Anatomy of the L5-S1 Spinal Motion Segment
The L5-S1 segment is located between the lumbar and sacral spine in the lower back. Here, the curvature of the spine changes from lumbar lordosis (forward curve) to sacral kyphosis (backward curve). The L5-S1 segment transfers the loads from the spine into the pelvis and legs.
This segment consists of the following structures:
- L5 and S1 vertebrae. The L5 and S1 vertebrae are different in their characteristics:
L5 is a vertebral body in front and an arch in the back with 3 bony apophysis designed to attach the ligaments: a spinous process in the middle and two transverse ones on the sides.
S1, or the sacral base, is the upper and wider end of the triangular-shaped sacrum. S1’s body is characterized by wing-shaped bones on the top on either side, called the alae. At its back, the S1 vertebra has the median ridge or a long bony prominence. This ridge is surrounded by bony openings (foramina) on both sides.
The lumbosacral facet joints bridge L5 and S1 with articular cartilage.
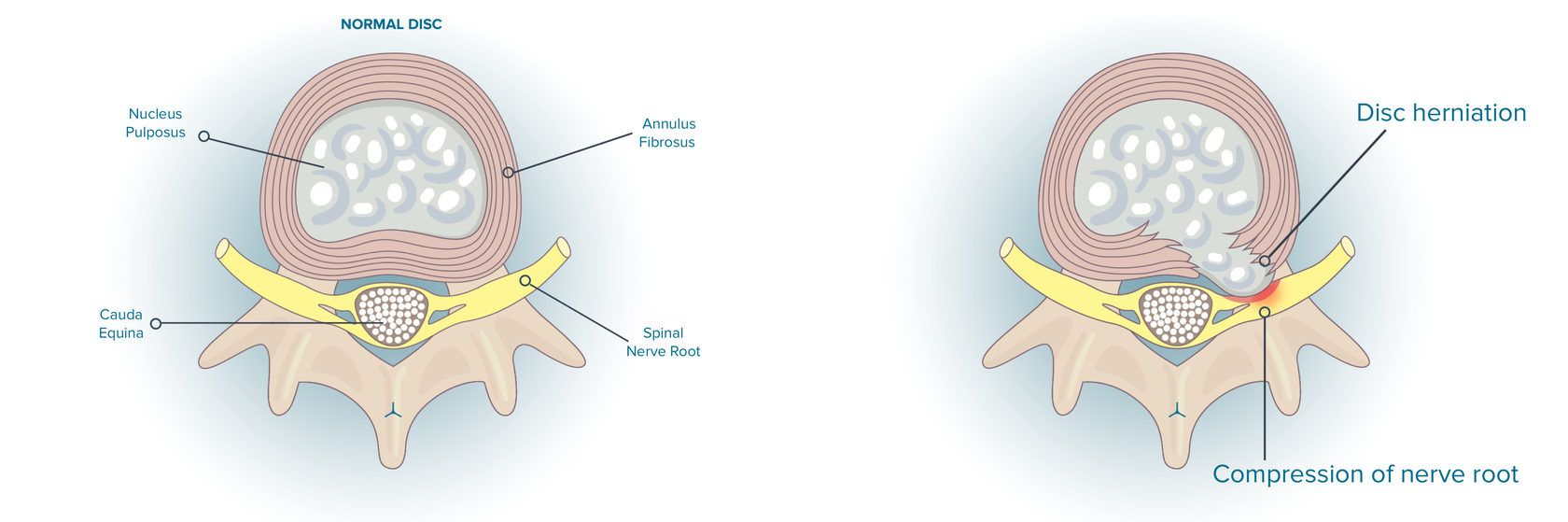
- L5-S1 intervertebral disc. A disc from a gel-like material (nucleus pulposus) surrounded by a thick fibrous ring (annulus fibrosus) is located between the vertebral bodies of L5 and S1. This disc functions as a cushion and shock-absorber and protects the vertebrae when the spine moves.
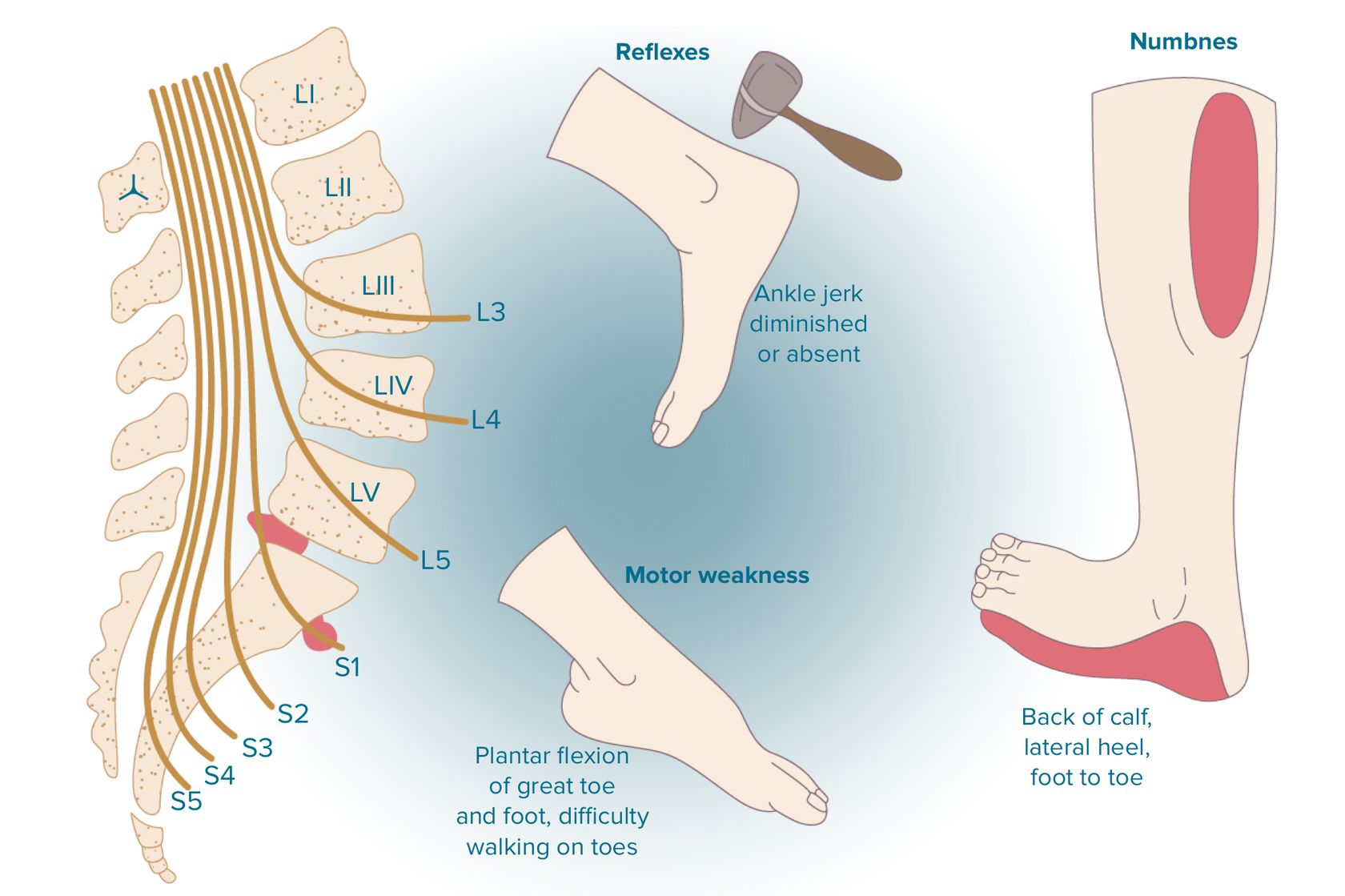
- S1 Nerve runs to the back, into the buttock, lateral or posterior thigh, posterior calf, lateral or plantar foot. When this nerve is damaged, a person can experience the following difficulties: sensory loss on the posterior calf, lateral or plantar side of foot; weakness on hip extension, knee flexion, plantar flexion of the foot. A person can also have gastrocnemius muscle paresis (in this case, a patient can’t go on his toes). A patient doesn’t show Achilles tendon reflex on the damaged side. Possible symptoms are urinary and fecal incontinence as well as sexual dysfunction.
- L5 Nerve runs through small bony openings (intervertebral foramina) on the left and right sides of the spinal canal. These nerve roots join with other nerves to form bigger nerves that extend down the spine and run down each leg.
There are three parts in a spinal disc:
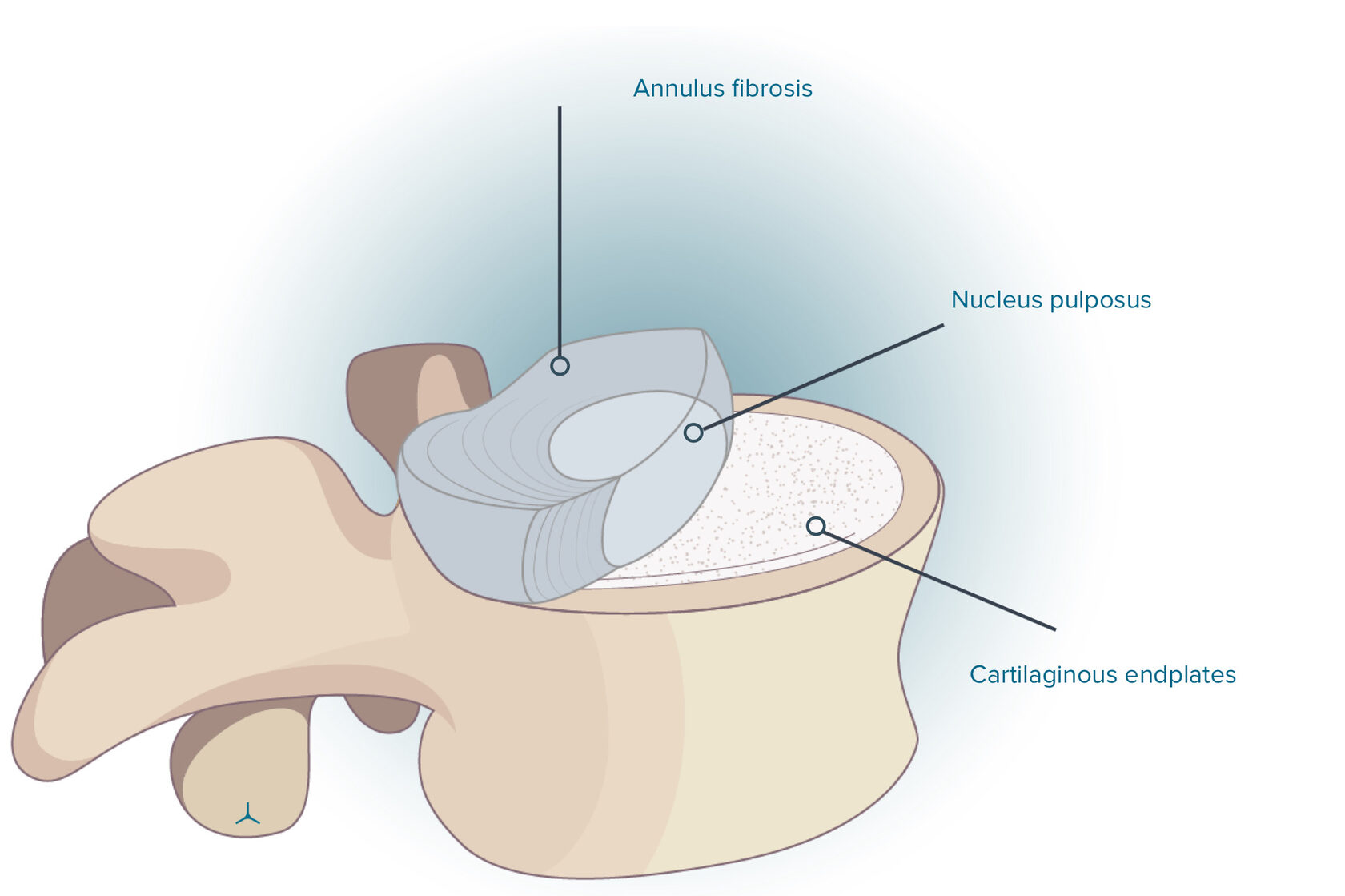
- Nucleus pulposus is at the center with some water, collagen type II (types VI, IX and XI are also possible), and proteoglycans. The percentage of water in healthy disc nuclei is approximately 77%. By balancing the load exerted on the disc, the nucleus distributes pressure outward.
- Annulus fibrosis consists of overlapping ligaments. The annulus keeps the nucleus tight and gives rupture-less flexibility for bending and twisting.
- Cartilaginous endplates represent two cartilages. Their purpose is to attach the upper and lower surfaces of the disc to the flat area of each neighboring vertebrae. The disc endplates maintain the health of the disc because they serve as gatekeepers for nutrients and water.
- Spacer. Spinal discs intermingle with the vertebrae along the spine and compose about one third of the spine’s height. The disc’s height is enough to include the joints, muscles, and nerve roots and to maintain their proper functions. A spinal segment includes a pair of vertebrae, a disc between them, and this structure movestogether as a joint.
- Shock absorber. The discs absorb loading pressure exerted on the spine.
- Motion unit. The disc is flexible enough to move forward, backward, to rotate and to perform side-to-side movements. Besides, it stabilizes the spine and keeps it upright.
