Geriatric Anesthesiology - The Global Regional Anesthesia Website
Geriatric Anesthesiology - The Global Regional Anesthesia Website
Geriatric Anesthesiology - The Global Regional Anesthesia Website
Create successful ePaper yourself
Turn your PDF publications into a flip-book with our unique Google optimized e-Paper software.
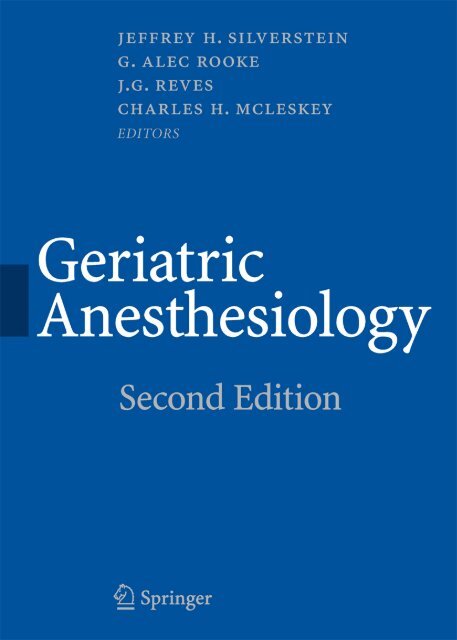
<strong>Geriatric</strong> <strong>Anesthesiology</strong><br />
Second Edition
<strong>Geriatric</strong><br />
<strong>Anesthesiology</strong><br />
Second Edition<br />
Jeffrey H. Silverstein<br />
G. Alec Rooke<br />
J.G. Reves<br />
Charles H. McLeskey<br />
Editors
Jeffrey H. Silverstein, MD<br />
Professor<br />
Department of <strong>Anesthesiology</strong>, Surgery,<br />
and <strong>Geriatric</strong>s and Adult Development<br />
Vice Chairman for Research<br />
Associate Dean for Research<br />
Mount Sinai School of Medicine<br />
New York, NY, USA<br />
J.G. Reves, MD<br />
Vice President for Medical Affairs<br />
Dean, College of Medicine<br />
Department of <strong>Anesthesiology</strong>/College<br />
of Medicine<br />
Medical University of South Carolina<br />
Charleston, SC, USA<br />
G. Alec Rooke, MD, PhD<br />
Professor<br />
Department of <strong>Anesthesiology</strong><br />
University of Washington and the Veterans<br />
Affairs Puget Sound Health Care System<br />
Seattle, WA<br />
and<br />
Visiting Professor of <strong>Anesthesia</strong>, Critical<br />
Care, and Pain Medicine<br />
Harvard Medical School<br />
Beth Israel Deaconess Medical Center<br />
Boston, MA, USA<br />
Charles H. McLeskey, MD<br />
Salt Lake City, UT, USA<br />
Library of Congress Control Number: 2007926756<br />
ISBN: 978-0-387-72526-0 e-ISBN: 978-0-387-72527-7<br />
Printed on acid-free paper.<br />
© 2008 Springer Science+Business Media, LLC.<br />
All rights reserved. This work may not be translated or copied in whole or in part without the written<br />
permission of the publisher (Springer Science+Business Media, LLC, 233 Spring Street, New York, NY<br />
10013, USA), except for brief excerpts in connection with reviews or scholarly analysis. Use in connection<br />
with any form of information storage and retrieval, electronic adaptation, computer software, or by<br />
similar or dissimilar methodology now known or hereafter developed is forbidden.<br />
<strong>The</strong> use in this publication of trade names, trademarks, service marks, and similar terms, even if they are<br />
not identified as such, is not to be taken as an expression of opinion as to whether or not they are subject<br />
to proprietary rights.<br />
While the advice and information in this book are believed to be true and accurate at the date of going<br />
to press, neither the authors nor the editors nor the publisher can accept any legal responsibility for any<br />
errors or omissions that may be made. <strong>The</strong> publisher makes no warranty, express or implied, with respect<br />
to the material contained herein.<br />
9 8 7 6 5 4 3 2 1<br />
springer.com
To my Grandparents, Regina and David Silverstein and Blanche and Daniel<br />
Klein, MD. <strong>The</strong>ir love and their sufferings provided endless opportunities and<br />
insights. I hope, and believe, they would have liked this result.<br />
—JHS<br />
To my Children, Douglas and Linnea.<br />
—GAR<br />
To Margaret Cathcart and her late Husband, Dr. John W. Cathcart.<br />
—JGR<br />
To my Parents, Marion and Hamilton McLeskey, who encouraged care and<br />
consideration for our elderly.<br />
—CHM
Preface to the Second Edition<br />
Do not go gentle into that good night,<br />
Old age should burn and rave at close of day;<br />
Rage, rage against the dying of the light.<br />
Dylan Thomas<br />
<strong>The</strong> goal of getting older is to age successfully. Unfortunately, the majority of our<br />
older patients will have acquired one or more chronic medical conditions as they<br />
age, and, even if a perfectly healthy older patient presents for surgery, that patient’s<br />
ability to handle physiologic stress will be diminished, including the stress of surgery.<br />
Nearly half of all surgical procedures involve patients older than age 65, and that<br />
percentage is likely to increase as the U.S. population ages. Thus, the perioperative<br />
care of the older patient represents one of the primary future frontiers of anesthetic<br />
practice. Even though perioperative mortality has diminished for the elderly, as well<br />
as for the population in general, the growing number of cases spotlights perioperative<br />
morbidity and mortality as an important issue for patients and health care<br />
systems alike. <strong>The</strong> vision set forward by the first edition (i.e., to apply the growing<br />
body of knowledge in this subspecialty area to the everyday practice of anesthesiology)<br />
remains the mission and vision of this second edition. <strong>The</strong> editors believe that<br />
the updated contents of this edition represent an important opportunity to consolidate<br />
and organize the information that has been acquired since 1997 and to apply<br />
that knowledge to the current practice of anesthesiology.<br />
Part I contains several new chapters on topics that may not always seem to be<br />
directly involved with anesthetic care, but are important to the future of medical<br />
and anesthesia care. An understanding of the aging process may lead to methods of<br />
slowing its progression, or at least of ameliorating some of its consequences, including<br />
the development of chronic disease. Most anesthesiology residency programs<br />
provide limited formal teaching of geriatric anesthesia. <strong>The</strong> editors believe the<br />
incorporation of relevant subspecialty material in the anesthesiology curriculum is<br />
needed to improve care for this patient population. <strong>The</strong> realities of reimbursement<br />
for services rendered to the older patient, either by Medicare or other payers,<br />
warrant the attention of all anesthesiologists who provide care for older patients.<br />
Ethics as applied to treatment of the older patient is also addressed. <strong>The</strong> medical<br />
management of this population is often complicated by issues such as patient goals<br />
that differ from physician expectations, physician “ageism,” patient cognitive impairment,<br />
and the physician’s failure to recognize the true risk of surgery and attendant<br />
recovery time. <strong>The</strong> last chapter of Part I reviews current knowledge and suggests<br />
research areas where the greatest impact on patient outcomes might be realized.<br />
Parts II and III review the physiology of aging and the basic anesthetic management<br />
of the geriatric patient, and Part IV examines selected surgical procedures<br />
vii
viii<br />
Preface to the Second Edition<br />
frequently performed in older patients. Not all of these chapters are specific to<br />
anesthetic management. <strong>Geriatric</strong> medicine is a broad field with many relevant<br />
topics. Wound healing is a perfect example. <strong>The</strong> reality is that anesthesiologists can<br />
likely have a positive impact on patient care by being better able to recognize conditions<br />
that may compromise skin when other medical professionals may fail to and,<br />
as a result, can improve protection of the skin, especially during long operating room<br />
cases. In contrast, polypharmacy and drug interactions, major topics in geriatric<br />
medicine, have direct relevance to anesthetic management. <strong>The</strong> cardiac surgery<br />
chapter is an example of how age affects outcomes after a specific type of surgical<br />
procedure. <strong>The</strong> unusual aspects of anesthetic management for cardiac surgery<br />
revolve mostly around the patient’s underlying disease status rather than there<br />
being anything specific to cardiac anesthesia in the older patient beyond the principles<br />
delineated in Parts II and III.<br />
For chapters similar to those in the first edition, an effort has been made to update<br />
content and incorporate studies that examine outcome. Such work helps us challenge<br />
conventional wisdom and sometimes test novel ideas that prove beneficial.<br />
Even the most casual reader of this textbook will recognize huge gaps in our present<br />
knowledge. It is not sufficient, for example, to take an understanding of the physiology<br />
of aging and draw conclusions regarding anesthetic management from that<br />
information. Oftentimes, however, we are forced to do just that when making anesthetic<br />
management decisions. <strong>The</strong> editors hope the future will provide better research<br />
and answers that advance the field of geriatric anesthesiology.<br />
<strong>The</strong> editors thank the many authors of this text. In addition to their hard work,<br />
they responded to entreaties for revisions and updates with admirable patience and<br />
promptness. <strong>The</strong>ir contributions expand our knowledge and will improve the care<br />
of elderly patients.<br />
Lastly, the editors thank Stacy Hague and Elizabeth Corra from Springer. Without<br />
their vision and determination, this book would not exist.<br />
Jeffrey H. Silverstein, MD<br />
G. Alec Rooke, MD, PhD<br />
J.G. Reves, MD<br />
Charles H. McLeskey, MD
Preface to the First Edition<br />
Approximately 14% of the current U.S. population is 65 years of age or older. By<br />
the year 2020, it is predicted that 20% or 60,000,000 Americans will reach this milestone.<br />
Further, if today’s statistics continue unchanged, at least half of these individuals<br />
will undergo anesthesia and surgery, likely of increasing complexity, prior to<br />
their eventual demise. <strong>The</strong> geriatric patient population represents a huge and<br />
growing challenge for anesthesia providers the world over.<br />
My interest in the anesthetic management of geriatric patients was kindled 15<br />
years ago while on the faculty at Bowman Gray. One of our surgeons asked me to<br />
anesthetize his healthy 72-year-old father. All went well in the intraoperative and<br />
postoperative periods and he was discharged home in the customary time frame.<br />
However, my colleague later reported that he had observed subtle psychomotor<br />
changes in his father which persisted postoperatively for 7 weeks. It dawned on me<br />
that perhaps the geriatric patient is not simply an older adult, but rather, a truly<br />
different physiologic entity. What could explain the relatively commonly observed<br />
delayed postoperative return of normal mentation in the geriatric surgical patient?<br />
It is this and other unanswered questions regarding the anesthetic management of<br />
the elderly that stimulated the development of this text.<br />
<strong>Geriatric</strong> <strong>Anesthesiology</strong> is designed to be a comprehensive text that methodically<br />
addresses the aging process while emphasizing important clinical anesthetic considerations.<br />
<strong>The</strong> first two sections of the text define the demographics of our aging population<br />
and describe age-related physiologic changes that occur in each major organ<br />
system. <strong>The</strong> third section addresses the multitude of factors that contribute to a safe<br />
and successful anesthetic with suggested adjustments in technique that may improve<br />
anesthetic management of the elderly. Topics range from preoperative evaluation and<br />
risk assessment to the altered effects of various classes of drugs with further discussion<br />
regarding positioning, thermoregulation, perioperative monitoring, and postoperative<br />
recovery. In addition, issues such as management of pain syndromes, outpatient<br />
anesthesia, medicolegal implications, and even special CPR techniques in this age<br />
group are considered. <strong>The</strong> fourth section identifies the ten most commonly performed<br />
surgical procedures in the elderly, and for each, offers recommended anesthetic<br />
techniques. <strong>The</strong> text ends with an intriguing exploration into future research opportunities<br />
in the field, including molecular mechanisms of aging.<br />
Considerable energy has gone into the creation of this text. I am grateful for<br />
the significant efforts made by all the contributing authors and especially appreciate<br />
contributions made by the editors from Williams & Wilkins. <strong>The</strong> text would<br />
have been impossible to complete without the encouragement, dogged determination,<br />
and professionalism of Ms. Tanya Lazar and Mr. Carroll Cann. Tim Grayson<br />
was innovative and supportive during the original design and formulation of<br />
this project.<br />
ix
x<br />
Preface to the First Edition<br />
I am optimistic that this text will heighten the awareness of the very real clinical<br />
differences presented by the geriatric patient population. Perhaps by referring to<br />
appropriate sections in this text, anesthesia providers will be armed with a better<br />
understanding of the physiologic changes of aging and the recommended considerations<br />
and modifications of anesthetic technique, which we hope will contribute to<br />
an ever-improving outcome for the geriatric surgical patient population.<br />
Charles H. McLeskey, MD
Contents<br />
Preface to the Second Edition . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . .<br />
Preface to the First Edition . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . .<br />
Contributors . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . .<br />
vii<br />
ix<br />
xiii<br />
Part I Introduction to Clinical <strong>Geriatric</strong>s<br />
1 <strong>The</strong> Practice of <strong>Geriatric</strong> <strong>Anesthesia</strong> . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 3<br />
Jeffrey H. Silverstein<br />
2 Demographics and Economics of <strong>Geriatric</strong> Patient Care . . . . . . . . . . . . 15<br />
Maria F. Galati and Roger D. London<br />
3 <strong>The</strong>ories of Aging . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 29<br />
Stanley Muravchick<br />
4 Ethical Management of the Elderly Patient . . . . . . . . . . . . . . . . . . . . . . . 38<br />
Paul J. Hoehner<br />
5 Teaching <strong>Geriatric</strong> <strong>Anesthesiology</strong> to Practitioners, Residents,<br />
and Medical Students . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 58<br />
Sheila J. Ellis<br />
6 Research Priorities in <strong>Geriatric</strong> <strong>Anesthesiology</strong> . . . . . . . . . . . . . . . . . . . 66<br />
Christopher J. Jankowski and David J. Cook<br />
Part II Cardinal Manifestations of Aging and Disease in the Elderly<br />
7 Alterations in Metabolic Functions and Electrolytes . . . . . . . . . . . . . . . 97<br />
Michael C. Lewis<br />
8 Perioperative <strong>The</strong>rmoregulation . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 107<br />
Daniel I. Sessler<br />
9 Postoperative Central Nervous System Dysfunction . . . . . . . . . . . . . . . . 123<br />
Deborah J. Culley, Terri G. Monk, and Gregory Crosby<br />
10 Alterations in Circulatory Function . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 137<br />
Thomas J. Ebert and G. Alec Rooke<br />
11 <strong>The</strong> Aging Respiratory System: Anesthetic Strategies to<br />
Minimize Perioperative Pulmonary Complications . . . . . . . . . . . . . . . . . 149<br />
Rodrigo Cartin-Ceba, Juraj Sprung, Ognjen Gajic, and<br />
David O. Warner<br />
xi
xii<br />
Contents<br />
12 Operative Debridements of Chronic Wounds . . . . . . . . . . . . . . . . . . . . . 165<br />
Andrew M. Hanflik, Michael S. Golinko, Melissa Doft,<br />
Charles Cain, Anna Flattau, and Harold Brem<br />
Part III Anesthetic Management of the Aged Surgical Candidate<br />
13 Preoperative Risk Stratification and Methods to Reduce Risk . . . . . . . 181<br />
Linda L. Liu and Jacqueline M. Leung<br />
14 Anesthetic Implications of Chronic Medications . . . . . . . . . . . . . . . . . . . 197<br />
Tamas A. Szabo and R. David Warters<br />
15 <strong>The</strong> Pharmacology of Opioids . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 209<br />
Steven L. Shafer and Pamela Flood<br />
16 Intravenous Hypnotic Anesthetics . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 229<br />
Matthew D. McEvoy and J.G. Reves<br />
17 Inhalational Anesthetics . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 246<br />
Gary R. Haynes<br />
18 Relaxants and <strong>The</strong>ir Reversal Agents . . . . . . . . . . . . . . . . . . . . . . . . . . . . 266<br />
Cynthia A. Lien and Takahiro Suzuki<br />
19 Management of <strong>Regional</strong> <strong>Anesthesia</strong> . . . . . . . . . . . . . . . . . . . . . . . . . . . . 278<br />
Bernadette Veering<br />
20 Fluid Management . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 293<br />
Jessica Miller, Lee A. Fleisher, and Jeffrey L. Carson<br />
21 Pain Management . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 308<br />
Jack M. Berger<br />
22 <strong>Anesthesia</strong> Considerations for <strong>Geriatric</strong> Outpatients . . . . . . . . . . . . . . . 322<br />
Kathryn E. McGoldrick<br />
Part IV <strong>Anesthesia</strong> for Common Surgical Procedures in the Aged<br />
23 Sedation and Monitoring . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 341<br />
Sheila R. Barnett<br />
24 Total Hip Replacement, Joint Replacement, and Hip Fracture . . . . . . 355<br />
Idit Matot and Shaul Beyth<br />
25 Transurethral Prostatectomy Syndrome and Other Complications<br />
of Urologic Procedures . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 368<br />
Daniel M. Gainsburg<br />
26 Thoracic Procedures . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 378<br />
Steven M. Neustein and James B. Eisenkraft<br />
27 Cardiac Procedures . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 390<br />
James H. Abernathy III<br />
28 Vascular Procedures . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 398<br />
Leanne Groban and Sylvia Y. Dolinski<br />
29 Abdominal Procedures . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 416<br />
Jeffrey H. Silverstein<br />
Index . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 429
Contributors<br />
James H. Abernathy, III, MD, MPH<br />
Assistant Professor<br />
Department of <strong>Anesthesia</strong> and<br />
Perioperative Medicine<br />
Medical University of South Carolina<br />
Charleston, SC, USA<br />
Sheila R. Barnett, MD<br />
Associate Professor<br />
Department of <strong>Anesthesiology</strong><br />
Harvard Medical School<br />
Beth Israel Deaconess Medical Center<br />
Boston, MA, USA<br />
Jack M. Berger, MD, PhD<br />
Clinical Professor<br />
Department of <strong>Anesthesiology</strong><br />
Keck School of Medicine<br />
University of Southern California<br />
Los Angeles, CA, USA<br />
Shaul Beyth, MD, MSc<br />
Department of Orthopedic Surgery<br />
Hadassah Hebrew University Medical Center<br />
Jerusalem, Israel<br />
Harold Brem, MD<br />
Associate Professor<br />
Director, Wound Healing<br />
Department of Surgery—Wound Healing Program<br />
Columbia University Medical Center<br />
New York, NY, USA<br />
Charles Cain, MD, MBA<br />
Clinical Professor<br />
Department of <strong>Anesthesiology</strong><br />
Columbia University Medical Center<br />
New York, NY, USA<br />
Jeffrey L. Carson, MD<br />
Richard C. Reynolds Professor of Medicine<br />
Chief<br />
Division of General Internal Medicine<br />
Department of Medicine<br />
UMDNJ—Robert Wood Johnson Medical School<br />
New Brunswick, NJ, USA<br />
Rodrigo Cartin-Ceba, MD<br />
Critical Care Medicine Fellow<br />
Department of Critical Care Service<br />
Mayo Clinic<br />
Rochester, MN, USA<br />
David J. Cook, MD<br />
Professor<br />
Department of <strong>Anesthesiology</strong><br />
Mayo Clinic College of Medicine<br />
Rochester, MN, USA<br />
Gregory Crosby, MD<br />
Associate Professor<br />
Department of <strong>Anesthesiology</strong><br />
Brigham and Women’s Hospital<br />
Harvard Medical School<br />
Boston, MA, USA<br />
Deborah J. Culley, MD<br />
Assistant Professor<br />
Department of <strong>Anesthesiology</strong><br />
Brigham and Women’s Hospital<br />
Harvard Medical School<br />
Boston, MA, USA<br />
Melissa Doft, MD<br />
Surgical Resident<br />
Department of Surgery<br />
Columbia University Medical Center<br />
New York, NY, USA<br />
xiii
xiv<br />
Contributors<br />
Sylvia Y. Dolinski, MD, FCCP<br />
Associate Professor<br />
Department of <strong>Anesthesiology</strong> and Critical Care<br />
Medical College of Wisconsin<br />
Milwaukee, WI, USA<br />
Thomas J. Ebert, MD, PhD<br />
Professor and Vice-Chair for Education<br />
Department of <strong>Anesthesiology</strong><br />
Medical College of Wisconsin<br />
Milwaukee, WI, USA<br />
James B. Eisenkraft, MD<br />
Professor<br />
Department of <strong>Anesthesiology</strong><br />
Mount Sinai School of Medicine<br />
New York, NY, USA<br />
Sheila J. Ellis, MD<br />
Associate Professor<br />
Department of <strong>Anesthesiology</strong><br />
University of Nebraska Medical Center<br />
Omaha, NE, USA<br />
Anna Flattau, MD<br />
Assistant Professor<br />
Department of Surgery and Family<br />
Medicine—Wound Healing Program<br />
Columbia University Medical Center<br />
New York, NY, USA<br />
Lee A. Fleisher, MD<br />
Robert D. Dripps Professor<br />
Department of <strong>Anesthesiology</strong> and Critical Care<br />
Chair of <strong>Anesthesiology</strong> and Critical Care<br />
Hospital of the University of Pennsylvania<br />
Philadelphia, PA, USA<br />
Pamela Flood, MD<br />
Associate Professor<br />
Department of <strong>Anesthesiology</strong><br />
Columbia University<br />
New York, NY, USA<br />
Daniel M. Gainsburg, MD<br />
Assistant Professor<br />
Department of <strong>Anesthesiology</strong><br />
Mount Sinai School of Medicine<br />
New York, NY, USA<br />
Ognjen Gajic, MD, MSc, FCCP<br />
Assistant Professor<br />
Department of Internal Medicine<br />
Mayo Clinic College of Medicine<br />
Rochester, MN, USA<br />
Maria F. Galati, MBA<br />
Vice Chair, Administration<br />
Department of <strong>Anesthesiology</strong><br />
Mount Sinai School of Medicine<br />
New York, NY, USA<br />
Michael S. Golinko, MD<br />
Post-Doctoral Research Scientist<br />
Department of Surgery—Wound Healing Program<br />
Columbia University Medical Center<br />
New York, NY, USA<br />
Leanne Groban, MD<br />
Associate Professor<br />
Department of <strong>Anesthesiology</strong><br />
Wake Forest University School of Medicine<br />
Winston-Salem, NC, USA<br />
Andrew M. Hanflik, BS<br />
Medical Student<br />
Keck School of Medicine<br />
University of Southern California<br />
Los Angeles, CA, USA<br />
Gary R. Haynes, MD, PhD<br />
Professor<br />
Department of <strong>Anesthesia</strong> and Perioperative Medicine<br />
Medical University of South Carolina<br />
Charleston, SC, USA<br />
Paul J. Hoehner, MD, MA, FAHA<br />
Director<br />
Department of Cardiovascular and Thoracic<br />
<strong>Anesthesiology</strong><br />
Central Maine Heart Associates<br />
Central Maine Heart and Vascular Institute<br />
Lewiston, ME<br />
Harvey Fellow in <strong>The</strong>ology<br />
Ethics and Culture<br />
Department of Religious Studies<br />
University of Virginia Graduate School of Arts<br />
and Sciences<br />
Charlottesville, VA, USA<br />
Christopher J. Jankowski, MD<br />
Assistant Professor and Consultant<br />
Department of <strong>Anesthesiology</strong><br />
Mayo Clinic College of Medicine<br />
Rochester, MN, USA<br />
Jacqueline M. Leung, MD, MPH<br />
Professor<br />
Department of <strong>Anesthesia</strong> and Perioperative Care<br />
University of California San Francisco<br />
San Francisco, CA, USA
Contributors<br />
xv<br />
Michael C. Lewis, MD<br />
Associate Professor<br />
Department of <strong>Anesthesiology</strong><br />
Miller School of Medicine<br />
University of Miami<br />
Miami, FL, USA<br />
Cynthia A. Lien, MD<br />
Professor<br />
Department of <strong>Anesthesiology</strong><br />
Weill Medical College of Cornell University<br />
New York, NY, USA<br />
Linda L. Liu, MD<br />
Associate Professor<br />
Department of <strong>Anesthesia</strong> and Perioperative Care<br />
University of California San Francisco<br />
San Francisco, CA, USA<br />
Roger D. London, MD, MBA<br />
Vice President and Medical Director<br />
Flagship Patient Advocates<br />
New York, NY, USA<br />
Idit Matot, MD<br />
Associate Professor<br />
Department of <strong>Anesthesiology</strong> and Critical<br />
Care Medicine<br />
Hadassah Hebrew University Medical Center<br />
Jerusalem, Israel<br />
Matthew D. McEvoy, MD<br />
Assistant Professor<br />
Department of <strong>Anesthesia</strong> and<br />
Perioperative Medicine<br />
Medical University of South Carolina<br />
Charleston, SC, USA<br />
Kathryn E. McGoldrick, MD<br />
Professor and Chair<br />
Department of <strong>Anesthesiology</strong><br />
New York Medical College<br />
Valhalla, NY, USA<br />
Charles H. McLeskey, MD<br />
Salt Lake City, UT, USA<br />
Jessica Miller, MD<br />
Fellow<br />
Department of Pediatric <strong>Anesthesiology</strong> and<br />
Critical Care<br />
Children’s Hospital of Philadelphia<br />
Philadelphia, PA, USA<br />
Terri G. Monk, MD<br />
Professor<br />
Department of <strong>Anesthesiology</strong><br />
Duke University Health System<br />
Durham, NC, USA<br />
Stanley Muravchick, MD, PhD<br />
Professor<br />
Department of <strong>Anesthesiology</strong> and Critical Care<br />
Hospital of the University of Pennsylvania<br />
Philadelphia, PA, USA<br />
Steven M. Neustein, MD<br />
Associate Professor<br />
Department of <strong>Anesthesiology</strong><br />
Mount Sinai School of Medicine<br />
New York, NY, USA<br />
J.G. Reves, MD<br />
Vice President for Medical Affairs<br />
Dean, College of Medicine<br />
Department of <strong>Anesthesiology</strong>/College of Medicine<br />
Medical University of South Carolina<br />
Charleston, SC, USA<br />
G. Alec Rooke, MD, PhD<br />
Professor<br />
Department of <strong>Anesthesiology</strong><br />
University of Washington and the Veterans Affairs<br />
Puget Sound Health Care System<br />
Seattle, WA<br />
Visiting Professor of <strong>Anesthesia</strong>, Critical Care, and<br />
Pain Medicine<br />
Harvard Medical School<br />
Beth Israel Deaconess Medical Center<br />
Boston, MA, USA<br />
Daniel I. Sessler, MD<br />
Chair<br />
Department of Outcomes Research<br />
<strong>The</strong> Cleveland Clinic<br />
Cleveland, OH, USA<br />
Steven L. Shafer, MD<br />
Professor<br />
Department of <strong>Anesthesia</strong><br />
Stanford University<br />
Palo Alto, CA<br />
Professor<br />
Department of Biopharmaceutical Sciences and<br />
<strong>Anesthesia</strong><br />
University of California San Francisco<br />
San Francisco, CA, USA
xvi<br />
Contributors<br />
Jeffrey H. Silverstein, MD<br />
Professor<br />
Department of <strong>Anesthesiology</strong>, Surgery,<br />
and <strong>Geriatric</strong>s and Adult Development<br />
Vice Chairman for Research<br />
Associate Dean for Research<br />
Mount Sinai School of Medicine<br />
New York, NY, USA<br />
Juraj Sprung, MD, PhD<br />
Professor<br />
Department of <strong>Anesthesiology</strong><br />
Mayo Clinic College of Medicine<br />
Rochester, MN, USA<br />
Takahiro Suzuki, MD, PhD<br />
Assistant Professor<br />
Department of <strong>Anesthesiology</strong><br />
Nihon University Surugadai Hospital<br />
Tokyo, Japan<br />
Tamas A. Szabo, MD, PhD<br />
Assistant Professor<br />
Department of <strong>Anesthesiology</strong><br />
Ralph H. Johnson Veterans Administration<br />
Medical Center<br />
Charleston, SC, USA<br />
Bernadette Veering, MD, PhD<br />
Associate Professor<br />
Department of <strong>Anesthesiology</strong><br />
Leiden University Medical Center<br />
Leiden, <strong>The</strong> Netherlands<br />
David O. Warner, MD<br />
Professor<br />
Department of <strong>Anesthesiology</strong><br />
Mayo Clinic College of Medicine<br />
Rochester, MN, USA<br />
R. David Warters, MD<br />
Professor<br />
Department of <strong>Anesthesiology</strong><br />
Ralph H. Johnson Veterans Administration<br />
Medical Center<br />
Charleston, SC, USA
Part I<br />
Introduction to Clinical <strong>Geriatric</strong>s
1<br />
<strong>The</strong> Practice of <strong>Geriatric</strong> <strong>Anesthesia</strong><br />
Jeffrey H. Silverstein<br />
<strong>The</strong> approach to and management of surgery and anesthesia<br />
in geriatric patients is different and frequently<br />
more complex than in younger patients. In caring for<br />
the elderly in the operating room, recovery room, and<br />
intensive care unit, the members of the perioperative<br />
medical team should be aware of the nature of aging<br />
physiology, the interaction of these alterations with<br />
pathologies, and the likelihood of multiple diagnoses<br />
and polypharmacy. <strong>The</strong> context of geriatric care encompasses<br />
multiple levels, stretching from primary care,<br />
through acute hospitalization, acute and subacute rehabilitation,<br />
nursing home care, and hopefully back to sufficient<br />
function to require additional primary care. By the<br />
nature of their practices, anesthesiologists and geriatricians<br />
have different approaches to patient care and the<br />
time frame over which such care occurs. In communicating<br />
with patients and geriatricians, one should understand<br />
that expectations for recovery are frequently different<br />
than in younger patients, marked by issues of maintenance<br />
of function and independence. <strong>The</strong>re is an evolving<br />
understanding that specific approaches taken in the perioperative<br />
period have an impact that remains apparent<br />
months to years following surgery. Integrating care across<br />
this continuum can be difficult but invariably improves<br />
patient outcomes.<br />
<strong>Geriatric</strong> medical care has evolved from an empiric<br />
specialty in the 1950s and 1960s to a largely evidencebased<br />
practice today. An excellent short reference guide<br />
called <strong>Geriatric</strong>s at Your Fingertips is available in a<br />
small pocket edition as well as on the Internet 1 (http://<br />
www.geriatricsatyourfingertips.org/). Perioperative geriatrics,<br />
however, is very much at the beginning of the<br />
process of developing sufficient primary data on which<br />
to base practice guidelines. <strong>The</strong>re are few randomized<br />
controlled trials that provide class I evidence regard -<br />
ing perioperative care of the elderly, leaving the practitioner<br />
to extra polate data from literature that has<br />
accumulated on geriatric care in other contexts, from retrospective<br />
reviews, and from the nonoperative geriatric<br />
literature.<br />
This introductory chapter presents some of the common<br />
concepts of geriatrics and a general approach to caring<br />
for geriatric patients presenting for anesthesia and<br />
surgery. Virtually every chapter in this book elaborates<br />
on this foundation chapter. In approaching the elderly as<br />
patients, the anesthesiologist must understand that there<br />
is tremendous heterogeneity or variability in aging, both<br />
in the body as a whole as well as in individual systems.<br />
Thus, the alterations described in this and the following<br />
chapters are likely, on average, to be present in geriatric<br />
surgical patients. However, each individual patient will<br />
manifest these changes differently. <strong>The</strong> reader is encouraged<br />
to develop expertise and judgment and to identify<br />
those areas in need of improved approaches with the goal<br />
of developing an evidence-based practice for perioperative<br />
geriatrics.<br />
Demography<br />
As a result of nationwide improvements in health care,<br />
nutrition, education, and general living standards, the<br />
elderly account for an increasing percentage of the United<br />
States population (Figure 1-1). One in eight Americans<br />
were elderly (age 65 and older) in 1997. By 2030, according<br />
to the United States Bureau of the Census, one in five<br />
could be elderly. Between 2010 and 2030, as the baby<br />
boom generation reaches age 65, anesthesiologists will<br />
face a variety of challenges. <strong>The</strong> fastest-growing segment<br />
of the population is that aged 85 and older.<br />
<strong>The</strong> average life expectancy in the United States<br />
is almost 72 years for men and 79 years for women.<br />
However, those who reach the age of 65 can expect to<br />
live 17.4 more years; a life expectancy of 82.4 years. <strong>The</strong>re<br />
are racial disparities in longevity. In the United States,<br />
white men who reach age 65 can expect to live 15.7 more<br />
3
4 J.H. Silverstein<br />
MILLIONS<br />
80<br />
60<br />
40<br />
Figure 1-1. Growth of the Elderly Population, 1900–2030.<br />
(Reprinted from He W, Sengupta M, Velkoff VA, DeBarros KA.<br />
U.S. Census Bureau. Current Population Reports, P23-209, 65+<br />
in the United States: 2005. Washington, DC: U.S. Government<br />
Printing Office; 2005.)<br />
20<br />
0<br />
1900 1920 1940 1960 1980 2000 2020<br />
1910 1930 1950 1970 1990 2010 2030<br />
YEAR<br />
years whereas black men who reach 65 can expect to live<br />
13.6 more years. Women are generally longer lived<br />
than men; however, the racial discrepancy is similar, with<br />
19.4 and 17.6 additional years, respectively, of additional<br />
life expected for white and black women who reach<br />
age 65.<br />
In 2004, 7.9 million patients over the age of 65 underwent<br />
a surgical procedure. 2 <strong>The</strong> number of patients over<br />
the age of 65 years who undergo noncardiac surgery has<br />
been projected to increase to 14 million over the next<br />
three decades 3 with similar increases expected for cardiac<br />
surgery. Seventy years ago, surgery was considered a desperate<br />
measure for patients older than 50 years of age,<br />
who were thought to be incapable of sustaining the rigors<br />
of even an inguinal hernia repair. 4 Advances in anesthesia<br />
during the past century have allowed surgeons to develop<br />
an extraordinary array of procedures with excellent outcomes<br />
in an increasingly aged population. Recent estimates<br />
confirm that the amount of surgical activity in the<br />
aging population is increasing. 5 Bolstered by the evolving<br />
demographics noted above, anesthesiologists can expect<br />
an ever-increasing portion of their overall workload to<br />
involve geriatric patients.<br />
Definitions of Aging<br />
Aging is a process of gradual and spontaneous change<br />
resulting first in maturation and subsequently decline<br />
through middle and late life. Senescence is the process by<br />
which the capacity for growth, function, and capacity for<br />
cell division are lost over time, ultimately leading to<br />
death. Aging comprises both a positive component of<br />
development (e.g., wisdom and experience) along with<br />
the negative component of physiologic and often cognitive<br />
decline.<br />
Researchers and clinicians have found advantages in<br />
differentiating normal aging from age-related disease<br />
processes. Normal aging is those changes measured, on<br />
average, across the population. Some of these changes,<br />
for example, decrease in muscle mass, occur even in the<br />
well-conditioned, exercising elderly. In order to distinguish<br />
aging from disease, researchers have had to carefully<br />
screen patients for disease processes. This process<br />
has allowed gerontologists to determine that many longheld<br />
truisms concerning aging were not accurate. For<br />
example, it is now clear that aging per se does not involve<br />
neuronal loss in the brain, and cognitive decline is not an<br />
inevitable aspect of aging. Although it is evident to clinicians<br />
that diseases progressively accumulate in aging,<br />
many of these processes are no longer considered synonymous<br />
with increased age. That is not to suggest that<br />
aging is an innocent bystander, that is, that age-related<br />
disease accumulation could occur simply as a function<br />
of time. Lakatta and Levy, 6 in their studies of cardiac<br />
physiology, explained that age-related changes alter the<br />
substrate upon which disease processes evolve. In this<br />
conception, age affects the severity of disease manifestations<br />
for a given time at risk.<br />
In contrast to normal aging, Rowe and Kahn 7 de -<br />
scribed the idea of successful aging. In successful aging,<br />
the deleterious effects of senescence are minimized<br />
such that the individuals suffer few of the unwanted<br />
features of aging. <strong>The</strong>se individuals are vibrant and active<br />
into late age, with limited impairment. <strong>The</strong> combi -<br />
nation of genetic and environmental status that leads to<br />
longevity is discussed in the chapter <strong>The</strong>ories of Aging<br />
(Chapter 3). <strong>The</strong> distinction between normal and successful<br />
aging highlights one of the principal phenomena in<br />
gerontology: that there is tremendous variability in aging<br />
between individuals of a given species. Although it is<br />
extremely convenient to categorize and even stereotype
1. <strong>The</strong> Practice of <strong>Geriatric</strong> <strong>Anesthesia</strong> 5<br />
patients by age, chronological age is a poor predictor of<br />
physiologic aging.<br />
Currently, morbidity, mortality, and recovery times<br />
for elderly patients undergoing surgery are substantially<br />
greater than those for younger patients. 8 (See also<br />
the section Surgical Outcomes and Functional Decline<br />
later in this chapter.) Age frequently alters the presentation<br />
of surgical illness. Symptoms of disease may be<br />
diminished, ignored, or inappropriately attributed to old<br />
age. Obtaining an accurate history can be challenging in<br />
the elderly. One of the results of the complexity of the<br />
patient population is an increased likelihood of preventable<br />
adverse events and consequences. 9 Thus, improving<br />
anesthetic care for geriatric patients represents the<br />
primary challenge of anesthesiology in the next few<br />
decades.<br />
Physiologic<br />
Reserves<br />
Available<br />
“<strong>The</strong> Precipice”<br />
Increasing Age<br />
Physiologic<br />
Reserves<br />
Already in Use<br />
Figure 1-2. Schematic of homeostenosis. This diagram shows<br />
that maintaining homeostasis is a dynamic process. <strong>The</strong> older<br />
person uses or consumes physiologic reserves just to maintain<br />
homeostasis, and therefore there are fewer reserves available<br />
for meeting new challenges. (Reprinted with permission from<br />
Taffet GE. Physiology of aging. In: Cassel CK, Leipzig R, Cohen<br />
HJ, Larson EB, Meier DE, eds. <strong>Geriatric</strong> Medicine: An Evidence-Based<br />
Approach. 4th ed. New York: Springer; 2003.)<br />
General Physiology of Aging<br />
A homeostatic system is an open system that maintains<br />
its structure and functions by means of a multiplicity of<br />
dynamic equilibriums rigorously controlled by interdependent<br />
regulatory mechanisms. 10 Such a system reacts<br />
to change through a series of modifications of equal size<br />
and opposite direction to those that created the disturbance.<br />
<strong>The</strong> goal of these modifications is to maintain the<br />
internal balances. <strong>The</strong> term homeostenosis has been used<br />
to describe the progressive constriction of homeostatic<br />
reserve capacity. Another common means of expressing<br />
this idea is that aging results in a progressive decrease in<br />
reserve capacity. Diminishing reserve capacity can be<br />
identified at a cellular, organ, system, or whole-body level.<br />
As an example, glomerular filtration rate (GFR) progressively<br />
decreases with aging, limiting the capacity to deal<br />
with any stress on this excretory mechanism, be that a<br />
fluid load or excretion of medications or other toxic substances.<br />
Once again, the variability associated with aging<br />
is a key modifier of the decrease in physiologic function.<br />
So, although in general GFR decreases 1 mL/year, 30%<br />
of participants in a large study that defined this change<br />
had no change in GFR whereas others showed much<br />
greater decrements. 11 <strong>The</strong> concept of reserve has also<br />
been used in describing cognitive function. 12 Taffet has<br />
expanded the general interpretation of the decrease in<br />
physiologic reserve to emphasize that the reserve capacity<br />
is not an otherwise invisible organ capacity but the<br />
available organ function that will be used to maximal<br />
capacity by the elderly to maintain homeostasis (Figure<br />
1-2). When the demands exceed the capacity of the organ<br />
or organism to respond, pathology ensues. This is ever<br />
more likely as aging decreases the capacity of any system<br />
to respond. <strong>The</strong> concept of organ reserve will be invoked<br />
in many chapters of this textbook.<br />
Frailty<br />
A term frequently applied to elderly patients is “frail.”<br />
One would expect the frail elderly to be at higher risk<br />
for functional decline following surgery. Unfortunately,<br />
much like Justice Potter Stewart’s 1964 definition of<br />
obscenity, most physicians can identify frailty when<br />
they see it, but a clinically relevant scientific definition<br />
has been elusive. Linda Fried and colleagues 13 have<br />
defined frailty, focusing primarily on muscle loss, or sarcopenia,<br />
as a clinical syndrome in which three or more<br />
of the following criteria are present: unintentional weight<br />
loss (10 lbs. in past year), self-reported exhaustion,<br />
weakness (grip strength), slow walking speed, and low<br />
physical activity. In the initial evaluation of the participants<br />
from the Cardiovascular Health Study (5317 men<br />
and women 65 years and older), the overall prevalence<br />
of frailty was 6.9%. 13 Frailty is perceived, in this context,<br />
as a cyclical decline that perpetuates itself (Figure 1-3).<br />
Frailty has been described as a form of predisability,<br />
which is distinct from functional impairment. 14 However,<br />
in the setting of sarcopenia, further muscle loss associated<br />
with surgical illness could be functionally disastrous.<br />
Indeed, Wolfe 15,16 has recently shown that the catabolic<br />
response to the stress of surgery and the subsequent loss<br />
of muscle mass is of even greater concern in the elderly.<br />
Frailty as a specific measure has not been prospectively<br />
characterized as a preoperative risk factor. <strong>The</strong> American<br />
Society of Anesthesiologists physical status score does<br />
not easily capture frailty, although clinicians may factor<br />
significant frailty into their assessment of a patient’s physical<br />
status. Current research efforts should help define the<br />
relevance of frailty in the assessment and management of<br />
elderly patients.
6 J.H. Silverstein<br />
Neuroendocrine<br />
Dysregulation<br />
Anoreria<br />
of aging<br />
Total Energy Expenditure<br />
Chronic<br />
Undernutrition<br />
[Inadequate intake<br />
of protein and<br />
energy micronutrient<br />
deficiencies]<br />
Aging:<br />
Senescent<br />
musculoskeletal changes<br />
Negative Energy Balance<br />
Negative Nitrogen Balance<br />
Disease<br />
Weight Loss<br />
Loss of musele mass<br />
Sarcopenia<br />
Activity<br />
Walking<br />
Speed<br />
Disability<br />
Resting<br />
Metabolic<br />
Rate<br />
Strength<br />
&<br />
Power<br />
.<br />
VO 2 max<br />
Dependency<br />
Figure 1-3. Cycle of frailty hypothesized as consistent with<br />
demonstrated pairwise associations and clinical signs and<br />
symptoms of frailty. (Reprinted with permission from Fried<br />
LP, Tangen CM, Walston J, Newman AB, Hirsch C,<br />
Gottdiener J, Seeman T, Tracy R, Kop WJ, Burke G, McBurnie<br />
MA; Cardiovascular Health Study Collaborative Research<br />
Group. Frailty in older adults: evidence for a phenotype. J<br />
Gerontol A Biol Sci Med Sci. 2001 Mar; 56(3):M146–56.)<br />
Surgical Outcomes and<br />
Functional Decline<br />
Traditional surgical outcomes include morbidity and<br />
mortality within a defined period following a procedure,<br />
frequently 30 days. Data from the Veterans Administrations<br />
National Surgical Quality Improvement Program<br />
(NSQIP) provides the most current insight into surgical<br />
outcomes for elderly patients. Hamel et al. 17 reported on<br />
26,648 patients aged ≥80 (median age 82) and 568,263<br />
patients 80 (Table 1-1). Mortality was low<br />
(80 had one or more complications, and the presence of<br />
a complication increased mortality from 4% to 26%.<br />
Respiratory and urinary tract complications were the<br />
most common.<br />
For the mid- to late-life patient, symptoms and disability<br />
are the principal outcomes of most disease processes.<br />
<strong>The</strong>y may become the focus of protracted care. In<br />
order to conceptualize disability in a format that supports<br />
medical and survey research, Verbrugge and Jette 18 elucidated<br />
<strong>The</strong> Disablement Process. <strong>The</strong> pathway to disability<br />
(Figure 1-4) begins with a disease or pathology.<br />
Impairments occur at the organ-system level and are dysfunctional<br />
and structural abnormalities in specific body<br />
systems, such as cardiovascular or neurologic. Functional<br />
limitations subsequently occur at the organism, or entire<br />
Table 1-1. Thirty-day mortality for operations.<br />
80 years<br />
General surgery 4.3 11.4<br />
Vascular surgery 4.1 9.4<br />
Thoracic surgery 6.3 13.5<br />
Urologic surgery 0.7 1.9<br />
Neurosurgery 2.4 8.6<br />
Otolaryngological surgery 2.5 8.8<br />
Orthopedic surgery 1.2 8.3<br />
Source: Hamel et al. 17<br />
Note: Median age for the 80 = 82 years.
1. <strong>The</strong> Practice of <strong>Geriatric</strong> <strong>Anesthesia</strong> 7<br />
Pathology<br />
Diagnoses of<br />
disease, injury,<br />
congenital<br />
condition<br />
Impairments<br />
Dysfunction and<br />
structural<br />
abnormalities in<br />
specific body<br />
systems, i.e.,<br />
cardiovascular<br />
<strong>The</strong> Disablement Process<br />
Main Pathway<br />
Functional Limitations<br />
Restriction in basic<br />
physical and mental<br />
actions: ambulate, stoop,<br />
produce intelligible<br />
speech<br />
Disability<br />
Difficulty doing<br />
activities of daily<br />
life, job,<br />
household<br />
management, etc.<br />
Figure 1-4. <strong>The</strong> disablement process: main pathway. (Adapted with permission from Verbrugge and Jette. 18 )<br />
being, level and comprise restrictions in basic physical<br />
and mental abilities such as ambulation, reaching, bending,<br />
and communicating intelligibly. Disability occurs when<br />
there is an insurmountable gap between an individual<br />
and environmental demands such that their expected<br />
social role is compromised. Intra-individual (e.g., age,<br />
socioeconomic status) and extra-individual (e.g., acute<br />
medical events, preventive interventions) factors can<br />
influence the Disablement Process in either direction.<br />
<strong>The</strong>se factors may be preexisting or new occurrences.<br />
<strong>The</strong> goals of therapy for a geriatric patient are frequently<br />
motivated by a desire to avoid disability and<br />
preserve or perhaps improve functional status. <strong>The</strong><br />
most common measures of functional status are called<br />
activities of daily living (ADL) and instrumental activities<br />
of daily living (IADL) 19 (Tables 1-2 and 1-3). ADLs<br />
are those basic activities fundamental to self-care whereas<br />
IADLs are those functions necessary to live independently.<br />
ADLs and IADLs are subjective reported measures.<br />
In a research context, it is common to include<br />
objective measures of function to assess strength, time to<br />
perform specific activities, or distance covered in a fixed<br />
period of time. Measurement of cognitive function by<br />
neuropsychologic tests is analogous to measures of physical<br />
function. In general medical patients, there has been<br />
extensive research regarding both the basis for functional<br />
decline as well as approaches to improving outcomes in<br />
elderly patients hospitalized for acute illness. Many of the<br />
published clinical trials studied variations of the comprehensive<br />
geriatric assessment, described below.<br />
<strong>The</strong> disablement process model is the theoretical basis<br />
for a model of elements that influence functional<br />
recovery after elective major surgery (Figure 1-5). <strong>The</strong>re<br />
are two types of preexisting factors or determinants:<br />
1) variable elements of function that may be modifiable<br />
or amenable to interventions; 2) relatively fixed elements<br />
in the context of daily living, which shape function<br />
and the roles of the variable elements, but may not be<br />
feasible targets for improving recovery. Variable elements<br />
are a comprehensive array of psychosocial, behavioral,<br />
and preoperative biomedical factors that can influence<br />
the evolution of function directly or indirectly through<br />
their influences on, and/or interaction with, other determinants.<br />
<strong>The</strong>se elements are potentially amendable to<br />
intervention prior to an elective surgical procedure.<br />
Fixed elements are a separate constellation of contextual<br />
factors of daily living in which determinants and functional<br />
evolution interact and unfold. <strong>Anesthesia</strong> incorporates<br />
pharmacologic techniques to eliminate pain and<br />
the stress response attendant to surgical procedures.<br />
Within the acute event, there are surgical options (e.g.,<br />
laparoscopic procedures) that may decrease the stress of<br />
the surgical procedure as well as the potential for anesthetic<br />
choices that may impact the trajectory of recovery.<br />
<strong>The</strong> model is qualitatively similar to a model for acute<br />
medical illness developed by Palmer et al. 20 and provides<br />
a framework for the identification of potential interventions<br />
to enhance postoperative recovery, prevent disability,<br />
and prolong independence in elders undergoing<br />
surgery.<br />
<strong>The</strong> impact of surgery on functional outcomes in elderly<br />
patients has been most clearly described by Lawrence<br />
et al. 21 in their report on a prospective cohort of 372 patients,<br />
60 years or older, undergoing abdominal surgery by surgeons<br />
in private practice and two university-affiliated<br />
hospitals in the San Antonio area. <strong>The</strong> participants were<br />
assessed preoperatively and postoperatively at 1, 3, and 6<br />
weeks, 3 and 6 months, using self-report and performancebased<br />
measures ADL, IADL, the Medical Outcomes Study<br />
Short Form-36 (SF-36) Physical Component and Mental
8 J.H. Silverstein<br />
Table 1-2. Activities of daily living. In each category, circle the item that most closely describes the person’s highest level of<br />
functioning and record the score assigned to that level (either 1 or 0) in the blank at the beginning of the category.<br />
A. Toilet _______<br />
1. Care for self at toilet completely; no incontinence 1<br />
2. Needs to be reminded, or needs help in cleaning self, or has rare (weekly at most) accidents 0<br />
3. Soiling or wetting while asleep more than once a week 0<br />
4. Soiling or wetting while awake more than once a week 0<br />
5. No control of bowels or bladder 0<br />
B. Feeding _______<br />
1. Eats without assistance 1<br />
2. Eats with minor assistance at meal times and/or helps with special preparation of food, or in cleaning up after meals 0<br />
3. Feeds self with moderate assistance and is untidy 0<br />
4. Requires extensive assistance for all meals 0<br />
5. Does not feed self at all and resists efforts of others to feed him or her 0<br />
C. Dressing _______<br />
1. Dresses, undresses, and selects clothes from own wardrobe 1<br />
2. Dresses and undresses self with minor assistance 0<br />
3. Needs moderate assistance in dressing and selection of clothes 0<br />
4. Needs major assistance in dressing but cooperates with efforts of others to help 0<br />
5. Completely unable to dress self and resists efforts of others to help 0<br />
D. Grooming (neatness, hair, nails, hands, face, clothing) _______<br />
1. Always neatly dressed and well-groomed without assistance 1<br />
2. Grooms self adequately with occasional minor assistance, e.g., with shaving 0<br />
3. Needs moderate and regular assistance or supervision with grooming 0<br />
4. Needs total grooming care but can remain well-groomed after help from others 0<br />
5. Actively negates all efforts of others to maintain grooming 0<br />
E. Physical ambulation _______<br />
1. Goes about grounds or city 1<br />
2. Ambulates within residence or about one-block distance 0<br />
3. Ambulates with assistance of (check one) a ( ) another person, b ( ) railing, c ( ) cane, d ( ) walker, e ( ) wheelchair 0<br />
1. ________ Gets in and out without help.<br />
2. ________ Needs help getting in and out<br />
4. Sits unsupported in chair or wheelchair but cannot propel self without help 0<br />
5. Bedridden more than half the time 0<br />
F. Bathing _______<br />
1. Bathes self (tub, shower, sponge bath) without help 1<br />
2. Bathes self with help getting in and out of tub 0<br />
3. Washes face and hands only but cannot bathe rest of body 0<br />
4. Does not wash self but is cooperative with those who bathe him or her 0<br />
5. Does not try to wash self and resists efforts to keep him or her clean 0<br />
Source: Lawton and Brody. 19<br />
Scoring interpretation: For ADLs, the total score ranges from 0 to 6. In some categories, only the highest level of function receives a 1; in others,<br />
two or more levels have scores of 1 because each describes competence at some minimal level of function. <strong>The</strong>se screens are useful for indicating<br />
specifically how a person is performing at the present time. When they are also used over time, they serve as documentation of a person’s functional<br />
improvement or deterioration.<br />
Component Scales (PCS, MCS), <strong>Geriatric</strong> Depression<br />
Scale (GDS), Folstein Mini-Mental State Exam (MMSE),<br />
timed walk, functional reach, and hand-grip strength. <strong>The</strong><br />
mean recovery times were: MMSE, 3 weeks; timed walk, 6<br />
weeks; ADL, SF-36 PCS, and functional reach, 3 months;<br />
and IADL, 6 months (Figure 1-6). Mean grip strength did<br />
not return to preoperative status by 6 months. This result,<br />
that most functional recovery takes 3 to 6 months or longer,<br />
provides an indication of the impact that surgery makes on<br />
an elderly population. It should be noted that this cohort<br />
was accumulated before the popularity of laparoscopic<br />
procedures, so the stress of surgery and the recovery period<br />
may now be, on average, shorter.<br />
In preparing a patient for surgery, informing him or her<br />
regarding the prolonged time that it will take to recover<br />
to preoperative status or better can be extremely important.<br />
Patients who understand that recovery is a prolonged<br />
process are less likely to become discouraged and<br />
more likely to continue prolonged efforts to regain<br />
strength and endurance.<br />
Approach to the Patient<br />
Although a variety of investigations in elderly patients<br />
have explored specific issues in geriatric care, a comprehensive<br />
evidence-based approach to the perioperative<br />
care of the elderly is not available in 2007. <strong>The</strong>refore, the<br />
current approach is based on the few studies that have<br />
addressed these issues directly, extrapolation from studies
1. <strong>The</strong> Practice of <strong>Geriatric</strong> <strong>Anesthesia</strong> 9<br />
Table 1-3. Instrument (independent) activities of daily living. In each category, circle the item that most closely describes the person’s<br />
highest level of functioning and record the score assigned to that level (either 1 or 0) in the blank at the beginning of the category.<br />
A. Ability to use telephone _______<br />
1. Operates telephone on own initiative; looks up and dials numbers 1<br />
2. Dials a few well-known numbers 1<br />
3. Answers telephone but does not dial 1<br />
4. Does not use telephone at all 0<br />
B. Shopping _______<br />
1. Takes care of all shopping needs independently 1<br />
2. Shops independently for small purchases 0<br />
3. Needs to be accompanied on any shopping trip 0<br />
4. Completely unable to shop 0<br />
C. Food preparation _______<br />
1. Plans, prepares, and serves adequate meals independently 1<br />
2. Prepares adequate meals if supplied with ingredients 0<br />
3. Heats and serves prepared meals or prepares meals but does not maintain adequate diet 0<br />
4. Needs to have meals prepared and served 0<br />
D. Housekeeping _______<br />
1. Maintains house alone or with occasional assistance (e.g., domestic help for heavy work) 1<br />
2. Performs light daily tasks such as dishwashing, bedmaking 1<br />
3. Performs light daily tasks but cannot maintain acceptable level of cleanliness 1<br />
4. Needs help with all home maintenance tasks 1<br />
5. Does not participate in any housekeeping tasks 0<br />
E. Laundry _______<br />
1. Does personal laundry completely 1<br />
2. Launders small items; rinses socks, stockings, etc. 1<br />
3. All laundry must be done by others 0<br />
F. Mode of transportation _______<br />
1. Travels independently on public transportation or drives own car 1<br />
2. Arranges own travel via taxi but does not otherwise use public transportation 1<br />
3. Travels on public transportation when assisted or accompanied by another 1<br />
4. Travel limited to taxi or automobile with assistance of another 0<br />
5. Does not travel at all 0<br />
G. Responsibility for own medications _______<br />
1. Is responsible for taking medication in correct dosages at correct time 1<br />
2. Takes responsibility if medication is prepared in advance in separate dosages 0<br />
3. Is not capable of dispensing own medication 0<br />
H. Ability to handle finances _______<br />
1. Manages financial matters independently (budgets, writes checks, pays rent and bills, goes to bank); collects and keeps 1<br />
track of income<br />
2. Manages day-to-day purchases but needs help with banking, major purchases, etc. 1<br />
3. Incapable of handling money 0<br />
Source: Lawton and Brody. 19 Copyright by the Gerontological Society of America.<br />
Scoring interpretation: For IADLs, from 0 to 8. In some categories, only the highest level of function receives a 1; in others, two or more levels<br />
have scores of 1 because each describes competence at some minimal level of function. <strong>The</strong>se screens are useful for indicating specifically how a<br />
person is performing at the present time. When they are also used over time, they serve as documentation of a person’s functional improvement<br />
or deterioration.<br />
that provide some insight into the broader care of elderly<br />
surgical patients, and some general suggestions derived<br />
from the experience of the author and his colleagues.<br />
Stanley Muravchik nicely delineated the approach to<br />
the preanesthetic assessment of the elderly by specifying<br />
an organ-based vertical approach, as opposed to the horizontal<br />
approach of traditional diagnostic medicine (Figure<br />
1-7). <strong>The</strong> specific age-related changes to major organ<br />
systems as well as the interaction between aging and<br />
disease processes are each covered in individual chapters<br />
in this book. For each organ system, the anesthesiologists<br />
should determine the functional status and attempt to<br />
assess the reserve capacity. In some cases, reserve<br />
capacity can be directly tested, as in a cardiac stress test.<br />
Many systems, particularly many of the homeostatic<br />
mechanisms of concern in the elderly, e.g., the autonomic<br />
nervous system, immune system, or even thermoregulatory<br />
control, remain difficult to assess. Neither baseline<br />
function nor reserve capacity have easily administered<br />
tests with reliable results for these systems. Maintenance<br />
of intraoperative normothermia can be a challenging goal<br />
in some elderly patients, although it is difficult to predict<br />
which will be particularly resistant. 22 (See Chapter 8.) <strong>The</strong><br />
clinician should be attempting to distinguish age-related<br />
changes from disease, acknowledging that there are<br />
important interactions between the two, and that it can
10 J.H. Silverstein<br />
Figure 1-5. This model, developed by<br />
Valerie Lawrence, MD, from the University<br />
of Texas Medical Center at San<br />
Antonio, Texas, and Jeffrey H. Silverstein,<br />
MD, from the Mount Sinai School<br />
of Medicine in New York, divides preoperative<br />
elements into those that are<br />
potentially variable and those that are<br />
not amenable to preoperative alteration.<br />
An important aspect is the management<br />
of the acute event. <strong>The</strong> combination<br />
of these factors determines the functional<br />
outcomes of patients undergoing<br />
surgery.<br />
be difficult to determine what is aging and what is actual<br />
disease.<br />
In addition to a focus on senescent physiology of standard<br />
organ systems, proper evaluation in elderly patients<br />
requires attention to areas that are not frequently evaluated<br />
in younger patients (Table 1-4). Sometimes it is difficult<br />
to imagine an anesthesiologist evaluating a patient’s<br />
pressure points for early skin breakdown or specifically<br />
asking a patient about incontinence. <strong>The</strong> thrust of this<br />
chapter is that someone on the perioperative team must<br />
be cognizant of these issues. <strong>The</strong> team taking care of the<br />
patient has to have both the acute event and the recovery<br />
period as their focus of cooperation.<br />
<strong>The</strong> skin and musculoskeletal system can undergo tremendous<br />
alterations. Up to 10% of elderly patients<br />
develop serious skin breakdown during prolonged operations<br />
in which pressure is exerted over debilitated areas. 23<br />
Patients with severe arthritis, other limitations of range of<br />
motion, or prosthetic joints should, to the extent possible,<br />
be positioned on an operating room table in a position<br />
they find comfortable before the induction of anesthesia.<br />
This avoids severe strain on ligaments and joints that can<br />
be severely painful in the postoperative period.<br />
<strong>The</strong> elderly take a large percentage of the medications<br />
prescribed in the United States. Patients frequently<br />
consume multiple medications. <strong>The</strong> management of these<br />
medications is frequently chaotic. <strong>The</strong> patient may present<br />
a bag full of prescription bottles and is not totally sure<br />
which one they take, or, somewhat more likely, convey a<br />
few of the many medications that they have been prescribed.<br />
Many of these medications have interactions<br />
with drugs used by anesthesiologists in the perioperative<br />
period. <strong>The</strong>se issues are presented in some detail in<br />
Chapter 14.<br />
Acquiring information can be challenging and may<br />
involve discussion with not only the patient, but also their<br />
immediate caregiver as well as reference to previous<br />
medical records. A comprehensive approach to caring for<br />
the geriatric surgical patient may assign some of the<br />
assessment goals to the geriatrician, anesthesiologist, or<br />
surgeon. Additional time should be scheduled to accomplish<br />
an appropriate preoperative assessment. <strong>The</strong> area<br />
in which the preoperative assessment is conducted should<br />
be relatively quiet and well lit.<br />
Hearing loss is a common complaint and should be<br />
generally understood by the anesthesiologist. Presbyacusia<br />
generally involves impaired sensitivity, particularly to<br />
higher pitched sounds, a derangement in loudness perception,<br />
impaired sound localization, and a decrease in timerelated<br />
processing tasks. <strong>The</strong> summary behavior is<br />
frequently expressed as “I can hear you, but I can’t understand<br />
you.” <strong>The</strong> examiner can maximize the potential for<br />
communicating effectively with the patient by placing<br />
themselves 3–6 feet away, directly facing the patient. Use<br />
deliberate, clear speech at a somewhat slower (not comically<br />
or sarcastically) rate. <strong>The</strong> general tendency to speak<br />
louder needs to be tempered by the realization that shouted<br />
speech is often perceived as distorted by the elderly who<br />
are hard of hearing. Hearing aid technology has expanded<br />
dramatically and includes a variety of both external and<br />
surgically implantable technologies. 24 In general, patients<br />
should always be interviewed with their hearing aids in
1. <strong>The</strong> Practice of <strong>Geriatric</strong> <strong>Anesthesia</strong> 11<br />
Mean<br />
Summary<br />
Score<br />
7<br />
8<br />
9<br />
10<br />
11<br />
21<br />
Mean<br />
Change<br />
Score<br />
Percent Not Recovered<br />
Total Number Assessed<br />
Activities of Daily Living Instrumental Activities of Daily Living SF36 Physical Component<br />
0<br />
1<br />
2<br />
3<br />
4<br />
Pre<br />
Op<br />
*<br />
1<br />
Wk<br />
60%<br />
345<br />
*<br />
3<br />
Wk<br />
–<br />
372<br />
26%<br />
328<br />
*<br />
6<br />
Wk<br />
17%<br />
321<br />
3<br />
Mo<br />
14%<br />
293<br />
6<br />
Mo<br />
9%<br />
290<br />
Mean<br />
Summary<br />
Score<br />
8<br />
10<br />
12<br />
14<br />
16<br />
18<br />
24<br />
Mean<br />
Change<br />
Score<br />
Percent Not Recovered<br />
Total Number Assessed<br />
1<br />
3<br />
5<br />
7<br />
9<br />
Pre<br />
Op<br />
*<br />
1<br />
Wk<br />
92%<br />
345<br />
*<br />
3<br />
Wk<br />
–<br />
372<br />
76%<br />
328<br />
*<br />
6<br />
Wk<br />
55%<br />
321<br />
*<br />
3<br />
Mo<br />
34%<br />
293<br />
6<br />
Mo<br />
19%<br />
290<br />
Mean<br />
Summary<br />
Score<br />
100<br />
45<br />
40<br />
35<br />
30<br />
25<br />
0<br />
Mean<br />
Change<br />
Score<br />
Percent Not Recovered<br />
Total Number Assessed<br />
10<br />
5<br />
0<br />
–5<br />
–10<br />
*<br />
Pre 1 3<br />
Op Wk Wk<br />
– –– 56%<br />
372 327<br />
*<br />
6<br />
Wk<br />
36%<br />
320<br />
*<br />
3<br />
Mo<br />
19%<br />
292<br />
*<br />
6<br />
Mo<br />
16%<br />
289<br />
Mean<br />
Summary<br />
Score<br />
100<br />
60 10<br />
55<br />
50<br />
45<br />
0<br />
Mean<br />
Change<br />
Score<br />
Percent Not Recovered<br />
Total Number Assessed<br />
SF36 Mental Component<br />
5<br />
0<br />
–5<br />
Pre<br />
Op<br />
–<br />
372<br />
1<br />
Wk<br />
––<br />
3<br />
Wk<br />
30%<br />
327<br />
*<br />
6<br />
Wk<br />
27%<br />
320<br />
*<br />
3<br />
Mo<br />
19%<br />
292<br />
*<br />
6<br />
Mo<br />
17%<br />
289<br />
Mean<br />
Summary<br />
Score<br />
5<br />
6<br />
7<br />
8<br />
9<br />
10<br />
30<br />
Mean<br />
Change<br />
Score<br />
Percent Not Recovered<br />
Total Number Assessed<br />
<strong>Geriatric</strong> Depression Scale<br />
–3<br />
–2<br />
–1<br />
0<br />
1<br />
2<br />
Pre<br />
Op<br />
1<br />
Wk<br />
46%<br />
339<br />
3<br />
Wk<br />
–<br />
366<br />
40%<br />
323<br />
*<br />
6<br />
Wk<br />
31%<br />
317<br />
*<br />
3<br />
Mo<br />
30%<br />
289<br />
*<br />
6<br />
Mo<br />
25%<br />
286<br />
30<br />
28<br />
Mean<br />
Summary<br />
Score<br />
27<br />
26<br />
Mean<br />
Change<br />
Score<br />
Percent Not Recovered<br />
Total Number Assessed<br />
1.0<br />
0.5<br />
0<br />
–0.5<br />
Folstein MMSE<br />
*<br />
–1<br />
Pre 1 3<br />
Op Wk<br />
–<br />
372<br />
44%<br />
342<br />
Wk<br />
31%<br />
326<br />
*<br />
6<br />
Wk<br />
23%<br />
320<br />
3<br />
Mo<br />
32%<br />
291<br />
6<br />
Mo<br />
27%<br />
288<br />
Mean<br />
Seconds<br />
12<br />
14<br />
16<br />
18<br />
20<br />
22<br />
24<br />
Mean<br />
Change<br />
Score<br />
Percent Not Recovered<br />
Total Number Assessed<br />
–4<br />
–2<br />
10<br />
0<br />
2<br />
4<br />
6<br />
8<br />
Pre<br />
Op<br />
Timed Up and Go Functional Reach Grip Strength<br />
*<br />
1<br />
Wk<br />
84%<br />
317<br />
*<br />
60%<br />
301<br />
3<br />
Wk<br />
–<br />
341<br />
*<br />
6<br />
Wk<br />
41%<br />
294<br />
* *<br />
3<br />
Mo<br />
35%<br />
268<br />
6<br />
Mo<br />
37%<br />
265<br />
Mean<br />
Number of<br />
inches<br />
12<br />
11 0<br />
Mean<br />
Change<br />
10 Score –1<br />
9<br />
8<br />
Percent Not Recovered<br />
Total Number Assessed<br />
–2<br />
–3<br />
Pre<br />
Op<br />
*<br />
1<br />
Wk<br />
75%<br />
295<br />
*<br />
3<br />
Wk<br />
–<br />
323<br />
61%<br />
278<br />
*<br />
6<br />
Wk<br />
62%<br />
276<br />
3<br />
Mo<br />
54%<br />
250<br />
6<br />
Mo<br />
58%<br />
248<br />
Mean<br />
Kilograms<br />
of<br />
Pressure<br />
29<br />
28<br />
27<br />
26<br />
25<br />
24<br />
23<br />
Mean<br />
Change<br />
Score<br />
Percent Not Recovered<br />
Total Number Assessed<br />
1<br />
1<br />
–1<br />
–2<br />
–3<br />
Pre<br />
Op<br />
*<br />
1<br />
Wk<br />
68%<br />
323<br />
*<br />
68%<br />
309<br />
3<br />
Wk<br />
–<br />
354<br />
*<br />
6<br />
Wk<br />
63%<br />
301<br />
*<br />
3<br />
Mo<br />
61%<br />
271<br />
6<br />
Mo<br />
52%<br />
258<br />
Figure 1-6. Functional recovery after major abdominal operation. Recovery is<br />
shown as mean individual change from preoperative baseline and 95% confidence<br />
intervals, with worsened function below a zero line representing preoperative status;<br />
a score of −1 indicates a one-point worsening relative to the preoperative baseline.<br />
An additional “shadow” y-axis is shown for orientation to mean summary or total<br />
scores. Asterisks indicate statistically significant differences from preoperative baseline,<br />
adjusted for multiple comparisons. MMSE, Mini-Mental State Exam; SF36,<br />
Medical Outcomes Study Short Form-36. (Reprinted with permission from Lawrence<br />
et al. 21 )
12 J.H. Silverstein<br />
place, and, barring an operation in which the ear is within<br />
the sterile operative field, hearing aids can be left in during<br />
surgery. Modern hearing aids do not pose a risk to the<br />
patient associated with the use of electrocautery and, if not<br />
within the primary electrical path, are not at risk for<br />
damage from electrocautery units. Having the hearing aid<br />
in place assists communication during emergence and in<br />
the postanesthesia care unit.<br />
Loss of visual acuity is also common in the elderly. Visual<br />
acuity is included in a number of geriatric-care paradigms,<br />
including those that approach the prevention of perioperative<br />
delirium by means of making visual orientation easier.<br />
Cataracts can be particularly problematic. Before major<br />
surgery that is truly elective and schedulable, such as a<br />
total hip replacement, serious thought should be given to<br />
correcting the patient’s vision if they have bilateral dense<br />
cataracts. Although less likely to have major impact, given<br />
the opportunity, a visit to an eye doctor to maximize visual<br />
acuity, perhaps through a change in correction, may be<br />
beneficial to the patient. <strong>The</strong> patient may be better able to<br />
read and utilize rehabilitation aids.<br />
A particularly important issue in perioperative geriatrics<br />
is the role of the geriatrician. In the 1980s, geriatricians<br />
began evaluating a concept generally referred to as<br />
comprehensive geriatric assessment (CGA). CGA is a<br />
multidimensional, interdisciplinary, diagnostic process to<br />
identify care needs, plan care, and improve outcomes of<br />
frail older people. 25 <strong>The</strong> benefits of CGA are to improve<br />
diagnostic accuracy, optimize medical treatment, and<br />
improve medical outcomes (including functional status<br />
and quality of life).<br />
Figure 1-7. Organ system–based vertical approach to preoperative<br />
assessment of the elderly patient by an anesthesiologist<br />
differs from the traditional diagnostic approach because it<br />
applies the various techniques of inquiry (shaded bars) sequentially<br />
to each major organ system (open bars) in order to assess<br />
organ function and functional reserve. <strong>The</strong> primary objective of<br />
preoperative assessment should be evaluation of physical status<br />
rather than the identification of specific underlying disorders.<br />
(Reprinted with permission from Muravchick S. Preoperative<br />
assessment of the elderly patient. Anesthesiol Clin North Am<br />
2000;18(1):71–89, vi.)<br />
Table 1-4. Focus areas for assessment of geriatric patients.<br />
Medical<br />
Organ function and reserve<br />
Medical illnesses<br />
Medications<br />
Nutrition<br />
Dentition<br />
Hearing<br />
Vision<br />
Pain<br />
Urinary incontinence<br />
Mental<br />
Cognitive status<br />
Emotional status<br />
Spiritual status<br />
Physical<br />
Functional status<br />
Balance and gait<br />
Falls<br />
Environmental<br />
Social, financial status<br />
Environmental hazards<br />
In the perioperative arena, cooperative programs that<br />
feature some version of CGA have been evaluated. <strong>The</strong><br />
most common perioperative environment for these programs<br />
has been hip fracture services. In a review of orthogeriatric<br />
care, Heyburn and colleagues 26 described four<br />
models that have been applied to hip fracture patients:<br />
the traditional model in which care is directed by the<br />
orthopedic surgeon and medical queries are directed to a<br />
consultant; the second is a variation in which multidisciplinary<br />
rounds with geriatricians and surgeons increase<br />
awareness of cross-specialty issues; the third involves<br />
early postoperative transfer to a geriatric rehabilitation<br />
unit; and the fourth is combined orthogeriatric care in<br />
which the patient is admitted to a specialized ward where<br />
care is coordinated by geriatricians and orthopedic surgeons.<br />
Delirium is a common complication following hip<br />
fracture and has been the primary outcome of interest<br />
for some of these studies. (See also Chapters 9 and 24.)<br />
Edward Marcantonio conducted a randomized trial of<br />
proactive geriatric consultation based on a structured protocol<br />
for patients with hip fractures (Table 1-5). <strong>The</strong> intervention<br />
reduced delirium by more than one-third.<br />
In his review for the Freeman lecture, Rubenstein succinctly<br />
summed up the general state of affairs when he<br />
remarked that, despite the relatively consistent body of<br />
evidence supporting the utility of CGA and other geriatric<br />
follow-up programs, they have failed to be instituted<br />
on a wide scale. Soon after the initial successful reports,<br />
the institution of prospective payment diagnostic related<br />
groups (DRG) as part of the Medicare program made<br />
any additional stay in the hospital unprofitable. In fact,<br />
although CGA is effective at preventing rehospitaliza-
1. <strong>The</strong> Practice of <strong>Geriatric</strong> <strong>Anesthesia</strong> 13<br />
Table 1-5. Module with recommendations from Marcantonio’s Active <strong>Geriatric</strong> Consultation.<br />
1. Adequate central nervous system oxygen delivery:<br />
a) Supplemental oxygen to keep saturation >90%, preferably >95%<br />
b) Treatment to increase systolic blood pressure >2/3 baseline or >90 mm Hg<br />
c) Transfusion to keep hematocrit >30%<br />
2. Fluid/electrolyte balance:<br />
a) Treatment to restore serum sodium, potassium, glucose to normal limits (glucose
14 J.H. Silverstein<br />
maintains the Syllabus on <strong>Geriatric</strong> <strong>Anesthesiology</strong> which<br />
can be found on the ASA’s Web site, www.asahq.org/<br />
clinical/geriatrics/geron.htm. <strong>The</strong> Society for the Advancement<br />
of <strong>Geriatric</strong> <strong>Anesthesia</strong> (SAGA) was formed in<br />
1999 with the mission of improving the care of older<br />
patients having surgery. SAGA sponsors an annual<br />
meeting and provides organizational guidance for individuals<br />
interested in the perioperative care of the elderly<br />
(www.sagahq.org). A longer-standing effort in the United<br />
Kingdom is the Age Anaesthesia Association (www.<br />
aaa-online.org.uk/). <strong>The</strong> American <strong>Geriatric</strong>s Society<br />
has developed a Section on Surgical and Related Specialties<br />
that organizes educational efforts as well as supports<br />
a number of research funding opportunities to sup -<br />
port investigation into perioperative geriatrics (www.<br />
americangeriatrics.org/specialists/). <strong>The</strong> Section supports<br />
the <strong>Geriatric</strong> Syllabus for Specialists as well as the<br />
Research Agenda Setting Process. 28<br />
Conclusion<br />
This introductory chapter outlines the broad scope of<br />
perioperative geriatric care and provides a perspective<br />
with which to utilize the information in the remainder of<br />
this text. <strong>Geriatric</strong> care is, by nature complex, multidisciplinary,<br />
and evolving. <strong>The</strong>re is much yet to be learned in<br />
the area of perioperative geriatrics, but still many practices<br />
and procedures are known and can be used to<br />
improve the quality of perioperative care today.<br />
References<br />
1. Reuben DB, Herr KA, Pacala JT, Pollock BG, Potter JF,<br />
Semla TP. <strong>Geriatric</strong>s at Your Fingertips. 8th ed. New York:<br />
American <strong>Geriatric</strong>s Society; 2006.<br />
2. DeFrances CJ, Podgornik MN. 2004 National Discharge<br />
Survey. 371. 5-4-2006. Hyattsville, MD: National Center for<br />
Health Statistics. Advance Data from Vital and Health<br />
Statistics.<br />
3. Mangano DT. Preoperative risk assessment: many studies,<br />
few solutions. Is a cardiac risk assessment paradigm possible?<br />
<strong>Anesthesiology</strong> 1995;83:897–901.<br />
4. Ochsner A. Is risk of operation too great in the elderly?<br />
<strong>Geriatric</strong>s 1927;22:121.<br />
5. Klopfenstein CE, Herrmann FR, Michel JP, Clergue F,<br />
Forster A. <strong>The</strong> influence of an aging surgical population on<br />
the anesthesia workload: a ten-year survey. Anesth Analg<br />
1998;86:1165–1170.<br />
6. Lakatta EG, Levy D. Arterial and cardiac aging: major<br />
shareholders in cardiovascular disease enterprises. Part I.<br />
Aging arteries: a “setup” for vascular disease. Circulation<br />
2003;107:139–146.<br />
7. Rowe JW, Kahn RL. Human aging: usual and successful.<br />
Science 1987;237:143–149.<br />
8. Tiret L, Desmonts JM, Hatton F, Vourch G. Complications<br />
associated with anaesthesia: a prospective survey in France.<br />
Can Anaesth Soc J 1986;33:336–344.<br />
9. Rothschild JM, Bates DW, Leape LL. Preventable medical<br />
injuries in older patients. Arch Intern Med 2000;160:2717–<br />
2728.<br />
10. de Rosnay J. Homeostasis: resistance to change. Heylighen<br />
F, Joslyn C, Turchin V, eds. Brussels: Pincipia Cybernetica;<br />
1997. Available at: http://cleamc11.vub.ac.be/homeosta.html.<br />
11. Lindeman RD. Renal physiology and pathophysiology of<br />
aging. Contrib Nephrol 1993;105:1–12.<br />
12. Whalley LJ, Deary IJ, Appleton CL, Starr JM. Cognitive<br />
reserve and the neurobiology of cognitive aging. Ageing<br />
Res Rev 2004;3:369–382.<br />
13. Fried LP, Tangen CM, Walston J, et al. Frailty in older adults:<br />
evidence for a phenotype. J Gerontol A Biol Sci Med Sci<br />
2001;56:M146–M156.<br />
14. Morley JE, Haren MT, Rolland Y, Kim MJ. Frailty. Med Clin<br />
North Am 2006;90:837–847.<br />
15. Wolfe RR. <strong>The</strong> underappreciated role of muscle in health<br />
and disease. Am J Clin Nutr 2006;84:475–482.<br />
16. Wolfe RR. Optimal nutrition, exercise, and hormonal<br />
therapy promote muscle anabolism in the elderly. J Am Coll<br />
Surg 2006;202:176–180.<br />
17. Hamel MB, Henderson WG, Khuri SF, Daley J. Surgical<br />
outcomes for patients aged 80 and older: morbidity and<br />
mortality from major noncardiac surgery. J Am Geriatr Soc<br />
2005;53:424–429.<br />
18. Verbrugge LM, Jette AM. <strong>The</strong> disablement process. Soc Sci<br />
Med 1994;38:1–14.<br />
19. Lawton MP, Brody EM. Assessment of older people:<br />
self-maintaining and instrumental activities of daily living.<br />
Gerontologist 1969;9:179–186.<br />
20. Palmer RM, Counsell S, Landefeld CS. Clinical inter -<br />
vention trials: the ACE unit. Clin Geriatr Med 1998;14:<br />
831–849.<br />
21. Lawrence VA, Hazuda HP, Cornell JE, et al. Functional<br />
independence after major abdominal surgery in the elderly.<br />
J Am Coll Surg 2004;199:762–772.<br />
22. Sessler DI. Perianesthetic thermoregulation and heat<br />
balance in humans. FASEB J 1993;7:638–644.<br />
23. Aronovitch SA. Intraoperatively acquired pressure ulcer<br />
prevalence: a national study. J Wound Ostomy Continence<br />
Nurs 1999;26:130–136.<br />
24. Kim HH, Barrs DM. Hearing aids: a review of what’s new.<br />
Otolaryngol Head Neck Surg 2006;134:1043–1050.<br />
25. Rubenstein LZ, Joseph T. Freeman award lecture: comprehensive<br />
geriatric assessment—from miracle to reality.<br />
J Gerontol A Biol Sci Med Sci 2004;59:473–477.<br />
26. Heyburn G, Beringer T, Elliott J, Marsh D. Orthogeriatric<br />
care in patients with fractures of the proximal femur. Clin<br />
Orthop Relat Res 2004;(425):35–43.<br />
27. Vidan M, Serra JA, Moreno C, Riquelme G, Ortiz J. Efficacy<br />
of a comprehensive geriatric intervention in older patients<br />
hospitalized for hip fracture: a randomized, controlled trial.<br />
J Am Geriatr Soc 2005;53:1476–1482.<br />
28. Solomon DH, LoCicero J, Rosenthal RA, eds. New Frontiers<br />
in <strong>Geriatric</strong>s Research. An Agenda for the Surgical and<br />
Related Medical Specialties. New York: American <strong>Geriatric</strong>s<br />
Society; 2004.
2<br />
Demographics and Economics of <strong>Geriatric</strong><br />
Patient Care<br />
Maria F. Galati and Roger D. London<br />
Anesthesiologists in geriatric practice care primarily for<br />
patients who are insured via Medicare, the federal health<br />
insurance program for citizens over the age of 65. <strong>The</strong><br />
Medicare program has grown steadily in complexity and<br />
cost since its inception in 1965. It is expected to come<br />
under significant financial pressure as the population of<br />
the United States ages and the costs of providing health<br />
care continue to grow at ever-increasing rates.<br />
This chapter is intended to provide those anesthesiologists<br />
who care for the geriatric patient population with<br />
an introduction to key health policy issues related to the<br />
Medicare program and to facilitate understanding of the<br />
demographics and economics of geriatric care with special<br />
emphasis on Medicare. <strong>The</strong> first part of the chapter is a<br />
general introduction and overview of the demographic<br />
and financial issues facing Medicare in the near future.<br />
<strong>The</strong> second part of the chapter raises some of the major<br />
policy issues that are specific to the practice of anesthesiology<br />
under the Medicare program.<br />
Medicare Demographics and<br />
Financing Issues<br />
<strong>The</strong> Enactment of the Medicare Program<br />
Medicare is the federal program that provides health care<br />
insurance to all citizens who are at least 65 years old and<br />
to some disabled Americans. <strong>The</strong> program was enacted<br />
in 1965 with passage of one of the most important pieces<br />
of domestic legislation of the post-World War II period,<br />
but the legislative process that preceded it was marked<br />
by years of debate and controversy.<br />
From the Eisenhower administration forward, the<br />
United States government struggled with how best to<br />
meet the high cost of health care for the elderly. Results<br />
of the 1950 census revealed that since 1900 the aged<br />
population had grown from 4% to 8% of the total population.<br />
Two-thirds of the elderly had annual incomes of<br />
less than $1000, and only 1 in 8 had health insurance. 1 In<br />
response to the crisis, bills proposing hospital insurance<br />
for the aged were introduced in every Congress from<br />
1952 through 1965. 2<br />
Legislators recognized and feared the power of organized<br />
medicine to thwart passage of legislation that<br />
involved government-sponsored health insurance. <strong>The</strong>refore,<br />
when the Johnson Administration made its proposal,<br />
it included only a mandatory plan for covering hospital<br />
expenses for the elderly. This plan is what eventually<br />
became known as “Medicare Part A.”<br />
It was the Chairman of the House Ways and Means<br />
Committee in 1965, Congressman Wilbur Mills, who fashioned<br />
a compromise that led to the creation of “Medicare<br />
Part B,” a voluntary plan for coverage of physician<br />
expenses for the elderly that was acceptable to the<br />
American Medical Association (AMA). In the compromise<br />
proposal for Medicare Part B, physician expenses<br />
were to be reimbursed on “usual and customary” charges<br />
as long as they were “reasonable.” 3 Physicians also<br />
retained the right to bill patients directly and in excess of<br />
the amount reimbursed by the government.<br />
On July 30, 1965, President Lyndon Johnson enacted<br />
the Medicare and Medicaid programs by signing the<br />
Social Security Act of 1965 with these words:<br />
<strong>The</strong>re are men and women in pain who will find ease. <strong>The</strong>re are<br />
those alone and suffering who will now hear the sound of ap -<br />
pro aching help. <strong>The</strong>re are those fearing the terrible darkness<br />
of despair and poverty—despite long years of labor and expectation—who<br />
will now see the light of hope and realization. 4<br />
<strong>The</strong> Organization and Funding of Medicare<br />
<strong>The</strong> Social Security Administration administered the Medicare<br />
program from 1965 until 1977, when Medicare was<br />
reorganized under the Health Care Financing Administration<br />
(HCFA) within the Department of Health, Education<br />
and Welfare. In July 2001, HCFA was renamed the Centers<br />
for Medicare and Medicaid Services (CMS). 5 In 1966, the<br />
15
16 M.F. Galati and R.D. London<br />
Medicare program covered more than 19 million citizens<br />
over the age of 65. Coverage for the disabled began in 1973<br />
and, as of 2003, the program served more than 40 million<br />
Americans: 35 million elderly and 6 million disabled. 6<br />
<strong>The</strong> Medicare program provides coverage to the aged,<br />
the permanently disabled, and people with end-stage<br />
renal disease under two parts: Hospital Insurance (HI) or<br />
Medicare Part A, and Supplementary Medical Insurance<br />
(SMI) or Medicare Part B. <strong>The</strong> Medicare + Choice<br />
managed-care plan, also known as the “Medicare Advantage”<br />
program or Medicare Part C, was added by the<br />
Balanced Budget Act of 1997 and allows beneficiaries to<br />
opt for enrollment in private-sector–managed Medicare<br />
insurance plans. <strong>The</strong> Medicare Prescription Drug Improvement<br />
and Modernization Act of 2003 became effective in<br />
2006, and extended a new prescription drug benefit to<br />
Medicare beneficiaries known as Medicare Part D.<br />
<strong>The</strong> CMS contracts with private-sector agents to<br />
administer Medicare program services, including provider<br />
enrollment and claims administration processes.<br />
Contractors that process Part A claims are known as<br />
fiscal intermediaries and those that administer Part B<br />
claims are known as carriers. <strong>The</strong>se contractors are usually<br />
insurance companies, many of which are Blue Cross-Blue<br />
Shield plans around the United States that can act as both<br />
fiscal intermediaries and contractors. Contractors are<br />
barred by law from making a profit on services provided<br />
to the Medicare program.<br />
Enrollment in Medicare Part A is automatic for eligible<br />
beneficiaries and covers inpatient hospital care, afterhospital<br />
care in skilled nursing facilities, hospice care, and<br />
some home health services. Beneficiary enrollment in<br />
Medicare Part B is voluntary and covers physician services,<br />
outpatient hospital services, diagnostic tests, some<br />
home health services, and medical equipment and supplies.<br />
By law, 25% of Part B program costs must come<br />
from beneficiary premiums.<br />
Employers and employees who make mandatory contributions<br />
to the Part A Hospital Insurance Trust Fund<br />
finance the majority of the Medicare program costs. Other<br />
funding sources include general tax revenues, and the<br />
premiums, deductibles, and copayments paid by the<br />
beneficiaries. Of the Medicare program’s annual expenses<br />
($214.6 billion in 1997), 89% are funded by people under<br />
the age of 65 in the form of payroll and income taxes and<br />
interest from the trust fund. Only 11% comes from<br />
monthly premiums paid by the beneficiaries. 7<br />
Twenty-First Century Realities and the Future<br />
of the Medicare Program<br />
Baby Boomer Demographics<br />
<strong>The</strong> so-called “baby boomer generation,” the post-World<br />
War II Americans born between 1946 and 1964, will have<br />
a significant impact on the demographics of our society<br />
and on the Medicare program. It is predicted that as the<br />
boomers age, the number of people in the United States<br />
aged 65 years and older is expected to roughly double to<br />
77 million by the year 2030. 8<br />
Given the existing Medicare funding system, it is clear<br />
that the aging of the American population will bring fiscal<br />
pressures to bear on the Medicare program in two ways.<br />
<strong>The</strong>re will be more retired beneficiaries, as boomers age<br />
and live longer than their parents, and there will be fewer<br />
workers to pay for the retiree expenses. 9<br />
It is predicted that the over-65 age group will grow<br />
from approximately 13% of the total population in 2000<br />
to 20% in 2030 and will remain above 20% for at least<br />
several decades thereafter. 10 In addition, life expectancies<br />
are continuing to increase, and typical boomers are<br />
projected to live approximately 2 years longer than their<br />
parents did, spending more years in retirement (Figure<br />
2-1). At the same time, the labor force is expected to grow<br />
much more slowly than the population of retirees, resulting<br />
in many fewer workers per retiree. In 2000, there were<br />
4.8 people ages 20 to 64 for each person age 65 or older.<br />
This ratio is expected to decrease to approximately 2.9<br />
people ages 20 to 64 for each person age 65 or older by<br />
2030 (Figure 2-2).<br />
Although baby boomers report an intention to work<br />
longer than their parents did, it remains to be seen<br />
whether employers will accommodate this expectation<br />
and what effect this may have on the projected decrease<br />
in the worker–retiree ratio. Thus, retirement of the baby<br />
boomer generation will strain the already vulnerable<br />
Medicare program. <strong>The</strong> Social Security and Medicare<br />
90<br />
85<br />
80<br />
Women<br />
Actual<br />
Men<br />
Projected<br />
75<br />
0<br />
1940 1960 1980 2000 2020 2040 2060 2080<br />
Figure 2-1. Life expectancy of 65-year-olds. (From Congressional<br />
Budget Office based on Social Security Administration.<br />
<strong>The</strong> 2003 annual report of the Board of Trustees of the Federal<br />
Old-Age and Survivors Insurance and Disability Insurance<br />
Trust Funds. March 17, 2003. p. 86. Available at: www.ssa.gov/<br />
OACT/TR/TR03/tr03.pdf.)
2. Demographics and Economics of <strong>Geriatric</strong> Patient Care 17<br />
6<br />
5<br />
4<br />
3<br />
2<br />
1<br />
Actual<br />
Projected<br />
0<br />
1960 1980 2000 2020 2040 2060 2080<br />
Figure 2-2. Ratio of population ages 20 to 64 to population<br />
ages 65 and older. (From Congressional Budget Office based on<br />
Social Security Administration. <strong>The</strong> 2003 annual report of the<br />
Board of Trustees of the Federal Old-Age and Survivors<br />
Insurance and Disability Insurance Trust Funds. March 17, 2003.<br />
p. 82. Available at: www.ssa.gov/OACT/TR/TR03/tr03.pdf.)<br />
Boards of Trustees are predicting that starting in 2010,<br />
when the baby boom generation begins to retire, the<br />
Hospital Insurance Trust Funds will experience rapidly<br />
growing annual deficits leading to fund exhaustion by<br />
2019. 11 <strong>The</strong> report also predicts that the Supplemental<br />
Medical Insurance Trust Fund, which pays for physician<br />
services and the new prescription drug benefit, will have<br />
to be funded by large increases in premiums and increased<br />
transfers from general revenues.<br />
Baby Boomer Expectations<br />
<strong>The</strong> baby boomer generation will bring millions of people<br />
into the Medicare program and these new beneficiaries<br />
will also bring with them a new set of expectations. Baby<br />
boomers constitute the first generation born to the Medicare<br />
program and the first with significant experience<br />
with managed medical insurance plans. Baby boomers<br />
also include a significant number of women with working<br />
experience and, in general, are more affluent than their<br />
forebears. <strong>The</strong>y expect to enter retirement with more<br />
assets and with high expectations of the retirement<br />
experience.<br />
A survey conducted by Roper Starch Worldwide for<br />
the American Association of Retired Persons (AARP)<br />
and entitled, “Baby-Boomers Envision <strong>The</strong>ir Retirement:<br />
An AARP Segmentation Analysis,” examined the expectations,<br />
attitudes, and concerns of the baby boomers as<br />
they approach retirement. <strong>The</strong>re were several key attitudinal<br />
findings from the survey. Most baby boomers<br />
believe that they will still be working during their retirement<br />
years. This is unlike previous generations and has<br />
important implications for employers as well as the Medicare<br />
program.<br />
Only one in five boomers expects to move to a new<br />
geographic area when they retire and almost one in four<br />
expects to receive an inheritance that will affect their<br />
retirement planning. Only approximately 35% expect<br />
that they will have to scale back their lifestyle during<br />
retirement and only 16% believe that they will have<br />
serious health problems when they are retired (AARP<br />
op. cit.). <strong>The</strong>se are very optimistic views of the extent to<br />
which baby boomers’ retirement years will be disrupted<br />
by particular life events. 12<br />
Less optimistic conclusions emerged when the survey<br />
examined attitudes toward Social Security and Medicare:<br />
55% had a very or somewhat favorable view of Social<br />
Security and 60% had a favorable view of Medicare.<br />
However, only 46% said that they were very or somewhat<br />
knowledgeable about Medicare and only 40% were confident<br />
that Medicare would be available to them during<br />
retirement. Indeed, baby boomers were much less confident<br />
in their abilities under Medicare to access care,<br />
choose their own doctors, or to consult specialists at<br />
the same level as under their current health plan (AARP<br />
op. cit.).<br />
Medicare Coverage Gaps<br />
<strong>The</strong>se less optimistic baby boomer attitudes may reflect<br />
an astute appreciation of the limitations of the Medicare<br />
program. Benefits under the Medicare program are significantly<br />
limited. One study has found that 80% of<br />
employer-sponsored fee-for-service plans cover a larger<br />
proportion of medical expenses than Medicare does. 13<br />
Medicare has not traditionally covered services such as<br />
long-term nursing care, outpatient prescription drugs, or<br />
routine vision, dental, hearing, and foot care. <strong>The</strong><br />
Balanced Budget Act of 1997 extended coverage to<br />
include annual mammograms, Pap smears, prostate and<br />
colorectal screenings, diabetes management, and osteoporosis<br />
diagnosis. In December 2003, when the new prescription<br />
drug benefit was signed into law, it was projected that<br />
average out-of-pocket prescription drug spending for<br />
Medicare beneficiaries would be lower; however, it was<br />
also expected that 25% of beneficiaries would actually<br />
pay more as a result of the new coverage. 14 Furthermore,<br />
it is estimated that 3.1 million low-income subsidy-eligible<br />
beneficiaries are not receiving this assistance and therefore<br />
still face financial barriers in accessing necessary prescription<br />
drugs. 15 It will take years to fully assess the<br />
impact of this latest change in Medicare benefits on beneficiaries,<br />
providers, and the program itself.<br />
Medicare beneficiaries rely on privately purchased or<br />
government-sponsored supplemental insurance plans to<br />
“tie in” and complement the array of services covered by<br />
the Medicare program. Supplemental insurance coverage
18 M.F. Galati and R.D. London<br />
As a result of these various coverage options, Medicare<br />
beneficiaries are either not covered at all or are partly<br />
covered in a somewhat unpredictable way. This variability<br />
challenges practicing geriatric medicine providers to<br />
become knowledgeable about the specific situation in<br />
which each of their Medicare-eligible patients can find<br />
themselves, especially as it may relate to the patient’s<br />
ability to comply with treatment plans.<br />
Figure 2-3. Supplemental insurance status of Medicare beneficiaries,<br />
1999. (From Rice and Bernstein. 16 )<br />
for these services has been historically provided by Medicaid<br />
plans (for the poor) and by so-called “Medigap”<br />
policies for those able to afford additional coverage.<br />
In 1999, approximately 91% of Medicare beneficiaries<br />
relied on supplemental insurance plans. Of those with<br />
supplemental insurance, 27% purchased Medigap insurance<br />
and 36% received supplemental insurance related<br />
to employment. An additional 17% were enrolled in<br />
Medicare + Choice plans and 11% qualified for coverage<br />
through Medicaid. <strong>The</strong> remaining 9% had no supplemental<br />
coverage (Figure 2-3). 16 In 1996, Medigap premiums<br />
across the nation ranged from $233 annually for the leastexpensive<br />
basic coverage, to $2205 annually for the most<br />
comprehensive plan. 17<br />
Some employers, mostly large companies, also sponsor<br />
plans that cover retired workers and their spouses. In<br />
2006, 35% of firms with more than 200 employees offered<br />
retiree health benefits, with 77% of firms in this category<br />
covering Medicare-eligible retirees. In 1988, before implementation<br />
of the Part D drug benefit, 66% of large firms<br />
offered retiree coverage. 18<br />
<strong>The</strong> poorest Medicare recipients have their medical<br />
costs paid in part by the Medicaid program. Of these<br />
“dual eligibles,” those with incomes and resources substantially<br />
below the federal poverty line are entitled to<br />
full Medicaid coverage. Specifically, eligibility for full<br />
Medicaid coverage is determined by whether an individual<br />
qualifies for Supplemental Security Income, an income<br />
maintenance program designed for very poor aged,<br />
disabled, and blind Americans. Thus, Medicaid provides<br />
complementary coverage for a portion of Medicare<br />
beneficiaries.<br />
Unlike Medicare, Medicaid coverage includes benefits<br />
such as prescription drugs, hearing aids, and payment<br />
for nursing home services. <strong>The</strong> Medicaid program also<br />
makes premium payments and pays a portion of Medicare<br />
deductibles and other copayments required of<br />
beneficiaries. Because this assistance must be claimed<br />
by beneficiaries through an application process, a substantial<br />
portion of potentially eligible low-income individuals,<br />
perhaps as many as 3.9 million, do not receive<br />
this aid. 19<br />
Prescription Drug Benefit<br />
Medicare was late in providing prescription drug coverage<br />
compared with most private insurance plans, and the<br />
universal public health plans in other developed nations,<br />
that have traditionally provided this benefit as an important<br />
part of comprehensive health coverage. Drug therapies<br />
can reduce the need for hospitalization by effectively<br />
managing chronic health problems of the elderly such as<br />
heart disease, diabetes, and depression. Chronically ill<br />
patients have been found to underuse essential medications<br />
because of cost considerations and to suffer serious<br />
health consequences, including an increased number of<br />
emergency room visits and inpatient admissions, as a<br />
result. 20<br />
In 1998, 73% of noninstitutionalized Medicare beneficiaries<br />
had drug coverage of some kind for at least a<br />
portion of the year through supplemental insurance, such<br />
as managed Medicare plans, employer-sponsored plans,<br />
and Medigap plans. 21 However, the out-of-pocket spending<br />
by older Americans for prescription drugs amounts<br />
on average to 50% of total costs, compared with just 34%<br />
of costs for those under age 65. 22 <strong>The</strong> prices of the prescription<br />
drugs used most often by the elderly have been<br />
increasing in recent years. Expensive new brand-name<br />
drugs, some of which are more effective than the older<br />
drugs that they are superseding, are being brought to<br />
market at an increasingly rapid rate. 23<br />
In a recent nationwide survey of chronically ill older<br />
adults, it was reported that 33% underuse prescription<br />
drugs because of concerns about out-of-pocket drug<br />
costs. Furthermore, 66% of these patients failed to discuss<br />
their intention to underuse medications with a clinician<br />
citing that no one asked about their ability to pay and<br />
that they did not believe that providers could offer any<br />
assistance. 20<br />
Impact on the Near-Poor<br />
It is the near-poor, those with annual incomes between<br />
$10,000 and $20,000, who are most often caught in the<br />
prescription drug cost quandary. In 1999, only 55% of the<br />
near-poor had coverage for the entire year and more than<br />
20% of those with prescription drug coverage received it<br />
via a Medicare Advantage plan. Access to prescription<br />
drugs and levels of reimbursement for prescription<br />
drugs has decreased significantly under these managed-
2. Demographics and Economics of <strong>Geriatric</strong> Patient Care 19<br />
$250<br />
Benefit Limit<br />
$2,250<br />
Limit for Catastrophic Care<br />
$5,100<br />
Beneficiary responsible for costs<br />
Costs covered by Medicare<br />
100<br />
Prescription-Drug<br />
Coverage (%)<br />
75<br />
50<br />
25<br />
Medicare covers<br />
75%<br />
Beneficiary pays 100%<br />
of discounted drug price Medicare covers 95%<br />
0<br />
0 1,000 2,000 3,000 4,000 5,000 6,000 7,000 8,000 9,000 10,000<br />
Beneficiary’s Prescription-Drug Costs in a Year ($)<br />
Figure 2-4. Prescription drug coverage under Medicare effective 2006. (Reproduced with permission from Iglehart. 25 Copyright<br />
© 2004 Massachusetts Medical Society. All Rights Reserved.)<br />
Medicare plans since the Balanced Budget Act of 1997.<br />
As a result, the near-poor had higher out-of-pocket costs<br />
for prescription drugs in 1999 than other Medicare<br />
beneficiaries who were poorer (and therefore, Medicaideligible),<br />
and those with higher incomes. 24 Unfortu -<br />
nately, the new prescription drug benefit may not lead<br />
to a significant reduction in out-of-pocket prescription<br />
drug costs for these near-poor beneficiaries who will<br />
incur costs that fall through gaps in the coverage<br />
(Figure 2-4).<br />
In the intervening years before implementation of the<br />
new prescription drug benefit, there were some opportunities<br />
for the more than 33% of beneficiaries with no<br />
prescription drug benefits at all. Between 2004 and 2006,<br />
Medicare beneficiaries were eligible for drug-discount<br />
cards that were expected to save them up to 10%–15%<br />
on their total drug costs. In addition, beneficiaries with<br />
incomes below 135% of the federal poverty level were<br />
eligible for a $600 per year subsidy. 25 <strong>The</strong>se opportunities<br />
expired when the new drug benefit took effect in 2006.<br />
Medicare and the Academic Health Center<br />
<strong>The</strong> Medicare program has many shortcomings and, over<br />
the next two decades, significant reform will be required<br />
to maintain even the current level of protection that it<br />
offers to America’s elderly. This looming crisis in health<br />
care insurance for the elderly as well as the more than 40<br />
million uninsured is of great concern to lawmakers and<br />
the public but should also be of great concern to health<br />
care providers, hospitals, and physicians, who rely on<br />
Medicare as a significant source of their revenues.<br />
In 2000, payments made by the Medicare program<br />
accounted for 31% of total national spending on hospital<br />
care and 21% of total national spending on physician and<br />
clinical services. 26<br />
Physicians in academic practice have even greater<br />
reason to be interested in the plight of the Medicare<br />
program. In addition to the significant flow of funds<br />
received by Academic Health Centers (AHCs) in the<br />
form of clinical revenues, AHCs are dependent on the<br />
Medicare program for support of graduate medical education<br />
(GME) and care provided to indigent patients. All<br />
undergraduate medical students and almost 50% of all<br />
residents are trained in AHCs, which also provide most<br />
of the charity care and medical specialty services such as<br />
neonatal, burn and trauma intensive care, and organ<br />
transplant services. 27<br />
Graduate Medical Education Payments<br />
Since the initiation of the Medicare Prospective Hospital<br />
Payment System in the mid-1980s, GME payments have<br />
been made to AHCs to reimburse them for Medicare’s<br />
share of the costs of resident physician education. AHCs<br />
are eligible for two types of reimbursements: direct GME,<br />
covering direct costs such as resident and faculty salaries<br />
and benefits; and indirect GME, recognizing the relatively<br />
larger inpatient costs at hospitals with teaching<br />
programs.<br />
<strong>The</strong> Federal government has provided more than $100<br />
billion in GME support to AHCs since the mid-1980s.<br />
<strong>The</strong>se funds are distributed to approximately 1000 institutions<br />
based on the number of residents trained, their<br />
costs in the reference year 1985, and their share of Medicare<br />
beneficiaries served. <strong>The</strong> top ten AHCs receive an<br />
average of $60 million each (12% of the total), and the<br />
next 40 institutions receive approximately $30 million
20 M.F. Galati and R.D. London<br />
each (24% of the total). <strong>The</strong> remaining institutions share<br />
approximately 64% of the total. 27<br />
<strong>The</strong> Federal government also provides disproportionate<br />
share payments to 4000 institutions based on the<br />
number of Medicare and Medicaid patients served. <strong>The</strong><br />
top ten institutions receive only 5% of the total or an<br />
average of $20 million each and the next 40 institutions<br />
receive approximately 11% of the total for an average<br />
of $10 million each. <strong>The</strong> remaining institutions share<br />
approximately 85% of the total. 27<br />
Hospital and physician providers at the AHCs serve<br />
important roles in meeting the health care needs of<br />
underserved populations and in advancing the science of<br />
health care through education and research. <strong>The</strong>se providers<br />
are paid by Medicare to play this important role<br />
in shaping the future of the health care system. However,<br />
the same federal system continually challenges these providers<br />
to maintain a commitment to education, research,<br />
and charity care despite declining reimbursement for<br />
these important activities.<br />
“Pay for Performance” Initiatives<br />
<strong>The</strong> CMS has recognized the need to provide incentives<br />
to hospital and physician providers who can innovate to<br />
create improved patient outcomes at lower costs. Several<br />
demonstration projects are in place to provide hospitals<br />
with reimbursement bonuses if they meet quality standards<br />
and report their results to CMS.<br />
Physicians got their first opportunity to apply to Medicare’s<br />
physician Pay for Performance (P4P) initiative<br />
effective in April 2005. <strong>The</strong> CMS selected 10 physician<br />
group practices, with 200 or more physicians, which were<br />
eligible to earn performance payments in addition to<br />
usual fee-for-service payments. <strong>The</strong> payments were based<br />
on how well the groups managed the care of patients to<br />
prevent complications and avoidable hospitalizations<br />
thereby enhancing quality and reducing costs under both<br />
Part A and Part B of the Medicare program. 28 <strong>The</strong>se<br />
programs do not reward academic activities such as<br />
teaching, research, and grant work. <strong>The</strong>refore, success of<br />
P4P programs in the academic setting will depend on how<br />
much of physician compensation is based on clinical<br />
activity. 29<br />
Summary<br />
Many solutions to the looming Medicare crisis have<br />
been proposed. Common reform measures include<br />
changes to the age of eligibility, linking premiums to beneficiary<br />
incomes, increasing revenues via higher payroll<br />
taxes or counting Medicare benefits as taxable income,<br />
and altering the concept of Medicare as a defined benefit<br />
program.<br />
Pundits will continue to debate the strategy of choice<br />
for addressing the Medicare funding crisis. Meanwhile,<br />
physicians and hospitals, especially those with academic<br />
missions, can have an important role in the public policy<br />
debate. Health care providers, working with their professional<br />
organizations, can serve as patient advocates in the<br />
ongoing debate to facilitate the improvement of insurance<br />
coverage and the quality of health care services<br />
provided to the growing elderly population.<br />
Medicare Policy Issues for the<br />
<strong>Geriatric</strong> Anesthesiologist<br />
<strong>The</strong> regulations and processes governing a physician’s<br />
interaction with the Medicare program are quite complex<br />
and a full description is well beyond the scope of this<br />
chapter. However, it is the authors’ intention to provide<br />
the practicing geriatric anesthesiologist with an introduction<br />
to policy issues specific to the practice of <strong>Anesthesiology</strong><br />
under the Medicare program. <strong>The</strong>se key issues<br />
include:<br />
1) Participation status in the Medicare program<br />
2) Medicare’s Resource Based Relative Value System<br />
(RBRVS) for physician reimbursement<br />
3) Medicare’s rules for the anesthesia care team<br />
4) Compliance-related issues for anesthesiologists<br />
<strong>The</strong> CMS provides a specialty-specific page on its Web<br />
site that is dedicated to Medicare regulations and information<br />
specific to the practice of <strong>Anesthesiology</strong>. Physicians<br />
interested in further study of Medicare claims processing,<br />
fees and policies for the reimbursement of anesthesia services<br />
should consult CMS’s anesthesiologist Web page at:<br />
http://www.cms.hhs.gov/center/anesth.asp.<br />
Anesthesiologist Participation in<br />
the Medicare Program<br />
<strong>The</strong> decision to enroll as a participating provider in the<br />
Medicare program is one of the first decisions that an<br />
anesthesiologist faces when starting a clinical practice.<br />
Anesthesiologists employed in geriatric practice can<br />
expect that the Medicare program will be the primary<br />
insurer for most of their patients. Anesthesiologists, who<br />
typically encounter their patients in an operating room<br />
setting where they are not the patient’s primary provider,<br />
need to be aware of the political, patient satisfaction, and<br />
reimbursement issues related to their participation status<br />
in the Medicare program.<br />
In 1990, only 30.8% of anesthesiologists participated in<br />
the Medicare program; this was the lowest rate of participation<br />
as a percentage of physicians by medical specialty.<br />
By 2003, participation by anesthesiologists had increased
2. Demographics and Economics of <strong>Geriatric</strong> Patient Care 21<br />
to 95.5%. This rate of participation closely matches that<br />
of physicians in related practices such as surgery, cardiovascular<br />
disease, ophthalmology, orthopedic surgery,<br />
pathology, radiology, urology, and nephrology. 30<br />
It is likely that the anesthesiologist’s obligation to care<br />
for all surgical patients and new Medicare rules limiting<br />
charges from nonparticipating providers, influenced anesthesiologist<br />
enrollment decisions in the 1990s. Unfortunately,<br />
as anesthesiologist Medicare participation rates<br />
increased dramatically in the period from 1990 to 2003,<br />
the Medicare anesthesia conversion factor in the same<br />
period was decreased by almost 20%. 31 One might speculate<br />
that, during a decade of significant growth in managed<br />
care and public outcry concerning increasing health care<br />
costs, the pressures from patients, colleagues, local government,<br />
affiliated institutions, and the Medicare charge<br />
limitations combined to favor participation by anesthesiology<br />
providers.<br />
In general, participation in the Medicare program by<br />
anesthesiologists is a voluntary decision. [Medicare participation<br />
by Certified Registered Nurse Anesthetists<br />
(CRNAs) and Anesthesiologist Assistants (AAs) is mandatory.<br />
32 ] However, some states encourage physician<br />
participation through legislative actions and regulatory<br />
requirements, such as in <strong>The</strong> Commonwealth of Massachusetts,<br />
where Medicare participation is a condition<br />
of medical licensure. Physicians can consult with their<br />
local Medicare carrier or their regional CMS office for<br />
local Medicare participation requirements. 33<br />
Physicians who enroll as participating providers enter<br />
into a 1-year, automatically renewable agreement to<br />
accept assignment for all covered services provided to<br />
Medicare beneficiaries. When a physician accepts assignment,<br />
they agree to accept the Medicare allowable charge<br />
as payment in full for the covered services rendered.<br />
After patients satisfy an annual deductible, Medicare<br />
pays 80% of the approved allowable charge. <strong>The</strong> remaining<br />
20% is termed the “coinsurance” and it is the responsibility<br />
of the patient to pay this and any remaining<br />
portion of the annual deductible. Participating providers<br />
must bill the patient, or the patient’s Medigap insurance<br />
plan, for coinsurance, deductible, and charges not covered<br />
by the Medicare Part B program.<br />
In addition to the likely political and patient sat -<br />
isfaction advantages to Medicare participation, there<br />
are also financial and administrative opportunities. <strong>The</strong><br />
most significant are that Medicare fee schedule allowances<br />
are 5% higher for participating physicians, and<br />
assigned Medicare claims filed with Medigap insurance<br />
information are automatically forwarded by Medicare<br />
to supplemental insurance carriers for processing of<br />
coinsurance and deductible charges. 34 A copy of the<br />
Medicare Participating Physician or Supplier Agreement<br />
(Form CMS-460) is available at http://www.cms.hhs.gov/<br />
cmsforms/downloads/cms460.pdf.<br />
Medicare Payment Methodologies for<br />
<strong>Anesthesia</strong> Services<br />
Medicare’s Resource Based Relative Value System<br />
In 1992, Medicare implemented the Resource Based<br />
Relative Value System (RBRVS) that established a<br />
Medicare Fee Schedule (MFS) of national values for each<br />
clinical procedure code. <strong>The</strong> value comprises three relative<br />
value units that represent the physician’s work effort<br />
in rendering the service, the practice’s overhead expenses<br />
for items such as rent, office staff salaries and supplies,<br />
and malpractice insurance premiums. Under RBRVS,<br />
Medicare also implemented a new definition of allowed<br />
charges that paid physicians based on the lesser of the<br />
submitted charge or the new relative value scale feeschedule–based<br />
amount. 35<br />
At the time of the introduction of the MFS in 1992,<br />
<strong>Anesthesiology</strong> had already had a relative value scale for<br />
anesthesia payment in place for 30 years. 36 <strong>The</strong> American<br />
Society of Anesthesiologists (ASA) Relative Value Guide,<br />
adopted almost in its entirety by the HCFA in 1989, uses<br />
values that represent components of anesthesia services:<br />
the base unit value related to the complexity of the service<br />
performed; and the time units based on the actual time<br />
the anesthesiologist spends with a patient.<br />
Note the CMS definition of anesthesia time:<br />
<strong>Anesthesia</strong> time means the time during which an anesthesia<br />
practitioner is present with the patient. It starts when the anesthesia<br />
practitioner begins to prepare the patient for anesthesia<br />
services in the operating room or an equivalent area and ends<br />
when the anesthesia practitioner is no longer furnishing anesthesia<br />
services to the patient, that is, when the patient may be<br />
placed safely under postoperative care. . . . 37<br />
Medicare does not reimburse for modifier units, such<br />
as those designated by the ASA recognizing physical<br />
status, extremes of age, or unusual risk. 38<br />
Medicare reimburses anesthesia services via a separate<br />
methodology under RBRVS that uses the sum of procedure-specific<br />
relative value units and the variable time<br />
units. <strong>The</strong> sum of these units is then multiplied by an<br />
anesthesia-specific conversion factor that is corrected for<br />
geographic cost differences. It was the retention of the<br />
time unit factor in the anesthesia payment methodology<br />
that drove HCFA to create a separate anesthesia conversion<br />
factor under RBRVS.<br />
<strong>The</strong> Medicare Fee Schedule for <strong>Anesthesia</strong> Services<br />
<strong>The</strong> distinction in the MFS for anesthesiologists has<br />
disadvantaged the specialty. A good illustration of the<br />
problem is the differential between Medicare and private<br />
insurance fees for anesthesiologists versus the differential<br />
for other medical and surgical specialists. <strong>The</strong> AMA<br />
reports that Medicare’s conversion factor for physician
22 M.F. Galati and R.D. London<br />
services represents approximately 83% of the conversion<br />
factor paid by private insurers. For anesthesiologists, the<br />
Medicare conversion factor represents less than 40% of<br />
a private insurer’s rate. <strong>The</strong>refore, Medicare payments for<br />
anesthesia services are less than half of Medicare payments<br />
for other medical and surgical services. 39<br />
<strong>The</strong> ASA has raised this issue of disparity in Medicare<br />
fees many times with the AMA/Specialty Society Relative<br />
Value Update Committee (RUC). <strong>The</strong> RUC is the<br />
body charged with reviewing and advising CMS on<br />
updates to work-related relative value units that are<br />
required, by law, at least every 5 years. In the first 5-year<br />
review, HCFA acknowledged the undervaluation and<br />
approved a nearly 23% increase in work values for anesthesia<br />
procedures, effective January 1, 1997. 40 In the fee<br />
schedule effective after the second 5-year review, CMS<br />
again received endorsements for reconsideration of the<br />
anesthesia work relative value units but responded with<br />
an insignificant adjustment. 41<br />
<strong>The</strong> MFS is often referenced by private insurers as a<br />
standard in setting physician reimbursement rates. It is<br />
also common for physicians from other specialties, who<br />
enjoy a more favorable Medicare-to-private insurer fee<br />
ratio, to suggest the MFS as a proxy for valuing physician<br />
services. This often occurs during joint negotiations such<br />
as those used in dividing fees for contracts paid on a<br />
global basis to physician groups. Anesthesiologists are<br />
disadvantaged when the MFS is used in this manner. It<br />
is, therefore, important for anesthesiologists to remain<br />
active in the discussion of these physician payment disparities<br />
and to work to educate others and thereby mitigate<br />
the effect of these disparities in the Medicare system<br />
and beyond.<br />
Proposed Changes to the <strong>Anesthesia</strong><br />
Payment Methodology<br />
Anesthesiologists are involved in these important public<br />
policy debates via the activities of their professional<br />
society, the ASA, and the ASA Political Action Committee.<br />
In late 2003, the ASA charged the “Task Force to<br />
Study Payment Methodology” with studying the relationship<br />
of the anesthesiology payment methodology to<br />
Medicare’s relative value payment system. <strong>The</strong> Task Force<br />
projected the threat of decreasing revenues from the<br />
ongoing undervaluation of anesthesia services under<br />
Medicare, the adoption of the MFS and payment policies<br />
by private insurers, and the projected increase in numbers<br />
of Medicare beneficiaries in the United States.<br />
<strong>The</strong> Task Force estimated that, with Medicare beneficiaries<br />
representing approximately 30% of anesthesia<br />
services nationwide, a blended conversion factor of<br />
Medicare and private insurers is $40.25. When Medicare<br />
accounts for 50% of services, the blended conversion<br />
factor will decrease to $33.75. Furthermore, if the MFS<br />
becomes the model for a single-payer system, they predict<br />
that the blended conversion factor will decrease to $17.50<br />
(personal communication, Karin Bierstein, Esq., American<br />
Society of Anesthesiologists, November 30, 2004).<br />
<strong>The</strong> Task Force has been exploring a flat fee payment<br />
methodology that would capture elements both of the<br />
time and the complexity of care for a continuous period<br />
of anesthesia for each operative period, involving one or<br />
more surgical procedures. This methodology would rely<br />
on a greatly expanded anesthesia code set that would<br />
incorporate an average anesthesia time representative of<br />
procedures performed in both the private practice and<br />
academic settings.<br />
<strong>The</strong> Task Force recommendations for a new Medicare<br />
anesthesia payment methodology will be presented to the<br />
RUC and, if approved, will be reflected in future fee<br />
schedule revisions. <strong>The</strong> principles of the new methodology<br />
were announced in the following Task Force resolution<br />
passed by the ASA House of Delegates in October<br />
2004:<br />
RESOLVED, That the Executive Committee in consultation<br />
with the Administrative Council is authorized to propose a<br />
restructuring of Medicare payments for anesthesia services<br />
based on the following principles:<br />
That any new coding system must accurately reflect both the<br />
complexity and duration of the associated surgical procedures<br />
to compensate for the elimination of separately reported anesthesia<br />
time;<br />
That the inevitable influence of a uniform Medicare conversion<br />
factor on payment rates in the private sector be thoroughly<br />
considered; and<br />
That any transition to a uniform Medicare conversion factor<br />
must be based on a value sufficient to protect the specialty, as<br />
a whole and in aggregate, from economic damage.<br />
<strong>The</strong>se resolutions were referred for further study, and<br />
the ASA does not expect that a modification in the<br />
anesthesia payment methodology will occur in the near<br />
term. 42<br />
<strong>The</strong> Sustainable Growth Rate Formula<br />
<strong>The</strong> CMS uses a Sustainable Growth Rate (SGR) system<br />
to determine annual changes in the physician fee schedule.<br />
This system compares physician spending based on the<br />
volume and intensity of services provided against spending<br />
targets tied to inflation and the gross domestic product,<br />
and adjusts physician fee schedules accordingly to meet<br />
the targets. In 2002, this process resulted in a 5.4% reduction<br />
in physician fees, and the need for ongoing reductions<br />
was predicted up through 2016. This triggered congressional<br />
interventions that overrode the SGR system in the<br />
years 2003, 2004, and 2005 and mandated a Government<br />
Accounting Office (GAO) review of the problem. 43<br />
Anesthesiologists have a large stake in securing the<br />
success of these efforts, and other efforts to reform the
2. Demographics and Economics of <strong>Geriatric</strong> Patient Care 23<br />
Medicare payment methodology specific to anesthesia<br />
services. However, it is important to note that unless<br />
there is modification of the SGR statute, any updates to<br />
the MFS must meet spending targets and, therefore,<br />
where one physician group gains, others must lose.<br />
In a period when the Medicare program faces many<br />
economic challenges, it is unlikely that the interests of<br />
any one group of physicians will prevail without a strong,<br />
well-targeted political effort. A focus of this political<br />
effort in the future will be the discussion of the looming<br />
problem of access to anesthesia care by the ever-growing<br />
numbers of Medicare beneficiaries.<br />
<strong>The</strong> <strong>Anesthesia</strong> Care Team<br />
<strong>The</strong>re are a variety of ways for anesthesiologists to<br />
provide services for reimbursement under Part B of the<br />
Medicare program. Medicare reimburses the services of<br />
an anesthesiologist when the physician personally provides<br />
them or if an anesthesia care team provides them<br />
under medical direction or supervision. <strong>Anesthesia</strong> claims<br />
modifiers are used to denote whether services were<br />
provided personally, “medically directed,” or “medically<br />
supervised.” Medicare reduces reimbursement based on<br />
the series of claims modifiers that denote how the services<br />
were delivered (Table 2-1).<br />
<strong>The</strong> anesthesia care team is defined as an anesthesiologist<br />
working with any of the following professionals:<br />
CRNAs<br />
AAs<br />
Residents or interns<br />
Student Nurse Anesthetists (SNAs) 44<br />
In most cases, when an anesthesiologist and a CRNA<br />
are providing a single anesthesia service, Medicare<br />
recognizes the service as if personally performed by the<br />
anesthesiologist.<br />
Medical Direction Versus Supervision of<br />
Concurrent Procedures<br />
When an anesthesiologist is involved in directing up to<br />
four concurrent procedures, Medicare recognizes the services<br />
as concurrent medical direction and sets out specific<br />
guidelines for documentation and reimbursement of<br />
these services. (See Compliance section for documentation<br />
requirements.)<br />
Anesthesiologists are allowed to furnish additional<br />
services to other patients under an exception to the four<br />
concurrent case limits. This exception, which varies by<br />
state, generally applies to the following services, if they<br />
do not “substantially diminish the scope of control exercised<br />
by the physician” providing the medical direction:<br />
Addressing an emergency of short duration in the immediate<br />
area;<br />
Administering an epidural or caudal anesthetic to ease<br />
labor pain;<br />
Providing periodic, rather than continuous monitoring, of<br />
an obstetric patient;<br />
Receiving patients entering the operating suite for the<br />
next surgery;<br />
Discharging patients in the recovery room; or<br />
Handling scheduling matters. 44<br />
When services are provided in excess of four concurrent<br />
cases and the allowed exceptions, the services will<br />
fail to meet the medical direction requirements. <strong>The</strong>se<br />
services are provided under what Medicare terms medical<br />
“supervision” and are reimbursed to the physician at a<br />
fraction of the MFS allowable through limits in billing for<br />
base and time units. Under the supervision requirements,<br />
Table 2-1. CMS <strong>Anesthesia</strong> Care Team Claims Modifiers Matrix.<br />
Modifier CMS definition Payment % of allowable to provider<br />
AA <strong>Anesthesia</strong> services performed personally by anesthesiologist 100% to anesthesiologist<br />
AA/GC <strong>Anesthesia</strong> services performed personally by anesthesiologist with resident 100% to anesthesiologist<br />
involvement<br />
QK Medical direction of up to 4 concurrent anesthesia procedures involving 50% to anesthesiologist<br />
qualified individuals<br />
50% to qualified provider*<br />
QK/GC Medical direction of up to 4 concurrent anesthesia procedures involving 50% to anesthesiologist<br />
2–4 residents<br />
QX CRNA service with anesthesiologist medical direction (reported by CRNA) 50% to CRNA<br />
QY Medical direction of CRNA by anesthesiologist for 1 case (reported by 50% to anesthesiologist<br />
anesthesiologist)<br />
AD Medical supervision by a physician; more than 4 concurrent anesthesia 3 base units, no time units. 1 unit if<br />
procedures<br />
anesthesiologist documented presence at<br />
induction<br />
Source: Author’s compilation from Medicare Carriers Manual, Part 3: Claims Process. Transmittal 1690, Section 4830, Claims for <strong>Anesthesia</strong> Services<br />
Performed on and after January 1, 1992. Department of Health and Human Services, <strong>The</strong> Health Care Financing Administration. Published<br />
January 5, 2001.<br />
*Residents are not qualified for reimbursement.
24 M.F. Galati and R.D. London<br />
the physician must still ensure that a qualified individual<br />
performs any procedure in which they do not personally<br />
participate. 45<br />
Requirements of the Attending<br />
Physician Relationship<br />
Physicians in academic practice fall under additional<br />
Medicare requirements that govern the “attending physician”<br />
relationship. This relationship exists when an attending<br />
anesthesiologist provides care to a patient in a teaching<br />
hospital involving anesthesia residents.<br />
In 1992, when RBRVS was introduced, a new rule was<br />
announced that was to eliminate the practice of full reimbursement<br />
for an anesthesiologist medically directing<br />
two concurrent cases with anesthesia residents. <strong>The</strong> ASA<br />
was able to persuade Medicare to postpone implementation<br />
of the new rules until 1994; however, the impact of<br />
this change has been significant. <strong>The</strong> ASA estimates that<br />
the cost to academic anesthesiology programs of this<br />
change alone exceeds $50 million annually. 46 <strong>The</strong> ASA<br />
has been working to encourage CMS to restore full<br />
payment for two concurrent teaching cases.<br />
In January 2004, CMS took an interim step toward<br />
changes in the reimbursement guidelines for medical<br />
direction of residents. <strong>The</strong> new rule expands billing<br />
options for teaching anesthesiologists who are involved<br />
in providing care with residents for two concurrent anesthesia<br />
cases. In the new ruling, anesthesiologists can<br />
choose to bill the usual base units and anesthesia time<br />
only for the period they are actually present with the<br />
resident if they are present throughout pre- and postanesthesia<br />
care and if this is documented.<br />
In the rule, CMS has also included language that allows<br />
the attending anesthesiologist to determine if a request<br />
for payment of the full time payment for both cases is<br />
warranted. This request must be provided with written<br />
documentation that he/she spent “sufficient time” with<br />
each patient considering factors such as patient condition,<br />
residents’ experience, proximity of the operating rooms,<br />
and the actual time the attending anesthesiologist spent<br />
in each operating room in making the determination. 47<br />
Anesthesiologists choosing to use the interim rule as a<br />
revenue opportunity must weigh potential benefits against<br />
the compliance risks and the investments in faculty education<br />
and system modifications needed to support a new<br />
documentation and billing process.<br />
Compliance Issues<br />
All physicians who interact with the Medicare program<br />
are obligated to assure that their business practices<br />
conform to the requirements of the program. This can be<br />
a daunting task because although a busy participating<br />
physician can delegate Medicare transaction authority to<br />
others, he/she retains all of the responsibility and risks<br />
related to the actions of his/her agents. Furthermore, the<br />
stakes for providers are high. Physicians who are found<br />
to be in violation of Medicare regulations can suffer both<br />
civil and criminal penalties as well as exclusion from the<br />
program. Physician practices can minimize the risks by<br />
adopting comprehensive compliance plans and assuring<br />
thorough internal controls, and training for all physicians<br />
and staff.<br />
<strong>The</strong> Office of the Inspector General (OIG) does not<br />
mandate the adoption of compliance programs, but they<br />
have formulated seven fundamental elements of an effective<br />
compliance program. <strong>The</strong>se elements are:<br />
• Implement written policies, procedures, and standards<br />
of conduct<br />
• Designate a compliance officer and compliance committee<br />
(e.g., a billing clerk and physician in a small<br />
practice)<br />
• Conduct effective training and education<br />
• Develop effective lines of communication<br />
• Enforce standards through well-publicized disciplinary<br />
guidelines<br />
• Conduct internal monitoring and auditing<br />
• Respond promptly to detected offenses and develop<br />
corrective action plans 48<br />
Anesthesiologists should consult with their compliance<br />
officers to gain what should be an in-depth understanding<br />
of their obligations as providers in the Medicare program.<br />
An introduction to some of the key compliance issues<br />
affecting anesthesia practice, including reassignment of<br />
benefits, Medicare fraud and abuse initiatives, and medical<br />
record documentation follows.<br />
For further information on compliance programs, one<br />
should consult the OIG postings in the Federal Register<br />
and on the OIG Web site at http://oig.hhs.gov/fraud/<br />
complianceguidance.html.<br />
Reassignment of Medicare Benefits<br />
Anesthesiologists who provide care to Medicare beneficiaries<br />
undertake responsibility for compliance with<br />
myriad complex and sometimes conflicting regulations.<br />
Anesthesiologists who practice in a group or academic<br />
setting, where administrative duties for billing and collections<br />
are delegated and Medicare payments are frequently<br />
reassigned to another entity, should be best informed of<br />
these responsibilities.<br />
When a physician reassigns benefits under the Medicare<br />
program, they legally authorize another person or<br />
entity to bill Medicare on their behalf and to receive<br />
payments that would otherwise be sent directly to them.<br />
However, despite this written delegation of authority,<br />
the physician retains all responsibility for ensuring that<br />
the claims made on their behalf are in full compliance
2. Demographics and Economics of <strong>Geriatric</strong> Patient Care 25<br />
with Medicare regulations. In addition, the physician<br />
retains responsibility for assuring that their agent meets<br />
all confidentiality obligations and other state and federal<br />
regulations.<br />
Even the best-intentioned physician may encounter<br />
difficulties in determining how to meet his/her obligations<br />
for compliance with Medicare regulations. <strong>The</strong><br />
GAO tested the accuracy of carriers’ responses to inquiries<br />
in a telephone audit. <strong>The</strong> GAO asked staff at the<br />
Medicare carriers to respond to “frequently asked questions”<br />
concerning physician billing procedures that were<br />
taken from the carriers’ own Web sites. <strong>The</strong> GAO survey<br />
report concluded that physicians who do call their carriers<br />
with questions would “more often than not receive<br />
wrong or inaccurate answers.” <strong>The</strong>se problems were<br />
attributed to limits on resources for information system<br />
modernization and oversight activities, and limits on<br />
CMS’s authority imposed by the Congress and Executive<br />
branches. 49<br />
Medicare Fraud and Abuse<br />
Although the federal government has chosen to limit<br />
CMS resources for facilitating its administrative mission,<br />
it has significantly increased resources for the investigation<br />
of fraud and abuse. Public administration experts<br />
have noted that these resources could be better spent on<br />
preventive measures such as improved management of<br />
the program and effective measures to monitor and deter<br />
inappropriate payments, thereby minimizing the need<br />
for enforcement. However, this has not occurred and,<br />
as of 2000, CMS spent more than 25% of its total administrative<br />
expenses in its campaign against fraud and<br />
abuse. 49<br />
Many federal agencies are involved in protecting the<br />
Medicare program and ensuring provider compliance<br />
with all regulations. <strong>The</strong> OIG in the Department of<br />
Health and Human Services investigates suspected Medicare<br />
fraud or abuse and develops cases against providers.<br />
It has the authority to audit and inspect CMS programs<br />
and to act against individual providers with civil money<br />
penalties and/or exclusion from participation in all federal<br />
health care programs. <strong>The</strong> OIG also has authority to refer<br />
cases to the United States Department of Justice for<br />
criminal or civil action. 50 In its 2006 semiannual report,<br />
the OIG evidenced an active role in combating waste,<br />
fraud, and abuse, citing savings of more than $38.2 billion,<br />
3425 exclusions, 472 criminal actions against individuals<br />
and entities, and 272 civil actions. 51<br />
Medicare defines fraud as “the intentional deception<br />
or misrepresentation that an individual knows to be false<br />
or does not believe to be true and makes, knowing that<br />
the deception could result in some unauthorized benefit<br />
to himself/herself or some other person.” Abuse relates<br />
to practices that directly or indirectly result in unnecessary<br />
costs to the Medicare program. It is similar to fraud<br />
but is found when there is no evidence that the acts were<br />
committed knowingly, willfully, and intentionally. 52<br />
Some examples of fraud that should be immediately<br />
apparent to providers include activities such as the<br />
falsification of records, billing for services that were not<br />
furnished, or misrepresenting the type of service provided<br />
by using inappropriate codes. However, other<br />
actions that also constitute fraud and abuse may not be<br />
as apparent to providers. <strong>The</strong>se include providing incentives<br />
to Medicare patients not provided to other patients<br />
such as the routine waiving or discounting of patient<br />
coinsurance and deductible payments. Other actions<br />
include billing Medicare on a higher fee schedule than<br />
other patients, breaching the agreements to accept assignment<br />
or participate in the Medicare program, or failing<br />
to provide timely refund of overpayments made by Medicare<br />
and beneficiaries. 52<br />
Physicians at Teaching Hospitals: Office of the<br />
Inspector General Initiative<br />
Physicians in academic practice have been made most<br />
keenly aware of government efforts to enforce compliance<br />
with Medicare rules. Over the past decade, the government<br />
recovered $149 million from 15 universities that<br />
failed to document compliance with Medicare payment<br />
policies related to attending physician supervision of services<br />
provided with resident involvement. 49<br />
<strong>The</strong> Physicians at Teaching Hospitals (P.A.T.H.) initiative<br />
of the OIG has had long-lasting and costly effects on<br />
academic practices. Physician groups that paid settlements<br />
or were subject to civil or criminal prosecution<br />
were required to enter into multi-year Institutional Compliance<br />
Agreements with the federal government. <strong>The</strong>se<br />
agreements impose requirements that closely follow the<br />
structure of a compliance program but can be more stringent.<br />
53 <strong>The</strong>y obligate practices to develop and adhere to<br />
a rigorous set of compliance standards involving audits<br />
of physician billing practices and annual physician and<br />
staff education, under threat of additional penalties.<br />
AHCs have reported that annual compliance program<br />
costs, after P.A.T.H. settlement, are absorbing millions<br />
of dollars. 54<br />
Documentation Requirements<br />
Medical record documentation is the primary source<br />
used for judging compliance with Medicare regulations.<br />
Documentation should be timely and must support the<br />
medical necessity of the service as well as the level and<br />
scope of service provided. As with all medical record<br />
documentation, it must be legible and signed by the<br />
provider. Bills should not be submitted unless adequate<br />
documentation exists for the services.
26 M.F. Galati and R.D. London<br />
Documentation of <strong>Anesthesia</strong> Time<br />
<strong>The</strong> prominence of time in the Medicare reimbursement<br />
methodology for anesthesiologist services drives documentation<br />
requirements. Since January 1, 1994, Medicare<br />
has reimbursed anesthesia time based on the actual<br />
number of minutes of anesthesia provided calculated in<br />
fractions of 15-minute units, rounded to one decimal<br />
place. 37 This standard for the precise documentation and<br />
reporting of anesthesia time presents challenges, especially<br />
in practices without automated anesthesia recordkeeping<br />
systems.<br />
Unsynchronized timepieces within the operating room<br />
suite can create disparities in timekeeping documentation<br />
as recorded by the anesthesiologist and other<br />
members of the surgical team such as nurses, perfusionists,<br />
and surgeons. Unsynchronized timepieces between<br />
anesthetizing locations and a lack of diligence can also<br />
cause an anesthesiologist to create the appearance of<br />
overlap of anesthesia services (i.e., concurrency) when<br />
indeed the services were provided consecutively. <strong>The</strong>se<br />
discrepancies frequently become apparent upon subsequent<br />
audit of the documentation when it is more difficult<br />
to initiate corrections.<br />
Documentation of Medical Direction<br />
When an anesthesiologist is involved in directing up to<br />
four concurrent procedures, Medicare recognizes the services<br />
as concurrent medical direction.<br />
Documentation of concurrent medical direction must<br />
support the physician’s completion of “7 steps.” This documentation<br />
evidences that the physician:<br />
Performs a preanesthesia examination and evaluation;<br />
Prescribes the anesthesia plan;<br />
Personally participates in the most demanding procedures<br />
in the anesthesia plan, including, if applicable,<br />
induction and emergence;<br />
Ensures that a qualified individual performs any procedures<br />
in the anesthesia plan that he or she does not<br />
perform;<br />
Monitors the course of anesthesia administration at frequent<br />
intervals;<br />
Remains physically present and available for immediate<br />
diagnosis and treatment of emergencies; and<br />
Provides indicated postanesthesia care. 44<br />
In May 2004, CMS issued new interpretive guidelines<br />
for surveyors regarding the documentation of the inpatient<br />
postanesthesia assessment as required in the Hospital<br />
Conditions of Participation for the Medicare Program.<br />
<strong>The</strong> revision allows the postanesthesia follow-up to be<br />
performed and documented by the individual who administered<br />
the anesthesia, or by a delegated practitioner who<br />
is qualified to administer anesthesia. 55<br />
Documentation by Teaching Physicians<br />
In January 1997, Medicare imposed a requirement for use<br />
of the “GC” claim modifier to denote the involvement of<br />
residents in the delivery of anesthesia services and to<br />
certify that the teaching anesthesiologist was present<br />
during key portions of the service and immediately<br />
available during other parts of the service. In 1999, CMS<br />
extended the requirement to include a written attestation<br />
from the attending physician that these requirements<br />
were met. 56<br />
In November 2002, CMS implemented revised guidelines<br />
governing the documentation requirements for<br />
teaching physicians who care for patients with the involvement<br />
of resident physicians. <strong>The</strong>se requirements restrict<br />
payment for teaching physician services to those that<br />
support the presence of the teaching physician during key<br />
portions of an anesthesia procedure and during the entire<br />
time for separately reimbursable procedures such as line<br />
and catheter insertions.<br />
<strong>The</strong> most complex of these guidelines govern the<br />
documentation of teaching physician involvement with<br />
residents in the provision of evaluation and management<br />
services. Interested physicians should consult the Medicare<br />
Carriers Manual, Section 15016 for specifics of these<br />
guidelines. However, there are important general principles<br />
that the anesthesiologist should follow in all cases<br />
whether or not the resident and teaching physician services<br />
are provided contemporaneously:<br />
• Teaching physicians cannot evidence their presence<br />
and participation via documentation of these activities<br />
by the resident or by “countersigning” a resident’s note.<br />
<strong>The</strong>y may reference the resident’s note in their own<br />
note, but must independently document presence and<br />
participation in the critical portions of the service.<br />
• <strong>The</strong> composite of the teaching physician’s note and the<br />
resident’s note may be used to support the medical<br />
necessity and level of service billed. 57<br />
Physician providers must be proactive in assuring compliance<br />
with the complex and dynamic requirements of<br />
participation in the Medicare program. Development of<br />
a compliance program, review of physician billing and<br />
documentation, and ongoing education and training of<br />
providers and staff will help physicians minimize compliance<br />
risk.<br />
Summary<br />
Medicare is the primary health plan serving our nation’s<br />
elderly, an important source of revenue for physician and<br />
hospital providers, and a major underwriter of medical<br />
education and charity care in the United States. <strong>The</strong><br />
program will experience growing, annual deficits start -<br />
ing in 2010 when Medicare costs are first predicted to
2. Demographics and Economics of <strong>Geriatric</strong> Patient Care 27<br />
exceed financing sources as the baby boomers begin to<br />
retire. In the interim, strategies for dealing with the<br />
impending crisis in Medicare will be a continual source<br />
of debate and providers should be represented in the<br />
discussions.<br />
A large majority of anesthesiologists in the United<br />
States are enrolled as participating providers in the Medicare<br />
program. Many of the rules and regulations governing<br />
their interactions with the program are unique to the<br />
practice of anesthesiology and have significant implications<br />
for how clinical and business operations are conducted<br />
and whether, indeed, participation remains a<br />
viable strategy for anesthesiologists in the future. <strong>Geriatric</strong><br />
anesthesiologists, by virtue of their subspecialty focus,<br />
should be best informed of Medicare policy issues and<br />
should participate in ongoing discussions to reshape<br />
Medicare as it enters an uncertain future.<br />
References<br />
1. Corning PA. <strong>The</strong> evolution of Medicare . . . from idea to<br />
law. Available at: http://www.ssa.gov/history/. Accessed<br />
September 28, 2004.<br />
2. Gluck MG, Reno V, eds. Reflections on Implementing<br />
Medicare. Washington, DC: National Academy of Social<br />
Insurance; 2001:43.<br />
3. Marmor TR. <strong>The</strong> Politics of Medicare. Chicago: Aldine Publishing;<br />
1973.<br />
4. Gluck MG, Reno V, eds. Reflections on Implementing<br />
Medicare. Washington, DC: National Academy of Social<br />
Insurance; January 2001:iii.<br />
5. U.S. Social Security Administration. http://www.ssa.gov/<br />
history/. Accessed September 28, 2004.<br />
6. <strong>The</strong> Centers for Medicare and Medicaid Services. http://<br />
ww.cms.hhs.gov/MedicareEnRpts. Accessed October 17,<br />
2004.<br />
7. Iglehart JK. <strong>The</strong> American health care system: Medicare.<br />
Health Policy Rep 1999;340:327–332.<br />
8. Moon M. Health policy 2001: Medicare. N Engl J Med 2001;<br />
344:928–931.<br />
9. Lubitz J, Beebe J, Baker C. Longevity and Medicare expenditures.<br />
N Engl J Med 1995;332:999–1003.<br />
10. U.S. Census Bureau. www.census.gov/population/www/<br />
projections/natdet-D1A.html. Accessed October 18, 2004.<br />
11. <strong>The</strong> Centers for Medicare and Medicaid Services.<br />
http://ww.cms.hhs.gov/publications/trusteesreport. Accessed<br />
October 18, 2004.<br />
12. http://www.AARP.org/econ/boomer. Accessed October 9,<br />
2004.<br />
13. Center for Medicare Education. http://www.medicareed.<br />
org/resources. Accessed October 18, 2004.<br />
14. Estimates of medicare beneficiaries’ out-of pocket drug<br />
spending in 2006. Available at: http://www.kff.org. Accessed<br />
November 24, 2004.<br />
15. <strong>The</strong> Medicare prescription drug benefit. Available at: http://<br />
www.kff.org/medicare. Accessed December 8, 2006.<br />
16. Rice T, Bernstein J. Supplemental Health Insurance<br />
for Medicare Beneficiaries. Medicare Brief No. 6.<br />
Available at: http://www.nasi.org/Medicare/Briefs/medbr6.<br />
htm. Washington, DC: National Academy of Social Insurance;<br />
November 1999.<br />
17. Rowland D, Feder J, Seliger Keenan P. Managed care for<br />
low-income elderly people. Generations: Q J Am Soc Aging<br />
1998(Summer);22:45.<br />
18. Kaiser Family Foundation and Health Research and Educational<br />
Trust. Employer health benefits: 2006 summary<br />
of findings. Available at http://www.kff.org/insurance/7527/<br />
upload/7528.pdf. Washington, DC. Accessed December 8,<br />
2006.<br />
19. Families USA Foundation. Shortchanged: Billions With -<br />
held from Medicare Beneficiaries. Publication No. 98-103.<br />
Washington, DC. July 1998. p. 1.<br />
20. Piette JD, Heisler M, Wagner TH. Cost-related medication<br />
underuse. Arch Intern Med 2004;164:1749–1755.<br />
21. Poisal JA, Murray L. Growing differences between Medicare<br />
beneficiaries with and without drug coverage. Health<br />
Aff 2001;20:74–85.<br />
22. Davis M, Poisal J, Chulis G, et al. Prescription drug coverage,<br />
utilization, and spending among Medicare beneficiaries.<br />
Health Aff 1999;18:231–243.<br />
23. National Institute for Health Care Management Research<br />
and Education Foundation. Factors affecting the growth of<br />
prescription drug expenditures. Available at http://www.<br />
hihcm.org. Accessed July 9, 1999.<br />
24. <strong>The</strong> Commonwealth Fund. Caught in Between: Prescription<br />
Drug Coverage of Medicare Beneficiaries Near Poverty.<br />
Issue Brief No. 669. New York; August 2003.<br />
25. Iglehart J. <strong>The</strong> new Medicare prescription-drug benefit—a<br />
pure power play. N Engl J Med 2004;350:826–833.<br />
26. <strong>The</strong> Centers for Medicare and Medicaid Services. http://<br />
www.cms.hhs.gov/charts/series/sec3-C.pdf. Accessed December<br />
3, 2004.<br />
27. National Academy of Science. <strong>The</strong> Roles of Academic<br />
Health Centers in the 21st Century: A Workshop Summary.<br />
Washington, DC; 2002.<br />
28. <strong>The</strong> Centers for Medicare and Medicaid Services. http://<br />
www.cms.hhs.gov/media. January 31, 2005, release accessed<br />
February 7, 2005.<br />
29. Vuletich M. Pay for performance: is it right for an academic<br />
practice? MGMA Connex 2005;69.<br />
30. <strong>The</strong> Centers for Medicare and Medicaid Services. http://<br />
www.cms.hhs.gov/researchers/pubs/datacompendium/2003.<br />
Accessed October 18, 2004.<br />
31. <strong>The</strong> Centers for Medicare and Medicaid Services. http://<br />
www.cms.hhs.gov/faca/ppac/oral_asa.pdf. Accessed November<br />
29, 2004.<br />
32. <strong>The</strong> Centers for Medicare and Medicaid Services. http://<br />
www.cms.hs.gov/manuals/14_car/3btoc.asp. Chapter 17.<br />
Accessed December 6, 2004.<br />
33. <strong>The</strong> Centers for Medicare and Medicaid Services http://<br />
www.cms.hhs.gov/about/regions/professionals.asp. Accessed<br />
December 6, 2004.<br />
34. Centers for Medicare and Medicaid Services. Medicare<br />
Resident and New Physician Guide: Helping Health Care<br />
Professionals Navigate Medicare. 7th ed. Baltimore: Centers<br />
for Medicare and Medicaid Services; August 2003:16.<br />
35. <strong>The</strong> Centers for Medicare and Medicaid Services www.cms.<br />
hhs.gov/publications/overview. Accessed November 29, 2004.
28 M.F. Galati and R.D. London<br />
36. Ogunnaike BO, Giesecke AH. ASA Relative Value Guide<br />
(RVG): a defining moment in fair pricing of medical services.<br />
ASA Newslett 2004;68:15–17.<br />
37. Medicare carriers’ manual. Part 3. Chapter 15, Section G.<br />
Rev. 1690 p. 15. Available at: http://www.cms.hhs.gov/<br />
manuals. Accessed November 1, 2004.<br />
38. <strong>The</strong> Centers for Medicare and Medicaid Services.<br />
http://www.cms.hhs.gov/physicians/pfs/wrvu-ch1.asp.<br />
Accessed November 29, 2004.<br />
39. Bierstein K. Medicare is still the wrong benchmark. ASA<br />
Newslett 2002;66:25–27.<br />
40. Scott M. <strong>The</strong> American Society of Anesthesiologists. http://<br />
www.asahq.org/newsletters/1997/-1_97/washington_0197.<br />
html. Accessed October 12, 2004.<br />
41. <strong>The</strong> Centers for Medicare and Medicaid Services. http://<br />
www.cms.hhs.gov/faca/ppac/oral_asa.pdf. Accessed November<br />
29, 2004.<br />
42. Novak LC, Cohen NA. <strong>The</strong> American Society of Anesthesiologists.<br />
http://www.asahq.org/Newsletters/2005/09-05/<br />
whatsNew09_05.html. Accessed December 8, 2006.<br />
43. U.S. Government Accountability Office. http://www.gao.<br />
gov/docsearch/abstract.php?rptno=GAO-05-85. Accessed<br />
October 20, 2004.<br />
44. Carrier’s manual. Part 3. Chapter 8. Available at: http://www.<br />
cms.hhs.gov/manuals/14_car/3b8000.asp. Accessed November<br />
1, 2004.<br />
45. Carrier’s manual. Part 3. Chapter 8. Revision 1690, Section<br />
15018. Fee schedule for physicians’ services. Available at:<br />
http://www.cms.hhs.gov/manuals/pm_trans/R1690B3.pdf.<br />
Accessed December 6, 2004.<br />
46. Hannenberg A, Scott M. <strong>The</strong> American Society of Anesthesiologists.<br />
http://www.asahq.org/Newsletters/2002/12_02/<br />
hannenberg.html. Accessed October 12, 2004.<br />
47. <strong>The</strong> Centers for Medicare and Medicaid Services. http:///<br />
www.cms.hhs.gov/manuals/ CMS transmittal 34, December<br />
24, 2003. Accessed December 7, 2004, and 8310 conditions<br />
for payment of charges—anesthesiology services, rev. 1287/<br />
pp. 8–53. Accessed November 1, 2004.<br />
48. <strong>The</strong> Centers for Medicare and Medicaid Services. http://<br />
www.cms.hhs.gov/medlearn/mrnp-guide.pdf. p. 121. Accessed<br />
October 17, 2004.<br />
49. Iglehart J. <strong>The</strong> Centers for Medicare and Medicaid Services.<br />
N Engl J Med 2001;345:1920–1924.<br />
50. <strong>The</strong> Centers for Medicare and Medicaid Services. http://<br />
www.cms.hhs.gov/medlearn/mrnp-guide.pdf. p. 9. Acc essed<br />
October 17, 2004.<br />
51. Office of Inspector General. http://www.oig.hhs.gov/<br />
publications/docs/semiannual/2006. Accessed December 8,<br />
2006.<br />
52. <strong>The</strong> Centers for Medicare and Medicaid Services. http://<br />
www.cms.hhs.gov/medlearn/mrnp-guide.pdf. pp. 124–126.<br />
Accessed October 17, 2004.<br />
53. <strong>The</strong> Centers for Medicare and Medicaid Services. http://<br />
www.cms.hhs.gov/medlearn/mrnp-guide.pdf. pp. 131–132.<br />
Accessed October 17, 2004.<br />
54. Swann M. Fast-tracking compliance training in academic<br />
practices. Am Coll Med Pract Exec Coll Rev 1999;16:<br />
61–88.<br />
55. <strong>The</strong> Centers for Medicare and Medicaid Services. Interpretive<br />
guidelines §482.52(b)(4). Available at: http://www.cms.<br />
hhs.gov/manuals/107_som/som107_appendixtoc.asp.<br />
Accessed January 31, 2005.<br />
56. <strong>The</strong> Centers for Medicare and Medicaid Services. http://<br />
www.cms.hhs.gov/manuals/. CMS transmittals 1690 and<br />
1723, January 5, 2001 and September 26, 2001. Accessed<br />
November 1, 2004.<br />
57. <strong>The</strong> Centers for Medicare and Medicaid Services. http://<br />
www.cms.hhs.gov/medlearn/mrnp-guide.pdf. pp. 134–135.<br />
Accessed October 17, 2004.
3<br />
<strong>The</strong>ories of Aging<br />
Stanley Muravchick<br />
“Gerontology” refers to the application of the various<br />
scientific disciplines to the study of aging. Aging manifests<br />
itself in most organisms as a gradual decline in the<br />
capacity to maintain anabolic processes or to respond to<br />
environmental change. Degenerative changes in both the<br />
physical structure and the functional capacity of organs<br />
and tissues are the clinical characteristics of human aging.<br />
In all species, regardless of how aging makes itself apparent,<br />
the implied consequence of aging is an increased<br />
probability of death as a function of time.<br />
Longevity can be expressed either in terms of lifespan<br />
or life expectancy (Figure 3-1). Lifespan is an idealized,<br />
species-unique parameter that quantifies maximum<br />
attainable age under optimal environmental conditions.<br />
Life expectancy represents an empirical estimate of typical<br />
longevity under prevailing or predicted circumstances.<br />
Increased life expectancy is therefore a socioeconomic,<br />
not a biologic, phenomenon. Consequently, biogerontologists<br />
usually limit the scope of their investigations to the<br />
physiologic and biochemical mechanisms of aging and to<br />
those biologic factors that determine lifespan.<br />
Concepts of Aging<br />
It is clear that genetics are intrinsically and fundamentally<br />
involved in aging and therefore in longevity, but<br />
exactly how this occurs is only now being established.<br />
Almost a century ago, a controversial and apparently<br />
flawed study of chick fibroblasts cells grown in vitro<br />
suggested that immortality might be achievable in the<br />
absence of all noxious or detrimental environmental<br />
influences. 1 However, it now seems that freedom from<br />
senescence may be possible only for cancer cells, not for<br />
fully differentiated cells or functional tissues. 2 <strong>The</strong>refore,<br />
at least for the foreseeable future, human aging and death<br />
are inevitable realities.<br />
<strong>The</strong> precise mechanisms that underlie the aging process<br />
and ultimately determine lifespan in biologic systems<br />
remain unknown. To date, no single theory of aging has<br />
explained satisfactorily all the observed patterns of<br />
human senescence or accounted for the differences<br />
between human aging and the aging of other species. 3 In<br />
general, however, theories of aging fall into two major<br />
categories. One category encompasses nonrandom,<br />
predictable, and centrally determined or preprogrammed<br />
processes. <strong>The</strong> other grouping includes several theories<br />
that describe random or “stochastic” mechanisms.<br />
Programmed Aging<br />
<strong>The</strong>ories of programmed or predetermined aging are<br />
similar in that they invoke a common theme of a “biologic<br />
clock” or “life pacemaker” that confers the unique<br />
longevity of each species. For example, there is good correlation<br />
between species lifespan and the number of cell<br />
doublings that can be expected when cells of a single type<br />
such as an embryonic fibroblast are taken from a wide<br />
variety of animals and grown in culture. 4 This suggests<br />
that there may be an intracellular mechanism that limits<br />
reproductive capacity, or perhaps there is a section of the<br />
nuclear genome that provides a species-specific phenotype<br />
dedicated to lifespan. Similarly, the “codon restriction<br />
theory” suggests that there are programmed changes<br />
in the capacity of cells that vary the kinds of proteins that<br />
will be generated during different stages of life. 5<br />
If either of these theories are valid, experimental<br />
manipulation of the “pacemaker” or “clock” sections of<br />
the genome should produce dramatic changes in lifespan.<br />
Every genomic segment is, however, also subject to the<br />
processes of natural selection that affect the entire<br />
genome. 6 <strong>The</strong>re is little selective evolutionary advantage<br />
for a species to survive past the age of sexual maturity<br />
and rearing of offspring. For humans, for example, this<br />
would require a lifespan of only 30–40 years. 7 Because<br />
reproductive capacity seems to be the major determinant<br />
of species survival, phenotypic changes that favor longevity<br />
without altering fecundity should be unaffected by<br />
29
30 S. Muravchick<br />
Figure 3-1. <strong>The</strong> concept of organ system functional reserve has<br />
been described as a “wedge” broadest at birth that then declines<br />
progressively after maturity. Applying this concept to human<br />
aging, genetically determined organ system functional reserve<br />
may determine lifespan but life expectancy reflects “real world”<br />
estimates of human longevity given extrinsic environmental<br />
factors. (Data from Jazwinski SM. Longevity, genes, and aging.<br />
Science 1996;273:54–59.)<br />
evolutionary processes. Consequently, evolutionary theories<br />
of aging and longevity are unable to support the<br />
concept that there are specific genes that cause aging or<br />
control lifespan. 8 A “programmed aging” locus would<br />
have no species survival value and therefore would not<br />
be expected to persist intact in the genome throughout<br />
the long time course of evolution, although some evidence<br />
suggests that human cellular senescence could be<br />
a manifestation of evolutionary pressures to prevent<br />
malignant transformation. 9<br />
In fact, favorable changes in the genome segments that<br />
control reproduction and enhance species survival could<br />
have deleterious effects on postmaturation viability and<br />
lifespan. Senescence characterized by decreasing viability<br />
may be the price to be paid to sustain immortality of the<br />
species-specific germline at the expense of individual survival.<br />
10 A genomic locus that determines lifespan is rarely<br />
found in nature unless the reproduction of that species<br />
requires the death of the mature adult as the final step of<br />
the reproductive process. This phenomenon is seen in<br />
plants, insects, and some fishes where the linkage between<br />
reproduction and death is mediated by programmed neuroendocrine<br />
mechanisms. 11<br />
Mammals express a well-defined aging phenotype with<br />
great similarities between mammalian species, yet many<br />
amphibians, reptiles, and sharks and other primitive fishes<br />
fail to show obvious physical signs of aging. Mammalian<br />
aging could therefore have evolved along with other<br />
unique phenotypic mammalian characteristics, and it may<br />
not be the same process as the age-related biologic phenomena<br />
seen in some nonmammals. 12 Examination of the<br />
properties of genetic variation in Drosophila also supports<br />
the concept that aberrancies and mutations may not<br />
be nearly as important in determining longevity as is the<br />
underlying species phenotype. 13<br />
An external pacemaker tissue or organ must also<br />
be present to coordinate the aging-related interac -<br />
tions between tissues and multiple organ systems that<br />
characterize normal senescence, especially in humans.<br />
<strong>The</strong>refore, this type of theory usually requires that<br />
neuroendocrine or immune mechanisms have a central<br />
role in processes of aging. Despite considerable investigation<br />
and some early data suggesting the importance of<br />
changes in hypothalamic activity in aging, 14 however,<br />
there has been little objective evidence that a neuroendocrine<br />
or other hormonal “pacemaker” tissue as envisioned<br />
actually exists. It is therefore highly unlikely that<br />
aging or longevity are precisely programmed genetic<br />
events. 15<br />
Stochastic Aging<br />
Stochastic aging theories include a thermodynamic perspective<br />
that looks at increases or decreases in specific<br />
entropy production (SEP). In effect, viability is seen as a<br />
struggle against breakdown of intracellular order and<br />
structure. Growth and development represent an increase<br />
in order but aging is characterized as a breakdown in<br />
biologic order and an increase in randomness. 16 <strong>The</strong><br />
higher and more complex the organism, the greater the<br />
maximum SEP. Biologic stress and aging have similar<br />
thermodynamic properties and their underlying principles<br />
have been described using common parameters. 17<br />
Cells and tissues are conceptualized as “open systems”<br />
that are subject to energy and material flux and therefore<br />
require active energy expenditure to maintain<br />
physical order. <strong>The</strong>y are in a nonequilibrium or “far-fromequilibrium”<br />
steady state. From this perspective, “normal”<br />
aging is an evolving, slowly changing state characterized<br />
by increased cell damage (less order) and decreased bioenergetic<br />
capacity. SEP therefore declines during aging<br />
as the ability to extract energy from the environment<br />
decreases.<br />
In simplest terms, stochastic theories propose that<br />
physical and biochemical signs of aging may be a simple<br />
function of time and probability. <strong>The</strong> now-classic “genetic<br />
wear and tear” or “error-catastrophe” theory of aging is<br />
an example of this group. Originally, it suggested that<br />
degradation of the integrity of nuclear DNA (nDNA)<br />
over time generated random errors of genomic reproduction<br />
and transcription that accumulate. Eventually, the<br />
essential molecules needed for cell viability are no longer
3. <strong>The</strong>ories of Aging 31<br />
synthesized. 18 Progressive compromise of cellular and<br />
tissue function over time, therefore, produces the physical<br />
and clinical signs of aging. This theory predicts that<br />
there is an age-related increase in the fraction of proteins<br />
that are functionally defective, and that the error rate<br />
eventually rises exponentially as the key components of<br />
protein synthesis are themselves subject to defects or<br />
shortages.<br />
Overall, however, the evidence that mammalian aging<br />
is a random breakdown in biologic order because of lifelong<br />
accumulation of genomic errors caused by genetic<br />
mutations, remains very weak. 19 At least in human cells,<br />
faulty protein accumulates slowly throughout adulthood<br />
and the geriatric years and damage to the cells and microarchitecture<br />
seems to reflect secondary, not primary,<br />
errors in amino acid sequence. Nor does biologic order<br />
deteriorate at an accelerating or exponential rate.<br />
It is true, however, that many of the enzymes that accumulate<br />
in the tissues of older subjects are less active and<br />
more susceptible to heat inactivation and proteolysis, 20<br />
but these seem to be oxidized proteins that appear<br />
gradually, usually with methionine moieties or as various<br />
“glycated” molecules. Biologic amines can react nonenzymatically<br />
with glucose and other reducing sugars to<br />
form yellow-brown or fluorescent crosslinked complexes.<br />
<strong>The</strong>y are precursors to irreversibly bound crosslinking<br />
agents called advanced glycation end products (AGEs).<br />
Advanced glycation, originally seen in vitro, now is known<br />
to occur in living tissues. AGEs randomly interconnect<br />
lipoproteins and proteins and disrupt uniform molecular<br />
alignment, reducing elasticity and increasing “stiffness” in<br />
tissues containing structural collagen. 21<br />
AGEs in the vascular tree may accumulate even more<br />
rapidly with chronic exposure to high levels of reducing<br />
sugars, as occurs in poorly controlled diabetics, and may<br />
predispose to intravascular plaque formation and produce<br />
loss of cardiovascular elasticity. 22 Ethanol is metabolized<br />
in vivo to acetaldehyde which then produces a chemically<br />
stabilized complex that resists rearrangement in the presence<br />
of reducing sugars and therefore does not progress<br />
to AGE formation. This may explain the so-called “French<br />
paradox,” by which moderate chronic ethanol ingestion,<br />
for example, daily wine consumption, seems to confer a<br />
significant degree of protection from coronary artery<br />
disease. 23 Work in laboratory animals confirms that drugs<br />
or chemicals that block glycation or act as “crosslink<br />
breakers” 24 may reverse at least some of the clinical stigmata<br />
of the senescent cardiovascular system. However,<br />
confirmation of this concept in human studies has yet to<br />
be reported.<br />
Aging is also associated with a progressive decline in<br />
the ability of cells and organelles to scavenge and degrade<br />
these and other types of defective proteins. 25 Normally,<br />
oxidized proteins undergo preferential degradation<br />
within the cell by the proteasomal system. <strong>The</strong>re is a<br />
multicatalytic protease complex–-the proteasome–-as<br />
well as numerous other regulatory factors involved in<br />
the degradation of oxidized proteins. 26 <strong>The</strong> proteasome is<br />
present in the cytosol, nucleus, and endoplasmic reticulum<br />
of mammalian cells, but is itself subject to oxidative<br />
deterioration during aging and therefore may become<br />
progressively less effective in older individuals. 27<br />
Telomere shortening is another form of stochastic<br />
nDNA damage that has been invoked as a possible source<br />
of age-related decline. Located at the ends of eukaryotic<br />
chromosomes and synthesized by telomerase, telomeres<br />
are the genomic units that maintain the length of chromosomes.<br />
Human cancer cells demonstrate high telomerase<br />
activity. However, although there is a general<br />
association between cellular senescence and telomere<br />
shortening in vitro, 28 there is little evidence that telomere<br />
shortening is intrinsically associated with, or causally<br />
related to, normal human aging. Similarly, there is general<br />
correlation between species longevity and nDNA repair<br />
capacity but no firm evidence that the ability to recover<br />
from random nDNA damage is, in fact, progressively or<br />
universally compromised in older human subjects.<br />
Other potential stochastic mechanisms include random<br />
nDNA methylation, a process that correlates with transcriptional<br />
silence of many genes. When nDNA mutations<br />
occur, enzyme systems that repair DNA are a second<br />
line of defense designed to return nDNA to its original<br />
genetic integrity. Another potential genomic mechanism<br />
for aging, therefore, is compromised expression of the<br />
enhancer and repressor/suppressor elements that, in turn,<br />
activate or inhibit gene expression, particularly of the<br />
components of DNA repair mechanisms. This may<br />
become important in cancer biology because tumor genes<br />
are not expressed until the environmental stimuli that<br />
maintain the suppression are removed. A similar process<br />
could be important in aging. A third possible mechanism<br />
of aging at the cellular level relates to messenger RNA<br />
(mRNA) production. Many proteins and enzymes<br />
decrease in concentration with aging. This seems in some<br />
cases to be a direct result of decreases in the mRNA<br />
levels which encode the protein. Hence, age-related limitation<br />
of the rate or accuracy of the transcription of<br />
mRNA from nDNA may be involved.<br />
Altered Receptor Systems<br />
Recent research in the discipline of molecular pharmacology<br />
has generated huge amounts of data with regard<br />
to biologic receptor systems, especially within the nervous<br />
system. With aging, there are decreases in acetylcholine<br />
synthesis and release as well as reduction of muscarinic<br />
receptor plasticity. This suggests a causal connection<br />
between impairment of central cholinergic function and<br />
aging. A “cholinergic” theory of aging 29 is even more<br />
attractive given the clear role of cholinergic deficiencies
32 S. Muravchick<br />
in Alzheimer-type dementia 30 and perhaps other<br />
age-related neurodegenerative disorders. Gammaaminobutyric<br />
acid (GABA), a major inhibitory<br />
neurotransmitter, is an important site of drug action for<br />
anesthetic agents and another possible locus for aging<br />
within the nervous system. GABA receptors and other<br />
ligand-gated ion channels have been shown to have<br />
decreased specificity to their agonist molecules in older<br />
adults. 31 Although the demonstration of consistently<br />
decreased anesthetic requirement in older adults 32 is<br />
another intriguing clue supporting the concept of a link<br />
between aging and altered neurotransmitter dynamics,<br />
these observations have yet to be formulated into a<br />
coherent theory of aging that proposes a fundamental<br />
role for central nervous system receptors.<br />
Oxidative Stress<br />
Not all stochastic theories of aging focus on the state of<br />
DNA within the cell nucleus. Reactive oxygen species<br />
(ROS) or “free radicals” are routinely produced in the<br />
mitochondria as a byproduct of aerobic metabolism and<br />
oxidative phosphorylation. 33 If allowed to accumulate to<br />
high levels, ROS such as superoxide, impose a state of<br />
“oxidative stress” within the cell that can damage or<br />
destroy organelle and even molecular microarchitecture.<br />
34 <strong>The</strong>se toxic effects may be direct or they may be<br />
the consequences of a cascade of biochemical events.<br />
Investigations of oxidative phosphorylation in aging<br />
mitochondria confirm that aging is associated with both<br />
progressive decreases in mitochondrial energy generation<br />
35 and increased levels of defective mitochondrial<br />
DNA (mtDNA), 36 presumably because of excessive ROS.<br />
Older mitochondria also demonstrate a loss of membrane<br />
potential and a decrease of both fusion and fission activity.<br />
37 It is less clear whether increased ROS levels in the<br />
cytosol of a cell can damage nDNA, which is centrally<br />
located in the nucleus and relatively shielded from<br />
oxidation.<br />
According to this general concept, sustained and lifelong<br />
oxidative stress compromises the enzymatic machinery<br />
required for full bioenergetic capacity and also<br />
damages the mtDNA needed for synthesis of enzymes<br />
such as glutathione peroxidase and superoxide dismutase.<br />
<strong>The</strong>se enzymes protect cells from metabolic byproducts<br />
by scavenging ROS as they are produced in the mitochondria.<br />
Two centuries ago, the renowned scientist<br />
Joseph Priestly, discoverer of oxygen’s life-sustaining<br />
properties, speculated quite presciently that too much<br />
oxygen might lead to premature failure of oxidative processes.<br />
<strong>The</strong>refore, from this perspective at least, aging at<br />
a cellular level can be considered a form of chronic<br />
oxygen toxicity. ROS, the byproducts of aerobic metabolism<br />
that is essential for life in all higher organisms, may<br />
generate a “vicious cycle” of progressive bioenergetic<br />
Figure 3-2. Insidious increases in concentrations of reactive<br />
oxygen species (ROS) throughout the adult years generate a<br />
“cycle of aging” that may explain both the decreased bioenergetic<br />
capacity that characterizes senescent tissues and the<br />
increased morbidity and mortality exhibited by a geriatric<br />
patient population. (Data from Ozawa. 66 )<br />
failure and functional compromise in the mitochondria<br />
(Figure 3-2).<br />
Reconciling the <strong>The</strong>ories<br />
Nevertheless, purely stochastic theories such as those<br />
invoking oxidative stress fail to explain the dramatically<br />
different patterns of aging that are seen in various animals<br />
despite the fact that virtually all species share a common<br />
ecosystem, have similar metabolic processes and byproducts,<br />
and are exposed to similar catabolic environmental<br />
forces. In fact, aging may reflect the degenerative consequences<br />
of a lifetime of exposure to the byproducts of<br />
aerobic metabolism that have not been successfully<br />
detoxified by the genetically determined processes available<br />
to protect the integrity of the cell genome, maintain<br />
normal neurotransmitter dynamics, and preserve full<br />
bioenergetic capacity (Figure 3-3). Viewed as progressive<br />
failure of a species-specific, genetically predetermined<br />
capacity to avoid or repair random damage to proteins,<br />
lipids, nDNA, and mtDNA by ROS, a concept that identifies<br />
accumulated oxidative stress as the underlying driving<br />
force of aging is compatible with most aging theories,<br />
both stochastic and nonstochastic. 38 Nor does the consistency<br />
of observed lifespan for a given species necessarily<br />
imply a discrete “biologic clock” or a “lifespan” gene for<br />
each species. Rather, it may reflect the net effect of many<br />
genes in the phenotype of each species whose expression<br />
influences the aging and longevity of that life form. <strong>The</strong>se<br />
genetic factors have been described as “gerontogenes.” 39
3. <strong>The</strong>ories of Aging 33<br />
Figure 3-3. Proposed molecular mechanisms of aging include damage to the cellular and mitochondrial genome and disruption<br />
of cellular microarchitecture, including membrane-bound receptor complexes.<br />
It is becoming plausible, therefore, that lifespan may<br />
reflect a stochastic interaction between the genetically<br />
determined biochemical and physiologic attributes of<br />
each species and the internal and external destructive<br />
factors that disorder biologic systems. 40 Consequently,<br />
exploring how each species is equipped genetically to<br />
deal with metabolic and environmental stress, therefore,<br />
has become a fundamental and crucial step in understanding<br />
the molecular biology of aging. <strong>The</strong> “theory of<br />
disposable soma” postulates that some species have<br />
increased their reproductive capacity in exchange for<br />
decreased lifespan. 41 However, other evolution theory<br />
suggests that the longer-lived species have evolved<br />
because of their greater degree of genetic investment<br />
in a more durable soma, including mechanisms, many<br />
perhaps complex and requiring considerable cell re -<br />
sources, that enhance cellular resistance to stress. “Hormesis,”<br />
the low-level state of chronic oxidative stress that<br />
induces expression of genes that can increase the effectiveness<br />
of stress responses in mammals (also described<br />
as ischemic, hypoxic, or anesthetic “preconditioning”),<br />
may be more easily initiated in some species than in<br />
others. In fact, stress-induced expression of genes that<br />
facilitate cell repair is well established: cold stress has<br />
been shown to prolong lifespan in the nematode Caenorhabditis<br />
elegans 42 and heat stress significantly increases<br />
longevity of the fruit fly, Drosophila melanogaster.<br />
Birds, and perhaps other nonmammalian species, also<br />
possess a mitochondrial lipid structure that is more resistant<br />
to oxidative damage than that of mammals. 43 This<br />
may confer a special adaptation that prevents the agerelated<br />
tissue damage seen in mammals that is caused<br />
by ROS or AGEs. Avian lifespan is markedly prolonged<br />
relative to that of most mammals with comparable metabolic<br />
rates. Bird mitochondria also produce significantly<br />
less ROS than those of mammals, but it is not clear<br />
whether their specific bioenergetic capacity is significantly<br />
different. 44 In the nematode C. elegans, a genetic<br />
mutation with increased activities of antioxidative<br />
enzymes also has lifespan significantly greater than the<br />
wild-type strain.<br />
Point mutations and deletions of mtDNA accumulate<br />
in adult humans, monkeys, and some laboratory rodents.<br />
Although these mutations are only a small proportion of<br />
total mtDNA and are randomly or clonally distributed in<br />
different tissues, the amount of defective mtDNA found<br />
in the heart and brain of mammalian species ranging in<br />
maximum lifespan from 3.5 to 46 years has been shown<br />
to be inversely correlated with lifespan. In addition,<br />
genetically altered mice that express a proofreadingdeficient<br />
version of mtDNA polymerase develop into a<br />
young adult mouse phenotype with a three- to fivefold<br />
increase in mtDNA point mutations and increased<br />
mtDNA deletions. In these mice, the increased number
34 S. Muravchick<br />
of somatic mtDNA mutations has recently been shown<br />
to be associated in young adulthood with age-related<br />
phenotypic characteristics such as reduced subcutaneous<br />
fat, hair loss, and osteoporosis as well as significantly<br />
reduced lifespan. 45 However, it remains unclear whether<br />
these changes are similar to, or actual premature manifestations,<br />
of aging.<br />
It has also not yet been demonstrated that genetic<br />
manipulation of mtDNA repair and replication mechanisms<br />
can produce mice with decreased mtDNA mutation<br />
rates and increased longevity, although it has been<br />
shown that there is less mitochondrial ROS generation in<br />
long-lived than in short-lived mammalian species. Most<br />
relevant to human aging, cellular resistance to oxidative<br />
stress has recently been shown to be closely correlated<br />
with mammalian longevity. Skin fibroblasts and lymphocytes<br />
from eight mammalian species with a range of lifespans<br />
show a direct correlation between cellular resistance<br />
to chemical, alkaline, and oxidative stress and the<br />
maximum lifespan of the species. 46 <strong>The</strong>se results agree<br />
with the concept that ROS in mitochondria produce<br />
accumulating oxidative damage to mtDNA 47,48 (Figure<br />
3-4) and perhaps to other key cellular components that<br />
in some way is related to the aging rate of each mammalian<br />
species. 49<br />
<strong>The</strong> theory that aging is a direct consequence of the<br />
accumulation of oxidative damage caused by ROS is consistent<br />
with the observed effectiveness of caloric restriction<br />
as a therapy that prolongs the life expectancy of<br />
laboratory rodents. 50 Caloric restriction may lower mitochondrial<br />
ROS levels and may reduce oxidative damage<br />
to mtDNA. This or a similar mechanism may also explain<br />
the evolution of species with different longevities. 51<br />
Species with higher metabolic rates, or, within a given<br />
species, individuals with an increased demand for oxidative<br />
energy may have a higher “rate of living” that generates<br />
more ROS and reduces life expectancy. Alternatively,<br />
some recent data suggest that caloric restriction, perhaps<br />
through selective gene expression, actually increases<br />
mitochondrial bioenergetic efficiency and is associated<br />
with suppression of metabolic stress responses. 52 Changes<br />
in the glucose–fatty acid cycle that occur in response to<br />
near starvation may be protective when calories are<br />
reduced in aging tissues. 53<br />
Nevertheless, it would be premature to attribute aging,<br />
in particular human aging, to simple bioenergetic deterioration<br />
caused by oxidative stress. 54 <strong>The</strong>re is a general<br />
correlation between species longevity and the capacity to<br />
repair damaged DNA but evidence that the ability to<br />
recover from random oxidative DNA damage is progressively<br />
or universally compromised in older human<br />
subjects remains elusive. 55 In addition, although several<br />
investigations have confirmed that defective mtDNA<br />
increases in the cells of older subjects, it is not established<br />
that this produces a critical reduction of the macromolecules<br />
needed for normal bioenergetics. 56 In addition, the<br />
interaction between ROS and the bioenergetic apparatus<br />
is now known to be far more complex than was once<br />
believed. Peroxiredoxins represent a group of at least six<br />
isoforms of a multifunctional peroxidase. 57 <strong>The</strong>y have<br />
recently been identified in many species and are believed<br />
to provide protection against the low-level oxidative<br />
stress associated with peroxide accumulation yet they do<br />
not appear to influence longevity. 58 Similarly, the overexpression<br />
of superoxide dismutase and catalase enhances<br />
resistance to experimental oxidative stress but decreases,<br />
rather than increases, lifespan of transgenic Drosophila<br />
melanogaster. 59 Taken together, these observations<br />
suggest that normal lifespan reflects a subtle and complex<br />
equilibrium between the byproducts of oxidative metabolism<br />
and endogenous mechanisms that respond to oxidative<br />
stress.<br />
Human Aging and <strong>Geriatric</strong>s<br />
Figure 3-4. Recent studies of human tissues support the evolving<br />
concept that accumulation of damaged mitochondrial DNA<br />
(mtDNA) in the early geriatric era leads to a progressive decline<br />
in bioenergetic capacity and oxidative phosphorylation. (Data<br />
from Mandavilli et al. 47 )<br />
<strong>The</strong> term “geriatrics” was coined at the start of the twentieth<br />
century 60 to describe the clinical subspecialty area<br />
of medicine that focuses on care of the elderly patient.<br />
But, as yet, there is still no consensus as to when the<br />
“geriatric” era begins in human subjects or whether any<br />
single physiologic marker can unequivocally identify a<br />
patient as “elderly.” <strong>The</strong>refore, establishing rigid or finite<br />
chronologic definitions of the term “geriatric” has little<br />
value other than for administrative, actuarial, or epidemiologic<br />
applications. Nevertheless, although it may have
3. <strong>The</strong>ories of Aging 35<br />
increased rapidly from the onset of human evolution<br />
until about 100,000 years ago, when the brain weight/<br />
body ratio of our hominid ancestors stabilized at the<br />
current value for modern humans, 61 empirical evidence<br />
and historical anecdote suggest that human lifespan has<br />
remained constant at about 120 years for at least the past<br />
20 centuries.<br />
In contrast, the past century has seen dramatic advances<br />
in medical science and health care that have greatly<br />
increased life expectancy in industrialized societies,<br />
especially in Japan and the United States, increasing the<br />
relative “agedness” of those societies. 62 However, the<br />
increased life expectancy so often invoked in discussions<br />
of “the graying of America” is a socioeconomic, rather<br />
than a biologic, phenomenon that steadily enlarges that<br />
fraction of the general human population considered<br />
“elderly.” If, in fact, maximum human lifespan is fixed but<br />
life expectancy increases in response to elimination of<br />
disease and other external threats to longevity, the human<br />
survival curve may continue to undergo the “rectangularization”<br />
63 that results in the compression of age-related<br />
morbidity and mortality into the later years of the geriatric<br />
era. 64 Yet, there is some evidence that human lifespan<br />
may not yet have reached its ultimate maximum<br />
value. <strong>The</strong> time perspective of metrics used in modern<br />
biology is so limited relative to the many millennia of<br />
human existence that subtle increases in lifespan may<br />
actually be occurring undetected.<br />
Clinical Studies of Aging<br />
All geriatricians accept increased interindividual variability<br />
as a hallmark of their patient populations. As they<br />
age, adults continually exhibit a progressively more varied<br />
array of physical responses to concurrent disease states<br />
which, in turn, reflect their lifelong exposure to environmental<br />
and socioeconomic conditions and to the accumulated<br />
stigmata of prior traumatic injuries and medical<br />
therapies. Prolonged longevity also enables complete<br />
expression of intrinsic genetic qualities in all their subtle<br />
physiologic manifestations. In effect, people are never<br />
more alike than they are at birth, nor more different or<br />
unique than when they enter the geriatric era.<br />
<strong>The</strong>refore, interpretation of clinical studies of human<br />
aging remains difficult and progress in understanding<br />
mechanisms of aging has been correspondingly slow. Yet,<br />
much has been learned about the relative strengths and<br />
weaknesses of the various forms of epidemiologic<br />
investigation used by gerontologists and geriatricians.<br />
Cross-sectional studies measure physiologic parameters<br />
simultaneously in young and in elderly subjects. Changes<br />
caused by undiagnosed age-related disease may be erroneously<br />
attributed to aging, and this experimental design<br />
cannot be controlled for cohort-specific factors such as<br />
nutritional and environmental history, genetic background,<br />
or prior exposure to infectious agents. Crosssectional<br />
designs do not provide sufficient evidence for<br />
the interdependence of aging-related changes and therefore<br />
they probably should not serve as the final basis for<br />
theories and hypotheses of aging. 65<br />
Longitudinal designs provide a much stronger basis for<br />
inference regarding rates and characteristics of human<br />
aging. <strong>The</strong>y require that the investigator obtain repeated<br />
measurements in each individual subject over several<br />
decades. Each subject therefore generates his own “young<br />
adult” control value for comparison with subsequent<br />
measurements. If any of the subjects in a longitudinal<br />
study eventually manifest signs of age-related disease,<br />
their data points can be excluded from the study, thereby<br />
leaving behind a smaller but more homogeneous group<br />
of healthy elderly subjects. Survival to and through adulthood<br />
and beyond also permits the full expression of even<br />
the subtlest genetic differences between individuals that<br />
might not be fully apparent over shorter lifespan intervals.<br />
In longitudinal studies, the signs and symptoms of<br />
aging become progressively more apparent or severe<br />
with increasing chronologic age. Any changes in structure<br />
or function that are not found in all members of a geriatric<br />
population, or those changes that do not seem to<br />
have a direct relationship between severity and chronologic<br />
age, can be attributed to age-related disease rather<br />
than to aging itself.<br />
Although difficult and expensive to organize and maintain,<br />
long-term longitudinal studies have therefore produced<br />
substantial amounts of extremely valuable data<br />
related to human aging. Nevertheless, this methodology<br />
has some pitfalls. It requires establishing a chronologic<br />
“starting point” for the geriatric era, an arbitrary value<br />
that may change significantly during the study because of<br />
increases in life expectancy. In addition, the validity and<br />
utility of the data may be compromised by the inevitable<br />
evolution or revision of physiologic concepts and the<br />
refinement of measurement techniques that invariably<br />
occur over the time periods required to study human<br />
aging. Last, it is difficult to attract new physician scientists<br />
to a form of clinical investigation in which the answers to<br />
the scientific questions that are being asked may not be<br />
known during the lifetime of the investigator himself.<br />
Summary<br />
<strong>The</strong>re is currently great scientific interest and experimental<br />
activity under way to fully define the role of long-term<br />
oxidative stress as a cause of increasing damage to<br />
mtDNA and intracellular protein. 66 As awareness of the<br />
roles of mitochondrial genetics and oxidative stress in<br />
mechanisms of senescence and death has increased<br />
among biogerontologists, the various theories of aging<br />
have begun to coalesce and unify. Genetically determined
36 S. Muravchick<br />
ability to scavenge ROS and to repair accumulated or<br />
randomly acquired damage to intracellular enzymes and<br />
organelles does, in general, correlate with longevity, both<br />
in humans and in other species that show phenotypic<br />
change with age. Declining bioenergetics and a reduction<br />
in capacity for oxidative phosphorylation also seems to<br />
explain the age-related clinical deterioration of maximal<br />
organ function that inevitably occurs throughout human<br />
adulthood, even in the most fit older subjects. In fact,<br />
many researchers already believe that it is progressive<br />
failure of mitochondrial bioenergetics that produces<br />
normal human aging as well as many aspects of agerelated<br />
degenerative disease. 67<br />
References<br />
1. Carel A. On the permanent life of tissues outside of the<br />
organism. J Exp Med 1912;15:516–528.<br />
2. Hayflick L. <strong>The</strong> limited in vitro lifetime of human diploid<br />
cell strains. Exp Cell Res 1965;57:614–636.<br />
3. Hayflick L. Biologic and theoretical perspectives of human<br />
aging. In: Katlic MR, ed. <strong>Geriatric</strong> Surgery: Comprehensive<br />
Care of the Elderly Patient. Baltimore: Urban and Schwarzenberg;<br />
1990:3–21.<br />
4. Hayflick L. <strong>The</strong> biology of human aging. Am J Med Sci 1973;<br />
265:433–445.<br />
5. Strehler BL. Aging: concepts and theories. In: Viidik A, ed.<br />
Lectures on Gerontology. New York: Academic Press; 1982:<br />
1–57.<br />
6. Gershon H, Gershon D. Paradigms in aging research: a<br />
critical review and assessment. Mech Ageing Dev 2000;117:<br />
21–28.<br />
7. Bidder GP. Senescence. Br Med J 1932;15:5831.<br />
8. Ameisen JC. On the origin, evolution, and nature of programmed<br />
cell death: a timeline of four billion years. Cell<br />
Death Diff 2002;9:367–393.<br />
9. Troen BR. <strong>The</strong> biology of aging. Mt Sinai J Med 2003;70:<br />
3–22.<br />
10. Kirkwood TB. Sex and ageing. Exp Gerontol 2001;36:413–<br />
418.<br />
11. Sacher GA. Molecular versus systemic theories on the<br />
genesis of aging. Exp Gerontol 1968;3:265–271.<br />
12. de Magalhaes JP, Toussaint O. <strong>The</strong> evolution of mammalian<br />
aging. Exp Gerontol 2002;37:769–775.<br />
13. Partridge L. Evolutionary theories of ageing applied to<br />
long-lived organisms. Exp Gerontol 2001;36:641–650.<br />
14. Finch CE. Neuroendocrine mechanisms and aging. Fed Proc<br />
1979;38:178–183.<br />
15. Harman D. Aging: overview. Ann NY Acad Sci 2001;928:<br />
1–21.<br />
16. Strehler BL. Genetic instability as the primary cause of<br />
human aging. Exp Gerontol 1986;21:283–319.<br />
17. Toussaint O, Schneider ED. <strong>The</strong> thermodynamics and evolution<br />
of complexity in biological systems. Comp Biochem<br />
Physiol A Molec Integr Physiol 1998;120:3–9.<br />
18. Orgel LE. <strong>The</strong> maintenance of the accuracy of protein synthesis<br />
and its relevance to ageing. Proc Natl Acad Sci USA<br />
1963;49:517–521.<br />
19. Orgel LE. <strong>The</strong> maintenance of the accuracy of protein synthesis<br />
and its relevance to ageing: a correction. Proc Natl<br />
Acad Sci USA 1970;67:1476.<br />
20. Stadtman ER. Protein oxidation in aging and age-related<br />
diseases. Ann NY Acad Sci 2001;928:22–38.<br />
21. Lee AT, Cerami A. Role of glycation in aging. Ann NY Acad<br />
Sci 1992;663:63–70.<br />
22. Ulrich P, Cerami A. Protein glycation, diabetes, and aging.<br />
Recent Prog Horm Res 2001;56:1–21.<br />
23. Al Abed Y, Mitsuhashi T, Li H, et al. Inhibition of advanced<br />
glycation end product formation by acetaldehyde: role in<br />
the cardioprotective effect of ethanol. Proc Natl Acad Sci<br />
USA 1999;96:2385–2390.<br />
24. Vaitkevicius PV, Lane M, Spurgeon H, et al. A cross-link<br />
breaker has sustained effects on arterial and ventricular<br />
properties in older rhesus monkeys. Proc Natl Acad Sci<br />
USA 2001;98:1171–1175.<br />
25. Reznick AZ, Lavie L, Gershon HE, et al. Age-associated<br />
accumulation of altered FDP aldolase B in mice: conditions<br />
of detection and determination of aldolase half life in young<br />
and old animals. FEBS Lett 1981;128:221–224.<br />
26. Stolzing A, Grune T. <strong>The</strong> proteasome and its function in the<br />
ageing process. Clin Exp Dermatol 2001;26:566–572.<br />
27. Gray DA, Tsirigotis M, Woulfe J. Ubiquitin, proteasomes,<br />
and the aging brain. Sci Aging Knowledge Environ 2003:<br />
2003(34):RE6.<br />
28. Ahmed A, Tollefsbol T. Telomeres and telomerase: basic<br />
science implications for aging. J Am Geriatr Soc 2001;49:<br />
1105–1109.<br />
29. Gallagher M, Colombo PJ. Ageing: the cholinergic hypothesis<br />
of cognitive decline. Curr Opin Neurobiol 1995;5:<br />
161–168.<br />
30. Yew DT, Li WP, Webb SE, et al. Neurotransmitters, peptides,<br />
and neural cell adhesion molecules in the cortices of normal<br />
elderly humans and Alzheimer patients: a comparison. Exp<br />
Gerontol 1999;34:117–133.<br />
31. McGeer EG, McGeer PL. Age changes in the human for<br />
some enzymes associated with metabolism of catecholamines,<br />
GABA, and acetylcholine. Adv Behav Biol 1975;16:<br />
287–305.<br />
32. Munson ES, Hoffman JC, Eger EI II. Use of cyclopropane<br />
to test generality of anesthetic requirement in the elderly.<br />
Anesth Analg 1984;63:998–1000.<br />
33. Nagy IZ. On the true role of oxygen free radicals in the<br />
living state, aging, and degenerative disorders. Ann NY<br />
Acad Sci 2001;928:187–199.<br />
34. Sohal RS, Weindruch R. Oxidative stress, caloric restriction,<br />
and aging. Science 1996;273:59–63.<br />
35. Knight JA. <strong>The</strong> biochemistry of aging. Adv Clin Chem 2000;<br />
35:1–62.<br />
36. Wei YH, Lee HC. Oxidative stress, mitochondrial DNA<br />
mutation, and impairment of antioxidant enzymes in aging.<br />
Exp Biol Med 2002;227:671–682.<br />
37. Jendrach M, Pohl S, Voth M, Kowald A, Hammerstein P,<br />
Bereiter-Hahn J. Morpho-dynamic changes of mitochondria<br />
during ageing of human endothelial cells. Mech Ageing Dev<br />
2005;126:813–821.<br />
38. Golden TR, Melov S. Mitochondrial DNA mutations,<br />
oxidative stress, and aging. Mech Ageing Dev 2001;122:<br />
1577–1589.
3. <strong>The</strong>ories of Aging 37<br />
39. Rattan SI. Ageing, gerontogenes, and hormesis. Indian J<br />
Exp Biol 2000;38:1–5.<br />
40. Skulachev VP. Programmed death phenomena: from organelle<br />
to organism. Ann NY Acad Sci 2002;959:214–237.<br />
41. Mangel M. Complex adaptive systems, aging and longevity.<br />
J <strong>The</strong>or Biol 2001;213:559–571.<br />
42. Lithgow GJ, Walker GA. Stress resistance as a determinate<br />
of C. elegans lifespan. Mech Ageing Dev 2002;123:765–771.<br />
43. Herrero A, Barja G. H 2 O 2 production of heart mitochondria<br />
and aging rate are slower in canaries and parakeets than in<br />
mice: sites of free radical generation and mechanisms<br />
involved. Mech Ageing Dev 1998;103:133–146.<br />
44. Holmes DJ, Fluckiger R, Austad SN. Comparative biology<br />
of aging in birds: an update. Exp Gerontol 2001; 36:869–<br />
883.<br />
45. Trifunovic A, Wredenberg A, Falkenberg M, et al. Premature<br />
ageing in mice expressing defective mitochondrial<br />
DNA polymerase. Nature 2004;429:417–423.<br />
46. Kapahi P, Boulton ME, Kirkwood TB. Positive correlation<br />
between mammalian life span and cellular resistance to<br />
stress. Free Radic Biol Med 1999;26:495–500.<br />
47. Mandavilli BS, Santos JH, Van Houten B. Mitochondrial<br />
DNA repair and aging. Mutat Res 2002;509:127–151.<br />
48. Sugiyama S, Hattori K, Hayakawa M, et al. Quantitative<br />
analysis of age-associated accumulation of mitochondrial<br />
DNA with deletion in human hearts. Biochem Biophys Res<br />
1991;180:894–899.<br />
49. Barja G, Herrero A. Oxidative damage to mitochondrial<br />
DNA is inversely related to maximum life span in the heart<br />
and brain of mammals. FASEB J 2000;14:312–318.<br />
50. Masoro EJ, Bertrand H, Liepa G, et al. Analysis and exploration<br />
of age-related changes in mammalian structure and<br />
function. Fed Proc 1979;38:1956–1961.<br />
51. Barja G. Endogenous oxidative stress: relationship to aging,<br />
longevity and caloric restriction. Ageing Res Rev 2002;1:<br />
397–411.<br />
52. Lee C-K, Klopp RG, Weindruch R, et al. Gene expression<br />
profile of aging and its retardation by caloric restriction.<br />
Science 1999;285:1390–1392.<br />
53. Heininger K. Aging is a deprivation syndrome driven by a<br />
germ-soma conflict. Ageing Res Rev 2002;1:481–536.<br />
54. Huang H, Manton KG. <strong>The</strong> role of oxidative damage in<br />
mitochondria during aging: a review. Front Biosci 2004;9:<br />
1100–1117.<br />
55. Lieber MR, Karanjawala ZE. Ageing, repetitive genomes<br />
and DNA damage. Nat Rev Mol Cell Biol 2004;5:69–75.<br />
56. Maklashina E, Ackrell BA. Is defective electron transport<br />
at the hub of aging? Aging Cell 2004;3:21–27.<br />
57. Rhee SG, Chae HZ, Kim K. Peroxiredoxins: a historical<br />
overview and speculative preview of novel mechanisms and<br />
emerging concepts in cell signaling. Free Radic Biol Med<br />
2005;38:1543–1552.<br />
58. Immenschuh S, Baumgart-Vogt E. Peroxiredoxins, oxidative<br />
stress, and cell proliferation. Antioxid Redox Signal<br />
2005;7:768–777.<br />
59. Bayne AC, Mockett RJ, Orr WC, Sohal RS. Enhanced catabolism<br />
of mitochondrial superoxide/hydrogen peroxide and<br />
aging in transgenic Drosophila. Biochem J 2005;391(Pt 2):<br />
277–284.<br />
60. Nascher IL. <strong>Geriatric</strong>s. NY Med J 1909;90:358–359.<br />
61. Hofman MA. Energy metabolism, brain size and longevity<br />
in mammals. Q Rev Biol 1983;58:495–512.<br />
62. Schneider EL, Reed JD Jr. Life extension. N Engl J Med<br />
1985;312:1159–1168.<br />
63. Comfort A. <strong>The</strong> Biology of Senescence. 3rd ed. New York:<br />
Elsevier; 1979:414 pp.<br />
64. Fries JF. Aging, natural death, and the compression of morbidity.<br />
N Engl J Med 1980;303:130–135.<br />
65. Hofer SM, Sliwinski MJ. Understanding ageing: an<br />
evaluation of research designs for assessing the interdependence<br />
of ageing-related changes. Gerontology 2001;47:341–<br />
352.<br />
66. Ozawa T. Genetic and functional changes in mitochondria<br />
associated with aging. Physiol Rev 1997;77:425–464.<br />
67. Calabrese V, Scapagnini G, Giuffrida Stella AM, et al. Mitochondrial<br />
involvement in brain function and dysfunction:<br />
relevance to aging, neurodegenerative disorders and longevity.<br />
Neurochem Res 2001;26:739–764.
4<br />
Ethical Management of the Elderly Patient<br />
Paul J. Hoehner<br />
Because of the increasing growth of the elderly population,<br />
geriatric care is rapidly emerging as a unique medical<br />
specialty in its own right. Advancements in medical<br />
science and changes in the health care delivery system<br />
that impact the care of the elderly are accompanied by<br />
myriad ethical dilemmas that confront not only the physician<br />
and patient, but social workers, nursing home staff,<br />
and relatives. Settings involving the extremes of age and<br />
illness are the most complex in ethical deliberation.<br />
Although anesthesiologists may confront a variety of<br />
ethical issues, such as patient confidentiality, care of Jehovah’s<br />
Witnesses, substance abuse, and so forth, this chapter<br />
will focus on those issues unique to and more likely to be<br />
encountered in the elderly patient.<br />
Social Views of Aging<br />
Social views of aging are inherently present and basically<br />
informative within any application of ethical principles to<br />
ethical problems involving the elderly. <strong>The</strong>refore, it is<br />
important to recognize that one’s view of aging can and<br />
will influence both clinical decision making as well as the<br />
application of ethical principles to individual concrete<br />
situations. Although contemporary views of aging are<br />
complex and varied, Gadow 1 helpfully outlines a spectrum<br />
of views, each of which contribute to the apparent<br />
social and moral value of the elderly patient and the resolution<br />
of ethical problems. First, aging can be viewed as<br />
the antithesis of health and vigor. This negative interpretation<br />
of the aging process is expressed in deceptively<br />
“objective” descriptions of the clinical changes in aging<br />
as “deterioration,” “disorganization,” and “disintegration,”<br />
from the level of psyche to the level of cellular<br />
physiology. Gadow points out, however, that there is<br />
nothing a priori degenerative about changes in aging<br />
unless one “uncritically accepts as the only ideal of health<br />
the condition that younger individuals manifest.” 1,2 Furthermore,<br />
it is a mistake to think of the elderly as generally<br />
sick and impaired. Patricia Jung notes that, “Clearly,<br />
to expose as false those myths that portray the old as<br />
inescapably and increasingly physically decrepit, mentally<br />
incompetent, desexualized persons best kept isolated<br />
in nursing homes is an important first step toward<br />
discerning what it means to age.” 3 For many, old age is<br />
not a time of disability or disease; instead it is a time of<br />
remarkably good health. According to one government<br />
study, 72.3% of noninstitutionalized elderly persons<br />
described their health as “excellent,” “very good,” or<br />
“good,” and only 27.6% described their health as “fair”<br />
or “poor.” 4 Nevertheless, this same study showed that in<br />
1990 persons over the age of 65 experienced more than<br />
two and a half times the number of days of activity restriction<br />
because of acute and chronic conditions as persons<br />
between the ages of 25 and 44, with 37.5% of people over<br />
the age of 65 experiencing some activity limitation caused<br />
by chronic conditions. Health care workers, whose contact<br />
with the elderly is naturally skewed toward those who<br />
are acute or chronically ill, and/or institutionalized, are<br />
especially prone to this unambiguously negative account<br />
found in the “decline model” that so powerfully dominates<br />
our cultural interpretation of aging.<br />
Second, aging can be viewed as an unwelcome reminder<br />
of our mortality. Medicine, at least a little like Shelley’s<br />
modern Prometheus, 5 tends to seek for and attain progress<br />
within the human condition in ways that defy its own<br />
ability to know what to do next. Shaped by the pervasive<br />
story of our therapeutic culture, 6 health care workers and<br />
their patients are driven by an interest in longevity that<br />
reaches far beyond the merely academic, emanating as it<br />
does from a desire to avoid suffering and certainly from<br />
a fear of death. Growing old in our therapeutic culture<br />
encourages us to desire perpetual youthfulness and gives<br />
us the power to strive for it (to some degree successfully,<br />
or, at least, cosmetically), but also forces us to ask just<br />
how old we really want to live to be. And as we age, for<br />
how long and in what ways do we care for ourselves?<br />
Advances in medicine bring new psychologic and ethical<br />
38
4. Ethical Management of the Elderly Patient 39<br />
challenges, both for those who are older and for those<br />
who are living with and caring for them. For instance, the<br />
more natural and acceptable mortality is thought to be<br />
for the elderly, the more unthinkable it is for the nonelderly.<br />
This view can lead to the avoidance of the elderly<br />
as symbols of the unthinkable.<br />
Medical and social views of aging can reflect the full<br />
diversity of a spectrum ranging from the philosophy that<br />
the elderly have less social and moral value than other<br />
individuals, to the other extreme of having greater value<br />
than others. <strong>The</strong> most positive of all attitudes is that of<br />
the elderly as a cultural treasure, a repository of wisdom,<br />
and an embodiment of history. Gadow 1 also observes<br />
another emerging perspective that treats the elderly as<br />
underprivileged citizens. This view bypasses the question<br />
of the intrinsic value of the elderly for society and brings<br />
them “out of the closet” to become recipients of our<br />
benevolence toward them as an “oppressed” group. <strong>The</strong><br />
potential danger with this view is that by designating<br />
the elderly as “handicapped” individuals, and thereby<br />
as a special group needing services, the beneficiaries<br />
remain subordinate to the benefactor and may even<br />
become victim to the extremes of unwarranted paternalistic<br />
care.<br />
A development inherent to the rise of geriatric medicine<br />
as a specialty is the view of aging as a clinical entity<br />
in its own right. Positively, aging is viewed as a unique<br />
human phenomenon worthy of specialized attention. <strong>The</strong><br />
elderly are not health deviants but present special problems<br />
as well as special strengths not found in other populations.<br />
Surely this is a welcome view that will, and has<br />
already, greatly contributed to the understanding and<br />
care of many issues unique to this growing population<br />
(the focus of this textbook being one example). Negatively,<br />
the subspecialty approach to geriatric medicine<br />
may become a model for a broader social approach to<br />
the elderly whereby aging would be of interest as a “highly<br />
specific class of unusual phenomena, bearing little relation<br />
to the more general features of experience shared<br />
by persons of all ages.” 1 Aging may be viewed not as<br />
a normal life process, with little or no purpose, but as a<br />
disease in itself. Yet much of what has been assumed<br />
mistakenly to be the “plight” of the elderly is in fact the<br />
consequence of specific pathologies not properly associated<br />
with aging. Chronic illnesses and degenerative diseases<br />
often associated with aging are frequently a result<br />
of lifestyle choices. Although aging may be associated<br />
with some rote memory loss, recent studies repeatedly<br />
indicate that the basic cognitive competence of the elderly<br />
does not deteriorate with age. <strong>The</strong>re is some evidence of<br />
positive growth in certain more complex, integrative<br />
mental abilities. Peter Mayer notes in his essay “Biological<br />
<strong>The</strong>ories about Aging” that even physical changes<br />
such as osteoporosis among postmenopausal women and<br />
immune system decline which were once presumed to be<br />
an inevitable result of growing old are now understood<br />
to be the consequence of specific medical conditions or<br />
other factors such as malnutrition. 7<br />
Ethical Principles<br />
In our modern society, categories of right and wrong or<br />
decisions regarding the “good” are frequently characterized<br />
by competing rational philosophical theories (such<br />
as deontology, utilitarianism, natural law), as cultural and<br />
tradition-dependent artifacts, or as arising from individualistic<br />
or relativistic (e)motives. <strong>The</strong> classic paradigm of<br />
modern medical ethics, often referred to as “principlism,”<br />
originated in a pragmatic attempt to overcome the<br />
impasse of these competing ethical theories in order to<br />
derive common and self-evident “principles” that would<br />
serve to guide a common language/paradigm of biomedical<br />
ethical decision making. This almost universally<br />
accepted paradigm of modern medical ethics revolves<br />
around the principles of respect for personal autonomy,<br />
beneficence, nonmaleficence, and justice. This paradigm,<br />
which has been extensively discussed in many basic<br />
medical ethics texts, will be assumed for the remainder of<br />
this chapter.<br />
Recent work in medical ethics has focused on alternative<br />
frameworks based on such concepts as “virtue ethics,”<br />
the “narrative life,” and “personhood.” <strong>The</strong>se concepts<br />
may overcome some of the philosophical limitations of<br />
the traditional approach and provide a more firm theoretical<br />
grounding that can thereby proceed to the level of<br />
principles more appropriate for use in the elderly population.<br />
One exemplary approach is that of Spielman 8 who<br />
appropriates the moral anthropology of Hauerwas to<br />
build a more adequate principled approach to geriatric<br />
ethics. Hauerwas emphasizes an ethic of virtue that grows<br />
out of his conviction that “what one does or does not do<br />
is dependent on possessing a ‘self’ sufficient to take<br />
responsibility for one’s actions.” 9 Three aspects of the self,<br />
which are relevant to applying Hauerwas’ work, are its<br />
temporal dimension, its social dimension, and its tragic or<br />
limited dimension.<br />
Unlike the standard account of post-Kantian ethics in<br />
which the moral life is seen in terms of obedience to a set<br />
of rational, timeless principles, Hauerwas presents character,<br />
developed within the context of a particular story<br />
or narrative, as the key to the moral life. According to this<br />
temporal dimension, life is not seen as a series of discontinuous<br />
decisions but rather as a challenge to be faithful<br />
to a true story or history. Contemporary ethical theory<br />
tends to view the ideal human as a self-sufficient,<br />
independent moral agent, without social ties. Hauerwas’<br />
social dimension emphasizes the fact that we are all historical<br />
beings and cannot avoid being part of larger<br />
communities. Our ability to think and our ability to act
40 P.J. Hoehner<br />
Figure 4-1. Principles of a geriatric ethic derived from<br />
Hauerwas’ dimensions of human nature. (Adapted with permission<br />
from Spielman. 8 )<br />
are embedded in a social structure in which even the<br />
descriptions of our actions depend on language, which is<br />
a public possession. Human existence also has a necessarily<br />
tragic or limited dimension. Medicine cannot eradicate<br />
suffering and death in our lives. By using MacIntyre’s<br />
characterization of medicine as a tragic profession, Hauerwas<br />
suggests that medical ethics cannot be limited to<br />
casuistic analyses of particular sets of problems and issues.<br />
He notes the continuity between the kind, of issues raised<br />
by medicine and the rest of our lives and raises important<br />
issues involved in the practice of medicine relative to the<br />
elderly, such as limited resource allocation. Hauerwas<br />
shows that not only are the history and the relationships<br />
of the self significant, but that the limitations inherent in<br />
medical treatment of the elderly cannot be ignored. 10<br />
Figure 4-1 illustrates how the temporal, social, and<br />
tragic or limited dimensions of human existence can be<br />
used to develop principles more appropriate to developing<br />
a geriatric ethic according to Spielman. <strong>The</strong> dimensions<br />
of temporality and sociality can be recognized in<br />
the increasing dependence on others as one ages. A more<br />
useful principle than autonomy is one of continuity. This<br />
principle may be stated as: “Act so that you avoid disrupting<br />
the continuity of past, present, and future values, commitments,<br />
and relationships in older people’s lives.” <strong>The</strong><br />
purpose of the principle is to prevent the loss, as one ages,<br />
of a sense of the unity of one’s life. Balancing the aspects<br />
of limitation and sociality helps to recognize and not<br />
ignore the elderly patient’s social needs and desire to<br />
maintain some degree of independence. This avoids the<br />
temptation of caregivers to rely on institutional care<br />
when independence cannot be maintained. Silverstone 11<br />
notes that the tendency for the physician to view chronically<br />
impaired patients with a biomedical disease-oriented<br />
framework contributes to a hospital-like solution<br />
to the patient’s problems. This principle can be stated:<br />
“seek out the appropriate level of support and care for<br />
older patient,” a level of care that maximizes independence<br />
and maintains the highest level of functioning.<br />
Because complete independence is usually neither possible<br />
nor desirable, “interdependence” with friends, relatives,<br />
and service providers more aptly describes this<br />
principle. Finally, the aspects of limitation and temporality<br />
suggest the principle of normality. Aging does not<br />
have to be seen as a disease or as a form of deviance. This<br />
principle would argue against treating every age-related<br />
change as a disease or problem to be solved. Rather, the<br />
aging process is valued, given the limitations it imposes,<br />
as a normal part of the human life narrative.<br />
Informed Consent in the Elderly<br />
Respect for Personal Autonomy<br />
Many ethical conundrums in medical ethics are the result<br />
of specific principles coming into conflict in specific cases.<br />
<strong>The</strong> principle of respect for personal autonomy is sometimes<br />
taken to be the overriding principle in modern<br />
ethical deliberation. However, respect for personal autonomy<br />
does not, and should not, exhaust moral deliberation.<br />
Other principles are important and not only when<br />
autonomy reaches its limits. Childress notes that focusing<br />
on the principle of respect for personal autonomy can<br />
foster indifference and that the principles of care and<br />
beneficence are important even in discussions of informed<br />
consent. <strong>The</strong> role played by the principle of respect for<br />
personal autonomy is one of setting limits, such that,<br />
“without the limits set by the principle of respect for<br />
autonomy, these principles (beneficence, nonmaleficence,<br />
and justice) may support arrogant enforcement of “the<br />
good” for others.” 12 Yet, the principle of respect for<br />
autonomy is not absolutely binding and does not outweigh<br />
all other principles at all times. Two different<br />
approaches have been used by ethicists to resolve conflicts<br />
or apparent contradictions between competing<br />
principles. First is to construct an a priori serial ranking<br />
of the principles, such that some take absolute priority<br />
over others. Second, principles can be viewed as prima<br />
facie binding, competing equally with other prima facie<br />
principles in particular circumstances. This view requires<br />
one to view more closely the complexities and particularities<br />
of individual cases and is more situational in<br />
context. <strong>The</strong> prima facie principle of respect for autonomy<br />
can be overridden or justifiably infringed when the<br />
following conditions are satisfied: (1) when there are<br />
stronger competing principles (proportionality); (2) when<br />
infringing on the principle of respect for personal autonomy<br />
would probably protect the competing principles<br />
(effectiveness); (3) when infringing the principle of<br />
respect for personal autonomy is necessary to protect the<br />
competing principle(s) (last resort); and (4) when the<br />
infringement of the principle of respect for personal<br />
autonomy is the least intrusive or restrictive in the circumstances,<br />
consistent with protecting the competing<br />
principle(s) (least infringement). 12
4. Ethical Management of the Elderly Patient 41<br />
Shared Decision Making<br />
Aside from the legal requirements and the specter of<br />
malpractice, recent discussions of “informed consent”<br />
have focused on the concept of “shared decision making”<br />
and the clinical-therapeutic role of the informed consent<br />
process in improving patient care. <strong>The</strong>se discussions<br />
recognize that there should be a collaborative effort<br />
between physicians and patients to arrive at appropriate<br />
treatment decisions. <strong>The</strong> physician brings knowledge and<br />
trained judgment to the process, whereas the patient<br />
brings individual and unique priorities, needs, concerns,<br />
beliefs, and fears. Focusing on the process of informed<br />
consent, as opposed to bare legal requirements, increases<br />
a patient’s participation in his or her own care, which<br />
may result in increased patient compliance and selfmonitoring.<br />
Informed consent as “teaching” (indeed, the<br />
origin of the word “doctor” is from “teacher”) further<br />
diminishes patients’ misconceptions or inaccurate fears<br />
about their situation and prospects and may improve<br />
patient recovery or comfort with a better understanding<br />
of the care that is being provided. No good data are available<br />
regarding these “therapeutic” effects of informed<br />
consent, and further studies seem warranted. Despite<br />
these theoretical positive aspects, issues surrounding<br />
informed consent remain vexing for physicians in a<br />
number of clinical situations from both legal and ethical<br />
perspectives. Even the ideal model of “shared decision<br />
making” does not address many of the realities of medical<br />
practice, including emergency situations, conflicts of interest,<br />
and questions of futility.<br />
By emphasizing informed consent as a temporal<br />
“process,” one can avoid the pitfalls of viewing informed<br />
consent as a single event. Informed consent can never be<br />
reduced to a signature on a consent form. “Perhaps the<br />
most fundamental and pervasive myth about informed<br />
consent is that informed consent has been obtained when<br />
a patient signs a consent form. Nothing could be further<br />
from the truth, as many courts have pointed out to physicians<br />
who were only too willing to believe this myth.” 13<br />
Although a matter of routine in many institutions because<br />
they are seen as providing protection against liability,<br />
informed consent forms actually provide very little. <strong>The</strong><br />
informed consent form does have value in that it provides<br />
an opportunity for the patient to read the information on<br />
the form and to create a locus for the appropriate patient–<br />
physician discussion that is the key element. An informed<br />
consent form merely documents that the “process” of<br />
informed consent has taken place.<br />
Traditionally, consent to anesthesia in the past was<br />
subsumed under the consent to the surgical procedure<br />
and included within the surgery consent form. <strong>The</strong> anesthesiologist<br />
was one step removed from the formal<br />
consent process. Today, separate specific consent for anesthesia<br />
is required in most states. It is imperative that the<br />
Table 4-1. Elements of the process of informed consent.<br />
Threshold elements (preconditions)<br />
Decision-making capacity or competency<br />
Freedom or voluntariness and absence of overriding state or legal<br />
interests<br />
Informational elements<br />
Adequate disclosure of material information<br />
Recommendation<br />
Understanding<br />
Consent elements<br />
Decision<br />
Authorization<br />
anesthesiologist make a concerted effort to adequately<br />
complete this process with the patient and, when appropriate,<br />
the patient’s family regarding the anesthetic procedure<br />
and adequately document in a note the patient’s<br />
consent on the chart or anesthetic record (above and<br />
beyond any signature on a standard form issued by a<br />
ward clerk).<br />
Beauchamp and Childress 14 have broken down the<br />
process of informed consent into seven elements (Table<br />
4-1). <strong>The</strong>se include threshold elements or preconditions,<br />
which include (1) decision-making capacity or competency<br />
of the patient, (2) freedom or voluntariness in decision<br />
making, including absence of overriding legal or<br />
state interests; informational elements including (3) adequate<br />
disclosure of material information, (4) recommendations,<br />
and (5) an understanding of the above; consent<br />
elements, which include (6) decision by the patient in<br />
favor of a plan and (7) authorization of that plan. Several<br />
of these elements can pose particular challenges in the<br />
elderly population.<br />
Threshold Elements<br />
Decision-Making Capacity<br />
Physicians are frequently faced with the problem of<br />
making treatment decisions for elderly patients who no<br />
longer have decision-making capacity. Many diseases and<br />
conditions that can make continued life contingent on<br />
life-prolonging therapies can also destroy or substantially<br />
impair a person’s decision-making capacity and are more<br />
likely to do so in older people. In addition, Alzheimer’s<br />
disease and other forms of dementia are more likely to<br />
be present in older persons. One estimate is that 5% to<br />
7% of persons over 65, and 25% of those over 84, suffer<br />
from severe dementia. 15 Assessment of decision-making<br />
capacity even in cases of mild dementia can be particularly<br />
difficult. 16 Decision-making capacity requires: (1) a<br />
capacity to understand and communicate, (2) a capacity<br />
to reason and deliberate, and (3) possession of a set of
42 P.J. Hoehner<br />
values and goals. 17–19 Although there is general agreement<br />
regarding these three requirements, there is no single,<br />
universally accepted standard of decision-making capacity.<br />
This is because decision-making capacity is not an<br />
all-or-nothing concept. Decision making is also a taskrelated<br />
concept and the requisite skills and abilities vary<br />
according to the specific decision or task. <strong>The</strong> relevant<br />
criteria should also vary according to the risk to a patient.<br />
Basically, one must ask the following questions: Does the<br />
patient understand his or her medical condition? Does<br />
the patient understand the options and the consequences<br />
of his or her decision? Is the patient capable of reasonable<br />
deliberation? Is the patient able to communicate<br />
his or her decision? Does the patient possess a coherent<br />
set of values and/or goals? Several reviews provide<br />
helpful discussions of the clinical assessment of elderly<br />
patients’ decision-making capacity within these contexts.<br />
20–22 Instruments such as the MacArthur Competence<br />
Assessment Tool-Treatment (MacCAT-T) may<br />
provide a flexible yet structured method with which physicians<br />
and other caregivers can assess, rate, and report<br />
patients’ abilities relevant for evaluating capacity to make<br />
treatment decisions. 23<br />
Informed consent in the elderly patient presents other<br />
unique aspects. 24 Sugarman et al. 25 conducted a structured<br />
literature review in the published empiric research<br />
on informed consent with older adults (aged 60 years and<br />
older). Diminished understanding of informed consent<br />
information was associated with older age and with fewer<br />
years of education. Although showing some impairment<br />
in their quality of reasoning, the elderly are able to reach<br />
reasonable risk-taking decisions to the same degree as<br />
young adults. 26,27<br />
To what extent must a patient “understand” his or her<br />
condition, treatment options, and risks? 28 If fully<br />
“informed” is meant to mean fully “educated” 29 then<br />
“informed” consent may be seen as an impossible standard.<br />
However, the primary object of information is to<br />
facilitate the patients’ care rather than providing a litany<br />
of possible complications in order to avoid a lawsuit.<br />
Factual knowledge is used, not as an end in itself, but as<br />
a means to extend the patients’ own understanding in<br />
such a way as to meet their own unique priorities, needs,<br />
concerns, beliefs, and fears so that they may decide about<br />
their care in the manner in which they normally make<br />
similar choices. This will vary from patient to patient and<br />
with the risks of the procedure involved. It is a mistake<br />
to assume that a patient must understand information to<br />
the same extent and in the same manner as a physician,<br />
or even as a well-educated layman. This may indeed be<br />
seen as just as paternalistic as not permitting patients to<br />
participate in decision making at all. 13<br />
Visual and hearing impairments and diminished<br />
memory and comprehension in the elderly patient require<br />
the clinician to exercise particular caution when obtaining<br />
informed consent. 30 One must also be careful to avoid<br />
the mistake of equating recall, a standard endpoint in<br />
many studies on the adequacy of informed consent and<br />
which may be problematic in the elderly, with understanding<br />
and comprehension. Meisel and Kuczewski 13<br />
note that, “While it may be true that someone who cannot<br />
retain information for a few seconds might not be said to<br />
understand it, people often make reasonable decisions<br />
but cannot later recall the premises that supported the<br />
reasoning or the process that led to the conclusion.”<br />
Distant recall of the informed consent process may be an<br />
indicator of the adequacy of a patient’s understanding,<br />
but its absence says little about the patient’s understanding<br />
at the time of consent. Physicians also tend to underestimate<br />
patients’ desire for information and discussion<br />
and, at the same time, overestimate patients’ desire to<br />
make decisions. 31–33 Elderly patients and their physicians<br />
often differ on patient quality-of-life assessments that<br />
may be associated with clinical decisions. 34 <strong>The</strong>se studies<br />
and others underscore the need for clear communication,<br />
individualization, and compassion in obtaining adequate<br />
informed consent in the elderly. New strategies to maximize<br />
comprehension of informed consent information<br />
(e.g., storybooks, videos, and so forth) also may be<br />
useful. 25<br />
Assessment of patient capacity to enter into the process<br />
of informed consent or competency to make rational<br />
medical decisions is a complicated issue. Much has<br />
been written on the criteria for determining individual<br />
capacity and the legally defined characteristic of “competency.”<br />
19,35–38 Competency, unlike the decision-making<br />
capacity, is a legal term and an all-or-nothing concept<br />
specific to a given task. In the absence of a clear medical<br />
diagnosis such as delirium or unconsciousness, decisions<br />
regarding competency must be made with assistance from<br />
psychiatric services, ethics consult services, and/or legal<br />
counsel. In general, decisions must be made in these situations<br />
on the patient’s behalf, either by “substituted judgment”<br />
(a decision based on what the patient would have<br />
wanted, assuming some knowledge of what the patient’s<br />
wishes would have been) with or without the help of<br />
proxy consent or by a decision made according to the<br />
“best interests” of the patient on the basis of a balancing<br />
of a “benefit versus burdens” ratio. An appropriate hierarchy<br />
for surrogate decision makers is delineated, for<br />
example, in a provision of the Virginia Health Care Decisions<br />
Act (Code of Virginia §54.1–2981) as follows: 1. A<br />
legally appointed guardian or committee. 2. <strong>The</strong> patient’s<br />
spouse if no divorce action has been filed. 3. An adult son<br />
or daughter of the patient. 4. <strong>The</strong> patient’s parent. 5. An<br />
adult brother or sister of the patient. 6. Any other relative<br />
of the patient in descending order of relationship. It must<br />
be remembered that the caregiver has an ethical obligation<br />
to evaluate the competency of the surrogate’s<br />
decisions with regard to (1) lack of conflict of interest,
4. Ethical Management of the Elderly Patient 43<br />
(2) reliability of the evidence of the patient’s desires on<br />
which the surrogate is relying, (3) the surrogate’s knowledge<br />
of the patient’s own value system, and (4) the surrogate’s<br />
responsible commitment to the decision-making<br />
process. 39 All these situations involve complex issues and,<br />
again, may require the assistance of hospital ethics committees<br />
or consult services.<br />
Voluntariness<br />
A second threshold element is one of freedom or voluntariness.<br />
Here one asks the question of whether the<br />
patient’s decision is free from external constraints. <strong>The</strong>se<br />
constraints can consist of myriad social, familial, and<br />
even financial factors that can be difficult, if not impossible,<br />
to sort out. However, it is not true that the principle<br />
of respect for autonomy is at odds with all forms of heteronomy,<br />
authority, tradition, etc. Competent individuals<br />
may autonomously choose to yield first-order decisions<br />
(i.e., their decisions about the rightness and wrongness<br />
of particular modes of conduct) to a professional, family,<br />
spouse, or to a religious institution. In these instances, the<br />
person is exercising second-order autonomy in selecting<br />
the professional, person, or institution to which they<br />
choose to be subordinate. In these cases, second-order<br />
autonomy becomes central. 40 <strong>The</strong> distinguishing feature<br />
becomes whether the second-order decision was free and<br />
voluntary. Frequently, elderly patients decide on specific<br />
treatment options with respect for the opinions of family<br />
members, or a concern for their psychologic, physical,<br />
and/or financial well-being. As Waymack and Taler<br />
observe, “It is often the case that health care professionals<br />
find themselves in the care of elderly patients where,<br />
because of the nature of chronic care, families often ask<br />
or are asked to play a significant role.” 41 It is perfectly<br />
appropriate for elderly patients to consider the preferences<br />
of loved ones, and they should not automatically<br />
be encouraged to make decisions concerning treatment<br />
options, particularly life-extending treatments, for exclusively<br />
self-regarding or purely selfish reasons. Moreover,<br />
although undue pressure and influence are clearly<br />
improper, it is a mistake to assume that any advice and<br />
counsel from family members constitutes undue pressure<br />
or influence. However, when elderly patients possess<br />
decision-making capacity, generally they and only they<br />
have the moral authority to decide how much weight to<br />
give the preferences and interests of family members.<br />
While it is true that elderly patients can have ethical<br />
obligations toward family members that have a bearing<br />
on treatment decisions and the interests of family<br />
members can be “ethically relevant whether or not the<br />
patient is inclined to consider them,” 42 they should generally<br />
retain decision-making authority even if physicians<br />
believe that they are failing to give due consideration to<br />
the interests of family members. 43<br />
Informational Elements<br />
Adequate Disclosure<br />
<strong>The</strong> first of the informational elements of informed<br />
consent is adequate disclosure. This is the process of<br />
properly informing the patient of his or her diagnosis,<br />
prognosis, treatment options, risks, and possible outcomes.<br />
<strong>The</strong> anesthesiologist should reveal the specific risks and<br />
benefits of each anesthetic option, the complications of<br />
instrumentation of the airway, the risks and benefits of<br />
invasive monitoring, the presence and use of a fallback<br />
plan, and basis for the anesthesiologist’s recommendations.<br />
44 “Transparency” is a useful term describing the<br />
openness by which the anesthesiologist discusses the<br />
treatment plans with a patient. By “thinking out loud”<br />
regarding the options and plans, the anesthesiologist<br />
communicates the thought processes that he is making<br />
that is going into his or her recommendation, thus<br />
allowing the patient to understand and participate in this<br />
process. Most patients and parents of patients want assurance<br />
and explanation regarding anesthesia, not necessarily<br />
detailed and exhaustive information.<br />
<strong>The</strong> discussion of risks and hazards of the diagnostic<br />
or therapeutic options, as well as information about anticipated<br />
pain or suffering, are, in theory and practice, the<br />
most troublesome aspects of informed consent. According<br />
to the President’s Commission for the Study of Ethical<br />
Problems in Medicine and Biomedical and Behavioral<br />
Research, “Adequate informed consent requires effort on<br />
the part of the physician to ensure comprehension; it<br />
involves far more than just a signature on the bottom of<br />
a list of possible complications. Such complications can<br />
be so overwhelming that patients are unable to appreciate<br />
the truly significant information and to make sound<br />
decisions.” 19 <strong>The</strong> law does not require one to give a list<br />
of every possible complication of a planned procedure<br />
(which may inflict an undue amount of emotional distress),<br />
but only a “reasonable” amount of information.<br />
Negligence is not failure to achieve a good outcome, nor<br />
failure to disclose all remote risks. 45<br />
But just how does one define “reasonable”? <strong>The</strong> courts<br />
have had difficulty as well assessing what a “reasonable”<br />
standard of disclosure may be. <strong>The</strong> most cited standard is<br />
the professional practice standard. 46 This standard defines<br />
reasonable disclosure as what a capable and reasonable<br />
medical practitioner in the same field would reveal to a<br />
patient under the same or similar circumstances. Some<br />
courts have ignored this prevailing standard of disclosure<br />
and shifted the focus from the professional community as<br />
forming the standard to the patients themselves. It focuses<br />
on the “new consumerism” in health care, an extension<br />
of the patient’s right of self-determination, where the<br />
patient is viewed as consumer of health care and the<br />
physician as provider. 47 <strong>The</strong> “reasonable patient standard”<br />
asks what a reasonable patient would consider
44 P.J. Hoehner<br />
reasonable and material to the decision of whether to<br />
consent to a procedure offered. <strong>The</strong> burden, however, is<br />
still on the physician to ascertain just what is reasonable<br />
and material for a hypothetical “reasonable patient.” This<br />
recognizes a significant shift in consent law. As legal standards<br />
continue to evolve, the reasonable patient standard<br />
may become more commonly accepted and eventually<br />
displace the professional practice standard as the majority<br />
opinion in American informed consent law. A further<br />
extension of this line of thinking is the “subjective person<br />
standard.” This standard recognizes that all patients are<br />
different, there is no hypothetical “reasonable person,”<br />
and hence the standard of disclosure must recognize not<br />
only the local standard of care but individual patient<br />
needs and idiosyncrasies as well. One important factor in<br />
all the above is the notion of “causality,” i.e., would additional<br />
information have affected this particular patient’s<br />
decision? What specific, individual concerns did the<br />
patient have that would have most affected his or her<br />
decision whether or not they are part of the local standard<br />
of care for disclosure? <strong>The</strong> risk of vocal cord damage<br />
from a routine intubation may be so small as to not<br />
require mentioning in the normal situation (although this<br />
is debatable). It may, however, be very important for a<br />
professional singer in opting between regional or general<br />
anesthesia.<br />
Recommendation and Understanding<br />
Providing a recommendation and patient understanding<br />
are the other two informational elements in the informed<br />
consent process. <strong>The</strong> principle of patient autonomy does<br />
not require the physician to present the information in<br />
a totally neutral manner, if this were even possible.<br />
Indeed, part of the informed consent process is to present<br />
information to the patient in a way that buttresses a<br />
physician’s recommendations. Persuasion is a justifiable<br />
way for educating patients. This is different from manipulation,<br />
which is defined as inappropriately causing a<br />
certain behavior, and coercion, which is actually threatening<br />
a patient with a plausible punishment so the patient<br />
will act in a certain way.<br />
Assessing patient understanding of the information<br />
presented can be a difficult issue, especially if “standard”<br />
consent forms are relied upon. In one study, 27% of postoperative<br />
surgical patients signing consent forms did not<br />
know which organ had been operated upon, and 44% did<br />
not know the nature of the procedure. 48 Cassileth et al. 49<br />
showed that 55% of cancer patients could list only one of<br />
the major complications for chemotherapy within 1 day<br />
of signing consent forms. Other studies have shown that<br />
risk-specific consent forms do not aid retention 50 and that<br />
decision makers often sign consent forms that they do not<br />
understand. 51 Attempts must be made to educate patients<br />
according to their individual needs and, as has been stated<br />
previously, not to assume a patient must have complete<br />
understanding, but only that necessary given their own<br />
particular situation to come to a reasonable decision. This<br />
will vary from patient to patient and from situation to<br />
situation, and consent forms cannot be relied upon to<br />
provide this information, no matter how detailed.<br />
Consent Elements: Decision and<br />
Autonomous Authorization<br />
Finally, there are the two consent elements: decision and<br />
autonomous authorization. <strong>The</strong> patient must be able to<br />
reach a decision and authorize the physician to provide<br />
the care decided upon. <strong>The</strong> physician must document the<br />
consented-to technique as well as the invasive monitoring<br />
to be used. <strong>The</strong> patient may consent either verbally or in<br />
writing, both are ethically and legally just as valid. It may<br />
be more difficult to provide evidence of verbal consent<br />
after the fact, however, making it all the more important<br />
to document adequately the patient’s response in the<br />
chart. Although lack of an objection is not equivalent to<br />
an authorization, cooperation of patients during performance<br />
of a procedure in the absence of overt verbal<br />
authorization has usually been deemed equivalent to<br />
implied consent and sufficient in cases specifically<br />
addressing these issues. 52<br />
Advance Directives<br />
Advance directives are statements that a patient makes,<br />
while still retaining decision-making capacity, about how<br />
treatment decisions should be made when they no longer<br />
have the capacity to make those decisions. California was<br />
the first state to legalize the “living will” in 1976; by 1985,<br />
35 states and the District of Columbia had enacted similar<br />
laws. In 1991, the Patient Self-Determination Act (PSDA)<br />
became federal law involving all Medicare and Medicaid<br />
providers. <strong>The</strong> PSDA provides that all health care providers<br />
must give all patients written information at the time<br />
of their admission advising them of their rights to refuse<br />
any treatments and to have an advance directive. <strong>The</strong><br />
presence of an advance directive must be documented in<br />
the patient’s record, and discrimination against a person<br />
because they do or do not have an advance directive is<br />
prohibited.<br />
<strong>The</strong>re are two general forms of advance directives.<br />
Living wills are documents stating the desires of the<br />
patient for treatment alternatives, usually to die a<br />
“natural” death and not to be kept alive by advanced<br />
life-support measures. In many states, the patient may<br />
also stipulate wishes regarding fluid and nutrition discontinuation<br />
in the event of persistent vegetative state. Living<br />
wills become effective on the determination of “terminal<br />
illness” or when death is imminent (within 6 months) or
4. Ethical Management of the Elderly Patient 45<br />
Table 4-2. Living will.<br />
Strengths<br />
1. Allows the physician to understand the patient’s wishes and<br />
motivations.<br />
2. Extends the patient’s autonomy, self-control, and<br />
self-determination.<br />
3. Relieves the patient’s anxiety about unwanted treatment.<br />
4. Relieves physician’s anxiety about legal liability.<br />
5. Reduces family strife and sense of guilt.<br />
6. Improves communication and trust between patient and physician.<br />
Weaknesses<br />
1. Applicable only to those in persistent vegetative state or the<br />
terminally ill (patients who have a disease that is incurable and<br />
who will die regardless of treatment).<br />
2. Death must be imminent (likely to occur within 6 months).<br />
3. Ambiguous terms may be difficult to later interpret.<br />
4. <strong>The</strong>re is no proxy decision maker, so:<br />
• It requires prediction of final illness scenario and available<br />
treatment.<br />
• It requires physician to make decisions on the basis of an<br />
interpretation of a document.<br />
Source: Junkerman C, Schiedermayer D. Practical Ethics for Students,<br />
Interns, and Residents. 2nd ed. Hagerstown, MD: University Publishing<br />
Group; 1998. Copyright © 1998 by University Publishing Group. Used<br />
with permission. All rights reserved.<br />
family members with vested interests), legal or regulatory<br />
obstacles, or other problems may hinder a clear decisionmaking<br />
process. <strong>The</strong> American <strong>Geriatric</strong> Society Ethics<br />
Committee has published a position statement that outlines<br />
a strategy for dealing with these situations. 54 <strong>The</strong>y<br />
recommend that health care providers and institutions<br />
develop methods to make decisions for incapacitated<br />
persons without surrogates and to establish mechanisms<br />
for intra-institutional conflict resolution, such as an ethics<br />
committee, to mediate conflicting situations. <strong>The</strong>y also<br />
recommend that surrogate decision-making laws and<br />
policies should not hinder the patient’s ability to die naturally<br />
and comfortably. Evidence from competent patients<br />
in similar circumstances should shape the plan of care for<br />
an individual patient in the absence of evidence that the<br />
patient’s wishes would be otherwise. 54 Other strategies<br />
include the “prior competent choice” standard, which<br />
stresses the values the patient held while competent.<br />
<strong>The</strong> “best interest standard” moves the focus to the<br />
patient’s subjective experience at the time the treatment<br />
is considered. 21<br />
when two physicians make the diagnosis of persistent<br />
vegetative state. <strong>The</strong> strengths and weaknesses of the<br />
living will are outlined in Table 4-2. Living wills have<br />
several weaknesses, including the frequent lack of specific<br />
instructions and the impossibility of any person foreseeing<br />
all the contingencies of a future illness. 53 <strong>The</strong>refore,<br />
many advocate an alternative form of advance directive<br />
known as a Power of Attorney for Healthcare (PAHC).<br />
A PAHC provides for the appointment of a person to act<br />
as a health care agent, proxy, or surrogate to make treatment<br />
decisions when the patient is no longer able. <strong>The</strong><br />
PAHC allows a person to add specific directives and often<br />
will give the designated agent authority to have feeding<br />
tubes withheld or withdrawn. Most PAHCs become<br />
effective when two physicians, or one physician and a<br />
psychologist, determine that the patient no longer has<br />
decision-making capacity. However, this requirement is<br />
not universal, and individual state statutes may vary.<br />
Table 4-3 lists the advantages of the PAHC that may<br />
make it a better option than a living will. Individual state<br />
statutes may differ regarding certain components such as<br />
witnesses and need for notarization. Whichever form of<br />
advance directive a patient chooses to use, both serve a<br />
valuable role in preventing ethical dilemmas if designed<br />
properly and implemented.<br />
In many instances, elderly patients who lack decisionmaking<br />
capacity have neither executed an advance<br />
directive nor previously discussed their preferences<br />
regarding treatment options. Even when surrogates are<br />
available, disagreements among parties (particularly<br />
Table 4-3. Power of Attorney for Healthcare (PAHC).<br />
Activation of PAHC<br />
Lack of decision-making capacity must be certified by two physicians<br />
or one physician and a psychologist who have examined the patient.<br />
Until then, the patient makes all the decisions.<br />
Advantages<br />
1. Physician has someone to talk with—a proxy, a knowledgeable<br />
surrogate—who can provide a substituted judgment of how the<br />
patient would have chosen. If the agent is unable to provide a<br />
substituted judgment, the agent and physician together can use the<br />
best-interest standard (how a reasonable person might choose in<br />
consideration of the benefit–burden concept of proportionality).<br />
2. Provides flexibility; this decreases ambiguity and uncertainty<br />
because there is no way to predict all possible scenarios.<br />
3. Authority of agent can be limited as person desires.<br />
4. Avoids family conflict about rightful agent.<br />
5. Provides legal immunity for physicians who follow dictates.<br />
6. Allows appointment of a nonrelative (especially valuable for<br />
persons who may be alienated from their families).<br />
7. Most forms can be completed without an attorney.<br />
8. Principal may add specific instructions to the agent, such as the<br />
following: “I value a full life more than a long life. If my suffering<br />
is intense and irreversible, or if I have lost the ability to interact<br />
with others and have no reasonable hope of regaining this ability<br />
even though I have no terminal illness, I do not want to have my<br />
life prolonged. I would then ask not to be subjected to surgery or<br />
to resuscitation procedures, or to intensive care services or to other<br />
life-prolonging measures, including the administration of antibiotics<br />
or blood products or artificial nutrition and hydration.” (Adapted<br />
with permission from Bok S. Personal directions from care at the<br />
end of life. N Engl J Med 1976;295:362–369.)<br />
Source: Junkerman C, Schiedermayer D. Practical Ethics for Students,<br />
Interns, and Residents. 2nd ed. Hagerstown, MD: University Publishing<br />
Group; 1998. Copyright © 1998 by University Publishing Group. Used<br />
with permission. All rights reserved.
46 P.J. Hoehner<br />
<strong>The</strong>re remains an urgent role for physicians to educate<br />
their patients, their institutions, and their legislatures<br />
regarding the important role of advance directives in<br />
clinical decision making and the need to remove legislative<br />
and institutional hindrances to providing excellent<br />
care to dying patients and their families. Although playing<br />
an important role in unique circumstances, advance directives<br />
are not a substitute for adequate communication<br />
among physicians, patients, and family about end-of-life<br />
decision making and, in themselves, do not substantially<br />
enhance physician–patient communication or decision<br />
making. 55<br />
Do-Not-Attempt-Resuscitation Orders<br />
in the Operating Room<br />
<strong>The</strong> anesthesiologist is most likely to come into contact<br />
with ethical issues involving advance directives when a<br />
patient is scheduled for surgery with a “do-notresuscitate”<br />
(DNR, or the preferred and more realistic<br />
terminology “do-not-attempt-resuscitation,” DNAR 56 )<br />
order on the chart. As many as 15% of patients with<br />
DNAR orders will undergo a surgical procedure. 57 Wenger<br />
et al. 58 studied a subgroup of the SUPPORT (Study to<br />
Understand Prognoses and Preferences for Outcomes<br />
and Risks of Treatment) database and found that of 745<br />
patients presenting to the operating room (OR), 57 had<br />
a DNAR order. Operative procedures ranged in complexity<br />
and risk from tracheostomy and vascular access<br />
to liver transplantation and coronary artery bypass grafting.<br />
Twenty of the 57 patients had their DNAR order<br />
reversed preoperatively. Two of these patients suffered an<br />
intraoperative cardiac arrest and were resuscitated. Both<br />
patients subsequently died postoperatively. Only one<br />
patient without DNAR order reversal arrested during<br />
surgery and died without attempted resuscitation.<br />
Anesthesiologists and surgeons are generally reluctant<br />
to proceed with surgical intervention if they are not<br />
allowed to intervene in the dying process. <strong>The</strong>y feel that<br />
consent for anesthesia and surgery implies consent for<br />
resuscitation and is inconsistent with a DNAR order. 59,60<br />
Anesthesiologists tend to claim that the induction and<br />
maintenance of anesthesia can often involve creating<br />
conditions in which resuscitation is required. 59 Indeed,<br />
anesthesia itself has at times been referred to as a “controlled<br />
resuscitation.” Because anesthetic agents or procedures<br />
may create conditions requiring resuscitation,<br />
the anesthesiologist ought to have the right to correct<br />
those conditions when possible. Surgeons and physicians<br />
doing other procedures use similar arguments to claim<br />
that if cardiac or pulmonary arrest is a consequence of<br />
their actions they should be allowed to prevent or reverse<br />
those conditions. In a 1993 survey of anesthesiologists by<br />
Clemency and Thompson, 60 almost two thirds of the<br />
respondents assumed DNAR suspension in the perioperative<br />
period and only half discussed this assumption<br />
with the patient/guardian.<br />
This dilemma represents a classic problem in the principled<br />
approach to medical ethics: the conflict of two or<br />
more prima facie ethical principles. If the physician<br />
chooses to act paternalistically to provide what is believed<br />
to be the best treatment at the time, he is giving precedence<br />
to the concept of beneficence over the patient’s<br />
autonomy. If, however, the physician acts to preserve<br />
patient autonomy, he may feel that the duty to do good,<br />
as directed by the principle of beneficence, has been compromised.<br />
Further complicating the issue is that “DNAR”<br />
has multiple definitions and interpretations and involves<br />
a spectrum of procedures that the general public is not<br />
aware of. 61<br />
Although automatic suspension of DNAR orders<br />
during a surgical procedure and for an arbitrary period<br />
postoperatively is the most unambiguous and straightforward<br />
policy, it is now argued that this is inappropriate. 62,63<br />
Statements from both the American Society of Anesthesiologists<br />
and the American College of Surgeons recognize<br />
that this policy effectively removes patients from the<br />
decision-making process, even if they are willing to accept<br />
the risk of operative mortality. <strong>The</strong>y recommend instead<br />
a policy of “required reconsideration” of the DNAR<br />
order, as the patient who undergoes a surgical procedure<br />
faces a different risk/benefit ratio. Both statements are,<br />
however, ambiguous about just how resuscitation is to be<br />
handled in the OR. Two alternatives are presented: (1) to<br />
suspend the DNAR order in the perioperative period,<br />
and (2) to limit resuscitation to certain procedures and<br />
techniques. Because of the complexities surrounding the<br />
nature of resuscitation, public misconceptions and lack of<br />
awareness of these complexities, and the desire to honor<br />
the goals reflected in a patient’s decision to forgo CPR,<br />
a third alternative has been proposed involving a valuescentered<br />
61 or goal-directed 64 approach. By ascertaining<br />
the patient’s goals, values, and preferences rather than<br />
individual procedures, the anesthesiologist is given<br />
greater flexibility in honoring the objectives of the DNAR<br />
order within the clinical context of the arrest. Although<br />
seeking to honor both the autonomy of the patient and<br />
the physician’s duty to beneficence within the spirit of<br />
the original DNAR order, this alternative is not without<br />
its problems. 65 <strong>The</strong> establishment of a physician–patient<br />
relationship that will facilitate a full understanding of a<br />
patient’s values and goals is a daunting, if not impossible,<br />
task for the anesthesiologist confronted with the demands<br />
of a limited preoperative encounter. <strong>The</strong>se concerns may<br />
be even more profound in the elderly population. 66 Physicians<br />
have not been good at predicting the wishes of their<br />
patients regarding resuscitation in other situations, even<br />
after discussion has taken place. 67–69 It does, however,
4. Ethical Management of the Elderly Patient 47<br />
provide a third alternative and recognizes that, despite its<br />
practical limitations and high regard for patient autonomy<br />
in our society, there must always exist a degree of<br />
physician–patient trust in any clinical encounter.<br />
Anesthesiologists need to be actively involved in<br />
their own institutions to develop policies for DNAR<br />
orders in the OR. Open communication among the anesthesiologist,<br />
surgeon, and patient or family must exist to<br />
reach an agreement about DNAR status. Appropriate<br />
exceptions to suspension of a DNAR order in the OR<br />
should be honored. Timing of reinstitution of DNAR<br />
status should also be addressed and agreed upon before<br />
the procedure. Actual experience shows that very few<br />
times will a patient insist on a DNAR status during the<br />
procedure.<br />
Treatment Futility<br />
With respect to informed consent, what if the patient’s<br />
decision is counter to the recommendations of the anesthesiologist<br />
or amounts to something the anesthesiologist<br />
regards as dangerous? Must the physician necessarily do<br />
whatever a patient wants? In short, no. In nonemergent<br />
circumstances, physicians are not obligated to provide<br />
care that they feel is not in their patients’ best interest.<br />
“First, do no harm” is the operative principle in these<br />
situations. It is important again to distinguish in these<br />
cases the negative and positive rights based on or related<br />
to the principle of respect for personal autonomy and to<br />
recognize that the limits on positive rights may be greater<br />
than the limits on negative rights. For example, the positive<br />
right to request a particular treatment may be severely<br />
limited by appropriate clinical standards of care, physician<br />
judgment, or just allocation schemes. Clinicians<br />
should, however, be very cautious when making this claim<br />
and should only do so if absolutely convinced that no<br />
other options are available.<br />
Occasionally, physicians have found it necessary to<br />
justify unilaterally deciding that certain medical interventions<br />
(such as CPR) are “futile” and withhold these interventions<br />
even when a patient or a patient’s family wants<br />
them. <strong>The</strong> notion of medical futility is particularly confusing<br />
and open to different interpretations and abuses.<br />
“Futility” can be defined in several senses. “Strict sense<br />
futility” or “medical” futility is defined when a medical<br />
intervention has no demonstrable physiologic benefit,<br />
e.g., when there have been no survivors after CPR under<br />
the given circumstances in well-designed studies, or in<br />
cases of progressive septic or cardiogenic shock despite<br />
maximal treatment. <strong>The</strong>re are no obligations for physicians<br />
to provide medically futile treatment, even when<br />
families want “everything done.” Unilateral decisions to<br />
withhold treatment (such as DNAR orders) are appropriate<br />
under these circumstances. Usually a DNAR order<br />
may be written on the basis of “futility” when two or<br />
more staff physicians concur in writing and give justification<br />
for their decision. <strong>The</strong> patient or surrogate need not<br />
agree with the decision but must be notified. If there is<br />
disagreement, an ethics consultation may be appropriate<br />
and helpful.<br />
It is rare that a given medical intervention is unlikely<br />
to have any physiologic effect whatsoever and hence futility<br />
may also be defined in a “less strict sense.” In this<br />
instance, there may be a low survival rate but the rate is<br />
not zero. In this case, although the physician may have the<br />
particular expertise to determine whether a particular<br />
intervention is reasonable according to a particular standard<br />
of reasonableness, setting a particular standard<br />
involves a value judgment that goes beyond that expertise.<br />
For example, a 79-year-old cancer patient wants CPR in<br />
the event that he suffers cardiopulmonary arrest because<br />
he believes that any chance that CPR will restore cardiopulmonary<br />
function is worthwhile and that any prolongation<br />
of his life is also valuable and worthwhile (for instance,<br />
by allowing for a family member to return from overseas).<br />
Whereas the physician may assess that the chance of CPR<br />
restoring function is x%, x is greater than zero and whether<br />
the chance of restoring function is reasonable, valuable, or<br />
worthwhile only if it is greater than x% depends primarily<br />
on the patient’s own values. Unilateral decisions may not<br />
be appropriate in this instance, and discussions with the<br />
patient and family should be initiated to provide information<br />
and advice.<br />
Whereas a physician may have the expertise to assess<br />
whether a particular intervention is likely to achieve a<br />
specified outcome, determining whether an outcome is an<br />
appropriate or valuable objective for a patient is dependent<br />
on the patient’s own value judgments. A medical<br />
intervention can be futile in a third sense when it will<br />
have no reasonable chance to achieve the patient’s goals<br />
and objectives. For example, CPR is futile in this sense if<br />
there is no reasonable chance that it will achieve the<br />
patient’s goal of leaving the hospital and living an independent<br />
life. Because medical interventions are futile in<br />
relation to the patient’s goals, this sense of futility provides<br />
a very limited basis for unilateral decisions to<br />
withhold medication interventions that patients want.<br />
<strong>The</strong> American Medical Association Council of Judicial<br />
and Ethical Affairs has commented that resuscitative<br />
efforts “would be considered futile if they could not be<br />
expected to achieve the goals expressed by the informed<br />
patient. This definition of futility not only respects the<br />
autonomy and value judgments of individual patients but<br />
also allows for the professional judgment and guidance<br />
of physicians who render care to patients.” 70<br />
Because the term “futility” tends to communicate a<br />
false sense of scientific objectivity and finality and to<br />
obscure the inherent evaluative nature of the judgments,<br />
it is recommended that physicians avoid using the term
48 P.J. Hoehner<br />
to justify unilateral decisions to withhold life-sustaining<br />
treatment. Rather, physicians should explain the specific<br />
grounds for concluding that interventions generally, or<br />
particular life-sustaining measures, are inappropriate in<br />
the given circumstances. Whereas the statement that a<br />
given intervention is futile tends to discourage discussion,<br />
explaining the grounds for a given judgment in light of<br />
the circumstances and with an understanding of the<br />
patient’s own values and goals tends to invite discussion<br />
and point it in the right direction.<br />
Treatment Redirection and<br />
Palliative Care<br />
Jean Paul Sartre said that “the meaning of life is found<br />
in death,” and how we deal with the aging process determines<br />
how we deal with death and our philosophy of life.<br />
This is most important for the physician and patient when<br />
faced with end-of-life decision making involving treatment<br />
redirection and palliative care options.<br />
Treatment redirection refers to that point in the<br />
patient’s care plan when the patient or surrogate, along<br />
with the health care team, recognizes the need to move<br />
from aggressive curative treatment to supportive palliative<br />
care. <strong>The</strong> 1995 SUPPORT study found that as many<br />
as 50% of patients were subjected to burdensome, curative<br />
treatment because the patient, family, and physician<br />
had not recognized or discussed the realities of the<br />
patient’s condition. 71 Potter suggests three barriers to<br />
meeting the need for treatment redirection. 72 First, clinicians<br />
and patients often are narrowly focused on curative<br />
or ameliorative intervention. Lack of communication<br />
between the physician, who assumes that “they want<br />
everything done,” and the patients and families, who have<br />
different expectations, contributes to this problem. Furthermore,<br />
patients and their families often assume that<br />
physicians have reliable knowledge about what therapies<br />
are effective and which are not because of their intense<br />
focus on curative treatment. A study by Feinstein and<br />
Horwitz, 73 however, shows that evidence-based medical<br />
decisions can only be claimed for less than 20% of clinical<br />
situations.<br />
Second, physicians and patients are often reluctant<br />
or unable to discuss palliation as a treatment option. 74<br />
Although evidence suggests that physicians are more<br />
willing to withhold or withdraw treatment from seriously<br />
ill patients, 57 patients and families continue to report that<br />
there is a lack of physician communication in the area of<br />
shifting treatment to palliative care. 75 Disparity of beliefs<br />
and preferences causes much of this communication<br />
problem.<br />
Finally, there is a lack of knowledge of and confidence<br />
in palliative care by both physicians 76 and society. 77 Part<br />
of the problem is that patients are referred to palliative<br />
care and hospice programs far too late in their hospital<br />
course to do any good. Furthermore, Potter notes that,<br />
“although there is a growing trend toward patients<br />
wanting to be in control of their own death, cultural<br />
diversity factors, belief in the power of medical technology,<br />
and a strong tendency to deny death prevent a<br />
working consensus about how to approach the experience<br />
of dying.” 72 Patients and their families may also be<br />
suspicious that palliative care is a way to save money, a<br />
form of rationing, although there is no empirical evidence<br />
that palliative care is more cost effective. 78<br />
Effective treatment-redirection involves three sequential<br />
steps. 72 First, there must be a system to recognize<br />
clues, both patient signals and physiologic signs, to indicate<br />
that the current form of treatment may not be wanted<br />
or may not be warranted. 79 Second, there must be deliberation<br />
as part of the informed consent process that<br />
focuses on the appropriateness of the current treatment<br />
options. Potter reminds one that “because the patient is<br />
embedded in a social context of family and friends, there<br />
must be an inclusive attitude that searches out the wider<br />
origin of beliefs and preferences in the patient’s moral<br />
community.” 72 Furthermore, the health care providers<br />
themselves must analyze their own personal beliefs and<br />
preferences that can create biases and distort clinical<br />
judgment. An open dialog is a necessary part of the deliberation<br />
process. Third and finally, there must be an implementation<br />
plan that activates excellent palliative care. 80<br />
<strong>The</strong> aim is for both the patient and the health care team<br />
to make a smooth transition from the ultimate goal of<br />
curing to that of caring.<br />
End-of-Life Care<br />
End-of-life palliative care options and decision making<br />
have become increasingly complicated as new forms of<br />
therapy and pain control become available. Pain control<br />
in the terminal stages of many illnesses is one of the<br />
primary goals of effective palliative care and is an area<br />
in which anesthesiologists have a great deal to offer. One<br />
of the most pervasive causes of anxiety among patients,<br />
their families, and the public is the perception that physicians’<br />
efforts toward the relief of pain are sadly deficient.<br />
Studies indicate that their fears may be justified. In a<br />
study of 1227 elderly patients, approximately 20% experienced<br />
moderate or severe pain during the last month of<br />
life and the final 6 hours before death. 81 In another study<br />
of a random sample of 200 elderly community residents<br />
in the last month before death, 66% had pain all or most<br />
of the time. 82 Pain influenced behavioral competence,<br />
perceived quality of life, psychologic well-being, depression,<br />
and diminished happiness. A recent editorial raises<br />
concern that medical, radiation, and surgical oncologists
4. Ethical Management of the Elderly Patient 49<br />
are not effectively treating the pain of patients with<br />
cancer. 83<br />
Fear of inadequate pain relief during the terminal<br />
stages of illness may be responsible for the increasing<br />
interest in euthanasia and physician-assisted suicide<br />
(PAS). It is now commonly accepted that the administration<br />
of large quantities of narcotic analgesics is not euthanasia<br />
when the purpose is to alleviate pain and suffering,<br />
not to shorten the life of the patient. Wanzer et al. 84 note<br />
that:<br />
In the patient whose dying process is irreversible, the balance<br />
between minimizing pain and suffering and potentially hastening<br />
death should be struck clearly in favor of pain relief. Narcotics<br />
and other pain medications should be given in whatever dose<br />
and by whatever route is necessary for relief. It is morally<br />
correct to increase the dose of narcotics to whatever dose is<br />
needed, even though the medication may contribute to the<br />
depression of respiration or blood pressure, the dulling of consciousness<br />
or even death, providing the primary goal of the<br />
physician is to relieve suffering. <strong>The</strong> proper dose of pain medication<br />
is the dose that is sufficient to relieve pain and suffering,<br />
even to the point of unconsciousness.<br />
In this regard, there is clearly a strong need for increased<br />
physician and patient education as well as careful ethical<br />
analysis.<br />
<strong>The</strong> terminal stages of the dying process can be accompanied<br />
by a number of other disturbing symptoms, both<br />
for the family and the patient. Symptoms recorded in the<br />
last 48 hours of life include noisy and moist breathing<br />
(death rattle), restlessness and agitation, incontinence of<br />
urine, dyspnea, retention of urine, nausea and vomiting,<br />
sweating, jerking, twitching, plucking, confusion, and<br />
delirium. 85–87 Appropriate palliative care must take into<br />
account the comfort and care of the patient with regard<br />
to these symptoms as well. 88,89<br />
Despite even the highest quality of palliative care,<br />
many patients still report significant pain 1 week before<br />
death, 90 some of whom request help in hastening death.<br />
Furthermore, patients request a hastened death not<br />
simply because of unrelieved pain, but because of<br />
the wide variety of other unrelieved physical symptoms<br />
in combination with loss of meaning, dignity, and<br />
independence. 91<br />
Confusion may exist about the physician’s moral<br />
responsibility for contributing to the patient’s death. <strong>The</strong><br />
principle of double effect has an important role in ethical<br />
decision making in these instances. Double effect<br />
acknowledges that the intent and desired effect of treatment<br />
is mitigation of symptoms rather than cessation of<br />
life, even though life may be shortened. As frequently<br />
formulated, the principle stipulates that one may rightfully<br />
cause evil (shortening of life) through an act of<br />
choice (treatment of pain) if four conditions are verified:<br />
(1) the act itself, apart from the evil caused, is good or at<br />
least indifferent; (2) the good effect of the act is what the<br />
agent intends directly, only permitting the evil effect; (3)<br />
the good effect must not come about by means of the evil<br />
effect; and (4) there must be some proportionately grave<br />
reason for permitting the evil effect to occur. 92<br />
Public and professional debate and confusion over<br />
PAS continues even after its legalization in Oregon, the<br />
trials of Jack Kevorkian in Michigan, and the experience<br />
in the Netherlands. Anesthesiologists should be particularly<br />
concerned with the debate for two reasons: (1)<br />
because of their unique skills, anesthesiologists may have<br />
a very active role as practitioners of euthanasia, 93 and (2)<br />
the fear of uncontrolled pain relief, an area that anesthesiologists<br />
can provide particular expertise, is a primary<br />
motivation for euthanasia and PAS. 94<br />
PAS differs from euthanasia in that the physician is not<br />
the direct agent in PAS whereby in euthanasia the physician<br />
is the direct agent. However, not all ethicists agree<br />
that PAS and euthanasia differ significantly because of<br />
agency. <strong>The</strong> 1994 edition of the American Medical Association<br />
Code of Medical Ethics states that PAS and<br />
euthanasia are, “fundamentally incompatible with the<br />
physician’s role as healer, would be difficult or impossible<br />
to control, and would pose serious societal risks.” 95 <strong>The</strong><br />
Second Edition (1989) of the American College of<br />
Physicians Ethics Manual reads, “Although a patient may<br />
refuse a medical intervention and the physician may<br />
comply with this refusal, the physician must never intentionally<br />
and directly cause death or assist a patient to<br />
commit suicide.” 96 <strong>The</strong> position statement of the American<br />
<strong>Geriatric</strong>s Society Ethics Committee recommends<br />
that, “For patients whose quality of life has become so<br />
poor as to make continued existence less preferable than<br />
death, the professional standard of care should be that of<br />
aggressive palliation, not that of intentional termination<br />
of life. . . . Laws prohibiting VAE [voluntary active euthanasia]<br />
and PAS should not be changed.” 97 A study by<br />
Koenig et al. 98 showed that the majority of elderly patients<br />
attending a geriatrics clinic did not favor legalization of<br />
PAS. Furthermore, relatives of these patients could not<br />
consistently predict the patients’ attitudes or agree among<br />
themselves. Recently, public and professional attitudes<br />
toward PAS and euthanasia have shifted. <strong>The</strong> Third<br />
Edition (1993) of the American College of Physicians<br />
Ethics Manual, although maintaining that physicians<br />
should make relief of suffering in the terminally ill patient<br />
their highest priority, does not include the strict prohibition<br />
included in the previous edition and is much more<br />
ambiguous regarding PAS and euthanasia. 99<br />
<strong>The</strong> politics of euthanasia and PAS remain controversial.<br />
Physicians should be concerned that renewed interest<br />
in euthanasia and PAS will not divert attention from<br />
the pressing concerns of adequate pain control, treatment<br />
of depression, and symptom management in the terminally<br />
ill and should actively seek alternate ways to address<br />
patient worries regarding loss of control, indignity, and
50 P.J. Hoehner<br />
dependence during the final stages of an illness. <strong>The</strong><br />
elderly, particularly the severely demented, are at the<br />
cutting edge of the debate over PAS and VAE. “Senicide”<br />
is a very real entity in cultural anthropology. It is not<br />
unthinkable that in our aging society, pressure will mount<br />
to take moral guidance from anthropologic data, with<br />
economic concerns replacing the nomadic. 100 Physicians<br />
need to resolve not to let public policy matters interfere<br />
with their duty to the health and welfare of their individual<br />
patients, regardless of age, and to maintain a commitment<br />
to both healing and caring. Anesthesiologists<br />
can provide a unique service to their physician colleagues,<br />
patients, and general population through education and<br />
consultation regarding chronic pain and symptom control<br />
in the terminally ill. Measures must go beyond education<br />
and become an established part of quality assurance. 101<br />
Anesthesiologists can contribute by assisting their hospitals<br />
with means to monitor the treatment of patients in<br />
pain. Despite the growing acceptance among the general<br />
population and the medical community regarding physician<br />
involvement in euthanasia, it is not compatible with<br />
the healer’s mission and art. At its core, killing patients<br />
should never be the means by which symptoms or sufferings,<br />
psychologic or physical, are relieved.<br />
Resource Allocation and the Elderly<br />
Concerned over the increasing cost of health care in the<br />
United States, many health care policy makers claim that<br />
health care rationing is unavoidable. Rationing by age<br />
seems to offer a means of reducing spending on health<br />
care. 102 Many patient-selection decisions in the United<br />
States, such as for heart transplantation, intensive care,<br />
and kidney dialysis and transplantation, have long been<br />
based on age criteria. 103–106 A recent study by Hamel et<br />
al. 107 concludes that older age was associated with higher<br />
rates of decisions to withhold ventilator support, surgery,<br />
and dialysis even after adjustments for differences in<br />
patients’ prognoses and preferences. Older patients with<br />
coronary artery disease were less likely to undergo invasive<br />
and noninvasive testing, 108–110 although studies in<br />
octogenarians show that coronary artery bypass surgery<br />
is highly cost effective and improves their quality of life<br />
in a manner equal to that of a younger population. 111–113<br />
“Age-rationing” implies that elderly patients are denied<br />
access to potentially beneficial health care services to<br />
which younger patients are not denied access. This is to<br />
be distinguished from cost-containment measures that<br />
merely result in withholding medical services that are not<br />
expected to benefit these patients. 114<br />
<strong>The</strong>re are several arguments advanced to defend the<br />
denial of access to scarce and/or costly medical care to<br />
the elderly. One argument is to suggest that elderly<br />
patients are not medically suitable candidates for certain<br />
life-sustaining measures. Even if these measures were to<br />
succeed, the quality of elderly patients’ lives, because of<br />
continued ill health and chronically poor functioning, will<br />
remain poor. Extending life under such circumstances is<br />
not deemed to provide a substantial benefit. This argument<br />
is “ageist” at its core because it is based on false<br />
universal generalizations regarding all elderly patients.<br />
Although the chances of experiencing ill health and<br />
impaired functioning increase with age, many elderly<br />
people are medically suitable candidates for a wide range<br />
of treatment options, and many enjoy good health and<br />
unimpaired functioning. A patient’s overall health status<br />
is generally a more reliable indicator of medical suitability<br />
than age alone.<br />
Another defense of age-rationing holds that greater<br />
benefits are obtained when life-extending treatments are<br />
received by younger patients. <strong>The</strong>se benefits include<br />
overall social welfare (because younger persons are more<br />
productive than the elderly) and cost effectiveness<br />
(because younger patients can be expected to benefit<br />
more and at a lower cost). 115 <strong>The</strong>re are three major difficulties<br />
with this line of argument. First, it again is ageist<br />
in its underlying generalizations. It assumes that elderly<br />
persons are unproductive and fails to take into account<br />
other standards of productivity (general health status,<br />
employment history, and current employment status,<br />
etc.). Second, elderly persons who would fail to receive<br />
treatments and who would die because of age rationing<br />
would bear the burdens, but they would not enjoy any of<br />
the benefits derived from the increased productivity that<br />
is said to result from this argument. <strong>The</strong> shift in the<br />
benefit–burden ratio to a particular class on the basis of<br />
age reveals its injustice and inherent age bias. Finally,<br />
even if it can be claimed that it is more cost effective to<br />
deny certain classes of people access to beneficial health<br />
care, this fails to provide a reason for it being fair or just.<br />
Justice can require greater expenditures.<br />
<strong>The</strong> economic, social, and public policy issues are enormously<br />
complicated and beyond the scope of this chapter.<br />
Rationing scarce medical resources purely on the basis of<br />
a certain age cut-off, however, does not seem to be ethically<br />
justifiable. 114,116–118 <strong>The</strong> growing support in the United<br />
States for age criteria in health care does not have a<br />
sound medical basis. Support more likely reflects certain<br />
social, economic, or even philosophical attitudes and<br />
values not universally shared by society or by other cultures.<br />
This is different from saying that age cannot be<br />
taken into account as a predictor of medical benefit or<br />
prognosis. Kilner 119 endorses the use of age as a “symptom”<br />
or “rule of thumb” in relation to medical assessments of<br />
patients. He states that age “may serve as a tool the physician<br />
uses in applying a medical criterion, not as a criterion<br />
in its own right.” Both the acute physiology and chronic<br />
health evaluation (APACHE) III and the SUPPORT<br />
model include age as one prognostic element, along with
4. Ethical Management of the Elderly Patient 51<br />
other physiologic variables. In neither study does age<br />
seem to have a major role, compared with other variables.<br />
120,121 Physicians must utilize the best available data<br />
on treatment outcomes and costs and assume responsibility<br />
for developing criteria for appropriateness and medical<br />
necessity across the spectrum of patient age and economic<br />
status. Physicians should practice appropriatenessbased,<br />
not cost-based medicine. 122 <strong>The</strong> rapid changes<br />
occurring in the health care system and the recurring<br />
emphases on “bottom-line” management require physicians<br />
to be involved in allocation decisions at both the<br />
professional and public policy level. Rationing policies<br />
and managed care plans must be accompanied by full<br />
disclosure to patients regarding the limits to their care<br />
resulting from these policies and plans, along with a<br />
process of patient advocacy and appeal. Gag rules that<br />
restrict such disclosures are inherently unethical. 123<br />
Clinical Research and the<br />
Elderly Patient<br />
<strong>The</strong> elderly patient with severe dementia or depression,<br />
or incapacitated in the critical care or emergency setting,<br />
represents an extremely vulnerable population, not unlike<br />
that of young children or infants, and presents unique<br />
dilemmas in the area of clinical research ethics. <strong>The</strong><br />
ethical issues raised can be summarized as one of balancing:<br />
(1) protecting potentially vulnerable research par -<br />
ticipants, and (2) advancing knowledge and providing<br />
potentially beneficial new therapies for a special group of<br />
patients. <strong>The</strong>se issues become most manifest when dealing<br />
with psychiatric patients, children, and the adult or elderly<br />
incapacitated patient, usually in a critical care or emergency<br />
setting. 124–130<br />
In terms of the elderly population in particular, there<br />
is no doubt or argument against the proposition that<br />
including the elderly, even those incapacitated or suffering<br />
from severe dementia or depression, in clinical<br />
research designed to benefit this particular population is<br />
both important and necessary. Simply to exclude such<br />
patients from clinical research trials because they lack the<br />
capability for providing informed consent subjects the<br />
entire population of such patients to a trial-and-error,<br />
anecdotally driven practice of medicine that may, ultimately,<br />
end up doing more harm to these patients and<br />
result in increased and unnecessary morbidity and mortality<br />
in the long term. Balanced against this noble task<br />
of advancing our knowledge base for the benefit of future<br />
patients, is the necessity of maintaining high ethical standards<br />
in the process and protecting those participants in<br />
current research trials who may or may not directly<br />
benefit from being subject to the nontherapeutic particularities<br />
and randomization of a research program design.<br />
<strong>The</strong> focus on the prior concern is on the many, i.e., the<br />
entire population of patients who will potentially benefit<br />
from such studies. <strong>The</strong> focus on the latter is the one,<br />
i.e., the individual patient who, by voluntary informed<br />
consent, has forfeited the right to individualized and<br />
purely therapeutic concern for participation in the artificial<br />
environment of the research protocol, whereby the<br />
focus of concern will be primarily on the efficient and<br />
statistically valid accumulation of specific information<br />
for the sake of future benefits. For this reason, patients<br />
who elect to participate in clinical research studies are<br />
protected from study designs that impose more than<br />
minimal risk, that are not designed with expectations to<br />
maintain or improve the condition of the patient, or that<br />
are flawed in their design such that a valid answer to an<br />
appropriate question cannot be obtained. <strong>The</strong> bar for<br />
protection needs to be raised to a higher level for those<br />
patients who are incapacitated and cannot understand<br />
the nature of the research proposal and/or cannot provide<br />
appropriate consent to participate. <strong>The</strong>se patients represent<br />
a particularly vulnerable population that can easily<br />
be exploited.<br />
Proxy or surrogate consent has a longstanding history<br />
in the realm of the purely therapeutic clinical situation.<br />
But to what extent does the ethical reasoning inherent<br />
in proxy or surrogate consent still apply in the clinical<br />
research situation and can the ethical conclusions drawn<br />
from the purely therapeutic physician/patient situation<br />
be univocally transferred to the physician-researcher/<br />
patient-subject research situation? It is common for clinical<br />
researchers to presuppose that there is no problem<br />
with transferring the standards of proxy consent that<br />
exist in the therapeutic relationship into the domain of<br />
clinical research.<br />
<strong>The</strong>re are two major difficulties with this view. <strong>The</strong>se<br />
difficulties stem from a close examination of the two<br />
theoretical foundations upon which proxy or surrogate<br />
consent to treatment rests. <strong>The</strong> first relies on the ability<br />
of close family members, friends, or appointed surrogates<br />
to provide evidence of the patient’s own wishes as to what<br />
they would want in a particular foreseeable circumstance<br />
(substituted judgment). This can either be through personal<br />
knowledge or through available written documents<br />
executed by the patient beforehand. Few patients,<br />
however, actually end up discussing relative issues in any<br />
direct way with friends, family, or their physicians regarding<br />
their future medical care. 14,131 Even fewer are likely<br />
to discuss involvement in clinical research trials in the<br />
event they are incapacitated by an injury or illness. Even<br />
when these discussions have been conducted, studies<br />
show that surrogates and physicians do not accurately<br />
predict patient wishes, in both therapeutic and research<br />
situations. 128,132–134 Many ethicists have raised the question<br />
as to whether anyone can speak with authority for “what<br />
the patient would have wanted” and question whether<br />
this “mythological foundation” for proxy consent should,
52 P.J. Hoehner<br />
in fact, be abandoned. Yet even if a case could be made<br />
that sickness, illness, and death are universal concerns<br />
that can provide at least a point of “sympathy” for a close<br />
friend or relative and thereby provide a modest grounding<br />
for substituted judgment, this is categorically different<br />
from choices that involve participating in medical<br />
research. Choosing to forgo the “therapeutic” for the<br />
“experimental” is, with few extenuating circumstances, a<br />
uniquely personal decision, a decision that is grounded<br />
on the individual particularities of any given research<br />
protocol. If this foundation for substituted judgment<br />
(speaking for what the patient would have wanted) in<br />
the therapeutic situation is in any sense called into question,<br />
it certainly must be even more so in the experimental<br />
situation. Richard McCormick 135 states, “Whether a<br />
person ought to do such things [enroll in a research study]<br />
is a highly individual affair and cannot be generalized<br />
in the way the good of self-preservation can be. And if<br />
we cannot say of an individual that he ought to do these<br />
things, proxy consent has no reasonable presumptive<br />
basis.”<br />
<strong>The</strong> second foundation for proxy or surrogate consent<br />
is that of speaking for the “best interest” of the patient.<br />
<strong>The</strong>rapeutic decisions are often made, in the absence of<br />
any compelling evidence of what the patient specifically<br />
would have wanted, on the basis of what would be in the<br />
best interest of the patient (in emergency situations, treatment<br />
is often assumed to be in the “best interest” of any<br />
patient until proven otherwise). Yet it is difficult to apply<br />
this to the research situation, for in this situation the “best<br />
interest” of the patient is always relegated to the needs<br />
of the study design (e.g., randomization to a particular<br />
treatment group). To think otherwise is to fall victim to<br />
the so-called “therapeutic misconception.” 136–138 Even<br />
physician-investigators are prone to blur clinical trial and<br />
patient care such that their attention is diverted from the<br />
inherent conflicts between the pursuit of science and the<br />
protection of research participants. 139 <strong>The</strong> ethical challenge<br />
is to define the limits on the kinds of research risks<br />
that the proxy can accept on behalf of a noncompetent<br />
patient/subject. Most ethicists and institutional review<br />
boards (IRBs) would agree that if the research is potentially<br />
beneficial or presents minimal risks and that the<br />
knowledge that may be gained would be important to the<br />
class of subjects under study, it would be appropriate for<br />
a surrogate or proxy to grant consent on behalf of the<br />
patient/subject. But how does one define what “minimal<br />
risk” and reasonable benefit is within the context of any<br />
given research proposal? Similarly, how does one balance<br />
the risks against the potential benefits for the subjects or<br />
against the knowledge the research may produce?<br />
In a recent commentary, Karlawish 130 proposes that a<br />
distinction should be made between risks that are justified<br />
by potential benefits for the subjects and risks that are not<br />
justified by those benefits. Proxy consent is permissible if<br />
the risks posed by the components of the research that do<br />
not offer potential benefits for the subjects are no more<br />
than minimal and are justified by the importance of the<br />
knowledge to be gained. <strong>The</strong> risks posed by components<br />
with potential benefits are justified by the state of equipoise:<br />
the expert consensus is that the interventions being<br />
compared are within the standard of care so that equilibrium<br />
exists in the balance between risks and benefits in<br />
the intervention and control groups.<br />
Federal regulations for the protection of research participants,<br />
known as the “common rule,” require that<br />
research involving “vulnerable” subjects include “additional<br />
safeguards” and that the investigator obtains<br />
informed consent from a “legally authorized representative.”<br />
140 Although the rule does not describe safeguards<br />
in detail, and most states have not addressed the question<br />
of who is legally authorized to provide consent, it does<br />
underscore the necessity of protecting vulnerable patients<br />
and their families from exploitation. One possible consideration<br />
(variously proposed by others) is to provide for<br />
two patient surrogates, one of which would be the normal<br />
surrogate that would be provided for in the strict therapeutic<br />
context, and the other a court-designated or IRBapproved<br />
representative that would be able to look after<br />
the particular interests of the patient and family within<br />
the research context. Consent would be required from<br />
both, and either would be able to withdraw the patient<br />
from the clinical trial at any time. Truog et al. 141 have<br />
noted, “<strong>The</strong> most effective protection against exploitation<br />
comes not from the process of informed consent, but,<br />
rather, from the careful oversight and scrutiny of conscientious<br />
institutional review boards.” If this is the case,<br />
then review and control boards, particularly those of<br />
organizations responsible for the publication and dissemination<br />
of the results of research studies, need to take<br />
their role very seriously. <strong>The</strong> identification and discussion<br />
of ethical flaws in current research studies need to be<br />
more openly discussed in the mainstream medical literature<br />
in the hope that these discussions would elevate the<br />
level of ethical practices in human research conducted by<br />
physician-scientists. 142<br />
Summary<br />
1. A clinician’s own view of aging can and will influence<br />
both clinical decision making as well as the application<br />
of ethical principles to individual concrete situations.<br />
Aging does not have to be seen as a disease or as a form<br />
of deviance but rather, the aging process can be valued<br />
given the limitations it imposes as a normal part of the<br />
human life narrative. Furthermore, the geriatric patient<br />
can present with a number of unique perioperative ethical<br />
dilemmas that can challenge accepted medical ethics<br />
paradigms.
4. Ethical Management of the Elderly Patient 53<br />
2. Informed consent is a temporal “process” and can<br />
never be reduced to a signature on a consent form. Proper<br />
informed consent is centered on the notions of open communication<br />
and shared decision making. Compassion,<br />
understanding, and creativity are necessary to overcome<br />
many of the challenges geriatric patients present to the<br />
formal elements of the informed consent process.<br />
3. Advance directives are statements that a patient<br />
makes, while still retaining decision-making capacity,<br />
about how treatment decisions should be made when<br />
they no longer have the capacity to make those decisions.<br />
<strong>The</strong>re are two general forms of advance directives: living<br />
wills and PAHC. PAHCs have several advantages over<br />
living wills. Although playing an important role in unique<br />
circumstances, advance directives are not a substitute for<br />
adequate communication among physicians, patients, and<br />
family about end-of-life decision making.<br />
4. Anesthesiologists need to be actively involved in<br />
their own institutions to develop policies for DNAR<br />
orders in the OR. Open communication among the anesthesiologist,<br />
surgeon, and patient or family must exist to<br />
reach an agreement about DNAR status. Clinicians<br />
should not automatically assume DNAR status to be suspended<br />
in the OR and appropriate exceptions to suspension<br />
of a DNAR order in the OR should be honored.<br />
Timing of reinstitution of DNAR status should also be<br />
addressed and agreed upon before the procedure and<br />
carefully documented.<br />
5. “Futility” is a value-laden term and tends to communicate<br />
a false sense of scientific objectivity and finality.<br />
It is recommended that clinicians avoid the use of the<br />
term and focus on explaining the specific grounds for<br />
concluding that particular interventions are inappropriate<br />
in the given circumstances. Whereas the statement<br />
that a given intervention is futile tends to discourage<br />
discussion, explaining the grounds for a given judgment<br />
in light of the circumstances and with an understanding<br />
of the patient’s own values and goals tends to invite discussion<br />
and point it in the right direction.<br />
6. <strong>The</strong>re are times when clinicians, patients, and their<br />
families need to redirect care from aggressive curative<br />
treatment to supportive palliative care without a sense of<br />
“abandoning” the patient. Anesthesiologists have an<br />
active role in end-of-life palliative care, both in terms of<br />
pain and symptom management. Inadequate pain relief<br />
in the terminal stages of most diseases is a continuing<br />
problem. Anesthesiologists can contribute by assisting<br />
their hospitals with means to monitor the treatment of<br />
patients in pain. Despite the growing acceptance among<br />
the general population and the medical community<br />
regarding physician involvement in euthanasia, it is not<br />
compatible with the healer’s mission and art. Whereas<br />
there are times the dying process should not be prolonged,<br />
it should not be intentionally hastened either. At<br />
its core, killing patients should never be the means by<br />
which symptoms or sufferings, psychologic or physical,<br />
are “relieved.”<br />
7. “Age rationing” implies that elderly patients are<br />
denied access to potentially beneficial health care services<br />
to which younger patients are not denied access.<br />
This is to be distinguished from cost-containment measures<br />
that merely result in withholding medical services<br />
that are not expected to benefit these patients.<br />
8. Some elderly patients in particular settings (such as<br />
with severe dementia or depression, or incapacitated in a<br />
critical care or emergency setting) are extremely vulnerable,<br />
similar to young children or infants, and may present<br />
unique dilemmas in the area of clinical research ethics.<br />
Whereas including the elderly in clinical research designed<br />
to benefit this particular population is both important<br />
and necessary, there is the equal and sometimes competing<br />
necessity of maintaining high ethical standards in the<br />
process and protecting those patients in research trials<br />
who may or may not directly benefit from being subject<br />
to the nontherapeutic particularities and randomization<br />
of a research program design.<br />
References<br />
1. Gadow S. Medicine, ethics, and the elderly. Gerontologist<br />
1980;20(6):680–685.<br />
2. Leach E. Society’s expectations of health. J Med Ethics<br />
1977;1(85):89.<br />
3. Jung PB. Differences among the elderly: who is on the road<br />
to Bremen? In: Hauerwas S, Stoneking CB, Meador KG,<br />
Cloutier D, eds. Growing Old in Christ. Grand Rapids:<br />
William B. Eerdmans; 2003:115.<br />
4. US Department of Health and Human Services. Vital<br />
and Health Statistics: Current Estimates from the National<br />
Health Survey, 1990, Series 10: Data from the National<br />
Health Survey, No. 181. Hyattsville, MD: DHHS, Publication<br />
No. [PHS] 92-1509; 1991.<br />
5. Shelley M. Frankenstein: Or, <strong>The</strong> Modern Prometheus.<br />
London: Penguin Books; 1994.<br />
6. Rieff P. <strong>The</strong> Triumph of the <strong>The</strong>rapeutic: Uses of Faith after<br />
Freud. New York: Harper & Row; 1966.<br />
7. Mayer PJ. Biological theories about aging. In: Silverman P,<br />
ed. <strong>The</strong> Elderly as Modern Pioneers. Bloomington, IN:<br />
Indiana University Press; 1987:21.<br />
8. Spielman BJ. On developing a geriatric ethic: personhood<br />
in the thought of Stanley Hauerwas. J Relig Aging 1989;<br />
5(1/2):23–33.<br />
9. Hauerwas S. A Community of Character: Toward a Constructive<br />
Christian Social Ethic. Notre Dame: University<br />
of Notre Dame Press; 1981.<br />
10. Hauerwas S, Bondi R, Burrell DB. Truthfulness and<br />
Tragedy. Notre Dame: University of Notre Dame Press;<br />
1977.<br />
11. Silverstone B. Preface. In: Haug MR, ed. Elderly Patients<br />
and <strong>The</strong>ir Doctors. New York: Springer; 1981:xii.<br />
12. Childress JF. <strong>The</strong> place of autonomy in bioethics. Hastings<br />
Cent Rep 1990;20:12–17.
54 P.J. Hoehner<br />
13. Meisel A, Kuczewski M. Legal and ethical myths about<br />
informed consent. Arch Intern Med 1996;156:2521–<br />
2526.<br />
14. Beauchamp TL, Childress JF. Principles of Biomedical<br />
Ethics. Oxford: Oxford University Press; 1994.<br />
15. US Congress Office of Technology Assessment. Losing a<br />
Million Minds: Confronting the Tragedy of Alzheimer’s<br />
Disease and Other Dementias. Washington, DC: US Government<br />
Printing Office; 1987.<br />
16. Marson DC, McInturff B, Hawkins L, Bartolucci A, Harrell<br />
LE. Consistency of physician judgments of capacity to<br />
consent in mild Alzheimer’s disease. J Am Geriatr Soc<br />
1998;45(4):453–457.<br />
17. Buchanan AE, Brock DW. Deciding for Others: <strong>The</strong> Ethics<br />
of Surrogate Decision Making. Cambridge: Cambridge<br />
University Press; 1989.<br />
18. President’s Commission for the Study of Ethical Problems<br />
in Medicine and Biomedical Research. Deciding to Forgo<br />
Life-Sustaining Treatment. Washington, DC: US Government<br />
Printing Office; 1982.<br />
19. President’s Commission for the Study of Ethical Problems<br />
in Medicine and Biomedical Research. Making Health<br />
Care Decisions, Volume One: Report. Washington, DC: US<br />
Government Printing Office; 1992.<br />
20. Appelbaum PS, Grisso T. Assessing patients’ capacities<br />
to consent to treatment. N Engl J Med 1988;319(25):<br />
1635–1638.<br />
21. Fellows LK. Competency and consent in dementia. J Am<br />
Geriatr Soc 1998;46(7):922–926.<br />
22. Fitten LJ, Lusky R, Hamann C. Assessing treatment decision-making<br />
capacity in elderly nursing home residents. J<br />
Am Geriatr Soc 1990;38(10):1097–1104.<br />
23. Grisso T, Appelbaum PS, Hill-Fotouhi C. <strong>The</strong> MacCAT-T:<br />
a clinical tool to assess patients’ capacities to make treatment<br />
decisions. Psychiatr Serv 1997;48(11):1415–1419.<br />
24. Ratzan RM. Informed consent in clinical geriatrics. J Am<br />
Geriatr Soc 1984;32(3):176.<br />
25. Sugarman J, McCrory DC, Hubal RC. Getting meaningful<br />
informed consent from older adults: a structured literature<br />
review of empirical research. J Am Geriatr Soc 1998;46(4):<br />
517–524.<br />
26. Dror IE, Katona M, Mungur K. Age differences in decision<br />
making: to take a risk or not? Gerontology 1998;44(2):<br />
67–71.<br />
27. Stanley B, Guido J, Stanley M, Shortell D. <strong>The</strong> elderly<br />
patient and informed consent: empirical findings. JAMA<br />
1984;252(10):1302–1306.<br />
28. Lieberman M. <strong>The</strong> physician’s duty to disclose risks of<br />
treatment. Bull NY Acad Med 1974;50:943–948.<br />
29. Ingelfinger FJ. Informed (but uneducated) consent. N Engl<br />
J Med 1971;287:465–466.<br />
30. Taub HA. Informed consent, memory, and age. Gerontologist<br />
1980;20(6):686–690.<br />
31. Johnston SC, Pfeifer MP. Patient and physician roles in<br />
end-of-life decision making. End-of-Life Study Group. J<br />
Gen Intern Med 1998;13(1):43–45.<br />
32. Stiggelbout AM, Kiebert GM. A role for the sick role.<br />
Patient preferences regarding information and participation<br />
in clinical decision-making. Can Med Assoc J 1997;<br />
157(4):383–389.<br />
33. Strull WM, Lo B, Charles G. Do patients want to participate<br />
in medical decision making? JAMA 1984;252(21):<br />
2990–2994.<br />
34. Starr TJ, Pearlman RA, Uhlmann RF. Quality of life and<br />
resuscitation decisions in elderly patients. J Gen Intern<br />
Med 1986;1:373–379.<br />
35. Midwest Bioethics Center Ethics Committee Consortium.<br />
Guidelines for the determination of decisional incapacity.<br />
Midwest Bioethics Cent Bull 1996:1–13.<br />
36. Weinstock R, Copelan R, Bagheri A. Competence to give<br />
informed consent for medical procedures. Bull Am Acad<br />
Psychiatry Law 1984;12(2):117–125.<br />
37. Roth LH, Meisel A, Lidz CW. Tests of competency to<br />
consent to treatment. Am J Psychiatry 1977;134:279–284.<br />
38. Grisso T, Appelbaum PS. Assessing Competence to<br />
Consent to Treatment: A Guide for Physicians and Other<br />
Health Professionals. Oxford: Oxford University Press;<br />
1998.<br />
39. Pinkerton JV, Finnerty JJ. Resolving the clinical and ethical<br />
dilemma involved in fetal-maternal conflicts. Am J Obstet<br />
Gynecol 1996;175(2):289–295.<br />
40. Dworkin G. Autonomy and behavior control. Hastings<br />
Cent Rep 1976;6(1):23–28.<br />
41. Waymack MH, Taler GA. Medical Ethics and the Elderly:<br />
A Case Book. Chicago: Pluribus; 1988.<br />
42. Hardwig J. What about the family? Hastings Cent Rep<br />
1990;20(2):8.<br />
43. Nelson JL. Taking families seriously. Hastings Cent Rep<br />
1992;22(4):6–12.<br />
44. Waisel DB, Truog RD. Informed consent. <strong>Anesthesiology</strong><br />
1997;87(4):968–978.<br />
45. Crooke D. Ethical issues and consent in obstetric anesthesia.<br />
In: Birnbach DJ, Sanjay S, Gatt SP, eds. Textbook of<br />
Obstetric <strong>Anesthesia</strong>. New York: WB Saunders; 2000:<br />
744–753.<br />
46. Waltz JR, Scheunemann T. Informed consent and therapy.<br />
Northwestern Univ Law Rev 1970;64:628.<br />
47. Gild WM. Informed consent: a review. Anesth Analg 1989;<br />
68:649–653.<br />
48. Byrne J, Napier A. How informed is signed consent? Br<br />
Med J 1988;296:839–840.<br />
49. Cassileth BR, Zupkis RV, Sutton-Smith K, March V.<br />
Informed consent—why are its goals imperfectly realized?<br />
N Engl J Med 1980;302:896–900.<br />
50. Clark SK, Leighton BL, Seltzer JL. A risk-specific anesthesia<br />
consent form may hinder the informed consent process.<br />
J Clin Anesth 1991;3:11–13.<br />
51. Waisel DB, Truog RD. <strong>The</strong> benefits of the explanation of<br />
the risks of anesthesia in the day surgery patient. J Clin<br />
Anesth 1995;7:200–204.<br />
52. Knapp RM. Legal view of informed consent for anesthesia<br />
during labor. <strong>Anesthesiology</strong> 1990;72(1):211.<br />
53. Teno JM, Licks S, Lynn J, et al. Do advance directives<br />
provide instructions that direct care? SUPPORT Investigators.<br />
Study to Understand Prognoses and Preferences<br />
for Outcomes and Risks of Treatment. J Am Geriatr Soc<br />
1997;45(4):508–512.<br />
54. American <strong>Geriatric</strong>s Society Ethics Committee. Making<br />
treatment decisions for incapacitated older adults without<br />
advance directives. J Am Geriatr Soc 1996;44(8):986–987.
4. Ethical Management of the Elderly Patient 55<br />
55. Teno JM, Lynn J, Wenger N, et al. Advance directives for<br />
seriously ill hospitalized patients: effectiveness with the<br />
patient self-determination act and the SUPPORT intervention.<br />
SUPPORT Investigators. Study to Understand<br />
Prognoses and Preferences for Outcomes and Risks of<br />
Treatment. J Am Geriatr Soc 1997;45(4):500–507.<br />
56. Jonsen AR, Siegler M, Winslade WJ. Clinical Ethics. 4th ed.<br />
New York: McGraw-Hill; 1998.<br />
57. La Puma J, Silverstein MD, Stocking CB, Roland D, Siegler<br />
M. Life-sustaining treatment: a prospective study of<br />
patients with DNR orders in a teaching hospital. Arch<br />
Intern Med 1988;148(2193):2198.<br />
58. Wenger NS, Greengold NL, Oye RK, Kussin P, Phillips RS.<br />
Patients with DNR orders in the operating room: surgery,<br />
resuscitation, and outcomes. J Clin Ethics 1997;8:250–257.<br />
59. Truog RD. “Do-not-resuscitate” orders during anesthesia<br />
and surgery. <strong>Anesthesiology</strong> 1991;74(3):606–608.<br />
60. Clemency MV, Thompson NJ. “Do not resuscitate” (DNR)<br />
orders and the anesthesiologist: a survey. Anesth Analg<br />
1993;76:394–401.<br />
61. Thurber CF. Public awareness of the nature of CPR: a case<br />
for values-centered advance directives. J Clin Ethics<br />
1996;7(1):55–59.<br />
62. Committee on Ethics, American College of Surgeons.<br />
Statement on advance directives by patients: do not resuscitate<br />
in the operating room. Am Coll Surg Bull 1994;<br />
79:29.<br />
63. Committee on Ethics, American Society of Anesthesiologists.<br />
Ethical guidelines for the anesthesia care of patients<br />
with do not resuscitate orders or other directives that limit<br />
treatment (1993). 1997:12–13. ASA Standards, Guidelines<br />
and Statements.<br />
64. Truog RD, Waisel DB, Burns JP. DNR in the OR: a goaldirected<br />
approach. <strong>Anesthesiology</strong> 1999;90(1):289–295.<br />
65. Jackson SH, Van Norman GA. Goals- and values-directed<br />
approach to informed consent in the ‘DNR’ patient presenting<br />
for surgery: more demanding of the anesthesiologist?<br />
<strong>Anesthesiology</strong> 1999;90(1):3–6.<br />
66. Sayers GM, Schofield R, Aziz M. An analysis of CPR<br />
decision-making by elderly patients. J Med Ethics 1997;<br />
23:207–212.<br />
67. Krumholz HM, Phillips RS, Hamel MB, et al. Resuscitation<br />
preferences among patients with severe congestive heart<br />
failure: results from the SUPPORT Project. Circulation<br />
1998;98(648):655.<br />
68. Rosin AJ, Sonnenblick M. Autonomy and paternalism in<br />
geriatric medicine. <strong>The</strong> Jewish ethical approach to issues<br />
of feeding terminally ill patients, and to cardiopulmonary<br />
resuscitation. J Med Ethics 1998;24:44–48.<br />
69. Uhlmann R, Pearlman R, Cain K. Physicians’ and spouses’<br />
predictions of elderly patients’ resuscitation preferences.<br />
J Gerontol 1988;43:M115–M121.<br />
70. American Medical Association Council on Ethical and<br />
Judicial Affairs. Guidelines for the appropriate use of donot-resuscitate<br />
orders. JAMA 1981;265(14):1868–1871.<br />
71. SUPPORT Investigators. A controlled trial to improve<br />
care for seriously ill hospitalized patients. <strong>The</strong> study to<br />
understand prognoses and preferences for outcomes<br />
and risks of treatments (SUPPORT). JAMA 1995;274(20):<br />
1591–1598.<br />
72. Potter RL. Treatment redirection: moving from curative to<br />
palliative care. Bioethics Forum 1998;14(2):3–9.<br />
73. Feinstein AR, Horwitz RI. Problems in the ‘evidence’ of<br />
‘evidence-based medicine.’ Am J Med 1997;103:529–535.<br />
74. Weeks JC, Cook EF, O’Day SJ, et al. Relationship between<br />
cancer patients’ predictions of prognosis and their treatment<br />
preferences. JAMA 1998;279(1709):1714.<br />
75. Hanson LC, Danis M, Tulsky JA. What is wrong with endof-life<br />
care? Opinions of bereaved family members. J Am<br />
Geriatr Soc 1997;45:1339–1344.<br />
76. Bulger RJ. <strong>The</strong> quest for mercy: the forgotten ingredient<br />
in health care reform. West J Med 1997;167:362–373.<br />
77. Lynn J, Teno JM, Phillips RS, et al. Perceptions by family<br />
members of the dying experience of older and seriously ill<br />
patients. Ann Intern Med 1997;126(2):97–106.<br />
78. Emanuel E. Cost savings at the end of life. Crit Care Med<br />
1996;25:1907–1914.<br />
79. Randolph AG, Guyatt GH, Richardson WS. Prognosis in<br />
the intensive care unit: finding accurate and useful estimates<br />
for counseling patients. Crit Care Med 1998;26(4):<br />
767–772.<br />
80. Rudberg MA, Teno JM, Lynn J. Developing and implementing<br />
measures of quality of care at the end of life: a<br />
call for action. J Am Geriatr Soc 1997;45(4):528–530.<br />
81. Kaiser HE, Brock DB. Comparative aspects of the quality<br />
of life in cancer patients. In Vivo 1992;6(4):333–337.<br />
82. Moss MS, Lawton MP, Glicksman A. <strong>The</strong> role of pain in<br />
the last year of life of older persons. J Gerontol 1991;56:<br />
P51–P57.<br />
83. Cherny NI, Catane R. Professional negligence in the management<br />
of cancer pain. Cancer 1995;76(2181):2185.<br />
84. Wanzer SH, Federman DD, Adelstein SJ, et al. <strong>The</strong> physician’s<br />
responsibility toward hopelessly ill patients: a second<br />
look. N Engl J Med 1989;320(13):844–849.<br />
85. Lichter I, Hunt E. <strong>The</strong> last 48 hours of life. J Palliat Care<br />
1990;6(4):7–115.<br />
86. Martin EW. Confusion in the terminally ill: recognition<br />
and management. Am J Hosp Palliat Care 1990;73:20–24.<br />
87. Massie MJ, Holland J, Glass E. Delirium in terminally<br />
ill cancer patients. Am J Psychiatry 1983;140(8):1048–<br />
1050.<br />
88. Voltz R, Borasio GD. Palliative therapy in the terminal<br />
stage of neurological disease. J Neurol 1997;244(Suppl 4):<br />
S2–S10.<br />
89. Power D, Kearney M. Management of the final 24 hours.<br />
Ir Med J 1992;85(3):93–95.<br />
90. Coyle N, Adelhardt J, Foley KM, Portenoy RK. Character<br />
of terminal illness in the advanced cancer patient. J Pain<br />
Symptom Manage 1990;5:83–93.<br />
91. Back AL, Wallace JI, Starks HE, Pearlman RA. Physicianassisted<br />
suicide and euthanasia in Washington State. JAMA<br />
1996;275:919–925.<br />
92. May WE. Double effect. In: Reich WT, ed. Encyclopedia<br />
of Bioethics. New York: <strong>The</strong> Free Press; 1978:316–320.<br />
93. Benrubi GI. Euthanasia—the need for procedural safeguards.<br />
N Engl J Med 1992;326(3):197–199.<br />
94. Jonsen AR. To help the dying die: a new duty for anesthesiologists?<br />
<strong>Anesthesiology</strong> 1993;78(2):225–228.<br />
95. American Medical Association Council on Ethical and<br />
Judicial Affairs. Code of Medical Ethics: Current Opinions
56 P.J. Hoehner<br />
with Annotations. Chicago: American Medical Association;<br />
1994.<br />
96. American College of Physicians Ethics Committee. Ethics<br />
Manual. 2nd ed. Ann Intern Med 1989;111(245):335.<br />
97. American <strong>Geriatric</strong>s Society Ethics Committee. Physicianassisted<br />
suicide and voluntary active euthanasia. J Am<br />
Geriatr Soc 1995;43(5):579–580.<br />
98. Koenig HG, Wildman-Hanlon D, Schmader K. Attitudes of<br />
elderly patients and their families toward physician-assisted<br />
suicide. Arch Intern Med 1996;156(19):2240–2248.<br />
99. American College of Physicians Ethics Committee. Ethics<br />
Manual. 3rd ed. Ann Intern Med 1992;117:947–960.<br />
100. Post SG. Euthanasia, senicide, and the aging society. J Religious<br />
Gerontol 1991;8(1):57–65.<br />
101. Hill CS. When will adequate pain treatment be the norm?<br />
JAMA 1995;274:1880–1881.<br />
102. Hamel MB, Phillips RS, Teno JM, Lynn J, Galanos AN,<br />
Davis RB. Seriously ill hospitalized adults: do we spend<br />
less on older patients? SUPPORT Investigators. Study to<br />
Understand Prognoses and Preference for Outcomes and<br />
Risks of Treatment. J Am Geriatr Soc 1996;44:1043–1048.<br />
103. Evans RW, Yagi J. Social and medical considerations<br />
affecting selection of transplant recipients: the case of<br />
heart transplantation. In: Cowan DH, ed. Human Organ<br />
Transplantation. Ann Arbor: Health Administration Press;<br />
1987:27–41.<br />
104. Kjellstrand CM. Age, sex, and race inequality in renal<br />
transplantation. Arch Intern Med 1988;148:1305–1309.<br />
105. Kjellstrand CM, Logan GM. Racial, sexual and age<br />
inequalities in chronic dialysis. Nephron 1987;45:257–263.<br />
106. McClish DK, Powell SH, Montenegro H, Nochomovitz M.<br />
<strong>The</strong> impact of age on utilization of intensive care resources.<br />
J Am Geriatr Soc 1987;35(11):983–988.<br />
107. Hamel MB, Teno JM, Goldman L, et al. Patient age and<br />
decisions to withhold life-sustaining treatments from seriously<br />
ill, hospitalized adults. Ann Intern Med 1999;130:<br />
116–125.<br />
108. Gurwitz JH, Osganian V, Goldberg RJ, Chen ZY, Gore JM,<br />
Alpert JS. Diagnostic testing in acute myocardial infarction:<br />
does patient age influence utilization patterns? <strong>The</strong><br />
Worcester Heart Attack Study. Am J Epidemiol 1991;134:<br />
948–957.<br />
109. Bearden DM, Allman RM, Sundarum SV, Burst NM,<br />
Bartolucci AA. Age-related variability in the use of cardiovascular<br />
imaging procedures. J Am Geriatr Soc 1993;<br />
41:1075–1082.<br />
110. Naylor CD, Levinton CM, Baigrie RS, Goldman BS.<br />
Placing patients in the queue for coronary surgery: do age<br />
and work status alter Canadian specialists’ decisions? J<br />
Gen Intern Med 1992;7:492–498.<br />
111. Sollano JA, Roe EA, Williams DL, et al. Cost-effectiveness<br />
of coronary artery bypass surgery in octogenarians. Ann<br />
Surg 1998;228(3):297–306.<br />
112. Ott RA, Gutfinger DE, Miller M, et al. Rapid recovery of<br />
octogenarians following coronary artery bypass grafting.<br />
J Card Surg 1997;12(5):309–313.<br />
113. Kirsch M, Guesnier L, LeBesnerais P, et al. Cardiac operations<br />
in octogenarians: perioperative risk factors for death<br />
and impaired autonomy. Ann Thorac Surg 1998;66(1):<br />
60–67.<br />
114. Jecker NS, Pearlman RA. Ethical constraints on rationing<br />
medical care by age. J Am Geriatr Soc 1989;37:1067–<br />
1075.<br />
115. Avorn J. Benefit and cost analysis in geriatric care: turning<br />
age discrimination into health policy. N Engl J Med 1984;<br />
310(20):1294–1301.<br />
116. Cassel CK, Neugarten B. <strong>The</strong> goals of medicine in an aging<br />
society. In: Binstock RH, Post SG, eds. Too Old for Health<br />
Care? Controversies in Medicine, Law, Economics, and<br />
Ethics. Baltimore: Johns Hopkins University Press; 1991.<br />
117. Dougherty CJ. Ethical problems in healthcare rationing.<br />
Testimony to the Senate Special Committee on Aging.<br />
Health Prog 1991;72:32–39.<br />
118. Evans JG. Aging and rationing [editorial]. Br Med J 1991;<br />
303:869–870.<br />
119. Kilner JF. Age as a basis for allocating lifesaving medical<br />
resources: an ethical analysis. J Health Polit Policy Law<br />
1988;13(3):405–423.<br />
120. Knaus WA, Harrell FE, Lynn J, et al. <strong>The</strong> SUPPORT prognostic<br />
model. Objective estimates of survival for seriously<br />
ill hospitalized adults. Study to understand prognoses and<br />
preferences for outcomes and risks of treatments. Ann<br />
Intern Med 1995;122(3):191–203.<br />
121. Knaus WA, Wagner DP, Draper EA, et al. <strong>The</strong> APACHE<br />
III prognostic system. Risk prediction of hospital mortality<br />
for critically ill hospitalized adults. Chest 1992;102(6):<br />
1919–1920.<br />
122. Rosenfeld KE, Pearlman RA. Allocating medical resources:<br />
recommendations for a professional response. J Am<br />
Geriatr Soc 1997;45(7):886–888.<br />
123. Biblo JD, Christopher MJ, Johnson L, Potter RL. Ethical<br />
issues in managed care: guidelines for clinicians and<br />
recommendations to accrediting organizations. Bioethics<br />
Forum 1996;12(1):MC/1–MC/24.<br />
124. Karlawish JHT, Sachs GA. Research on the cognitively<br />
impaired: lessons and warnings from the emergency<br />
research debate. J Am Geriatr Soc 1997;45(4):474–481.<br />
125. Capron AM. Incapacitated research. Hastings Cent Rep<br />
1997;27(2):25–27.<br />
126. Prabhu VC, Kelso TK, Sears TD. An update on the PEG-<br />
SOD study involving incompetent subjects: FDA permits<br />
an exception to informed consent. IRB 1994;16(1–2):<br />
16–18.<br />
127. Haimowitz S, Delano SJ, Oldham JM. Uninformed decision<br />
making: the case of surrogate research consent. Hastings<br />
Cent Rep 1997;27(6):9–16.<br />
128. Warren JW, Sobal J, Tenney JH, et al. Informed consent by<br />
proxy: an issue in research with elderly patients. N Engl J<br />
Med 1986;315(18):1124–1128.<br />
129. American College of Physicians. Cognitively impaired subjects.<br />
Ann Intern Med 1989;111(10):843–848.<br />
130. Karlawish JHT. Research involving cognitively impaired<br />
adults. N Engl J Med 2003;348(14):1389–1392.<br />
131. Baskin SA, Morris J, Ahronheim JC, Meier DE, Morrison<br />
RS. Barriers to obtaining consent in dementia research:<br />
implications for surrogate decision-making. J Am Geriatr<br />
Soc 1998;46(3):287–290.<br />
132. Coppolino M, Ackerson L. Do surrogate decision makers<br />
provide accurate consent for intensive care research?<br />
Chest 2001;119(2):603–612.
4. Ethical Management of the Elderly Patient 57<br />
133. Emanuel EJ, Emanuel LL. Proxy decision making for<br />
incompetent patients. JAMA 1992;267:2067–2071.<br />
134. Secker AB, Meier DE, Mulvihill M, Paris BE. Substituted<br />
judgment: how accurate are proxy predictions? Ann Intern<br />
Med 1991;115:92–98.<br />
135. McCormick R. Proxy consent in the experimentation situation.<br />
Perspect Biol Med 1974;18(1):2–20.<br />
136. Appelbaum PS, Roth LH, Lidz CW, Benson P, Winslade W.<br />
False hopes and best data: consent to research and<br />
the therapeutic misconception. Hastings Cent Rep 1987;<br />
April(17):2–20.<br />
137. Hochhauser M. “<strong>The</strong>rapeutic misconception” and “recruiting<br />
doublespeak” in the informed consent process. IRB<br />
2002;24(1):11–12.<br />
138. Miller FG, Rosenstein DL. <strong>The</strong> therapeutic orientation to<br />
clinical trials. N Engl J Med 2003;348(14):1383–1386.<br />
139. Miller FG, Rosenstein DL, DeRenzo EG. Professional<br />
integrity in clinical research. JAMA 1998;280:1449–1454.<br />
140. Department of Health and Human Services. Common<br />
rule, 45 CFR 46. Federal policy for the protection of human<br />
subjects; notices and rules. Federal Register 1991;56:<br />
28003–28032.<br />
141. Truog RD, Robinson W, Randolph A, Morris A. Is informed<br />
consent always necessary for randomized, controlled<br />
trials? N Engl J Med 1999;340(10):804–807.<br />
142. Sade RM. Publication of unethical research studies: the<br />
importance of informed consent. Ann Thorac Surg 2003;<br />
75(2):325–328.
5<br />
Teaching <strong>Geriatric</strong> <strong>Anesthesiology</strong> to<br />
Practitioners, Residents, and Medical Students<br />
Sheila J. Ellis<br />
Care of the geriatric patient will continue to grow in<br />
importance as the geriatric proportion of the population<br />
continues to grow. <strong>The</strong> increasing life expectancy in the<br />
United States and improvements in medical care allow<br />
expansion of surgical procedures into populations once<br />
considered too unstable or frail to recover from the stress<br />
of surgery. <strong>Geriatric</strong> patients undergo the same range of<br />
surgical procedures as younger patients. Some procedures,<br />
such as cataract surgery or prostate resection, may<br />
be performed more frequently in the geriatric patient.<br />
Virtually every medical provider will need to have a thorough<br />
understanding of the needs, complications, and<br />
changes in the elderly. Thus, education in geriatric anesthesia<br />
is essential.<br />
<strong>Geriatric</strong>s in Educational Programs<br />
Medical School<br />
Ideally, the introduction to geriatrics begins in medical<br />
school. <strong>The</strong> geriatric curriculum in medical schools has<br />
grown a great deal in the past several decades. <strong>The</strong><br />
Longitudinal Study of Training and Practice in <strong>Geriatric</strong><br />
Medicine by the Association of Directors of <strong>Geriatric</strong><br />
Academic Programs found that in the academic year<br />
2000 to 2001, 116 of 125 (93%) responding medical<br />
schools included geriatric topics as part of an existing<br />
required course, and 10 of 125 (8%) had a separate<br />
required course. Electives with geriatric topics were<br />
offered as separate courses in 68 schools (54%) and as<br />
part of an elective course in 35 institutions (28%). 1<br />
<strong>Anesthesiology</strong> Residency<br />
<strong>The</strong> formal course of geriatric education usually concludes<br />
with the end of medical school. However, it is now<br />
recognized that structured geriatric education should be<br />
included in anesthesiology training. <strong>The</strong> Accreditation<br />
Council for Graduate Medical Education (ACGME)<br />
requires “appropriate didactic instruction and sufficient<br />
clinical experience in managing problems of the geriatric<br />
population” in accredited anesthesiology residency programs.<br />
2 <strong>The</strong> type and amount of clinical experience that<br />
qualifies as sufficient and the amount of appropriate<br />
didactic instruction remains undefined.<br />
<strong>The</strong> joint American Board of <strong>Anesthesiology</strong> (ABA)/<br />
American Society of Anesthesiologists (ASA) content<br />
outline for in-training examinations also includes a section<br />
titled “<strong>Geriatric</strong> <strong>Anesthesia</strong>/Aging: <strong>The</strong> Pharmacological<br />
Implications, MAC Changes and the Physiological<br />
Implications on CNS, Circulatory, Respiratory, Renal,<br />
and Hepatic Organ Systems.” This is a very incomplete<br />
list, obviously.<br />
<strong>Geriatric</strong>s as Part of<br />
Core Competencies<br />
Residency education in geriatrics can be used to establish<br />
a curriculum to meet the updated required ACGME<br />
competencies. ACGME requires evidence of training and<br />
proficiency in six core areas, including patient care,<br />
medical knowledge, practice-based learning and improvement,<br />
interpersonal and communication skills, professionalism,<br />
and systems-based practice (Table 5-1). 3<br />
Communication Skills<br />
Incorporating these competencies into a geriatric curriculum<br />
may provide a method to evaluate these principles<br />
while advancing geriatric education. A preoperative<br />
assessment of a confused patient can be an opportunity<br />
to teach and assess residents on communication skills.<br />
Interacting with the patient’s caregiver provides an<br />
opportunity for development of interpersonal skills. 4 This<br />
preoperative assessment may be complicated because the<br />
58
5. Teaching <strong>Geriatric</strong> <strong>Anesthesiology</strong> 59<br />
Table 5-1. Core competencies of accreditation council for<br />
graduate medical education.<br />
Patient care<br />
Medical knowledge<br />
Practice-based learning and improvement<br />
Interpersonal and communication skills<br />
Professionalism<br />
Systems-based practice<br />
confused patient may have difficulty transmitting a complete<br />
medical history. Sensory changes such as hearing<br />
loss may challenge the anesthesia trainee to utilize additional<br />
modalities for clear communication, such as hearing<br />
amplification devices or written communication. Transmitting<br />
information to the elderly patient regarding preoperative<br />
medication usage and oral intake requires the<br />
ability to assess patient understanding. All of these communication<br />
skills can be directly observed or can be videotaped<br />
for discussion and additional feedback.<br />
Teaching residents the skills needed for completing<br />
such a challenging preoperative assessment can be<br />
accomplished in a similar manner by direct observation<br />
or through a media presentation. A taped interview can<br />
be used to show students and residents methods for eliciting<br />
information and increasing the information obtained<br />
by improved interpersonal communication. Providing<br />
written instructions for patients can demonstrate improvement<br />
in communication skills.<br />
Communication with other health care providers is<br />
also an important component of care of the elderly<br />
patient. Multiple providers may be involved such as<br />
primary care physicians, specialist physicians, home health<br />
attendants, and caregivers. Maintaining appropriate and<br />
adequate communication with all of these sources should<br />
be encouraged and evaluated.<br />
Systems-Based Practice<br />
A discussion of end-of-life issues and do-not-resuscitate<br />
orders in the perioperative period may be a way to teach<br />
systems-based practice. Systems-based practice requires<br />
an awareness of the larger context and system of<br />
health care. It is essential to understand what a do-notresuscitate<br />
order means in the perioperative period. <strong>The</strong><br />
institutional requirements regarding such notations can<br />
be reviewed while assessing or reconsidering such an<br />
order with the patient or surrogate. Clarification and, if<br />
necessary, modification of a do-not-resuscitate order<br />
should be documented in the medical record. This discussion<br />
can be integrated into the larger experience of health<br />
care beyond the immediate anesthetic needs. Such a discussion<br />
can also be useful to educate the resident and<br />
student in the core competency of professionalism and<br />
adherence to ethical principles in care of the patient.<br />
Practice-Based Learning and Improvement<br />
Practice-based learning and improvement requires the<br />
ability to determine an area that needs improvement,<br />
identify and apply an intervention, and measure impact<br />
of the intervention. 5 Patient-based learning and improvement<br />
seeks to improve patient care through appraisal of<br />
scientific evidence. Perioperative beta blockade can be a<br />
rich source of material for practice-based learning. <strong>The</strong><br />
ability to recognize the current practice regarding perioperative<br />
use of beta blockade and the appropriate application<br />
of this therapy can be an important part of geriatric<br />
education. Incorporating these competencies into a geriatric<br />
curriculum can be a very effective method both for<br />
teaching the student and resident geriatric anesthesia,<br />
and providing a place for evaluation and assessment for<br />
the educational program.<br />
Importance of <strong>Geriatric</strong> Training<br />
For completion of anesthesiology residency, specific criteria<br />
must be fulfilled for pediatrics, including experience<br />
with a set number of anesthetics on a child younger than<br />
1 year of age. In adult patients, the emphasis is on physiologic<br />
changes and specialized procedures, not on the age<br />
of the patient. By requiring a set number of cardiac procedures,<br />
for example, the trainee in anesthesiology will<br />
most likely include a number of elderly patients, but this<br />
is not guaranteed. It is possible that a resident could<br />
have an adequate number of cardiovascular procedures<br />
without performing the majority of these cases on geriatric<br />
patients. Does this matter? Is there a difference in<br />
cardiovascular disease in patients 45 versus 85 years of<br />
age? <strong>The</strong> disease processes may have widely varying<br />
causes, and the patients may have very different intraoperative<br />
and postoperative courses. Elderly patients may<br />
present with atypical presentations of common problems<br />
such as angina that may delay or alter treatment.<br />
<strong>The</strong> older patient has the potential for many adverse<br />
perioperative events. <strong>The</strong> hazards of hospitalization and<br />
surgery in the elderly include adverse drug events, delirium,<br />
functional decline, infection, malnutrition, thromboembolism,<br />
and untreated or undertreated pain. 6<br />
Hospitalization is often followed by an irreversible<br />
decline in functional status and a change in quality and<br />
style of life. Only 20% of patients in a large group returned<br />
to their preoperative functional level after repair of a hip<br />
fracture. 7 In a study of community-dwelling, noninstitutionalized<br />
patients aged 70 years or older hospitalized for<br />
acute medical illness, 31% of the patients declined in<br />
activities of daily living (ADL) at discharge compared<br />
with baseline after a mean length of admission of 8.6 days.<br />
At a 3-month follow-up, 40% reported disabilities related<br />
to ADL or instrumental ADL such as meal preparation
60 S.J. Ellis<br />
or shopping for groceries compared with preadmission<br />
baseline. 8<br />
<strong>The</strong>refore, it is important to have exposure to and<br />
experience with elderly patients, not just to diseases<br />
frequently seen in elderly patients. As a practical matter,<br />
a sampling of cases on a typical day at a hospital,<br />
ambulatory setting, or pain clinic servicing a general<br />
population will provide a number of elderly patients. <strong>The</strong><br />
key should be to look at the patients in these settings as<br />
valuable educational opportunities. We believe that a<br />
resident diary of the number of patients cared for over<br />
the age of 75 would be important to determine if residents<br />
were exposed to an adequate number of geriatric<br />
patients.<br />
Growth of <strong>Geriatric</strong> <strong>Anesthesia</strong><br />
<strong>The</strong> subspecialty fellowship in gerontology continues to<br />
grow with 338 fellows in training programs during 2001–<br />
2001. 9 However, the number of trainees in fellowship<br />
programs still falls short of the number needed to serve<br />
the expanding geriatric population.<br />
<strong>The</strong> field of geriatric anesthesiology is relatively new.<br />
<strong>The</strong> Society for the Advancement of <strong>Geriatric</strong> <strong>Anesthesiology</strong><br />
(SAGA) was established in the United States<br />
in 2000. <strong>The</strong>re is also the Age Anaesthesia Association<br />
that functions in the United Kingdom. As of 2004, there<br />
is not a fellowship or subspecialty track in geriatrics<br />
for anesthesiology trainees. <strong>The</strong>re is a dearth of specific<br />
citations in the medical literature related to the teaching<br />
of geriatric anesthesiology. It is expected that the recognition<br />
of geriatric anesthesia as a separate entity and<br />
the need for further expertise will fuel this branch of<br />
anesthesia.<br />
Teaching <strong>Geriatric</strong>s<br />
Education in geriatric anesthesia is a process that can<br />
be defined separately from teaching. Teaching implies<br />
an activity by an individual or a group causing another<br />
person to know new facts or how to accomplish a new<br />
task. <strong>The</strong> focus is on the teacher, not the learner. 10<br />
However, education is a broader process that results in<br />
a change in behavior on the part of the student. <strong>The</strong> focus<br />
of education is the learner, not the teacher. 10 <strong>The</strong> desired<br />
end result is not a specific ability to perform a task, or<br />
retention of a set of data. <strong>The</strong> goal is a change in behavior<br />
based on experiences. <strong>The</strong>se experiences may be from<br />
direct interaction, indirect observations, or a more remote<br />
learning from lectures, but the desired end result is the<br />
same. If the instruction produces a change in behavior<br />
(and, most likely, attitude), education has been<br />
achieved.<br />
Who is the target audience for education in ger -<br />
iatric anesthesia? Certainly residents in anesthesiology,<br />
student nurse anesthetists, student anesthesiology assistants,<br />
and medical students are focus groups for this<br />
training, and fully trained anesthesiologists through<br />
continuing medical education. Other individuals who will<br />
participate in anesthesia and the other aspects of patient<br />
care are also important and should be included when<br />
considering the establishment or expansion of an education<br />
program for geriatric anesthesia. Preoperative and<br />
postoperative recovery nurses, emergency room personnel,<br />
anesthesia technicians and anesthesia aides, and<br />
respiratory therapists can be included in geriatric education.<br />
Primary care physicians and surgeons certainly<br />
should be exposed to geriatric issues regarding perioperative<br />
medicine.<br />
All of these groups are adult learners who should be<br />
independent and self-directed. 11 <strong>The</strong>re may be many different<br />
reasons for seeking further education but the usual<br />
common factor is a desire for improvement as a clinician.<br />
Whereas formal training programs serve a large number<br />
of adult learners, there are many who utilize other educational<br />
avenues. This may take the form of self-study<br />
continuing medical education courses, lectures at medical<br />
meetings, Internet-based learning, and other opportunities.<br />
<strong>The</strong> desire for professional improvement and the<br />
active search for educational sources make adult learners<br />
very involved in their own education. <strong>The</strong> self-direction<br />
and independence of adult learners is a key trait in producing<br />
changes in their behavior.<br />
Adult learners also use their own experiences as a<br />
resource for learning. <strong>The</strong>y may view the current experience<br />
differently based on their background from others<br />
without a similar amount of experience. This can enhance<br />
education but must be acknowledged and accepted, not<br />
rejected by educators. 12 For example, an anesthesiology<br />
resident with a prior career in nephrology may treat<br />
acid-base management in the operating room differently<br />
from a resident without this experience. A faculty member<br />
who can acknowledge the experience of the student<br />
in this situation will not only provide better clinical care<br />
but also enhance the education of the student. This<br />
approach validates the adult learner and makes the<br />
learner more receptive to education in other areas. <strong>The</strong><br />
previous learning may color the education of the adult<br />
learner so the educator must work to integrate and build<br />
on this, not reject the learning and, in doing so, reject the<br />
learner.<br />
Principles to guiding adult teaching include having the<br />
learner be an active contributor and utilize as much as<br />
possible the current knowledge and experience in the<br />
learner. 11 Learning should closely relate to understanding<br />
and solving real problems that the learner will encounter.<br />
<strong>The</strong>re should be opportunities for practice, with assessment<br />
and constructive feedback from the educator.
5. Teaching <strong>Geriatric</strong> <strong>Anesthesiology</strong> 61<br />
Developing a <strong>Geriatric</strong> Curriculum<br />
Faculty Development<br />
In developing a program for teaching geriatric anesthesia,<br />
the prime consideration is to identify an individual who<br />
will develop geriatric expertise and an interest in geriatric<br />
education. A leader who will take responsibility is vital.<br />
This key person, it is hoped, will provide a core of other<br />
people who can be viewed as mentors to facilitate and<br />
maintain a geriatric curriculum. In other faculty members<br />
with specific areas of interest or expertise, increased<br />
knowledge and emphasis on geriatrics can be used to<br />
supplement the geriatric anesthesia experts. For example,<br />
a cardiovascular anesthesiologist may provide education<br />
in the changes in cardiac function in the elderly whereas<br />
an anesthesia provider with advanced skills in regional<br />
anesthesia may provide insight into peripheral nerve<br />
blocks in this population.<br />
An impediment to faculty development in geriatric<br />
anesthesiology can be the attitude that geriatric anesthesiology<br />
is not sufficiently interesting or academically<br />
rigorous enough to justify the effort toward further development.<br />
Because general anesthesiologists already care<br />
for older patients, many do not feel the need to develop<br />
skills or devote additional clinical or academic time<br />
that is already in short supply. This attitude can be countered<br />
by the requirements for geriatric anesthesia education<br />
from ACGME and the ASA/ABA content outline,<br />
the growth in this area in number of patients and understanding<br />
of aging, and the likelihood for career<br />
advancement.<br />
<strong>The</strong> designation of a geriatric anesthesia faculty<br />
member can be an opportunity for personal career<br />
growth. <strong>The</strong> emergence of geriatric anesthesia as a distinct<br />
subspecialty can allow anesthesiologists to interact<br />
with gerontologists, pharmacists, ethicists, and other specialists.<br />
As an expanding field, there will be multiple possibilities<br />
for research, publication, and leadership. <strong>The</strong><br />
recognition of a host of common perioperative problems<br />
in the elderly such as postoperative cognitive dysfunction<br />
and postoperative delirium that have important longterm<br />
consequences can be an area of research and academic<br />
interest.<br />
Assessment of Resources<br />
Table 5-2. Resources for teaching geriatric anesthesia.<br />
Faculty development programs<br />
Society for Advancement of <strong>Geriatric</strong> <strong>Anesthesia</strong> (SAGA)<br />
Age Anaesthesia Association (United Kingdom)<br />
American Society of Anesthesiologists Syllabus for <strong>Geriatric</strong>s<br />
Portal of <strong>Geriatric</strong>s Online Education (POGOe)<br />
American <strong>Geriatric</strong>s Society<br />
<strong>Geriatric</strong>s Syllabus for Specialists<br />
<strong>Geriatric</strong>s at Your Fingertips<br />
Stanford University <strong>Geriatric</strong>s Education Resource Center<br />
<strong>The</strong> John A. Hartford Foundation Consortium for <strong>Geriatric</strong>s in<br />
Residency Training<br />
After identifying the person (or persons) who has an<br />
interest in geriatric anesthesia and educating others in<br />
this field, there should be an assessment of the resources<br />
available for increasing expertise. Is there a Department<br />
of <strong>Geriatric</strong>s at the educational institution that will<br />
partner with the anesthesiology department? If not, one<br />
could seek local experts in geriatrics in other fields who<br />
would be willing to provide mentoring and advice. Creating<br />
a network with others interested in geriatric anesthesia<br />
can provide support, information, and guidance. This<br />
can be aided by joining societies and organizations<br />
that promote and specialize in geriatrics and geriatric<br />
anesthesiology.<br />
Membership in geriatric-oriented organizations can<br />
provide resources such as didactic lectures, speakers,<br />
journals, and meetings. For anesthesia providers, there is<br />
the SAGA in the United States and Age Anaesthesia<br />
Association in the United Kingdom (vide supra). Membership<br />
in the American <strong>Geriatric</strong> Society (AGS) promotes<br />
interaction with geriatric-oriented individuals in<br />
surgical and related subspecialties, national educational<br />
meetings, and monthly journals. <strong>The</strong> ASA has a geriatric<br />
syllabus available at no cost on their Web site. 13 Organizations<br />
such as these can provide lists of current, peerreviewed<br />
geriatric articles in the medical literature,<br />
available educational grants, geriatric-related meetings,<br />
and speakers (Table 5-2).<br />
Specific institutions may choose to develop multidisciplinary<br />
or specialty-specific seminars for faculty development<br />
in geriatrics. 14 Grants may provide funds for<br />
providing speakers and resources for these seminars or<br />
internal faculty with current geriatric expertise may be<br />
utilized to lead this expansion of geriatric expertise.<br />
Determining a Program’s Needs<br />
Once the geriatric anesthesia specialists have been identified<br />
and outfitted with resources, there should be an<br />
assessment of departmental needs. One method to determine<br />
the needs and desires of the learners is to survey<br />
the students and residents. This can be done to discover<br />
areas of interest or areas that are inadequately covered<br />
by the current curriculum. Determining the aspects of<br />
caring for the elderly patient that are troubling or rewarding<br />
may be helpful. Do the residents and students think<br />
the geriatric curriculum, teaching, and experience are<br />
adequate? If not, what would they change? Assessing<br />
the confidence in teaching geriatric skills to fellow residents<br />
or students may determine areas for improvement.
62 S.J. Ellis<br />
<strong>The</strong> faculty can also be surveyed to find areas of expertise<br />
and interest that may be utilized for teaching geriatric<br />
anesthesia. <strong>The</strong> surveys may be repeated to assess the<br />
efficacy of the geriatric curriculum, and evaluation and<br />
feedback from the learners may help to guide needed<br />
changes.<br />
A survey used at the University of Nebraska Medical<br />
Center sought information regarding the anesthesiology<br />
residents’ confidence in performing specific tasks with<br />
the elderly patient such as functional assessment, discussion<br />
of advance directives and end-of-life issues,<br />
assessment of nutritional status, evaluation of sensory<br />
changes, risk and benefit discussion of proposed surgery,<br />
management of postoperative pain, evaluation for depression,<br />
and determination of the patient’s social support<br />
(personal communication, Dr. Edward Vandenberg,<br />
Omaha, NE, May 5, 2004). <strong>The</strong> survey also included the<br />
residents’ self-assessment of ability to distinguish between<br />
delirium and dementia and provide appropriate care for<br />
each, utilize information on aging physiology and agerelated<br />
pharmacologic changes, and discuss relevant<br />
regulations regarding Medicare. <strong>The</strong> survey assessed the<br />
residents’ desire to learn more about the above topics.<br />
This information was gathered on an annual basis to<br />
determine the areas of change desired in the curriculum<br />
as well as an assessment of the efficacy of the current<br />
curriculum.<br />
Producing a <strong>Geriatric</strong> Curriculum<br />
After an assessment of the department’s resources and<br />
needs is completed, a curriculum for geriatric education<br />
can be developed. Multiple teaching modalities should be<br />
incorporated into the development of this curriculum.<br />
<strong>The</strong>re may be considerable overlap between the curriculum<br />
for residents and medical students although it may<br />
be necessary to condense the curriculum and didactics for<br />
medical students. Medical students’ exposure to geriatrics<br />
will likely be covered in primary care rotations or separate<br />
geriatric clerkships. In many schools of medicine, it<br />
is part of a longitudinal educational continuum over at<br />
least 2 years. <strong>Geriatric</strong> anesthesia can be included in these<br />
or in the anesthesiology rotation.<br />
Sample Curriculum<br />
Table 5-3 shows an example of a geriatric curriculum for<br />
an anesthesiology residency.<br />
Didactics<br />
<strong>The</strong> geriatric curriculum can be integrated into the educational<br />
program of the residency program as a specific<br />
dedicated geriatric unit or integrated into the educational<br />
cycle of each subspecialty rotation. At the University of<br />
Nebraska Medical Center, the residency curriculum is 18<br />
Table 5-3. Sample geriatric curriculum for an anesthesiology<br />
residency.<br />
A. Physiology of aging<br />
1. Gerontology<br />
2. Cardiovascular<br />
3. Respiratory<br />
4. Central and autonomic nervous system<br />
5. Renal and hepatic<br />
B. Pharmacology of aging<br />
1. Induction agents<br />
2. Opioids<br />
3. Neuromuscular blockade<br />
4. Sedatives and hypnotics<br />
5. Cardiovascular medications<br />
C. Preanesthetic evaluation<br />
1. Anesthetic risk and the elderly<br />
2. Guidelines for cardiac evaluation for noncardiac surgery<br />
3. Age-related disease<br />
4. Managing medical illness in the surgical patient<br />
5. Atypical presentations of common diseases in the elderly<br />
D. Pain control in the elderly patient<br />
1. Acute pain control<br />
2. Chronic pain management<br />
E. <strong>Regional</strong> anesthesia<br />
F. Ethics and palliative care in geriatrics<br />
G. Postoperative delirium and postoperative cognitive dysfunction<br />
H. Special concerns in caring for the elderly<br />
1. <strong>The</strong> elderly ambulatory surgery patient<br />
2. Critical care<br />
3. Sedation and procedures in remote locations<br />
4. <strong>The</strong> elderly trauma patient<br />
months in length so that residents are exposed to the<br />
entire didactic schedule twice during residency. <strong>The</strong> geriatric<br />
curriculum is inserted into the appropriate block.<br />
For example, during the time frame for preanesthesia<br />
evaluation and anesthetic risk, a lecture is given focusing<br />
on the preanesthetic evaluation of the geriatric patient<br />
and perioperative beta blockade is emphasized.<br />
For didactic lectures, speakers may be utilized from<br />
complementary departments including gerontology, pharmacology,<br />
surgery, and internal medicine. Visiting professors<br />
can also be invited to provide information.<br />
Discussion Groups<br />
Journal clubs may be used to provide a more informal<br />
setting for a geriatric discussion group. This can be led<br />
and organized by the faculty member responsible for<br />
geriatric education or residents, and can provide interaction<br />
outside of the operating room. Case conferences and<br />
problem-based learning discussions allow specific examples<br />
and small group discussions that may provide for a<br />
more personal level of interaction and feedback. Such<br />
discussions with more relevant, reality-based learning in<br />
a smaller group may be more interesting to the adult<br />
learner than limiting geriatric education to lectures.<br />
Problem-based learning discussions can be based on
5. Teaching <strong>Geriatric</strong> <strong>Anesthesiology</strong> 63<br />
actual cases or can be altered to incorporate a variety of<br />
teaching points in a concise manner.<br />
Journal clubs, problem-based learning discussions, and<br />
case conferences are excellent opportunities to discuss<br />
current controversies in medical care, examine the<br />
medical literature, and reinforce topics covered in didactic<br />
lectures.<br />
Reference Books<br />
A library of geriatric anesthesiology references is helpful<br />
for consolidating information in an easily accessible location.<br />
<strong>The</strong>re are multiple textbooks in geriatric medicine,<br />
gerontology, geriatric anesthesia, and geriatric surgery<br />
that should be available for consultation. <strong>The</strong>se books<br />
should be available to the department members. <strong>The</strong><br />
“<strong>Geriatric</strong> Syllabus for Specialists” and “<strong>Geriatric</strong>s at<br />
Your Fingertips,” produced by the AGS, are valuable,<br />
pocket-sized resources that can be maintained in a reference<br />
library or acquired for each resident.<br />
Computer-Based Materials<br />
Internet-based resources are growing both in number<br />
and accessibility. <strong>The</strong> Portal of <strong>Geriatric</strong>s Online Education<br />
(POGOe) is an online clearinghouse that provides a<br />
single source of peer-reviewed educational products for<br />
those interested in geriatric education. <strong>The</strong>ir site, www.<br />
pogoe.org, is funded by a grant from the Donald<br />
W. Reynolds Foundation to the Association of <strong>Geriatric</strong><br />
Academic Programs. Physicians in training and practicing<br />
physicians may use the programs available.<br />
Other educational materials that may be utilized are<br />
computer-based self-instruction modules in geriatrics.<br />
<strong>The</strong>se may be available via the Internet or on CD or<br />
DVD formats. <strong>The</strong> Stanford University <strong>Geriatric</strong>s Education<br />
Resource Center and other locations have teaching<br />
resources available. An initiative funded by the John A.<br />
Hartford Foundation has developed the Consortium for<br />
<strong>Geriatric</strong>s in Residency Training. Institutions or individual<br />
faculty members may also choose to develop their<br />
own educational materials tailored to their specific<br />
requirements. Web-based computer modules can be<br />
created or utilized from sites such as POGOe or the<br />
Stanford University <strong>Geriatric</strong>s Education Resource<br />
Center to be used for education of medical students or<br />
residents. <strong>The</strong>se offerings may also be available to practitioners<br />
who are not in a formal training program. Such<br />
computer modules can be case-oriented and allow the<br />
learner to progress at his or her own pace. This can expose<br />
the student or resident to topics that may not be covered<br />
in a clinical situation and allow for immediate feedback<br />
and evaluation. Pre- and postmodule examinations can<br />
be used to determine information retention. If further<br />
discussion and evaluation is desired, a faculty-led discussion<br />
session can emphasize learning points and provide<br />
another avenue for those using the modules to provide<br />
feedback and evaluation. <strong>The</strong> Web-based modules can<br />
either be tailored to medical student or resident educational<br />
needs, or both groups can use the same module.<br />
Simulation<br />
<strong>The</strong> use of simulators for education is increasing as a<br />
greater number of institutions acquire the equipment and<br />
gain experience with the advantages of simulation education.<br />
<strong>The</strong> simulators can be used for multiple types of<br />
cases and provide a wide range of experience for the<br />
student and trainee. Simulation should include patients<br />
with coexisting morbidities and intraoperative and postoperative<br />
changes in organ systems, as well as providing<br />
experience with life-threatening processes or rare conditions<br />
that may not be experienced by the trainee in a<br />
clinical situation. Simulation can be primarily software<br />
based or may have intricate mannequins, creating the feel<br />
and responsiveness of an actual geriatric patient. <strong>The</strong>re<br />
are many types available, from whole-body simulators to<br />
specific airway or regional anesthesia modes. Receiving<br />
feedback and constructive criticism with objective data<br />
can be a very valuable part of the experience. <strong>The</strong> encounters<br />
may be videotaped, and the computer will maintain<br />
information on each action. An advantage of simulators<br />
is the ability to teach all levels of learners and a wide<br />
variety of careers such as anesthesia practitioners, critical<br />
care nurses, allied health professionals, and medical<br />
students.<br />
Evaluation of Curriculum<br />
<strong>The</strong> effectiveness of a geriatric anesthesia curriculum<br />
must be evaluated; this can be accomplished in a number<br />
of ways. If the geriatric curriculum is covered in a core<br />
unit, a posttest can be used to determine informational<br />
retention and attainment of basic facts and knowledge. A<br />
pretest before introduction of the geriatric curriculum<br />
could be useful to gauge the change in basic knowledge<br />
that will be demonstrated in the posttest. An evaluation<br />
of attitude change and self-perception of knowledge may<br />
be garnered from a survey of the participants.<br />
Behavioral change is the ultimate desire of education.<br />
<strong>The</strong> ability to measure a change in behavior is difficult<br />
but may be reflected in the learner’s professionalism and<br />
practice patterns. In a residency program, the use of 360-<br />
degree evaluations may be a useful tool for assessment.<br />
Faculty members, nurses, and other health care and<br />
support personnel can evaluate the resident attitudes and<br />
actions. <strong>The</strong> use of patient and family comments can be<br />
utilized in a constructive manner to note positive aspects<br />
of performance as well as areas for improvement. Feedback<br />
with suggestions for improvement can be given to<br />
the residents and students.
64 S.J. Ellis<br />
Summary<br />
<strong>The</strong> number of geriatric patients is certain to increase. It<br />
is recognized that the academic programs in anesthesiology<br />
need to address the topic of geriatric anesthesia and<br />
prepare students to care for elderly patients. <strong>The</strong> expected<br />
growth in the older population and the increase in the<br />
number of operations for patients defined as elderly<br />
demand a well-trained profession able to meet the needs<br />
of this group. <strong>The</strong>re are many avenues of medical knowledge<br />
such as postoperative cognitive dysfunction that are<br />
just beginning to be explored, along with further insight<br />
into the physiologic changes of aging and the effects of<br />
coexisting medical conditions.<br />
<strong>The</strong> medical school curriculum has changed in the past<br />
several decades to reflect an increased emphasis on geriatrics<br />
in the primary care fields. Beyond the primary care<br />
fields, the establishment of geriatric specialists has been<br />
lagging. <strong>The</strong> education of students and residents in geriatric<br />
anesthesiology will require an increased emphasis in<br />
these training programs.<br />
Establishing a geriatric anesthesiology curriculum<br />
requires an understanding of the needs of the adult learner<br />
who is self-directed, independent, and driven by internal<br />
motivation and the need for self-improvement. <strong>The</strong> adult<br />
student brings a set of experiences that can serve as a<br />
resource for further education but must be acknowledged<br />
and validated by the teacher. <strong>The</strong> desire for education that<br />
is practical and useful in everyday situations places an<br />
emphasis on teaching methods that utilize this, such as<br />
problem-based learning or case-oriented discussions with<br />
less desire for traditional lectures.<br />
Identifying a single individual to be responsible for<br />
geriatric anesthesiology education is imperative. Identifying<br />
and encouraging other faculty interested in geriatric<br />
anesthesia is a key component in establishing and maintaining<br />
a geriatric curriculum. This interest can be<br />
enhanced by the realization that a great opportunity<br />
exists to have an impact on a field that is rapidly growing<br />
and gaining in recognition. Even one individual can have<br />
an effect on an institution and, by networking with other<br />
similarly interested people locally and at a distance, on<br />
the profession as a whole.<br />
<strong>The</strong> involvement in geriatric anesthesia and geriatric<br />
societies provides a source of information and benefits<br />
such as scholarly journals, meetings, and educational<br />
opportunities.<br />
Development of a geriatric anesthesia program requires<br />
an inventory of a department’s resources and needs.<br />
Surveys and evaluations can be used to determine areas<br />
of strength or inadequate coverage in the current or proposed<br />
curriculum. Many modalities may be incorporated<br />
in the educational program including faculty lectures,<br />
visiting speakers, computer-based modules, journal clubs,<br />
case conferences and problem-based learning groups,<br />
simulations, discussion groups, and Internet-based<br />
resources. Educational materials may be tailored to a<br />
specific anesthesia program or adapted from available<br />
sources such as the POGOe.<br />
Increasing geriatric anesthesiology education in a<br />
residency program may allow incorporation of core<br />
competencies required for graduate medical education.<br />
Education and evaluation in practice-based learning and<br />
improvement, professionalism, and systems-based practice<br />
can be used in conjunction with geriatric anesthesiology.<br />
Proficiency in medical knowledge, patient care, and<br />
communication are all essential attributes for geriatric<br />
anesthesiology.<br />
<strong>Geriatric</strong> anesthesiology and geriatric anesthesia education<br />
will continue to grow and improve. By focusing<br />
time and resources on training anesthesia providers in<br />
the care of the elderly patient, the results will be better<br />
trained practitioners who can meet the needs of this<br />
growing population. <strong>The</strong> field of anesthesiology must<br />
incorporate geriatric anesthesiology education in all<br />
levels of its teaching.<br />
References<br />
1. <strong>The</strong> Association of Directors of <strong>Geriatric</strong> Academic<br />
Programs. Longitudinal study of training and practice in<br />
geriatric medicine. Available at: www.adgapstudy.uc.edu.<br />
Accessed August 13, 2004.<br />
2. Accreditation Council for Graduate Medical Education.<br />
Program requirements for anesthesiology. Available at:<br />
www.acgme.org/downloads/RRC_progReq.040pr703_u804.<br />
pdf. Accessed January 15, 2007.<br />
3. Accreditation Council for Graduate Medical Education.<br />
Outcome project, general competencies. Available at: www.<br />
acgme.org/outcome/comp/compMin.asp. Accessed January<br />
15, 2007.<br />
4. Barnett SR. <strong>Geriatric</strong> education: “Start low, go slow.” ASA<br />
Newslett 2004;68(5):9–10.<br />
5. Lynch DC, Swing SR, Horowitz DS, et al. Assessing<br />
practice-based learning and improvement. Teach Learn<br />
Med 2004;16(1):85–92.<br />
6. Interdisciplinary Leadership Group of the American <strong>Geriatric</strong>s<br />
Society. A statement of principles: toward improved<br />
care of older patients in surgical and medical specialties. J<br />
Am Geriatr Soc 2000;48:699–701.<br />
7. Creditor MC. Hazards of hospitalization in the elderly. Ann<br />
Intern Med 1993;118(3):219–223.<br />
8. Sager MA, Franke T, Inouye SK, et al. Functional outcomes<br />
of acute medical illness and hospitalization in older persons.<br />
Arch Intern Med 1996;156(6):645–652.<br />
9. Warshaw GA, Bragg EJ, Shaull RW, et al. <strong>Geriatric</strong><br />
medicine fellowship programs: a national study from the<br />
Association of Directors of <strong>Geriatric</strong> Academic Programs’<br />
Longitudinal Study of training and practice in geriatric<br />
medicine. J Am Geriatr Soc 2003;51(7):1023–1030.<br />
10. Schwartz AJ. Teaching anesthesia. In: Miller RD, ed.<br />
<strong>Anesthesia</strong>. 6th ed. New York: Churchill Livingstone; 2005:<br />
3105–3117.
5. Teaching <strong>Geriatric</strong> <strong>Anesthesiology</strong> 65<br />
11. Kaufman DM. Applying educational theory in practice.<br />
BMJ 2003;326:213–216.<br />
12. Newman P, Peile E. Valuing learners’ experience and<br />
supporting further growth: educational models to help<br />
experienced adult learners in medicine. BMJ 2002;325:<br />
200–202.<br />
13. American Society of Anesthesiologists. Syllabus on ger -<br />
iatric anesthesiology. Available at: www.asahq.org/clinical/<br />
geriatrics/syllabus.htm. Accessed August 15, 2004.<br />
14. Williams BC. Building geriatrics curricula in medical and<br />
surgical house officer programs through faculty development.<br />
Acad Med 2002;77(5):458.
6<br />
Research Priorities in <strong>Geriatric</strong><br />
<strong>Anesthesiology</strong>*<br />
Christopher J. Jankowski and David J. Cook<br />
<strong>The</strong> implications of an aging population on the practice<br />
of anesthesiology are profound. Normal aging results in<br />
diminished functional reserve across organ systems. <strong>The</strong>se<br />
normal physiologic changes and age-related disease<br />
combine to limit the ability of the elderly to tolerate<br />
the stress of the perioperative period. Thus, geriatric<br />
issues affect every aspect of the care provided by the<br />
anesthesiologist.<br />
For example, age-related physiologic changes and<br />
disease make the preoperative evaluation of geriatric<br />
patients more complex than that of younger patients.<br />
Baseline functional reserve is often difficult to assess<br />
because of limits in physical ability, either from deconditioning,<br />
age-related disease, cognitive impairment, or a<br />
combination of the three. <strong>The</strong> same issues make the maintenance<br />
of intraoperative homeostasis more challenging<br />
in this population. Finally, geriatric issues such as postoperative<br />
respiratory complications and cognitive changes,<br />
as well as acute and chronic pain management can make<br />
postoperative care challenging.<br />
Despite these issues, surprisingly little research has<br />
been done to address the perioperative care of the aged,<br />
per se. This chapter will review some of the literature<br />
pertaining to this population in order to identify potentially<br />
fruitful areas of research.<br />
First, some of the normal physiologic changes that<br />
occur with aging will be reviewed. This is essential to<br />
frame any discussion of preoperative assessment or intraand<br />
postoperative management. Second, the preoperative<br />
evaluation of the older surgical patient will be<br />
discussed. Third, research related to the intraoperative<br />
management of geriatric patients will be described. Last,<br />
*This chapter is based on work performed for “New Frontiers<br />
in <strong>Geriatric</strong>s Research: An Agenda for Surgical and Related<br />
Medical Specialties,” a component of the American <strong>Geriatric</strong>s<br />
Society’s <strong>Geriatric</strong>s-for-Specialists Initiative (GSI), funded by<br />
the John A. Hartford Foundation of New York. With permission<br />
of the American <strong>Geriatric</strong>s Society.<br />
the chapter will address geriatric issues in postoperative<br />
management, emphasizing postoperative respiratory and<br />
cognitive complications, as well as acute and chronic pain<br />
management. Each section will conclude with a list of<br />
potential research agenda items. <strong>The</strong> end of the chapter<br />
identifies research agenda items of the highest priority.<br />
Physiologic Changes Relevant to<br />
Perioperative Care<br />
<strong>The</strong> physiology of aging bears on preoperative assessment,<br />
intraoperative and postoperative management, and<br />
the types and likelihood of major adverse events. Agerelated<br />
changes in cardiac, respiratory, neurologic, renal,<br />
and pharmacokinetics have been well defined. <strong>The</strong> most<br />
important generalization from physiologic studies of<br />
aging is that the basal function of the various organ<br />
systems is relatively uncompromised by the aging process.<br />
However, functional reserve, specifically the ability to<br />
compensate for physiologic stress, is reduced (Figure 6-1).<br />
This has profound implications for the preoperative<br />
assessment and the perioperative care of geriatric<br />
patients.<br />
Cardiovascular Changes<br />
Numerous changes in cardiovascular function with aging<br />
have implications for anesthetic care. With aging, a progressive<br />
decrease in the elasticity of the arterial vasculature<br />
leads to an increase in systolic blood pressure.<br />
Diastolic blood pressure increases through middle age<br />
and typically decreases after age 60. 1 <strong>The</strong>re is also a<br />
decrease in the cross-sectional area of the peripheral vascular<br />
bed, resulting in higher peripheral vascular resistance.<br />
2 A decrease in the peripheral vasodilatory response<br />
to β-adrenergic stimulation may also contribute to the<br />
hypertension of aging. 3<br />
66
6. Research Priorities in <strong>Geriatric</strong> <strong>Anesthesiology</strong> 67<br />
important as the chronic changes in the myocardium and<br />
vasculature.<br />
It is evident that age-related changes in the cardiovascular<br />
system involve alterations in both mechanics<br />
and control mechanisms; the same can be said of the<br />
pulmonary system.<br />
Pulmonary Changes<br />
Figure 6-1. Functional reserve is the difference between<br />
maximal (broken line) and basal (solid line) function. Aging<br />
inevitably reduces functional reserve even in individuals who<br />
are physiologically “young.” <strong>The</strong> configuration of the curve for<br />
“basal” function is adapted from longitudinal measurements of<br />
total (not weight-specific) basal metabolic rate. (Reprinted with<br />
permission from Muravchick S. Geroanesthesia: Principles for<br />
Management of the Elderly Patient. St. Louis: Mosby-Year<br />
Book; 1997.)<br />
Progressive ventricular hypertrophy develops in<br />
response to increased afterload and leads to cellular<br />
hypertrophy and deposition of fibrotic tissue. Ventricular<br />
hypertrophy increases wall stress and myocardial O 2<br />
demand, making the ventricle more prone to ischemia.<br />
Although intrinsic contractility and resting cardiac<br />
output are unaltered with aging, ventricular hypertrophy<br />
and stiffening limit the ability of the heart to adjust stroke<br />
volume. 4 Ventricular hypertrophy impairs the passive<br />
filling phase of diastole. Thus, ventricular preload is more<br />
dependent on the contribution of atrial contraction. At<br />
the same time, fatty infiltration and fibrosis of the heart<br />
increases the incidence of sinus, atrioventricular, and<br />
ventricular conduction defects. 5,6 In addition, there are<br />
decreases in myocardial responsiveness to catecholamines;<br />
maximal heart rate response is correspondingly<br />
decreased. 4,7,8 <strong>The</strong> reduction in ventricular compliance<br />
and the attenuated response to catecholamines compromise<br />
the heart’s ability to buffer decreases in circulatory<br />
volume resulting in a disposition to hypotension.<br />
Similarly, even modest increases in circulatory volume<br />
lead to congestive heart failure.<br />
From the standpoint of perioperative hemodynamic<br />
stability, age-related changes in the autonomic control<br />
of heart rate, cardiac output, peripheral vascular re -<br />
sistance, and the baroreceptor response 9–13 are as<br />
<strong>The</strong> pulmonary system also undergoes age-related<br />
changes independent of comorbid disease processes.<br />
Functionally, there are remarkable parallels with changes<br />
in the heart. With aging, the thorax becomes stiffer. 14,15<br />
This may not be evident in the sedentary patient, but<br />
reduced chest wall compliance increases the work of<br />
breathing and reduces maximal minute ventilation. 14,16<br />
Loss of thoracic skeletal muscle mass further aggravates<br />
this process. 17 Because of a decrease in elastic lung recoil,<br />
the closing volume increases such that it exceeds functional<br />
residual capacity by age 65. 18 Inspiratory and expiratory<br />
functional reserve decrease with aging, and the<br />
normal matching of ventilation and perfusion becomes<br />
impaired. 19,20 <strong>The</strong> latter process increases the alveolararterial<br />
O 2 gradient and decreases the resting PaO 2 . 18,21<br />
<strong>The</strong> respiratory response to hypoxia diminishes in the<br />
aged 22 (Figure 6-2). In addition, ciliary function and cough<br />
are reduced. 15 Finally, pharyngeal sensation and the motor<br />
function required for swallowing are diminished in the<br />
elderly. 23,24<br />
<strong>The</strong>se changes have important implications in the perioperative<br />
period. First, it is difficult to predict from a<br />
preoperative interview how an inactive, elderly patient<br />
will respond to the perioperative respiratory challenges.<br />
.<br />
VI<br />
(liter/min<br />
BTPS)<br />
60<br />
50<br />
40<br />
30<br />
20<br />
10<br />
0<br />
40 50 60 70 80 90 100<br />
PA O2 (mm Hg)<br />
Figure 6-2. Ventilatory response (V I ) to isocapnic progressive<br />
hypoxia in eight young normal men (broken line) and eight<br />
normal men aged 64–73 (solid line). Values are means ± SEM.<br />
(Reprinted with permission from Kronenberg and Drage. 22 )
68 C.J. Jankowski and D.J. Cook<br />
Anesthetics, postoperative pain, the supine position, narcotics,<br />
as well as thoracic and upper abdominal operations<br />
impair pulmonary function and further depress<br />
respiratory drive. 14,25,26 Although blood gas analysis or<br />
spirometric tests may offer some value before thoracic<br />
operations, the alterations in pulmonary function after<br />
surgery are complex and typically not predictable from<br />
preoperative pulmonary function testing. 14,20,27 Agerelated<br />
changes in pulmonary mechanics and respiratory<br />
control increase the risk of postoperative hypoxia 28,29 and<br />
perioperative aspiration in the elderly. 23,30<br />
Neurologic Changes<br />
Pulmonary and cardiac complications account for much<br />
of the morbidity and mortality in older surgical patients.<br />
However, neurologic morbidity affects many patients as<br />
well. Also, age-related degenerative changes in the central<br />
and peripheral nervous systems contribute to a variety of<br />
other morbidities. In themselves, neurologic complications<br />
have a dramatic impact on length of stay, discharge<br />
disposition, functional status, and quality of life.<br />
Independent of any comorbid process, both the central<br />
and peripheral nervous systems are affected by aging. 31<br />
<strong>The</strong>re is a loss of cortical gray matter through middle age,<br />
resulting in cerebral atrophy, 32 although how much of this<br />
is attributable to aging itself versus degenerative diseases<br />
is a subject of ongoing investigation. 33 At the level of the<br />
neuron, there is a reduction in the complexity of neuronal<br />
connections, a decrease in the synthesis of neurotransmitters,<br />
and an increase in the enzymes responsible for their<br />
postsynaptic degradation. 33–35 Although cerebral metabolism,<br />
blood flow, and autoregulation generally remain<br />
intact, 32 neuronal loss and the deficiency of neurotransmitters<br />
limit the ability of the older brain to integrate<br />
multiple neural inputs. This has been described as a loss<br />
of “fluid” intelligence. Neuronal loss and demyelinization<br />
also occur in the spinal cord. 36 Functionally, there are<br />
changes in spinal cord reflexes and reductions in proprioception.<br />
<strong>The</strong>re are also important decreases in hypoxic<br />
and hypercarbic respiratory drive. 22,37 Decreases in visual<br />
and auditory function further complicate the ability of<br />
the nervous system to acquire and process information.<br />
This combination of changes limits the ability of the older<br />
patient to understand and process information in<br />
the perioperative period and probably contributes to<br />
postoperative delirium, drug toxicity, and falls.<br />
Aging is also associated with neuronal loss in the autonomic<br />
nervous system. Both sympathetic and parasympathetic<br />
ganglia lose neurons, and there is fibrosis of<br />
peripheral sympathetic neurons. Peripheral autonomic<br />
neuronal loss is associated with impairment of cardiovascular<br />
reflexes. At the same time, decreases in adrenoceptor<br />
responsiveness result in increased adrenomedullary<br />
output and plasma catecholamine concentrations. 11,13,36<br />
Skeletal muscle innervation decreases, translating into<br />
loss of motor units, and a decrease in strength, coordination,<br />
and fine motor control. 38 Joint position and vibration<br />
sense may be compromised, and the literature suggests<br />
some diminution in the processing of painful stimuli. 39–42<br />
However, this effect, if it exists, seems to be modest at best<br />
and does not affect all nerve types equally. 42–45 Furthermore,<br />
given the enormous inter-patient variability in<br />
nervous system function and in the experience of pain,<br />
alterations in subtypes of pain perception do not translate<br />
into a decreased need for analgesia in the elderly. 44–48<br />
Renal Changes<br />
Aging is accompanied by a progressive decrease in renal<br />
blood flow and loss of renal parenchyma. 49,50 By age 80,<br />
renal blood flow is reduced by half. Renal cortical atrophy<br />
results in a 30% decrease in nephrons by the end of<br />
middle age. 49,51 Furthermore, aging is associated with sclerosis<br />
of nephrons so that some of those remaining are<br />
dysfunctional. 50,52 Together, these processes result in a<br />
progressive decrease in glomerular capillary surface area<br />
and glomerular filtration rate. 50,52–54 However, because of<br />
loss of muscle mass, aging is not associated with an<br />
increase in serum creatinine. This physiologic, and often<br />
occult, aspect of senescence has practical implications in<br />
the perioperative period.<br />
<strong>The</strong> old kidney has difficulty in maintaining circulating<br />
blood volume and sodium homeostasis in the perioperative<br />
period. 11,53–55 Sodium conservation and excretion are<br />
both impaired by aging. Additionally, fluid homeostasis is<br />
complicated by alterations in thirst mechanisms and antidiuretic<br />
hormone release that frequently result in dehydration.<br />
53–56 During the perioperative period, metabolic<br />
acidosis is also relatively common because elderly patients<br />
are less efficient in the renal excretion of acid. 57<br />
Reductions in basal renal blood flow render the elderly<br />
kidney particularly susceptible to the deleterious effects<br />
of low cardiac output, hypotension, hypovolemia, and<br />
hemorrhage. Anesthetics, surgical stress, pain, sympathetic<br />
stimulation, and renal vasoconstrictive drugs all<br />
may compound subclinical renal insufficiency. <strong>The</strong> likelihood<br />
of acute renal insufficiency is especially great following<br />
aortic and intraabdominal operations. Finally,<br />
age-related decreases in glomerular filtration rate reduce<br />
the clearance of a number of drugs given in the perioperative<br />
period.<br />
Aging, Pharmacokinetics, and<br />
Pharmacodynamics<br />
Aging is associated with multiple physiologic changes<br />
that affect drug pharmacology. 58 Decreased lean body<br />
mass and total body water and an increased proportion<br />
of body fat alter the volume of distribution of drugs, their
6. Research Priorities in <strong>Geriatric</strong> <strong>Anesthesiology</strong> 69<br />
redistribution between body compartments, and, subsequently,<br />
Table 6-1. Age and drug reactions.<br />
their rates of clearance and elimination. 59–61 <strong>The</strong> Age of patients (years) No. with reactions Rate (%)<br />
effect of changes in body composition on drug distribution<br />
and action varies depending on the lipid or aqueous 20–29 3 3.0<br />
10–19 2 3.1<br />
solubility of the drug. Water-soluble drugs have higher 30–39 7 5.7<br />
serum concentration and lower redistribution, whereas<br />
fat-soluble drugs tend to undergo wider distribution and<br />
40–49<br />
50–59<br />
12<br />
18<br />
7.5<br />
8.1<br />
60–69 27 10.7<br />
accumulation, followed by delayed release.<br />
70–79 38 21.3<br />
While age-related changes in the proportions of different<br />
plasma proteins make predictions about pharmaco-<br />
Total 118 10.2<br />
80–89 11 18.6<br />
kinetics complex in the elderly, for many drugs, decreased<br />
protein binding and increased free fraction have the Source: Modified with permission from Hurwitz. 66<br />
potential to increase the pharmacologic effect of drugs<br />
administered in the perioperative period. 58 Potential<br />
alterations in cardiac output, renal, or hepatic clearance<br />
also may change effective plasma concentrations and<br />
Pharmacokinetic changes, particularly decreased<br />
duration of action. 62 Neuronal loss and decreased levels<br />
metabolism, plus drug interactions coupled with polypharmacy,<br />
conspire to make the elderly prone to adverse<br />
of neurotransmitters in the central nervous system<br />
increase sensitivity to anesthetic agents. <strong>The</strong> changes in<br />
drug effects. 66,67 <strong>The</strong>re is an almost linear increase in<br />
pharmacokinetics that occur with aging make it difficult<br />
adverse drug reactions with age from below 10% at age<br />
to identify an independent effect of aging on pharmacodynamics.<br />
However, age-related changes in the central<br />
25 to above 20% at age 80. 68,69 <strong>The</strong> likelihood of adverse<br />
drug reactions increases with the number of drugs administered<br />
(Table 6-1). 66,67 Because many patients come to<br />
nervous system seem to increase the sensitivity to a<br />
variety of anesthetic agents (Figure 6-3). 63–65 surgery already taking multiple medications, the addition<br />
of several drugs in the perioperative period makes adverse<br />
reactions likely.<br />
Implications<br />
It is clear from a review of normal changes in physiologic<br />
function with aging that even the fit elderly patient’s<br />
ability to compensate for perioperative stress is compromised.<br />
<strong>The</strong> cardiac, pulmonary, neurologic, neuroendocrine,<br />
renal, and pharmacokinetic/pharmacodynamic<br />
changes that occur with aging make hypotension, low<br />
cardiac output, hypoxia, hypercarbia, disordered fluid<br />
regulation, and adverse drug effects more likely in the<br />
perioperative period. Additionally, because baseline<br />
cardiac, pulmonary, renal, and neurologic function are<br />
generally adequate, in the absence of acute challenges, it<br />
can be difficult to predict the effect of perioperative stress<br />
on the older patient.<br />
Preoperative Assessment of<br />
the Elderly<br />
Figure 6-3. With advancing age, anesthetic requirement for<br />
unsedated human subjects expressed as relative median effective<br />
dose (ED 50 ) or its inhalational equivalent, minimum alveolar<br />
concentration (MAC), is progressively and consistently<br />
reduced. Anesthetic requirement declines both for inhalational<br />
(C, D, H, I, S) and for intravenous (T) anesthetics. (Reprinted<br />
with permission from Muravchick S. Geroanesthesia: Principles<br />
for Management of the Elderly Patient. St. Louis: Mosby-Year<br />
Book; 1997.)<br />
<strong>The</strong> underlying health of the patient and the type and<br />
urgency of the procedure determine the extent of the<br />
preoperative assessment. <strong>The</strong> preoperative evaluation<br />
serves several purposes in most patients. Historically, it<br />
has served two primary functions: to alert the perioperative<br />
care providers to physiologic conditions that may<br />
alter perioperative management and to determine if<br />
medical intervention is indicated before proceeding. Two
70 C.J. Jankowski and D.J. Cook<br />
more contemporary uses of the preoperative assessment<br />
are to provide an index of risk, therefore contributing to<br />
decisions about the most appropriate intervention, and to<br />
provide baseline data on which the success of a surgical<br />
intervention might be judged.<br />
Physiologic studies of aging and clinical experience<br />
with this population yield three important conclusions<br />
regarding preoperative assessment. First, there is tremendous<br />
heterogeneity in the geriatric population. As<br />
Muravchick 70 notes, humans are never so similar as at<br />
birth, and never so dissimilar as in old age. Second,<br />
whereas basal function in most elderly patients is sufficient<br />
to meet daily needs, under conditions of physiologic<br />
stress, impairment in functional reserve becomes evident<br />
(see above). Third, most older surgical patients have significant<br />
comorbidities. Up to 80% of elderly surgical<br />
patients have at least one comorbid condition and one<br />
third have three or more. 71,72<br />
Despite those concerns, even extreme age is not a<br />
contraindication to surgery. Acceptable outcomes are<br />
reported for operations even in very old patients. 73–77<br />
What is less clear is how to identify which patients will<br />
do well and which will do poorly. Although this has been<br />
the subject of considerable research, no area of perioperative<br />
anesthetic care and management requires more<br />
investigation. <strong>The</strong> preoperative assessment of the patient<br />
is composed of four interrelated functions: risk stratification<br />
using population-based studies; history and physical<br />
examination of the individual patient; preoperative<br />
testing; and, in some cases, preoperative optimization.<br />
Each of these areas requires development and better<br />
definition for the geriatric surgical population.<br />
Risk Stratification<br />
Because age itself adds very little additional risk in the<br />
absence of comorbid disease, 78 most risk factor identification<br />
and risk predictive indexes have been disease oriented.<br />
79–83 <strong>The</strong>se investigations typically have studied a<br />
broad age range of patients and in multivariate analyses<br />
identified the relative contribution of age and comorbid<br />
conditions to surgical morbidity and mortality. 80,81,84–87<br />
Others have examined the predictive value of the number<br />
of comorbid diseases independent of the operative condition<br />
or evaluated the impact of American Society of<br />
Anesthesiologists status, specific surgical factors, and<br />
intraoperative management. 81,87–92<br />
<strong>The</strong> applicability of many existing risk indices to the<br />
geriatric population is unclear. Because of the prevalence<br />
of comorbid conditions, it is difficult to stratify the older<br />
patient population into smaller subsets with better-defined<br />
risk. <strong>The</strong> paucity of population studies of perioperative<br />
risk and outcomes specifically in geriatric populations can<br />
make choosing the most suitable course of care difficult.<br />
Furthermore, elderly patients have unique perioperative<br />
risks. In addition to death, myocardial infarction, or congestive<br />
heart failure, older patients are unusually prone to<br />
postoperative delirium, aspiration, urosepsis, adverse drug<br />
interactions, pressure sores, malnutrition, falls, and failure<br />
to return to ambulation or to home. <strong>The</strong>refore, preoperative<br />
assessment tools and the variables evaluated in outcomes<br />
trials require expansion for application to the<br />
geriatric surgical population. Population studies need to<br />
examine not only mortality and major cardiopulmonary<br />
morbidity, but also outcomes specific to the geriatric population.<br />
Once completed, epidemiologic studies that better<br />
stratify older patients would help define the preoperative<br />
assessment appropriate to older patients.<br />
Functional Assessments<br />
<strong>The</strong> efficacy of preoperative functional evaluation in<br />
elderly surgical patients requires investigation. This is<br />
important for several reasons. <strong>The</strong> evaluation of the<br />
“resting” patient does not indicate how the patient will<br />
respond to the cardiac, pulmonary, and metabolic<br />
demands of the perioperative period. This approach is<br />
emphasized in the American College of Cardiology/<br />
American Heart Association guidelines for preoperative<br />
cardiac evaluation in which the patient’s activity level,<br />
expressed in metabolic units, is a primary determinant of<br />
the need for subsequent evaluation. 79 However, this<br />
concept must be expanded because the geriatric population<br />
has a unique need for functional evaluation in more<br />
areas than just cardiopulmonary capacity. Because of<br />
patient heterogeneity, functional assessments may be<br />
indicated to better characterize patient differences,<br />
whether it is for activities of daily living (ADL), instrumental<br />
ADL, cognitive and emotional status, or urologic<br />
function. 93,94 Scales such as the Medical Outcomes Study<br />
Short Form-36 95 have multiple domains that are particularly<br />
useful in the geriatric population. Although these<br />
metrics have been applied successfully in orthopedic and<br />
thoracic surgery 96–98 and can have predictive value for<br />
longer-term outcomes, 99–103 multidimensional assessment<br />
and perioperative functional assessment is largely lacking<br />
in the surgical literature. 97,104,105<br />
An example of their application is provided in the<br />
study of hip fracture patients by Keene and Anderson, 101<br />
who scored patients preoperatively on the basis of physical<br />
condition, ambulation, ADL, preoperative living situation,<br />
and preexisting disabilities. <strong>The</strong> scoring system was<br />
then used to predict which patients would be discharged<br />
to nursing homes after surgery. <strong>The</strong> actual outcome after<br />
surgery was observed for 1 year and compared with the<br />
models’ predictions (Table 6-2). Although the study is<br />
small, it serves as an example for the type of research<br />
needed in geriatric surgery.<br />
In regard to preoperative functional assessment, cognitive<br />
and psychologic evaluation of the elderly surgical
6. Research Priorities in <strong>Geriatric</strong> <strong>Anesthesiology</strong> 71<br />
Table 6-2. Predicted outcomes, actual outcomes, and average scores on functional rating scale of 39 patients discharged to nursing<br />
homes who were alive 1 year after hip fracture.<br />
Nursing home placement<br />
No. of patients Residence before fracture (predicted outcome) Actual outcome 1 year after fracture Average score<br />
10 Home Temporary Temporary 72<br />
8 Home Temporary Permanent 52<br />
6 Home Permanent Permanent 51<br />
15 Nursing home Permanent Permanent 30<br />
Source: Modified with permission from Keene and Anderson. 101<br />
patient deserves special comment. Although frank delirium<br />
or dementia at admission is very evident and clearly<br />
predicts poorer acute and long-term outcomes, 106,107 subtle<br />
forms of cognitive impairment are much more common<br />
in the elderly. In the absence of screening, preoperative<br />
cognitive deficits may not be evident until the postoperative<br />
period. Subtle forms of cognitive impairment can<br />
predict subsequent delirium in hospitalized medical<br />
patients 108 and worsened cognitive outcome in cardiac,<br />
orthopedic, and gastrointestinal surgery patients. 109–113<br />
<strong>The</strong>refore, preoperative mental status examination 114,115<br />
should be considered in all geriatric surgical patients. Preoperative<br />
depression and alcohol abuse occur frequently<br />
and can affect postoperative outcomes in similar<br />
ways, 106,116–118 and, similar to mental status batteries, a<br />
variety of assessment tools for depression are available.<br />
119,120 <strong>The</strong> impact of screening for mental status,<br />
depression, and alcohol abuse on perioperative management<br />
of elderly patients is a huge potential area of<br />
investigation.<br />
Preoperative functional assessment is also important<br />
because the goal should be to return the patient to at least<br />
their preoperative activity level. <strong>The</strong> success of surgery<br />
must be questioned if the procedure is technically adequate,<br />
but the patient suffers loss of independence. Multidimensional<br />
assessment may help redefine standards for<br />
success of surgery and reset therapeutic priorities. 96,97,121–123<br />
Mangione and colleagues 97 applied this type of assessment<br />
by longitudinally measured quality of life indicators in<br />
patients undergoing hip, thoracic, and aortic surgery. A<br />
variety of metrics, including the Short Form-36, were used<br />
to measure physical, psychologic and social functions, and<br />
health perceptions preoperatively as well as 1, 6, and 12<br />
months after surgery (Figure 6-4). Major morbidity and<br />
Physical Function<br />
Social Function<br />
Deviation from population-based<br />
SF-36 sub-scale score (0–100)<br />
30<br />
20<br />
10<br />
0<br />
–10<br />
–20<br />
–30<br />
–40<br />
30<br />
20<br />
10<br />
0<br />
–10<br />
–20<br />
–30<br />
–40<br />
–50<br />
Preop 1 mo 6 mo 12 mo<br />
–50<br />
Preop 1 mo 6 mo 12 mo<br />
Time<br />
Time<br />
Role-Mental<br />
Figure 6-4. Deviation from age- and gender-adjusted population-based<br />
Short Form-36 subgroup scores by surgical procedure.<br />
Triangles indicate thoracic surgery for lung cancer; filled<br />
circles, total hip arthroplasty; open circles, abdominal aortic<br />
aneurysm; dotted line, age- and gender-adjusted populationbased<br />
value. (Modified with permission from Mangione et al. 97<br />
Published by Blackwell Publishing.)
72 C.J. Jankowski and D.J. Cook<br />
mortality aside, these types of measures address what<br />
is fundamentally most important in the management of<br />
older patients: whether the surgical intervention improves<br />
functional status and well-being. <strong>The</strong>se measures are of<br />
unique importance to the elderly because, unlike younger<br />
patients, the aged are at far greater risk for long-term<br />
functional compromise after surgery.<br />
Preoperative Testing<br />
<strong>The</strong> third area contributing to the preoperative evaluation<br />
of the elderly surgical patient is preoperative testing.<br />
Work in this area has been done for large populations of<br />
mixed age groups. However, it is not clear whether<br />
selected preoperative screening tests have a different<br />
yield in the elderly or, more likely, if specific testing is<br />
indicated for geriatric patients undergoing certain surgical<br />
procedures.<br />
In the general population, there is agreement that the<br />
bulk of routine preoperative testing is not indicated. 124–127<br />
In an evaluation of preoperative screening in 1010 individuals<br />
undergoing cholecystectomy, abnormal results<br />
were found in only 4.5% of tests. 124 In another investigation<br />
of 3131 patients aged 0–98 years who underwent<br />
38,286 tests, unexpected abnormal results were found in<br />
15% of patients. 125 However, only 3% had a change in<br />
their anesthetic or surgical plan based on those results.<br />
Unfortunately, in neither report were age-specific data<br />
provided, so it is unclear if the results can be translated<br />
to an older surgical population.<br />
Smaller studies in elderly populations suggest a higher<br />
yield for specific tests. Seymour et al. 128 examined the<br />
value of routine chest X-ray (CXR) in 223 patients older<br />
than 65 years undergoing general surgery. Of these, 40%<br />
had an abnormality regarded as clinically significant,<br />
although in only 5% did the CXR affect the course of<br />
treatment. <strong>The</strong> same authors also examined the value of<br />
the electrocardiogram (ECG) in routine screening in 222<br />
patients older than 65 years 129 and found that only 21%<br />
of patients had a normal ECG and that 53% had a major<br />
abnormality. <strong>The</strong>y reported that, although only 1% of<br />
patients had abnormalities that delayed surgery, 30%<br />
developed new ECG abnormalities postoperatively. <strong>The</strong><br />
authors concluded that the screening ECG has little or<br />
no value for predicting cardiac complications, but recommended<br />
preoperative ECG in all elderly patients to<br />
provide a basis for comparison and as a means of detecting<br />
patients for whom surgery should be deferred. 129<br />
In a small study of acutely ill elderly (mean age = 81<br />
years) medical patients (50 admissions), Sewell and colleagues<br />
130 examined the value of full blood count, sedimentation<br />
rate, urinalysis, electrolyte, liver, thyroid tests,<br />
and CXR. Six of 28 patients had abnormalities on CXR<br />
(21%), although management was only influenced in one.<br />
<strong>The</strong> most important finding in the screening battery was<br />
the frequency of unknown urinary tract infections (16/50<br />
patients, 32%). A retrospective analysis of 86 patients<br />
undergoing hip arthroplasty evaluated the impact of<br />
24 laboratory tests on postoperative course. 131 In four<br />
patients (4.6%), care was altered, three of whom had<br />
urinary tract infections. A cost-benefit analysis justified<br />
routine urinary analysis to reduce hip infections in elderly<br />
patients undergoing total hip arthroplasties.<br />
Assessment of nutritional status is useful in certain<br />
subpopulations of surgical patients. <strong>The</strong> 44-center<br />
Veterans Administration study found that serum albumin<br />
concentration was a better predictor of surgical outcomes<br />
than many other patient characteristics. 132,133 Although it<br />
can be difficult to separate the role of the disease process<br />
resulting in protein-calorie malnutrition from the effect<br />
of the malnutrition itself, 134 in elderly hospitalized nonsurgical<br />
patients, adverse outcomes can be attributed to<br />
malnutrition independent of greater acuity of illness or<br />
comorbidity. 135 Because of wide confidence limits, laboratory<br />
assessment of nutritional assessments may make<br />
their application to individual patients less useful than to<br />
populations. 134 Thus, it may prove useful to combine laboratory<br />
tests with anthropomorphic measurements, such<br />
as body mass index, limb circumferences, and weight<br />
loss. 136–139 <strong>The</strong> latter instruments are simple and inexpensive,<br />
but their clinical yield has not been determined.<br />
Nutritional assessment may have implications for preoperative<br />
management, and the timing of surgery as well as<br />
for risk stratification in certain types of surgery, but nutritional<br />
evaluation has not been adequately studied in<br />
elderly surgical patients.<br />
A recent study of preoperative testing in 18,000<br />
patients undergoing cataract procedures deserves<br />
comment. Patients were randomly assigned to undergo<br />
or not undergo routine testing (ECG, complete blood<br />
count, electrolytes, blood urea nitrogen, creatinine, and<br />
glucose). 140 <strong>The</strong> analysis was stratified by age and showed<br />
no benefit to routine testing for any group of patients.<br />
Similar conclusions were drawn in the recent study of 544<br />
elderly noncardiac surgical patients by Dzankic et al. 141<br />
From these investigations, and a body of work in<br />
younger subjects, three themes are evident. First, routine<br />
screening in a general population of elderly patients<br />
does not add significantly to information obtained in<br />
the clinical history. Second, in a general population, the<br />
positive predictive value of abnormal findings on routine<br />
screening is limited. Third, positive results on screening<br />
tests have relatively little impact on the course of patient<br />
care. Despite those observations, further research is<br />
required.<br />
Although the yield for routine screening is very low, it<br />
can be clinically valuable and cost-effective to develop<br />
guidelines for preoperative testing based on the type of<br />
surgery. Differing types of surgery impose different types<br />
and degrees of physiologic stress. As such, the results of
6. Research Priorities in <strong>Geriatric</strong> <strong>Anesthesiology</strong> 73<br />
the cataract trial will not be applicable to patients undergoing<br />
vascular surgery. Preoperative tests such as echocardiography<br />
and thallium scanning can have clinically<br />
relevant predictive value and potentially alter the course<br />
of care and outcomes if applied to specific populations at<br />
high risk for perioperative cardiac complications. 79,142,143<br />
Similarly, nutritional assessment 133,144 might be useful<br />
before abdominal or major orthopedic surgery, but would<br />
be of much lower value before carotid endarterectomy.<br />
Screening for urinary tract infection before orthopedic<br />
surgery or pulmonary function testing before thoracic<br />
surgery are other examples. Because the interaction of<br />
the patient factors and the surgical insult determines<br />
outcome, specific testing might be equally indicated in a<br />
very physiologically challenged older patient undergoing<br />
minimally stressful surgery (e.g., hernia repair), and in the<br />
mildly compromised older patient undergoing surgery<br />
that imposes severe physiologic stress (e.g., aortic aneurysm<br />
surgery). <strong>The</strong>refore, future studies in older patients<br />
will need to stratify patients as to the severity of their<br />
preexisting risk factors (low, intermediate, or high) and<br />
specifically examine their interaction with the specific<br />
surgical challenges most common in the elderly.<br />
Preoperative Optimization<br />
In addition to providing (1) an assessment of risk based<br />
on population studies, (2) functional data to help define<br />
surgical success, and (3) specific information to guide<br />
perioperative management, the fourth purpose of preoperative<br />
evaluation is to determine if medical intervention<br />
is indicated before proceeding. To some extent, this function<br />
has been lost with the foreshortening of the preoperative<br />
period, the “A.M. admit,” and a progressive<br />
elimination of preoperative testing.<br />
<strong>The</strong> research agenda for the care of elderly surgery<br />
patients must include preoperative optimization of medical<br />
status. This is an area in which relatively little work has<br />
been done. Again, in specific populations undergoing<br />
high-risk surgery, the value of preoperative optimization,<br />
particularly of cardiac and pulmonary status, can be demonstrated.<br />
Pulmonary toilet, antibiotics, and steroid therapy<br />
for some types of thoracic surgery, intervention for coronary<br />
disease before vascular surgery, and preoperative β-<br />
blockade for high-risk patients are areas in which the data<br />
are compelling. 142,143,145–149 Nevertheless, many areas have<br />
not been evaluated, particularly in the elderly. In addition<br />
to modifying cardiopulmonary risk, improving nutritional<br />
status before major elective surgery, preoperative hydration,<br />
and optimization of renal function in those with<br />
chronic or acute insufficiency could have broad impact.<br />
Preoperative management of antibiotic therapy, anticoagulation,<br />
antiplatelet therapy, and anemia are other obvious<br />
areas to examine. <strong>The</strong>re are also suggestions that preoperative<br />
education, psychologic support, and physical therapy<br />
might facilitate pain management and rehabilitation after<br />
some types of surgery, 150,151 but this area has not been<br />
adequately assessed.<br />
In today’s environment, it will be difficult to conduct<br />
studies on preoperative optimization. For example, in<br />
studies of preoperative nutritional optimization, it would<br />
be difficult to justify randomizing a clearly malnourished<br />
patient to a control group proceeding directly to the<br />
operating room without nutritional therapy when surgery<br />
could be delayed. Conversely, intervention and delay will<br />
add costs. However, limited studies in orthopedic and<br />
cardiac surgical patients suggest that appropriately<br />
applied preoperative care can be cost effective in that it<br />
shortens hospital stays and improves functional status<br />
after discharge. 151,152 Preoperative optimization will not<br />
be practical or necessary in many instances. However,<br />
much geriatric surgery is elective, so these studies can be<br />
conducted and, if positive, could influence the care and<br />
outcome of many patients.<br />
Preoperative Research Agenda Items<br />
• <strong>The</strong>re is a need for epidemiologic studies describing<br />
outcomes, relatively unique to older surgical patients,<br />
for the most common types of surgery. <strong>The</strong> frequency<br />
is probably underestimated by retrospective analysis in<br />
much of the literature. With few exceptions, future<br />
studies will need to be prospective, cross-sectional<br />
studies. In the second phase, patient and surgeryspecific<br />
risk factors for geriatric complications would<br />
be identified by multivariate analysis. <strong>The</strong>se investigations<br />
would stratify surgical risk as low, intermediate,<br />
or high depending on type of surgery.<br />
• <strong>The</strong> most pressing need for preoperative assessment is<br />
to develop better tools to predict which patients will<br />
do well and which will do poorly. <strong>The</strong> positive predictive<br />
value of these instruments would be first determined<br />
in prospective nonrandomized or prospective<br />
cohort trials. After that, prospective randomized trials<br />
would determine whether the application of these<br />
metrics could improve outcomes either by perioperative<br />
intervention or altering the surgical intervention<br />
based on the patient risk profile.<br />
• <strong>The</strong> contribution of simple preoperative functional<br />
studies to surgical decision making has largely not been<br />
investigated. Prospective cohort or case-control studies<br />
would be required to determine if assessment of<br />
preoperative functional status changes surgical decision<br />
making (timing or type of surgery) or pre- or<br />
postoperative care strategies.<br />
• <strong>The</strong> impact of screening for cognitive impairment,<br />
depression, and alcohol abuse on perioperative management<br />
of elderly patients is a huge potential area of<br />
investigation. Existing literature provides an incidence<br />
for these preexisting conditions, but an incomplete
74 C.J. Jankowski and D.J. Cook<br />
understanding of risk factors. Prospective crosssectional<br />
or cohort studies will better identify association<br />
between these patient preexisting conditions and<br />
adverse geriatric outcomes by multivariate analysis.<br />
Subsequently, prospective randomized trials could<br />
determine the effect of pre- or postoperative interventions<br />
on adverse outcomes related to these risk<br />
factors.<br />
• Assessment of preoperative nutritional status, hydration,<br />
and renal function may have implications for preoperative<br />
management and the timing of surgery as<br />
well as for risk stratification but this has not been<br />
adequately studied in the elderly. First, the positive or<br />
negative predictive value of instruments to evaluate<br />
nutrition and hydration would be tested in prospective<br />
studies. Second, prospective cohort or case-control<br />
studies would be used to determine if application of<br />
these metrics would change preoperative care, timing,<br />
or choice of surgery perioperative management and<br />
reduce complications.<br />
Intraoperative Management<br />
By its nature, anesthetic care is episodic, so most of the<br />
criteria to judge the success of anesthetic interventions<br />
are short term. Studies of anesthetic drugs and techniques<br />
typically address hemodynamic stability, time to awakening,<br />
extubation time, postoperative nausea and vomiting,<br />
recovery room time, and length of stay. Awareness of the<br />
physiologic and pharmacokinetic changes in the elderly<br />
has led investigators to examine the effects of a host of<br />
anesthetic agents and adjuncts in this population. <strong>The</strong><br />
effects of intravenous induction agents, narcotics, benzodiazepines,<br />
volatile anesthetics, neuromuscular blocking<br />
agents, and various types of local anesthetics all have<br />
been evaluated in the elderly. Studies have included use<br />
of these agents for inpatient surgical procedures, outpatient<br />
procedures, premedication, sedation, and their<br />
administration by bolus and infusion techniques. Because<br />
there is a theoretical advantage to shortening recovery<br />
time in patients for whom awakening, ambulation, and<br />
discharge might otherwise be delayed (e.g., the elderly),<br />
much of the more recent work in the elderly has been<br />
devoted to the ultra–short-acting agents.<br />
Some of these studies have identified age-related alterations<br />
in the pharmacokinetics, induction, awakening, or<br />
recovery room stay. However, perspective is needed.<br />
Although a drug may shorten extubation time by 10<br />
minutes, recovery room time by 45 minutes, or total hospitalization<br />
in an outpatient procedure by 90 minutes, the<br />
clinical impact of these changes on patient outcomes is<br />
probably minimal. <strong>The</strong>re is a role for this type of research<br />
in geriatric anesthesia, but in an era of limited time and<br />
research dollars, efforts should probably be directed<br />
elsewhere.<br />
In addition to the numerous studies on the pharmacology<br />
and short-term recovery in aged surgical patients,<br />
a second major area of research effort has been to<br />
compare the risks and benefits of regional versus general<br />
anesthesia.<br />
<strong>Regional</strong> Versus General <strong>Anesthesia</strong><br />
Because most general anesthetic agents depress cardiovascular<br />
and pulmonary function, as well as alter consciousness,<br />
regional anesthesia has been advocated in<br />
geriatric patients. Many of the most common procedures<br />
in the elderly can be performed with regional techniques,<br />
and many investigations have been conducted. Taken<br />
as a whole, these studies have broad implications for<br />
determining directions for research.<br />
Anesthesiologists taking care of elderly patients undergoing<br />
orthopedic procedures have been the de facto<br />
leaders in research in geriatric anesthesia. <strong>The</strong> studies in<br />
this area have examined intraoperative cardiovascular<br />
stability in the elderly, cardiac, pulmonary and thrombotic<br />
complications, pain control, and cognitive outcomes.<br />
This subject was reviewed recently by Roy. 153<br />
A few early studies reported that regional anesthesia<br />
for hip surgery was associated with better outcomes. 154,155<br />
Reduced mortality, higher postoperative PaO 2 , and fewer<br />
mental changes have been reported in patients receiving<br />
regional anesthesia. 154,155 However, these studies were<br />
very small and their assessment of cognitive function<br />
would not meet current standards for reliability or<br />
validity. 156<br />
Subsequent investigations in elderly patients undergoing<br />
hip surgery found that intraoperative hypotension<br />
was more common with regional anesthesia, and although<br />
the incidence of deep vein thrombosis (DVT) and blood<br />
loss were typically lower with regional techniques, no<br />
difference in major morbidity or mortality could be<br />
identified. 84,157–162 Because most of these studies were<br />
underpowered for rare events, meta-analysis has been<br />
used to help address statistical limitations.<br />
<strong>The</strong> benefit of regional or general anesthesia was<br />
addressed in a 1992 meta-analysis. 163 Sorenson and Pace<br />
examined 13 randomized controlled trials conducted<br />
between 1966 and 1991 that reported follow-up to at least<br />
1 month. Meta-analysis endpoints were mortality, DVT,<br />
and blood loss. Other complications or adverse events<br />
were not evaluated because of inconsistencies in definitions<br />
or “the absence of systematic and unbiased application<br />
of diagnostic tests to record these events.” Sorenson<br />
and Pace were unable to identify any statistically significant<br />
difference in mortality or blood loss by anesthetic<br />
technique, although there was a clearly reduced incidence<br />
of DVT in regional anesthesia groups. Much of the data
6. Research Priorities in <strong>Geriatric</strong> <strong>Anesthesiology</strong> 75<br />
Outcome<br />
T/P Incidence (regional) Incidence (general) Peto OR (95% CI) Peto OR (95% CI)<br />
Mortality—1 month<br />
7/1578<br />
49/766 (6.4%)<br />
76/812 (9.4%)<br />
0.66 (0.47–0.96)<br />
Mortality—3 months<br />
6/1491<br />
88/726 (12.1%)<br />
98/765 (12.8%)<br />
0.91 (0.67–1.24)<br />
Mortality—6 months<br />
3/1264<br />
103/613 (16.8%)<br />
105/651 (16.1%)<br />
1.05 (0.78–1.41)<br />
Mortality—12 months<br />
2/726<br />
80/354 (22.5%)<br />
78/372 (21.0%)<br />
1.10 (0.77–1.57)<br />
Operative hypotension<br />
7/873<br />
146/426 (34.3%)<br />
116/447 (26.0%)<br />
1.51 (1.12–2.02)+<br />
1.21 (0.65–2.25)*<br />
Patients receiving transfusion<br />
3/228<br />
63/108 (58.3%)<br />
68/120 (56.7%)<br />
1.02 (0.58–1.80)<br />
Postoperative hypoxia<br />
1/57<br />
10/28 (35.7%)<br />
14/29 (48.3%)<br />
0.60 (0.21–1.71)<br />
Pneumonia<br />
8/1096<br />
27/529 (5.1%)<br />
31/567 (5.5%)<br />
0.92 (0.53–1.59)<br />
Myocardial infarction<br />
4/888<br />
4/431 (0.9%)<br />
8/457 (1.8%)<br />
0.51 (0.16–1.63)<br />
Cerebrovascular accident<br />
7/1085<br />
10/529 (1.9%)<br />
6/556 (1.1%)<br />
1.72 (0.64–4.63)<br />
Congestive cardiac failure<br />
6/902<br />
11/439 (2.5%)<br />
12/463 (2.6%)<br />
0.97 (0.42–2.23)<br />
Renal failure<br />
4/796<br />
2/382 (0.5%)<br />
3/414 (0.7%)<br />
0.77 (0.13–4.50)<br />
Acute confusional state<br />
3/167<br />
10/83 (12.0%)<br />
19/84 (22.6%)<br />
0.47 (0.21–1.06)<br />
Urine retention<br />
2/97<br />
10/48 (20.8%)<br />
10/49 (20.4%)<br />
1.02 (0.39–2.71)<br />
Nausea and vomiting<br />
2/95<br />
2/46 (4.3%)<br />
3/49 (6.1%)<br />
0.69 (0.12–4.13)<br />
Deep vein thrombosis<br />
4/259<br />
39/129 (30.2%)<br />
61/130 (46.9%)<br />
0.41 (0.23–0.72)+<br />
Pulmonary embolism<br />
9/1184<br />
8/575 (1.4%)<br />
10/609 (1.6%)<br />
0.84 (0.33–2.13)<br />
0.1 0.2 0 5 10<br />
Figure 6-5. Comparison of outcome between regional and<br />
general anesthesia for dichotomous variables. All results were<br />
derived using fixed effects analysis except those marked with<br />
an asterisk, which were derived using random effects analysis.<br />
Statistically significant results are indicated by a plus sign.<br />
Results to the left of the vertical line indicate an advantage for<br />
regional anesthesia over general anesthesia. Results show the<br />
incidence of each outcome measure. T = number of trials, P =<br />
number of patients, OR = odds ratio, CI = confidence intervals.<br />
(Reprinted with permission from Urwin et al. 164 )<br />
in the study by Sorenson and Pace was recently reanalyzed<br />
in another meta-analysis with the addition of other<br />
trials. 164 Similar to Sorenson and Pace, the analysis by<br />
Urwin et al. 164 identified reduced DVT and 1-month mortality<br />
in 2162 hip fracture patients receiving regional anesthesia,<br />
although no other outcome measure reached<br />
statistical significance (Figure 6-5). <strong>The</strong> reduction in mortality<br />
was not evident at 3, 6, or 12 months when those<br />
data were available. Subsequent large single-center observational<br />
studies involving 741, 165 1333, 166 and 9425 167<br />
patients have also not identified meaningful differences in<br />
cardiopulmonary morbidity or mortality between regional<br />
and general anesthesia in hip surgery patients.<br />
Another meta-analysis was conducted by Rodgers et<br />
al. 168 Those authors examined the effects of regional anesthesia<br />
in 141 randomized trials including 9559 patients.<br />
As in the report by Urwin et al., they describe reductions<br />
in 30-day mortality and DVT in the regional group, with<br />
the effect on mortality not evident beyond 1 month. <strong>The</strong>y<br />
also describe reductions in pulmonary embolism, transfusion,<br />
respiratory depression, myocardial infarction, and<br />
renal failure. Although the results are enticing, the reporting<br />
of many outcomes was incomplete across studies so<br />
the analysis was based on smaller subsets of patients.<br />
Additionally, studies were not rated for quality, and data<br />
were included in the meta-analysis that were not reported<br />
in the published trials. Studies for general, obstetric and<br />
gynecologic, urologic, orthopedic, and “other” surgeries<br />
were combined, and no information about age is provided.<br />
Finally, it is difficult to make practice recommendations<br />
based on the results of this meta-analysis because<br />
all of the following treatment modalities were combined<br />
into the regional anesthesia group: (1) those receiving<br />
spinal anesthesia alone, (2) epidural anesthesia alone, (3)
76 C.J. Jankowski and D.J. Cook<br />
general anesthesia followed by postoperative regional<br />
anesthesia, (4) general anesthesia combined with intraoperative<br />
spinal anesthesia, and (5) general anesthesia<br />
combined with intraoperative epidural anesthesia. Additionally,<br />
in 22 studies in which general anesthesia was<br />
combined with regional anesthesia, the general anesthetic<br />
in the combined regional/general anesthesia group differed<br />
from that in the general anesthesia alone group.<br />
Thus, it is difficult to determine if the effects described in<br />
the meta-analysis are real and, if so, their origin or to<br />
which patients they would apply.<br />
In addition to the more typical outcome measures,<br />
several of the studies in orthopedic surgery patients have<br />
examined the effect of anesthetic technique on cognitive<br />
or functional outcome, often following patients for 3<br />
months or longer. Although each of the prospective<br />
studies is small, only the study by Hole et al. 155 has been<br />
able to identify any difference in cognitive outcome in<br />
elderly patients undergoing regional versus general anesthesia<br />
for hip or knee surgery. <strong>The</strong> bulk of investigations<br />
could identify no difference. 116,156,169–171<br />
In a well-designed, randomized prospective, doubleblinded<br />
study, Norris and colleagues 172 examined the<br />
effect of general versus combined general/epidural anesthesia<br />
and intravenous patient-controlled opiate versus<br />
epidural analgesia in patients undergoing abdominal<br />
aortic aneurysm repair. <strong>The</strong>re were no differences in<br />
length of stay, mortality, major morbidity, and pain<br />
scores.<br />
Although not all studies are in agreement, 173,174 similar<br />
conclusions must be drawn for patients undergoing<br />
regional or general anesthesia for transurethral prostatectomy,<br />
and peripheral vascular surgery. 171,175–178 In<br />
carotid surgery, there is a suggestion of a better outcome<br />
with regional techniques; however, most investigations<br />
are retrospective or nonrandomized, so the effect of<br />
patient selection cannot be eliminated. 179–182 Additionally,<br />
in the multicenter North American Symptomatic Carotid<br />
Endarterectomy Trial, an independent effect of anesthetic<br />
technique (or intraoperative monitoring) on carotid<br />
surgical outcome could not be found. 183<br />
<strong>The</strong> difficulty in identifying clear and meaningful difference<br />
between regional and general anesthesia has tremendous<br />
implications for the conduct of research in<br />
geriatric anesthesia. Probably the most substantive difference<br />
in the choice of anesthetic is whether the patient<br />
undergoes a regional or a general anesthetic. <strong>The</strong> pharmacologic<br />
difference with that choice is far greater than<br />
the difference between different induction agents, narcotics,<br />
local anesthetics or muscle relaxants, or different<br />
doses of those medications. If little or no difference in<br />
outcome can be identified for elderly patients undergoing<br />
major procedures with general or regional anesthesia,<br />
then the yield for similar outcome studies on differing<br />
anesthetic agents is likely to be low.<br />
Physiologic Management<br />
In addition to establishing a surgical plane of anesthesia,<br />
the anesthesiologist maintains physiologic stability.<br />
Although numerous studies have examined the relationship<br />
between intraoperative physiologic management<br />
and outcome, outside of relatively rare catastrophic<br />
events, such as loss of the airway or uncontrolled hemorrhage,<br />
it seems that physiologic management has a modulatory<br />
rather than a primary role in outcomes. <strong>The</strong> best<br />
example is in cardiac surgery, for which the acute changes<br />
in blood pressure, hematocrit, and temperature typically<br />
exceed those seen with any other type of surgery. Additionally,<br />
most of the patients are older. Despite that, it has<br />
been difficult to demonstrate a direct relationship<br />
between physiologic management and outcome. 184–186<br />
Rather, the primary determinants of outcome are<br />
technical issues during surgery and the comorbidities<br />
that the patent brings to the operating room. 187,188<br />
Although there is a role for specific studies related to<br />
physiologic or pharmacologic management in the elderly,<br />
those investigations are likely to have a smaller yield than<br />
risk stratification based on population studies and subsequent<br />
tailoring of the surgical procedure to the patient<br />
based on the preoperative assessment.<br />
<strong>The</strong>se conclusions are not an indictment on anesthetic<br />
practice or the role of the anesthesiologist in the operating<br />
room. Just the opposite is true. Over the past three<br />
decades, anesthesiology has made tremendous strides in<br />
patient safety, monitoring, drugs, and education that<br />
have made the intraoperative period extremely safe.<br />
Those advances have, and will continue, to expand what<br />
is possible surgically. At the same time, it is because<br />
the advances in intraoperative care have been so great<br />
that the greatest needs for research lie in the preoperative<br />
assessment and the postoperative management of<br />
patients.<br />
<strong>The</strong>re are also broad areas related to intraoperative<br />
management (rather than the specifics of anesthetic<br />
choice) in which research in the elderly would be productive.<br />
It is clear that anesthetics and alterations in autonomic<br />
function make it more difficult for older patients<br />
to maintain their body temperature and that postoperative<br />
hypothermia increases risk of adverse outcomes. 189–193<br />
Thus, studies of temperature control in older patients<br />
could be expanded.<br />
Perioperative β-adrenergic blockade reduces mortality<br />
and cardiac morbidity in high-risk patients. 194,195 Intraoperative<br />
β-blockade, per se, may also improve cardiac outcomes<br />
as well as improve early anesthetic recovery<br />
and decrease postoperative analgesic requirements. 147 In<br />
addition, perioperative clonidine may reduce cardiac<br />
morbidity and mortality. 196 Thus, the appropriate place<br />
for prophylactic β-blockade and central sympatholysis in<br />
elderly surgical patients needs to be examined. Similarly,
6. Research Priorities in <strong>Geriatric</strong> <strong>Anesthesiology</strong> 77<br />
studies need to address the appropriate roles for antiplatelet<br />
agents and H 2 -blockers.<br />
Recent data suggest that tight glucose control may<br />
improve perioperative outcomes. In a randomized, prospective<br />
trial involving critically ill, primarily surgical<br />
patients, van den Berghe et al. 197 found that using an<br />
insulin infusion to maintain blood glucose 80 and 110 mg/<br />
dL reduced intensive care unit (ICU) and in-hospital<br />
mortality as well as a variety of morbidities compared<br />
with treating only for blood glucose in excess of 215 mg/<br />
dL and a goal of 180–200 mg/dL. Further study is needed<br />
to determine applicability of this therapy in the elderly<br />
surgical patient and whether there is benefit to tight<br />
intraoperative glucose control.<br />
Given that the immune response may be attenuated in<br />
the elderly and that infectious complications are very<br />
common, the appropriate dosage and scheduling for perioperative<br />
antibiotics may be a useful area of research.<br />
Furthermore, elderly patients receive most of the blood<br />
given in the perioperative period, so investigation into<br />
the immunosuppressive effects of homologous blood<br />
transfusion would be instructive. Older patients are also<br />
at increased risk for musculoskeletal and nerve injury as<br />
well as thrombotic complications. <strong>The</strong>refore, documenting<br />
the relationship among patient positioning, nerve and<br />
skin injury, and thrombotic complications is indicated.<br />
Similarly, the timing of the preoperative fast, and its<br />
relationship to hypovolemia, and aspiration risk in the<br />
elderly would be an area of research with a large potential<br />
impact on practice and patient satisfaction.<br />
In perspective, the lack of an independent effect of<br />
anesthetic choice or physiologic management on outcome<br />
is not surprising. Very large studies of perioperative morbidity<br />
and mortality indicate that the anesthetic episode<br />
per se seems to have little or no impact on 30-day outcomes<br />
apart from rare, catastrophic events. 88,91,198 And,<br />
although certain pathophysiologic processes may be initiated<br />
during the intraoperative period, with few exceptions,<br />
major morbidity and mortality in the operating<br />
room is rare.<br />
Intraoperative Research Agenda Items<br />
• Perioperative management of β-blockade, central sympatholysis,<br />
antiplatelet therapy, anticoagulation, and<br />
anemia are areas to examine in elderly patients. First,<br />
cross-sectional or retrospective case-control studies<br />
could be used to identify the incidence of adverse<br />
cardiac or thrombotic-embolic complications in elderly<br />
patients undergoing surgery with and without preoperative<br />
β-blockade, central sympatholysis, antithrombotic<br />
or antiplatelet therapy, or a hematocrit above a<br />
target value. <strong>The</strong>se studies should be in surgeries identified<br />
as intermediate or high risk for related complications.<br />
Subsequently, prospective cohort, case-control or<br />
randomized studies would be used to determine if<br />
pre- or intraoperative therapies would reduce related<br />
complications in the elderly.<br />
• A similar approach as above should be used to examine<br />
perioperative glucose control.<br />
• <strong>The</strong> appropriate dosage and scheduling for perioperative<br />
antibiotics in prevention of perioperative infection<br />
in the elderly are important areas of research. As for<br />
β-blockade or antithrombotic strategies, initial studies<br />
would use retrospective or cross-sectional studies to<br />
identify any relationship between the use or timing of<br />
perioperative antibiotic therapy and postoperative<br />
pneumonia or wound infection. Differences, if any,<br />
between younger and older patients undergoing the<br />
same type of surgery could also be compared. Subsequently,<br />
prospective, nonrandomized studies would be<br />
used to determine if preoperative or postoperative<br />
antibiotic therapies can reduce infectious-related<br />
complications.<br />
• Because elderly patients receive most blood given<br />
in the perioperative period, the immunosuppressive<br />
effects of homologous blood transfusion deserves<br />
further investigation in this population. Multicenter<br />
studies of a prospective case-control or prospective<br />
cohort design would examine the incidence of perioperative<br />
infection and immunosuppression in elderly<br />
patients receiving or not receiving blood in the perioperative<br />
period. Multivariate analysis would be required<br />
to separate the effect of homologous blood transfusion<br />
from the comorbid conditions, making transfusion<br />
more likely. If a significant independent effect of<br />
blood transfusion was identified, subsequent analysis<br />
would need to statistically compare the transfusionassociated<br />
risk with that of not receiving transfusion.<br />
Alternate strategies, such as delaying surgery or erythropoietin<br />
therapy, would need to be compared with<br />
blood transfusion in case-cohort or prospective, nonrandomized<br />
trials because a randomized trial could not<br />
be justified.<br />
Appropriate preoperative fasting, its relationship to<br />
hypovolemia, and aspiration risk in the elderly would be<br />
a practical area of research. In prospective cohort or<br />
case-control studies, the incidence of perioperative<br />
hypotension, aspiration, and renal insufficiency should be<br />
compared in patients undergoing standard fasting orders<br />
before surgery with elderly patients who would be allowed<br />
clear liquids closer to the time of surgery. This study<br />
would need to be conducted in patients undergoing<br />
specific types of procedures:<br />
• where liberalization of fluid intake is not contraindicated<br />
for surgical reasons,<br />
• in patients undergoing procedures in which they are at<br />
greater risk for developing hypovolemia (bowel prep),<br />
and
78 C.J. Jankowski and D.J. Cook<br />
• in instances in which preoperative hypovolemia<br />
may contribute to complications (angiographic<br />
procedures).<br />
Postoperative Management<br />
Most surgical morbidity and mortality occur in the postoperative<br />
period. Pedersen et al. 84 examined perioperative<br />
mortality in 7306 adult patients undergoing lowerrisk<br />
surgery (no cardiac, thoracic, or neurosurgical<br />
procedures) and found that mortality during anesthesia<br />
was 0.05% (1 : 1800). In the first 24 hours, the mortality<br />
was twice as high, 0.1%, and increased fivefold over<br />
the next 6 days to 0.56%. 84 Morbidity, including myocardial<br />
ischemia and infarction, stroke, renal insufficiency,<br />
pneumonia, and delirium, is also most common<br />
postoperatively. 183,199,200<br />
Postoperative Respiratory Insufficiency<br />
Respiratory morbidity is very common after noncardiac<br />
surgery. In the 84,000-patient Veterans Administration<br />
study (97% male, mean age of 60), 17% of patients<br />
experienced complications with pneumonia in 3.6%, ventilatory<br />
failure in 3.2%, and unplanned intubation in<br />
2.4%. 87 In a study conducted by Seymour and Vaz 201 of 288<br />
general surgical patients over age 65, 17% of patients had<br />
atelectasis, 12% acute bronchitis, and 10% developed<br />
pneumonia.<br />
Although most elderly patients do not require invasive<br />
monitoring postoperatively, the appropriate use of pulse<br />
oximetry, ventilation monitoring, and O 2 therapy requires<br />
study. 202,203 As highlighted previously, elderly patients<br />
have an increased A-a gradient, reduced respiratory<br />
muscle strength, and decreased hypoxic and hypercarbic<br />
drives at baseline. 14,20,27 Additionally, aging is associated<br />
with a progressive loss of airway reflexes. 18 And apnea<br />
and periodic breathing following administration of narcotics<br />
are more common in older patients. 25,204 Postoperative<br />
pain, atelectasis, and fluid shifts further increase the<br />
likelihood of respiratory complications, as do shivering<br />
and reductions in cardiac output and hemoglobin concentration<br />
191 <strong>The</strong> supine position during recovery increases<br />
the transpulmonary shunt and makes hypoxia more<br />
likely. 18 Finally, orthopedic and upper abdominal surgeries<br />
common in the elderly have an independent effect in<br />
increasing postoperative hypoxia and respiratory complications.<br />
26,201,205 For these reasons, hypoxia may occur in<br />
20%–60% of elderly surgical patients. 28,29<br />
Despite the frequency of postoperative hypoxia and<br />
hypercarbia in the elderly, clear guidelines for O 2 therapy,<br />
pulse oximetry, and capnography in older patients have<br />
not been developed. This issue is of pressing importance<br />
as “day surgery” becomes more common and continued<br />
efforts are made to abbreviate the time to discharge.<br />
Further, more and more patients, most of them elderly,<br />
undergo conscious sedation outside the operating room<br />
environment. Although the study by Bailey and colleagues<br />
206 is more than 10 years old, its implications are<br />
unchanged. In a study of hypoxemia and apnea after<br />
sedation with fentanyl and midazolam, the authors<br />
describe deaths associated with the use of these drugs. Of<br />
86 reported US deaths, “all but three . . . occurred outside<br />
the operating room . . . where patients are typically unattended<br />
by anesthesia personnel.” Determination of the<br />
requirements for O 2 therapy, pulse oximetry, and capnography<br />
in elderly patients undergoing inpatient and outpatient<br />
surgery, as well as procedures with conscious<br />
sedation, are indicated.<br />
<strong>The</strong> risk of postoperative aspiration in the elderly also<br />
requires attention. Because of alterations in pharyngeal<br />
function, diminished cough, and an increased incidence<br />
of gastroesophageal reflux, elderly patients are at<br />
increased risk of aspiration. 23,24 This risk is accentuated<br />
by the effect of anesthesia, sedatives, and narcotics as well<br />
as by endotracheal intubation, nasogastric tube placement,<br />
and upper abdominal or neck surgery. 30,207,208<br />
Although the incidence of aspiration in the operative<br />
period is low and is uncommonly associated with<br />
clinically important pneumonitis or pneumonia, 209 the<br />
risk for aspiration extends well beyond the acute<br />
operative period.<br />
It is likely that instrumentation of the pharynx, whether<br />
from an endotracheal tube, 30 nasogastric tube, 208 or a<br />
transesophageal echocardiography probe, 207 alters sensation,<br />
motor function, and the protective reflexes preventing<br />
aspiration. For patients with prolonged endotracheal<br />
intubation (>24 hours), this effect is persistent for at least<br />
48 hours after extubation. 30 Nasogastric tubes may also<br />
contribute to aspiration by increasing the incompetence<br />
of the gastroesophageal junction. Although pharyngeal<br />
dysfunction and aspiration may be related to a greater<br />
acuity of illness, pharyngeal trespass itself has independent<br />
effects.<br />
Given perioperative risk factors, the frequency of aspiration,<br />
and the incidence of postoperative respiratory<br />
morbidity, insufficient research has been directed to these<br />
issues in elderly surgical patients. Pharmacologic interventions<br />
to reduce gastric volume or increase pH have<br />
received attention in the anesthesia literature, but the<br />
investigation by Warner et al. 209 of aspiration occurring<br />
within 2 hours of surgery implies that research on aspiration<br />
and postoperative pneumonia must look beyond the<br />
immediate operative period. 210 More important research<br />
will focus on establishing appropriate use of nasogastric<br />
tubes, restoration of pharyngeal and tracheal reflexes and<br />
gastrointestinal motility, and advancement of feeding<br />
following surgery in the elderly. General studies as well<br />
as surgery-specific studies are indicated.
6. Research Priorities in <strong>Geriatric</strong> <strong>Anesthesiology</strong> 79<br />
Acute Pain Management<br />
<strong>The</strong> same questions that dominate research in pain management<br />
in the general population apply to the elderly.<br />
However, in many ways, the questions are more pressing<br />
in the elderly because they might receive the most potential<br />
harm as well as the greatest potential benefit from<br />
the treatment of postoperative pain. Because of ischemic<br />
heart disease, diminished pulmonary capacity, altered<br />
drug clearance, or increased drug sensitivity, the elderly<br />
patient is probably more vulnerable to the physiologic<br />
consequences of inadequate analgesia as well as the<br />
side effects related to analgesic use. Additionally, there is<br />
evidence in the literature indicating that in certain circumstances<br />
pain in the elderly may be less adequately<br />
treated. 48<br />
Pain and Adverse Outcomes<br />
<strong>The</strong> perioperative period results in stress and inflammatory<br />
responses that peak postoperatively when cardiopulmonary<br />
and neurologic complications occur. <strong>The</strong>refore,<br />
efforts have been made to link the adequacy of analgesia<br />
with the magnitude of the stress response. In particular,<br />
it has been proposed that inadequate postoperative analgesia<br />
may be associated with myocardial ischemia and<br />
pulmonary failure. Researchers have examined the effect<br />
of the intraoperative anesthetic 211–214 and postoperative<br />
epidural analgesia on plasma levels of cortisol, epinephrine,<br />
norepinephrine, leucocyte counts, and acute phase<br />
proteins and tried to relate these to cardiopulmonary<br />
outcomes. 173,211,215–219 Both negative and positive conclusions<br />
have been reached.<br />
When this subject was reviewed by Liu et al., 220 they<br />
concluded that intensive analgesia using regional techniques<br />
had a limited impact on cardiopulmonary outcomes<br />
or the stress response in a general population of<br />
surgical patients. <strong>The</strong>y also concluded that pain and the<br />
stress response were not directly coupled because the<br />
neuroendocrine response was still demonstrated (al -<br />
though blunted) in the presence of intense surgical analgesia<br />
with local anesthetics or opioids. 220 However, studies<br />
in the highest-risk groups suggest a possible improvement<br />
in outcome with intense analgesia using regional<br />
techniques. 173,221 Intensive pain management strategies<br />
may be indicated in high-risk elderly patients or in lowrisk<br />
elderly patients undergoing high-risk surgery. Defining<br />
the circumstances under which epidural analgesia or<br />
any other pain management strategy can improve outcomes<br />
is an important area for future research.<br />
In addition to the stress response typically associated<br />
with the sympathetic-adrenal axis, most types of surgery<br />
initiate a significant catabolic state. Although an inhibitory<br />
effect of analgesia on protein wasting has been<br />
suggested, 222–224 a more pressing area for research is to<br />
understand postsurgical catabolism in the elderly. <strong>The</strong><br />
relationship between preoperative nutritional status and<br />
postoperative catabolism must be better understood.<br />
Experience with some critically ill patients suggests that<br />
catabolism may become dissociated from the initial surgical<br />
stress. Because elderly patients have decreased nutritional<br />
and metabolic reserve, they are most challenged<br />
by the postoperative catabolic state. Basic investigation<br />
into postoperative catabolism in the elderly is fundamental<br />
as are investigations into interventions that might<br />
attenuate catabolism or facilitate the transition back to<br />
an anabolism.<br />
Although the adequacy of postoperative analgesia<br />
does not seem to be an independent determinant of outcomes<br />
in the general population of surgical patients, a<br />
variety of other issues related to postoperative analgesia<br />
require attention. <strong>The</strong> relative benefit of patient-controlled<br />
analgesia (PCA) 225 versus a PRN or scheduled<br />
analgesic administration is of special importance in the<br />
elderly surgical patient. Because of the physiologic and<br />
psychologic heterogeneity in the geriatric population, it<br />
is unlikely that fixed formulae for age-appropriate drug<br />
dosing can be identified. Thus, administration of narcotics<br />
on a set schedule in the elderly is fraught with the potential<br />
for both over- and under-dosing. <strong>The</strong>se considerations<br />
potentially make PCA analgesia an ideal choice. Nevertheless,<br />
the issue is complicated. <strong>The</strong> side-effect profile for<br />
PCA analgesics in the elderly has not been established.<br />
226,227 It has also been suggested that many elderly<br />
patients may struggle with the technology. Similarly, the<br />
application of PCA for patients with altered mental status<br />
is problematic. Outcomes with PCA in the elderly must<br />
be compared with fixed and PRN dosing techniques as<br />
well as with postoperative pain control by regional<br />
blockade.<br />
<strong>The</strong> same is true regarding route of administration for<br />
analgesic agents. Is there a clear advantage or disadvantage<br />
to the use of the intravenous, epidural, or intrathecal<br />
routes for analgesic administration in the elderly? <strong>The</strong><br />
elderly are unusually susceptible to drug interactions and<br />
have an increased incidence of respiratory depression,<br />
urinary retention, ileus, constipation, and postoperative<br />
falls. <strong>The</strong>se are influenced by choices in postoperative<br />
analgesia and may differ by route of administration. 226–229<br />
As such, investigations into analgesic strategies for<br />
elderly surgical patients will need to determine not only<br />
quality of analgesia, but also a comprehensive examination<br />
of risks and benefits specific to that population.<br />
Additionally, because narcotics are associated with frequent<br />
side effects in the elderly, the use of analgesic<br />
adjuncts in postoperative pain management requires<br />
further investigation. Drugs such as ketorolac, clonidine,<br />
dexmedetomidine, and cyclooxygenase-2 inhibitors have<br />
the potential to achieve adequate analgesia with lower<br />
doses of opioids, potentially reducing side effects. 230–234
80 C.J. Jankowski and D.J. Cook<br />
A final reason why studies of acute pain management<br />
in the elderly are required is that acute pain management<br />
may bear on rehabilitation and subsequently on functional<br />
status on discharge. 235 This has been shown with<br />
analgesic programs for continuous passive motion<br />
machines used after knee replacement. 235–237 Research is<br />
required after other types of surgical procedures to determine<br />
whether facilitation of rehabilitation by acute pain<br />
management can improve other functional outcomes.<br />
Another opportunity for research in the postoperative<br />
care of hospitalized patients is related to polypharmacy<br />
and adverse drug events in the elderly. <strong>The</strong>re is a tendency<br />
for elderly patients to accumulate drug prescriptions<br />
over time, and there is a clear relationship between<br />
the number of drugs taken and the incidence of adverse<br />
drug-related events. 66–69 This problem will be compounded<br />
during the surgical period when additional medications<br />
are added.<br />
A study by Cullen and colleagues 238 prospectively compared<br />
adverse drug events in ICU and non-ICU, surgical<br />
and medical, hospitalized patients and found that the rate<br />
of preventable and potential adverse drug events was<br />
related to the number of drugs administered rather than<br />
the type of care delivered (ICU or non-ICU, surgical or<br />
medical). An earlier report of the same data on 4031<br />
adult hospital admissions identified, among other things,<br />
the incidence of adverse drug events, their preventability,<br />
and the classes of drugs that caused most events. 239 Those<br />
results have particular bearing for the perioperative care<br />
of the elderly.<br />
In that investigation by Bates et al., 239 analgesics were<br />
the class of drug associated with the most adverse drug<br />
events. Antibiotics caused the second-greatest number of<br />
adverse reactions. Analgesics were also the leading class<br />
of drug with preventable adverse drug events followed<br />
by sedatives and then antibiotics (Table 6-3). In the 20<br />
adverse events related to analgesics, 40% were caused by<br />
overmedication.<br />
<strong>The</strong>re is a pressing need for research in pain management<br />
of the elderly surgical patient. <strong>The</strong>re is also a<br />
Table 6-3. Adverse events by drug class.<br />
Adverse drug events Preventable adverse drug<br />
Drug class No. (%) (n = 247) events No. (%) (n = 70)<br />
Analgesics 73 (30) 20 (29)<br />
Antibiotics 59 (24) 6 (9)<br />
Sedatives 20 (8) 7 (10)<br />
Antineoplastic 18 (7) 3 (4)<br />
Cardiovascular 9 (4) 3 (4)<br />
Anticoagulants 8 (3) 3 (4)<br />
Antipsychotics 6 (2) 5 (7)<br />
Diabetes 5 (2) 4 (6)<br />
Electrolytes 3 (1) 3 (4)<br />
Other 46 (19) 16 (23)<br />
Source: Modified with permission from Bates et al. 239<br />
compelling need for research into prevention of adverse<br />
drug events in hospitalized patients. <strong>The</strong> intersection of<br />
pain management and the incidence of preventable<br />
adverse events related to analgesics and sedatives places<br />
anesthesiologists squarely in a leadership role for research<br />
into appropriate analgesic and sedative strategies for the<br />
elderly.<br />
In patients who are hospitalized, there is also a window<br />
of opportunity to review patient medications, in particular<br />
to examine redundancy in therapeutic profile and look<br />
for combinations that may make complications such as<br />
respiratory depression, aspiration, confusion, postural<br />
hypotension, urinary retention, and falls more likely. <strong>The</strong><br />
development of pharmacy and electronic drug databases<br />
for this work would be appropriate and are more within<br />
the resources of hospitals than community practitioners.<br />
Although it would not be practical or appropriate to<br />
modify most patient chronic drug regimes in the postoperative<br />
period, the surgical hospitalization might provide<br />
an opportunity for drug review and recommendation in<br />
an effort to reduce iatrogenic complications in the<br />
elderly.<br />
Delirium and Cognitive Decline<br />
Postoperative delirium or cognitive decline affects 5%–<br />
50% of elderly patients; both have similar predisposing<br />
factors but the syndromes are not equivalent. 110,200,240–242<br />
Disordered thinking and confusion that waxes and wanes<br />
characterize postoperative delirium. <strong>The</strong> onset is typically<br />
on the first to third postoperative day. It may be sustained<br />
for more than a week and is associated with other medical<br />
complications, prolonged hospitalization, and decreased<br />
functional status on discharge. 113,120,200,241,243–245 To date,<br />
much of the research on postoperative delirium has<br />
centered on the impact of regional versus general anesthesia<br />
in orthopedic surgery. 116,117,156,169–171,246 Postoperative<br />
cognitive dysfunction, a deterioration of psychomotor<br />
capacities such as memory, central processing time, and<br />
acquisition of new information, has been well described<br />
in both cardiac and noncardiac surgical patients. 247–250 It<br />
may be subtle or clinically obvious. <strong>The</strong> relationship<br />
between postoperative delirium and cognitive dysfunction<br />
has not been well studied.<br />
<strong>The</strong> effect of differing anesthetics on postoperative<br />
delirium has been studied, 117,156,171,251–254 and a leading<br />
hypothesis has been that offending agents aggravate an<br />
age-associated central cholinergic insufficiency. 116,255,256<br />
However, from review of the literature, it becomes<br />
evident that delirium can be triggered by many different<br />
perioperative events; no single cause is identifiable. Thus,<br />
no single intervention is likely to be successful.<br />
In addition to being linked to opiates, sedatives,<br />
and anticholinergics, delirium has been associated<br />
with urinary tract infection, pneumonia, hypoxia or
6. Research Priorities in <strong>Geriatric</strong> <strong>Anesthesiology</strong> 81<br />
hyper carbia, fever, blood loss, and electrolyte disturbances.<br />
200,240,241,257–259 Chronic patient factors such as<br />
preexisting frank or subclinical dementia, other organic<br />
brain disease, and vision and hearing loss are also predictors<br />
of postoperative delirium and cognitive de -<br />
cline. 102,110,113,200,240,260,261 Finally, pain, sleep deprivation,<br />
sensory deprivation, and an unfamiliar environment may<br />
contribute to delirium. 112,200,240,262,263<br />
Although most of the research in the anesthesia literature<br />
has focused on the effect of anesthetic and analgesic<br />
agents, the literature in medical patients suggests that the<br />
yield for those studies will be low. Studies of the type<br />
conducted by Inouye et al. might serve as a model for<br />
research in anesthesia. 103,108,259–261,264–266 Inouye describes a<br />
multifactorial model for delirium involving the interrelationship<br />
between a vulnerable patient and acute<br />
insults. 259,264 For example, a minor insult may result in<br />
delirium in highly vulnerable patients, whereas in less<br />
vulnerable patients, a major insult may be required to<br />
precipitate delirium. In a study of elderly medical patients,<br />
multivariate modeling identified four risk factors for<br />
developing hospitalization delirium: vision impairment,<br />
severe illness, preexisting cognitive impairment, and a<br />
blood urea nitrogen/creatinine ratio ≥18. 264,267 Patients<br />
were then divided into low-, intermediate-, and high-risk<br />
groups depending on the number of risk factors. In a<br />
subsequent validation cohort, the rates of delirium in the<br />
low-, intermediate-, and high-risk groups were 3%, 16%,<br />
and 32%, respectively (Table 6-4). 264 In those patients, the<br />
rate of death or nursing home placement was 3%, 14%,<br />
and 26%, respectively, an eightfold increase from the<br />
lowest to highest risk group. 267 Precipitating factors for<br />
delirium in hospitalized medical patients have also been<br />
described by Inouye and Charpentier. 259 Twenty-five<br />
factors occurring at least 24 hours before the onset of<br />
delirium were considered. Of those, a multivariate model<br />
identified five as predictive: use of physical restraints,<br />
Table 6-4. In-hospital events and risk of delirium.<br />
Risk group No. of factors Delirium rate, by person* RR<br />
Low 0 5/125 (4)† 1.0<br />
Intermediate 1–2 31/156 (20)† 5.0<br />
High ≥3 11/31 (35)† 8.9<br />
Source: Modified with permission from Inouye. 264 Published by S.<br />
Karger AG, Basel.<br />
RR = relative risk.<br />
Each patient’s risk group was determined by adding one point for each<br />
precipitating factor present: use of restraints, urinary catheter, more<br />
than three medications added, any iatrogenic event, and malnutrition.<br />
Figures in parentheses represent percentage.<br />
*Corresponds with percentage of patients developing delirium per<br />
day.<br />
†x 2 overall = 24.8, p < 0.001; x 2 trend = 24.8, p < 0.001.<br />
Performance of the predictive model for delirium in medical patients<br />
in the validation cohort.<br />
malnutrition, more than three medications added, use of<br />
a bladder catheter, and any iatrogenic event (volume<br />
overload, urinary tract infection, pressure ulcer, etc.). 259<br />
Although the precipitating factors were independent of<br />
each other, the authors note that “. . . baseline and precipitating<br />
factors are highly interrelated and contribute<br />
to delirium in a cumulative fashion.” 259<br />
In a subsequent publication, Inouye and colleagues 265<br />
determined the effect of interventions based on their<br />
predictive model. Four hundred twenty-six elderly<br />
medical patients in an intervention group were matched<br />
to an equal number in a “usual care” group. In the<br />
intervention group, six risk factors for delirium were targeted<br />
for intervention: cognitive impairment, sleep deprivation,<br />
immobility, visual and hearing impairment, and<br />
dehydration. <strong>The</strong> group receiving intervention, by an<br />
interdisciplinary team, had a 9.9% incidence of delirium<br />
versus 15% in the usual care group (a 34% decline).<br />
Subdivision of patients into intermediate- or high-risk<br />
groups demonstrated that intervention reduced delirium<br />
in intermediate-risk patients, but the tendency to reduce<br />
delirium in the high-risk group was not statistically<br />
significant. 265<br />
<strong>The</strong>se studies indicate that presence and severity of<br />
cognitive deficit are strong predictors of the likelihood of<br />
delirium during the hospitalization. 264 <strong>The</strong> same effect has<br />
been identified in surgical patients. 110–113 This brings us<br />
back to the recurring theme that subclinical decrements<br />
in functional status may become evident during the perioperative<br />
period. <strong>The</strong>se findings are extended by the<br />
observation that postoperative delirium or cognitive<br />
decline may be a harbinger of a potentially permanent<br />
decrease in mental status. 247,268<br />
Together, the data on the predictive value of preoperative<br />
cognitive status 264 and the effect of that assessment<br />
on the success of intervention 265 provide a compelling<br />
rationale to conduct a simple, short mental status examination<br />
as part of the preoperative interview. Short functional<br />
scales have been designed which might be applicable<br />
in the preoperative interview. 115,269,270 <strong>The</strong> practicality of<br />
such metrics in elderly surgical patients must be established.<br />
After that, the incidence of preoperative cognitive<br />
impairment and its severity could be identified in populations<br />
of elderly patients undergoing different types of<br />
procedures. Research into the effectiveness of differing<br />
preventative strategies could follow. For example, pharmacologic<br />
prophylaxis of delirium shows promise. 271<br />
Those investigations could also examine if reductions in<br />
delirium translate into reduced medical complications or<br />
improved functional status on discharge.<br />
Chronic Pain<br />
A significant proportion of the geriatric population suffers<br />
from chronic pain conditions. 46,47 Much of this is related
82 C.J. Jankowski and D.J. Cook<br />
to osteoarthritis, but many older patients have a variety<br />
of neuropathic pain disorders including herpes zoster,<br />
diabetic neuropathies, and complex regional pain syndromes.<br />
272 Care of these patients is complex and for many<br />
of these painful conditions therapy is inadequate.<br />
<strong>The</strong> factors limiting therapeutic success in chronic pain<br />
in the elderly are multiple. First, in contrast to acute postoperative<br />
pain, the conditions responsible for chronic<br />
pain are typically not reversible. Second, pain conditions<br />
may have a central nervous system component. Third,<br />
effective treatment of chronic pain is hampered by the<br />
side effects of medications and complications from polypharmacy.<br />
Fourth, depression and behavioral changes<br />
frequently complicate therapy. 273 Fifth, assessment of<br />
pain in older patients can be difficult. 46 And, finally,<br />
chronic pain in the elderly is often associated with unrelated<br />
comorbid conditions that may alter treatment<br />
plans. 43,274 Despite these limitations, geriatric patients<br />
benefit from chronic pain therapy in a manner similar to<br />
younger patients. 43,275,276<br />
Most pain syndromes can be classified into one of four<br />
types: nociceptive, neuropathic, mixed, or unspecified and<br />
psychogenic. 47 <strong>The</strong> usefulness of different classes of analgesic<br />
agents in these types of syndromes is reasonably<br />
well described. Nociceptive pain includes the pain typically<br />
associated with arthropathies, myalgias, and ischemic<br />
disorders; the mainstays of analgesia are initially<br />
acetaminophen and nonsteroidal antiinflammatory drugs,<br />
followed later by narcotics. 46,47,272 In contrast, narcotics<br />
are thought to have a lesser place in neuropathies such<br />
as diabetic neuropathy, postherpetic neuralgia (PHN),<br />
and complex regional pain syndromes. 272,277,278 Instead, the<br />
primary pharmacologic therapies are tricyclic antidepressants<br />
and anticonvulsant agents. 46,272,279–281 Antiarrhythmic<br />
drugs are second-tier agents for neuropathic conditions.<br />
Treatment of mixed or unspecified pain syndromes is<br />
challenging, because the mechanisms are unknown and<br />
treatment may require trials of differing analgesic<br />
approaches. 47 For patients whose pain has been classified<br />
as psychogenic, psychiatric intervention rather than analgesic<br />
agents is indicated. 47<br />
In addition to familiar analgesics and adjuncts, there<br />
is a clear need for a multidimensional approach to<br />
chronic pain in the elderly. Neuraxial opioids, local anesthetics,<br />
and steroids have a role in some patients, as do<br />
peripheral or central neuromodulatory techniques and a<br />
host of physical, physiatric, and cognitive-behavorial<br />
strategies. 43,46,47<br />
Defining research priorities for anesthesiologists in<br />
such a broad and complex area is difficult. <strong>The</strong> first priority<br />
is that chronic pain trials must have sufficient control<br />
groups and statistical power. As noted by Stanton-Hicks<br />
and colleagues, 280 studies of neuropathic pain conditions<br />
are typically small and anecdotal with few experimental<br />
findings and “without adequate predictors for the choice<br />
of therapy, current practice is chaotic, and continues to<br />
use the trial-and-error approach.”<br />
After design issues are addressed, probably the most<br />
salient research recommendation for any of these types<br />
of pain conditions is that outcomes should emphasize<br />
functional status 276,282 rather than a change in a pain score,<br />
per se. This is superbly outlined in the Consensus Report<br />
on Complex <strong>Regional</strong> Pain Syndromes. 280 Although<br />
quantifying pain is relevant, ultimately, determination of<br />
which interventions facilitate rehabilitation, maintain or<br />
increase mobility, and support the activities of daily living<br />
is a priority. 276,282<br />
<strong>The</strong> second broad area requiring further investigation<br />
relates to prevention. One of the best examples is in PHN.<br />
Although the rash of acute herpes zoster is very common<br />
in the elderly, a lesser, but significant, percentage of those<br />
affected develop the chronic debilitating pain condition<br />
of PHN. 283 Because zoster is chronic and recurring, the<br />
percentage of the population affected with PHN increases<br />
with age. 283 Although PHN may develop in fewer than<br />
5% of younger patients with zoster, it may develop in half<br />
of patients over age 60. 284 Once established, PHN is difficult<br />
to treat. Further research is indicated to determine<br />
whether antiviral, analgesic, antiinflammatory therapies<br />
during acute zoster can prevent the development of<br />
chronic PHN. 285–288 In addition, immunotherapeutic<br />
modalities show promise and deserve more study. 289–298 If<br />
a better understanding of precipitating events can be<br />
developed for other chronic pain conditions (as in<br />
PHN 299 ), it might allow the introduction of preventive<br />
measures.<br />
In addition to directing research efforts toward functional<br />
effects and trying to define opportunities for prevention<br />
of chronic pain conditions, for any strategy, it is<br />
important to examine the risk–benefit ratio, emphasizing<br />
adverse outcomes that are more likely to occur in a geriatric<br />
population. As in acute pain management, the effect<br />
of chronic therapy on the incidence of complications such<br />
as confusion, postural hypotension, falls, urinary retention,<br />
and constipation must be reported.<br />
Finally, cognitive impairment is a continuum and in<br />
milder forms is very common. <strong>The</strong>re is a two-way relationship:<br />
pain may impair cognition and cognitive impairment<br />
can interfere with the communication of pain. 46,300<br />
<strong>The</strong>refore, a further area of investigation relevant to the<br />
care of patients with chronic pain is its assessment in the<br />
cognitively impaired.<br />
Postoperative Research Agenda Items<br />
• Large cross-sectional studies describing analgesic practice<br />
and its complications in the elderly are needed.<br />
<strong>The</strong> effect of regional analgesic techniques, nonopioid<br />
adjunctive drugs, and nonpharmacologic interventions<br />
would be investigated in prospective cohort or
6. Research Priorities in <strong>Geriatric</strong> <strong>Anesthesiology</strong> 83<br />
case-control studies. <strong>The</strong>se investigations must emphasize<br />
the type and incidence of adverse drug events in<br />
the elderly. After that, randomized controlled trials<br />
comparing outcomes with analgesic programs specific<br />
to types of surgery could be designed and conducted.<br />
Those prospective trials should determine if analgesic<br />
regimes designed for the elderly patient could reduce<br />
in-hospital morbidity or improve functional status on<br />
discharge.<br />
• Prospective studies that better identify patient and<br />
procedural risk factors for respiratory failure, aspiration,<br />
and pneumonia are required. Randomized trials<br />
could then determine if respiratory monitoring, prophylactic<br />
antibiotics, changes in pharyngeal instrumentation,<br />
or the way feeding is advanced reduce respiratory<br />
failure, aspiration, and postoperative pneumonia.<br />
• <strong>The</strong> relationship between postoperative nutritional<br />
support and functional outcome must be better understood.<br />
Cross-sectional studies that could identify if a<br />
relationship between nutritional support in high-risk<br />
surgery and functional status on discharge (chronic<br />
respiratory failure, ambulation, independent living,<br />
etc.) are the first step. Data from those investigations<br />
could then be used to design prospective-cohort or<br />
randomized controlled trials comparing feeding strategies<br />
in elderly patients at risk for malnutrition and<br />
muscle wasting following major surgery. In addition to<br />
protein and caloric support, interventions that might<br />
attenuate postoperative catabolism or facilitate the<br />
transition to an anabolism in the elderly could be<br />
compared with standard care.<br />
• Practice governing stopping or resuming anticoagulation<br />
in the perioperative period is largely empiric.<br />
Studies determining the relationship between perioperative<br />
termination of anticoagulation and thromboembolic<br />
and bleeding risk are indicated. <strong>The</strong> effect of<br />
timing of termination and resumption as well as the<br />
temporizing use of antiplatelet agents should be compared<br />
in case-control or prospective cohort studies.<br />
• <strong>The</strong> surgical hospitalization might provide an opportunity<br />
for drug review and recommendation in an effort<br />
to reduce iatrogenic complications in the elderly. Initially,<br />
a retrospective review could identify the incidence<br />
of polypharmacy with combinations of drugs<br />
that might contribute to geriatric complications (hypotension,<br />
bradycardia, falls, confusion, bleeding diathesis,<br />
constipation, and urinary retention). Subsequently,<br />
the presence or absence of an effect of simplifying drug<br />
regimens in hospital or the effect of communicating<br />
that information to primary care physicians could be<br />
identified in nonrandomized controlled trials.<br />
• Using the models established in medical patients, evaluating<br />
prevention strategies for postoperative delirium<br />
must be tested. It should first be determined by crosssectional<br />
studies, with multivariate analysis, if the risk<br />
factors for delirium in surgical patients are the same as<br />
those for medical patients. After that, prospective controlled<br />
trials in patients at moderate to high risk could<br />
determine the effect of preoperative or postoperative<br />
interventions on the incidence of delirium.<br />
• <strong>The</strong> first priority in chronic pain trials is large crosssectional<br />
studies that might identify any relationship<br />
between pain intervention and functional outcomes.<br />
After that, it must be determined prospectively if specific<br />
chronic pain therapies can improve functional outcomes<br />
in treatment groups relative to a historical or<br />
concurrent, nonrandomized control.<br />
• Given the frequency of herpes zoster in the geriatric<br />
population, further prospective studies are needed to<br />
determine if antiviral, analgesic, or antiinflammatory<br />
therapies during acute zoster can reduce, relative to<br />
standard care, the development of chronic PHN.<br />
• As in acute pain management, cross-sectional studies<br />
documenting the effect of chronic pain therapy on the<br />
incidence of complications such as confusion, postural<br />
hypotension, falls, urinary retention, and constipation<br />
in the elderly are indicated.<br />
• Assessment and treatment of acute or chronic pain in<br />
the cognitively impaired is largely empiric. Cross-sectional<br />
studies that describe pain management in this<br />
population relative to a nonimpaired population are<br />
indicated. Additionally, pain assessment tools for the<br />
cognitively impaired must be compared prospectively<br />
to standard assessment methods. After that, prospective<br />
trials comparing different analgesic strategies with<br />
regard to clinical and functional endpoints could be<br />
conducted.<br />
Summary and Conclusions<br />
Perioperative care of the geriatric patient is complex.<br />
Age-related physiologic changes and disease limit functional<br />
reserve and render the elderly less able to tolerate<br />
the challenges of the perioperative period. Thus, they are<br />
at increased risk for a host of complications. Furthermore,<br />
it is probably easier to precipitate these complications<br />
than to directly prevent them.<br />
Despite the unique challenges of the perioperative<br />
care of the elderly, existing literature offers clinicians<br />
insufficient guidance. Nevertheless, previous studies<br />
provide a framework to guide future research. Rather<br />
than focus attention on the choice of anesthetic technique<br />
or on short-term outcomes such as time to extubation<br />
or recovery room stay, improvement in patient<br />
outcomes will be better served by studies that yield better<br />
risk-stratification in the elderly. To some extent, pertinent<br />
patient risk factors will probably be surgery-specific. Subsequently,<br />
it can be determined if identified risk factors<br />
are amenable to therapy and whether such intervention
84 C.J. Jankowski and D.J. Cook<br />
improves outcome. An essential element of both types of<br />
investigations will be a focus on preoperative functional<br />
status and other pertinent geriatric outcomes rather than<br />
just major cardiopulmonary morbidity and mortality.<br />
Surgical outcome is determined by the interaction of<br />
patient factors and the challenges introduced by an operation.<br />
Clearly, the surgical insult varies by procedure.<br />
<strong>The</strong>refore, development of comprehensive care strategies<br />
for specific types of surgery common in the elderly is<br />
indicated. This approach is more likely to generate positive<br />
results and practical guidelines than pooling elderly<br />
patients undergoing differing types of surgery. Development<br />
of comprehensive clinical pathways specific to the<br />
care of the elderly patient undergoing specific types of<br />
surgeries is indicated because it would coordinate preoperative,<br />
intraoperative, and postoperative management in<br />
a particularly vulnerable population. This approach could<br />
improve outcomes and serve as a foundation for assessing<br />
alternative strategies. It might have particular value<br />
in postoperative care, including prevention of delirium,<br />
respiratory monitoring, and pain management.<br />
<strong>The</strong> perioperative care of the elderly is a growing<br />
public health issue. Anesthesiologists are involved in the<br />
care of older surgical patients from the preoperative<br />
evaluation through the postoperative period. Because of<br />
this perspective, we offer unique insights into their care.<br />
Applying these to appropriately conceived studies will<br />
lead to improved perioperative outcomes and, ultimately,<br />
benefit society.<br />
Highest Priority Research Questions<br />
in <strong>Geriatric</strong> <strong>Anesthesiology</strong><br />
1. What preoperative assessments are useful in developing<br />
patient management plans for surgeries common in<br />
the elderly?<br />
Hypothesis-generating: Large, observational studies are<br />
needed to identify preoperative risk factors for adverse<br />
geriatric outcomes, such as decreased functional status or<br />
postoperative delirium, following common surgeries.<br />
<strong>The</strong>se studies will identify both patient and surgerydependent<br />
factors. Assessment tools for mental status,<br />
nutrition, hydration, thrombotic risk, and activities of<br />
daily living must be applied or developed when necessary.<br />
It then should be determined which risk factors are<br />
potentially modifiable.<br />
Hypothesis-testing: Randomized controlled trials to<br />
determine if preoperative or postoperative intervention<br />
against modifiable risk factors will result in a decrease in<br />
perioperative geriatric complications. <strong>The</strong> adverse effects<br />
of such interventions, such as delay of surgery or postoperative<br />
bleeding, must be examined along with the<br />
potential benefits of the intervention. Examples for<br />
which such interventions could be reasonably attempted<br />
include nutrition and hydration, postoperative delirium,<br />
pre- or postoperative rehabilitation programs for activities<br />
of daily living, and antiplatelet therapy for thrombotic<br />
and embolic complications.<br />
2. Can postoperative analgesic techniques reduce postoperative<br />
morbidity or improve functional status at<br />
discharge?<br />
Hypothesis-generating: Large prospective studies describing<br />
analgesic practice and its complications in the elderly<br />
are needed. <strong>The</strong> efficacy and complications of regional<br />
analgesic techniques, nonopioid adjunctive drugs, and<br />
physiatric interventions must be investigated. <strong>The</strong>se<br />
investigations must emphasize the type and incidence of<br />
adverse drug events in the elderly.<br />
Hypothesis-testing: Prospective randomized trials are<br />
needed to determine if perioperative intensive analgesic<br />
techniques (including traditional narcotic, regional, nonopioid<br />
adjunctive drugs, and physiatric interventions)<br />
designed for the elderly patient reduce in-hospital morbidity<br />
or improve functional status on discharge.<br />
3. How can postoperative pulmonary complications in<br />
the elderly be reduced?<br />
Hypothesis-generating: Cross-sectional or cohort studies<br />
that better identify high-risk procedures or perioperative<br />
periods of vulnerability for postoperative hypoxia, respiratory<br />
failure, and pneumonia in the elderly surgical<br />
patient are indicated. <strong>The</strong>se investigations could identify<br />
both patient and procedure risk factors as well as their<br />
interaction for these complications.<br />
Hypothesis-testing: Randomized trials to determine if<br />
respiratory monitoring, prophylactic antibiotics, changes<br />
in pharyngeal instrumentation, or the way feeding is<br />
advanced reduce respiratory failure, aspiration, and<br />
postoperative pneumonia.<br />
References<br />
1. Franklin SS, Gustin WT, Wong ND, et al. Hemodynamic<br />
patterns of age-related changes in blood pressure. <strong>The</strong><br />
Framingham Heart Study. Circulation 1997;96:308–315.<br />
2. Landahl S, Bengtsson C, Sigurdsson JA, Svanborg A,<br />
Svardsudd K. Age-related changes in blood pressure.<br />
Hypertension 1986;8:1044–1049.<br />
3. Pan HY, Hoffman BB, Pershe RA, Blaschke TF. Decline<br />
in beta adrenergic receptor-mediated vascular relaxation<br />
with aging in man. J Pharmacol Exp <strong>The</strong>r 1986;239:802–<br />
807.<br />
4. Folkow B, Svanborg A. Physiology of cardiovascular aging.<br />
Physiol Rev 1993;73:725–764.<br />
5. Falk RH. Etiology and complications of atrial fibrillation:<br />
insights from pathology studies. Am J Cardiol 1998;82:<br />
10N–17N.
6. Research Priorities in <strong>Geriatric</strong> <strong>Anesthesiology</strong> 85<br />
6. Mackstaller LL, Alpert JS. Atrial fibrillation: a review of<br />
mechanism, etiology, and therapy. Clin Cardiol 1997;20:<br />
640–650.<br />
7. Lakatta EG. Age-related alterations in the cardiovascular<br />
response to adrenergic mediated stress. Fed Proc 1980;<br />
39:3173–3177.<br />
8. Rodeheffer RJ, Gerstenblith G, Becker LC, Fleg JL,<br />
Weisfeldt ML, Lakatta EG. Exercise cardiac output is<br />
maintained with advancing age in healthy human subjects:<br />
cardiac dilatation and increased stroke volume compensate<br />
for a diminished heart rate. Circulation 1984;69:<br />
203–213.<br />
9. Collins KJ, Exton-Smith AN, James MH, Oliver DJ. Functional<br />
changes in autonomic nervous responses with ageing.<br />
Age Ageing 1980;9:17–24.<br />
10. McGarry K, Laher M, Fitzgerald D, Horgan J, O’Brien E,<br />
O’Malley K. Baroreflex function in elderly hypertensives.<br />
Hypertension 1983;5:763–766.<br />
11. Phillips PA, Hodsman GP, Johnston CI. Neuroendocrine<br />
mechanisms and cardiovascular homeostasis in the elderly.<br />
Cardiovasc Drugs <strong>The</strong>r 1991;4(Suppl 6):1209–1213.<br />
12. Cleroux J, Giannattasio C, Bolla G, et al. Decreased cardiopulmonary<br />
reflexes with aging in normotensive humans.<br />
Am J Physiol 1989;257:H961–H968.<br />
13. Rowe JW, Troen BR. Sympathetic nervous system and<br />
aging in man. Endocr Rev 1980;1:167–179.<br />
14. Wahba WM. Influence of aging on lung function—clinical<br />
significance of changes from age twenty. Anesth Analg<br />
1983;62:764–776.<br />
15. Zaugg M, Lucchinetti E. Respiratory function in the<br />
elderly. Anesthesiol Clin North Am 2000;18:47–58, vi.<br />
16. Fowler RW. Ageing and lung function. Age Ageing 1985;<br />
14:209–215.<br />
17. Tolep K, Kelsen SG. Effect of aging on respiratory skeletal<br />
muscles. Clin Chest Med 1993;14:363–378.<br />
18. Pontoppidan H, Geffin B, Lowenstein E. Acute respiratory<br />
failure in the adult. 1. N Engl J Med 1972;287:690–698.<br />
19. Kitamura H, Sawa T, Ikezono E. Postoperative hypoxemia:<br />
the contribution of age to the maldistribution of ventilation.<br />
<strong>Anesthesiology</strong> 1972;36:244–252.<br />
20. Lynne-Davies P. Influence of age on the respiratory system.<br />
<strong>Geriatric</strong>s 1977;32:57–60.<br />
21. Cerveri I, Zoia MC, Fanfulla F, et al. Reference values<br />
of arterial oxygen tension in the middle-aged and elderly.<br />
Am J Respir Crit Care Med 1995;152:934–941.<br />
22. Kronenberg RS, Drage CW. Attenuation of the ventila -<br />
tory and heart rate responses to hypoxia and hypercapnia<br />
with aging in normal men. J Clin Invest 1973;52:1812–<br />
1819.<br />
23. Aviv JE. Effects of aging on sensitivity of the pharyngeal<br />
and supraglottic areas. Am J Med 1997;103:74S–76S.<br />
24. Marik PE. Aspiration pneumonitis and aspiration pneumonia.<br />
N Engl J Med 2001;344:665–671.<br />
25. Arunasalam K, Davenport HT, Painter S, Jones JG. Ventilatory<br />
response to morphine in young and old subjects.<br />
Anaesthesia 1983;38:529–533.<br />
26. Sari A, Miyauchi Y, Yamashita S, Yokota K, Ogasahara H,<br />
Yonei A. <strong>The</strong> magnitude of hypoxemia in elderly patients<br />
with fractures of the femoral neck. Anesth Analg 1986;<br />
65:892–894.<br />
27. Kronenberg RS, Drage CW, Ponto RA, Williams LE. <strong>The</strong><br />
effect of age on the distribution of ventilation and perfusion<br />
in the lung. Am Rev Respir Dis 1973;108:576–586.<br />
28. Clayer M, Bruckner J. Occult hypoxia after femoral neck<br />
fracture and elective hip surgery. Clin Orthop 2000:<br />
265–271.<br />
29. Moller JT, Jensen PF, Johannessen NW, Espersen K.<br />
Hypoxaemia is reduced by pulse oximetry monitoring in<br />
the operating theatre and in the recovery room. Br J<br />
Anaesth 1992;68:146–150.<br />
30. de Larminat V, Montravers P, Dureuil B, Desmonts JM.<br />
Alteration in swallowing reflex after extubation in intensive<br />
care unit patients. Crit Care Med 1995;23:486–490.<br />
31. Morris JC, McManus DQ. <strong>The</strong> neurology of aging: normal<br />
versus pathologic change. <strong>Geriatric</strong>s 1991;46:47–48,<br />
51–54.<br />
32. Creasey H, Rapoport SI. <strong>The</strong> aging human brain. Ann<br />
Neurol 1985;17:2–10.<br />
33. Morrison JH, Hof PR. Life and death of neurons in the<br />
aging brain. Science 1997;278:412–419.<br />
34. Severson JA. Neurotransmitter receptors and aging. J Am<br />
Geriatr Soc 1984;32:24–27.<br />
35. Wong DF, Wagner HN Jr, Dannals RF, et al. Effects of<br />
age on dopamine and serotonin receptors measured by<br />
positron tomography in the living human brain. Science<br />
1984;226:1393–1396.<br />
36. Muravchick S. Central nervous system. In: Geroanesthesia:<br />
Principles for Management of the Elderly Patient. St.<br />
Louis: Mosby-Year Book; 1997:78–113.<br />
37. Peterson DD, Pack AI, Silage DA, Fishman AP. Effects<br />
of aging on ventilatory and occlusion pressure responses<br />
to hypoxia and hypercapnia. Am Rev Respir Dis 1981;<br />
124:387–391.<br />
38. Muravchick S. Peripheral and autonomic nervous system.<br />
In: Geroanesthesia: Principles for Management of the<br />
Elderly Patient. St. Louis: Mosby-Year Book; 1997:<br />
114–148.<br />
39. Gibson SJ, Helme RD. Age differences in pain perception<br />
and report: a review of physiological, psychological, laboratory<br />
and clinical studies. Pain Rev 1995;2:111–137.<br />
40. Tucker MA, Andrew MF, Ogle SJ, Davison JG. Ageassociated<br />
change in pain threshold measured by transcutaneous<br />
neuronal electrical stimulation. Age Ageing<br />
1989;18:241–246.<br />
41. Potvin AR, Syndulko K, Tourtellotte WW, Lemmon JA,<br />
Potvin JH. Human neurologic function and the aging<br />
process. J Am Geriatr Soc 1980;28:1–9.<br />
42. Chakour MC, Gibson SJ, Bradbeer M, Helme RD. <strong>The</strong><br />
effect of age on A delta- and C-fibre thermal pain perception.<br />
Pain 1996;64:143–152.<br />
43. Helme RD, Gibson SJ. Pain in the elderly. In: Jensen TS,<br />
Turner JA, Wiesenfeld-Hallin Z, eds. Proceedings of the<br />
8th World Congress on Pain. Parkville, Australia: IASP<br />
Press; 1997:919–944.<br />
44. Harkins SW. <strong>Geriatric</strong> pain. Pain perceptions in the old.<br />
Clin Geriatr Med 1996;12:435–459.<br />
45. Harkins SW, Davis MD, Bush FM, Kasberger J. Suppression<br />
of first pain and slow temporal summation of second<br />
pain in relation to age. J Gerontol A Biol Sci Med Sci 1996;<br />
51:M260–M265.
86 C.J. Jankowski and D.J. Cook<br />
46. Ferrell BA. Pain management in elderly people. J Am<br />
Geriatr Soc 1991;39:64–73.<br />
47. Anonymous. <strong>The</strong> management of chronic pain in older<br />
persons: AGS Panel on Chronic Pain in Older Persons.<br />
American <strong>Geriatric</strong>s Society. J Am Geriatr Soc 1998;46:<br />
635–651.<br />
48. Jones JS, Johnson K, McNinch M. Age as a risk factor for<br />
inadequate emergency department analgesia. Am J Emerg<br />
Med 1996;14:157–160.<br />
49. McLachlan MS. <strong>The</strong> ageing kidney. Lancet 1978;2:143–<br />
145.<br />
50. Anderson S, Brenner BM. <strong>The</strong> aging kidney: structure,<br />
function, mechanisms, and therapeutic implications. J Am<br />
Geriatr Soc 1987;35:590–593.<br />
51. Epstein M. Aging and the kidney. J Am Soc Nephrol<br />
1996;7:1106–1122.<br />
52. Anderson S, Brenner BM. Effects of aging on the renal<br />
glomerulus. Am J Med 1986;80:435–442.<br />
53. Shannon RP, Minaker KL, Rowe JW. Aging and water<br />
balance in humans. Semin Nephrol 1984;4:346–353.<br />
54. Miller M. Fluid and electrolyte balance in the elderly.<br />
<strong>Geriatric</strong>s 1987;42:65–76.<br />
55. Phillips PA, Rolls BJ, Ledingham JG, et al. Reduced thirst<br />
after water deprivation in healthy elderly men. N Engl J<br />
Med 1984;311:753–759.<br />
56. Rowe JW, Minaker KL, Sparrow D, Robertson GL. Agerelated<br />
failure of volume-pressure-mediated vasopressin<br />
release. J Clin Endocrinol Metab 1982;54:661–664.<br />
57. Kliger AS. <strong>The</strong> role of the kidney in fluid, electrolyte,<br />
and acid-base disorders. Int Anesthesiol Clin 1984;22:65–<br />
82.<br />
58. Lamy PP, Wiser TH. <strong>Geriatric</strong> anesthesia. In: Katlic MR,<br />
ed. Pharmacotherapeutic Considerations in the Elderly<br />
Surgical Patient. Baltimore: Urban & Schwarzenberg;<br />
1990:209–239.<br />
59. Greenblatt DJ, Sellers EM, Shader RI. Drug therapy:<br />
drug disposition in old age. N Engl J Med 1982;306:<br />
1081–1088.<br />
60. Shafer SL. <strong>The</strong> pharmacology of anesthetic drugs in elderly<br />
patients. Anesthesiol Clin North Am 2000;18:1–29, v.<br />
61. Matteo RS, Ornstein E. Pharmacokinetics and pharmacodynamics<br />
of injected drugs in the elderly. Adv Anesth<br />
1988;5:25–52.<br />
62. Silverstein JH, Bloom HG, Cassel CK. New challenges in<br />
anesthesia: new practice opportunities. Anesthesiol Clin<br />
North Am 1999;17:453–465.<br />
63. Dundee JW, Robinson FP, McCollum JS, Patterson CC.<br />
Sensitivity to propofol in the elderly. Anaesthesia 1986;<br />
41:482–485.<br />
64. Jacobs JR, Reves JG, Marty J, White WD, Bai SA, Smith<br />
LR. Aging increases pharmacodynamic sensitivity to the<br />
hypnotic effects of midazolam. Anesth Analg 1995;80:<br />
143–148.<br />
65. Homer TD, Stanski DR. <strong>The</strong> effect of increasing age<br />
on thiopental disposition and anesthetic requirement.<br />
<strong>Anesthesiology</strong> 1985;62:714–724.<br />
66. Hurwitz N. Predisposing factors in adverse reactions to<br />
drugs. Br Med J 1969;1:536–539.<br />
67. Hurwitz N, Wade OL. Intensive hospital monitoring of<br />
adverse reactions to drugs. Br Med J 1969;1:531–536.<br />
68. Patterson C. Iatrogenic disease in late life. Clin Geriatr<br />
Med 1986;2:121–136.<br />
69. Williamson J, Chopin JM. Adverse reactions to prescribed<br />
drugs in the elderly: a multicentre investigation. Age<br />
Ageing 1980;9:73–80.<br />
70. Muravchick S. <strong>The</strong> biology of aging and preoperative evaluation.<br />
In: Geroanesthesia: Principles for Management of<br />
the Elderly Patient. St. Louis: Mosby-Year Book; 1997:<br />
1–34.<br />
71. Thomas DR, Ritchie CS. Preoperative assessment of older<br />
adults. J Am Geriatr Soc 1995;43:811–821.<br />
72. Vaz FG, Seymour DG. A prospective study of elderly<br />
general surgical patients: I. Preoperative medical problems.<br />
Age Ageing 1989;18:309–315.<br />
73. Schneider JR, Droste JS, Schindler N, Golan JF. Carotid<br />
endarterectomy in octogenarians: comparison with patient<br />
characteristics and outcomes in younger patients. J Vasc<br />
Surg 2000;31:927–935.<br />
74. Hoballah JJ, Nazzal MM, Jacobovicz C, Sharp WJ,<br />
Kresowik TF, Corson JD. Entering the ninth decade is<br />
not a contraindication for carotid endarterectomy.<br />
Angiology 1998;49:275–278.<br />
75. Hosking MP, Warner MA, Lobdell CM, Offord KP, Melton<br />
LJd. Outcomes of surgery in patients 90 years of age and<br />
older [see comments]. JAMA 1989;261:1909–1915.<br />
76. Warner MA, Saletel RA, Schroeder DR, Warner DO,<br />
Offord KP, Gray DT. Outcomes of anesthesia and surgery<br />
in people 100 years of age and older. J Am Geriatr Soc<br />
1998;46:988–993.<br />
77. Laskin RS. Total knee replacement in patients older than<br />
85 years. Clin Orthop 1999:43–49.<br />
78. Tiret L, Desmonts JM, Hatton F, Vourc’h G. Complications<br />
associated with anaesthesia—a prospective survey in<br />
France. Can Anaesth Soc J 1986;33:336–344.<br />
79. Eagle KA, Brundage BH, Chaitman BR, et al. Guidelines<br />
for perioperative cardiovascular evaluation for noncardiac<br />
surgery. Report of the American College of Cardiology/<br />
American Heart Association Task Force on Practice<br />
Guidelines. Committee on Perioperative Cardiovascular<br />
Evaluation for Noncardiac Surgery. Circulation 1996;93:<br />
1278–1317.<br />
80. Goldman L. Cardiac risks and complications of noncardiac<br />
surgery. Ann Intern Med 1983;98:504–513.<br />
81. Liu LL, Leung JM. Predicting adverse postoperative<br />
outcomes in patients aged 80 years or older. J Am Geriatr<br />
Soc 2000;48:405–412.<br />
82. Arvidsson S, Ouchterlony J, Sjostedt L, Svardsudd K.<br />
Predicting postoperative adverse events. Clinical efficiency<br />
of four general classification systems. <strong>The</strong> project perioperative<br />
risk. Acta Anaesthesiol Scand 1996;40:783–<br />
791.<br />
83. Detsky AS, Abrams HB, Forbath N, Scott JG, Hilliard JR.<br />
Cardiac assessment for patients undergoing noncardiac<br />
surgery. A multifactorial clinical risk index. Arch Intern<br />
Med 1986;146:2131–2134.<br />
84. Pedersen T, Eliasen K, Henriksen E. A prospective study<br />
of risk factors and cardiopulmonary complications associated<br />
with anaesthesia and surgery: risk indicators of<br />
cardiopulmonary morbidity. Acta Anaesthesiol Scand<br />
1990;34:144–155.
6. Research Priorities in <strong>Geriatric</strong> <strong>Anesthesiology</strong> 87<br />
85. Pedersen T, Eliasen K, Henriksen E. A prospective study<br />
of mortality associated with anaesthesia and surgery: risk<br />
indicators of mortality in hospital. Acta Anaesthesiol<br />
Scand 1990;34:176–182.<br />
86. Browner WS, Li J, Mangano DT. In-hospital and long-term<br />
mortality in male veterans following noncardiac surgery.<br />
<strong>The</strong> Study of Perioperative Ischemia Research Group.<br />
JAMA 1992;268:228–232.<br />
87. Khuri SF, Daley J, Henderson W, et al. <strong>The</strong> National Veterans<br />
Administration Surgical Risk Study: risk adjustment<br />
for the comparative assessment of the quality of surgical<br />
care. J Am Coll Surg 1995;180:519–531.<br />
88. Arvidsson S, Ouchterlony J, Nilsson S, Sjostedt L, Svardsudd<br />
K. <strong>The</strong> Gothenburg study of perioperative risk. I.<br />
Preoperative findings, postoperative complications. Acta<br />
Anaesthesiol Scand 1994;38:679–690.<br />
89. Mohr DN. Estimation of surgical risk in the elderly: a correlative<br />
review. J Am Geriatr Soc 1983;31:99–102.<br />
90. Cheng KW, Wang CH, Ho RT, Jawan B, Lee JH. Outcome<br />
of surgery and anesthesia in patients 80 years of age and<br />
older. Acta Anaesthesiol Sin 1994;32:37–43.<br />
91. Cohen MM, Duncan PG, Tate RB. Does anesthesia<br />
contribute to operative mortality? JAMA 1988;260:2859–<br />
2863.<br />
92. Cohen MM, Duncan PG. Physical status score and trends<br />
in anesthetic complications. J Clin Epidemiol 1988;41:<br />
83–90.<br />
93. Goldman L, Hashimoto B, Cook EF, Loscalzo A. Comparative<br />
reproducibility and validity of systems for assessing<br />
cardiovascular functional class: advantages of a new<br />
specific activity scale. Circulation 1981;64:1227–1234.<br />
94. Lawton MP, Brody EM. Assessment of older people: selfmaintaining<br />
and instrumental activities of daily living.<br />
Gerontologist 1969;9:179–186.<br />
95. Ware JE, Sherbourne CD. <strong>The</strong> MOS 36-item short-form<br />
health survey (SF-36). Med Care 1992;30:473–483.<br />
96. Moy ML, Ingenito EP, Mentzer SJ, Evans RB, Reilly JJ Jr.<br />
Health-related quality of life improves following pulmonary<br />
rehabilitation and lung volume reduction surgery.<br />
Chest 1999;115:383–389.<br />
97. Mangione CM, Goldman L, Orav EJ, et al. Health-related<br />
quality of life after elective surgery: measurement of longitudinal<br />
changes. J Gen Intern Med 1997;12:686–697.<br />
98. Hannan EL, Magaziner J, Wang JJ, et al. Mortality and<br />
locomotion 6 months after hospitalization for hip fracture:<br />
risk factors and risk-adjusted hospital outcomes. JAMA<br />
2001;285:2736–2742.<br />
99. Tammela T, Kontturi M, Lukkarinen O. Postoperative<br />
urinary retention. I. Incidence and predisposing factors.<br />
Scand J Urol Nephrol 1986;20:197–201.<br />
100. Duits AA, Boeke S, Taams MA, Passchier J, Erdman RA.<br />
Prediction of quality of life after coronary artery bypass<br />
graft surgery: a review and evaluation of multiple, recent<br />
studies. Psychosom Med 1997;59:257–268.<br />
101. Keene JS, Anderson CA. Hip fractures in the elderly.<br />
Discharge predictions with a functional rating scale.<br />
JAMA 1982;248:564–567.<br />
102. McCartney JR, Palmateer LM. Assessment of cognitive<br />
deficit in geriatric patients. A study of physician behavior.<br />
J Am Geriatr Soc 1985;33:467–471.<br />
103. Inouye SK, Peduzzi PN, Robison JT, Hughes JS, Horwitz<br />
RI, Concato J. Importance of functional measures in<br />
predicting mortality among older hospitalized patients.<br />
JAMA 1998;279:1187–1193.<br />
104. Raja SN, Haythornthwaite JA. Anesthetic management<br />
of the elderly: measuring function beyond the imme -<br />
diate perioperative horizon. <strong>Anesthesiology</strong> 1999;91:909–<br />
911.<br />
105. Heyland DK, Guyatt G, Cook DJ, et al. Frequency and<br />
methodologic rigor of quality-of-life assessments in the<br />
critical care literature. Crit Care Med 1998;26:591–598.<br />
106. Holmes J, House A. Psychiatric illness predicts poor<br />
outcome after surgery for hip fracture: a prospective<br />
cohort study. Psychol Med 2000;30:921–929.<br />
107. Dolan MM, Hawkes WG, Zimmerman SI, et al. Delirium<br />
on hospital admission in aged hip fracture patients: prediction<br />
of mortality and 2-year functional outcomes. J Gerontol<br />
A Biol Sci Med Sci 2000;55:M527–M534.<br />
108. Inouye SK, Schlesinger MJ, Lydon TJ. Delirium: a symptom<br />
of how hospital care is failing older persons and a window<br />
to improve quality of hospital care. Am J Med 1999;106:<br />
565–573.<br />
109. Millar K, Asbury AJ, Murray GD. Pre-existing cognitive<br />
impairment as a factor influencing outcome after cardiac<br />
surgery. Br J Anaesth 2001;86:63–67.<br />
110. Dyer CB, Ashton CM, Teasdale TA. Postoperative delirium.<br />
A review of 80 primary data-collection studies. Arch<br />
Intern Med 1995;155:461–465.<br />
111. Ni Chonchubhair A, Valacio R, Kelly J, O’Keefe S. Use of<br />
the abbreviated mental test to detect postoperative delirium<br />
in elderly people. Br J Anaesth 1995;75:481–482.<br />
112. Kaneko T, Takahashi S, Naka T, Hirooka Y, Inoue Y,<br />
Kaibara N. Postoperative delirium following gastrointestinal<br />
surgery in elderly patients. Surg Today 1997;27:<br />
107–111.<br />
113. Gustafson Y, Berggren D, Brannstrom B, et al. Acute confusional<br />
states in elderly patients treated for femoral neck<br />
fracture. J Am Geriatr Soc 1988;36:525–530.<br />
114. McDowell I, Kristjansson B, Hill GB, Hebert R. Community<br />
screening for dementia: the Mini Mental State Exam<br />
(MMSE) and Modified Mini-Mental State Exam (3MS)<br />
compared. J Clin Epidemiol 1997;50:377–383.<br />
115. Folstein MF, Folstein SE, McHugh PR. “Mini-mental<br />
state.” A practical method for grading the cognitive<br />
state of patients for the clinician. J Psychiatr Res 1975;12:<br />
189–198.<br />
116. Berggren D, Gustafson Y, Eriksson B, et al. Postoperative<br />
confusion after anesthesia in elderly patients with femoral<br />
neck fractures. Anesth Analg 1987;66:497–504.<br />
117. Williams-Russo P, Urquhart BL, Sharrock NE, Charlson<br />
ME. Post-operative delirium: predictors and prognosis in<br />
elderly orthopedic patients [see comments]. J Am Geriatr<br />
Soc 1992;40:759–767.<br />
118. de Graeff A, de Leeuw JR, Ros WJ, Hordijk GJ, Blijham<br />
GH, Winnubst JA. Pretreatment factors predicting quality<br />
of life after treatment for head and neck cancer. Head<br />
Neck 2000;22:398–407.<br />
119. Lyness JM, Noel TK, Cox C, King DA, Conwell Y, Caine<br />
ED. Screening for depression in elderly primary care<br />
patients. A comparison of the Center for Epidemiologic
88 C.J. Jankowski and D.J. Cook<br />
Studies-Depression Scale and the <strong>Geriatric</strong> Depression<br />
Scale. Arch Intern Med 1997;157:449–454.<br />
120. Roca R. Psychosocial aspects of surgical care in the elderly<br />
patient. Surg Clin North Am 1994;74:223–243.<br />
121. Bradley EH, Bogardus ST Jr, van Doorn C, Williams CS,<br />
Cherlin E, Inouye SK. Goals in geriatric assessment: are<br />
we measuring the right outcomes? Gerontologist 2000;<br />
40:191–196.<br />
122. Heijmeriks JA, Pourrier S, Dassen P, Prenger K, Wellens HJ.<br />
Comparison of quality of life after coronary and/or valvular<br />
cardiac surgery in patients > or =75 years of age with<br />
younger patients. Am J Cardiol 1999;83:1129–1132, A9.<br />
123. Katz S. Assessing self-maintenance: activities of daily<br />
living, mobility, and instrumental activities of daily living.<br />
J Am Geriatr Soc 1983;31:721–727.<br />
124. Turnbull JM, Buck C. <strong>The</strong> value of preoperative screening<br />
investigations in otherwise healthy individuals. Arch Intern<br />
Med 1987;147:1101–1105.<br />
125. Perez A, Planell J, Bacardaz C, et al. Value of routine preoperative<br />
tests: a multicentre study in four general hospitals.<br />
Br J Anaesth 1995;74:250–256.<br />
126. Kaplan EB, Sheiner LB, Boeckmann AJ, et al. <strong>The</strong> usefulness<br />
of preoperative laboratory screening. JAMA 1985;<br />
253:3576–3581.<br />
127. Narr BJ, Warner ME, Schroeder DR, Warner MA. Outcomes<br />
of patients with no laboratory assessment before<br />
anesthesia and a surgical procedure. Mayo Clin Proc 1997;<br />
72:505–509.<br />
128. Seymour DG, Pringle R, Shaw JW. <strong>The</strong> role of the routine<br />
pre-operative chest X-ray in the elderly general surgical<br />
patient. Postgrad Med J 1982;58:741–745.<br />
129. Seymour DG, Pringle R, MacLennan WJ. <strong>The</strong> role of<br />
the routine pre-operative electrocardiogram in the elderly<br />
surgical patient. Age Ageing 1983;12:97–104.<br />
130. Sewell JM, Spooner LL, Dixon AK, Rubenstein D.<br />
Screening investigations in the elderly. Age Ageing 1981;<br />
10:165–168.<br />
131. Sanders DP, McKinney FW, Harris WH. Clinical evaluation<br />
and cost effectiveness of preoperative laboratory<br />
assessment on patients undergoing total hip arthroplasty.<br />
Orthopedics 1989;12:1449–1453.<br />
132. Grimes CJ, Younathan MT, Lee WC. <strong>The</strong> effect of preoperative<br />
total parenteral nutrition on surgery outcomes.<br />
J Am Diet Assoc 1987;87:1202–1206.<br />
133. Gibbs J, Cull W, Henderson W, Daley J, Hur K, Khuri SF.<br />
Preoperative serum albumin level as a predictor of operative<br />
mortality and morbidity: results from the National VA<br />
Surgical Risk Study. Arch Surg 1999;134:36–42.<br />
134. Baker JP, Detsky AS, Wesson DE, et al. Nutritional assessment:<br />
a comparison of clinical judgement and objective<br />
measurements. N Engl J Med 1982;306:969–972.<br />
135. Covinsky KE, Martin GE, Beyth RJ, Justice AC, Sehgal<br />
AR, Landefeld CS. <strong>The</strong> relationship between clinical<br />
assessments of nutritional status and adverse outcomes in<br />
older hospitalized medical patients. J Am Geriatr Soc 1999;<br />
47:532–538.<br />
136. Mazolewski P, Turner JF, Baker M, Kurtz T, Little AG. <strong>The</strong><br />
impact of nutritional status on the outcome of lung volume<br />
reduction surgery: a prospective study. Chest 1999;116:<br />
693–696.<br />
137. Cohendy R, Gros T, Arnaud-Battandier F, Tran G, Plaze<br />
JM, Eledjam J. Preoperative nutritional evaluation of<br />
elderly patients: the Mini Nutritional Assessment as a<br />
practical tool. Clin Nutr 1999;18:345–348.<br />
138. McClave SA, Snider HL, Spain DA. Preoperative issues in<br />
clinical nutrition. Chest 1999;115:64S–70S.<br />
139. Moore AA, Siu AL. Screening for common problems in<br />
ambulatory elderly: clinical confirmation of a screening<br />
instrument. Am J Med 1996;100:438–443.<br />
140. Schein OD, Katz J, Bass EB, et al. <strong>The</strong> value of routine<br />
preoperative medical testing before cataract surgery. Study<br />
of Medical Testing for Cataract Surgery. N Engl J Med<br />
2000;342:168–175.<br />
141. Dzankic S, Pastor D, Gonzalez C, Leung JM. <strong>The</strong> prevalence<br />
and predictive value of abnormal preoperative laboratory<br />
tests in elderly surgical patients. Anesth Analg<br />
2001;93:301–308.<br />
142. Berlauk JF, Abrams JH, Gilmour IJ, O’Connor SR, Knighton<br />
DR, Cerra FB. Preoperative optimization of cardiovascular<br />
hemodynamics improves outcome in peripheral<br />
vascular surgery. A prospective, randomized clinical trial.<br />
Ann Surg 1991;214:289–297;discussion 298–299.<br />
143. Leppo JA. Preoperative cardiac risk assessment for noncardiac<br />
surgery. Am J Cardiol 1995;75:42D–51D.<br />
144. Roubenoff R, Roubenoff RA, Preto J, Balke CW. Malnutrition<br />
among hospitalized patients. A problem of physician<br />
awareness. Arch Intern Med 1987;147:1462–1465.<br />
145. Del Guercio LR, Cohn JD. Monitoring operative risk in<br />
the elderly. JAMA 1980;243:1350–1355.<br />
146. Smith MS, Muir H, Hall R. Perioperative management<br />
of drug therapy, clinical considerations. Drugs 1996;51:<br />
238–259.<br />
147. Zaugg M, Tagliente T, Lucchinetti E, et al. Beneficial<br />
effects from beta-adrenergic blockade in elderly patients<br />
undergoing noncardiac surgery. <strong>Anesthesiology</strong> 1999;91:<br />
1674–1686.<br />
148. Yeager RA, Moneta GL, Edwards JM, Taylor LMJ, McConnell<br />
DB, Porter JM. Reducing perioperative myocardial<br />
infarction following vascular surgery: the potential role of<br />
beta-blockade. Arch Surg 1995;130:869–873.<br />
149. Bisson A, Stern M, Caubarrere I. Preparation of high-risk<br />
patients for major thoracic surgery. Chest Surg Clin North<br />
Am 1998;8:541–555, viii.<br />
150. Debigare R, Maltais F, Whittom F, Deslauriers J, LeBlanc<br />
P. Feasibility and efficacy of home exercise training before<br />
lung volume reduction. J Cardiopulm Rehabil 1999;19:<br />
235–241.<br />
151. Arthur HM, Daniels C, McKelvie R, Hirsh J, Rush B.<br />
Effect of a preoperative intervention on preoperative and<br />
postoperative outcomes in low-risk patients awaiting elective<br />
coronary artery bypass graft surgery. A randomized,<br />
controlled trial. Ann Intern Med 2000;133:253–262.<br />
152. Fisher DA, Trimble S, Clapp B, Dorsett K. Effect of a<br />
patient management system on outcomes of total hip and<br />
knee arthroplasty. Clin Orthop 1997:155–160.<br />
153. Roy RC. Choosing general versus regional anesthesia for<br />
the elderly. Anesthesiol Clin North Am 2000;18:91–104,<br />
vii.<br />
154. McLaren AD, Stockwell MC, Reid VT. Anaesthetic techniques<br />
for surgical correction of fractured neck of femur.
6. Research Priorities in <strong>Geriatric</strong> <strong>Anesthesiology</strong> 89<br />
A comparative study of spinal and general anaesthesia in<br />
the elderly. Anaesthesia 1978;33:10–14.<br />
155. Hole A, Terjesen T, Breivik H. Epidural versus general<br />
anaesthesia for total hip arthroplasty in elderly patients.<br />
Acta Anaesthesiol Scand 1980;24:279–287.<br />
156. Nielson WR, Gelb AW, Casey JE, Penny FJ, Merchant RN,<br />
Manninen PH. Long-term cognitive and social se -<br />
quelae of general versus regional anesthesia during<br />
arthroplasty in the elderly. <strong>Anesthesiology</strong> 1990;73:1103–<br />
1109.<br />
157. Davis FM, Woolner DF, Frampton C, et al. Prospective,<br />
multi-centre trial of mortality following general or spinal<br />
anaesthesia for hip fracture surgery in the elderly. Br J<br />
Anaesth 1987;59:1080–1088.<br />
158. McKenzie PJ, Wishart HY, Dewar KM, Gray I, Smith G.<br />
Comparison of the effects of spinal anaesthesia and general<br />
anaesthesia on postoperative oxygenation and perioperative<br />
mortality. Br J Anaesth 1980;52:49–54.<br />
159. McKenzie PJ, Wishart HY, Gray I, Smith G. Effects of<br />
anaesthetic technique on deep vein thrombosis. A comparison<br />
of subarachnoid and general anaesthesia. Br J<br />
Anaesth 1985;57:853–857.<br />
160. Hendolin H, Mattila MA, Poikolainen E. <strong>The</strong> effect of<br />
lumbar epidural analgesia on the development of deep<br />
vein thrombosis of the legs after open prostatectomy. Acta<br />
Chir Scand 1981;147:425–429.<br />
161. White PF. Anesthetic techniques for the elderly outpatient.<br />
Int Anesthesiol Clin 1988;26:105–111.<br />
162. Valentin N, Lomholt B, Jensen JS, Hejgaard N, Kreiner S.<br />
Spinal or general anaesthesia for surgery of the fractured<br />
hip? A prospective study of mortality in 578 patients. Br J<br />
Anaesth 1986;58:284–291.<br />
163. Sorenson RM, Pace NL. Anesthetic techniques during surgical<br />
repair of femoral neck fractures. A meta-analysis.<br />
<strong>Anesthesiology</strong> 1992;77:1095–1104.<br />
164. Urwin SC, Parker MJ, Griffiths R. General versus regional<br />
anaesthesia for hip fracture surgery: a meta-analysis of<br />
randomized trials. Br J Anaesth 2000;84:450–455.<br />
165. Gilbert TB, Hawkes WG, Hebel JR, et al. Spinal anesthesia<br />
versus general anesthesia for hip fracture repair: a longitudinal<br />
observation of 741 elderly patients during 2-year<br />
follow-up. Am J Orthop 2000;29:25–35.<br />
166. Sutcliffe AJ, Parker M. Mortality after spinal and general<br />
anaesthesia for surgical fixation of hip fractures. Anaesthesia<br />
1994;49:237–240.<br />
167. O’Hara DA, Duff A, Berlin JA, et al. <strong>The</strong> effect of anesthetic<br />
technique on postoperative outcomes in hip fracture<br />
repair. <strong>Anesthesiology</strong> 2000;92:947–957.<br />
168. Rodgers A, Walker N, Schug S, et al. Reduction of postoperative<br />
mortality and morbidity with epidural or spinal<br />
anaesthesia: results from overview of randomised trials.<br />
BMJ 2000;321:1493.<br />
169. Riis J, Lomholt B, Haxholdt O, et al. Immediate and longterm<br />
mental recovery from general versus epidural anesthesia<br />
in elderly patients. Acta Anaesthesiol Scand 1983;<br />
27:44–49.<br />
170. Bigler D, Adelhoj B, Petring OU, Pederson NO, Busch P,<br />
Kalhke P. Mental function and morbidity after acute hip<br />
surgery during spinal and general anaesthesia. Anaesthesia<br />
1985;40:672–676.<br />
171. Ghoneim MM, Hinrichs JV, O’Hara MW, et al. Comparison<br />
of psychologic and cognitive functions after general or<br />
regional anesthesia. <strong>Anesthesiology</strong> 1988;69:507–515.<br />
172. Norris EJ, Beattie C, Perler BA, et al. Double-masked randomized<br />
trial comparing alternate combinations of intraoperative<br />
anesthesia and postoperative analgesia in abdominal<br />
aortic surgery. <strong>Anesthesiology</strong> 2001;95:1054–1067.<br />
173. Yeager MP, Glass DD, Neff RK, Brinck-Johnsen T. Epidural<br />
anesthesia and analgesia in high-risk surgical patients.<br />
<strong>Anesthesiology</strong> 1987;66:729–736.<br />
174. Chung F, Meier R, Lautenschlager E, Carmichael FJ,<br />
Chung A. General or spinal anesthesia: which is better in<br />
the elderly? <strong>Anesthesiology</strong> 1987;67:422–427.<br />
175. Asbjorn J, Jakobsen BW, Pilegaard HK, Blom L,<br />
Ostergaard A, Brandt MR. Mental function in elderly<br />
men after surgery during epidural analgesia. Acta<br />
Anaesthesiol Scand 1989;33:369–373.<br />
176. Edwards ND, Callaghan LC, White T, Reilly CS. Perioperative<br />
myocardial ischaemia in patients undergoing transurethral<br />
surgery: a pilot study comparing general with spinal<br />
anaesthesia. Br J Anaesth 1995;74:368–372.<br />
177. Bode RH, Lewis KP, Zarich SW, et al. Cardiac outcome<br />
after peripheral vascular surgery. Comparison of general<br />
and regional anesthesia. <strong>Anesthesiology</strong> 1996;84:3–13.<br />
178. Christopherson R, Beattie C, Frank SM, et al. Perioperative<br />
morbidity in patients randomized to epidural or<br />
general anesthesia for lower extremity vascular surgery.<br />
Perioperative Ischemia Randomized <strong>Anesthesia</strong> Trial<br />
Study Group. <strong>Anesthesiology</strong> 1993;79:422–434.<br />
179. Corson JD, Chang BB, Shah DM, Leather RP, DeLeo BM,<br />
Karmody AM. <strong>The</strong> influence of anesthetic choice on<br />
carotid endarterectomy outcome. Arch Surg 1987;122:<br />
807–812.<br />
180. Papavasiliou AK, Magnadottir HB, Gonda T, Franz D,<br />
Harbaugh RE. Clinical outcomes after carotid endarterectomy:<br />
comparison of the use of regional and general<br />
anesthetics. J Neurosurg 2000;92:291–296.<br />
181. Fiorani P, Sbarigia E, Speziale F, et al. General anaesthesia<br />
versus cervical block and perioperative complications in<br />
carotid artery surgery. Eur J Vasc Endovasc Surg 1997;<br />
13:37–42.<br />
182. Bowyer MW, Zierold D, Loftus JP, Egan JC, Inglis KJ,<br />
Halow KD. Carotid endarterectomy: a comparison of<br />
regional versus general anesthesia in 500 operations. Ann<br />
Vasc Surg 2000;14:145–151.<br />
183. Ferguson GG, Eliasziw M, Barr HW, et al. <strong>The</strong> North<br />
American Symptomatic Carotid Endarterectomy Trial:<br />
surgical results in 1415 patients [see comments]. Stroke<br />
1999;30:1751–1758.<br />
184. Slogoff S, Reul GJ, Keats AS, et al. Role of perfusion pressure<br />
and flow in major organ dysfunction after cardiopulmonary<br />
bypass. Ann Thorac Surg 1990;50:911–918.<br />
185. Wong BI, McLean RF, Naylor CD, et al. Centralnervous-system<br />
dysfunction after warm or hypothermic<br />
cardiopulmonary bypass. Lancet 1992;339:1383–1384.<br />
186. Gold JP, Charlson ME, Williams-Russo P, et al. Improvement<br />
of outcomes after coronary artery bypass. A randomized<br />
trial comparing intraoperative high versus low mean<br />
arterial pressure. J Thorac Cardiovasc Surg 1995;110:<br />
1302–1311; discussion 1311–1314.
90 C.J. Jankowski and D.J. Cook<br />
187. Roach GW, Kanchuger M, Mangano CM, et al. Adverse<br />
cerebral outcomes after coronary bypass surgery.<br />
Multicenter Study of Perioperative Ischemia Research<br />
Group and the Ischemia Research and Education Foundation<br />
Investigators. N Engl J Med 1996;335:1857–1863.<br />
188. Cook DJ. Neurologic effects. In: Gravlee GP, Davis RF,<br />
Kurusz M, Utley JR, eds. Cardiopulmonary Bypass:<br />
Principles and Practice. 2nd ed. Philadelphia: Lippincott<br />
Williams & Wilkins; 2000:403–431.<br />
189. Frank SM, Beattie C, Christopherson R, et al. Unintentional<br />
hypothermia is associated with postoperative myocardial<br />
ischemia. <strong>The</strong> Perioperative Ischemia Randomized<br />
<strong>Anesthesia</strong> Trial Study Group. <strong>Anesthesiology</strong> 1993;78:<br />
468–476.<br />
190. Frank SM, El-Rahmany HK, Cattaneo CG, Barnes RA.<br />
Predictors of hypothermia during spinal anesthesia.<br />
<strong>Anesthesiology</strong> 2000;92:1330–1334.<br />
191. Frank SM, Fleisher LA, Breslow MJ, et al. Perioperative<br />
maintenance of normothermia reduces the incidence of<br />
morbid cardiac events. A randomized clinical trial. JAMA<br />
1997;277:1127–1134.<br />
192. Frank SM, Fleisher LA, Olson KF, et al. Multivariate<br />
determinants of early postoperative oxygen consumption<br />
in elderly patients. Effects of shivering, body temperature,<br />
and gender. <strong>Anesthesiology</strong> 1995;83:241–249.<br />
193. Frank SM, Higgins MS, Breslow MJ, et al. <strong>The</strong> catecholamine,<br />
cortisol, and hemodynamic responses to mild<br />
perioperative hypothermia. A randomized clinical trial.<br />
<strong>Anesthesiology</strong> 1995;82:83–93.<br />
194. Mangano DT, Layug EL, Wallace A, Tateo I. Effect of atenolol<br />
on mortality and cardiovascular morbidity after noncardiac<br />
surgery. Multicenter Study of Perioperative Ischemia<br />
Research Group. N Engl J Med 1996;335:1713–1720.<br />
195. Poldermans D, Boersma E, Bax JJ, et al. <strong>The</strong> effect of<br />
bisoprolol on perioperative mortality and myocardial<br />
infarction in high-risk patients undergoing vascular surgery.<br />
Dutch Echocardiographic Cardiac Risk Evaluation Applying<br />
Stress Echocardiography Study Group. N Engl J Med<br />
1999;341:1789–1794.<br />
196. Nishina K, Mikawa K, Uesugi T, et al. Efficacy of clonidine<br />
for prevention of perioperative myocardial ischemia: a<br />
critical appraisal and meta-analysis of the literature. <strong>Anesthesiology</strong><br />
2002;96:323–329.<br />
197. van den Berghe G, Wouters P, Weekers F, et al. Intensive<br />
insulin therapy in the critically ill patients. N Engl J Med<br />
2001;345:1359–1367.<br />
198. Cohen MM, Duncan PG, Tweed WA, et al. <strong>The</strong> Canadian<br />
four-centre study of anaesthetic outcomes: I. Description<br />
of methods and populations. Can J Anaesth 1992;39:<br />
420–429.<br />
199. Rao TL, Jacobs KH, El-Etr AA. Reinfarction following<br />
anesthesia in patients with myocardial infarction. <strong>Anesthesiology</strong><br />
1983;59:499–505.<br />
200. O’Keeffe ST, Ni Chonchubhair A. Postoperative delirium<br />
in the elderly. Br J Anaesth 1994;73:673–687.<br />
201. Seymour DG, Vaz FG. A prospective study of elderly<br />
general surgical patients: II. Post-operative complications.<br />
Age Ageing 1989;18:316–326.<br />
202. Moller JT, Johannessen NW, Espersen K, et al. Randomized<br />
evaluation of pulse oximetry in 20,802 patients: II.<br />
Perioperative events and postoperative complications.<br />
<strong>Anesthesiology</strong> 1993;78:445–453.<br />
203. Moller JT, Svennild I, Johannessen NW, et al. Perioperative<br />
monitoring with pulse oximetry and late postoperative<br />
cognitive dysfunction. Br J Anaesth 1993;71:340–347.<br />
204. Pontoppidan H, Beecher HK. Progressive loss of protective<br />
reflexes in the airway with the advance of age. JAMA<br />
1960;174:2209–2213.<br />
205. Pedersen T, Viby-Mogensen J, Ringsted C. Anaesthetic<br />
practice and postoperative pulmonary complications. Acta<br />
Anaesthesiol Scand 1992;36:812–818.<br />
206. Bailey PL, Pace NL, Ashburn MA, Moll JW, East KA,<br />
Stanley TH. Frequent hypoxemia and apnea after seda -<br />
tion with midazolam and fentanyl. <strong>Anesthesiology</strong> 1990;73:<br />
826–830.<br />
207. Hogue CW Jr, Lappas GD, Creswell LL, et al. Swallowing<br />
dysfunction after cardiac operations. Associated adverse<br />
outcomes and risk factors including intraoperative transesophageal<br />
echocardiography. J Thorac Cardiovasc Surg<br />
1995;110:517–522.<br />
208. Mitchell CK, Smoger SH, Pfeifer MP, et al. Multivariate<br />
analysis of factors associated with postoperative pulmonary<br />
complications following general elective surgery.<br />
Arch Surg 1998;133:194–198.<br />
209. Warner MA, Warner ME, Weber JG. Clinical significance<br />
of pulmonary aspiration during the perioperative period.<br />
<strong>Anesthesiology</strong> 1993;78:56–62.<br />
210. Roberts JR, Shyr Y, Christian KR, Drinkwater D, Merrill<br />
W. Preemptive gastrointestinal tract management reduces<br />
aspiration and respiratory failure after thoracic operations.<br />
J Thorac Cardiovasc Surg 2000;119:449–452.<br />
211. Breslow MJ, Parker SD, Frank SM, et al. Determinants of<br />
catecholamine and cortisol responses to lower extremity<br />
revascularization. <strong>The</strong> PIRAT Study Group. <strong>Anesthesiology</strong><br />
1993;79:1202–1209.<br />
212. Rem J, Nielsen OS, Brandt MR, Kehlet H. Release mechanisms<br />
of postoperative changes in various acute phase<br />
proteins and immunoglobulins. Acta Chir Scand Suppl<br />
1980;502:51–56.<br />
213. Kilickan L, Toker K. <strong>The</strong> effects of preemptive intravenous<br />
versus preemptive epidural morphine on postoperative<br />
analgesia and surgical stress response after orthopaedic<br />
procedures. Minerva Anestesiol 2000;66:649–655.<br />
214. Schulze S, Schierbeck J, Sparso BH, Bisgaard M, Kehlet H.<br />
Influence of neural blockade and indomethacin on leucocyte,<br />
temperature, and acute-phase protein response to<br />
surgery. Acta Chir Scand 1987;153:255–259.<br />
215. Klasen JA, Opitz SA, Melzer C, Thiel A, Hempelmann G.<br />
Intraarticular, epidural, and intravenous analgesia after<br />
total knee arthroplasty. Acta Anaesthesiol Scand 1999;43:<br />
1021–1026.<br />
216. Schulze S, Sommer P, Bigler D, et al. Effect of combined<br />
prednisolone, epidural analgesia, and indomethacin on the<br />
systemic response after colonic surgery. Arch Surg 1992;<br />
127:325–331.<br />
217. Rem J, Brandt MR, Kehlet H. Prevention of postoperative<br />
lymphopenia and granulocytosis by epidural analgesia.<br />
Lancet 1980;1:283–284.<br />
218. Hjortso NC, Andersen T, Frosig F, Neumann P, Rogon E,<br />
Kehlet H. Failure of epidural analgesia to modify postop-
6. Research Priorities in <strong>Geriatric</strong> <strong>Anesthesiology</strong> 91<br />
erative depression of delayed hypersensitivity. Acta Anaesthesiol<br />
Scand 1984;28:128–131.<br />
219. Rutberg H, Hakanson E, Anderberg B, Jorfeldt L,<br />
Martensson J, Schildt B. Effects of the extradural administration<br />
of morphine, or bupivacaine, on the endocrine<br />
response to upper abdominal surgery. Br J Anaesth 1984;<br />
56:233–237.<br />
220. Liu S, Carpenter RL, Neal JM. Epidural anesthesia and<br />
analgesia. <strong>The</strong>ir role in postoperative outcome. <strong>Anesthesiology</strong><br />
1995;82:1474–1506.<br />
221. Tuman KJ, McCarthy RJ, March RJ, DeLaria GA, Patel<br />
RV, Ivankovich AD. Effects of epidural anesthesia and<br />
analgesia on coagulation and outcome after major vascular<br />
surgery. Anesth Analg 1991;73:696–704.<br />
222. Giesecke K, Klingstedt C, Ljungqvist O, Hagenfeldt L.<br />
<strong>The</strong> modifying influence of anaesthesia on postoper -<br />
ative protein catabolism. Br J Anaesth 1994;72:697–<br />
699.<br />
223. Heindorff H, Schulze S, Mogensen T, Almdal T, Kehlet H,<br />
Vilstrup H. Hormonal and neural blockade prevents the<br />
postoperative increase in amino acid clearance and urea<br />
synthesis. Surgery 1992;111:543–550.<br />
224. Carli F, Halliday D. Continuous epidural blockade arrests<br />
the postoperative decrease in muscle protein fractional<br />
synthetic rate in surgical patients. <strong>Anesthesiology</strong> 1997;<br />
86:1033–1040.<br />
225. Wasylak TJ, Abbott FV, English MJ, Jeans ME. Reduction<br />
of postoperative morbidity following patient-controlled<br />
morphine. Can J Anaesth 1990;37:726–731.<br />
226. Petros JG, Alameddine F, Testa E, Rimm EB, Robillard RJ.<br />
Patient-controlled analgesia and postoperative urinary<br />
retention after hysterectomy for benign disease. J Am Coll<br />
Surg 1994;179:663–667.<br />
227. Petros JG, Mallen JK, Howe K, Rimm EB, Robillard RJ.<br />
Patient-controlled analgesia and postoperative urinary<br />
retention after open appendectomy. Surg Gynecol Obstet<br />
1993;177:172–175.<br />
228. Carpenter RL, Abram SE, Bromage PR, Rauck RL. Consensus<br />
statement on acute pain management. Reg Anesth<br />
1996;21:152–156.<br />
229. Carpenter RL. Gastrointestinal benefits of regional<br />
anesthesia/analgesia. Reg Anesth 1996;21:13–17.<br />
230. Kumar A, Bose S, Bhattacharya A, Tandon OP, Kundra P.<br />
Oral clonidine premedication for elderly patients undergoing<br />
intraocular surgery. Acta Anaesthesiol Scand 1992;<br />
36:159–164.<br />
231. Singelyn FJ, Gouverneur JM. Extended “three-in-one”<br />
block after total knee arthroplasty: continuous versus<br />
patient-controlled techniques. Anesth Analg 2000;91:176–<br />
180.<br />
232. De Kock MF, Pichon G, Scholtes JL. Intraoperative clonidine<br />
enhances postoperative morphine patient-controlled<br />
analgesia. Can J Anaesth 1992;39:537–544.<br />
233. Wong HY, Carpenter RL, Kopacz DJ, et al. A randomized,<br />
double-blind evaluation of ketorolac tromethamine for<br />
postoperative analgesia in ambulatory surgery patients.<br />
<strong>Anesthesiology</strong> 1993;78:6–14.<br />
234. Milligan KR, Convery PN, Weir P, Quinn P, Connolly D.<br />
<strong>The</strong> efficacy and safety of epidural infusions of levobupivacaine<br />
with and without clonidine for postoperative pain<br />
relief in patients undergoing total hip replacement. Anesth<br />
Analg 2000;91:393–397.<br />
235. Capdevila X, Barthelet Y, Biboulet P, Ryckwaert Y, Rubenovitch<br />
J, d’Athis F. Effects of perioperative analgesic<br />
technique on the surgical outcome and duration of<br />
rehabilitation after major knee surgery. <strong>Anesthesiology</strong><br />
1999;91:8–15.<br />
236. Mahoney OM, Noble PC, Davidson J, Tullos HS. <strong>The</strong> effect<br />
of continuous epidural analgesia on postoperative pain,<br />
rehabilitation, and duration of hospitalization in total knee<br />
arthroplasty. Clin Orthop 1990:30–37.<br />
237. Williams-Russo P, Sharrock NE, Haas SB, et al. Randomized<br />
trial of epidural versus general anesthesia: outcomes<br />
after primary total knee replacement. Clin Orthop 1996:<br />
199–208.<br />
238. Cullen DJ, Sweitzer BJ, Bates DW, Burdick E, Edmondson<br />
A, Leape LL. Preventable adverse drug events in hospitalized<br />
patients: a comparative study of intensive care and<br />
general care units. Crit Care Med 1997;25:1289–1297.<br />
239. Bates DW, Cullen DJ, Laird N, et al. Incidence of adverse<br />
drug events and potential adverse drug events. Implications<br />
for prevention. ADE Prevention Study Group. JAMA<br />
1995;274:29–34.<br />
240. Parikh SS, Chung F. Postoperative delirium in the elderly.<br />
Anesth Analg 1995;80:1223–1232.<br />
241. Ritchie K, Polge C, de Roquefeuil G, Djakovic M, Ledesert<br />
B. Impact of anesthesia on the cognitive functioning of the<br />
elderly. Int Psychogeriatr 1997;9:309–326.<br />
242. Grichnik KP, Ijsselmuiden AJ, D’Amico TA, et al.<br />
Cognitive decline after major noncardiac operations: a<br />
preliminary prospective study. Ann Thorac Surg 1999;68:<br />
1786–1791.<br />
243. Billig N, Stockton P, Cohen-Mansfield J. Cognitive and<br />
affective changes after cataract surgery in an elderly population.<br />
Am J Geriatr Psychiatry 1995;4:29–38.<br />
244. Goldstein MZ, Young BL, Fogel BS, Benedict RH. Occurrence<br />
and predictors of short-term mental and functional<br />
changes in older adults undergoing elective surgery under<br />
general anesthesia. Am J Geriatr Psychiatry 1998;6:<br />
42–52.<br />
245. Rogers MP, Liang MH, Daltroy LH, et al. Delirium after<br />
elective orthopedic surgery: risk factors and natural history.<br />
Int J Psychiatry Med 1989;19:109–121.<br />
246. Williams-Russo P, Sharrock NE, Mattis S, Szatrowski TP,<br />
Charlson ME. Cognitive effects after epidural vs general<br />
anesthesia in older adults. A randomized trial. JAMA<br />
1995;274:44–50.<br />
247. Moller JT, Cluitmans P, Rasmussen LS, et al. Long-term<br />
postoperative cognitive dysfunction in the elderly<br />
ISPOCD1 study. (ISPOCD investigators. International<br />
Study of Post-Operative Cognitive Dysfunction). Lancet<br />
1998;351:857–861.<br />
248. McKhann GM, Goldsborough MA, Borowicz LM Jr, et al.<br />
Cognitive outcome after coronary artery bypass: a<br />
one-year prospective study. Ann Thorac Surg 1997;63:<br />
510–515.<br />
249. Newman MF, Kramer D, Croughwell ND, et al. Differential<br />
age effects of mean arterial pressure and rewarming<br />
on cognitive dysfunction after cardiac surgery. Anesth<br />
Analg 1995;81:236–242.
92 C.J. Jankowski and D.J. Cook<br />
250. Selnes OA, Goldsborough MA, Borowicz LM, Enger C,<br />
Quaskey SA, McKhann GM. Determinants of cognitive<br />
change after coronary artery bypass surgery: a multifactorial<br />
problem. Ann Thorac Surg 1999;67:1669–1676.<br />
251. Chung FF, Chung A, Meier RH, Lautenschlaeger E, Seyone<br />
C. Comparison of perioperative mental function after<br />
general anaesthesia and spinal anaesthesia with intravenous<br />
sedation. Can J Anaesth 1989;36:382–387.<br />
252. Marcantonio ER, Juarez G, Goldman L, et al. <strong>The</strong> relationship<br />
of postoperative delirium with psychoactive medications.<br />
JAMA 1994;272:1518–1522.<br />
253. Herrick IA, Ganapathy S, Komar W, et al. Postoperative<br />
cognitive impairment in the elderly. Choice of patientcontrolled<br />
analgesic opioid. Anaesthesia 1996;51:356–<br />
360.<br />
254. Crul BJ, Hulstijn W, Burger IC. Influence of the type of<br />
anaesthesia on post-operative subjective physical wellbeing<br />
and mental function in elderly patients. Acta<br />
Anaesthesiol Scand 1992;36:615–620.<br />
255. Tune LE, Damlouji NF, Holland A, Gardner TJ, Folstein<br />
MF, Coyle JT. Association of postoperative delirium with<br />
raised serum levels of anticholinergic drugs. Lancet 1981;<br />
2:651–653.<br />
256. Brebner J, Hadley L. Experiences with physostigmine in<br />
the reversal of adverse post-anaesthetic effects. Can<br />
Anaesth Soc J 1976;23:574–581.<br />
257. Marcantonio ER, Goldman L, Orav EJ, Cook EF, Lee TH.<br />
<strong>The</strong> association of intraoperative factors with the development<br />
of postoperative delirium. Am J Med 1998;105:<br />
380–384.<br />
258. Dodds C, Allison J. Postoperative cognitive deficit in the<br />
elderly surgical patient. Br J Anaesth 1998;81:449–462.<br />
259. Inouye SK, Charpentier PA. Precipitating factors for delirium<br />
in hospitalized elderly persons. Predictive model and<br />
interrelationship with baseline vulnerability. JAMA 1996;<br />
275:852–857.<br />
260. Inouye SK. Delirium in hospitalized older patients: recognition<br />
and risk factors. J Geriatr Psychiatry Neurol 1998;<br />
11:118–125; discussion 157–158.<br />
261. Inouye SK. Delirium in hospitalized older patients. Clin<br />
Geriatr Med 1998;14:745–764.<br />
262. Lynch EP, Lazor MA, Gellis JE, Orav J, Goldman L,<br />
Marcantonio ER. <strong>The</strong> impact of postoperative pain on the<br />
development of postoperative delirium. Anesth Analg<br />
1998;86:781–785.<br />
263. Koenig HG, George LK, Stangl D, Tweed DL. Hospital<br />
stressors experienced by elderly medical inpatients: developing<br />
a Hospital Stress Index. Int J Psychiatry Med 1995;<br />
25:103–122.<br />
264. Inouye SK. Predisposing and precipitating factors for<br />
delirium in hospitalized older patients. Dement Geriatr<br />
Cogn Disord 1999;10:393–400.<br />
265. Inouye SK, Bogardus ST Jr, Charpentier PA, et al. A multicomponent<br />
intervention to prevent delirium in hospitalized<br />
older patients [see comments]. N Engl J Med 1999;<br />
340:669–676.<br />
266. Inouye SK, Rushing JT, Foreman MD, Palmer RM, Pompei<br />
P. Does delirium contribute to poor hospital outcomes? A<br />
three-site epidemiologic study. J Gen Intern Med 1998;<br />
13:234–242.<br />
267. Inouye SK, Viscoli CM, Horwitz RI, Hurst LD, Tinetti ME.<br />
A predictive model for delirium in hospitalized elderly<br />
medical patients based on admission characteristics. Ann<br />
Intern Med 1993;119:474–481.<br />
268. Goldstein MZ. Cognitive change after elective surgery in<br />
nondemented older adults. Am J Geriatr Psychiatry 1993;<br />
1:118–125.<br />
269. McDowell I, Newell C. Measuring Health: a Guide to<br />
Rating Scales and Questionnaires. 2nd ed. New York:<br />
Oxford University Press; 1996.<br />
270. Froehlich TE, Robison JT, Inouye SK. Screening for dementia<br />
in the outpatient setting: the time and change test [see<br />
comments]. J Am Geriatr Soc 1998;46:1506–1511.<br />
271. Kalisvaart KJ, de Jonghe JF, Bogaards MJ, et al. Haloperidol<br />
prophylaxis for elderly hip-surgery patients at risk for<br />
delirium: a randomized placebo-controlled study. J Am<br />
Geriatr Soc 2005;53:1658–1666.<br />
272. Freedman GM, Peruvemba R. <strong>Geriatric</strong> pain management.<br />
<strong>The</strong> anesthesiologist’s perspective. Anesthesiol Clin North<br />
Am 2000;18:123–141, vii.<br />
273. Parmelee PA, Katz IR, Lawton MP. <strong>The</strong> relation of pain<br />
to depression among institutionalized aged. J Gerontol<br />
1991;46:15–21.<br />
274. Farrell MJ, Gerontol M, Gibson SJ, Helme RD. <strong>The</strong> effect<br />
of medical status on the activity level of older pain clinic<br />
patients. J Am Geriatr Soc 1995;43:102–107.<br />
275. Sorkin BA, Rudy TE, Hanlon RB, Turk DC, Stieg RL.<br />
Chronic pain in old and young patients: differences appear<br />
less important than similarities. J Gerontol 1990;45:<br />
64–68.<br />
276. Cutler RB, Fishbain DA, Rosomoff RS, Rosomoff HL.<br />
Outcomes in treatment of pain in geriatric and younger<br />
age groups. Arch Phys Med Rehabil 1994;75:457–464.<br />
277. Lipman AG. Analgesic drugs for neuropathic and sympathetically<br />
maintained pain. Clin Geriatr Med 1996;12:<br />
501–515.<br />
278. Arner S, Meyerson BA. Lack of analgesic effect of opioids<br />
on neuropathic and idiopathic forms of pain. Pain 1988;<br />
33:11–23.<br />
279. Swerdlow M. Anticonvulsants in the therapy of neuralgic<br />
pain. Pain Clinic 1986;1:9–19.<br />
280. Stanton-Hicks M, Baron R, Boas R, et al. Complex regional<br />
pain syndromes: guidelines for therapy. Clin J Pain 1998;<br />
14:155–166.<br />
281. Max MB, Kishore-Kumar R, Schafer SC, et al. Efficacy of<br />
desipramine in painful diabetic neuropathy: a placebocontrolled<br />
trial. Pain 1991;45:3–9; discussion 1–2.<br />
282. Cutler RB, Fishbain DA, Lu Y, Rosomoff RS, Rosomoff<br />
HL. Prediction of pain center treatment outcome for<br />
geriatric chronic pain patients. Clin J Pain 1994;10:<br />
10–17.<br />
283. Carmichael JK. Treatment of herpes zoster and postherpeutic<br />
neuralgia. Am Fam Physician 1991;44:203–210.<br />
284. Watson CP, Evans RJ, Watt VR. Post-herpetic neuralgia<br />
and topical capsaicin. Pain 1988;33:333–340.<br />
285. Hwang SM, Kang YC, Lee YB, Yoon KB, Ahn SK, Choi<br />
EH. <strong>The</strong> effects of epidural blockade on the acute pain in<br />
herpes zoster. Arch Dermatol 1999;135:1359–1364.<br />
286. Chiarello SE. Tumescent infiltration of corticosteroids,<br />
lidocaine, and epinephrine into dermatomes of acute her-
6. Research Priorities in <strong>Geriatric</strong> <strong>Anesthesiology</strong> 93<br />
petic pain or postherpetic neuralgia. Arch Dermatol 1998;<br />
134:279–281.<br />
287. Alper BS, Lewis PR. Does treatment of acute herpes zoster<br />
prevent or shorten postherpetic neuralgia? J Fam Pract<br />
2000;49:255–264.<br />
288. Kost RG, Straus SE. Postherpetic neuralgia. Predicting<br />
and preventing risk. Arch Intern Med 1997;157:1166–<br />
1167.<br />
289. Weller TH. Varicella and herpes zoster. Changing concepts<br />
of the natural history, control, and importance of a not-sobenign<br />
virus. N Engl J Med 1983;309:1434–1440.<br />
290. Ragozzino MW, Melton LJ 3rd, Kurland LT, Chu CP, Perry<br />
HO. Population-based study of herpes zoster and its<br />
sequelae. Medicine (Baltimore) 1982;61:310–316.<br />
291. Donahue JG, Choo PW, Manson JE, Platt R. <strong>The</strong> in -<br />
cidence of herpes zoster. Arch Intern Med 1995;155:<br />
1605–1609.<br />
292. Choo PW, Galil K, Donahue JG, Walker AM, Spiegelman<br />
D, Platt R. Risk factors for postherpetic neuralgia. Arch<br />
Intern Med 1997;157:1217–1224.<br />
293. Galil K, Choo PW, Donahue JG, Platt R. <strong>The</strong> sequelae<br />
of herpes zoster. Arch Intern Med 1997;157:1209–<br />
1213.<br />
294. Miller AE. Selective decline in cellular immune response to<br />
varicella-zoster in the elderly. Neurology 1980;30:582–587.<br />
295. Berger R, Florent G, Just M. Decrease of the lymphoproliferative<br />
response to varicella-zoster virus antigen in the<br />
aged. Infect Immun 1981;32:24–27.<br />
296. Burke BL, Steele RW, Beard OW, Wood JS, Cain TD,<br />
Marmer DJ. Immune responses to varicella-zoster in the<br />
aged. Arch Intern Med 1982;142:291–293.<br />
297. Levin MJ, Murray M, Rotbart HA, Zerbe GO, White CJ,<br />
Hayward AR. Immune response of elderly individuals to<br />
a live attenuated varicella vaccine. J Infect Dis 1992;166:<br />
253–259.<br />
298. Oxman MN, Levin MJ, Johnson GR, et al. A vaccine to<br />
prevent herpes zoster and postherpetic neuralgia in older<br />
adults. N Engl J Med 2005;352:2271–2284.<br />
299. Byrd JC, McGrail LH, Hospenthal DR, Howard RS,<br />
Dow NA, Diehl LF. Herpes virus infections occur frequently<br />
following treatment with fludarabine: results of a<br />
prospective natural history study. Br J Haematol 1999;<br />
105:445–447.<br />
300. Sengstaken EA, King SA. <strong>The</strong> problems of pain and its<br />
detection among geriatric nursing home residents. J Am<br />
Geriatr Soc 1993;41:541–544.
Part II<br />
Cardinal Manifestations of Aging and Disease<br />
in the Elderly
7<br />
Alterations in Metabolic Functions<br />
and Electrolytes<br />
Michael C. Lewis<br />
Aging has been characterized as a comprehensive, progressive,<br />
and irreversible biologic process resulting in the<br />
maintenance of life but with a diminishing capability for<br />
adaptation. 1,2 In fact, it has been estimated that after the<br />
age of 30 years, organ systems lose approximately 1% of<br />
their function per annum. 3 Implied in this description are<br />
the concepts of increased biologic entropy, functional<br />
deterioration, loss of viability, and an augmented likelihood<br />
of death. 4<br />
<strong>The</strong> aging population is rapidly growing 5–7 and utilizes<br />
a growing proportion of medical resources, 8–10 including<br />
surgery. 11–14 However, because of factors such as decreased<br />
functional reserve, existing comorbidity, and polypharmacy,<br />
older patients have higher morbidity 15 and mortality,<br />
16 especially when the surgery is emergent. 17,18 <strong>The</strong>ir<br />
medical management is becoming one of the greatest<br />
challenges to anesthesiologists. Yet, despite this reality,<br />
little time is spent on formal training in geriatrics during<br />
anesthesia residency training. 19<br />
<strong>The</strong> Concept of Functional Reserve<br />
Organ function in the elderly is usually well maintained<br />
under basal conditions. One measure of “health” in the<br />
aged is their ability to tolerate increased physiologic<br />
loads. When an individual can maintain a steady state in<br />
the face of increased physiologic demand, they are said<br />
to demonstrate a good functional reserve. In contrast,<br />
when there is latent disease and diminished ability to<br />
maintain function in the face of stressors, there is said to<br />
be decreased functional reserve. Age leads to a gradual<br />
reduction in functional reserve (Figure 7-1). Consequently,<br />
when stress exceeds functional reserve, imbalance<br />
within systems will likely develop and result in a<br />
breakdown of homeostatic compensation.<br />
Aging per se is typified by a decreased performance of<br />
many biologic regulatory processes in the face of biologic<br />
stress. Because these regulatory mechanisms provide<br />
functional integration between cells and organ systems,<br />
growing old may be associated with a failure to maintain<br />
homeostatic functions. This impaired capability affects<br />
diverse regulatory systems uniquely in aged subjects and<br />
may at least partly explain the increased interindividual<br />
variability in functional reserve that occurs as people get<br />
older. <strong>The</strong> decline in functional reserve is inconsistent<br />
among individuals, with the variability in deterioration<br />
rooted within lifestyle choices, environmental factors,<br />
genetics, and the presence of age-related disease. A<br />
decline in functional reserve may precipitate a serious<br />
decline in performance when the elderly patient is<br />
exposed to stress such as those of surgery and anesthesia,<br />
and thereby increases the risk of age-related disease.<br />
Aims<br />
This chapter will function primarily as an introduction to<br />
the complex area of metabolic changes in the elderly. In<br />
addition, issues concerning the fluid and electrolyte status<br />
of the elderly patient will be touched upon. Within each<br />
of its sections, the impact of these changes on the anesthetic<br />
management of these patients will be examined,<br />
and the concept of reduced functional reserve and its<br />
consequences will be continually reemphasized.<br />
Basal Metabolic Rate<br />
Mitochondria, being the powerhouse of biologic processes,<br />
underlie all of the metabolic functions of the body.<br />
<strong>The</strong>se organelles provide the power that fuels metabolic<br />
functions.<br />
<strong>The</strong> energy required to maintain basic cellular functions<br />
is termed basal metabolic rate (BMR) and it is generally<br />
accepted that it decreases with advancing age. It decreases<br />
by approximately 1%–2% per decade from the ages of<br />
20–80 years, 20–22 and additive declines in BMR have been<br />
shown to decrease the rate of drug metabolism. 23<br />
97
98 M.C. Lewis<br />
Body Composition<br />
% Maximal organ function<br />
Maximal<br />
Basal<br />
Functional<br />
reserve<br />
Age (years)<br />
Figure 7-1. <strong>The</strong> functional reserve is the difference between<br />
basal function (solid line) and maximal function (broken line).<br />
Even in healthy elderly individuals, this functional reserve will<br />
be reduced. (Modified from Muravchick S. Geroanesthesia:<br />
Principles for Management of the Elderly Patient. St. Louis:<br />
Mosby-Year Book; 1997. Copyright © 1997 with permission<br />
from Elsevier.)<br />
This decreased BMR is associated with increased levels<br />
of circulating epinephrine 24,25 and reduced β-receptor<br />
sensitivity. 26 <strong>The</strong>se receptors are involved in sympathetically<br />
mediated thermogenesis, hence, the fact that the β-<br />
response becomes blunted has been used to explain a<br />
predisposition to obesity. 21 Such a tendency to obesity in<br />
the elderly may contribute to the observed increase in<br />
incidence of both Type 2 diabetes 27 and cardiac disease. 28<br />
Moreover, this diminution of β-receptor sensitivity in the<br />
elderly results in a decreased ability to cope with physiologic<br />
stressors.<br />
Impaired thermogenesis and reduced BMR predispose<br />
the elderly to more severe postoperative hypothermia<br />
and a protracted recovery from this phenomenon. 29 Slowness<br />
to recover from hypothermia is also partly attributable<br />
to the reduced amount of shivering compared with<br />
younger patients 30 with total body oxygen consumption<br />
increasing only about 38% in the elderly. 31 Such vulnerability<br />
to hypothermia increases the risk of adverse<br />
physiologic outcomes such as increased risk of wound<br />
infections 32 and myocardial ischemia. 33<br />
In summary, changes in BMR in the elderly are characterized<br />
by:<br />
• Gradual decline in BMR even allowing for changes in<br />
body composition<br />
• Increase in circulating catecholamines, together with<br />
decreased β-receptor sensitivity, increasing the predisposition<br />
to obesity<br />
• Impaired ability to protect against and recover from<br />
hypothermia exposing the geriatric patient to increased<br />
intra- and postoperative complications<br />
<strong>The</strong> changes in body structure with aging are typified by<br />
an increase in the percentage of body fat, 34 a loss of<br />
protein, 35 and intracellular dehydration. 36 <strong>The</strong>se changes<br />
in body composition have been shown to be even greater<br />
in women. 18<br />
Changes in Body Fat<br />
Age-related accumulation of body fat increases the deposition<br />
of lipid-soluble drugs including anesthetics. 37 Consequently,<br />
the larger concentration of these agents in fat<br />
tissue results in a longer time for redistribution and a<br />
slower elimination time thereby prolonging anesthetic<br />
effects. 38,39<br />
Loss of Protein<br />
<strong>The</strong>re is a significant loss of body protein with aging. 40<br />
<strong>The</strong> following section will describe the sources of this<br />
protein loss.<br />
Muscle Mass<br />
<strong>The</strong> majority of the age-related loss of body protein is<br />
accounted for by the up to 20% decrease of skeletal<br />
muscle mass 41 of unknown etiology 42 and is termed sarcopenia.<br />
43 This occurs even in the fit adult and is associated<br />
with a loss of strength. For a person in their second<br />
decade, muscle comprises up to 60% of the lean body<br />
mass, and yet at 70 years of age, this decreases to less than<br />
40%. Although the decrease in muscle tissue begins<br />
around the age of 50 years, it becomes more dramatic<br />
beyond the 60th year of life. 44 This decline can be partially<br />
reversed using resistance exercises. 45<br />
Despite this degree of muscle loss, there is no difference<br />
in sensitivity of the elderly to muscle relaxants. 46 <strong>The</strong><br />
pharmacokinetics of such agents are characterized by<br />
decreased elimination. <strong>The</strong> initial administration of such<br />
drugs may not have to be reduced, 47 but the total dose<br />
administered should be generally reduced. 48 However,<br />
because of decreased elimination, their effect should be<br />
carefully monitored using a component of neuromuscular<br />
function such as the train-of-four tests.<br />
Transport Proteins<br />
Intravenous anesthetic induction agents are transported<br />
through the body bound to plasma proteins. Any agent<br />
attached to such proteins is not capable of crossing biologic<br />
membranes to produce the desired drug effect. Conversely,<br />
the segment that remains free in plasma is able<br />
to cross these lipid membranes, including the blood–brain
7. Alterations in Metabolic Functions and Electrolytes 99<br />
barrier, and in the case of induction agents produces the<br />
preferred effect.<br />
Albumin<br />
This is the primary transport carrier 49 and is responsible<br />
for transporting most of the acidic drugs in the plasma.<br />
Its synthesis represents a major component of the proteins<br />
produced by the liver. Increasing age is associated<br />
with a slight decrease in the concentration of albumin 50<br />
by 0.54 g/L per decade. <strong>The</strong> decrease amounts to a total<br />
reduction in plasma albumin concentration of around<br />
10% in older people. 51 This reduction in albumin plasma<br />
level has been shown to reduce the unbound fraction of<br />
certain drugs. 52 On average, the unbound fraction of drugs<br />
increases by approximately 10%, paralleling the agerelated<br />
decrease in albumin. 18,53 <strong>The</strong>oretically, the net<br />
effect is that anesthetic drugs that bind to albumin, such<br />
as thiopental, should have their dose decreased. However,<br />
overall age-related effects on protein binding do not<br />
produce clinical differences. 54 Because of the polypharmacy<br />
often seen in the geriatric patient, concomitant diseases,<br />
and the reduced circulating albumin level, there<br />
may be a greater opportunity for displacement reactions<br />
between drugs.<br />
Renal failure has been associated with decreased levels<br />
of circulating albumin. 55 As a result, the pharmacokinetics<br />
of anesthetic agents can be altered. 56,57 However, those<br />
patients with global hypoproteinemia, not just decreased<br />
albumin, will have decreased binding of both acidic and<br />
basic drugs. 58<br />
A 20%–30% reduction in blood volume occurs by age 75<br />
with total body water (TBW), plasma volume and intracellular<br />
water content all decreasing. 60 Consequently,<br />
intravenous administration of an anesthetic drug will be<br />
distributed in a reduced blood volume producing a higher<br />
than expected initial plasma drug concentration. Such<br />
changes can have very important implications on the<br />
action of anesthetic agents. 61 For example, a patient who<br />
is relatively dehydrated and is given a bolus of an induction<br />
agent, will distribute this drug into a reduced circulating<br />
volume. Anesthetic and hemodynamic effects of<br />
the drug will be exaggerated. This resultant exaggerated<br />
pharmacologic effect could give the impression of an augmented<br />
sensitivity to the agent. Such changes in the distribution<br />
and half-life of a particular anesthetic agent will<br />
depend on its relative lipid and water solubility as well as<br />
the degree of protein binding.<br />
In summary, changes in body composition in the elderly<br />
are characterized by:<br />
• A decrease in protein content, mostly in the form of<br />
muscle loss, but also in carrier proteins<br />
• Adipose tissue comprising an increased proportion of<br />
body mass<br />
• A decrease in TBW, with this reduction manifest mostly<br />
in the intracellular component but somewhat in the<br />
extracellular compartment also<br />
Hepatic Function in the Elderly<br />
<strong>The</strong> effects of maturation on drug clearance by the liver<br />
have been examined extensively 62,63 and the contentious<br />
question of whether or not liver function is compromised<br />
in the aged has still not been clearly determined. As is<br />
the general pattern with most aging organs, the decline<br />
in function is gradual and minimal. Senescence is only<br />
experienced when the normal homeostatic mechanisms<br />
fail. Decline in biochemical functions are slow and negligible<br />
and are reflected in assays of liver function such as<br />
total bilirubin and liver enzymes. 64<br />
Alpha 1 Acid Glycoprotein<br />
Whereas acidic drugs are primarily bound to albumin,<br />
basic drugs tend to be bound to alpha 1 acid glycoprotein.<br />
Data suggest that this transport protein is either not<br />
affected by aging 59 or even slightly increased, 54 probably<br />
reflecting the age-associated increases in inflammatory<br />
disease. 11 <strong>The</strong> binding and consequent dosage of basic<br />
anesthetic drugs, such as lidocaine, is therefore unaffected<br />
by aging.<br />
Changes in Total Body Water<br />
Morphologic Changes<br />
Gross Changes<br />
<strong>The</strong> aging liver develops a classic gross anatomic<br />
appearance termed “brown atrophy.” 65,66 This discoloration<br />
is attributed to hepatocyte accumulation of the<br />
pigment lipofuscin, but it is not clear whether these morphologic<br />
changes are associated with alteration in<br />
function. 67,68<br />
Hepatic blood flow decreases with increasing age. 69–71<br />
Most of this reduction is associated with a 35% decrease in<br />
liver mass. 72–76 <strong>The</strong> reduction in hepatic blood flow is probably<br />
slightly greater than can be explained by the decrease<br />
in liver mass, 51 resulting in a 10% decrease in blood flow per<br />
unit mass of liver. 51 However, the large size of the aging<br />
liver provides a large measure of functional reserve therefore<br />
conserving its function relatively well. 51,54,55<br />
Microscopic Changes<br />
Age-related subcellular changes in the liver are slight. 26,77<br />
Hepatocyte volume increases, probably as a function of
100 M.C. Lewis<br />
intracellular swelling. 78 <strong>The</strong>re are some characteristic<br />
age-related organelle changes. For example, it has been<br />
shown that the number and the density of the mitochondria<br />
decrease with increasing age. 79,80 In addition, there is<br />
a decline in the amount of both rough and smooth endoplasmic<br />
reticulum. 81 <strong>The</strong> reduction in the amount of rough<br />
endoplasmic reticulum may be a reflection of a reduced<br />
ability to synthesize proteins. However, the decrease in<br />
the quantity of smooth endoplasmic reticulum may correlate<br />
with the decline in the yield of microsomal<br />
protein. 82<br />
Physiologic Changes<br />
Drug Metabolism<br />
Although there is variability in published reports concerning<br />
hepatic clearance, 83 it is clear that the hepatic<br />
metabolism of anesthetic agents is affected by the reduced<br />
hepatic blood flow. This is probably a reflection of the<br />
confounding variables already discussed in this chapter,<br />
such as differences in functional reserve, the effects of<br />
comorbid conditions, polypharmacy, and numerous environmental<br />
factors.<br />
Minimal changes have been noted in the mixed function<br />
oxidase activity. However, the total capability of the<br />
liver to metabolize many drugs by these enzymes may be<br />
reduced 84,85 with aging. This decline is erratic and unpredictable,<br />
84,86,87 varying from drug to drug and from<br />
individual to individual.<br />
<strong>The</strong> liver converts lipid-soluble drugs into inactive and<br />
water-soluble metabolites by a number of processes that<br />
can be divided into two distinct phases, both of which are<br />
not radically altered 88,89 in the elderly patient:<br />
• Phase 1 renders functionally reactive chemical locations<br />
inactive. <strong>The</strong>se reactions consist of oxidation,<br />
reduction, and hydrolysis, which seem to be the most<br />
changed with aging. Although the levels of drug-metabolizing<br />
enzymes in the cytochrome P-450 systems<br />
do not decline significantly with age, overall hepatic<br />
metabolism of some drugs by these enzymes is diminished.<br />
Such changes in phase I reactions, however,<br />
are probably less significant than the effects of<br />
alcohol, tobacco, 90 and environmental factors on liver<br />
function. 91–93<br />
• Phase 2 reactions involve the addition of a polar group,<br />
rendering the altered molecule more water-soluble.<br />
<strong>The</strong>se reactions include glucuronidation, methylation,<br />
sulfation, and acylation.<br />
Compounds with a suitable reactive site may skip<br />
Phase 1 conversion and pass straight into Phase 2. This is<br />
the case with acetaminophen 94 which contains a hydroxyl<br />
group and is, for the most part, directly glucuronidated<br />
and sulfated.<br />
<strong>The</strong> decrease in liver mass may have a role in the<br />
decline 66 in hepatic drug metabolism. As described before,<br />
total hepatic blood flow is reduced in elderly subjects and<br />
this may affect drug clearance. 63,64 Also, the reduction in<br />
hepatic first-pass metabolism of highly extracted drugs in<br />
the elderly (extraction ratio >0.8 such as morphine 11 )<br />
results in increased plasma drug concentrations and a<br />
propensity to dose-dependent adverse effects.<br />
Laboratory Tests<br />
Routine clinical tests of liver function do not change significantly<br />
with age. <strong>The</strong> aminotransferases and the serum<br />
bilirubin levels remain normal in the elderly. It has been<br />
postulated that a correlation exists between age-associated<br />
impairment of cell metabolism and specific changes<br />
in mitochondrial function and structure.<br />
In summary, hepatic metabolic function in the elderly is<br />
characterized by:<br />
• Decrease in hepatic blood flow<br />
• Decrease in liver size by 35%<br />
• No clinically significant change in routine tests of<br />
function<br />
• Phase I and II metabolism not significantly impaired<br />
Renal Function<br />
In both human and animal models, the aging process<br />
results in structural and functional renal changes 95–98 that<br />
diminish functional reserve. This creates homeostatic<br />
limitations on the kidney’s capability to respond properly<br />
to either volume excess or deficit.<br />
Renal Blood Flow<br />
This function progressively decreases by about 10% per<br />
decade after the age of 50. 99 <strong>The</strong> elderly often have associated<br />
medical conditions such as hypertension, vascular<br />
disease, diabetes, and heart disease that may exacerbate<br />
the effects of these renal abnormalities. Such reductions<br />
in flow, paired with a reduced response to vasodilatory<br />
stimuli, 100–103 render the elderly kidney particularly susceptible<br />
to the harmful effects of reduced cardiac output,<br />
hypotension, hypovolemia, and hemorrhage. Anesthetic<br />
and surgical stress, pain, sympathetic stimulation, and<br />
renal vasoconstrictive drugs may contribute to perioperative<br />
renal dysfunction.<br />
Renal Mass<br />
<strong>The</strong> decrease in blood flow as in the case of the liver is<br />
accompanied by a reduction in renal parenchyma. 104,105<br />
Primarily there is a loss of about 20%–25% of the renal
7. Alterations in Metabolic Functions and Electrolytes 101<br />
cortical mass between the age of 30 and 80 years. At the<br />
light microscopic level, the aging human kidney is characterized<br />
by increased fibrosis, tubular atrophy, and arteriosclerosis.<br />
106,107 <strong>The</strong> presence of small vessel pathology<br />
in older people without apparent renal disease or hypertension,<br />
suggests that even in healthy elderly individuals,<br />
renal changes may be secondary to vascular disease and<br />
altered vascular responsiveness.<br />
Changes in Glomerular Filtration Rate<br />
A microscopic assessment confirms the loss of the kidney’s<br />
functional units with increasing age. 108,109 As many<br />
as half of the glomeruli present in a young adult may be<br />
gone or rendered nonfunctional by 80 years of age.<br />
Although the number of glomeruli is decreased, the<br />
remaining ones are relatively large in size. <strong>The</strong> reductions<br />
in cortical mass are accompanied by progressive sclerosis<br />
of the kidney’s functional units and by the eighth decade<br />
10%–30% of the remaining nephrons are sclerotic. <strong>The</strong><br />
net result of these changes is that there is a gradual<br />
decline in the surface area available for filtration and a<br />
steady reduction of the glomerular filtration rate (GFR).<br />
Age-related decline in GFR is often considered the most<br />
important pharmacokinetic change in old age. GFR, normally<br />
about 125 mL/min in a young adult, decreases to<br />
approximately 80 mL/min at 60 years of age, and to about<br />
60 mL/min at 80 years.<br />
Because GFR decreases less than renal plasma flow,<br />
the filtration fraction increases to a state of hyperfiltration.<br />
This compensates to a certain extent for the<br />
decreased number of functional glomeruli. As a result,<br />
the pressure within the glomerulus increases, possibly<br />
accelerating glomerulosclerosis.<br />
Creatinine Clearance<br />
Because of the decrease in muscle mass with aging, the<br />
decrease in GFR does not result in an increase in serum<br />
creatinine. However, creatinine clearance can be used for<br />
the approximation of GFR. 110 Although the structural<br />
and functional changes seem to have minimal consequences<br />
under normal circumstances, they attain clinical<br />
significance when the remaining renal function is challenged<br />
by the imposition of acute physiologic stress.<br />
When GFR decreases below 80 mL/min, dose adjustments<br />
should be made to renally excreted drugs. Dosing<br />
periods for medications that are renally excreted, such as<br />
aminoglycoside antibiotics and pancuronium need to be<br />
adjusted, and where indicated, drug levels closely watched.<br />
Logic dictates that nephrotoxic drugs should be avoided.<br />
Creatinine clearance decreases by approximately 1 mL/<br />
min/year after the age of 40 years. Renal changes with<br />
aging also result in very tangible problems in the perioperative<br />
period. Drugs that depend on renal function for<br />
clearance may accumulate in the elderly, an effect that<br />
may be exaggerated by preexisting renal disease. In addition,<br />
the elderly are prone to fluid and electrolyte abnormalities<br />
and drug-induced renal failure. 108<br />
Tubular Function<br />
Fluid and electrolyte status should be carefully monitored<br />
in the elderly patient during the perioperative<br />
period. In the absence of disease, and under normal “nonstress”<br />
conditions, the concentrations of electrolytes in<br />
the extracellular fluid are within the normal range. In the<br />
face of physiologic stress, however, the aging kidney has<br />
difficulty maintaining electrolyte balance and circulating<br />
volume, 111 because both sodium conservation and excretion<br />
become more limited with age.<br />
Under normal conditions, age has no effect on the<br />
ability of the individual to maintain extracellular fluid<br />
volume. However, the adaptive systems responsible for<br />
controlling fluid balance are impaired in the elderly and<br />
the aging kidney has a decreased ability to dilute and<br />
concentrate urine. Studies show that tubular function is<br />
generally decreased in the elderly, 108,112 limiting the degree<br />
to which urine can be concentrated in response to water<br />
deprivation. Similarly, the rate at which a salt load can be<br />
excreted becomes more impaired with age. Additionally,<br />
the elderly cannot maximally suppress antidiuretic<br />
hormone secretion when serum osmolarity is reduced.<br />
<strong>The</strong>se observations, together with decreased efficiency<br />
of the renin-angiotensin system, means that elderly<br />
patients’ failure to retain sodium effectively under conditions<br />
of plasma volume contraction is not solely attributable<br />
to reductions in the GFR.<br />
Concentration capacity is an additional sensitive indicator<br />
of renal function. When fluid is restricted, the aged<br />
patient shows a reduced capability to concentrate the<br />
urine. <strong>The</strong> activity of the renin-angiotensin system<br />
declines with age, 113 and above 40 years of age there is a<br />
decline in both plasma renin aldosterone activity, and the<br />
kidney is less efficient at retaining salt with restricted<br />
intake.<br />
Sick patients, especially very elderly ill individuals,<br />
have a tendency to inadequately regulate their intake of<br />
nutrients and water, 114 and have impaired release of<br />
antidiuretic hormone. 106 <strong>The</strong>refore, in the perioperative<br />
period, inadequate electrolyte (via food) and water ingestion<br />
may result in dehydration plus net sodium loss from<br />
obligatory sodium excretion. It has been reported that<br />
11% of acutely ill, aged patients have hyponatremia. This<br />
figure increases to 22% in those patients in chronic care<br />
institutions. 115 Often, the characteristics of their fluid<br />
administration are poorly documented and this contributes<br />
to the less-than-adequate management. 116<br />
Low sodium plasma levels may lead to disturbed<br />
cardiac electrophysiologic function. 117 In addition, the
102 M.C. Lewis<br />
age-related reduction in muscle mass decreases total<br />
body potassium content. However, serum electrolytes are<br />
generally maintained within the same range as is found<br />
in younger adults, 54,118 until situations of surgical stress<br />
abnormalities develop. <strong>The</strong> relationship between abnormal<br />
preoperative potassium levels and arrhythmias is<br />
unclear. 119 Yet, if the surgery is significant, it may be<br />
worthwhile to replenish very low levels. 103<br />
<strong>The</strong> aging kidney is able to maintain acid-base homeostasis<br />
when functioning under baseline conditions. 120<br />
However, the impaired tubular ability of the elderly<br />
kidney to excrete an acid load as compared with that of<br />
the younger patient contributes to the higher incidence<br />
of metabolic acidosis in the elderly. 121<br />
Among elderly surgical patients, acute renal failure is<br />
responsible for up to one-fifth of all perioperative<br />
deaths. 122 Following thoracic surgery, perioperative renal<br />
failure may be as much as 30% 123 with an associated<br />
mortality of 20%–90%. 124,125 Fifty percent of all patients<br />
requiring acute dialysis do so because of perioperative<br />
renal failure. <strong>The</strong> cause of renal failure leading to dialysis<br />
is not clearly understood. However, most cases are attributable<br />
to acute tubular necrosis.<br />
In summary, renal metabolic function in the elderly is<br />
characterized by:<br />
• Decreases in renal blood flow<br />
• Decreases in kidney size<br />
• Morphologic changes include a decrease in the<br />
number of glomeruli, compensatory increase in the<br />
size of the remaining nephrons, and significant<br />
glomerulosclerosis<br />
• No clinically significant changes in routine laboratory<br />
tests, but decreases in creatinine clearance, maximum<br />
sodium concentrating ability, and free water excretion<br />
• Decreases in tubular function, including impaired<br />
ability to handle an acid load, as well as impaired reninangiotensin<br />
and antidiuretic hormone systems<br />
• Decreased thirst response<br />
Implications for <strong>Anesthesiology</strong><br />
Practice<br />
In light of the previous discussion, it is clear that aging<br />
results in important changes in drug pharmacokinetics,<br />
including anesthetic medications. 126,127 <strong>The</strong>se changes are<br />
summarized in Table 7-1.<br />
In What Way Does This Affect Our Practice?<br />
Age-related alterations in the pharmacokinetics of<br />
administered anesthetic agents give rise to changes in the<br />
magnitude of effect of anesthetic agents. Reduced lean<br />
body mass and TBW, and increased percentage of body<br />
fat alter the volume of distribution of anesthetic agents.<br />
Altered renal and liver function reduces drug clearance<br />
from the body. Such changes account for differences<br />
between younger adult patients and their older contemporaries.<br />
This has been demonstrated in studies that have<br />
been performed in the adult population with ages that<br />
range from 20 to 80 years of age. 14,19 This phenomenon<br />
affects drugs not usually thought of when considering<br />
age-related decreases in metabolism. For example, it has<br />
been shown that the rate of propofol elimination declines<br />
with age above 60 years of age. 128<br />
However, much of the information concerning the<br />
pharmacology of anesthetic or any other agent in the<br />
elderly is lacking because the aged are often methodically<br />
excluded from drug trials. 129 Because many drugs are<br />
tested and formulated for younger adults, consideration<br />
must be given to the changes described above when<br />
determining proper dosages for their use in the geriatric<br />
population. Conclusions are often drawn from inference.<br />
Although some models of practice have been accepted,<br />
there remain some contentious issues with regard to<br />
aging effects. Failure to recognize such reductions in both<br />
metabolism and excretion will result in adverse drug<br />
effects. 130<br />
Table 7-1. Physiologic changes in the elderly and their effect on pharmacokinetics.<br />
Pharmacologic factor Change with aging Importance<br />
Absorption<br />
↑ Gastric pH<br />
↓ Gastric emptying<br />
↓ Absorption<br />
↓ Absorptive surface<br />
↓ Splanchnic blood flow<br />
Distribution ↑ Body fat ↑ VD L , lipophilic drugs<br />
↑ α 1 glycoprotein<br />
↓ Free fraction of basic drugs<br />
↓ Albumin<br />
↑ Free fraction of acidic drugs<br />
↓ Body water<br />
↑ Concentration of polar drugs<br />
Metabolism ↓ Hepatic metabolism ↓ Biotransformation<br />
Elimination ↓ Glomerular filtration rate ↓ Elimination fluid, pH, and electrolyte disturbance<br />
↓ Renal tubular function
7. Alterations in Metabolic Functions and Electrolytes 103<br />
Adverse Drug Reactions and Aging<br />
Not surprisingly, the older patient is at risk of adverse drug<br />
reactions from chronic medications. Pharmacokinetic<br />
changes, polypharmacy, and drug interactions summate to<br />
make adverse drug interactions more likely. 131,132 Drug<br />
elimination is decreased in the aged, leading to higher<br />
blood concentrations and hence a higher possibility of a<br />
type A adverse reaction (exaggerated or excessive but otherwise<br />
normal pharmacologic action of a drug). 133,134 In<br />
fact, there is an almost linear increase of adverse drug<br />
reactions with age. 135 <strong>Geriatric</strong> patients are up to three<br />
times more likely to experience adverse drug reactions. 136<br />
In addition, the risk of adverse drug reactions increases<br />
with the number of medications given. Thus, the addition<br />
of several drugs, even short-acting ones, in the perioperative<br />
period makes adverse reactions more likely. 137 This<br />
situation is further complicated by the fact that advanced<br />
age is accompanied by comorbidity and the consequent<br />
polypharmacy for treatment of these disease states. 138,139 If<br />
we, as perioperative physicians of the elderly, are going to<br />
use these drugs in a rational and safe manner, it is incumbent<br />
upon us to acquire an understanding of how such<br />
age-dependent change occurs. An example of how this<br />
information may be useful is seen with hypertension. This<br />
disease is highly prevalent in the elderly and often requires<br />
multiple medications for its management. Concomitant<br />
medications, such as β-adrenergic blocking drugs and<br />
diuretics might further impair reflex heart rate and cardiac<br />
output increases. <strong>The</strong> use of a volatile anesthetic in these<br />
patients may give rise to exaggerated decreases in blood<br />
pressure, especially if the patient is hypovolemic.<br />
Summary<br />
<strong>The</strong> perioperative care of the elderly patient is challenging.<br />
Aging progressively diminishes functional reserve,<br />
and therefore diminishes the patient’s ability to handle<br />
stress. As illustrated in this chapter, a global understanding<br />
of the metabolic alterations that take place with aging<br />
helps us to better manage and respond to pharmacokinetic<br />
and pharmacodynamic reactions within this patient<br />
population. Such knowledge will aid us in providing an<br />
optimal anesthetic for each elderly patient. Part of our<br />
role as perioperative physicians may well include the<br />
detection and possible correction of metabolic abnormalities.<br />
We, as anesthesiologists, should act as “homeostasis<br />
in absentia.” This may help to preserve existing<br />
function, and avoid adverse outcomes.<br />
References<br />
1. Travis KW, Mihevc NT, Orkin FK, Zeitlin GL. Age and<br />
anesthetic practice: a regional perspective. J Clin Anesthesiol<br />
1999;11:175–186.<br />
2. Gibson JR, Mendenhall MK, Axel NJ. <strong>Geriatric</strong> anesthesia:<br />
minimizing the risk. Clin Geriatr Med 1985;1:313–321.<br />
3. Medawar P. An unsolved problem of biology. An inaugural<br />
lecture delivered at University College London, 6 December<br />
1951. London: H.K. Lewis; 1952.<br />
4. Sehl ME, Yates FE. Kinetics of human aging: I. Rates of<br />
senescence between ages 30 and 70 years in healthy people.<br />
J Gerontol A Biol Sci Med Sci 2001;56:198–208.<br />
5. Clergue F, Auroy Y, Pequignot F, Jougla E, Lienhart A,<br />
Lexenaire MC. French survey of anesthesia in 1996. <strong>Anesthesiology</strong><br />
1999;91:1509–1520.<br />
6. US Census Bureau: population projections program. Population<br />
Division. Projections of the total resident population<br />
by 5-year age groups, and sex with special age<br />
categories: middle series, 2025 to 2045. Washington, DC;<br />
2000.<br />
7. http://factfinder.census.gov/jsp/saff/SAFFInfo.jsp?_<br />
pageId=tp2_aging. Accessed August 15, 2007.<br />
8. Sloan RW. Principles of drug therapy in geriatric patients.<br />
Am Fam Physician 1992;45:2709–2718.<br />
9. Ergina P, Gold S, Meakins J. Perioperative care of the<br />
elderly patient. World J Surg 1993;17:192–198.<br />
10. Klopfenstein CE, Herrmann FR, Michel JP, et al. <strong>The</strong> influence<br />
of an aging surgical population on the anesthesia<br />
workload: a ten-year survey. Anesth Analg 1998;86:<br />
1165–1170.<br />
11. Hosking MP, Warner MA, Lobdell CM, et al. Outcomes<br />
of surgery in patients 90 years of age and older. JAMA<br />
1989;261:1909–1915.<br />
12. Ackerman RJ, Vogel RL, Johnson LA, et al. Surgery in<br />
nonagenarians: morbidity, mortality and functional outcomes.<br />
J Fam Pract 1996;40:129–135.<br />
13. Warner MA, Saletel DR, Schroeder DR, Warner DO,<br />
Offord KP, Gray DT. Outcomes of anesthesia and surgery<br />
in people 100 years of age and older. J Am Geriatr Soc<br />
1998;46:988–993.<br />
14. Graves EJ, Gillum BS. Advance Data from Vital and<br />
Health Statistics [1994 Summary: National Hospital Discharge<br />
Survey]. Atlanta: Centers for Disease Control and<br />
Prevention; 1996:278.<br />
15. Seymour DG, Vaz FG. A prospective study of elderly<br />
general surgical patients. Post-operative complications.<br />
Age Aging 1989;18:316–326.<br />
16. Linn BS, Linn MW, Wallen N. Evaluation of results of surgical<br />
procedures in the elderly. Ann Surg 1982;195:90.<br />
17. Pofahl WE, Pories WJ. Current status and future directions<br />
of geriatric general surgery. J Am Geriatr Soc 2003;51:<br />
S351–S354.<br />
18. Palmberg S, Hirsjarvi E. Mortality in geriatric surgery.<br />
With special reference to the type of surgery, anaesthesia,<br />
complicating diseases, and prophylaxis of thrombosis.<br />
Gerontology 1979;25:103–112.<br />
19. Silverstein JH, Bloom HG, Cassel CK. <strong>Geriatric</strong>s and anesthesia.<br />
Anesthesiol Clin North Am 1999;17:453–465.<br />
20. Roberts SB, Fuss P, Heyman MB, Young VR. Influence of<br />
age on energy requirements. Am J Clin Nutr 1995;62:<br />
1053S–1058S.<br />
21. Fukagawa NK, Bandini LG, Young JB. Effect of age on<br />
body composition and resting metabolic rate. Am J Physiol<br />
1990;259:E233–E238.
104 M.C. Lewis<br />
22. Henry CJK. Mechanisms of changes in basal metabolism<br />
during ageing. Eur J Clin Nutr 2000;54:77–91.<br />
23. Muravchick S. <strong>The</strong> aging process: anesthetic implications.<br />
Acta Anaesthesiol Belg 1998;49:85–90.<br />
24. Schwartz RS, Jaeger LF, Veith RC. <strong>The</strong> importance of body<br />
composition to the increase in plasma norepinephrine<br />
appearance rate in elderly men. J Gerontol 1987;42:<br />
546–551.<br />
25. Daniëlle AJ, Kerckhoffs M, Blaak EE, Van Baak MA, Saris<br />
WHM. Effect of aging on β-adrenergically mediated<br />
thermogenesis in men. Am J Physiol Endocrinol Metab<br />
1998;274:E1075–E1079.<br />
26. Zeeh J, Platt D. <strong>The</strong> aging liver: structural and functional<br />
changes and their consequences for drug treatment in old<br />
age. Gerontology 2002;48:121–127.<br />
27. Busby-Whitehead J. <strong>The</strong> epidemic in your waiting room.<br />
<strong>Geriatric</strong>s 2004;59:6–7.<br />
28. Straus SE. <strong>Geriatric</strong> medicine. Clinical review. BMJ 2001;<br />
322:86–89.<br />
29. Vaughan MS, Vaughan RW, Cork RC. Postoperative hypothermia<br />
in adults: relationship of age, anesthesia, and<br />
shivering to rewarming. Anest Analg 1981;60:746–751.<br />
30. Frank SM, Fleisher LA, Olson KF, et al. Multivariate<br />
determinants of early postoperative oxygen consumption<br />
in elderly patients. Effects of shivering, body temperature,<br />
and gender. <strong>Anesthesiology</strong> 1995;83:241–249.<br />
31. El-Gamal N, El-Kassabany N, Frank SM, et al. Age-related<br />
thermoregulatory differences in a warm operating room<br />
environment (approximately 26 degrees C). Anesth Analg<br />
2000;90:694–698.<br />
32. Sessler DI, Kurz A, Lenhardt R. Re: Hypothermia reduces<br />
resistance to surgical wound infections. Am Surg 1999;<br />
65:1193–1196.<br />
33. Frank SM, Beattie C, Christopherson R, et al. Unintentional<br />
hypothermia is associated with postoperative myocardial<br />
ischemia. <strong>The</strong> Perioperative Ischemia Randomized<br />
<strong>Anesthesia</strong> Trial Study Group. <strong>Anesthesiology</strong> 1993;78:<br />
468–476.<br />
34. Leslie K, Sessler DI. <strong>The</strong> implications of hypothermia for<br />
early tracheal extubation following cardiac surgery. J Cardiothorac<br />
Vasc Anesth 1998;12:30–34.<br />
35. Beaufrere B, Morio B. Fat and protein redistribution with<br />
aging: metabolic considerations. Eur J Clin Nutr 2000;54:<br />
S48–S53.<br />
36. Forbes GB, Reina JC. Adult lean body mass declines with<br />
age: some longitudinal observations. Metabolism 1970;19:<br />
653–663.<br />
37. Muravchick S. Current concepts: anesthetic pharmacology<br />
in the geriatric patient. Prog Anesthesiol 1987;1:2.<br />
38. Greenblatt DJ, Abernethy DR, Locniskar A, Harmatz JS,<br />
Limjuco RA, Shader RI. Effect of age, gender, and obesity<br />
on midazolam kinetics. <strong>Anesthesiology</strong> 1984;61:27–35.<br />
39. Saraiva RA, Lunn JN, Mapleson WW, Willis BA, France<br />
JM. Adiposity and the pharmacokinetics of halothane.<br />
<strong>The</strong> effect of adiposity on the maintenance of and re -<br />
covery from halothane anaesthesia. Anaesthesia 1977;32:<br />
240–246.<br />
40. Pierson RN Jr. Body composition in aging: a biological<br />
perspective. Curr Opin Clin Nutr Metab Care 2003;6:<br />
15–20.<br />
41. Doherty TJ. Invited review: aging and sarcopenia. J Appl<br />
Physiol 2003;95:1717–1727.<br />
42. Roubenoff R. Sarcopenia and its implications for the<br />
elderly. Eur J Clin Nutr 2000;54:S40–S47.<br />
43. Rosenberg IH. Summary comments. Am J Clin Nutr<br />
1989;50:1231–1233.<br />
44. Deschenes MR. Effects of aging on muscle fibre type and<br />
size. Sports Med 2004;34:809–824.<br />
45. Short KR, Vittone JL, Bigelow ML, Proctor DN, Nair KS.<br />
Age and aerobic exercise training effects on whole body<br />
and muscle protein metabolism. Am J Physiol Endocrinol<br />
Metab 2004;286:E92–101.<br />
46. Ornstein E, Matteo RS, Schwartz AE, Jamdar SC, Diaz J.<br />
Pharmacokinetics and pharmacodynamics of pipecuronium<br />
bromide (Arduan) in elderly surgical patients.<br />
Anesth Analg 1992;74:841–844.<br />
47. Lauven PM, Nadstawek J, Albrecht S. <strong>The</strong> safe use of<br />
anaesthetics and muscle relaxants in older surgical patients.<br />
Drugs Aging 1993;3:502–509.<br />
48. Rupp SM, Castagnoli KP, Fisher DM, Miller RD. Pancuronium<br />
and vecuronium pharmacokinetics and pharmacodynamics<br />
in younger and elderly adults. <strong>Anesthesiology</strong><br />
1987;67:45–49.<br />
49. Koch-Weser J, Sellers EM. Binding of drugs to serum<br />
albumin. N Engl J Med 1976;294:311–316.<br />
50. Greenblatt DJ, Sellers EM, Shader RI. Drug therapy:<br />
drug disposition in old age. N Engl J Med 1982;306:1081–<br />
1088.<br />
51. Campion EW, deLabry LO, Glynn RJ. <strong>The</strong> effect of age on<br />
serum albumin in healthy males: report from the Normative<br />
Aging Study. J Gerontol 1988;43:M18–20.<br />
52. Greenblatt DJ. Reduced serum albumin concentration in<br />
the elderly: a report from the Boston Collaborative Drug<br />
Surveillance Program. J Am Geriatr Soc 1979;27:20–22.<br />
53. Boudinot SG, Funderburg ED, Boudinot FD. Effects of<br />
age on the pharmacokinetics of piroxicam in rats. J Pharm<br />
Sci 1993;82:254–257.<br />
54. Grandison MK, Boudinot FD. Age-related changes in<br />
protein binding of drugs: implications for therapy. Clin<br />
Pharmacokinet 2000;38:271–290.<br />
55. Bernus I, Dickinson RG, Hooper WD, Eadie MJ. Anticonvulsant<br />
therapy in aged patients. Clinical pharmacokinetic<br />
considerations. Drugs Aging 1997;10:278–289.<br />
56. Grossman SB, Yap SH, Shafritz DA. Influence of chronic<br />
renal failure on protein synthesis and albumin metabolism<br />
in rat liver. J Clin Invest 1977;59:869–887.<br />
57. Christensen JH, Andreasen F, Jansen J. Pharmacokinetics<br />
and pharmacodynamics of thiopental in patients undergoing<br />
renal transplantation. Acta Anaesthesiol Scand<br />
1983;27:513–518.<br />
58. Riant P, Barre J, Albengres E, Lemaire M, Tillement JP.<br />
Plasma binding of drugs in chronic renal failure. Nephrologie<br />
1986;7:89–93.<br />
59. Veering BT, Burm AG, Souverijn JH, Serree JM, Spierdijk<br />
J. <strong>The</strong> effect of age on serum concentrations of albumin<br />
and alpha 1-acid glycoprotein. Br J Clin Pharmacol 1990;<br />
29:201–206.<br />
60. Lamy PP. Comparative pharmacokinetic changes and drug<br />
therapy in an older population. J Am Geriatr Soc 1982;30:<br />
S11–S19.
7. Alterations in Metabolic Functions and Electrolytes 105<br />
61. Matteo RS, Ornstein E, Schwartz AE, Ostapkovich N,<br />
Stone JG. Pharmacokinetics and pharmacodynamics of<br />
rocuronium (Org 9426) in elderly surgical patients. Anesth<br />
Analg 1993;77:1193–1197.<br />
62. LeCouteur DG, McLean AJ. <strong>The</strong> aging liver: drug clearance<br />
and an oxygen diffusion barrier hypothesis. Clin<br />
Pharmacokinet 1998;34:359–373.<br />
63. Schmucker DL. Liver function and phase I drug metabolism<br />
in the elderly: a paradox. Drugs Aging 2001;18:<br />
837–851.<br />
64. Tietz NW, Shuey DF, Wekstein DR. Laboratory values in<br />
fit aging individuals—sexagenarians through centenarians.<br />
Clin Chem 1992;38:1167–1185.<br />
65. Zeeh J, Platt D. Age related changes in the liver. Consequences<br />
for drug therapy. Fortschr Med 1990;108:651–653.<br />
66. Wynne HA, James OFW. <strong>The</strong> aging liver. Age Ageing<br />
1990;19:1–3.<br />
67. Ettore GM, Sommacale D, Farges O, et al. Postoperative<br />
liver function after elective right hepatectomy in elderly<br />
patients. Br J Surg 2001;88:73–76.<br />
68. Marchesini G, Bua V, Brunori A, et al. Galactose elimination<br />
capacity and liver volume in aging man. Hepatology<br />
1988;8:1079–1083.<br />
69. Schmucker DL. Aging and the liver: an update. J Gerontol<br />
Biol Sci 1998;53A:B315–320.<br />
70. Vestal RE. Drug use in the elderly. A review of problems<br />
and special consideration. Drugs 1978;16:358–382.<br />
71. Muravchick S. <strong>The</strong> aging patient and age related disease.<br />
ASA Annual Refresher Course Lecture #151. Park Ridge,<br />
IL: American Society of Anesthesiologists; 1987.<br />
72. Vestal RE. Aging and determinants of hepatic drug<br />
clearance. Hepatology 1989;9:331–334.<br />
73. Vestal RE. Pharmacology and aging. J Am Geriatr Soc<br />
1982;30:191–200.<br />
74. Woodhouse KW, James OFW. Hepatic drug metabolism<br />
and aging. Br Med Bull 1980;46:22–35.<br />
75. Wynne HA, Cope E, Mutch E, Rawlins MD, Woodhouse<br />
KW, James OF. <strong>The</strong> effects of age upon liver volume and<br />
apparent liver blood flow in healthy man. Hepatology<br />
1989;9:297–301.<br />
76. Zoli M, Magalotti D, Bianchi G, et al. Total and functional<br />
hepatic blood flow decrease in parallel with aging. Age<br />
Aging 1999;28:29–33.<br />
77. Seaman DS. Adult living donor transplantation: current<br />
status. J Clin Gastroenterol 2001;33:97–106.<br />
78. LeCouteur DG, McLean AJ. <strong>The</strong> aging liver. Drug clearance<br />
and an oxygen diffusion barrier hypothesis. Clin<br />
Pharmacokinet 1998;34:359–373.<br />
79. Pieri C, Zs-Nagy I, Mazzufferi G, Giuli C. <strong>The</strong> aging of rat<br />
liver as revealed by electron microscopic morphometry.<br />
I. Basic parameters. Exp Gerontol 1975;10:291–304.<br />
80. Sastre J, Pallardo FV, Pla R, et al. Aging of the liver: ageassociated<br />
mitochondrial damage in intact hepatocytes.<br />
Hepatology 1996;24:1199–1205.<br />
81. Schmucker DL, Wang RK. Age related changes in the<br />
hepatic endoplasmic reticulum: a quantitative analysis.<br />
Science 1977;197:1005–1008.<br />
82. Wynne H, Mutch E, James OF, Rawlins MD, Woodhouse<br />
KW. <strong>The</strong> effect of age on mono-oxygenase enzyme kinetics<br />
in rat liver microsomes. Age Ageing 1987;16:153–158.<br />
83. Sheweita SA. Drug-metabolizing enzymes: mechanisms<br />
and functions. Curr Drug Metab 2000;1:107–132.<br />
84. Kato R, Vassanelli P, Frontino G. Variation in the activity<br />
of liver microsomal drug metabolizing enzymes in rats<br />
in relation to age. Biochem Pharmacol 1964;12:1037–<br />
1051.<br />
85. Sutter MA, Wood WG, Williamson LS, Strong R, Pickham<br />
K, Richardson A. Comparison of the hepatic mixed function<br />
oxidase system of young, adult, and old non-human<br />
primates (Macaca nemestrina). Biochem Pharmacol 1985;<br />
34:2983–2987.<br />
86. Williams RT. Comparative patterns of drug metabolism.<br />
Fed Proc 1967;26:1029–1039.<br />
87. Crooks J, O’Malley K, Stevenson LH. Pharmacokinetics in<br />
the elderly. Clin Pharmacokinet 1976;1:280–296.<br />
88. Seifalian AM, Stansby GP, Hobbs KE, Hawkes DJ,<br />
Colchester AC. Measurement of liver blood flow: a review.<br />
HPB Surg 1991;4:171–186.<br />
89. Hunt CM, Westerkam WR, Stave GM. Effects of age and<br />
gender on the activity of human hepatic CYP3A. Biochem<br />
Pharmacol 1992;44:275–283.<br />
90. Vestal RE, Wood AJ. Influence of age and smoking on<br />
drug kinetics in man. Clin Pharmacokinet 1980;5:309–<br />
318.<br />
91. Sellers EM, Frecker RC, Romach MK. Drug metabolism<br />
in the elderly: confounding of age, smoking and ethanol<br />
effects. Drug Metab Rev 1983;14:225–250.<br />
92. Kinirons MT, O’Mahony MS. Drug metabolism and ageing.<br />
Br J Clin Pharmacol 2004;57:540–544.<br />
93. Herd B, Wynne H, Wright P, James O, Woodhouse K.<br />
<strong>The</strong> effect of age on glucuronidation and sulphation of<br />
paracetamol by human liver fractions. Br J Clin Pharmacol<br />
1991;32:768–770.<br />
94. Bessems JG, Vermeulen NP. Paracetamol (acetaminophen)-induced<br />
toxicity: molecular and biochemical<br />
mechanisms, analogues and protective approaches. Crit<br />
Rev Toxicol 2001;31:55–138.<br />
95. Anderson S, Brenner BM. Effects of aging on the renal<br />
glomerulus. Am J Med 1986;80:435–442.<br />
96. Kaysen GA, Myers BD. <strong>The</strong> aging kidney. Clin Geriatr<br />
Med 1985;1:207–222.<br />
97. Goldstein RS, Tarloff JB, Hook JB. Age related nephropathy<br />
in laboratory rats. FASEB J 1988;2:2241–2251.<br />
98. Tauchi H, Tsuboi K, Okutomi J. Age changes in the human<br />
kidney of different races. Gerontologica 1971;17:87–97.<br />
99. Epstein M. Aging and the kidney. J Am Soc Nephrol 1996;<br />
7:1106–1122.<br />
100. Nyengaard JR, Bendtsen TF. Glomerular number and size<br />
in relation to age, kidney weight and body surface in<br />
normal man. Anat Rec 1992;232:194–201.<br />
101. Baylis C, Fredericks M, Wilson C, Munger K, Colins R.<br />
Renal vasodilatory response to intravenous glycine in the<br />
aging rat kidney. Am J Kidney Dis 1990;15:244–251.<br />
102. Fuiano G, Sund S, Mazza G, et al. Renal hemodynamic<br />
response to maximal vasodilating stimulus in healthy older<br />
subjects. Kidney Int 2001;59:1052–1058.<br />
103. Fliser D, Ritz E. Renal hemodynamics in the elderly.<br />
Nephrol Dial Transplant 1996;11(Suppl 9):2–8.<br />
104. Beck LH. Changes in renal function with aging. Clin<br />
Geriatr Med 1998;14:199–209.
106 M.C. Lewis<br />
105. Neugarten J, Gallo G, Silbiger S, Kasiske B. Glomerulosclerosis<br />
in aging humans is not influenced by gender. Am<br />
J Kidney Dis 1999;34:884–888.<br />
106. Goyal VK. Changes with age in the human kidney. Exp<br />
Gerontol 1982;17:321–331.<br />
107. Corman B, Barrault MB, Klinger C, et al. Renin gene<br />
expression in the aging kidney: effect of sodium restriction.<br />
Mech Ageing Dev 1995;84:1–13.<br />
108. Muhlberg W, Platt D. Age-dependent changes of the<br />
kidneys: pharmacological implications. Gerontology 1999;<br />
45:243–253.<br />
109. Kaplan C, Pasternack B, Shah H, Gallo G. Age-related<br />
incidence of sclerotic glomeruli in human kidneys. Am J<br />
Pathol 1975;80:227–234.<br />
110. Miller M. Fluid and electrolyte balance in the elderly.<br />
<strong>Geriatric</strong>s 1987;42:65–76.<br />
111. Sunderam SG, Mankikar GD. Hyponatremia in the elderly.<br />
Age Ageing 1983;12:77–80.<br />
112. Dontas AS, Marketos S, Papanayiotou P. Mechanisms of<br />
renal tubular defects in old age. Postgrad Med J 1972;<br />
48:295–303.<br />
113. Phillips PA, Hodsman GP, Johnson CI. Neuroendo -<br />
crine mechanisms and cardiovascular homeostasis in<br />
the elderly. Cardiovasc Drugs <strong>The</strong>r 1991;4(Suppl 6):1209–<br />
1213.<br />
114. Kleinfeld M, Casmir M, Borra S. Hyponatremia as observed<br />
in a chronic disease facility. J Am <strong>Geriatric</strong> Soc 1979;29:<br />
156–161.<br />
115. O’Neill PA, Faragher DS, Davies I, Wears R, McLean KA,<br />
Fairweather DS. Reduced survival with increased plasma<br />
osmolality in elderly continued care patients. Age Ageing<br />
1990;19:68–71.<br />
116. National confidential enquiry into patient outcome and<br />
death (1999). Available at: http://www.ncepod.org.uk/pdf/<br />
1999/99eld.pdf.<br />
117. Amar D, Hao Z, Leung DHY, Roistacher N, Kadish AH.<br />
Older age is the strongest predictor of postoperative atrial<br />
fibrillation. <strong>Anesthesiology</strong> 2002;96:352–356.<br />
118. Morimoto S, Ogihara T. Physiological and pathological<br />
aging and electrolyte metabolism. Nippon Ronen Igakkai<br />
Zasshi 1991;28:325–330.<br />
119. Wahr JA, Parks R, Boisvert D, Comunale M, Fabian J,<br />
Mangano DT. Preoperative serum potassium levels and<br />
perioperative outcomes in cardiac surgery patients. Multicentre<br />
study of Perioperative Ischemia Research Group.<br />
JAMA 1999;281:2203–2210.<br />
120. Frasseto L, Sebastian A. Age and systemic acid-base equilibrium:<br />
analysis of published data. J Gerontol A Biol Sci<br />
Med Sci 1996;51:B91–99.<br />
121. Okusawa S, Aikawa N, Abe O. Postoperative metabolic<br />
alkalosis following general surgery: its incidence and possible<br />
etiology. Jpn J Surg 1989;19:312–318.<br />
122. Aronson S. Renal function monitoring. In: Miller RD, ed.<br />
<strong>Anesthesia</strong>. 4th ed. New York: Churchill Livingstone;<br />
1994:1293–1317.<br />
123. Cowan JA Jr, Dimick JB, Wainess RM, Henke PK, Stanley<br />
JC, Upchurch GR Jr. Ruptured thoracoabdominal aortic<br />
aneurysm treatment in the United States: 1988 to 1998.<br />
J Vasc Surg 2003;38:319–322.<br />
124. Wilkes BM, Mailloux LU. Acute renal failure: pathogenesis<br />
and prevention. Am J Med 1986;80:1129–1136.<br />
125. Carmichael P, Carmichael AR. Acute renal failure in the<br />
surgical setting. ANZ J Surg 2003;73:144–153.<br />
126. Shafer SL. Pharmacokinetics and pharmacodynamics of<br />
the elderly. In: McLesky CH, ed. <strong>Geriatric</strong> <strong>Anesthesiology</strong>.<br />
Baltimore: Williams & Wilkins; 1997:123–142.<br />
127. Crome P. What’s different about older people? Toxicology<br />
2003;192:49–54.<br />
128. Schuttler J, Ihmsen H. Population pharmacokinetics of propofol:<br />
a multicenter study. <strong>Anesthesiology</strong> 2000;92:727–738.<br />
129. Cheitlin MD, Gerstenblith G, Hazzard WR, et al. Database<br />
Conference January 27–30, 2000, Washington D.C.: Do<br />
existing databases answer clinical questions about geriatric<br />
cardiovascular disease and stroke? Am J Geriatr Cardiol<br />
2001;10:207–223.<br />
130. Vancura EJ. Guard against unpredictable drug responses<br />
in the aging. <strong>Geriatric</strong>s 1979;34:63–65, 69–70, 73.<br />
131. Hurwitz N. Predisposing factors in adverse reactions to<br />
drugs. Br Med J 1969;1:536–539.<br />
132. Hurwitz N, Wade OL. Intensive hospital monitoring of<br />
adverse reactions to drugs. Br Med J 1969;1:531–536.<br />
133. Editorial: medications for the elderly. J R Coll Phys Lond<br />
1984;18:7–17.<br />
134. Schmucker DL. Age related changes in drug disposition.<br />
Pharmacol Rev 1979;30:445–456.<br />
135. Paterson C. Iatrogenic disease in late life. Clin Geriatr Med<br />
1986;2:121–136.<br />
136. Woodhouse KW, Mortimer O, Wilhom BE. Hepatic adverse<br />
drug reactions. In: Kitani K, ed. <strong>The</strong> Effects of Age in Liver<br />
and Ageing. Amsterdam: Elsevier; 1986:75–80.<br />
137. Williamson J, Chopin JM. Adverse reactions to prescribed<br />
drugs in the elderly: a multicenter investigation. Age<br />
Ageing 1980;9:73–80.<br />
138. Hughes SG. Prescribing for the elderly patient: why do we<br />
need to exercise caution? Br J Clin Pharmacol 1998;46:<br />
531–533.<br />
139. Turnheim K. Drug dosage in the elderly. Is it rational?<br />
Drugs Aging 1998;13:357–379.
8<br />
Perioperative <strong>The</strong>rmoregulation<br />
Daniel I. Sessler<br />
Perioperative thermal disturbances are common and<br />
there is considerable evidence that disturbances are especially<br />
frequent in the elderly. <strong>The</strong> most common perioperative<br />
thermal disturbance—hypothermia—is both more<br />
likely and more severe in the elderly than in younger<br />
patients. Anesthetic drugs impair thermoregulation in all<br />
patients, and delayed or insufficient thermoregulatory<br />
defenses are the primary causes of hypothermia in most<br />
patients. Excessive hypothermia in the elderly results<br />
largely because central and efferent thermoregulatory<br />
controls are particularly disturbed in these patients.<br />
Perioperative hypothermia has long been associated<br />
with complications including decreased drug metabolism<br />
and postoperative shivering. In recent years, mild hypothermia<br />
has been shown to significantly alter patient outcomes<br />
by increasing the incidence of myocardial ischemia,<br />
augmenting blood loss, decreasing resistance to surgical<br />
wound infections, and prolonging hospitalization. <strong>The</strong>re<br />
is no reason to believe that the elderly are resistant to<br />
complications associated with hypothermia. Instead, they<br />
are especially susceptible to many of them because of<br />
normal age-related changes in organ function and because<br />
many have substantial underlying diseases. In contrast,<br />
thermal management in the elderly does not differ importantly<br />
from that in younger patients.<br />
Normal <strong>The</strong>rmoregulation<br />
Core body temperature is among the most jealously<br />
guarded physiologic parameters and is justifiably considered<br />
one of the “vital signs.” <strong>The</strong> major thermoregulatory<br />
defenses are behavior, 1,2 sweating, 3 precapillary vasodilation,<br />
4 arteriovenous shunt vasoconstriction, 5 nonshivering<br />
thermogenesis, 6 and shivering. 7 Each can be<br />
<strong>The</strong> author does not consult for, accept honoraria from, or own<br />
stock or stock options in any company related to products discussed<br />
in this chapter.<br />
characterized by its threshold (triggering core temperature),<br />
gain (intensity increase with further core-temperature<br />
deviation), and maximum intensity. 8 Temperatures<br />
between the first autonomic warm response (sweating)<br />
and the first autonomic cold defense (vasoconstriction)<br />
define the interthreshold range; these temperatures do<br />
not trigger autonomic thermoregulatory defenses. 9<br />
Precise control of core temperature is maintained by a<br />
powerful thermoregulatory system incorporating afferent<br />
inputs, central control, and efferent defenses. 10 Efferent<br />
defenses can be broadly divided into autonomic<br />
responses (i.e., sweating and shivering) and behavioral<br />
responses (i.e., closing a window, putting on a sweater).<br />
Autonomic responses depend largely on core temperature<br />
and are mostly mediated by the anterior hypothalamus.<br />
In contrast, behavioral responses are mostly<br />
determined by skin temperature and are controlled by<br />
the posterior hypothalamus 11 (Figure 8-1).<br />
Afferent Input<br />
Warm afferent signals are conveyed by unmyelinated C-<br />
fibers, as is pain. In contrast, cold signals traverse myelinated<br />
A-delta fibers, both of which are widely distributed. 12<br />
Most thermal input is conducted along the spinothalamic<br />
tracts, although both afferent and efferent thermal signals<br />
are diffusely distributed within the neuraxis. 13<br />
<strong>The</strong> central thermoregulatory control system accepts<br />
thermal input from tissues all over the body. <strong>The</strong> relative<br />
contributions of most tissues have yet to be determined<br />
in humans. However, animal studies suggest that the<br />
hypothalamus, other portions of the brain, the spinal<br />
cord, and deep thoracic and abdominal tissues each contribute<br />
very roughly 20%. 8,14–16<br />
Mean skin temperature contributes 5%-20% as much<br />
as core temperature (deep central tissues and brain) to<br />
control of sweating and active vasodilation; furthermore,<br />
the relation between mean skin and core temperatures at<br />
response thresholds is linear. 4,17–20 That is, a 1°C increase<br />
107
108 D.I. Sessler<br />
Core<br />
Skin<br />
Core<br />
Skin<br />
in skin temperature reduces the sweating and active capillary<br />
vasodilation thresholds (expressed in terms of core<br />
temperature) by 0.05–0.2°C. Arithmetically, this relation<br />
takes the form<br />
Thres MBT = βT skin + (1 − β)T core ,<br />
where Thres MBT is the sweating or vasodilation threshold<br />
in terms of physiologic (rather than anatomic) mean<br />
body temperature, T skin is mean skin temperature, and<br />
T core is core temperature, all in degrees centigrade.<br />
<strong>The</strong> proportionality constant, β, in this case is 0.05–0.2.<br />
<strong>The</strong> skin surface contributes 20% ± 6% to control of<br />
vasoconstriction and 19% ± 8% to control of shivering,<br />
and the contribution in linear 16 (Figure 8-2). <strong>Regional</strong><br />
sensory contributions to thermoregulatory control have<br />
not been specifically evaluated in the elderly. However,<br />
there is little reason to believe that temperature sensation<br />
fails in the elderly or that integration differs<br />
markedly.<br />
Central Control<br />
Anterior<br />
Hypothalamus<br />
Posterior<br />
Hypothalamus<br />
Autonomic Responses<br />
Behavioral Responses<br />
Figure 8-1. Control of autonomic and behavioral thermoregulatory<br />
defenses. Efferent defenses can be broadly divided into<br />
autonomic responses (e.g., sweating and shivering) and behavioral<br />
responses (e.g., closing a window, putting on a sweater).<br />
Autonomic responses depend largely on core temperature and<br />
are mediated largely by the anterior hypothalamus. In contrast,<br />
behavioral responses are mostly determined by skin temperature<br />
and are controlled by the posterior hypothalamus.<br />
<strong>The</strong>rmal afferent signals are integrated at numerous<br />
levels within the neuraxis, including the spinal cord and<br />
brain stem. <strong>The</strong> dominant controller in mammals, however,<br />
is the hypothalamus. (Interestingly, the spinal cord dominates<br />
in birds.) Although core temperature varies with a<br />
daily circadian rhythm, 21 body temperature is normally<br />
controlled to within a few tenths of a degree centigrade<br />
almost irrespective of the environment. 22 Such precise<br />
control is maintained by a powerful thermoregulatory<br />
system incorporating afferent inputs, central control, and<br />
efferent defenses.<br />
<strong>The</strong> thresholds triggering thermoregulatory defenses<br />
are uniformly about 0.3°C greater during the follicular<br />
phase in women than in men, 22 and would be an additional<br />
≈10.5°C greater during the luteal phase. 23 However,<br />
men and women regulate core body temperature with<br />
comparable precision, usually maintaining core temperature<br />
within a few tenths of a °C of the target temperature<br />
(Figure 8-3).<br />
<strong>The</strong> major autonomic warm defenses, sweating and<br />
active vasodilation, are triggered at about the same temperature<br />
and seem to operate synchronously. 24 In contrast,<br />
vasoconstriction is the first autonomic response to<br />
cold. 22 Only when vasoconstriction is insufficient to maintain<br />
core temperature (in a given environment), is nonshivering<br />
thermogenesis or shivering initiated. In humans,<br />
nonshivering thermogenesis is restricted to infancy, and<br />
infants use this defense in preference to shivering. 25<br />
In contrast, nonshivering thermogenesis is of little<br />
importance in adult humans, 26–28 although it is the most<br />
important cold defense in small animals.<br />
When one efferent response is inadequate to maintain<br />
core temperature in a given environment, others are acti-<br />
36<br />
34<br />
Core 38<br />
Temperature<br />
(°C) 36<br />
Vasoconstriction<br />
38 #1<br />
34<br />
38<br />
36<br />
Shivering<br />
#2<br />
#3 #4<br />
#5<br />
#6<br />
34<br />
30 34 38 30 34 38<br />
Skin Temperature(°C)<br />
Figure 8-2. <strong>The</strong> relative contribution of mean skin temperature<br />
to control of thermoregulatory vasoconstriction and shivering<br />
in six men. <strong>The</strong> threshold (triggering core temperature) for each<br />
response is plotted vertically against mean skin temperature.<br />
Core and skin temperatures at the vasoconstriction and shivering<br />
thresholds were linearly related. <strong>The</strong> extent to which mean<br />
skin temperature contributed to central thermoregulatory<br />
control (β) was calculated from the slopes (S) of the skin-temperature<br />
versus core-temperature regressions, using the formula:<br />
β = S/(S − 1). Cutaneous contribution to vasoconstriction averaged<br />
20% ± 6%, which did not differ significantly from the<br />
contribution to shivering: 19% ± 8%. (Reprinted with permission<br />
from Cheng et al. 16 Copyright © Lippincott Williams &<br />
Wilkins.)
8. Perioperative <strong>The</strong>rmoregulation 109<br />
Threshold<br />
(°C)<br />
38<br />
37<br />
36<br />
35<br />
Figure 8-3. <strong>The</strong> thresholds (triggering core temperatures) for<br />
the three major autonomic thermoregulatory defenses: sweating,<br />
vasoconstriction, and shivering. Temperatures between the<br />
sweating and vasoconstriction threshold define the interthreshold<br />
range, temperatures not triggering autonomic responses.<br />
<strong>The</strong> thresholds are uniformly about 0.3°C greater during the<br />
follicular phase in women than in men, and would be an additional<br />
≈0.5°C greater during the luteal phase. However, men<br />
and women regulate core body temperature with comparable<br />
precision. Results are presented as means ± SD. (Reprinted with<br />
permission from Lopez et al. 22 Copyright © Lippincott Williams<br />
& Wilkins.)<br />
vated. Similarly, secondary defenses compensate for those<br />
working poorly. For example, when arteriovenous shunt<br />
vasoconstriction is defeated by administration of a vasodilating<br />
drug, core hypothermia will initiate shivering.<br />
Because autonomic responses are to some extent compromised<br />
in the elderly, behavioral responses are probably<br />
more important in this population—although this<br />
theory has yet to be formally evaluated.<br />
Efferent Responses<br />
Women<br />
Men<br />
Sweating Constriction Shivering<br />
Sweating is mediated by postganglionic, cholinergic<br />
nerves that terminate on sweat follicles. 29 <strong>The</strong>se follicles<br />
apparently have no purpose other than thermoregulation.<br />
In this regard, they differ from most other thermoregulatory<br />
effectors which seem to have been co-opted<br />
by the thermoregulatory system but continue to<br />
have important roles, for example vasomotion in blood<br />
pressure control or skeletal muscles in postural<br />
maintenance.<br />
Heat exposure can increase cutaneous water loss from<br />
trivial amounts to 500 mL/h. Losses in trained athletes<br />
can even exceed 1 L/h. In a dry, convective environment,<br />
sweating can dissipate enormous amounts of heat—<br />
perhaps to 10 times the basal metabolic rate. Sweating is<br />
the only thermoregulatory defense that continues to dissipate<br />
heat when environmental temperature exceeds<br />
core temperature.<br />
Active precapillary vasodilation is mediated by a yetto-be-identified<br />
factor released from sweat glands, and<br />
thus occurs synchronously with sweating. Although originally<br />
thought to be bradykinin, 30 recent evidence supports<br />
nitric oxide as the mediator. 31,32 Active dilation can<br />
increase cutaneous capillary flow enormously, perhaps to<br />
as much as 7.5 L/min. 33 <strong>The</strong> purpose of this dilation, presumably,<br />
is to transport heat from muscles and the core<br />
to the skin surface where it can be dissipated to the environment<br />
by evaporation of sweat.<br />
Active arteriovenous shunt vasoconstriction is adrenergically<br />
mediated. <strong>The</strong> shunts are 100-µm–diameter vessels<br />
that convey 10,000 times as much blood as a comparable<br />
length of 10-µm capillary. 5 Anatomically, they are restricted<br />
to the fingers, toes, nose, and nipples. Despite this restriction,<br />
shunt vasoconstriction is among the most frequently<br />
used and important thermoregulatory defenses. <strong>The</strong><br />
reason is that the blood traversing shunts in the extremities<br />
must flow through the arms and legs, thus altering heat<br />
content of these relatively large tissue masses.<br />
Shivering is an involuntary, thermogenic tonic tremor. 7<br />
Typically, it doubles metabolic rate, 34,35 although greater<br />
increases can be sustained briefly. <strong>The</strong> shivering threshold<br />
is normally ≈1°C less than the vasoconstriction threshold,<br />
suggesting that it is activated only under critical conditions<br />
and is not the preferred means of maintaining core<br />
temperature. One reason may be that shivering is a relatively<br />
inefficient response. Although shivering effectively<br />
transfers metabolic energy sources into heat, the heat is<br />
largely produced in the periphery where the largest<br />
muscles are located. Loss of the peripherally produced<br />
heat to a cold environment is further accentuated by the<br />
metabolic needs of shivering muscle and the resulting<br />
vasodilation.<br />
Impaired <strong>The</strong>rmoregulation<br />
in the Elderly<br />
<strong>The</strong>re is considerable epidemiologic evidence that the<br />
elderly often fail to adequately regulate body temperature.<br />
Accidental hypothermia is especially likely in three<br />
populations: drug abusers (especially alcoholics), people<br />
suffering extreme exposure (such as cold-water immersion),<br />
and the elderly. 36 While extreme—and usually prolonged—cold<br />
exposure is required to produce clinical<br />
hypothermia in young, healthy individuals, serious hypothermia<br />
is common among alcohol abusers even with<br />
mild exposure. 37 Hypothermia in these patients presumably<br />
results from drug-induced inhibition of thermoregulatory<br />
defenses. <strong>The</strong> extent to which alcohol impairs<br />
autonomic defenses remains controversial 38–41 ; however,<br />
alcohol at the very least significantly impairs appropriate<br />
behavioral responses to cold exposure.<br />
Hypothermia in the elderly can occur in only moderately<br />
cold environments and is typically not associated<br />
with drug use. 36,37 This observation suggests that hypo-
110 D.I. Sessler<br />
Shivering<br />
Threshold<br />
(°C)<br />
37<br />
36<br />
35<br />
34<br />
40 60 80 100<br />
Age (yr)<br />
Figure 8-4. <strong>The</strong> effect of aging on the shivering threshold.<br />
Fifteen patients aged
8. Perioperative <strong>The</strong>rmoregulation 111<br />
moregulatory control. For example, the sweating threshold<br />
is linearly increased by propofol, 54 alfentanil, 55<br />
isoflurane, 24 and desflurane. 56 Reduction of the vasoconstriction<br />
and shivering thresholds is also a linear function<br />
of propofol, 54 dexmedetomidine, 57 meperidine, 58 and<br />
alfentanil 55 concentrations. Desflurane and isoflurane,<br />
however, produce a nonlinear reduction in the major<br />
cold-response thresholds, reducing the vasoconstriction<br />
and shivering thresholds disproportionately at higher<br />
anesthetic concentrations 56 (Figure 8-5). <strong>The</strong> result is that<br />
clinical doses of all anesthetics markedly increase the<br />
interthreshold range, substantially impairing thermoregulatory<br />
defenses.<br />
Anesthetic-Induced <strong>The</strong>rmoregulatory<br />
Impairment in the Elderly<br />
39<br />
37<br />
Threshold 35<br />
(°C)<br />
33<br />
31<br />
Sweating<br />
Vasoconstriction<br />
Shivering<br />
0 0.5 0.8<br />
Desflurane (MAC Fraction)<br />
Figure 8-5. <strong>The</strong>rmoregulatory response thresholds during desflurane<br />
anesthesia. <strong>The</strong> sweating threshold increased linearly,<br />
but slightly, during desflurane anesthesia. Desflurane markedly—although<br />
nonlinearly—reduced the vasoconstriction<br />
threshold. Consequently, the interthreshold range (temperatures<br />
not triggering autonomic thermoregulatory defenses)<br />
increased enormously during desflurane administration. In contrast,<br />
the vasoconstriction-to-shivering range remained essentially<br />
unchanged. Results are presented as means ± SD. MAC =<br />
minimal anesthetic concentration. (Reprinted with permission<br />
from Annadata et al. 56 Copyright © Lippincott Williams &<br />
Wilkins.)<br />
Threshold<br />
(°C)<br />
35<br />
34<br />
33<br />
Young<br />
Intraoperative hypothermia is more common and more<br />
severe in the elderly than in younger patients. 59 Because<br />
a major cause of intraoperative hypothermia is anesthetic-induced<br />
inhibition of thermoregulatory responses,<br />
these two observations suggest that anesthetics impair<br />
thermoregulation more in elderly than in young patients.<br />
This thesis is supported by the observation that the vasoconstriction<br />
threshold is approximately 1°C lower in<br />
elderly surgical patients than in younger ones 60 (Figure<br />
8-6).<br />
Intraoperative hypothermia is not only more common<br />
in the elderly, but lasts longer postoperatively. 61 It is associated<br />
with less shivering than in younger patients, 59,62 and<br />
what shivering does occur is at a low intensity. 63 Prolonged<br />
hypothermia without shivering suggests that thermoregulatory<br />
defenses are not being activated, which is<br />
consistent with reduced perioperative vasoconstriction 60<br />
and shivering 50 thresholds in the elderly.<br />
An additional factor to consider is the age-dependent<br />
effects of anesthetic drugs. Renal and hepatic function is<br />
often reduced in the elderly. Consequently, clinically<br />
important plasma concentrations are likely to persist at<br />
high levels for longer in the elderly. Equally important,<br />
any given plasma concentrations of many drugs produce<br />
a greater effect in the elderly. <strong>The</strong> minimum alveolar<br />
concentration of volatile anesthetics, for example,<br />
decreases about 25% in the elderly. 64,65 Similarly, the<br />
effect of midazolam is markedly age-dependent. 66 Combined<br />
pharmacokinetic and pharmacodynamic augmentation<br />
of anesthetic drug effects is thus likely to further<br />
impair thermoregulation in the elderly.<br />
Perioperative Heat Balance<br />
Elderly<br />
Figure 8-6. <strong>The</strong> effect of aging on thermoregulatory vasoconstriction<br />
during general anesthesia. <strong>The</strong> vasoconstriction threshold<br />
was significantly less in the elderly (33.9 ± 0.6°C, mean ±<br />
SD) than in younger patients (35.1 ± 0.3°C) (p < 0.01). Filled<br />
squares indicate the vasoconstriction threshold in each patient;<br />
the open circles show the mean and standard deviations in each<br />
group. (Reprinted with permission from Kurz et al. 60 Copyright<br />
© Lippincott Williams & Wilkins.)<br />
Both physical and physiologic factors contribute to<br />
perioperative hypothermia. Hypothermia would be<br />
unlikely without anesthetic-induced inhibition of thermoregulatory<br />
control because thermoregulatory defenses<br />
would normally be sufficient to prevent core-temperature<br />
perturbations even in a cool operating room environment.<br />
However, all anesthetics so far tested markedly increase<br />
the range of temperatures not triggering thermoregulatory<br />
defenses. 67 Within this interthreshold range, bodytemperature<br />
changes are determined by patients’ physical<br />
interactions with their immediate environments. Larger<br />
operations and colder rooms are thus associated with greater<br />
hypothermia. Once triggered, however (in patients<br />
becoming sufficiently hypothermic), thermoregulatory
112 D.I. Sessler<br />
vasoconstriction usually prevents further hypothermia—<br />
no matter how large and long the operation might be. 68<br />
Despite multiple modalities of heat loss, each described<br />
by different (and mostly nonlinear) equations, cutaneous<br />
heat loss in patients is a roughly linear function of the<br />
difference between skin and ambient temperatures. <strong>The</strong><br />
physical laws and equations characterizing heat transfer<br />
are comparably valid for all animate and inanimate substances<br />
and, of course, apply equally in young and elderly<br />
patients.<br />
Mechanisms of Heat Transfer<br />
<strong>The</strong>re are four types of heat transfer: radiation, convection,<br />
conduction, and evaporation. 69 Among these, radiation<br />
and convection are by far the most important in<br />
patients, together accounting for approximately 85% of<br />
the total loss. 70 Fractional losses via each route are,<br />
however, determined by numerous physical and physiologic<br />
factors including incision size, amount of administered<br />
(cold) intravenous fluid, and thermoregulatory<br />
vasoconstriction.<br />
Radiative losses are mediated by photons and do not<br />
depend on any intervening media. Losses via this mechanism<br />
are related to surface properties (emissivity) and<br />
the difference of the fourth power of exposed skin and<br />
wall temperature (in degrees Kelvin). Radiative losses<br />
are thus not directly influenced by ambient temperature,<br />
although ambient temperature indirectly influences both<br />
wall and skin temperature. Radiation probably contributes<br />
about 60% to total heat loss. 70,71<br />
Conduction is defined by direct transfer of heat energy<br />
between opposing surfaces. It is related only to the insulating<br />
properties of the surfaces (or of an intervening<br />
layer) and the temperature difference between the surfaces.<br />
It is unlikely that conduction contributes more than<br />
about 5% to overall heat loss in the perioperative period.<br />
<strong>The</strong> reason conduction contributes so little is that only a<br />
small fraction of the body surface area is in direct contact<br />
with another solid surface, and that surface is likely to be<br />
the operating table mattress which is a good insulator.<br />
Body heat required to warm cold intravenous fluids is<br />
probably best considered as a conductive loss. Loss via<br />
this route usually far exceeds conventional surface-tosurface<br />
heat transfer.<br />
Convection, which is often termed “facilitated conduction,”<br />
contributes considerably more than conduction,<br />
perhaps about 25% of the total loss. Normally there is<br />
essentially no conduction into air because still air is an<br />
excellent insulator and because a small layer of still air is<br />
maintained adjacent to the skin surface. When warm air<br />
next to the skin is moved away, however, it is replaced by<br />
cool air from the surrounding environment. This air is<br />
itself warmed by extracting heat from the skin, only in<br />
turn to be replaced by additional cool air. <strong>The</strong> equation<br />
describing convection is similar to that characterizing<br />
conduction, with addition of a factor for the square root<br />
of air speed.<br />
<strong>The</strong> heat of vaporization of water is among the highest<br />
of any substances: 0.58 kcal/g. Evaporation of large<br />
amounts of water thus absorbs enormous amounts of<br />
heat, which is why sweating is such an effective defense<br />
against heat stress. Except in infants though, insensible<br />
cutaneous water loss is negligible 72,73 and evaporative<br />
heat loss a tiny fraction of the total. Evaporative loss<br />
contributes to surgical hypothermia during skin preparation<br />
when the skin surface is scrubbed with water- or<br />
alcohol-based solution that is subsequently allowed to<br />
evaporate. Because skin preparation is usually restricted<br />
to a relatively small area and because evaporation is permitted<br />
for only a brief time, total heat loss is generally<br />
relatively small. 74<br />
Water is also vaporized and lost from the lungs when<br />
they are ventilated with dry, cold gases. Numerous clinical<br />
studies 75,76 and thermodynamic calculations 77 indicate that<br />
respiratory heat loss in adults is less than 10% of the total.<br />
Other studies identify effects of airway heating and<br />
humidification on core temperature that seem difficult to<br />
reconcile with thermodynamic calculations of heat transfer<br />
78–80 ; in some cases, these aberrant results are attributable<br />
to study design flaws. (In contrast, respiratory losses<br />
are somewhat more important in infants and children<br />
than in adults. 81,82 ) And finally, heat is lost when water<br />
evaporates from exposed surfaces within surgical incisions.<br />
<strong>The</strong> extent of this loss in humans remains unknown,<br />
although clinical experience suggests that it may be substantial<br />
because patients undergoing large operations<br />
become considerably more hypothermic than those having<br />
smaller procedures. Evaporative loss from within large<br />
incisions can may be up to half of the total heat loss in<br />
animals, 83 although this ratio is likely less in humans.<br />
Distribution of Heat Within the Body<br />
Intraoperative hypothermia develops with a characteristic<br />
three-phase pattern. <strong>The</strong> first is a rapid, 1–1.5°C<br />
decrease in core temperature occurring during the first<br />
hour after induction of anesthesia. 84 This is followed by a<br />
slower, nearly linear decrease in core temperature lasting<br />
2–3 hours. 85 And finally, core temperature reaches a<br />
plateau and does not decrease further. 68 Each portion of<br />
this curve has a different etiology.<br />
<strong>The</strong> initial, rapid decrease in core temperature after<br />
induction of general anesthesia results from a core-toperipheral<br />
redistribution of body heat. Redistribution<br />
results when anesthetic-induced inhibition of tonic thermoregulatory<br />
vasoconstriction allows heat to flow from<br />
the relatively warm core thermal compartment to cooler<br />
peripheral tissues. (Surprisingly, anesthetic-induced vasodilation<br />
increases cutaneous heat loss only slightly. 86 )<br />
Although redistribution, by definition, does not alter<br />
body-heat content, it does markedly decrease core tem-
8. Perioperative <strong>The</strong>rmoregulation 113<br />
100<br />
Cutaneous<br />
Loss 80<br />
(kcal/h)<br />
60<br />
² Temp<br />
(°C)<br />
0<br />
-1<br />
-2<br />
-3<br />
-3 -2 -1 0 1 2 3<br />
Time (h)<br />
Metabolic<br />
Production<br />
(kcal/h)<br />
perature. Internal redistribution of body heat is a major<br />
cause of core hypothermia in most patients 84 (Figure 8-7).<br />
Redistribution is also a major cause of hypothermia<br />
during epidural anesthesia. 87<br />
<strong>The</strong> 2- to 3-hour-long linear decrease in core temperature<br />
results simply from heat loss exceeding heat production.<br />
75 In part, this results from an ≈30% reduction in<br />
metabolic heat production during general anesthesia. 84<br />
<strong>The</strong> slope of this curve thus depends on the difference<br />
between metabolic heat production and cutaneous and<br />
respiratory heat loss. Metabolic heat production is nearly<br />
constant during anesthesia and minimally influenced by<br />
anesthetic technique. 68,88 Respiratory heat (even with a<br />
nonrebreathing circuit and unwarmed, dry gases) loss is<br />
simply a linear function of metabolic rate. In contrast,<br />
70<br />
50<br />
30<br />
Mean Body<br />
Redistribution<br />
Core<br />
Figure 8-7. Changes in body-heat content and distribution of<br />
heat within the body during induction of general anesthesia.<br />
Heat loss and metabolic heat production were initially similar.<br />
Overall heat balance was thus near zero before induction of<br />
anesthesia (at elapsed time zero), but subsequently decreased<br />
≈31 kcal/h. <strong>The</strong> contributions of decreased overall heat balance<br />
and internal redistribution of body heat to the decrease in core<br />
temperature were separated by multiplying the change in<br />
overall heat balance by body weight and the specific heat of<br />
humans. <strong>The</strong> resulting change in mean body temperature<br />
(“mean body”) was subtracted from the change in core temperature<br />
(“core”), leaving the core hypothermia specifically<br />
resulting from redistribution (“redistribution”). After 1 hour of<br />
anesthesia, core temperature had decreased 1.6 ± 0.3°C, with<br />
redistribution contributing 81% to the decrease. During the<br />
subsequent 2 hours of anesthesia, core temperature decreased<br />
an additional 1.1 ± 0.3°C, with redistribution contributing only<br />
43%. Redistribution thus contributed 65% to the entire 2.8 ±<br />
0.5°C decrease in core temperature during the 3 hours of anesthesia.<br />
All results are shown as means ± SD. (Reprinted with<br />
permission from Matsukawa et al. 87 Copyright © Lippincott<br />
Williams & Wilkins.)<br />
cutaneous heat loss is determined largely by surface insulation<br />
and ambient temperature, and can therefore be<br />
altered by anesthetic management.<br />
After 3–4 hours of anesthesia, core temperature usually<br />
reaches a plateau and does not decrease further. This<br />
plateau is generally associated with arteriovenous shunt<br />
vasoconstriction. Vasoconstriction contributes to the<br />
plateau via two distinct mechanisms. <strong>The</strong> first is simply<br />
decreasing cutaneous heat loss. 89 <strong>The</strong> second is by constraining<br />
metabolic heat to the core thermal compartment,<br />
thus re-forming the normal core-to-peripheral<br />
temperature gradient that was obliterated by the initial<br />
redistribution hypothermia. Because heat loss may continue<br />
to exceed heat production during the core-temperature<br />
plateau, body-heat content often continues to<br />
decrease during this period—even though core temperature<br />
is constant 68 (Figure 8-8). For a detailed discussion<br />
Heat<br />
(kcal/h)<br />
Constraint<br />
(kcal)<br />
110<br />
90<br />
70<br />
50<br />
20<br />
10<br />
0<br />
-10<br />
Loss<br />
Production<br />
Core<br />
Mean Body<br />
-2 -1 0 1 2 3<br />
Elapsed Time (h)<br />
1.0<br />
0.5<br />
0.0<br />
-0.5<br />
-1.0<br />
²Temp<br />
(°C)<br />
Figure 8-8. Changes in body-heat content and distribution of<br />
heat within the body during the core-temperature plateau in<br />
anesthetized subjects. Vasoconstriction decreased cutaneous<br />
heat loss ≈25 kcal/h. However, heat loss exceeded heat production<br />
throughout the study. Consequently, mean body temperature,<br />
which decreased at a rate of ≈0.6°C/h before vasoconstriction,<br />
subsequently decreased at a rate of ≈0.2°C/h. Core temperature<br />
also decreased at a rate of ≈0.6°C before vasoconstriction, but<br />
remained virtually constant during the subsequent 3 hours.<br />
Because mean body temperature and body-heat content continued<br />
to decrease, constraint of metabolic heat to the core<br />
thermal compartment contributed to the core-temperature<br />
plateau. That is, vasoconstriction reestablished the normal coreto-peripheral<br />
temperature gradient by preventing metabolic<br />
heat (which is largely generated in the core) from escaping to<br />
peripheral tissues. Constrained heat is presented cumulatively,<br />
referenced to the onset of intense vasoconstriction defined as<br />
time zero; data are expressed as means ± SD. (Reprinted with<br />
permission from Kurz et al. 68 Copyright © Lippincott Williams<br />
& Wilkins.)
114 D.I. Sessler<br />
of perioperative heat balance, readers are referred to a<br />
recent review. 89<br />
Benefits of Mild Hypothermia<br />
Severe hypothermia (i.e., core temperatures near 28°C)<br />
has been known for decades to be protective against<br />
cerebral ischemia. 90 <strong>The</strong> basis for this protection was<br />
thought to be a decrease in the cerebral metabolic rate<br />
to about half of normal levels. 91 Although decreased metabolic<br />
rate surely contributes to hypothermic protection,<br />
there is increasing evidence that other mechanisms contribute<br />
as much or more. <strong>The</strong>se include decreased release<br />
of excitatory amino acids (such as glutamate) and free<br />
fatty acids, 92,93 inhibition of calcium/calmodulindependent<br />
protein kinase II, 94 preservation of the blood–<br />
brain barrier, 95,96 reduced synthesis of nitric oxide 97 and<br />
ubiquitin. 98<br />
More than 100 animal studies in virtually every<br />
ischemic model demonstrate that just 1–3°C brain hypothermia<br />
provides substantial protection against ischemia.<br />
93,99–102 In each case, the protection seems to far<br />
exceed that resulting simply from reduced metabolic rate.<br />
<strong>The</strong>re is also evidence that mild hypothermia also protects<br />
the spinal cord and liver against ischemia. 103 Furthermore,<br />
mild hypothermia seems protective during<br />
spinal cord ischemia 104 and is beneficial during hypoxia<br />
and shock.<br />
<strong>The</strong> benefits of mild hypothermia in ameliorating cerebral<br />
ischemia in humans have only been demonstrated<br />
after cardiac arrest. 105,106 Many neuroanesthesiologists<br />
nonetheless allow patients undergoing neurosurgery to<br />
become at least slightly hypothermic (i.e., ≈34°C) even<br />
though a major trial of hypothermia for intracranial<br />
aneurysm surgery failed to identify a benefit from therapeutic<br />
hypothermia. 107 <strong>The</strong> elderly are probably at greater<br />
risk of ischemia because of age-related vascular compromise<br />
while simultaneously being at greater risk of hypothermia-related<br />
complications.<br />
Complications of Mild Hypothermia<br />
Although once considered the major complication associated<br />
with hypothermia, shivering is now known to be a<br />
relatively unimportant response that is easily treated<br />
using a variety of techniques. Furthermore, shivering is<br />
now less common than it was previously, perhaps because<br />
the use of opioids and propofol has increased. Postoperative<br />
shivering is especially uncommon in the elderly, and<br />
its intensity modest in any case. In contrast, recent years<br />
have seen publication of numerous studies documenting<br />
other major complications of hypothermia, some of which<br />
have been shown to alter patient outcome.<br />
Table 8-1. Mild intraoperative hypothermia increases the incidence<br />
of myocardial ischemia in elderly patients.<br />
Myocardial Ischemia and Arrhythmias<br />
Myocardial infarction remains one of the leading causes of<br />
perioperative mortality. <strong>The</strong> incidence of myocardial ischemia<br />
within 24 hours of surgery is tripled by ≈2°C core<br />
hypothermia in elderly patients undergoing vascular<br />
surgery 108 (Table 8–1). Surprisingly, ischemia is not related<br />
to postoperative shivering and the mechanism by which<br />
hypothermia triggers ischemia remains unknown. One<br />
factor may be significantly increased concentrations of circulating<br />
norepinephrine, with concomitant arterial hypertension.<br />
109 Perhaps related to increased catecholamine<br />
concentrations, the incidence of ventricular tachycardia is<br />
significantly increased by mild hypothermia. 110 Hypothermia<br />
thus increases the risk of morbid perioperative cardiac<br />
outcomes, but may be therapeutically useful for preserving<br />
myocardium once an infarction has occurred.<br />
Perioperative ischemia presumably requires underlying<br />
coronary artery disease, a predisposition that would<br />
be unusual in young patients but is typical in the elderly.<br />
It is thus the elderly that are most susceptible to perioperative<br />
ischemia and have most to benefit from maintenance<br />
of perioperative normothermia.<br />
Coagulopathy and Allogeneic<br />
Transfusion Requirement<br />
Normothermic Hypothermic p Value<br />
Initial postoperative core 35.9 ± 0.1 34.2 ± 0.1
8. Perioperative <strong>The</strong>rmoregulation 115<br />
Table 8-2. Mild intraoperative hypothermia increases blood<br />
loss during hip arthroplasty.<br />
allogeneic blood transfusion, as shown in some 115,116 but<br />
not all 117 studies (Table 8-2).<br />
Surgical Wound Infections and<br />
Duration of Hospitalization<br />
Normothermic Hypothermic p Value<br />
Final intraoperative core 36.6 ± 0.4 35.0 ± 0.5
116 D.I. Sessler<br />
threshold proportionately. A typical forced-air warmer<br />
increases mean skin temperature ≈3°C, thereby reducing<br />
the shivering threshold ≈0.6°C. If a shivering patient’s<br />
core temperature is within 0.6°C of the shivering threshold,<br />
cutaneous warming can thus increase the threshold<br />
sufficiently to stop shivering. 142<br />
Numerous drugs have also been proven effective for<br />
the treatment of postoperative shivering. <strong>The</strong> prototypical<br />
drug for this purpose is meperidine, which is far more<br />
effective than equianalgesic doses of other opioids. 136 For<br />
example, meperidine reduces the shivering threshold<br />
twice as much as equianalgesic concentrations of alfentanil.<br />
55 Furthermore, meperidine markedly reduces the<br />
gain of shivering, whereas alfentanil does not. 143 <strong>The</strong><br />
special antishivering activity of meperidine was thought<br />
to result from its kappa-receptor activity, 144 but kappaopioids<br />
do not share disproportionately to reduce the<br />
shivering threshold. 145 Meperidine’s central anticholinergic<br />
activity also fails to explain this drug’s special antishivering<br />
activity. 145 Clonidine 146–148 and ketanserin 148 are<br />
also effective treatments for postoperative shivering, as<br />
are magnesium 149 and doxapram. 150–152 <strong>The</strong> efficacy of<br />
various antishivering treatments has been the subject<br />
of a recent meta-analysis. 153 For a detailed discussion of<br />
perioperative shivering, readers are referred to a recent<br />
review. 154<br />
Impaired Drug Metabolism<br />
<strong>The</strong> pharmacokinetic effects of mild hypothermia are<br />
poorly documented. Nonetheless, the duration of action<br />
of vecuronium, for example, is doubled by just 2°C core<br />
hypothermia. 155 Hypothermia prolongs the duration of<br />
action of atracurium less, ≈70% with 3°C reduction in<br />
core temperature, 156 perhaps because Hoffman elimination<br />
is relatively temperature-insensitive compared with<br />
enzymatic degradation. Antagonism of the neuromuscular<br />
block is not compromised with either drug. 155,156 And<br />
finally, steady-state plasma concentrations of propofol<br />
(during a constant-rate infusion) were increased ≈30% by<br />
3°C core hypothermia. 156<br />
Whether the pharmacokinetic effects of hypothermia<br />
are aggravated in the elderly has yet to be studied.<br />
However, drug metabolism in the elderly is often already<br />
compromised. It thus seems likely that hypothermiainduced<br />
prolongation of drug action, combined with<br />
age-related deficiencies in drug metabolism, may result<br />
in anesthetic drugs lasting unexpectedly long times in<br />
elderly, hypothermic patients. <strong>The</strong>se pharmacokinetic<br />
effects will, in many cases, be confounded by pharmacodynamic<br />
ones. Although the magnitude of these effects<br />
has yet to be quantified, it would seem prudent to prevent<br />
hypothermia in the elderly and use minimum required<br />
drug doses to minimize drug-induced thermoregulatory<br />
impairment.<br />
<strong>The</strong>rmal Management<br />
<strong>The</strong> combination of anesthetic-induced inhibition of<br />
thermoregulatory defenses and cold exposure makes<br />
most unwarmed surgical patients hypothermic. Hypothermia<br />
produces complications in both young and<br />
elderly patients, and the severity of these complications<br />
seems worse in the elderly. Consequently, active thermal<br />
management is especially important in elderly patients.<br />
<strong>The</strong> physical principles of heat transfer, however, apply<br />
equally in all patients. Thus, the same warming techniques<br />
proven effective in the general surgical population will<br />
also be useful in the elderly. For a detailed discussion of<br />
patient warming techniques, readers are referred to a<br />
recent review. 157<br />
Ambient Temperature, Passive Insulation,<br />
and Cutaneous Warming<br />
Heat loss is a (very) roughly linear function of the<br />
difference between skin and environmental temper -<br />
ature. Typical intraoperative skin temperature is near<br />
34°C, which is ≈14°C above ambient temperature.<br />
Consequently, each 1°C increase in ambient temperature<br />
reduces heat loss ≈7%. Patients become hypothermic<br />
most rapidly during the initial 30 minutes after induc -<br />
tion of anesthesia, and this is the period when patients<br />
are most likely to be undraped. However, core hypo -<br />
thermia during this period results from internal redistribution<br />
of body heat, not primarily from heat loss to<br />
the environment. 84 Increasing ambient temperature<br />
for the brief period before and after induction of<br />
anesthesia therefore has little impact on patient<br />
temperature. 158<br />
A single layer of passive insulation decreases cutaneous<br />
heat loss ≈30%. However, the type of insulation<br />
makes little difference, with the efficacy of cotton blankets,<br />
plastic bags, cloth or paper surgical drapes, and<br />
“space blankets” all being comparable 159 (Figure 8-9).<br />
Patients who remain normothermic during surgery while<br />
covered only with a single layer of insulation require no<br />
additional thermal management. But surprisingly, increasing<br />
the number of layers makes relatively little difference,<br />
reducing loss by a total of only 50%; furthermore, warm<br />
and cold blankets provide similar insulation. 160 It is thus<br />
unlikely that progressive intraoperative hypothermia will<br />
be successfully treated simply by providing additional<br />
layers of insulation. Instead, active cutaneous warming<br />
will be required.<br />
Circulating-water mattresses remain a common meth -<br />
od of thermal management, despite evidence that these<br />
devices are nearly ineffective 161 and cause pressure-heat<br />
necrosis (“burns”). 162,163 <strong>The</strong> efficacy of circulating<br />
water is restricted because relatively little heat is lost
8. Perioperative <strong>The</strong>rmoregulation 117<br />
Heat<br />
Loss<br />
(W)<br />
100<br />
80<br />
60<br />
40<br />
20<br />
0<br />
-20 0 20 40 60<br />
Time (min)<br />
from patients’ backs into the foam insulation covering<br />
most operating tables. 75 Instead, most heat is lost by<br />
radiation and convection from patients’ anterior surfaces,<br />
loss that cannot be prevented by a water mattress.<br />
Forced-air warming is far more effective than circulating<br />
water, and is safer. 161 However, recently developed circulating<br />
water garments transfer even more heat than<br />
forced-air. 164–167<br />
Fluid Warming<br />
1 Unwarmed<br />
1 Warm<br />
3 Unwarmed<br />
3 Warm<br />
Figure 8-9. Mean cutaneous heat loss during the control period<br />
(−20 to 0 elapsed minutes) and when the volunteers were<br />
covered with a single warmed or unwarmed blanket (“1 Warm”<br />
or “1 Unwarmed”) or three warmed or unwarmed blankets (“3<br />
Warm” or “3 Unwarmed”). <strong>The</strong>re was no clinically important<br />
difference between warmed and unwarmed blankets. Increasing<br />
the number of layers from one to three slightly decreased heat<br />
loss, but the decrease was unlikely to be sufficient to prevent<br />
further intraoperative hypothermia. (Reprinted with permission<br />
from Sessler and Schroeder. 160 Copyright © Lippincott<br />
Williams & Wilkins.)<br />
It is not possible to warm patients by warming intravenous<br />
fluids. Fluid warming alone is thus unlikely to maintain<br />
perioperative normothermia because it will not<br />
compensate for redistribution hypothermia, much less<br />
heat loss from the skin and from within surgical incisions.<br />
However, it is certainly possible to cool patients by<br />
administering fluids much below body temperature. <strong>The</strong><br />
amount of cooling is easy to calculate: in a typically sized<br />
adult, 1 L of fluid at ambient temperature decreases mean<br />
body temperature 0.25°C. One unit of blood at refrigerator<br />
temperatures causes a similar decrease in body temperature.<br />
168 Fluid warming should thus be restricted to<br />
patients who are already being warmed with some effective<br />
surface technique such as forced-air and in whom<br />
large amounts of fluid (>1 L/h) is being given. Cooling of<br />
fluid in tubing between warmers and patients is clinically<br />
unimportant except in the occasional neonate who<br />
requires large amounts of fluid. 169<br />
Prewarming<br />
Internal core-to-peripheral redistribution of body heat is<br />
among the most important causes of hypothermia in most<br />
patients. 84 Because the internal flow of heat is large, it has<br />
proven difficult to treat with surface warming. 75 An alternative<br />
is to prevent redistribution. One method of minimizing<br />
redistribution is to produce drug-induced<br />
peripheral vasodilation well before induction of anesthesia.<br />
Because central thermoregulatory control remains<br />
normal before induction of anesthesia, behavioral compensation<br />
protects core temperature. <strong>The</strong> result is a constant<br />
core temperature, accompanied by increased<br />
peripheral tissue temperature. Because heat flows only<br />
down a temperature gradient, induction of anesthesia is<br />
associated with little redistribution because the core-toperipheral<br />
temperature gradient is small. This concept<br />
has been demonstrated using nifedipine, 170 phenylephrine,<br />
171 and ketamine, 172 all of which support the importance<br />
of redistribution hypothermia.<br />
An alternative method of minimizing redistribution<br />
hypothermia is to actively warm peripheral tissues before<br />
induction of anesthesia. Even just 30 minutes of forcedair<br />
“prewarming” increases peripheral tissue heat content<br />
≈69 kcal, and 1 hour of prewarming transfers nearly<br />
136 kcal. 173 Either amount should be sufficient to minimize<br />
redistribution. <strong>The</strong> benefits of prewarming have<br />
been demonstrated in both volunteers 174 and surgical<br />
patients 138,175,176 (Figure 8-10). Assuming intraoperative<br />
forced-air warming is anticipated, there is no additional<br />
patient cost to prewarming because the same disposable<br />
cover can be used before and during surgery.<br />
Core<br />
Temp<br />
(°C)<br />
38<br />
37<br />
36<br />
35<br />
Before induction<br />
Prewarmed<br />
Control<br />
Surgery<br />
0 30<br />
60<br />
30<br />
60<br />
Time (min)<br />
Figure 8-10. Core temperatures during the preinduction period<br />
did not change significantly in the control group (open circles)<br />
or patients prewarmed with forced-air (solid circles). After<br />
induction of anesthesia, core temperature in the control group<br />
decreased at nearly twice the rate of that in the prewarmed<br />
patients. After 1 hour of anesthesia, core temperatures were<br />
0.6°C greater in the prewarmed patients than in the control<br />
group. Results presented as means ± SEM. (Reprinted with<br />
permission from Camus et al. 175 Copyright © 1995 Elsevier.)
118 D.I. Sessler<br />
Summary<br />
Normal thermoregulatory control is impaired in the<br />
elderly, as is thermoregulation during general anesthesia.<br />
A major factor influencing intraoperative core-temperature<br />
changes is internal core-to-peripheral redistribution<br />
of body heat that results from anesthetic-induced inhibition<br />
of thermoregulatory control. Many of the identified<br />
complications of mild perioperative hypothermia are<br />
likely to be more common or more severe in the elderly.<br />
Similarly, the core-temperature plateau results from<br />
reemergence of thermoregulatory control, which may be<br />
impaired in the elderly. In contrast, the physical factors<br />
influencing heat loss do not differ much in young and<br />
elderly patients and thermal management strategies are<br />
similar in young and elderly patients.<br />
References<br />
1. Cabanac M, Dib B. Behavioural responses to hypothalamic<br />
cooling and heating in the rat. Brain Res 1983;264:<br />
79–87.<br />
2. Satinoff E, McEwen GN Jr, Williams BA. Behavioral fever<br />
in newborn rabbits. Science 1976;193:1139–1140.<br />
3. Nadel ER, Pandolf KB, Roberts MF, Stolwijk JAJ. Mechanisms<br />
of thermal acclimation to exercise and heat. J Appl<br />
Physiol 1974;37:515–520.<br />
4. Nadel ER, Cafarelli E, Roberts MF, Wenger CB. Circulatory<br />
regulation during exercise in different ambient temperatures.<br />
J Appl Physiol 1979;46:430–437.<br />
5. Hales JRS. Skin arteriovenous anastomoses, their control<br />
and role in thermoregulation. In: Johansen K, Burggren W,<br />
eds. Cardiovascular Shunts: Phylogenetic, Ontogenetic and<br />
Clinical Aspects. Copenhagen: Munksgaard; 1985:433–451.<br />
6. Nedergaard J, Cannon B. <strong>The</strong> uncoupling protein thermogenin<br />
and mitochondrial thermogenesis. New Comp<br />
Biochem 1992;23:385–420.<br />
7. Israel DJ, Pozos RS. Synchronized slow-amplitude modulations<br />
in the electromyograms of shivering muscles.<br />
J Appl Physiol 1989;66:2358–2363.<br />
8. Jessen C, Mayer ET. Spinal cord and hypothalamus as<br />
core sensors of temperature in the conscious dog. I.<br />
Equivalence of responses. Pflügers Arch 1971;324:189–<br />
204.<br />
9. Sessler DI. Perianesthetic thermoregulation and heat<br />
balance in humans. FASEB J 1993;7:638–644.<br />
10. Satinoff E. Neural organization and evolution of thermal<br />
regulation in mammals—several hierarchically arranged<br />
integrating systems may have evolved to achieve precise<br />
thermoregulation. Science 1978;201:16–22.<br />
11. Satinoff E, Rutstein J. Behavioral thermoregulation in<br />
rats with anterior hypothalamic lesions. J Comp Physiol<br />
Psychol 1970;71:77–82.<br />
12. Poulos DA. Central processing of cutaneous temperature<br />
information. Fed Proc 1981;40:2825–2829.<br />
13. Kosaka M, Simon E, Walther O-E, Thauer R. Response of<br />
respiration to selective heating of the spinal cord below<br />
partial transection. Experientia 1969;25:36–37.<br />
14. Jessen C. Independent clamps of peripheral and central<br />
temperatures and their effects on heat production in the<br />
goat. J Physiol (Lond) 1981;311:11–22.<br />
15. Jessen C, Feistkorn G. Some characteristics of core temperature<br />
signals in the conscious goat. Am J Physiol 1984;<br />
247:R456–R464.<br />
16. Cheng C, Matsukawa T, Sessler DI, et al. Increasing mean<br />
skin temperature linearly reduces the core-temperature<br />
thresholds for vasoconstriction and shivering in humans.<br />
<strong>Anesthesiology</strong> 1995;82:1160–1168.<br />
17. Wyss CR, Brengelmann GL, Johnson JM, et al. Altered<br />
control of skin blood flow at high skin and core temperatures.<br />
J Appl Physiol 1975;38:839–845.<br />
18. Nadel ER, Mitchell JW, Stolwijk JAJ. Control of local and<br />
total sweating during exercise transients. Int J Biometeorol<br />
1971;15:201–206.<br />
19. Tam H-S, Darling RC, Cheh H-Y, Downey JA. <strong>The</strong> dead<br />
zone of thermoregulation in normal and paraplegic man.<br />
Can J Physiol Pharmacol 1978;56:976–983.<br />
20. Wenger CB, Roberts MF, Stolwijk JJA, Nadel ER. Forearm<br />
blood flow during body temperature transients produced<br />
by leg exercise. J Appl Physiol 1975;38:58–63.<br />
21. Mistlberger T, Rusak B. Mechanisms and models of the<br />
circadian time keeping system. In: Kryger MH, Dement<br />
WC, eds. Principles and Practice of Sleep Medicine. Philadelphia:<br />
WB Saunders; 1989:141–152.<br />
22. Lopez M, Sessler DI, Walter K, et al. Rate and<br />
gender dependence of the sweating, vasoconstriction, and<br />
shivering thresholds in humans. <strong>Anesthesiology</strong> 1994;80:<br />
780–788.<br />
23. Stephenson LA, Kolka MA. Menstrual cycle phase and<br />
time of day alter reference signal controlling arm blood<br />
flow and sweating. Am J Physiol 1985;249:R186–R191.<br />
24. Washington D, Sessler DI, Moayeri A, et al. <strong>The</strong>rmoregulatory<br />
responses to hyperthermia during isoflurane anesthesia<br />
in humans. J Appl Physiol 1993;74:82–87.<br />
25. Mestyan J, Jarai I, Bata G, Fekete M. <strong>The</strong> significance of<br />
facial skin temperature in the chemical heat regulation of<br />
premature infants. Biol Neonat 1964;7:243–254.<br />
26. Jessen K. An assessment of human regulatory non -<br />
shivering thermogenesis. Acta Anaesthesiol Scand 1980;24:<br />
138–143.<br />
27. Jessen K, Rabøl A, Winkler K. Total body and splanchnic<br />
thermogenesis in curarized man during a short exposure<br />
to cold. Acta Anaesthesiol Scand 1980;24:339–344.<br />
28. Joy RJT, Matone JC, Newcomb GW, Bradford WC.<br />
Responses of cold-acclimatized men to infused norepinephrine.<br />
J Appl Physiol 1963;18:1209–1212.<br />
29. Brück K. <strong>The</strong>rmoregulation: control mechanisms and<br />
neural processes. In: Sinclair JC, ed. Temperature Regulation<br />
and Energy Metabolism in the Newborn. New York:<br />
Grune & Stratton; 1978:157–185.<br />
30. Fox RH, Hilton SM. Bradykinin formation in human<br />
skin as a factor of heat vasodilatation. J Physiol 1958;142:<br />
219–232.<br />
31. Warren JB. Nitric oxide and human skin blood flow<br />
responses to acetylcholine and ultraviolet light. FASEB J<br />
1994;8:247–251.<br />
32. Hall DM, Buettner GR, Matthes RD, Gisolfi CV.<br />
Hyperthermia stimulates nitric oxide formation: electron
8. Perioperative <strong>The</strong>rmoregulation 119<br />
paramagnetic resonance detection of .NO-heme in blood.<br />
J Appl Physiol 1994;77:548–553.<br />
33. Detry J-MR, Brengelmann GL, Rowell LB, Wyss C.<br />
Skin and muscle components of forearm blood flow in<br />
directly heated resting man. J Appl Physiol 1972;32:506–<br />
511.<br />
34. Giesbrecht GG, Sessler DI, Mekjavic IB, et al. Treatment<br />
of immersion hypothermia by direct body-to-body contact.<br />
J Appl Physiol 1994;76:2373–2379.<br />
35. Horvath SM, Spurr GB, Hutt BK, Hamilton LH. Metabolic<br />
cost of shivering. J Appl Physiol 1956;8:595–602.<br />
36. Danzl DF, Pozos RS. Accidental hypothermia. N Engl J<br />
Med 1994;331:1756–1760.<br />
37. Lønning PE, Skulberg A, Abyholm F. Accidental hypothermia:<br />
review of the literature. Acta Anaesthesiol Scand<br />
1986;30:601–613.<br />
38. Kalant H, Le AD. Effects of ethanol on thermoregulation.<br />
Pharmacol <strong>The</strong>r 1984;23:313–364.<br />
39. Fellows I, Bennett T, Macdonald IA. Influence of environmental<br />
temperature on the thermoregulatory responses to<br />
ethanol. In: Hales JRS, ed. <strong>The</strong>rmal Physiology. New York:<br />
Raven Press; 1984:221–223.<br />
40. Fox GR, Hayward JS, Hobson GN. Effect of alcohol on<br />
thermal balance of man in cold water. Can J Physiol<br />
Pharmacol 1979;57:860–865.<br />
41. Hobson GN, Collis ML. <strong>The</strong> effects of alcohol upon cooling<br />
rates of humans immersed in 7.5° C water. Can J Physiol<br />
Pharmacol 1977;55:744–746.<br />
42. MacMillan AL, Corbett JL, Johnson RH, et al. Temperature<br />
regulation in survivors of accidental hypothermia of<br />
the elderly. Lancet 1967;2:165–169.<br />
43. Khan F, Spence VA, Belch JJF. Cutaneous vascular re -<br />
sponses and thermoregulation in relation to age. Clin Sci<br />
1992;82:521–528.<br />
44. Wagner JA, Robinson S, Marino RP. Age and temperature<br />
regulation of humans in neutral and cold environments.<br />
J Appl Physiol 1974;37:562–565.<br />
45. McDonald RB, Day C, Carlson K, et al. Effect of age<br />
and gender on thermoregulation. Am J Physiol 1989;257:<br />
R700–R704.<br />
46. Tankersley CG, Smolander J, Kenney WL, Fortney SM.<br />
Sweating and skin blood flow during exercise: effects of<br />
age and maximal oxygen uptake. J Appl Physiol 1991;71:<br />
236–242.<br />
47. Inoue Y, Nakao M, Araki T, Murakami H. <strong>Regional</strong> differences<br />
in the sweating responses of older and younger men.<br />
J Appl Physiol 1991;71:2453–2459.<br />
48. Falk B, Bar-Or O, Macdougall JD, et al. Sweat lactate in<br />
exercising children and adolescents of varying physical<br />
maturity. J Appl Physiol 1991;71:1735–1740.<br />
49. Yousef MK, Dill DB, Vitez TS, et al. <strong>The</strong>rmoregulatory<br />
responses to desert heat: age, race and sex. J Gerontol<br />
1984;39:406–414.<br />
50. Vassilieff N, Rosencher N, Sessler DI, Conseiller C. <strong>The</strong><br />
shivering threshold during spinal anesthesia is reduced in<br />
the elderly. <strong>Anesthesiology</strong> 1995;83:1162–1166.<br />
51. Clark RE, Orkin LR, Rovenstine EA. Body temperature<br />
studies in anesthetized man: effect of environmental temperature,<br />
humidity, and anesthesia system. JAMA 1954;<br />
154:311–319.<br />
52. Kurz A, Sessler DI, Annadata R, et al. Midazolam minimally<br />
impairs thermoregulatory control. Anesth Analg<br />
1995;81:393–398.<br />
53. Mokhtarani M, Mahgob AN, Morioka N, et al. Buspirone<br />
and meperidine synergistically reduce the shivering threshold.<br />
Anesth Analg 2001;93:1233–1239.<br />
54. Matsukawa T, Kurz A, Sessler DI, et al. Propofol linearly<br />
reduces the vasoconstriction and shivering thresholds.<br />
<strong>Anesthesiology</strong> 1995;82:1169–1180.<br />
55. Kurz A, Go JC, Sessler DI, et al. Alfentanil slightly increases<br />
the sweating threshold and markedly reduces the vasoconstriction<br />
and shivering thresholds. <strong>Anesthesiology</strong><br />
1995;83:293–299.<br />
56. Annadata RS, Sessler DI, Tayefeh F, et al. Desflurane<br />
slightly increases the sweating threshold, but produces<br />
marked, non-linear decreases in the vasoconstriction<br />
and shivering thresholds. <strong>Anesthesiology</strong> 1995;83:1205–<br />
1211.<br />
57. Talke P, Li J, Jain U, et al. Effects of perioperative dexmedetomidine<br />
infusion in patients undergoing vascular<br />
surgery. <strong>Anesthesiology</strong> 1995;82:620–633.<br />
58. Kurz A, Ikeda T, Sessler DI, et al. Meperidine decreases<br />
the shivering threshold twice as much as the vasoconstriction<br />
threshold. <strong>Anesthesiology</strong> 1997;86:1046–1054.<br />
59. Vaughan MS, Vaughan RW, Cork RC. Postoperative hypothermia<br />
in adults: relationship of age, anesthesia, and<br />
shivering to rewarming. Anesth Analg 1981;60:746–751.<br />
60. Kurz A, Plattner O, Sessler DI, et al. <strong>The</strong> threshold for<br />
thermoregulatory vasoconstriction during nitrous oxide/<br />
isoflurane anesthesia is lower in elderly than young patients.<br />
<strong>Anesthesiology</strong> 1993;79:465–469.<br />
61. Frank SM, Beattie C, Christopherson R, et al. Epidural<br />
versus general anesthesia, ambient operating room temperature,<br />
and patient age as predictors of inadvertent<br />
hypothermia. <strong>Anesthesiology</strong> 1992;77:252–257.<br />
62. Roe CF, Goldberg MJ, Blair CS, Kinney JM. <strong>The</strong> influence<br />
of body temperature on early postoperative oxygen<br />
consumption. Surgery 1966;60:85–92.<br />
63. Frank SM, Fleisher LA, Olson KF, et al. Multi -<br />
variate determinants of early postoperative oxygen consumption<br />
in elderly patients. <strong>Anesthesiology</strong> 1995;83:<br />
241–249.<br />
64. Nakajima R, Nakajima Y, Ikeda K. Minimum alveolar concentration<br />
of sevoflurane in elderly patients. Br J Anaesth<br />
1993;70:273–275.<br />
65. Stevens WC, Dolan WM, Gibbons RT, et al. Minimum<br />
alveolar concentrations (MAC) of isoflurane with and<br />
without nitrous oxide in patients of various ages. <strong>Anesthesiology</strong><br />
1975;42:197–200.<br />
66. Jacobs JR, Reves JG, Marty J, et al. Aging increases<br />
pharmacodynamic sensitivity to the hypnotic effects of<br />
midazolam. Anesth Analg 1995;80:143–148.<br />
67. Sessler DI. Perioperative hypothermia. N Engl J Med<br />
1997;336:1730–1737.<br />
68. Kurz A, Sessler DI, Christensen R, Dechert M. Heat<br />
balance and distribution during the core-temperature<br />
plateau in anesthetized humans. <strong>Anesthesiology</strong> 1995;83:<br />
491–499.<br />
69. English MJM, Farmer C, Scott WAC. Heat loss in exposed<br />
volunteers. J Trauma 1990;30:422–425.
120 D.I. Sessler<br />
70. Robins HI, Grossman J, Davis TE, et al. Preclinical trial of<br />
a radiant heat device for whole-body hyperthermia using<br />
a porcine model. Cancer Res 1983;43:2018–2022.<br />
71. Hardy JD, Milhorat AT, DuBois EF. Basal metabolism and<br />
heat loss of young women at temperatures from 22 degrees<br />
C to 35 degrees C. J Nutr 1941;21:383–403.<br />
72. Baumgart S. Radiant energy and insensible water loss in<br />
the premature newborn infant nursed under a radiant<br />
warmer. Clin Perinatol 1982;9:483–503.<br />
73. Hammarlund K, Sedin G. Transepidermal water loss in<br />
newborn infants. III. Relation to gestational age. Acta<br />
Paediatr Scand 1979;68:795–801.<br />
74. Sessler DI, Sessler AM, Hudson S, Moayeri A. Heat loss<br />
during surgical skin preparation. <strong>Anesthesiology</strong> 1993;78:<br />
1055–1064.<br />
75. Hynson J, Sessler DI. Intraoperative warming therapies:<br />
a comparison of three devices. J Clin Anesth 1992;4:<br />
194–199.<br />
76. Deriaz H, Fiez N, Lienhart A. Influence d’un filtre<br />
hygrophobe ou d’un humidificateur-réchauffeur sur<br />
l’hypothermie periopératoire. Ann Fr Anesth Réanim<br />
1992;11:145–149.<br />
77. Hendrickx HHL, Trahey GE, Argentieri MP. Paradoxical<br />
inhibition of decreases in body temperature by use of<br />
heated and humidified gases [letter]. Anesth Analg 1982;<br />
61:393–394.<br />
78. Ip Yam PC, Carli F. Maintenance of body temperature in<br />
elderly patients who have joint replacement surgery. <strong>Anesthesia</strong><br />
1990;45:563–565.<br />
79. Goldberg MI, Epstein R, Rosenblum F, et al. Do heated<br />
humidifiers or heat and moisture exchangers prevent<br />
temperature drop during lower abdominal surgery? J Clin<br />
Anesth 1992;4:16–20.<br />
80. Stone DR, Downs JB, Paul WL, Perkins HM. Adult body<br />
temperature and heated humidification of anesthetic<br />
gases during general anesthesia. Anesth Analg 1981;60:<br />
736–741.<br />
81. Bissonnette B, Sessler DI. Passive or active inspired gas<br />
humidification in infants and children. <strong>Anesthesiology</strong><br />
1989;71:381–384.<br />
82. Bissonnette B, Sessler DI. Passive or active inspired gas<br />
humidification increases thermal steady-state temperatures<br />
in anesthetized infants. Anesth Analg 1989;69:783–<br />
787.<br />
83. Roe CF. Effect of bowel exposure on body temperature<br />
during surgical operations. Am J Surg 1971;122:13–15.<br />
84. Matsukawa T, Sessler DI, Sessler AM, et al. Heat flow and<br />
distribution during induction of general anesthesia. <strong>Anesthesiology</strong><br />
1995;82:662–673.<br />
85. Kurz A, Sessler DI, Narzt E, Lenhart R. Morphometric<br />
influences on intraoperative core temperature changes.<br />
Anesth Analg 1995;80:562–567.<br />
86. Sessler DI, McGuire J, Moayeri A, Hynson J. Isofluraneinduced<br />
vasodilation minimally increases cutaneous heat<br />
loss. <strong>Anesthesiology</strong> 1991;74:226–232.<br />
87. Matsukawa T, Sessler DI, Christensen R, et al. Heat flow<br />
and distribution during epidural anesthesia. <strong>Anesthesiology</strong><br />
1995;83:961–967.<br />
88. Stevens WC, Cromwell TH, Halsey MJ, et al. <strong>The</strong> cardiovascular<br />
effects of a new inhalation anesthetic, Forane, in<br />
human volunteers at constant arterial carbon dioxide<br />
tension. <strong>Anesthesiology</strong> 1971;35:8–16.<br />
89. Sessler DI. Perioperative heat balance. <strong>Anesthesiology</strong><br />
2000;92:578–596.<br />
90. Todd MM, Warner DS. A comfortable hypothesis re -<br />
evaluated: cerebral metabolic depression and brain protection<br />
during ischemia [editorial]. <strong>Anesthesiology</strong> 1992;76:<br />
161–164.<br />
91. Hagerdal M, Harp JR, Nilsson L, Siesjo BK. <strong>The</strong> effect of<br />
induced hypothermia upon oxygen consumption in the rat<br />
brain. J Neurochem 1975;24:311–316.<br />
92. Busto R, Globus MY-T, Dietrich WD, et al. Effect of mild<br />
hypothermia on ischemia-induced release of neurotransmitters<br />
and free fatty acids in rat brain. Stroke 1989;<br />
20:904–910.<br />
93. Illievich UM, Zornow MH, Choi KT, et al. Effects of hypothermia<br />
or anesthetics on hippocampal glutamate and<br />
glycine concentrations after repeated transient global<br />
cerebral ischemia. <strong>Anesthesiology</strong> 1994;80:177–186.<br />
94. Churn SB, Taft WC, Billingsley MS, et al. Temperature<br />
modulation of ischemic neuronal death and inhibition of<br />
calcium/calmodulin-dependent protein kinase II in gerbils.<br />
Stroke 1990;21:1715–1721.<br />
95. Dietrich WD, Busto R, Halley M, Valdes I. <strong>The</strong> importance<br />
of brain temperature in alterations of the blood-brain<br />
barrier following cerebral ischemia. J Neuropathol Exp<br />
Neurol 1990;49:486–497.<br />
96. Jurkovich GJ, Pitt RM, Curreri PW, Granger DN. Hypothermia<br />
prevents increased capillary permeability following<br />
ischemia-reperfusion injury. J Surg Res 1988;44:514–521.<br />
97. Kader A, Frazzini VI, Baker CJ, et al. Effect of mild hypothermia<br />
on nitric oxide synthesis during focal cerebral<br />
ischemia. Neurosurgery 1994;35:272–277.<br />
98. Yamashita I, Eguchi Y, Kajiwara K, Ito H. Mild hypothermia<br />
ameliorates ubiquitin synthesis and prevents delayed<br />
neuronal death in the gerbil hippocampus. Stroke 1991;22:<br />
1574–1581.<br />
99. Busto R, Dietrich WD, Globus MY-T, Ginsberg MD. Postischemic<br />
moderate hypothermia inhibits CA1 hippocampal<br />
ischemic neuronal injury. Neurosci Lett 1989;101:<br />
299–304.<br />
100. Minamisawa H, Smith M-L, Siesjo BK. <strong>The</strong> effect of mild<br />
hyperthermia and hypothermia on brain damage following<br />
5, 10, and 15 minutes of forebrain ischemia. Ann Neurol<br />
1990;28:26–33.<br />
101. Sakai F, Amaha K. <strong>The</strong> effects of hypothermia on a cloned<br />
human brain glutamate transporter (hGLT-1) expressed in<br />
Chinese hamster ovary cells: –[3H]L-glutamate uptake<br />
study. Anesth Analg 1999;89:1546–1550.<br />
102. Popovic R, Liniger R, Bickler PE. Anesthetics and mild<br />
hypothermia similarly prevent hippocampal neuron death<br />
in an in vitro model of cerebral ischemia. <strong>Anesthesiology</strong><br />
2000;92:1343–1349.<br />
103. Vacanti RX, Ames A III. Mild hypothermia and Mg ++<br />
protect against irreversible damage during CNS ischemia.<br />
Stroke 1984;15:695–698.<br />
104. Pontius RG, Brockman HL, Hardy EG, et al. <strong>The</strong> use of<br />
hypothermia in the prevention of paraplegia following<br />
temporary aortic occlusion: experimental observations.<br />
Surgery 1954;36:33–38.
8. Perioperative <strong>The</strong>rmoregulation 121<br />
105. Bernard SA, Gray TW, Buist MD, et al. Treatment of<br />
comatose survivors of out-of-hospital cardiac arrest with<br />
induced hypothermia. N Engl J Med 2002;346:557–563.<br />
106. Hypothermia after Cardiac Arrest Study Group. Mild<br />
therapeutic hypothermia to improve the neurologic<br />
outcome after cardiac arrest. N Engl J Med 2002;346:<br />
549–556.<br />
107. Todd MM, Hindman BJ, Clarke WR, Torner JC. Mild intraoperative<br />
hypothermia during surgery for intracranial<br />
aneurysm. N Engl J Med 2005;352:135–145.<br />
108. Frank SM, Beattie C, Christopherson R, et al. Unintentional<br />
hypothermia is associated with postoperative myocardial<br />
ischemia. <strong>Anesthesiology</strong> 1993;78:468–476.<br />
109. Frank SM, Higgins MS, Breslow MJ, et al. <strong>The</strong> catecholamine,<br />
cortisol, and hemodynamic responses to mild<br />
perioperative hypothermia. <strong>Anesthesiology</strong> 1995;82:83–<br />
93.<br />
110. Frank SM, Fleisher LA, Breslow MJ, et al. Perioperative<br />
maintenance of normothermia reduces the incidence of<br />
morbid cardiac events: a randomized clinical trial. JAMA<br />
1997;277:1127–1134.<br />
111. Michelson AD, MacGregor H, Barnard MR, et al. Reversible<br />
inhibition of human platelet activation by hypothermia<br />
in vivo and in vitro. Thromb Haemost 1994;71:<br />
633–640.<br />
112. Valeri CR, Khabbaz K, Khuri SF, et al. Effect of skin<br />
temperature on platelet function in patients undergoing<br />
extracorporeal bypass. J Thorac Cardiovasc Surg 1992;104:<br />
108–116.<br />
113. Reed L, Johnston TD, Hudson JD, Fischer RP. <strong>The</strong> disparity<br />
between hypothermic coagulopathy and clotting studies.<br />
J Trauma 1992;33:465–470.<br />
114. Rohrer M, Natale A. Effect of hypothermia on the coagulation<br />
cascade. Crit Care Med 1992;20:1402–1405.<br />
115. Schmied H, Kurz A, Sessler DI, et al. Mild intraoperative<br />
hypothermia increases blood loss and allogeneic transfusion<br />
requirements during total hip arthroplasty. Lancet<br />
1996;347:289–292.<br />
116. Winkler M, Akça O, Birkenberg B, et al. Aggressive<br />
warming reduces blood loss during hip arthroplasty.<br />
Anesth Analg 2000;91:978–984.<br />
117. Johansson T, Lisander B, Ivarsson I. Mild hypothermia<br />
does not increase blood loss during total hip arthroplasty.<br />
Acta Anaesthesiol Scand 1999;43:1005–1010.<br />
118. Culver DH, Horan TC, Gaynes RP, et al. Surgical wound<br />
infection rates by wound class, operative procedure, and<br />
patient risk index. National Nosocomial Infections Surveillance<br />
System. Am J Med 1991;91:152S–157S.<br />
119. Bremmelgaard A, Raahave D, Beir-Holgersen R, et al.<br />
Computer-aided surveillance of surgical infections<br />
and identification of risk factors. J Hosp Infect 1989;13:<br />
1–18.<br />
120. Haley RW, Culver DH, Morgan WM, et al. Identifying<br />
patients at high risk of surgical wound infection: a simple<br />
multivariate index of patient susceptibility and wound<br />
contamination. Am J Epidemiol 1985;121:206–215.<br />
121. Leslie K, Sessler DI, Bjorksten A, et al. Propofol causes a<br />
dose-dependent decrease in the thermoregulatory threshold<br />
for vasoconstriction, but has little effect on sweating.<br />
<strong>Anesthesiology</strong> 1994;81:353–360.<br />
122. Sessler DI, Rubinstein EH, Moayeri A. Physiological<br />
responses to mild perianesthetic hypothermia in humans.<br />
<strong>Anesthesiology</strong> 1991;75:594–610.<br />
123. Chang N, Mathes SJ. Comparison of the effect of bacterial<br />
inoculation in musculocutaneous and random-pattern<br />
flaps. Plast Reconstr Surg 1982;70:1–10.<br />
124. Jonsson K, Hunt TK, Mathes SJ. Oxygen as an isolated<br />
variable influences resistance to infection. Ann Surg 1988;<br />
208:783–787.<br />
125. van Oss CJ, Absolom DR, Moore LL, et al. Effect of temperature<br />
on the chemotaxis, phagocytic engulfment, digestion<br />
and O 2 consumption of human polymorphonuclear<br />
leukocytes. J Reticuloendothel Soc 1980;27:561–565.<br />
126. Leijh CJ, Van den Barselaar MT, Van Zwet TL, et al.<br />
Kinetics of phagocytosis of Staphylococcus aureus and<br />
Escherichia coli by human granulocytes. Immunology<br />
1979;37:453–465.<br />
127. Prockop DJ, Kivirikko KI, Tuderman L, Guzman NA. <strong>The</strong><br />
biosynthesis of collagen and its disorders: part one. N Engl<br />
J Med 1979;301:13–23.<br />
128. De Jong L, Kemp A. Stoichiometry and kinetics of the<br />
prolyl 4-hydroxylase partial reaction. Biochim Biophys<br />
Acta 1984;787:105–111.<br />
129. Hunt TK, Pai MP. Effect of varying ambient oxygen tensions<br />
on wound metabolism and collagen synthesis. Surg<br />
Gynecol Obstet 1972;135:257–260.<br />
130. Jönsson K, Jensen JA, Goodson WH, et al. Tissue oxygenation,<br />
anemia, and perfusion in relation to wound healing<br />
in surgical patients. Ann Surg 1991;214:605–613.<br />
131. Sheffield CW, Sessler DI, Hunt TK. Mild hypothermia<br />
during isoflurane anesthesia decreases resistance to E. coli<br />
dermal infection in guinea pigs. Acta Anaesthesiol Scand<br />
1994;38:201–205.<br />
132. Sheffield CW, Sessler DI, Hunt TK, Scheuenstuhl H. Mild<br />
hypothermia during halothane anesthesia decreases resistance<br />
to S. aureus dermal infection in guinea pigs. Wound<br />
Repair Regen 1994;2:48–56.<br />
133. Kurz A, Sessler DI, Lenhardt RA. Study of wound infections<br />
and temperature group. Perioperative normothermia<br />
to reduce the incidence of surgical-wound infection<br />
and shorten hospitalization. N Engl J Med 1996;334:<br />
1209–1215.<br />
134. Flacke JW, Flacke WE. Inadvertent hypothermia: frequent,<br />
insidious, and often serious. Semin Anesth 1983;2:183–<br />
196.<br />
135. Flacke W. Temperature regulation and anesthesia. Int<br />
Anesthesiol Clin 1963;2:43–54.<br />
136. Guffin A, Girard D, Kaplan JA. Shivering following cardiac<br />
surgery: hemodynamic changes and reversal. J Cardiothorac<br />
Vasc Anesth 1987;1:24–28.<br />
137. Just B, Delva E, Camus Y, Lienhart A. Oxygen uptake<br />
during recovery following naloxone. <strong>Anesthesiology</strong> 1992;<br />
76:60–64.<br />
138. Just B, Trévien V, Delva E, Lienhart A. Prevention of intraoperative<br />
hypothermia by preoperative skin-surface<br />
warming. <strong>Anesthesiology</strong> 1993;79:214–218.<br />
139. Horn E-P, Sessler DI, Standl T, et al. Nonthermoregulatory<br />
shivering in patients recovering from<br />
isoflurane or desflurane anesthesia. <strong>Anesthesiology</strong> 1998;<br />
89:878–886.
122 D.I. Sessler<br />
140. Horn E-P, Schroeder F, Wilhelm S, et al. Postoperative pain<br />
facilitates non-thermoregulatory tremor. <strong>Anesthesiology</strong><br />
1999;91:979–984.<br />
141. Panzer O, Ghazanfari N, Sessler DI, et al. Shivering and<br />
shivering-like tremor during labor with and without epidural<br />
analgesia. <strong>Anesthesiology</strong> 1999;90:1609–1616.<br />
142. Sharkey A, Lipton JM, Murphy MT, Giesecke AH.<br />
Inhibition of postanesthetic shivering with radiant heat.<br />
<strong>Anesthesiology</strong> 1987;66:249–252.<br />
143. Ikeda T, Sessler DI, Tayefeh F, et al. Meperidine and alfentanil<br />
do not reduce the gain or maximum intensity of shivering.<br />
<strong>Anesthesiology</strong> 1998;88:858–865.<br />
144. Kurz M, Belani K, Sessler DI, et al. Naloxone, meperidine,<br />
and shivering. <strong>Anesthesiology</strong> 1993;79:1193–1201.<br />
145. Greif R, Laciny S, Rajek AM, et al. Neither nalbuphine nor<br />
atropine possess special antishivering activity. Anesth<br />
Analg 2001;93:620–627.<br />
146. Delaunay L, Bonnet F, Duvaldestin P. Clonidine de -<br />
creases postoperative oxygen consumption in patients<br />
recovering from general anaesthesia. Br J Anaesth 1991;<br />
67:397–401.<br />
147. Delaunay L, Bonnet F, Liu N, et al. Clonidine comparably<br />
decreases the thermoregulatory thresholds for vasoconstriction<br />
and shivering in humans. <strong>Anesthesiology</strong> 1993;<br />
79:470–474.<br />
148. Joris J, Banache M, Bonnet F, et al. Clonidine and ketanserin<br />
both are effective treatments for postanesthetic shivering.<br />
<strong>Anesthesiology</strong> 1993;79:532–539.<br />
149. Kizilirmak S, Karakas SE, Akça O, et al. Magnesium sulfate<br />
stops postanesthetic shivering. Ann NY Acad Sci 1997;<br />
813:799–806.<br />
150. Singh P, Dimitriou V, Mahajan RP, Crossley AW. Doubleblind<br />
comparison between doxapram and pethidine in the<br />
treatment of postanaesthetic shivering. Br J Anaesth 1993;<br />
71:685–688.<br />
151. Gautier H. Doxapram and shivering. Anaesthesia 1991;<br />
46:1092–1093.<br />
152. Sarma V, Fry EN. Doxapram after general anaesthesia. Its<br />
role in stopping shivering during recovery. Anaesthesia<br />
1991;46:460–461.<br />
153. Kranke P, Eberhart LH, Roewer N, Tramer MR. Pharmacological<br />
treatment of postoperative shivering: a quantitative<br />
systematic review of randomized controlled trials.<br />
Anesth Analg 2002;94:453–460.<br />
154. De Witte J, Sessler DI. Perioperative shivering: physiology<br />
and pharmacology. <strong>Anesthesiology</strong> 2002;96:467–484.<br />
155. Heier T, Caldwell JE, Sessler DI, Miller RD. Mild intraoperative<br />
hypothermia increases duration of action and<br />
spontaneous recovery of vecuronium blockade during<br />
nitrous oxide-isoflurane anesthesia in humans. <strong>Anesthesiology</strong><br />
1991;74:815–819.<br />
156. Leslie K, Sessler DI, Bjorksten AR, Moayeri A. Mild hypothermia<br />
alters propofol pharmacokinetics and increases<br />
the duration of action of atracurium. Anesth Analg<br />
1995;80:1007–1014.<br />
157. Sessler DI. Complications and treatment of mild hypothermia.<br />
<strong>Anesthesiology</strong> 2001;95:531–543.<br />
158. Roizen MF, Sohn YJ, L’Hommedieu CS, et al. Operating<br />
room temperature prior to surgical draping: effect on<br />
patient temperature in recovery room. Anesth Analg<br />
1980;59:852–855.<br />
159. Sessler DI, McGuire J, Sessler AM. Perioperative thermal<br />
insulation. <strong>Anesthesiology</strong> 1991;74:875–879.<br />
160. Sessler DI, Schroeder M. Heat loss in humans covered<br />
with cotton hospital blankets. Anesth Analg 1993;77:<br />
73–77.<br />
161. Kurz A, Kurz M, Poeschl G, et al. Forced-air warming<br />
maintains intraoperative normothermia better than circulating-water<br />
mattresses. Anesth Analg 1993;77:89–95.<br />
162. Gendron F. “Burns” occurring during lengthy surgical<br />
procedures. J Clin Eng 1980;5:20–26.<br />
163. Gendron FG. Unexplained Patient Burns: Investigating<br />
Iatrogenic Injuries. Brea, CA: Quest Publishing; 1988.<br />
164. Nesher N, Zisman E, Wolf T, et al. Strict thermoregulation<br />
attenuates myocardial injury during coronary artery bypass<br />
graft surgery as reflected by reduced levels of cardiacspecific<br />
troponin I. Anesth Analg 2003;96:328–335.<br />
165. Hofer CK, Worn M, Tavakoli R, et al. Influence of body<br />
core temperature on blood loss and transfusion requirements<br />
during off-pump coronary artery bypass grafting: a<br />
comparison of 3 warming systems. J Thorac Cardiovasc<br />
Surg 2005;129:838–843.<br />
166. Motta P, Mossad E, Toscana D, et al. Effectiveness of a<br />
circulating-water warming garment in rewarming after<br />
pediatric cardiac surgery using hypothermic cardiopulmonary<br />
bypass. J Cardiothorac Vasc Anesth 2004;18:<br />
148–151.<br />
167. Taguchi A, Ratnaraj J, Kabon B, et al. Effects of a circulating-water<br />
garment and forced-air warming on body heat<br />
content and core temperature. <strong>Anesthesiology</strong> 2004;100:<br />
1058–1064.<br />
168. Sessler DI. Consequences and treatment of perioperative<br />
hypothermia. Anesth Clin North Am 1994;12:425–456.<br />
169. Presson RGJ, Bezruczko AP, Hillier SC, McNiece WL.<br />
Evaluation of a new fluid warmer effective at low to moderate<br />
flow rates. <strong>Anesthesiology</strong> 1993;78:974–980.<br />
170. Vassilieff N, Rosencher N, Deriaz H, et al. Effect of premedication<br />
by nifedipine on intraoperative hypothermia.<br />
Ann Fr Anesth Réanim 1992;11:484–487.<br />
171. Ikeda T, Ozaki M, Sessler DI, et al. Intraoperative phenylephrine<br />
infusion decreases the magnitude of redistribution<br />
hypothermia. Anesth Analg 1999;89:462–465.<br />
172. Ikeda T, Kazama T, Sessler DI, et al. Induction of anesthesia<br />
with ketamine reduces the magnitude of redistribution<br />
hypothermia. Anesth Analg 2001;93:934–938.<br />
173. Sessler DI, Schroeder M, Merrifield B, et al. Optimal duration<br />
and temperature of pre-warming. <strong>Anesthesiology</strong><br />
1995;82:674–681.<br />
174. Hynson JM, Sessler DI, Moayeri A, et al. <strong>The</strong> effects of<br />
pre-induction warming on temperature and blood pressure<br />
during propofol/nitrous oxide anesthesia. <strong>Anesthesiology</strong><br />
1993;79:219–228.<br />
175. Camus Y, Celva E, Sessler DI, Lienhart A. Pre-induction<br />
skin-surface warming minimizes intraoperative core hypothermia.<br />
J Clin Anesth 1995;7:384–388.<br />
176. Horn EP, Schroeder F, Gottschalk A, et al. Active warm -<br />
ing during cesarean delivery. Anesth Analg 2002;94:<br />
409–414.
9<br />
Postoperative Central Nervous<br />
System Dysfunction<br />
Deborah J. Culley, Terri G. Monk, and Gregory Crosby<br />
This chapter reviews common forms and causes of central<br />
nervous system (CNS) morbidity in the elderly after<br />
routine surgery and anesthesia. <strong>The</strong>se include, in order of<br />
descending prevalence, delirium, prolonged postoperative<br />
cognitive dysfunction (POCD), and perioperative<br />
stroke. Although these same conditions are also common<br />
during and after cardiac surgery, we will not deal with<br />
those situations here because the contributing factors are<br />
somewhat different and cognitive morbidity after cardiac<br />
surgery is a topic unto itself. We begin with a brief overview<br />
of how the brain changes during healthy and pathologic<br />
aging because aging of the CNS is a prominent<br />
factor in determining susceptibility to cognitive and<br />
neurologic morbidity after surgery and anesthesia.<br />
Central Nervous System Changes<br />
of Aging<br />
Normal Aging<br />
Healthy aging is associated with significant changes in the<br />
morphology, physiology, and biochemistry of the brain<br />
(Table 9-1). Brain size and weight inevitably decline with<br />
age. <strong>The</strong>se changes begin in young adulthood but accelerate<br />
after age 60, resulting in a 15% decrease in the ratio<br />
of brain/skull volume in nonarians whereas ventricular<br />
volume triples. 1 <strong>The</strong>re are also age-associated decreases<br />
in neuronal size, loss of complexity of the dendritic tree,<br />
and a reduced number of synapses. 2 In contrast, the physiology<br />
of the cerebral circulation appears to be remarkably<br />
normal in the healthy aged. <strong>Global</strong> cerebral blood<br />
flow (CBF) is decreased 10%–20% with advanced age,<br />
not because of “hardening of the arteries,” but rather<br />
because there is less brain mass to perfuse. 3 <strong>The</strong>refore,<br />
the lower CBF seems to be a consequence of reduced<br />
metabolic demand, not a cause of it. Hence, although<br />
CBF and cerebral metabolic rate decline progressively<br />
with age, they remain tightly coupled. 4 Similarly, cerebral<br />
autoregulation and responsiveness to carbon dioxide/<br />
hypoxemia are reasonably well preserved. 5 Neurotransmitters<br />
do not fare as well. <strong>The</strong> range of neurotransmitter<br />
systems affected by aging is extensive; dopamine uptake<br />
sites, transporters, and levels are reduced, as are cortical<br />
serotonergic, α 2 and β 1 , and +-aminobutyric acid binding<br />
sites, among others. 6 Markers of central cholinergic activity<br />
also decrease, which is a finding of particular significance<br />
because failure of cholinergic neurotransmission<br />
is a central feature of Alzheimer’s disease. 7 Moreover,<br />
beginning at age 40 and continuing into late old age, there<br />
is reduced expression in the human brain of genes<br />
involved in learning and memory and neuronal survival. 8<br />
Nevertheless, not all the news is bad. Dendritic complexity<br />
and growth can increase in cognitively normal octogenarians,<br />
suggesting that neuronal mechanisms involved<br />
in neural plasticity crucial for learning and memory are<br />
retained in the aged but healthy CNS. 2 Furthermore, consistent<br />
with this concept but counter to what many of us<br />
learned in medical school, the adult brain makes new<br />
neurons and this capability is preserved, albeit at reduced<br />
levels, into old age. 9,10 Thus, although it loses some of its<br />
capacity for plasticity, the healthy brain continues to<br />
adapt and mold to its environment into old age.<br />
<strong>The</strong> real issue, however, is the degree to which these<br />
changes in brain morphology, physiology, and biochemistry<br />
affect brain function. Intellectual decline does not<br />
invariably accompany aging but it is common and there<br />
are some consistently observed changes. 11 Both reaction<br />
time and cognitive processing slow with age such that<br />
there is an inverse relationship between age and speed of<br />
motor performance, which becomes exaggerated with<br />
increasing task complexity. 12 In addition, “fluid” intelligence<br />
(i.e., the ability to dynamically evaluate, accommodate,<br />
and respond to novel environmental events)<br />
deteriorates. In contrast, vocabulary, math, and comprehension<br />
skills are reasonably well maintained, as is “crystallized”<br />
intelligence (i.e., accumulated knowledge), at<br />
least into the seventh decade of life. Not surprisingly,<br />
123
124 D.J. Culley, T.G. Monk, and G. Crosby<br />
Table 9-1. Neurobiologic changes of aging.<br />
• Decreased brain weight/volume<br />
Cell shrinkage and loss<br />
• Decreased neurotransmitter system function<br />
Acetylcholine, 5-hydroxytryptamine, dopamine, serotonin,<br />
γ aminobutyric acid, adrenergic, glutamate<br />
• Decreased neuronal gene expression<br />
• Alzheimer-type changes<br />
Amyloid plaques and neurofibrillary tangles<br />
short-term memory dysfunction is reported by 30% to<br />
50% of elders. 13 Much of this impairment is in working<br />
memory—which requires not only retention but also<br />
manipulation of information. 14 Thus, the ability to store<br />
recently processed information while simultaneously<br />
acquiring new data is compromised in the otherwise<br />
healthy aged brain.<br />
Pathologic Aging<br />
Unfortunately, not all brain aging is healthy or normal.<br />
With advanced age, the prevalence of dementia increases<br />
rapidly from 10% to 15% in persons aged 65 to nearly<br />
50% at age 85. 11 Dementia is always a disease process and<br />
is characterized by a chronic, progressive decline in cognitive<br />
performance that interferes with all cognitive domains.<br />
Although pathologic brain aging can be caused by a<br />
number of systemic and neurologic disorders (e.g., stroke,<br />
Parkinson’s disease), Alzheimer’s disease is the most<br />
common. 15 <strong>The</strong> histopathologic hallmarks of Alzheimer’s<br />
disease—neurofibrillary tangles, extracellular amyloid<br />
deposits, and neuritic plaques—are also seen in normal<br />
aging, albeit to a markedly lesser degree. 6,16 In the<br />
Alzheimer’s brain, loss of brain mass occurs at 2.5 times<br />
the rate observed in healthy aging and neurotransmitter<br />
hypofunction is likewise more pronounced. 17 Accordingly,<br />
Alzheimer’s dementia should be considered a major CNS<br />
and systemic illness; consistent with this perspective, the<br />
average lifespan from diagnosis to death is 3–4 years. 18<br />
From the perspective of CNS aging, therefore, the “take<br />
home” message is that the elderly are heterogeneous. <strong>The</strong>re<br />
is no such thing as a “typical” older person and chronologic<br />
age is often not a predictor of cognitive capability. This<br />
makes studies of this population difficult and means that<br />
any attempt to evaluate changes in cognition should include<br />
evaluation of baseline cognitive performance.<br />
Postoperative Central Nervous<br />
System Dysfunction<br />
Delirium<br />
Delirium is the most common form of cognitive impairment<br />
in hospitalized patients. It is an acute transient<br />
organic brain syndrome characterized by disturbances of<br />
consciousness and cognition that develop over a relatively<br />
short period of time (hours to days) and fluctuate<br />
over the course of the day. Delirium can nonetheless be<br />
subtle enough that it is frequently underdiagnosed by<br />
health care providers. <strong>The</strong> diagnosis is based on Diagnostic<br />
and Statistical Manual-IV diagnostic criteria, which<br />
include disturbance of consciousness with altered awareness<br />
of the environment; reduced ability to focus, sustain<br />
or shift attention; and a change in cognition or development<br />
of perceptual disturbances that are not better<br />
accounted for by a preexisting, established, or evolving<br />
dementia. 19 Delirium is generally divided into three types:<br />
hyperactive, hypoactive, and mixed. Agitation, irritability,<br />
restlessness, and aggression characterize the hyperactive<br />
form whereas hypoactive delirium is typified by somnolence,<br />
latency in reaction and response to verbal stimulation,<br />
and psychomotor slowing. As noted above, the<br />
diagnosis can be difficult for nonpsychiatrists to make,<br />
meaning many cases go undetected. To aid medical personnel<br />
without psychiatric training in this regard, a simple,<br />
standardized assessment tool has been developed. That<br />
tool, the Confusion Assessment Method (CAM), is the<br />
most widely used instrument for diagnosing delirium<br />
because it has the benefits of ease, speed, reliability, and<br />
validity (Table 9-2). 20 A variant of the CAM, the CAM-<br />
ICU, has been validated for delirium assessment of intubated,<br />
nonverbal patients in an intensive care unit. 21<br />
Delirium is common in hospitalized elderly patients<br />
regardless of whether the hospitalization is for medical<br />
Table 9-2. Confusion assessment method.*<br />
1. Acute onset and fluctuating course<br />
Is there evidence of an acute change in mental status from the<br />
patient’s baseline?<br />
AND<br />
Did this behavior tend to come and go or increase and decrease in<br />
severity during the past day?<br />
2. Inattention<br />
Does the patient have difficulty focusing attention (i.e., easily<br />
distractible or having difficulty keeping track of what is being<br />
said)?<br />
3. Disorganized thinking<br />
Is the patient’s speech disorganized or incoherent (rambling or<br />
irrelevant conversations, unclear or illogical flow of ideas, or<br />
unpredictable switching from subject to subject)?<br />
4. Altered level of consciousness<br />
Is the patient’s level of consciousness alert (normal), vigilant<br />
(hyperalert), lethargic (drowsy, easily aroused), stuporous (difficult<br />
to arouse), or comatose (unarousable)?<br />
Source: Adapted with permission from Inouye et al. 20<br />
*<strong>The</strong> diagnosis of delirium requires features 1 and 2 plus either 3<br />
or 4.
9. Postoperative Central Nervous System Dysfunction 125<br />
or surgical reasons. It occurs as a comorbidity in 40% of<br />
elderly, hospitalized medical patients. 22 Postoperative<br />
delirium is also quite common in surgical patients but the<br />
reported incidence varies from 9% to 74%, probably<br />
reflecting differences in the study population, diagnostic<br />
criteria, and the methods of surveillance. 23–27 Delirium<br />
usually presents during postoperative days 1–4, often<br />
following a lucid interval. Postoperative delirium has traditionally<br />
been considered a temporary or transient phenomenon<br />
but it can last for days to weeks after the<br />
surgical procedure, extend hospital stay, increase costs,<br />
and may even be a marker for subsequent cognitive<br />
deterioration and predictor of higher mortality.<br />
Conditions contributing to delirium can be divided into<br />
nonmodifiable and modifiable factors and there are clinical<br />
prediction algorithms that take these into account. 28<br />
Among the former, age greater than 70 years, preexisting<br />
cognitive impairment, a history of delirium, depression,<br />
multiple comorbidities, and poor functional status are<br />
positive predictors for the development of postoperative<br />
delirium. 25,28–31 Also included in this category is the type<br />
of surgical procedure; organ transplantation, orthopedic,<br />
cardiac, thoracic, major vascular, and emergency surgery<br />
carry the greatest risk. 23 <strong>The</strong> duration of surgery, however,<br />
does not seem to be a risk factor.<br />
<strong>The</strong> modifiable factors are more interesting because of<br />
the potential to intervene. Among the more obvious of<br />
these is the type of anesthesia but, surprisingly, the anesthetic<br />
technique does not seem to affect delirium risk. 23,27<br />
Specifically, there is no benefit of regional anesthesia.<br />
However, certain anesthetic adjuvants such as benzodiazepines<br />
and anticholinergic drugs may increase the risk<br />
of postoperative delirium perhaps, at least in the latter<br />
case, by reducing further cholinergic neurotransmission<br />
in the already compromised elderly brain. 26,32,33 Thus,<br />
regardless of whether an elderly patient requires regional<br />
or general anesthesia, one should choose anesthetic adjuvants<br />
carefully and consider using an anticholinergic<br />
agent that does not readily cross the blood–brain barrier<br />
(e.g., glycopyrrolate) if such an agent is needed. <strong>The</strong> roles<br />
of perfusion pressure and oxygen delivery have also been<br />
investigated. Intraoperative hypotension may contribute<br />
to the development of postoperative delirium but not all<br />
studies agree. 23,34,35 For example, in elderly patients having<br />
knee surgery under epidural anesthesia, those randomly<br />
assigned to a mean arterial blood pressure (MAP) of<br />
45–55 mm Hg were no more or less likely to develop postoperative<br />
delirium than those whose MAP was maintained<br />
between 55–70 mm Hg. 35 In a similar vein, there is<br />
evidence that low perioperative hematocrit is associated<br />
with development of postoperative delirium. 23 However,<br />
no studies have investigated whether blood transfusion<br />
decreases the incidence. 23 Hypoxia may in subtle ways<br />
also be a factor. That is, delirium may be a delayed manifestation<br />
of hypoxia, with nocturnal oxygen desaturation<br />
by pulse oximetry on postoperative day 2 correlating with<br />
altered mental status on day 3. 36,37 Whether enhancing<br />
oxygen delivery with supplemental oxygen or blood<br />
transfusion reduces the incidence of delirium is another<br />
matter but hypoxemia is best avoided or treated.<br />
Pain can be an important contributor to delirium in the<br />
postoperative period. Elderly, cognitively intact patients<br />
with undertreated postoperative pain are nine times<br />
more likely to develop delirium than those whose pain is<br />
adequately treated. 38 In fact, the specifics of pain treatment<br />
are less important so long as the pain is<br />
controlled. 26,39 Thus, in a study comparing intravenous<br />
fentanyl with epidural analgesia for management of postoperative<br />
pain after bilateral total knee replacement<br />
surgery, the incidence of postoperative delirium was<br />
similar. 26 Indeed, in the postoperative period, low but not<br />
high narcotic utilization is a factor in the development of<br />
delirium. 26,32,38 This is relevant because studies show that<br />
cognitively impaired patients receive only 30%–50% as<br />
much narcotic as cognitively intact patients. This suggests<br />
that suboptimal pain management in demented and delirious<br />
patients may contribute further to their cognitive<br />
deterioration. 38,40 Meperidine is an exception to this rule<br />
and should probably be avoided in geriatric patients<br />
because it has been associated with the development of<br />
postoperative delirium, presumably attributable either to<br />
accumulation of toxic metabolites or its anticholinergic<br />
activity. 32,38<br />
Perhaps the most important way to mitigate the risk of<br />
postoperative delirium is with attentive, careful medical<br />
management. This is because numerous medical complications<br />
including hypoxemia, sepsis, electrolyte and<br />
metabolic disturbances, cardiopulmonary events such as<br />
myocardial ischemia or pneumonia, and inadequate<br />
nutrition can trigger delirium. 37 As such, one should expeditiously<br />
identify and treat these complications. Medications<br />
can be another problem. More than six medications<br />
or three new inpatient medications have been shown to<br />
be precipitating factors for delirium, as have drugs with<br />
anticholinergic properties that cross the blood–brain<br />
barrier (i.e., atropine, scopolamine). 33,41,42 Hence, eliminating<br />
unnecessary or potentially toxic medications may<br />
be helpful. Another potentially beneficial intervention is<br />
ambulation. This is best studied in orthopedic surgical<br />
patients but, given evidence that even minimal exercise<br />
preserves cognition, is likely to be worthwhile for any<br />
bedridden hospitalized elderly person. 43–45 Accordingly,<br />
early ambulation may be an important and simple way to<br />
prevent postoperative delirium.<br />
Delirium and Adverse Outcomes<br />
Postoperative delirium is associated with significant morbidity<br />
and mortality. 25,28,31,46 <strong>The</strong> cost of care increases<br />
because of longer hospitalization and, reflecting a decline
126 D.J. Culley, T.G. Monk, and G. Crosby<br />
in activities of daily living, the patient must often be<br />
placed in a long-term care facility. Postoperative delirium<br />
may also be a predictor of subsequent dementia; in one<br />
small study of cognitively intact elderly patients, nearly<br />
70% of those who developed postoperative delirium were<br />
demented 5 years later whereas only 20% of those who<br />
did not experience delirium became demented. 34 Moreover,<br />
5-year mortality was 70% in the patients that had<br />
postoperative delirium whereas it was 35% in those who<br />
remained cognitively intact postoperatively. 34 Although it<br />
is unclear whether delirium triggers a dementing process<br />
or is simply a marker for preclinical dementia, it is apparent<br />
that postoperative delirium has important short- and<br />
long-term implications for the elderly patient.<br />
Treatment/Prevention<br />
Effective prevention and treatment of delirium is hampered<br />
by the fact that some risk factors (e.g., advanced<br />
age, preexisting cognitive impairment, type of surgical<br />
procedure) are not modifiable and by poor understanding<br />
of how the aged brain responds to the rigors of surgery,<br />
anesthesia, and hospitalization. Thus, the mainstay of<br />
treatment remains prompt diagnosis and treatment of the<br />
underlying medical conditions and/or discontinuation of<br />
unnecessary or toxic medications. Once this is done,<br />
attention should be directed toward creating a calm, quiet<br />
environment populated with the familiar faces of the<br />
patient’s family and friends. Although scientific rationale<br />
for this recommendation is lacking, there is a growing<br />
body of evidence that a broad spectrum of preventative<br />
interventions may be modestly effective. Specifically,<br />
pre- and postoperative geriatric consultation decreases<br />
the incidence of delirium by as much as 30%, offering<br />
hope that relatively simple measures may be useful in<br />
decreasing the incidence and/or severity of postoperative<br />
delirium. 46,47 That said, there is no evidence that such<br />
programs improve the outcome of patients who still<br />
become delirious.<br />
<strong>The</strong> role of medications in treating perioperative delirium<br />
is a controversial topic, with some experts arguing<br />
that pharmacologic intervention prolongs the delirious<br />
phase. Low-dose haloperidol is still considered the standard<br />
for treatment of hyperactive delirium but evidence<br />
for its efficacy is not as strong as one might like and atypical<br />
antipsychotics such as risperidone and olanzapine,<br />
although gaining in popularity, lack evidence from welldesigned<br />
clinical studies to demonstrate superiority. 48,49<br />
Before embarking on a course of pharmacotherapy,<br />
however, one should be aware of the unique pharmacology<br />
of psychoactive agents in the elderly. First, as mentioned<br />
previously, three or more new inpatient medi -<br />
cations is an independent precipitating factor for delirium<br />
in hospitalized elderly persons. 42 This suggests that sometimes<br />
discontinuing medications is the best course of<br />
action. Second, certain frequently used sedatives can<br />
actually increase delirium risk. Diphenhydramine, often<br />
prescribed for sleep or sedation in elderly hospitalized<br />
patients, nearly doubles the risk of delirium. 50 Meperidine,<br />
but not other opiates, nearly triples the risk. 32 Third,<br />
given the paucity of sound clinical evidence to guide the<br />
choice of pharmacologic agents for treating delirium in<br />
elderly postoperative patients and their greater susceptibility<br />
to psychoactive medications, some drugs are used<br />
inappropriately. Even atypical antipsychotics such as<br />
haloperidol, the mainstay of pharmacologic treatment of<br />
agitated delirium, are often given in dosages higher than<br />
those recommended for elderly patients and have a high<br />
incidence of extrapyramidal and anticholinergic side<br />
effects. 51 Lorazepam and other benzodiazepines, used for<br />
sedation or anxiolysis, have themselves been implicated<br />
in the development of delirium and can produce a paradoxic<br />
reaction of agitation and disinhibition. 51 Thus, pharmacotherapy<br />
has a place in the management in agitated<br />
delirium in the elderly postsurgical patient but one should<br />
resort to it only after seeking and treating remediable<br />
medical or pharmacologic causes of delirium and abiding<br />
by the geriatrician’s adage to “start low and go slow.”<br />
Postoperative Cognitive Dysfunction<br />
It has been suspected for more than 50 years that general<br />
anesthesia and surgery lead to cognitive dysfunction in<br />
the elderly. 52 Interest in the topic is increasing, driven<br />
partially by patients (or their family members) who often<br />
complain that the ability to think and concentrate is<br />
impaired for months after surgery and anesthesia. 53<br />
Recent work justifies concern but we are still far from<br />
sure about the etiology of the problem. 54,55 What is clear<br />
is that the structural and functional changes associated<br />
with normal aging render the elderly more vulnerable to<br />
the development of mild POCD. 56<br />
Since Bedford, in a retrospective chart review, first<br />
reported in 1955 that general anesthesia produces longterm<br />
cognitive dysfunction in the elderly, there have been<br />
numerous subsequent studies of the problem. 52–54 Most<br />
are flawed or inconclusive because they lack a control<br />
group, did not perform formal neuropsychometric testing,<br />
or were small and retrospective. That changed in 1998<br />
with publication of a large, prospective, controlled international<br />
study. <strong>The</strong> International Study of Postoperative<br />
Cognitive Dysfunction (ISPOCD1) included 1218 patients<br />
aged 60 years or older from 13 hospitals in eight European<br />
countries and the United States who underwent a<br />
variety of noncardiac, nonneurosurgical procedures plus<br />
176 United Kingdom and 145 nonhospitalized, community<br />
controls. 57 Cognitive performance was assessed with<br />
a battery of neuropsychometric tests completed before<br />
surgery as well as 1 week and approximately 3 months<br />
after surgery. Using this design, nearly a quarter of elderly
9. Postoperative Central Nervous System Dysfunction 127<br />
Table 9-3. Incidence of cognitive dysfunction after surgery and<br />
general anesthesia in the elderly.<br />
Control Surgery and anesthesia<br />
(321) (1218)<br />
1 week postoperatively 3.4% 25.8%*<br />
3 months postoperatively 2.8% 9.9%†<br />
Source: Moller et al. 57<br />
*p < 0.01.<br />
†p < 0.0001.<br />
patients had cognitive deficits the first week after surgery<br />
and general anesthesia and, more remarkably, almost<br />
10% were still impaired 3 months postoperatively (Table<br />
9-3). 57 In contrast, only about 3% of the age-matched<br />
community controls were impaired. 57 A subsequent study<br />
of middle-aged patients (40–60 years) using similar<br />
methods and criteria for impairment found a slightly<br />
lower incidence of cognitive impairment during the first<br />
postoperative week (19%) but no residual deficit by<br />
objective testing at 3 months postoperatively (Table<br />
9-4). 58 However, 29% of the patients felt subjectively<br />
impaired at 3 months, associated in many cases with<br />
depression. Together, these studies convincingly demonstrate<br />
that middle-aged and elderly patients experience<br />
short-term cognitive dysfunction after surgery<br />
and general anesthesia but that, judging by objective criteria,<br />
the elderly are uniquely vulnerable to persistent<br />
cognitive impairment. Further substantiating the agedependence<br />
of POCD is the fact that incidence is highest<br />
among patients 75 years of age or older, with nearly 15%<br />
impaired at 3 months postoperatively. 57<br />
<strong>The</strong> natural history of POCD in the elderly has not<br />
been thoroughly studied but there is some encouraging<br />
news. <strong>The</strong> only follow-up study reevaluated 336 older<br />
adults and 47 controls from the English and Danish sites<br />
of the original ISPOCD1 study and found that 35 of the<br />
336 tested (10.4%) still had cognitive dysfunction 1–2<br />
years later. 59 However, among the 47 controls who had<br />
not been hospitalized, 10.6% (n = 5) also met criteria for<br />
POCD—an incidence similar to that of the surgery<br />
patients. Thus, in elderly persons, cognitive changes occur<br />
over time even when surgery is not performed. This<br />
emphasizes the importance of a control group in studies<br />
Table 9-4. Incidence of cognitive dysfunction after surgery and<br />
general anesthesia in middle-aged patients.<br />
Control Surgery and anesthesia<br />
(183) (463)<br />
1 week postoperatively 4.0% 19.2%*<br />
3 months postoperatively 4.1% 6.2%<br />
Source: Johnson et al. 58<br />
*p < 0.001.<br />
Table 9-5. Potential risk factors for postoperative cognitive<br />
dysfunction.<br />
• Patient<br />
Age<br />
Educational level<br />
Mental health status<br />
Preoperative alcohol, benzodiazepine use<br />
Comorbidities<br />
• Physiology<br />
Inadequate oxygen delivery (hypoxia, hypotension, hypocarbia,<br />
anemia)<br />
• Surgery<br />
Inpatient versus outpatient<br />
Duration<br />
Type (cardiac/thoracic, orthopedic, major abdominal)<br />
Stress<br />
Immobility<br />
• <strong>Anesthesia</strong><br />
investigating POCD and suggests that POCD is a reversible<br />
condition in the majority of elderly patients undergoing<br />
general surgery. That said, the small size of the study<br />
prevents firm conclusions and other considerations give<br />
reason for concern. First, of the 318 surgery patients who<br />
completed cognitive testing at each of the three time<br />
points postoperatively (discharge, 3 months, 1–2 years),<br />
three met criteria for POCD at every one. <strong>The</strong> likelihood<br />
that the same subject would meet criteria for POCD<br />
at all three times by chance is remote (1:64,000 or<br />
0.0002%), making it probable that POCD is permanent<br />
in some persons. Second, 2-year follow-up may not be<br />
sufficient. In a prospective but uncontrolled study of<br />
cardiac surgery patients, for instance, the incidence of<br />
cognitive impairment decreased from 53% at hospital<br />
discharge to 24% at 6 months postoperatively but<br />
increased again to 42% by 5 years postoperatively. 60 Such<br />
longer-term follow-up of noncardiac patients with POCD<br />
is not yet available.<br />
<strong>The</strong> search for causes of POCD and ways it might be<br />
prevented or treated is under way but is complicated by<br />
the fact that it is likely to be a complicated entity with<br />
numerous contributing factors. For the purposes of this<br />
review, we will group them into patient, surgical, physiologic,<br />
and anesthetic conditions (Table 9-5).<br />
Patient Factors<br />
Advanced age is the most consistent and least controversial<br />
risk factor for POCD in both cardiac and noncardiac<br />
surgery. 55,57,58,61 <strong>The</strong> close association between age and<br />
POCD implies that the normal and pathologic changes<br />
of brain aging contribute in an important way. <strong>The</strong> association<br />
between age and POCD is most clearly demonstrated<br />
by the ISPOCD investigations discussed above.<br />
<strong>The</strong> key difference between elderly and middle-aged<br />
patients in this regard is that objective impairment
128 D.J. Culley, T.G. Monk, and G. Crosby<br />
persists for at least 3 months in the former but not the<br />
latter. 57,58 Thus, POCD may be problematic for many<br />
adult patients early during recuperation, but it is primarily<br />
older patients who experience subtle cognitive dysfunction<br />
for a longer period of time.<br />
Other putative patient-related risk factors include<br />
years of education, mental health, comorbid diseases,<br />
gender, and genetics. A low level of education predicts<br />
cognitive decline at 3 months after noncardiac surgery<br />
and, conversely, education seems to protect against cognitive<br />
decline after surgery involving cardiopulmonary<br />
bypass. 57,61 <strong>The</strong> reasons for this protective effect of formal<br />
education are unknown, but possibilities include greater<br />
“cognitive reserve,” better test-taking abilities in the<br />
better educated, and known interrelationships between<br />
educational advancement, social support, and quality of<br />
medical care. <strong>The</strong> roles of preexisting mental health status<br />
and comorbid conditions in POCD are difficult to ascertain.<br />
In the ISPOCD studies, there was no association<br />
between functional status, as defined by American Society<br />
of Anesthesiologists physical status classification, and the<br />
development of POCD in elderly patients whereas it was<br />
a predictor of early POCD in middle-aged patients. 57,58<br />
Similarly, whereas presurgical depression is associated<br />
with POCD in middle-aged patients, its contribution to<br />
POCD in the elderly has not been systematically evaluated.<br />
58 <strong>The</strong> main reason data on these subjects are limited<br />
is that most studies of POCD exclude individuals who<br />
have major depression or anxiety disorders, multiple systemic<br />
disease, severe systemic illness, or perform below a<br />
certain cognitive level on screening measures. 57,58,62<br />
Indeed, even when comorbidity is entered into the final<br />
multivariate analyses as a possible predictor, the indices<br />
and score range (e.g., Charlson Comorbidity Index) may<br />
be too insensitive to serve as a viable predictor of POCD. 63<br />
<strong>The</strong> role of gender in POCD is also unresolved because<br />
the ISPOCD1 study found no differences in the incidence<br />
of POCD by gender 57 but evidence from cardiac surgery<br />
hints that it could be a factor under some circumstances.<br />
Thus, although the frequency of cognitive impairment<br />
after cardiac surgery is statistically equivalent between<br />
genders, women decline on tasks believed to depend<br />
more on the frontal lobes and right hemisphere and have<br />
worse functional outcome and decreased quality of life<br />
than men. 64,65 Likewise, women have a higher risk for<br />
perioperative neurologic deficits than men after cardiac<br />
surgery. 66 Finally, largely unexplored are genetic factors.<br />
<strong>The</strong> only gene investigated thus far is the apolipoprotein<br />
ε4 (apoE4) allele, a gene that has been associated with<br />
greater vulnerability of the brain to various insults such<br />
as Alzheimer’s disease and head trauma. 67–69 Although no<br />
link with POCD risk was identified, more studies of this<br />
nature should be forthcoming because it is likely that<br />
certain patients are predisposed to POCD by virtue of<br />
their unique genetic profile.<br />
Preoperative drug usage—particularly for alcohol and<br />
benzodiazepines—is another potentially important risk<br />
factor for POCD. 58 Here again, the data are mixed. In the<br />
elderly undergoing a major surgical procedure, there is<br />
no association between moderate preoperative alcohol<br />
consumption and susceptibility to POCD but, curiously,<br />
lack of preoperative alcohol consumption predicts early<br />
POCD in middle-aged patients and aged patients undergoing<br />
minor surgical procedures. 57,58,70 With respect to<br />
benzodiazepines, there was a favorable association<br />
between preoperative usage and protection against<br />
POCD 3 months postoperatively, 57 but this is likely attributable<br />
to a change in use of benzodiazepines postoperatively.<br />
Nearly half of the patients using benzodiazepines<br />
preoperatively in that study were no longer taking them<br />
3 months postoperatively; among these, none met POCD<br />
criteria. In contrast, those patients still taking benzodiazepines<br />
3 months postoperatively had an incidence of<br />
POCD similar to the study population as a whole. <strong>The</strong><br />
most reasonable interpretation of these data is that discontinuation<br />
of benzodiazepines postoperatively, not<br />
preoperative usage, improves cognitive performance. <strong>The</strong><br />
fact that there is also no correlation between blood concentration<br />
of benzodiazepines and POCD 1 week postoperatively<br />
71 supports this conclusion.<br />
Surgery/Illness Factors<br />
Not surprisingly, the type, duration, and complexity of<br />
surgery seem to contribute to the risk of POCD. Thus,<br />
elderly patients undergoing minor surgical procedures<br />
have a lower incidence of both early and late POCD than<br />
those undergoing major procedures 57,70 and, even when<br />
controlling for the nature and duration of the surgical<br />
procedure, the incidence of early POCD is lowest in<br />
patients cared for on an outpatient versus inpatient<br />
basis. 70 This suggests that for minor surgical procedures,<br />
an outpatient setting may benefit the elderly and that<br />
postoperative hospitalization contributes importantly to<br />
development of POCD. Similarly, the duration of the procedure<br />
(and hence the anesthetic) has repeatedly been<br />
associated with development of POCD, such that risk is<br />
greater with longer procedures. 57,58<br />
<strong>The</strong> type of operation also matters, at least in middleaged<br />
persons. In elderly patients, the incidence of POCD<br />
at either 1 week or 3 months postoperatively does not<br />
correlate with the type of surgical procedure but in<br />
middle-aged adults the incidence at 1 week is highest<br />
after upper abdominal (33%) and orthopedic surgery<br />
(20%). 57,58 <strong>The</strong> reasons for these associations are not<br />
known but proposed mechanisms include endotoxin<br />
release and cerebral emboli. Interleukin-6 and -8 increase<br />
during major abdominal surgery, perhaps because of<br />
bowel hypoperfusion or manipulation. 72 Interleukins,<br />
which act on the CNS, are peptide mediators of the
9. Postoperative Central Nervous System Dysfunction 129<br />
systemic inflammatory cascade and are stimulated by<br />
endotoxin, a component of the gram-negative bacterial<br />
cell wall. 73 Although no studies have directly investigated<br />
the role of interleukins in POCD in general surgical<br />
patients, evidence from cardiac surgery shows that a low<br />
preoperative level of an antiendotoxin core antibody is<br />
associated with POCD. 73 This suggests that a reduced<br />
immune response to endotoxin may contribute to development<br />
of POCD. In the case of POCD after orthopedic<br />
surgery, indirect evidence suggests cerebral microemboli<br />
could be a culprit. Fatty emboli are common during<br />
certain orthopedic procedures (e.g., total knee replacement)<br />
and many reach the brain via paradoxical embolization<br />
through a patent foramen ovale or the pulmonary<br />
vasculature. 74,75 Although a plausible mechanism for cognitive<br />
decline in these patients, the hypothesis has not<br />
yet been systematically tested.<br />
Surgery, and the associated illness requiring it, may also<br />
contribute to POCD indirectly. Surgery involves stress,<br />
loss of mobility, and oftentimes social isolation, each of<br />
which has been associated with cognitive deterioration in<br />
the elderly. For instance, chronically elevated plasma cortisol<br />
is associated with hippocampal atrophy and impaired<br />
cognitive performance. 76 Similarly, given substantial evidence<br />
that modest physical exercise and social involvement<br />
improves cognitive performance in both the healthy<br />
and cognitively impaired elderly, 43,44,77 it is easy to see how<br />
a stressed, relatively immobile, socially isolated elderly<br />
surgical patient may suffer cognitive consequences.<br />
Physiologic Factors<br />
Perhaps the oldest and most intuitive hypothesis is that<br />
perioperative hypoxia or hypotension has a role in the<br />
development of POCD. Unfortunately, POCD does not<br />
seem to be that simple. In particular, in the large international<br />
study, there was no correlation between perioperative<br />
hypotension (MAP 2 minutes) and POCD in the elderly. 57<br />
Moreover, another study of elderly patients having<br />
knee arthroplasty under epidural anesthesia found no<br />
difference in cognitive outcome between those maintained<br />
at a MAP of 45–55 versus 55–70 mm Hg. 35 This is<br />
not to say that perioperative hypoxia or hypotension<br />
cannot cause significant CNS impairment—because we<br />
know it can—but rather that variations of the magnitude<br />
and duration that characterize routine, uncomplicated<br />
anesthesia do not seem to be responsible for the subtle<br />
but persistent perioperative cognitive changes that define<br />
POCD.<br />
Other physiologic conditions that influence cerebral<br />
oxygenation have also been implicated but, again, with<br />
limited evidence. Anemia is one such factor. Anemia<br />
obviously occurs sometimes during surgery and is associated<br />
with changes in CBF and oxygenation in animals. 78<br />
Nevertheless, support for a link to cognitive dysfunction<br />
is indirect, coming mainly from evidence that isovolemic<br />
anemia to a hemoglobin concentration of 5–6 g/dL in<br />
healthy adults is associated with subtle changes in cognitive<br />
functioning and that normalizing hematocrit with<br />
erythropoietin in chronic renal failure patients improves<br />
cognitive performance. 79,80 For similar reasons (i.e.,<br />
reduced cerebral oxygen delivery), there has been concern<br />
about inadvertent hyperventilation. Studies that have<br />
looked at this are too small to be conclusive but fail to<br />
identify an adverse effect of hyperventilation on cognition<br />
and even suggest that mild hypoventilation is worse<br />
in this regard than mild hyperventilation. 81<br />
Anesthetic Factors<br />
Despite the fact that general anesthesia is obviously a<br />
form of profound CNS dysfunction, its role in prolonged<br />
cognitive impairment has received surprisingly little<br />
attention. <strong>The</strong>re is clinical evidence that general anesthesia<br />
contributes to early POCD, with one study showing a<br />
higher incidence after general, as opposed to regional,<br />
anesthesia 1 week postoperatively 82 and several demonstrating<br />
an association between POCD and the duration<br />
of anesthesia. 57,58 Prolonged POCD is another matter.<br />
Some studies show that the risk of POCD is similar with<br />
regional or general anesthesia. For instance, the frequency<br />
of cognitive impairment 6 months postoperatively was<br />
similar (4%–6%) between epidural and general anesthesia<br />
in elderly patients undergoing total knee replacement,<br />
but the study lacked a concurrent control. 62 Moreover,<br />
intravenous sedation is often used to supplement regional<br />
anesthetic techniques, making it difficult to isolate the<br />
influence of anesthesia itself in most, but not all, such<br />
studies. 62,82 To complicate matters further, there is a strong<br />
association of supplementary epidural anesthesia/analgesia<br />
and POCD 1 week postoperatively in middle-aged<br />
patients. 58 Whether this is a feature of intraoperative use<br />
of the epidural or accumulation of local anesthetic in the<br />
blood or cerebrospinal fluid because of continuous postoperative<br />
epidural infusion is unclear, but it emphasizes<br />
the sensitivity of the brain to even seemingly minor pharmacologic<br />
interventions.<br />
<strong>The</strong> only studies that have examined the long-term<br />
effects of general anesthesia without surgery on learning<br />
and memory have been performed in animals. Most, but<br />
not all of them, demonstrate long-lasting impairment.<br />
One recent study in aged mice found no persistent<br />
memory impairment after isoflurane anesthesia but they<br />
were also unable to detect well-known differences<br />
between young and old animals in this regard, indicating<br />
the behavioral paradigm used was probably not capable<br />
of detecting more subtle anesthesia-induced changes. 83 In<br />
contrast, several studies in aged rats with isoflurane–<br />
nitrous oxide and isoflurane alone, demonstrate spatial
130 D.J. Culley, T.G. Monk, and G. Crosby<br />
learning impairment for weeks after general anesthesia<br />
without surgery. 84–86 This was true for a task that was<br />
partially learned beforehand as well as for one testing<br />
acquisition of entirely new memory. <strong>The</strong>se results may<br />
have implications for understanding POCD. Because the<br />
agents are long cleared from the brain by the time behavioral<br />
testing was begun 48 h to 2 weeks after anesthesia,<br />
the data imply that general anesthesia alters the brain in<br />
some lasting way. <strong>The</strong>re is some biochemical support for<br />
this notion; the profile of protein expression in the brain<br />
is changed for at least 72 hours after general anesthesia<br />
in rats. 87 <strong>The</strong>re is also emerging evidence that some<br />
general anesthetics (e.g., ketamine, nitrous oxide) can be<br />
toxic to the brain during certain phases of the lifespan,<br />
including old age, producing vacuolation, swelling, and<br />
programmed cell death of neurons. 88–91 Additionally,<br />
based on recent work in cell culture, it seems that some<br />
general anesthetics may increase the cytotoxicity of β-<br />
amyloid, a protein implicated in the pathogenesis of<br />
Alzheimer’s disease but also present in the normally<br />
aging brain. 92 Although the relevance of this information<br />
to the genesis of POCD is the subject of debate, it is<br />
conceivable—but not yet firmly established—that general<br />
anesthetics may contribute to lingering postoperative<br />
cognitive impairment in the elderly. 90,93<br />
In summary, one can say that POCD occurs commonly<br />
during the early weeks and months after surgery and<br />
anesthesia. <strong>The</strong> etiology of POCD is likely to be multifactorial<br />
and the relative contributions of age- and<br />
disease-related processes, surgery, physiologic perturbations,<br />
anesthesia, and hospitalization are still unclear.<br />
Longitudinal studies using age- and disease-matched<br />
control groups will be necessary to clarify the long-term<br />
impact of surgery on patients’ ultimate cognitive health<br />
and such investigations will best be accomplished<br />
through collaborative efforts of anesthesiologists, surgeons,<br />
neuropsychologists, and geriatricians. Until then,<br />
because the fundamental mechanisms are uncertain, it is<br />
difficult to identify prevention or treatment strategies. In<br />
particular, there is presently no scientific basis for recommending<br />
(or avoiding) a specific anesthetic agent or technique<br />
in this regard. This will change as further research<br />
is conducted on this common, subtle, and troubling complication.<br />
In the meantime, it is reassuring that the prognosis<br />
for recovery from POCD seems to be good.<br />
Perioperative Stroke<br />
<strong>The</strong> development of a stroke after routine surgery<br />
is uncommon and seldom expected. Although the elderly<br />
represent a high-risk group for this devastating ad -<br />
verse perioperative outcome, questions remain as to<br />
whether perioperative stroke is a random event or one<br />
provoked by perioperative management or altered<br />
physiology.<br />
Table 9-6. Risk factors for perioperative stroke.<br />
• Age<br />
• Cardiac disease<br />
• Peripheral vascular disease<br />
• Hypertension<br />
• Smoking<br />
• Previous cerebrovascular insult<br />
<strong>The</strong>re is a growing body of evidence indicating that the<br />
risk of stroke increases in the perioperative period but<br />
that the etiology is often unknown. One large retrospective,<br />
case-control study reported that the risk of ischemic<br />
stroke during the first 30 days after routine anesthesia<br />
and surgery is three times that of nonsurgical controls. 94<br />
Several smaller studies report similar data, with most<br />
placing the elderly at substantially greater risk. 95–97 In one<br />
retrospective study involving patients undergoing general<br />
surgical procedures, the overall incidence of perioperative<br />
stroke was 0.07% but the risk was 0.22% when only<br />
patients over age 65 were considered. 95 <strong>The</strong> greater risk<br />
of perioperative stroke in the elderly is presumably<br />
explained by the prevalence of age-related risk factors<br />
for stroke such as a history of stroke, hypertension,<br />
smoking, peripheral vascular and cardiac disease, and<br />
aspirin or anticoagulant use (Table 9-6). 97,98–101 Nonetheless,<br />
whereas the risk of stroke seems to be greater in the<br />
perioperative period, conditions that predispose elderly<br />
surgical patients to it are not obvious. 95,96<br />
Factors that have been considered include preexisting<br />
cerebrovascular disease, hypotension, and thromboembolic<br />
events. As for cerebrovascular disease, there is good<br />
agreement that an asymptomatic carotid bruit, which is<br />
present in 14% of surgical patients 55 years or older and<br />
20% of vascular surgical patients, is not itself a risk factor<br />
for perioperative stroke. 102–104 Hence, elective general surgical<br />
procedures probably need not be delayed in individuals<br />
without symptoms of focal cerebral ischemia<br />
but such individuals should be referred for subsequent<br />
evaluation because carotid endarterectomy may reduce<br />
long-term stroke risk. 98,105–107 Relationships between<br />
symptomatic cerebrovascular disease and perioperative<br />
stroke are controversial. <strong>The</strong>re has been disagreement as<br />
to whether transient ischemic events, which are predictors<br />
of stroke in the general patient population, are also<br />
associated with a higher incidence of perioperative<br />
stroke. 108,109 However, it is often recommended that<br />
patients undergoing elective general surgical procedures<br />
with symptomatic carotid stenosis and a greater than<br />
70% arterial narrowing be evaluated preoperatively for<br />
possible carotid endarterectomy or stenting. 106 At the<br />
other extreme, prior stroke does increase the risk of perioperative<br />
cerebral reinfarction. In a small study, stroke<br />
was 5–10 times more common in those patients with a<br />
history of stroke. 96 <strong>The</strong> reasons for greater vulnerability
9. Postoperative Central Nervous System Dysfunction 131<br />
to perioperative reinfarction after a previous stroke are<br />
unknown but may relate to a prolonged period of altered<br />
cerebrovascular reactivity after a stroke and known alterations<br />
in cerebral autoregulation and carbon dioxide<br />
reactivity in vessels distal to a carotid stenosis. 110,111 After<br />
an acute cerebral ischemic event, the clinical and radiographic<br />
picture evolves over days to weeks, indicating<br />
that stroke is not a static event and suggesting that there<br />
may be an interval of special vulnerability to physiologic<br />
perturbations. Perhaps for this reason, it may be prudent<br />
to defer elective surgery after a stroke but there is no<br />
demonstrated benefit of doing so and no consensus on<br />
the optimal timing of elective surgery in patients with a<br />
recent ischemic stroke. 104<br />
Hypotension is another potential cause of perioperative<br />
stroke. Certainly there is no question that hypotension<br />
can produce cerebral ischemia and infarction if it is<br />
severe and prolonged. 112 That said, retrospective analyses<br />
indicate that most patients who had a stroke postoperatively<br />
experienced hypotension intraoperatively and yet<br />
emerged from anesthesia without a neurologic deficit. 95,98<br />
Furthermore, in cases in which perioperative hypotension<br />
is proposed as an inciting event, there may be a long<br />
asymptomatic interval between the hypotensive episode<br />
and the stroke. 101 Thus, at levels of hypotension frequently<br />
encountered in routine clinical situations, a cause-andeffect<br />
relationship between hypotension and stroke is<br />
often difficult to establish, in part because the consequences<br />
may be delayed and occur by as yet unknown<br />
mechanisms.<br />
Further confusing the story of hypotension and cerebral<br />
ischemia are results of an old underpowered study<br />
that deliberately exposed conscious patients with transient<br />
ischemic attacks to as much as a 60% decrease in<br />
systolic blood pressure. 113 Despite such profound, transient<br />
hypotension, no patient had a stroke and only one<br />
had a true transient ischemic attack, even though most<br />
developed unrelated focal signs or evidence of global<br />
cerebral ischemia. Also, as described earlier, induced<br />
hypotension (MAP 45–55 versus 55–70 mm Hg) during<br />
epidural anesthesia in elderly patients was not associated<br />
with either stroke or a higher incidence of cognitive<br />
impairment. 35 Although underpowered for a rare event<br />
such as stroke, assuming that cerebral infarction occurs<br />
at lower levels of perfusion than deterioration in cognitive<br />
performance, the data support the idea that the aged<br />
brain tolerates a moderate and transient reduction in<br />
perfusion pressure relatively well. However, in hypertensive<br />
patients, strokes have been precipitated by a rapid,<br />
pharmacologically induced, moderate blood pressure<br />
reduction, suggesting that there may be a vulnerable<br />
patient population that has not been clearly defined. 114<br />
Accordingly, although it is difficult to prove that transient<br />
intraoperative hypotension is benign, there is also little<br />
evidence to establish a cause-and-effect relationship<br />
between transient intraoperative hypotension and perioperative<br />
stroke.<br />
Indeed, in most cases, perioperative stroke is attributable<br />
to thrombotic or embolic events. 101 <strong>The</strong> risk of<br />
this type of stroke may be related to common perioperative<br />
complications including cardiac arrhythmias, withholding<br />
antithrombotic therapy, and hypercoagulability<br />
related to surgery and anesthesia. Dissection and/or<br />
thrombosis of the carotid or vertebral arteries have been<br />
reported perioperatively, ostensibly in conjunction with<br />
malpositioning of the neck. 99 Similar neurologic catastrophes<br />
are also reported after common activities such as<br />
coughing or sneezing, however, so the relationship to<br />
positioning is speculative at best. With respect to embolic<br />
events, one retrospective review found that cardiogenic<br />
embolism accounted for 40% of perioperative strokes<br />
and the majority of these occurred postoperatively. 95 An<br />
antecedent myocardial infarction was present in 17% of<br />
the patients and 33% were in atrial fibrillation at the time<br />
of the stroke. Moreover, perioperative embolic phenomena<br />
may be more common than previously appreciated,<br />
at least in certain procedures. Tourniquet deflation during<br />
total knee replacement is associated with venous and<br />
cerebral embolization in a large percentage of patients<br />
even if they do not have a patent foramen ovale or atrial<br />
or ventricular septal defect. 74,75 Perioperative changes in<br />
coagulation are also theorized to have a role because<br />
alterations in plasma concentrations of coagulation<br />
factors, platelet number and function, and altered fibrinolysis<br />
are well documented and may produce a hypercoagulable<br />
state. 100<br />
Neurologic consultation and additional diagnostic<br />
procedures should be sought expediently if a new and<br />
persistent focal neurologic deficit is identified in the perioperative<br />
period. Early detection becomes important<br />
as promising new therapeutic modalities to reverse or<br />
minimize the permanent consequences of injury are<br />
tested. Accordingly, the history should be carefully<br />
reviewed and a through neurologic examination performed.<br />
In view of the high incidence of embolic stroke,<br />
an echocardiogram can be diagnostically useful. Precordial<br />
echocardiograms are not reliable for detecting a<br />
patent foramen ovale and passage of surgical debris<br />
through the pulmonary veins is well documented. 74 Hence,<br />
a negative study does not eliminate the possibility of a<br />
perioperative paradoxical embolism. 95,115,116 Computed<br />
tomography and magnetic resonance imaging have long<br />
been used to provide information about infarct type, size,<br />
and location but until recently ischemic areas were not<br />
identifiable radiographically for hours to days after an<br />
event. This has changed with newer diagnostic modalities<br />
such as perfusion and diffusion weighted magnetic resonance<br />
imaging, which permit the detection of cerebral<br />
ischemia within a few hours after the onset of neurologic<br />
symptoms. 117
132 D.J. Culley, T.G. Monk, and G. Crosby<br />
If an acute stroke is diagnosed, care should conform to<br />
guidelines recently established by the American Heart<br />
Association. 118,119 Defining the type of stroke (ischemic<br />
versus hemorrhagic) is essential because certain aspects<br />
of management are quite different. 118,119 <strong>The</strong> emphasis in<br />
both cases is on good physiologic management because<br />
more specific “protective” measures have proven ineffective.<br />
120–122 Thus, the ABCs (airway, breathing, circulation)<br />
of basic life support, including supplemental oxygen until<br />
the diagnosis is confirmed and/or endotracheal intubation<br />
as necessary for hypoxia, hypercarbia, or prevention<br />
of aspiration, are crucial. 118,119 <strong>The</strong> guidelines for blood<br />
pressure management differ markedly for patients with<br />
hemorrhagic and ischemic stroke. 118,119 In the former,<br />
assuming a history of hypertension, it is recommended<br />
that MAP be maintained between 90–130 mm Hg. 119 In<br />
contrast, a more cautious approach is recommended for<br />
patients with ischemic stroke, with antihypertensives<br />
given only when systolic blood pressure is >220 mm Hg or<br />
diastolic pressure is >120 mm Hg. 118 Likewise, if intracranial<br />
pressure monitoring is available, cerebral perfusion<br />
pressure should be maintained above 70 mm Hg with<br />
osmotherapy, hyperventilation (PaCO 2 30–35 mm Hg),<br />
sedatives, and neuromuscular blocking agents as needed.<br />
Fever should be treated with antipyretics and hypovolemia<br />
and hyperglycemia avoided. 118,119 As already noted,<br />
although the search for an effective stroke treatment has<br />
been extensive, no neuroprotective agent has proven<br />
effective. 123 Thus, none is recommended for treatment of<br />
acute stroke. However, there is a correlation between<br />
administration of benzodiazepines, dopamine antagonists,<br />
α-2 agonists, α-1 antagonists, and phenytoin or phenobarbital<br />
in the first 28 days after stroke and adverse<br />
neurologic outcome. 124 Although use of such drugs may<br />
be a marker for illness severity, these data caution that<br />
common drugs may have unanticipated neurologic consequences<br />
among patients with cerebral ischemia and<br />
that unnecessary pharmacotherapy should be avoided.<br />
<strong>The</strong> greatest advance in stroke management in recent<br />
years is the realization that stroke can be treated.<br />
Whereas treatment of stroke was simply supportive and<br />
rehabilitative in the past (with the exception of hyperbaric<br />
therapy for treatment of air emboli), today stroke<br />
is considered a medical emergency. 125 <strong>The</strong> main impetus<br />
for this important change in thinking is the success of<br />
low-molecular-weight heparin and thrombolytics for<br />
acute ischemic stroke. 126 Several studies demonstrate that<br />
tissue plasminogen activator administered within 3 hours<br />
improves overall neurologic outcome. 127 Although the<br />
safety of thrombolytics and heparins in the treatment of<br />
the surgical patient with acute stroke has not been established<br />
and the risk of hemorrhage remains a concern,<br />
there are reports of safe and successful administration of<br />
these agents in the acute postoperative setting. 128 Thus,<br />
although stroke is a rare and unpredictable complication<br />
of anesthesia and surgery, it is important to make the<br />
diagnosis expediently because, for the first time, there is<br />
real potential for effective treatment and promptness of<br />
treatment is an important factor.<br />
Conclusion<br />
<strong>The</strong> aged brain is different from the young brain in many<br />
respects, making elders more vulnerable to common perioperative<br />
complications such as POCD, delirium, and<br />
stroke. With the population aging, the challenge for the<br />
decades ahead is to better understand the role of surgery<br />
and anesthesia in causation of these complications so that<br />
perioperative physicians can tailor care for the elderly<br />
patient with the aged brain in mind.<br />
References<br />
1. Coffey CE, Wilkinson WE, Parashos IA, et al. Quantitative<br />
cerebral anatomy of the aging human brain: a cross-sectional<br />
study using magnetic resonance imaging. Neurology<br />
1992;42(3 Pt 1):527–536.<br />
2. Selkoe DJ. Aging brain, aging mind. Sci Am 1992;267(3):<br />
134–142.<br />
3. Davis SM, Ackerman RH, Correia JA, et al. Cerebral<br />
blood flow and cerebrovascular CO 2 reactivity in strokeage<br />
normal controls. Neurology 1983;33(4):391–399.<br />
4. Bentourkia M, Bol A, Ivanoiu A, et al. Comparison of<br />
regional cerebral blood flow and glucose metabolism<br />
in the normal brain: effect of aging. J Neurol Sci 2000;<br />
181(1–2):19–28.<br />
5. Carey BJ, Panerai RB, Potter JF. Effect of aging on dynamic<br />
cerebral autoregulation during head-up tilt. Stroke 2003;<br />
34(8):1871–1875.<br />
6. Mrak RE, Griffin ST, Graham DI. Aging-associated<br />
changes in human brain. J Neuropathol Exp Neurol 1997;<br />
56(12):1269–1275.<br />
7. Francis PT, Palmer AM, Snape M, Wilcock GK. <strong>The</strong> cholinergic<br />
hypothesis of Alzheimer’s disease: a review of progress.<br />
J Neurol Neurosurg Psychiatry 1999;66(2):\137–147.<br />
8. Lu T, Pan Y, Kao SY, et al. Gene regulation and DNA<br />
damage in the ageing human brain. Nature 2004;429(6994):<br />
883–891.<br />
9. Eriksson PS, Perfilieva E, Bjork-Eriksson T, et al. Neurogenesis<br />
in the adult human hippocampus. Nat Med 1998;<br />
4(11):1313–1317.<br />
10. Shors TJ, Miesegaes G, Beylin A, Zhao M, Rydel T, Gould<br />
E. Neurogenesis in the adult is involved in the formation<br />
of trace memories. Nature 2001;410(6826):372–376.<br />
11. Keefover RW. Aging and cognition. Neurol Clin 1998;<br />
16(3):635–648.<br />
12. Morris JC, McManus DQ. <strong>The</strong> neurology of aging: normal<br />
versus pathologic change. <strong>Geriatric</strong>s 1991;46(8):47–54.<br />
13. Compton DM, Bachman LD, Brand D, Avet TL.<br />
Age associated changes in cognitive function in highly<br />
educated adults: emerging myths and realities. Int J Geriatr<br />
Psychiatry 2000;15(1):75–85.
9. Postoperative Central Nervous System Dysfunction 133<br />
14. Gilbert DK, Rogers WA. Age-related differences in the<br />
acquisition, utilization, and extension of a spatial mental<br />
model. J Gerontol B Psychol Sci Soc Sci 1999;54(4):246–<br />
255.<br />
15. Richards SS, Hendrie HC. Diagnosis, management, and<br />
treatment of Alzheimer disease: a guide for the internist.<br />
Arch Intern Med 1999;159(8):789–798.<br />
16. Growdon JH. Biomarkers of Alzheimer disease. Arch<br />
Neurol 1999;56(3):281–283.<br />
17. Jack CR Jr, Petersen RC, Xu Y, et al. Rate of medial temporal<br />
lobe atrophy in typical aging and Alzheimer’s disease.<br />
Neurology 1998;51(4):993–999.<br />
18. Wolfson C, Wolfson DB, Asgharian M, et al. A reevaluation<br />
of the duration of survival after the onset of dementia. N<br />
Engl J Med 2001;344(15):1111–1116.<br />
19. Diagnostics and Statistical Manual of Mental Disorders—<br />
Text Revision. Washington, DC: American Psychiatric<br />
Association; 2000.<br />
20. Inouye SK, van Dyck CH, Alessi CA, Balkin S, Siegal AP,<br />
Horwitz RI. Clarifying confusion: the confusion assessment<br />
method. A new method for detection of delirium.<br />
Ann Intern Med 1990;113(12):941–948.<br />
21. Ely EW, Inouye SK, Bernard GR, et al. Delirium in<br />
mechanically ventilated patients: validity and reliability<br />
of the confusion assessment method for the inten -<br />
sive care unit (CAM-ICU). JAMA 2001;286(21):2703–<br />
2710.<br />
22. Sandberg O, Gustafson Y, Brannstrom B, Bucht G. Clinical<br />
profile of delirium in older patients. J Am Geriatr Soc<br />
1999;47(11):1300–1306.<br />
23. Marcantonio ER, Goldman L, Orav EJ, Cook EF, Lee TH.<br />
<strong>The</strong> association of intraoperative factors with the development<br />
of postoperative delirium. Am J Med 1998;105(5):<br />
380–384.<br />
24. Zakriya K, Sieber FE, Christmas C, Wenz JF Sr,<br />
Franckowiak S. Brief postoperative delirium in hip<br />
fracture patients affects functional outcome at three<br />
months. Anesth Analg 2004;98(6):1798–1802.<br />
25. Litaker D, Locala J, Franco K, Bronson DL, Tannous Z.<br />
Preoperative risk factors for postoperative delirium. Gen<br />
Hosp Psychiatry 2001;23(2):84–89.<br />
26. Williams-Russo P, Urquhart BL, Sharrock NE, Charlson<br />
ME. Post-operative delirium: predictors and prognosis in<br />
elderly orthopedic patients. J Am Geriatr Soc 1992;40(8):<br />
759–767.<br />
27. Dyer CB, Ashton CM, Teasdale TA. Postoperative delirium.<br />
A review of 80 primary data-collection studies. Arch<br />
Intern Med 1995;155(5):461–465.<br />
28. Marcantonio ER, Goldman L, Mangione CM, et al. A clinical<br />
prediction rule for delirium after elective noncardiac<br />
surgery. JAMA 1994;271(2):134–139.<br />
29. Galanakis P, Bickel H, Gradinger R, Von GS, Forstl H.<br />
Acute confusional state in the elderly following hip surgery:<br />
incidence, risk factors and complications. Int J Geriatr Psychiatry<br />
2001;16(4):349–355.<br />
30. Zakriya KJ, Christmas C, Wenz JF Sr, Franckowiak S,<br />
Anderson R, Sieber FE. Preoperative factors associated<br />
with postoperative change in confusion assessment method<br />
score in hip fracture patients. Anesth Analg 2002;94(6):<br />
1628–1632.<br />
31. Weed HG, Lutman CV, Young DC, Schuller DE. Preoperative<br />
identification of patients at risk for delirium after<br />
major head and neck cancer surgery. Laryngoscope 1995;<br />
105(10):1066–1068.<br />
32. Marcantonio ER, Juarez G, Goldman L, et al. <strong>The</strong> relationship<br />
of postoperative delirium with psychoactive medications.<br />
JAMA 1994;272(19):1518–1522.<br />
33. Tune L, Carr S, Cooper T, Klug B, Golinger RC. Association<br />
of anticholinergic activity of prescribed medications<br />
with postoperative delirium. J Neuropsychiatry Clin<br />
Neurosci 1993;5(2):208–210.<br />
34. Lundstrom M, Edlund A, Bucht G, Karlsson S, Gustafson<br />
Y. Dementia after delirium in patients with femoral neck<br />
fractures. J Am Geriatr Soc 2003;51(7):1002–1006.<br />
35. Williams-Russo P, Sharrock NE, Mattis S, et al. Randomized<br />
trial of hypotensive epidural anesthesia in older adults.<br />
<strong>Anesthesiology</strong> 1999;91(4):926–935.<br />
36. Rosenberg J, Kehlet H. Postoperative mental confusion—<br />
association with postoperative hypoxemia. Surgery 1993;<br />
114(1):76–81.<br />
37. Aakerlund LP, Rosenberg J. Postoperative delirium: treatment<br />
with supplementary oxygen. Br J Anaesth 1994;72(3):<br />
286–290.<br />
38. Morrison RS, Magaziner J, Gilbert M, et al. Relationship<br />
between pain and opioid analgesics on the development<br />
of delirium following hip fracture. J Gerontol A Biol Sci<br />
Med Sci 2003;58(1):76–81.<br />
39. Lynch EP, Lazor MA, Gellis JE, Orav J, Goldman L,<br />
Marcantonio ER. <strong>The</strong> impact of postoperative pain on the<br />
development of postoperative delirium. Anesth Analg<br />
1998;86(4):781–785.<br />
40. Adunsky A, Levy R, Mizrahi E, Arad M. Exposure to<br />
opioid analgesia in cognitively impaired and delirious<br />
elderly hip fracture patients. Arch Gerontol Geriatr 2002;<br />
35(3):245–251.<br />
41. Han L, McCusker J, Cole M, Abrahamowicz M, Primeau<br />
F, Elie M. Use of medications with anticholinergic<br />
effect predicts clinical severity of delirium symptoms in<br />
older medical inpatients. Arch Intern Med 2001;161(8):<br />
1099–1105.<br />
42. Inouye SK, Charpentier PA. Precipitating factors for delirium<br />
in hospitalized elderly persons. Predictive model and<br />
interrelationship with baseline vulnerability. JAMA 1996;<br />
275(11):852–857.<br />
43. Weuve J, Kang JH, Manson JE, Breteler MM, Ware JH,<br />
Grodstein F. Physical activity, including walking, and<br />
cognitive function in older women. JAMA 2004;292(12):<br />
1454–1461.<br />
44. Heyn P, Abreu BC, Ottenbacher KJ. <strong>The</strong> effects of exercise<br />
training on elderly persons with cognitive impairment and<br />
dementia: a meta-analysis. Arch Phys Med Rehabil 2004;<br />
85(10):1694–1704.<br />
45. Kamel HK, Iqbal MA, Mogallapu R, Maas D, Hoffmann<br />
RG. Time to ambulation after hip fracture surgery: relation<br />
to hospitalization outcomes. J Gerontol A Biol Sci Med Sci<br />
2003;58(11):1042–1045.<br />
46. Marcantonio ER, Flacker JM, Michaels M, Resnick NM.<br />
Delirium is independently associated with poor functional<br />
recovery after hip fracture. J Am Geriatr Soc 2000;48(6):<br />
618–624.
134 D.J. Culley, T.G. Monk, and G. Crosby<br />
47. Marcantonio ER, Flacker JM, Wright RJ, Resnick NM.<br />
Reducing delirium after hip fracture: a randomized trial.<br />
J Am Geriatr Soc 2001;49(5):516–522.<br />
48. Mittal D, Jimerson NA, Neely EP, et al. Risperidone in the<br />
treatment of delirium: results from a prospective openlabel<br />
trial. J Clin Psychiatry 2004;65(5):662–667.<br />
49. Han CS, Kim YK. A double-blind trial of risperidone and<br />
haloperidol for the treatment of delirium. Psychosomatics<br />
2004;45(4):297–301.<br />
50. Agostini JV, Leo-Summers LS, Inouye SK. Cognitive<br />
and other adverse effects of diphenhydramine use in hospitalized<br />
older patients. Arch Intern Med 2001;161(17):<br />
2091–2097.<br />
51. Carnes M, Howell T, Rosenberg M, Francis J, Hildebrand<br />
C, Knuppel J. Physicians vary in approaches to the clinical<br />
management of delirium. J Am Geriatr Soc 2003;51(2):<br />
234–239.<br />
52. Bedford PD. Adverse cerebral effects of anaesthesia on<br />
old people. Lancet 1955;269:259–263.<br />
53. Dijkstra JB, Jolles J. Postoperative cognitive dysfunction<br />
versus complaints: a discrepancy in long-term findings.<br />
Neuropsychol Rev 2002;12(1):1–14.<br />
54. Dodds C, Allison J. Postoperative cognitive deficit in the<br />
elderly surgical patient. Br J Anaesth 1998;81(3):449–462.<br />
55. Rasmussen LS, Siersma VD. Postoperative cognitive<br />
dysfunction: true deterioration versus random variation.<br />
Acta Anaesthesiol Scand 2004;48(9):1137–1143.<br />
56. Crosby G, Culley DJ. <strong>Anesthesia</strong>, the aging brain, and the<br />
surgical patient. Can J Anaesth 2003;50:R1–R5.<br />
57. Moller JT, Cluitmans P, Rasmussen LS, et al. Long-term<br />
postoperative cognitive dysfunction in the elderly<br />
ISPOCD1 study. ISPOCD investigators. International<br />
Study of Post-Operative Cognitive Dysfunction. Lancet<br />
1998;351(9106):857–861.<br />
58. Johnson T, Monk T, Rasmussen LS, et al. Postoperative<br />
cognitive dysfunction in middle-aged patients. <strong>Anesthesiology</strong><br />
2002;96(6):1351–1357.<br />
59. Abildstrom H, Rasmussen LS, Rentowl P, et al. Cognitive<br />
dysfunction 1–2 years after non-cardiac surgery in the<br />
elderly. ISPOCD group. International Study of Post-<br />
Operative Cognitive Dysfunction. Acta Anaesthesiol<br />
Scand 2000;44(10):1246–1251.<br />
60. Newman MF, Kirchner JL, Phillips-Bute B, et al. Longitudinal<br />
assessment of neurocognitive function after coronary-artery<br />
bypass surgery. N Engl J Med 2001;344(6):<br />
395–402.<br />
61. Newman MF, Croughwell ND, Blumenthal JA, et al.<br />
Predictors of cognitive decline after cardiac operation.<br />
Ann Thorac Surg 1995;59:1326–1330.<br />
62. Williams-Russo P, Sharrock NE, Mattis S, Szatrowski TP,<br />
Charlson ME. Cognitive effects after epidural vs general<br />
anesthesia in older adults. A randomized trial. JAMA<br />
1995;274(1):44–50.<br />
63. Charlson ME, Pompei P, Ales KL, MacKenzie CR. A new<br />
method of classifying prognostic comorbidity in longitudinal<br />
studies: development and validation. J Chronic Dis<br />
1987;40(5):373–383.<br />
64. Hogue CW, Lillie R, Hershey T, et al. Gender influence<br />
on cognitive function after cardiac operation. Ann Thorac<br />
Surg 2003;76(4):1119–1125.<br />
65. Phillips BB, Mathew J, Blumenthal JA, et al. Female gender<br />
is associated with impaired quality of life 1 year after coronary<br />
artery bypass surgery. Psychosom Med 2003;65(6):<br />
944–951.<br />
66. Hogue CW Jr, Sundt T III, Barzilai B, Schecthman KB,<br />
Vila-Roman VG. Cardiac and neurologic complications<br />
identify risks for mortality for both men and women<br />
undergoing coronary artery bypass graft surgery.<br />
<strong>Anesthesiology</strong> 2001;95(5):1074–1078.<br />
67. Bennett DA, Wilson RS, Schneider JA, et al. Apolipoprotein<br />
E epsilon4 allele, AD pathology, and the clinical<br />
expression of Alzheimer’s disease. Neurology 2003;60(2):<br />
246–252.<br />
68. Sundstrom A, Marklund P, Nilsson LG, et al. APOE influences<br />
on neuropsychological function after mild head<br />
injury: within-person comparisons. Neurology 2004;62(11):<br />
1963–1966.<br />
69. Abildstrom H, Christiansen M, Siersma VD, Rasmussen<br />
LS. Apolipoprotein E genotype and cognitive dysfunction<br />
after noncardiac surgery. <strong>Anesthesiology</strong> 2004;101(4):855–<br />
861.<br />
70. Canet J, Raeder J, Rasmussen LS, et al. Cognitive dysfunction<br />
after minor surgery in the elderly. Acta Anaesthesiol<br />
Scand 2003;47(10):1204–1210.<br />
71. Rasmussen LS, Steentoft A, Rasmussen H, Kristensen PA,<br />
Moller JT. Benzodiazepines and postoperative cognitive<br />
dysfunction in the elderly. ISPOCD Group. International<br />
Study of Postoperative Cognitive Dysfunction. Br J<br />
Anaesth 1999;83(4):585–589.<br />
72. Lu CH, Chao PC, Borel CO, et al. Preincisional intra -<br />
venous pentoxifylline attenuating perioperative cytokine<br />
response, reducing morphine consumption, and improv -<br />
ing recovery of bowel function in patients undergoing<br />
colorectal cancer surgery. Anesth Analg 2004;99(5):<br />
1465–1471.<br />
73. Hindman BJ. Emboli, inflammation, and CNS impairment:<br />
an overview. Heart Surg Forum 2002;5(3):249–253.<br />
74. Sulek CA, Davies LK, Enneking FK, Gearen PA, Lobato<br />
EB. Cerebral microembolism diagnosed by transcranial<br />
Doppler during total knee arthroplasty: correlation with<br />
transesophageal echocardiography. <strong>Anesthesiology</strong> 1999;<br />
91(3):672–676.<br />
75. Ogino Y, Tatsuoka Y, Matsuoka R, et al. Cerebral infarction<br />
after deflation of a pneumatic tourniquet during total<br />
knee replacement. <strong>Anesthesiology</strong> 1999;90(1):297–298.<br />
76. Lupien SJ, de Leon M, de Santi S, et al. Cortisol levels<br />
during human aging predict hippocampal atrophy and<br />
memory deficits. Nat Neurosci 1998;1(1):69–73.<br />
77. Bassuk SS, Glass TA, Berkman LF. Social disengagement<br />
and incident cognitive decline in community-dwelling<br />
elderly persons. Ann Intern Med 1999;131(3):165–173.<br />
78. Morimoto Y, Mathru M, Martinez-Tica JF, Zornow MH.<br />
Effects of profound anemia on brain tissue oxygen tension,<br />
carbon dioxide tension, and pH in rabbits. J Neurosurg<br />
Anesthesiol 2001;13(1):33–39.<br />
79. Weiskopf RB, Kramer JH, Viele M, et al. Acute severe<br />
isovolemic anemia impairs cognitive function and memory<br />
in humans. <strong>Anesthesiology</strong> 2000;92(6):1646–1652.<br />
80. Pickett JL, <strong>The</strong>berge DC, Brown WS, Schweitzer SU,<br />
Nissenson AR. Normalizing hematocrit in dialysis patients
9. Postoperative Central Nervous System Dysfunction 135<br />
improves brain function. Am J Kidney Dis 1999;33(6):<br />
1122–1130.<br />
81. Linstedt U, Meyer O, Berkau A, Kropp P, Zenz M, Maier<br />
C. Does intraoperative hyperventilation improve neurological<br />
functions of older patients after general anaesthesia?<br />
Anaesthesist 2002;51(6):457–462.<br />
82. Rasmussen LS, Johnson T, Kuipers HM, et al. Does anaesthesia<br />
cause postoperative cognitive dysfunction? A randomised<br />
study of regional versus general anaesthesia in<br />
438 elderly patients. Acta Anaesthesiol Scand 2003;47(3):<br />
260–266.<br />
83. Butterfield NN, Graf P, Ries CR, MacLeod BA. <strong>The</strong> effect<br />
of repeated isoflurane anesthesia on spatial and psychomotor<br />
performance in young and aged mice. Anesth Analg<br />
2004;98(5):1305–1311.<br />
84. Culley DJ, Yukhananov R, Baxter MG, Crosby G. <strong>The</strong><br />
memory effects of general anesthesia persist for weeks<br />
in young and aged rats. Anesth Analg 2003;96(4):1004–<br />
1009.<br />
85. Culley DJ, Yukhananov R, Baxter MG, Crosby G. Longterm<br />
impairment of acquisition of a spatial memory task<br />
following isoflurane-nitrous oxide anesthesia in rats.<br />
<strong>Anesthesiology</strong> 2004;100:309–314.<br />
86. Culley DJ, Yukhananov R, Baxter MG, Crosby G. Impaired<br />
acquisition of spatial memory two weeks after isoflurane<br />
and isoflurane-nitrous oxide anesthesia in aged rats. Anesth<br />
Analg 2004;99:1393–1397.<br />
87. Futterer CD, Maurer MH, Schmitt A, Feldmann RE Jr,<br />
Kuschinsky W, Waschke KF. Alterations in rat brain proteins<br />
after desflurane anesthesia. <strong>Anesthesiology</strong> 2004;<br />
100(2):302–308.<br />
88. Jevtovic-Todorovic V, Beals J, Benshoff N, Olney JW.<br />
Prolonged exposure to inhalational anesthetic nitrous<br />
oxide kills neurons in adult rat brain. Neuroscience 2003;<br />
122(3):609–616.<br />
89. Jevtovic-Todorovic V, Hartman RE, Izumi Y, et al. Early<br />
exposure to common anesthetic agents causes widespread<br />
neurodegeneration in the developing rat brain and persistent<br />
learning deficits. J Neurosci 2003;23(3):876–882.<br />
90. Anand KJ, Soriano SG. Anesthetic agents and the immature<br />
brain: are these toxic or therapeutic? <strong>Anesthesiology</strong><br />
2004;101(2):527–530.<br />
91. Olney JW, Young C, Wozniak DF, Ikonomidou C, Jevtovic-<br />
Todorovic V. <strong>Anesthesia</strong>-induced developmental neuroapoptosis.<br />
Does it happen in humans? <strong>Anesthesiology</strong><br />
2004;101(2):273–275.<br />
92. Eckenhoff RG, Johansson JS, Wei H, et al. Inhaled anesthetic<br />
enhancement of amyloid-beta oligomerization and<br />
cytotoxicity. <strong>Anesthesiology</strong> 2004;101(3):703–709.<br />
93. Todd MM. Anesthetic neurotoxicity: the collision between<br />
laboratory neuroscience and clinical medicine. <strong>Anesthesiology</strong><br />
2004;101(2):272–273.<br />
94. Wong GY, Warner DO, Schroeder DR, et al. Risk of surgery<br />
and anesthesia for ischemic stroke. <strong>Anesthesiology</strong> 2000;<br />
92(2):425–432.<br />
95. Hart R, Hindman B. Mechanisms of perioperative cerebral<br />
infarction. Stroke 1982;13(6):766–773.<br />
96. Landercasper J, Merz BJ, Cogbill TH, et al. Perioperative<br />
stroke risk in 173 consecutive patients with a past history<br />
of stroke. Arch Surg 1990;125:986–989.<br />
97. Larsen SF, Zaric D, Boysen G. Postoperative cerebrovascular<br />
accidents in general surgery. Acta Anaesthesiol Scand<br />
1988;32(8):698–701.<br />
98. Parikh S, Cohen JR. Perioperative stroke after general<br />
surgical procedures. NY State J Med 1993;93(3):162–165.<br />
99. Kim J, Gelb AW. Predicting perioperative stroke.<br />
J Neurosurg Anesthesiol 1995;7(3):211–215.<br />
100. Kam PC, Calcroft RM. Peri-operative stroke in general<br />
surgical patients. Anaesthesia 1997;52(9):879–883.<br />
101. Limburg M, Wijdicks EF, Li H. Ischemic stroke after surgical<br />
procedures: clinical features, neuroimaging, and risk<br />
factors. Neurology 1998;50(4):895–901.<br />
102. Shorr RI, Johnson KC, Wan JY, et al. <strong>The</strong> prognostic significance<br />
of asymptomatic carotid bruits in the elderly.<br />
J Gen Intern Med 1998;13(2):86–90.<br />
103. Ropper AH, Wechsler LR, Wilson LS. Carotid bruit and<br />
the risk of stroke in elective surgery. N Engl J Med 1982;<br />
307:1388–1390.<br />
104. Blacker DJ, Flemming KD, Link MJ, Brown RD Jr. <strong>The</strong><br />
preoperative cerebrovascular consultation: common cerebrovascular<br />
questions before general or cardiac surgery.<br />
Mayo Clin Proc 2004;79(2):223–229.<br />
105. Dodick DW, Meissner I, Meyer FB, Cloft HJ. Evaluation<br />
and management of asymptomatic carotid artery stenosis.<br />
Mayo Clin Proc 2004;79(7):937–944.<br />
106. Barnett HJ, Taylor DW, Eliasziw M, et al. Benefit of carotid<br />
endarterectomy in patients with symptomatic moderate or<br />
severe stenosis. North American Symptomatic Carotid<br />
Endarterectomy Trial Collaborators. N Engl J Med 1998;<br />
339(20):1415–1425.<br />
107. Halliday A, Mansfield A, Marro J, et al. Prevention of disabling<br />
and fatal strokes by successful carotid endarterectomy<br />
in patients without recent neurological symptoms:<br />
randomised controlled trial. Lancet 2004;363(9420):1491–<br />
1502.<br />
108. Turnipseed WD, Berkoff HA, Belzer FO. Postoperative<br />
stroke in cardiac and peripheral vascular disease. Ann Surg<br />
1980;192(3):365–368.<br />
109. Evans BA, Wijdicks EF. High-grade carotid stenosis<br />
detected before general surgery: is endarterectomy indicated?<br />
Neurology 2001;57(7):1328–1330.<br />
110. Widder B, Kleiser B, Krapf H. Course of cerebrovascular<br />
reactivity in patients with carotid artery occlusions. Stroke<br />
1994;25(10):1963–1967.<br />
111. White RP, Markus HS. Impaired dynamic cerebral autoregulation<br />
in carotid artery stenosis. Stroke 1997;28(7):<br />
1340–1344.<br />
112. Blacker DJ, Flemming KD, Wijdicks EF. Risk of ischemic<br />
stroke in patients with symptomatic vertebrobasilar stenosis<br />
undergoing surgical procedures. Stroke 2003;34(11):<br />
2659–2663.<br />
113. Kendell RE, Marshall J. Role of hypotension in the genesis<br />
of transient focal cerebral ischaemic attacks. Br Med J<br />
1963;2:344–348.<br />
114. Fischberg GM, Lozano E, Rajamani K, Ameriso S, Fisher<br />
MJ. Stroke precipitated by moderate blood pressure reduction.<br />
J Emerg Med 2000;19(4):339–346.<br />
115. Oliver S, Cucchiara RF, Nishimura R, Michenfelder JD.<br />
Parameters affecting the occurrence of paradoxical air<br />
embolism. <strong>Anesthesiology</strong> 1987;(3A).
136 D.J. Culley, T.G. Monk, and G. Crosby<br />
116. Black S, Muzzi DA, Nishimura RA, Cucchiara RF. Preoperative<br />
and intraoperative echocardiography to detect<br />
right-to-left shunt in patients undergoing neurosurgical<br />
procedures in the sitting position. <strong>Anesthesiology</strong> 1990;<br />
72(3):436–438.<br />
117. Bonaffini N, Altieri M, Rocco A, Di Piero V. Functional<br />
neuroimaging in acute stroke. Clin Exp Hypertens 2002;<br />
24(7–8):647–657.<br />
118. Adams HP Jr, Adams RJ, Brott T, et al. Guidelines for<br />
the early management of patients with ischemic stroke:<br />
a scientific statement from the Stroke Council of the<br />
American Stroke Association. Stroke 2003;34(4):1056–<br />
1083.<br />
119. Broderick JP, Adams HP Jr, Barsan W, et al. Guidelines for<br />
the management of spontaneous intracerebral hemorrhage:<br />
a statement for healthcare professionals from a<br />
special writing group of the Stroke Council, American<br />
Heart Association. Stroke 1999;30(4):905–915.<br />
120. Warner DS. Perioperative neuroprotection: are we<br />
asking the right questions? Anesth Analg 2004;98(3):563–<br />
565.<br />
121. Patel P. No magic bullets: the ephemeral nature of anesthetic-mediated<br />
neuroprotection. <strong>Anesthesiology</strong> 2004;<br />
100(5):1049–1051.<br />
122. Auer RN. Non-pharmacologic (physiologic) neuroprotection<br />
in the treatment of brain ischemia. Ann NY Acad Sci<br />
2001;939:271–282.<br />
123. De Keyser J, Sulter G, Luiten PG. Clinical trials with neuroprotective<br />
drugs in acute ischaemic stroke: are we doing<br />
the right thing? Trends Neurosci 1999;22(12):535–540.<br />
124. Goldstein LB. Common drugs may influence motor recovery<br />
after stroke. <strong>The</strong> Sygen In Acute Stroke Study Investigators.<br />
Neurology 1995;45(5):865–871.<br />
125. Shank ES, Muth CM. Decompression illness, iatrogenic gas<br />
embolism, and carbon monoxide poisoning: the role of<br />
hyperbaric oxygen therapy. Int Anesthesiol Clin 2000;38(1):<br />
111–138.<br />
126. Warlow C, Wardlaw J. <strong>The</strong>rapeutic thrombolysis for acute<br />
ischaemic stroke. BMJ 2003;326(7383):233–234.<br />
127. Albers GW, Amarenco P, Easton JD, Sacco RL, Teal P.<br />
Antithrombotic and Thrombolytic <strong>The</strong>rapy for Ischemic<br />
Stroke: <strong>The</strong> Seventh ACCP Conference on Antithrombotic<br />
and Thrombolytic <strong>The</strong>rapy. Chest 2004;126(3 Suppl):<br />
483S–512S.<br />
128. Moazami N, Smedira NG, McCarthy PM, et al. Safety and<br />
efficacy of intraarterial thrombolysis for perioperative<br />
stroke after cardiac operation. Ann Thorac Surg 2001;72(6):<br />
1933–1937.
10<br />
Alterations in Circulatory Function<br />
Thomas J. Ebert and G. Alec Rooke<br />
According to a 2006 statistical update published by the<br />
American Heart Association, 37.3% of all deaths in the<br />
United States in 2003 were attributable to cardiovascular<br />
disease (CVD). 1 About 83% of the deaths related to<br />
CVD occur in people age 65 and older. <strong>The</strong> prevalence<br />
of CVD in American men and women aged 65–74 are<br />
68.5% and 75%, respectively. For those aged 75+, prevalence<br />
is 77.8% and 86.4%, respectively. <strong>The</strong>se numbers<br />
demonstrate the strong association between adverse<br />
cardiac events and the aging process.<br />
With advancing age, the frequency of concurrent<br />
disease processes increases in a nearly exponential<br />
manner, such that many of the CVDs in the elderly have<br />
been considered an expected process of aging. We now<br />
recognize that preventing or delaying these disease processes<br />
through good nutrition and an active lifestyle can<br />
achieve “healthy or successful” aging. It is also recognized<br />
that preoperative “medical fitness” (a synonym for “successful<br />
aging”), rather than chronologic age, is an important<br />
determinant of postoperative outcome in the elderly<br />
surgical patient 2 (Figure 10-1).<br />
Even in the absence of the confounding influences of<br />
disease and lifestyle, the rate of functional aging on an<br />
organ or system, such as the cardiovascular system, varies<br />
from individual to individual. To better understand the<br />
expected effects of the “usual” aging process on the cardiovascular<br />
system, we must appreciate the net effect of<br />
the multiple, interdependent variables of heart rate, coronary<br />
blood flow, afterload or impedance, preload or diastolic<br />
filling, and inotropic state in describing cardiac<br />
function. All show age-dependent changes. <strong>The</strong> autonomic<br />
nervous system (ANS) modulates each of these<br />
variables through both sympathetic and parasympathetic<br />
mechanisms, and aging of the ANS further contributes to<br />
modifying cardiovascular function in the elderly.<br />
Although there is a general bias that age weakens the<br />
heart, in fact, this is not the case. Several functional adaptations<br />
of the heart help maintain resting and exercise<br />
cardiovascular physiology. 3 However, some of these<br />
adaptations account for problematic physiology in the<br />
elderly that adversely affects anesthetic management.<br />
This chapter will identify the critical changes in the cardiovascular<br />
system related to the aging process and the<br />
consequent modifications to the clinical management of<br />
the elderly undergoing anesthesia and surgery.<br />
Heart and Vessel Structural Alterations<br />
As the human body ages, it undergoes a variety of<br />
changes. Some of these changes are relatively benign.<br />
However, there are alterations that influence and<br />
even impair the overall health of the aging person. An<br />
example of such a detrimental digression accompanying<br />
increasing age is the increased stiffness of the heart and<br />
vascular tree.<br />
Many factors contribute to stiffening of the vascular<br />
tree. Aging can radically transform the endothelial<br />
layers via changes in extracellular matrix compositions.<br />
Elasticity in connective tissues depends primarily on the<br />
properties of its constituent collagen and elastin. Both<br />
connective tissue proteins are long-lived but slow in<br />
their production. By the age of 25, production of elastin<br />
has essentially ceased, and the rate of turnover of collagen<br />
decreases with increasing age. <strong>The</strong> consequent<br />
increase in the collagen-to-elastin ratio, plus an accumulating<br />
damage to collagen by glycation and free radicals,<br />
results in progressive connective tissue stiffness. Thus<br />
arteries, veins, and myocardium become less compliant<br />
over time.<br />
Nonenzymatic glycation is a reaction between reducing<br />
sugars and proteins on the vascular endothelium. Over<br />
time, these glycation sites cause tight crosslinking of proteins<br />
called advanced glycation end-products (AGE).<br />
This AGE formation leads to changes in the physiochemical<br />
properties of endothelial tissues. AGE crosslinking<br />
structurally results in vessels with less elasticity and<br />
137
138 T.J. Ebert and G.A. Rooke<br />
80<br />
*<br />
70<br />
60<br />
Active<br />
Inactive<br />
% Post-op Complications<br />
50<br />
40<br />
30<br />
*<br />
*<br />
*<br />
*<br />
20<br />
*<br />
10<br />
0<br />
Nil Chest Heart Acute<br />
Confusional<br />
State<br />
Wound<br />
Any Medical<br />
Complication<br />
Any Surgical<br />
Complication<br />
Life-<br />
Threatening<br />
Complication<br />
Figure 10-1. Preoperative activity level and percent occurrence<br />
of postoperative complications. Active = patients who normally<br />
left their home without assistance, at least two times per<br />
week. *p < 0.05. (Adapted with permission from Seymour DG,<br />
Pringle R. Post-operative complications in the elderly surgical<br />
patient. Gerontology 1983;29(4):262–270. Basel, Switzerland:<br />
S. Karger.)<br />
compliance. 4 Furthermore, the interaction of AGE<br />
with receptors for AGE (RAGE) on endothelial cells<br />
has been implicated as an initiating event in atherogenesis.<br />
In smooth muscle cells, binding of AGE-modified<br />
proteins to RAGE is associated with increased cellular<br />
proliferation of smooth muscle cells. This interaction<br />
also causes an increase in vascular cell adhesion molecule-1,<br />
which enhances binding of macrophages to the<br />
endothelial surface. This induces oxidative stress on<br />
the vascular endothelium and contributes to vascular<br />
stiffness. 5<br />
Several studies have shown that the nitric oxide<br />
pathway deteriorates with age. This has implications<br />
on vascular compliance. Nitric oxide suppresses key<br />
events in atherosclerotic development such as vascular<br />
smooth muscle proliferation and migration. It also<br />
inhibits the adhesion of monocytes and leukocytes in the<br />
endothelium, as well as platelet–vessel interaction.<br />
Furthermore, nitric oxide is known to regulate endothelial<br />
permeability, reducing the flux of lipoproteins into<br />
the vessel wall. 6 <strong>The</strong> reduced effects of nitric oxide on all<br />
of these pathways may contribute to vascular stiffness<br />
in aging.<br />
<strong>The</strong> above mechanisms serve to explain the pathogenesis<br />
of vascular stiffness associated with aging. As arterial<br />
walls stiffen, blood vessel compliance is reduced, leading<br />
to an increase in systolic blood pressure and pulse wave<br />
velocity (Figure 10-2). <strong>The</strong> reflected waves return earlier<br />
to the thoracic aorta, arriving by late ejection instead of<br />
early diastole. Thus, the left ventricle must pump against<br />
a higher pressure in late ejection than under normal circumstances.<br />
This additional afterload places an increased<br />
MEAN AORTIC PRESSURE (mmHg)<br />
120<br />
115<br />
110<br />
105<br />
100<br />
95<br />
90<br />
85<br />
80<br />
10 25 35 45 55 65 75<br />
AGE<br />
1300<br />
1200<br />
1100<br />
1000<br />
900<br />
800<br />
700<br />
600<br />
Figure 10-2. Mean aortic pressure (triangles) and pulse wave<br />
velocity (circles) in two Chinese populations: rural Guanzhou<br />
(unfilled symbols) and urban Beijing (filled symbols). (Adapted<br />
with permission from Avolio AP, Chen SG, Wang RP, Zhang CL,<br />
Li MF, O’Rourke MF. Effects of aging on changing arterial<br />
compliance and left ventricular load in a northern Chinese<br />
urban community. Circulation 1983;68:50–58.)<br />
AORTIC PULSE WAVE VELOCITY (cm/s)
10. Alterations in Circulatory Function 139<br />
LV thickness (mm/m 2 )<br />
7<br />
6<br />
5<br />
4<br />
3<br />
2<br />
1<br />
0<br />
y=3.08 + 0.035x<br />
r=0.64<br />
n=62<br />
10 20 30 40 50 60 70 80 90<br />
Age (yr)<br />
Figure 10-3. Left ventricular (LV) posterior wall thickness<br />
(mm/m 2 ) in normotensive men as a function of age (years).<br />
(Adapted with permission from Gerstenblith G, Frederiksen J,<br />
Yin FC, Fortuin NJ, Lakatta EG, Weisfeldt ML. Echocardiographic<br />
assessment of a normal adult aging population.<br />
Circulation 1977;56:273–278.)<br />
burden on the heart, particularly because it occurs late in<br />
systole when the myocardial muscle is normally losing its<br />
strength, and therefore provides a significant stimulus for<br />
cardiac hypertrophy (Figure 10-3).<br />
<strong>The</strong> cardiac muscle hypertrophy that develops secondary<br />
to the increased late systolic afterload also leads to<br />
myocardial stiffening and diastolic dysfunction. Diastolic<br />
dysfunction is defined as impairment in the relaxation<br />
phase of the ventricles. <strong>The</strong> aging heart contains AGE<br />
crosslinked collagen, which has the same effect on stiffness<br />
as it does in the peripheral vascular system. It is<br />
implicated in the signaling of macrophage recruitment in<br />
hypertensive myocardial fibrosis that contributes to deteriorating<br />
diastolic function. 4<br />
In diastolic dysfunction, there also is a functional component<br />
to the impairment of relaxation. It has been proposed<br />
that alterations in the myocyte calcium-handling<br />
proteins disturb the calcium transient in failing hearts.<br />
Calcium uptake in the sarcoplasmic reticulum declines<br />
with heart failure because of reduced expression of<br />
certain calcium channel enzymes. 7 This contributes to<br />
delayed relaxation of the myocardial muscle fibers, and<br />
the stiff ventricles have less ability to “spring open” in<br />
early diastole.<br />
As a consequence, there is a progressive decrease in<br />
the early diastolic filling period between the ages of 20<br />
and 80. At its worst, the diastolic filling period is reduced<br />
by 50% compared with younger controls. With increased<br />
stiffness, there also is a decline in the diastolic filling rate<br />
(Figure 10-4). However, resting end-diastolic volume<br />
does not change with increasing age. Because the passive<br />
early ventricular filling is impaired with age, the heart is<br />
increasingly dependent on an adequate atrial filling pressure<br />
and the atrial contraction (Figure 10-5). <strong>The</strong> atrial<br />
PEAK FILLING RATE (EDV/s)<br />
14<br />
12<br />
10<br />
8<br />
6<br />
4<br />
2<br />
LV Filling<br />
Young<br />
Advance Age<br />
A<br />
0<br />
20 30 40 50 60<br />
AGE (yr)<br />
70 80 90<br />
Figure 10-4. Changes in early diastolic left ventricular filling<br />
and the atrial contribution to filling associated with increased<br />
age. Age and peak filling rate relationship was obtained at rest<br />
(squares) and maximum workload (triangles). Inset: top image<br />
= left ventricular filling, young; bottom image = left ventricular<br />
filling, advanced age. (Adapted with permission from Lakatta<br />
EG. Cardiovascular aging in health. Clin Geriatr Med<br />
2000;16(3):419–444. Copyright © 2000 Elsevier.)<br />
Figure 10-5. Echo-Doppler evaluation of diastolic filling in<br />
healthy men and women as a function of age. A: Early diastolic<br />
filling volume (% of total volume). B: Diastolic filling caused<br />
by atrial contraction (% of total volume). (Adapted with<br />
permission from Lakatta. 3 )<br />
B
140 T.J. Ebert and G.A. Rooke<br />
Figure 10-6. <strong>The</strong> increased ventricular stiffness associated with<br />
age requires an increased atrial pressure to achieve the same<br />
end-diastolic volume. (Adapted with permission from Dauchot<br />
PJ, Cascorbi H, Fleisher LA, Prough DS, eds. Problems in <strong>Anesthesia</strong>:<br />
Management of the Elderly Surgical Patient. Vol. 9,<br />
No. 4. Philadelphia: Lippincott-Raven; 1997:482–497.)<br />
pressures must rise to maintain the end-diastolic volume<br />
in the presence of stiffened ventricles. <strong>The</strong> increased<br />
atrial pressure can result in increased pulmonary blood<br />
pressures and ultimately lead to congestion in the systemic<br />
venous circulation. <strong>The</strong> cumulative effect of these<br />
alterations results in diastolic dysfunction (Figure 10-6).<br />
About half of heart failure in the elderly population<br />
(older than 75 years) is associated with impaired<br />
left ventricular diastolic function, but preserved left<br />
ventricular systolic function. 8 Unfortunately, patients<br />
with isolated left ventricular diastolic dysfunction are<br />
not as likely to present with the traditional physical<br />
manifestations of heart failure. Instead, they are frequently<br />
asymptomatic or present with only mild pulmonary<br />
congestion, exertional dyspnea, and orthopnea.<br />
<strong>The</strong>se symptoms may be aggravated by systemic stressors<br />
such as fever, exercise, tachycardia, or anemia. As a<br />
result, prevention and detection of diastolic heart<br />
failure may be difficult since it is often recognized only<br />
by echocardiography.<br />
Systolic function of the heart also is affected by the<br />
aging process. From a functional standpoint, the prolonged<br />
myocardial contraction maintains the flow delivered<br />
to the stiffened arterial tree, thereby maintaining<br />
cardiac output (Figure 10-7). <strong>The</strong> functional adaptation<br />
to vascular stiffening and afterload is able to maintain<br />
Arterial stiffening<br />
Increased arterial<br />
systolic and<br />
pulse pressure<br />
Increased pulse wave velocity<br />
Early reflected waves<br />
Late peak in systolic pressure<br />
Increased aortic root size<br />
Increased aortic wall thickness<br />
Increased aortic impedance<br />
and LV loading<br />
Increased LV wall<br />
tension<br />
Increased LV<br />
hypertrophy<br />
Prolonged myocardial<br />
contraction<br />
Increased left<br />
atrial size<br />
Increased<br />
atrial filling<br />
Normalization<br />
of LV wall<br />
tension<br />
Increased<br />
myocardial<br />
contraction<br />
velocity<br />
Prolonged force<br />
bearing capacity<br />
Decreased early<br />
diastolic filling rate<br />
Increased<br />
energetic efficiency<br />
Slightlly increased<br />
end-diastolic volume<br />
Preserved endsystolic<br />
volume and<br />
ejection fraction<br />
Maintenance of ejection time<br />
Figure 10-7. A cascade of functional adaptations to vascular stiffening in the elderly. LV = left ventricular. (Adapted with permission<br />
from Lakatta EG. Cardiovascular aging in health. Clin Geriatr Med 2000;16(3):419–444. Copyright © 2000 Elsevier.)
10. Alterations in Circulatory Function 141<br />
cardiac output at rest; however, an age-related decline in<br />
systolic function may be unmasked in the presence of<br />
exercise or sympathetic stimulation. For example,<br />
administration of an α-adrenergic agonist such as phenylephrine<br />
will acutely increase afterload to the heart,<br />
increasing left ventricular wall stress during systole,<br />
unmasking an age-related decrease in contractile<br />
reserve. 9<br />
Further studies have shown that there is abnormal systolic<br />
function in many patients who have hypertensioninduced<br />
concentric hypertrophy with a normal ejection<br />
fraction. Reduced midwall shortening in relation to stress<br />
is clearly evident in patients with greater relative wall<br />
thickness. This translates to abnormal pump function and<br />
reduced cardiac output. Subtle systolic dysfunction may<br />
be present even if patients have seemingly normal ejection<br />
fractions and are without clinical heart failure, and<br />
it would be incorrect to equate a normal ejection fraction<br />
with normal systolic function. 10<br />
Reduced vascular compliance, diastolic dysfun -<br />
ction, and systolic dysfunction in the elderly are all interconnected.<br />
It is reasonable to assume that these are not<br />
separate pathologies and in fact develop in parallel.<br />
Reduced vascular compliance resulting in hypertension,<br />
increased afterload, and eventual cardiac remodeling is<br />
an extremely common finding in the aging population. In<br />
a large portion of this group, this inevitably results in<br />
some evidence of diastolic dysfunction. Furthermore, the<br />
above concepts demonstrate that some systolic dysfunction<br />
exists in many of these same hypertensive elderly<br />
patients.<br />
<strong>The</strong> interrelationships among vascular stiffening,<br />
hypertension, diastolic dysfunction, and even systolic dysfunction<br />
in the absence of overt cardiac disease have led<br />
to a reexamination of our concepts of hypertension and<br />
its management. Conventional wisdom suggests that<br />
patients who have hypertension can sometimes be classified<br />
as “systolic” hypertension or “diastolic” hypertension<br />
if their hypertension is limited to their systolic or diastolic<br />
pressure, respectively. However, an emerging concept is<br />
of “pulse pressure” hypertension and is characterized by<br />
a large difference between systolic and diastolic pressure,<br />
for example, 80 mm Hg or greater. 11<br />
A relatively high systolic pressure in comparison to<br />
diastolic is harmful for several reasons. First, a high pulse<br />
pressure indicates that the patient’s arterial conduit<br />
system is stiff. Low compliance means that a high systolic<br />
pressure is required in order to distend the aorta and<br />
other large arteries as the stroke volume is received.<br />
Even though this increase in pressure occurs relatively<br />
early in ejection, it still forces the ventricle to pump<br />
against a high pressure and stimulates hypertrophy<br />
that, in turn, increases myocardial stiffness and further<br />
impairs diastolic relaxation. Indeed, there is a strong correlation<br />
between the severity of reduced arterial compliance<br />
and the severity of diastolic dysfunction. 12 Second,<br />
when the diastolic pressure is low compared with systolic<br />
pressure, there is an immediate predisposition to an<br />
imbalance of myocardial oxygen supply and demand.<br />
Demand correlates most closely to systolic pressure, 13<br />
whereas coronary blood flow occurs mostly during diastole,<br />
making supply highly dependent on diastolic pressure.<br />
With rapid transit of reflected arterial waves, there<br />
is loss of the accentuated pressure in early diastole. This<br />
lowering of aortic pressure during diastole potentially<br />
diminishes coronary perfusion. In patients with coronary<br />
stenoses, this imbalance could result in subendocardial<br />
ischemia, thereby worsening diastolic relaxation and<br />
increasing atrial pressure.<br />
Because of the consequences of arterial stiffening, arterial<br />
compliance has been suggested as a better measure<br />
of biologic age, as opposed to chronologic age. 14 And it is<br />
not surprising that there is great interest in strategies to<br />
reduce or even reverse arterial stiffening in the hope of<br />
preventing CVD. Current human therapy primarily<br />
involves drugs that relax smooth muscle tone. 15 Statins<br />
not only inhibit myocardial remodeling but may reduce<br />
vascular stiffness. Angiotensin blockers and aldosterone<br />
seem to lessen fibrosis. In recent studies that have largely<br />
been limited to animals, drugs have been used to break<br />
the stiffening links in connective tissue proteins caused<br />
by glycosylation. 15,16 In the meantime, exercise slows<br />
vascular stiffening and remains a useful therapy for all<br />
ages.<br />
Reflex Control Mechanisms and Aging<br />
<strong>The</strong> aging process affects autonomic cardiovascular<br />
control mechanisms in a nonuniform manner. Attenuated<br />
respiratory sinus arrhythmia in older individuals suggests<br />
that parasympathetic control of sinus node function<br />
declines with age. Because the reflex regulation of heart<br />
rate in humans is primarily dependent on cardiac vagal<br />
activity, it is correct to assume that the impaired baroreflex<br />
regulation of heart rate is related to deficient parasympathetic<br />
mechanisms (Figure 10-8). Although the<br />
parasympathetic component of the arterial baroreflex<br />
becomes diminished in the aging population, the baroreflex<br />
control of sympathetic outflow and the vascular<br />
response to sympathetic stimulation are well maintained<br />
in moderately old, active individuals. 17 It is well established<br />
that basal levels of plasma catecholamines and<br />
sympathetic nerve activity increase with age. Plasma noradrenaline<br />
levels increase 10%–15% per decade. 18 In<br />
addition, there is an age-dependent reduction in activity<br />
of the cardiac neuronal noradrenaline reuptake mechanism,<br />
resulting in higher concentrations of noradrenaline<br />
at β 1 -receptor sites in the heart. 19
142 T.J. Ebert and G.A. Rooke<br />
A<br />
B<br />
msec<br />
mm Hg<br />
cardiac<br />
baroslope.<br />
40<br />
30<br />
20<br />
10<br />
y = -0.31x + 27.9<br />
r = 0.608, n = 66<br />
R·R interval, msec<br />
1400<br />
1200<br />
1000<br />
800<br />
18-34 yr, n = 35<br />
35-50 yr, n = 15<br />
51-70 yr, n = 16<br />
0<br />
10 20 30 40 50 60 70 80<br />
age, yr<br />
Figure 10-8. A: Individual cardiac baroreflex sensitivities<br />
versus age. Regression revealed a significant (p < 0.05) inverse<br />
relationship between reflex sensitivity and age. B: Mean regression<br />
lines describing relationship between mean arterial<br />
pressure and corresponding R-R interval for each of the three<br />
600<br />
70 80 90 100 110<br />
mean arterial pressure, mm Hg<br />
age groups. Regression line slopes were smaller in older and<br />
middle-aged subjects than in younger subjects. Baseline values<br />
(mean ± SE) are superimposed on regression lines. (Adapted<br />
with permission from Ebert et al. 17 )<br />
Adrenergic Receptor Activity<br />
and Aging<br />
Aging has been associated with a decrease in the response<br />
to stimulation of β-receptors. This is noted in the peripheral<br />
circulation by a reduced arterial and venous dilation<br />
response to the β-agonist, isoproterenol, and the mixed<br />
agonist, epinephrine, in the elderly (Figure 10-9). In<br />
CHANGE IN HEART RATE (bpm)<br />
30<br />
25<br />
20<br />
15<br />
10<br />
5<br />
0<br />
0.00 0.25 0.50 1.00 2.00 4.00<br />
ISOPROTERENOL (mcg)<br />
Figure 10-9. <strong>The</strong> effect of intravenous isoproterenol infusions<br />
on increasing heart rate in healthy young (filled circles) and<br />
older (unfilled circles) men at rest. (Adapted with permission<br />
from Lakatta EG. Cardiovascular aging in health. Clin Geriatr<br />
Med 2000;16(3):419–444. Copyright © 2000 Elsevier.)<br />
cardiac muscle, there is a reduction in the inotropic<br />
response to exercise and to the administration of catecholamines<br />
in the aging patient. 20 In isolated cardiac<br />
myocytes, it has been shown that the EC 50 for isoprenaline<br />
(a β 1 - and β 2 -agonist) is nearly twice as high in the<br />
elderly. 18 A result of the decreased contractile response<br />
to β-adrenergic stimulation in the elderly is a greater<br />
dependency on the Frank-Starling (length-tension)<br />
mechanism of contraction to maintain cardiac output.<br />
Although multiple studies indicate that the heart rate<br />
increase to β-stimulation of the heart is attenuated with<br />
age, recent data question the age-related attenuated<br />
chronotropic response. 20 Studies also provide conflicting<br />
results regarding age-related changes in myocardial β-<br />
adrenoceptor density. <strong>The</strong> mechanism for decreased<br />
cardiac inotropic response to sympathetic stimulation is<br />
more likely attributable to changes in the second messenger<br />
system. Impaired coupling of the β-adrenoceptor<br />
to the Gs protein and to the catalytic unit of adenylyl<br />
cyclase is consistently observed in the elderly myocardium.<br />
Furthermore, an increase in Gi protein levels<br />
observed in aged myocardial tissue indicates a reduction<br />
in the catalytic subunit of adenylyl cyclase. 21 Both of these<br />
mechanisms will attenuate adenosine 3′,5′-cyclic monophosphate<br />
(cAMP) formation and subsequent β-adrenoceptor<br />
response. This desensitization of the intracellular<br />
processing of receptor signaling is likely a compensatory<br />
adaptation to an increase in endogenous norepinephrine<br />
resulting from age-related increases in sympathetic activity<br />
and reduced neuronal uptake of norepinephrine.<br />
This attenuated β-adrenoceptor response as a result of<br />
changes in second messenger function has implications in
10. Alterations in Circulatory Function 143<br />
the peripheral vascular system. Vasorelaxation is accomplished<br />
in vascular smooth muscle cells via cAMP. cAMP<br />
activates protein kinase A (PKA) that then lowers cytosolic<br />
calcium levels, causing vasorelaxation. Decreased<br />
generation of cAMP in the vasculature leads to impairment<br />
of this pathway. This may be a contributing factor<br />
for hypertension in the elderly. And because cAMP is an<br />
antiproliferative agent, this deficiency may be associated<br />
with the progression of atherosclerosis. 21<br />
Genetic variation in β-adrenoceptors is now documented<br />
and may have a significant role in CVD heterogeneity<br />
among individuals. <strong>The</strong>re are many known<br />
polymorphisms of both β 1 - and β 2 -adrenoceptor subtypes.<br />
<strong>The</strong>se variants may have differing effects on the cardiovascular<br />
system with age. <strong>The</strong> most common polymorphism,<br />
whose allele frequency is 60%, causes enhanced<br />
down regulation of β 2 -adrenoceptors. Because peripheral<br />
β 2 -receptors cause vasodilation and a reduction in blood<br />
pressure, individuals with this polymorphism are more<br />
prone to hypertension with increasing age. This fact has<br />
been confirmed in familial studies, which show increased<br />
prevalence of this allele in families with a history of<br />
essential hypertension. Another β-adrenoceptor polymorphism<br />
with important implications in cardiac disease<br />
is one that causes blunted agonist responsiveness. Studies<br />
have shown that in heart failure patients, this variant<br />
carries a relative risk of death or transplant of 4.8 compared<br />
with the normal allele. <strong>The</strong>re also exists a particular<br />
polymorphism that tends to improve survival in those<br />
with heart failure. <strong>The</strong> existence of β-receptor polymorphisms<br />
may have additional implications for the efficacy<br />
of β-blockade. However, at this time, little is known about<br />
their particular impact on patient therapy. 22<br />
It would seem logical to expect a down regulation of<br />
α-adrenergic receptors with age, but surprisingly the<br />
number of α 1 -receptors remains well preserved. Interestingly,<br />
in normotensive older subjects, an increased rate of<br />
infusion of an α-agonist is required to achieve the same<br />
degree of vasoconstriction compared with young subjects.<br />
8 Animal studies have shown that maximal binding<br />
of vascular α 1 -receptors is significantly reduced with<br />
age. 23 <strong>The</strong> α 2 -receptors appear to show some age-related<br />
decline. Normally, α 2 -receptors predominate in the venous<br />
side of the circulation, suggesting that a compromised<br />
venoconstrictor response to the upright posture, secondary<br />
to α 2 -receptor loss, might contribute to orthostatic<br />
intolerance in the elderly. 17 <strong>The</strong> evidence of adrenergic<br />
receptor desensitization with age has further implications<br />
as hypertension develops in the elderly. In normotensive<br />
elderly subjects, the decrease in responsiveness of α-<br />
adrenergic receptors seems to be a regulated compensatory<br />
effect of the heightened level of sympathetic nervous<br />
system activity in the elderly. Despite some evidence of<br />
diminished α-adrenergic responsiveness, it seems that the<br />
overall baroreflex control of vasoconstriction is well preserved<br />
with age and might be heightened compared with<br />
young adults. 7,24<br />
As with β-adrenoceptors, polymorphisms in α-<br />
adrenergic receptors may have implications on hypertension<br />
and cardiac disease in the elderly. It has been<br />
proposed that individuals with a particular α 2B -adrenergic<br />
receptor polymorphism may be at greater risk for<br />
acute coronary events and sudden cardiac death. 25 <strong>The</strong> in<br />
vivo effect of the α 2 -agonist dexmedetomidine on patients<br />
with this polymorphism has been investigated and there<br />
is a trend toward an increased systolic blood pressure<br />
response to dexmedetomidine in patients with this<br />
polymorphism. 25<br />
Vagal Activity and Aging<br />
Baroreflex control of heart rate is known to be diminished<br />
in older individuals. Indeed, there clearly is an<br />
attenuated respiratory sinus arrhythmia suggesting either<br />
reduced vagal outflow or reduced intracellular responses<br />
to muscarinic receptor activation with age. 26 Both changes<br />
seem to be present in the elderly. Lower resting vagal<br />
tone in the elderly has been implicated in the diminished<br />
heart rate increase in response to a large dose of atropine<br />
compared with younger controls. 8 Studies have shown<br />
that right atrial muscarinic receptor density is significantly<br />
and negatively correlated with age. Furthermore,<br />
it has also been shown that muscarinic receptor function<br />
declines in the elderly population. This is evident by a<br />
reduction in carbachol-induced inhibition of forskolinactivated<br />
adenylyl cyclase in muscarinic receptors of aged<br />
myocardium. 27 All of these mechanisms, taken together,<br />
contribute to reduced vagal activity in the elderly. Finally,<br />
autoantibodies to M 2 -muscarinic receptors exist in the<br />
sera of normal individuals, and are found in high levels<br />
in those with idiopathic dilated cardiomyopathy. <strong>The</strong><br />
prevalence of these autoantibodies is significantly<br />
increased in the elderly. 28 <strong>The</strong> implications of these findings<br />
on muscarinic receptor function and cardiac performance<br />
have yet to be determined.<br />
Renin and Vasopressin Activity<br />
As already described, there are many vascular changes<br />
associated with aging. <strong>The</strong>se changes contribute to renal<br />
damage and functionally result in decreased glomerular<br />
filtration rate and renal blood flow. Aging also affects<br />
sodium balance in the kidney. This results in decreased<br />
ability to conserve sodium in the face of sodium restriction<br />
as well as a decreased sodium excretion in the presence<br />
of increased sodium load. Despite the increased<br />
sympathetic activity accompanying old age, the elderly<br />
experience a decrease in plasma and renal levels of renin.
144 T.J. Ebert and G.A. Rooke<br />
Plasma renin activity is diminished in the supine position,<br />
and physiologic stimuli such as hemorrhage, sodium<br />
restriction, and orthostasis are followed by attenuated<br />
increases in renin release and consequently lower concentrations<br />
of angiotensin in the circulation. 29 Although<br />
renin-angiotensin levels are decreased in the elderly, the<br />
aging population shows an enhanced vasoconstriction in<br />
response to angiotensin I and angiotensin II. <strong>The</strong> above<br />
finding helps to explain the key role that angiotensinconverting<br />
enzyme inhibitors and angiotensin II receptor<br />
blockers have in improving renal structure and function<br />
in the elderly. 30<br />
In the elderly, there seems to be an elevation in plasma<br />
vasopressin levels under basal conditions and a heightened<br />
response to an osmotic challenge such as water<br />
deprivation. Surprisingly, after a water restriction period,<br />
older subjects had a relatively low spontaneous fluid<br />
consumption as well as diminished thirst. 29 In addition,<br />
by age 80, the total body water content has declined to<br />
50% of body mass from the average content of 60% in<br />
younger persons. 31 Such decreases in thirst mechanism,<br />
total body water, and fluid consumption in combination<br />
with an age-related decrease in glomerular function cause<br />
older persons to be increasingly vulnerable to water<br />
imbalance.<br />
Arrhythmias<br />
Several changes with aging predispose the older patient<br />
to arrhythmias. Sinus node dysfunction develops with the<br />
progressive loss of pacemaker cells, and contributes to<br />
the risk of sick sinus syndrome and/or bradycardia. 32 Bradycardia<br />
promotes atrial fibrillation as does age-related<br />
atrial fibrosis and atrial enlargement. <strong>The</strong> incidence of<br />
atrial fibrillation increases with age such that it is present<br />
in 10% of those over 80. This predisposition to atrial<br />
fibrillation undoubtedly contributes to the relatively high<br />
incidence of new onset atrial fibrillation (and supraventricular<br />
tachycardia) not only after thoracic and cardiac<br />
surgery, but after most major surgical procedures. Patients<br />
presenting for surgery who are found to have previously<br />
undiagnosed atrial fibrillation should be evaluated before<br />
surgery, including an echocardiogram to rule out structural<br />
abnormality. Perioperatively, the management of<br />
new onset atrial fibrillation is initially rate control, with<br />
restoration of sinus rhythm within 24 hours as the next<br />
goal in order to reduce the risk of clot formation and<br />
thromboembolus. 33 For patients with chronic atrial<br />
fibrillation, early anticoagulation after surgery may be<br />
important, especially if the patient is at high risk for<br />
thromboembolism.<br />
Heart block and ventricular ectopy are examples of<br />
other arrhythmias prevalent in older patients. 34 Heart<br />
block below the atrioventricular node most often occurs<br />
secondary to idiopathic degeneration of the conduction<br />
system, but is not likely to carry adverse consequences<br />
unless there is concomitant cardiac disease.<br />
Ischemic Preconditioning<br />
An episode of myocardial ischemia reduces the severity<br />
of myocardial damage associated with a subsequent,<br />
more prolonged ischemic event. This phenomenon, known<br />
as ischemic preconditioning, exists in both an immediate<br />
(minutes to a few hours) and delayed (many hours to<br />
days) form. 35 Clinically, ischemic preconditioning is likely<br />
involved with warm-up angina in which patients who<br />
exert to the onset of angina, rest, and exert again can then<br />
achieve higher levels of exertion before developing the<br />
second bout of angina. 36 Patients who suffer a myocardial<br />
infarction are much less likely to die or develop heart<br />
failure if they experienced angina within 48 hours of their<br />
myocardial infarction. 37 Exposure to volatile anesthetics<br />
yields a preconditioning effect as well. 35<br />
Unfortunately, aging is associated with the loss of ischemic<br />
preconditioning. Warm-up angina is nonexistent<br />
beyond age 75 38 and in patients older than 65, myocardial<br />
infarction with or without antecedent angina is associated<br />
with the same high rates of death and heart failure as<br />
younger subjects who did not have prior angina. 37 At least<br />
in an animal model, anesthetic cardioprotection from<br />
preconditioning is essentially abolished in aged rats. 39,40<br />
Implications in <strong>Anesthesia</strong><br />
Although normal aging affects virtually all components<br />
of the cardiovascular system, perhaps the most important<br />
changes that influence anesthetic management in the<br />
elderly are the stiffened cardiac and vascular system,<br />
the diminished β-adrenergic receptor response, and the<br />
impaired autonomic reflex control of heart rate. Compounding<br />
these age-related changes are the well-described<br />
effects of the intravenous and volatile anesthetics on the<br />
myocardium, vascular tone, and the ANS.<br />
Many of the elderly patients coming to the operating<br />
room are in a relatively volume-depleted state because<br />
of NPO guidelines, reduced thirst mechanisms, and diminished<br />
renal capacity to conserve water and salt. Additionally,<br />
increases in heart rate and contractility during volume<br />
loss are limited by diminished reflex control systems and<br />
by reduced β-receptor responses. Consequently, further<br />
hypovolemia, e.g., intraoperative blood loss, can result in<br />
substantial hypotension. This volume sensitivity of the<br />
elderly has been demonstrated in the laboratory during<br />
head-up tilt testing after subjects had been made hypovolemic<br />
with diuretics and low salt intake. <strong>The</strong> older subjects<br />
had greater decreases in blood pressure during
10. Alterations in Circulatory Function 145<br />
Figure 10-10. Hemodynamic response to high spinal anesthesia<br />
in older men with a history of cardiac disease. MAP = mean<br />
arterial pressure, SVR = systemic vascular resistance, CO =<br />
cardiac output, HR = heart rate, SV = stroke volume, EF =<br />
ejection fraction, EDV = left ventricular end-diastolic volume.<br />
(Adapted with permission from Rooke et al. 48 )<br />
upright tilting than both the younger hypovolemic control<br />
subjects and the older normovolemic control subjects. 41<br />
Impaired responses to hypovolemia are further confounded<br />
by volatile anesthetics and the sedative-hypnotics<br />
that impair baroreflex control mechanisms. 42,43 Healthy<br />
or preserved baroreflex control mechanisms clearly minimize<br />
the cardiovascular changes that result from anesthetics.<br />
For example, diabetic patients with preserved<br />
autonomic reflexes had a lower incidence of hypotension<br />
during induction and maintenance of anesthesia than<br />
patients with impaired reflexes. 44 Thus, the net effect of<br />
physiologic changes with adult aging compounded by<br />
anesthetic effects should be more frequent and more significant<br />
blood pressure changes in the elderly. Such blood<br />
pressure lability has been observed in older patients. 45,46<br />
In the aged patient, the relative hypovolemic state has<br />
many important clinical implications. <strong>The</strong> elderly heart is<br />
heavily dependent on an adequate end-diastolic volume<br />
to maintain stroke volume, and cardiac filling is in turn<br />
dependent on higher atrial filling pressures because of a<br />
stiffened ventricle and possible diastolic dysfunction. As<br />
a result, the elderly are very sensitive to hypovolemia. In<br />
this setting, decreased systemic blood pressure should<br />
generally be treated with intravenous fluids rather than<br />
vasopressors to maintain proper diastolic function. One<br />
study has shown that volatile anesthetics do not impair<br />
diastolic function whereas propofol has some negative<br />
effects. 47<br />
As important as maintenance of an adequate cardiac<br />
preload is to an older patient, it is equally important to<br />
avoid excess fluid administration. <strong>The</strong>re are two ways in<br />
which one can be misled into administration of excess<br />
volume. First, with anesthetic-induced relaxation of vascular<br />
smooth muscle and/or sympathectomy comes venodilation<br />
and increased venous pooling of blood.<br />
Restoration of preload would therefore seem to require<br />
significant volume administration just to compensate for<br />
the effects of the anesthetic. However, once the anesthetic<br />
is worn off, vascular smooth muscle relaxation<br />
lessens and sympathetic tone is not only restored, but<br />
quite possibly heightened because of pain or recovery<br />
from the surgical trauma. Restoration of normal to<br />
increased venous tone will then shift that excess volume<br />
back to the heart and potentially lead to pulmonary and<br />
cardiac dysfunction as the elderly heart copes with what<br />
now is volume overload.<br />
<strong>The</strong> second mechanism that can mislead practitioners<br />
into giving excess volume occurs when cardiac filling and<br />
cardiac output are not diminished, but the patient is still<br />
hypotensive from arterial vasodilation. <strong>The</strong> natural reaction<br />
to hypotension is to assume the patient is hypovolemic<br />
and therefore give more volume. That treatment may<br />
not be appropriate with older patients. Young, healthy<br />
patients have minimal sympathetic tone when supine and<br />
at rest. Thus, anesthesia is likely to decrease blood pressure<br />
in young patients more by the direct effects of the<br />
anesthetic on blood vessels than by removal of sympathetic<br />
tone. Elderly patients, however, often have high<br />
levels of sympathetic tone 17 and removal of that tone can<br />
produce more than just an apparent hypovolemia. In a<br />
study of older men with varying degrees of cardiac disease,<br />
high spinal anesthesia produced an average decrease in<br />
blood pressure of 33% (Figure 10-10). 48 Even though<br />
pooling of blood in the abdomen and legs caused a 19%<br />
decrease in left ventricular end-diastolic volume, cardiac<br />
output only decreased by 10%, largely because the<br />
decrease in blood pressure (afterload reduction) allowed<br />
the ejection fraction to increase. <strong>The</strong> primary mechanism<br />
for hypotension, however, was the 26% decrease in systemic<br />
vascular resistance. It is physically impossible to<br />
increase end-diastolic volume indefinitely and fully compensate<br />
for such a significant decrease in vascular resistance.<br />
In fact, it could be argued that the attempt would<br />
merely predispose the patient to volume overload, especially<br />
on emergence as discussed above. Increased left<br />
ventricular end-diastolic pressures from excessive volume<br />
could also precipitate or aggravate myocardial ischemia<br />
by creating high left ventricular subendocardial wall<br />
stress. 49<br />
In all but the sickest of older patients, therefore, the<br />
most likely mechanism of intraoperative hypotension is<br />
either decreased vascular resistance or hypovolemia.<br />
Should bradycardia be a limiting factor, it is easily detected<br />
and treated. What should be done, then, to manage the<br />
patient who is hypotensive with a stable heart rate even<br />
after adequate volume deficits are replaced? Vasopressors<br />
are the likely treatment of choice, with ephedrine and<br />
phenylephrine being the most frequently used agents.<br />
Phenylephrine has the advantage over ephedrine in that<br />
it does not exhibit tachyphylaxis and will not promote
146 T.J. Ebert and G.A. Rooke<br />
tachycardia. Furthermore, α-receptor activation generally<br />
results in venoconstriction in addition to vasoconstriction,<br />
thereby shifting blood from the periphery back to the<br />
heart and alleviating the anesthetic-induced peripheral<br />
pooling. 50 As with all drugs, adverse consequences can<br />
occur. Coronary vasoconstriction, decreased cardiac<br />
output, imbalance in the distribution of the cardiac output,<br />
and wall motion abnormalities are all potential undesired<br />
effects. <strong>The</strong> key to the rational use of pressors such as<br />
phenylephrine is to minimize hypovolemia, and not feel<br />
obliged to return overall vascular resistance back to preanesthetic<br />
levels. In other words, tolerate a mild decrease<br />
in blood pressure. <strong>The</strong> cardiac dysfunction that has been<br />
observed with the use of phenylephrine typically occurs<br />
when blood pressure is increased to levels above the<br />
patient’s awake baseline, 9 or under unusual loading conditions<br />
such as excessive anesthesia. 51<br />
How can we foresee, prevent, or treat the elderly patient<br />
who has not successfully aged such that he has a decreased<br />
cardiovascular reserve and is to be exposed to anesthetic<br />
and surgical stresses? A pulmonary artery catheter and/or<br />
transesophageal echocardiography to monitor cardiac<br />
filling pressures/volumes along with invasive blood pressure<br />
monitoring are the obvious answers that would<br />
permit very tight control of preload and afterload.<br />
However, this approach should be reserved for the elderly<br />
patient with significant limitation of cardiac performance<br />
related to coexisting CVD (e.g., coronary artery disease,<br />
congestive heart failure, or documented significant myocardial<br />
injury). <strong>The</strong> need for such extensive monitoring<br />
also must be weighed against the risks for blood loss and<br />
stress associated with the planned surgical intervention.<br />
A more realistic approach is to obtain a careful history<br />
and chart review to get a reasonably good idea of the<br />
biologic age of the patient. <strong>The</strong> importance of determining<br />
the biologic age or “medical fitness” of the elderly<br />
patient has been emphasized by a prospective study demonstrating<br />
a significant relationship between coexisting<br />
diseases in the elderly patient and postoperative morbidity<br />
and mortality 52 (Figure 10-11). In addition, the preoperative<br />
level of physical activity proved to be a sensitive<br />
predictor of postoperative morbidity.<br />
In a patient who has aged “successfully,” routine monitoring<br />
with close attention to fluid status and a more<br />
gradual titration and thoughtful selection of anesthetics<br />
may be sufficient to minimize the nearly unavoidable<br />
hypotension. A useful approach in the anesthetic management<br />
of the elderly is to replace NPO deficits before<br />
anesthetic induction and to induce anesthesia with etomidate.<br />
It has been demonstrated that there is a good preservation<br />
of sympathetic outflow and autonomic reflexes<br />
with this sedative/hypnotic. 53 However, opioids or esmolol<br />
must be given to avoid the reflex response to tracheal<br />
intubation that is poorly attenuated by etomidate. Benzodiazepines<br />
should be minimized or avoided because<br />
Figure 10-11. <strong>The</strong> influence of age and comorbid disease on<br />
major perioperative complications. Increased comorbid disease<br />
is associated with increased risk of complications, regardless of<br />
age. In patients free of disease, age has a minimal effect on risk.<br />
In patients with multiple diseases, however, the effect of age is<br />
substantial. (Adapted with permission from Tiret et al. 52 )<br />
they interact with opioids to produce sympatho-inhibition<br />
and hypotension.<br />
<strong>The</strong> goal of anesthesia in the elderly is cardiac stability.<br />
Volatile agents are direct vasodilators and are known to<br />
depress baroreflex responses. Furthermore, volatile anesthetics<br />
can produce myocardial depression and nodal<br />
rhythms that are poorly tolerated in patients with cardiac<br />
abnormalities such as aortic stenosis, mitral stenosis, or<br />
hypertrophic obstructive cardiomyopathy. 54 A preference<br />
might be given to the new, less soluble, volatile anesthetics<br />
because they can be titrated up or down quickly, and<br />
emergence times as well as time to orientation are remarkably<br />
better than with the older volatile anesthetics. 55<br />
Maintenance can include nitrous oxide when appropriate,<br />
because it helps to maintain sympathetic outflow and<br />
lessens the need for higher concentrations of the potent<br />
volatile anesthetics.<br />
Hypertension and tachycardia should be recognized as<br />
undesirable events in the elderly because of the increased<br />
myocardial oxygen demand and the reduced time for<br />
atrial filling and coronary flow. Esmolol can be given<br />
(0.5–1.0 mg/kg) to attenuate the intubation response and<br />
avoid excessive increases in heart rate. α 2 -Agonists such<br />
as clonidine or dexmedetomidine also are effective in<br />
reducing the sympathetic response to laryngoscopy and<br />
intubation, but add to intraoperative hypotension because<br />
of their long half-lives. Additionally, adequate analgesia<br />
is an important aspect of heart rate and blood pressure<br />
control. Fentanyl can be titrated (1–3 µg/kg) before intubation<br />
to attenuate the sympathetic response. Naloxone
10. Alterations in Circulatory Function 147<br />
should be avoided or used with extreme caution in the<br />
elderly, because large doses can cause pain, leading to an<br />
acute increase in catecholamine levels. This may result in<br />
life-threatening complications such as pulmonary edema,<br />
myocardial ischemia, arrhythmias, and cardiac arrest. 54<br />
In patients at higher risk of coronary ischemia and<br />
undergoing noncardiac surgery, prophylactic, perioperative<br />
β-blockade should be considered. Many studies have<br />
shown a decreased incidence of myocardial ischemia,<br />
as well as an overall survival benefit when β-blockers<br />
are administered perioperatively, 56 although optimal<br />
duration of β-blockade both pre- and postoperatively<br />
remains uncertain. β-Blockade may induce protective<br />
effects via many mechanisms. It may reduce the neuroendocrine<br />
stress response with surgery, it may reduce the<br />
incidence of acute coronary plaque rupture by reducing<br />
shear stress, and it may decrease the incidence of cardiac<br />
arrhythmias. 54 For those patients receiving chronic β-<br />
blocker therapy, it should be continued in the perioperative<br />
period. In fact, an increase in the dosage may be<br />
prudent. 49<br />
Postoperatively, the older patient will be at risk for<br />
developing pulmonary congestion when significant third<br />
spaced fluid becomes mobilized. Patients with no history<br />
of heart failure, but who have borderline diastolic dysfunction,<br />
stiff vessels, and/or poor renal function, may<br />
experience significant increases in atrial pressure with<br />
even modest increases in blood volume. Careful and frequent<br />
bedside examination of the patient during the first<br />
several postoperative days may permit timely use of<br />
diuretics; avoiding fluid overload may prevent progression<br />
to more serious complications such as hypoxia, respiratory<br />
failure, cardiac dysfunction, or myocardial<br />
infarction.<br />
Summary<br />
A stiffened heart and vascular system, impaired autonomic<br />
control mechanisms, and altered β-receptor function<br />
characterize an aging cardiovascular system. <strong>The</strong>se<br />
alterations make the aged heart more sensitive to volume<br />
changes in the face of minimal ability to compensate<br />
via the ANS. When biologic age (“medical fitness”)<br />
exceeds chronologic age, these changes are likely worsened.<br />
<strong>The</strong> addition of volatile anesthetics or propofol<br />
causes further changes in the ANS and increases the risk<br />
of hemodynamic fluctuations. Finally, compounding biologic<br />
age and anesthetics with surgical stress and blood<br />
loss could lead to substantial hemodynamic instability. It<br />
is only with a clear understanding of these additive factors<br />
(age, fitness, anesthesia, and surgical events) that the<br />
anesthesia provider can effectively predict and manage<br />
blood pressure and cardiac function during the perioperative<br />
period.<br />
References<br />
1. Thom T, Haase N, Rosamond W, et al. Heart disease and<br />
stroke statistics—2006 update: a report from the American<br />
Heart Association Statistics Committee and Stroke Statistics<br />
Subcommittee. Circulation 2006;113:85–151.<br />
2. Seymour DG, Vaz FG. A prospective study of elderly general<br />
surgical patients: II. Post-operative complications. Age<br />
Ageing 1989;18:316–326.<br />
3. Lakatta EG. Changes in cardiovascular function with aging.<br />
Eur Heart J 1990;11:22–29.<br />
4. Bakris GL, Bank AJ, Kass DA, et al. Advanced glycation<br />
end-product cross-link breakers. A novel approach to cardiovascular<br />
pathologies related to the aging process. Am J<br />
Hypertens 2004;17:23S–30S.<br />
5. Aronson D, Rayfield EJ. How hyperglycemia promotes atherosclerosis:<br />
molecular mechanisms. Cardiovasc Diabetol<br />
2002;1:1–10.<br />
6. Yu BP, Chung HY. Oxidative stress and vascular aging. Diabetes<br />
Res Clin Pract 2001;54:S73–80.<br />
7. Kass DA, Bronzwaer JGF, Paulus WJ. What mechanisms<br />
underlie diastolic dysfunction in heart failure? Circ Res<br />
2004;94:1533–1542.<br />
8. Rooke GA. Cardiovascular aging and anesthetic implications.<br />
J Cardiothorac Vasc Anesth 2003;17:512–523.<br />
9. Turner MJ, Mier CM, Spina RJ, et al. Effects of age and<br />
gender on cardiovascular responses to phenylephrine.<br />
J Gerontol Med Sci 1999;54A:M17–24.<br />
10. Vinch CS, Aurigemma GP, Simon HU, et al. Analysis of left<br />
ventricular systolic function using midwall mechanics in<br />
patients >60 years of age with hypertensive heart disease<br />
and heart failure. Am J Cardiol 2005;96:1299–1303.<br />
11. Aronson S, Fontes ML. Hypertension: a new look at an old<br />
problem. Curr Opin Anaesthesiol 2006;19:59–64.<br />
12. Mottram PM, Haluska BA, Leano R, et al. Relation of arterial<br />
stiffness to diastolic dysfunction in hypertensive heart<br />
disease. Heart 2005;91:1551–1556.<br />
13. Rooke GA, Feigl EO. Work as a correlate of canine left<br />
ventricular oxygen consumption, and the problem of<br />
catecholamine oxygen wasting. Circ Res 1982;50:273–286.<br />
14. Bulpitt CJ, Rajkumar C, Cameron JD. Vascular compliance<br />
as a measure of biological age. J Am Geriatr Soc 1999;47:<br />
657–663.<br />
15. Kass DA. Ventricular arterial stiffening—integrating the<br />
pathophysiology. Hypertension 2005;46:185–193.<br />
16. Najjar SS, Scuteri A, Lakatta EG. Arterial aging—is it an<br />
immutable cardiovascular risk factor? Hypertension 2005;<br />
46:454–462.<br />
17. Ebert TJ, Morgan BJ, Barney JA, et al. Effects of aging on<br />
baroreflex regulation of sympathetic activity in humans. Am<br />
J Physiol 1992;263:H798–H803.<br />
18. Brodde O-E, Leineweber K. Autonomic receptor systems<br />
in the failing and aging human heart: similarities and differences.<br />
Eur J Pharmacol 2004;500:167–176.<br />
19. Leineweber K, Wangemann T, Giessler C, et al. Agedependent<br />
changes of cardiac neuronal noradrenaline reuptake<br />
transport (uptake 1 ) in the human heart. J Am Coll<br />
Cardiol 2002;40:1459–1465.<br />
20. Hees PS, Fleg JL, Mirza ZA, et al. Effects of normal aging<br />
on left ventricular lusitropic, inotropic, and chronotropic
148 T.J. Ebert and G.A. Rooke<br />
responses to dobutamine. J Am Coll Cardiol 2006;47:<br />
1440–1447.<br />
21. Alemany R, Perona JS, Sánchez-Dominguez JM, et al. G<br />
protein-coupled receptor systems and their lipid environment<br />
in health disorders during aging. Biochim Biophys<br />
Acta 2007;1768(4):964–975.<br />
22. McNamara DM, MacGowan GA, London B. Clinical importance<br />
of beta-adrenoceptor polymorphisms in cardiovascular<br />
disease. Am J Pharmacogenomics 2002;2:73–78.<br />
23. Passmore JC, Rowell PP, Joshua IG, et al. Alpha 1 adrenergic<br />
receptor control of renal blood vessels during aging.<br />
Can J Physiol Pharmacol 2005;83:335–342.<br />
24. Folkow B, Svanborg A. Physiology of cardiovascular aging.<br />
Physiol Rev 1993;73:725–764.<br />
25. Talke P, Stapelfeldt C, Lobo E, et al. Effect of α 2b -<br />
adrenoceptor polymorphism on peripheral vasoconstriction<br />
in healthy volunteers. <strong>Anesthesiology</strong> 2005;102:536–542.<br />
26. Mancia G, Mark AL. Arterial baroreflexes in humans. In:<br />
Shepherd JT, ed. <strong>The</strong> Cardiovascular System. Bethesda,<br />
MD: American Physiological Society; 1983:755–793.<br />
27. Brodde O-E, Konschak U, Becker K, et al. Cardiac muscarinic<br />
receptors decrease with age. In vitro and in vivo studies.<br />
J Clin Invest 1998;101:471–478.<br />
28. Liu HR, Zhao RR, Zhi JM, et al. Screening of serum autoantibodies<br />
to cardiac beta 1 -adrenoceptors and M 2 -muscarinic<br />
acetylcholine receptors in 408 healthy subjects of<br />
varying ages. Autoimmunity 1999;29:43–51.<br />
29. Ferrari AU. Modifications of the cardiovascular system with<br />
aging. Am J Geriatr Cardiol 2002;11:30–43.<br />
30. Long DA, Mu W, Price KL, et al. Blood vessels and the aging<br />
kidney. Nephron Exp Nephrol 2005;101:e95–99.<br />
31. Kugler JP, Hustead T. Hyponatremia and hypernatremia in<br />
the elderly. Am Fam Physician 2000;15:3623–3630.<br />
32. Podrid PJ. Atrial fibrillation in the elderly. Cardiol Clin<br />
1999;17:173–188.<br />
33. Amar D. Perioperative atrial tachyarrhythmias. <strong>Anesthesiology</strong><br />
2002;97:1618–1623.<br />
34. Gupta AK, Maheshwari A, Tresch DD, et al. Cardiac<br />
arrhythmias in the elderly. Card Electrophysiol Rev 2002;<br />
6:120–128.<br />
35. Riess ML, Stowe DF, Warltier DC. Cardiac pharmacological<br />
preconditioning with volatile anesthetics: from bench to<br />
bedside? Am J Physiol 2004;286:H1603–1607.<br />
36. Maybaum S, Ilan M, Mogilevsky J, et al. Improvement in<br />
ischemic parameters during repeated exercise testing: a possible<br />
model for myocardial preconditioning. Am J Cardiol<br />
1996;78:1087–1091.<br />
37. Abete P, Ferrara N, Cacciatore F, et al. Angina-induced protection<br />
against myocardial infarction in adult and elderly<br />
patients: a loss of preconditioning mechanism in the aging<br />
heart? J Am Coll Cardiol 1997;30:947–954.<br />
38. Longobardi G, Abete P, Ferrara N, et al. “Warm-up”<br />
phenomenon in adult and elderly patients with coronary<br />
artery disease: further evidence of the loss of “ischemic<br />
preconditioning” in the aging heart. J Gerontol 2000;55A:<br />
M124–129.<br />
39. Sniecinski R, Liu H. Reduced efficacy of volatile anesthetic<br />
preconditioning with advanced age in isolated rat myocardium.<br />
<strong>Anesthesiology</strong> 2004;100:589–597.<br />
40. Riess ML, Camara AK, Rhodes SS, et al. Increasing<br />
heart size and age attenuate anesthetic preconditioning in<br />
guinea pig isolated hearts. Anesth Analg 2005;101:1572–<br />
1576.<br />
41. Shannon RP, Wei JY, Rosa RM, et al. <strong>The</strong> effect of age and<br />
sodium depletion on cardiovascular response to orthostasis.<br />
Hypertension 1986;8:438–443.<br />
42. Ebert TJ, Harkin CP, Muzi M. Cardiovascular responses<br />
to sevoflurane: a review. Anesth Analg 1995;81:S11–<br />
S22.<br />
43. Ebert TJ, Muzi M. Propofol and autonomic reflex function<br />
in humans. Anesth Analg 1994;78:369–375.<br />
44. Burgos LG, Ebert TJ, Asiddao C, et al. Increased intraoperative<br />
cardiovascular morbidity in diabetics with autonomic<br />
neuropathy. <strong>Anesthesiology</strong> 1989;70:591–597.<br />
45. Forrest JB, Rehder K, Cahalan MK, et al. Multicenter<br />
study of general anesthesia. III. Predictors of severe<br />
perioperative adverse outcomes. <strong>Anesthesiology</strong> 1992;76:<br />
3–15.<br />
46. Carpenter RL, Caplan RA, Brown DL, et al. Incidence and<br />
risk factors for side effects of spinal anesthesia. <strong>Anesthesiology</strong><br />
1992;76:906–916.<br />
47. Filipovic M, Wang J, Michaux I, et al. Effects of halothane,<br />
sevoflurane and propofol on left ventricular diastolic<br />
function in humans during spontaneous and mechanical<br />
ventilation. Br J Anaesth 2005;94:186–192.<br />
48. Rooke GA, Freund PR, Jacobson AF. Hemodynamic<br />
response and change in organ blood volume during spinal<br />
anesthesia in elderly men with cardiac disease. Anesth<br />
Analg 1997;85:99–105.<br />
49. Levine WC, Mehta V, Landesberg G. <strong>Anesthesia</strong> for the<br />
elderly: selected topics. Curr Opin Anaesthesiol 2006;19:<br />
320–324.<br />
50. Stanton-Hicks M, Hock A, Stuhmeier K-D, et al. Venoconstrictor<br />
agents mobilize blood from different sources and<br />
increase intrathoracic filling during epidural anesthesia in<br />
supine humans. <strong>Anesthesiology</strong> 1987;66:317–322.<br />
51. Smith JS, Roizen MF, Cahalan MK, et al. Does anesthetic<br />
technique make a difference? Augmentation of systolic<br />
blood pressure during carotid endarterectomy: effects of<br />
phenylephrine versus light anesthesia and of isoflurane<br />
versus halothane on the incidence of myocardial ischemia.<br />
<strong>Anesthesiology</strong> 1988;69:846–853.<br />
52. Tiret L, Desmonts JM, Hatton F, et al. Complications associated<br />
with anaesthesia—a prospective survey in France. Can<br />
Anaesth Soc J 1986;33:336–344.<br />
53. Ebert TJ, Muzi M, Berens R, et al. Sympathetic responses<br />
to induction of anesthesia in humans with propofol or<br />
etomidate. <strong>Anesthesiology</strong> 1992;76:725–733.<br />
54. Sear JW, Higham H. Issues in the perioperative management<br />
of the elderly patient with cardiovascular disease.<br />
Drugs Aging 2002;19:429–451.<br />
55. Ebert TJ, Robinson BJ, Uhrich TD, et al. Recovery<br />
from sevoflurane anesthesia: a comparison to isoflurane<br />
and propofol anesthesia. <strong>Anesthesiology</strong> 1998;89:1524–<br />
1531.<br />
56. Mangano DT, Layug EL, Wallace A, et al. Effect of atenolol<br />
on mortality and cardiovascular morbidity after noncardiac<br />
surgery. N Engl J Med 1996;335:1713–1720.
11<br />
<strong>The</strong> Aging Respiratory System: Anesthetic<br />
Strategies to Minimize Perioperative<br />
Pulmonary Complications<br />
Rodrigo Cartin-Ceba, Juraj Sprung, Ognjen Gajic, and David O. Warner<br />
Because of increased life expectancy, the number of elderly<br />
individuals over the age of 65 is increasing all over the<br />
world, especially in developed countries. Although respiratory<br />
function is relatively well preserved in resting<br />
elderly patients, reduced respiratory reserve may lead to<br />
problems in the setting of acute illness or surgery. To anticipate<br />
and prevent potential problems that may result from<br />
reduced respiratory reserve, it is important to understand<br />
the effects of aging on respiratory function. Such changes<br />
may have particular significance during the perioperative<br />
period when numerous anesthetic and surgical factors,<br />
such as body positioning, residual effects of anesthetics on<br />
control of respiration, structural and functional disruption<br />
of respiratory muscles, and perioperative changes in lung<br />
fluid balance, may impose additional burdens on elderly<br />
patients with diminished pulmonary reserve. Indeed, postoperative<br />
respiratory complications account for approximately<br />
40% of the perioperative deaths in patients over<br />
65 years of age. 1 In this chapter, we review the effects of<br />
aging on pulmonary function and the effects of anesthesia<br />
and surgery on this function. Particular emphasis is directed<br />
to the surgical and anesthetic factors that stress the respiratory<br />
system of the elderly and how these factors increase<br />
the risk of postoperative pulmonary complications, such<br />
as respiratory failure.<br />
<strong>The</strong> Physiology of the Aging Lung<br />
Cellular Mechanisms<br />
Lung function gradually deteriorates with age even in<br />
healthy individuals who attempt to maintain aerobic<br />
capacity. 2,3 Aging is a complex process that begins at the<br />
cellular level. Normal cells undergo senescence as a result<br />
of multiple mechanisms such as telomere shortening<br />
during continuous proliferation, oxidative stress, DNA<br />
damage, and aberrant oncogene activation. 4 Normal<br />
mitochondrial respiration is associated with oxidative<br />
stress for the cell because of a continuous production of<br />
superoxide and hydrogen peroxide, inevitably resulting<br />
in minor macromolecular damage. Damaged cellular<br />
components are not completely recycled by autophagy<br />
and other cellular repair systems, leading to a progressive<br />
age-related accumulation of biologic “waste” material,<br />
including defective mitochondria, cytoplasmic protein<br />
aggregates, and an intralysosomal undegradable material<br />
called lipofuscin. 5 At the physiologic level, aging is associated<br />
with multiple changes in the respiratory system,<br />
including structural changes in both the lungs and chest<br />
wall, leading to alteration in measurable mechanical<br />
properties of the respiratory system, interference with<br />
gas exchange, and impaired response to hypoxia and<br />
hypercapnia.<br />
<strong>The</strong> respiratory system is a network of organs and<br />
tissues that exchanges gases between the individual and<br />
the environment, delivering oxygen to venous blood<br />
in exchange for carbon dioxide. 6 <strong>The</strong> lungs continue to<br />
develop throughout life with the maximal number of<br />
alveoli attained before 12 years of age. <strong>The</strong> maximal function<br />
of the respiratory system, defined as a maximal<br />
ability to exchange gas, is achieved at approximately the<br />
mid-third decade of life. 7<br />
<strong>The</strong> three most important physiologic changes associated<br />
with aging are: a decrease in strength of respiratory<br />
muscles, a decrease in the elastic recoil 8 (Figure 11-1)<br />
of the lung, and a decrease in the compliance of the<br />
chest wall. 7<br />
Age-Related Changes in Mechanics<br />
of Breathing<br />
Chest Wall and Respiratory Muscles<br />
<strong>The</strong> chest wall progressively stiffens with aging because<br />
of structural changes of the intercostal muscles, intercos-<br />
149
150 R. Cartin-Ceba et al.<br />
Lung compliance increases with aging primarily because<br />
of the loss in parenchymal elasticity (Table 11-1). 7,8 As a<br />
result, elastic recoil pressure of the lungs decreases with<br />
aging (Figure 11-1). 7,8,14 A presumed mechanism of<br />
decrease in elasticity is attributed to changes in the spatial<br />
arrangement and/or crosslinking of the elastic fiber<br />
network. 9 <strong>The</strong> changes in lung parenchyma become more<br />
pronounced after 50 years of age, resulting in a homogeneous<br />
enlargement of air spaces causing the reduction of<br />
alveolar surface area from 75 m 2 at age 30 to 60 m 2 at age<br />
70. 9 Because these changes functionally resemble emphysema,<br />
they are sometimes referred to as “senile<br />
emphysema.” 6,15<br />
Figure 11-1. Static elastic recoil decreases throughout life<br />
starting around the age of 20. TLC = total lung capacity. Shaded<br />
area represents mean ± 1 SD. (Reprinted with permission from<br />
Janssens et al. 7 ; publisher: European Respiratory Journal; and<br />
adapted with permission from Turner et al. 8 ; publisher: American<br />
Physiological Society.)<br />
tal joints, and rib-vertebral articulations, leading to a<br />
decrease in static chest wall compliance. 8,9 <strong>The</strong> increase<br />
in the rigidity of the rib cage with age is secondary to<br />
multiple factors, including changes in rib-vertebral articulations,<br />
changes in the shape of the chest (mainly because<br />
of osteoporosis that increases both dorsal kyphosis and<br />
anteroposterior chest diameter), costal cartilage calcification,<br />
and narrowing in the intervertebral disk spaces. 7,9<br />
<strong>The</strong> changes in the chest wall geometry with aging<br />
result in flattening of the diaphragm curvature (Figure<br />
11-2), 1 which has a negative effect on the maximal transdiaphragmatic<br />
pressure. 1,7 Associated reduction in muscle<br />
mass contributes to a decrease in the force produced by<br />
respiratory muscles. In a 70-year-old individual, maximal<br />
skeletal muscle electromyographic activity is reduced<br />
by approximately 50%. 10 Respiratory muscle strength<br />
may be further affected by nutritional status, which may<br />
be deficient in the elderly. 11,12 <strong>The</strong> main consequence of<br />
the reduction in the maximal transdiaphragmatic pressure<br />
is predisposition of the diaphragm to fatigue in the<br />
presence of increased ventilatory load, 13 which may lead<br />
to difficulty in weaning an elderly patient from the<br />
ventilator.<br />
Lung Parenchyma<br />
Spirometry: Static and Dynamic Tests and<br />
Underlying Physiology<br />
All lung volumes increase from birth until somatic growth<br />
stops. Total lung capacity (TLC) decreases slightly with<br />
age. However, TLC is correlated with height, and, given<br />
the fact that height diminishes with age (because of flattening<br />
of the intervertebral disks), TLC, normalized for<br />
height, remains unchanged (Figure 11-3). 7,16,17 Furthermore,<br />
the overall effect of loss of inward elastic recoil of<br />
the lung with aging is somewhat balanced by the decline<br />
in the chest wall outward force such that the TLC remains<br />
unchanged. 9 Because TLC remains unchanged, an<br />
increase in residual volume (RV) of 5%–10% per decade<br />
results in a decrease in vital capacity (VC); after age 20,<br />
VC decreases 20–30 mL per year. 18 <strong>The</strong> RV/TLC ratio<br />
increases from 25% at 20 years to 40% in a 70-year-old<br />
subject. Functional residual capacity (FRC) is determined<br />
by the balance between the inward recoil of the lungs and<br />
the outward recoil of the chest wall. FRC increases by<br />
1%–3% per decade (Figure 11-3) because at relaxed endexpiration,<br />
the rate of decrease in lung recoil with aging<br />
exceeds that of the rate of increase in chest wall<br />
stiffness. 18,19<br />
Forced expiratory volume in 1 second (FEV 1 ) and<br />
forced VC (FVC) increase up to 20 years of age in females<br />
and up to 27 years of age in males, followed by gradual<br />
decrease (up to 30 mL per year) (Figure 11-4). 9,20,21 After<br />
Figure 11-2. Aging-induced reduction of elastic recoil results<br />
in enlargement (barrel shaped) of the thorax and flattening of<br />
the diaphragm. <strong>The</strong> flatter diaphragm is less efficient in generating<br />
more muscle power which increases the work of breathing.<br />
<strong>The</strong> loss of elastic recoil results in a narrowing of small air -<br />
ways. Left panel: juvenile lung, right panel: aged lung. (Reprinted<br />
with permission from Zaugg and Lucchinetti. 1 Publisher:<br />
WB Saunders. Copyright © 2000 Elsevier.)
11. <strong>The</strong> Aging Respiratory System 151<br />
Table 11-1. Changes in respiratory function associated with aging and pathophysiologic mechanisms that explain perioperative<br />
complications.<br />
Function alteration Change Pathophysiology Potential complications<br />
Upper airway patency ↓ Hypotonia of hypopharyngeal and genioglossal Upper airway obstruction and OSA<br />
muscles, obesity (redundant tissues)<br />
Swallowing reflexes and ↓ Clearance of secretions Aspiration risk, inefficient expectoration,<br />
cough<br />
pneumonia, atelectasis, hypoxemia<br />
Chest wall compliance ↓ Structural changes of the intercostal muscles and ↑ Work of breathing; delayed<br />
joints; and rib-vertebral articulations<br />
weaning from mechanical ventilation<br />
Airway resistance ↑ ↓ Diameter of small airways Air trapping, propensity for developing<br />
intraoperative atelectasis; ↓ maximal<br />
expiratory flow (airflow limitation)<br />
during exercise<br />
Lung compliance ↑ ↓ Lung static elastic recoil pressure Air trapping, potential for dynamic<br />
hyperinflation during mechanical<br />
ventilation<br />
Closing volume ↑ Closing of small airways, sometimes within normal Intraoperative hypoxemia, especially<br />
tidal volume breathing<br />
with ↓ FRC (mean lung volume)<br />
after induction of anesthesia; airflow<br />
limitation<br />
Gas exchange ↓ ↑ Ventilation/perfusion heterogeneity and Hypoxemia<br />
Oxygenation ↓ diffusing capacity<br />
Gas exchange ↔ In CO 2 ↑ In dead space ventilation counteracted by ↓ in<br />
CO 2 production because of ↓ in basal metabolic<br />
rate<br />
Exercise capacity ↓ ↓ V˙ O 2 max because of ↓ in cardiac output Associated with higher incidence of<br />
Deconditioning<br />
postoperative pulmonary complications<br />
Regulation of breathing ↓ Dysfunction of central chemoreceptors and ↓ Ventilatory response to hypoxemia.<br />
peripheral mechanoreceptors<br />
Risk of hypercarbia and hypoxemia<br />
during use of opioids<br />
V˙ O 2 max = maximal oxygen uptake, CO 2 = carbon dioxide, OSA = obstructive sleep apnea, FRC = functional residual capacity, ↑ = increased,<br />
↓ = decreased or reduced, ↔ = no change.<br />
Figure 11-3. Evolution of lung volumes with aging. TLC = total<br />
lung volume, VC = vital capacity, IRV = inspiratory reserve<br />
volume, ERV = expiratory reserve volume, FRC = functional<br />
residual capacity, RV = residual volume. Aging produces an<br />
increase in RV with consequent reduction in ERV and VC,<br />
without changing TLC. (Reprinted with permission from<br />
Janssens et al. 7 ; publisher: European Respiratory Journal; and<br />
adapted with permission from Crapo et al. 17 ; publisher: European<br />
Respiratory Journal.)<br />
Figure 11-4. Effect of aging on FEV 1 (forced expiratory volume<br />
in 1 second) and FVC (forced vital capacity) in males and<br />
females. Both progressively decline after 20 years of age.<br />
(Reprinted with permission from Crapo 9 ; and adapted with<br />
permission from Burrows et al. 21 ; publisher: Taylor & Francis<br />
Group.)
152 R. Cartin-Ceba et al.<br />
65 years of age, this decline may be accelerated (38 mL<br />
per year). 22 Chronic smoking dramatically accelerates<br />
these age-related changes in FEV 1 and FVC. 23 In healthy,<br />
elderly subjects from 65 to 85 years of age, the normal<br />
FEV 1 /FVC ratio may be as low as 55%, compared with<br />
expected ≥70% in younger individuals. 24 Lung volume is<br />
a major determinant of airway resistance but, when<br />
adjusted for age-related change in mean lung volume,<br />
aging has no significant effect on airway resistance. 25 A<br />
decrease in small airway diameter with aging, associated<br />
with reduced mean lung volume (Figure 11-2, Table 11-1),<br />
contributes to a decrement in maximal expiratory flow<br />
with aging, 26 present even in lifetime nonsmokers. 27<br />
Airway Closure Concept (Closing Volume)<br />
<strong>The</strong> loss of elastic recoil 7,17 also affects the caliber of<br />
intrathoracic airways (Figure 11-2). 26 <strong>The</strong>se airways are<br />
normally distended by the transpulmonary pressure gradient<br />
(P tp ), i.e., the pressure gradient from inside the<br />
airway to the pleural space (Figure 11-5A). 28 In upright<br />
subjects, there is vertical gradient in pleural pressure,<br />
which results in gradient of P tp from the top (high P tp ) to<br />
the bottom (low P tp ) of the lung. This P tp gradient creates<br />
differences in the distending forces acting on small<br />
airways and causes airway diameter to be smaller in the<br />
dependent lung zones (Figure 11-5B). 28 When the patient<br />
exhales, the intrapleural pressure becomes less subatmospheric.<br />
At some point, the pressure at dependent parts<br />
of pleural space equals or exceeds atmospheric, and the<br />
airways in the dependent lung zones close (Figure 11-5B).<br />
Subsequent research has shown that this concept is an<br />
Figure 11-5. Effects of transpulmonary pressure (P tp ) on airway<br />
diameter at functional residual capacity (A) and at residual<br />
volume (B). Because of the vertical gradient of transpulmonary<br />
pressure, at residual volume the distending pressure across<br />
dependent airways becomes negative, and these dependent<br />
airways collapse. <strong>The</strong> lung volume at which this first occurs to<br />
a significant extend has been termed the “closing volume.”<br />
(Reprinted with permission from Sykes et al. 28 )<br />
oversimplification of a complicated process. Nonetheless,<br />
this concept of “closing volume” is a useful means of<br />
conceptualizing lung behavior at low volumes. Because<br />
lung static recoil decreases with age, closing volume<br />
increases with age. In younger subjects, closing volume is<br />
less than FRC, and the airways remain open during<br />
resting tidal volume breathing. <strong>The</strong> increases in FRC with<br />
aging are less than increases in closing volume, such that<br />
in erect subjects without lung disease the closing volume<br />
starts to exceed FRC around the age of 65. 27 Because<br />
FRC decreases when a subject assumes the supine position,<br />
airway closure may be present during resting tidal<br />
volume breathing, and this typically occurs around the<br />
age of 45. When airways are closed during tidal breathing,<br />
it may lead to gas-exchange abnormalities (discussed<br />
below); indeed, changes in closing volume with age are<br />
correlated with hypoxemia. 1<br />
Just as the lung volume is determined by the P tp<br />
gradient (as discussed above), the diameter of intrathoracic<br />
airways during breathing is determined in part by<br />
the transmural pressure gradient, i.e., the gradient of<br />
pressure from inside the airway to the intrapleural space. 29<br />
For the larger intrathoracic airways, the pressure outside<br />
the airways is the same as intrapleural pressure (Figure<br />
11-6A). 28 This transmural gradient is increased with<br />
increases in lung volume so that airway diameter increases<br />
with inspiration (Figure 11-6B). 28 During late nonforced<br />
expiration, the gradient of pressure between the pleural<br />
space and inside the airway is small, causing narrowing<br />
of the airway (Figure 11-6C). During forced expiration,<br />
active contraction of the expiratory muscles generates<br />
pleural pressure that is above atmospheric, and this<br />
creates a larger gradient of pressure down the airways<br />
(Figure 11-6D). <strong>The</strong> point in the small airway where intrapleural<br />
pressure equals the intra-airway pressure is called<br />
“equal pressure point.” From that point downstream, the<br />
pleural pressure exceeds the intra-airway pressure causing<br />
it to close. Compression of airways limits the effectiveness<br />
of the expiratory muscles and sets a maximal flow<br />
rate for each lung volume (“airflow limitation”). 29–31 With<br />
aging-induced loss of the lung elastic recoil pressure,<br />
“flow limitation” occurs at higher lung volumes compared<br />
with younger subjects. This expiratory airflow limitation<br />
in elderly subjects causes a significant alteration of ventilatory<br />
response to exercise compared with younger<br />
adults (Figure 11-7). 32,33 Older subjects have less ventilatory<br />
reserve to accommodate the increased ventilatory<br />
demand of exercise because of marked airflow limitation.<br />
33 During similar levels of maximal exercise (minute<br />
ventilation of 114 L/min), 45% of the tidal volume of the<br />
70-year-old subject is flow-limited because of airway<br />
compression, in comparison to less than 20% in the 30-<br />
year-old untrained adult (Figure 11-7). 32 Despite these<br />
limitations, arterial Pco 2 and Po 2 are well maintained,<br />
even during maximal exercise.
11. <strong>The</strong> Aging Respiratory System 153<br />
Figure 11-6. Factors affecting airway diameter. Schematic presentation<br />
of alveolus and intrathoracic airways. (A) At FRC:<br />
<strong>The</strong> intrapleural pressure (−5 cm H 2 O) is generated by the<br />
elastic recoil pressure of the alveoli (−5 cm H 2 O). <strong>The</strong> inside of<br />
the alveoli and airways are at atmospheric pressure (0 cm H 2 O).<br />
A transairway pressure of 5 cm H 2 O maintains airway patency.<br />
(B) Early inspiration: <strong>The</strong> gradient of pressure from alveolus<br />
(−5 cm H 2 O) to pleural space (−10 cm H 2 O) causes the alveolus<br />
to expand and draw air in through the airways. <strong>The</strong> resistance<br />
of the airways creates a gradient of pressure along the airways<br />
so that the transairway pressure gradient is greatest in the<br />
airways closer to the mouth. (C) Late expiration: <strong>The</strong> activity<br />
of the inspiratory muscles has ceased and the lung elastic recoil<br />
pressure is +6 cm H 2 O. <strong>The</strong> resultant transairway gradient of<br />
+4 cm H 2 O drives the remaining air out of the alveoli. <strong>The</strong> gradient<br />
of pressure between the pleural space and inside the airways<br />
is reversed and the airway is narrowed. (D) Forced expiration:<br />
Active contraction of the expiratory muscles generates aboveatmospheric<br />
pleural pressure. Although the pressure in the<br />
alveolus still exceeds pleural pressure because of the lung elastic<br />
recoil pressure, there is a large gradient of pressure down the<br />
airways. <strong>The</strong> pleural pressure equals the intra-airway pressure<br />
at equal pressure point (EPP). Downstream from that point the<br />
pleural pressure exceeds the intraluminal pressure in the downstream<br />
portion of the airway which thus closes. This “dynamic<br />
compression” of the airway limits determines the maximal flow<br />
achievable at a given lung volume. (Reprinted with permission<br />
from Sykes et al. 28 )<br />
<strong>The</strong> Effects of Aging on Gas Exchange<br />
Figure 11-7. Flow limitation with progressive exercise in 30-<br />
year-old untrained adults and in 70-year-old adults. At a given<br />
minute ventilation, the incidence of flow limitation during tidal<br />
breathing is greater in the elderly than in the young. (Adapted<br />
with permission from Johnson et al. 32 ; publisher: Elsevier.)<br />
<strong>The</strong> efficiency of alveolar gas exchange decreases with<br />
age. One explanation is an imbalance in the ventilation/<br />
perfusion ratio mainly caused by increase in physiologic<br />
dead space and shunting. 34,35 This imbalance leads to<br />
a gradual decrease in arterial Po 2 with aging (Figure<br />
11-8). 19,36,37 At the same time, once arterial Pco 2 reaches<br />
40 mm Hg in the newborn, it remains virtually constant<br />
for the remainder of life, and the CO 2 elimination remains<br />
unaffected despite an increase in dead space ventilation 38<br />
and reduction in CO 2 sensitivity with aging. <strong>The</strong> latter is<br />
attributable at least in part to a decline in CO 2 production<br />
associated with a decrease in basal metabolic rate. Multiple<br />
factors contribute to the decline in arterial Po 2<br />
related to age. In young, seated subjects breathing air at<br />
rest, the alveolar-arterial pressure difference for oxygen<br />
(A-aDO 2 ) is between 5 and 10 mm Hg. An increase in the<br />
A-aDO 2 with age occurs because of an increase in venti-
154 R. Cartin-Ceba et al.<br />
increases with aging, unrelated to oxyhemoglobin desaturation<br />
or increase in metabolic acidosis. 45<br />
Figure 11-8. Arterial oxygenation (Po 2 ) as a function of age<br />
from birth to 80 years. Note the decline in arterial Po 2 after the<br />
age of 20. (Reprinted with permission from Murray. 19 Copyright<br />
© 1986 Elsevier.)<br />
lation/perfusion heterogeneity, thought to be caused by a<br />
decrease in alveolar surface area and increase in closing<br />
volume. 39 Additionally, increased body mass index, as<br />
seen with obesity, that frequently accompanies aging, can<br />
contribute to the widening of A-aDO 2 . After 75 years of<br />
age, arterial oxygen tension remains relatively stable at<br />
around 83 mm Hg. 40 <strong>The</strong> diffusing capacity of the lungs<br />
decreases with aging 41 at a rate between 0.2 and 0.3 mL/<br />
min/mm Hg/year, 19 with this decline being more pronounced<br />
after the age of 40. This deterioration is attributed<br />
to an increase in ventilation/perfusion mismatching,<br />
decline in pulmonary capillary blood volume, 41 and/or the<br />
loss of the alveolar surface area. 42<br />
Regulation of Breathing<br />
In humans, ventilation is adjusted by inputs from different<br />
chemoreceptors that respond to metabolic factors<br />
and by inputs from mechanoreceptors that provide feedback<br />
from the chest wall, lungs, and airways. Minute ventilation<br />
at rest is similar in young and elderly subjects, but<br />
tidal volumes are smaller and respiratory rates are higher<br />
in the elderly. 46 <strong>The</strong> mechanism is not fully understood,<br />
but it may represent an adaptation to decreases in chest<br />
wall compliance, as well as changes in the function of<br />
central chemoreceptors and peripheral mechanoreceptors<br />
in the chest wall and lung parenchyma. 47 Compared<br />
with younger subjects, elderly individuals have approximately<br />
50% and 60% reduction in the ventilatory<br />
response to hypoxia and hypercapnia, respectively. 48<br />
Moreover, studies have shown that the average increase<br />
in ventilation in response to an alveolar pressure of<br />
oxygen of 40 mm Hg in older men is 10 L/min, in contrast<br />
to 40 L/min for younger individuals. 49 Responses to normocapnic<br />
hypoxemia during sleep can be even more<br />
depressed. For example, elderly individuals may not<br />
arouse from the REM phase of sleep until their oxyhemoglobin<br />
saturation decreases below 70%. Although<br />
in elderly subjects the ventilatory response to hypercapnia<br />
is blunted compared with younger subjects, the ventilatory<br />
response to exercise is actually increased: for a<br />
given CO 2 production during exercise, the ventilatory<br />
response increases with aging compared with younger<br />
individuals. 45 This cannot be explained by either increased<br />
anaerobiosis or oxyhemoglobin desaturation, but it seems<br />
Aging and Exercise Capacity<br />
Age is a significant factor determining maximal O 2 uptake<br />
(V˙ O 2 max). V˙ O 2 reaches a peak between 20 and 30 years<br />
of age and then decreases at a rate of 9% per decade<br />
(Figure 11-9). 19,43 <strong>The</strong> V˙ O 2 max decrease is more pronounced<br />
in sedentary elderly subjects than in the physically<br />
active. 44 In elderly individuals who maintain athletic<br />
exercise, the decline in V˙ O 2 max is slowed. Factors that<br />
limit the V˙ O 2 max in the elderly include a decrease in<br />
maximal minute ventilation, decrease in the maximum<br />
arterial-venous O 2 content difference, decrease in O 2<br />
extraction by the tissues, and reduced peripheral muscle<br />
mass. <strong>The</strong> decrease in O 2 transport capacity during senescence<br />
is also linked to an age-related decrease in cardiac<br />
output. <strong>The</strong> O 2 cost of breathing (i.e., proportion of O 2<br />
consumption by respiratory muscles) is higher than in<br />
younger subjects. Also, compared with younger individuals,<br />
the elderly are more responsive to CO 2 during exercise;<br />
for a given CO 2 production, the ventilatory response<br />
Figure 11-9. Maximal oxygen uptake (V˙ O 2 max) measured<br />
during maximal exercise as a function of age. Note the decline<br />
in V˙ O 2 max starting near 30 years of age. (Reprinted with permission<br />
from Murray. 19 Copyright © 1986 Elsevier; and adapted<br />
from Grimby and Saltin 43 by permission from Taylor & Francis<br />
Group.)
11. <strong>The</strong> Aging Respiratory System 155<br />
that increased ventilation in the elderly compensates for<br />
increased inefficiency of gas exchange, allowing for the<br />
maintenance of normocapnia during exercise. 50<br />
Other respiratory control mechanisms may be altered<br />
in the elderly because of reduced efficiency in distinguishing<br />
respiratory stimuli and/or altered integration of perception<br />
of stimuli within the central nervous system. 51–53<br />
<strong>The</strong> elderly also have a lesser ability to perceive methacholine-induced<br />
bronchoconstriction. 41 <strong>The</strong> loss of im -<br />
portant protective and adaptive mechanisms, which may<br />
result in lesser awareness of disease and delayed diagnosis<br />
of pulmonary dysfunction in the elderly, are influenced<br />
by the blunted response to hypoxia and hypercapnia<br />
and a lower ability to perceive disease states such as<br />
bronchoconstriction.<br />
Upper Airway Dysfunction<br />
Hypotonia of the hypopharyngeal and genioglossal<br />
muscles predispose elderly subjects to upper airway<br />
obstruction, and the prevalence of sleep-disordered<br />
breathing increases with age. 54 Studies have found that<br />
up to 75% of subjects over 65 years old have obstructive<br />
sleep apnea (OSA). 55,56 Indeed, the prevalence of OSA in<br />
the elderly is so high that authorities are questioning<br />
whether OSA in the elderly is a different disease from<br />
OSA in middle age. 55 Some of the consequences of<br />
chronic hypoxemia associated with OSA may include<br />
cognitive impairment, personality changes, and hypertension.<br />
56 OSA may be even more prevalent in elderly obese<br />
individuals, who may have increased postoperative risk<br />
of respiratory complications. 57<br />
<strong>The</strong> protective mechanisms of cough and swallowing<br />
are altered in elderly individuals, which may lead to ineffective<br />
clearance of secretions and increased susceptibility<br />
to aspiration. Mucociliary transport is also impaired<br />
in the elderly. Coughing is also less efficient in terms of<br />
volume, force, and flow rate. <strong>The</strong> loss of protective upperairway<br />
reflexes is presumably attributable to an agerelated<br />
alteration in peripheral signaling together with<br />
decreased central nervous system reflex activity. 58 In<br />
addition, elderly individuals have an increased prevalence<br />
of neurologic diseases that may be associated with<br />
dysphagia and an impaired cough reflex leading to the<br />
increased likelihood of pulmonary aspiration 58 and pneumonia,<br />
59 which may have a significant impact on perioperative<br />
morbidity and mortality.<br />
Perioperative Pulmonary<br />
Complications in the Elderly<br />
With increased longevity, more elderly patients are<br />
potential candidates for major surgical procedures. For<br />
example, in 1997 in the United States, the Agency for<br />
Healthcare Policy and Research reported 1,350,000 major<br />
procedures in the 65- to 84-year-old age group and 233,000<br />
procedures in the 85 and older age group. 60 Postoperative<br />
pulmonary complications, including atelectasis, pneumonia,<br />
respiratory failure, and exacerbation of underlying<br />
chronic lung disease, have a significant role in the risk for<br />
anesthesia and surgery. 61 <strong>The</strong>se complications have been<br />
reported in 5%–10% of the general patient population 62<br />
and usually prolong the hospital stay by an average of<br />
1–2 weeks. 63 Pulmonary complications in nonthoracic<br />
surgery are as prevalent as cardiovascular complications<br />
and contribute in a similar manner to morbidity, mortality,<br />
and length of stay. 64,65<br />
Numerous factors may contribute to the development<br />
of postoperative pulmonary complications in the elderly<br />
(Figure 11-10). Advanced age is a significant independent<br />
predictor of pulmonary complications even after adjustment<br />
for various comorbid conditions. 61,64,66 Age increases<br />
the risk of pulmonary complications with an odds ratio<br />
of 2.1 for patients 60–69 years old, and 3.0 for those 70–79<br />
years old compared with patients younger than 60<br />
years. 61,64,67 Older age represents the second most common<br />
identified risk factor for pulmonary complications after<br />
the presence of chronic lung disease. 61,66,68 A multifactorial<br />
risk index for predicting postoperative respiratory<br />
failure in men after major noncardiac surgery 69 showed<br />
that age above 70 conferred a 2.6-fold increase in the risk<br />
of respiratory failure compared with subjects less than 60<br />
years old.<br />
Factors contributing to an increased risk of pulmonary<br />
complications in the elderly are: (a) decreases in chest wall<br />
compliance and muscle strength (increasing the work of<br />
breathing and the risk for respiratory failure); (b) changes<br />
in lung mechanics (including increased tendency for small<br />
airway closure which may impair gas exchange and promote<br />
atelectasis); (c) increased aspiration risk secondary to swallowing<br />
dysfunction; and (d) alterations in the control of<br />
breathing, including impaired responses to hypercapnia<br />
and hypoxia and increased sensitivity to drugs used during<br />
anesthesia (especially opioids) in the elderly. 70<br />
Intraoperative alterations in chest wall function lead<br />
to atelectasis, which forms within minutes after the<br />
induction of anesthesia and is an important cause of<br />
intraoperative gas-exchange abnormalities. Chest wall<br />
dysfunction persists into the postoperative period because<br />
of pain (which limits the voluntary actions of the chest<br />
wall muscles), reflex inhibition of the respiratory muscles,<br />
and mechanical disruption of respiratory muscles (surgery<br />
in the thoracic and abdominal cavities). Consequently,<br />
after thoracic or upper abdominal surgery, FRC and VC<br />
decrease and breathing becomes rapid and shallow, all of<br />
which may contribute to the development of pulmonary<br />
complications. 71 <strong>The</strong>se effects apply to all ages but may<br />
be of special significance in the elderly patient with<br />
reduced respiratory reserve.
156 R. Cartin-Ceba et al.<br />
N<br />
U<br />
R<br />
Figure 11-10. Perioperative strategies used to minimize pulmonary complications.<br />
Older, nonanesthetized individuals have less efficient<br />
gas exchange compared with younger subjects. 36 Upon<br />
assuming the supine position, there is a decrease in FRC<br />
and hence an increase in airway resistance, which is more<br />
marked in the elderly (especially those who are obese). 36<br />
Alveolar gas exchange during anesthesia is less efficient<br />
in the elderly, and there is an inverse relationship between<br />
increased age and arterial Po 2 in spontaneously breathing<br />
anesthetized patients. 37,39 After the induction of anesthesia,<br />
atelectasis develops in dependent lung regions and<br />
may produce significant shunting. However, both the<br />
amount of atelectasis and pulmonary shunting do not<br />
increase significantly with age. 72,73 A similar phenomenon<br />
occurs in patients with chronic obstructive pulmonary<br />
disease (COPD); after the induction of anesthesia, there<br />
is less formation of atelectasis and less shunting compared<br />
with normal patients, which is explained by changes<br />
in the chest wall secondary to hyperinflation that prevents<br />
alveolar collapse. 74<br />
Decreased respiratory muscle strength, combined with<br />
diminished cough and swallowing reflexes (neurologic<br />
disorders, stroke, etc.), may diminish clearance of secretions<br />
and increase the risk of aspiration in the elderly. 75,76<br />
This risk is even higher in the presence of gastroesophageal<br />
reflux, which is also more prevalent in the elderly.<br />
Selective, rather than routine, nasogastric tube decompression<br />
after abdominal surgery may improve the return<br />
of bowel function and reduce the risk of postoperative<br />
pulmonary complications, specifically a lower rate of atelectasis<br />
and pneumonia. 77,78 Interestingly a the aspiration<br />
rate was not lower in patients with selective nasogastric<br />
decompression. 78 Finally, age-related changes in control<br />
of breathing, increased sensitivity to anesthetic agents,<br />
and diminished response to gas-exchange abnormalities<br />
predispose elderly patients to postoperative respiratory<br />
failure. Elderly patients also have a higher incidence of<br />
postoperative sleep apnea episodes. 70,79<br />
General Health Status<br />
Multiple measures of functional status and general health<br />
predict the risk of postoperative pulmonary complications.<br />
An American Society of Anesthesiologists Physical<br />
Status Classification above II, poor exercise capacity, the
11. <strong>The</strong> Aging Respiratory System 157<br />
presence of COPD, and congestive heart failure are all<br />
associated with increased risk of pulmonary complications<br />
in the elderly. 64,80,81 COPD is more prevalent in the<br />
elderly population and is the most important patientrelated<br />
risk factor for the development of postoperative<br />
pulmonary complications, producing a three- to fourfold<br />
increase in relative risk. 66,81,82 Although obesity is prevalent<br />
in elderly patients and is associated with decreased<br />
perioperative arterial oxygenation, obesity is not a significant<br />
independent predictor of risk. 64,80,83<br />
Decreased functional status, which may accompany<br />
aging, is an independent risk factor for pulmonary complications.<br />
64 Objective measurement of exercise capacity<br />
in geriatric patients demonstrated that inability to perform<br />
2-minute supine bicycle exercise and an increase in<br />
the heart rate to above 99 beats/min was the best predictor<br />
of perioperative cardiopulmonary complications in<br />
patients older than 65 years undergoing elective abdominal<br />
or noncardiac thoracic surgery. 84 Patients with better<br />
exercise tolerance by self-report, better walking distance,<br />
or better cardiovascular classification had lower rates of<br />
postoperative pulmonary complications. 85<br />
Strategies Used to Minimize Pulmonary Risk<br />
in Elderly Patients: Preoperative<br />
Considerations<br />
Preoperative Testing<br />
<strong>The</strong> value of routine preoperative pulmonary function<br />
testing is controversial. For lung resection surgery, the<br />
results of pulmonary function testing, including measurement<br />
of arterial blood gases, have proven useful in predicting<br />
pulmonary complications and postoperative<br />
function; however, spirometry does not predict postoperative<br />
pulmonary complications after abdominal<br />
surgery. 85,86 Warner et al. 87 have demonstrated that the<br />
degree of airway obstruction assessed by spirometry does<br />
not represent an independent risk factor for postoperative<br />
respiratory failure, even in smokers with severe lung<br />
disease. 87 Spirometry, chest radiograms, and arterial blood<br />
gases should be obtained as indicated from the history<br />
and physical examination as a part of this evaluation, but<br />
should not be routinely ordered. 78<br />
Preoperative <strong>The</strong>rapies<br />
To minimize postoperative pulmonary complications in<br />
elderly patients, it is important to optimize the respiratory<br />
status, beginning with a careful assessment of general<br />
physical status, with particular attention to the cardiopulmonary<br />
system. Specific therapy should be instituted preoperatively<br />
if such treatment is likely to result in improved<br />
functional status, so long as the therapeutic benefit outweighs<br />
any risk from surgical delay (Figure 11-10).<br />
Preoperative spirometry should be used only to monitor<br />
the degree of therapeutic response to treatments such as<br />
bronchodilators used to treat reactive airway disease.<br />
Patients with a reversible component of airway obstruction<br />
must be treated with bronchodilators and/or corticosteroids.<br />
Antibiotics must be given if a pulmonary<br />
infection is suspected. Preoperative smoking cessation<br />
may decrease postoperative pulmonary complications,<br />
and all patients who smoke should be given help to<br />
quit. 88,89 Past studies have been interpreted as demonstrating<br />
that quitting within a few weeks of surgery actually<br />
increases pulmonary complications by stimulating<br />
mucous production. 90 However, careful review of these<br />
studies and more recent data show that, although it may<br />
take several weeks of abstinence before pulmonary outcomes<br />
are improved, brief abstinence does not worsen<br />
outcomes. 89,90 Thus, this consideration should not prevent<br />
practitioners from promoting preoperative abstinence<br />
from smoking, even for a brief period before surgery.<br />
Strategies Used to Minimize Pulmonary Risk<br />
in Elderly Patients: Intraoperative<br />
Considerations<br />
Surgical Considerations<br />
<strong>The</strong> surgical site is the most important risk factor for the<br />
development of postoperative pulmonary complications<br />
and outweighs other patient-related risk factors. 67,69 <strong>The</strong>re<br />
is a higher likelihood of pulmonary complications with<br />
incisions closer to the diaphragm because of diaphragmatic<br />
dysfunction, splinting, and decreased ability to take<br />
deep breaths. For example, pulmonary complications<br />
caused by upper abdominal surgeries range from 13% to<br />
33% as compared with lower abdominal surgeries that<br />
range from 0% to 16%. 80 Duration of surgery also has a<br />
significant role in the development of pulmonary complications,<br />
and surgeries that last more than 3 hours have an<br />
increased risk of pulmonary complications. 91 When surgically<br />
feasible, laparoscopic techniques should be considered;<br />
however, significant respiratory dysfunction can<br />
occur even after laparoscopically performed operations, 78<br />
and whether laparoscopic procedures may reduce the<br />
risk of clinically important pulmonary complications is<br />
not clear. Nonetheless, other considerations such as<br />
reduced postoperative pain and length of stay often<br />
favor the use of laparoscopic techniques. Placement of an<br />
aortic stent instead of an open aortic aneurysm repair<br />
may be desirable in patients with significant pulmonary<br />
comorbidity.<br />
Induction of <strong>Anesthesia</strong><br />
Preoxygenation is recommended before the induction<br />
of general anesthesia. In contrast to younger patients,
158 R. Cartin-Ceba et al.<br />
performing only four deep breaths before the induction<br />
may not be sufficient in elderly patients, who may require<br />
a full 3 minutes of 100% oxygen breathing to avoid oxyhemoglobin<br />
desaturation during rapid sequence induction.<br />
92 In patients with intact oropharyngeal reflexes but<br />
significant reactive airway disease, avoidance of endotracheal<br />
intubation by using a laryngeal mask airway may<br />
be desirable.<br />
Use of Muscle Relaxants During <strong>Anesthesia</strong><br />
In elderly patients, inadequate reversal of muscle paralysis<br />
may be an important factor for postoperative complications<br />
leading to hypoventilation and hypoxemia. 86<br />
Pulmonary complications are three times higher among<br />
patients receiving a long-acting neuromuscular blocker<br />
than among those receiving shorter-acting relaxants. 93<br />
Short-acting neuromuscular blocking agents should be<br />
used in the elderly to avoid prolonged muscle paralysis,<br />
and adequacy of reversal of neuromuscular block should<br />
be tested before extubation. 78<br />
Use of <strong>Regional</strong> Anesthetic Techniques for Surgery<br />
Evidence is conflicting whether the use of regional techniques<br />
instead of general anesthesia will prevent postoperative<br />
pulmonary complications. 78 <strong>Regional</strong> anesthesia<br />
may be indicated for a variety of reasons in the elderly,<br />
but it has its own potential respiratory-related risks in<br />
these patients. Unintentional high anesthetic level during<br />
neuraxial anesthesia may be associated with paralysis of<br />
the chest wall (respiratory muscles) that may be poorly<br />
tolerated by the elderly, especially those with COPD.<br />
<strong>Regional</strong> techniques performed at the level of the neck<br />
(interscalene block, stellate ganglion block, axillary block)<br />
may be associated with paralysis of the phrenic nerve<br />
(diaphragm), and, if performed bilaterally, the patient<br />
may develop acute respiratory failure requiring urgent<br />
tracheal intubation.<br />
Intraoperative Lung Expansion During<br />
General <strong>Anesthesia</strong><br />
As discussed before, in contrast to younger patients, atelectasis<br />
may be a less important cause of intraoperative<br />
hypoxemia during general anesthesia in the elderly 72 ;<br />
however, in elderly obese patients, atelectasis may have<br />
a significant role in deterioration of intraoperative arterial<br />
oxygenation. 94 <strong>The</strong> isolated use of positive end-expiratory<br />
pressure (PEEP) does not predictably reverse<br />
atelectasis or increase arterial oxygenation. 95 Recently,<br />
there has been a considerable interest in maneuvers designated<br />
to recruit atelectatic lung regions. To reexpand<br />
the atelectatic lung, it is necessary to use a sustained lung<br />
insufflation (5–10 seconds long) with high inflation pressures<br />
(40 cm H 2 O or above). 96–98 This technique is called<br />
a “recruitment maneuver” or “vital capacity maneuver”<br />
and should be followed by sufficient PEEP to maintain<br />
the alveolar units open. 99 It is crucial to closely monitor<br />
changes in blood pressure and heart rate while performing<br />
the recruitment maneuver because significant hypotension,<br />
especially in hypovolemic patients, may ensue.<br />
Strategies Used to Minimize Pulmonary Risk<br />
in Elderly Patients: Postoperative<br />
Considerations<br />
Neuraxial Blocks for Pain Management<br />
Good postoperative pain control is necessary in all<br />
patients. <strong>The</strong>re is a longstanding debate regarding whether<br />
neuraxial techniques such as epidural analgesia reduce<br />
the frequency of pulmonary complications. It is clear that<br />
these techniques provide excellent analgesia, but their<br />
benefits regarding pulmonary outcomes are less clear. 71<br />
In one meta-analysis, 100 regional techniques reduced mortality<br />
by about a third with reductions of pulmonary<br />
embolism and pneumonia of 55% and 39%, respectively.<br />
However, many of the studies used in this and other<br />
meta-analyses have methodologic limitations. A recent<br />
unblinded, large clinical trial found few differences in<br />
outcome between those receiving and not receiving epidural<br />
analgesia, with the exceptions that: (1) respiratory<br />
failure was less frequent for some types of operations,<br />
and (2) postoperative pain control was improved by epidural<br />
analgesia. 101 A prospective, double-blind randomized<br />
trial performed by Jayr et al. 102 demonstrated that<br />
the use of epidural analgesia provided superior postoperative<br />
comfort without affecting the frequency of postoperative<br />
pulmonary complications. In addition, another<br />
blinded trial performed by Norris et al. 103 showed that in<br />
patients undergoing surgery of the abdominal aorta, thoracic<br />
epidural anesthesia combined with a light general<br />
anesthesia and followed by either intravenous or epidural<br />
patient-controlled analgesia offers no major advantage or<br />
disadvantage except for slightly shorter time to extubation.<br />
Postoperative pain management may include the<br />
use of a full range of adjunctive analgesia techniques,<br />
such as surgical field infiltration with local anesthetics,<br />
utilization of peripheral nerve blocks, nonsteroidal antiinflammatory<br />
agents, clonidine, and dexmedetomidine. 104<br />
This “multimodal approach” of using the drugs that are<br />
associated with low potential for respiratory depression<br />
may be beneficial in elderly patients prone to developing<br />
postoperative respiratory depression.<br />
Caution Regarding Perioperative Use of Opioids<br />
Elderly patients may be especially sensitive to medications<br />
because of age-related altered pharmacokinetics<br />
and pharmacodynamics of the drugs. 70,105 Aging affects
11. <strong>The</strong> Aging Respiratory System 159<br />
all pharmacokinetic processes, but the most important<br />
change is the reduction in the renal drug elimination. At<br />
the same time, pharmacodynamic changes also occur<br />
at the receptor or signal-transduction level or at the level<br />
of the homeostatic mechanisms. 105 This situation explains<br />
why the dosing of all anesthetic drugs should reflect the<br />
differences in pharmacokinetics and pharmacodynamics<br />
that accompany aging. Opioids are of particular concern<br />
in the elderly. Opioids reduce the respiratory response to<br />
chemical (hypoxemia, hypercapnia) load resulting in<br />
hypoventilation and hypoxemia. Given the fact that<br />
elderly patients may be particularly sensitive to opioids,<br />
they should be titrated carefully in order to avoid postoperative<br />
respiratory depression. 70<br />
Postoperative Respiratory Assistance to Maintain<br />
Lung Expansion<br />
Decreased lung volumes and atelectasis attributable to<br />
surgery-related shallow breathing, bed rest, diaphragmatic<br />
dysfunction, pain, and impaired mucociliary clearance<br />
may be the first events in a cascade leading to<br />
postoperative pulmonary complications. 78 Postoperative<br />
use of lung expansion therapy such as incentive spirometry,<br />
chest physical therapy, effective cough, postural<br />
drainage, percussion-vibration, ambulation, continuous<br />
positive airway pressure (CPAP), and intermittent positive-pressure<br />
breathing is the mainstay of postoperative<br />
prevention of pulmonary complications in the elderly.<br />
Preoperative education in these maneuvers may reduce<br />
pulmonary complications more efficiently than when<br />
instruction is given after surgery. 106,107 Lung expansion<br />
maneuvers, when performed appropriately, lower the risk<br />
of atelectasis by 50%. 108 No modality seems superior, and<br />
combined modalities do not seem to provide additional<br />
risk reduction. 78 Incentive spirometry may be the least<br />
labor-intensive, whereas CPAP may be particularly beneficial<br />
for patients who cannot participate in incentive<br />
spirometry or deep-breathing exercises. 78 However, a<br />
most recent systematic review of randomized trials<br />
suggested that routine respiratory physiotherapy may not<br />
seem to be justified as a strategy for reducing postoperative<br />
pulmonary complications after abdominal surgery. 109<br />
All patients with diagnosed OSA should have their status<br />
evaluated preoperatively, and, if they are CPAP-dependent,<br />
they should receive the CPAP treatment immediately<br />
after tracheal extubation. In addition, they may<br />
need close postoperative monitoring (i.e., oxygenation<br />
and ventilation). Depending on the severity of OSA, type<br />
of surgery, and anesthesia, they may require admission to<br />
a monitored bed overnight.<br />
Noninvasive Positive Pressure Ventilation<br />
Noninvasive positive pressure ventilation (NPPV) is the<br />
delivery of mechanically assisted breaths without placement<br />
of an artificial airway, such as an endotracheal or a<br />
tracheostomy tube. Bilevel positive airway pressure<br />
(BiPAP) is noninvasive ventilatory modality that seems<br />
to be more efficient than CPAP in supporting breathing.<br />
With BiPAP, continuous inspiratory positive airway pressure<br />
provides inspiratory assistance and expiratory positive<br />
airway pressure prevents alveolar closure. 104<br />
NPPV may be used in patients with COPD exacerbations,<br />
cardiogenic pulmonary edema, hypercapnic re -<br />
spiratory failure caused by neuromuscular disease,<br />
obesity-hypoventilation syndrome, and immunocompromised<br />
patients with respiratory failure. <strong>The</strong> role of nasal<br />
intermittent positive pressure ventilation (NIPPV) in<br />
hypoxemic respiratory failure attributable to other causes<br />
is still controversial and lacks adequate evidence support.<br />
<strong>The</strong> idea of utilizing NIPPV to manage patients with<br />
postextubation respiratory failure came from several<br />
trials demonstrating efficacy of NIPPV in postoperative<br />
respiratory failure, particularly when cardiogenic pulmonary<br />
edema was the etiology. 110–114 Immediately after<br />
extubation, elderly patients may need additional ventilatory<br />
support to maintain ventilation and oxygenation.<br />
CPAP has been successfully used to avoid tracheal reintubation<br />
in patients who developed hypoxemia after elective<br />
major abdominal surgery, and the use of CPAP was<br />
associated with lower incidence of other severe postoperative<br />
complications. 115 Outcomes of patients with postoperative<br />
postextubation hypoxemia treated by CPAP 115<br />
may differ from that in the general intensive care population<br />
116 or in patients with acute exacerbation of COPD. 117,118<br />
Thus, Esteban et al. 116 demonstrated that NPPV does not<br />
prevent the need for reintubation and may be harmful in<br />
intensive care unit patients who develop respiratory<br />
failure after tracheal extubation. In contrast, in patients<br />
with acute exacerbation of COPD, comparing noninvasive<br />
ventilation with a standard intensive care unit<br />
approach in which endotracheal intubation was performed<br />
after failure of medical treatment, the use of noninvasive<br />
ventilation reduced complications, length of stay<br />
in the intensive care unit, and mortality. 117 <strong>The</strong> application<br />
of NIPPV has also been used successfully in the postoperative<br />
period with morbid obesity patients who were<br />
undergoing bariatric surgery. 119,120 Prophylactic BiPAP<br />
used during the first 12–24 hours after bariatric surgery<br />
resulted in significantly higher measures of pulmonary<br />
function, but did not translate into fewer hospital days or<br />
a lower complication rate. 119<br />
Mechanical Ventilation in the Elderly<br />
An aging population is projected to substantially increase<br />
the demand for intensive care unit services during the<br />
next 25 years. 121,122 An increasing number of elderly<br />
patients will also require intensive care treatment<br />
after surgery. <strong>The</strong> risk of respiratory failure requiring
160 R. Cartin-Ceba et al.<br />
mechanical ventilation in response to a variety of physiologic<br />
insults, including surgery, is increased in the elderly<br />
because of underlying pulmonary disease, loss of muscle<br />
mass, and other comorbid conditions. 123 In patients that<br />
develop adult respiratory distress syndrome, older age is<br />
clearly associated with higher mortality rates. 124,125 Ely<br />
et al. 126 prospectively studied whether age represents an<br />
independent effect on the outcomes in a cohort of patients<br />
requiring mechanical ventilation after admission to an<br />
intensive care unit. After adjustment for severity of illness,<br />
elderly patients, compared with younger patients, required<br />
a comparable length of mechanical ventilation. <strong>The</strong>se<br />
effects could not be attributed to the differences in mortality;<br />
therefore, mechanical ventilation should not be<br />
withheld from elderly patients with respiratory failure on<br />
the basis of chronologic age. 126<br />
Patients aged 65 years or older account for 47% of<br />
intensive care unit admissions. 127 With aging, there are<br />
several factors known to affect weaning, such as decrease<br />
in lung elasticity, reduction in FVC, decreased respiratory<br />
muscle strength, and decreased chest wall compliance. 128<br />
Kleinhenz and Lewis 129 reviewed the challenges of<br />
caring for elderly patients with chronic ventilator dependency.<br />
Long-term ventilator dependence, defined as need<br />
for mechanical ventilation for 6 hours per day for more<br />
than 21 days, is disproportionately higher in patients over<br />
70 years of age. 129 Long-term ventilator dependence complicates<br />
9% to 20% of the episodes of mechanical ventilation<br />
treated in the intensive care units of acute care<br />
hospitals, and it is associated with an average mortality<br />
rate of 40%. 129 This is an important socioeconomic issue,<br />
and more research is needed regarding the causes that<br />
may lead to respiratory failure in elderly patients. <strong>The</strong>re<br />
is an ongoing investigation of the effects of “protective<br />
ventilatory strategies” (lower tidal volume, higher PEEP,<br />
recruitment lung strategies, as well as effects of intraoperatively<br />
administered fluids and blood products) on<br />
postoperative pulmonary outcomes. Literature evidence<br />
is slowly accumulating showing that the use of “protective<br />
ventilatory strategies” in high-risk patients may be<br />
beneficial in preventing postoperative ventilatory<br />
failure 130–133 ; however, more studies are necessary before<br />
making definitive recommendations. Some specific areas<br />
that require further investigation are the relationship<br />
between the influence of age on weaning and the relationship<br />
between age and the work of breathing.<br />
Conclusion<br />
Aging causes significant changes in respiratory function,<br />
which leads to ventilation perfusion mismatching and<br />
diminished efficiency of gas exchange. <strong>The</strong> perioperative<br />
period represents a time of increased functional demand<br />
on the respiratory system, and elderly patients with<br />
reduced respiratory function may be prone to developing<br />
pulmonary complications. <strong>The</strong>se complications are a significant<br />
source of morbidity, mortality, and prolonged<br />
hospitalization. <strong>The</strong>se pulmonary complications may be<br />
attributed to diminished protective reflexes, increased<br />
sensitivity to respiratory depressants, and altered<br />
responses to hypoxemia and hypercapnia. After identifying<br />
patients at risk for postoperative pulmonary complications,<br />
anesthesiologists must consider strategies to try<br />
to reduce the risk throughout the perioperative period.<br />
Besides optimization of underlying comorbid conditions,<br />
anesthesiologists and other perioperative physicians may<br />
utilize strategies that facilitate lung expansion such as<br />
deep-breathing exercises, incentive spirometry, and adequate<br />
postoperative pain control. Select patients may<br />
benefit from postoperative application of NPPV.<br />
References<br />
1. Zaugg M, Lucchinetti E. Respiratory function in the<br />
elderly. Anesthesiol Clin North Am 2000;18(1):47–58, vi.<br />
2. Pollock ML, Mengelkoch LJ, Graves JE, et al. Twenty-year<br />
follow-up of aerobic power and body composition of older<br />
track athletes. J Appl Physiol 1997;82(5):1508–1516.<br />
3. McClaran SR, Babcock MA, Pegelow DF, Reddan WG,<br />
Dempsey JA. Longitudinal effects of aging on lung function<br />
at rest and exercise in healthy active fit elderly adults.<br />
J Appl Physiol 1995;78(5):1957–1968.<br />
4. Kiyokawa H. Senescence and cell cycle control. Results<br />
Probl Cell Differ 2006;42:257–270.<br />
5. Terman A, Gustafsson B, Brunk UT. Mitochondrial damage<br />
and intralysosomal degradation in cellular aging. Mol<br />
Aspects Med 2006;27(5–6):471–482.<br />
6. Campbell EJ, Lefrak SS. How aging affects the structure<br />
and function of the respiratory system. <strong>Geriatric</strong>s 1978;<br />
33(6):68–74.<br />
7. Janssens JP, Pache JC, Nicod LP. Physiological changes in<br />
respiratory function associated with ageing. Eur Respir J<br />
1999;13(1):197–205.<br />
8. Turner JM, Mead J, Wohl ME. Elasticity of human lungs in<br />
relation to age. J Appl Physiol 1968;25(6):664–671.<br />
9. Crapo RO. <strong>The</strong> aging lung. In: Mahler DA, ed. Pulmonary<br />
Disease in the Elderly Patient. New York: Marcel Dekker;<br />
1993:1–21.<br />
10. Larsson L. Histochemical characteristics of human skeletal<br />
muscle during aging. Acta Physiol Scand 1983;117(3):469–<br />
471.<br />
11. Enright P, Kronmal R, Manolio T, Schenker M, Hyatt R.<br />
Respiratory muscle strength in the elderly. Correlates and<br />
reference values. Cardiovascular Health Study Research<br />
Group. Am J Respir Crit Care Med 1994;149(2):430–438.<br />
12. Arora NS, Rochester DF. Respiratory muscle strength and<br />
maximal voluntary ventilation in undernourished patients.<br />
Am Rev Respir Dis 1982;126(1):5–8.<br />
13. Tolep K, Higgins N, Muza S, Criner G, Kelsen SG. Comparison<br />
of diaphragm strength between healthy adult<br />
elderly and young men. Am J Respir Crit Care Med 1995;<br />
152(2):677–682.
11. <strong>The</strong> Aging Respiratory System 161<br />
14. Niewohner D, Kleinerman J, Liotta L. Elastic behaviour of<br />
post-mortem human lungs: effects of aging and mild<br />
emphysema. J Appl Physiol 1975;25:664–671.<br />
15. Verbeken E, Cauberghs M, Mertens I, Clement J, Lauweryns<br />
J, Van de Woestijne K. <strong>The</strong> senile lung. Comparison<br />
with normal and emphysematous lungs. 2. Functional<br />
aspects. Chest 1992;101(3):800–809.<br />
16. Levitzky MG. Effects of aging on the respiratory system.<br />
Physiologist 1984;27(2):102–107.<br />
17. Crapo RO, Morris AH, Clayton PD, Nixon CR. Lung<br />
volumes in healthy nonsmoking adults. Bull Eur Physiopathol<br />
Respir 1982;18(3):419–425.<br />
18. Knudson RJ, Clark DF, Kennedy TC, Knudson DE. Effect<br />
of aging alone on mechanical properties of the normal<br />
adult human lung. J Appl Physiol 1977;43(6):1054–1062.<br />
19. Murray JF. Aging. In: Murray JF, ed. <strong>The</strong> Normal Lung.<br />
Philadelphia: WB Saunders; 1986:339–360.<br />
20. Knudson RJ, Slatin RC, Lebowitz MD, Burrows B. <strong>The</strong><br />
maximal expiratory flow-volume curve. Normal standards,<br />
variability, and effects of age. Am Rev Respir Dis 1976;<br />
113(5):587–600.<br />
21. Burrows B, Cline MG, Knudson RJ, Taussig LM, Lebowitz<br />
MD. A descriptive analysis of the growth and decline of<br />
the FVC and FEV1. Chest 1983;83(5):717–724.<br />
22. Brandstetter RD, Kazemi H. Aging and the respiratory<br />
system. Med Clin North Am 1983;67(2):419–431.<br />
23. Griffith KA, Sherrill DL, Siegel EM, Manolio TA, Bonekat<br />
HW, Enright PL. Predictors of loss of lung function in the<br />
elderly: the Cardiovascular Health Study. Am J Respir Crit<br />
Care Med 2001;163(1):61–68.<br />
24. Enright PL, Kronmal RA, Higgins M, Schenker M,<br />
Haponik EF. Spirometry reference values for women and<br />
men 65 to 85 years of age. Cardiovascular health study.<br />
Am Rev Respir Dis 1993;147(1):125–133.<br />
25. Anthonisen N. Tests of mechanical function. In: Handbook<br />
of Physiology. Bethesda, MD: American Physiology<br />
Society; 1986:753–784.<br />
26. Niewohner D, Kleinerman J. Morphologic basis of pulmonary<br />
resistance in human lung and effects of aging. J Appl<br />
Physiol 1974;36:412–418.<br />
27. Fowler RW, Pluck RA, Hetzel MR. Maximal expiratory<br />
flow-volume curves in Londoners aged 60 years and over.<br />
Thorax 1987;42(3):173–182.<br />
28. Sykes MK, McNicol MW, Campbell EJM. <strong>The</strong> mechanics<br />
of respiration. In: Sykes MK, McNicol MW, Campbell<br />
EJM, eds. Respiratory Failure. London: Blackwell Scientific<br />
Publications; 1976:3–30.<br />
29. Hyatt RE, Flath RE. Influence of lung parenchyma on<br />
pressure-diameter behavior of dog bronchi. J Appl Physiol<br />
1966;21(5):1448–1452.<br />
30. Hyatt RE. Expiratory flow limitation. J Appl Physiol 1983;<br />
55(1 Pt 1):1–7.<br />
31. Babb TG, Rodarte JR. Mechanism of reduced maximal expiratory<br />
flow with aging. J Appl Physiol 2000;89(2):505–511.<br />
32. Johnson BD, Badr MS, Dempsey JA. Impact of the aging<br />
pulmonary system on the response to exercise. Clin Chest<br />
Med 1994;15(2):229–246.<br />
33. DeLorey DS, Babb TG. Progressive mechanical ventilatory<br />
constraints with aging. Am J Respir Crit Care Med<br />
1999;160(1):169–177.<br />
34. Wagner PD, Laravuso RB, Uhl RR, West JB. Continuous<br />
distributions of ventilation-perfusion ratios in normal subjects<br />
breathing air and 100 per cent O 2 . J Clin Invest 1974;<br />
54(1):54–68.<br />
35. Wagner PD, Saltzman HA, West JB. Measurement of continuous<br />
distributions of ventilation-perfusion ratios: theory.<br />
J Appl Physiol 1974;36(5):588–599.<br />
36. Craig DB, Wahba WM, Don HF, Couture JG, Becklake<br />
MR. “Closing volume” and its relationship to gas exchange<br />
in seated and supine positions. J Appl Physiol 1971;31(5):<br />
717–721.<br />
37. Sorbini CA, Grassi V, Solinas E, Muiesan G. Arterial<br />
oxygen tension in relation to age in healthy subjects. Respiration<br />
1968;25(1):3–13.<br />
38. Raine JM, Bishop JM. A-a difference in O 2 tension and<br />
physiological dead space in normal man. J Appl Physiol<br />
1963;18:284–288.<br />
39. Wahba WM. Influence of aging on lung function—clinical<br />
significance of changes from age twenty. Anesth Analg 1983;<br />
62(8):764–776.<br />
40. Cerveri I, Zoia MC, Fanfulla F, et al. Reference values of<br />
arterial oxygen tension in the middle-aged and elderly. Am<br />
J Respir Crit Care Med 1995;152(3):934–941.<br />
41. Guenard H, Marthan R. Pulmonary gas exchange in elderly<br />
subjects. Eur Respir J 1996;9(12):2573–2577.<br />
42. Thurlbeck WM, Angus GE. Growth and aging of the<br />
normal human lung. Chest 1975;67(2 Suppl):3S–6S.<br />
43. Grimby G, Saltin B. Physiological effects of physical training.<br />
Scand J Rehabil Med 1971;3(1):6–14.<br />
44. Mahler DA, Cunningham LN, Curfman GD. Aging and<br />
exercise performance. Clin Geriatr Med 1986;2(2):433–<br />
452.<br />
45. Poulin MJ, Cunningham DA, Paterson DH, Rechnitzer PA,<br />
Ecclestone NA, Koval JJ. Ventilatory response to exercise<br />
in men and women 55 to 86 years of age. Am J Respir Crit<br />
Care Med 1994;149(2 Pt 1):408–415.<br />
46. Krumpe PE, Knudson RJ, Parsons G, Reiser K. <strong>The</strong><br />
aging respiratory system. Clin Geriatr Med 1985;1(1):143–<br />
175.<br />
47. Mahler DA, Rosiello RA, Loke J. <strong>The</strong> aging lung. Part 1.<br />
Loss of elasticity. Clin Geriatr Med 1986;2(2):215–225.<br />
48. Peterson DD, Pack AI, Silage DA, Fishman AP. Effects of<br />
aging on ventilatory and occlusion pressure responses<br />
to hypoxia and hypercapnia. Am Rev Respir Dis 1981;<br />
124(4):387–391.<br />
49. Kronenberg RS, Drage CW. Attenuation of the ventilatory<br />
and heart rate responses to hypoxia and hypercapnia with<br />
aging in normal men. J Clin Invest 1973;52(8):1812–1819.<br />
50. Brischetto MJ, Millman RP, Peterson DD, Silage DA, Pack<br />
AI. Effect of aging on ventilatory response to exercise and<br />
CO 2 . J Appl Physiol 1984;56(5):1143–1150.<br />
51. Tack M, Altose MD, Cherniack NS. Effect of aging on<br />
respiratory sensations produced by elastic loads. J Appl<br />
Physiol 1981;50(4):844–850.<br />
52. Tack M, Altose MD, Cherniack NS. Effect of aging on the<br />
perception of resistive ventilatory loads. Am Rev Respir<br />
Dis 1982;126(3):463–467.<br />
53. Manning H, Mahler D, Harver A. Dyspnea in the elderly.<br />
In: Mahler D, ed. Pulmonary Disease in the Elderly Patient.<br />
New York: Marcel Dekker; 1993:81–111.
162 R. Cartin-Ceba et al.<br />
54. Hoch CC, Reynolds CF 3rd, Monk TH, et al. Comparison<br />
of sleep-disordered breathing among healthy elderly in the<br />
seventh, eighth, and ninth decades of life. Sleep 1990;13(6):<br />
502–511.<br />
55. Epstein CD, El-Mokadem N, Peerless JR. Weaning older<br />
patients from long-term mechanical ventilation: a pilot<br />
study. Am J Crit Care 2002;11(4):369–377.<br />
56. Ancoli-Israel S, Coy T. Are breathing disturbances in<br />
elderly equivalent to sleep apnea syndrome? Sleep 1994;<br />
17(1):77–83.<br />
57. Krieger J, Sforza E, Boudewijns A, Zamagni M, Petiau C.<br />
Respiratory effort during obstructive sleep apnea: role<br />
of age and sleep state [see comment]. Chest 1997;112(4):<br />
875–884.<br />
58. Marik PE, Kaplan D. Aspiration pneumonia and dysphagia<br />
in the elderly. Chest 2003;124(1):328–336.<br />
59. Rosenthal RA, Kavic SM. Assessment and management of<br />
the geriatric patient. Crit Care Med 2004;32(4 Suppl):<br />
S92–105.<br />
60. McCormick KA, Cummings MA, Kovner C. <strong>The</strong> role of<br />
the Agency for Health Care Policy and Research (AHCPR)<br />
in improving outcomes of care. Nurs Clin North Am<br />
1997;32(3):521–542.<br />
61. Qaseem A, Snow V, Fitterman N, et al. Risk assessment for<br />
and strategies to reduce perioperative pulmonary complications<br />
for patients undergoing noncardiothoracic surgery:<br />
a guideline from the American College of Physicians. Ann<br />
Intern Med 2006;144(8):575–580.<br />
62. Wightman JA. A prospective survey of the incidence of<br />
postoperative pulmonary complications. Br J Surg 1968;<br />
55(2):85–91.<br />
63. Lawrence VA, Dhanda R, Hilsenbeck SG, Page CP. Risk<br />
of pulmonary complications after elective abdominal<br />
surgery. Chest 1996;110(3):744–750.<br />
64. Smetana GW, Lawrence VA, Cornell JE. Preoperative pulmonary<br />
risk stratification for noncardiothoracic surgery:<br />
systematic review for the American College of Physicians.<br />
Ann Intern Med 2006;144(8):581–595.<br />
65. Lawrence VA, Hilsenbeck SG, Noveck H, Poses RM,<br />
Carson JL. Medical complications and outcomes after<br />
hip fracture repair. Arch Intern Med 2002;162(18):2053–<br />
2057.<br />
66. Pedersen T, Eliasen K, Henriksen E. A prospective study<br />
of risk factors and cardiopulmonary complications associated<br />
with anaesthesia and surgery: risk indicators of cardiopulmonary<br />
morbidity. Acta Anaesthesiol Scand 1990;<br />
34(2):144–155.<br />
67. Smetana GW. Preoperative pulmonary assessment of the<br />
older adult. Clin Geriatr Med 2003;19(1):35–55.<br />
68. McAlister FA, Khan NA, Straus SE, et al. Accuracy of the<br />
preoperative assessment in predicting pulmonary risk<br />
after nonthoracic surgery. Am J Respir Crit Care Med<br />
2003;167(5):741–744.<br />
69. Arozullah AM, Daley J, Henderson WG, Khuri SF.<br />
Multifactorial risk index for predicting postoperative<br />
respiratory failure in men after major noncardiac surgery.<br />
<strong>The</strong> National Veterans Administration Surgical Quality<br />
Improvement Program. Ann Surg 2000;232(2):242–253.<br />
70. Freye E, Levy JV. Use of opioids in the elderly—pharmacokinetic<br />
and pharmacodynamic considerations [German].<br />
Anasthesiol Intensivmed Notfallmed Schmerzther 2004;<br />
39(9):527–537.<br />
71. Warner DO. Preventing postoperative pulmonary complications:<br />
the role of the anesthesiologist. <strong>Anesthesiology</strong><br />
2000;92(5):1467–1472.<br />
72. Gunnarsson L, Tokics L, Gustavsson H, Hedenstierna G.<br />
Influence of age on atelectasis formation and gas exchange<br />
impairment during general anaesthesia. Br J Anaesth<br />
1991;66(4):423–432.<br />
73. Holland J, Milic-Emili J, Macklem PT, Bates DV. <strong>Regional</strong><br />
distribution of pulmonary ventilation and perfusion in<br />
elderly subjects. J Clin Invest 1968;47:81–92.<br />
74. Gunnarsson L, Tokics L, Lundquist H, et al. Chronic<br />
obstructive pulmonary disease and anaesthesia: formation<br />
of atelectasis and gas exchange impairment. Eur Respir J<br />
1991;4(9):1106–1116.<br />
75. Sekizawa K, Ujiie Y, Itabashi S, Sasaki H, Takishima T.<br />
Lack of cough reflex in aspiration pneumonia. Lancet<br />
1990;335(8699):1228–1229.<br />
76. Smithard DG, O’Neill PA, Parks C, Morris J. Complications<br />
and outcome after acute stroke. Does dysphagia<br />
matter? Stroke 1996;27(7):1200–1204.<br />
77. Nelson R, Tse B, Edwards S. Systematic review of prophylactic<br />
nasogastric decompression after abdominal operations.<br />
Br J Surg 2005;92(6):673–680.<br />
78. Lawrence VA, Cornell JE, Smetana GW. Strategies to<br />
reduce postoperative pulmonary complications after noncardiothoracic<br />
surgery: systematic review for the American<br />
College of Physicians. Ann Intern Med 2006;144(8):<br />
596–608.<br />
79. Trayner E Jr, Celli BR. Postoperative pulmonary<br />
complications. Med Clin North Am 2001;85(5):1129–<br />
1139.<br />
80. Smetana GW. Preoperative pulmonary evaluation [see<br />
comment]. N Engl J Med 1999;340(12):937–944.<br />
81. Wong DH, Weber EC, Schell MJ, Wong AB, Anderson CT,<br />
Barker SJ. Factors associated with postoperative pulmonary<br />
complications in patients with severe chronic ob -<br />
structive pulmonary disease. Anesth Analg 1995;80(2):<br />
276–284.<br />
82. Tarhan S, Moffitt EA, Sessler AD, Douglas WW, Taylor WF.<br />
Risk of anesthesia and surgery in patients with chronic<br />
bronchitis and chronic obstructive pulmonary disease.<br />
Surgery 1973;74(5):720–726.<br />
83. Moulton MJ, Creswell LL, Mackey ME, Cox JL, Rosenbloom<br />
M. Obesity is not a risk factor for significant adverse<br />
outcomes after cardiac surgery. Circulation 1996;94<br />
(9 Suppl):II87–92.<br />
84. Gerson MC, Hurst JM, Hertzberg VS, Baughman R, Rouan<br />
GW, Ellis K. Prediction of cardiac and pulmonary complications<br />
related to elective abdominal and noncardiac<br />
thoracic surgery in geriatric patients. Am J Med 1990;88(2):<br />
101–107.<br />
85. Williams-Russo P, Charlson ME, MacKenzie CR, Gold JP,<br />
Shires GT. Predicting postoperative pulmonary complications.<br />
Is it a real problem? Arch Intern Med 1992;152(6):<br />
1209–1213.<br />
86. Beard K, Jick H, Walker AM. Adverse respiratory events<br />
occurring in the recovery room after general anesthesia.<br />
<strong>Anesthesiology</strong> 1986;64(2):269–272.
11. <strong>The</strong> Aging Respiratory System 163<br />
87. Warner DO, Warner MA, Offord KP, Schroeder DR,<br />
Maxson P, Scanlon PD. Airway obstruction and perioperative<br />
complications in smokers undergoing abdominal<br />
surgery. <strong>Anesthesiology</strong> 1999;90(2):372–379.<br />
88. Warner DO. Helping surgical patients quit smoking: why,<br />
when, and how. Anesth Analg 2005;101(2):481–487.<br />
89. Warner DO. Perioperative abstinence from cigarettes:<br />
physiologic and clinical consequences. <strong>Anesthesiology</strong><br />
2006;104(2):356–367.<br />
90. Moller AM, Villebro N, Pedersen T, Tonnesen H. Effect<br />
of preoperative smoking intervention on postoperative<br />
complications: a randomised clinical trial. Lancet 2002;<br />
359(9301):114–117.<br />
91. Garibaldi RA, Britt MR, Coleman ML, Reading JC, Pace<br />
NL. Risk factors for postoperative pneumonia. Am J Med<br />
1981;70(3):677–680.<br />
92. Valentine SJ, Marjot R, Monk CR. Preoxygenation in<br />
the elderly: a comparison of the four-maximal-breath<br />
and three-minute techniques. Anesth Analg 1990;71(5):<br />
516–519.<br />
93. Berg H, Roed J, Viby-Mogensen J, et al. Residual neuromuscular<br />
block is a risk factor for postoperative pulmonary<br />
complications. A prospective, randomised, and blinded<br />
study of postoperative pulmonary complications after<br />
atracurium, vecuronium and pancuronium. Acta Anaesthesiol<br />
Scand 1997;41(9):1095–1103.<br />
94. Eichenberger A, Proietti S, Wicky S, et al. Morbid obesity<br />
and postoperative pulmonary atelectasis: an underestimated<br />
problem. Anesth Analg 2002;95(6):1788–1792.<br />
95. Bindslev L, Hedenstierna G, Santesson J, Norlander O,<br />
Gram I. Airway closure during anaesthesia, and its prevention<br />
by positive end expiratory pressure. Acta Anaesthesiol<br />
Scand 1980;24(3):199–205.<br />
96. Rothen HU, Sporre B, Engberg G, Wegenius G, Hedenstierna<br />
G. Reexpansion of atelectasis during general anaesthesia<br />
may have a prolonged effect. Acta Anaesthesiol<br />
Scand 1995;39(1):118–125.<br />
97. Rothen HU, Sporre B, Engberg G, Wegenius G, Hedenstierna<br />
G. Re-expansion of atelectasis during general anaesthesia:<br />
a computed tomography study. Br J Anaesth 1993;<br />
71(6):788–795.<br />
98. Whalen FX, Gajic O, Thompson GB, et al. <strong>The</strong> effects of<br />
the alveolar recruitment maneuver and positive end-expiratory<br />
pressure on arterial oxygenation during laparoscopic<br />
bariatric surgery. Anesth Analg 2006;102(1):298–305.<br />
99. Lachmann B. Open up the lung and keep the lung open.<br />
Intensive Care Med 1992;18(6):319–321.<br />
100. Rodgers A, Walker N, Schug S, et al. Reduction of postoperative<br />
mortality and morbidity with epidural or spinal<br />
anaesthesia: results from overview of randomised trials.<br />
BMJ 2000;321(7275):1493.<br />
101. Myles PS, Power I, Jamrozik K. Epidural block and outcome<br />
after major surgery. Med J Aust 2002;177(10):536–537.<br />
102. Jayr C, Thomas H, Rey A, Farhat F, Lasser P, Bourgain JL.<br />
Postoperative pulmonary complications. Epidural analgesia<br />
using bupivacaine and opioids versus parenteral opioids.<br />
<strong>Anesthesiology</strong> 1993;78(4):666–676; discussion 22A.<br />
103. Norris EJ, Beattie C, Perler BA, et al. Double-masked<br />
randomized trial comparing alternate combinations of<br />
intraoperative anesthesia and postoperative analgesia<br />
in abdominal aortic surgery. <strong>Anesthesiology</strong> 2001;95(5):<br />
1054–1067.<br />
104. Sprung J, Gajic O, Warner DO. Review article: age related<br />
alterations in respiratory function—anesthetic considerations<br />
[Article de synthese : Les modifications de fonction<br />
respiratoire liees a l’age—considerations anesthesiques].<br />
Can J Anaesth 2006;53(12):1244–1257.<br />
105. Turnheim K. When drug therapy gets old: pharmacokinetics<br />
and pharmacodynamics in the elderly. Exp Gerontol<br />
2003;38(8):843–853.<br />
106. Celli BR, Rodriguez KS, Snider GL. A controlled trial of<br />
intermittent positive pressure breathing, incentive spirometry,<br />
and deep breathing exercises in preventing pulmonary<br />
complications after abdominal surgery. Am Rev<br />
Respir Dis 1984;130(1):12–15.<br />
107. Castillo R, Haas A. Chest physical therapy: comparative<br />
efficacy of preoperative and postoperative in the elderly.<br />
Arch Phys Med Rehabil 1985;66(6):376–379.<br />
108. Brooks-Brunn JA. Postoperative atelectasis and pneumonia.<br />
Heart Lung 1995;24(2):94–115.<br />
109. Pasquina P, Tramer MR, Granier JM, Walder B. Respiratory<br />
physiotherapy to prevent pulmonary complications<br />
after abdominal surgery: a systematic review. Chest 2006;<br />
130(6):1887–1899.<br />
110. Pennock BE, Kaplan PD, Carlin BW, Sabangan JS,<br />
Magovern JA. Pressure support ventilation with a simplified<br />
ventilatory support system administered with a nasal<br />
mask in patients with respiratory failure. Chest 1991;100(5):<br />
1371–1376.<br />
111. Gust R, Gottschalk A, Schmidt H, Bottiger BW, Bohrer H,<br />
Martin E. Effects of continuous (CPAP) and bi-level positive<br />
airway pressure (BiPAP) on extravascular lung water<br />
after extubation of the trachea in patients following coronary<br />
artery bypass grafting. Intensive Care Med 1996;<br />
22(12):1345–1350.<br />
112. Matte P, Jacquet L, Van Dyck M, Goenen M. Effects of<br />
conventional physiotherapy, continuous positive airway<br />
pressure and non-invasive ventilatory support with bilevel<br />
positive airway pressure after coronary artery bypass<br />
grafting. Acta Anaesthesiol Scand 2000;44(1):75–81.<br />
113. Aguilo R, Togores B, Pons S, Rubi M, Barbe F, Agusti AG.<br />
Noninvasive ventilatory support after lung resectional<br />
surgery. Chest 1997;112(1):117–121.<br />
114. Kindgen-Milles D, Buhl R, Gabriel A, Bohner H, Muller<br />
E. Nasal continuous positive airway pressure: a method to<br />
avoid endotracheal reintubation in postoperative high-risk<br />
patients with severe nonhypercapnic oxygenation failure.<br />
Chest 2000;117(4):1106–1111.<br />
115. Squadrone V, Coha M, Cerutti E, et al. Continuous positive<br />
airway pressure for treatment of postoperative hypoxemia:<br />
a randomized controlled trial. JAMA 2005;293(5):589–595.<br />
116. Esteban A, Frutos-Vivar F, Ferguson ND, et al. Noninvasive<br />
positive-pressure ventilation for respiratory failure<br />
after extubation. N Engl J Med 2004;350(24):2452–2460.<br />
117. Brochard L, Mancebo J, Wysocki M, et al. Noninvasive<br />
ventilation for acute exacerbations of chronic obstructive<br />
pulmonary disease. N Engl J Med 1995;333(13):817–822.<br />
118. Brochard L. Non-invasive ventilation for acute exacerbations<br />
of COPD: a new standard of care. Thorax 2000;55(10):<br />
817–818.
164 R. Cartin-Ceba et al.<br />
119. Ebeo CT, Benotti PN, Byrd RP Jr, Elmaghraby Z, Lui J.<br />
<strong>The</strong> effect of bi-level positive airway pressure on postoperative<br />
pulmonary function following gastric surgery for<br />
obesity. Respir Med 2002;96(9):672–676.<br />
120. Joris JL, Sottiaux TM, Chiche JD, Desaive CJ, Lamy ML.<br />
Effect of bi-level positive airway pressure (BiPAP) nasal<br />
ventilation on the postoperative pulmonary restrictive<br />
syndrome in obese patients undergoing gastroplasty. Chest<br />
1997;111(3):665–670.<br />
121. Angus DC, Kelley MA, Schmitz RJ, White A, Popovich J<br />
Jr. Caring for the critically ill patient. Current and projected<br />
workforce requirements for care of the critically<br />
ill and patients with pulmonary disease: can we meet<br />
the requirements of an aging population? JAMA 2000;<br />
284(21):2762–2770.<br />
122. Rice DP, Fineman N. Economic implications of increased<br />
longevity in the United States. Annu Rev Public Health<br />
2004;25:457–473.<br />
123. Sevransky JE, Haponik EF. Respiratory failure in elderly<br />
patients. Clin Geriatr Med 2003;19(1):205–224.<br />
124. Sloane PJ, Gee MH, Gottlieb JE, et al. A multicenter registry<br />
of patients with acute respiratory distress syndrome.<br />
Physiology and outcome. Am Rev Respir Dis 1992;146(2):<br />
419–426.<br />
125. Luhr OR, Karlsson M, Thorsteinsson A, Rylander C,<br />
Frostell CG. <strong>The</strong> impact of respiratory variables on mortality<br />
in non-ARDS and ARDS patients requiring mechanical<br />
ventilation. Intensive Care Med 2000;26(5):508–517.<br />
126. Ely EW, Evans GW, Haponik EF. Mechanical ventilation<br />
in a cohort of elderly patients admitted to an intensive care<br />
unit. Ann Intern Med 1999;131(2):96–104.<br />
127. Groeger JS, Guntupalli KK, Strosberg M, et al. Descriptive<br />
analysis of critical care units in the United States: patient<br />
characteristics and intensive care unit utilization. Crit Care<br />
Med 1993;21(2):279–291.<br />
128. Thompson LF. Failure to wean: exploring the influence of<br />
age-related pulmonary changes. Crit Care Nurs Clin North<br />
Am 1996;8(1):7–16.<br />
129. Kleinhenz ME, Lewis CY. Chronic ventilator dependence<br />
in elderly patients. Clin Geriatr Med 2000;16(4):735–756.<br />
130. Gajic O, Dara SI, Mendez JL, et al. Ventilator-associated<br />
lung injury in patients without acute lung injury at the<br />
onset of mechanical ventilation. Crit Care Med 2004;32(9):<br />
1817–1824.<br />
131. Fernandez-Perez ER, Keegan MT, Brown DR, Hubmayr<br />
RD, Gajic O. Intraoperative tidal volume as a risk factor<br />
for respiratory failure after pneumonectomy. <strong>Anesthesiology</strong><br />
2006;105(1):14–18.<br />
132. Choi G, Wolthuis EK, Bresser P, et al. Mechanical ventilation<br />
with lower tidal volumes and positive end-expiratory<br />
pressure prevents alveolar coagulation in patients without<br />
lung injury. <strong>Anesthesiology</strong> 2006;105(4):689–695.<br />
133. Michelet P, D’Journo XB, Roch A, et al. Protective ventilation<br />
influences systemic inflammation after esophagectomy:<br />
a randomized controlled study. <strong>Anesthesiology</strong> 2006;<br />
105(5):911–919.
12<br />
Operative Debridements of Chronic Wounds<br />
Andrew M. Hanflik, Michael S. Golinko, Melissa Doft, Charles Cain,<br />
Anna Flattau, and Harold Brem<br />
<strong>The</strong> term “chronic wound” does not refer to duration over<br />
time, but rather describes a wound that is physiologically<br />
impaired. All venous, pressure, and diabetic foot ulcers are<br />
defined as chronic wounds. Elderly patients are more likely<br />
to experience venous and pressure ulcers, 1–4 which lead to<br />
more than half of all lower extremity amputations in<br />
persons with diabetes. 5 Chronic wounds heal at the same<br />
frequency of closure in elderly populations as they do in<br />
younger populations, but may heal at a slower rate, primarily<br />
because of comorbidities associated with age. 6–9 <strong>The</strong><br />
comorbidities that delay healing are prevalent among older<br />
populations and include venous insufficiency and diabetes.<br />
Although there are age-related changes to the skin, it has<br />
yet to be shown, clinically, that age alone decreases an<br />
elderly person’s ability to heal. 7,10,11 A synergistic effect of<br />
advanced age and diabetes significantly slows healing. 12<br />
Chronic wounds in elderly patients heal successfully if<br />
the care regimen includes a coordinated effort to treat<br />
skin breakdown early and to prevent further ulceration.<br />
In the absence of ischemia and osteomyelitis, prompt<br />
medical treatment will heal most venous ulcers, diabetic<br />
foot ulcers, and stage I, II, and III pressure ulcers (defined<br />
below). 6 Delayed wound treatment, combined with multiple<br />
comorbidities affecting the elderly population, can<br />
lead to amputations, sepsis, and death. <strong>The</strong> established<br />
pathway from untreated chronic wound to death has<br />
been used as evidence for the manslaughter convictions<br />
of several care providers of the elderly. 13<br />
Pain is a complex and almost universal complication of<br />
this population, and appropriate pain management by an<br />
anesthesiologist is becoming increasingly recognized as<br />
essential in the optimal treatment of these patients.<br />
<strong>The</strong> Operating Room<br />
<strong>The</strong> only universally accepted treatment for chronic<br />
wounds is surgical debridement. This is the standard of<br />
care for nonviable and infected tissue and for the stimulation<br />
of healing. 14 Because these patients usually have<br />
multiple comorbidities and American Society of Anesthesiologists<br />
(ASA) scores of 3 or 4, we recommend<br />
operative debridement under local or regional anesthesia<br />
whenever possible. <strong>Regional</strong> blocks of the sciatic, popliteal,<br />
and femoral nerves are ideal. Many patients will<br />
require general anesthesia. It is essential that the patient<br />
and primary care physician understand this, as well as<br />
understand that the risks of not performing the debridement,<br />
i.e., leaving necrotic or infected tissue in an elderly<br />
person, is greater than the risks of anesthesia itself. For<br />
patients with peripheral arterial disease, treatment of<br />
underlying ischemia must be achieved before elective<br />
debridements unless infection is present.<br />
Chronic Wounds in the Elderly Result<br />
in Significant Morbidity and Mortality<br />
Diabetic Foot Ulcers<br />
<strong>The</strong>re are 20.8 million Americans diagnosed with diabetes.<br />
15 <strong>The</strong> elderly are the largest constituent of this group<br />
because diabetes affects more than 18% of Americans<br />
greater than 60 years old. 16 In the United States between<br />
1997 and 2004, the number of new cases of diabetes<br />
increased 54%. 17 By the year 2030, 366 million persons<br />
worldwide are estimated to have diabetes, with 130<br />
million of them over the age of 64. 18 All of these patients<br />
are at risk for diabetic complications including retinopathy,<br />
nephropathy, neuropathy, and accelerated atherosclerosis.<br />
Neuropathy and atherosclerosis are associated with<br />
the development of diabetic foot ulcers and impaired<br />
healing. 19–21<br />
In the United States, the elderly account for 53.3% of<br />
diabetes-associated amputations per annum. 5 Diabetic<br />
foot ulcers are defined as any breakdown of skin on the<br />
foot of a diabetic person. Recent prevalence is as high<br />
as 12% of all people with diabetes. 22 <strong>The</strong>se ulcers act<br />
165
166 A.M. Hanflik et al.<br />
A B C<br />
Figure 12-1. Examples of diabetic foot ulcers. Note: any break<br />
in the epidermis on the foot of a patient with diabetes is considered<br />
a diabetic foot ulcer. A: Typical-appearing ulcer under<br />
the fifth metatarsal head. B: A more advanced ulcer on the toe.<br />
C: A callous surrounded by central ulceration on the plantar<br />
aspect of the foot.<br />
as portals for infectious organisms. A large multicenter<br />
study recently reported 58% of all patients with ulcers<br />
had concomitant foot infection. 23 Half of the patients who<br />
develop one foot lesion subsequently develop a contralateral<br />
wound. 24 Each wound is considered to be chronic<br />
from its inception and should be treated early. Individuals<br />
with diabetes have a 30- to 40-fold higher risk of lower<br />
limb amputation. 25 See Figure 12-1A–C for examples of<br />
the typical locations of diabetic foot ulcers.<br />
Pressure Ulcers<br />
<strong>The</strong> four stages of pressure ulcers are defined as 26,27 :<br />
Stage I—Observable pressure-related alteration of intact<br />
skin whose indicators as compared with the adjacent<br />
or opposite area on the body may include changes in<br />
one or more of the following: skin temperature (warmth<br />
or coolness), tissue consistency (firm or boggy feel),<br />
and/or sensation (pain, itching). <strong>The</strong> ulcer appears as a<br />
defined area of persistent redness in lightly pigmented<br />
skin, whereas in darker skin tones the ulcer may<br />
appear with persistent red, blue, or purple hues. See<br />
Figure 12-2A.<br />
Stage II—Partial-thickness skin loss involving epidermis,<br />
dermis, or both. <strong>The</strong> ulcer is superficial and presents<br />
clinically as an abrasion, blister, or shallow crater. See<br />
Figure 12-2B.<br />
Stage III—Full-thickness skin loss involving damage to,<br />
or necrosis of, subcutaneous tissue that may extend<br />
down to, but not through, underlying fascia. <strong>The</strong> ulcer<br />
presents clinically as a deep crater with or without<br />
undermining of adjacent tissue. See Figure 12-2C.<br />
Stage IV—Full-thickness skin loss with ulceration extending<br />
through the fascia, with extensive destruction, tissue<br />
necrosis, or damage to muscle, bone, or supporting<br />
structures (e.g., tendon, joint, capsule). Undermining<br />
and sinus tracts are frequently associated with stage IV<br />
pressure ulcers. See Figure 12-2D.<br />
In 2003, 455,000 patients in the United States alone<br />
were hospitalized for pressure ulcers, representing a 63%<br />
increase from 1993: the most common reason for admission<br />
was septicemia. 28 <strong>The</strong> true incidence and prevalence<br />
of pressure ulcers is not known. A recent national study<br />
of acute care settings found that the prevalence of pressure<br />
ulcers ranged between 14% and 17%, whereas the<br />
incidence was between 7% and 9%. 29 At least 10% of<br />
hospitalized patients, more than 20% of nursing home<br />
patients, and 20%–30% of spinal cord injury patients are<br />
affected. 30 In a nursing home study, 6.5%–19.3% of<br />
patients developed a new pressure ulcer over a 3- to 21-<br />
month period. Patients at highest risk were those who<br />
had diabetes or fecal incontinence. 31 Recent studies have<br />
demonstrated that both age and immobility are strongly<br />
linked to development of pressure ulcers 32,33 as well as<br />
cognitive ability. 34<br />
<strong>The</strong> presence of a pressure ulcer doubles the risk of<br />
mortality in an elderly patient. 35,36 Elderly patients discharged<br />
with a hospital-acquired pressure ulcer have a<br />
much greater risk of death within a year than patients<br />
without a pressure ulcer, indicating that stage IV pressure<br />
ulcers should never be ignored. 37 A recent study of more<br />
than 100,000 patients revealed an overall age-adjusted<br />
mortality rate of 3.79%, for which pressure ulcers were<br />
listed as the cause of death in 18.7% of patients. 38 Stage<br />
IV pressure ulcers often lead to sepsis, a common cause<br />
of death in the elderly. 39,40<br />
Venous Ulcers<br />
It is estimated that 1.7% of the elderly population is<br />
affected by venous ulcers, indicating that they are more<br />
prevalent in the elderly than in younger populations. 41–43
12. Operative Debridements of Chronic Wounds 167<br />
A B C<br />
D<br />
Figure 12-2. Examples of different stages of pressure ulcers. A: Stage<br />
I, heel. B: Stage II, ischium. C: Stage III, trochanter. D: Stage IV,<br />
ischium.<br />
Venous ulcers are often misdiagnosed as traumatic injuries<br />
and are therefore undertreated. 44 Although these<br />
wounds are not frequently associated with osteomyeli -<br />
tis or amputation, when undertreated, they provide a<br />
gateway for infection that results in multiple hospitalizations,<br />
substantial suffering, and health care costs exceeding<br />
$1 billion annually. 45,46<br />
Venous ulcers are secondary to venous reflux disease,<br />
which correlates with increased age. 41,47,48 An example of<br />
a typical venous ulcer is shown in Figure 12-3. Venous<br />
reflux disease occurs when valvular incompetence prevents<br />
normal blood flow from superficial veins to deep<br />
veins. <strong>The</strong> most common etiologies for valvular dysfunction<br />
of the deep venous system are advanced age 41,49 and<br />
a history of deep vein thrombosis (DVT). 50 Valvular<br />
incompetence causes increased venous pressures, leading<br />
to venous distention and activation of apoptotic pathways,<br />
resulting in ulceration. Another hypothesis is that<br />
leukocytes and other large molecules become trapped in<br />
the dermis in response to endothelial damage and venous<br />
hypertension. 51 It is thought the extravasation of these<br />
large molecules, proteins, and leukocytes inhibits growth<br />
factors from reaching their targets. 52<br />
Ischemic Wounds<br />
Peripheral arterial disease is often the primary etiology<br />
of an ischemic wound. It can also impair healing in venous,<br />
pressure, and diabetic foot ulcers because of a decreased<br />
blood flow to the affected area. Age, hypertension,<br />
smoking, and diabetes are each independent risk factors<br />
for developing peripheral arterial disease. 4,53 Although<br />
the incidence of peripheral arterial disease is only 4.3%<br />
in patients over 40 years old, the incidence sharply<br />
increases to 14.5% in patients over 70. 4 Additionally, a<br />
large study of Asian patients with diabetes over the age
168 A.M. Hanflik et al.<br />
macrophage function in the older animals. 63–65 <strong>The</strong><br />
decrease in angiogenesis causes an initial delay in wound<br />
healing; yet, despite this, wounds contract with comparable<br />
frequency. 66 <strong>The</strong>refore, a decreased angiogenic<br />
response in older animals contributes to an impaired<br />
wound-healing rate.<br />
Decreased Immune Response<br />
Review of experimental and clinical research has shown<br />
physiologic impairments in the immune response of the<br />
elderly, making them prone to infection. 67 Older animals<br />
have a markedly decreased adaptive immune response<br />
(B and T cells), 67 a bolstered but possibly dysfunctio -<br />
nal regulatory T cell population (CD4+ CD25+), 68,69 a<br />
decrease in T cell receptor diversity, 70 and a decrease in<br />
toll-like receptors 65 and γδ-T cells. 71 <strong>The</strong> decreased<br />
immune response makes the elderly more susceptible to<br />
pathogenic invasion.<br />
Figure 12-3. Example of a typical lower extremity venous<br />
ulcer.<br />
of 50 showed the prevalence of peripheral arterial disease<br />
to be 17.7%. 54 Many if not most of these patients are<br />
asymptomatic. 55,56<br />
Experimental Evidence of Physiologic<br />
Impairments in the Elderly<br />
Clinical and experimental studies have demonstrated<br />
that there is a greater frequency of physiologic impairments<br />
to wound healing in the elderly population.<br />
Angiogenesis in Wound Healing<br />
Laboratory research has identified more than 30 regulatory<br />
mechanisms of angiogenesis that occur during wound<br />
healing, including growth factors, growth factor receptors,<br />
chemotactic agents, and matrix metalloproteinases. In<br />
animal models, decreased angiogenesis significantly<br />
inhibits wound healing. 16,57–59 In these models, angiogenic<br />
cytokines such as vascular endothelial growth factor are<br />
present in smaller concentrations in the wounds of older<br />
animals compared with younger animals, resulting in<br />
smaller capillary densities within the wound bed. 60–62 It is<br />
theorized that the discrepancy is secondary to decreased<br />
A Multidisciplinary Approach for<br />
Treating Venous, Pressure, and<br />
Diabetic Foot Ulcers<br />
Many wounds that appear minor on initial physical examination<br />
signal extensive necrosis beneath the skin’s<br />
surface and consequently may still be a significant source<br />
of sepsis (Figure 12-4). It is therefore critical to treat all<br />
wounds early and comprehensively. In the elderly population,<br />
patient care frequently focuses on the patient’s<br />
comorbidities, whereas wounds are simply covered with<br />
a bandage and ignored. Too often, untreated wounds lead<br />
to preventable complications such as amputation, sepsis,<br />
and death. As part of an ongoing multidisciplinary collaboration<br />
among many specialists who care for elderly<br />
patients with chronic wounds, we have developed protocols<br />
to treat venous, 44 pressure, and diabetic foot<br />
ulcers. 6,44,72,73 Outlined below are the precepts of our<br />
treatment protocol (Table 12-1).<br />
1. Contact the Primary Care Physician:<br />
A strong relationship with the primary care physician<br />
is essential to optimize the many comorbidities of the<br />
elderly patient. Common medical diseases that must be<br />
assessed include: coronary artery disease, diabetes,<br />
obesity, hypertension, dyslipidemia, chronic renal insufficiency,<br />
malnutrition, muscular atrophy, hepatic disease,<br />
chronic obstructive pulmonary disease, coagulopathy,<br />
and pain. In the diabetic population, seeking the counsel<br />
of a diabetologist may be necessary to maintain proper<br />
glucose control. <strong>The</strong> primary care physician, along with<br />
the assistance of a nutritionist, can also be helpful in<br />
evaluating the patient’s nutritional status. A small number<br />
of prospective studies has found that nutritional
12. Operative Debridements of Chronic Wounds 169<br />
Figure 12-4. Pressure ulcers can be deceptively large. Pressure<br />
ulcers are often much larger than they appear to be. Wounds<br />
that may look quite small can contain extensive undermining<br />
and/or tunneling. This figure demonstrates three cases in which,<br />
upon debridement, the wound was shown to be substantially<br />
larger than it appeared at presentation.<br />
supplements are beneficial in treating chronic wounds in<br />
malnourished patients. 74–76<br />
2. Comprehensive Physical Examination of At-Risk<br />
Patients:<br />
Table 12-1. Summary of the current standard of care for the<br />
healing of venous ulcers, pressure ulcers, and diabetic foot<br />
ulcers.<br />
1. Contact the primary care physician<br />
2. Comprehensive physical examination of at-risk patients<br />
3. Prevention of deep vein thrombosis<br />
4. Laboratory and radiologic evaluations<br />
5. Evaluation of blood flow in the lower extremities<br />
6. Objective measurement of every wound weekly with digital<br />
photography, planimetry, and documentation of the woundhealing<br />
process<br />
7. Elimination of cellulitis, drainage, and infection<br />
8. Local wound care<br />
9. Debridement of nonviable tissue and wound bed preparation<br />
10. Offloading pressure from the wound and compression therapy<br />
11. Growth factor therapies<br />
12. Addressing comorbidities that may affect anesthesia<br />
13. Physical therapy<br />
14. Pain management<br />
Diabetic and bed-bound patients are at high risk for<br />
developing diabetic foot and pressure ulcers, respectively.<br />
<strong>The</strong>se patients often lack protective sensation. As a consequence,<br />
they do not sense skin breakdown and are<br />
unable to assess wound progression. All diabetics must<br />
have their feet examined daily for evidence of skin breakdown.<br />
All bed-bound patients should have their pressure<br />
points (heels, ischia, trochanters, and sacrum) examined<br />
daily for evidence of pressure ulcer development.<br />
3. Prevention of Deep Vein Thrombosis:<br />
<strong>The</strong> physical therapy team should ensure that every<br />
patient who is able to ambulate is doing so. In nonambulatory<br />
patients, we recommend moving from the bed to a<br />
chair at least twice a day. Standard deep vein prophylaxis<br />
is mandatory, including pneumatic compression boots and<br />
subcutaneous heparin or low-molecular-weight heparin.<br />
4. Laboratory and Radiologic Evaluation:<br />
Baseline laboratory tests should be obtained to evaluate<br />
the patient’s overall health and to potentially detect<br />
underlying disease states. We recommend a complete<br />
blood count with differential, coagulation profile, creatinine<br />
and blood urea nitrogen levels, electrolyte panel,
170 A.M. Hanflik et al.<br />
lipid panel, glycosylated hemoglobin, albumin and prealbumin,<br />
erythrocyte sedimentation rate, hepatic panel,<br />
and thyroid-stimulating hormone level. Plain films of<br />
the affected area are recommended for all leg and foot<br />
wounds. Magnetic resonance imaging or bone scan is<br />
recommended to assess for osteomyelitis in stage IV<br />
pressure ulcers and in diabetic foot ulcers.<br />
5. Evaluation of Blood Flow in the Lower Extremities:<br />
Peripheral arterial disease and venous stasis disease<br />
are prevalent in the elderly population. All patients with<br />
limb ulcers should undergo arterial testing, regardless of<br />
what the primary etiology is thought to be, because the<br />
etiology may be multifactorial. Arterial testing is crucial<br />
because patients with ischemia should be revascularized<br />
before debridement and should not undergo compression<br />
therapy. Testing for venous stasis disease should be done<br />
in patients who clinically appear to have venous stasis<br />
ulcers.<br />
Noninvasive flow studies, which include bilateral<br />
ankle brachial indices (comparison of pressures in ankles<br />
and arms) and pulse volume recordings (to determine<br />
the amount of blood flow when pressures are falsely<br />
elevated), are necessary to detect lower extremity ischemia.<br />
In particular, recent studies have suggested<br />
high sensitivity to detect peripheral arterial disease using<br />
the low ankle pressure test defined as the quotient of<br />
the lowest ankle artery pressure of two measurements<br />
and the highest of two brachial artery pressure measurements.<br />
77,78 Depression of these values is associated with<br />
a greater risk of amputation. 79 An ankle brachial index<br />
less than 0.9 indicates significant arterial disease that<br />
requires referral to a vascular surgeon. 80 An elevated<br />
ankle brachial index greater than 1.30 has been found to<br />
be predictive of major amputation 81 and, particularly in<br />
the context of poor waveforms (i.e., monophasic), 82<br />
may indicate atherosclerosis requiring vascular surgery<br />
referral.<br />
When indicated, revascularization should proceed as<br />
soon as possible. Bypass grafting procedures are often<br />
avoided in elderly patients because their comorbidities<br />
make them poor surgical candidates. Alternatively, endovascular<br />
revascularization provides a minimally invasive<br />
and effective surgical option. Endovascular correction of<br />
arterial disease has proven safe and leads to 5-year limb<br />
salvage rates of more than 89% in diabetic and elderly<br />
populations. 83–87 If wound debridement is necessary, it<br />
should be done shortly after revascularization so as to<br />
utilize the improved blood supply. 88<br />
Duplex ultrasonography testing determines the presence<br />
and degree of venous insufficiency in patients with<br />
venous ulcers. Because venous incompetence is often<br />
attributable to a previous DVT, it is possible that the<br />
patient may concurrently have a DVT and a venous ulcer.<br />
In this scenario, the DVT will be identified by the venous<br />
flow studies.<br />
Once venous ulcers have healed, venous insufficiency<br />
should be corrected. Minimally invasive techniques such<br />
as radiofrequency ablation of the greater saphenous vein,<br />
percutaneous vein valve bioprosthesis, and subfascial<br />
endoscopic perforator vein surgery are treatment<br />
options. 89–91 Correction of the underlying venous disease<br />
prevents recurrence of venous ulcers. 92–94<br />
6. Objective Assessment of Wound Healing:<br />
Weekly wound-healing assessments should be objectively<br />
calculated by digital photography and planimetric<br />
measurements. Although a simple ruler has been shown<br />
to be reliable for predicting wound healing, 95 digital photography<br />
and computer-based wound measurements are<br />
more accurate for larger wounds and allow for easy transportation<br />
of data. Ideally, all data can be compiled into a<br />
wound electronic medical record (WEMR), if available,<br />
which plots a wound graph, demonstrating the healing<br />
curve of the wound based on planimetric measurements<br />
and allowing the team to objectively follow the progress<br />
of the wound. Serial objective measurements of the<br />
wound area allow the treatment team to accurately and<br />
rapidly detect a failure to heal and to adjust the treatment<br />
plan accordingly. A WEMR can also store the patient’s<br />
medical history, wound history (wound graph, drainage,<br />
pain, associated pathology, surgery history, radiology, and<br />
microbiology), laboratory values, antibiotic history, vascular<br />
studies, medications, wound picture, and contact<br />
information for the patient’s primary care doctor, pharmacist,<br />
and next of kin. <strong>The</strong> WEMR provides all of the<br />
patient’s pertinent data needed for thorough treatment<br />
in an easy-to-read format.<br />
7. Elimination of Infection:<br />
Infection substantially impairs chronic wound healing.<br />
Drainage, cellulitis, and pain are indicators of infection.<br />
Deep tissue cultures reflect the pathogens populating the<br />
wound bed and surrounding tissue, and they allow the<br />
physician to tailor the patient’s antibiotic regimen to<br />
cover only the pathogens grown from cultures, thereby<br />
helping to prevent drug-resistant organisms. 96–99 Deep<br />
tissue cultures are taken when the wound is debrided. If<br />
definitive debridement is not immediately planned, then<br />
an initial deep culture should be obtained at bedside, in<br />
the emergency room, or in the outpatient clinic, at the<br />
time when antibiotics are started.<br />
8. Local Wound Care:<br />
Homecare nursing is an integrated element in the<br />
wound-healing team. All wounds must be properly<br />
cleaned, treated with topical medications, and covered<br />
with the appropriate noncompressive or compressive<br />
dressing. Cleaning the wound includes washing with antimicrobial<br />
soap and water and scrubbing the wound with<br />
sterile saline and gauze. <strong>The</strong> topical therapy, such as<br />
cadexomer iodine (Iodosorb or Iodoflex; Smith &<br />
Nephew, Largo, FL), Acticoat (Smith &Nephew), and
12. Operative Debridements of Chronic Wounds 171<br />
Collagenase (Healthpoint, Fort Worth, TX), should<br />
provide a moist wound-healing environment and prevent<br />
bacterial colonization.<br />
9. Debridement of Nonviable Tissue and Wound Bed<br />
Preparation:<br />
Debridement of a chronic wound accelerates healing. 88<br />
It is a recommended treatment for diabetic foot ulcers,<br />
pressure ulcers, and venous ulcers. 100–103 For ischemic<br />
ulcers, debridement should be deferred until after revascularization.<br />
Gene expression is altered in the nonhealing<br />
edge of a chronic wound, resulting in hyperkeratotic epidermis<br />
and up-regulation of the oncogene c-myc. 104<br />
Debriding past this edge into healthy tissue stimulates<br />
the healthy epithelium to release growth factors and<br />
reduces local inflammation. It is thought that debridement<br />
encourages new fibroblasts to invade and replace<br />
the senescent cells of chronic wound beds, as well as<br />
release of various growth factors that stimulate wound<br />
healing, although few rigorous studies demonstrate this. 88<br />
Debridement also allows the surgeon to obtain microbiology<br />
and pathology samples that tailor antibiotic treatments<br />
and guide future debridements. For patients with<br />
active infection (such as cellulitis, fever, or elevated white<br />
blood cell count), debridement removes infected necrotic<br />
tissue that is the source of infection.<br />
Venous ulcers should be debrided deeply enough to<br />
remove all underlying scar and infected tissue; only several<br />
millimeters of the surrounding epithelium need to be<br />
debrided. Pressure ulcers should be debrided to remove<br />
all infected, necrotic, and scarred tissue, as well as to allow<br />
deep packing during dressing changes. Diabetic foot<br />
ulcers often appear as a callus with a central ulceration.<br />
We consider the callus as part of the wound, and we recommend<br />
debridement of a diabetic foot ulcer 2–3 mm<br />
beyond the callus into healthy epithelium (Figure 12-5).<br />
Figure 12-5. Proper debridement of diabetic foot ulcers. Diabetic<br />
foot ulcers are often associated with a thick hyperkeratotic<br />
callus. This callus impedes the healing process and needs to be<br />
removed. Debridement of diabetic foot ulcers must extend<br />
several millimeters past the nonmigratory edge into healthy<br />
epithelium. Debridement will aid in healing by removing nonviable<br />
tissue while stimulating reepithelialization with healthy<br />
tissue.
172 A.M. Hanflik et al.<br />
<strong>The</strong> surgeon should take pathology samples from the<br />
postoperative wound bed to confirm whether the remaining<br />
tissue is healthy. Almost all patients require multiple<br />
debridements, and the pathology results will guide the<br />
extent of future debridements.<br />
Although it is possible to debride some ulcers at the<br />
bedside, many elderly patients are debrided in the operating<br />
room because of their significant cardiac and pulmonary<br />
comorbidities, the size of their wounds, dementia,<br />
pain control, and concerns regarding hemostasis. <strong>The</strong> personnel<br />
involved and close monitoring make the operating<br />
room the safest place for most elderly patients who<br />
require debridement.<br />
Pressure ulcers often have a significant amount of<br />
tunneling and undermining that are revealed only after<br />
debridement has begun (Figure 12-4). Bone resection can<br />
cause significant bleeding, and most debridements of<br />
wounds extending to bone should be considered for the<br />
operating room (Figure 12-6). Because of venous reflux<br />
disease, venous ulcer debridement often causes significant<br />
blood loss from capillary bleeding, varicose veins,<br />
and venous perforators. Large venous ulcer debridements<br />
should be done in the operating room.<br />
10. Offloading Pressure from the Wound and Compression<br />
<strong>The</strong>rapy:<br />
Pressure is a significant contributor to the development<br />
and progression of pressure and diabetic foot ulcers. Pressure<br />
can be alleviated in pressure ulcer patients by using<br />
specialized air fluidized or alternating air mattresses.<br />
Heel pressure ulcer patients should be given a Multi-<br />
Podus splint (Restorative Care of America, St. Petersburg,<br />
FL) or a foam-based Heelift (DM Systems, Evanston,<br />
IL) to relieve pressure. Frequent turning and attentive<br />
skin care are mandatory for the treatment of all patients.<br />
Many devices have been created to offload pressure from<br />
diabetic foot ulcers. 105–109<br />
For venous ulcers, compression therapy with a measured<br />
multilayered bandage such as the Profore system<br />
(Smith &Nephew) should be used in conjunction with<br />
topical therapies. 110 <strong>The</strong>se bandages decrease superficial<br />
vein distention and venous pressure, and they increase<br />
the efficacy of venous valves. This promotes the proper<br />
flow of blood from superficial to deep veins. High compression<br />
is more effective than low compression bandages,<br />
but their use is limited to nonischemic patients. 111<br />
It is therefore imperative that all venous ulcer patients<br />
be evaluated for arterial insufficiency before compression<br />
therapy. Compression therapy should not be applied in<br />
the presence of active infection.<br />
11. Growth Factor <strong>The</strong>rapies:<br />
For the topical treatment of diabetic foot ulcers, the<br />
Food and Drug Administration has approved only Dermagraft<br />
112 (Advanced Tissue Sciences, La Jolla, CA),<br />
Human Skin Equivalent (HSE), Apligraf, 113 a bilayered,<br />
A<br />
B<br />
Figure 12-6. Proper hemostatic control often necessitates use<br />
of the operating room. A: Preoperative photo. B: Intraoperative<br />
debridement. <strong>The</strong> operating room provides a much higher level<br />
of hemostatic control than can be achieved at the bedside. This<br />
patient was admitted with a stage IV pressure ulcer. <strong>The</strong> wound<br />
permeated deep into the bone, and because of the large amount<br />
of bleeding that can be associated with the debridement of bone<br />
in these wounds, this case was safely completed in the operating<br />
room.<br />
biologically active construct composed of a bovine collagen<br />
scaffold seeded with a layer of keratinocytes covering<br />
a layer of fibroblasts (Organogenesis Inc., Canton, MA),<br />
and Becaplermin (recombinant platelet-derived growth<br />
factor) 114,115 for safety and efficacy. Only Apligraf is<br />
approved for safety and efficacy in venous ulcers. 116 No<br />
treatment is approved for safety and efficacy in pressure<br />
ulcers. <strong>The</strong>se agents should not be applied in the presence<br />
of active infection (cellulitis or wound drainage) and<br />
should be used only after surgical wound debridement.<br />
12. Comorbidities Affecting <strong>Anesthesia</strong>:<br />
Complicated cardiac conditions are common in the<br />
elderly and must be appropriately evaluated before
12. Operative Debridements of Chronic Wounds 173<br />
surgery. If the patient has risk factors for coronary artery<br />
disease, an exercise stress test should be considered<br />
before surgery. If the patient has a history of coronary<br />
atherosclerosis, pacemaker placement, valvular disease,<br />
congestive heart failure, or cardiac arrhythmia, cardiac<br />
function should optimized.<br />
Nephropathy is a common comorbidity in the elderly.<br />
<strong>The</strong> hypoproteinemia and acidemia seen in end-stage<br />
kidney disease patients can significantly affect the pharmacokinetics<br />
and pharmacodynamics of certain drugs<br />
used in anesthesia. 117 We recommend that end-stage<br />
kidney disease patients be dialyzed before surgery and<br />
that blood chemistries be closely monitored perioperatively.<br />
A venous blood gas is a safe, common approach<br />
to rapid evaluation of serum potassium and other<br />
electrolytes.<br />
Neuropathy is also a common complication in people<br />
with diabetes and most notably in the vast majority of<br />
persons with diabetic foot ulcers: in a recent study, 78%<br />
of diabetic patients with ulcers also had neuropathy. 118<br />
Because of the decrease in lower extremity sensation, it<br />
is rarely necessary to use a stronger anesthetic approach<br />
than a regional ankle block or Monitored <strong>Anesthesia</strong><br />
Care with local anesthetic injections.<br />
Pressure ulcers frequently affect spinal cord injury<br />
patients. <strong>The</strong> level of the spinal cord injury is particularly<br />
important. If the patient’s injury is above thoracic vertebra<br />
6, then the patient is at risk for autonomic dysreflexia.<br />
119 Autonomic dysreflexia is an abrupt and<br />
exaggerated autonomic response to stimuli in patients<br />
with spinal cord injuries or dysfunction above the splanchnic<br />
sympathetic outflow (T5–6). 120 It is imperative that all<br />
patients with a T6 lesion or higher be debrided in the<br />
operating room under spinal or general anesthesia and<br />
with close blood pressure monitoring.<br />
13. Physical <strong>The</strong>rapy:<br />
Physical therapy is advised for patients with limited<br />
mobility and those with venous ulcers. For patients with<br />
limited mobility, physical therapy (1) decreases the incidence<br />
of DVT, (2) decreases respiratory complications,<br />
(3) increases mental acuity, and (4) decreases the development<br />
of contractures. 121 In patients with venous ulcers,<br />
musculoskeletal changes attributable to calf pain and<br />
venous hypertension dramatically affect the patient’s<br />
gait. Physical therapy has been shown to improve underlying<br />
venous disease and patient ambulation. 122<br />
14. Pain Management:<br />
Pain is common in patients with ulcers, and effective<br />
pain management regimens must be instituted. Pain<br />
should be quantified by the patient at each clinic visit. By<br />
using a Verbal Analogue Score in conjunction with the<br />
wound-healing graph from a wound data sheet, a physician<br />
can track the success of pain treatments as they<br />
relate to functional outcomes. 123 <strong>The</strong> end goal is to reduce<br />
morbidity by eliminating pain. Pain control also facilitates<br />
appropriate cleaning and dressing of the wound,<br />
because patients may avoid these tasks if they are very<br />
painful. It may be necessary to incorporate a pain specialist<br />
into the treatment team.<br />
Each category of chronic wounds presents with a unique<br />
type of pain. In venous ulcers, pain is believed to occur as<br />
a result of tissue damage, which stimulates the release of<br />
inflammatory mediators, sensitizing peripheral somatic<br />
pain receptors. 124 Because of intense pain in many venous<br />
ulcer patients, we recommend using a tiered system of<br />
pain medications based on the World Health Organization<br />
analgesic ladder, 125 in which patients are started on<br />
nonopioid drugs with or without adjuvant medications,<br />
to which increasing strengths of opioid medications are<br />
added depending on pain-control needs. 123,124 Patients<br />
with multiple comorbidities may have contraindications<br />
to common pain medications. In addition, in elderly<br />
patients, special attention must be given to the potential<br />
side effects of pain medications, such as constipation or<br />
mental status changes from narcotics.<br />
Although often associated with neuropathy, diabetic<br />
foot ulcers and pressure ulcers can present with substantial<br />
pain management challenges. <strong>The</strong> pain associated<br />
with neuropathic diabetic foot ulcers can be treated with<br />
tricyclic antidepressants, anticonvulsants, capsaicin, mexiletine,<br />
lidocaine patches, N-methyl-d-aspartate (NMDA)<br />
inhibitors, clonidine, and tramadol. 124 All have been<br />
used with varying degrees of success. Spinal cord injury<br />
patients with pressure ulcers develop central pain that<br />
occurs when there is neuropathy in the area of the wound.<br />
Thus, spinal cord patients may also need pain control<br />
even though the wounded area is insensate.<br />
Intraoperative Risk and Precautions<br />
for Development of Pressure Ulcers<br />
Elderly patients with fragile skin and comorbid conditions<br />
are at highest risk for development of intraoperative<br />
pressure ulcers. Patients with a high ASA grade may<br />
be more likely to develop pressure ulcers. 126 <strong>The</strong> most<br />
comprehensive study was conducted in the United States<br />
in 1998 involving 104 hospitals and 1128 surgical patients,<br />
all undergoing procedures longer than 3 hours in duration.<br />
An overall prevalence of stage I and stage II pressure<br />
ulcers was 7.8% when examining patients up to 4<br />
days postoperatively. 127<br />
Part of the intraoperative risk can be assessed by type<br />
of procedure. Vascular surgery, cardiac surgery, and orthopedic<br />
surgery are associated with higher risks, although<br />
rigorous studies have yet to emerge. 128 <strong>The</strong> risk may<br />
double for operations lasting more than 2.5 hours. 129 In a<br />
prospective Dutch study 130 of patients undergoing operations<br />
lasting more than 4 hours, 44 patients (21.2%)
174 A.M. Hanflik et al.<br />
developed 70 pressure ulcers in the first 2 days postoperatively.<br />
All but three were stage I and II.<br />
Various locations may be at higher risk than others.<br />
<strong>The</strong> same Dutch study found that most heel ulcers were<br />
associated with cardiac procedures. <strong>The</strong>y also found head<br />
and neck procedures most often associated with sacral<br />
ulcers and that use of a semi-Fowler position (elevating<br />
both head and lower extremities to 30 degrees) may be<br />
beneficial. 130<br />
Full examination of all areas at risk including the<br />
sacrum, heels, ischia, and trochanteric areas with documentation<br />
of any skin changes and existing ulcers can<br />
help identify postoperative changes. Because the heel has<br />
the smallest surface area, this area may be at greatest risk<br />
intraoperatively. An ordinary head-pillow placed underneath<br />
each heel during the operation and through the<br />
time the patient is immobile is likely the most effective<br />
pressure-reducing device, followed by a siliconized<br />
hollow-fiber–based heel protector. 131 Further studies into<br />
a variety of mattress (foam versus gel) and alternative<br />
positioning have yet to be evaluated by rigorous randomized<br />
controlled trials.<br />
In most cases, if a wound is identified, extra care should<br />
be taken to relieve as much pressure from the surface as<br />
possible and to provide extra dressings either with 4 × 4<br />
sterile gauze or circumferential roll gauze to account for<br />
extra drainage from the wound during prolonged procedures.<br />
After the procedure, the dressings on all chronic<br />
wounds should be examined and changed as necessary.<br />
Conclusion<br />
Elderly patients are frequently affected by chronic<br />
wounds including pressure, venous, and diabetic foot<br />
ulcers. <strong>The</strong> elderly have the ability to heal from chronic<br />
wounds, but they are prone to multiple comorbidities that<br />
may slow the rate of healing, and complications from<br />
infection pose significant risks to patients who are already<br />
fragile. Operative debridement is usually most important<br />
to remove the source of infection. Safety of the elderly<br />
patient can be optimized by focusing on glycemic control,<br />
hydration, and often beta-blockade. If all wounds are<br />
treated using the protocol described herein, we postulate<br />
that amputations will be decreased, stage IV pressure<br />
ulcers nearly eliminated, and morbidity from venous<br />
ulcers reduced.<br />
References<br />
1. Walker N, Rodgers A, Birchall N, Norton R, MacMahon S.<br />
<strong>The</strong> occurrence of leg ulcers in Auckland: results of a<br />
population-based study. NZ Med J 2002;115:159–162.<br />
2. Livesley NJ, Chow AW. Infected pressure ulcers in elderly<br />
individuals. Clin Infect Dis 2002;35:1390–1396.<br />
3. Margolis DJ, Bilker W, Santanna J, Baumgarten M. Venous<br />
leg ulcer: incidence and prevalence in the elderly. J Am<br />
Acad Dermatol 2002;46:381–386.<br />
4. Selvin E, Erlinger TP. Prevalence of and risk factors for<br />
peripheral arterial disease in the United States: results<br />
from the National Health and Nutrition Examination<br />
Survey, 1999–2000. Circulation 2004;110:738–743.<br />
5. Data &Trends. National Diabetes Surveillance System.<br />
Hospitalizations for nontraumatic lower extremity amputation,<br />
1980–2003: Centers for Disease Control (CDC).<br />
Available at: http://www.cdc.gov/diabetes/statistics/lea/<br />
byAgetable1_2.htm. Accessed September 30, 2006.<br />
6. Brem H, Tomic-Canic M, Tarnovskaya A, et al. Healing of<br />
elderly patients with diabetic foot ulcers, venous stasis ulcers,<br />
and pressure ulcers. Surg Technol Int 2003;11:161–167.<br />
7. Gosain A, DiPietro LA. Aging and wound healing. World<br />
J Surg 2004;28:321–326.<br />
8. Margolis DJ, Allen-Taylor L, Hoffstad O, Berlin JA. Diabetic<br />
neuropathic foot ulcers: predicting which ones will<br />
not heal. Am J Med 2003;115:627–631.<br />
9. Margolis DJ, Allen-Taylor L, Hoffstad O, Berlin JA. <strong>The</strong><br />
accuracy of venous leg ulcer prognostic models in a wound<br />
care system. Wound Repair Regen 2004;12:163–168.<br />
10. Van de Kerkhof PC, Van Bergen B, Spruijt K, Kuiper JP.<br />
Age-related changes in wound healing. Clin Exp Dermatol<br />
1994;19:369–374.<br />
11. Thomas DR. Age-related changes in wound healing. Drugs<br />
Aging 2001;18:607–620.<br />
12. Brem H, Tomic-Canic M, Entero H, et al. <strong>The</strong> synergism<br />
of age and db/db genotype impairs wound healing. Exp<br />
Gerontol 2007 Jan 31.<br />
13. Di Maio VJ, Di Maio TG. Homicide by decubitus ulcers.<br />
Am J Forensic Med Pathol 2002;23:1–4.<br />
14. Attinger CE, Janis JE, Steinberg J, Schwartz J, Al-Attar A,<br />
Couch K. Clinical approach to wounds: debridement<br />
and wound bed preparation including the use of dressings<br />
and wound-healing adjuvants. Plast Reconstr Surg 2006;<br />
117:72S–109S.<br />
15. National Institute of Diabetes and Digestive and Kidney<br />
Diseases. National diabetes statistics fact sheet: general<br />
information and national estimates on diabetes in the<br />
United States, 2005. Bethesda, MD: U.S. Department of<br />
Health and Human Services, National Institute of Health.<br />
Available at: http://diabetes.niddk.nih.gov/. Accessed<br />
February 8, 2007.<br />
16. Klein SA, Bond SJ, Gupta SC, Yacoub OA, Anderson GL.<br />
Angiogenesis inhibitor TNP-470 inhibits murine cutaneous<br />
wound healing. J Surg Res 1999;82:268–274.<br />
17. Data &Trends. National Diabetes Surveillance System.<br />
Annual number (in thousands) of new cases of diagnosed<br />
diabetes among adults aged 18–79 years, United States,<br />
1997–2004: Centers for Disease Control (CDC). Available<br />
at: http://www.cdc.gov/diabetes/statistics/incidence/fig1.<br />
htm. Accessed September 30, 2006.<br />
18. Wild S, Roglic G, Green A, Sicree R, King H. <strong>Global</strong> prevalence<br />
of diabetes: estimates for the year 2000 and projections<br />
for 2030. Diabetes Care 2004;27:1047–1053.<br />
19. Pecoraro RE, Reiber GE, Burgess EM. Pathways to<br />
diabetic limb amputation. Basis for prevention. Diabetes<br />
Care 1990;13:513–521.
12. Operative Debridements of Chronic Wounds 175<br />
20. Boyko EJ, Ahroni JH, Stensel V, Forsberg RC, Davignon<br />
DR, Smith DG. A prospective study of risk factors for<br />
diabetic foot ulcer. <strong>The</strong> Seattle Diabetic Foot Study.<br />
Diabetes Care 1999;22:1036–1042.<br />
21. Abbott CA, Carrington AL, Ashe H, et al. <strong>The</strong> North-West<br />
Diabetes Foot Care Study: incidence of, and risk factors<br />
for, new diabetic foot ulceration in a community-based<br />
patient cohort. Diabet Med 2002;19:377–384.<br />
22. Aguiar ME, Burrows NR, Wang J, Boyle JP, Geiss LS,<br />
Engelgau MM. History of foot ulcer among persons with<br />
diabetes—United States, 2000–2002. MMWR Morb Mortal<br />
Wkly Rep 2003;52:1098–1102.<br />
23. Prompers L, Huijberts M, Apelqvist J, et al. High prevalence<br />
of ischaemia, infection and serious comorbidity in<br />
patients with diabetic foot disease in Europe. Baseline<br />
results from the Eurodiale study. Diabetologia 2007;50(1):<br />
18–25.<br />
24. Klamer TW, Towne JB, Bandyk DF, Bonner MJ. <strong>The</strong><br />
influence of sepsis and ischemia on the natural history<br />
of the diabetic foot. Am Surg 1987;53:490–494.<br />
25. Cevera JJ, Bolton LL, Kerstein MD. Options for diabetic<br />
patients with chronic heel ulcers. J Diabetes Complications<br />
1997;11:358–366.<br />
26. Pressure ulcers prevalence, cost and risk assessment:<br />
consensus development conference statement—<strong>The</strong><br />
National Pressure Ulcer Advisory Panel. Decubitus 1989;<br />
2:24–28.<br />
27. Margolis DJ. Definition of a pressure ulcer. Adv Wound<br />
Care 1995;8:Suppl 8–10.<br />
28. Russo CA, Elixhauser A. Hospitalizations Related to Pressure<br />
Sores, 2003 HCUP Statistical Brief #3. Rockville, MD:<br />
Agency for Healthcare Research and Quality; 2006.<br />
29. Whittington KT, Briones R. National Prevalence and<br />
Incidence Study: 6-year sequential acute care data. Adv<br />
Skin Wound Care 2004;17:490–494.<br />
30. Brem H, Nierman DM, Nelson JE. Pressure ulcers in the<br />
chronically critically ill patient. Crit Care Clin 2002;18:<br />
683–694.<br />
31. Brandeis GH, Ooi WL, Hossain M, Morris JN, Lipsitz LA.<br />
A longitudinal study of risk factors associated with the<br />
formation of pressure ulcers in nursing homes. J Am<br />
Geriatr Soc 1994;42:388–393.<br />
32. Allman RM, Goode PS, Patrick MM, Burst N, Bartolucci<br />
AA. Pressure ulcer risk factors among hospitalized patients<br />
with activity limitation. JAMA 1995;273:865–870.<br />
33. Eachempati SR, Hydo LJ, Barie PS. Factors influencing the<br />
development of decubitus ulcers in critically ill surgical<br />
patients. Crit Care Med 2001;29:1678–1682.<br />
34. Mecocci P, von Strauss E, Cherubini A, et al. Cognitive<br />
impairment is the major risk factor for development of<br />
geriatric syndromes during hospitalization: results from<br />
the GIFA study. Dement Geriatr Cogn Disord 2005;20:<br />
262–269.<br />
35. Berlowitz DR, Brandeis GH, Anderson J, Du W, Brand H.<br />
Effect of pressure ulcers on the survival of long-term<br />
care residents. J Gerontol A Biol Sci Med Sci 1997;52:<br />
M106–110.<br />
36. Dale MC, Burns A, Panter L, Morris J. Factors affecting<br />
survival of elderly nursing home residents. Int J Geriatr<br />
Psychiatry 2001;16:70–76.<br />
37. Thomas DR, Goode PS, Tarquine PH, Allman RM.<br />
Hospital-acquired pressure ulcers and risk of death. J Am<br />
Geriatr Soc 1996;44:1435–1440.<br />
38. Redelings MD, Lee NE, Sorvillo F. Pressure ulcers: more<br />
lethal than we thought? Adv Skin Wound Care 2005;18:<br />
367–372.<br />
39. Anderson RN, Smith BL. Deaths: leading causes for 2002.<br />
Natl Vital Stat Rep 2005;53:1–89.<br />
40. Angus DC, Linde-Zwirble WT, Lidicker J, Clermont G,<br />
Carcillo J, Pinsky MR. Epidemiology of severe sepsis in<br />
the United States: analysis of incidence, outcome, and associated<br />
costs of care. Crit Care Med 2001;29:1303–1310.<br />
41. Baker SR, Stacey MC, Jopp-McKay AG, Hoskin SE,<br />
Thompson PJ. Epidemiology of chronic venous ulcers.<br />
Br J Surg 1991;78:864–867.<br />
42. Abbade LPF, Lastoria S. Venous ulcer: epidemiology,<br />
physiopathology, diagnosis and treatment. Int J Dermatol<br />
2005;44:449–456.<br />
43. Margolis DJ, Bilker W, Santanna J, Baumgarten M. Venous<br />
leg ulcer: incidence and prevalence in the elderly. J Am<br />
Acad Dermatol 2002;46:381–386.<br />
44. Brem H, Kirsner RS, Falanga V. Protocol for the successful<br />
treatment of venous ulcers. Am J Surg 2004;188:1–8.<br />
45. Wissing U, Ek AC, Unosson M. Life situation and function<br />
in elderly people with and without leg ulcers. Scand J<br />
Caring Sci 2002;16:59–65.<br />
46. Valencia IC, Falabella A, Kirsner RS, Eaglstein WH.<br />
Chronic venous insufficiency and venous leg ulceration.<br />
J Am Acad Dermatol 2001;44:401–421; quiz 422–424.<br />
47. Capitao LM, Menezes JD, Gouveia-Oliveira A. A multivariate<br />
analysis of the factors associated with the severity<br />
of chronic venous insufficiency [in Portuguese]. Acta Med<br />
Port 1993;6:501–506.<br />
48. Delis KT. Perforator vein incompetence in chronic venous<br />
disease: a multivariate regression analysis model. J Vasc<br />
Surg 2004;40:626–633.<br />
49. Scott TE, LaMorte WW, Gorin DR, Menzoian JO. Risk<br />
factors for chronic venous insufficiency: a dual case-control<br />
study. J Vasc Surg 1995;22:622–628.<br />
50. van Haarst EP, Liasis N, van Ramshorst B, Moll FL. <strong>The</strong><br />
development of valvular incompetence after deep vein<br />
thrombosis: a 7 year follow-up study with duplex scanning.<br />
Eur J Vasc Endovasc Surg 1996;12:295–299.<br />
51. Falanga V, Eaglstein WH. <strong>The</strong> “trap” hypothesis of venous<br />
ulceration. Lancet 1993;341:1006–1008.<br />
52. Higley HR, Ksander GA, Gerhardt CO, Falanga V.<br />
Extravasation of macromolecules and possible trapping<br />
of transforming growth factor-beta in venous ulceration.<br />
Br J Dermatol 1995;132:79–85.<br />
53. Kweon SS, Shin MH, Park KS, et al. Distribution of the<br />
ankle-brachial index and associated cardiovascular risk<br />
factors in a population of middle-aged and elderly Koreans.<br />
J Korean Med Sci 2005;20:373–378.<br />
54. Rhee SY, Guan H, Liu ZM, et al. Multi-country study<br />
on the prevalence and clinical features of peripheral<br />
arterial disease in Asian type 2 diabetes patients at high<br />
risk of atherosclerosis. Diabetes Res Clin Pract 2007;76:<br />
82–92.<br />
55. Cimminiello C. PAD: epidemiology and pathophysiology.<br />
Thromb Res 2002;106:V295–V301.
176 A.M. Hanflik et al.<br />
56. Doubeni CA, Yood RA, Emani S, Gurwitz JH. Identifying<br />
unrecognized peripheral arterial disease among asymptomatic<br />
patients in the primary care setting. Angiology<br />
2006;57:171–180.<br />
57. Brem H, Tsakayannis D, Folkman J. Time dependent suppression<br />
of wound healing with the angiogenesis inhibitor,<br />
AGM-1470. J Cell Biol 1991;115:403a.<br />
58. O’Reilly MS, Brem H, Folkman J. Treatment of murine<br />
hemangioendotheliomas with the angiogenesis inhibitor<br />
AGM-1470. J Pediatr Surg 1995;30:325–330.<br />
59. Bond SJ, Klein SA. TNP-470 reduces collagen and macrophage<br />
accumulation in expanded polytetrafluoroethylene<br />
tube implants. J Surg Res 2001;101:99–103.<br />
60. Rivard A, Berthou-Soulie L, Principe N, et al. Agedependent<br />
defect in vascular endothelial growth factor<br />
expression is associated with reduced hypoxia-inducible<br />
factor 1 activity. J Biol Chem 2000;275:29643–29647.<br />
61. Rivard A, Fabre JE, Silver M, et al. Age-dependent impairment<br />
of angiogenesis. Circulation 1999;99:111–120.<br />
62. Swift ME, Kleinman HK, DiPietro LA. Impaired wound<br />
repair and delayed angiogenesis in aged mice. Lab Invest<br />
1999;79:1479–1487.<br />
63. Nathan CF. Secretory products of macrophages. J Clin<br />
Invest 1987;79:319–326.<br />
64. Cohen BJ, Danon D, Roth GS. Wound repair in mice as<br />
influenced by age and antimacrophage serum. J Gerontol<br />
1987;42:295–301.<br />
65. Plowden J, Renshaw-Hoelscher M, Engleman C, Katz J,<br />
Sambhara S. Innate immunity in aging: impact on macrophage<br />
function. Aging Cell 2004;3:161–167.<br />
66. Ballas CB, Davidson JM. Delayed wound healing in aged<br />
rats is associated with increased collagen gel remodeling<br />
and contraction by skin fibroblasts, not with differences in<br />
apoptotic or myofibroblast cell populations. Wound Repair<br />
Regen 2001;9:223–237.<br />
67. Yoshikawa TT. Perspective: aging and infectious diseases—<br />
past, present, and future. J Infect Dis 1997;176:1053–1057.<br />
68. Gregg R, Smith CM, Clark FJ, et al. <strong>The</strong> number of human<br />
peripheral blood CD4 CD25 regulatory T cells increases<br />
with age. Clin Exp Immunol 2005;140:540–546.<br />
69. Dejaco C, Duftner C, Schirmer M. Are regulatory T-cells<br />
linked with aging? Exp Gerontol 2006;41(4):339–345.<br />
70. Naylor K, Li G, Vallejo AN, et al. <strong>The</strong> influence of age on<br />
T cell generation and TCR diversity. J Immunol 2005;<br />
174:7446–7452.<br />
71. Colonna-Romano G, Aquino A, Bulati M, et al. Impairment<br />
of gamma/delta T lymphocytes in elderly: implications<br />
for immunosenescence. Exp Gerontol 2004;39:<br />
1439–1446.<br />
72. Brem H, Lyder C. Protocol for the successful treatment of<br />
pressure ulcers. Am J Surg 2004;188:9–17.<br />
73. Brem H, Sheehan P, Rosenberg HJ, Schneider JS, Boulton<br />
AJ. Evidence-based protocol for diabetic foot ulcers. Plast<br />
Reconstr Surg 2006;117:193S–209S; discussion 210S–211S.<br />
74. Berlowitz DR, Wilking SV. Risk factors for pressure sores.<br />
A comparison of cross-sectional and cohort-derived data.<br />
J Am Geriatr Soc 1989;37:1043–1050.<br />
75. Bergstrom N, Braden B. A prospective study of pressure<br />
sore risk among institutionalized elderly. J Am Geriatr Soc<br />
1992;40:747–758.<br />
76. Breslow RA, Hallfrisch J, Guy DG, Crawley B, Goldberg<br />
AP. <strong>The</strong> importance of dietary protein in healing pressure<br />
ulcers. J Am Geriatr Soc 1993;41:357–362.<br />
77. Niazi K, Khan TH, Easley KA. Diagnostic utility of the two<br />
methods of ankle brachial index in the detection of peripheral<br />
arterial disease of lower extremities. Catheter Cardiovasc<br />
Interv 2006;68:788–792.<br />
78. Schroder F, Diehm N, Kareem S, et al. A modified calculation<br />
of ankle-brachial pressure index is far more sensitive<br />
in the detection of peripheral arterial disease. J Vasc Surg<br />
2006;44:531–536.<br />
79. Carter SA, Tate RB. <strong>The</strong> relationship of the transcutaneous<br />
oxygen tension, pulse waves and systolic pressures to the<br />
risk for limb amputation in patients with peripheral arterial<br />
disease and skin ulcers or gangrene. Int Angiol 2006;<br />
25:67–72.<br />
80. ACC/AHA 2005 Practice Guidelines for the Management<br />
of Patients with Peripheral Arterial Disease (Lower<br />
Extremity, Renal, Mesenteric, and Abdominal Aortic): A<br />
Collaborative Report from the American Association for<br />
Vascular Surgery/Society for Vascular Surgery, Society for<br />
Cardiovascular Angiography and Interventions, Society<br />
for Vascular Medicine and Biology, Society of Interventional<br />
Radiology, and the ACC/AHA Task Force on Practice<br />
Guidelines (Writing Committee to Develop Guidelines<br />
for the Management of Patients with Peripheral Arterial<br />
Disease): Endorsed by the American Association of Cardiovascular<br />
and Pulmonary Rehabilitation; National Heart,<br />
Lung, and Blood Institute; Society for Vascular Nursing;<br />
TransAtlantic Inter-Society Consensus; and Vascular<br />
Disease Foundation. Circulation 2006;113:e463–654.<br />
81. Silvestro A, Diehm N, Savolainen H, et al. Falsely high<br />
ankle-brachial index predicts major amputation in critical<br />
limb ischemia. Vasc Med 2006;11:69–74.<br />
82. Williams DT, Harding KG, Price P. An evaluation of<br />
the efficacy of methods used in screening for lower-limb<br />
arterial disease in diabetes. Diabetes Care 2005;28:2206–<br />
2210.<br />
83. Laird JR, Zeller T, Gray BH, et al. Limb salvage following<br />
laser-assisted angioplasty for critical limb ischemia: results<br />
of the LACI multicenter trial. J Endovasc <strong>The</strong>r 2006;<br />
13:1–11.<br />
84. Costanza MJ, Queral LA, Lilly MP, Finn WR. Hemodynamic<br />
outcome of endovascular therapy for transatlantic<br />
intersociety consensus type B femoropopliteal arterial<br />
occlusive lesions. J Vasc Surg 2004;39:343–350.<br />
85. Becquemin J-P, Favre J-P, Marzelle J, Nemoz C, Corsin C,<br />
Leizorovicz A. Systematic versus selective stent placement<br />
after superficial femoral artery balloon angioplasty: a<br />
multicenter prospective randomized study. J Vasc Surg<br />
2003;37:487–494.<br />
86. Faglia E, Mantero M, Caminiti M, et al. Extensive use of<br />
peripheral angioplasty, particularly infrapopliteal, in the<br />
treatment of ischaemic diabetic foot ulcers: clinical results<br />
of a multicentric study of 221 consecutive diabetic subjects.<br />
J Intern Med 2002;252:225–232.<br />
87. Kudo T, Chandra FA, Ahn SS. <strong>The</strong> effectiveness of percutaneous<br />
transluminal angioplasty for the treatment of critical<br />
limb ischemia: a 10-year experience. J Vasc Surg 2005;<br />
41:423–435.
12. Operative Debridements of Chronic Wounds 177<br />
88. Steed DL. Debridement. Am J Surg 2004;187:S71–S74.<br />
89. Elias SM, Frasier KL. Minimally invasive vein surgery: its<br />
role in the treatment of venous stasis ulceration. Am J Surg<br />
2004;188:26–30.<br />
90. Puggioni A, Kalra M, Gloviczki P. Superficial vein surgery<br />
and SEPS for chronic venous insufficiency. Semin Vasc<br />
Surg 2005;18:41–48.<br />
91. Ting AC, Cheng SW, Ho P, Poon JT, Wu LL, Cheung GC.<br />
Reduction in deep vein reflux after concomitant subfascial<br />
endoscopic perforating vein surgery and superficial vein<br />
ablation in advanced primary chronic venous insufficiency.<br />
J Vasc Surg 2006;43:546–550.<br />
92. Barwell J, Davies CE, Deacon J, et al. Comparison of<br />
surgery and compression with compression alone in<br />
chronic venous ulceration (ESCHAR study): randomised<br />
controlled trial. Lancet 2004;363:1854–1859.<br />
93. TenBrook J, John A, Iafrati MD, et al. Systematic review<br />
of outcomes after surgical management of venous disease<br />
incorporating subfascial endoscopic perforator surgery.<br />
J Vasc Surg 2004;39:583–589.<br />
94. Roka F, Binder M, Bohler-Sommeregger K. Mid-term<br />
recurrence rate of incompetent perforating veins after<br />
combined superficial vein surgery and subfascial endoscopic<br />
perforating vein surgery. J Vasc Surg 2006;44:<br />
359–363.<br />
95. Kantor J, Margolis DJ. Efficacy and prognostic value of<br />
simple wound measurements. Arch Dermatol 1998;134:<br />
1571–1574.<br />
96. Edmonds M, Foster A. <strong>The</strong> use of antibiotics in the diabetic<br />
foot. Am J Surg 2004;187:25S–28S.<br />
97. Weigelt J, Kaafarani HM, Itani KM, Swanson RN. Linezolid<br />
eradicates MRSA better than vancomycin from<br />
surgical-site infections. Am J Surg 2004;188:760–766.<br />
98. Ruiz de Gopegui E, Oliver A, Ramirez A, Gutierrez O,<br />
Andreu C, Perez JL. Epidemiological relatedness of methicillin-resistant<br />
Staphylococcus aureus from a tertiary hospital<br />
and a geriatric institution in Spain. Clin Microbiol<br />
Infect 2004;10:339–342.<br />
99. Fridkin SK, Hageman JC, Morrison M, et al. <strong>The</strong> Active<br />
Bacterial Core Surveillance Program of the Emerging<br />
Infections Program Network. Methicillin-resistant Staphylococcus<br />
aureus disease in three communities. N Engl J<br />
Med 2005;352:1436–1444.<br />
100. Zacur H, Kirsner RS. Debridement: rationale and therapeutic<br />
options. Wounds Sep 2002;14:2S–6S.<br />
101. Saap LJ, Falanga V. Debridement performance index and<br />
its correlation with complete closure of diabetic foot ulcers.<br />
Wound Repair Regen 2002;10:354–359.<br />
102. Steed DL, Donohoe D, Webster MW, Lindsley L. Effect<br />
of extensive debridement and treatment on the healing<br />
of diabetic foot ulcers. Diabetic Ulcer Study Group. J Am<br />
Coll Surg 1996;183:61–64.<br />
103. Williams D, Enoch S, Miller D, Harris K, Price P, Harding<br />
KG. Effect of sharp debridement using curette on recalcitrant<br />
nonhealing venous leg ulcers: a concurrently controlled,<br />
prospective cohort study. Wound Repair Regen<br />
2005;13:131–137.<br />
104. Stojadinovic O, Brem H, Vouthounis C, et al. <strong>The</strong> role of<br />
the beta-catenin and c-myc in pathogenesis of cutaneous<br />
wound healing. Am J Pathol 2005;167:59–69.<br />
105. Steed DL. Foundations of good ulcer care. Am J Surg<br />
1998;176:20S–25S.<br />
106. Mueller MJ, Diamond JE, Sinacore DR, et al. Total contact<br />
casting in treatment of diabetic plantar ulcers. Controlled<br />
clinical trial. Diabetes Care 1989;12:384–388.<br />
107. Armstrong DG, Nguyen HC, Lavery LA, van Schie CH,<br />
Boulton AJ, Harkless LB. Off-loading the diabetic foot<br />
wound: a randomized clinical trial. Diabetes Care 2001;<br />
24:1019–1022.<br />
108. Armstrong DG, Short B, Espensen EH, Abu-Rumman PL,<br />
Nixon BP, Boulton AJM. Technique for fabrication of an<br />
“instant total-contact cast” for treatment of neuropathic<br />
diabetic foot ulcers. J Am Podiatr Med Assoc 2002;92:<br />
405–408.<br />
109. Boulton AJ, Kirsner RS, Vileikyte L. Clinical practice.<br />
Neuropathic diabetic foot ulcers. N Engl J Med 2004;<br />
351:48–55.<br />
110. Nelson EA, Iglesias CP, Cullum N, Torgerson DJ. Randomized<br />
clinical trial of four-layer and short-stretch compression<br />
bandages for venous leg ulcers (VenUS I). Br J Surg<br />
2004;91:1292–1299.<br />
111. Fletcher A, Cullum N, Sheldon TA. A systematic review of<br />
compression treatment for venous leg ulcers. BMJ 1997;<br />
315:576–580.<br />
112. Marston WA, Hanft J, Norwood P, Pollak R. <strong>The</strong> efficacy<br />
and safety of Dermagraft in improving the healing of<br />
chronic diabetic foot ulcers: results of a prospective randomized<br />
trial. Diabetes Care 2003;26:1701–1705.<br />
113. Veves A, Falanga V, Armstrong DG, Sabolinski ML.<br />
Graftskin, a human skin equivalent, is effective in the<br />
management of noninfected neuropathic diabetic foot<br />
ulcers: a prospective randomized multicenter clinical trial.<br />
Diabetes Care 2001;24:290–295.<br />
114. Steed DL. Clinical evaluation of recombinant human<br />
platelet-derived growth factor for the treatment of lower<br />
extremity diabetic ulcers. Diabetic Ulcer Study Group.<br />
J Vasc Surg 1995;21:71–78; discussion 79–81.<br />
115. Steed DL. Clinical evaluation of recombinant human<br />
platelet-derived growth factor for the treatment of lower<br />
extremity ulcers. Plast Reconstr Surg 2006;117:143S–149S;<br />
discussion 150S–151S.<br />
116. Falanga V, Margolis D, Alvarez O, et al. Rapid healing<br />
of venous ulcers and lack of clinical rejection with an<br />
allogeneic cultured human skin equivalent. Human Skin<br />
Equivalent Investigators Group. Arch Dermatol 1998;134:<br />
293–300.<br />
117. Goyal P, Puri GD, Pandey CK, Srivastva S. Evaluation of<br />
induction doses of propofol: comparison between endstage<br />
renal disease and normal renal function patients. Anaesth<br />
Intensive Care 2002;30:584–587.<br />
118. Reiber GE, Vileikyte L, Boyko EJ, et al. Causal pathways<br />
for incident lower-extremity ulcers in patients with diabetes<br />
from two settings. Diabetes Care 1999;22:157–162.<br />
119. Curtin CM, Gater DR, Chung KC. Autonomic dysreflexia:<br />
a plastic surgery primer. Ann Plast Surg 2003;51:325–329.<br />
120. Assadi F, Czech K, Palmisano JL. Autonomic dysreflexia<br />
manifested by severe hypertension. Med Sci Monit 2004;10:<br />
CS77–79.<br />
121. Adam S, Forrest S. ABC of intensive care: other supportive<br />
care. BMJ 1999;319:175–178.
178 A.M. Hanflik et al.<br />
122. Padberg J, Frank T, Johnston MV, Sisto SA. Structured<br />
exercise improves calf muscle pump function in chronic<br />
venous insufficiency: a randomized trial. J Vasc Surg 2004;<br />
39:79–87.<br />
123. Freedman G, Cean C, Duron V, Tarnovskaya A, Brem H.<br />
Pathogenesis and treatment of pain in patients with chronic<br />
wounds. Surg Technol Int 2003;11:168–179.<br />
124. Freedman G, Entero H, Brem H. Practical treatment of<br />
pain in patients with chronic wounds: pathogenesis-guided<br />
management. Am J Surg 2004;188:31–35.<br />
125. World Health Organization. Cancer pain relief. Geneva:<br />
World Health Organization; 1996.<br />
126. Scott EM, Leaper DJ, Clark M, Kelly PJ. Effects of warming<br />
therapy on pressure ulcers—a randomized trial. AORN J<br />
2001;73:921–927, 929–933, 936–938.<br />
127. Aronovitch S. Hospital acquired pressure ulcers: a comparison<br />
of costs in medical versus surgical patients, 1–18<br />
First Annual OR-Acquired Pressure Ulcer Symposium.<br />
Atlanta, GA, 1998.<br />
128. Scott EM, Buckland R. Pressure ulcer risk in the perioperative<br />
environment. Nurs Stand 2005;20:74, 76, 78<br />
passim.<br />
129. Hoshowsky VM, Schramm CA. Intraoperative pressure<br />
sore prevention: an analysis of bedding materials. Res Nurs<br />
Health 1994;17:333–339.<br />
130. Schoonhoven L, Defloor T, Grypdonck MH. Incidence of<br />
pressure ulcers due to surgery. J Clin Nurs 2002;11:479–487.<br />
131. De Keyser G, Dejaeger E, De Meyst H, Eders GC.<br />
Pressure-reducing effects of heel protectors. Adv Wound<br />
Care 1994;7:30–32, 34.
Part III<br />
Anesthetic Management of the Aged<br />
Surgical Candidate
13<br />
Preoperative Risk Stratification and<br />
Methods to Reduce Risk<br />
Linda L. Liu and Jacqueline M. Leung<br />
Aging increases the likelihood that a patient will have an<br />
operative procedure. Approximately 12% of those aged<br />
45 to 60 years are operated on each year, and this number<br />
will increase to more than 21% by the year 2025. 1 Whereas<br />
operations performed on patients older than 50 years of<br />
age were contraindicated in the past, an increasingly<br />
larger number of elderly patients are undergoing surgery<br />
at present. Studies of perioperative outcomes in the<br />
elderly have shown a decline in perioperative mortality<br />
rate from 20% in the 1960s 2 to 10% in the 1970s 3 to 5%–<br />
8% in the 1980s. 4 <strong>The</strong>se relatively low mortality rates<br />
have been attributed to improvement in anesthetic and<br />
surgical care. 5 As a result, many patients, including those<br />
who are elderly, do quite well after surgery and have<br />
improved quality of life as a result of their surgery.<br />
In contrast to the immediate fatal postoperative complications,<br />
which are infrequent, more common occurrences<br />
are complications, which result in morbidity<br />
instead of mortality. As discussed in the previous chapters,<br />
age-related changes occur in most organ systems.<br />
Under normal conditions, the physiologic changes that<br />
occur with aging usually lead to minimal functional<br />
impairment. With an acute disease or a surgical procedure,<br />
however, the elderly may be more prone to complications<br />
given their diminished reserve capacity, their<br />
decreased ability to respond to stress, and pathologic<br />
changes resulting from their coexisting disease. Recent<br />
studies suggest that surgical risk increases as a result of<br />
this increased prevalence of comorbid disease and/or<br />
decreased physiologic reserve rather than simply as a<br />
result of increased age alone. 6,7<br />
<strong>The</strong> increasing number of elderly patients presenting<br />
for surgery will have a tremendous impact on anesthesia<br />
practice. As an example, in 1980, one million postoperative<br />
complications involving the cardiac system alone<br />
occurred, leading to an estimated $20 billion in annual<br />
costs from in-hospital and long-term care. 8 A critical component<br />
of the perioperative care of elderly patients is to<br />
identify and modify preoperative risk in order to decrease<br />
postoperative morbidity and mortality. This chapter will<br />
discuss how to perform risk stratification of elderly<br />
patients awaiting major surgery and to determine methods<br />
to reduce perioperative morbidity and mortality using an<br />
evidence-based approach.<br />
<strong>The</strong> Importance of Coexisting Disease<br />
Several previous studies have examined risk predictors<br />
of postoperative morbidity and mortality after major<br />
surgery and anesthesia. <strong>The</strong> majority of the studies agree<br />
that the most consistent risk predictor identified is the<br />
presence of coexisting disease. For example, Tiret et al. 9<br />
determined that ASA PS classification (American Society<br />
of Anesthesiologists physical status), age, surgical procedure<br />
(major versus minor), and type (elective versus<br />
emergency) were significant predictors. Pedersen et al. 10<br />
found similar predictors of risk, which included age,<br />
history of congestive heart failure, renal disease, emergency<br />
surgery, and the type of surgery to be performed.<br />
Rorbaek-Madsen et al. 11 studied 594 octogenarians<br />
undergoing surgery in Denmark. Mortality rates in this<br />
study ranged from 0% in those with no complicating<br />
coexisting disease undergoing elective surgery to 21% in<br />
those with coexisting disease who were undergoing emergency<br />
surgery. Bufalari et al. 12 found only the ASA PS,<br />
presence of two associated diseases, and laparotomy procedures<br />
to be predictors of risk in surgical octogenarians<br />
in Italy from 1989 to 1993. <strong>The</strong> combined results from our<br />
two previous studies in patients aged ≥80 years and those<br />
≥70 years confirmed that the severity of preoperative<br />
comorbidities is a more important predictor of postoperative<br />
adverse outcomes than even intraoperative<br />
factors. 6,7<br />
Given the important impact of coexisting disease on<br />
anesthetic outcome, it should be noted that comorbid conditions<br />
are prevalent in elderly patients. Vaz and Seymour 13<br />
prospectively studied 288 general surgical patients aged<br />
181
182 L.L. Liu and J.M. Leung<br />
65 years and older, and found a high prevalence of preexisting<br />
health problems in their cohort. Overall, 30% of the<br />
patients had three or more preoperative medical problems,<br />
involving pulmonary disease, a history of congestive<br />
heart failure, angina, and prior cerebrovascular accidents.<br />
In a consecutive cohort of patients ≥70 years of age undergoing<br />
noncardiac surgery, we similarly found that nearly<br />
30% of patients had three or more comorbid conditions<br />
including a history of hypertension, cardiopulmonary<br />
disease, and neurologic disease. 6,7 In a study of a cohort of<br />
centenarians presenting for surgery, Warner et al. 14 found<br />
that nearly all of these very old patients had one or more<br />
pre-existing medical conditions.<br />
Because mortality and morbidity rates are more<br />
affected by coexisting disease as opposed to age alone,<br />
efforts should be made to optimize any coexisting disease,<br />
if possible, before surgery. <strong>The</strong> remainder of this chapter<br />
will present evidence-based data addressing which of the<br />
coexisting diseases can be modified to reduce the likelihood<br />
of perioperative morbidity and mortality. However,<br />
for geriatric patients, postponing surgery to optimize any<br />
medical conditions must be weighed against the risk of<br />
delaying surgery because emergency surgical treatment<br />
is associated with higher morbidity and mortality. Certain<br />
surgical procedures, such as cancer surgery, may substantially<br />
alter the prognosis of the patients if delayed. As a<br />
result, good communication among the anesthesiologists,<br />
surgeons, and primary care physicians is critical to developing<br />
an optimal plan as to when a geriatric patient<br />
should be scheduled for the planned surgery.<br />
Cognitive Dysfunction and Delirium<br />
after Noncardiac Surgery<br />
One of the most common postoperative outcomes is an<br />
adverse event involving the neurologic system, with postoperative<br />
delirium and cognitive decline being the two<br />
most frequently occurring events in geriatric patients.<br />
Our previous retrospective cohort study in surgical octogenarians<br />
demonstrated that postoperative neurologic<br />
complications occurred in 15% of the patients, of which<br />
91% were related to the occurrence of postoperative<br />
delirium. 6 Delirium is an acute disorder of attention and<br />
cognition and a serious problem for hospitalized geriatric<br />
patients. In contrast, cognitive dysfunction includes a<br />
wider range of neuropsychologic changes in several functional<br />
domains, and is often more subtle than delirium. It<br />
requires a different methodology for ascertainment and<br />
is frequently underestimated by health care professionals.<br />
A multinational study reported that postoperative cognitive<br />
dysfunction (POCD) was present in 26% of patients<br />
1 week after surgery and in 10% of patients even 3 months<br />
after surgery. 15<br />
In the surgical setting, as demonstrated by our previous<br />
work 6,7 and work from others, postoperative delirium is<br />
common in elderly surgical patients. 16 In one study, 36%<br />
of elderly patients undergoing surgery for hip fracture<br />
under a variety of anesthetic agents were “confused” on<br />
the first postoperative day. 17 Patients who developed<br />
delirium required a hospital stay approximately four<br />
times longer than those who remained lucid. 18 More<br />
importantly, delirium resulted in increased rates of<br />
nursing home placement, and associated hospital mortality<br />
rates of 10%–65%. 19 Numerous risk factors for delirium<br />
in medical patients have been previously identified.<br />
<strong>The</strong>y include the use of physical restraints, malnutrition,<br />
use of a bladder catheter, any iatrogenic event, and the<br />
use of more than three medications. 20–22<br />
In the perioperative setting, limited data exist as to<br />
whether specific intraoperative management precipitates<br />
POCD or delirium. <strong>The</strong> main areas that deserve consideration<br />
include:<br />
1. Drugs: Although previous studies have demonstrated<br />
that certain drugs may be associated with postoperative<br />
delirium, 23 there has been no prospective<br />
randomized clinical trials to determine if the elimination<br />
of certain drugs used in the perioperative period will<br />
actually lead to a lowering of the incidence of delirium.<br />
As a result, no definitive guidelines can be provided at<br />
present regarding avoiding certain drugs in the perioperative<br />
period. However, a sensible guideline is that<br />
“polypharmacy” is best avoided in elderly patients<br />
because delirium has been shown to be related to the<br />
number of medications prescribed. 22,23<br />
2. Anesthetic techniques: Controversy persists as to<br />
whether any anesthetic technique (regional versus general)<br />
has an impact on postoperative neurologic dysfunction.<br />
Earlier studies suggested an association between a<br />
higher incidence of cognitive dysfunction and general<br />
anesthesia relative to epidural anesthesia. 18,24 More recent<br />
studies, in contrast, have concluded that there is no relationship<br />
between anesthetic technique and the magnitude<br />
or pattern of POCD. 25 In a study by Moller et al., 15<br />
only the duration of anesthesia was found to be one of<br />
the risk factors for early POCD. A retrospective cohort<br />
study of consecutive hip fracture patients, aged ≥60 years,<br />
undergoing surgical repair at 20 United States hospitals<br />
also found that the anesthesia technique (regional versus<br />
general) had no impact on postoperative mental status<br />
change. 26 More recently, a multicenter trial of patients<br />
≥60 years of age, although not adequately powered,<br />
reported that the incidence of cognitive dysfunction at 3<br />
months after surgery was not different after either general<br />
or regional anesthesia. 27<br />
3. Anesthetic management: Specifically, is the role of<br />
blood pressure or intraoperative hypotension associated<br />
with POCD? In a prospective, randomized study of older
13. Preoperative Risk Stratification and Methods to Reduce Risk 183<br />
adults (age >50 years) undergoing total hip replacement,<br />
Williams-Russo et al. 28 demonstrated that patients who<br />
underwent epidural anesthesia and were rendered markedly<br />
hypotensive had similar incidence of POCD as those<br />
who were maintained in the normotensive state. Moller<br />
et al., 15 by a larger cohort study, also determined that<br />
neither hypotension nor hypoxemia were related to<br />
POCD.<br />
4. Postoperative pain management: In one study of<br />
older patients undergoing major elective noncardiac<br />
operations, 29 after adjusting for known preoperative risk<br />
factors for delirium, higher pain scores at rest were associated<br />
with a slightly increased risk of delirium in the first<br />
three postoperative days. It remains to be proven whether<br />
better control of postoperative pain will reduce POCD.<br />
Despite the importance and prevalence of postoperative<br />
neurologic decline, no single anesthetic technique<br />
has been identified to be superior for elderly surgical<br />
patients in minimizing POCD or delirium. Until more<br />
definitive clinical studies become available, minimizing<br />
the number of medications used, avoiding hypoxemia<br />
and hypercarbia, and providing adequate postoperative<br />
pain control seem to be the best approaches in minimizing<br />
the occurrence of postoperative delirium in geriatric<br />
surgical patients.<br />
Cardiovascular Complications<br />
<strong>The</strong> elderly are more likely to develop postoperative cardiovascular<br />
complications. Pedersen et al. 30 presented<br />
data on 7306 patients undergoing surgery in Denmark.<br />
<strong>The</strong> octogenarians had a 16.7% incidence of cardiovascular<br />
complications compared with a 2.6% incidence in<br />
patients younger than 50 years of age. <strong>The</strong> cardiovascu -<br />
lar complications in this study were defined as systolic<br />
hypotension or hypertension (systolic blood pressures<br />
200 mm Hg, respectively), cardiac arrest,<br />
second- or third-degree heart block, chest pain, ventricular<br />
tachyarrhythmias, supraventricular tachycardia<br />
requiring treatment, myocardial infarction, or congestive<br />
heart failure. A high incidence of cardiovascular complications<br />
(40%) was found in patients with preoperative<br />
heart disease, especially in those with clinical signs of<br />
congestive heart failure, history of ischemic heart disease,<br />
or previous myocardial infarction. In two separate cohort<br />
studies of nearly 1000 patients older than 70 and 80 years<br />
of age undergoing noncardiac surgery, respectively, we<br />
found a similar cardiovascular complication rate of 10%–<br />
12%. 6,7 <strong>The</strong> most common postoperative cardiovascular<br />
events in these two separate cohorts were congestive<br />
heart failure, arrhythmias, and ischemic complications. In<br />
contrast to the Pedersen study, in which the severity of<br />
the operative case and elective versus emergent surgery<br />
Table 13-1. Comparison between cardiac risk indexes developed<br />
by Goldman and Lee.<br />
Goldman<br />
• Preoperative S 3 or JVD<br />
• Myocardial infarction within<br />
6 months<br />
• PVC >5 bpm<br />
• Rhythm other than sinus or<br />
presence of PACs<br />
• Age >70 years<br />
• Intraperitoneal, intrathoracic, or<br />
aortic operations<br />
• Emergency surgery<br />
• Important valvular aortic stenosis<br />
• Poor general medical condition<br />
Lee<br />
• High-risk type of surgery<br />
• Ischemic heart disease<br />
• History of congestive heart<br />
failure<br />
• History of cerebrovascular<br />
disease<br />
• Insulin therapy for diabetes<br />
• Preoperative serum creatinine<br />
>2 mg/dL<br />
Source: Data from Goldman et al. 31 and Lee et al. 32<br />
JVD = jugular venous distention, PVC = premature ventricular contractions,<br />
PAC = premature atrial contractions.<br />
were associated with the occurrence of cardiovascular<br />
complications, we found that intraoperative variables<br />
such as type of anesthesia and surgical procedure did not<br />
increase postoperative cardiovascular complications.<br />
What are the characteristics of patients who develop<br />
postoperative complications? Many previous investigations<br />
have focused on clinical variables and diagnostic<br />
test procedures obtained preoperatively to identify<br />
patients at risk for postoperative complications. For<br />
example, a cardiac risk index was developed by Goldman<br />
et al. in 1977 31 and subsequently revised in 1999 32 to<br />
predict the occurrence of postoperative cardiac complications<br />
(Table 13-1). In this latter revised cardiac index, 32<br />
variables that were associated with increased risk of postoperative<br />
cardiac complications included high-risk<br />
surgery, history of ischemic heart disease, congestive<br />
heart failure, or cerebrovascular disease, preoperative<br />
treatment of diabetes with insulin, and preoperative creatinine<br />
>2.0 mg/dL. Rates of major cardiac complication<br />
with 0, 1, 2, or ≥3 of the factors were 0.5%, 1.3%, 4%, and<br />
9%, respectively.<br />
<strong>The</strong> American College of Cardiology/American Heart<br />
Association (ACC/AHA) Task Force recently updated<br />
the guidelines for preoperative cardiac evaluation for<br />
patients presenting for noncardiac surgery 33 in an attempt<br />
to unify the risk stratification process. Although these<br />
guidelines are based on studies performed in the general<br />
surgical population and do not specifically target the geriatric<br />
population, some of the general principles are applicable.<br />
<strong>The</strong> main decision points of the guidelines are<br />
based on the patient’s medical conditions, functional<br />
capacity, and the acuity and risk of the planned surgical<br />
procedure.<br />
<strong>The</strong> first step is to stratify the patient by medical condition.<br />
Table 13-2 lists the minor, intermediate, and major
184 L.L. Liu and J.M. Leung<br />
clinical predictors as defined by the ACC/AHA guidelines.<br />
Advanced age, by itself, is considered only one of<br />
the minor clinical predictors. However, it should be noted<br />
that advanced age is associated with increased incidence<br />
of comorbid conditions, which may be intermediate predictors<br />
of postoperative cardiovascular complications.<br />
Diseases such as diabetes mellitus, renal insufficiency, and<br />
compensated congestive heart failure, are more likely to<br />
occur in the older population. Major predictors are unstable<br />
coronary syndromes, decompensated congestive heart<br />
failure, significant arrhythmias, and severe valvular<br />
disease.<br />
<strong>The</strong> next area of focus in the guideline is the assessment<br />
of functional capacity. According to the ACC/AHA<br />
guidelines, the inability to perform activities beyond four<br />
metabolic equivalents (METs) requires further evaluation.<br />
A summary of how to evaluate METs is provided in<br />
Table 13-3. However, the accurate assessment of functional<br />
capacity may be difficult in the geriatric population<br />
because many elderly patients may have comorbid conditions<br />
or chronic pain, which limits their functional capacity.<br />
As a result, the functional limitation may be secondary<br />
to noncardiac causes, rather than attributable to a primary<br />
cardiac cause as the guideline would suggest. <strong>The</strong>refore,<br />
direct adoption of the ACC/AHA algorithm without<br />
knowing the reason for the functional limitation may<br />
result in a great majority of elderly patients needing additional<br />
preoperative cardiac stress testing.<br />
<strong>The</strong> ACC/AHA guidelines also take into account the<br />
operative procedure itself, which has an impact on the<br />
occurrence of cardiac morbidity and mortality. Emergency<br />
major operations, major vascular surgery, and any<br />
prolonged surgical procedures associated with large fluid<br />
shifts are stratified as procedures carrying higher cardiac<br />
Table 13-2. Major, intermediate, and minor predictors of cardiovascular<br />
risk.<br />
Predictors<br />
Major<br />
Intermediate<br />
Minor<br />
Source: Data adapted from Eagle et al. 33<br />
Unstable coronary syndromes<br />
Decompensated heart failure<br />
Significant arrhythmias<br />
Significant valvular disease<br />
Stable angina pectoris<br />
History of myocardial infarction<br />
Compensated heart failure<br />
Diabetes<br />
Renal insufficiency<br />
Advanced age<br />
Abnormal electrocardiogram<br />
Rhythm other than sinus<br />
Poor exercise capacity<br />
History of cerebrovascular accident<br />
Uncontrolled hypertension<br />
Table 13-3. Estimate of metabolic equivalent for different<br />
activities.<br />
MET estimate<br />
Activity<br />
1 MET Activities of daily living<br />
Eating<br />
Dressing<br />
Walking indoors (2–3 mph)<br />
Dishwashing<br />
4 MET More strenuous activities<br />
Climbing stairs (1 flight)<br />
Walking (4 mph)<br />
Running short distance<br />
Scrubbing floors<br />
Playing golf, doubles tennis<br />
10 MET Playing sports<br />
Swimming<br />
Singles tennis<br />
Football<br />
Source: Data adapted from Eagle et al. 33<br />
MET = metabolic equivalent.<br />
risk. More minor surgeries such as cataract removal are<br />
deemed to be of low surgical risk. Taken together, the<br />
results of the medical history, current symptoms, and<br />
physical examination allow the physician to identify<br />
clinical predictors of increased perioperative cardiovascular<br />
risk. <strong>The</strong> clinical predictors, combined with an<br />
assessment of the patient’s exercise tolerance and the<br />
risk of surgery, then provides additional guidance to the<br />
clinicians in determining the value of additional cardiac<br />
stress testing.<br />
Strategies to Reduce Cardiac Risk<br />
<strong>The</strong> basis of performing preoperative cardiac risk stratification<br />
assumes the possibility that some or all of these<br />
risk factors identified may be modifiable with the ultimate<br />
goal of improving patients’ outcomes. However, this<br />
assumption has not been completely proven. Eagle et al. 34<br />
determined that the risk of coronary artery bypass graft<br />
(CABG) surgery itself, when added to the risk of the<br />
noncardiac surgery, often exceeded the risk of the same<br />
surgery in patients who have not undergone CABG<br />
surgery. <strong>The</strong>y showed that performance of CABG surgery<br />
before the planned noncardiac surgery may not be justified.<br />
In other words, it seems that for some of the patients,<br />
the risk of modifying their perioperative myocardial<br />
infarction risk by cardiac surgery may actually outweigh<br />
the benefits because of the risk of cardiac surgery itself. 34<br />
In fact, a recent randomized multicenter trial in 510 male<br />
veterans scheduled for vascular operations demonstrates<br />
that coronary artery revascularization before elective<br />
vascular surgery does not significantly alter the long-term<br />
outcome. 35 As a result, a reexamination and further inves-
13. Preoperative Risk Stratification and Methods to Reduce Risk 185<br />
tigation of the appropriateness of the 2002 ACC/AHA<br />
guidelines for preoperative cardiac evaluation for elderly<br />
patients needs to be conducted.<br />
Despite the varied nature of each study patient population,<br />
congestive heart failure (CHF) continues to be identified<br />
as a major predictor of surgical outcomes. In a<br />
prospective study of octogenarians, clinical signs of congestive<br />
heart failure increased the odds of an adverse<br />
cardiac event (odds ratio = 2.1, confidence interval =<br />
1.1–5.1). 7 <strong>The</strong> strong association between clinical signs<br />
of CHF and postoperative complications emphasizes<br />
the importance of preoperative optimization of heart<br />
function in the elective surgical patient. <strong>The</strong> adequacy<br />
and accuracy of preoperative assessment of heart function<br />
seems to be a critical area deserving further<br />
investigation.<br />
For the elderly patient, heart failure can often be<br />
caused by diastolic dysfunction associated with left ventricular<br />
hypertrophy. Older patients with CHF frequently<br />
present with normal left ventricular ejection fraction, suggesting<br />
the importance of diastolic dysfunction in this age<br />
group. 36 In fact, up to one third of patients with heart<br />
failure may have normal systolic function. 37 Other causes<br />
of diastolic dysfunction may include myocardial ischemia,<br />
accelerated hypertension, or intrinsic myocardial diseases<br />
such as fibrosis. 38 Unfortunately, this diagnosis may not<br />
be readily apparent preoperatively and the therapeutic<br />
approach is different. 39 <strong>The</strong> prognostic significance of diastolic<br />
function assessment, such as with preoperative<br />
Doppler echocardiography in patients with a history of<br />
heart failure remains to be determined. More studies are<br />
needed to better characterize diastolic function including<br />
defining normality in older patients before recommendations<br />
for preoperative care can be made.<br />
<strong>The</strong> association between hypertension and end organ<br />
damage, such as ischemic heart disease, heart failure,<br />
cerebrovascular disease, and renal impairment, has been<br />
well established, 40,41 but in assessing perioperative risk,<br />
hypertension has not been recognized as a major predictor<br />
of perioperative cardiac risk. 31,32 Patients diagnosed<br />
with hypertension have increased systemic vascular resistance<br />
and cardiovascular lability during anesthesia. 42,43<br />
Reich et al. 44 reported an association between intraoperative<br />
hypertension and tachycardia and adverse outcome<br />
in protracted surgery, but a direct causal relationship<br />
between hypertension and perioperative adverse cardiac<br />
outcomes is not as evident. In a meta-analysis of 30<br />
studies, the risk of perioperative cardiovascular complications<br />
in hypertensive patients was only slightly increased<br />
(odds ratio = 1.35, confidence interval = 1.17–1.56) and<br />
the authors advised cautious interpretation of the data<br />
because of the heterogeneity of the observational<br />
studies. 45<br />
To date, there is no evidence to support the approach<br />
of deferring elective surgery to allow hypertension to be<br />
treated in order to reduce perioperative risk. 45 <strong>The</strong> ACC/<br />
AHA guidelines state that mild/moderate hypertension<br />
is not an independent risk factor for perioperative cardiovascular<br />
complications, but severe hypertension (systolic<br />
blood pressure ≥180 mm Hg and/or diastolic blood<br />
pressure ≥110 mm Hg) should be controlled before<br />
surgery. 33 Unfortunately, there are no data to suggest that<br />
this strategy reduces perioperative risk. In a meta-analysis<br />
report, Howell et al. 41 have suggested that surgery may<br />
proceed, but care should be taken to ensure perioperative<br />
cardiovascular stability, invasive arterial pressure monitoring<br />
should be started, and mean arterial blood pressure<br />
should be kept within 20% of baseline. In patients<br />
with severe hypertension and evidence of end organ<br />
damage, Howell et al. did suggest that it would be appropriate<br />
to defer surgery when possible, but this suggestion<br />
is based on evidence from medical patients, not from data<br />
in surgical patients.<br />
In patients without contraindications, the use of perioperative<br />
beta-blockade may be of value in controlling<br />
blood pressure and also reducing perioperative myocardial<br />
ischemia. Several clinical trials have examined the<br />
potential beneficial effects of using beta-adrenergic<br />
blocking agents to improve perioperative surgical outcomes.<br />
46,47 None, however, has directly focused on geriatric<br />
patients. <strong>The</strong> mechanism of beta-adrenergic blockade<br />
in prophylaxis of perioperative ischemia and postoperative<br />
cardiac events is probably multifactorial. Proposed<br />
mechanisms include decreased myocardial demand from<br />
a reduction in the inotropic and chronotropic state of the<br />
myocardium, and possible improved perfusion to ischemic<br />
regions from redistribution of myocardial blood<br />
flow. Because perioperative tachycardia increases myocardial<br />
oxygen demand and has been shown to be associated<br />
with myocardial ischemia, 48 the adequacy of the<br />
heart rate response to beta-blockers should be a critical<br />
guide to the dosing of the drug.<br />
<strong>The</strong> hemodynamic effects of beta-blockers depend on<br />
the patient’s cardiovascular status, underlying sympathetic<br />
tone, concurrent anesthesia, and vasoactive drug<br />
therapy. <strong>The</strong> decreased response to beta receptor stimulation<br />
with aging, together with interaction with anesthetic<br />
agents, may increase the risk for hypotension in the<br />
setting of prophylactic beta-blockade. 49 In a study of 63<br />
elderly patients, Zaugg et al. 50 reported that perioperative<br />
beta-blockade actually resulted in better hemodynamic<br />
stability, decreased analgesic requirements, faster recovery<br />
from anesthesia, and decreased myocardial damage<br />
as diagnosed by increased levels of troponin I. This study<br />
is limited in size, but it is one of the first to suggest the<br />
relative safety and efficacy of beta-blockade in the<br />
elderly.<br />
Current practice seems to suggest that beta-blockers<br />
are underutilized in all patients, especially the elderly.<br />
In a retrospective study, only 30% of patients who met
186 L.L. Liu and J.M. Leung<br />
Table 13-4. Beta-blockers and suggested dosages used in the<br />
literature for perioperative myocardial protection.<br />
Drug name<br />
Atenolol<br />
Metoprolol<br />
Bisoprolol<br />
criteria for perioperative beta-blockade after cholecystectomy<br />
received therapy. 51 This number is even lower for<br />
eligible elderly patients. Gottlieb et al. 52 performed a<br />
chart review of more than 200,000 cases after myocardial<br />
infarction. <strong>The</strong>y determined that of the patients who<br />
should receive beta-blockade, only 27% of those 84 years<br />
old received beta-blockers versus 37% of those 60, impaired preoperative<br />
cognitive function, smoking history within the past 8<br />
weeks, body mass index, history of cancer, and abdominal<br />
incision site were independent risk factors for postoperative<br />
pulmonary complications.<br />
Of note, preoperative spirometry did not reliably<br />
predict the occurrence of postoperative complications<br />
in patients with obstructive lung disease. 60 In a study<br />
involving critically ill patients, the CO 2 levels on arterial<br />
blood gas and not spirometric testing predicted the<br />
need for postoperative intubation. 61 Taken together,<br />
the evidence to date suggests that pulmonary function<br />
tests should be selectively performed in patients undergoing<br />
nonthoracic surgery, because they can assess<br />
the presence and severity of the disease, but they do not<br />
have great predictive value for postoperative pulmonary<br />
complications.<br />
Strategies to Reduce Pulmonary Risk<br />
Preoperative optimization of respiratory function may<br />
improve patient outcomes. Several factors that deserve<br />
consideration include smoking cessation, optimization of<br />
asthma medications, and treatment of obstructive sleep<br />
apnea. Cigarette smoking is a known risk factor for<br />
COPD, coronary artery disease, and peripheral vascular<br />
disease. Current smokers are four times more likely to<br />
develop pulmonary complications than those who have<br />
never smoked. 62 Other trials have shown that smokers<br />
have a higher rate of wound infection than nonsmokers. 63<br />
<strong>The</strong> institution of a smoking intervention program 6–8<br />
weeks before joint replacement surgery reduced postoperative<br />
morbidity. 64 Warner et al. 65 showed that smoking<br />
cessation at least 2 months preoperatively maximized the<br />
reduction of postoperative respiratory complications.
13. Preoperative Risk Stratification and Methods to Reduce Risk 187<br />
From the above data, it seems that preoperative cessation<br />
of smoking will improve patient outcomes by decreasing<br />
adverse postoperative pulmonary outcomes and the incidence<br />
of wound infections. Smoking cessation should be<br />
encouraged even immediately before surgery, because<br />
smoking cessation has been associated with immediate<br />
decreases of carbon monoxide levels and reduced operative<br />
risk measured 6 weeks after surgery. 65<br />
Another condition common in geriatric patients is<br />
asthma. Asthma is often underdiagnosed in the elderly,<br />
and for those with the diagnosis, treatment may not<br />
be optimized. Asthma is often underdiagnosed in elderly<br />
for multiple reasons: (1) patient failure to report symptoms<br />
to the physician because of a lack of awareness of<br />
symptoms or misinterpreting the symptoms as deconditioning<br />
or normal process of aging; (2) presence of<br />
other conditions such as cardiac failure, ischemic cardiac<br />
failure, gastroesophageal reflux disease, respiratory tract<br />
tumors, laryngeal dysfunction, constrictive bronchiolitis,<br />
hypersensitive pneumonitis, or the use of medications<br />
(beta-blockers, angiotensin-converting enzyme inhibitors)<br />
that can mimic symptoms of asthma; (3) presence<br />
of other respiratory conditions such as COPD; or (4)<br />
general misperception that new-onset asthma is rare in<br />
the elderly. 66 With the appropriate diagnosis made, aggressive<br />
pulmonary rehabilitation, which includes exercise<br />
training, patient education, psychosocial, nutritional, and<br />
respiratory therapy counseling, smoking cessation, and<br />
optimization of medications, has been shown to be effective<br />
in the elderly population. 67 Unfortunately, some<br />
practitioners limit the use of beta agonists. <strong>The</strong>y fear that<br />
systemic absorption of inhaled medications may result<br />
in tachycardia and hypertension, and precipitate cardiac<br />
ischemia in patients with coronary artery disease or result<br />
in drug interactions that may prolong the QT interval.<br />
<strong>The</strong> use of beta agonists is relatively safe in the elderly.<br />
Some earlier studies reported a decreased therapeutic<br />
response to inhaled beta receptor agonist with increasing<br />
age, but a recent study did not find any difference in<br />
the response to albuterol or ipratropium bromide with<br />
respect to age. 68<br />
Another comorbidity that is increasing in prevalence<br />
in the elderly is obesity and obstructive sleep apnea syndrome<br />
(OSAS). <strong>The</strong> prevalence of obesity is increasing<br />
at an alarming rate. 69 <strong>The</strong> number of obese adults aged<br />
60 and older will increase from 32% in 2000 to 37.4% in<br />
2010. 70 This increase has been attributed to a complex<br />
interaction between age-associated alterations in the<br />
metabolic rate, dietary changes, and sedentary lifestyles.<br />
Obesity causes diabetes, hypertension, hyperlipidemia,<br />
sleep apnea, and arthritis, resulting in reduced quality of<br />
life and life expectancy. 71 No specific studies addressed<br />
the impact of OSAS on postoperative complications in<br />
the elderly. However, in patients undergoing hip or knee<br />
replacement, procedures typically performed in older<br />
individuals, those with a preoperative diagnosis of OSAS<br />
were more than two times more likely to develop complications<br />
than those without OSAS. In fact, serious complications<br />
occurred in 24% of the OSAS group versus 9%<br />
in the control group, and hospital stay was significantly<br />
longer in the OSAS group. 72<br />
<strong>The</strong> data regarding the perioperative risk and best<br />
management techniques for patients with OSAS are<br />
scant and virtually nonexistent for elderly patients with<br />
OSAS. A Clinical Practice Review Committee of the<br />
American Academy of Sleep Medicine was unable to<br />
develop a standard of practice recommendation. <strong>The</strong>y<br />
were only able to make a clinical practice statement<br />
based on a consensus of clinical experience and a few<br />
published peer-reviewed studies. <strong>The</strong>y stated that important<br />
components of the perioperative management of<br />
OSAS patients include a high degree of clinical suspicion,<br />
control of the airway throughout the perioperative period,<br />
judicious use of medications, and appropriate monitoring.<br />
73 At this point, this advice may be extrapolated to the<br />
elderly patient with OSAS. Other potentially prudent<br />
suggestions include having a lower threshold of admitting<br />
these patients to more intensive postoperative monitoring,<br />
use of supplemental oxygen, and use of nighttime<br />
continuous positive airway pressure.<br />
Renal Dysfunction<br />
<strong>The</strong> prevalence of renal insufficiency is quite common in<br />
the elderly because of a decrease in glomerular function<br />
with age. In populations ≥age 70, moderately or severely<br />
decreased glomerular filtration rate was observed in 75%<br />
of community-dwelling elderly, 78% of the patients from<br />
the geriatric ward, and 91% of nursing home patients. In<br />
populations ≥age 85, 99% had evidence of renal impairment<br />
necessitating dosing adjustments for drugs. 74 Kohli<br />
et al. 75 showed that surgery and nephrotoxic drugs are<br />
independent predictors of acute renal failure in elderly<br />
patients. <strong>The</strong>y also found that mortality in patients with<br />
acute renal failure was significantly higher than similar<br />
patients without acute renal failure. In fact, it is estimated<br />
that acute renal failure contributes to at least one of<br />
every five perioperative deaths in elderly surgical<br />
patients. 76 A history of postoperative renal complications<br />
is a significant predictor of decreased long-term survival. 77<br />
<strong>The</strong>re are no clinical trials demonstrating that preoperative<br />
assessment for renal dysfunction will lead to better<br />
outcomes. However, recognizing that elderly patients<br />
are at risk of developing renal complications as a<br />
result of decreased renal function, effect of nephrotoxic<br />
drugs (aminoglycosides, nonsteroidal antiinflammatory<br />
drugs, angiotensin-converting enzyme inhibitors, and<br />
contrast dye), volume depletion, and hypotension seems<br />
prudent.
188 L.L. Liu and J.M. Leung<br />
Diabetes Mellitus<br />
Internationally, adults over age 60 will comprise two<br />
thirds of the diabetic population in developed countries<br />
by the year 2025. 78 In the United States, because of<br />
improvements in the identification of chronic diseases,<br />
declining death rates, and people living longer, diabetes<br />
is also increasing among persons aged 60 and older. 79<br />
Currently, nearly one of every five adults in the United<br />
States over age 60 has diabetes, which puts them at<br />
increased risk for disability and morbidity. 80 Furthermore,<br />
the mortality risk is substantially higher in diabetics than<br />
nondiabetics. For example, McBean et al. 81 found that in<br />
individuals with diabetes, the overall risk of dying was 1.6<br />
times greater than those without diabetes in a retrospective<br />
analysis of a 5% random sample of Medicare fee-forservice<br />
beneficiaries. <strong>The</strong> duration of diabetes also has a<br />
significant impact on the rate of developing complications<br />
as evidenced by a study demonstrating that patients<br />
with more than 10 years of diabetes have more significant<br />
compromise in one or more end-organ systems. 82 Diabetes<br />
is considered an intermediate clinical predictor for<br />
risk of perioperative myocardial ischemia 33 and is associated<br />
with increased risk of complications and death after<br />
myocardial infarction.<br />
<strong>The</strong> recently published guidelines from the California<br />
Healthcare Foundation/American <strong>Geriatric</strong>s Society<br />
Panel on Improving Care for Elders with Diabetes provided<br />
recommendations on diabetes management for the<br />
elderly. <strong>The</strong>se guidelines suggested that elderly persons<br />
in otherwise good health should have the same glycemic<br />
control goals as younger persons, which is a standard<br />
hemoglobin A1c target of
13. Preoperative Risk Stratification and Methods to Reduce Risk 189<br />
identified preoperative albumin level as a good predictor<br />
of postoperative mortality in the geriatric population. 94<br />
<strong>The</strong> National Veterans Administration Surgical Risk<br />
Study examined 43 preoperative risk factors, 14 preoperative<br />
laboratory values, and 12 operative variables for<br />
predicting postoperative complications. <strong>The</strong> mean age in<br />
this study was 61 ± 13 years, and 97% of the subjects were<br />
men, but the results should apply to the general elderly<br />
surgical patient. <strong>The</strong> most important variable in predicting<br />
postoperative mortality was preoperative albumin<br />
level with ASA PS classification as the second best predictor.<br />
Albumin levels
190 L.L. Liu and J.M. Leung<br />
Table 13-7. Instrumental activities of daily living.<br />
Instrumental activity<br />
Definition of independence<br />
Telephone<br />
Shopping<br />
Food preparation<br />
Housekeeping<br />
Laundry<br />
Mode of transportation<br />
Responsible for medications<br />
Handles finances<br />
medications, and ability to handle finances. Functional<br />
status before hospitalization has been found to be predictive<br />
of functional outcome, length of stay, mortality, and<br />
need for nursing home placement. Davis et al. 110 showed<br />
that ADL impairment was a powerful predictor of inhospital<br />
mortality for the elderly and it was the single<br />
most important predictor of functional outcomes at 2 and<br />
12 months after hospitalization.<br />
A preoperative home-based physical therapy program,<br />
prehabilitation, has been described as a method of<br />
enhancing the functional capacity of a patient. It has been<br />
evaluated in frail, community-dwelling elders 111 and in<br />
preparation for the stress of an orthopedic surgical procedure<br />
112 or an intensive care unit admission. 113 <strong>The</strong> goals<br />
of prehabilitation are to prevent deconditioning and<br />
improve the ability of the patient to withstand musculoskeletal<br />
and cardiovascular stressors of surgery. <strong>The</strong> efficacy<br />
of this type of approach remains to be validated by<br />
randomized controlled trials before prehabilitation can<br />
be recommended as a routine preoperative strategy in<br />
elderly patients.<br />
Laboratory Values<br />
Able to use telephone; able to dial a<br />
few well-known numbers; able to<br />
answer the telephone<br />
Takes care of all shopping needs<br />
Plans, prepares, serves adequate meals<br />
Performs light daily tasks, washes<br />
dishes, makes bed<br />
Does laundry<br />
Travels by driving, or using public<br />
transportation alone or<br />
accompanied by another<br />
Takes correct dosages at correct time<br />
Manages day-to-day finances, can<br />
require assistance with banking or<br />
major purchases<br />
Routine preoperative medical testing before elective<br />
surgery is estimated to cost $30 billion annually, but data<br />
show that laboratory abnormalities on routine screen<br />
often do not lead to changes in management. Schein et<br />
al. 114 studied nearly 20,000 patients undergoing cataract<br />
surgery who were randomized to either routine laboratory<br />
testing or no routine testing. <strong>The</strong>y reported no difference<br />
in perioperative morbidity and mortality between<br />
those who did versus those who did not receive routine<br />
testing. In patients with few comorbidities, there is a low<br />
prevalence of abnormal laboratory tests. For example, in<br />
a population study of 7196 ambulatory patients, the prevalence<br />
of hemoglobin, glucose, and creatinine abnormalities<br />
was small (5.5%, 8.3%, and 2.7%, respectively). 115<br />
In contrast, a substantially higher prevalence of abnormal<br />
results was demonstrated in a group of institutionalized<br />
elderly patients (11%–33% for hemoglobin, 25%–29%<br />
for glucose, and 11%–15% for creatinine). 116–118 Dzankic<br />
et al. 119 used a prospective cohort of patients ≥70 years of<br />
age undergoing elective noncardiac surgery to evaluate<br />
the prevalence and predictive value of abnormal preoperative<br />
laboratory tests. <strong>The</strong> prevalence of abnormal laboratory<br />
tests was quite high—electrolyte abnormalities<br />
(0.7%–5%), abnormal platelet counts (1.9%), glucose<br />
(7%), hemoglobin (10%), and abnormal creatinine<br />
(12%)—but in a separate analysis for patients classified<br />
as ASA 1–2, the incidence of laboratory abnormalities<br />
was as low as those in the general population (3.6%). In<br />
fact, in the entire elderly cohort, none of the abnormal<br />
laboratory values were significant independent predictors<br />
of adverse outcomes with multivariate regression.<br />
<strong>The</strong>se results suggest that routine preoperative testing in<br />
geriatric surgical patients, particularly in those patients<br />
classified as ASA 1–2, generally produces few abnormal<br />
results.<br />
Electrocardiogram (ECG) abnormalities also increase<br />
with age. 120 <strong>The</strong> most common abnormalities in a cohort<br />
of octogenarians 121 included arrhythmias, Q waves diagnosing<br />
previous myocardial infarction, left ventricular<br />
hypertrophy, bundle-branch block, and nonspecific<br />
segment changes. Although these abnormalities are<br />
common, they had limited value in predicting postoperative<br />
cardiac complications. <strong>The</strong>re is no demonstrable evidence<br />
that measurement and investigation of preoperative<br />
ECGs reduce adverse outcomes, but current recommendations<br />
to obtain preoperative ECGs for men over age<br />
40, women over age 50, and other patients with known<br />
coronary artery disease or cardiovascular risk factors<br />
such as diabetes or hypertension, are probably reasonable<br />
so that a baseline ECG is available before major<br />
surgery to determine whether subsequent abnormalities<br />
are new or preexistent. 122<br />
Preoperative chest X-rays (CXRs) have increased clinical<br />
relevance with increasing age and presence of cardiopulmonary<br />
disease. 123,124 In patients younger than age 50,<br />
the likelihood of an abnormal chest film ranges from 0%<br />
to 20%, whereas the likelihood increases to 20% to 60%<br />
in patients older than 50. 125 An evaluation of routine<br />
preoperative CXRs in vascular surgery patients demonstrated<br />
that no surgery cancellations occurred because of<br />
an abnormal X-ray, but the beneficial effects of a CXR<br />
increased in patients with known pulmonary disease. <strong>The</strong><br />
study recommended that CXRs be ordered preoperatively<br />
only if there is clinical indication in the history and<br />
physical examination. 126<br />
<strong>The</strong>re are no controlled clinical trials to show that<br />
routine laboratory tests, ECG or CXR, are associated
13. Preoperative Risk Stratification and Methods to Reduce Risk 191<br />
with a decreased adverse event rate. However, information<br />
from preoperative ECG and/or CXR may be of<br />
value in the postoperative management because new<br />
abnormalities may be identified if preoperative baseline<br />
measurements are available. Although the actual rate of<br />
laboratory abnormalities is small in the elderly, it is still<br />
higher compared with the younger population. 127 <strong>The</strong>refore,<br />
total abandonment of routine testing based on age<br />
must be weighed against the probability that unexpected<br />
disease may be detected by the testing and that the extent<br />
of surgery may be modified. 128<br />
Medications<br />
Elderly patients frequently take multiple medications,<br />
both prescription and over-the-counter medications. <strong>The</strong><br />
elderly constitute approximately 13% of the population<br />
but consume 32% of all prescription drugs in the United<br />
States. 129 Studies show that greater consumption of medications<br />
contributes to decreased medication adherence 130<br />
and to greater risk of adverse drug events. 131 <strong>The</strong> impact<br />
of common herbal and alternative medicines is unclear,<br />
but is already becoming an important focus. In a survey<br />
of more than 2500 preoperative patients ≥age 18, almost<br />
40% of the patients admitted to using some form of alternative<br />
medicine supplements. 132 Women ≥age 65 reported<br />
using an average of 2.6 herbal products. 133 Most important<br />
was the fact that more than 50% of the patients in<br />
the study indicated that they did not inform the anesthesiologists<br />
before surgery regarding their use of these<br />
products. 132 <strong>The</strong> Food and Drug Administration does not<br />
control these supplements and, therefore, quality is not<br />
rigorously regulated. Some reported side effects from<br />
herbal remedies include bleeding when warfarin is combined<br />
with ginkgo, garlic, or ginseng 134 ; possible monoamine<br />
oxidase inhibition by St. John’s wort 135 ; coma when<br />
benzodiazepines are combined with kava 136 ; and mania<br />
when antidepressants are combined with ginseng. 134<br />
Other reported risks include contamination, inconsistencies<br />
and adulteration, and lead poisoning. 137 <strong>The</strong>re are<br />
no randomized controlled trials to examine the effects<br />
of herbal medications in the perioperative period and<br />
to determine when the supplements should be stopped<br />
preoperatively. A few review articles made several suggestions<br />
(stopping ephedra, ginkgo, and kava 24–36 hours<br />
before surgery, and stopping garlic, ginseng, and St. John’s<br />
wort 5–7 days before surgery) based on limited information<br />
on the pharmacokinetics of these agents 138,139<br />
(Table 13-8).<br />
In terms of prescription medications, the older patient<br />
is at risk for inappropriate drug use. Inappropriate medications<br />
may be defined as drugs that pose more risk than<br />
benefit. 140 In 1996, more than 20% of community-dwelling<br />
elderly received some inappropriate medication. 141<br />
Table 13-8. Recommendations for preoperative discontinuation<br />
of herbal medications.<br />
Discontinue<br />
Herbal medicine Perioperative interactions before surgery<br />
Echinacea • Allergic reactions No data<br />
• Immunosuppression<br />
Ephedra • Hypertension 24 hours<br />
• Arrhythmias<br />
Garlic • Inhibits platelet aggregation 7 days<br />
• Increases risk of bleeding<br />
Ginkgo • Inhibits platelet aggregation 36 hours<br />
• Increases risk of bleeding<br />
Ginseng • Hypoglycemia 7 days<br />
• Increases risk of bleeding<br />
Kava • Interactions with sedatives 24 hours<br />
St. John’s wort • Induces cytochrome P-450 5 days<br />
• Affects multiple drug levels<br />
Source: Data adapted from Ang-Lee et al. 138 and Adusumilli et al. 139<br />
For example, specific medications such as antihistamines<br />
or benzodiazepines contribute to the risk of falls or confusion.<br />
Agostini et al. 142 showed that there is a linear<br />
relationship between the number of medications used<br />
and the risk of two frequently reported adverse drug<br />
effects—weight loss and impaired balance. This effect was<br />
apparent even when comorbidities and indications for<br />
many of the medications were adjusted for. In terms of<br />
risk reduction, a study showed that time taken to educate<br />
the patient on dosages and frequency of medicines,<br />
reasons for taking medicines, and information about<br />
adverse side effects improved patient compliance and<br />
outcomes. 143 <strong>The</strong> perioperative period has been proposed<br />
as an ideal time to critically review the medication list for<br />
polypharmacy, drug interactions, and adverse drug<br />
events. 144 Although these proposals make intuitive sense,<br />
no randomized trials have specifically addressed this<br />
issue.<br />
Comprehensive <strong>Geriatric</strong> Assessment<br />
<strong>The</strong> team approach to the elderly patient involves the<br />
geriatrician, nurse coordinator, physical therapist, and<br />
social worker. Randomized controlled trials have been<br />
variable in the benefits of a comprehensive geriatric<br />
assessment (CGA). <strong>The</strong> selective use of the CGA has<br />
been proven to be beneficial in the perioperative period.<br />
For instance, in community-dwelling elders who failed a<br />
screen for falls, urinary incontinence, depression, or functional<br />
impairment, CGA was found to be efficacious and<br />
cost-effective. Although not studied in the surgical population,<br />
a meta-analysis showed that CGA, along with<br />
long-term management, is effective for improving survival<br />
and function. 145 One recent randomized clinical trial<br />
that targeted patients aged ≥65 years after hip fracture
192 L.L. Liu and J.M. Leung<br />
surgery demonstrated that “proactive geriatric consultation”<br />
reduced delirium by more than one third and<br />
reduced severe delirium by more than half. 146 This important<br />
study demonstrates that certain adverse outcomes<br />
after surgery such as delirium may be modifiable, and<br />
suggests that similar strategies, which are multifactorial<br />
and targeted, may be possible to reduce the trajectory of<br />
decline after major surgery in the older population.<br />
Conclusion<br />
Although surgery in the geriatric population is not<br />
without risk, the mortality rate has decreased markedly.<br />
With more emphasis on preoperative medical optimization,<br />
along with early identification of surgical issues,<br />
most patients can expect to do well. Patients ≥80 years of<br />
age undergoing noncardiac surgery who did not have<br />
postoperative complications were found to survive just as<br />
well as the age- and gender-matched general population.<br />
77 Chronologic age is less important as an independent<br />
risk predictor. A more important predictor is the<br />
presence of coexisting diseases. With the identification of<br />
the major risk factors associated with postoperative morbidity,<br />
opportunity to improve perioperative outcomes in<br />
elderly patients will be possible when risk factors for<br />
these adverse events can be modified through randomized<br />
prospective clinical trials. As more information<br />
becomes available on risk modification through future<br />
research, practitioners can then develop a comprehensive<br />
set of quality indicators for elderly surgical care and<br />
thereby improve the quality and safety of perioperative<br />
surgical care of geriatric patients.<br />
References<br />
1. Projections of the total resident population by 5-year age<br />
groups, and sex with special age categories: middle series,<br />
2025–2045. Vol 2004. US Census Bureau; 2000.<br />
2. Herron PW, Jesseph JE, Harkins HN. Analysis of 600<br />
major operations in patients over 70 years of age. Ann Surg<br />
1960;152:686–698.<br />
3. Burnett W, McCaffrey J. Surgical procedures in the elderly.<br />
Surg Gynecol Obstet 1972;134:221–226.<br />
4. Seymour DG, Vaz FG. A prospective study of elderly<br />
general surgical patients: II. Post-operative complications.<br />
Age Ageing 1989;18:316–326.<br />
5. Milamed DR, Hedley-Whyte J. Contributions of the<br />
surgical sciences to a reduction of the mortality rate in<br />
the United States for the period 1968 to 1988. Ann Surg<br />
1994;219:94–102.<br />
6. Liu LL, Leung JM. Predicting adverse postoperative outcomes<br />
in patients aged 80 years or older. J Am Geriatr Soc<br />
2000;48:405–412.<br />
7. Leung JM, Dzankic S. Relative importance of preoperative<br />
health status versus intraoperative factors in predicting<br />
postoperative adverse outcomes in geriatric surgical<br />
patients. J Am Geriatr Soc 2001;49:1080–1085.<br />
8. Mangano DT. Perioperative cardiac morbidity. <strong>Anesthesiology</strong><br />
1990;72:153–184.<br />
9. Tiret L, Hatton F, Desmonts JM, et al. Prediction of<br />
outcome of anaesthesia in patients over 40 years: a multifactorial<br />
risk index. Stat Med 1988;7:947–954.<br />
10. Pedersen T, Eliasen K, Henriksen E. A prospective study<br />
of mortality associated with anaesthesia and surgery: risk<br />
indicators of mortality in hospital. Acta Anaesthesiol<br />
Scand 1990;34:176–182.<br />
11. Rorbaek-Madsen M, Dupont G, Kristensen K, et al.<br />
General surgery in patients aged 80 years and older. Br J<br />
Surg 1992;79:1216–1218.<br />
12. Bufalari A, Ferri M, Cao P, et al. Surgical care in octogenarians.<br />
Br J Surg 1996;83:1783–1787.<br />
13. Vaz FG, Seymour DG. A prospective study of elderly<br />
general surgical patients: I. Pre-operative medical problems.<br />
Age Ageing 1989;18:309–315.<br />
14. Warner MA, Saletel RA, Schroeder DR, et al. Outcomes<br />
of anesthesia and surgery in people 100 years of age and<br />
older. J Am Geriatr Soc 1998;46:988–993.<br />
15. Moller JT, Cluitmans P, Rasmussen LS, et al. Long-term<br />
postoperative cognitive dysfunction in the elderly<br />
ISPOCD1 study. ISPOCD investigators. International<br />
Study of Post-Operative Cognitive Dysfunction. Lancet<br />
1998;351:857–861.<br />
16. Marcantonio ER, Goldman L, Mangione CM, et al. A clinical<br />
prediction rule for delirium after elective noncardiac<br />
surgery. JAMA 1994;271:134–139.<br />
17. Williams M, Holloway J, Winn M, et al. Nursing activities<br />
and acute confusional states in elderly hip-fractured<br />
patients. Nurs Res 1979;26:25–35.<br />
18. Berggren D, Gustafson Y, Eriksson B, et al. Post -<br />
operative confusion after anesthesia in elderly patients<br />
with femoral neck fractures. Anesth Analg 1987;66:497–<br />
504.<br />
19. Inouye S. <strong>The</strong> dilemma of delirium: clinical and research<br />
controversies regarding diagnosis and evaluation of delirium<br />
in hospitalized elderly medical patients. Am J Med<br />
1994;97:278–288.<br />
20. Gustafson Y, Berggren D, Brannstrom B, et al. Acute confusional<br />
states in elderly patients treated for femoral neck<br />
fracture. J Am Geriatr Soc 1988;36:525–530.<br />
21. Francis J, Kapoor WN. Delirium in hospitalized elderly.<br />
J Gen Intern Med 1990;5:65–79.<br />
22. Inouye SK, Charpentier PA. Precipitating factors for delirium<br />
in hospitalized elderly persons. Predictive model and<br />
interrelationship with baseline vulnerability. JAMA 1996;<br />
275:852–857.<br />
23. Larson EB, Kukull WA, Buchner D, et al. Adverse<br />
drug reactions associated with global cognitive impairment<br />
in elderly persons. Ann Intern Med 1987;107:169–<br />
173.<br />
24. Hole A, Terjesen T, Breivik H. Epidural versus general<br />
anaesthesia for total hip arthroplasty in elderly patients.<br />
Acta Anaesthesiol Scand 1980;24:279–287.<br />
25. Williams-Russo P, Sharrock NE, Mattis S, et al. Cognitive<br />
effects after epidural vs general anesthesia in older adults.<br />
A randomized trial. JAMA 1995;274:44–50.
13. Preoperative Risk Stratification and Methods to Reduce Risk 193<br />
26. O’Hara DA, Duff A, Berlin JA, et al. <strong>The</strong> effect of anesthetic<br />
technique on postoperative outcomes in hip fracture<br />
repair. <strong>Anesthesiology</strong> 2000;92:947–957.<br />
27. Rasmussen LS, Johnson T, Kuipers HM, et al. Does anaesthesia<br />
cause postoperative cognitive dysfunction? A randomised<br />
study of regional versus general anaesthesia in<br />
438 elderly patients. Acta Anaesthesiol Scand 2003;47:<br />
260–266.<br />
28. Williams-Russo P, Sharrock NE, Mattis S, et al. Randomized<br />
trial of hypotensive epidural anesthesia in older adults.<br />
<strong>Anesthesiology</strong> 1999;91:926–935.<br />
29. Lynch EP, Lazor MA, Gellis JE, et al. <strong>The</strong> impact of postoperative<br />
pain on the development of postoperative<br />
delirium. Anesth Analg 1998;86:781–785.<br />
30. Pedersen T, Eliasen K, Henriksen E. A prospective study<br />
of risk factors and cardiopulmonary complications associated<br />
with anaesthesia and surgery: risk indicators of cardiopulmonary<br />
morbidity. Acta Anaesthesiol Scand 1990;<br />
34:144–155.<br />
31. Goldman L, Caldera DL, Nussbaum SR, et al. Multifactorial<br />
index of cardiac risk in noncardiac surgical procedures.<br />
N Engl J Med 1977;297:845–850.<br />
32. Lee TH, Marcantonio ER, Mangione CM, et al. Derivation<br />
and prospective validation of a simple index for prediction<br />
of cardiac risk of major noncardiac surgery. Circulation<br />
1999;100:1043–1049.<br />
33. Eagle KA, Berger PB, Calkins H, et al. ACC/AHA guideline<br />
update for perioperative cardiovascular evaluation for<br />
noncardiac surgery—executive summary. A report of the<br />
American College of Cardiology/American Heart Association<br />
Task Force on Practice Guidelines (Committee to<br />
Update the 1996 Guidelines on Perioperative Cardiovascular<br />
Evaluation for Noncardiac Surgery). Circulation<br />
2002;105:1257–1267.<br />
34. Eagle KA, Rihal CS, Mickel MC, et al. Cardiac risk of<br />
noncardiac surgery: influence of coronary disease and type<br />
of surgery in 3368 operations. CASS Investigators and<br />
University of Michigan Heart Care Program. Coronary<br />
Artery Surgery Study. Circulation 1997;96:1882–1887.<br />
35. McFalls EO, Ward HB, Moritz TE, et al. Coronary-artery<br />
revascularization before elective major vascular surgery.<br />
N Engl J Med 2004;351:2795–2804.<br />
36. Aronow WS, Ahn C, Kronzon I. Normal left ventricular<br />
ejection fraction in older persons with congestive heart<br />
failure. Chest 1998;113:867–869.<br />
37. Vasan RS, Benjamin EJ, Levy D. Prevalence, clinical features<br />
and prognosis of diastolic heart failure: an epidemiologic<br />
perspective. J Am Coll Cardiol 1995;26:1565–1574.<br />
38. Tresch DD, McGough MF. Heart failure with normal systolic<br />
function: a common disorder in older people. J Am<br />
Geriatr Soc 1995;43:1035–1042.<br />
39. Hamlin SK, Villars PS, Kanusky JT, et al. Role of diastole<br />
in left ventricular function. II: diagnosis and treatment. Am<br />
J Crit Care 2004;13:453–466; quiz 467–468.<br />
40. Stamler J, Stamler R, Neaton JD. Blood pressure, systolic<br />
and diastolic, and cardiovascular risks. US population data.<br />
Arch Intern Med 1993;153:598–615.<br />
41. Howell SJ, Sear JW, Foex P. Hypertension, hypertensive<br />
heart disease and perioperative cardiac risk. Br J Anaesth<br />
2004;92:570–583.<br />
42. Prys-Roberts C, Meloche R, Foex P. Studies of anaesthesia<br />
in relation to hypertension. I. Cardiovascular responses<br />
of treated and untreated patients. Br J Anaesth 1971;43:<br />
122–137.<br />
43. Prys-Roberts C, Greene LT, Meloche R, et al. Studies of<br />
anaesthesia in relation to hypertension. II. Haemodynamic<br />
consequences of induction and endotracheal intubation.<br />
Br J Anaesth 1971;43:531–547.<br />
44. Reich DL, Bennett-Guerrero E, Bodian CA, et al. Intraoperative<br />
tachycardia and hypertension are independently<br />
associated with adverse outcome in noncardiac surgery of<br />
long duration. Anesth Analg 2002;95:273–277.<br />
45. Stevens A, Abrams K. Consensus, reviews and metaanalysis.<br />
In: Stevens A, Abrams K, Brazier J, et al., eds.<br />
Methods in Evidence Based Healthcare. London: Sage;<br />
2001:367–369.<br />
46. Wallace A, Layug B, Tateo I, et al. Prophylactic atenolol<br />
reduces postoperative myocardial ischemia. McSPI<br />
Research Group. <strong>Anesthesiology</strong> 1998;88:7–17.<br />
47. Poldermans D, Boersma E, Bax JJ, et al. <strong>The</strong> effect of<br />
bisoprolol on perioperative mortality and myocardial<br />
infarction in high-risk patients undergoing vascular surgery.<br />
Dutch Echocardiographic Cardiac Risk Evaluation Applying<br />
Stress Echocardiography Study Group. N Engl J Med<br />
1999;341:1789–1794.<br />
48. Mangano DT, Hollenberg M, Fegert G, et al. Perioperative<br />
myocardial ischemia in patients undergoing noncardiac<br />
surgery. I: incidence and severity during the 4 day perioperative<br />
period. <strong>The</strong> Study of Perioperative Ischemia (SPI)<br />
Research Group. J Am Coll Cardiol 1991;17:843–850.<br />
49. Tuman KJ, McCarthy RJ. Individualizing beta-adrenergic<br />
blocker therapy: patient-specific target-based heart rate<br />
control. Anesth Analg 1999;88:475–476.<br />
50. Zaugg M, Tagliente T, Lucchinetti E, et al. Beneficial<br />
effects from beta-adrenergic blockade in elderly patients<br />
undergoing noncardiac surgery. <strong>Anesthesiology</strong> 1999;91:<br />
1674–1686.<br />
51. Lindenauer PK, Fitzgerald J, Hoople N, et al. <strong>The</strong> potential<br />
preventability of postoperative myocardial infarction:<br />
underuse of perioperative beta-adrenergic blockade. Arch<br />
Intern Med 2004;164:762–766.<br />
52. Gottlieb SS, McCarter RJ, Vogel RA. Effect of betablockade<br />
on mortality among high-risk and low-risk<br />
patients after myocardial infarction. N Engl J Med 1998;<br />
339:489–497.<br />
53. Soumerai SB, McLaughlin TJ, Spiegelman D, et al.<br />
Adverse outcomes of underuse of beta-blockers in elderly<br />
survivors of acute myocardial infarction. JAMA 1997;<br />
277:115–121.<br />
54. Schmidt M, Lindenauer PK, Fitzgerald JL, et al. Forecasting<br />
the impact of a clinical practice guideline for perioperative<br />
beta-blockers to reduce cardiovascular morbidity<br />
and mortality. Arch Intern Med 2002;162:63–69.<br />
55. Mohr DN. Estimation of surgical risk in the elderly: a correlative<br />
review. J Am Geriatr Soc 1983;31:99–102.<br />
56. Dzankic S, Leung J. <strong>Anesthesia</strong> and aging. In: Lake C,<br />
Johnson J, McLoughlin T, eds. Advances in <strong>Anesthesia</strong>. Vol<br />
21. Philadelphia: Mosby; 2003:1–42.<br />
57. Zaugg M, Lucchinetti E. Respiratory function in the<br />
elderly. Anesthesiol Clin North Am 2000;18:47–58.
194 L.L. Liu and J.M. Leung<br />
58. Lawrence VA, Hilsenbeck SG, Mulrow CD, et al. Incidence<br />
and hospital stay for cardiac and pulmonary compli -<br />
cations after abdominal surgery. J Gen Intern Med 1995;<br />
10:671–678.<br />
59. Brooks-Brunn JA. Predictors of postoperative pulmonary<br />
complications following abdominal surgery. Chest 1997;<br />
111:564–571.<br />
60. Lawrence VA, Dhanda R, Hilsenbeck SG, et al. Risk of<br />
pulmonary complications after elective abdominal surgery.<br />
Chest 1996;110:744–750.<br />
61. Jayr C, Matthay MA, Goldstone J, et al. Preoperative and<br />
intraoperative factors associated with prolonged mechanical<br />
ventilation. A study in patients following major abdominal<br />
vascular surgery. Chest 1993;103:1231–1236.<br />
62. Bluman LG, Mosca L, Newman N, et al. Preoperative<br />
smoking habits and postoperative pulmonary complications.<br />
Chest 1998;113:883–889.<br />
63. Sorensen LT, Karlsmark T, Gottrup F. Abstinence from<br />
smoking reduces incisional wound infection: a randomized<br />
controlled trial. Ann Surg 2003;238:1–5.<br />
64. Moller AM, Villebro N, Pedersen T, et al. Effect of preoperative<br />
smoking intervention on postoperative complications:<br />
a randomised clinical trial. Lancet 2002;359:<br />
114–117.<br />
65. Warner MA, Offord KP, Warner ME, et al. Role of preoperative<br />
cessation of smoking and other factors in postoperative<br />
pulmonary complications: a blinded prospective<br />
study of coronary artery bypass patients. Mayo Clin Proc<br />
1989;64:609–616.<br />
66. Banerjee DK, Lee GS, Malik SK, et al. Underdiagnosis of<br />
asthma in the elderly. Br J Dis Chest 1987;81:23–29.<br />
67. Couser JI Jr, Guthmann R, Hamadeh MA, et al. Pulmonary<br />
rehabilitation improves exercise capacity in older<br />
elderly patients with COPD. Chest 1995;107:730–734.<br />
68. Kradjan WA, Driesner NK, Abuan TH, et al. Effect of age<br />
on bronchodilator response. Chest 1992;101:1545–1551.<br />
69. Mokdad AH, Bowman BA, Ford ES, et al. <strong>The</strong> continuing<br />
epidemics of obesity and diabetes in the United States.<br />
JAMA 2001;286:1195–1200.<br />
70. Arterburn DE, Crane PK, Sullivan SD. <strong>The</strong> coming epidemic<br />
of obesity in elderly Americans. J Am Geriatr Soc<br />
2004;52:1907–1912.<br />
71. Must A, Spadano J, Coakley EH, et al. <strong>The</strong> disease burden<br />
associated with overweight and obesity. JAMA 1999;282:<br />
1523–1529.<br />
72. Gupta RM, Parvizi J, Hanssen AD, et al. Postoperative<br />
complications in patients with obstructive sleep apnea syndrome<br />
undergoing hip or knee replacement: a case-control<br />
study. Mayo Clin Proc 2001;76:897–905.<br />
73. Meoli AL, Rosen CL, Kristo D, et al. Upper airway management<br />
of the adult patient with obstructive sleep apnea<br />
in the perioperative period—avoiding complications. Sleep<br />
2003;26:1060–1065.<br />
74. Nygaard HA, Naik M, Ruths S, et al. Clinically important<br />
renal impairment in various groups of old persons. Scand<br />
J Prim Health Care 2004;22:152–156.<br />
75. Kohli HS, Bhaskaran MC, Muthukumar T, et al. Treatmentrelated<br />
acute renal failure in the elderly: a hospital-based<br />
prospective study. Nephrol Dial Transplant 2000;15:<br />
212–217.<br />
76. John AD, Sieber FE. Age associated issues: geriatrics.<br />
Anesthesiol Clin North Am 2004;22:45–58.<br />
77. Manku K, Bacchetti P, Leung JM. Prognostic significance<br />
of postoperative in-hospital complications in elderly<br />
patients. I. Long-term survival. Anesth Analg 2003;96:<br />
583–589.<br />
78. King H, Aubert RE, Herman WH. <strong>Global</strong> burden of diabetes,<br />
1995–2025: prevalence, numerical estimates, and<br />
projections. Diabetes Care 1998;21:1414–1431.<br />
79. Mokdad AH, Ford ES, Bowman BA, et al. Diabetes trends<br />
in the U.S.: 1990–1998. Diabetes Care 2000;23:1278–1283.<br />
80. Jack L Jr, Boseman L, Vinicor F. Aging Americans and<br />
diabetes. A public health and clinical response. <strong>Geriatric</strong>s<br />
2004;59:14–17.<br />
81. McBean AM, Li S, Gilbertson DT, et al. Differences in<br />
diabetes prevalence, incidence, and mortality among the<br />
elderly of four racial/ethnic groups: whites, blacks, Hispanics,<br />
and Asians. Diabetes Care 2004;27:2317–2324.<br />
82. Schiff RL, Welsh GA. Perioperative evaluation and management<br />
of the patient with endocrine dysfunction. Med<br />
Clin North Am 2003;87:175–192.<br />
83. Brown AF, Mangione CM, Saliba D, et al. Guidelines for<br />
improving the care of the older person with diabetes mellitus.<br />
J Am Geriatr Soc 2003;51:S265–280.<br />
84. American Diabetes Association. Implications of the diabetes<br />
control and complications trial. Diabetes Care 2003;<br />
26(Suppl 1):S25–27.<br />
85. Malone DL, Genuit T, Tracy JK, et al. Surgical site infections:<br />
reanalysis of risk factors. J Surg Res 2002;103:89–95.<br />
86. Guvener M, Pasaoglu I, Demircin M, et al. Perioperative<br />
hyperglycemia is a strong correlate of postoperative infection<br />
in type II diabetic patients after coronary artery<br />
bypass grafting. Endocr J 2002;49:531–537.<br />
87. Zerr KJ, Furnary AP, Grunkemeier GL, et al. Glucose<br />
control lowers the risk of wound infection in diabetics after<br />
open heart operations. Ann Thorac Surg 1997;63:356–361.<br />
88. Van den Berghe G, Wouters P, Weekers F, et al. Intensive<br />
insulin therapy in the critically ill patients. N Engl J Med<br />
2001;345:1359–1367.<br />
89. Connery LE, Coursin DB. Assessment and therapy of<br />
selected endocrine disorders. Anesthesiol Clin North Am<br />
2004;22:93–123.<br />
90. Marks JB. Perioperative management of diabetes. Am Fam<br />
Physician 2003;67:93–100.<br />
91. Guigoz Y, Lauque S, Vellas BJ. Identifying the elderly at<br />
risk for malnutrition. <strong>The</strong> Mini Nutritional Assessment.<br />
Clin Geriatr Med 2002;18:737–757.<br />
92. Shils ME. Recalling a 63-year nutrition odyssey. Nutrition<br />
2000;16:582–585.<br />
93. Studley HO. Percentage of weight loss: a basic indicator of<br />
surgical risk in patients with chronic peptic ulcer. 1936.<br />
Nutr Hosp 2001;16:141–143.<br />
94. Gibbs J, Cull W, Henderson W, et al. Preoperative serum<br />
albumin level as a predictor of operative mortality and<br />
morbidity: results from the National VA Surgical Risk<br />
Study. Arch Surg 1999;134:36–42.<br />
95. Carney DE, Meguid MM. Current concepts in nutritional<br />
assessment. Arch Surg 2002;137:42–45.<br />
96. Prealbumin in Nutritional Care Consensus Group. Measurement<br />
of visceral protein status in assessing protein and
13. Preoperative Risk Stratification and Methods to Reduce Risk 195<br />
energy malnutrition: standard of care. Nutrition 1995;11:<br />
169–171.<br />
97. Winkler MF, Gerrior SA, Pomp A, et al. Use of retinolbinding<br />
protein and prealbumin as indicators of the<br />
response to nutrition therapy. J Am Diet Assoc 1989;<br />
89:684–687.<br />
98. Hedlund JU, Hansson LO, Ortqvist AB. Hypoalbuminemia<br />
in hospitalized patients with community-acquired<br />
pneumonia. Arch Intern Med 1995;155:1438–1442.<br />
99. Souba WW. Nutritional support. N Engl J Med 1997;336:<br />
41–48.<br />
100. Vellas B, Guigoz Y, Garry PJ, et al. <strong>The</strong> Mini Nutritional<br />
Assessment (MNA) and its use in grading the nutritional<br />
state of elderly patients. Nutrition 1999;15:116–122.<br />
101. Gazzotti C, Arnaud-Battandier F, Parello M, et al. Prevention<br />
of malnutrition in older people during and after hospitalisation:<br />
results from a randomised controlled clinical<br />
trial. Age Ageing 2003;32:321–325.<br />
102. Holte K, Kehlet H. Epidural anaesthesia and analgesia—<br />
effects on surgical stress responses and implications for<br />
postoperative nutrition. Clin Nutr 2002;21:199–206.<br />
103. Gerson MC, Hurst JM, Hertzberg VS, et al. Prediction of<br />
cardiac and pulmonary complications related to elective<br />
abdominal and noncardiac thoracic surgery in geriatric<br />
patients. Am J Med 1990;88:101–107.<br />
104. Gulati M, Pandey DK, Arnsdorf MF, et al. Exercise capacity<br />
and the risk of death in women: the St James Women<br />
Take Heart Project. Circulation 2003;108:1554–1559.<br />
105. Myers J, Prakash M, Froelicher V, et al. Exercise capacity<br />
and mortality among men referred for exercise testing.<br />
N Engl J Med 2002;346:793–801.<br />
106. Reilly DF, McNeely MJ, Doerner D, et al. Self-reported<br />
exercise tolerance and the risk of serious perioperative<br />
complications. Arch Intern Med 1999;159:2185–2192.<br />
107. Pinholt EM, Kroenke K, Hanley JF, et al. Functional<br />
assessment of the elderly. A comparison of standard instruments<br />
with clinical judgment. Arch Intern Med 1987;147:<br />
484–488.<br />
108. Katz S, Ford AB, Moskowitz RW, et al. Studies of illness<br />
in the aged. <strong>The</strong> index of ADL: a standardized measure<br />
of biological and psychosocial function. JAMA 1963;185:<br />
914–919.<br />
109. Lawton MP, Brody EM. Assessment of older people: selfmaintaining<br />
and instrumental activities of daily living.<br />
Gerontologist 1969;9:179–186.<br />
110. Davis RB, Iezzoni LI, Phillips RS, et al. Predicting inhospital<br />
mortality. <strong>The</strong> importance of functional status<br />
information. Med Care 1995;33:906–921.<br />
111. Gill TM, Baker DI, Gottschalk M, et al. A prehabilitation<br />
program for the prevention of functional decline: effect on<br />
higher-level physical function. Arch Phys Med Rehabil<br />
2004;85:1043–1049.<br />
112. Ditmyer MM, Topp R, Pifer M. Prehabilitation in preparation<br />
for orthopaedic surgery. Orthop Nurs 2002;21:43–51;<br />
quiz 52–54.<br />
113. Topp R, Ditmyer M, King K, et al. <strong>The</strong> effect of bed rest<br />
and potential of prehabilitation on patients in the intensive<br />
care unit. AACN Clin Issues 2002;13:263–276.<br />
114. Schein OD, Katz J, Bass EB, et al. <strong>The</strong> value of routine<br />
preoperative medical testing before cataract surgery. Study<br />
of Medical Testing for Cataract Surgery. N Engl J Med<br />
2000;342:168–175.<br />
115. Collen MF, Feldman R, Siegelaub AB, et al. Dollar cost per<br />
positive test for automated multiphasic screening. N Engl<br />
J Med 1970;283:459–463.<br />
116. Domoto K, Ben R, Wei JY, et al. Yield of routine annual<br />
laboratory screening in the institutionalized elderly. Am J<br />
Public Health 1985;75:243–245.<br />
117. Levinstein MR, Ouslander JG, Rubenstein LZ, et al. Yield<br />
of routine annual laboratory tests in a skilled nursing<br />
home population. JAMA 1987;258:1909–1915.<br />
118. Wolf-Klein GP, Holt T, Silverstone FA, et al. Efficacy of<br />
routine annual studies in the care of elderly patients. J Am<br />
Geriatr Soc 1985;33:325–329.<br />
119. Dzankic S, Pastor D, Gonzalez C, et al. <strong>The</strong> prevalence<br />
and predictive value of abnormal preoperative laboratory<br />
tests in elderly surgical patients. Anesth Analg 2001;93:<br />
301–308.<br />
120. Gold BS, Young ML, Kinman JL, et al. <strong>The</strong> utility of preoperative<br />
electrocardiograms in the ambulatory surgical<br />
patient. Arch Intern Med 1992;152:301–305.<br />
121. Liu LL, Dzankic S, Leung JM. Preoperative electrocardiogram<br />
abnormalities do not predict postoperative cardiac<br />
complications in geriatric surgical patients. J Am Geriatr<br />
Soc 2002;50:1186–1191.<br />
122. Smetana GW, Macpherson DS. <strong>The</strong> case against routine<br />
preoperative laboratory testing. Med Clin North Am<br />
2003;87:7–40.<br />
123. Arozullah AM, Conde MV, Lawrence VA. Preoperative<br />
evaluation for postoperative pulmonary complications.<br />
Med Clin North Am 2003;87:153–173.<br />
124. Seymour DG, Pringle R, Shaw JW. <strong>The</strong> role of the routine<br />
pre-operative chest X-ray in the elderly general surgical<br />
patient. Postgrad Med J 1982;58:741–745.<br />
125. Marcello PW, Roberts PL. “Routine” preoperative studies.<br />
Which studies in which patients? Surg Clin North Am<br />
1996;76:11–23.<br />
126. Tape TG, Mushlin AI. How useful are routine chest X-rays<br />
of preoperative patients at risk for postoperative chest<br />
disease? J Gen Intern Med 1988;3:15–20.<br />
127. Monro J, Booth A, Nicholl J. Routine preoperative testing:<br />
a systematic study of the evidence. Health Technol Assess<br />
1997;1:1–62.<br />
128. Fleisher LA. Routine laboratory testing in the elderly:<br />
is it indicated? Anesth Analg 2001;93:249–250.<br />
129. Chrischilles EA, Foley DJ, Wallace RB, et al. Use of medications<br />
by persons 65 and over: data from the established<br />
populations for epidemiologic studies of the elderly.<br />
J Gerontol 1992;47:M137–144.<br />
130. Gray SL, Mahoney JE, Blough DK. Medication ad -<br />
herence in elderly patients receiving home health services<br />
following hospital discharge. Ann Pharmacother 2001;35:<br />
539–545.<br />
131. Nolan L, O’Malley K. Prescribing for the elderly. Part I:<br />
sensitivity of the elderly to adverse drug reactions. J Am<br />
Geriatr Soc 1988;36:142–149.<br />
132. Leung JM, Dzankic S, Manku K, et al. <strong>The</strong> prevalence and<br />
predictors of the use of alternative medicine in presurgical<br />
patients in five California hospitals. Anesth Analg 2001;<br />
93:1062–1068.
196 L.L. Liu and J.M. Leung<br />
133. Yoon SL, Horne CH. Perceived health promotion practice<br />
by older women: use of herbal products. J Gerontol Nurs<br />
2004;30:9–15.<br />
134. Fugh-Berman A. Herb-drug interactions. Lancet 2000;355:<br />
134–138.<br />
135. Bennett DA Jr, Phun L, Polk JF, et al. Neuropharmacology<br />
of St. John’s wort (Hypericum). Ann Pharmacother 1998;<br />
32:1201–1208.<br />
136. Almeida JC, Grimsley EW. Coma from the health food<br />
store: interaction between kava and alprazolam. Ann<br />
Intern Med 1996;125:940–941.<br />
137. Slifman NR, Obermeyer WR, Aloi BK, et al. Contamination<br />
of botanical dietary supplements by Digitalis lanata.<br />
N Engl J Med 1998;339:806–811.<br />
138. Ang-Lee MK, Moss J, Yuan CS. Herbal medicines and<br />
perioperative care. JAMA 2001;286:208–216.<br />
139. Adusumilli PS, Ben-Porat L, Pereira M, et al. <strong>The</strong> prevalence<br />
and predictors of herbal medicine use in surgical<br />
patients. J Am Coll Surg 2004;198:583–590.<br />
140. Beers MH. Explicit criteria for determining potentially<br />
inappropriate medication use by the elderly. An update.<br />
Arch Intern Med 1997;157:1531–1536.<br />
141. Zhan C, Sangl J, Bierman AS, et al. Potentially inappropriate<br />
medication use in the community-dwelling elderly:<br />
findings from the 1996 Medical Expenditure Panel Survey.<br />
JAMA 2001;286:2823–2829.<br />
142. Agostini JV, Han L, Tinetti ME. <strong>The</strong> relationship be -<br />
tween number of medications and weight loss or impaired<br />
balance in older adults. J Am Geriatr Soc 2004;52:<br />
1719–1723.<br />
143. Lowe CJ, Raynor DK, Courtney EA, et al. Effects of self<br />
medication programme on knowledge of drugs and compliance<br />
with treatment in elderly patients. BMJ 1995;<br />
310:1229–1231.<br />
144. Rich MW, Gray DB, Beckham V, et al. Effect of a multidisciplinary<br />
intervention on medication compliance in<br />
elderly patients with congestive heart failure. Am J Med<br />
1996;101:270–276.<br />
145. Stuck AE, Siu AL, Wieland GD, et al. Comprehensive<br />
geriatric assessment: a meta-analysis of controlled trials.<br />
Lancet 1993;342:1032–1036.<br />
146. Marcantonio ER, Flacker JM, Wright RJ, et al. Reducing<br />
delirium after hip fracture: a randomized trial. J Am<br />
Geriatr Soc 2001;49:516–522.
14<br />
Anesthetic Implications of Chronic Medications<br />
Tamas A. Szabo and R. David Warters<br />
<strong>The</strong> safe administration of anesthesia to elderly patients<br />
<strong>The</strong> prevention and recognition of drug-related problems<br />
21.3% among noninstitutionalized elderly patients. 5 pam (Valium) are the primary benzodiazepines used in<br />
in older adults are of paramount importance. Medicationrelated<br />
problems are estimated to cause 106,000 deaths<br />
annually at a cost of $75–85 billion. Elderly patients presenting<br />
for surgery are often taking a large number and<br />
wide variety of chronic medications, greatly complicating<br />
their preoperative assessment and anesthesia management.<br />
requires a thorough evaluation and understanding of<br />
chronic medications and the potential for interactions.<br />
<strong>The</strong> aim of this chapter is to highlight (1) drugs that are<br />
common in elderly patients, and (2) drugs that have a<br />
potential interaction with medications used in the anesthetic<br />
practice.<br />
<strong>The</strong> often daunting task of evaluating the potential<br />
interactions of these medications with one another as<br />
well as anesthetic medications is further complicated by<br />
the large number of inappropriate medications prescribed<br />
in this age group.<br />
Neuropsychiatric and Pain-Related<br />
Medications<br />
Inappropriate medications for elderly patients are<br />
Benzodiazepines<br />
defined as medications for which a better alternative drug<br />
exists and for which the potential risk outweighs the<br />
potential benefit. In 1997, Beers 1 devised a comprehensive<br />
set of explicit criteria for potentially inappropriate drug<br />
use in ambulatory older adults aged 65 years and older.<br />
Drugs were classified as inappropriate in three categories:<br />
(1) drugs that generally should be avoided in the elderly,<br />
(2) drugs that exceed a maximum recommended daily<br />
dose, and (3) drugs to be avoided in combination with<br />
specific comorbidities. Recently, the 1997 criteria were<br />
updated and presented as the 2002 Beers criteria. 2 In these<br />
updated criteria, the comorbidity list was modified, new<br />
medications were added, and several drugs were removed.<br />
<strong>The</strong> Beers criteria may not identify all causes of potentially<br />
inappropriate prescribing (e.g., drug–drug interactions<br />
Benzodiazepines cause sedation, anterograde amnesia,<br />
anxiolysis, and muscle relaxation, as well as hypnotic and<br />
anticonvulsant effects. All effects and side effects of benzodiazepines<br />
are mediated through γ-aminobutyric acid<br />
(GABA) A receptors.<br />
Long-acting benzodiazepines are considered potentially<br />
inappropriate in elderly patients 2,6 because of the<br />
risk of producing prolonged sedation and increasing<br />
the potential for falls and fractures. Patients most likely<br />
to be prescribed benzodiazepines are the elderly with a<br />
secondary complaint of insomnia. Although sleep fragmentation<br />
may be reduced by benzodiazepines, their<br />
long-term use may also elicit health problems, such<br />
as complete obstructive sleep apnea in heavy snorers. 7<br />
are not included); however, they represent a widely Examples of long-acting benzodiazepines include<br />
used and standardized tool for pharmacologic research,<br />
despite the fact that nothing can substitute careful clinical<br />
judgment. A Dutch population-based cohort study<br />
revealed that 20% of ambulatory older adults receive at<br />
least one inappropriate drug prescription per year 3 ; moreover,<br />
halazepam (Paxipam), quazepam (Doral), flurazepam<br />
(Dalmane), chlordiazepoxide (Librium), chlordiazepoxide-amitriptyline<br />
(Limbitrol), clidinium-chlordiazepoxide<br />
(Librax), diazepam (Valium), and chlorazepate (Tranxene).<br />
Because of the increased sensitivity of long-acting<br />
an epidemiologic study 4 from the United States benzodiazepines in elderly patients, smaller doses of<br />
reported that 23.5% of people aged >65 years receive >1<br />
of the 20 medications on the Beers list. <strong>The</strong> prevalence of<br />
potentially inappropriate medications was found to be<br />
short- or intermediate-acting benzodiazepines are considered<br />
preferable, safer, and more effective.<br />
Midazolam (Versed), lorazepam (Ativan), and diaze-<br />
197
198 T.A. Szabo and R.D. Warters<br />
the anesthetic practice. 8 All three are highly protein<br />
bound, mainly by albumin. Patients with cirrhosis or<br />
chronic liver failure and subsequent hypoalbuminemia<br />
have a greater unbound fraction of benzodiazepines,<br />
which may increase their sensitivity to these agents.<br />
Midazolam undergoes rapid hepatic metabolism to<br />
both active and inactive metabolites. Drugs that inhibit<br />
the cytochrome P-450 enzyme system [i.e., cimetidine,<br />
erythromycin, calcium channel blockers (CCBs), and<br />
antifungal agents] reduce the hepatic clearance of<br />
midazolam. 9<br />
Diazepam is metabolized in the liver through oxidative<br />
demethylation and glucuronidation to inactive metabolites<br />
that are excreted by the kidneys. An increased<br />
volume of distribution and reduced metabolic clearance<br />
may significantly increase the elimination half-life of<br />
diazepam in patients with cirrhosis. Elderly and/or obese<br />
patients are also susceptible to prolonged diazepam<br />
effects secondary to an increased volume of distribution.<br />
Lorazepam is hepatically conjugated to an inactive<br />
metabolite.<br />
Respiratory depression secondary to the decrease in<br />
hypoxic drive is the most significant side effect of benzodiazepine<br />
administration. This effect is greater with midazolam<br />
than with lorazepam and diazepam in equipotent<br />
doses. Opioids may significantly enhance the respiratory<br />
depressant effects of benzodiazepines in patients with<br />
chronic obstructive pulmonary disease. Alpha 2 agonists,<br />
such as dexmedetomidine, have shown synergistic sedative<br />
effects, 10 while reversing the cardiovascular de -<br />
pressant effects of benzodiazepines. Moreover, the<br />
administration of even small doses of benzodiazepines in<br />
conjunction with opioids, propofol, or thiopental can also<br />
result in significant hypotension caused by the synergistic<br />
effects of these agents. 11<br />
Clinically significant hypotension may follow parenteral<br />
benzodiazepine administration in elderly patients.<br />
Parenteral benzodiazepines may be less effective in<br />
patients who take oral benzodiazepines on a chronic<br />
basis; moreover, the benzodiazepine antagonist flumazenil<br />
may precipitate withdrawal seizures in these patients. 12<br />
Benzodiazepines reduce the anesthetic requirements for<br />
both intravenous and inhalational anesthetics, but may<br />
also decrease the analgesic effects of opiates. 13 <strong>The</strong>refore,<br />
flumazenil may enhance the postoperative analgesic<br />
effects of morphine, reduce morphine requirements, and<br />
decrease the sedative, emetic, and cardiopulmonary<br />
depressant effects of morphine in patients who have<br />
received benzodiazepines after surgery.<br />
Carbamazepine<br />
Carbamazepine (Tegretol, Equetro, Carbatrol) is an anticonvulsant<br />
that blocks voltage- and frequency-dependent<br />
fast sodium currents. Sodium channels are kept in the<br />
inactivated state, inhibiting the spread of synchronized<br />
depolarization that is associated with the onset of seizures.<br />
Carbamazepine is structurally similar to tricyclic<br />
antidepressants.<br />
<strong>The</strong> therapeutic index of carbamazepine for neurologic<br />
side effects is 8:1, making it a relatively nontoxic medication.<br />
Negative side effects include gastrointestinal (GI)<br />
irritation, diplopia, ataxia, vertigo, and sedation. Acute<br />
intoxication may lead to respiratory depression, unconsciousness,<br />
seizures, and cardiovascular collapse. 14<br />
<strong>The</strong> hepatic metabolism of carbamazepine may be<br />
inhibited by erythromycin, isoniazid, cimetidine, and propoxyphene,<br />
15 leading to increased, possibly toxic, plasma<br />
levels. Carbamazepine can induce hepatic enzyme function<br />
and increase the metabolism of medications dependent<br />
on hepatic metabolism, including itself. <strong>The</strong>refore,<br />
the half-life tends to decrease with regular use. Carbamazepine<br />
may reduce the plasma levels of primidone, valproic<br />
acid, phenytoin, and haloperidol.<br />
Gabapentin<br />
Gabapentin is a weak inhibitor of GABA transaminase<br />
which was originally developed for seizure disorder but<br />
is frequently used for postherpetic neuralgia and neuropathic<br />
pain. It has also been proposed as a component of<br />
perioperative pain control. It acts by increasing GABA<br />
synthesis. Nausea, vomiting, dizziness, somnolence, headache,<br />
ataxia, and fatigue are the most common side effects<br />
of the drug. Rarely, confusion, hallucinations, depression,<br />
and psychoses may occur.<br />
Gabapentin is relatively free of drug interactions,<br />
its gastric absorption may be reduced by administra -<br />
tion of antacids containing hydroxides of aluminum or<br />
magnesium, and its renal clearance can be reduced by<br />
cimetidine.<br />
Monoamine Oxidase Inhibitors<br />
Monoamine oxidase inhibitors (MAOIs) are used in the<br />
treatment of severe depression unresponsive to other<br />
antidepressants. Intraneuronal monoamine oxidase<br />
(MAO) is the primary enzyme involved in the oxidative<br />
deamination of amine neurotransmitters (epinephrine,<br />
norepinephrine, dopamine, and serotonin). MAOIs in -<br />
crease the level of intraneuronal transmitters, resulting in<br />
augmented postsynaptic depolarization and adrenergic<br />
stimulation. MAO exists in two isoforms: MAO-A preferentially<br />
metabolizes serotonin, dopamine, and norepinephrine,<br />
whereas MAO-B preferentially metabolizes<br />
phenylethylamine and tyramine.<br />
Phenelzine (Nardil) is a nonselective MAOI that irreversibly<br />
inhibits the enzyme, and synthesis of new enzyme<br />
can take 10–14 days. It decreases pseudocholinesterase<br />
activity and subsequently prolongs depolarizing block-
14. Anesthetic Implications of Chronic Medications 199<br />
ade. Tranylcypromine (Parnate) is a slightly shorter-acting<br />
MAOI derived from amphetamine. Selegiline (Deprenyl),<br />
a selective MAO-B inhibitor, is used as an adjunct<br />
in the treatment of Parkinson’s disease.<br />
<strong>The</strong> interactions of MAOIs with certain drugs (notably<br />
meperidine, which blocks neuronal uptake of serotonin)<br />
and foods containing tyramine (aged cheeses, chocolate,<br />
liver, fava beans, avocados, and Chianti wine) have limited<br />
their use. 16,17 Concurrent use of MAOI and meperidine<br />
may result in fatal excitatory reactions. Respiratory<br />
depression, hypotension, and coma are the signs of a<br />
depressive form that is secondary to the accumulation<br />
of free narcotic and has been described after the use of<br />
fentanyl, alfentanil, or sufentanil. If foods high in tyramine<br />
are ingested, there is the potential for massive displacement<br />
of norepinephrine into the cleft and for a<br />
life-threatening hypertensive crisis. Many patients taking<br />
MAOIs have symptoms of autonomic dysfunction such<br />
as orthostatic hypotension, because tyramine is not catabolized<br />
and remains at high levels in plasma. Tyramine is<br />
then taken up by sympathetic nerve terminals as a “false<br />
transmitter” and is converted to the biologically inactive<br />
octopamine.<br />
MAOIs exaggerate the actions of indirect-acting and,<br />
to a lesser extent, direct-acting (phenylephrine, norepinephrine,<br />
epinephrine) sympathomimetics. A reduced<br />
dose of a direct-acting sympathomimetic is recommended<br />
8 for the treatment of hypotension. Ketamine and<br />
pancuronium should not be used to avoid stimulation of<br />
the sympathetic nervous system. Morphine may be used<br />
for perioperative analgesia.<br />
Selective Serotonin Reuptake Inhibitors<br />
Selective serotonin reuptake inhibitors (SSRIs) inhibit<br />
the neuronal reuptake of serotonin. <strong>The</strong>y are used primarily<br />
as antidepressants, but are also effective in the<br />
treatment of panic disorder, obsessive/compulsive disorder,<br />
posttraumatic stress disorder, and social phobia.<br />
SSRIs do not have anticholinergic effects, have little<br />
effect on norepinephrine reuptake, do not cause postural<br />
hypotension, do not cause delayed conduction of cardiac<br />
impulses, and do not affect the seizure threshold.<br />
Fluoxetine is a potent inhibitor of certain hepatic cytochrome<br />
P-450 enzymes and may subsequently increase<br />
plasma concentrations of drugs that depend on hepatic<br />
metabolism. MAOIs, lithium, or carbamazepine combined<br />
with fluoxetine may cause the development of the<br />
potentially fatal (11% mortality) serotonin syndrome 18<br />
characterized by hypo- or hypertension, anxiety, restlessness,<br />
confusion, chills, ataxia, insomnia, and seizures. This<br />
syndrome is most often reported in patients taking two<br />
or more medications that increase central nervous system<br />
(CNS) serotonin levels by different mechanisms.<br />
Tricyclic Antidepressants<br />
Amitriptyline and protriptyline are tricyclic antidepressants<br />
that exhibit the most prominent anticholinergic<br />
effects (tachycardia, blurred vision, dry mouth, delayed<br />
gastric emptying, urinary retention); therefore, they may<br />
be avoided in patients with glaucoma or prostatic hypertrophy.<br />
Cardiovascular abnormalities, including orthostatic<br />
hypotension and cardiac dysrhythmias (increased<br />
PR and QT intervals, widened QRS complexes), can be<br />
caused by these drugs. 19 Patients with coexisting heart<br />
block or prolonged QT intervals may be at increased risk<br />
for cardiac toxicity. Overdose may lead to cardiac conduction<br />
abnormalities, hypotension, mental status changes,<br />
seizures, coma, rhabdomyolysis, and renal failure. <strong>The</strong><br />
sedation associated with tricyclic antidepressants may be<br />
beneficial for patients experiencing insomnia.<br />
Patients taking tricyclic antidepressants may exhibit<br />
exaggerated systemic blood pressure responses after the<br />
administration of indirect-acting vasopressors because of<br />
the increased availability of norepinephrine at the postsynaptic<br />
receptors of the peripheral sympathetic nervous<br />
system. <strong>The</strong> combination of imipramine and pancuronium<br />
or ketamine may predispose anesthetized patients to<br />
tachydysrhythmias. 20 Postoperative delirium and confusion<br />
may result by the additive anticholinergic effects of<br />
the tricyclic antidepressants and centrally active anticholinergic<br />
drugs.<br />
Antiparkinson Medications<br />
<strong>The</strong> treatment of Parkinson’s disease is directed toward<br />
increasing dopamine levels in the brain but preventing<br />
adverse peripheral effects of dopamine. Levodopa is the<br />
single most effective therapy for patients with Parkinson’s<br />
disease. Side effects of levodopa administration<br />
include orthostatic hypotension, hypovolemia, depletion<br />
of myocardial norepinephrine stores, and peripheral<br />
vasoconstriction. <strong>The</strong> half-life of levodopa is short, and<br />
interruption of therapy for more than 6–12 hours can<br />
result in severe skeletal muscle rigidity that interferes<br />
with ventilation. Levodopa may alter some liver function<br />
tests, blood urea nitrogen, and positive Coombs test. Phenothiazines,<br />
butyrophenones (droperidol), and metoclopramide<br />
antagonize the effects of dopamine in the basal<br />
ganglia and should be avoided. 21<br />
Antidementia Drugs<br />
Donepezil, rivastigmine, galantamine, and tacrine are<br />
reversible acetylcholinesterase inhibitors used in the<br />
treatment of mild to moderately severe dementia in<br />
Alzheimer’s disease. Adverse effects include abdominal<br />
pain, nausea, vomiting, diarrhea, dizziness, headache,<br />
somnolence, muscle cramps, insomnia, sweating, tremor,
200 T.A. Szabo and R.D. Warters<br />
and syncope. Angina, sinoatrial (SA), atrioventricular<br />
(AV), and bundle-branch blocks, bradycardia, cardiac<br />
arrest, peptic ulcers, GI hemorrhage, extrapyramidal<br />
symptoms, seizures, depression, hallucinations, agitation,<br />
confusion, and bladder outflow obstruction have been<br />
observed. 22 Rivastigmine, tacrine, and donepezil may<br />
prolong the action of succinylcholine. Cholinergic crisis<br />
may result from overdose.<br />
Donepezil is selective for the CNS. It is highly protein<br />
bound, mainly by albumin. It undergoes partial metabolism<br />
via the cytochrome P-450 system. Ketoconazole,<br />
erythromycin, fluoxetine, and quinidine increase plasma<br />
donepezil concentrations by inhibiting the isoenzymes<br />
CYP 3A4 and CYP 2D6. Conversely, donepezil concentrations<br />
may be reduced by enzyme inducers such as<br />
phenytoin, carbamazepine, and rifampin.<br />
Rivastigmine is selective for the CNS and has also been<br />
tried in the treatment of vascular dementia and in the<br />
treatment of psychosis in patients with Parkinson’s<br />
disease. It is approximately 40% bound to plasma<br />
proteins and readily crosses the blood–brain barrier.<br />
<strong>The</strong> drug is metabolized by cholinesterase-mediated<br />
hydrolysis. 23<br />
Galantamine may also be effective in the treatment of<br />
vascular dementia. It is not recommended for treatment<br />
of mild cognitive impairment because of an association<br />
with increased mortality. Galantamine is partially metabolized<br />
by the cytochrome P-450 system. A reduced dose<br />
may be necessary in patients with hepatic or renal impairment<br />
or when galantamine is given with drugs that inhibit<br />
CYP 2D6 and CYP 3A4, such as quinidine, fluoxetine,<br />
fluvoxamine, paroxetine, and ketoconazole.<br />
Tacrine may delay cognitive decline but many patients<br />
cannot tolerate the dosage required and have to stop<br />
treatment because of GI effects or signs of hepatotoxicity.<br />
It undergoes an extensive first-pass effect in the liver, and<br />
is metabolized by the cytochrome P-450 system. It may<br />
competitively inhibit the metabolism of other drugs that<br />
are also metabolized by the cytochrome P-450 isoenzyme<br />
CYP 1A2. Cimetidine has been shown to inhibit the<br />
metabolism of tacrine. Increased serum alanine aminotransferase<br />
concentrations, mostly within the first 12<br />
weeks of therapy, are likely to occur in about 50% of<br />
patients. 24 Some patients may develop unpredictable lifethreatening<br />
hepatotoxicity. <strong>The</strong>re is no significant correlation<br />
between plasma-tacrine concentrations and<br />
hepatotoxicity. Abruptly stopping tacrine therapy may<br />
result in a decline in cognitive function.<br />
<strong>The</strong> N-methyl-d-aspartate (NMDA) receptor antagonist<br />
memantine is used in the treatment of moderately<br />
severe to severe Alzheimer’s disease and is thought to act<br />
through modulation of the effects of glutamate. It undergoes<br />
partial hepatic metabolism. <strong>The</strong> majority is excreted<br />
unchanged via the kidney. Use of other NMDA antagonists<br />
such as amantadine, ketamine, or dextromethorphan<br />
may increase the incidence and severity of adverse effects<br />
and should be avoided. <strong>The</strong> effects of dopaminergics and<br />
antimuscarinics may also be enhanced, whereas memantine<br />
may reduce the actions of barbiturates and antipsychotics.<br />
Adverse effects include anxiety, hallucinations,<br />
confusion, constipation, dizziness, headache, somnolence,<br />
abnormal gait, hypertension, and seizures. Dosage adjustment<br />
may be required in patients with recent myocardial<br />
infarction, congestive heart failure, uncontrolled hypertension,<br />
and renal impairment. 25<br />
Cardiovascular Drugs<br />
Alpha 2 -Adrenergic Agonists<br />
Three categories of alpha 2 agonists exist: phenylethylates<br />
(e.g., methyldopa), imidazolines (e.g., clonidine, dexmedetomidine),<br />
and oxaloazepines. <strong>The</strong> most prominent<br />
hemodynamic effects of alpha 2 agonists are hypotension<br />
and bradycardia. Hypotension can be reversed by standard<br />
vasoactive agents. <strong>The</strong> pressor response to ephedrine<br />
and phenylephrine are enhanced, but the response<br />
to norepinephrine is not. 26 <strong>The</strong> response to dopamine and<br />
to atropine is mildly attenuated. Rebound hypertension<br />
may occur after abrupt discontinuation of these drugs<br />
after chronic administration. <strong>The</strong> anesthetic-sparing<br />
and sedative effects of alpha 2 agonists result from inactivation<br />
of the locus ceruleus. <strong>The</strong> sedative effect is antagonized<br />
by alpha 1 agonists. Alpha 2 agonist or benzodia -<br />
zepine premedication may attenuate the high incidence<br />
(up to 30%) of ketamine-induced disturbing emergence<br />
reactions. Alpha 2 agonists reduce GI motility and co -<br />
administration of opioids produces a synergistic inhibition<br />
of GI transit.<br />
<strong>The</strong> potential for CNS adverse effects and orthostatic<br />
hypotension may contraindicate the use of clonidine in<br />
the elderly, whereas methyldopa (Aldomet) and methyldopa-hydrochlorothiazide<br />
(Aldoril) may cause bradycardia<br />
and exacerbate depression in elderly patients. 2<br />
Alpha 1 -Adrenergic Antagonists<br />
Doxazosin (Cardura) may cause orthostatic hypotension,<br />
edema, hepatitis, dry mouth, and urinary retention. Hypotension<br />
during epidural anesthesia may be exaggerated<br />
in the presence of alpha 1 -blockers and the resulting<br />
decrease in systemic vascular resistance may not be<br />
responsive to alpha 1 -adrenergic agonists (e.g., phenylephrine).<br />
<strong>The</strong> combination of alpha 1 -blockers and a betablocker<br />
could result in refractory hypotension because of<br />
potentially blunted response to beta 1 as well as alpha 1<br />
agonists. 26 Intoxication may result in nausea, vomiting,<br />
abdominal pain, hypotension, reflex tachycardia, and<br />
seizures.
14. Anesthetic Implications of Chronic Medications 201<br />
Digoxin<br />
Digoxin inhibits Na + /K + adenosine triphosphatase, leads<br />
to an increase in the intracellular concentration of Na + ,<br />
and thus (by stimulation of Na + –Ca 2+ exchange) an<br />
increase in the intracellular concentration of Ca 2+ . <strong>The</strong><br />
beneficial effects of digoxin result from direct actions on<br />
cardiac muscle, as well as indirect actions on the cardiovascular<br />
system mediated by effects on the autonomic<br />
nervous system. <strong>The</strong> autonomic effects include: (1) a<br />
vagomimetic action, which is responsible for the effects<br />
of digoxin on the SA and AV nodes, and (2) baroreceptor<br />
sensitization, which results in increased afferent inhibitory<br />
activity and reduced activity of the sympathetic<br />
nervous system and renin-angiotensin system for any<br />
given increment in mean arterial pressure. <strong>The</strong> pharmacologic<br />
consequences of these direct and indirect effects<br />
are: (1) a positive inotropic effect, (2) a decrease in the<br />
degree of activation of the sympathetic nervous system<br />
and renin-angiotensin system (neurohormonal deactivating<br />
effect), and (3) negative dromotropic and negative<br />
chronotropic effects. <strong>The</strong> effects of digoxin in heart failure<br />
are mediated by its positive inotropic and neurohormonal<br />
deactivating effects, whereas the effects of the drug in<br />
atrial arrhythmias are related to its vagomimetic actions.<br />
<strong>The</strong> most frequent cause of toxicity is renal failure. 27<br />
Digitalis toxicity is markedly increased in the presence<br />
of hypokalemia, and digitalis toxicity may be reversed to<br />
some degree by the administration of K + . Other causes of<br />
digitalis toxicity include hypomagnesemia, hypercalcemia,<br />
and hypothyroidism. Administration of digitalis can<br />
lead to the development of a wide variety of arrhythmias<br />
including sinus bradycardia and arrest, AV conduction<br />
delays, and second- or third-degree heart blocks. 28 Sympathomimetics<br />
with beta-adrenergic agonist effects as<br />
well as pancuronium 29 and intravenous administration of<br />
Ca 2+ may increase the likelihood of cardiac dysrhythmias.<br />
Oral antacids decrease the GI absorption of digitalis. 30,31<br />
Amiodarone<br />
Amiodarone is a potent class III antidysrhythmic agent<br />
with a wide spectrum of activity against refractory supraventricular<br />
and ventricular tachydysrhythmias. <strong>The</strong> antiarrhythmic<br />
effect of amiodarone may be attributed to at<br />
least two major properties: (1) a prolongation of the myocardial<br />
cell-action potential duration and refractory<br />
period, and (2) noncompetitive alpha- and beta-adrenergic<br />
inhibition. Antiadrenergic and Ca 2+ channel blocking<br />
effects contribute to peripheral vasodilation, bradycardia,<br />
conduction disturbances, negative inotropic effects, and<br />
hypotension. After oral dosing, however, amiodarone<br />
produces no significant change in left ventricular ejection<br />
fraction (LVEF), even in patients with depressed LVEF.<br />
After acute intravenous dosing, it may have a mild negative<br />
inotropic effect. Volatile anesthetics, beta-blockers,<br />
lidocaine, diltiazem, and verapamil can potentiate the<br />
cardiovascular and negative inotropic effects of amiodarone.<br />
32 Proarrhythmic side effects of amiodarone are<br />
reported in less than 1%–2% of patients. Pulmonary toxicity<br />
is a severe complication that may occur in up to 17%<br />
of patients treated long term. 33 Pulmonary complications<br />
may progress to adult respiratory distress syndrome and<br />
pulmonary fibrosis. Both hypothyroidism and hyperthyroidism<br />
can occur with chronic amiodarone therapy. 34<br />
Amiodarone treatment may also lead to increased liver<br />
function tests. Amiodarone inhibits CYP metabolisms<br />
resulting in increased levels of digoxin (by as much as<br />
70%), procainamide, quinidine, warfarin, and cyclosporine.<br />
It may also directly depress vitamin K-dependent<br />
clotting factors. Cimetidine can reduce the metabolism of<br />
amiodarone, and phenytoin increases its metabolism.<br />
Disopyramide<br />
Disopyramide is a class IA antiarrhythmic indicated in<br />
the treatment of life-threatening ventricular arrhythmias<br />
and is also used to treat supraventricular arrhythmias<br />
caused by reentrant mechanisms. Of all antiarrhythmic<br />
drugs, this is the most potent negative inotrope and<br />
reversible heart failure has been reported after its use. As<br />
many as 50% of patients with a history of heart failure<br />
may have a recurrence of the disease with an incidence<br />
of less than 5% in other patients. Disopyramide should<br />
not be used in patients with cardiogenic shock, AV block,<br />
or long QT intervals. It can lead to the development of<br />
second- or third-degree AV block or torsade de pointes<br />
ventricular tachycardia. 35 Disopyramide has strong anticholinergic<br />
side effects including dry mouth, impotence,<br />
urinary retention, constipation, and exacerbation of glaucoma.<br />
Because of the large number and severity of side<br />
effects, disopyramide is contraindicated in elderly<br />
patients.<br />
Beta Receptor Antagonists<br />
Beta receptors are G protein–coupled receptors found<br />
throughout the myocardium and nodal conduction tissue.<br />
Beta receptor blockers are competitive antagonists<br />
at beta-adrenergic receptor sites and are used in the<br />
management of hypertension, stable and unstable angina<br />
pectoris, cardiac arrhythmias, myocardial infarction,<br />
and heart failure. <strong>The</strong>se drugs have been shown to reduce<br />
mortality when administered prophylactically to patients<br />
undergoing major vascular surgery 36 who are at high<br />
risk for ischemia. Beta-blockers have also been found<br />
to reduce mortality and morbidity rates in patients with<br />
myocardial infarction 37 and congestive heart failure. 38<br />
<strong>The</strong>y are also given to control symptoms of sym -<br />
pathetic overactivity in alcohol withdrawal, anxiety states,
202 T.A. Szabo and R.D. Warters<br />
hyperthyroidism, and tremor, and in the prophylaxis of<br />
migraine and of bleeding associated with portal hypertension.<br />
Beta receptor antagonism manifests in decreased<br />
heart rate and increased diastolic perfusion.<br />
Beta-blockers belong to two general classifications,<br />
based on whether they are selective beta 1 antagonists or<br />
combined beta 1 and beta 2 antagonists. <strong>The</strong> beta 1 antagonists<br />
or those with intrinsic sympathomimetic activity at<br />
beta 2 receptors are “cardioselective” and are better suited<br />
for use in patients with asthma and bronchospastic disease<br />
and hypertension. With increasing doses of the cardioselective<br />
drugs, there is a decrease in receptor specificity.<br />
<strong>The</strong> beta-blockers with proven effects on prognosis<br />
include two selective beta 1 receptor blockers—metoprolol<br />
and bisoprolol—and three nonselective beta-blockers—timolol,<br />
propranolol, and carvedilol. Sotalol, a<br />
nonselective beta-blocker, which also has a pronounced<br />
class III antiarrhythmic effect, does not seem to have a<br />
significant effect on postinfarction mortality.<br />
Beta-blockers are generally well tolerated and most<br />
adverse effects are mild. <strong>The</strong> most frequent and serious<br />
adverse effects are heart failure, heart block, and bronchospasm.<br />
For this reason, these drugs must be used judiciously<br />
in patients with severe obstructive pulmonary<br />
disease, bradycardia, heart block, or uncompensated congestive<br />
heart failure. Abrupt withdrawal of beta-blockers<br />
may exacerbate angina and may lead to sudden death.<br />
Reduced peripheral circulation may exacerbate peripheral<br />
vascular disease such as Raynaud’s syndrome. CNS<br />
effects include headache, depression, dizziness, hallucinations,<br />
confusion, and sleep disturbances.<br />
Beta-blockers are eliminated by several metabolic<br />
pathways. Propranolol and metoprolol undergo hepatic<br />
metabolism, esmolol is biotransformed in the blood by<br />
esterases, atenolol is renally excreted, and timolol is eliminated<br />
by the kidney and the liver. <strong>The</strong> metabolism and<br />
route of excretion is important when considering patients<br />
with renal or hepatic disease.<br />
Coadministration of beta-blockers and propofol might<br />
result in cardiac events including severe bradycardia,<br />
sinus arrest, heart block, or even asystole. <strong>The</strong> myocardial<br />
depression seen with halothane is also exacerbated by<br />
beta-blockers. 39<br />
Calcium Channel Blockers<br />
CCBs inhibit the cellular influx of calcium by binding to<br />
specific drug receptors on L-type calcium channels and<br />
maintaining the channels in an inactive state. <strong>The</strong> L-type<br />
channel is the predominant type in heart and vascular<br />
smooth muscle.<br />
Three major classes of CCBs exist: the dihydropyridines,<br />
the phenylalkylamines, and the benzothiazepines.<br />
Each class binds to a unique site on the alpha 1 -subunit of<br />
the L-type channel. Dihydropyridine CCBs (such as nifedipine,<br />
nimodipine, and amlodipine) have a greater<br />
selectivity for vascular smooth muscle than for myocardium<br />
and their main effect is vasodilatation. <strong>The</strong>y have<br />
little or no action at the SA or AV nodes, and negative<br />
inotropic and chronotropic effects are minimal. <strong>The</strong>y are<br />
used for their antihypertensive and antianginal properties.<br />
Nimodipine crosses the blood–brain barrier and is<br />
used in cerebral ischemia. Benzothiazepine CCBs (such<br />
as diltiazem) and phenylalkylamine CCBs (such as verapamil)<br />
have less selective vasodilator activity. <strong>The</strong>y<br />
depress SA and AV nodal conduction and are used for<br />
their antiarrhythmic, antianginal, and antihypertensive<br />
properties. Verapamil has the most prominent negative<br />
inotropic effect and it may precipitate congestive heart<br />
failure in patients with preexisting left ventricular dysfunction.<br />
Diltiazem also reduces contractility, but the concurrent<br />
peripheral vasodilation may preserve cardiac<br />
output. Verapamil, nifedipine, and nicardipine are 90%<br />
protein-bound, and their clinical effects can be enhanced<br />
by drugs that increase the pharmacologically active<br />
unbound fraction (such as lidocaine or diazepam). Liver<br />
disease may necessitate reduced dosing of verapamil and<br />
diltiazem. 40<br />
CCBs may be responsible for several drug inter -<br />
actions and may have numerous adverse effects. <strong>The</strong><br />
coadministration of diltiazem and beta-blockers may<br />
yield profound bradycardia. Diltiazem decreases the<br />
clearance of a single dose of propranolol, metoprolol,<br />
and possibly atenolol; therefore, elevated concentrations<br />
of beta-blockers may be responsible for the brady -<br />
cardic effects. Cimetidine causes increases in plasmadiltiazem<br />
concentrations and in plasma-deacetyldiltiazem<br />
concentrations.<br />
<strong>The</strong> combination of verapamil and beta-blockers may<br />
result in bradycardia, heart block, and left ventricular<br />
failure. <strong>The</strong> risks are especially increased when both<br />
drugs are given intravenously. Bradycardia has also been<br />
reported in a patient treated with oral verapamil and<br />
timolol eye drops. 41 Verapamil is extensively metabolized<br />
in the liver and interactions may occur with drugs that<br />
inhibit or enhance hepatic metabolism. Verapamil inhibits<br />
the cytochrome P-450 isoenzyme CYP 3A4 and<br />
therefore may increase plasma concentrations of carbamazepine,<br />
cyclosporine, digoxin (by up to 70%), midazolam,<br />
sim vastatin, and theophylline. Verapamil and<br />
diltiazem have significant local anesthetic properties,<br />
because they block fast sodium channels, and therefore<br />
the risk of local anesthetic toxicity may be increased in<br />
patients taking these medications.<br />
Enhanced antihypertensive effects may be seen with<br />
the combination of nifedipine and beta-blockers. Heart<br />
failure has also been reported in a few patients with<br />
angina who were given nifedipine and a beta-blocker.<br />
Nifedipine may modify insulin and glucose responses.<br />
Nifedipine is extensively metabolized in the liver by the
14. Anesthetic Implications of Chronic Medications 203<br />
cytochrome P-450 isoenzyme CYP 3A4, and interactions<br />
may occur with quinidine (resulting in increased serum<br />
nifedipine concentrations), which shares the same metabolic<br />
pathway, and with enzyme inducers, such as carbamazepine,<br />
phenytoin, and rifampicin. Inhibition of the<br />
cytochrome P-450 system by cimetidine and erythromycin<br />
may lead to potentiation of the hypotensive effect.<br />
Decreased blood pressure from volatile anesthetics can<br />
be potentiated by concurrent administration of CCBs.<br />
Volatile anesthetics significantly decrease intracellular<br />
Ca 2+ in the myocardium, and thus augment the negative<br />
inotropic, dromotropic, and vasodilatory effects of<br />
CCBs. 42 CCBs potentiate depolarizing and nondepolarizing<br />
neuromuscular blockade, 43 and the antagonism of a<br />
nondepolarizing neuromuscular blockade may be blunted,<br />
because calcium is essential for the release of acetylcholine<br />
at the neuromuscular junction. Edrophonium may be<br />
more effective than neostigmine in reversing neuromuscular<br />
blockade that has been enhanced by CCBs. 44<br />
Angiotensin-Converting Enzyme Inhibitors<br />
Angiotensin-converting enzyme (ACE) inhibitors de -<br />
crease angiotensin II and aldosterone levels. <strong>The</strong>y have<br />
been shown to slow renal dysfunction in diabetic nephropathy<br />
and to improve long-term outcomes in heart failure<br />
trials. 45 Accumulation of captopril, lisinopril, and enalaprilat<br />
occurs in patients with renal impairment, and<br />
decreased glomerular filtration rate is seen in patients<br />
treated with ACE inhibitors. <strong>The</strong>se drugs should be<br />
avoided in patients with renal artery stenosis. Hyperkalemia<br />
is possible 46 because of reduced production of aldosterone;<br />
therefore, potassium levels should be monitored.<br />
<strong>The</strong> adverse effects of ACE inhibitors on the kidneys may<br />
be potentiated by other drugs, such as nonsteroidal antiinflammatory<br />
drugs (NSAIDs). Several ACE inhibitors<br />
are designed as prodrugs, and they must undergo hepatic<br />
conversion. Enalapril is the prodrug of the active ACE<br />
inhibitor, enalaprilat, and conversion may be affected in<br />
patients with hepatic dysfunction. Captopril and lisinopril<br />
are not prodrugs.<br />
<strong>The</strong> combination of NSAIDs and ACE inhibitors may<br />
have variable effects on renal function because they act<br />
at different parts of the glomerulus. When given to<br />
patients whose kidneys are underperfused (heart failure,<br />
hypovolemia, or cirrhosis), renal function may deteriorate.<br />
Indomethacin and possibly other NSAIDs, including<br />
aspirin, have been reported to reduce the hypotensive<br />
action of ACE inhibitors. Part of the hypotensive effect<br />
of ACE inhibitors may be prostaglandin-dependent,<br />
which might explain this interaction with drugs such as<br />
NSAIDs that block prostaglandin synthesis. Marked<br />
hypotension may occur during general anesthesia in<br />
patients receiving ACE inhibitors, therefore discontinuation<br />
of ACE inhibitor therapy before anesthesia should<br />
be considered. Excessive hypotension may occur when<br />
ACE inhibitors are used concurrently with diuretics or<br />
other antihypertensives. An additive hyperkalemic effect<br />
is possible in patients receiving ACE inhibitors with<br />
potassium-sparing diuretics, potassium supplements, or<br />
other drugs that can cause hyperkalemia (such as cyclosporine<br />
or indomethacin). Potassium-sparing diuretics<br />
and potassium supplements should generally be stopped<br />
before initiating ACE inhibitors in patients with heart<br />
failure.<br />
Pulmonary Drugs<br />
Beta Agonists<br />
Inhaled beta receptor agonists are a mainstay in the treatment<br />
of asthma. <strong>The</strong> primary action of beta agonists is to<br />
stimulate adenylyl cyclase, and thus increase adenosine<br />
3′,5′-cyclic monophosphate (cAMP). Increased levels of<br />
cAMP mediate smooth muscle relaxation and inhibit the<br />
inflammatory mediator release from mast cells. Metaproterenol<br />
was the first beta 2 selective agonist; however, albuterol<br />
is currently the most widely used agent. Adverse<br />
effects include tremor, tachycardia, hypertension, palpitations,<br />
nausea, and vomiting. 47 Direct-acting beta agonists<br />
should be administered with extreme caution to patients<br />
who are being treated with MAOIs (clorgyline, isocarboxazid,<br />
pargyline, phenelzine, selegiline), or within 2<br />
weeks of the discontinuation of an MAOI, because the<br />
action of the beta agonist on the vascular system may be<br />
exaggerated. Acute metabolic responses include hyperglycemia,<br />
hypokalemia, and hypomagnesemia. Despite<br />
the relative beta 2 selectivity of these agents, higher doses<br />
can stimulate both beta 1 and beta 2 receptors. Prophylactic<br />
administration of beta agonists 1 hour before induction<br />
of general anesthesia results in reduced airway resistance<br />
after endotracheal intubation. 48<br />
<strong>The</strong>ophylline<br />
<strong>The</strong>ophylline is a phosphodiesterase inhibitor, leading to<br />
increased cellular concentrations of cAMP and cGMP<br />
(cyclic guanosine 3′,5′-monophosphate). <strong>The</strong> combination<br />
of phosphodiesterase inhibition, inflammatory inhibition,<br />
and catecholamine release may all contribute to<br />
smooth muscle relaxation and bronchodilation. <strong>The</strong>ophylline<br />
is eliminated mainly by hepatic metabolism and<br />
usual doses can be given to patients with renal impairment.<br />
Its metabolism and clearance are greatly affected<br />
by concurrent disease states and altered physiology<br />
including liver disease, pulmonary edema, chronic<br />
obstructive pulmonary disease, and thyroid disease. Phenytoin<br />
markedly decreases the elimination half-life and<br />
increases the clearance of theophylline by up to 350%,
204 T.A. Szabo and R.D. Warters<br />
probably as a result of hepatic enzyme induction. Carbamazepine<br />
and rifampin have been observed to increase<br />
theophylline elimination. However, cimetidine, erythromycin,<br />
amiodarone, mexiletine, and tacrine inhibit its<br />
hepatic metabolism. <strong>The</strong>ophylline may enhance lithium<br />
elimination with a consequent loss of effect.<br />
Specific drug interactions with numerous anestheticrelated<br />
medications have been described. <strong>The</strong>re is a risk<br />
of synergistic toxicity if theophylline is used in the presence<br />
of halothane 49 because of the sensitizing effects of<br />
halothane on the myocardium to increased catecholamines<br />
released by theophylline. Larger doses of benzodiazepines<br />
may be needed to achieve a desired effect,<br />
because benzodiazepines increase the CNS concentrations<br />
of adenosine, a potent CNS depressant, whereas<br />
theophylline blocks adenosine receptors. Ketamine may<br />
decrease the theophylline seizure threshold, 50 and theophylline<br />
can antagonize the effect of nondepolarizing<br />
neuromuscular blockers possibly because of phosphodiesterase<br />
inhibition. <strong>The</strong>ophylline can precipitate sinus<br />
tachycardia, multifocal atrial tachycardia, and supraventricular<br />
and ventricular premature contractions at therapeutic<br />
or supratherapeutic serum concentrations. It can<br />
also potentiate hypokalemia associated with the administration<br />
of beta 2 agonists, corticosteroids, and diuretics.<br />
Gastrointestinal Drugs<br />
Cimetidine<br />
Cimetidine is a competitive antagonist for histamine at<br />
the H 2 receptor. Cimetidine is metabolized in the liver<br />
where it binds to cytochrome P-450 and interferes with<br />
the metabolism of several drugs including amiodarone,<br />
warfarin, theophylline, phenytoin, lidocaine, quinidine,<br />
tricyclic antidepressants, and propranolol. 51 <strong>The</strong> effects of<br />
cimetidine on carbamazepine plasma concentration may<br />
be temporary; however, carbamazepine toxicity, manifesting<br />
in ataxia, nystagmus, diplopia, headache, vomiting,<br />
apnea, seizures, and coma, may occur with cimetidine<br />
coadministration. Carvedilol is significantly metabolized<br />
by the cytochrome P-450 enzyme system. Increased<br />
adverse effects of carvedilol (dizziness, insomnia, GI<br />
symptoms, postural hypotension) may result when the<br />
drug is administered with cimetidine. Cimetidine also<br />
decreases the clearance of benzodiazepines that are<br />
metabolized by hydroxylation or dealkylation (e.g., diazepam,<br />
chlordiazepoxide, clorazepate, flurazepam, prazepam,<br />
halazepam, alprazolam, triazolam, midazolam,<br />
quazepam, bromazepam). Adverse effects such as pronounced<br />
sedation and impaired cognitive and psychomotor<br />
function have been reported. Benzodiazepines for<br />
which nitroreduction is a prominent metabolic pathway<br />
might also have their clearance decreased by cimetidine<br />
(e.g., nitrazepam, clonazepam). Those benzodiazepines<br />
eliminated primarily by glucuronidation do not interact<br />
with cimetidine (e.g., lorazepam, oxazepam, temazepam).<br />
Hepatic metabolism of cimetidine may be enhanced if<br />
phenobarbital is administered concurrently. Cimetidine<br />
crosses the blood–brain barrier and interacts with cerebral<br />
H 2 receptors. Consequently, headaches, somnolence,<br />
confusion, and delirium may occur. Delayed awakening<br />
from anesthesia has been attributed to lingering CNS<br />
effects of cimetidine. Bradycardia, tachycardia, cardiac<br />
dysrhythmias, and hypotension may occur because of<br />
interaction with cardiac H 2 receptors. <strong>The</strong>se events have<br />
generally been associated with rapid intravenous infusion.<br />
Cimetidine may cause impotence, loss of libido, and<br />
gynecomastia (by increasing the plasma concentration of<br />
prolactin) in male patients.<br />
Metoclopramide<br />
Metoclopramide is a dopamine antagonist and a selective<br />
peripheral cholinergic agonist useful for reducing gastric<br />
fluid volume by increasing lower esophageal sphincter<br />
tone, speeding gastric emptying time, and acting as an<br />
antiemetic. Side effects include hypotension, sedation,<br />
dysphoria, rash, and dry mouth. Anxiety, restlessness, and<br />
drowsiness may occur with rapid administration of undiluted<br />
metoclopramide. Bradycardia, supraventricular<br />
arrhythmias, complete heart block, and asystole have also<br />
been reported after administration of single doses of<br />
intravenous metoclopramide. <strong>The</strong> drug blocks dopaminergic<br />
receptors in the CNS, thereby inducing secretion<br />
of prolactin and creating the possibility of extrapyramidal<br />
symptoms. 51 Metoclopramide should be avoided in the<br />
presence of GI obstruction or after GI surgery and in<br />
patients taking MAOIs, tricyclic antidepressants, or other<br />
drugs that may cause extrapyramidal symptoms. By inhibiting<br />
pseudocholinesterase, metoclopramide may elicit<br />
prolonged responses to succinylcholine. 52<br />
Oral Anticoagulants<br />
Warfarin<br />
Warfarin is an anticoagulant that inhibits the hepatic conversion<br />
of four vitamin K-dependent coagulation factors<br />
(II, VII, IX, and X) and two anticoagulant proteins<br />
(protein C and S). It is indicated for the prophylaxis and/<br />
or treatment of venous thrombosis, pulmonary embolism,<br />
thromboembolic complications associated with atrial<br />
fibrillation, and/or cardiac valve replacement, and to<br />
reduce the risk of death, recurrent myocardial infarction,<br />
and stroke after myocardial infarction. An anticoagulation<br />
effect generally occurs within 24 hours after drug<br />
administration. However, peak anticoagulant effect may
14. Anesthetic Implications of Chronic Medications 205<br />
be delayed 72–96 hours when the vitamin K-dependent<br />
procoagulant proteins are reduced by 30%–50% of<br />
normal, which is consistent with international normalized<br />
ratio (INR) values in the range of 2–3. Warfarin is metabolized<br />
by hepatic cytochrome P-450 to inactive hydroxylated<br />
metabolites (predominant route) and by reductases<br />
to reduced metabolites. <strong>The</strong> metabolites are principally<br />
excreted into the urine and bile. No dosage adjustment is<br />
necessary for patients with renal failure. Hepatic dysfunction<br />
can potentiate the response to warfarin through<br />
impaired synthesis of clotting factors and decreased<br />
metabolism of warfarin. Discontinuation of warfarin will<br />
result in normalization of the prothrombin time (PT)/<br />
INR in 3 days unless the patient has substantial liver<br />
disease or vitamin K deficiency. Warfarin is >98% bound<br />
to albumin, meaning that only 1%–2% of the circulating<br />
drug accounts for the entire biologic effect.<br />
Pyrazole NSAIDs (e.g., phenylbutazone) compete<br />
effectively for the same binding sites and may significantly<br />
increase bleeding risks when coadministered with<br />
warfarin. Amiodarone also inhibits the metabolic clearance<br />
of warfarin. Second- and third-generation cephalosporins<br />
augment the anticoagulant effect by inhibiting<br />
the cyclic interconversion of vitamin K. Aspirin and<br />
NSAIDs inhibit platelet function and have the potential<br />
to increase the risk of warfarin-associated bleeding. 53,54<br />
Patients 60 years or older seem to exhibit greater than<br />
expected PT/INR response to the anticoagulant effects<br />
of warfarin. <strong>The</strong> cause of the increased sensitivity to warfarin<br />
in this age group is unknown. <strong>The</strong>refore, as patient<br />
age increases, a lower dose of warfarin is usually<br />
required.<br />
Ticlopidine<br />
Ticlopidine is a platelet aggregation inhibitor. Its active<br />
metabolite blocks platelet surface adenosine 5′-diphosphate<br />
(ADP) receptors and, subsequently, ADP-induced<br />
binding of fibrinogen to the platelet GPIIb/IIIa receptor<br />
is inhibited. Ticlopidine may also block the binding of von<br />
Willebrand factor to platelets. <strong>The</strong> effect on platelet function<br />
is irreversible. Ticlopidine should be stopped 2 weeks<br />
before elective surgery. It may cause hepatic impairment,<br />
neutropenia, agranulocytosis, and thrombotic thrombocytopenic<br />
purpura. It should be avoided in patients with<br />
hepatic insufficiency. Intracranial and GI bleeding are also<br />
serious complications. 55–57 Ticlopidine potentiates the<br />
effect of aspirin or other NSAIDs on platelet aggregation.<br />
In clinical studies, ticlopidine was used concomitantly with<br />
beta-blockers, CCBs, and diuretics without evidence of<br />
clinically significant adverse interactions. <strong>The</strong> safety of<br />
concomitant use of ticlopidine and NSAIDs has not been<br />
established. Clearance of ticlopidine decreases with age.<br />
Steady-state trough values in elderly patients are approximately<br />
twice those in younger volunteer populations.<br />
Nonsteroidal Antiinflammatory Drugs<br />
NSAIDs are the most frequently prescribed drugs worldwide<br />
and are responsible for 21% of all adverse reactions<br />
reported each year to the spontaneous drug reporting<br />
system of the United States Food and Drug Administration.<br />
58 NSAIDs are nonselective inhibitors of both<br />
cyclooxygenase (COX)-1 and COX-2. Absorption, peak<br />
plasma concentration, and metabolism can be significantly<br />
affected by GI pH, concomitant administration of<br />
other drugs, and the disease state of the patient. Antacids<br />
and mucoprotective agents can delay the absorption of<br />
NSAIDs. Elimination is largely dependent on hepatic<br />
biotransformation and renal excretion. <strong>The</strong>refore, patients<br />
with hepatic and renal disease often demonstrate greater<br />
and more prolonged peak plasma concentrations. Acute<br />
renal impairment, papillary necrosis, acute interstitial<br />
nephritis, and nephrotic syndrome have all been attributed<br />
to NSAIDs. 59 In the presence of renal vasoconstriction,<br />
the vasodilator action of prostaglandins increases<br />
renal blood flow and thereby helps to maintain renal<br />
function. Patients whose renal function is being maintained<br />
by prostaglandins are therefore at risk from<br />
NSAIDs. Such patients include those with impaired circulation,<br />
the elderly, those taking diuretics, and those with<br />
heart failure or renal vascular disease. Serious hepatotoxicity<br />
is rare with typical therapeutic doses. <strong>The</strong> underlying<br />
mechanism seems to be immunologic; however, aspirin<br />
and phenylbutazone may have direct toxic effects. <strong>The</strong>se<br />
drugs are frequently administered with opioid agents to<br />
enhance their analgesic potential. Naproxen (Naprosyn,<br />
Avaprox, Aleve), oxaprozin (Daypro), and piroxicam<br />
(Feldene) are considered potentially inappropriate for<br />
the elderly, because these medications all have the potential<br />
to produce hypertension, heart failure, renal failure,<br />
and GI adverse effects.<br />
Ketorolac<br />
Immediate and long-term use should be avoided in older<br />
patients, because a significant number have asymptomatic<br />
GI pathologic conditions. NSAID gastropathy (dyspepsia,<br />
nausea, epigastric pain) is one of the most frequent<br />
drug-related side effects in the United States. 60<br />
Indomethacin<br />
All NSAIDs should be considered capable of causing<br />
confusion in the elderly. <strong>The</strong> more readily lipid-soluble<br />
agents would be expected to cross the blood–brain barrier<br />
easier and hence cause greater CNS adverse effects<br />
than less lipophilic NSAIDs. Of all available NSAIDs,<br />
indomethacin produces the most CNS adverse effects,<br />
including cognitive dysfunction, confusion, excessive
206 T.A. Szabo and R.D. Warters<br />
somnolence, and behavioral disturbances. 61 Indomethacin<br />
may also accelerate the rate of cartilage destruction<br />
in patients with osteoarthritis.<br />
H 1 Receptor Antagonists<br />
<strong>The</strong>se drugs are competitive, selective, and reversible<br />
antagonists of histamine on the H 1 receptor. First-generation<br />
antagonists may also activate muscarinic cholinergic,<br />
serotonin, or alpha-adrenergic receptors. Second-generation<br />
antagonists are unlikely to produce CNS side effects.<br />
Nonanticholinergic antihistamines are preferred in<br />
elderly patients when treating allergic reactions.<br />
Diphenhydramine<br />
Diphenhydramine is a first-generation H 1 receptor antagonist.<br />
It may cause confusion and sedation. Anticholinergic<br />
effects such as dry mouth, blurred vision, and urinary<br />
retention may be noted. Tachycardia, cardiac dysrhythmias,<br />
and prolongation of the QT interval may occur. <strong>The</strong><br />
drug should not be used as a hypnotic, and when used to<br />
treat emergency allergic reactions, it should be used in<br />
the smallest possible dose. 62<br />
Hydroxyzine, Chlor-Trimeton<br />
<strong>The</strong>se are first-generation H 1 receptor antagonists with<br />
potent anticholinergic properties and as such are considered<br />
potentially inappropriate for older adults.<br />
Opioids<br />
Administration of narcotics (with the exception of meperidine)<br />
usually results in decreased heart rate. SA node<br />
depression and prolonged AV conduction can occur, as<br />
can sinus arrest and even asystole. Decreased sympathetic<br />
tone and histamine release (morphine and meperidine)<br />
can contribute to hypotension. Hypotensive effects<br />
are most prominent in patients with increased sympathetic<br />
tone, such as those with congestive heart failure or<br />
hypovolemia. Orthostatic hypotension may be seen in<br />
patients with autonomic neuropathy (e.g., diabetics).<br />
Meperidine, because of its structural similarity to atropine,<br />
may increase the heart rate. In large doses it has<br />
negative inotropic effects and can prolong the duration<br />
of action potential, potentiating class I antiarrhythmics.<br />
Meperidine has a bad reputation in the elderly for causing<br />
confusion and delirium. 63 Opioids may lessen total anesthetic<br />
requirements: a single dose of fentanyl may<br />
decrease the minimal anesthetic concentration (MAC) of<br />
isoflurane or desflurane by 50%. Likewise, alfentanil and<br />
remifentanil may also exhibit anesthetic-sparing effects.<br />
Mixed agonist-antagonists are less effective than pure<br />
agonists in reducing MAC. <strong>The</strong> ceiling effect for MAC<br />
parallels the ceiling effect for respiratory depression.<br />
Nalbuphine decreases MAC by only 8%.<br />
Pentazocine<br />
Pentazocine is a benzomorphan derivative that possesses<br />
agonist (delta and kappa receptors) as well as weak<br />
antagonist actions. <strong>The</strong> most common side effect of pentazocine<br />
is sedation, followed by diaphoresis and dizziness.<br />
Pentazocine increases the plasma concentration of<br />
catecholamines, which may account for increases in heart<br />
rate, systemic blood pressure, and pulmonary artery pressure.<br />
Confusion and hallucinations limit its use in the<br />
elderly. 64 Pentazocine decreases MAC by 20%.<br />
Propoxyphene<br />
Propoxyphene offers few analgesic advantages over acetaminophen<br />
or aspirin, yet has the adverse effects of other<br />
narcotics. <strong>The</strong> only clinical use of propoxyphene is treatment<br />
of mild-to-moderate pain that is not adequately<br />
relieved by the above two drugs. It does not possess<br />
antipyretic or antiinflammatory effects, and its antitussive<br />
activity is not significant. <strong>The</strong> most common side effects<br />
of propoxyphene are vertigo, sedation, nausea, and<br />
vomiting. Overdose—especially in combination with<br />
alcohol—is complicated by seizures and depression of<br />
ventilation. 65,66 Propoxyphene may slow the metabolism<br />
of concomitantly administered antidepressants, anticonvulsants,<br />
or warfarin-like drugs. Severe neurologic signs,<br />
including coma, have occurred with concurrent use of<br />
carbamazepine.<br />
Conclusions<br />
<strong>The</strong> large number and variety of chronic medications<br />
prescribed to elderly patients presenting for surgery<br />
greatly complicate the preoperative assessment and anesthetic<br />
management of geriatric patients. <strong>The</strong> various<br />
interactions of medications on metabolism and end effects<br />
must be understood and considered when formulating an<br />
appropriate anesthetic plan.<br />
References<br />
1. Beers MH. Explicit criteria for determining potentially<br />
inappropriate medication use by the elderly. An update.<br />
Arch Intern Med 1997;157(14):1531–1536.<br />
2. Fick DM, Cooper JW, Wade WE, et al. Updating the Beers<br />
criteria for potentially inappropriate medication use in<br />
older adults. Arch Intern Med 2003;163(22):2716–2724.<br />
3. van der Hooft CS, Jong GW, Dieleman JP, et al. Inappropriate<br />
drug prescribing in older adults: the updated 2002 Beers
14. Anesthetic Implications of Chronic Medications 207<br />
criteria—a population-based cohort study. Br J Clin Pharmacol<br />
2005;60(2):137–144.<br />
4. Willcox SM, Himmelstein DU, Woolhandler S. Inappropriate<br />
drug prescribing for the community-dwelling elderly.<br />
JAMA 1994;272(4):292–296.<br />
5. Zhan C, Sangl J, Bierman AS, et al. Potentially inappropriate<br />
medication use in the community-dwelling elderly: findings<br />
from the 1996 Medical Expenditure Panel Survey.<br />
JAMA 2001;286(22):2823–2829.<br />
6. Pitkala KH, Strandberg TE, Tilvis RS. Inappropriate drug<br />
prescribing in home-dwelling, elderly patients: a populationbased<br />
survey. Arch Intern Med 2002;162(15):1707–1712.<br />
7. Guilleminault C. Benzodiazepines, breathing, and sleep. Am<br />
J Med 1990;88(3A):25S–28S.<br />
8. Faust RJ, Cucchiara RF, Rose SH, et al. <strong>Anesthesiology</strong><br />
Review. 3rd ed. Philadelphia: Churchill Livingstone; 2002.<br />
9. Sanders LD, Whitehead C, Gildersleve CD, et al. Interaction<br />
of H2-receptor antagonists and benzodiazepine sedation. A<br />
double-blind placebo-controlled investigation of the effects<br />
of cimetidine and ranitidine on recovery after intravenous<br />
midazolam. Anaesthesia 1993;48(4):286–292.<br />
10. Salonen M, Reid K, Maze M. Synergistic interaction between<br />
alpha 2-adrenergic agonists and benzodiazepines in rats.<br />
<strong>Anesthesiology</strong> 1992;76(6):1004–1011.<br />
11. Ruff R, Reves JG. Hemodynamic effects of a lorazepamfentanyl<br />
anesthetic induction for coronary artery bypass<br />
surgery. J Cardiothorac Anesth 1990;4(3):314–317.<br />
12. Spivey WH. Flumazenil and seizures: analysis of 43 cases.<br />
Clin <strong>The</strong>r 1992;14(2):292–305.<br />
13. Luger TJ, Hill HF, Schlager A. Can midazolam diminish<br />
sufentanil analgesia in patients with major trauma? A retrospective<br />
study of 43 patients. Drug Metabol Drug Interact<br />
1992;10:177–184.<br />
14. Megarbane B, Leprince P, Deye N, et al. Extracorporeal life<br />
support in a case of acute carbamazepine poisoning with<br />
life-threatening refractory myocardial failure. Intensive<br />
Care Med 2006;32(9):1409–1413.<br />
15. Spina E, Pisani F, Perucca E. Clinically significant pharmacokinetic<br />
drug interactions with carbamazepine. An update.<br />
Clin Pharmacokinet 1996;31(3):198–214.<br />
16. Sweet RA, Brown EJ, Heimberg RG, et al. Monoamine<br />
oxidase inhibitor dietary restrictions: what are we asking<br />
patients to give up? J Clin Psychiatry 1995;56(5):196–201.<br />
17. Brown C, Taniguchi G, Yip K. <strong>The</strong> monoamine oxidase<br />
inhibitor-tyramine interaction. J Clin Pharmacol 1989;<br />
29(6):529–532.<br />
18. Gillman PK. Monoamine oxidase inhibitors, opioid analgesics<br />
and serotonin toxicity. Br J Anaesth 2005;95(4):<br />
434–441.<br />
19. Pacher P, Kecskemeti V. Cardiovascular side effects of<br />
new antidepressants and antipsychotics: new drugs, old concerns?<br />
Curr Pharm Des 2004;10(20):2463–2475.<br />
20. Tung A, Chang JL, Garvey E, et al. Tricyclic antidepressants<br />
and cardiac arrhythmias during halothane-pancuronium<br />
anesthesia. Anesth Prog 1981;28(2):44, 48–49.<br />
21. Young R. Update on Parkinson’s disease. Am Fam Physician<br />
1999;59(8):2155–2167.<br />
22. Jackson S, Ham RJ, Wilkinson D. <strong>The</strong> safety and tolerability<br />
of donepezil in patients with Alzheimer’s disease. Br J Clin<br />
Pharmacol 2004;58:1–8.<br />
23. Hossain M, Jhee SS, Shiovitz T, et al. Estimation of the<br />
absolute bioavailability of rivastigmine in patients with mild<br />
to moderate dementia of the Alzheimer’s type. Clin Pharmacokinet<br />
2002;41:225–234.<br />
24. Watkins PB, Zimmermann HJ, Knapp MJ, et al. Hepato -<br />
toxic effects of tacrine administration in patients with<br />
Alzheimer’s disease. JAMA 1994;271:992–998.<br />
25. Burns A, O’Brien J, BAP Dementia Consensus Group,<br />
et al. Clinical practice with anti-dementia drugs: a consensus<br />
statement from British Association for Psychopharmacology.<br />
J Psychopharmacol 2006;20:732–755.<br />
26. Stoelting RK. Pharmacology and Physiology in Anesthetic<br />
Practice. 3rd ed. Philadelphia: Lippincott-Raven; 1999.<br />
27. Van Deusen SK, Birkhahn RH, Gaeta TJ. Treatment of<br />
hyperkalemia in a patient with unrecognized digitalis toxicity.<br />
J Toxicol Clin Toxicol 2003;41(4):373–376.<br />
28. Dec GW. Digoxin remains useful in the management of<br />
chronic heart failure. Med Clin North Am 2003;87(2):317–<br />
337.<br />
29. Bartolone RS, Rao TL. Dysrhythmias following muscle<br />
relaxant administration in patients receiving digitalis. <strong>Anesthesiology</strong><br />
1983;58(6):567–569.<br />
30. Crome P, Curl B, Holt D, et al. Digoxin and cimetidine:<br />
investigation of the potential for a drug interaction. Hum<br />
Toxicol 1985;4(4):391–399.<br />
31. Mouser B, Nykamp D, Murphy JE, et al. Effect of cimetidine<br />
on oral digoxin absorption. DICP 1990;24(3):286–288.<br />
32. Rooney RT, Marijic J, Stommel KA, et al. Additive cardiac<br />
depression by volatile anesthetics in isolated hearts after<br />
chronic amiodarone treatment. Anesth Analg 1995;85(5):<br />
917–924.<br />
33. Camus P, Martin WJ 2nd, Rosenow EC 3rd. Amiodarone<br />
pulmonary toxicity. Clin Chest Med 2004;25(1):65–75.<br />
34. Ursella S, Testa A, Mazzone M, et al. Amiodarone-induced<br />
thyroid dysfunction in clinical practice. Eur Rev Med Pharmacol<br />
Sci 2006;10(5):269–278.<br />
35. Choudhury L, Grais IM, Passman RS. Torsades de pointes<br />
due to drug interaction between disopyramide and clarithromycin.<br />
Heart Dis 1999;1(4):206–207.<br />
36. Feringa HH, Bax JJ, Boersma E, et al. High-dose betablockers<br />
and tight heart rate control reduce myocardial<br />
ischemia and troponin T release in vascular surgery patients.<br />
Circulation 2006;114(1 Suppl):I344–349.<br />
37. Kopecky SL. Effect of beta blockers, particularly carvedilol,<br />
on reducing the risk of events after acute myocardial infarction.<br />
Am J Cardiol 2006;98(8):1115–1119.<br />
38. Pedersen ME, Cockcroft JR. <strong>The</strong> latest generation of betablockers:<br />
new pharmacologic properties. Curr Hypertens<br />
Rep 2006;8(4):279–286.<br />
39. Hayashi Y, Sumikawa K, Kuro M, et al. Roles of beta 1- and<br />
beta 2-adrenoceptors in the mechanism of halothane myocardial<br />
sensitization in dogs. Anesth Analg 1991;72(4):<br />
435–439.<br />
40. Grossman E, Messerli FH. Calcium antagonists. Prog Cardiovasc<br />
Dis 2004;47(1):34–57.<br />
41. Pringle SD, MacEwen CJ. Severe bradycardia due to interaction<br />
of timolol eye drops and verapamil. BMJ 1987;<br />
294:155–156.<br />
42. Wood M. Pharmacokinetic drug interactions in anaesthetic<br />
practice. Clin Pharmacokinet 1991;21(4):285–307.
208 T.A. Szabo and R.D. Warters<br />
43. Wali FA. Interaction of verapamil with gallamine and pancuronium<br />
and reversal of combined neuromuscular blockade<br />
with neostigmine and edrophonium. Eur J Anaesthesiol<br />
1986;3(5):385–393.<br />
44. Baciewicz AM, Baciewicz FA Jr. Effect of cimetidine and<br />
ranitidine on cardiovascular drugs. Am Heart J 1989;118(1):<br />
144–154.<br />
45. Ray S, Dargie H. Infarct-related heart failure: the choice of<br />
ACE inhibitor does not matter. Cardiovasc Drugs <strong>The</strong>r<br />
1994;8(3):433–436.<br />
46. Cruz CS, Cruz A, Marcilio de Souza CA. Hyperkalaemia<br />
in congestive heart failure patients using ACE inhibitors<br />
and spironolactone. Nephrol Dial Transplant 2003;18(9):<br />
1814–1819.<br />
47. Huerta C, Lanes SF, Garcia Rodriguez LA. Respiratory<br />
medications and the risk of cardiac arrhythmias. Epidemiology<br />
2005;16(3):360–366.<br />
48. Wu RS, Wu KC, Wong TK, et al. Effects of fenoterol and<br />
ipratropium on respiratory resistance of asthmatics after<br />
tracheal intubation. Br J Anaesth 2000;84(3):358–362.<br />
49. Koehntop DE, Liao JC, Van Bergen FH. Effects of pharmacologic<br />
alterations of adrenergic mechanisms by cocaine,<br />
tropolone, aminophylline, and ketamine on epinephrineinduced<br />
arrhythmias during halothane-nitrous oxide anesthesia.<br />
<strong>Anesthesiology</strong> 1977;46(2):83–93.<br />
50. Hirshman CA, Krieger W, Littlejohn G, et al. Ketamineaminophylline-induced<br />
decrease in seizure threshold. <strong>Anesthesiology</strong><br />
1982;56(6):464–467.<br />
51. Flockhart DA, Desta Z, Mahal SK. Selection of drugs to<br />
treat gastro-oesophageal reflux disease: the role of drug<br />
interactions. Clin Pharmacokinet 2000;39(4):295–309.<br />
52. Kao YJ, Tellez J, Turner DR. Dose-dependent effect of<br />
metoclopramide on cholinesterases and suxamethonium<br />
metabolism. Br J Anaesth 1990;65(2):220–224.<br />
53. Gaga BF, Birman-Deych E, Kerzner R, et al. Incidence of<br />
intracranial hemorrhage in patients with atrial fibrillation<br />
who are prone to fall. Am J Med 2005;118(6):612–617.<br />
54. Cappuzzo KA. Anticoagulation in elderly patients who fall<br />
frequently: a therapeutic dilemma. Consult Pharm 2005;<br />
20(7):601–605.<br />
55. Sloane PD, Zimmerman S, Brown LC, et al. Inappropriate<br />
medication prescribing in residential care/assisted living<br />
facilities. J Am Geriatr Soc 2002;50(6):1001–1011.<br />
56. Kubler PA, Pillans PI, Marrinan MC, et al. Concordance<br />
between clopidogrel use and prescribing guidelines. Intern<br />
Med J 2004;34(12):663–667.<br />
57. Maio V, Yuen EJ, Novielli K, et al. Potentially inappropriate<br />
medication prescribing for elderly outpatients in Emilia<br />
Romagna, Italy: a population-based cohort study. Drugs<br />
Aging 2006;23(11):915–924.<br />
58. Rossi AC, Hsu JP, Faich GA. Ulcerogenicity of piroxicam:<br />
an analysis of spontaneously reported data. Br Med J (Clin<br />
Res Ed) 1987;294(6565):147–150.<br />
59. Johnson AG, Day RO. <strong>The</strong> problems and pitfalls of NSAID<br />
therapy in the elderly. Drugs Aging 1991;1(2):130–143.<br />
60. Butt JH, Barthel JS, Moore RA. Clinical spectrum of<br />
the upper gastrointestinal effects of nonsteroidal antiinflammatory<br />
drugs. Natural history, symptomatology, and<br />
significance. Am J Med 1988;84(2A):5–14.<br />
61. Goodwin JS, Regan M. Cognitive dysfunction associated<br />
with naproxen and ibuprofen in the elderly. Arthritis Rheum<br />
1982;25(8):1013–1015.<br />
62. Caterino JM, Emond JA, Camargo CA Jr. Inappropriate<br />
medication administration to the acutely ill elderly: a<br />
nationwide emergency department study, 1992–2000. J Am<br />
Geriatr Soc 2004;52(11):1847–1855.<br />
63. Fong HK, Sands LP, Leung JM. <strong>The</strong> role of postoperative<br />
analgesia in delirium and cognitive decline in elderly<br />
patients: a systematic review. Anesth Analg 2006;102:1255–<br />
1266.<br />
64. Davis MP, Srivastava M. Demographics, assessment and<br />
management of pain in the elderly. Drugs Aging 2003;<br />
20(1):23–57.<br />
65. Barkin RL, Barkin SJ, Barkin DS. Propoxyphene (dextropropoxyphene):<br />
a critical review of a weak opioid analgesic<br />
that should remain in antiquity. Am J <strong>The</strong>r 2006;13(6):<br />
534–542.<br />
66. Kamal-Bahl SJ, Stuart BC, Beers MH. Propoxyphene use<br />
and risk for hip fractures in older adults. Am J Geriatr<br />
Pharmacother 2006;4(3):219–226.
15<br />
<strong>The</strong> Pharmacology of Opioids<br />
Steven L. Shafer and Pamela Flood<br />
<strong>The</strong>re are a lot of old people. In the 1990 census, patients<br />
over the age of 65 comprised 12% of the United States<br />
population, or 30,000,000 people. That grew modestly, to<br />
12.5%, by 2000. However, based on the United States<br />
population of 301,165,915 as of today,* that amounts to<br />
38 million individuals. It should come as no surprise,<br />
therefore, that health care for the elderly consumes 5%<br />
of the United States gross domestic product. 1<br />
It is important that anesthesiologists understand the<br />
differences in pharmacology of opioids in elderly patients<br />
in order to be able to properly titrate these important<br />
analgesics. Below are the key points for this chapter:<br />
1. Elderly patients need about half the dose as younger<br />
patients.<br />
2. <strong>The</strong> reason is primarily pharmacodynamic (change<br />
in intrinsic sensitivity of the brain to the drug). <strong>The</strong> pharmacokinetic<br />
changes with age are modest.<br />
3. Studies in elderly animals show reduced numbers of<br />
µ receptors with increased age. That does not explain the<br />
reduction in dose, as decreased receptor density should<br />
decrease sensitivity to opioids. <strong>The</strong> enhancement in drug<br />
effect seen in the clinic is more likely attributable to<br />
changes in cyclonucleotide coupling and other downstream<br />
changes that occur in aging.<br />
4. Meperidine is a difficult drug to use in elderly<br />
patients. It should never be used in patient-controlled<br />
analgesia (PCA) and is best reserved for shivering.<br />
General Observations<br />
Opioids are among the most effective, and the most dangerous,<br />
of the drugs administered by anesthesiologists.<br />
This is why the World Health Organization proposed a<br />
three-step analgesic ladder for the treatment of chronic<br />
pain. <strong>The</strong>y recommended starting with acetaminophen<br />
*www.census.gov. Accessed February 17, 2007.<br />
and nonsteroidal analgesics, progressing to opioids of<br />
intermediate strength, such as codeine, and treating<br />
severe pain with strong opioids such as morphine. 2<br />
<strong>The</strong> Agency for Health Care Policy and Research (now<br />
called the Agency for Healthcare Research and Quality)<br />
has issued similar guidelines. 3 Particular care must<br />
be taken when using opioids in elderly patients. It is<br />
nearly tautologic that elderly patients are more likely to<br />
suffer from chronic diseases than their younger counterparts.<br />
Some fortunate individuals remain physically vigorous<br />
until very late in life, whereas others seem to<br />
deteriorate physically at younger ages. Additionally, the<br />
cumulative effects of smoking, alcohol, and environmental<br />
toxins can accelerate the deterioration of aging in<br />
exposed individuals. Thus, it is not surprising that variability<br />
in physiology increases throughout life. 4 Increased<br />
physiologic variability results in increased pharmacokinetic<br />
and pharmacodynamic variability in elderly subjects.<br />
<strong>The</strong> clinical result of this increased variability is an<br />
increased incidence of adverse drug reactions in elderly<br />
patients. 5 Thus, elderly patients require more careful<br />
titration and, where possible and appropriate, therapeutic<br />
drug monitoring. 6<br />
In their secondary analysis of a retrospective cohort<br />
study, Cepeda and colleagues 7 noted that the risk of<br />
opioid-induced ventilatory depression increased with<br />
increasing age, with patients 61–70 years of age having<br />
2.8 times the risk of ventilatory depression compared<br />
with patients 16–45 years old. Interestingly, in their analysis,<br />
they converted all of the opioids into morphine equivalents,<br />
and the conversion did not account for the<br />
increased potency of opioids in the elderly that will be<br />
described subsequently.<br />
Although the risk of respiratory depression from<br />
opioids is greater in older people, the same is not true for<br />
all opioid side effects. Opioids are among the major<br />
causes of postoperative nausea and vomiting, increasing<br />
the risk nearly fourfold. 8 In the study by Cepeda et al.,<br />
age was not a risk factor for nausea and vomiting. 7 In<br />
209
210 S.L. Shafer and P. Flood<br />
fact, age may actually decrease the risk of nausea and<br />
vomiting. Sinclair and colleagues 9 observed a 13% de -<br />
crease in the risk of postoperative nausea and vomiting<br />
with each additional decade of life. This is consistent with<br />
the findings of Junger and colleagues. 8<br />
<strong>The</strong> Opioid Receptor<br />
<strong>The</strong> existence of an opioid receptor was long suspected<br />
because of the high potency and stereoselectivity of<br />
pharmacologic antagonists. <strong>The</strong> biochemical discovery<br />
of opioid receptors was independently reported in 1973,<br />
by laboratories of Pert, 10 Simon, 11 and Terenius. 12 <strong>The</strong><br />
finding of stereoselectivity led to an intense search<br />
for endogenous ligands, with identification of encephalin<br />
in 1975. 13 Other endogenous peptide ligands were isolated<br />
subsequently. 14,15 <strong>The</strong> fact that endogenous opioid<br />
ligands differed in their structure and binding sites<br />
suggested the existence of different opioid receptor<br />
types. 16 Three classes of opioid receptors were identified<br />
pharmacologically in the 1980s: µ (mu), 17 δ (delta), 18 and<br />
κ (kappa). 19<br />
Activation of the µ receptor is responsible for both<br />
the analgesic efficacy of the frequently used opioids<br />
and, unfortunately, for the majority of opioid toxicities.<br />
Shortly after characterization of the µ receptor, Pasternak<br />
and colleagues 20 demonstrated that there were<br />
two populations of opioid receptors: a high-affinity site,<br />
associated with analgesia and blocked by naloxazone,<br />
and a lower-affinity site, which was not blocked by naloxazone<br />
and seemed responsible for morphine lethality.<br />
It was subsequently demonstrated that morphine-induced<br />
analgesia was mediated by a population of receptors<br />
blocked by naloxonazine, which were termed µ 1 receptors,<br />
whereas morphine-induced ventilatory depression<br />
was blocked by a population of receptors that were not<br />
affected by naloxonazine, which were termed the µ 2<br />
receptors. 21,22 To further complicate matters, a selective<br />
morphine-6-glucuronide antagonist was identified, 3-Omethylnaxtrexone,<br />
that had little effect on morphine<br />
analgesia. 23 This suggested that there was variability<br />
within the µ 1 receptor itself. Although identification of a<br />
specific µ 1 antagonist led to the hope that a µ 1 -specific<br />
agonist could be developed, no such agonist has ever<br />
been identified.<br />
Additional evidence for µ receptor subtypes comes<br />
from the clinical observation of incomplete cross-tolerance<br />
among the opioids in patients, 24 so that if a patient<br />
is switched from an opioid to which the patient has<br />
become tolerant to an “equianalgesic” dosage of another<br />
opioid, the potential exists for serious overdose. 25 Additional<br />
evidence for multiple µ receptor subtypes comes<br />
from variance in the potency for analgesic efficacy and<br />
toxicity among patients, such that there is no single opioid<br />
that has the best therapeutic window for all patients. 25 An<br />
extreme example of differential response to opioids is<br />
found in the CXBK mouse, which is insensitive to morphine<br />
but has normal sensitivity to fentanyl and<br />
morphine-6-glucuronide. 26<br />
<strong>The</strong> µ opioid subtypes have unique distributions<br />
within the body. 27 Specifically, µ 1 is expressed in the<br />
brain, whereas µ 2 is expressed in the brain, gastrointestinal<br />
tract, and the respiratory tract. 28 Activation of both µ<br />
receptor subtypes acts to decrease calcium and potassium<br />
conductance and intracellular adenosine 3′,5′-cyclic<br />
monophosphate (cAMP). <strong>The</strong> recently discovered µ 3<br />
receptor is expressed on monocytes, granulocytes, and the<br />
vascular endothelium, where it acts to release nitric<br />
oxide. 29 Some of the vasodilatation that is associated with<br />
opioid administration that has been attributed to histamine<br />
release may be attributable to activation of the<br />
µ 3 receptor.<br />
<strong>The</strong> µ receptor is encoded by a single gene Oprm,<br />
located on chromosome 10 in the mouse 30,31 and on<br />
chromosome 6 in the human. 32 A variety of polymorphisms<br />
of Oprm have been identified in humans, as<br />
recently reviewed by Lötsch and Geisslinger. 32 <strong>The</strong> polymorphism<br />
that has generated the most interest has been<br />
the substitution of an aspartate for an asparagine in<br />
the 118 position, which is abbreviated the 118A > G<br />
SNP. This polymorphism has been associated with a<br />
decreased analgesic response to morphine. However, it<br />
does not reduce sensitivity to opioid-induced ventilatory<br />
depression. 33<br />
<strong>The</strong> Oprm gene gives rise to a family of µ receptors<br />
through selective splicing of the mRNA into µ opioid<br />
receptor subtypes. 34 In 1993, the first µ receptor was cloned,<br />
MOR-1. 35,36 Since then, at least 15 different splice variants<br />
of MOR-1 have been identified in mice, all derived from<br />
the same Oprm gene. 28 Several splice variants have been<br />
identified in humans as well. 37 Splice variants likely give<br />
rise to pharmacologically identified subtypes of µ receptors<br />
based on the exons that are translated. Unfortunately,<br />
mapping between individual splice variants and pharmacologically<br />
identified µ subtypes is incomplete. <strong>The</strong> currently<br />
identified splice variants are insufficient to explain<br />
the pharmacologic groupings, although this will likely<br />
become clearer as additional splice variants are discovered<br />
and characterized pharmacologically.<br />
All opioid receptors so far identified are coupled to G<br />
proteins. 38 At the cellular level, the opioid receptors have<br />
an inhibitory effect. When the receptors are occupied by<br />
opioid agonists, intracellular cAMP content is reduced.<br />
Reduced levels of cAMP both increase the activation of<br />
K + channels and reduce the open probability of voltagegated<br />
calcium channels. <strong>The</strong>se changes cause hyperpolarization<br />
of the membrane potential and thus reduce<br />
neuronal excitability. 39
15. <strong>The</strong> Pharmacology of Opioids 211<br />
Age and Opioid Receptors<br />
End-organ sensitivity to various ligands changes with<br />
age. Part of this change is from differences at the level of<br />
the drug receptor-effector mechanism. For example, the<br />
number and structure of the β-adrenergic receptor is<br />
unchanged in the elderly myocardium. <strong>The</strong> decreased<br />
chronotropic and inotropic response of elderly patients<br />
to β-adrenergic drugs seems to result from downstream<br />
changes in the mechanism by which binding at the receptor<br />
is coupled to adrenergic response mechanism. 40 In<br />
the brain, there seems to be both decreased α- and β-<br />
adrenergic receptor density in elderly individuals. 41<br />
<strong>The</strong>re is no decrease in the affinity or density of central<br />
nervous system benzodiazepine receptors with age. 42<br />
Barnhill and colleagues 43 studied benzodiazepine binding<br />
in response to acute or chronic stress. In the absence of<br />
stress, there was no difference in the number or affinity<br />
of benzodiazepine receptors. In young rats, receptor<br />
binding was increased by acute stress, a response not<br />
observed in older animals. Chronic stress enhanced<br />
binding in both young and old rats, but the recovery following<br />
cessation of stress was delayed in older animals.<br />
Thus, there are age-associated changes in benzodiazepine<br />
binding, but only in the poststress condition.<br />
Ueno and colleagues 44 examined opioid receptors in<br />
young, mature, and aged mice. Aged mice had reduced µ<br />
receptor density, but increased µ receptor affinity. Hess<br />
et al. 45 also observed decreased µ receptor density in rats<br />
with advancing age, associated with decreased sensitivity<br />
to pain. Similarly, Petkov and colleagues 46 observed<br />
decreased enkephalin receptors in aged rats, as well as<br />
decreased sensitivity to enkephalin. Aging may induce<br />
changes downstream of opioid receptor binding. In<br />
studies on opioid receptors in polymorphonuclear leucocytes,<br />
Fulop and colleagues 47 have shown that whereas<br />
cAMP was reduced on binding in cells from young adult<br />
animals, it was increased in cells from aged animals.<br />
Hoskins and Ho 48 have shown age-induced changes in the<br />
basal activities of adenylate cyclase, guanylate cyclase,<br />
cAMP phosphodiesterase, and cyclic guanosine monophosphate<br />
phosphodiesterase.<br />
Smith and Gray 49 examined the analgesic response to<br />
opioids in young and aged rats. <strong>The</strong>y applied noxious<br />
stimulus at two different stimulus intensities. At the lowintensity<br />
stimulus (immersing the tail in 50°C water),<br />
there was a trend toward increased sensitivity to opioids<br />
in the aged rats, but the difference was not statistically<br />
significant. However, when subjected to the high-intensity<br />
stimulus (immersing the tail in 55°C water), the aged<br />
rats were about twice as sensitive to opioids as the young<br />
rats, an effect that was statistically significant.<br />
Other investigators have reached quite different<br />
conclusions using similar experimental paradigms (tail<br />
flick after immersion in hot water). Van Crugten and<br />
colleagues 50 looked at morphine antinociception in<br />
aged rats, and found no difference in antinociception<br />
between aged and adult animals. Hoskins and colleagues 51<br />
found that aged mice were about half as sensitive<br />
to morphine as mature adult mice. Thus, the animal<br />
studies consistently show decreased numbers of opioid<br />
receptors in aged brains. However, the story about the<br />
antinociceptive response to morphine is less clear in<br />
animal models, with studies showing increased sensitivity,<br />
decreased sensitivity, or no change in sensitivity with<br />
advancing age.<br />
Aging and Pain Perception<br />
Pain is a part of daily life for many elderly patients, with<br />
about 50% of patients over the age of 70 reporting chronic<br />
pain. 52 Elderly patients are particularly more prone to<br />
chronic pain than younger people. 53,54 However, clinically<br />
it seems that pain in elderly subjects is indistinguishable<br />
from the experience of pain in younger subjects. 55<br />
<strong>The</strong>re are some interesting differences between young<br />
and older subjects in their response to experimental pain.<br />
<strong>The</strong>re is some evidence that older patients are more sensitive<br />
to experimental pain, 56 which may be explained, at<br />
least in part, by a reduction in the endogenous analge -<br />
sic response to pain, 57,58 possibly mediated by reduced<br />
production of β-endorphin in response to noxious stimulation.<br />
59 Older patients experience a more prolonged<br />
hyperalgesia after capsaicin injection compared with<br />
younger subjects. 60 However, older patients seem to also<br />
require a higher intensity of noxious stimulation before<br />
first reporting pain. 58<br />
Some of the differences between studies may also<br />
depend on exactly which pain pathways are activated<br />
during the assessment. Chakour and colleagues 61 demonstrated<br />
that pain transmission via C fibers was unchanged<br />
in young versus elderly subjects. However, there was a<br />
substantial reduction in pain transmission via Aδ fibers.<br />
Thus, the relative perceptions of pain in elderly subjects<br />
versus younger subjects were influenced by the extent of<br />
pain transmission via Aδ fibers.<br />
<strong>The</strong> Onset and Offset of Opioid<br />
Drug Effect<br />
Onset<br />
<strong>The</strong> onset of opioid drug effect is determined by the route<br />
of delivery, the delivered dose, the pharmacokinetics<br />
of the opioid that determine the plasma concentrations<br />
over time, and the rate of blood–brain equilibration<br />
between the plasma and the site of drug effect. Table 15-1<br />
shows adult pharmacokinetics of fentanyl, 62 alfentanil, 62
212 S.L. Shafer and P. Flood<br />
Table 15-1. Pharmacokinetic parameters for frequently used opioids.<br />
Fentanyl Alfentanil Sufentanil Remifentanil Morphine Methadone Meperidine Hydromorphone<br />
Volumes (L)<br />
V 1 12.7 2.2 17.8 4.9 17.8 7.7 18.1 11.5<br />
V 2 50 7 47 9 87 12 61 115<br />
V 3 295 15 476 5 199 184 166 968<br />
Clearances (L/min)<br />
Cl 1 0.62 0.20 1.16 2.44 1.26 0.13 0.76 1.33<br />
Cl 2 4.82 1.43 4.84 1.75 2.27 2.19 5.44 3.45<br />
Cl 3 2.27 0.25 1.29 0.06 0.33 0.38 1.79 0.92<br />
Exponents (min −1 )<br />
α 0.67 1.03 0.48 0.96 0.23 0.50 0.51 0.51<br />
β 0.037 0.052 0.030 0.103 0.010 0.025 0.031 0.012<br />
γ 0.0015 0.0062 0.0012 0.0116 0.0013 0.0005 0.0026 0.0005<br />
Half-lives (min)<br />
t 1/2 α 1.03 0.67 1.43 0.73 2.98 1.38 1.37 1.35<br />
t 1/2 β 19 13 23 7 68 28 22 59<br />
t 1/2 γ 475 111 562 60 548 1377 271 1261<br />
Blood–brain equilibration<br />
k e0 (min −1 ) 0.147 0.770 0.112 0.525 0.005 0.110 0.067 0.015<br />
t 1/2 k e0 (min) 4.7 0.9 6.2 1.3 139 6.3 10. 46<br />
T peak (min) 3.7 1.4 5.8 1.6 93.8 11.3 8.5 19.6<br />
VD peak effect (L) 76.9 6.0 94.9 17.0 590.2 30.9 143.3 383.3<br />
Note: <strong>The</strong> references for the pharmacokinetic parameters are given in the text.<br />
VD = volume of distribution.<br />
†<br />
Data extensively reanalyzed to obtain volume and clearance<br />
estimates.<br />
‡<br />
Original data provided by S. Bjorkman and fit using population<br />
model to create estimates in Table 15-1.<br />
§<br />
Based on a time to peak of 8.5 minutes in goats (!). It’s<br />
not great, but it’s the best onset data available.<br />
<br />
Based on a time to peak effect of 15–20 minutes.<br />
sufentanil, 63 remifentanil, 64 morphine, 65 methadone, 66†<br />
meperidine, 67‡ and hydromorphone. 68 Table 15-1 also<br />
shows k e0 , the rate constant for blood–effect-site equilibration,<br />
for fentanyl, 62 alfentanil, 62 sufentanil, 69 remifentanil,<br />
64 morphine, 65 methadone, 70 meperidine, 71§ and<br />
hydromorphone. 72 Based on these data, it is possible to<br />
predict the time course of concentration change in the<br />
plasma following an intravenous bolus, as seen in Figure<br />
15-1. <strong>The</strong> upper graph in Figure 15-1 shows the concentration<br />
during 24 hours following a bolus injection, whereas<br />
the lower graph just shows the first 30 minutes. In both<br />
cases, the curves have been normalized to start at 100%,<br />
which permits direct comparison of the pharmacokinetics<br />
despite differing potencies. As seen in the upper graph,<br />
the extremes of plasma elimination are remifentanil,<br />
which is ultra fast, and methadone, which has the longest<br />
half-life. Alfentanil has the second-shortest half-life<br />
among the eight opioids. Fentanyl, meperidine, sufentanil,<br />
hydromorphone, and morphine are all clustered in the<br />
middle. In particular, note how similar hydromorphone<br />
and morphine are when one examines the plasma pharmacokinetics.<br />
Approximately the same trend is observed<br />
in the first 30 minutes, although the initial distribution<br />
phase of hydromorphone takes it nearly as low as remifentanil<br />
in the first 10 minutes. As will be seen shortly, this<br />
is significant in terms of recovery.<br />
<strong>The</strong> plasma is not the site of drug effect, and thus<br />
the time course of concentration seen in Figure 15-1 will<br />
not reflect the time course of effect-site concentration<br />
or behavioral activity. By incorporating the plasma–<br />
effect-site equilibration delay into our calculations, we<br />
can examine the time course of the onset of drug effect,<br />
as shown in Figure 15-2. In this case, we have normalized<br />
the effect-site concentrations to peak-effect concentration<br />
73 to again permit comparisons of the time course of<br />
drugs independent of the differences in potency. Alfentanil<br />
and remifentanil both reach a peak about 1.5 minutes<br />
after bolus injection, although the overall remifentanil<br />
drug effect is more evanescent. <strong>The</strong> peak fentanyl concentration<br />
occurs about 3.5 minutes after bolus injection,<br />
whereas the peak sufentanil effect is about 6 minutes<br />
after bolus injection. Methadone and meperidine are<br />
nearly indistinguishable following bolus injection, each<br />
reaching a peak about 12 minutes after a bolus. <strong>The</strong> peak<br />
for hydromorphone is 15–20 minutes after the bolus.<br />
Morphine is the outlier in terms of onset. Five minutes<br />
after a bolus injection, morphine is at 50% of the peak<br />
concentration. However, morphine reaches its peak concentration<br />
in the effect site about 90 minutes after the<br />
bolus injection. Table 15-1 shows the time to reach peak<br />
concentration for each of the opioids, as well as the<br />
volume of distribution at the time of peak effect, which<br />
is useful for calculating initial loading doses. 74–76<br />
One of the key benefits to knowing the time course of<br />
drug effect following bolus injection is logical program-
15. <strong>The</strong> Pharmacology of Opioids 213<br />
ming of the lockout of PCA devices. A 10-minute lockout<br />
for hydromorphone and methadone is a logical choice,<br />
because patients are able to make a decision to redose<br />
themselves after reaching peak drug effect. <strong>The</strong> slower<br />
onset of morphine is somewhat problematic, because<br />
patients will administer another dose while the prior dose<br />
is still coming on, creating the possibility of stacking bolus<br />
doses.<br />
Considerable attention is given to “equianalgesic<br />
dosing” of opioids. <strong>The</strong> calculation of the equianalgesic<br />
dose is complicated by both the relative intrinsic potency<br />
of the opioids, the different pharmacokinetic profiles,<br />
and the large differences in the rate of blood–brain equilibration.<br />
Table 15-2 shows equianalgesic doses of frequently<br />
used opioids, based on the “minimum effective<br />
analgesic concentrations” or “MEAC” (also called<br />
“MEC”) of fentanyl, 77 alfentanil, 78 sufentanil, remifentanil,#<br />
morphine, 79 ** methadone, 80 meperidine, 81 and<br />
Figure 15-2. <strong>The</strong> time course of effect-site concentration following<br />
a bolus of fentanyl, alfentanil, sufentanil, remifentanil,<br />
morphine, methadone, meperidine, and hydromorphone, based<br />
on the pharmacokinetics and rate of plasma–effect-site equilibrium<br />
shown in Table 15-1. <strong>The</strong> curves have been normalized to<br />
the peak effect-site concentration, permitting comparison of the<br />
relative rate of increase independent of dose. <strong>The</strong> times to peak<br />
effect correspond to those shown in Table 15-1.<br />
hydromorphone. 82,83 †† Reflecting anesthesiologists’<br />
familiarity with fentanyl, all of the calculations have been<br />
made using fentanyl as the reference opioid. <strong>The</strong> calculation<br />
of an equianalgesic bolus dose depends on when the<br />
observation of drug effect is made. For example, because<br />
fentanyl has a very rapid onset, and morphine has a very<br />
slow onset, 5 mg of morphine has the same effect at 10<br />
minutes as 50 µg of fentanyl, whereas 60 minutes after the<br />
dose, 1 mg of morphine has the same effect as 50 µg of<br />
fentanyl. Similarly, because the drugs accumulate during<br />
infusions at different rates, the relative potencies of the<br />
opioids change depending on how long the infusion has<br />
been running, as shown in Table 15-2.<br />
Figure 15-3 shows the increase in effect-site concentration<br />
during a continuous infusion for each of these<br />
opioids. As expected, remifentanil increases the fastest,<br />
whereas methadone increases the slowest. Note, however,<br />
that even after 10 hours of drug administration, most of<br />
these opioids are only at 60%–80% of the eventual<br />
Figure 15-1. <strong>The</strong> time course of plasma concentration following<br />
a bolus of fentanyl, alfentanil, sufentanil, remifentanil, morphine,<br />
methadone, meperidine, and hydromorphone, based on<br />
the pharmacokinetics shown in Table 15-1. <strong>The</strong> y-axis is the<br />
percent of the initial concentration, which by definition is 100%<br />
at time 0, permitting display of the relative time courses of these<br />
opioids independent of the dose administered.<br />
Scaled to fentanyl based on relative electroencephalogram<br />
(EEG) potency of fentanyl 62 and sufentanil. 69<br />
#<br />
Scaled to fentanyl based on the relative EEG potency of fentanyl<br />
and remifentanil. 64<br />
**<strong>The</strong> MEC range given by Dahlstrom was 6–31 ng/mL, with a<br />
mean of 16 ng/mL. We chose 8 ng/mL, at the lower end of the<br />
reported range, because the average value of 16 ng/mL predicted<br />
equianalgesic morphine that seemed excessive.<br />
††<br />
This was the most difficult potency to determine from the literature.<br />
Hill and Zacny documented a tenfold bolus dose<br />
potency difference versus morphine, which was the final basis<br />
for calculating this number, and is similar to the value suggested<br />
by the Coda paper.
214 S.L. Shafer and P. Flood<br />
Table 15-2. Relative potency of frequently used opioids, based on the time of the observed effect.<br />
Fentanyl Alfentanil Sufentanil Remifentanil Morphine Methadone Meperidine Hydromorphone<br />
MEAC (ng/mL) 0.6 14.9 0.056 1.0 8 60 250 1.5<br />
Equipotent bolus dose at: (µg) (µg) (µg) (µg) (mg) (mg) (mg) (mg)<br />
Peak effect 50 92 5.5 17 4.9 1.9 37 0.6<br />
10 minutes 50 197 4.4 72 5.3 1.4 28 0.4<br />
30 minutes 50 174 3.9 282 2.0 0.9 17 0.2<br />
60 minutes 50 175 4.8 1680 1.0 0.9 14 0.1<br />
Equipotent infusion rate at: (µg/h) (µg/h) (µg/h) (µg/h) (mg/h) (mg/h) (mg/h) (mg/h)<br />
1 hour 100 323 8.8 135 5.3 2.3 43 0.6<br />
2 hours 100 332 9.6 182 3.3 2.3 38 0.4<br />
4 hours 100 365 11.6 252 2.3 2.6 36 0.4<br />
6 hours 100 409 13.0 310 2.1 2.9 37 0.4<br />
12 hours 100 536 15.1 436 2.2 3.1 40 0.5<br />
24 hours 100 675 16.3 554 2.4 2.9 45 0.6<br />
Note: <strong>The</strong> references for the relative potency are given in the text.<br />
MEAC = mean effective analgesic concentration.<br />
steady-state concentration. This speaks to the problem of<br />
background infusions for PCA. Even after many hours,<br />
patients are not at steady state, and the increasing drug<br />
concentration from the background infusion may expose<br />
a patient to toxicity 12–24 hours after initiation of the<br />
infusion. Given the increased sensitivity of elderly patients<br />
to the effects of opioids, background infusions are likely<br />
a particularly poor choice in this population.<br />
Offset<br />
<strong>The</strong> offset of drug effect is a function of both the pharmacokinetic<br />
behavior and the rate of blood–brain equilibration.<br />
<strong>The</strong> “context sensitive half-time” 73,84 is a useful<br />
way to consider the plasma pharmacokinetic portion of<br />
the offset time, as shown in Figure 15-4. <strong>The</strong> x-axis on<br />
Figure 15-4 is the duration of an infusion that maintains<br />
Figure 15-3. <strong>The</strong> increase to steady state during an infusion of<br />
fentanyl, alfentanil, sufentanil, remifentanil, morphine, methadone,<br />
meperidine, and hydromorphone, based on the pharmacokinetics<br />
and rate of plasma–effect-site equilibrium shown in<br />
Table 15-1. <strong>The</strong> curves have been normalized to the steady-state<br />
effect-site concentration, permitting comparison of the relative<br />
rate of increase independent of infusion rate. Only remifentanil<br />
and alfentanil are at steady state after 10 hours of continuous<br />
infusion.<br />
Figure 15-4. <strong>The</strong> “context-sensitive half-time” (50% plasma<br />
decrement time) for fentanyl, alfentanil, sufentanil, remifentanil,<br />
morphine, methadone, meperidine, and hydromorphone,<br />
based on the pharmacokinetics shown in Table 15-1. Remifentanil<br />
shows virtually no accumulation over time with continuous<br />
infusions, whereas the offset of fentanyl changes<br />
considerably as it is administered to maintain a steady plasma<br />
concentration.
15. <strong>The</strong> Pharmacology of Opioids 215<br />
a steady concentration of drug in the plasma. <strong>The</strong> y-axis<br />
is the time required for the concentrations to decrease by<br />
50% after the infusion is terminated. Remifentanil’s<br />
pharmacokinetics are so fast that the context-sensitive<br />
half-time blurs right into the x-axis. Perhaps surprisingly,<br />
fentanyl is the outlier here. Fentanyl accumulates in fat,<br />
and so an infusion that maintains a steady concentration<br />
in the plasma winds up giving patients a whopping dose<br />
of fentanyl, resulting in slow recovery. Meperidine similarly<br />
shows long recovery. Note that for infusions of less<br />
than 10 hours, morphine, hydromorphone, and sufentanil<br />
are nearly indistinguishable based on the plasma<br />
pharmacokinetics.<br />
Once again, we have to consider that the plasma is not<br />
the site of drug effect. <strong>The</strong>refore, we must consider the<br />
50% effect-site decrement time, 73,85 as shown in Figure<br />
15-5. Because fentanyl and remifentanil have very rapid<br />
plasma–effect-site equilibration, they have changed little<br />
between Figures 15-4 and 15-6. Note, however, the<br />
huge change for morphine and hydromorphone. One<br />
might have thought from Figure 15-4 that these drugs<br />
would result in rapid offset of drug effect following a<br />
continuous infusion. This is clearly not the case, because<br />
the blood–brain equilibration delay results in these drugs<br />
having far slower offset than alfentanil or sufentanil. <strong>The</strong><br />
“surprise” here is methadone. One would rarely think of<br />
methadone as a reasonable choice for infusion during<br />
anesthesia, but the pharmacokinetics of methadone<br />
Figure 15-6. <strong>The</strong> 20% effect-site decrement curves for fentanyl,<br />
alfentanil, sufentanil, remifentanil, morphine, methadone,<br />
meperidine, and hydromorphone, based on the pharmacokinetics<br />
and rate of plasma–effect-site equilibrium shown in Table<br />
15-1. <strong>The</strong> effect-site levels of all opioids, except morphine, will<br />
decrease by 20% quickly when an infusion is terminated. <strong>The</strong><br />
slower decrease for morphine is because of its slow plasma–<br />
effect-site equilibration.<br />
suggest that it might be a reasonable choice for anesthetics<br />
of 4 hours or less.<br />
Figure 15-6 shows the 20% effect-site decrement curve<br />
for these eight opioids. Figure 15-6 speaks to how often<br />
one might expect to redose a patient with chronic pain<br />
who is titrating the analgesic level to a just-adequate<br />
concentration. Because of its slow blood–brain equilibration,<br />
morphine would need to be given approximately<br />
every 2 hours. Hydromorphone, fentanyl, and methadone<br />
would need to be given approximately every hour.<br />
Specific Opioids<br />
Figure 15-5. <strong>The</strong> 50% effect-site decrement curves for fentanyl,<br />
alfentanil, sufentanil, remifentanil, morphine, methadone,<br />
meperidine, and hydromorphone, based on the pharmacokinetics<br />
and rate of plasma–effect-site equilibrium shown in Table<br />
15-1. For drugs with rapid plasma–effect-site equilibrium, the<br />
50% effect-site decrement curve closely follows the context<br />
sensitive half-time curve. However, for drugs with slow plasma–<br />
effect-site equilibration, a 50% decrement in effect-site concentration<br />
is considerably slower than a 50% decrement in plasma<br />
concentration (e.g., morphine).<br />
Morphine<br />
Morphine has three unique aspects among the opioids<br />
frequently used in anesthesia practice: it is an endogenous<br />
ligand of the µ receptor, has an active metabolite, and has<br />
a very slow onset of effect. Morphine was initially identified<br />
in the brains of mice that had never been exposed to<br />
exogenous morphine. 86 It has subsequently been found in<br />
the brains of cows, 87 rats, 88 and humans. 89 Codeine has<br />
also been identified as an endogenously synthesized substance.<br />
However, because codeine is mostly an inactive<br />
prodrug of morphine, its presence in the brain does not<br />
diminish morphine’s distinction as the only endogenous<br />
ligand of the µ receptor that is also a frequently administered<br />
drug.<br />
Morphine is metabolized by glucuronidation into two<br />
metabolites, morphine-3-glucuronide, which is mostly
216 S.L. Shafer and P. Flood<br />
Creatinine clearance (mls/min)<br />
250<br />
200<br />
150<br />
100<br />
50<br />
0<br />
20 30 40 50 60 70 80 90<br />
Age<br />
inactive, and morphine-6-glucuronide, which is itself a<br />
potent analgesic. 90 Although the potency of intrathecal<br />
morphine-6-glucuronide is 650-fold higher than that of<br />
morphine, 91 morphine-6-glucuronide crosses the blood–<br />
brain barrier very slowly, so slowly that it is unlikely that<br />
it contributes to the acute analgesia provided by morphine.<br />
92,93 However, with chronic administration, the<br />
levels of morphine-6-glucuronide will increase to pharmacologically<br />
active concentrations. 94<br />
Morphine-6-glucuronide is eliminated by the kidneys. 95<br />
Creatinine clearance is reduced with advancing age, as<br />
shown in the often cited equation of Cockroft and<br />
Gault 96 :<br />
Men: Creatinine clearance (mL/min)<br />
= {[140 − age (years)] × weight (kg)}/<br />
[72 × serum creatinine (mg%)]<br />
Women: 85% of the above.<br />
Creatinine<br />
Figure 15-7. <strong>The</strong> relationship among age, serum creatinine,<br />
and creatinine clearance, based on the equation of Cockroft<br />
and Gault. (Adapted with permission from Cockcroft and<br />
Gault. 96 )<br />
0.5<br />
1.0<br />
1.5<br />
2.0<br />
Figure 15-7 shows the relationship among creatinine,<br />
age, and creatinine clearance according to the above<br />
equation. <strong>The</strong> key observation from Figure 15-7 is that,<br />
even in the presence of normal creatinine, the creatinine<br />
clearance of an 80-year-old patient will be about half that<br />
in a 20-year-old patient. Thus, morphine-6-glucuronide<br />
will accumulate more in elderly patients, necessitating a<br />
reduction in dose of chronically administered morphine.<br />
Of course, if the patient has renal insufficiency, it might<br />
be better to select an opioid without an active<br />
metabolite.<br />
<strong>The</strong> second unique aspect to morphine is the slow<br />
onset of effect. <strong>The</strong> peak effect following a bolus dose of<br />
morphine occurs approximately 90 minutes after the<br />
bolus. This has been demonstrated using pupillometry, 97–99<br />
ventilatory depression, 98 and analgesia 99 as measures of<br />
morphine drug effect. <strong>The</strong> likely explanation for this is<br />
that morphine is a substrate for P-glycoprotein, which<br />
actively transports morphine out of the central nervous<br />
system. 100<br />
Figure 15-8 shows a simulation of the analgesic (y-axis<br />
> 1) and ventilatory (y-axis < 1) effects of three different<br />
morphine doses: a bolus of 0.2 mg/kg, a bolus of 0.2 mg/kg<br />
followed by an infusion of 1 mg/70 kg per hour, and<br />
repeated boluses of 0.1 mg/kg every 6 hours. 101 <strong>The</strong> solid<br />
line is the median prediction, whereas the shaded area<br />
represents the 95% confidence bounds. As seen in Figure<br />
15-8, the time course of analgesia and ventilatory depression<br />
is similar, although the analgesia wanes somewhat<br />
faster than the ventilatory depression.<br />
It is important to appreciate the slow onset of morphine<br />
when titrating to effect. Aubrun and colleagues 102,103<br />
have advocated postoperative titration of morphine in<br />
elderly patients by administering 2- to 3-mg boluses every<br />
5 minutes. This is not logical for a drug with a peak effect<br />
Effect<br />
4<br />
3<br />
2<br />
1<br />
A. Bolus 0.2 mg/kg B. 0.2 mg/kg + 1 mg/70 kg per h C. 0.1 mg/kg @ 6 h intervals<br />
4<br />
6<br />
3<br />
4<br />
3<br />
2<br />
2<br />
1<br />
1<br />
0.6<br />
0.4<br />
0.6<br />
0.6<br />
0.4<br />
0.4<br />
0 4 8 12 16 20 24 0 4 8 12 16 20 24 0 4 8 12 16 20 24<br />
TIME (h) TIME (h) TIME (h)<br />
Figure 15-8. Simulated analgesic (y > 1) and ventilatory (y < 1)<br />
effects of three different doses of morphine: 0.2 mg/kg (A),<br />
0.2 mg/kg plus an infusion of 1 mg/70 kg/h (B), and a bolus of<br />
0.1 mg/kg every 6 hours (C). <strong>The</strong> analgesic and ventilatory<br />
effects peak concurrently, about 90 minutes after the morphine<br />
bolus. Because the concentration versus response relationship<br />
is steeper for analgesia than ventilatory depression, the analgesic<br />
effect dissipates before the ventilatory depression. (Reprinted<br />
with permission from Dahan et al. 101 Copyright ©Lippincott<br />
Williams & Wilkins.)
15. <strong>The</strong> Pharmacology of Opioids 217<br />
about 1.5 hours after bolus injection. Aubrun and colleagues<br />
did not see any toxicity with this approach. That<br />
is surprising, given the potential for accumulation with<br />
repeated titration of small doses of morphine to effect.<br />
However, it does explain why their study is unique in<br />
finding that elderly patients require the same amount of<br />
opioid as younger patients.<br />
Meperidine<br />
<strong>The</strong> bottom line on meperidine is that it has little role in<br />
the management of pain. Meperidine is still a popular<br />
drug because of familiarity of its use, particularly among<br />
surgeons and obstetricians. Meperidine is unique among<br />
opioids in that it has significant local anesthetic activity.<br />
104,105 Meperidine has been used as the sole analgesic<br />
intrathecally for obstetric anesthesia, but its benefit over<br />
a combination of local anesthetic with another opioid is<br />
unclear. One logical use of meperidine is in the treatment<br />
of postoperative shivering, in which doses of 10–20 mg are<br />
typically effective.<br />
<strong>The</strong> problems with meperidine are its complex pharmacology<br />
and its toxic metabolite. Holmberg and colleagues 106<br />
examined the pharmacokinetics of an intravenous meperidine<br />
bolus in young and elderly surgical subjects. <strong>The</strong>y<br />
found that elderly patients had reduced meperidine clearance,<br />
resulting in a longer half-life for meperidine. <strong>The</strong>re<br />
was minimal change in the initial volume of distribution.<br />
<strong>The</strong> clinical implication is that the initial dose of meperidine<br />
in elderly subjects should not be reduced based on<br />
pharmacokinetics, but meperidine will accumulate in<br />
elderly subjects with repeated administration. This makes<br />
meperidine a particularly poor choice for administration<br />
by PCA in elderly patients. 107<br />
A worrisome aspect of meperidine is the toxic metabolite,<br />
normeperidine. In a subsequent study, Holmberg and<br />
colleagues examined the renal excretion of both meperidine<br />
and normeperidine in elderly surgical patients. 108<br />
Renal excretion was reduced in elderly patients, par -<br />
ticularly for normeperidine. <strong>The</strong> result is that normeperidine<br />
will likely accumulate with repeated doses in<br />
elderly patients. Because normeperidine is highly epileptogenic,<br />
meperidine is probably a poor choice for PCA<br />
or other forms of continuous opioid delivery in elderly<br />
patients.<br />
Meperidine has several other unique aspects to its<br />
pharmacology. It is the only negative inotrope among the<br />
opioids. 109 Meperidine also has intrinsic anticholinergic<br />
properties, which can result in tachycardia. Elderly<br />
patients with coronary artery disease are clearly at risk<br />
for adverse events if given drugs that have negative inotropic<br />
or positive chronotropic effects.<br />
Last, meperidine is associated with several unusual<br />
reactions, including the potential for acute serotonergic<br />
syndrome when combined with a monoamine oxidase<br />
(MAO)-A inhibitor. Fortunately, the classic MAO-A<br />
inhibitors, phenelzine (Nardil), tranylcypromine<br />
(Parnate), and isocarboxazid (Marplan) are now rarely<br />
used. Selegiline, often used in Parkinson’s disease, is a<br />
weak MAO-B inhibitor, and has been implicated in one<br />
nonfatal interaction with meperidine. 110 However, given<br />
the polypharmacy common in elderly patients, it would<br />
seem wise to avoid using meperidine when opioids with<br />
more selective pharmacology and inactive metabolites<br />
are available.<br />
Hydromorphone<br />
Hydromorphone in many aspects acts as a rapid-onset<br />
morphine. However, it lacks the histamine release associated<br />
with morphine and does not have active metabolites.<br />
<strong>The</strong>re are no studies explicitly examining the role of age<br />
in hydromorphone pharmacokinetics or pharmacodynamics.<br />
In fact, there are surprisingly few studies examining<br />
perioperative use of hydromorphone. Keeri-Szanto 111<br />
found intraoperative hydromorphone to be approximately<br />
8 times more potent than morphine, with a halflife<br />
of 4 hours versus 5 hours for morphine. Kopp et al. 112<br />
investigated whether 4 mg of hydromorphone provided<br />
any evidence of preemptive analgesia. It did not.<br />
Rapp and colleagues 113 compared hydromorphone<br />
PCA to morphine PCA in postoperative patients following<br />
lower abdominal surgery. <strong>The</strong>y found that hydromorphone<br />
PCA was associated with better mood scores, but<br />
with increased incidence of nausea and vomiting. <strong>The</strong>y<br />
found that 1 mg of hydromorphone was approximately<br />
equianalgesic with 5 mg of morphine. This is about twice<br />
as potent as suggested by Hill and Zacny, 83 who determined<br />
that hydromorphone was tenfold more potent<br />
than morphine. Although Rapp and colleagues did not<br />
specifically study the effects of age, one would expect this<br />
ratio to be independent of age in the immediate postoperative<br />
period. Because morphine has an active metabolite<br />
that accumulates and hydromorphone does not, the<br />
apparent potency of morphine relative to hydromorphone<br />
may increase with chronic administration.<br />
Lui and colleagues 114 compared epidural hydromorphone<br />
to intravenous hydromorphone, both administered<br />
by PCA in a double-blind/double-dummy protocol. <strong>The</strong>y<br />
found more pruritus in patients receiving epidural hydromorphone,<br />
but no differences in postoperative analgesia,<br />
bowel function, or patient satisfaction. Overall, hydromorphone<br />
in the epidural group was half of that in the<br />
intravenous group, indicating that hydromorphone is<br />
acting spinally when administered via the epidural route.<br />
Hydromorphone and morphine both reach their peak<br />
concentrations in the cervical cerebrospinal fluid about<br />
60 minutes after epidural administration, 115 suggesting<br />
they have similar potential for delayed ventilatory depression<br />
after epidural administration. In a study of obstetric
218 S.L. Shafer and P. Flood<br />
patients, Halpern and colleagues 116 found 0.6 mg of hydromorphone<br />
to be clinically indistinguishable from 3 mg<br />
of morphine, consistent with the 1 : 5 relative potency<br />
reported for intravenous hydromorphone and morphine<br />
in the postoperative period.<br />
Fentanyl<br />
Fentanyl is among the “cleanest” opioids in terms of<br />
pharmacology. It has a rapid onset, predictable metabolism,<br />
and inactive metabolites. It is (obviously) the first of<br />
the “fentanyl” series of opioids, notable for their rapid<br />
metabolism and selective µ potency. It is the only one of<br />
the opioids that is available for transdermal and transmucosal<br />
delivery, although these methods of administration<br />
are being investigated for sufentanil as well.<br />
Bentley et al. 117 studied aging and fentanyl pharmacokinetics<br />
in young and elderly groups of patients. <strong>The</strong>y<br />
found that fentanyl clearance was decreased among the<br />
elderly, resulting in a prolonged half-life.<br />
Scott and Stanski 62 used high-resolution arterial sampling<br />
during and after a brief fentanyl infusion to characterize<br />
the influence of age on the pharmacokinetics<br />
of fentanyl. <strong>The</strong>se investigators did not find any effect of<br />
age on the pharmacokinetics of fentanyl or alfentanil,<br />
except for a small change in rapid intercompartmental<br />
clearance.<br />
<strong>The</strong> minimal influence of age on the pharmacokinetics<br />
of fentanyl was subsequently confirmed by Singleton and<br />
colleagues. 118 <strong>The</strong>se investigators found no change in the<br />
dose-adjusted concentration of fentanyl between young<br />
and elderly patients, except for a transient increase in<br />
concentration in elderly individuals at 2 and 4 minutes<br />
after the start of the infusion. <strong>The</strong>se findings are consistent<br />
with the decreased rapid intercompartmental clearance<br />
reported by Scott and Stanski.<br />
Scott and Stanski used the EEG as a measure of drug<br />
effect to estimate the potency of fentanyl. 62,119 <strong>The</strong>y<br />
observed a decrease of approximately 50% in the dose<br />
required for 50% of maximal EEG suppression (C 50 )<br />
from age 20 to age 85, as shown in Figure 15-9. Because<br />
the pharmacokinetics of fentanyl seem nearly unchanged<br />
by age, it is likely that elderly patients require less fentanyl<br />
because of intrinsic increased sensitivity to opioids.<br />
Put another way—the elderly brain is twice as sensitive<br />
to opioids as a younger brain. This predicts that elderly<br />
patients require half of the fentanyl that younger patients<br />
require. Because the pharmacodynamics of fentanyl (i.e.,<br />
the C 50 ) is affected by age, and not the pharmacokinetics,<br />
the offset of fentanyl drug effect in elderly patients who<br />
receive an appropriately reduced dose of fentanyl should<br />
be as fast as it is in younger patients.<br />
<strong>The</strong> 50% reduction in fentanyl suggested by Scott and<br />
Stanski’s integrated pharmacokinetic/pharmacodynamic<br />
model is in reasonable agreement with an analysis by<br />
C 50 (ng/ml)<br />
14<br />
12<br />
10<br />
8<br />
6<br />
4<br />
2<br />
0<br />
20 30 40 50 60 70 80 90<br />
Age (years)<br />
Figure 15-9. <strong>The</strong> influence of age on the 50% maximal effective<br />
dose (C 50 ) of fentanyl, as measured by electroencephalogram<br />
depression. Although there is considerable variability, overall<br />
there is about a 50% reduction in C 50 from age 20 to age 80,<br />
reflecting increased brain sensitivity. This has been shown for<br />
alfentanil 62 and remifentanil, 64 and appears to be a class effect<br />
of opioids. (Adapted with permission from Scott JC, Stanski<br />
DR. Decreased fentanyl/alfentanil dose requirment with<br />
increasing age: A pharmacodynamic basis. J Pharmacol Exp<br />
<strong>The</strong>r 240:159–166, 1987.)<br />
Martin and colleagues 120 of intraoperative fentanyl utilization.<br />
Using the automated electronic record system in<br />
place at Duke University Hospital, they found that intraoperative<br />
doses of fentanyl decreased by about 10% per<br />
decade after age 30. Apparently, clinicians have integrated<br />
this information into their practice appropriately,<br />
at least at Duke University Hospital.<br />
Other Fentanyl Delivery Systems<br />
Fentanyl is also available in two unique dosage forms:<br />
oral transmucosal fentanyl citrate and transdermal fentanyl.<br />
Holdsworth and colleagues 121 studied pharmacokinetics<br />
and tolerability of a 20-cm 2 transdermal fentanyl<br />
patch in young and elderly subjects. Plasma fentanyl concentrations<br />
were nearly twofold higher in the elderly subjects<br />
compared with younger subjects, reflecting either<br />
increased absorption or decreased clearance. Given that<br />
fentanyl clearance seems unchanged in the elderly, the<br />
likely explanation is that transdermal fentanyl absorption<br />
is more rapid in elderly patients, possibly because the skin<br />
is thinner and poses less of a barrier to fentanyl absorption.<br />
<strong>The</strong> increased concentrations in elderly subjects<br />
were associated with increased adverse events—so much<br />
so that the patch was removed for the study in every<br />
elderly subject, whereas none of the patches were<br />
removed in younger subjects.<br />
Davis and colleagues 122 also noted that the time course<br />
of absorption of fentanyl through the skin is delayed in<br />
the elderly, with subcutaneous fat acting as secondary<br />
reservoir leading to prolonged release even after the<br />
removal of the patch.
15. <strong>The</strong> Pharmacology of Opioids 219<br />
Kharasch and colleagues 123 examined the influence of<br />
age on the pharmacokinetics and pharmacodynamics of<br />
oral transmucosal fentanyl citrate (the fentanyl “lollipop”).<br />
<strong>The</strong>y found no change in the pharmacokinetics of<br />
fentanyl with age, including the absorption characteristics<br />
of the buccal mucosa. Perhaps unexpectedly, they also<br />
found no increase in sensitivity to fentanyl, as measured<br />
by pupillary miosis. Thus, in their view, the data do not<br />
support reducing the dose of oral transmucosal fentanyl<br />
citrate in elderly patients.<br />
Alfentanil<br />
<strong>The</strong> relationship between opioids and age becomes more<br />
complex when we consider alfentanil. Scott and Stanski 62<br />
reported similar findings for alfentanil as previously<br />
described for fentanyl. In particular, they did not find any<br />
effect of age on the pharmacokinetics of alfentanil, except<br />
for a small change in the terminal half-life. Shafer et al. 124<br />
also reported no relationship between age and alfentanil<br />
pharmacokinetics. Sitar and colleagues 125 reported a<br />
modest decrease in alfentanil clearance and central compartment<br />
volume in elderly subjects. In a study that used<br />
historical control data, Kent and colleagues 126 also<br />
reported a modest decrease in alfentanil clearance with<br />
advancing age. Lemmens et al. 127 observed that the pharmacokinetics<br />
of alfentanil in men (as studied exclusively<br />
by Scott and Stanski) were unaffected by age, whereas<br />
the pharmacokinetics in women showed a clear negative<br />
correlation between age and clearance.<br />
In an effort to sort out these modestly conflicting<br />
results, Maitre et al. 128 pooled alfentanil concentration<br />
data from multiple prior studies and performed a population<br />
pharmacokinetic analysis to estimate the influence<br />
of age and gender on the pharmacokinetics of alfentanil.<br />
Maitre et al. found that clearance decreased with age, and<br />
that the volume of distribution at steady state increased<br />
with age, the net effect being a longer terminal half-life<br />
with increasing age. That might sound like the end of the<br />
story, except that Raemer and colleagues 129 prospectively<br />
tested the Maitre et al. pharmacokinetics in two groups<br />
of patients, young women and elderly men, using computer-controlled<br />
drug administration. In this prospective<br />
test, the pharmacokinetics reported by Maitre et al. did<br />
not accurately predict the observed plasma alfentanil<br />
concentrations. However, pharmacokinetics reported by<br />
Scott and Stanski, which predict no influence of age or<br />
gender on alfentanil pharmacokinetics, accurately predicted<br />
the concentrations in both young women and<br />
elderly men. From these results, we can conclude that<br />
pharmacokinetics of alfentanil do not change in a clinically<br />
significant manner with age.<br />
Although they found no change in pharmacokinetics<br />
with age, Scott and Stanski demonstrated that the C 50 for<br />
EEG depression with alfentanil decreased by 50% in<br />
elderly subjects, nearly identical to the increased potency<br />
of fentanyl in elderly subjects. 62 This would suggest that,<br />
based on pharmacokinetic alterations with age, the dose<br />
of alfentanil in elderly patients should be about half of<br />
the dose that would be used in younger patients. Unfortunately,<br />
subsequent studies by Lemmens et al., 130–132<br />
based on clinical endpoints, found no influence of age on<br />
the pharmacodynamics of alfentanil. However, Lemmens<br />
et al. 133 observed that the alfentanil dose required to<br />
maintain adequate anesthesia, when administered by<br />
target-controlled infusion, was decreased by approximately<br />
50% in elderly subjects. Thus, Lemmens et al. saw<br />
a similar change in dose-response relationship, in that the<br />
elderly required half as much opioid as younger subjects,<br />
but could not explain it as a pharmacodynamic difference.<br />
However, it is a bigger difference in concentration than<br />
any of the pharmacokinetic studies would have predicted,<br />
and there was no control group—the control group was<br />
a historical control group.<br />
Where this leaves us is that there are many studies<br />
suggesting that the alfentanil dose in elderly subjects is<br />
about half of the dose in younger subjects. <strong>The</strong> available<br />
data suggest that the change is probably pharmacodynamic,<br />
but there may be a pharmacokinetic component<br />
to the increased sensitivity as well. If the change is mostly<br />
pharmacodynamic, perhaps, with a modest change in terminal<br />
half-life in elderly subjects, then the offset of alfentanil<br />
should be as fast in older subjects as it is in younger<br />
subjects, provided the dose has been appropriately<br />
reduced.<br />
Sufentanil<br />
Sufentanil is the most potent of the available opioids,<br />
with potency approximately tenfold greater than fentanyl.<br />
134 Age has, at most, only a modest influence on<br />
sufentanil pharmacokinetics. Helmers and colleagues 135<br />
found no change in sufentanil pharmacokinetics between<br />
young and elderly subjects. Similarly, Gepts and colleagues<br />
136 found no effect of age on sufentanil pharmacokinetics<br />
in a complex population analysis. Matteo and<br />
colleagues 137 found that the central compartment volume<br />
of sufentanil was significantly decreased in elderly<br />
patients. This modest pharmacokinetic difference in<br />
elderly subjects would be expected to increase the effects<br />
of sufentanil in the first few minutes after a bolus dose<br />
and not subsequently. However, the elderly patients in<br />
Matteo’s study were far more sensitive to sufentanil than<br />
the younger subjects. Six of seven elderly patients required<br />
naloxone at the end of this study, whereas only one of<br />
seven young patients required naloxone. Matteo et al.<br />
concluded that elderly patients had increased sensitivity<br />
to a given concentration of sufentanil, similar to the<br />
increased sensitivity to fentanyl and alfentanil in elderly<br />
patients described by Scott and Stanski.
220 S.L. Shafer and P. Flood<br />
Thus, based on the twofold increase in brain sensitivity<br />
to opioids demonstrated for fentanyl and alfentanil in<br />
elderly patients, one might expect similar increase in<br />
brain sensitivity to sufentanil in elderly patients. Thus, it<br />
is surprising that Hofbauer and colleagues 138 did not<br />
observe any influence of age on the sufentanil requirement<br />
of mechanically ventilated patients in the intensive<br />
care unit.<br />
Remifentanil<br />
Remifentanil has the fastest and most predictable metabolism<br />
of any of the available opioids. Remifentanil was<br />
introduced into clinical practice under Food and Drug<br />
Administration guidelines that mandated explicit pharmacokinetic<br />
and pharmacodynamic analysis for special<br />
populations, including elderly subjects. Thus, the influence<br />
of age on remifentanil pharmacokinetics and pharmacodynamics<br />
was established in high-resolution trials about<br />
3 times larger than the trials for fentanyl, alfentanil, or<br />
sufentanil. <strong>The</strong> pharmacokinetic and pharmacodynamic<br />
models for remifentanil were reported by Minto and colleagues.<br />
64 In a companion article, Minto et al. 139 used<br />
computer simulation to examine the implications of the<br />
complex age-related changes on remifentanil dosing. <strong>The</strong><br />
pharmacokinetics of remifentanil change with age, as<br />
shown in Figure 15-10. With advancing age, V 1 , the volume<br />
of the central compartment, decreases about 20% from<br />
Figure 15-10. <strong>The</strong> influence of age on remifentanil pharmacokinetics.<br />
With advancing age, the volume of the central compartment<br />
decreases by 50% from age 20 to age 80, and the clearance<br />
decreases by 66%. (Adapted with permission from Minto<br />
et al. 64 )<br />
Figure 15-11. <strong>The</strong> influence of age on remifentanil pharmacodynamics.<br />
With advancing age, the 50% effective concentration<br />
(EC 50 ) declines, reflecting a nearly identical increase in intrinsic<br />
potency as seen with fentanyl and alfentanil. Additionally, halftime<br />
of blood–brain equilibration (t 1/2 k e0 ) increases. (Adapted<br />
with permission from Minto et al. 64 )<br />
age 20 to 80. Concurrently, clearance decreases about<br />
30% from age 20 to age 80. Figure 15-11 shows the agerelated<br />
changes in remifentanil pharmacodynamics. As<br />
also observed for fentanyl and alfentanil, the C 50 for EEG<br />
depression is reduced by 50% in elderly subjects, suggesting<br />
that remifentanil has about twice the intrinsic potency<br />
in elderly subjects as in younger subjects. <strong>The</strong> t 1/2 k e0 , halftime<br />
of plasma–effect-site equilibration, is also increased<br />
in elderly subjects. In the absence of other changes, this<br />
would mean that the onset and offset of remifentanil drug<br />
effect will be slower in elderly patients.<br />
Figure 15-12 uses computer simulations to examine the<br />
time course of blood concentration (solid lines) and<br />
effect-site concentration (dashed lines) after a unit bolus<br />
of remifentanil. <strong>The</strong> blood concentrations are higher in<br />
elderly subjects because of the smaller central compartment<br />
concentration. However, the slower t 1/2 k e0 in elderly<br />
subjects results in less-rapid equilibration. As a result, the<br />
effect-site concentrations in elderly individuals do not<br />
increase higher than the effect-site concentrations in<br />
young individuals. However, the onset and offset are<br />
slower in elderly individuals. For example, in a young<br />
individual, the peak drug effect is expected about 90<br />
seconds after a bolus injection. In an elderly individual,<br />
the peak effect is expected about 2–3 minutes after bolus<br />
injection.<br />
Figure 15-13 shows the influence of age and weight on<br />
remifentanil dosing. As seen in the top graph of Figure
15. <strong>The</strong> Pharmacology of Opioids 221<br />
Figure 15-12. Simulations showing the effect-site concentration<br />
from identical bolus doses in a 20-, 50-, and 80-year-old<br />
subject. <strong>The</strong> concentrations are highest in the 80-year-old subject<br />
because of the reduced size of the central compartment.<br />
However, because of the slower blood–brain equilibrium in the<br />
80-year-old subject, the peak effect-site concentration is almost<br />
identical in the three simulations. Thus, the smaller V 1 is offset<br />
by the slower plasma–effect-site equilibration. However, a bolus<br />
of remifentanil takes about a minute longer to reach peak<br />
effect-site concentrations in elderly subjects. (Adapted with<br />
permission from Minto et al. 139 )<br />
15-13, elderly subjects need about half of the bolus dose<br />
as younger subjects to achieve the same level of drug<br />
effect. This is not because of the change in pharmacokinetics.<br />
As shown in Figure 15-12, the peak effect-site<br />
levels after a bolus of remifentanil are nearly identical in<br />
young and elderly subjects. Rather, the remifentanil bolus<br />
is reduced in elderly subjects because of the increased<br />
sensitivity of the elderly brain to opioid drug effect,<br />
exactly as reported for fentanyl and alfentanil. <strong>The</strong> bottom<br />
graph in Figure 15-13 shows that elderly subjects require<br />
about one third as rapid an infusion as younger subjects.<br />
This reflects the combined influences of the increased<br />
sensitivity and the decreased clearance in elderly<br />
individuals.<br />
As seen in Figure 15-13, the influence of weight on<br />
remifentanil dosing is considerably less than the influence<br />
of age. We point this out because anesthesiologists reflexively<br />
adjust remifentanil infusions to body weight, but<br />
seem reluctant to make an adequate reduction in infusion<br />
rate for elderly individuals.<br />
Figure 15-14 shows the time required for decreases in<br />
effect-site concentration of 20%, 50%, and 80% as a function<br />
of remifentanil infusion duration. <strong>The</strong>se would be the<br />
“20% effect-site decrement time,” the “50% effect-site<br />
decrement time,” and the “80% effect-site decrement<br />
Figure 15-13. <strong>The</strong> influence of age and weight on remifentanil<br />
bolus dose and infusion rates. Bolus doses should be reduced<br />
by 50% in elderly subjects, reflecting the increased brain sensitivity.<br />
Infusion rates should be reduced by 66%, reflecting the<br />
combined effects of increased brain sensitivity and decreased<br />
clearance. LBM = lean body mass. (Adapted with permission<br />
from Minto et al. 139 )<br />
time,” respectively. For each decrement time, the expected<br />
relationship is shown for a 20-year-old patient and an<br />
80-year-old patient. Figure 15-14 suggests that elderly<br />
patients can be expected to recover from remifentanil<br />
Figure 15-14. <strong>The</strong> 20%, 50%, and 80% effect-site decrement<br />
curves for 20- and 80-year-old subjects. Provided remifentanil<br />
dose is adequately reduced, as shown in Figure 15-13, there<br />
should be little difference in the awakening time as a function<br />
of age.
222 S.L. Shafer and P. Flood<br />
about as fast as younger subjects, provided the dose has<br />
been appropriately reduced (e.g., Figure 15-13).<br />
<strong>The</strong> unique features of remifentanil are its rapid clearance<br />
and rapid k e0 , resulting in a rapid onset and offset<br />
of drug effect. It is tempting to speculate that these characteristics<br />
will make remifentanil an easy drug to titrate<br />
and that clinicians will not need to consider patient<br />
covariates such as advanced age when choosing a dosing<br />
regimen. However, the rapid onset of drug effect may be<br />
accompanied by rapid onset of adverse events such as<br />
apnea and muscle rigidity. <strong>The</strong> rapid offset of drug effect<br />
can result in patients who are in severe pain at a time<br />
when the anesthesiologist is ill-equipped to deal with the<br />
problem, for example, when the patient is in transit to the<br />
recovery room. It is thus important that anesthesiologists<br />
understand the proper dose adjustment required for the<br />
elderly. By adjusting the bolus and infusion doses, the<br />
anesthesiologist can hope to avoid the peaks and valleys<br />
in remifentanil concentration that might expose elderly<br />
patients to risk. When the proper adjustment is made, the<br />
variability in remifentanil pharmacokinetics is considerably<br />
less than for any other intravenous opioid. This<br />
makes remifentanil the most predictable opioid for treatment<br />
of the elderly.<br />
Methadone<br />
Methadone has several distinguishing characteristics,<br />
including having the longest terminal half-life and being<br />
supplied as a racemic mixture with surprising stereospecific<br />
pharmacology. As shown in Table 15-1 and as evident<br />
in Figure 15-1, the terminal half-life of methadone is<br />
approximately 1 day. 66 As a result, it will take nearly a<br />
week of methadone dosing to reach steady state. When<br />
methadone is used as a chronic analgesic, particularly in<br />
elderly patients, the patient and physician must be made<br />
aware that steady state will not be reached for several<br />
days, requiring vigilance for accumulation to toxicity<br />
during the “run-in” titration of methadone for analgesia.<br />
Also, adequate arrangements for rescue analgesia must<br />
be available during the period before steady-state<br />
levels.<br />
Methadone’s other unique feature is that it is supplied<br />
as a racemate with two enantiomers. l-Methadone is an<br />
opioid agonist, whereas d-methadone is an N-methyl-Daspartate<br />
(NMDA) antagonist. 140 <strong>The</strong> potency of the d-<br />
methadone in blocking NMDA is such that, at clinically<br />
used doses, it may be effective in attenuating opioid tolerance<br />
and preventing central sensitization (hyperalgesia).<br />
141,142 <strong>The</strong>re are no specific studies examining the<br />
pharmacokinetics and pharmacodynamics of methadone<br />
in elderly subjects. However, as the increased brain sensitivity<br />
to opioid drug effect seems to be a class effect for<br />
opioids, it seems prudent to reduce methadone doses by<br />
about 50% in elderly patients compared with younger<br />
patients. Additionally, the NMDA blocking activity of d-<br />
methadone may provide some analgesic synergy between<br />
the enantiomers. Provided methadone is titrated in a<br />
manner that is mindful of the long half-life and the potential<br />
for accumulation, methadone’s rapid onset and sustained<br />
effect make it a rational choice for postoperative<br />
analgesia.<br />
Patient-Controlled <strong>Anesthesia</strong><br />
PCA devices are very effective means to provide postoperative<br />
analgesia in elderly patients. Lavand’Homme and<br />
De Kock 143 have reviewed the use of PCA in the elderly.<br />
<strong>The</strong>y observed that poor pain management places elderly<br />
patients at risk of confusion and outright delirium, and<br />
this may be associated with poorer clinical outcomes.<br />
<strong>The</strong>y emphasized that increased monitoring and individualization<br />
of dosage are essentials in PCA management<br />
of elderly patients. <strong>The</strong>y also observed that elderly<br />
patients may need additional time to become familiar<br />
with PCA devices and that the devices will become ineffective<br />
if elderly patients become confused or agitated.<br />
Macintyre and Jarvis 144 examined morphine PCA in<br />
elderly patients and observed that age is the best predictor<br />
of postoperative morphine requirements. <strong>The</strong>y found<br />
that the average PCA morphine use in the first 24 hours<br />
after surgery was approximately 100 − age. However, they<br />
also emphasized that the dose needed to be individualized,<br />
because there was tenfold variation in the dose in<br />
each age category.<br />
This is similar to the results of Woodhouse and<br />
Mather. 145 <strong>The</strong>y found that elderly patients required significantly<br />
less fentanyl and morphine administered by<br />
PCA following surgery. <strong>The</strong>y also identified a similar<br />
trend for meperidine, but it was less steep and characterized<br />
by higher variability. As seen in Figure 15-15, elderly<br />
patients required about half as much morphine and fentanyl<br />
as younger subjects, consistent with the “50% reduction”<br />
suggestion at the beginning of the chapter.<br />
Gagliese and colleagues 146 also found an approximately<br />
50% reduction in PCA opioid use in elderly patients. In<br />
their study, patients in the younger group (average age =<br />
39) expected more severe pain than those in the older<br />
group (average age = 67). However, both groups obtained<br />
similar efficacy from their PCA devices and expressed<br />
similar levels of satisfaction with PCA as a means of managing<br />
postoperative analgesia. <strong>The</strong> average 24 hour dose<br />
of morphine (or morphine equivalents) in the younger<br />
patients was 67 mg at the end of day one and 44 mg at the<br />
end of day two. In the older patients, the average dose was<br />
39 mg at the end of day one and 28 mg at the end of day<br />
two. In an accompanying editorial, Ready 147 emphasized<br />
that patients must be able to understand and participate<br />
in their care, emphasizing the need to individualize therapy
15. <strong>The</strong> Pharmacology of Opioids 223<br />
sic therapy, be combined with PCA to provide adequate<br />
analgesia at the lowest possible opioid dose in elderly<br />
patients. Beattie et al. 148 have reported that ketorolac<br />
effectively reduces morphine doses in elderly subjects. In<br />
this case, the reduced opioid requirement must be balanced<br />
against the risk of gastric bleeding and fluid retention<br />
induced by ketorolac. However, in appropriate<br />
patients, one or two doses of ketorolac are associated<br />
with only modest risk and would be expected to provide<br />
significant synergy with morphine. 149,150<br />
Suggested Guidelines for Chronic Opioids<br />
in the Elderly<br />
<strong>The</strong> subject of opioids in the management of chronic pain<br />
in the elderly has been extensively reviewed. 151–153 A few<br />
basic principles will be emphasized here:<br />
Figure 15-15. Twenty-four-hour cumulative patient-controlled<br />
analgesia opioid administration as a function of age. Morphine<br />
and fentanyl both show the expected reduction in dose of<br />
about 50%, as predicted by the pharmacokinetic/pharmacodynamic<br />
modeling. Meperidine (pethidine) is more variable,<br />
perhaps reflecting its more complex pharmacology, or the<br />
stimulating effects of normeperidine. (Reprinted with permission<br />
from Woodhouse and Mather. 145 Copyright ©Blackwell<br />
Publishing.)<br />
for elderly patients in whom a cognitive assessment might<br />
be appropriate before using PCA.<br />
It is reasonable that other interventions, such as nerve<br />
blocks, infusions of local anesthetic, and adjuvant analge-<br />
1. In general, opioids should be reserved for those<br />
elderly patients in whom less-toxic alternatives, such as<br />
acetaminophen and nonsteroidal antiinflammatory drugs,<br />
have proven ineffective.<br />
2. It is best to start with the weaker opioids, such as<br />
codeine, and titrate to effect. <strong>The</strong> stronger opioids should<br />
be reserved for patients whose symptoms are inadequately<br />
treated by weaker opioids.<br />
3. Careful monitoring during the initial dose titration<br />
is absolutely essential, particularly with opioids or delivery<br />
systems associated with long half-lives and time to<br />
steady state, such as methadone, oral sustained-release<br />
preparations, and transdermal fentanyl.<br />
4. Opioid-induced constipation may be reduced by the<br />
use of a peripheral opioid antagonist, such as alvimopan<br />
154 and methylnaltrexone. 155 Elderly patients are at<br />
increased risk of drug interactions. <strong>The</strong> risk of drug interactions<br />
particularly precludes the use of chronic meperidine<br />
in elderly patients. However, opioids should be used<br />
with great caution if combined with any drugs that<br />
decrease consciousness (e.g., benzodiazepines). Figure<br />
15-16 shows the interaction between remifentanil and<br />
propofol on ventilation in healthy volunteers as reported<br />
by Nieuwenhuijs and colleagues. 156 Whereas propofol and<br />
remifentanil individually have modest effects on ventilation,<br />
when combined (solid triangles), they demonstrate<br />
profound depression of ventilation. This effect will be<br />
exaggerated in elderly patients because of the increased<br />
sensitivity to opioid drug effects.<br />
5. Elderly patients are at increased risk of confusion in<br />
response to opioids.<br />
6. Rotation of opioids may permit lower doses to be<br />
used, because of the incomplete cross-tolerance and individual<br />
differences in analgesic versus toxicity profiles<br />
among individuals.
224 S.L. Shafer and P. Flood<br />
Ventilation (L/min)<br />
35<br />
30<br />
25<br />
20<br />
15<br />
10<br />
5<br />
0<br />
35 40 45 50 55 60 65 70<br />
P ET CO 2 (mmHg)<br />
Conclusion<br />
Opioids are appropriate for both acute and chronic pain<br />
in elderly patients, particularly when nonopioid analgesics<br />
have failed to provide adequate pain relief. Elderly<br />
patients, on average, need about half the dose of opioids<br />
as younger patients to achieve the same level of analgesic<br />
effect. <strong>The</strong> biologic basis for the increased brain sensitivity<br />
(pharmacodynamic increased potency) to opioids<br />
in elderly patients is not completely understood. Elderly<br />
patients have factors that place them at increased risk<br />
of opioid toxicity, including increased pharmacologic<br />
variability, frequent polypharmacy, noncompliance with<br />
dosage regimens, and impaired renal and hepatic<br />
function.<br />
References<br />
control<br />
propofol (1.5 µg/ml)<br />
remifentanil (1 ng/ml)<br />
remifentanil + propofol<br />
(1 ng/ml) (1.5 µg/ml)<br />
Figure 15-16. <strong>The</strong> interaction between remifentanil and propofol<br />
on ventilation demonstrates a class effect for opioid/hypnotic<br />
synergy. In this figure, propofol very slightly changes the<br />
slope of the CO 2 versus ventilation curve, and remifentanil very<br />
slightly changes the apnea threshold without changing the slope.<br />
However, the combination of propofol and remifentanil (triangles,<br />
lower right) profoundly displaces both the slope and the<br />
apneic threshold. (Reprinted with permission from Nieuwenhuijs<br />
et al. 156 Copyright ©Lippincott Williams & Wilkins.)<br />
1. Anderson GF, Hussey PS. Population aging: a comparison<br />
among industrialized countries. Health Aff 2000;19:<br />
191–203.<br />
2. Ventafridda V, Tamburini M, Caraceni A, De Conno F,<br />
Naldi F. A validation study of the WHO method for cancer<br />
pain relief. Cancer 1987;59:850–856.<br />
3. Jacox A, Carr DB, Payne R. New clinical-practice guidelines<br />
for the management of pain in patients with cancer.<br />
N Engl J Med 1994;330:651–655.<br />
4. Bafitis H, Sargent F 2nd. Human physiological adapt -<br />
ability through the life sequence. J Gerontol 1977;32:402–<br />
410.<br />
5. Klein U, Klein M, Sturm H, et al. <strong>The</strong> frequency of adverse<br />
drug reactions as dependent upon age, sex and duration of<br />
hospitalization. Int J Clin Pharmacol Biopharm 1976;13:<br />
187–195.<br />
6. Crooks J. Aging and drug disposition—pharmacodynamics.<br />
J Chronic Dis 1983;36:85–90.<br />
7. Cepeda MS, Farrar JT, Baumgarten M, Boston R, Carr DB,<br />
Strom BL. Side effects of opioids during short-term administration:<br />
effect of age, gender, and race. Clin Pharmacol<br />
<strong>The</strong>r 2003;74:102–112.<br />
8. Junger A, Hartmann B, Benson M, et al. <strong>The</strong> use of an<br />
anesthesia information management system for prediction<br />
of antiemetic rescue treatment at the postanesthesia care<br />
unit. Anesth Analg 2001;92(5):1203–1209.<br />
9. Sinclair DR, Chung F, Mezei G. Can postoperative nausea<br />
and vomiting be predicted? <strong>Anesthesiology</strong> 1999;91:109–<br />
118.<br />
10. Pert CB, Snyder SH. Opiate receptor: demonstration in<br />
nervous tissue. Science 1973;179:1011–1014.<br />
11. Simon EJ, Hiller JM, Edelman I. Stereospecific binding<br />
of the potent narcotic analgesic (3H) Etorphine to ratbrain<br />
homogenate. Proc Natl Acad Sci USA 1973;70:<br />
1947–1949.<br />
12. Terenius L. Characteristics of the “receptor” for narcotic<br />
analgesics in synaptic plasma membrane fraction from<br />
rat brain. Acta Pharmacol Toxicol (Copenh) 1973;33:<br />
377–384.<br />
13. Hughes J, Smith TW, Kosterlitz HW, Fothergill LA, Morgan<br />
BA, Morris HR. Identification of two related pentapeptides<br />
from the brain with potent opiate agonist activity.<br />
Nature 1975;258:577–580.<br />
14. Li CH, Chung D. Isolation and structure of an untriakontapeptide<br />
with opiate activity from camel pituitary glands.<br />
Proc Natl Acad Sci USA 1976;73:1145–1148.<br />
15. Goldstein A, Tachibana S, Lowney LI, Hunkapiller M,<br />
Hood L. Dynorphin-(1-13), an extraordinarily potent<br />
opioid peptide. Proc Natl Acad Sci USA 1979;76:<br />
6666–6670.<br />
16. Martin WR, Eades CG, Thompson JA, Huppler RE, Gilbert<br />
PE. <strong>The</strong> effects of morphine- and nalorphine-like drugs in<br />
the nondependent and morphine-dependent chronic spinal<br />
dog. J Pharmacol Exp <strong>The</strong>r 1976;197:517–532.<br />
17. Chang KJ, Cooper BR, Hazum E, Cuatrecasas P. Multiple<br />
opiate receptors: different regional distribution in the<br />
brain and differential binding of opiates and opioid<br />
peptides. Mol Pharmacol 1979;16:91–104.<br />
18. Robson LE, Kosterlitz HW. Specific protection of the<br />
binding sites of D-Ala2-D-Leu5-enkephalin (delta-receptors)<br />
and dihydromorphine (mu-receptors). Proc R Soc<br />
Lond B Biol Sci 1979;205:425–432.<br />
19. Schulz R, Wuster M, Krenss H, Herz A. Selective development<br />
of tolerance without dependence in multiple opiate<br />
receptors of mouse vas deferens. Nature 1980;285:242–<br />
243.<br />
20. Pasternak GW, Childers SR, Snyder SH. Opiate analgesia:<br />
evidence for mediation by a subpopulation of opiate<br />
receptors. Science 1980;208:514–516.
15. <strong>The</strong> Pharmacology of Opioids 225<br />
21. Ling GS, Spiegel K, Nishimura SL, Pasternak GW. Dissociation<br />
of morphine’s analgesic and respiratory depressant<br />
actions. Eur J Pharmacol 1983;86:487–488.<br />
22. Ling GS, Spiegel K, Lockhart SH, Pasternak GW. Separation<br />
of opioid analgesia from respiratory depression: evidence<br />
for different receptor mechanisms. J Pharmacol Exp<br />
<strong>The</strong>r 1985;232:149–155.<br />
23. Brown GP, Yang K, King MA, et al. 3-Methoxynaltrexone,<br />
a selective heroin/morphine-6beta-glucuronide antagonist.<br />
FEBS Lett 1997;412:35–38.<br />
24. Crews JC, Sweeney NJ, Denson DD. Clinical efficacy of<br />
methadone in patients refractory to other mu-opioid<br />
receptor agonist analgesics for management of terminal<br />
cancer pain. Case presentations and discussion of incomplete<br />
cross-tolerance among opioid agonist analgesics.<br />
Cancer 1993;72:2266–2272.<br />
25. Mercadante S. Opioid rotation for cancer pain: rationale<br />
and clinical aspects. Cancer 1999;86:1856–1866.<br />
26. Chang A, Emmel DW, Rossi GC, Pasternak GW. Methadone<br />
analgesia in morphine-insensitive CXBK mice. Eur<br />
J Pharmacol 1998;351:189–191.<br />
27. Abbadie C, Rossi GC, Orciuolo A, Zadina JE, Pasternak<br />
GW. Anatomical and functional correlation of the endomorphins<br />
with mu opioid receptor splice variants. Eur J<br />
Neurosci 2002;16:1075–1082.<br />
28. Cadet P. Mu opiate receptor subtypes. Med Sci Monit<br />
2004;10:MS28–32.<br />
29. Stefano GB, Hartman A, Bilfinger TV, et al. Presence of<br />
the mu3 opiate receptor in endothelial cells. Coupling to<br />
nitric oxide production and vasodilation. J Biol Chem<br />
1995;270:30290–30293.<br />
30. Kozak CA, Filie J, Adamson MC, Chen Y, Yu L. Murine<br />
chromosomal location of the mu and kappa opioid receptor<br />
genes. Genomics 1994;21:659–661.<br />
31. Belknap JK, Mogil JS, Helms ML, et al. Localization to<br />
chromosome 10 of a locus influencing morphine analgesia<br />
in crosses derived from C57BL/6 and DBA/2 strains. Life<br />
Sci 1995;57:PL117–124.<br />
32. Lötsch J, Geisslinger G. Are mu-opioid receptor polymorphisms<br />
important for clinical opioid therapy? Trends Mol<br />
Med. 11:82–89, 2005.<br />
33. Romberg RR, Olofsen E, Bijl H, et al. Polymorphism<br />
of mu-opioid receptor gene (OPRM1:c.118A > G) does<br />
not protect against opioid-induced respiratory depression<br />
despite reduced analgesic response. <strong>Anesthesiology</strong> 2005;<br />
102:522–530.<br />
34. Pasternak GW. Multiple opiate receptors: deja vu all over<br />
again. Neuropharmacology 2004;47(Suppl 1):312–323.<br />
35. Chen Y, Mestek A, Liu J, Hurley JA, Yu L. Molecular<br />
cloning and functional expression of a mu-opioid receptor<br />
from rat brain. Mol Pharmacol 1993;44:8–12.<br />
36. Wang JB, Imai Y, Eppler CM, Gregor P, Spivak CE, Uhl<br />
GR. Mu opiate receptor: cDNA cloning and expression.<br />
Proc Natl Acad Sci USA 1993;90:10230–10234.<br />
37. Pan YX, Xu J, Mahurter L, Xu M, Gilbert AK, Pasternak<br />
GW. Identification and characterization of two new human<br />
mu opioid receptor splice variants, hMOR-1O and hMOR-<br />
1X. Biochem Biophys Res Commun 2003;301:1057–1061.<br />
38. Connor M, Christie MD. Opioid receptor signalling mechanisms.<br />
Clin Exp Pharmacol Physiol 1999;26:493–499.<br />
39. North RA. Opioid actions on membrane ion channels. In:<br />
Herz A, ed. Opioids. Handbook of Experimental Pharmacology.<br />
Vol 104. Berlin: Springer-Verlag; 1993:773–797.<br />
40. Scarpace PJ, Tumer N, Mader SL. Beta-adrenergic function<br />
in aging. Basic mechanisms and clinical implications. Drugs<br />
Aging 1991;1:116–129.<br />
41. Scarpace PJ, Abrass IB. Alpha- and beta-adrenergic receptor<br />
function in the brain during senescence. Neurobiol<br />
Aging 1988;9:53–58.<br />
42. Barnhill JG, Greenblatt DJ, Miller LG, Gaver A, Harmatz<br />
JS, Shader RI. Kinetic and dynamic components of<br />
increased benzodiazepine sensitivity in aging animals.<br />
J Pharmacol Exp <strong>The</strong>r 1990;253:1153–1161.<br />
43. Barnhill JG, Miller LG, Greenblatt DJ, Thompson ML,<br />
Ciraulo DA, Shader RI. Benzodiazepine receptor binding<br />
response to acute and chronic stress is increased in aging<br />
animals. Pharmacology 1991;42:181–187.<br />
44. Ueno E, Liu DD, Ho IK, Hoskins B. Opiate receptor characteristics<br />
in brains from young, mature and aged mice.<br />
Neurobiol Aging 1988;9:279–283.<br />
45. Hess GD, Joseph JA, Roth GS. Effect of age on sensitivity<br />
to pain and brain opiate receptors. Neurobiol Aging 1981;<br />
2:49–55.<br />
46. Petkov VV, Petkov VD, Grahovska T, Konstantinova E.<br />
Enkephalin receptor changes in rat brain during aging.<br />
Gen Pharmacol 1984;15:491–495.<br />
47. Fulop T Jr, Kekessy D, Foris G. Impaired coupling of naloxone<br />
sensitive opiate receptors to adenylate cyclase in<br />
PMNLs of aged male subjects. Int J Immunopharmacol<br />
1987;9(6):651–657.<br />
48. Hoskins B, Ho IK. Age-induced differentiation of morphine’s<br />
effect on cyclic nucleotide metabolism. Neurobiol<br />
Aging 1987;8:473–476.<br />
49. Smith MA, Gray JD. Age-related differences in sensitivity<br />
to the antinociceptive effects of opioids in male rats. Influence<br />
of nociceptive intensity and intrinsic efficacy at the mu<br />
receptor. Psychopharmacology (Berl) 2001;156:445–453.<br />
50. Van Crugten JT, Somogyi AA, Nation RL, Reynolds G.<br />
<strong>The</strong> effect of old age on the disposition and antinociceptive<br />
response of morphine and morphine-6 betaglucuronide<br />
in the rat. Pain 1997;71:199–205.<br />
51. Hoskins B, Burton CK, Ho IK. Differences in morphineinduced<br />
antinociception and locomotor activity in mature<br />
adult and aged mice. Pharmacol Biochem Behav 1986;25:<br />
599–605.<br />
52. Helme RD, Gibson SJ. Pain in older people. In: Crombie<br />
IK, Croft PR, Linton SJ, Le Resche L, Von Korff M, eds.<br />
<strong>The</strong> Epidemiology of Pain. 2nd ed. Seattle: IASP Press;<br />
1999:103–112.<br />
53. Helme RD, Gibson SJ. <strong>The</strong> epidemiology of pain in elderly<br />
people. Clin Geriatr Med 2001;17:417–431.<br />
54. Verhaak PF, Kerssens JJ, Dekker J, Sorbi MJ, Bensing JM.<br />
Prevalence of chronic benign pain disorder among adults:<br />
a review of the literature. Pain 1998;77:231–239.<br />
55. Sorkin BA, Rudy TE, Hanlon RB, Turk DC, Stieg RL. Chronic<br />
pain in old and young patients: differences appear less important<br />
than similarities. J Gerontol 1990;45:P64–P68.<br />
56. Edwards RR, Fillingim RB. Age-associated differences in<br />
responses to noxious stimuli. J Gerontol A Biol Sci Med<br />
Sci 2001;56:M180–M185.
226 S.L. Shafer and P. Flood<br />
57. Edwards RR, Fillingim RB, Ness TJ. Age-related differences<br />
in endogenous pain modulation: a comparison of<br />
diffuse noxious inhibitory controls in healthy older and<br />
younger adults. Pain 2003;101:155–165.<br />
58. Washington LL, Gibson SJ, Helme RD. Age-related differences<br />
in the endogenous analgesic response to repeated<br />
cold water immersion in human volunteers. Pain 2000;<br />
89:89–96.<br />
59. Casale G, Pecorini M, Cuzzoni G, de Nicola P. Betaendorphin<br />
and cold pressor test in the aged. Gerontology<br />
1985;31:101–105.<br />
60. Zheng Z, Gibson SJ, Khalil Z, Helme RD, McMeeken JM.<br />
Age-related differences in the time course of capsaicininduced<br />
hyperalgesia. Pain 2000;85:51–58.<br />
61. Chakour MC, Gibson SJ, Bradbeer M, Helme RD. <strong>The</strong><br />
effect of age on A delta- and C-fibre thermal pain perception.<br />
Pain 1996;64:143–152.<br />
62. Scott JC, Stanski DR. Decreased fentanyl/alfentanil dose<br />
requirement with increasing age: a pharmacodynamic<br />
basis. J Pharmacol Exp <strong>The</strong>r 1987;240:159–166.<br />
63. Hudson RJ, Bergstrom RG, Thomson IR, Sabourin MA,<br />
Rosenbloom M, Strunin L. Pharmacokinetics of sufentanil<br />
in patients undergoing abdominal aortic surgery. <strong>Anesthesiology</strong><br />
1989;70:426–431.<br />
64. Minto CF, Schnider TW, Egan T, et al. <strong>The</strong> influence of age<br />
and gender on the pharmacokinetics and pharmacodynamics<br />
of remifentanil. I. Model development. <strong>Anesthesiology</strong><br />
1997;86:10–23.<br />
65. Lotsch J, Skarke C, Schmidt H, Liefhold J, Geisslinger G.<br />
Pharmacokinetic modeling to predict morphine and morphine-6-glucuronide<br />
plasma concentrations in healthy<br />
young volunteers. Clin Pharmacol <strong>The</strong>r 2002;72:151–<br />
162.<br />
66. Inturrisi CE, Colburn WA, Kaiko RF, Houde RW, Foley<br />
KM. Pharmacokinetics and pharmacodynamics of methadone<br />
in patients with chronic pain. Clin Pharmacol <strong>The</strong>r<br />
1987;41:392–401.<br />
67. Bjorkman S. Reduction and lumping of physiologically<br />
based pharmacokinetic models: prediction of the disposition<br />
of fentanyl and pethidine in humans by successively<br />
simplified models. J Pharmacokinet Pharmacodyn 2003;<br />
30:285–307.<br />
68. Drover DR, Angst MS, Valle M, et al. Input character -<br />
istics and bioavailability after administration of immediate<br />
and a new extended-release formulation of hydromorphone<br />
in healthy volunteers. <strong>Anesthesiology</strong> 2002;97:<br />
827–836.<br />
69. Scott JC, Cooke JE, Stanski DR. Electroencephalographic<br />
quantitation of opioid effect: comparative pharmacodynamics<br />
of fentanyl and sufentanil. <strong>Anesthesiology</strong> 1991;<br />
74:34–42.<br />
70. Inturrisi CE, Portenoy RK, Max MB, Colburn WA, Foley<br />
KM. Pharmacokinetic-pharmacodynamic relationships of<br />
methadone infusions in patients with cancer pain. Clin<br />
Pharmacol <strong>The</strong>r 1990;47:565–577.<br />
71. Qiao GL, Fung KF. Pharmacokinetic-pharmacodynamic<br />
modelling of meperidine in goats (II): modelling. J Vet<br />
Pharmacol <strong>The</strong>r 1994;17:127–134.<br />
72. Hill JL, Zacny JP. Comparing the subjective, psychomotor,<br />
and physiological effects of intravenous hydromorphone<br />
and morphine in healthy volunteers. Psychopharmacology<br />
(Berl) 2000;152:31–39.<br />
73. Shafer SL, Varvel JR. Pharmacokinetics, pharmacodynamics,<br />
and rational opioid selection. <strong>Anesthesiology</strong> 1991;74:<br />
53–63.<br />
74. Shafer SL, Gregg KM. Algorithms to rapidly achieve and<br />
maintain stable drug concentrations at the site of drug<br />
effect with a computer-controlled infusion pump. J Pharmacokinet<br />
Biopharm 1992;20:147–169.<br />
75. Henthorn TK, Krejcie TC, Shanks CA, Avram MJ.<br />
Time-dependent distribution volume and kinetics of the<br />
pharmacodynamic effector site. J Pharm Sci 1992;81:<br />
1136–1138.<br />
76. Wada DR, Drover DR, Lemmens HJ. Determination of the<br />
distribution volume that can be used to calculate the intravenous<br />
loading dose. Clin Pharmacokinet 1998;35:1–7.<br />
77. Gourlay GK, Kowalski SR, Plummer JL, Cousins MJ, Armstrong<br />
PJ. Fentanyl blood concentration-analgesic response<br />
relationship in the treatment of postoperative pain. Anesth<br />
Analg 1988;67:329–337.<br />
78. Lehmann KA, Ribbert N, Horrichs-Haermeyer G.<br />
Postoperative patient-controlled analgesia with alfentanil:<br />
analgesic efficacy and minimum effective concentrations.<br />
J Pain Symptom Manage 1990;5:249–258.<br />
79. Dahlstrom B, Tamsen A, Paalzow L, Hartvig P. Patientcontrolled<br />
analgesic therapy. Part IV. Pharmacokinetics<br />
and analgesic plasma concentrations of morphine. Clin<br />
Pharmacokinet 1982;7:266–279.<br />
80. Gourlay GK, Willis RJ, Wilson PR. Postoperative pain<br />
control with methadone: influence of supplementary methadone<br />
doses and blood concentration-response relationships.<br />
<strong>Anesthesiology</strong> 1984;61:19–26.<br />
81. Mather LE, Glynn CJ. <strong>The</strong> minimum effective analgetic<br />
blood concentration of pethidine in patients with intractable<br />
pain. Br J Clin Pharmacol 1982;14:385–390.<br />
82. Coda B, Tanaka A, Jacobson RC, Donaldson G, Chapman<br />
CR. Hydromorphone analgesia after intravenous bolus<br />
administration. Pain 1997;71:41–48.<br />
83. Hill JL, Zacny JP. Comparing the subjective, psychomotor,<br />
and physiological effects of intravenous hydromorphone<br />
and morphine in healthy volunteers. Psychopharmacology<br />
(Berl) 2000;152:31–39.<br />
84. Hughes MA, Glass PS, Jacobs JR. Context-sensitive<br />
half-time in multicompartment pharmacokinetic models<br />
for intravenous anesthetic drugs. <strong>Anesthesiology</strong> 1992;76:<br />
334–341.<br />
85. Youngs EJ, Shafer SL. Pharmacokinetic parameters relevant<br />
to recovery from opioids. <strong>Anesthesiology</strong> 1994;81:<br />
833–842.<br />
86. Gintzler AR, Gershon MD, Spector S. A nonpeptide morphine-like<br />
compound: immunocytochemical localization in<br />
the mouse brain. Science 1978;199:447–448.<br />
87. Goldstein A, Barrett RW, James IF, et al. Morphine and<br />
other opiates from beef brain and adrenal. Proc Natl Acad<br />
Sci USA 1985;82:5203–5207.<br />
88. Donnerer J, Oka K, Brossi A, Rice KC, Spector S. Presence<br />
and formation of codeine and morphine in the rat. Proc<br />
Natl Acad Sci USA 1986;83:4566–4567.<br />
89. Cardinale GJ, Donnerer J, Finck AD, Kantrowitz JD, Oka<br />
K, Spector S. Morphine and codeine are endogenous com-
15. <strong>The</strong> Pharmacology of Opioids 227<br />
ponents of human cerebrospinal fluid. Life Sci 1987;40:<br />
301–306.<br />
90. Lotsch J, Geisslinger G. Morphine-6-glucuronide: an analgesic<br />
of the future? Clin Pharmacokinet 2001;40:485–499.<br />
91. Paul D, Standifer KM, Inturrisi CE, Pasternak GW. Pharmacological<br />
characterization of morphine-6 beta-glucuronide,<br />
a very potent morphine metabolite. J Pharmacol Exp<br />
<strong>The</strong>r 1989;251:477–483.<br />
92. Lotsch J, Kobal G, Stockmann A, Brune K, Geisslinger G.<br />
Lack of analgesic activity of morphine-6-glucuronide after<br />
short-term intravenous administration in healthy volunteers.<br />
<strong>Anesthesiology</strong> 1997;87(6):1348–1358.<br />
93. Lotsch J, Kobal G, Geisslinger G. No contribution of<br />
morphine-6-glucuronide to clinical morphine effects after<br />
short-term administration. Clin Neuropharmacol 1998;21:<br />
351–354.<br />
94. Wolff T, Samuelsson H, Hedner T. Morphine and morphine<br />
metabolite concentrations in cerebrospinal fluid and<br />
plasma in cancer pain patients after slow-release oral<br />
morphine administration. Pain 1995;62:147–154.<br />
95. Portenoy RK, Foley KM, Stulman J, et al. Plasma morphine<br />
and morphine-6-glucuronide during chronic morphine<br />
therapy for cancer pain: plasma profiles, steady-state concentrations<br />
and the consequences of renal failure. Pain<br />
1991;47:13–19.<br />
96. Cockcroft DW, Gault MH. Prediction of creatinine clearance<br />
from serum creatinine. Nephron 1976;16:31–41.<br />
97. Lotsch J, Skarke C, Schmidt H, Grosch S, Geisslinger G.<br />
<strong>The</strong> transfer half-life of morphine-6-glucuronide from<br />
plasma to effect site assessed by pupil size measurement<br />
in healthy volunteers. <strong>Anesthesiology</strong> 2001;95:1329–1338.<br />
98. Skarke C, Jarrar M, Erb K, Schmidt H, Geisslinger G,<br />
Lotsch J. Respiratory and miotic effects of morphine in<br />
healthy volunteers when P-glycoprotein is blocked by<br />
quinidine. Clin Pharmacol <strong>The</strong>r 2003;74:303–311.<br />
99. Skarke C, Darimont J, Schmidt H, Geisslinger G, Lotsch J.<br />
Analgesic effects of morphine and morphine-6-glucuronide<br />
in a transcutaneous electrical pain model in healthy<br />
volunteers. Clin Pharmacol <strong>The</strong>r 2003;73:107–121.<br />
100. Letrent SP, Polli JW, Humphreys JE, Pollack GM, Brouwer<br />
KR, Brouwer KL. P-glycoprotein-mediated transport of<br />
morphine in brain capillary endothelial cells. Biochem<br />
Pharmacol 1999;58:951–957.<br />
101. Dahan A, Romberg R, Teppema L, Sarton E, Bijl H,<br />
Olofsen E. Simultaneous measurement and integrated<br />
analysis of analgesia and respiration after an intravenous<br />
morphine infusion. <strong>Anesthesiology</strong> 2004;101:1201–1209.<br />
102. Aubrun F, Monsel S, Langeron O, Coriat P, Riou B. Postoperative<br />
titration of intravenous morphine in the elderly<br />
patient. <strong>Anesthesiology</strong> 2002;96:17–23.<br />
103. Aubrun F, Bunge D, Langeron O, Saillant G, Coriat P, Riou<br />
B. Postoperative morphine consumption in the elderly<br />
patient. <strong>Anesthesiology</strong> 2003;99:160–165.<br />
104. Wagner LE 2nd, Eaton M, Sabnis SS, Gingrich KJ.<br />
Meperidine and lidocaine block of recombinant voltagedependent<br />
Na+ channels: evidence that meperidine is a<br />
local anesthetic. <strong>Anesthesiology</strong> 1999;91:1481–1490.<br />
105. Wolff M, Olschewski A, Vogel W, Hempelmann G. Meperidine<br />
suppresses the excitability of spinal dorsal horn<br />
neurons. <strong>Anesthesiology</strong> 2004;100:947–955.<br />
106. Holmberg L, Odar-Cederlof I, Boreus LO, Heyner L,<br />
Ehrnebo M. Comparative disposition of pethidine and<br />
norpethidine in old and young patients. Eur J Clin Pharmacol<br />
1982;22:175–179.<br />
107. Seifert CF, Kennedy S. Meperidine is alive and well in the<br />
new millennium: evaluation of meperidine usage patterns<br />
and frequency of adverse drug reactions. Pharmacotherapy<br />
2004;24:776–783.<br />
108. Odar-Cederlof I, Boreus LO, Bondesson U, Holmberg L,<br />
Heyner L. Comparison of renal excretion of pethidine<br />
(meperidine) and its metabolites in old and young patients.<br />
Eur J Clin Pharmacol 1985;28:171–175.<br />
109. Huang YF, Upton RN, Rutten AJ, Mather LE. <strong>The</strong> hemodynamic<br />
effects of intravenous bolus doses of meperidine<br />
in conscious sheep. Anesth Analg 1994;78:442–449.<br />
110. Zornberg GL, Bodkin JA, Cohen BM. Severe adverse<br />
interaction between pethidine and selegiline. Lancet 1991;<br />
337:246.<br />
111. Keeri-Szanto M. Anaesthesia time/dose curves IX: the use<br />
of hydromorphone in surgical anaesthesia and postoperative<br />
pain relief in comparison to morphine. Can Anaesth<br />
Soc J 1976;23:587–595.<br />
112. Kopp A, Wachauer D, Hoerauf KH, Zulus E, Reiter WJ,<br />
Steltzer H. Effect of preemptive hydromorphone administration<br />
on postoperative pain relief—a randomized controlled<br />
trial. Wien Klin Wochenschr 2000;112:1002–1006.<br />
113. Rapp SE, Egan KJ, Ross BK, Wild LM, Terman GW, Ching<br />
JM. A multidimensional comparison of morphine and<br />
hydromorphone patient-controlled analgesia. Anesth<br />
Analg 1996;82:1043–1048.<br />
114. Liu S, Carpenter RL, Mulroy MF, et al. Intravenous versus<br />
epidural administration of hydromorphone. Effects on<br />
analgesia and recovery after radical retropubic prostatectomy.<br />
<strong>Anesthesiology</strong> 1995;82:682–688.<br />
115. Brose WG, Tanelian DL, Brodsky JB, Mark JB, Cousins<br />
MJ. CSF and blood pharmacokinetics of hydromorphone<br />
and morphine following lumbar epidural administration.<br />
Pain 1991;45:11–15.<br />
116. Halpern SH, Arellano R, Preston R, et al. Epidural<br />
morphine vs hydromorphone in post-caesarean section<br />
patients. Can J Anaesth 1996;43:595–598.<br />
117. Bentley JB, Borel JD, Nenad RE Jr, Gillespie TJ. Age<br />
and fentanyl pharmacokinetics. Anesth Analg 1982;61:968–<br />
971.<br />
118. Singleton MA, Rosen JI, Fisher DM. Pharmacokinetics of<br />
fentanyl in the elderly. Br J Anaesth 1988;60:619–622.<br />
119. Scott JC, Ponganis KV, Stanski DR. EEG quantitation of<br />
narcotic effect: the comparative pharmacodynamics of<br />
fentanyl and alfentanil. <strong>Anesthesiology</strong> 1985;62:234–241.<br />
120. Martin G, Glass PS, Breslin DS, et al. A study of anesthetic<br />
drug utilization in different age groups. J Clin Anesth<br />
2003;15:194–200.<br />
121. Holdsworth MT, Forman WB, Killilea TA, et al. Transdermal<br />
fentanyl disposition in elderly subjects. Gerontology<br />
1994;40:32–37.<br />
122. Davis MP, Srivastava M. Demographics, assessment and<br />
management of pain in the elderly. Drugs Aging 2003;20:<br />
23–57.<br />
123. Kharasch ED, Hoffer C, Whittington D. Influence of age<br />
on the pharmacokinetics and pharmacodynamics of oral
228 S.L. Shafer and P. Flood<br />
transmucosal fentanyl citrate. <strong>Anesthesiology</strong> 2004;101:<br />
738–743.<br />
124. Shafer A, Sung ML, White PF. Pharmacokinetics and pharmacodynamics<br />
of alfentanil infusions during general anesthesia.<br />
Anesth Analg 1986;65:1021–1028.<br />
125. Sitar DS, Duke PC, Benthuysen JL, Sanford TJ, Smith NT.<br />
Aging and alfentanil disposition in healthy volunteers and<br />
surgical patients. Can J Anaesth 1989;36:149–154.<br />
126. Kent AP, Dodson ME, Bower S. <strong>The</strong> pharmacokinetics and<br />
clinical effects of a low dose of alfentanil in elderly patients.<br />
Acta Anaesthesiol Belg 1988;39:25–33.<br />
127. Lemmens HJ, Burm AG, Hennis PJ, Gladines MP, Bovill JG.<br />
Influence of age on the pharmacokinetics of alfentanil.<br />
Gender dependence. Clin Pharmacokinet 1990;19:416–422.<br />
128. Maitre PO, Vozeh S, Heykants J, Thomson DA, Stanski<br />
DR. Population pharmacokinetics of alfentanil: the average<br />
dose-plasma concentration relationship and interindividual<br />
variability in patients. <strong>Anesthesiology</strong> 1987;68:59–67.<br />
129. Raemer DB, Buschman A, Varvel JR, et al. <strong>The</strong> prospective<br />
use of population pharmacokinetics in a computerdriven<br />
system for alfentanil. <strong>Anesthesiology</strong> 1990;73:<br />
66–72.<br />
130. Lemmens HJ, Burm AG, Bovill JG, Hennis PJ. Pharmacodynamics<br />
of alfentanil as a supplement to nitrous oxide<br />
anaesthesia in the elderly patient. Br J Anaesth 1988;<br />
61:173–179.<br />
131. Lemmens HJ, Bovill JG, Hennis PJ, Burm AG. Age has no<br />
effect on the pharmacodynamics of alfentanil. Anesth<br />
Analg 1988;67:956–960.<br />
132. Lemmens HJ, Burm AG, Bovill JG, Hennis PJ, Gladines<br />
MP. Pharmacodynamics of alfentanil. <strong>The</strong> role of plasma<br />
protein binding. <strong>Anesthesiology</strong> 1992;76:65–70.<br />
133. Lemmens HJ, Bovill JG, Burm AG, Hennis PJ. Alfentanil<br />
infusion in the elderly. Prolonged computer-assisted infusion<br />
of alfentanil in the elderly surgical patient. Anaesthesia<br />
1988;43:850–856.<br />
134. Scott JC, Cooke JE, Stanski DR. Electroencephalographic<br />
quantitation of opioid effect: comparative pharmacodynamics<br />
of fentanyl and sufentanil. <strong>Anesthesiology</strong> 1991;<br />
74:34–42.<br />
135. Helmers JH, van Leeuwen L, Zuurmond WW. Sufentanil<br />
pharmacokinetics in young adult and elderly surgical<br />
patients. Eur J Anaesthesiol 1994;11:181–185.<br />
136. Gepts E, Shafer SL, Camu F, et al. Linearity of pharmacokinetics<br />
and model estimation of sufentanil. <strong>Anesthesiology</strong><br />
1995;83:1194–1204.<br />
137. Matteo RS, Schwartz AE, Ornstein E, Young WL, Chang<br />
WJ. Pharmacokinetics of sufentanil in the elderly surgical<br />
patient. Can J Anaesth 1990;37:852–856.<br />
138. Hofbauer R, Tesinsky P, Hammerschmidt V, et al. No<br />
reduction in the sufentanil requirement of elderly patients<br />
undergoing ventilatory support in the medical intensive<br />
care unit. Eur J Anaesthesiol 1999;16:702–707.<br />
139. Minto CF, Schnider TW, Shafer SL. <strong>The</strong> influence of age<br />
and gender on the pharmacokinetics and pharmacodynamics<br />
of remifentanil. II. Model application. <strong>Anesthesiology</strong><br />
1997;86:24–33.<br />
140. Shimoyama N, Shimoyama M, Elliott KJ, Inturrisi CE.<br />
d-Methadone is antinociceptive in the rat formalin test.<br />
J Pharmacol Exp <strong>The</strong>r 1997;283:648–652.<br />
141. Davis AM, Inturrisi CE. d-Methadone blocks morphine<br />
tolerance and N-methyl-D-aspartate-induced hyperalgesia.<br />
J Pharmacol Exp <strong>The</strong>r 1999;289:1048–1053.<br />
142. Callahan RJ, Au JD, Paul M, Liu C, Yost CS. Functional<br />
inhibition by methadone of N-methyl-D-aspartate receptors<br />
expressed in Xenopus oocytes: stereospecific and<br />
subunit effects. Anesth Analg 2004;98:653–659.<br />
143. Lavand’Homme P, De Kock M. Practical guidelines on the<br />
postoperative use of patient-controlled analgesia in the<br />
elderly. Drugs Aging 1998;13:9–16.<br />
144. Macintyre PE, Jarvis DA. Age is the best predictor<br />
of postoperative morphine requirements. Pain 1996;64:<br />
357–364.<br />
145. Woodhouse A, Mather LE. <strong>The</strong> influence of age upon<br />
opioid analgesic use in the patient-controlled analgesia<br />
environment. Anaesthesia 1997;52:949–955.<br />
146. Gagliese L, Jackson M, Ritvo P, Wowk A, Katz J. Age is<br />
not an impediment to effective use of patient-controlled<br />
analgesia by surgical patients. <strong>Anesthesiology</strong> 2000;93:<br />
601–610.<br />
147. Ready LB. PCA is effective for older patients, but are<br />
there limits? <strong>Anesthesiology</strong> 2000;93:597–598.<br />
148. Beattie WS, Warriner CB, Etches R, et al. <strong>The</strong> addition of<br />
continuous intravenous infusion of ketorolac to a patientcontrolled<br />
analgetic morphine regime reduced postoperative<br />
myocardial ischemia in patients undergoing elective<br />
total hip or knee arthroplasty. Anesth Analg 1997;84:<br />
715–722.<br />
149. Malmberg AB, Yaksh TL. Pharmacology of the spinal<br />
action of ketorolac, morphine, ST-91, U50488H, and L-PIA<br />
on the formalin test and an isobolographic analysis of the<br />
NSAID interaction. <strong>Anesthesiology</strong> 1993;79:270–281.<br />
150. Lashbrook JM, Ossipov MH, Hunter JC, Raffa RB,<br />
Tallarida RJ, Porreca F. Synergistic antiallodynic effects<br />
of spinal morphine with ketorolac and selective COX1-<br />
and COX2-inhibitors in nerve-injured rats. Pain 1999;82:<br />
65–72.<br />
151. Gloth FM 3rd. Pain management in older adults: prevention<br />
and treatment. J Am Geriatr Soc 2001;49:188–199.<br />
152. Wilder-Smith OH. Opioid use in the elderly. Eur J Pain<br />
2005;9:137–140.<br />
153. Nikolaus T, Zeyfang A. Pharmacological treatments for<br />
persistent non-malignant pain in older persons. Drugs<br />
Aging 2004;21:19–41.<br />
154. Taguchi A, Sharma N, Saleem RM, et al. Selective postoperative<br />
inhibition of gastrointestinal opioid receptors.<br />
N Engl J Med 2001;345:935–940.<br />
155. Kurz A, Sessler DI. Opioid-induced bowel dysfunction:<br />
pathophysiology and potential new therapies. Drugs 2003;<br />
63:649–671.<br />
156. Nieuwenhuijs DJ, Olofsen E, Romberg RR, et al. Response<br />
surface modeling of remifentanil-propofol interaction on<br />
cardiorespiratory control and bispectral index. <strong>Anesthesiology</strong><br />
2003;98:312–322.
16<br />
Intravenous Hypnotic Anesthetics<br />
Matthew D. McEvoy and J.G. Reves<br />
This chapter discusses the pharmacology of frequently<br />
used intravenous hypnotic agents in the geriatric patient.<br />
<strong>The</strong> focus of this chapter is the changes in pharmacokinetics<br />
and pharmacodynamics in the geriatric patient<br />
specific to propofol, thiopental, midazolam, and etomidate,<br />
the four most popular intravenous agents for sedation,<br />
induction, and maintenance of general anesthesia.<br />
Propofol<br />
Propofol was first investigated in Europe in the 1980s.<br />
Initially the drug was suspended in a solvent that caused<br />
anaphylactoid reactions in some patients. It was reformulated<br />
in a different preparation and it has gained widespread<br />
use ever since. Because of its quick onset of action,<br />
fairly predictable dose-response, and quick termination<br />
of action, propofol is only second to thiopental in use for<br />
the intravenous induction of general anesthesia. 1 Propofol<br />
is also the focus of a tremendous amount of research<br />
in target-controlled infusion techniques, both in the operating<br />
room (OR) and in non-OR anesthesia.<br />
Pharmacology: Structure/Action<br />
Propofol (2,6-diisopropylphenol) is a hypnotic drug in<br />
the class of the alkylphenols that principally works at the<br />
gamma-aminobutyric acid-A (GABA A ) receptor site in<br />
the central nervous system (CNS). 2 However, it has also<br />
been postulated in recent years that propofol might have<br />
additional action at excitatory amino acid receptors. 2,3<br />
Propofol is composed of a phenol ring with two isopropyl<br />
groups attached to it. It is not water soluble and is thus<br />
prepared in an oil-water emulsion consisting of soybean<br />
oil, egg lecithin, and glycerol. 4 This is important because<br />
this preparation can support the growth of bacteria, even<br />
though it contains disodium edetate to retard bacterial<br />
growth. Because of this unique preparation, propofol is<br />
not considered to be antimicrobially preserved under<br />
United States Pharmacopeia specifications. Thus, the<br />
current recommendations are that sterile technique<br />
should be used when handling and administering this<br />
drug, as with all intravenous anesthetics, and that any<br />
propofol withdrawn from a vial should be used within<br />
6 hours and any vial that is spiked and used as an<br />
intravenous infusion should be completely used within<br />
12 hours. Any amount remaining after those times should<br />
be discarded. 5,6<br />
Pharmacodynamics<br />
Central Nervous System Effects<br />
Propofol has numerous effects on various organ systems<br />
throughout the body. Like thiopental, it has favorable<br />
effects on CNS parameters, as it lowers cerebral metabolic<br />
rate (CMRO 2 ), cerebral blood flow (CBF), and<br />
intracranial pressure (ICP) (Table 16-1). 7 If a large bolus<br />
is given, propofol does have the ability to lower the mean<br />
arterial pressure (MAP) considerably, possibly lowering<br />
cerebral perfusion pressure (CPP) below a critical level<br />
(
230 M.D. McEvoy and J.G. Reves<br />
Table 16-1. Cardiovascular, respiratory, and cerebral effects of several intravenous hypnotic agents.<br />
Cardiovascular* Respiratory* Cerebral*<br />
Agent HR MAP Vent B’dil CBF CMRO 2 ICP<br />
Propofol 0/↓↓ ↓↓↓ ↓↓/↓↓↓ ? ↓↓↓ ↓↓↓ ↓↓↓<br />
Thiopental ↑↑/↑ ↓↓/↓↓↓ ↓↓/↓↓↓ ↓ ↓↓↓ ↓↓↓ ↓↓↓<br />
Etomidate 0 0/↓ ↓/↓↓ 0 ↓↓↓ ↓↓↓ ↓↓↓<br />
Midazolam ↑ ↓↓ ↓↓/↓↓↓ 0 ↓↓ ↓↓ ↓↓<br />
Source: Modified with permission from Morgan GE Jr, Mikhail MS, Murray MJ. Clinical <strong>Anesthesiology</strong>. 3rd ed. New York/Stamford, CT: McGraw-<br />
Hill/Appleton & Lange; 2002.<br />
0 = no change, ↑/↓ = minimal change in corresponding direction, ↑↑/↓↓ = moderate change in corresponding direction, ↑↑↑/↓↓↓ = marked change<br />
in corresponding direction, HR = heart rate, MAP = mean arterial pressure, Vent = ventilation, B’dil = bronchodilation, CBF = cerebral blood<br />
flow, CMRO 2 = cerebral metabolic rate, ICP = intracranial pressure.<br />
*Where there is a difference between the young adult and the geriatric patient, the first set of arrows indicates the response in the young adult<br />
and the second set of arrows indicates the response in the geriatric patient.<br />
EEG stage is regained. 10 <strong>The</strong> EEG changes described<br />
above cause a shorter duration of seizure in the electroconvulsive<br />
therapy (ECT) patient, but they also allow for<br />
a blunted hypertensive and hyperdynamic response that<br />
is often seen in these patients. 11 Methohexital will allow<br />
for longer seizure duration, but it does not block the<br />
hypertensive response to ECT as much and thus it is not<br />
as ideal in the geriatric patient who is likely to have<br />
cardiac disease. Although propofol often allows for seizures<br />
of a clinically acceptable duration, 11 many psychiatrists<br />
prefer methohexital for ECT.<br />
<strong>The</strong> brain becomes more sensitive to propofol with<br />
increasing age. Schnider et al. 12 reported that geriatric<br />
patients were approximately 30% more sensitive to the<br />
pharmacodynamic effects of propofol than younger<br />
subjects, as measured by EEG changes. This was found<br />
to be true for both induction doses and infusions. Thus,<br />
it seems that increasing age causes changes in the brain<br />
that increase the effective potency of propofol for the<br />
geriatric patient.<br />
Respiratory Effects<br />
Propofol causes dose-related depression of ventilation<br />
and it is thought to produce some bronchodilation,<br />
although this is controversial (Table 16-1). 13,14 In standard<br />
induction doses, propofol causes apnea. 15 However, when<br />
compared with thiopental, respirations are lost later and<br />
recovered earlier. 16 With intravenous infusions for sedation,<br />
propofol causes increasing levels of respiratory<br />
depression, mainly by affecting the tidal volume. Furthermore,<br />
airway reflexes are depressed more so with propofol<br />
than with equivalent doses of thiopental or etomidate,<br />
and this effect is greatly enhanced by the addition of<br />
opioids. 17 Also, although propofol does not inhibit hypoxic<br />
pulmonary vasoconstriction, it does seem to blunt both<br />
the hypoxic and hypercapnic ventilatory responses. 16,18–20<br />
All of these changes described above have particular<br />
relevance for the elderly patient. Because of increases in<br />
closing capacity with increasing age, which will exceed<br />
functional residual capacity (FRC) even in the upright<br />
position in a 65-year-old individual, desaturation can<br />
occur at a faster rate. In the elderly, this occurs as a result<br />
of an increase in shunt fraction rather than a reduced<br />
FRC, as is seen with the obese or in patients with restrictive<br />
lung disorders. 21 <strong>The</strong> elderly also have a decreased<br />
cough reflex and thus a decreased ability to clear secretions.<br />
22 This inherently decreased cough reflex in the<br />
elderly patient combined with the suppression of this<br />
reflex from propofol puts the elderly person at higher risk<br />
for aspiration during its use. Furthermore, the elderly<br />
patient already has a blunted hypoxic and hypercapnic<br />
ventilatory response compared with the average adult<br />
patient. 22 <strong>The</strong>se changes call for great vigilance when<br />
administering propofol to an elderly patient for minimal<br />
alveolar concentration (MAC) anesthesia or even light<br />
sedation. Ventilation should be closely monitored, particularly<br />
if supplemental oxygen is used, because the<br />
hypercapnic ventilatory response will become the primary<br />
regulator of respiration. This is important because supplemental<br />
oxygen could prevent hypoxemia, but allow for a<br />
progressive hypercapnia that could be dangerous to the<br />
patient. Finally, all of these effects are increased with the<br />
concurrent use of opioids, thus requiring even greater<br />
attention in operative and procedural situations when the<br />
elderly patient is maintaining oxygenation and ventilation<br />
through spontaneous respirations without a secure airway<br />
or end-tidal carbon dioxide monitoring. However, all of<br />
the evidence cited thus far would suggest that increased<br />
pharmacodynamic sensitivity in the elderly patient moves<br />
in a parallel manner for respiratory depression and sedation/hypnosis;<br />
that is, the patient is not fully awake and<br />
merely experiencing decreased respiratory drive. Thus,<br />
in the spontaneously ventilating patient, the gradual
16. Intravenous Hypnotic Anesthetics 231<br />
titration of propofol matched with a vigilance attentive to<br />
signs of adequate respiration and level of sedation should<br />
provide for a safe and effective anesthetic.<br />
Cardiovascular Effects<br />
Propofol causes little change in heart rate but can cause<br />
profound changes in MAP when given in induction bolus<br />
doses (Table 16-1). 23 <strong>The</strong>se changes are caused by a reduction<br />
in systemic vascular resistance (via inhibition of sympathetic<br />
vasoconstriction) and preload, as well as through<br />
direct effects on myocardial contractility. This hypotension<br />
is more pronounced than that which is seen with the<br />
administration of thiopental, etomidate, or midazolam. In<br />
the normal adult patient, this hypotension is well tolerated<br />
and it is readily reversed during the stimulation of<br />
laryngoscopy and intubation. However, studies have<br />
shown that the degree of hypotension is increased and an<br />
adequate hemodynamic response to a bolus induction is<br />
decreased in the geriatric patient. This occurs by several<br />
mechanisms. First, propofol impairs the arterial baroreceptor<br />
reflex to hypotension, which is already decreased<br />
in the geriatric patient. 24 Second, the geriatric patient is<br />
more likely to have ventricular dysfunction. A decrease<br />
in preload in these patients may result in a significant<br />
decrease in cardiac output. Third, these patients are often<br />
taking beta-blockers and diuretics or other therapies that<br />
cause hypovolemia in the perioperative period. <strong>The</strong><br />
former will reduce the magnitude of any baroreceptormediated<br />
reflex tachycardia to a decrease in blood pressure,<br />
whereas the latter will tend to make the patient<br />
more sensitive to changes in systemic vascular resistance<br />
and preload secondary to being relatively intravascularly<br />
hypovolemic. 24 Finally, it is possible for a profound<br />
decrease in preload to result in a vagally mediated reflex<br />
bradycardia. 25 Practically speaking, these concerns can be<br />
applied clinically in two general categories. First, for the<br />
geriatric patient with significant cardiac disease, it is best<br />
to avoid a rapid bolus induction with propofol. Second,<br />
many of the untoward effects noted above can be greatly<br />
minimized if a slower infusion induction is performed<br />
with laryngoscopy being performed after reaching a<br />
pharmacodynamic endpoint, such as a bispectral index<br />
(BIS) value of less than 60 (see discussion below). 26<br />
Other Effects<br />
Two unique beneficial effects of propofol are noteworthy.<br />
Propofol has both antiemetic and antipruritic properties.<br />
27,28 Thus, its intraoperative and perioperative use has<br />
the potential to reduce the need for traditional antiemetic<br />
and possibly antipruritic medications in the postoperative<br />
period. This is particularly important in the geriatric<br />
patient who may be more susceptible to the untoward<br />
effects of drugs that work at cholinergic and dopaminergic<br />
sites in the normal treatment of nausea and pruritus.<br />
Metabolism and Disposition<br />
(Pharmacokinetics)<br />
<strong>The</strong> pharmacokinetics of propofol involve a very large<br />
volume of distribution, rapid redistribution, and rapid<br />
elimination via hepatic and extrahepatic routes. Because<br />
of high lipid solubility, it has an onset of action of one<br />
arm-to-brain circulation time (almost as fast as thiopental).<br />
Rapid awakening from a single bolus is the result of<br />
extensive redistribution to non-CNS sites throughout the<br />
body. Its initial distribution half-life in a healthy adult<br />
patient is approximately 2 minutes. 29,30<br />
<strong>The</strong>re are various changes in the pharmacokinetics of<br />
propofol in the elderly patient. <strong>The</strong> central volume of<br />
distribution is less, systemic clearance is reduced, and<br />
intercompartmental clearance is reduced. During a propofol<br />
infusion, the plasma concentration of the drug is<br />
about 20% higher in the elderly patient as compared with<br />
the average adult. 31 Furthermore, the context-sensitive<br />
half-time changes with increasing age. Studies have shown<br />
that the time required for a 50% reduction in effect-site<br />
concentration (50% effect-site decrement time) is significantly<br />
prolonged with advancing age in an exponential<br />
manner. For propofol infusions less than 1 hour, there<br />
is little difference between the young adult patient and<br />
the elderly patient in recovery time. However, after a 4-<br />
hour infusion, there is a doubling of the 50% effect-site<br />
decrement time in an 80-year-old versus a 20-year-old<br />
patient, and this difference becomes even greater with<br />
infusions of 10 hours and longer. 31 This fact is of particular<br />
importance because this assumes that there have<br />
already been dosage adjustments for other pharmacokinetic<br />
parameters such that the plasma concentration is<br />
the same in both patients. Thus, even at reduced infusion<br />
rates, the elderly patient will take longer to emerge than<br />
the young patient.<br />
Indications<br />
Propofol, as noted above, is routinely used for induction<br />
and maintenance phases of general anesthesia, as well as<br />
for various levels of sedation in OR, and non-OR anesthesia,<br />
1 as well as in the intensive care unit.<br />
Dosing in the Elderly<br />
When the pharmacokinetic and pharmacodynamic<br />
changes are considered together, the current literature<br />
suggests a 20% reduction in the induction dose of propofol,<br />
if given as a bolus. Practically, this has been reported<br />
as a reduction of the bolus dose from 2.0–2.5 to 1.5–<br />
1.8 mg/kg. 32 Of note, it is the authors’ clinical experience<br />
that if the induction dose is titrated to a neurologic endpoint<br />
(such as BIS or PSA4000) or given slowly in order<br />
to account for the effect-site hysteresis time (k e0 ), this
232 M.D. McEvoy and J.G. Reves<br />
Figure 16-1. Propofol infusion rate<br />
required to maintain 1 µg/mL plasma<br />
level of propofol in patients of various<br />
ages. <strong>The</strong>se dosing guidelines take into<br />
account the pharmacokinetic changes<br />
with aging. This correlates with a mild<br />
level of sedation. (Reprinted with permission<br />
from Schüttler and Ihmsen. 29 )<br />
dose is reduced to as low as 0.8–1.2 mg/kg in the elderly,<br />
which corresponds with the findings of Kazama et al. 26<br />
Furthermore, numerous reports have shown that there is<br />
less hemodynamic instability if this bolus is given over a<br />
longer period of time in the elderly patient than as one<br />
fast bolus. 26,29,31<br />
Dosing requirements during an infusion are even less<br />
for the elderly patient. Schüttler and Ihmsen 29 have shown<br />
that for continuous low plasma level infusions, such as<br />
those used during the maintenance phase of an anesthetic<br />
for sedation (plasma concentration 1 µg/mL), a 75-yearold<br />
patient will require approximately 30% less drug than<br />
a 25-year-old patient to maintain the same level of drug<br />
concentration. However, this only takes into account the<br />
pharmacokinetic changes with age (Figure 16-1). 29 <strong>The</strong><br />
age-related decline in the amount of propofol required<br />
for the same level of anesthesia becomes even more profound<br />
when one considers the pharmacodynamic data<br />
along with the pharmacokinetic data. For a surgical level<br />
of anesthesia, Shafer proposes an age-adjusted dosing<br />
guideline based on the compilation of several pharmacokinetic<br />
and pharmacodynamic studies (Figure 16-2). 12,32<br />
This pharmacodynamic change is also illustrated in Figure<br />
16-3, which shows that a 75-year-old patient will require<br />
350<br />
1.0<br />
Unconscious<br />
Infusion Rate (mg/kg/min)<br />
300<br />
250<br />
200<br />
150<br />
25 years old<br />
50 years old<br />
75 years old<br />
Probability of Unconsciousness<br />
0.8<br />
0.6<br />
0.4<br />
0.2<br />
75<br />
50 25<br />
100<br />
0<br />
Conscious<br />
0 10 20 30 40 50 60<br />
Time (min)<br />
Figure 16-2. Propofol infusion rate required to maintain<br />
adequate surgical anesthesia in patients of various ages. <strong>The</strong>se<br />
dosing guidelines account for the changes with age in propofol<br />
pharmacokinetics and pharmacodynamics. (Reprinted with<br />
permission from Shafer. 32 )<br />
0 2 4 6 8<br />
Plasma Propofol Concentration (µg/mL)<br />
Figure 16-3. Effect of age on propofol pharmacodynamics. This<br />
logistic regression shows the age-related probability of being<br />
asleep after a 1-hour infusion of propofol. A 75-year-old patient<br />
is 30%–50% more sensitive to propofol than is a 25-year-old<br />
patient. (Reprinted with permission from Schnider et al. 12 )
16. Intravenous Hypnotic Anesthetics 233<br />
Figure 16-4. Context-sensitive half-time of propofol in patients of various ages. Altered pharmacokinetics in the elderly become<br />
clinically significant after a 1-hour infusion. (Reprinted with permission from Schüttler and Ihmsen. 29 )<br />
a 50% lower propofol plasma concentration than a 25-<br />
year-old patient in order to have the same likelihood of<br />
being asleep after a 1-hour infusion. 12 Additionally, as<br />
aforementioned, it must be noted that a prolonged propofol<br />
infusion should be stopped earlier in the elderly<br />
patient in order to have recovery at the same time as the<br />
younger patient (Figure 16-4). 29<br />
Adverse Effects and Contraindications<br />
<strong>The</strong> major adverse effect of propofol, a significant<br />
decrease in blood pressure, has been mentioned already.<br />
If proper dosage adjustments are made, propofol is a<br />
well-tolerated induction and infusion medication in the<br />
elderly. However, in the patient with significant ventricular<br />
dysfunction or hemodynamic instability, it may be best<br />
to use etomidate or thiopental for bolus induction. It is<br />
also of note that propofol routinely causes pain on intravenous<br />
injection. However, this is normally brief and well<br />
tolerated if it is injected into a briskly running intravenous<br />
line.<br />
Future Considerations<br />
<strong>The</strong> dosing adjustments mentioned above are well supported<br />
in the pharmacokinetic and pharmacodynamic<br />
literature. 12,29–32 Clinical application of some of the mathematical<br />
models that have been simulated has proven<br />
successful for the authors without the use of targetcontrolled<br />
infusion pumps. <strong>The</strong> authors have confirmed a<br />
less profound hemodynamic change when several models<br />
have been tested. In our experience, many geriatric<br />
patients can be induced (as measured by a BIS of less<br />
than 60) with 0.8–1.2 mg/kg propofol over a 180- to 240-<br />
second time frame with a less than 10% change from<br />
baseline heart rate and blood pressure. This is done<br />
through the application of several pharmacokinetic<br />
and pharmacodynamic models mentioned above. For<br />
instance, slightly modifying models proposed by Schüttler,<br />
Schnider, and Kazama, we induce many geriatric<br />
patients at an initial rate of 400 µg/kg/min propofol with<br />
1–2 µg/kg fentanyl given 2–3 minutes before the start of<br />
the infusion. When the BIS reaches 70 (usually within<br />
90–150 seconds), the neuromuscular blocker (NMBD) of<br />
choice (normally cisatracurium or rocuronium) is given<br />
while the propofol infusion is continued. When sufficient<br />
time has passed for the NMBD to have taken effect and<br />
the BIS is
234 M.D. McEvoy and J.G. Reves<br />
Of further consideration with the use of propofol in the<br />
geriatric patient is the possible benefit of its antiinflammatory<br />
and antioxidant properties. 33,34 New research is<br />
being conducted which may show that a propofol infusion<br />
for the maintenance of anesthesia decreases the<br />
magnitude of the rise of inflammatory markers in the<br />
elderly patient compared with volatile agents. This is of<br />
profound importance when it is viewed in light of the<br />
research showing that increases in inflammatory markers,<br />
such as interleukin-6, tumor necrosis factor-alpha, C-<br />
reactive protein, and myeloperoxidase, are associated<br />
with increased rates of cardiovascular mortality and<br />
morbidity. 35,36<br />
Thiopental<br />
Barbituric acid, a combination of urea and malonic acid<br />
that is lacking in sedative properties, was first synthesized<br />
in 1864 by J.F.W. Adolph von Baeyer, a Nobel prizewinning<br />
organic chemist. 37 <strong>The</strong> thiobarbiturates were first<br />
described in 1903. However, because of fatal experiments<br />
in dogs, their use was not further explored until the<br />
1930s. 38–40 In 1935, Tabern and Volwiler synthesized a<br />
series of sulfur-containing barbiturates, of which thiopental<br />
became the most widely used. Thiopental was introduced<br />
clinically by Ralph Waters and John Lundy, and<br />
became preferred clinically because of its rapid onset of<br />
action and short duration, without the excitatory effects<br />
of hexobarbital. 41<br />
Pharmacology: Structure/Action<br />
Thiopental is a hypnotically active drug that works at<br />
GABA A receptor sites in the CNS. 42 Thiopental is in the<br />
class of thiobarbiturates, which is defined by having a<br />
sulfur substituted at the position C2. Substitutions at the<br />
5, 2, and 1 positions of the barbiturate ring confer different<br />
pharmacologic activities to the barbiturate nucleus.<br />
Substitutions at position 5 with either aryl or alkyl groups<br />
produce hypnotic and sedative effects. A phenyl group<br />
substitution at C5 produces anticonvulsant activity. An<br />
increase in length of one or both side-chains of an alkyl<br />
group at C5 increases hypnotic potency. Substitution of a<br />
sulfur at position 2 produces a more rapid onset of action,<br />
as seen with thiopental. 43<br />
Pharmacodynamics<br />
Thiopental produces sedation and sleep. Sufficient doses<br />
produce a CNS depression that is attended by loss of<br />
consciousness, amnesia, and respiratory and cardiovascular<br />
depression. <strong>The</strong> response to pain and other noxious<br />
stimulation during general anesthesia seems to be<br />
obtunded. However, the results of pain studies reveal<br />
that barbiturates may actually decrease the pain threshold<br />
in low doses, such as with small induction doses of<br />
thiopental or after emergence from thiopental when the<br />
blood levels are low. 44 <strong>The</strong> amnesic effect of barbiturates<br />
has not been well studied, but it is decidedly less pronounced<br />
than that produced by benzodiazepines or<br />
propofol. 45<br />
Central Nervous System Effects<br />
Barbiturates, similar to other CNS depressants, have<br />
potent effects on cerebral metabolism. Several studies in<br />
the 1970s demonstrated the effect of barbiturates as a<br />
dose-related depression of the CMRO 2 , which produces<br />
a progressive slowing of the EEG, a reduction in the rate<br />
of adenosine triphosphate consumption, and protection<br />
from incomplete or focal cerebral ischemia. 46,47 When the<br />
results of the EEG became isoelectric, a point at which<br />
cerebral metabolic activity is approximately 50% of<br />
baseline, no further decrements in CMRO 2 occurred. 48<br />
<strong>The</strong>se findings support the hypothesis that metabolism<br />
and function are coupled. However, it must be noted that<br />
it is the portion of metabolic activity concerned with<br />
neuronal signaling and impulse traffic that is reduced by<br />
barbiturates, not that portion corresponding to basal<br />
metabolic function. <strong>The</strong> only way to suppress baseline<br />
metabolic activity concerned with cellular activity is<br />
through hypothermia. Thus, the effect of barbiturates on<br />
cerebral metabolism is maximized at a 50% depression<br />
of cerebral function in which less oxygen is required as<br />
CMRO 2 is diminished, leaving all metabolic energy to be<br />
used for the maintenance of cellular integrity. 48 This may<br />
be of importance to the elderly patient undergoing neurosurgery<br />
for aneurysm clipping or carotid endarterectomy<br />
in which focal ischemia may occur.<br />
With the reduction in CMRO 2 , there is a parallel reduction<br />
in cerebral perfusion, which is seen in decreased<br />
CBF and ICP (Table 16-1). With reduced CMRO 2 , cerebral<br />
vascular resistance increases and CBF decreases. 49<br />
However, for thiopental, the ratio of CBF to CMRO 2 is<br />
unchanged. Thus, the reduction in CBF after the administration<br />
of barbiturates causes a concurrent decrease in<br />
ICP. Furthermore, even though the MAP decreases, barbiturates<br />
do not compromise the overall CPP, because the<br />
CPP = MBP – ICP. In this relationship, ICP decreases<br />
more relative to the decrease in MAP after barbiturate<br />
use, thus preserving CPP. This is in contrast to propofol,<br />
which has a greater likelihood in the elderly patient of<br />
decreasing MAP to an extent that may compromise CPP,<br />
as noted above. 50<br />
Onset of Central Nervous System Effects<br />
Barbiturates produce CNS effects when they cross the<br />
blood–brain barrier. <strong>The</strong>re are several well-known factors
16. Intravenous Hypnotic Anesthetics 235<br />
that help to determine the rapidity with which a drug<br />
enters the cerebral spinal fluid (CSF) and brain tissue.<br />
<strong>The</strong>se factors include the degree of lipid solubility, degree<br />
of ionization, level of protein binding, and the plasma<br />
drug concentration. Drugs with high lipid solubility and<br />
low degree of ionization cross the blood–brain barrier<br />
rapidly, producing a fast onset of action. Approximately<br />
50% of thiopental is nonionized at physiologic pH, which<br />
accounts in part for the rapid accumulation of thiopental<br />
in the CSF after intravenous administration. Protein<br />
binding also affects the onset of action in the CNS.<br />
Barbiturates are highly bound to albumin and other<br />
plasma proteins. Because only unbound drug (free drug)<br />
can cross the blood–brain barrier, an inverse relationship<br />
exists between the degree of plasma protein binding<br />
and the rapidity of drug passage across the blood–brain<br />
barrier.<br />
<strong>The</strong> final factor governing the rapidity of drug penetration<br />
of the blood–brain barrier is the plasma drug concentration.<br />
Simply because of concentration gradient,<br />
higher levels of drug concentrations in the plasma produce<br />
greater amounts of drug that diffuses into the CSF and<br />
brain. <strong>The</strong> two primary determinants of the plasma concentration<br />
are the dose administered and the rate (speed)<br />
of administration. <strong>The</strong> higher the dose and the more rapid<br />
its administration, the more rapid is the effect. This is of<br />
particular importance in the elderly patient who may<br />
have a reduced central volume of distribution and thus<br />
require a reduced dose of thiopental in order to reach the<br />
same plasma concentration as a younger adult. 51<br />
Cardiovascular System<br />
Cardiovascular depression from barbiturates is a result<br />
of both central and peripheral (direct vascular and<br />
cardiac) effects. 52 <strong>The</strong> hemodynamic changes produced<br />
by barbiturates have been studied in healthy subjects and<br />
in patients with heart disease. <strong>The</strong> primary cardiovascular<br />
effect of barbiturate induction is peripheral vasodilation<br />
that results in a pooling of blood in the venous system. A<br />
decrease in contractility is another effect, which is related<br />
to reduced availability of calcium to the myofibrils. <strong>The</strong>re<br />
is also an increase in heart rate. Mechanisms for the<br />
decrease in cardiac output include (1) direct negative<br />
inotropic action, (2) decreased ventricular filling because<br />
of increased capacitance, and (3) transiently decreased<br />
sympathetic outflow from the CNS. <strong>The</strong> increase in heart<br />
rate (10%–36%) that accompanies thiopental administration<br />
probably results from the baroreceptor-mediated<br />
sympathetic reflex stimulation of the heart in response to<br />
the decrease in output and pressure. Thiopental produces<br />
dose-related negative inotropic effects, which seem to<br />
result from a decrease in calcium influx into the cells with<br />
a resultant diminished amount of calcium at sarcolemma<br />
sites. <strong>The</strong> cardiac index is unchanged or is reduced, and<br />
the MAP is maintained or is slightly reduced. 52 Thiopental<br />
infusions and lower doses tend to be accompanied by<br />
smaller hemodynamic changes than those noted with<br />
rapid bolus injections. 26<br />
<strong>The</strong> increase in heart rate encountered in patients with<br />
coronary artery disease anesthetized with thiopental<br />
(1–4 mg/kg) is potentially deleterious because of the<br />
obligatory increase in myocardial oxygen consumption<br />
(MVO 2 ) that accompanies the increased heart rate.<br />
Patients who have normal coronary arteries have no difficulty<br />
in maintaining adequate coronary blood flow to<br />
meet the increased MVO 2 . 53 When thiopental is given to<br />
hypovolemic patients, there is a significant reduction in<br />
cardiac output (69%) as well as a substantial decrease in<br />
blood pressure. 38–41 Patients without adequate compensatory<br />
mechanisms, therefore, may have serious hemodynamic<br />
depression with thiopental induction. All of these<br />
concerns are of particular importance in geriatric patients,<br />
because they are more likely to have clinically significant<br />
coronary artery disease, they are more likely to be intravascularly<br />
hypovolemic, and their compensatory mechanisms<br />
to maintain heart rate and blood pressure may be<br />
reduced because of age-related alterations and pharmacologic<br />
treatments such as beta-blockers or calcium<br />
channel blockers. Thus, it is of prime importance in the<br />
elderly patient to understand proper dose reduction (discussed<br />
below) and the effects of the rate of administration<br />
of an induction bolus. If these are not heeded, it<br />
becomes common to have significant hypotension in the<br />
geriatric patient with the need to administer vasopressors<br />
after induction, a practice that can be avoided if a proper<br />
understanding of the above principle is gained.<br />
Respiratory System<br />
Barbiturates produce dose-related central respiratory<br />
depression. <strong>The</strong>re is also a significant incidence of transient<br />
apnea after their administration for induction of<br />
anesthesia. 16 <strong>The</strong> evidence for central depression is a correlation<br />
between EEG suppression and minute ventilation.<br />
54 With increased anesthetic effect, there is diminished<br />
minute ventilation. <strong>The</strong> time course of respiratory depression<br />
has not been fully studied, but it seems that peak<br />
respiratory depression (as measured by the slope of CO 2<br />
concentration in the blood) and minute ventilation after<br />
delivery of thiopental 3.5 mg/kg occurs 1–1.5 minutes<br />
after administration. <strong>The</strong>se parameters return to predrug<br />
levels rapidly, and within 15 minutes the drug effects are<br />
barely detectable. 55 Of note, respirations are lost sooner<br />
and return later than that seen with propofol. Patients<br />
with chronic lung disease are slightly more susceptible<br />
to the respiratory depression of thiopental. <strong>The</strong> usual<br />
ventilatory pattern with thiopental induction has been<br />
described as “double apnea.” <strong>The</strong> initial apnea that occurs<br />
during drug administration lasts a few seconds and is
236 M.D. McEvoy and J.G. Reves<br />
succeeded by a few breaths of reasonably adequate tidal<br />
volume, which is followed by a longer apneic period.<br />
During the induction of anesthesia with thiopental, ventilation<br />
must be assisted or controlled to provide adequate<br />
respiratory exchange. This is of particular concern<br />
in the elderly patient who will have an increased closing<br />
capacity, which will produce a shorter time to becoming<br />
hypoxemic, as compared with the young adult patient. 22<br />
Metabolism and Disposition<br />
(Pharmacokinetics)<br />
Thiopental pharmacokinetics have been described in both<br />
physiologic and compartmental models. <strong>The</strong>se models<br />
basically describe a rapid mixing of the drug with the<br />
central blood volume followed by a quick distribution<br />
of the drug to the highly perfused, low-volume tissues<br />
(i.e., brain) with a slower redistribution of the drug to lean<br />
tissue (muscle). In these models, adipose tissue uptake<br />
and metabolic clearance (elimination) have only a minor<br />
role in the termination of the effects of the induction dose<br />
because of the minimal perfusion ratio compared with<br />
other tissues and the slow rate of removal, respectively.<br />
Both of these pharmacokinetic models describe rapid<br />
redistribution as the primary mechanism that terminates<br />
the action of a single induction dose. 32,56<br />
Awakening may be delayed in older patients mainly<br />
because of a decreased central volume of distribution<br />
relative to younger adults. 57 <strong>The</strong> initial volume of distribution<br />
is less in elderly patients when compared with that<br />
in young patients (80-year-old versus 35-year-old), which<br />
explains a 50%–75% lower dose requirement for the<br />
onset of EEG and hypnotic effects. 51,57 However, except<br />
in disease states, the clearance of thiopental is not reduced<br />
in the elderly, and thus, awakening should only be prolonged<br />
in the elderly with a bolus administration and not<br />
with a constant infusion.<br />
Indications<br />
Thiopental is an excellent hypnotic for use as an intravenous<br />
induction agent. 1 <strong>The</strong> prompt onset (15–30 seconds)<br />
of action and smooth induction noted with its use make<br />
thiopental superior to most other available drugs. <strong>The</strong><br />
relatively rapid emergence, particularly after single use<br />
for induction, has also been a reason for the widespread<br />
use of thiopental in this setting. Thiopental does not<br />
possess analgesic properties and therefore it must be<br />
supplemented with analgesic drugs in order to obtund<br />
reflex responses to noxious stimuli during anesthesia<br />
induction and surgical procedures. Thiopental can be<br />
used to maintain general anesthesia, because repeated<br />
doses reliably sustain unconsciousness and contribute<br />
to amnesia. However, the ease of use of propofol for<br />
light sedation and total intravenous anesthesia has supplanted<br />
the use of thiopental for this purpose and relegated<br />
it mainly for use in the induction portion of an<br />
anesthetic.<br />
Dosing in the Elderly<br />
Numerous studies have shown that the brain of the<br />
elderly patient is not intrinsically more sensitive to the<br />
effects of thiopental than that of the younger patient. 51<br />
Further studies concluded that the need for a reduction<br />
in the induction dose of thiopental in the elderly is<br />
attributable to a reduction in the central volume of distribution.<br />
58 Shafer 32 collated the results of several studies<br />
to suggest that the optimal dose in an 80-year-old patient<br />
is 2.1 mg/kg, which is approximately 80% of the dose<br />
needed for a young adult. However, it should again be<br />
noted that slower bolusing of the induction dose will<br />
generally result in less-acute hemodynamic alterations.<br />
Furthermore, monitoring of an EEG-related endpoint<br />
during a slow induction can guide the amount of drug<br />
given and may allow for a more individualized dosing<br />
regimen. 59<br />
Adverse Effects and Contraindications<br />
<strong>The</strong> effects of barbiturates on various organ systems have<br />
been studied extensively. <strong>The</strong>re are several side effects<br />
that occur in unpredictable, varying proportions of<br />
patients, whereas the cardiovascular and pulmonary are<br />
dose-related. 60 <strong>The</strong> complications of injecting barbiturates<br />
include a garlic or onion taste (40% of patients),<br />
allergic reactions, local tissue irritation, and rarely, tissue<br />
necrosis. An urticarial rash may develop on the head,<br />
neck, and trunk that lasts a few minutes. More severe<br />
reactions such as facial edema, hives, bronchospasm, and<br />
anaphylaxis can occur. Treatment of anaphylaxis is to<br />
stop any further administration of the drug, administer<br />
1-mL increments of 1 : 10,000 epinephrine with boluses of<br />
intravenous fluids, give inhaled bronchodilators, such as<br />
albuterol, for bronchospasm, and then administer histamine<br />
antagonists, such as Benadryl and Pepcid.<br />
Studies have shown pain on injection to be 9% and<br />
phlebitis to be approximately 1% with thiopental use. 61<br />
Tissue and venous irritation are more common if a 5%<br />
solution is used rather than the standard 2.5% solution.<br />
Rarely, intraarterial injection can occur. <strong>The</strong> consequences<br />
of accidental arterial injection may be severe. <strong>The</strong> degree<br />
of injury is related to the concentration of the drug.<br />
Treatment consists of (1) dilution of the drug by the<br />
administration of saline into the artery, (2) heparinization<br />
to prevent thrombosis, and (3) brachial plexus block.<br />
Overall, the proper administration of thiopental intravenously<br />
into a briskly running IV is remarkably free of<br />
local toxicity. 60 However, it should be noted that thiopental<br />
can precipitate if the alkalinity of the solution is
16. Intravenous Hypnotic Anesthetics 237<br />
decreased, which is why it cannot be reconstituted with<br />
lactated Ringer’s solution or mixed with other acidic<br />
solutions. Examples of drugs that are not to be coadministered<br />
or mixed in solution with the barbiturates are<br />
pancuronium, vecuronium, atracurium, alfentanil, sufentanil,<br />
and midazolam. Studies have shown that in rapidsequence<br />
induction, the mixing of thiopental with<br />
vecuronium or pancuronium results in the formation of<br />
precipitate that may occlude the intravenous line. 62<br />
Midazolam<br />
<strong>The</strong> first benzodiazepine found to have sedative-hypnotic<br />
effects was chlordiazepam (Librium) in 1955. 63 Diazepam<br />
(Valium) was synthesized in 1959 and became the first<br />
benzodiazepine used for sedation and anesthesia induction.<br />
Subsequently, a number of benzodiazepines have<br />
been produced including lorazepam and the antagonist<br />
flumazenil. <strong>The</strong> benzodiazepines produce many of the<br />
elements important in anesthesia. <strong>The</strong>y produce their<br />
actions by occupying the benzodiazepine receptor, which<br />
was first presented in 1971. 62 In 1977, specific benzodiazepine<br />
receptors were described when ligands were found<br />
to interact with a central receptor. 64 <strong>The</strong> most frequently<br />
used benzodiazepine in the elderly is midazolam. Fryer<br />
and Walser’s 1976 synthesis of midazolam (Versed) produced<br />
the first clinically used water-soluble benzodiazepine<br />
65 and it also was the first benzodiazepine that was<br />
produced primarily for use in anesthesia. 66<br />
Pharmacology: Structure/Action<br />
Midazolam is water soluble in its formulation, but highly<br />
lipid soluble at physiologic pH. 67 Midazolam solution<br />
contains 1 or 5 mg/mL midazolam with 0.8% sodium<br />
chloride and 0.01% disodium edetate, with 1% benzyl<br />
alcohol as a preservative. <strong>The</strong> pH is adjusted to 3 with<br />
hydrochloric acid and sodium hydroxide. <strong>The</strong> imidazole<br />
ring of midazolam accounts for its stability in solution<br />
and rapid metabolism. <strong>The</strong> high lipophilicity accounts for<br />
the rapid CNS effect, as well as for the relatively large<br />
volume of distribution. 68<br />
Pharmacodynamics<br />
Central Nervous System Effects<br />
All benzodiazepines have hypnotic, sedative, anxiolytic,<br />
amnesic, anticonvulsant, and centrally produced musclerelaxant<br />
properties. <strong>The</strong> drugs differ in their potency and<br />
efficacy with regard to each of these pharmacodynamic<br />
actions. <strong>The</strong> binding of benzodiazepines to their respective<br />
receptors is of high affinity, is stereospecific, and is<br />
able to fully saturate the receptors; the order of receptor<br />
affinity (thus potency) of the three agonists is lorazepam<br />
> midazolam > diazepam. Midazolam is approximately<br />
three to six times as potent as diazepam. 69<br />
<strong>The</strong> mechanism of action of benzodiazepines is reasonably<br />
well understood. 70–72 <strong>The</strong> interaction of ligands with<br />
the benzodiazepine receptor represents an example in<br />
which the complex systems of biochemistry, molecular<br />
pharmacology, genetic mutations, and clinical behavioral<br />
patterns are seen to interact. Through recent genetic<br />
studies, the GABA A subtypes have been found to mediate<br />
the different effects (amnesic, anticonvulsant, anxiolytic,<br />
and sleep). 73 Sedation, anterograde amnesia, and anticonvulsant<br />
properties are mediated via a1 receptors, 73 and<br />
anxiolysis and muscle relaxation are mediated by the a2<br />
GABA A receptor. 73 <strong>The</strong> degree of effect exerted at these<br />
receptors is a function of plasma level. By using plasma<br />
concentration data and pharmacokinetic simulations, it<br />
has been estimated that a benzodiazepine receptor occupancy<br />
of less than 20% may be sufficient to produce the<br />
anxiolytic effect, whereas sedation is observed with 30%–<br />
50% receptor occupancy and unconsciousness requires<br />
60% or higher occupation of benzodiazepine agonist<br />
receptors. 73<br />
Agonists and antagonists bind to a common (or at least<br />
overlapping) area of the benzodiazepine portion of the<br />
GABA A receptor by forming differing reversible bonds<br />
with it. 74 <strong>The</strong> effects of midazolam can be reversed by use<br />
of flumazenil, a benzodiazepine antagonist that occupies<br />
the benzodiazepine receptor, but produces no activity<br />
and therefore blocks the actions of midazolam. <strong>The</strong> duration<br />
of reversal is dependent on the dose of flumazenil<br />
and the residual concentration of midazolam.<br />
<strong>The</strong> onset and duration of action of a bolus intravenous<br />
administration of midazolam depends largely on the dose<br />
given and time at which the dose is administered; the<br />
higher the dose given over a shorter time (bolus), the<br />
faster the onset. Midazolam has a rapid onset (usually<br />
within 30–60 seconds) of action. <strong>The</strong> time to establish<br />
equilibrium between plasma concentration and EEG<br />
effect of midazolam is approximately 2–3 minutes and is<br />
not affected by age. 75 Like onset, the duration of effect is<br />
related to lipid solubility and blood level. 76 Thus, termination<br />
of effect is relatively rapid after midazolam administration.<br />
But some physicians have a general sense that<br />
midazolam is associated with the production of confusion<br />
even after the termination of sedation. This has been<br />
reported in prior studies and case reports. 77,78 However, a<br />
more recent study suggests that this might not be the case,<br />
particularly at lower doses. 79 Taken together, these data<br />
seem to suggest that single, lower doses of midazolam<br />
(0.03 mg/kg) will not cause confusion, whereas higher<br />
doses (0.05–0.07 mg/kg) plus an infusion of midazolam<br />
will have a greater association with confusion in the geriatric<br />
patient, as opposed to that seen with the use of a<br />
low-dose propofol infusion.
238 M.D. McEvoy and J.G. Reves<br />
Respiratory Effects<br />
Midazolam, like most intravenous anesthetics and other<br />
benzodiazepines, produces dose-related central respiratory<br />
system depression. <strong>The</strong> peak decrease in minute ventilation<br />
after midazolam administration (0.15 mg/kg) is<br />
almost identical to that produced in healthy patients<br />
given diazepam (0.3 mg/kg). 80 Respiratory depression is<br />
potentiated with opioids and must be carefully monitored<br />
in elderly patients getting both. <strong>The</strong> peak onset of ventilatory<br />
depression with midazolam (0.13–0.2 mg/kg) is rapid<br />
(about 3 minutes), and significant depression remains for<br />
about 60–120 minutes. 56,81 <strong>The</strong> depression is dose-related.<br />
<strong>The</strong> respiratory depression of midazolam is more pronounced<br />
and of longer duration in patients with chronic<br />
obstructive pulmonary disease, and the duration of ventilatory<br />
depression is longer with midazolam (0.19 mg/kg)<br />
than with thiopental (3.3 mg/kg). 56<br />
At sufficient doses, apnea occurs with midazolam as<br />
with other hypnotics. <strong>The</strong> incidence of apnea after thiopental<br />
or midazolam when these drugs are given for<br />
induction of anesthesia is similar. In clinical trials, apnea<br />
occurred in 20% of 1130 patients given midazolam for<br />
induction and 27% of 580 patients given thiopental. 67<br />
Apnea is related to dose and is more likely to occur in<br />
the presence of opioids. Old age, debilitating disease, and<br />
other respiratory depressant drugs probably also increase<br />
the incidence and degree of respiratory depression and<br />
apnea with midazolam.<br />
Cardiovascular Effects<br />
Midazolam alone has modest hemodynamic effects. <strong>The</strong><br />
predominant hemodynamic change is a slight reduction<br />
in arterial blood pressure, resulting from a decrease in<br />
systemic vascular resistance. <strong>The</strong> hypotensive effect is<br />
minimal and about the same as seen with thiopental. 82<br />
Despite the hypotension, midazolam, in doses as high as<br />
0.2 mg/kg, is safe and effective for induction of anesthesia<br />
even in patients with severe aortic stenosis. <strong>The</strong> hemodynamic<br />
effects of midazolam are dose-related: the higher<br />
the plasma level, the greater the decrease in systemic<br />
blood pressure 83 ; however, there is a plateau plasma drug<br />
effect above which little change in arterial blood pressure<br />
occurs. <strong>The</strong> plateau plasma level for midazolam is<br />
100 ng/mL. 83 Heart rate, ventricular filling pressures, and<br />
cardiac output are maintained after induction of anesthesia<br />
with midazolam.<br />
<strong>The</strong> stresses of endotracheal intubation and surgery<br />
are not blocked by midazolam. 84 Thus, adjuvant anesthetics,<br />
usually opioids, are often combined with benzodiazepines.<br />
<strong>The</strong> combination of benzodiazepines with opioids<br />
and nitrous oxide has been investigated in patients with<br />
ischemic and valvular heart diseases. 85–88 Whereas the<br />
addition of nitrous oxide to midazolam (0.2 mg/kg) has<br />
trivial hemodynamic consequences, the combination of<br />
benzodiazepines with opioids does have a synergistic<br />
effect. 89 <strong>The</strong> combination of midazolam with fentanyl 86 or<br />
sufentanil 88 produces greater decreases in systemic blood<br />
pressure than does each drug alone.<br />
Metabolism and Disposition<br />
(Pharmacokinetics)<br />
Biotransformation of all benzodiazepines occurs in the<br />
liver. <strong>The</strong> two principal pathways involve either hepatic<br />
microsomal oxidation (N-dealkylation or aliphatic<br />
hydroxylation) or glucuronide conjugation. 90,91 <strong>The</strong> difference<br />
in the two pathways is significant, because oxidation<br />
is susceptible to outside influences and can be<br />
impaired by certain population characteristics (specifically<br />
old age), disease states (e.g., hepatic cirrhosis), or<br />
the coadministration of other drugs that can impair oxidizing<br />
capacity (e.g., cimetidine). Of the two, conjugation<br />
is less susceptible to these factors. 90 Midazolam undergoes<br />
oxidation reduction, or phase I reactions, in the<br />
liver. 92 <strong>The</strong> cytochrome P450 3A4 is primarily responsible<br />
for metabolism. 93 <strong>The</strong> fused imidazole ring of midazolam<br />
is oxidized rapidly by the liver, which accounts for<br />
the high rate of hepatic clearance. Neither age nor<br />
smoking decreases midazolam biotransformation. 94<br />
Chronic alcohol consumption increases the clearance of<br />
midazolam. 95<br />
<strong>The</strong> metabolites of the benzodiazepines can be important.<br />
Midazolam is biotransformed to hydroxymidazolams,<br />
which have activity, and when midazolam is given in<br />
prolonged infusions these metabolites can accumulate. 96<br />
<strong>The</strong>se metabolites are rapidly conjugated and excreted in<br />
the urine. <strong>The</strong> 1-hydroxymidazolam has an estimated<br />
clinical potency 20%–30% of midazolam. 97 It is primarily<br />
excreted by the kidneys and can cause profound sedation<br />
in patients with renal impairment. 98 Overall, the metabolites<br />
of midazolam are less potent and normally more<br />
rapidly cleared than the parent drug, making them of<br />
little concern in patients with normal hepatic and renal<br />
function. However, they may be a consideration in elderly<br />
patients with impaired renal function.<br />
Midazolam is classified as a short-lasting benzodiazepine.<br />
<strong>The</strong> plasma disappearance curves of midazolam can<br />
be fitted to a two- or three-compartment model. <strong>The</strong><br />
clearance rate of midazolam ranges from 6 to 11 mL/kg/<br />
min. 94 Although the termination of action of these drugs<br />
is primarily a result of redistribution of the drug from<br />
the CNS to other tissues after bolus or maintenance use<br />
for surgical anesthesia, after daily (long-term) repeated<br />
administration or after prolonged continuous infusion,<br />
midazolam blood levels will decrease more slowly.<br />
Factors known to influence the pharmacokinetics of<br />
benzodiazepines are age, gender, race, enzyme induction,<br />
and hepatic and renal disease. Age reduces the clearance
16. Intravenous Hypnotic Anesthetics 239<br />
of midazolam to a modest degree. 99 Among the pharmacokinetic<br />
parameters of midazolam that vary significantly<br />
with age, it is clearance which does so most consistently. 100<br />
In healthy adults, midazolam clearance is high, approximating<br />
50% of hepatic blood flow. 101 However, with<br />
advanced age, there is a loss of functional hepatic tissue<br />
and a decrease in hepatic perfusion such that clearance<br />
is reduced in the elderly by as much as 30% from that of<br />
a young adult. 39 As a result of the normal decline in lean<br />
tissue mass and concomitant increase in percent body fat<br />
in the aged, a slight increase is also observed in volume<br />
of distribution. 102 Moreover, according to one study,<br />
advanced age is in itself enough to cause the mean elimination<br />
half-life of midazolam to double. 38 Neither oral<br />
bioavailability nor midazolam protein binding are affected<br />
by age, despite reduced hepatic albumin synthesis and<br />
lower serum albumin concentrations in the elderly. 39,100<br />
Midazolam pharmacokinetics are affected by obesity.<br />
<strong>The</strong> volume of distribution is increased as drug goes from<br />
the plasma into the adipose tissue. Although clearance is<br />
not altered, elimination half-lives are prolonged, because<br />
of the delayed return of the drug to the plasma in obese<br />
persons. 99 This can be of concern in elderly obese patients.<br />
Although the pharmacokinetics of midazolam are clearly<br />
affected by age, they are, with the exception of total clearance,<br />
not consistently altered to statistical significance. 39,98<br />
<strong>The</strong>se pharmacokinetic changes with age do not explain<br />
the increased sensitivity of the elderly to midazolam discussed<br />
above. <strong>The</strong>re are pharmacodynamic factors that<br />
are yet to be fully understood that make midazolam more<br />
potent in the elderly than the young.<br />
Indications<br />
Intravenous Sedation<br />
Midazolam is used for sedation as preoperative premedication,<br />
intraoperatively during regional or local anesthesia,<br />
and postoperatively for sedation. <strong>The</strong> anxiolysis,<br />
amnesia, and elevation of the local anesthetic seizure<br />
threshold are desirable benzodiazepine actions for re -<br />
gional anesthesia. It should be given by titration for this<br />
use; endpoints of titration are adequate sedation or dysarthria<br />
and maintained ventilation. <strong>The</strong> onset of action is<br />
relatively rapid with midazolam, usually with peak effect<br />
reached within 2–3 minutes of administration. <strong>The</strong> duration<br />
of action depends primarily on the dose used. <strong>The</strong>re<br />
is often a disparity in the level of sedation compared with<br />
the presence of amnesia (patients can be seemingly conscious<br />
and coherent, yet they are amnesic for events and<br />
instructions). <strong>The</strong> degree of sedation and the reliable<br />
amnesia, as well as preservation of respiratory and hemodynamic<br />
function, are better overall with midazolam than<br />
with other sedative-hypnotic drugs used for conscious<br />
sedation. When midazolam is compared with propofol for<br />
sedation, the two are generally similar except that emergence<br />
or wake-up is more rapid with propofol and amnesia<br />
is more reliable with midazolam. Propofol requires closer<br />
medical supervision because of its respiratory depression<br />
and hypotension. 103,104 Despite the wide safety margin<br />
with midazolam, respiratory function must be monitored<br />
when it is used for sedation to prevent undesirable<br />
degrees of respiratory depression. This is especially true<br />
in the geriatric patient. <strong>The</strong>re may be a slight synergistic<br />
action between midazolam and spinal anesthesia with<br />
respect to ventilation. 103 Thus, the use of midazolam<br />
for sedation during regional and epidural anesthesia<br />
requires vigilance with regard to respiratory function, as<br />
when these drugs are given with opioids. Sedation for<br />
longer periods, for example, in the intensive care unit, is<br />
accomplished with benzodiazepines. Prolonged infusion<br />
will result in accumulation of drug and, in the case of<br />
midazolam, significant concentration of the active metabolite.<br />
<strong>The</strong> chief advantages are the amnesia and hemodynamic<br />
stability and the disadvantage, compared with<br />
propofol, is the longer dissipation of effects when infusion<br />
is terminated.<br />
Induction and Maintenance of <strong>Anesthesia</strong><br />
With midazolam, induction of anesthesia is defined as<br />
unresponsiveness to command and loss of the eyelash<br />
reflex. When midazolam is used in appropriate doses,<br />
induction occurs less rapidly than with thiopental or<br />
propofol, 67 but the amnesia is more reliable. Numerous<br />
factors influence the rapidity of action of midazolam.<br />
<strong>The</strong>se factors are dose, speed of injection, degree of<br />
premedication, age, American Society of Anesthesiologists<br />
(ASA) physical status, and concurrent anesthetic<br />
drugs. 67,105 In a well-premedicated, healthy patient, midazolam<br />
(0.2 mg/kg given in 5–15 seconds) will induce anesthesia<br />
in 28 seconds. Emergence time is related to the dose<br />
of midazolam as well as to the dose of adjuvant anesthetic<br />
drugs. 67 Emergence is more prolonged with midazolam<br />
than with propofol. 106,107 This difference accounts for some<br />
anesthesiologists’ preference for propofol induction for<br />
short operations. <strong>The</strong> best method of monitoring depth<br />
with midazolam is use of the EEG-BIS. 108<br />
<strong>The</strong> amnesic period after an anesthetic dose is about<br />
1–2 hours. Infusions of midazolam have been used to<br />
ensure a constant and appropriate depth of anesthesia. 109<br />
Experience indicates that a plasma level of more than<br />
50 ng/mL when used with adjuvant opioids (e.g., fentanyl)<br />
and/or inhalation anesthetics (e.g., nitrous oxide, volatile<br />
anesthetics) is achieved with a bolus loading dose of<br />
0.05–0.15 mg/kg and a continuous infusion of 0.25-1 µg/<br />
kg/min. 110 This is sufficient to keep the patient asleep and<br />
amnesic but arousable at the end of surgery. Lower infusion<br />
doses almost certainly are required in elderly patients<br />
and with certain opioids.
240 M.D. McEvoy and J.G. Reves<br />
Percent of Patients Demonstrating<br />
No Response Verbal Command<br />
100<br />
90<br />
80<br />
70<br />
60<br />
50<br />
40<br />
30<br />
20<br />
10<br />
0<br />
Age<br />
80<br />
70<br />
60<br />
50<br />
40<br />
0 200 400 600 800 1000 1200<br />
Steady-State Plasma Midazolam Concentration (ng/ml)<br />
Figure 16-5. Response curves to verbal commands in patients<br />
of various ages at varying plasma levels of midazolam. This<br />
demonstrates a pharmacodynamic change associated with aging<br />
in response to midazolam. (Reprinted with permission from<br />
Jacobs et al. 112 )<br />
Effects of Age on Pharmacology<br />
Elderly patients require lower doses of midazolam than<br />
younger patients to reach various standard clinical endpoints<br />
of sedation, such as response to verbal command<br />
(Figure 16-5). 111,112 <strong>The</strong> usual induction dose of midazolam<br />
in elderly premedicated patients is between 0.05 and<br />
0.15 mg/kg. Some studies show that patients older than<br />
55 years and those with ASA physical status higher than<br />
3 require a 20% or more reduction in the induction dose<br />
of midazolam. 67 However, Shafer, who collated the results<br />
of numerous pharmacokinetic and pharmacodynamic<br />
studies, recommends a 75% reduction in dose from the<br />
20-year-old to the 90-year-old. Thus, there is definitely a<br />
graded decrease in the amount of drug needed as a result<br />
of aging. 32 Furthermore, when midazolam is used with<br />
other anesthetic drugs (coinduction), there is a synergistic<br />
interaction, 110,113,114 and the induction dose is less than<br />
0.1 mg/kg. <strong>The</strong> synergy is seen when midazolam is used<br />
with opioids and/or other hypnotics such as thiopental,<br />
propofol, and etomidate.<br />
Awakening after midazolam anesthesia is the result of<br />
the redistribution of drug from the brain to other, less<br />
well-perfused tissues. <strong>The</strong> emergence (defined as orientation<br />
to time and place) of young, healthy volunteers<br />
who received 10 mg of intravenous midazolam occurred<br />
in about 15 minutes, 113 and, after an induction dose of<br />
0.15 mg/kg, it occurred in about 17 minutes. 78 <strong>The</strong> effect<br />
of age on emergence has not been studied, but it likely is<br />
prolonged compared with younger patients because of<br />
greater potency in the elderly.<br />
Adverse Effects and Contraindications<br />
Midazolam is a remarkably safe drug. It has a relatively<br />
high margin of safety, especially compared with barbiturates<br />
and propofol. It is also free of allergenic effects and<br />
does not suppress the adrenal gland. 114 <strong>The</strong> most significant<br />
problem with midazolam is respiratory depression.<br />
It is free of venous irritation and thrombophlebitis,<br />
problems related to aqueous insolubility and requisite<br />
solvents in other drug formulations. 67 When used as a<br />
sedative or for induction and maintenance of anesthesia,<br />
midazolam can produce an undesirable degree or prolonged<br />
interval of postoperative amnesia, sedation, and,<br />
rarely, respiratory depression. <strong>The</strong>se residual effects can<br />
be reversed with flumazenil.<br />
Etomidate<br />
Pharmacology: Structure/Action<br />
Etomidate is a hypnotic drug that is structurally unrelated<br />
to all other induction medications. It contains a<br />
carboxylated imidazole ring that provides water solubility<br />
in an acidic milieu and lipid solubility at physiologic<br />
pH. It is dissolved in propylene glycol, which often causes<br />
pain on injection. Etomidate works by depressing the<br />
reticular activating system and it enhances the inhibitory<br />
effects of GABA by binding to a subunit of the GABA A<br />
receptor and thereby increasing its affinity for GABA.<br />
However, unlike the barbiturates, which have global<br />
depressant effects on the reticular activating system,<br />
etomidate has some disinhibitory effects, which accounts<br />
for the 30%–60% rate of myoclonus with administration.<br />
Interestingly, one study has shown that this unwanted<br />
side effect can be reduced with pretreatment, similar to<br />
a defasciculating dose of NMBDs. 115<br />
Pharmacodynamics<br />
Central Nervous System Effects<br />
Etomidate induces changes in CBF, metabolic rate, and<br />
ICP to the same extent as thiopental and propofol.<br />
However, because this is not the result of a large reduction<br />
in arterial blood pressure, CPP is well maintained. 115<br />
This is of particular importance in the elderly person who<br />
is at risk for ischemic stroke secondary to carotid occlusion.<br />
Etomidate has EEG changes similar to thiopental<br />
with a biphasic pattern of activation followed by depression.<br />
However, etomidate has been shown to activate<br />
somatosensory evoked potentials. 50 Of note, etomidate<br />
does have a higher rate of postoperative nausea and vomiting<br />
associated with it than with the other intravenous<br />
induction drugs. 116 Finally, there are no pharmacodynamic<br />
changes with age with respect to etomidate as measured<br />
by EEG. 115<br />
Cardiovascular Effects<br />
Unlike propofol, etomidate has minimal effects on the<br />
cardiovascular system. <strong>The</strong>re is a slight decline in the
16. Intravenous Hypnotic Anesthetics 241<br />
arterial blood pressure secondary to a mild reduction<br />
in the systemic vascular resistance. Etomidate does not<br />
seem to have direct myocardial depressant effects,<br />
because myocardial contractility, heart rate, and cardiac<br />
output are usually unchanged. 117 Etomidate does not<br />
cause histamine release. <strong>The</strong>se aspects of the pharmacodynamics<br />
of etomidate make it very useful in the patient<br />
with compromised intravascular volume, coronary artery<br />
disease, or reduced ventricular function, as is often<br />
encountered in the elderly patient.<br />
Respiratory Effects<br />
Etomidate causes less respiratory depression than benzodiazepines,<br />
barbiturates, or propofol in induction doses.<br />
In fact, even an induction dose of etomidate often does<br />
not cause apnea. 118 This fact, combined with its minimal<br />
cardiovascular effects, makes etomidate a very useful<br />
drug in the setting of a hemodynamically brittle elderly<br />
patient with a possible difficult airway and little respiratory<br />
reserve.<br />
Endocrine Effects<br />
Induction doses of etomidate temporarily inhibit the synthesis<br />
of cortisol and aldosterone. 119 However, with a<br />
single bolus dose there is little clinical significance. Alternatively,<br />
long-term infusions or closely repeated exposures<br />
can lead to adrenocortical suppression, which may<br />
be associated with an increased susceptibility to infection<br />
and an increased mortality rate in the critically ill<br />
patient. 120<br />
Metabolism and Disposition<br />
(Pharmacokinetics)<br />
Etomidate is used only in intravenous formulations and<br />
is generally used for the induction of general anesthesia.<br />
Etomidate is similar to thiopental in its distribution and<br />
onset of action. Although it is highly protein bound,<br />
etomidate has a very rapid onset of action because of its<br />
high lipid solubility and its large nonionized fraction.<br />
Redistribution to noncentral compartments is responsible<br />
for its rapid offset of action. Hepatic microsomal<br />
enzymes as well as plasma esterases rapidly hydrolyze<br />
etomidate to its nonactive metabolites. This rate of biotransformation<br />
is five times greater than that of thiopental,<br />
but less than that of propofol.<br />
<strong>The</strong> volume of distribution is slightly larger than that<br />
of the barbiturates and the elimination clearance is<br />
greater. However, the elimination clearance is still less<br />
than propofol. Thus, the elimination half-life of etomidate<br />
is faster than thiopental, but longer than propofol. Both<br />
of these parameters are decreased in the elderly, which<br />
causes a higher plasma concentration of etomidate for<br />
any given dose. Furthermore, to our knowledge, no study<br />
has ever shown an increased brain sensitivity to etomidate<br />
with increasing age. <strong>The</strong>refore, like thiopental, any<br />
dose reduction in the elderly is attributable to pharmacokinetic,<br />
not pharmacodynamic, changes. 121<br />
Indications<br />
Etomidate is used for the intravenous induction of anesthesia.<br />
1 It can be used with an intermittent bolus technique<br />
for short procedures. Typically, 25% of the induction<br />
dose is given every 15–30 minutes to maintain surgical<br />
anesthesia. Etomidate is not approved in the United<br />
States for maintenance infusions.<br />
Dosing in the Elderly<br />
<strong>The</strong> standard induction dose of etomidate is intravenous<br />
0.3–0.4 mg/kg. However, the elderly may only require<br />
0.2 mg/kg. This change in dosage is attributable only to<br />
pharmacokinetic parameters, not pharmacodynamic. 121<br />
Adverse Effects and Contraindications<br />
Etomidate has a high incidence of side effects, most of<br />
which are minor. As mentioned above, etomidate has a<br />
higher rate of postoperative nausea and vomiting than<br />
either propofol or thiopental. <strong>The</strong> incidence of myoclonic<br />
movements on induction is reported to be as high as<br />
60%. This effect as well as pain on injection can be<br />
reduced with a slow injection into a rapidly running intravenous<br />
carrier line, preferably in a large vein. When<br />
etomidate is injected into veins in the hand, the incidence<br />
of pain is reported to exceed 40%. Furthermore, because<br />
of the propylene glycol solvent, studies have shown that<br />
10%–20% of patients experience venous sequelae after<br />
its use. 122<br />
Summary<br />
This chapter has surveyed the pharmacology of frequently<br />
used intravenous hypnotic agents in the geriatric patient.<br />
<strong>The</strong>re is substantial evidence of significant changes in<br />
the pharmacokinetic and pharmacodynamic behavior of<br />
propofol, thiopental, midazolam, and etomidate in this<br />
population. A few final points remain when considering<br />
the general changes for each of these hypnotic agents.<br />
First, practitioners should perform a thorough review of<br />
the cardiopulmonary status of all geriatric patients,<br />
because an absence of complaints in a review of systems<br />
may merely be a function of a sedentary lifestyle. A more<br />
extensive history may elicit findings that would alter the<br />
method of induction or the combination/doses of drugs<br />
used for anesthesia. Second, a full review of the current<br />
medical management of systemic disease should be
242 M.D. McEvoy and J.G. Reves<br />
performed, because the elderly population often presents<br />
for surgery with outpatient polypharmacy. Particular<br />
attention should be given to current use of antihypertensive,<br />
diuretic, antidepressant, anti-Parkinsonian, and erectile<br />
dysfunction agents, with vigilance given to careful<br />
blood pressure monitoring when using the induction<br />
agents reviewed in this chapter in patients who are taking<br />
one or several of these medications. Third, a thorough<br />
understanding of the changes in the pharmacokinetics<br />
and pharmacodynamics of opioids in the geriatric patient<br />
is critical when combining them for sedation or general<br />
anesthesia in this population. Finally, unless a rapid<br />
sequence induction is indicated, a slow and careful titration<br />
of the induction of anesthesia using smaller doses of<br />
hypnotic agents and some form of an EEG monitor will<br />
prevent overdosing, subsequent hypotension, and delayed<br />
awakening in this population.<br />
References<br />
1. Martin G, Glass PS, Breslin DS, et al. A study of anesthetic<br />
drug utilization in different age groups. J Clin Anesth 2003;<br />
15(3):194–200.<br />
2. Trifune M, Takarada T, Shimizu Y, et al. Propofol-induced<br />
anesthesia in mice is mediated by gamma-aminobutyric<br />
acid-A and excitatory amino acid receptors. Anesth Analg<br />
2003;97(2):424–429.<br />
3. Dong XP, Xu TL. <strong>The</strong> actions of propofol on gammaaminobutyric<br />
acid-A and glycine receptors in acutely dissociated<br />
spinal dorsal horn neurons of the rat. Anesth<br />
Analg 2002;95(4):907–914.<br />
4. Glen JB, Hunter SC. