INTRODUCTION
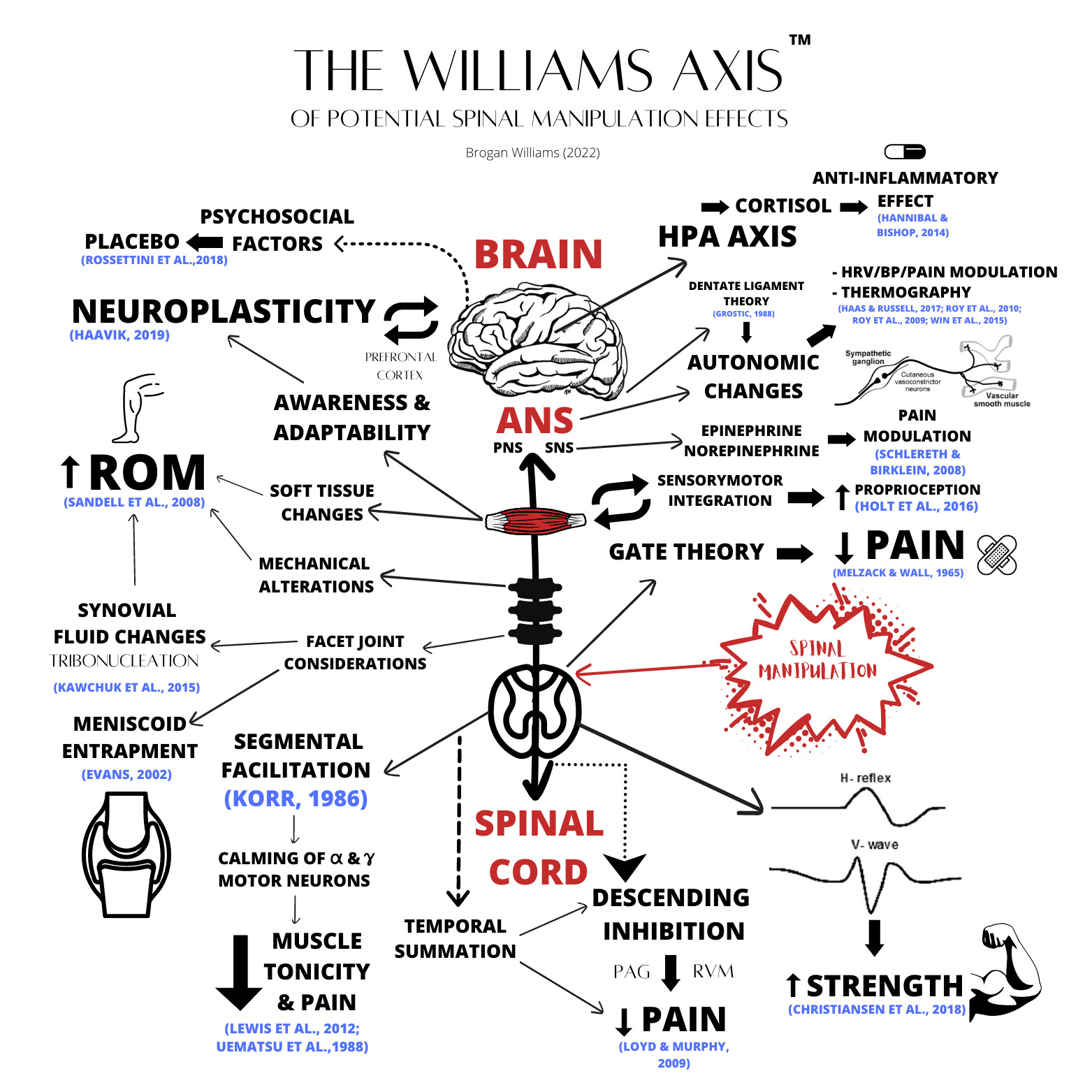
The objective of this study is to contribute to the body of evidence related to spinal manipulation (SM). The amount of research behind spinal manipulation is growing; however, little attention has been paid to the possible impact SM may have. The purpose of this paper is to not only describe the effects of SM and the possible mechanisms responsible but also to encourage clinicians to use the modality in practice.
What is spinal manipulation?
Spinal Manipulation (SM) (also known as an adjustment) is a high-velocity, low-amplitude (HVLA) thrust and directed at spinal segments and/or joints in the human body.1 SM distinguishes itself from other manual techniques by the speed by which the thrust is delivered and the audible cavitation that can often be heard as the fluid within the synovial membrane is redistributed.2,3 This occurs as the joint is swiftly being taken beyond its active range of motion and into the paraphysiological space, and involves the spontaneous redistribution of pressure, creation of gas and absorption in an enclosed fluid-filled system, consistent with a process called tribonucleation.2–4 The underlining mechanism of HVLA thrust, or spinal manipulation (SM) has been speculative for decades. Some of the more common theories focus on the local physiological and biochemical changes that occur to the synovial joint structures and the surrounding soft tissue – altering synovial fluid viscosity, increasing blood flow, altering tissue pliability and modulating pain perception via gate theory and/or descending inhibition.5–9 Others focus more on the possible neurological impact SM could have on the body, such as how the changes to afferent and efferent impulses to and from the brain could be impacting our immune system, brain neuroplasticity, proprioception, cortical drive and prefrontal cortex functions.10–15 Although the techniques are similar (chiropractic adjustments, spinal manipulation and HVLA), the purpose for using this technique varies from health profession to health profession, with the objective behind the technique being the defining factor; however, it is mostly associated with chiropractors and osteopaths, many of whom exclusively use the HVLA technique.
