Diabetic Neuropathy: Current Concepts - medIND
Diabetic Neuropathy: Current Concepts - medIND
Diabetic Neuropathy: Current Concepts - medIND
Create successful ePaper yourself
Turn your PDF publications into a flip-book with our unique Google optimized e-Paper software.
Introduction<br />
* Senior Resident<br />
** Professor<br />
Department of Endocrinology and<br />
Metabolism, Institute of Medical Sciences,<br />
Banaras Hindu University,<br />
Varanasi – 221005.<br />
REVIEW ARTICLE<br />
<strong>Diabetic</strong> <strong>Neuropathy</strong>: <strong>Current</strong> <strong>Concepts</strong><br />
<strong>Neuropathy</strong>, a common complication of diabetes<br />
mellitus, is generally considered to be related to<br />
duration and severity of hyperglycaemia. However,<br />
it may also occur acutely even with<br />
hypoglycaemia 1-3 . Usually more than 50% of<br />
patients with duration of diabetes of 25 years or<br />
more are affected, making it as one of the most<br />
common disease of the nervous system 4 . One of<br />
the largest published series reported a prevalence<br />
of 7.5% even at the time of diagnosis of diabetes 4 .<br />
The prevalence however, increases progressively<br />
without a plateau.<br />
Definition<br />
<strong>Diabetic</strong> neuropathy has been defined as presence<br />
of symptoms and/or signs of peripheral nerve<br />
dysfunction in diabetics after exclusion of other<br />
causes, which may range from hereditary,<br />
traumatic, compressive, metabolic, toxic,<br />
nutritional, infectious, immune mediated,<br />
neoplastic, and secondary to other systemic<br />
illnesses. Since the manifestations of diabetic<br />
neuropathy closely mimic chronic inflammatory<br />
demyelinating polyneuropathy, alcoholic<br />
neuropathy, and other endocrine neuropathies,<br />
hence, before labelling diabetic neuropathy it is<br />
mandatory to exclude all other causes of<br />
peripheral nerve dysfunction.<br />
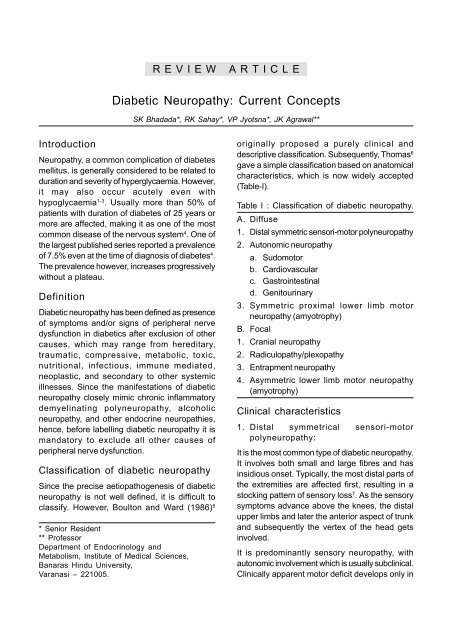
Classification of diabetic neuropathy<br />
Since the precise aetiopathogenesis of diabetic<br />
neuropathy is not well defined, it is difficult to<br />
classify. However, Boulton and Ward (1986) 5<br />
SK Bhadada*, RK Sahay*, VP Jyotsna*, JK Agrawal**<br />
originally proposed a purely clinical and<br />
descriptive classification. Subsequently, Thomas 6<br />
gave a simple classification based on anatomical<br />
characteristics, which is now widely accepted<br />
(Table-I).<br />
Table I : Classification of diabetic neuropathy.<br />
A. Diffuse<br />
1. Distal symmetric sensori-motor polyneuropathy<br />
2. Autonomic neuropathy<br />
a. Sudomotor<br />
b. Cardiovascular<br />
c. Gastrointestinal<br />
d. Genitourinary<br />
3. Symmetric proximal lower limb motor<br />
neuropathy (amyotrophy)<br />
B. Focal<br />
1. Cranial neuropathy<br />
2. Radiculopathy/plexopathy<br />
3. Entrapment neuropathy<br />
4. Asymmetric lower limb motor neuropathy<br />
(amyotrophy)<br />
Clinical characteristics<br />
1. Distal symmetrical sensori-motor<br />
polyneuropathy:<br />
It is the most common type of diabetic neuropathy.<br />
It involves both small and large fibres and has<br />
insidious onset. Typically, the most distal parts of<br />
the extremities are affected first, resulting in a<br />
stocking pattern of sensory loss 7 . As the sensory<br />
symptoms advance above the knees, the distal<br />
upper limbs and later the anterior aspect of trunk<br />
and subsequently the vertex of the head gets<br />
involved.<br />
It is predominantly sensory neuropathy, with<br />
autonomic involvement which is usually subclinical.<br />
Clinically apparent motor deficit develops only in
are cases. Its symptoms are extremely variable,<br />
ranging from severely painful symptoms at one<br />
extreme to the completely painless variety, which<br />
may present with an insensitive foot ulcer at the<br />
other end. The neuropathic symptoms may be<br />
positive or negative. The negative symptoms are -<br />
numbness and deadness in the lower limbs while<br />
the positive symptoms most commonly include<br />
burning pain, altered and uncomfortable<br />
temperature perception, paraesthesia, shooting,<br />
stabbing and lancinating pain, hyperaesthesia and<br />
allodynia. The feet and legs are most commonly<br />
affected, rarely less severe similar symptoms are<br />
experienced in the upper limbs also.<br />
The sensory symptoms and signs are more<br />
common than motor symptoms and signs.<br />
Common motor signs are absent or reduced ankle<br />
reflex, and minimal distal muscle weakness. Motor<br />
involvement results in foot deformity. This<br />
abnormality redistributes weight bearing and leads<br />
to callus and ulcer formation. The proprioceptive<br />
loss makes the gait more unsteady and there is a<br />
sense of walking on cotton wool.<br />
Acute painful neuropathy is a distinct variant of<br />
distal sensory neuropathy 8 , presenting acutely with<br />
severe sensory symptoms with few sensory or<br />
motor signs and often it follows a period of flux in<br />
glycaemic control.<br />
2. Autonomic neuropathy<br />
Autonomic neuropathy is a serious and often overlooked<br />
component of diabetic neuropathy. Any<br />
organ of body which is supplied by autonomic<br />
nerves can be affected. Studies have confirmed<br />
the presence of parasympathetic dysfuction in 65%<br />
of the type 2 diabetic patients 10 years after<br />
diagnosis and of combined parasympathetic and<br />
sympathetic neuropathy in 15.2% 9 . Autonomic<br />
neuropathy is not simply an “all or none”<br />
phenomenon and its symptoms range from minor<br />
to severe. The severe form may affect survival and<br />
can cause sudden death. Among autonomic<br />
neuropathic symptoms gustatory sweating is most<br />
common, followed by postural hypotension and<br />
diarrhoea 10 . Loss of sweating in the feet, sexual<br />
dysfunction, bladder abnormalities, and<br />
gastroparesis may also occur (Table II).<br />
Table II : Symptoms and signs of autonomic<br />
neuropathy.<br />
1. Cardiovascular<br />
Postural hypotension<br />
Resting tachycardia<br />
Painless myocardial infarction<br />
Sudden death (with or without association<br />
with general anaesthesia)<br />
Prolonged QT interval<br />
2. Gastrointestinal<br />
Oesophageal motor incoordination<br />
Gastric dysrhythmia, hypomotility<br />
(gastroparesis diabeticorum)<br />
Pylorospasm.<br />
Uncoordinated intestinal motility (diabetic<br />
diarrhoea, spasm)<br />
Intestinal hypomotility (constipation)<br />
Gallbladder hypocontraction (diabetic<br />
cholecystopathy)<br />
Anorectal dysfunction (faecal incontinence)<br />
3. Genitourinary<br />
<strong>Diabetic</strong> cystopathy (impaired bladder<br />
sensation, atonic bladder, post micturition<br />
dribbling, detrusor hyporeflexia or<br />
hyperreflexia)<br />
Male impotence<br />
Ejaculatory disorders<br />
Reduced vaginal lubrication, dyspareunia<br />
4. Respiratory<br />
Impaired breathing control (?)<br />
Sleep apnoea ?<br />
5. Thermoregulatory<br />
Sudomotor<br />
Vasomotor<br />
6. Pupillary<br />
Miosis<br />
Disturbances of dilatation<br />
Argyll Robertson pupil<br />
306 Journal, Indian Academy of Clinical Medicine Vol. 2, No. 4 October-December 2001
3. Proximal motor neuropathy<br />
It typically affects the elderly males (> 50 year)<br />
suffering from type 2 diabetes mellitus but it can<br />
also occur in females and type 1 diabetes mellitus.<br />
It may be symmetrical or asymmetrical, and with<br />
or without sensory loss. Patient usually presents<br />
with difficulty in getting up from squatting position,<br />
pain in climbing stairs and marked weight loss<br />
(sometimes upto 40% of original weight). It<br />
predominantly affects anterior (quadriceps) and<br />
adductor compartments of thigh. Wasting and<br />
weakness of quadriceps is so severe that the knee<br />
often gives way, and patient may fall. This has<br />
been labelled as diabetic amyotrophy also.<br />
The cause of diabetic amyotrophy is unknown but<br />
neurological deficit and anatomical distribution<br />
suggest nerve root involvement presumably due<br />
to occlusion of the vasa nervosum and infarction.<br />
Examination shows wasting and weakness of the<br />
anterior and adductor compartments of thigh. The<br />
knee jerk is absent, while the ankle jerk may be<br />
intact. Sometimes, other muscles, especially the<br />
anterior tibial and peroneal muscles may also be<br />
involved 11 .<br />
4. Focal neuropathies or mono-neuropathies<br />
The diabetic patients are also susceptible to a<br />
variety of asymmetric and focal neuropathies.<br />
a. Cranial <strong>Neuropathy</strong> : The third, fourth, and<br />
sixth cranial nerves are commonly involved 12 .<br />
Elderly patients are the most affected. The third<br />
cranial nerve palsy presents with eye pain,<br />
diplopia, and ptosis but pupillary response to light<br />
is usually spared 1 . The pupillary sparing favours<br />
vascular aetiology of IIIrd nerve palsy. Exclusion<br />
of other causes of IIIrd nerve palsy is necessary<br />
before labelling diabetes as a cause. Spontaneous<br />
recovery generally occurs within 6-12 weeks,<br />
although recurrent or bilateral lesion may also<br />
occur 2 .<br />
b. Truncal <strong>Neuropathy</strong> : Symptomatic truncal<br />
polyneuropathy though less common, tends to<br />
occur in the setting of long standing diabetes with<br />
other microvascular complications especially<br />
peripheral neuropathy. Most of the affected<br />
individuals are in the 5th or 6th decade of life,<br />
with a variable duration of diabetes 12 . It usually<br />
presents with gradual onset of pain and<br />
dysaesthesia in the lower anterior chest or upper<br />
abdomen with nocturnal intensification. On<br />
examination, hypoaesthesia or hyperaesthesia<br />
may be present in the appropriate thoracic<br />
segment and abdominal muscle weakness leading<br />
to abdominal swelling 13 . A careful sensory<br />
examination of abdomen and thorax is mandatory<br />
in a diabetic person presenting with unexplained<br />
thoracoabdominal pain. It resolves, spontaneously<br />
within 2 to 6 months.<br />
c. Entrapment neuropathy : Also known as<br />
pressure palsy, this is relatively uncommon. Median<br />
nerve is mostly affected and is secondary to soft<br />
tissue changes associated with limited joint<br />
mobility. Occasionally ulnar or lateral cutaneous<br />
nerve of thigh may also be affected.<br />
Pathogenesis of diabetic neuropathy<br />
The precise pathogenesis of diabetic peripheral<br />
neuropathy despite recent advances remains<br />
obscure; however, consensus is that neuropathy<br />
in diabetes mellitus is a multifactorial disease 14 .<br />
The possible aetiologic factors suggested include,<br />
hyperglycaemia, polyol pathway, non-enzymatic<br />
glycation, free radical and oxidative stress.<br />
Available evidence suggests that these various<br />
pathogenetic factors act synergistically 15 . Many of<br />
these hypotheses are based on studies of different<br />
animal models of diabetes, but none of these truly<br />
reproduce the changes as seen in diabetic<br />
neuropathies in humans 16 . Generally the nerve<br />
involvement has been correlated with glycaemic<br />
control, hyperglycaemia induced metabolic<br />
derangements and neurophysiological alterations,<br />
serum lipid changes, vascular coagulation, and<br />
thrombotic abnormalities 2 .<br />
a. Hyperglycaemia and polyol pathway<br />
Long-standing hyperglycaemia is the main<br />
culprit in the development of diabetic<br />
neuropathy. This has been shown in the results<br />
Journal, Indian Academy of Clinical Medicine Vol. 2, No. 4 October-December 2001 307
of the Diabetes Control and Complications<br />
Trial (DCCT) 17 . This randomised prospective<br />
study showed significant reduction in the<br />
development and progression of clinical<br />
neuropathy (64%), motor conduction velocity<br />
(44%), and autonomic dysfunction (53%) in<br />
type-1 diabetics with optimal glycaemic<br />
control 18 .<br />
The glucose uptake into peripheral nerve is<br />
insulin independent, therefore it is<br />
proportionate to ambient blood glucose<br />
concentration. The rate-limiting enzyme for<br />
polyol pathway is aldose reductase, which is<br />
expressed on Schwann cells. Excess glucose is<br />
shunted into the polyol pathway and is<br />
converted to sorbitol and fructose by the<br />
enzymes aldose reductase and sorbitol<br />
dehydrogenase respectively 14 . The nerve cell<br />
membrane is relatively impermeable to sorbitol<br />
and fructose, which tend to accumulate within<br />
the nerve 19 . Fructose and sorbitol both being<br />
osmotically active compounds lead to increase<br />
in the water content in the nerves. Further the<br />
oxidation/reduction status of the cell is altered<br />
with loss of reduced nicotinamide-adenine<br />
dinucleotide phosphate (NADPH) and<br />
glutathione stores. It leads to a cascade of<br />
events like a reduced membrane Na- K ATPase<br />
activity, intra-axonal sodium accumulation<br />
which reduces nerve conduction velocity and<br />
brings about structural breakdown of the<br />
nerve 14 (Fig. 1). Myoinositol level is decreased<br />
because elevated levels of both glucose and<br />
sorbitol compete for the uptake of myoinositol<br />
in the tissues and cells 20 . Moreover, reduced<br />
NADPH, a cofactor for the enzyme nitric oxide<br />
synthase, reduces nitric oxide formation<br />
leading to decreased vasodilatation, that<br />
impairs blood supply to the nerve 21 .<br />
Polyol pathway although appears to be a<br />
plausible cause for diabetic neuropathy, has<br />
many pit falls such as (a) the absence of<br />
morphological changes in diabetic neuropathy<br />
in humans as compared to animal models 22 ,<br />
(b) an increase, but not decrease, of Na + K + -<br />
Fig. 1:<br />
ATPase in the peripheral nerve of<br />
galactosaemic animals despite a reduction in<br />
the myo-inositol level 23 , (c) the lack of a<br />
convincingly demonstrable reduced level of<br />
myo-inositol in human nerve, and the failure<br />
of dietary myo-inositol supplementation to<br />
improve neuropathy in humans 24 , (d) the lack<br />
of unequivocal improvement from the use of<br />
a variety of aldose reductase inhibitors 25 .<br />
b. Advanced glycation end products (AGE)<br />
In the presence of hyperglycaemia, glucose can<br />
be incorporated non-enzymatically into<br />
proteins by an unregulated glycation reaction.<br />
Patient with normal blood sugar are protected<br />
by the tight control of blood glucose within<br />
normal limits. This glycation reaction occurs<br />
in two steps for formation of HbA 1C . In the first<br />
step there is formation of PreA 1C the Schiff base;<br />
it is a rapid and reversible reaction. Second<br />
step is a slow and irreversible step with the<br />
formation of HbA 1C , which is a ketoamine.If<br />
plasma glucose is normal for a week, levels of<br />
glycated serum proteins decrease by<br />
approximately 40% while HbA 1C drops by only<br />
10% 26 .<br />
The HbA 1C formation is an example of<br />
glycation of proteins. Like haemoglobin A,<br />
308 Journal, Indian Academy of Clinical Medicine Vol. 2, No. 4 October-December 2001
other body proteins such as plasma albumin,<br />
lipoproteins, fibrin, collagen, and glycoprotein<br />
recognition systems of hepatic endothelial cells<br />
may also undergo non-enzymatic glycation.<br />
The glycation of proteins alters or impairs their<br />
function, e.g., glycated LDL is not recognised<br />
by the normal LDL receptor, and its plasma<br />
half life is increased. Conversely glycated HDL<br />
turns over more rapidly than native HDL.<br />
Glycated collagen is less soluble and more<br />
resistant to degradation by collagenase than<br />
native collagen.<br />
Non-enzymatically glycated proteins slowly<br />
form fluoroscent cross-linked protein products<br />
called advanced glycation end products<br />
(AGEs). AGEs formation is accelerated by high<br />
ambient glucose concentration and by age.<br />
Patients with long standing diabetes have levels<br />
at least twice those of normal subjects 27 . The<br />
rate of glycation with fructose is seven or eight<br />
times than that with glucose. The glycation of<br />
myelin protein may contribute to the<br />
impairment of nerve conduction 28 . These<br />
advanced glycation end products are also<br />
present in peripheral nerves 29 which could<br />
interfere with axonal transports.<br />
AGES are also believed to cause tissue damage<br />
because of their reactivity and protein cross<br />
linking. Receptors for AGE proteins are<br />
expressed on endothelial cells, fibroblast,<br />
mesangial cells, and macrophages 30 . A<br />
macrophage monocyte receptor for AGE<br />
mediates the uptake of AGE modified proteins<br />
and the release of TNFα,IL-1, IGF-1, platelet<br />
derived growth factor 30 . Endothelial cell has<br />
AGE receptors which internalises AGE to the<br />
subepithelium, thereby enhancing permeability<br />
and endothelium dependent coagulant activity.<br />
AGE also produce alteration in RBC and<br />
lipoproteins.<br />
c. Miscellaneous<br />
i. Free radical and oxidative stress<br />
Oxygen free radicals could damage nerve by<br />
direct toxic effects or perhaps by inhibiting nitric<br />
oxide (NO) production by the endothelium,<br />
thereby reducing nerve blood flow. In diabetic<br />
tissues, free radical generation is enhanced<br />
by the processes of non-enzymatic glycation<br />
and polyol pathway, while the ability to<br />
neutralise free radicals is reduced because<br />
NADPH is consumed through increased activity<br />
of aldose reducatse 31 .<br />
ii. Biochemical abnormalities<br />
Levels of gamma-linolenic acid (GLA) in nerves<br />
are reduced, because insulin deficiency and<br />
hyperglycaemia inhibit the activity of d-6desaturase<br />
enzyme which governs its<br />
conversion from linoleic acid. GLA is precursor<br />
of prostanoids, including potent vasodilator,<br />
prostacyclin, and its deficiency has been<br />
implicated in the reduced blood flow of<br />
diabetic nerves. Supplementation of GLA<br />
decreases rate of deterioration in nerve<br />
conduction velocity 32 . Moreover, there is<br />
depletion of carnitine in diabetic nerves. The<br />
carnitine deficiency could impair ATP<br />
production. Administration of acetyl-L-carnitine<br />
to diabetic rats improves various indices of<br />
peripheral nerve function.<br />
iii. Vascular and haemorrheological<br />
abnormalities<br />
The endoneural vessels get blocked because of<br />
hyperplasia and swelling of endothelial cells,<br />
thickening of vessel wall with debris from<br />
degenerative pericytes as well as basement<br />
membrane material, and occlusion of the<br />
capillary lumen by fibrin or aggregated<br />
platelets 33 . Further various defects in nerve nitric<br />
oxide (NO) production, increased “quenching”<br />
of NO by AGE in the vessel wall, deficiency of<br />
prostacyclin and increased endothelial<br />
production of potent vasoconstrictor peptide,<br />
endothelin – 1 are responsible for increased<br />
vasoconstriction which in turn causes central<br />
nerve ischaemia. Glycosylation of RBC<br />
membrane occurs and that decreases<br />
malleability of RBC and impairs microcirculation.<br />
Journal, Indian Academy of Clinical Medicine Vol. 2, No. 4 October-December 2001 309
iv. Defects in nerve regeneration<br />
Peripheral nerves have abundant receptors for<br />
nerve growth factor (NGF). NGF is responsible<br />
for regeneration of nerves. Circulating NGF<br />
concentration is reduced in diabetic patients<br />
with neuropathy 34 . Treatment with NGF has<br />
improved peripheral nerve function. Insulin like<br />
growth factor and neurotrophin – 3 also helps<br />
in regeneration of nerves.<br />
Thus regardless of the exact pathogenesis of<br />
diabetic neuropathy, it is now clear that chronic<br />
hyperglycaemia has a pivotal role in the<br />
pathogenesis of diabetic neuropathy. The<br />
earliest effects of hyperglycaemia are generally<br />
metabolic while electrophysiologic and<br />
morphological changes are considered to be<br />
a late occurrence. Intensive control of blood<br />
sugar reduces the occurrence of clinical<br />
neuropathy. However, once diabetic<br />
neuropathy is established, significant recovery<br />
usually does not occur, even with good<br />
glycaemic control.<br />
Diagnosis of diabetic neuropathy (DN)<br />
The diagnosis of DN can be made on clinical<br />
examination but subsequently it needs to be<br />
confirmed by investigations (non-invasive/<br />
invasive). The diagnosis of DN in time is very<br />
important because effective intervention will be<br />
possible only during the subclinical or early phase<br />
of dysfunction. There are two approaches for<br />
diagnosis of DN (i) Traditional (ii) Newer.<br />
A. Traditional approaches<br />
1. Clinical examination : The traditional<br />
approach to diagnose DN, requires careful<br />
clinical assessment of “Signs” of sensory, motor,<br />
and autonomic function deterioration. Clinical<br />
examination yields a “valid” index of DN quickly,<br />
but inter-examiner variability limits the<br />
reproducibility and reliability of test results 35 .<br />
2. Test of sensory function : In-depth sensory<br />
examination is required because routine<br />
clinical examination will only detect<br />
abnormalities at a relatively advanced stage<br />
and selective involvement of fibre is not rare.<br />
Patient co-operation is mandatory for clinical<br />
examination.<br />
a. Vibration perception threshold (VPT) : It is<br />
usually assessed by 128 Hz tuning fork. Only<br />
large fibres are assessed by the test. Vibration<br />
perception is usually assessed at the tip of great<br />
toe or over lateral malleolus. Nowadays more<br />
sophisticated instruments are available for<br />
assessment of vibration perception threshold,<br />
e.g., biosthesiometer, vibrameter.<br />
Biosthesiometer uses an electromagnet to<br />
activate a spring loaded stimulator, according<br />
to an arbitrary scale from 0-50 volts. The risk<br />
of foot ulceration is increased 3-4 fold if the<br />
vibration perception threshold exceeds 25<br />
volts. Vibrameter is also based on the principle<br />
of biosthesiometer but results are given directly<br />
in mm of probe displacement.<br />
b. Light touch sensation : These sensations are<br />
carried by large myelinated Aα and Aβ fibres.<br />
Nylon Semmes Weintein mono-filaments are<br />
used for light touch assessment. A series of<br />
increasingly thick filaments are tested, and the<br />
threshold at which the first one can be felt when<br />
buckling is noted. The inability to feel the 10<br />
gm filament indicate that patient is prone to<br />
foot ulceration.<br />
c. Thermal thresholds : Warm and cold<br />
sensations should be tested separately. The<br />
former is mediated by the smallest<br />
unmyelinated C fibres and the latter by small<br />
myelinated Aδ fibres. The equipment used for<br />
thermal threshold assessment are expensive<br />
and mostly used for research purposes. Pain<br />
threshold can be determined either by<br />
application of high or low temperature or by<br />
using the “Pinchometer” or a series of weighted<br />
needles.<br />
d. Tests for autonomic function : Bedside<br />
cardiovascular tests have been developed to<br />
evaluate cardiovascular autonomic neuropathy<br />
(table-III) 36 . These tests are extremely sensitive<br />
310 Journal, Indian Academy of Clinical Medicine Vol. 2, No. 4 October-December 2001
and as many as one fifth of all diabetic patients<br />
have one or more abnormalities while very few<br />
suffer from symptomatic autonomic<br />
neuropathy, when non-specific symptoms such<br />
as diarrhoea or gastroparesis occur, autonomic<br />
tests must be abnormal. Other autonomic<br />
functions like blood pressure response to<br />
sustained hand grip and pupillary function<br />
require more sophisticated equipment and are<br />
mostly used as research tools rather than in<br />
routine clinical practice.<br />
e. Electrophysiology : Standard elctrophysiologic<br />
methods have also been used<br />
extensively to diagnose and follow the<br />
progression of DN 37 . Electrophysiology,<br />
particularly conduction velocity alone, may<br />
provide a poor measure of early dysfunction<br />
in some patients, because there is little<br />
demyelination in the early stages 38 . Although<br />
response amplitude can be correlated with<br />
density in a population, the onset of change<br />
in their measure may not be apparent in<br />
individual patients because of the considerable<br />
variability in amplitude measure.<br />
B. New approaches to the diagnosis of<br />
diabetic neuropathy<br />
1. Skin punch biopsy and immunohistochemical<br />
staining : Skin punch biopsy<br />
specimens (3-4 mm in diameter) obtained with<br />
the patient under local lidocaine anaesthesia<br />
under aseptic technique 39 is fixed in formalin,<br />
cut into 50 mm frozen sections and processed<br />
for immuno-histochemistry using commercially<br />
available polyclonal antibodies directed<br />
against human protein gene product 9.5. By<br />
this fibre density can be readily quantified, with<br />
reported interobserver agreement as high as<br />
96% 40 .<br />
Lindberger et al 41 has reported that levels of<br />
both substance P and calcitonin gene related<br />
peptide (CGRP) are reduced in skin biopsies<br />
from diabetic patients before clinical or<br />
neurophysiologic evidence of neuropathy. Levy<br />
et al 42 showed that there was a progressive<br />
loss in the number and area innervated by<br />
CGRP positive nerve fibres when normal<br />
subjects were compared with diabetic patients<br />
with clinical evidence of neuropathy.<br />
The combination of skin punch biopsy and<br />
immuno staining with specific antibodies has<br />
the advantage of minimal trauma to the<br />
patient, reliability, quantifiability, and a<br />
demonstrable correlation with clinically defined<br />
disease severity.<br />
The classical skin punch biopsy is more useful<br />
in diabetes because classic insult in diabetic<br />
somatic neuropathy is dying back of axons.<br />
This distal to proximal gradient of axonal<br />
pathology can be better evaluated by<br />
examination of multiple biopsies. <strong>Current</strong>ly,<br />
few centres have direct experience with this<br />
procedure, so available data are less.<br />
2. Quantitative sensory testing (QST) : It<br />
facilitates early diagnosis and accurate<br />
assessment of diabetic neuropathy. In QST,<br />
standardised sensory testing instruments are<br />
used to control and deliver specific stimuli at<br />
designated intensities to test sensory thresholds.<br />
It is defined as the minimum stimulus energy<br />
detectable 50% of the time.<br />
Quantitative sensory testing can be measured<br />
by i) Computer assisted sensory evaluation<br />
(Case IV). ii) Physitemp NTE-2a thermal tester.<br />
iii) Tactile circumferential discriminator.<br />
QST provides a parametric measure of<br />
sensory function that can target axons of<br />
specific fibre diameter. Abnormalities in QST<br />
reflect axonal pathology or alteration in<br />
sensory transduction. The latter effect may<br />
be of interest because recent results show<br />
that abnormalities in distal peptide<br />
neurotransmitter levels may occur in<br />
peripheral nerve fibres of diabetic patients<br />
before axonal loss is detectable 43 . Davis et<br />
al 44 showed that QST of vibratory thresholds<br />
can detect subclinical neuropathy in children<br />
Journal, Indian Academy of Clinical Medicine Vol. 2, No. 4 October-December 2001 311
and adolescents with type 1 diabetes.<br />
However, there are two important problems<br />
in QST, firstly, QST is only a semi-objective<br />
measure, and can be influenced by both<br />
attention and motivation of the patient and<br />
secondly, abnormal results from QST can<br />
result from spinal cord pathology as well as<br />
cortical lesions. Thus, QST though sensitive<br />
for peripheral neuropathy, is not specific for<br />
this condition.<br />
Treatment of diabetic neuropathy<br />
Definitive prevention, treatment, or cure of<br />
diabetic peripheral neuropathies must await the<br />
discovery of the exact aetiology and effective<br />
treatment of diabetes, however, the results of<br />
DCCT and pancreas transplantation studies on<br />
peripheral neuropathy clearly demonstrate that<br />
an effective and early treatment of<br />
hyperglycaemia is currently the only important<br />
factor in delaying the progression of<br />
neuropathy. The asymmetric and focal<br />
neuropathies are either self-limiting or do not<br />
respond to any treatment modality. So treatment<br />
is largely directed towards distal symmetric<br />
sensori-motor polyneuropathies and for<br />
symptoms related to autonomic neuropathy.<br />
The treatment of diabetic neuropathy can be<br />
broadly divided into two major groups : (i)<br />
Symptomatic treatment (ii) Treatment for nerve<br />
regeneration.<br />
Symptomatic treatment<br />
Pain is the most common symptom, which could<br />
be superficial, deep, or aching. The management<br />
of pain is often difficult and disappointing. There<br />
is no single correct approach to the management<br />
of any given patient with peripheral neuropathy.<br />
Often it requires patience on the part of patient<br />
and physician who must try a variety of different<br />
medications on a trial and error basis until a<br />
satisfactory regimen is established. Sometimes<br />
simple reassurance that the pain is not permanent,<br />
does produce great relief from pain, pain related<br />
anxiety, or depression. However, following<br />
measures can be taken in order of preference for<br />
pain relief :<br />
Capsaicin<br />
Superficial hyperaesthesia with burning and<br />
lancinating dysaesthetic pain is typical of c-fibre<br />
pain and may respond to local application of<br />
capsaicin. Capsaicin is trans-8methyl-N vanilly-<br />
6-nonemide 45 . Capsaicin is extracted from chilli<br />
pepper and can be prepared at home by mixing<br />
three teaspoons of cayenne pepper with a jar full<br />
of cold cream. Its topical application results in<br />
depletion of substance P, a principal neurotransmitter<br />
of poly model nociceptive afferent<br />
fibres. The mechanism of substance P depletion<br />
may be secondary to the release of substance P<br />
from nerve terminals, diminished axonal transport<br />
of substance P to replenish it in the nerve terminals,<br />
and inhibition of its synthesis 45 . Capsaicin is<br />
applied at a dose of 0.075%, four times a day to<br />
skin over the painful areas. The reported controlled<br />
studies suggest that the benefits of drug application<br />
become evident only after four weeks of its use.<br />
Analgesics<br />
The analgesics do not have a good reputation in<br />
the management of diabetic neuropathy. On one<br />
end they have poor efficacy and at the other end<br />
they have adverse effects. Long term NSAID<br />
ingestion causes hepatotoxicity, while narcotic<br />
analgesia causes addiction and worsening of<br />
autonomic neuropathic symptoms.<br />
Tricyclic anti-depressants (TCA)<br />
Tricyclic anti-depressants (TCA) are the most<br />
commonly used drugs for pain relief in diabetic<br />
peripheral neuropathy. Double blind trials of<br />
the tricyclic anti-depressants have demonstrated<br />
significant benefits in reducing pain that is<br />
burning, aching, sharp, throbbing, or stinging 46 .<br />
The use of amitriptyline is contraindicated in<br />
patients with heart block, recent myocardial<br />
infarction, heart failure, urinary tract<br />
obstruction, orthostatic hypotension, and<br />
narrow angle glaucoma. It should be started at<br />
312 Journal, Indian Academy of Clinical Medicine Vol. 2, No. 4 October-December 2001
low doses of 10 to 20 mg every night and<br />
increased gradually until pain control is<br />
achieved or dose limiting side effects occur.<br />
Achievement of pain relief may require as much<br />
as 150 mg of the drug per day for 3 to 6 weeks.<br />
Withdrawal from amitriptyline must be gradual<br />
so as to prevent rebound insomnia. These drugs<br />
act on the central nervous system, preventing<br />
the reuptake of norepinephrine and serotonin<br />
at synapses involved in pain inhibition. The<br />
benefits of tricyclics appear to be unrelated to<br />
relief of depression.<br />
Anti-convulsants<br />
Anti-convulsants are used, if treatment with<br />
amitriptyline is not successful. Commonly used<br />
anti-convulsants are carbamazepine,<br />
clonazepam, phenytoin, and gabapentin. The<br />
drugs are more effective in lancinating pain.<br />
Among anti-convulsants, carbamazepine is the<br />
most commonly used drug. When initiating<br />
carbamazepine, it is advisable to begin with a<br />
low dose of 100 mg and then increase gradually<br />
until there is significant relief of symptoms or<br />
side effects are encountered. Complete blood<br />
counts and liver functions should be checked at<br />
the onset and then on a monthly basis over the<br />
first three months because leukopenia is a<br />
common complication.<br />
Gabapentin has demonstrated significant<br />
efficacy in a recent multicentre, double blind,<br />
randomised, placebo-controlled study of 165<br />
patients with type 1 and type 2 diabetes47 .<br />
Common adverse effects are dizziness,<br />
somnolence, and headache. Gabapentin<br />
should be started at a dose of 300 mg/day and<br />
gradually increased until symptomatic relief<br />
occurs or until a maximum dose of 2,400 mg<br />
per day is reached. Clonazepam is also effective<br />
in restless leg syndrome.<br />
Others<br />
Baclofen (Gamma aminobutyric acid), clonidine<br />
(α2 adrenergic agonist), lignocaine, and<br />
tramadol hydrochloride are other drugs used<br />
in management of diabetic peripheral<br />
neuropathy. Non-pharmacological therapies<br />
that have also been tried with limited success<br />
are sympathectomy, spinal cord blockade, and<br />
electrical spinal cord stimulation.<br />
Treatment of autonomic neuropathy<br />
Treatment of autonomic neuropathy is only<br />
palliative. With the help of pharmacological and<br />
non-pharmacological means the quality of life<br />
can be improved in these patients.<br />
Postural hypotension<br />
Mild postural hypotension can be managed with<br />
simple measures such as a high sodium diet,<br />
raising the head end of bed during sleep and<br />
wearing of whole body stockings. The<br />
pharmacological treatments include the use of<br />
mineralo-corticoids like fludrocortisone,<br />
sympathomimetic agents (midodrine, clonidine,<br />
yohimbine), β blockers with or without intrinsic<br />
sympathomimetic activity (propranolol,<br />
pindolol), pressor agents (dihydroergotamine,<br />
caffeine), prostaglandin synthesis inhibitors<br />
(indomethacin, ibuprofen, naproxen) and antiserotonergic<br />
agents 48 . Therapy should be<br />
initiated with fludrocortisone (0.1 to 0.5 mg) 6<br />
hourly. A pressor sympathomimetic agent, or a<br />
prostaglandin synthetase inhibitor can be added<br />
to the drug regimen of those patients who<br />
remain symptomatic. Refractory symptoms may<br />
require a combination of above mentioned<br />
agents.<br />
Gastrointestinal problems (oesophageal<br />
dysmotility/gastroparesis and enteropathy)<br />
Autonomic damage to the upper gastointestinal<br />
tract is often asymptomatic. Oesophageal motility<br />
is sometimes reduced, causing dysphagia and<br />
heart burn. Gastroparesis, with delayed and<br />
uncoordinated emptying of the stomach can lead<br />
to abdominal discomfort, intractable vomiting,<br />
weight loss, and unstable diabetic control.<br />
Journal, Indian Academy of Clinical Medicine Vol. 2, No. 4 October-December 2001 313
Management of diabetic gastroparesis consists of<br />
multiple small feedings, reduction in dietary fat,<br />
good glycaemic control, and prokinetic drugs. The<br />
prokinetic drugs used for the management of<br />
gastroparesis are metoclopramide (10-20 mg 6<br />
hourly), domperidone (10-20 mg 4-6 hourly),<br />
cisapride (10 mg 8 hourly), and erythromycin (250<br />
mg 8 hourly). All are given 1/2 hours before meal.<br />
In patients who are unable to tolerate oral<br />
medication, metoclopramide or erythromycin can<br />
be given intravenously. In case of severe<br />
gastroparesis, patients may require hospitalisation,<br />
intravenous fluids, parental drugs, and nasogastric<br />
drainage; sometime they may require intra-jejunal<br />
feeding.<br />
Enteropathy includes both diarrhoea and<br />
constipation. The pathogenesis of diabetic<br />
diarrhoea includes abnormalities in gastrointestinal<br />
motility, decreased gut transit time,<br />
reduced fluid absorption, bacterial overgrowth,<br />
pancreatic insufficiency, coexistent coeliac disease,<br />
and abnormalities in bile salt metabolism. The<br />
pathophysiology of diabetic constipation is poorly<br />
understood but may reflect loss of post-prandial<br />
gastrocolic reflex 49 .<br />
Loperamide, diphenoxylate, or codeine<br />
phosphate are used for symptomatic treatment<br />
of diabetic diarrhoea, while clonidine is used<br />
to reduce α2 adrenergic receptor mediated<br />
intestinal absorption. A short course of broad<br />
spectrum antibiotics (ampicillin, tetracycline) is<br />
helpful for diarrhoea due to bacterial overgrowth.<br />
Cystopathy<br />
Patients with neurogenic bladder may not be able<br />
to sense bladder fullness. The patients should be<br />
instructed to palpate their bladder. The bladder<br />
may be emptied by mechanical measures such as<br />
manual suprapubic pressure (Crede’s maneuver)<br />
or intermittent self catheterisation. Parasympathomimetic<br />
agents such as bethanechol are some<br />
times helpful but often do not help to fully empty<br />
the bladder. While extended sphincter relaxation<br />
can be achieved with an α1 blocker such as<br />
doxazosin. If pharmacological measures fail,<br />
bladder neck surgery (in males) may help to relieve<br />
spasm of the internal sphincter.<br />
Sexual dysfunction in males can be managed with<br />
intrapenile injection of papaverine and by vacuum<br />
devices. If these therapies do not help, rigid or<br />
semirigid prostheses are available. The drug<br />
sildenafil citrate is now being increasingly used to<br />
manage erectile dysfunction. Being a potent<br />
inhibitor of cyclic guanosine monophosphate<br />
hydrolysis in the corpus covernosum, it therefore<br />
increases the penile response to sexual stimulation.<br />
One randomised, double-blind, flexible-dose,<br />
placebo-controlled study included only patients<br />
with erectile dysfunction attributed to complications<br />
of diabetes mellitus (n = 268). Patients were<br />
started on 50 mg and allowed to adjust the dose<br />
upto 100 mg or down to 25 mg of sildenafil. There<br />
were highly statistically significant improvements<br />
(in frequency of successful penetration during<br />
sexual activity and maintenance of erections after<br />
penetration) on sildenafil compared to placebo.<br />
Table III : Tests of cardiac autonomic function.<br />
Test<br />
Parasympathetic (heart rate response)<br />
Normal Borderline Abnormal<br />
Valsalva (Valsalva ratio) ≥ 1.21 1.11-1.20 ≤ 1.10<br />
Deep breathing (max/min HR) ≥ 15 beat/min 11-14 beast/min ≤ 10 beats/min<br />
Standing (30:15 ratio R-R) ≥ 1.04 1.01-1.03 ≤ 1.00<br />
Sympathetic (blood pressure response)<br />
Standing (↓ systolic) ≤10 mm Hg 11-29 mm Hg ≥ 30 mm Hg<br />
Exercise (↑ diastolic) ≥16 mm Hg 11-15 mm Hg ≤ 10 mm Hg<br />
314 Journal, Indian Academy of Clinical Medicine Vol. 2, No. 4 October-December 2001
57% of sildenafil patients reported improved<br />
erections versus 10% on placebo. Diary data<br />
indicated that on sildenafil, 48% of intercourse<br />
attempts were successful versus 12% on placebo.<br />
Treatment designed to modify the course of<br />
diabetes<br />
The outcome of management of diabetic<br />
peripheral neuropathy is not very good. However,<br />
people are trying to prevent neuropathy from<br />
developing (primary prevention) and to improve<br />
or even reverse established neuropathic damage<br />
(secondary prevention). For prevention, optimum<br />
glycaemic control is most important. The aldose<br />
reductase inhibitors, essential fatty acids, and<br />
vasodilator drugs are approaching clinical<br />
usefulness – while the rest are at an experimental<br />
stage.<br />
Optimised glycaemic control<br />
The DCCT and the UKPDS, both landmark studies<br />
in the history of diabetes, have shown that good<br />
control can prevent or delay the onset of diabetic<br />
peripheral neuropathy. The effectiveness of<br />
normoglycaemia in improving damaged nerves<br />
has been documented in some patients who have<br />
undergone combined pancreatic and renal<br />
transplantation 50 .<br />
Aldose reductase inhibitors (ARI)<br />
The aldose reductase inhibitors prevent conversion<br />
of glucose to sorbitol in presence of<br />
hyperglycaemia, Therefore, it prevents the polyol<br />
pathway cascade. ARIs are alreastat, tolerestat,<br />
epalrestat, sorbinil, and zopolrestat. There is great<br />
controversy about the mechanisms of action of<br />
the ARIs, and suggestions range from altered<br />
phosphoinositide metabolism and Na + - K +<br />
adenosine triphosphate activity, through reduced<br />
glutathione levels, to vasodilation and improved<br />
blood flow to nerve 51 . However, as compared to<br />
the marked effect of ARIs on nerve function in<br />
diabetic animals, the results of clinical trials in<br />
humans have been less convincing 52 . The results<br />
of more than 20 clinical trials conducted in past<br />
15-20 years on the effect of a variety of aldose<br />
Fig. 2 :<br />
reductase inhibitors generally have been<br />
disappointing 53 .<br />
Gamma linolenic acid (GLA)<br />
Gamma linolenic acid (GLA) is an important<br />
constituent of neuronal membrane phospholipids<br />
as well as a substrate for prostaglandin E and<br />
prostacyclin formation, which may be important<br />
for preservation of nerve blood flow. In diabetic<br />
patients, conversion of linolenic acid to GLA and<br />
subsequent metabolism is impaired, possibly<br />
contributing to the pathogenesis of diabetic<br />
neuropathy. A recent trial used GLA for one year<br />
and this resulted in significant improvements in<br />
both clinical measures as well as electrophysiologic<br />
test results 54 .<br />
Other measures like advanced glycation end<br />
products (AGE), N-acetyl-L-carnitine, gangliosides,<br />
and human intravenous immunoglobulin are still<br />
under trial.<br />
Treatment for nerve regeneration<br />
The agents used for nerve regeneration are<br />
known as neurotrophic factors. The<br />
neurotrophic factor is defined as a naturally<br />
occurring protein that is released by target<br />
tissues of responsive neurons, binds to specific<br />
receptors and is retrogradely transported to the<br />
Journal, Indian Academy of Clinical Medicine Vol. 2, No. 4 October-December 2001 315
cell body where it regulates gene expression<br />
through the actions of second messenger<br />
systems 55 .<br />
A large number of neurotrophic factors that<br />
exert effects on specific neuronal populations<br />
in the peripheral nervous system have been<br />
discovered. Some of these factors may prove<br />
useful for the treatment of diabetic peripheral<br />
neurophathy. All neurotrophic factors are still<br />
under trial and none of them is available for<br />
clinical use. Among the most promising are<br />
members of the neurotrophin gene familynerve<br />
growth factor (NGF), brain derived<br />
neurotrophic factors, neurotrophin, insulin<br />
like growth factor, and glial cell derived<br />
neurotrophic factor (Table IV).<br />
Table IV : Neurotrophic factors.<br />
Neurotrophins (NT)<br />
Nerve growth factor<br />
Brain- derived neurotrophic factor<br />
NT - 3<br />
NT-4/5<br />
NT - 6<br />
Haematopoietic cytokines<br />
Ciliary neurotrophic factor<br />
LIF<br />
Oncogene M<br />
Interleukin (IL) - 1<br />
IL - 3<br />
IL - 6<br />
IL - 7<br />
IL - 9<br />
IL - 11<br />
Granulocyte colony- stimulating factor<br />
Insulin - like growth factors (IGF)<br />
Insulin<br />
IGF - I<br />
IGF - II<br />
Heparin - binding family<br />
Acdic fibroblast growth factor (FGF)<br />
Basic FGF<br />
int - 2 onc<br />
hst/k-fgf onc<br />
FGF - 4<br />
FGF - 5<br />
FGF - 6<br />
Keratinocyte growth factor<br />
Epidermal growth factor (EGF) family<br />
EGF<br />
Transforming growth factor (TGF) - α<br />
TGF - β family<br />
TGF - β 1<br />
TGF - β 2<br />
TGF - β 3<br />
Glial - derived neurotrophic factor<br />
Neurturin<br />
Persephin<br />
Activin A<br />
BMP S<br />
Tyrosine kinase - associated cytokines<br />
Platelet - derived growth factor<br />
Colony - stimulating factor - 1<br />
Stem cell factor<br />
BMP = bone morphogenetic protein; LIF = leukaemia<br />
inhibitory factor.<br />
References<br />
1. Apfel SC. Introduction to diabetic neuropathy. Am J Med<br />
1999; 107 (Suppl): 1S-8S.<br />
2. Harati Y. Diabetes and the nervous system. Endo Metab<br />
Clin North Am 1996; 25: 325-59.<br />
3. Boulton AJM, Malik RA. <strong>Diabetic</strong> neuropathy. Med Clin<br />
North Am 1998; 82: 909-29.<br />
4. Pirat J. Diabetes mellitus and its degenrative<br />
complications : a prospective study of 4400 patients<br />
observed between 1947 and 1973. Diabetes Care 1978;<br />
1: 168-88.<br />
5. Boulton AJM, Ward JD. <strong>Diabetic</strong> neuropathies and pain.<br />
Clin Endocrinol Metab 1986; 16: 917-31.<br />
6. Thomas PK. Metabolic neuropathy. Jr Coll Physicians Lond<br />
1973; 7:154-60.<br />
7. Boulton AJM, Amstrong WD, Scarpello JHB, Ward JD.<br />
The natural history of painful diabetic neuropathy : A 4<br />
years study. Postgraduate Med J 1983; 59: 556-9.<br />
8. Thomes PK. Classification, differential diagnosis and<br />
staging of diabetic peripheral neurophathy. Diabetes<br />
1997; 46 (suppl-2): 54S-57S.<br />
9. Toyry JP, Niskaner LK, Mantysaari MJ et al. Occurrence<br />
predictors and clinical significance of autonomic<br />
neuropathy in NIDDM: Ten years follow up from<br />
diagnosis. Diabetes 1996; 45: 308-15.<br />
10. Watkins PJ, Edmonds ME. Clinical features of diabetic<br />
neuropathy. In Pickup J, Williams G (eds): Text Book of<br />
Diabetes 2nd edition, Blackwell Science 1997.<br />
11. Barohn RJ, Sahenk Z, Warmolts JR et al. The Bruns-<br />
Garland syndrome (diabetic amyotrophy). Arch Neuro<br />
1990; 48: 1130.<br />
316 Journal, Indian Academy of Clinical Medicine Vol. 2, No. 4 October-December 2001
12. Pourmand R. <strong>Diabetic</strong> neuropathy. Neurol Clin 1997; 15:<br />
569-76.<br />
13. Boulton AJM, Augur E, Ayyer DR et al. <strong>Diabetic</strong> thoracic<br />
polyradiculopathy presenting as an abdominal swelling.<br />
BMJ 1984; 289: 798-9.<br />
14. Greene DA, Sima AAF, Stevens MJ et al. Complications:<br />
<strong>Neuropathy</strong>, pathogenetic consideration. Diabetes Care<br />
1992; 15: 1902-25.<br />
15. Feldman EL, Stevens MJ, Greene DA. Pathogenesis of<br />
diabetic neuropathy. Clin Neuro Sci 1997; 4: 365-70.<br />
16. Sharma AK, Thomas PK. Animal Models : Pathology and<br />
pathophysiology. In Dyck PJ Thomas PK, Asbely AK et al<br />
(eds): <strong>Diabetic</strong> <strong>Neuropathy</strong>. Philadalphia, WB Saunders<br />
1987; p 237.<br />
17. Diabetes Control and Complications Trial (DCCT)<br />
Research Group. The effect of intensive treatment of<br />
diabetes on the development and progression of long<br />
term complication in insulin dependent diabetes mellitus.<br />
N Engl J Med 1993; 329: 977-86.<br />
18. DCCT Research Group. The effect of intensive diabetes<br />
therapy on the development and progression of<br />
neuropathy. Ann Intern Med 1995; 122: 561-88.<br />
19. Tornlinson DR. Polyols and myointositol in diabetic<br />
neuropathy of mice and men. Mayo Clin Proc 1989;<br />
64: 1030.<br />
20. Winegrade Al. Does a common mechanism induce the<br />
diverse complications of diabetes? Diabetes 1987; 36:<br />
396-406.<br />
21. Cameron NE, Cotter MA. The relationship of vascular<br />
changes to metabolic factors in diabetes mellitus and<br />
their role in the development of peripheral nerve<br />
complications. Diabetes Metab Res 1994; 10: 189-224.<br />
22. Thomas PK, Tomlinson DR. <strong>Diabetic</strong> and hypoglycemic<br />
neuropathy. In Dyck PJ, Thomas PK, Griffin JW et al (eds):<br />
Peripheral <strong>Neuropathy</strong>, Philidelphia, WB Saunders, 1993.<br />
23. Calcutt NA, Tomlinson DR, Biswas S. Co-existence of<br />
nerve conduction deficit with increased Na + /K + - ATPase<br />
activity in galactose fed mice. Diabetes 1990; 39: 663.<br />
24. Dyck PJ, Zimmerman RB, Vilen TH et al. Nerve glucose<br />
fructose, sorbitol, myoinositol and fiber degeneration and<br />
regenration in diabetic neuropathy. N Engl J Med 1988;<br />
319: 542-8.<br />
25. Sima AAF, Bril V, Nathanial V et al. Regeneratin and repair<br />
of myelinated fibres in sural nerve biopsies from patients<br />
with diabetic neuropathy treated with Sorbinil an<br />
investigational aldose reductase inhibitor. N Engl J Med<br />
1988; 319-548.<br />
26. Dolnofer R, Renner R, Wieland OH. Different behaviour<br />
of haemoglobin A and glycosylated albumin levels<br />
1C<br />
during recovery from diabetic ketoacidosis and non<br />
acidotic coma. Diabetologia 1981; 21: 211-5.<br />
27. Monnier VM, Vishwanath V, Frank KE et al. Relation<br />
between complication of type 1 diabetes mellitus and<br />
collagen linked fluroscence. N Engl J Med 1986; 314:<br />
403-8.<br />
28. Vlassara H, Brownlee M, Cerami A. Excessive non<br />
enzymatic glycosylation of peripheral and central nervous<br />
system myelin components in diabetic rats. Diabetes<br />
1983; 32: 670-4.<br />
29. Ryle C, Donaghy M. Glycation of peripheral nerve<br />
proteins in diabetes mellitus. J Neurol Sci 1995; 129:<br />
62-8.<br />
30. Vlassara H. Receptor mediated interactions of advanced<br />
glycosylated end products with cellular components<br />
within diabetic tissues. Diabetes 1992; 41: 52-6.<br />
31. Gingliano D, Ceriello A, Pawlisso G. Oxidalive stress<br />
and diabetic vascular complications. Diabetes Care<br />
1996; 19: 257-67.<br />
32. Jamal GA, Carmichael H. The effect of gamma linolenic<br />
acid on human diabetic peripheral neuropathy : a doulde<br />
blind placebocontrolled trial. Diabet Med 1990; 7: 319-<br />
23.<br />
33. Britland ST, Yound RJ, sharma AK, Clarke BF. Relationship<br />
of undo neural capillary abnormalities to type and severity<br />
of diabetic polyneuropathy. Diabetes 1990; 39; 909-<br />
13.<br />
34. Faradji V, Sotelo J. Low serum levels of nerve growth<br />
factor in diabetic neuropathy. Acta Neurol Scand 1990;<br />
81: 402-13.<br />
35. Vinik AL, Suwanwalaikorns, Stansberry KB et al.<br />
Quantitative measurement of cutaneous perception in<br />
diabetic neuropathy. Muscle Nerve 1995; 18: 574-84.<br />
36. Ewing DJ, Martyn CN, Young RJ, Clrve BF. The value of<br />
cardio vascular autonomic function tests : 10 years<br />
experience in diabetes. Diabetes Care 1985; 8: 491-8.<br />
37. Hyllienmark L, Bresman T, Ludvigsson J. Subclinical nerve<br />
dysfunction in children and adolescents with IDDM.<br />
Diabetologia 1995; 38: 685-92.<br />
38. Holland NR, Stocks A, Hauer P et al. Intra epidermal<br />
nerve fibre density in patients with painful sensory<br />
neuropathy. Neurology 1997; 48: 708-11.<br />
39. McCarthy BG, Hsieh ST, Stocks A et al. Cutaneous<br />
innervation in sensory neuropathies : evaluation by skin<br />
biopsy. Neurology 1995; 45: 1848-55.<br />
40. Holland NR, Crawfod TQ, Hauer P et al. Small fiber<br />
sensory neuropathies: clinical course and<br />
neuropathology of idiopathic cases. Ann Neurol 1998;<br />
44: 47-59.<br />
41. Lindberger M, Schroder HD, Schultzberg M et al. Nerve<br />
fiber studies in skin biopsies in peripheral neurophathies<br />
: Immunohistochemical analysis of neuropeptides in<br />
diabetes mellitus. J Neurol Sci 1989; 93: 289-96.<br />
42. Levy DM, Terenghi G, Gu X-H et al. Immunohistochemical<br />
measurements of nerves and neuropeptides in diabetic<br />
skin : relationship to tests of neurological function.<br />
Diabetologia 1992; 35: 889-97.<br />
43. Wallengren J, Badendick K, Sundler F et al. Innervation<br />
of the skin of the fore arm in diabetic patients : relation<br />
to nerve function. Acta Dermato-Venereoligica 1995; 75:<br />
37-42.<br />
Journal, Indian Academy of Clinical Medicine Vol. 2, No. 4 October-December 2001 317
44. Davis EA, Walsh P, Jones TW, Byrne GC. The use of<br />
biothesiometry to detect neuropathy in children and<br />
adolescents with IDDM. Diabetes Care 1997; 20:1448-<br />
53.<br />
45. Tanden R, Lewis GA, Krusinski PB. Topical capsaicin in<br />
painful diabetic neuropathy. Diabetes Care 1992; 8-15.<br />
46. Max MB, Culnane M, Schafer SC et al. Amitryptiline<br />
relieves diabetic neuropathy pain in patients with normal<br />
or depressed mood. Neurology 1987; 37: 589.<br />
47. Rosenberg JM, Harrell C, Risitic H et al. The effect of<br />
gabapentine on neuropathic pain. Clin J Pain 1997; 13:<br />
251-5.<br />
48. Onrot J, Goldberg MR, Hollister AS et al. Management<br />
of chronic orthostatic hypotension. Am J Med 1986; 80:<br />
454-64.<br />
49. Feldman M, Corbett DB, Tamsey EJ et al. Abnormal<br />
gastric function in long-standing insulin dependent<br />
diabetic patients. Gastroenterology 1979; 43: 65-75.<br />
50. Solders G, Tyden G, Persson A, Groth C-G. Improvement<br />
of nerve conduction in diabetic neuropathy. A follow up<br />
study 4 years after combined pancreatic and renal<br />
transplantation. Diabetes 1992; 41: 946-51.<br />
51. Cameron NE, Cotter MA. Potential therapeutic<br />
approaches to the treatment and prevention of diabetic<br />
neuropathy : Evidence from experimental studies. Diabet<br />
Med 1993; 10: 593-605.<br />
52. Tomlinson DR. Aldose reductase inhibitors and the<br />
complications of diabetes. Diabet Med 1993; 10: 214-<br />
30.<br />
53. Hariti Y. <strong>Diabetic</strong> peripheral neuropathies. Ann Intern<br />
Med 1987; 107: 546.<br />
54. Keen H, Paxan J, Allawi J et al. Treatment of diabetic<br />
neuropathy with gamma - linoleic acid. Diabetes Care.<br />
1993; 16: 8-15.<br />
55. Apfel SC. Neurotrophic factors in the therapy of diabetic<br />
neuropathy. Am J Med 1999; 107 (suppl): 34S-42S.<br />
318 Journal, Indian Academy of Clinical Medicine Vol. 2, No. 4 October-December 2001