritubular fluid surrounds the proximal convoluted tubule.
- The cells of the proximal convoluted tubule (PCT) have microvilli on their apical surface.
- The function of the PCT is primarily absorption but can do some secretion.
- The PCT absorbs organic nutrients, ions, water, and plasma proteins (if present).
- The PCT deposits its absorbants into the peritubular fluid.
[edit] The nephron loop
- Each limb (think "ascending" and "descending") contains a thick and thin segment; this refers to the thickness of the cells making up the wall, not to the diameter of the lumen.
- The wall of the thick segment is made up of cuboidal epithelial cells while the thin walls are made of squamous epithelial cells.
- The thick, descending loop pumps sodium and chloride ions out of the tubular fluid (which is especially noticeable in the juxtamedullar nephrons where extraordinarily high concentrations of ions are found in the peritubular fluid).
- The thin descending loop is permeable to water but not to solutes and therefore water moves from the tubular fluid to the peritubular fluid which serves to concentrate the tubular fluid (urine).
[edit] The distal convoluted tubule
- The distal convoluted tubule (DCT) has smaller a smaller diameter than the PCT and does not have microvilli on the apical surface.
- There are three important functions that occur at the DCT:
- the active secretion of ions, drugs, toxins, and acids,
- the selective reabsorption of sodium and calcium (helpful in regulating concentrations of these two ions in the blood plasma),
- the selective reabsorption of water (helpful in regulating concentration of urine).
Is it really the concentration of urine we care about or the regulation of blood volume and ion concentration?
- The juxtaglomerular complex:
- This complex is made up of the macular densa and the juxtaglomerular cells.
- The juxtaglomerular complex is responsible for secreting erythropoietin and renin.
[edit] Different segments of the nephron form urine by filtration, reabsorption, and secretion
- The goal of urine production is to maintain homeostasis through the regulation of blood volume and composition.
- There are three molecules of waste that are worth noting: urea (made when breaking down amino acids), creatine (made from breaking down creatine-phosphate in skeletal muscles), and uric acid (made when recycling bases from RNA molecules).
- Because these waste products are soluble, they must be removed as a solute, thus we urine as the solvent.
- If one couldn't concentrate these solutes in solvent, then far too much water would be lost and this could be lethal.
[edit] Basic Processes of Urine Formation
- There are three distinct processes that take place in the kidney in order to generate urine and maintain the blood volume and composition:
- Filtration occurs when blood pressure forces water and solute from the blood through the filtration meshwork at the glomerulus into the tubular fluid.
- Filtration is a function of size of the molecules.
- Reabsorption occurs when water and organic solutes are actively or passively moved from the tubular fluid, through the tubule epithelial cells, into the peritubular fluid.
- Secretion occurs when solutes are moved from the peritubular fluid, through the tubular epithelial cells, into the tubular filtrate.
- Secretion is important because not all wastes are moved into the filtrate at filtration.
- Secretion is often the main mechanism by which some compounds like drugs are removed from the blood.
- These processes generate a fluid that is very different than any other fluid of the body in that it has very high concentrations of wastes and low concentrations of useful organics.
[edit] Filtration
- Hydrostatic pressure from the pumping of the heart forces water and small molecules out of the blood, into the renal tubule.
- This same kind of force works at all the capillaries of the body.
- At the corpuscle, the specialized filtration meshwork keeps event he smallest proteins from exiting the blood stream while at the liver the pores are so large that many large, blood plasma proteins can enter the interstitial fluid space.
[edit] Reabsorption and Secretion
- These two mechanisms use a combination of osmosis, diffusion, channels, and active transporters.
- We'll focus on the channels and active transporters.
- There are four major types of carrier-mediated transporters:
- Facilitated diffusion: carrier proteins expend no energy moving a molecule along its concentration gradient.
- Active transport: energy is expended by a carrier protein to move a molecule against its concentration gradient.
- Cotransport: multiple molecules are moved along at least one of the molecule's concentration gradient.
- These are responsible for reabsorbing organic and inorganic molecules from the tubular fluid.
- Countertransport: at least two molecules are moved in opposite directions following one of their concentration gradients.
- There are five characterisitics about carrier-mediated movement that one must understand in order to understand renal function:
- A specific substrate binds to a carrier protein that facilitates movement across the membrane.
- A given carrier protein generally only carries its target in one direction.
- The direction can be determined by concentration gradient or by orientation.
- The distribution of carrier proteins can differ from one part of the cell to another (think "apical versus basal membranes").
- There can be many different carrier proteins on a given cell surface.
- Carrier proteins can become saturated.
- This isn't usually a problem for secretion but can be for absorption.
[edit] Tm and the Renal Threshold
- There is a concentration of a molecule in the tubular fluid at which point the carriers for that molecule cannot reabsorb all of the molecule because they are saturated.