DISCUSSION
Methods
The goal of this narrative review was to find and appraise a multitude of relevant research and studies regarding the possible mechanisms behind chiropractic adjustments and/or spinal manipulation (SM). The reported effects of SM in the literature are quite extensive and require an in-depth review to fully cover the breadth of currently available research. The search was conducted primarily through Google Scholar, PubMed, ResearchGate and the standard Google search engine. Keywords used to direct the search were: Spinal Manipulation; Chiropractic adjustment; High Velocity, Low Amplitude; Thrust; Manipulation; Manual Therapy; Osteopathic treatment; Lumbar Adjustment; Low; Back Adjustment; Lumbar Manipulation; Low Back Manipulation; Thoracic Adjustment; Thoracic Manipulation; Cervical Adjustment; Cervical Manipulation.
Results
164 resources were located and used in this review, this includes experimental evidence case studies, case series, randomised control trials, research reviews, research articles, population studies, cohort studies, case-control studies, and medical textbooks.
Neuroplasticity
Neuroplasticity is the brain’s ability to change, rewire, reorganise and alter neural connections due to external and environmental information – sometimes in the form of new information, sensory stimulation and/or various types of perceived damage.16 When our body goes through a series of negative adaptive changes, it is called maladaptation or maladaptive changes,17 and this happens frequently. One example is pain. The site of pain isn’t necessarily the cause of it, the severity of pain isn’t always equal to the degree of tissue damage, and the feeling of pain isn’t always due to the firing of nociceptive neurons.18 Rather, tissue damage and the firing of nociceptors is only 1 part of the process, and in totality, pain is extremely complicated and modulated by the brain; this impacts how our brain perceives the world, the environment and the information that is available around us.19 In fact, the literature shows that chronic pain (greater than 3 months) has this effect on the brain, a maladaptation.20 Studies show structural and functional changes to the brain when chronic pain is present. This includes synapse plasticity, glial cell changes, spinal cord adaptations, and alterations to grey matter volume, among others.21 Ultimately, chronic pain serves as an example of maladaptive plastic changes to the brain, and how the brain can create faulty inner maps, changing the brain itself.10 This research leads us away from the traditional structural pathology models of understanding pain and directs us toward a more neuroplasticity model, one that acknowledges not only all the many variables involved in and around pain but also how it can compromise one’s neurophysiology and possibly alter one’s awareness and adaptability.10,13–15
Changes occur all the time on the spectrum between positive and negative adaptation between the brain and body, and these changes again are not only driven by physical, pathological or biological factors, but a range of things that can include emotions, thoughts, various types of mental and/or physical trauma and many different types of daily life stressors such as sleep, diet, exercise, work and even social interactions.22,23 By the time any real symptoms begin to appear, it is likely some amount of maladaptation has been occurring, the patient simply unaware of it. By understanding the sheer complexity of pain, we can gather a greater overall understanding of how injuries really occur and how they work. For example, following low back injuries there can be an array of neurological negative changes, all of which modulated through the amygdala, hypothalamus, hippocampus and prefrontal cortex (PFC), and NOT only through nociception alone.24–27This supports the narrative that communication between the brain and the body is not only important but vital to an accurate inner map or brain schema.10
Beyond the acute period of low back pain, there can be multiple physical changes to the tissues, such as muscle fibrosis, fatty infiltration, twitch fiber changes, muscle atrophy, hypomobility and even degeneration at the joints28; and although this is important and can cause long-term dysfunction, we also see neurological motor deficits, such as cerebrocortical activity, postural motor changes, altered motor control of the spine and trunk muscles, delayed reflex responses, reduced feed-forward activation and changes in proprioception.29–34 There is a growing body of research showing that chiropractic adjustments and/or spinal manipulation have an impact on central processing.35 Studies show that post-manipulation there is an improvement in cortical drive, mental rotation, multimodal integration, cerebellum modulation and joint position sense; as well as changes to sensory motor integration, altered H-reflex/V-waves and cerebellum communication.13–39
This suggests that spinal manipulation improving spinal function has an impact on neuroplasticity and a neurological modulation effect on how the body interprets information and the brain’s awareness and ability to perceive the world around it – such as visual and sound information, body position awareness, objects in space and mental rotation.40 More research and quality literature are still needed as this is not yet a full picture; however, it is a peek into how powerful and beneficial spinal manipulation could be.10
Prefrontal Cortex
We are only now beginning to realise how much of an impact “stress” can truly have on the body and mind. Adverse childhood experiences (ACE) studies show a strong, graded relationship between exposure to household dysfunction and abuse (stress) during childhood and increased health risks for many causes of death in adults, including various mental disorders, such as depression, bipolar, anxiety disorders and suicide.41 In fact, further ACE studies showed children who experienced ACE had a higher risk of chronic pain later in life.42 One study showed that as the ACE score increased so did the prevalence of chronic headaches, showing a frightening relationship between early life stressors and chronic pain/mental health.43 The more we learn about stress, the more we begin to understand the profound physiological, emotional and mental effects the stress neuromatrix can have on our bodies, our quality and quantity of sleep, the pain we feel, inflammation and our overall well-being.44 These stressors can impact how our brain perceives pain and information; ultimately causing a stress induced maladaptive neuroplasticity in the brain.10
The prefrontal cortex (PFC) is like the administrator of the brain. Often associated with performing our executive higher functions, the PFC orchestrates our actions, thoughts, moods and emotions; it even plays a role in processing pain.45 It is the region of higher intelligence as a species, helping us differentiate between right and wrong, resolving internal conflicts, problem-solving and the suppression of unwanted emotional urges regulating our personality.46 Among many other things, the PFC has many connections with multiple areas of the brain, allowing the processing of multimodal sensory inputs which helps modulate our various behaviors.47 Recent studies have shown that the stress neuromatrix has a rather significant impact on the prefrontal cortex (PFC) by shutting down PFC regulation during major stress.27 Furthermore, research shows that a decrease in grey matter in the medial PFC has been seen in people with chronic pain.48
This opens the door to a greater understanding of how stress truly impacts the body and mind. It becomes a vicious cycle of stress, pain, maladaptive changes, PFC inhibition, physical and psychological issues.24 A 2016 study showed that spinal manipulation affects sensorimotor integration in the prefrontal cortex.40 Furthermore, a 2007 study showed cervical manipulation alters cortical somatosensory processing and a 2010 study showed that spinal manipulation (SM) may also alter the cortical integration of dual somatosensory input, theorizing to 1 of the possible mechanisms responsible for the reduction in pain an improvement in functional ability following SM.15,49 More research is needed to strengthen these findings and provide more details around this association; however, this is an interesting concept suggesting the extent of neurological response from SM.
Proprioception
The functional spinal unit is heavily dense with various sensory receptors since the deep paraspinal muscles play a crucial role in proprioceptive signalling, providing a “neural image” of our spine and the movement within, around or involved with it. A lack of incoming afferent information can inhibit the brain from reacting in real time, causing altered efferent output/abnormal proprioception and other dysfunction.50
There is some research to support this notion, showing an increase in proprioception post spinal manipulation through a mechanism called sensorimotor integration, which is the ability to incorporate sensory inputs that provide information about one’s body and the external environment to inform and shape motor output.13,14 For example, 1 study showed a significant increase in ankle dorsiflexion range of motion and proprioception in subjects with chronic recurrent ankle sprains following chiropractic adjustments/spinal manipulation.51 Another, by Haavik and Murphy, showed an increase in elbow joint position sense and proprioception following cervical chiropractic adjustments/spinal manipulation, and a randomized controlled trial (RCT) in 2016 showed an improvement in sensorimotor, multi-sensory integration, ankle joint sense, stepping reaction times and proprioception awareness in a group of 60 participants following chiropractic care.6,13
Feed-Forward Activation
One key area of interest is the positive impact chiropractic adjustments have on feed forward activation (FFA). Feed forward activation has been hypothesized to be a common prerequisite for avoiding injury.52 Studies show that prior to limb movement, various “core” muscles/supportive and postural trunk muscles contract first to stabilize and protect the structural systems involved, which are often the lumbar spine, connective tissues and joints.53 This is also supported by McGill’s “proximal stiffness” theory, which he has tested over the course of his 30-year career and had great success with helping clients all around the world abolish their low back pain.54,55 Further research also demonstrates that athletes with LBP have a significant decrease in measured FFA, which includes reduced muscle activation, less co-contraction patterns and decreased abdominal endurance.56 In recent years, it has become somewhat controversial whether “corrective exercises” can improve FFA,57 or produce not much of an effect at all, with research displaying both outcomes. However, 1 RCT demonstrated a significant amount of improvement (38.4%) in FFA times following a sacroiliac joint manipulation.58
Strength, MVC and Muscle Activation
An increase in “strength” is usually the last thing people associate with spinal manipulation, but there have been studies documenting this. Strength can be defined in a number of ways, but in this situation we are seeing a short-term increase post spinal manipulation that indicates a clear increase to what was tested prior. One method of testing is by measuring the participant’s maximal voluntary contraction (MVC) pre-and post SM, often on a movement such as plantar flexion and/or elbow flexion, while some studies have tested muscles like the anterior tibilalis and the abductor pollicus brevis.59 Regardless, the point is to monitor a muscle’s force output and the electrical potentials generated by the muscle cells, to give an indication of both strength output and muscle activation or muscle fibre recruitment.5 A helpful way to measure the amount of change that is occurring post SM is to measure H-reflex and V-waves also, H-reflex being associated with increased resistance to muscular fatigue and V-waves being associated with an increase in neural drive to the muscle cells, as it reflects the magnitude of motor output from the descending pathways.60,61
In 2018, a randomised controlled study of 11 athletes showed an increase in V-wave and MVC, aka strength, and corticospinal excitability following a single session of chiropractic care.5 Moreover, a 1996 study showed that 30 college students displayed an increase in quadriceps femoris muscle strength following a manipulation to the L3/4 motion segment. The authors concluded an overall statistically significant increase in strength was observed.62 Additionally, a recent randomized controlled crossover study showed a substantial increase of plantar flexor muscle strength in chronic stroke patients following a single session of chiropractic care and an older 1999 study showed a decrease in muscle inhibition and an increase in knee extensor ROM and muscle activation in patients with anterior knee pain following a sacroiliac joint chiropractic adjustment.36,63
Finally, a study from 2002 consisting of 16 patients with chronic neck pain, reduced cervical ROM and bicep/arm muscle inhibition demonstrated an increase in ROM, decrease in pain, decrease in muscle inhibition and an increase in elbow flexion strength following a cervical spine manipulation/adjustment.64 Although this may seem significant, and is a very interesting glimpse into the neurology of an adjustment, it needs for studies that gather long-term data and not only short-term changes. More conclusive studies are needed for a strong conclusion; however, it is exciting to see the possible benefits of SM explored, especially when it comes to strength, even if it is short term only.
Pain
Pain is complicated and a significant issue in today’s society. For example, lower back pain (LBP) specifically is a major issue for our health system, leading people (who are in pain) to consider drugs such as non-steroidal anti-inflammatory drugs (NSAIDs), opioids and muscle relaxants.65 In fact, 1 in 4 people are reported to have experienced LBP within the last 3 months,66 and 75-85% of the USA population have experienced it within their lifetime.67 It doesn’t stop there, because reports show that up to 94% of elite athletes experience LBP too,68 which makes sense as roughly 5-10% of all injuries in athletes are lower-back related.69
There is high-quality research demonstrating the effectiveness and efficacy of chiropractic and spinal manipulation for pain. The Manga Report presented an overwhelming body of evidence concluding that chiropractic care is both more cost-effective than traditional medical management and more effective at treating LBP than alternative treatments.70 Furthermore, a 2006 retrospective case study found chiropractic adjustments may be suitable and effective at decreasing lower back pain for pregnant women.71 Additionally, Descarreaux et al found that long-term maintenance chiropractic care (adjustments and spinal manipulation) was effective at decreasing even chronic pain. What’s more, another paper showed spinal manipulation to be effective at treating chronic tension-like headaches; demonstrating better long-term therapeutic benefits than amitriptyline.72,73 Likewise, a 1999 randomized control study consisting of 77 patients demonstrated spinal manipulation to be more effective at decreasing pain than acupuncture and NSAIDs,74 and a 2001 systematic review of 9 trials and over 600 patients suggessted cervical manipulation was effective at treating chronic headaches, even better than massage and some medication.75 Finally, a 2010 study shows manual therapy (manipulation and mobilisation) to have better pain outcomes than exercises alone,76 and a 2012 meta-analysis demonstrates that spinal manipulation increases a patient’s pain threshold, helping them better regulate pain.9
Descending inhibition
Descending inhibition is widely understood as a pain modulation effect that occurs when a stimulus received by the body elicits descending projections from the brain down to the spinal cord, providing a reduction in the pain that is perceived by the patient.77 Although not fully understood, there are many theories about the exact mechanism that causes these analgesic effects following spinal manipulation, although it is widely theorized that it is a neurophysiological modulation effect of some kind caused by descending inhibition.8 This mechanism is not exclusive to spinal manipulation, but likely any sensory input that is competing (so to speak) with the noxious or painful input signals, almost like a gate (more on that later). Regardless of the exact mechanism of how this is occurring, as discussed above there is a fair amount of research and literature showing the effects adjustments or spinal manipulation can have on pain and the perception of incoming pain signals.9,70–74 This seems to be a well-known fact, with $8.1 billion annually being spent on manual therapies alone in the US.78
The descending inhibitory modulation circuits include various neurotransmitters, most notably oxytocin, serotonin, vasopressin, adenosine, endocannabinoids and endogenous opioids (EOs). It is also relevant to note that the analgesic response from human touch is mediated by Eos.79–83 These neurotransmitters have been found to interact with the periaqueductal grey (PAG) of the midbrain and rostral ventromedial medulla (RVM) in a way that modulates the pain circuits and output of the brain.8 The PAG was identified in the 1960s for its noticeable descending projections into the RVM and dorsal horn of the spinal cord and for its ability to mediate pain and opioid-based analgesia. It is now widely accepted that the PAG-RVM-SC pathway is one of the essential neurological circuitry for opioid-based pain modulation or anti-nociception.77 Animal studies found that neurons were inhibited by “noxious” stimuli and the term "DNIC’’ was created (diffuse noxious inhibitory control).84 This term later became referred to as CPM (conditioned pain modulation). Human research and studies have since shown clear local and segmental hypoalgesic effects following spinal manipulation with the understanding that the HVLA thrust does have a profound influence on the descending inhibitory pain mechanism.85,86
Gate Theory
Within the central pain modulatory system (CPM) (as discussed above), is another well-known mechanism that attempts to explain how pain could be modulated through non-noxious input stimuli, the gate control theory.87 This theory of pain perception states that non-noxious input can suppress pain by modulating the output through inhibiting the nociceptors at the dorsal root that inform the brain.88,89 Like a gate, when the system is triggered by touch or a spinal manipulation, that pathway is open, closing the pathway that was facilitating pain. The non-threatening input stimulates the low-threshold A beta-fibers that inhibit the incoming pain signals from the A-delta and C afferent fibers.88 Our A-beta fibers within our spinal nerves carry information like touch from the brain to body, and the body to brain – these fibers are myelinated, larger and slower than the A-delta and C fibres, which are smaller but have a faster speed conduction rate.90
Psychosocial Factors
The influence of non-physiological factors playing a role in pain modulation is a concept we cannot overlook. A patient’s confidence in the practitioner or doctor providing the treatment may have an impact on clinical outcomes. The power imbalance between the patient and the doctor sometimes evokes an expectation that the intervention is going to work. What’s more, patients can be influenced by social cues, positive reinforcement, the environment and even the clinician’s personality. These factors can sometimes have a placebo effect on the patient.91 Although the exact mechanism of how this is happening is still unknown, one’s expectations can in fact influence his or her’s chemistry and physiology, resulting in the patient experiencing similar effects to the “sham” treatment they were told they were having. For example, 1 study showed that following the administration of a placebo that was communicated to the patients as a stimulant, the patients experienced a spike in blood pressure, heart rate and reaction speed. However, when the same placebo pill was given, but told to be a sleeping pill, the patient experienced the opposite effects.92
A 2013 study consisting of 146 patients ranging between 35-65 years of age who were experiencing either knee osteoarthritis or a meniscus tear found that an arthroscopic partial meniscectomy was no better than a sham surgical procedure. Now, of course, there are likely multiple factors contributing to this result but it asks what other variables played a role and had an impact on these patient outcomes.93 A recent study in the US which examined the placebo effect over 23 years through 84 trials found it becoming increasingly stronger. It may be that the placebo effect is becoming stronger due to the increase of direct-to-consumer drug advertising in America – which alters the expectation from the public that the drug “must work” as they are targeted to believe that via the advertising.94 Furthermore, a 2007 study found that placebo interventions can improve physical disease processes of peripheral organs more easily and effectively than biochemical processes.95
Range of Motion
In addition to the pain research, adjustments and spinal manipulation have been shown to also facilitate better movement by improving ROM. Range of motion is crucial for the health and function of all joints, especially throughout the spine; it also has a profound impact on rehabilitation post injury, as restoring passive and active ROM becomes paramount when progressing an injury back to full health and function. The mechanisms responsible for the ROM increase are still largely unknown; however, many believe it is caused by the various neurophysiological changes that occur during spinal manipulation. For example, taking the joint beyond its paraphysiological space can cause changes to the surrounding soft tissue structures,96 remodel the state and viscosity of the facet joint’s synovial fluid,97 briefly alter the spinal joints mechanics,98 and elicit physiological changes modulated through the nervous system, like muscle tonicity, pain modulation, sensory changes and improved feedback abilities.87,99–101
When we look at the literature, there are numerous high quality studies showing the positive impact spinal manipulation has on ROM. In fact, in a 2008 randomized controlled study 17 young athletes demonstrated an increase in hip extension ROM following sacroiliac (SI) joint manipulation.102 Furthermore, a 2006 study showed a greater increase in ROM and decrease in pain following chiropractic manual therapy and heat treatment opposed to heat treatment alone.7 Additionally, an increase in knee ROM, an increase in cervical (neck) ROM and an increase in ankle dorsiflexion were seen.51,63,64,103
Adverse Events
A chiropractic adjustment or spinal manipulation is a specific high-velocity, low-amplitude thrust, a type of manual therapy that has been implemented by chiropractors and other health professions for over 100 years, with research showing that it’s an effective method and treatment for chronic pain104,105 increasing ROM,98 improving healing outcomes106 and increasing proprioception awareness.40
Is it safe? There have been some literature reviews and case reports that suggest an association between cervical artery dissections and cervical manipulations or adjustments.107 It’s also important to note that these studies failed to prove any actual causation between cervical adjustments and stroke. Furthermore, a study in 2008 concluded the correlation is likely caused by patients seeking chiropractic care while already experiencing the symptoms of a stroke, such as headaches, migraines or neck pain; all symptoms that chiropractors are see frequently.108
A 2002 study showed that a single high-velocity, low-amplitude thrust only represents 1/9th of the strain it would take to reach mechanical failure of a vertebral artery.109 Furthermore, a population, case-control, case-crossover study looked at a population of 100 million and concluded there to be no evidence of ANY excess risk of vertebral artery dissection or stroke associated with chiropractic care compared to primary care.108 The key takeaway here is the importance of a thorough history and quality, detailed spinal examination prior to any treatment; to screen for patients who may be experiencing the early stages of a stroke.
Other Mechanisms of Action
Spinal manipulation is mostly known or associated with a cavitation, which is not only often believed to be the technical inclusion criteria for a successful thrust but also most of the time strangely satisfying for the patient. As many people likely already now, the noise is not the bones cracking or any other extreme process for that matter, but gas in the synovial fluid quickly redistributing within the joint and causing a reduction in pressure and a popping sound.100 In order for a synovial joint to reach this stage, it requires a high-velocity thrust taking the joint into its paraphysiological barrier.96
There are various ideas and theories out there around how and why spinal manipulation has such a profound effect. However, the mechanical mechanism of action is often explained through key theories that have emerged most commonly in the research and literature.
-
The release of spinal segments that have become restricted or have undergone various displacements.98,103,110,111
-
The physiological emancipation of trapped synovial folds or intraarticular meniscoids96,100,112,113
-
The restoration of movement and function disrupting periarticular restrictions and adhesions1,102,110,114
-
The stimulation of mechanoreceptors causing a relaxation effect to tight or hypertonic muscles via the “reflex” theory.99,100,115,116
Among these 4 theories, a recent critical review deemed only 1 of them (trapped synovial folds or intra-articular meniscoids) is likely viable as a reasonable and plausible explanation for the mechanism responsible for the clinical outcomes we see with spinal manipulation.96 However, there is also evidence to suggest that the gapping of the facet joints, or separation of the zygapophyseal joints during the cavitation process, is associated with other various physiological outcomes, in which the cavitation is necessary for them to occur.117,118
Additionally, another well-known theory within chiropractic is the dentate-ligament-mediated cord distortion theory. Although little has been published on this theory, many chiropractors use it to support the upper cervical technique (euphemistically called the Hole-in-one technique (HIO)) which was made famous by B.J Palmer in the 1920s/30s.119 John Grostic was the chief proponent of this theory. He claimed the thickness of the dentate ligament in the cervical region could cause compression and cord tension throughout the entire spine and become irritated upon cervical flexion.120,121 Many chiropractors found that adjusting the cervical spine exclusively provided results throughout the entire spine and body and could affect conditions such as back or hip pain.122
Grostic believed that dysfunction at the dentate ligament was what was causing interference to the spinal cord and thus the nervous system (traditional chiropractic subluxation theory). He narrowed it down to 2 key mechanisms; 1) Mechanical irritation to the dentate ligament, and 2) Ischemia or lack of blood flow due to traction of the dentate ligament. Interestingly enough, Jarzem et al set out to find whether this was even plausible; and concluded, using animal models, that spinal mechanical traction does cause a reduction in blood flow and an interruption to somatosensory action potentials.123 Since the Grostic theory was published in 1988, a thick segment of connective tissue has been identified decades later directly between the rectus capitis posterior minor muscle, the dura and the posterior atlanto-occipital membrane. This bridge of connective tissue is thought to stabilize the upper cervical region and prevent brainstem compression during cervical movement; however, it has also been associated with causing cervico-genic headaches.124,125
What’s more, many hypothesized that if Grostic’s theory was correct, then restoring alignment in the cervical spine should elicit a reduction in blood pressure, as 1 of the 2 mechanisms of the dentate theory is blood flow stasis. In 2007, Bakris et al. performed a double blind, placebo-controlled study that concluded that a National Upper Cervical chiropractic procedure (adjustment) of the atlas lowered systolic and diastolic blood pressure.126 The autonomic system may be involved in mediating the effects of spinal manipulation, from changes in thermography, HRV, pupillary reflex to potential blood pressure changes.12,127–129 However, in this specific case, further research was several years later that found no significant change in systolic and diastolic blood pressure compared to the sham procedure.130
Muscle Activity
Changes in muscle activity and tonicity is nothing new for manual practitioners when dealing with sore spots, aches and pains! However, does it have any real clinician relevance and can we use it as an objective measure on whether a treatment was successful? Defining the “tonus” of a muscle can be difficult – as to the patient it may feel “tight”, hard or maybe stuck; and to the clinician it may feel hypertonic, hot and maybe a little tougher or harder – but what does this really mean? Beyond the traditional inflammatory signs that may alter how the muscle is presenting; such as heat, redness, loss of function, edema and pain, a tight muscle could really include some or none of these accompanying factors. Muscle stiffness, so to speak, could be caused by many things, such as muscle damage post workout, electrolyte imbalances, mineral deficiencies, neuromuscular changes and sometimes serious underlying myopathies or disease.131–133 Whether you call it a muscle spasm, a knot, or a tight muscle, more may be happening than one thinks. Muscles adapt and change based on the forces that are applied onto them, or the bones or structures to which they are attached. Sometimes postural alterations, actual physical imbalances or simply just working out too hard can cause those muscles to tighten or lengthen.134
One theory that explains this model well is the upper-and-lower cross syndrome. Although this theory is outdated and many now believe it is a gross over simplification for a more complicated system, I will use it as a means to further explore this topic. Keep in mind, this is still taught largely in physiotherapy and chiropractic institutions around the world. Moving on, upper cross syndrome is a musculoskeletal diagnosis that is largely involved with posture and prolonged static positions. The upper cross refers to the pectoralis muscles, deep cervical flexors, levator scapula, trapezius and serratus anterior, which form a cross spanning across the upper body.135–137 Poor posture (among other things) causes a forward head carriage and rolled forward internally rotated shoulders, resulting in tight pectoralis muscles, tight upper trapezii, weak or tense (lengthened) deep neck flexors, levator scapula and lower trapezii or serratus anterior, and accompanied by pain.138 The posture or lack of movement for various reasons cause this tension, tightness and pain through the musculoskeletal system, and this happens throughout the whole body.
The Pain-Spasm-Pain Cycle
Another common theory is “the pain-spasm-pain cycle,” which describes muscular hypertonicity as a response to pain, leading to the muscle spasm causing nerve compression, tissue dysfunction or ischemic pain.101 One of the leading theories why spinal manipulation interacts with muscle hyperactivity is via muscular reflexogenic responses, since spinal manipulation may disrupt the pain-spasm cycle by evoking the appropriate muscular reflex pathway and reducing muscle activity.4 There are studies showing a link between thermal asymmetries and increased paraspinal muscle activity in patients who are experiencing back pain, showing that the link is evident between pain and muscle hypertonicity.139,140 What’s more, we have studies showing an alteration to those thermal asymmetries and muscle activation following spinal manipulation. However, some studies conclude SM increases muscle activation, and some say it decreases.128,141 However, although this may be confusing, we have already discussed the importance of strength, muscle activity and how SM can improve muscle strength. It thus makes sense that contextually the body responds using the force from the SM in the most advantageous way possible.5,62,114
Segmental Facilitation (Motor Neurons)
In addition to the above theories, Korr’s theory of segmental facilitation must be considered.142 The theory states that segments of the spine that constantly are barraged with stimulus become facilitated and over-sensitive, leading to an ongoing central excitatory state.143 Furthermore, Denslow et al demonstrated back in 1947 that areas of the spinal cord associated with somatic dysfunction also had an increase in hyper-responsiveness and seemed to remain in a state of maintained facilitation.144 Korr believed that these sites of somatic dysfunction mirrored sites of pain, and these areas over time allowed the build-up of gamma-motor neurons due to the increased traffic of stimuli through that specific spinal segment level. The increase in gamma neuron activity caused muscle hypertonicity by facilitating the excitement of alpha neurons and participated in the pain-spasm-pain cycle.101 Ultimately Korr’s answer to this painful problem was manipulation, theorizing that the bombardment of neurological afferent input from spinal manipulation caused a distracting and calming effect on the gamma neurons.142 Gamma motor neurons are low motor neurons (LMNs) that contribute to muscle contraction; however, they play an important role in modulating tension in muscle spindles that interact with alpha motor neurons, allowing them to fire and perform full muscle contraction. Alpha motor neurons primarily work to generate force via innervating extrafusal muscle fibers, while gamma motor neurons alter muscle spindle sensitivity by innervating intrafusal muscle fibers.145
Autonomic Changes
The autonomic system is responsible for regulating involuntary body functions such as blood flow, heart rate, digestion and breathing while controlling blood vessels, organs and glands. Dysautonomia is often defined as a disorder of the autonomic nervous system that causes disturbances to these autonomic functions, ultimately resulting in poor health outcomes. The autonomic system is also responsible for the sympathetic and parasympathetic divisions, which regulate fight and flight (sympathetic) and rest and digest (parasympathetic) systems. The body requires balance in order to function optimally; however, these systems that were designed to help humans survive thousands of years ago can become overly active and stimulated, often leaning towards the sympathetic range, leaving people in a constant state of fight or flight, providing an environment conducive to autonomic dysfunction.146
Healthcare professionals do have the ability to measure how the autonomic system is functioning via the variability of the space in between heart beats; a higher heart rate variability (HRV) is better, as low variability between heart beats indicates a system that is not adapting efficiently to the stresses being placed upon it. In fact, a 1994 study showed that monitoring a patient’s HRV was an accurate way of measuring cardiac autonomic tone.147 Furthermore, a study from 2016 concluded measuring HRV as an accurate operator fatigue analysis system reducing the risks that occur as a consequence of a fatigued operator.148
Furthermore, certain healthcare providers such as chiropractors claim they can test the sympathetic and parasympathetic systems via paraspinal thermography, which through infrared technology detects the varying degrees of temperatures across the surface of the skin. A 2011 study showed excellent intra-examiner and inter-examiner reproducibility of paraspinal thermography when using a commercially available unit and a 2007 study showed an excellent reliability of data by 3 different methods of computer-aided thermal pattern analysis.149,150 The idea is, a healthy system will adapt in symmetrical temperature alterations through the process of vasoconstriction/vasodilation. This is regulated via sympathetic pre-ganglionic signals that are part of the body’s autonomic thermoregulation system.151 A 2-part study from 1988 consisting of 144 patients demonstrated a strong link between those with low back pain/sciatica and thermal asymmetries, indicating temperature asymmetry may be an effective tool in evaluating patients with such conditions.140
There is some evidence showing spinal manipulation and chiropractic care can impact both HRV and spinal thermography. One study showed noticeable thermography changes to the L5 region following a lumbar L5 adjustment while a second, retrospective case series, showed a significant improvement of HRV in patients receiving continuous chiropractic care.128,129 Additionally, a 2009 randomized control trial consisting of 51 participants showed an increase in HRV and parasympathetic activity following a lumbar chiropractic adjustment.12 Additionally, there has been research showing changes to both blood pressure and the pupillary reflex following spinal manipulation, indicating ANS involvement.129,152 It is also widely accepted that there are considerable interactions between the autonomic nervous system and how we perceive pain, indicating that there may be some level of involvement happening regarding the modulation of pain following SM which is being regulated through the ANS.153
Sympathetic Nervous System and the Hypothalamic-Pituitary-Adrenal Axis
Stress has a very large impact on the human body, so it is not surprising the complicated systems that have been developed throughout evolution to help the human species manage and coordinate the body’s response to stress. The hypothalamus is widely known for its ability to coordinate incoming stress. The hypothalamic-pituitary-adrenal axis (HPA axis) is a complex neuroendocrine pathway consisting of various negative feedback loops that operate to manage the body’s homeostasis.154 When the body is subjected to stress, in whatever way that may present, the sympathetic nervous system (SNS) mediates an initial response as a mechanism of protection; the release of epinephrine and norepinephrine will prepare you to fight or flight, raising your heart rate and perspiration.155
Additionally, the HPA axis is also engaged which starts by the hypothalamus responding to the elevated hormones and change in physiology and secreting corticotropin-releasing hormone or CRH into the bloodstream. CRH causes the pituitary gland to release adrenocorticotropic hormone or ACTH and this hormone is what acts on the adrenal glands causing the secretion of glucocorticoids like cortisol.156
Cortisol is intriguing, because cortisol pretty much enhances anything in your body that is likely to be useful during a highly stressful time and inhibits anything that is not useful- like pain; furthermore, cortisol is known to be a potent anti-inflammatory and a hormone that helps modulates inflammation.157 A 2019 randomised controlled study consisting of 100 healthy participants concluded that cortisol does in fact affect pain sensitivity and a 2015 longitudinal cohort study concluded that a hyporesponsive HPA axis and low cortisol response to stress was associated with musculoskeletal pain in young adults.158,159 It is important to note that when stress is consistently prolonged and tempers into the chronic state, this HPA axis can turn from a healthy adaptation to a maladaptation causing both pain and inflammation dysfunctions. This ties into what was discussed earlier in this review when it touched on maladaptive neural changes and neuroplasticity.
It is also important to mention that the SNS is also associated with pain modulation. Schlereth and Birklein state that the activation of the SNS in healthy subjects usually supresses pain and nociceptive transmission by descending inhibition.160 The release of EOs, endorphins, serotonin, noradrenaline and GABA during an acute, fast stressful experience is extremely important, as these chemical mediators work to inhibit the action potentials causing pain resulting in descending pain inhibition and a reduction in pain.161
The effects induced by spinal manipulation on the nervous system, immune system, HPA axis and endocrine systems have been investigated for years with many contrasting and conflicting results; however, it is clear something is happening and we may not fully understand it all yet.162 For example, a 2017 study showed an observed change in HPA activity via salivary cortisol following SM.163 Additionally, many have explored this as a viable and plausible mechanism underlying the clinical success we see with SM.4 There is even evidence showing that SM is effective at reducing temporal summation, which is the increased build-up of pain due to multiple repetitive nociceptive stimuli.164 Moving forward we need more high-quality clinical trials looking at how SM exactly impacts the SNS, HPA axis and the neuro-endocrine systems.
Spinal Manipulation Effects (review summary)
CONCLUSION
The underlying mechanism of HVLA thrust, or spinal manipulation (SM) has been highly speculated for decades, and was further explored in this review. Various theories have been established throughout the literature covering both physiological and neurological mechanisms, such as the local physiological and biochemical changes that occur to the synovial joint structures and surrounding soft tissue – altering synovial fluid viscosity, increasing blood flow, altering tissue pliability and modulating pain perception via gate theory and/or descending inhibition. Neurological effects have also been highlighted regarding the impact of spinal manipulation on the brain via changes to afferent/efferent impulses; potentially altering the state of our immune system, brain neuroplasticity, proprioception, cortical drive and function of the prefrontal cortex. This review provides a framework for a better understanding and deeper comprehension of the potential mechanisms involved in spinal manipulation. This study is not only for the researcher, but also for the clinician, doctor, physical therapist, and other professionals who treat patients on a daily basis. In order to give the best evidence-based treatment possible, I hope that this review will offer high-quality, consolidated, palatable information that will help to clarify and equip the appropriate individuals to further expand their practice in line with the research.