Common Problems at L5-S1
The L5-S1 segment with its bottom position in the vertebral column is likely to experience excessive biomechanical stress, which results in more loads and could lead to an injury. Common disorders are as follows:
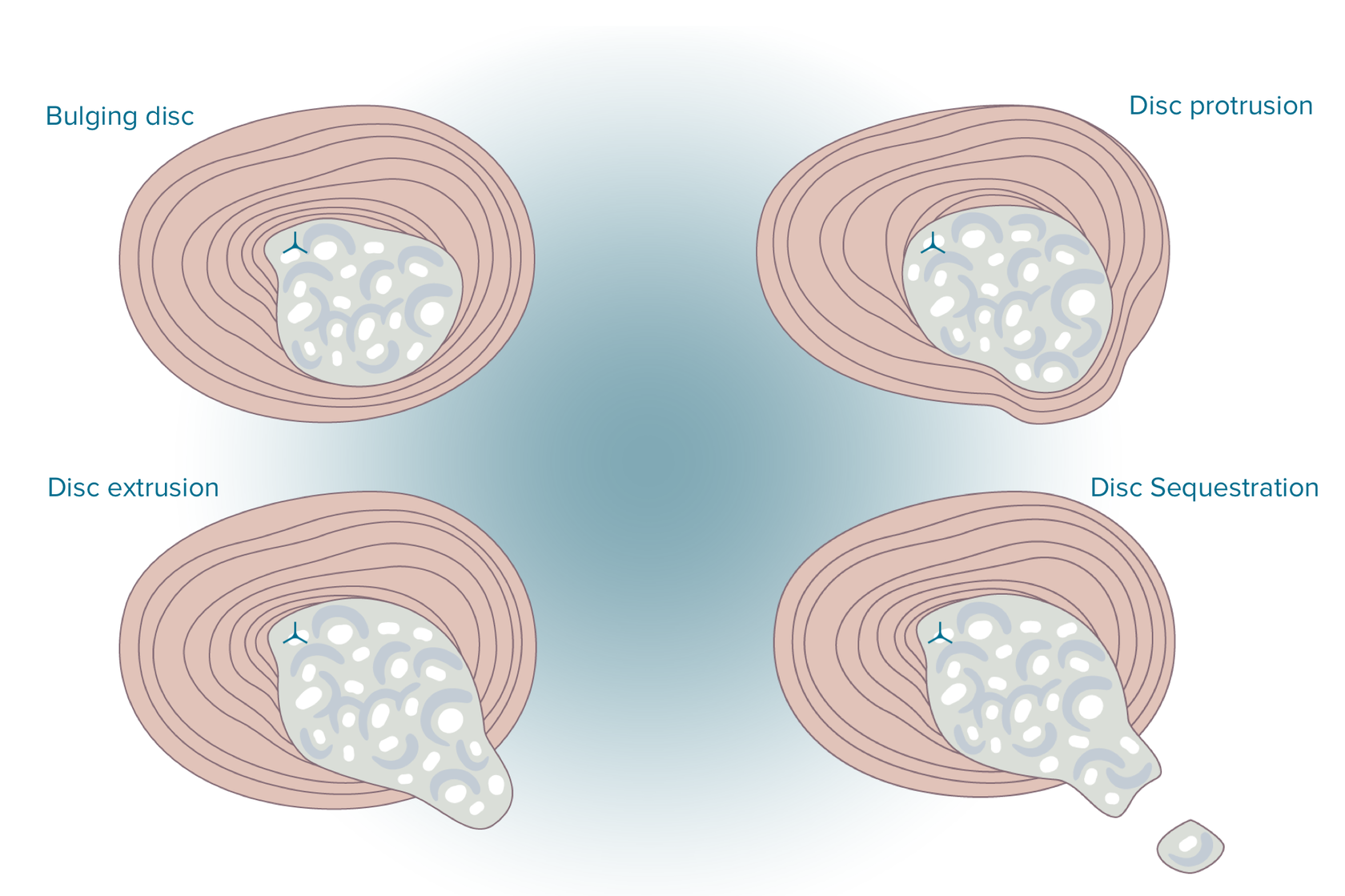
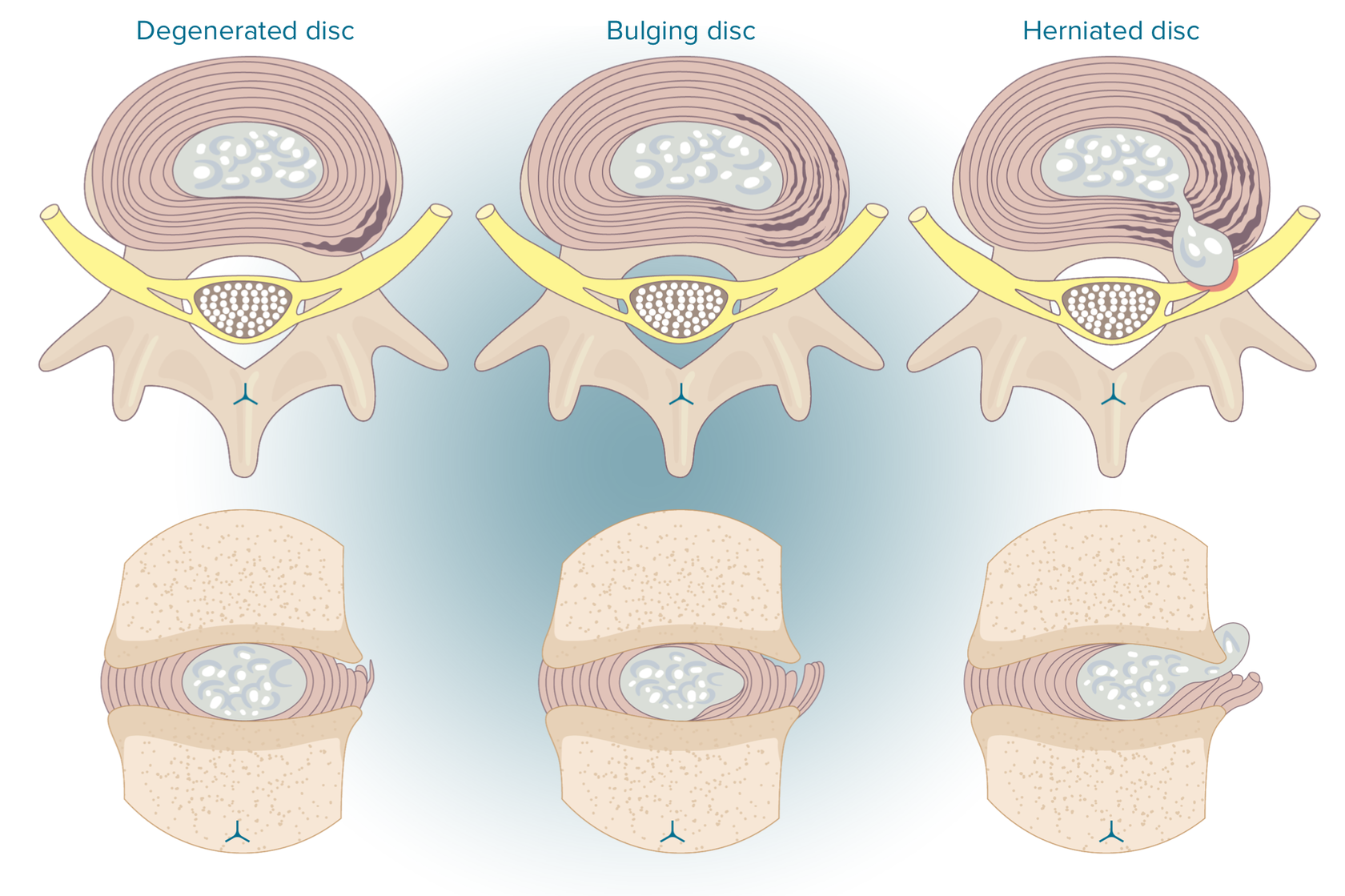
- Disc problems. The L5-S1 segment is highly likely to suffer from hernia. This disc inclines steeply, thus provoking shear stresses and increasing the risk of injury and disc degeneration. Small tears could appear due to the pressure on the outer layer of a disc. The jellylike material which the disc is made from can then penetrate into these cracks, this condition is called a herniated disc.
- Facet joint pain. The lumbosacral joint bears high load, this can be developed into wear-and-tear arthritis (osteoarthritis).4 Inflammation, e.g. rheumatoid arthritis or degenerative spondylolisthesis, may cause pain in the facet joints.
- Spondylolysis. The L5 vertebra is at risk of developing spondylolysis, which means the fracture of the pars interarticularis (defined as a small bony segment from the vertebral arch joining the facet joints) caused by a constant stress exerted on the bone. This condition may be developed on either side. As it may be the case when the bone does not break, but is under stress called a pars stress reaction.
- Spondylolisthesis. Spondylolisthesis occurs when the vertebra slip over S1 if the L5 pars fracture on both sides. The L5 spondylolisthesis frequently arises from an ongoing stress to the pars interarticularis and is most commonly expected to be seen in children and adolescents. A trauma-caused pars fracture is a rare phenomenon. A gradually or suddenly developing ventral displacement of a vertebra, usually V lumbar or lumbarized I sacral, or both is called spondylolisthesis. The displacement of the IV and V lumbar vertebrae is rare to be seen.
Spondylolisthesis develops through three stages:
a) standing over the promontory of the vertebral body Lv sacrum with partial exposure of the sacrum base;
b) a strong inclination of the vertebra, displaced anteriorly;
c) the descent of the vertebra into the small pelvis and the complete exposure of the sacrum site.
The L5-S1 segment could suffer from malignant tumors, e.g. sacral chondromas, which is quite rare. This level is also susceptible to the developmental variations in the S1 shape, a fusion of L5 with S1, and extra facet joints between L5-S1.
When the V lumbar vertebra changes into the sacral, this process is called sacralization, as a result the number of lumbar vertebrae decreases, while the number of sacral vertebrae increases by one. Lumbarization is the opposite process when the I sacral vertebra separates from the sacrum and turns into the lumbar (VI).
Why is a herniated disc L5/S1 so common?
The L5/S1 segment is known for its widely common problem - a herniated disc. Actually, 90% of people are likely to have a hernia at the L5-S1 segment if they suffer from a disc disorder.
Spinal discs can suffer wear and tear in the course of time due to the repetitive movements. This is a widely spread process and is painless.
However, if one part of the disc has shown more wear-and-tear damages than others, it can lead to a herniated disc.
Most often, everything starts plainly- with degenerative-dystrophic changes in the intervertebral disc, which at the initial stage lead to bulging / protrusion.
The classic initial symptoms of l5 s1 disc protrusion or l5 s1 bulge of the disc are frequent or persistent aching pain in the lower back and sacrum, which tends to intensify after prolonged walking, sitting or doing physical work and disappear after rest. More neglected l5 s1 disc bulge symptoms can be manifested by severe pain, impaired sensitivity of some parts of the body, numbness, muscle weakness and changes in the mobility of the lower extremities. l5 s1 disc bulge treatment should be сhosen individually. The most important thing is not to delay this process, which can lead to a deterioration in the condition of the disk.l5 s1 disc bulge recovery time should be started as soon as possible.
The figure given below illustrates the case where the strong outer fibers of the annulus fibrosus split and the disc’s fluid (nucleus pulposus) leaks through them, and the injury occurs.
The discs are very close to the nerves, that is why some inner material of the herniated disc can affect the nerve and trigger a range of symptoms.
The symptoms called sciatica arise when the sciatic nerve is innervated by the disc fluid. The term sciatica isn’t a disease, it’s just a word to describe a pain in the leg caused by the sciatic nerve.
If someone is diagnosed with a ruptured l5 s1 disc due to disc’s proximity to the sciatic nerve, the disc fluid affects the nerve and causes sciatica.
This is the main reason why a herniated disc L5/S1 is one of the most challenging disc herniations.
Besides, normal movement affects the discs that are located between two different types of vertebrae (i.e. cervical and thoracic (C7/T1) and lumbar and sacrum (L5/S1)) the most.
To recap, the disc at L5/S1 is both at the curve in the spine and at the junction between two types of level. It experiences the risk from the other vertebra and this contributes into the explanations why a herniated disc L5/S1 is so common.
Symptoms of a Herniated Disc L5-S1
Not all disk pathology is clinically important.
It is often the case that the patients with mild or moderate disk herniations first pay attention to the lower back pain corresponding to annular pressure and fissuring.
The result of this is frank tears in the anulus and herniation of inflammatogenic material; the lower back pain may become weaker while a radiculopathy manifested by pain, paresthesia, or weakness can appear due to the pressure on the nerve root.
Severe herniations are manifested in immediate lower extremity pain with little or no lower back involvement.
Lower back pain will be sporadic and is often caused by physical activity and worsened by sitting for a long time, changing the position from a seated to a standing one, or bending and twisting (any described movement can increase lumbar disk pressure).
Patients experiencing herniation of lumbar disks with radiculopathy may experience an exacerbating pain in the lower extremity.
Common symptoms of L5-S1 herniated disc
- Pain is sharp, shooting, and/or a patient experiences a searing feeling in the buttock, thigh, leg, foot, and/or toes
- Sciatica is a nerve pain from an injury or irritation to the sciatic nerve, which starts in a buttock/gluteal area.
- Numbness in the foot and/or toes
- Feeling of pins-and-needles and/or tingling
- Weakness in the leg and/or foot muscles and an inability to raise the foot (foot drop). The top of the foot can be numb as well.
Uncommon symptoms of L5-S1 herniated disc
- Leg shaking/spasms: these spasms are often taken for sciatica, they tense up the muscles. Muscle relaxants are the best medications to treat the symptom.
- Problems with the Bladder and Bowel: This symptom mustn’t be ignored and needs to be consulted with a medical worker. In this case, the nerves responsible for proper functioning of the bladder and the bowel are pressurized with the L5/S1herniated disc. The key symptoms are not being able to “go” or not being able to feel a full bladder/bowel. If you suffer from one of these symptoms, you should address your doctor as soon as possible.
- Numbness in the Private Areas: Here is one more symptom that requires immediate examination. It means that the lower nerves are under such a pressure that they can’t do their job. Unless it is treated, a patient might live with a permanent problem. Again, a trip to the emergency room should be your next step.
A herniated disc at lumbar segment 5 and sacral segment 1 (L5-S1) usually causes S1 nerve impingement. S1 nerve impingement (at the L5-S1 level) from a herniated disc may be manifested in the loss of the ankle reflex and/or weakness that doesn’t enable a patient to stand on their toes or on the ball of the foot. Numbness and/or pain can radiate along the outside of the calf, down to the sole or outside of the foot and the toes.
What are the symptoms of S1 nerve damage
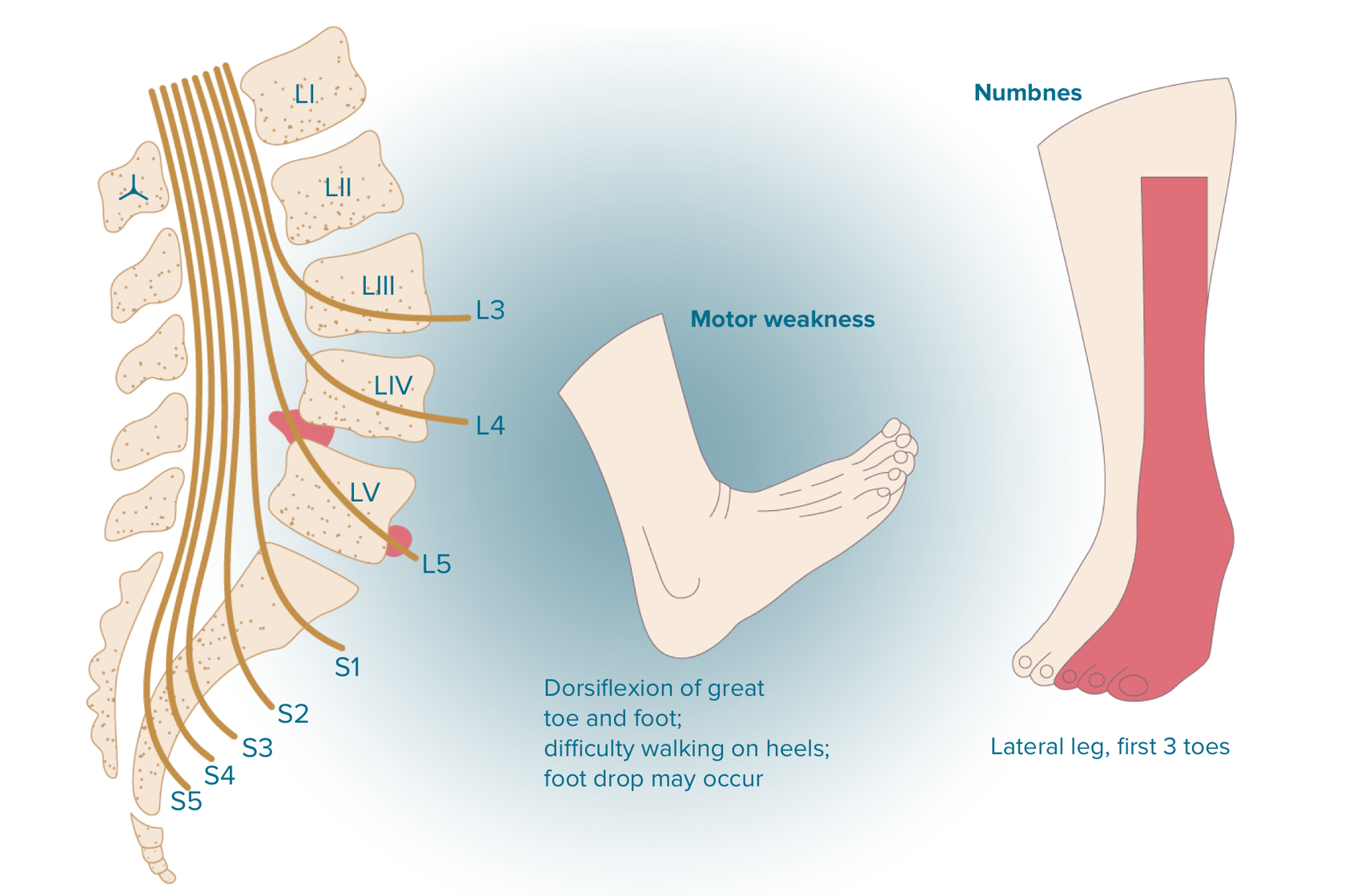
With L5 radicular syndrome the sensitivity of the skin (hypesthesia) decreases in the area of the outer surface of the thigh and lower leg. The pain radiates from the lower back through the buttock along the lateral surface of the thigh and lower leg into the first 2-3 toes. The area of pain coincides with the area of sensory disorders. Sometimes we observe paresis of the extensors of the big toe, and sometimes the entire foot.
What are the symptoms of l5 nerve damage
Treatments for Herniated disc l5 / S1
It is highly recommended to perform an imaging test before treatment. This could be helpful in excluding any other possible reasons for such symptoms as fracture, tumor, infection, or cauda equina syndrome.
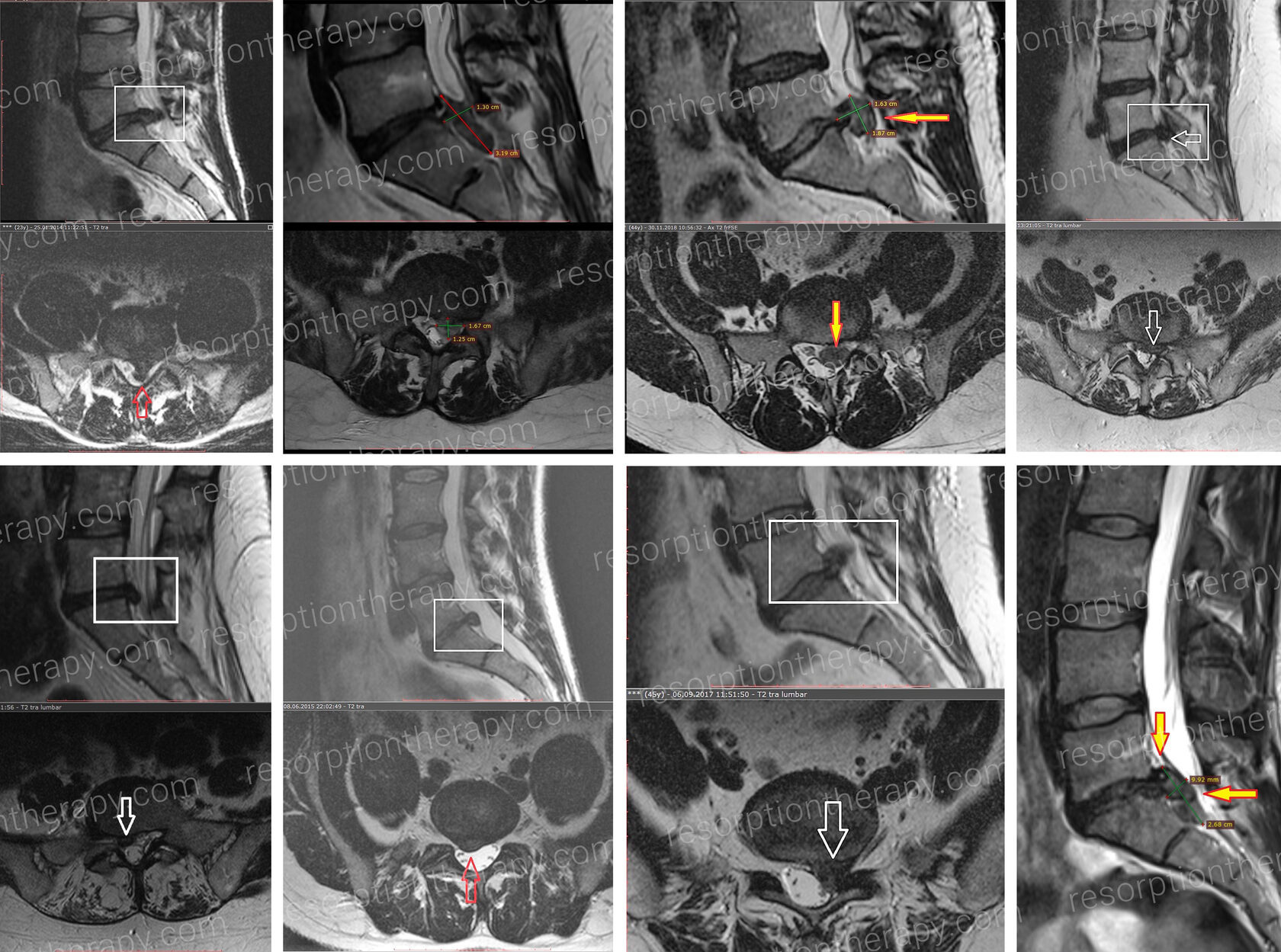
MRI is the most reliable and the most appropriate method to spot a herniated disc.
- MRI (magnetic resonance imaging) accurately examines the lumbar spine area, shows a herniation site and the affected nerves.
- CT (computed tomography) scan is recommended when an MRI is not possible for some reasons. However, this method is not good for predicting the future effect of treatment.
- X-rays are mainly used to identify such problems as a broken bone, bone abnormalities, infection, tumor, or problems with the alignment of the spine. A herniated disc is not diagnosed with X-rays only.
- Electromyography (EMG) can pinpoint the impacted nerve.
Nonsurgical Treatments for L5-S1
Initially, a herniated disc is treated in a conservative and nonsurgical manner. A doctor may advise the patient to observe a low, painless activity level for a few days to several weeks. This decreases the spinal nerve inflammation. Bedrest is not the best advice to recover.
For a mild or moderate pain, a herniated disc is treated with nonsteroidal anti-inflammatory medication. Extreme cases might require an epidural steroid injection, which should be performed under the instructions and X-ray manual to guide the medication to the exact level of the disc herniation.
The doctor may recommend physical therapy which will be described below.
● Medication
Over-the-counter (OTC) medications, such as non-steroidal anti-inflammatory drugs (NSAIDs) are usually the first line medication for pain originating from L5-S1. More severe pain might require the prescription of such medications as opioids, tramadol, and/or corticosteroids.
Pain medications are administered orally in tablets, capsules, and liquids. Here are the examples of pain killers.
● Local pain relievers
Topical pain relief medications are creams, gels, or patches applied to the skin. They can be prescribed and/or bought over-the-counter. They are often recommended to reduce localized pain.
Ingredients in the counterirritants, e.g. menthol, wintergreen, and eucalyptus, cause a hot or cold feeling. Counterirritant creams and gels are often used to treat sore muscles and are usually safe to be administered with other forms of pain killers. Some counterirritants, such as products with menthol, are available as skin patches.
Lidocaine is a local anesthetic cream, gel, or skin patch that brings temporary numbness, minimizes pain in the area it is applied on. Lidocaine is often combined with other ingredients in over the counter products. Versatis 5% medicated Plaster is one of the most popular one.
NSAID-containing ointments and gels (diclofenac, voltaren gels, finalgel, etc.) treat acute back pain, including pain, swelling, inflammation.
● Acupuncture
Pain can be relieved in a more effective and sustained manner with the help of acupuncture, which in turn may improve quality of life as well as productivity. Fine needles are applied to stimulate the nerves located in muscles and other tissues. Such an application triggers the release of endorphins and other neuro-humoral factors. It has been proven that acupuncture reduces inflammation by promoting the release of vascular and immunomodulatory factors and increasing local microcirculation. In turn, this may support better joint movement and relief of muscle stiffness.
● Physical therapy
L5-S1pain can be targeted by special exercises and physical therapies. These therapies stabilize the back and keep the muscles and joints well-conditioned for a long time. These therapies also treat the lower back tissues.
Typical physical therapy includes:
- Passive physical therapy is performed by the patient, such as heat application, ice packs and electrical stimulation. For example, l5 s1 pain relief exercises and stretches for herniated disc l5 s1 can be followed by applying a heating pad to warm up the muscles, and an ice pack may be used afterward to sooth the muscles and soft tissues.
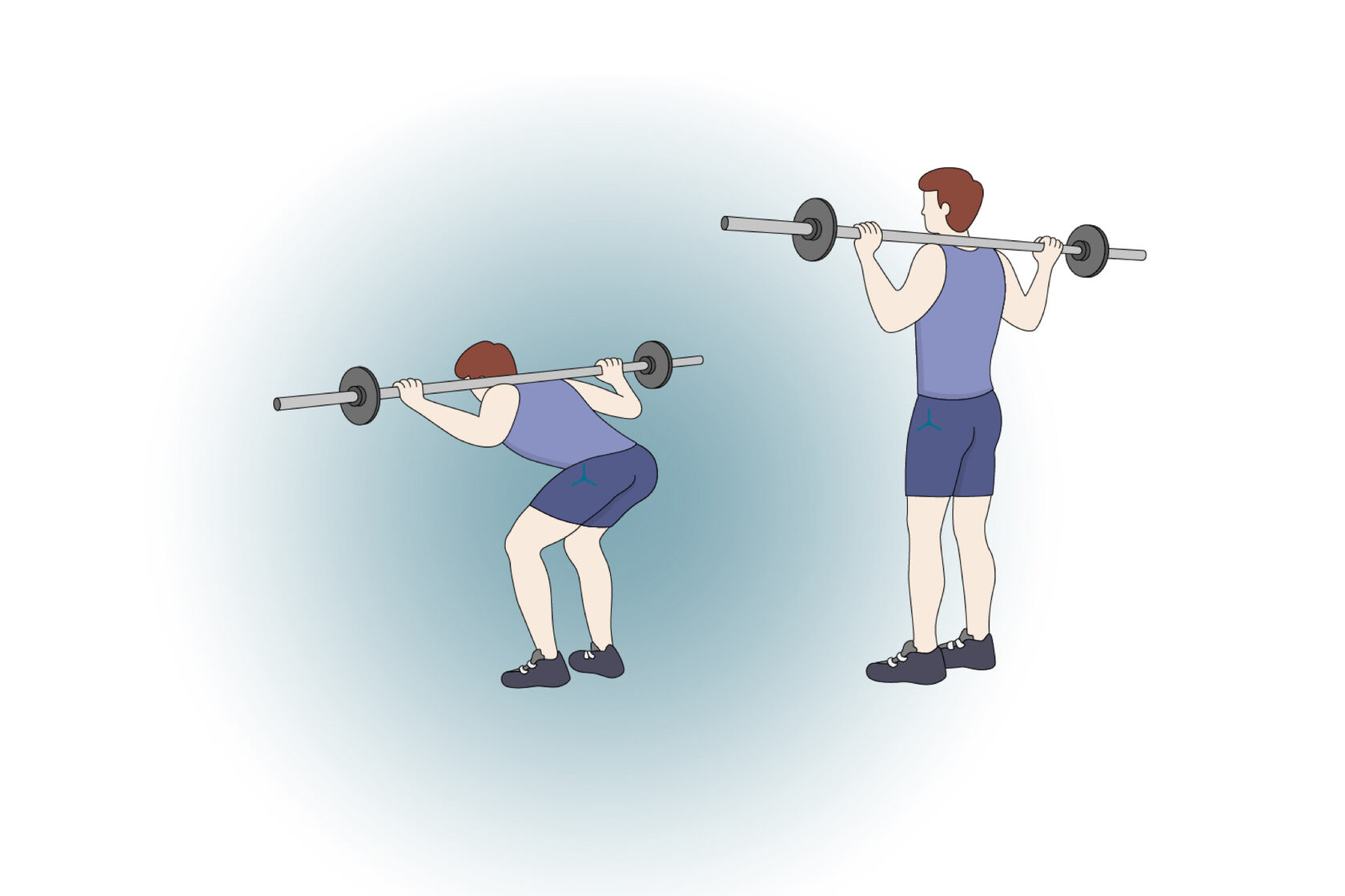
- Physiotherapy exercises are included into the medical rehabilitation of patients. It includes complex functional therapy with physical exercises as a way to maintain the patient's body in an active condition, to stimulate his internal resources, to prevent and treat diseases arisen due to forced hypodynamia. Walking, swimming, and Pilates are the most efficient and safest sports for patients with herniated discs of the lumbar spine area. Running, jumping, front flexions, weightlifting are prohibited.
NOTE! Consult a specialist if you want to perform the first two options. Unnecessary procedure (especially l5 s1 herniated disc exercises) or actions could harm patient’s health.
Prohibited l5 s1 exercises to avoid a lumbar herniation are:
"Good morning" - it's a weight-lifting exercise. Even if this exercise is performed by someone without a disc herniation, it could lead to problems. Performing a good morning, weight is placed on the shoulders, similar to when performing a traditional squat. The next step is to bend forward at the hips and allow your chest to drop toward the floor while maintaining a straight spine and legs. The exercise is a problem because it places a large working load on the lower back and buttocks.
"Standing hamstring stretch" - the common approach of “stand and reach for your toes” could cause serious issues when dealing with a herniation. The problem is that the l5 s1 stretch allows the back to compensate and bend forward, placing unnecessary stress on the front half of the disc.

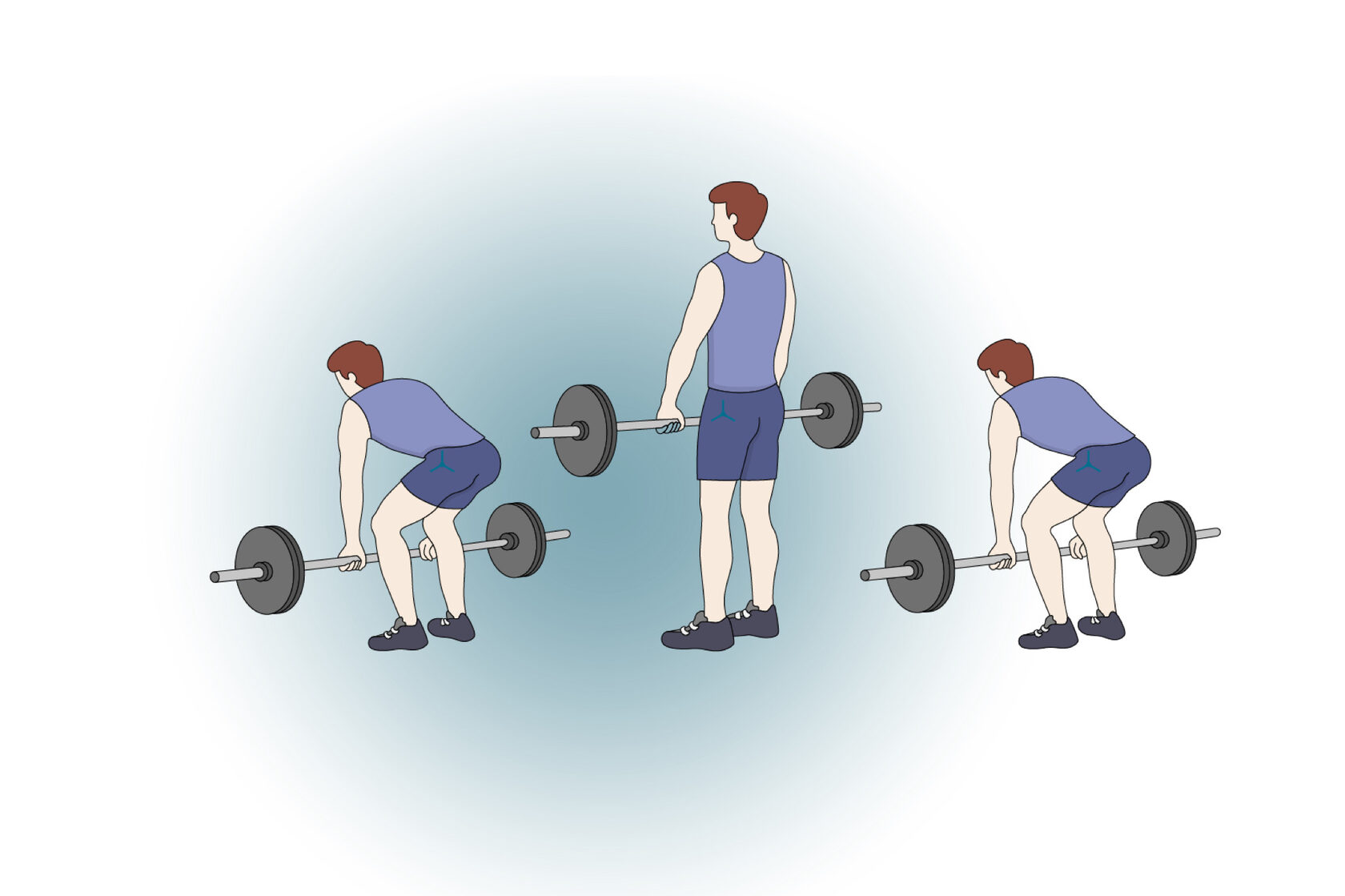
Deadlifts - one of the most common movement problems is allowing your lower back to round out while bending forward or lifting an object. A deadlift requires perfect mechanics. Even when done well, it will cause a great amount of compression at the disc.
- Therapeutic physiotherapy, which focuses on the physiotherapy. Laser therapy, magnetotherapy, phono- and electrophoresis are the most effective and safest treatment means for the lower back.
● Chiropractic manipulation
L5-S1 pain may be relieved by manipulating with the lumbar spine through chiropractic adjustment. Chiropractic is a health care profession which deals with the non-surgical treatment of disorders in the nervous system and/or musculoskeletal system. As a rule, chiropractors focus on spinal manipulation and treatment of the neighboring structures. When chiropractors treat patients with non-specific chronic low back pain, the long-term effects are enhanced by maintenance spinal manipulation after the initial intensive manipulative therapy. However, if you are diagnosed with a disc herniation, avoid manipulation of the affected segment. This is likely to increase the size or change the localization of the hernia, exacerbate the pathological process.
● Self-care
To promote healing and/or prevent an L5- S1 injury from becoming worse, you should avoiding:
- Repeated bending of the spine
- Sudden, abrupt movements, such as jumping
- High-intensity exercise and lifting heavy weights
Moreover, an active lifestyle, moderate exercising, no smoking and weight loss in overweight people can reduce the risk of L5-S1-related problems as well as herniation itself.
- Diet: you should optimise your diet especially if you are overweight. Anyway, consuming heath food is a must for every person.
- Hydration: it’s critical to consume much water. In case of a herniated disc L5/S1 compressing a nerve, any dehydration in that disc will worsen the compression.
- Overall activity: be active. You should walk as much as possible within the realms of comfort. Stop with pain, have a break, then return to it.
- Sleep: sleep is one of the key ingredients of a recovery from a herniated disc L5/S1 – sleep is when healing occurs. It’s impossible to get better without ample sleep each night.
Injection Treatments for L5-S1
Pain impulses from the abnormal L5-S1 segment structures into the central nervous system can be blocked by various types of injections.
- Paravertebral steroid injections in the lumbar area. Steroids injected directly into the paravertebral space can reduce inflammation and make nerve fibers less susceptible to pain with fewer pain signals. These injections have their strong effect on the inflammatory causes of pain, such as pain from inflammatory changes in the facet joints, edema and inflammation of the nerve root, and work the least for the compressive causes of pain.
- Lumbar epidural steroid injections. Steroids injected directly into the spinal epidural space can decrease inflammation and make nerve fibers less sensitive to pain with fewer pain signals. These injections work very well for the inflammatory causes of pain, such as pain from herniated disc fragments, and work less so for compressive causes of pain.
- Radiofrequency ablation. Pain from the L5-S1 facet joints may be healed with radiofrequency ablation. A part of the pain-transmitting nerve is heated with a radiofrequency needle to create a heat lesion. This lesion stops the pain signals from the nerve to the brain.
Injection treatments are typically accompanied with fluoroscopic (x-ray) guidance for correct needle placement. Fluoroscopic guidance and contrast dye improve diagnostic accuracy and decrease procedural risks.
Injectable treatments are usually considered when all conservative therapies have failed to be successful in their treatment for several weeks. These injections could cause bleeding and / or damage to nerves in the lumbar area.
Surgical Treatments for L5-S1
A neurologic deficit (numbness and / or weakness in the lower extremity) and pelvic dysfunction might require a surgical treatment. In this case, the pathology should be caused an anatomical problem which is known to be amenable to l5 s1 herniated disc surgery. Tumors, facet joint cysts, spondyloptosis, etc. could also become the reasons for performing surgery.
Lumbar spine surgeries with the aim to relieve nerve root compression and / or cauda equina syndrome are typically performed with minimally invasive techniques as follows:
- Microdiscectomy: A small part of the disc material near the nerve root is removed. Compression can be reduced by trimming a part of the bone adjacent to the nerve root. A l5 s1 discectomy presupposes small incisions. In case of an endoscopic microdiscectomy surgery, tissues are minimally disrupted as the instruments are inserted through a thin tube or tubes. A surgeon can use a tiny camera inserted through a tube for better visualization. While l5 s1 microdiscectomy and endoscopic microdiscectomy are considered to be low-risk procedures, all surgeries are characterized by some risks. About 10% of patients undergone microdiscectomy are likely to develop another disc herniation at the same site. This can happen within the first three months and years later. Multiple recurrences are typically dealt with lumbar fusion surgery. The disc material is completely removed, thus the discs are not fixed in their positions.
- Laminectomy: A part or all of the lamina (area of bone at the back of the vertebra) is removed for more space for the cauda equina. Lumbar laminectomy surgery achieves the following goals:
- Relieve neural tissue compression. Stenosis of the spinal canal in the lumbar region may compress the spinal cord, thecal sac, spinal dura, and/or the cauda equina. Compression of one or more of these structures leads to neurogenic claudication (leg pain while walking or bending the spine backward) and typically affects both lower extremities. Laminectomy widens the spinal canal and relieves the compression of these neural tissues.
- Improve leg function. Lumbar stenosis often decreases mobility due to pain and weakness in one or both legs. Laminectomy decreases pressure on the nerves, reduces leg pain, and potentially improves weakness and functions of the lower back and legs. A lumbar laminectomy can be determined by the amount of the removed lamina and the technique applied for providing less neural compression:
- Bilateral laminectomy: Both sides of the lamina of the affected vertebra are removed with or without widening of the intervertebral foramina and/or removal of adjacent tissue and bone.
- Unilateral laminotomy: A part of or the entire lamina on one side of the affected vertebra is removed with or without adjacent tissues. Unilateral laminotomy may also be performed with an endoscope (a small tube). Unlike an open surgery, this process is minimally invasive and requires a smaller incision. While minimally invasive techniques may be less traumatizing for the body and shorten the healing time, the overall success rates of open and minimally invasive decompression are usually at the same level. In some lumbar vertebrae, the facets may be partially or completely removed. In such cases, a fusion of the vertebrae is considered to retain stability.
- Foraminotomy: the spinal nerve root (intervertebral foramen) is relieved by trimming bony overgrowth.
- Facetectomy: The facet joints are trimmed to reduce compression of nerve roots.
- Lumbar interbody fusion: With a degenerated disc removed, L5-S1 vertebrae are fused together with implants or bone grafts. In case of a fusion surgery, the spinal fixation of the S1 segment usually gives a greater risk of failure (pseudarthrosis) compared to L5. To avoid this complication and to increase the likelihood of a successful L5-S1 fusion, the addition of an interbody support (device that holds the vertebrae together) is recommended.
- Lumbar artificial disc replacement. This surgery is not very popular as it completely replaces the intervertebral disc with the purpose to relieve nerve root compression and replace it with an artificial implant. Lumbar artificial disc replacement surgery may be the proper treatment for chronic, severe low back pain caused by degenerative disc disease. Disc replacement is only advised unless a minimum of 6 months of nonsurgical treatments give any effect, and if the pain decreases the quality of life. This surgery means replacing the painful spinal disc with a device designed to echo the disc’s movement. Artificial disc replacement aims to reduce micro-motion, stabilize the spinal segment, minimize inflammation, thus to alleviate pain.
FAQs
How long does it take for a herniated disc L5 S1 to heal?
However, if a person is diagnosed with a herniated disc L5/S1, it is impossible to accurately predict how long someone will suffer from it. Nevertheless, we try to give such a prognosis*.
*Resumption depends on the possibility of reducing the size of the intervertebral hernia after our treatment. This indicator is derived from the signal characteristics of the intervertebral hernia tissue on your MRI examination. It is typically the case, the healthier you are in general, the faster you will get better. Age also comes into play – people under 40 tend to recover a bit quicker than those over 40. And when you’ve been experiencing pain for a long time, the body changes, which impedes recovery.
Can Herniated Discs L5 S1 Heal on Their Own?
It is true that herniated disc symptoms can go away over time even without any treatment. But does that mean the herniated disc has healed on its own?
As it may happen, we can’t give a complete answer. Yes, your symptoms may disappear, but this does not necessarily mean the herniated disc itself has healed itself.
How do you sit with a L5 S1 herniated disc?
Sitting. Sitting for long periods of time isn’t the right choice for people with a herniated disc. A standing desk is better, but if you must sit, make sure your spine is firmly supported with the chair back, you sit up straight and don’t slouch (which puts some pressure on the spinal ligaments and aggravates a herniated disc). Your knees should be at the same level with your hips or slightly above the hips if you’re seated at a desk. Keep your feet flat on the floor, so make sure your chair fits this purpose.
To provide extra support, wedge a rolled-up towel or small pillow between the chair and the arch of your lower back. This also works when you’re in your car. If you do have to sit for a long period of time, try to have breaks as often as possible for muscle stretching.