- This concentration is considered the Tm or the renal threshold, above which the molecule will be found in the urine.
- The renal threshold is different for each molecule and is a function of the concentration and functionality of the carriers by which it is reabsorbed.
- Glycosuria is the name of the state of having glucose in one's blood.
- This may occur for a brief time after eating a meal heavy in carbohydrates and before the liver has responded by turning down the circulating glucose levels.
- Chronic glycosuria is a sign of diabetes mellitus.
- In a similar manner aminoaciduria is the state of having amino acids in one's urine and can occur for a short time after eating a protein-rich meal.
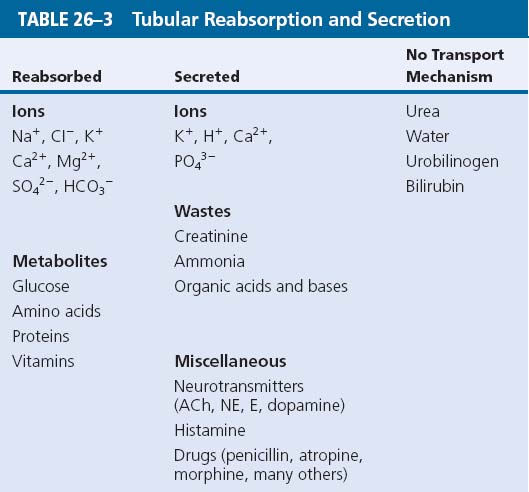
- Here is a list of managed and unmanaged molecules:
[edit] An Overview of Renal Function
- Overall, the kidney works like this:
- Filtration occurs exclusively in the renal corpuscle, across the filtration membrane.
- Water and solute reabsorption occurs primarily along the proximal convoluted tubules, but also elsewhere along the renal tubule and within the collecting system.
- Active secretion occurs primarily at the proximal and distal convoluted tubules.
- Regulation of the final volume and solute concentration of the urine results from the interaction between the collecting system and the nephron loops–especially the long loops of the juxtamedullary nephrons.
- Normal kidney function proceeds as long as all three function (filtration, reabsorption, and secretion) occur within relatively normal levels; otherwise, death can occur within hours to days.
- We'll now walk though all the parts of the nephron and describe how the tubular fluid is affected.
- We'll walk through a juxtamedullary nephron because of its special role in generation concentrated urine and retaining water. However, other than the role of the extra long nephron loop, the functions of the two types of nephrons are the same.
- See table 26-4 for review.
- Osmolarity is a measure of the number of solute particles in a given amount of solvent.
- It is usually measured in osmole per liter but can also be measured in milliosmoles (mOSm) or milli-equivalents (mEq) where the concentration of large solutes are measured in grams.
- Fresh water = 5 mOsm / liter; Blood = 300 mOsm / liter; Seawater = 1000 mOsm / liter.
[edit] Hydrostatic and colloid osmotic pressures influence glomerular filtration pressure, which in turn affects the glomerular filtration rate
- Recall that the filtration membrane across which filtrate must cross is made of the capillaria endothelium, the dense later, and the filtration slits (spaces between the processes of podocytes).
- These three components filter at different levels:
- The endothelial fenestrations are 60-100 nm across thus disallowing blood cells to enter the filtrate.
- The dense layer disallows all plasma proteins except the smallest to enter the filtrate.
- The filtration slits are 6-9 nm across and thus disallow plasma proteins (except the occasional albumin) from entering the filtrate.
- Note that since the plasma membranes are "all" that is left in the plasma, concentrations of organics, inorganics, and ions between the plasma and the filtrate will be approximately equivalent.
[edit] Filtration pressures
- The two major forces that cause movement of fluid during filtration are the hydrostatic pressure and the colloid osmotic pressure.
[edit] Hydrostatic pressure
- The glomerular hydrostatic pressure (GHP) is the pressure in the capillaries of the kidney.
- It forces fluid out of the blood into the filtrate.
- The renal capillaries have blood pressures similar to arterioles (unlike other capillaries in the systemic circuit which have lower pressures) because the blood flows from the capillaries into an efferent arteriole that has a smaller diameter than the afferent arteriole (unlike other capillaries in the systemic circuit which flow into low resistance veins).
- The hydrostatic pressure of the renal capillaries is resisted by the capsular hydrostatic pressure (CsHP).
- The net hydrostatic pressure (NHP) is the difference between the glomerular hydrostatic pressure and the capsular hydrostatic pressure:
- GHP - CsHP = NHP
- 50 mmHg - 15 mmHg = 15 mmHg.
[edit] Colloid osmotic pressure
- At the glomerulus, there are many proteins in the blood and none in the capsular space such that the colloid osmotic pressure acts to retain water in the blood.
- If the glomerulus is damaged such that proteins slip into the capsular space, the colloid pressure difference decreases and there is less osmotic pressure keeping water in the blood; this can cause increased water loss through the urine.
[edit] Filtration pressure
- The filtration pressure (FP) is the difference between the net hydrostatic pressure (NHP) and the blood colloid osmotic pressure (BCOP):
- NHP - BCOP = FP
- 35 mmHg - 25 mmHg = 10 mmHg
- The filtration pressure is the average pressure actinig to force water and dissolved material out of the blood, into the filtrate.
[edit] The Glomerular Filtration Rate
- The glomerular filtration rate (GFR) is the amount of filtrate the kidneys generate each minute.
- There is about 64 square feet of filtering real estate in the kidney such that the kidney can filter about 10% of the blood delivered to the kidney via the renal artery.
- One can get a rough estimate of the GFR by measuring the amount of creatine found in the urine and comparing it to the blood concentrations of creatin.
- This is only an estimation because some of the creatine found in the urine got there by way of secretion into the tubule from the peritubular fluid.
- A more accurate measurement can be found using inulin because it is not metabolized, reabsorbed, or secreted.
- Each day, about 180 liters of filtrate is generated and 99% is reabsorbed by the tubules.
- That would be a lot of pee!
- Any factor that changes the filtration pressure (see equation above) will change the filtration rate.
- For example, if hydrostatic blood pressure drops by more than 20% (from 50 to 40 mmHg) the filtration pressure will be zero and the kidney have essentially failed.
- Thus, "Hemorrhaging, shock, and dehydration are relatively common clinical conditions that can cause a dangerous decline in the GFR and lead to acute renal failure ."
[edit] Control of the GFR
- Proper filtration is vital to all other functions of the kidney and thus there are several mechanisms that tightly regulate filtration rate.
- There are three interacting levels of control that stabilize GFR: autoregulation, hormonal regulation, and autonomic regulation.
[edit] Autoregulation of GFR
- The most important autoregulation response occurs upon decrease of systemic blood pressure:
- The afferent arterioles dilate (to increase blood flow to the glomerulus), the supporting cells of the glomerulus capillaries relax (causing dilation and increased blood flow), and the efferent arterioles constrict (causing increased blood pressure by way of increased post-nephron resistance).
- Upon increased blood pressure at the renal afferent arterioles, the walls are stretched and smooth muscles are triggered to contract, thus decreasing the diameter and dereasing the blood flow to the glomerulus.
[edit] Hormonal control of GFR
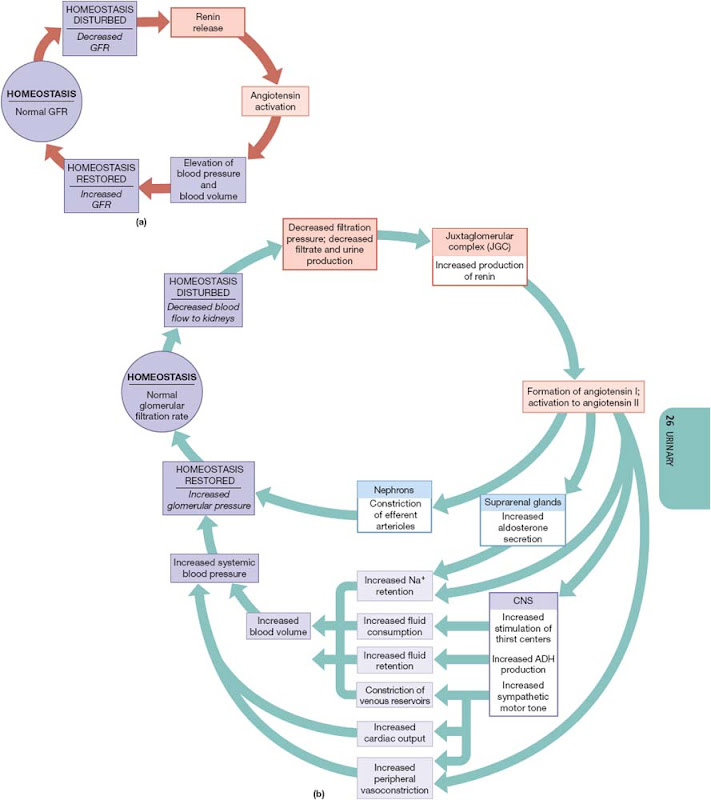
- Hormonal control of GFR uses the renin-angiotensin pathway and the natriuretic proteins (ANP and BNP).
- Recall that the juxtaglomerular complex releases renin.
- Renin can be released by three interrelated triggers:
- a decline in blood pressure at the glomerulus,
- stimulation of the juxtaglomerular complex by sympathetic innervation,
- a decline in the osmotic concentration of the tubular fluid at the macular densa.
- Renin converts angiotensin into angiotensin I (still inactive) then angiotensin-converting enzyme (ACE) converts angtiotensin I into angiotensing II.
- The combined effect of angiotensin II is an increase in systemic blood volume and blood pressure and the restoration of normal GFR:
- At the nephron angiotensin II causes constriction of the efferent arteriole (thus increasing blood pressure at the glomerulus and increasing filtration rate) and causes increased absorption of sodium and water at the proximal convoluted tubule,
- At the suprarenal cortex angiotensin II causes the release of aldosterone (which causes increased reabsorption of sodium and water at the distal convoluted tubules and cortical collecting areas),
- At the CNS angiotensin II causes increased thirst, the release of ADH (stimulating water reabsorption at the distal convoluted tubule and the collecting duct), and increases sympathetic motor tone (which mobilizes the venous blood supply, thus increasing blood pressure),
- At the peripheral capillary beds angiotensin II causes a brief but powerful constriction of arterioles just before the capillary beds (thus increasing arteriole blood pressure systemically).
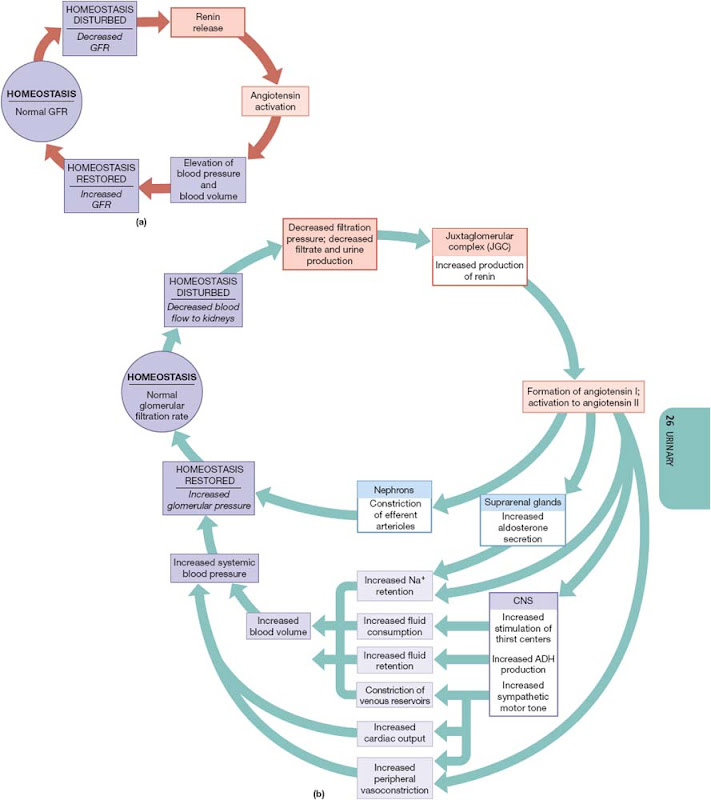
- Upon increased blood volume, the increased blood pressure increases the filtration rate which directly serves to decrease blood volume by generating more urine.
- There is an hormonal response to increased blood pressure, too, however:
- The atria of the heart releases ANP (atrial natriuretic peptide) and the ventricles release BNP (brain natriuretic peptide), each of which cause the afferent arterioles of the kidney to dilate and the efferent arterioles to constrict. This causes increased blood flow and increased hydrostatic pressure which both cause increased filtration which leads to increased urine production and a decreased in blood volume.
[edit] Autonomic regulation of GFR
- The sympathetic innervation serves to constrict the afferent arterioles, thus decreasing the GFP and retaining water.
- This is likely to occur in the case of an heart attack or acute blood pressure decreases.
- There is parasympathetic innervation but its function is no known.
- Innervation that affects blood flow throughout the rest of the body can have an affect on GFP, too.
- For example, when one shunts blood toward the epidermis on a hot day there is a decrease of blood flow to the kidney.
- These changes can be counteracted by varying degrees via hormonal and autoregulatory measures.
- During maximal effort over a long period of time (think "marathons" and "ultramarathons") the blood supply to the kidney may be only 25% of normal.
- This can cause hypoxia to the glomeruli and ultimately may lead to proteinuria (proteins in the urine) or hematuria (blood in the urine).
- 18% of marathon runners suffer proteinuria, but most cases resolve within 48 hours.
- "However, a small number of marathon and ultramarathon runners experience acute renal failure, with permanent impairment of kidney function."
[edit] Countercurrent multiplication and the influence of antidiuretic hormone and aldosterone affect reabsorption and secretion