EPIPHYSIOLYSIS OF THE CAPITELLUM HUMERI - rbrs
EPIPHYSIOLYSIS OF THE CAPITELLUM HUMERI - rbrs
EPIPHYSIOLYSIS OF THE CAPITELLUM HUMERI - rbrs
Create successful ePaper yourself
Turn your PDF publications into a flip-book with our unique Google optimized e-Paper software.
JBR–BTR, 2005, 88: 184-186.<br />
<strong>EPIPHYSIOLYSIS</strong> <strong>OF</strong> <strong>THE</strong> <strong>CAPITELLUM</strong> <strong>HUMERI</strong><br />
T. Lauwers 1 , E. Geusens 1 , S. Pans 1 , S. Nijs 2<br />
A four-year-old girl presents at the emergency department with left elbow pain after a fall. X-ray demonstrated an<br />
epiphysiolysis of the capitellum humeri, without a bony fragment, the so-called Salter Harris Type 1 fracture.<br />
The fracture was treated by open reduction and internal fixation. This case is unusual because avulsions of the<br />
capitellum are usually associated with a bony fracture.<br />
Key-words: Elbow, fractures – Children, skeletal system.<br />
Pure chondral fractures of the<br />
capitellum are unusual. These<br />
lesions are usually associated with a<br />
radiological visible bony fragment.<br />
We present a displaced avulsion of<br />
the capitellum, the so-called Salter<br />
Harris Type 1 fracture (SH1).<br />
Case history<br />
A four-year-old girl with a medical<br />
history of left plexus brachialis<br />
injury after shoulder dystocia due to<br />
birth trauma presented at the emergency<br />
department with left elbow<br />
pain. She had fallen from a slide.<br />
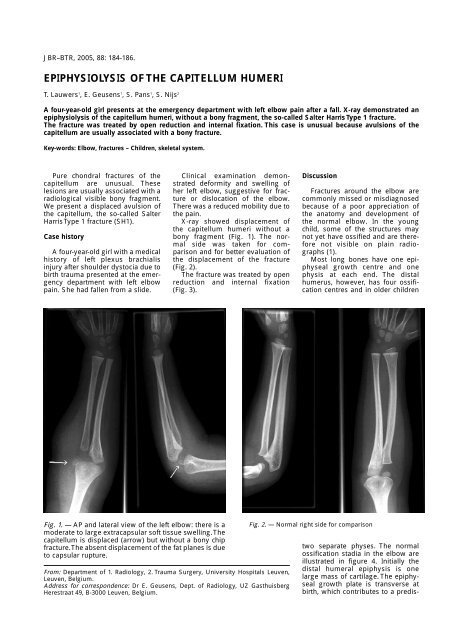
Fig. 1. — AP and lateral view of the left elbow: there is a<br />
moderate to large extracapsular soft tissue swelling. The<br />
capitellum is displaced (arrow) but without a bony chip<br />
fracture. The absent displacement of the fat planes is due<br />
to capsular rupture.<br />
Clinical examination demonstrated<br />
deformity and swelling of<br />
her left elbow, suggestive for fracture<br />
or dislocation of the elbow.<br />
There was a reduced mobility due to<br />
the pain.<br />
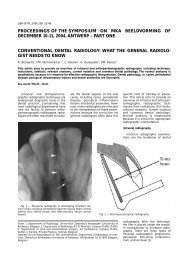
X-ray showed displacement of<br />
the capitellum humeri without a<br />
bony fragment (Fig. 1). The normal<br />
side was taken for comparison<br />
and for better evaluation of<br />
the displacement of the fracture<br />
(Fig. 2).<br />
The fracture was treated by open<br />
reduction and internal fixation<br />
(Fig. 3).<br />
From: Department of 1. Radiology, 2. Trauma Surgery, University Hospitals Leuven,<br />
Leuven, Belgium.<br />
Address for correspondence: Dr E. Geusens, Dept. of Radiology, UZ Gasthuisberg<br />
Herestraat 49, B-3000 Leuven, Belgium.<br />
Discussion<br />
Fractures around the elbow are<br />
commonly missed or misdiagnosed<br />
because of a poor appreciation of<br />
the anatomy and development of<br />
the normal elbow. In the young<br />
child, some of the structures may<br />
not yet have ossified and are therefore<br />
not visible on plain radiographs<br />
(1).<br />
Most long bones have one epiphyseal<br />
growth centre and one<br />
physis at each end. The distal<br />
humerus, however, has four ossification<br />
centres and in older children<br />
Fig. 2. — Normal right side for comparison<br />
two separate physes. The normal<br />
ossification stadia in the elbow are<br />
illustrated in figure 4. Initially the<br />
distal humeral epiphysis is one<br />
large mass of cartilage. The epiphyseal<br />
growth plate is transverse at<br />
birth, which contributes to a predis-
position to total separation of the<br />
epiphysis if significant trauma<br />
occurs. During maturation, separate<br />
ossification centres develop for the<br />
capitellum, the medial epicondyle,<br />
the trochlea and the lateral epicondyle.<br />
In early youth, the growth<br />
plate gradually extends obliquely<br />
downward and medially from a<br />
point just above the lateral epicondyle<br />
to below the medial epicondyle<br />
(Fig. 4).<br />
By age 4, the growth plate becomes<br />
more irregular and metaphyseal<br />
bone begins to project between<br />
the medial epicondyle and the capitellum,<br />
dividing the physis into two<br />
separate physes. Both of these factors<br />
aid stability and total separation<br />
of the epiphyses becomes more difficult.<br />
Anatomic peculiarities of the distal<br />
humerus may therefore explain<br />
the differences in age distribution of<br />
these injuries (2).<br />
Many classifications of physeal<br />
injuries have been proposed. The<br />
classification of Salter and Harris<br />
(Fig. 5) is the most commonly used:<br />
type 1: a fracture that involves epiphyseal<br />
separation because of a<br />
fracture through the physis only,<br />
type 2: a fracture through the physis<br />
and metaphysis, with a fragment of<br />
the metaphysis remaining attached<br />
to the epiphysis, type 3: a fracture<br />
that begins intra-articularly and travels<br />
through the epiphysis into the<br />
physis, type 4: a fracture that begins<br />
intra-articularly and travels through<br />
the epiphysis, physis and the metaphysis,<br />
and type 5: the physis is<br />
crushed (3).<br />
Anteroposterior and lateral radiographs<br />
of the injured elbow are<br />
<strong>EPIPHYSIOLYSIS</strong> <strong>OF</strong> <strong>THE</strong> <strong>CAPITELLUM</strong> <strong>HUMERI</strong> — LAUWERS et al 185<br />
Fig. 3. — Image during open reduction and internal fixation:<br />
note the displaced capitellum (arrow).<br />
essential for evaluation. Views of the<br />
opposite elbow in the same position<br />
provide a valuable basis for comparison<br />
in assessing injury, but should<br />
not be taken on a routine base. Intraarticular<br />
haematoma may displace<br />
the posterior fat pad of the distal<br />
humerus (the “fat pad sign”), which<br />
may be the only demonstrable sign<br />
in an undisplaced or spontaneously<br />
reduced fracture. But in case of capsular<br />
rupture, the intra-articular<br />
blood or fluid can leak in the sur-<br />
Fig. 4. — Schematic drawing of the normal age of ossification<br />
of the elbow. Numbers indicate the approximate age in years at<br />
which the centre begins to ossify.<br />
Fig. 5. — Schematic drawing of the Salter-Harris classification<br />
of physeal injuries.<br />
rounding tissues, and the fat pad<br />
sign can disappear. So, a normal fat<br />
pad does not exclude a fracture of<br />
the elbow.<br />
Because the epiphysis is primarily<br />
cartilaginous in young children,<br />
epiphyseal separation may be difficult<br />
to diagnose by routine radiographs.<br />
Ultrasound has gained an<br />
increasing role in the diagnosis of<br />
musculo-skeletal pathology (3). It is<br />
non-invasive, and does not require<br />
sedation. High resolution real-time
186 JBR–BTR, 2005, 88 (4)<br />
sonography of the musculo-skeletal<br />
system of infants and young children<br />
is being used with increasing<br />
frequency, in part because of the<br />
inability of plain film radiography to<br />
visualize unossified cartilage (4).<br />
Reasons to examine a patient with<br />
sonography include pain, limitation<br />
of motion, soft tissue swelling and<br />
clinical suspicion of joint abnormality<br />
when findings on plain films are<br />
inconclusive. Because we had a<br />
diagnosis on plain films alone, we<br />
did no perform ultrasound before<br />
surgery. MRI can also be of<br />
value (5), but anaesthesia is often<br />
needed in young children.<br />
Because this fracture involves<br />
both the articular surface and the<br />
physis, anatomic reduction is necessary<br />
and must be held until the fracture<br />
has united. This usually<br />
requires internal fixation.<br />
Malunion and non-union are frequent<br />
complications in untreated<br />
cases. These can cause deformity,<br />
loss of motion and degenerative<br />
arthrosis.<br />
In conclusion, we do not advocate<br />
the systematic use of comparative<br />
views, but in doubtful cases, the<br />
comparative view can be helpful in<br />
making the correct diagnosis.<br />
This case is unusual because<br />
avulsions of the capitellum are usually<br />
associated with a bony fracture.<br />
Pure chondral fractures of the<br />
capitellum are very unusual.<br />
References<br />
1. Paterson J.M.H.: Children’s fractures<br />
“not to be missed”. Hospital<br />
Medicine, 2002, 63: 426-428.<br />
2. Peterson H.A.: Physeal injuries of the<br />
distal humerus. Orthopedics, 1992,<br />
15: 799-808.<br />
3. Bar-On E., Howard C.B., Porat S.: The<br />
use of ultrasound in the diagnosis of<br />
atypical pathology in the unossified<br />
skeleton. J Paediatr Ortho, 1995, 15:<br />
817-820.<br />
4. Markowitz R.I., Davidson R.S.,<br />
Harty M.P., et al.: Sonography of the<br />
elbow in infants and children. AJR,<br />
1992, 159: 829-833.<br />
5. Della-Giustina K., Della-Giustina D.A.:<br />
Emergency department evaluation<br />
and treatment of pediatric orthopaedic<br />
injuries. Emerg Med Clin<br />
North Am, 1999, 17: 895-923.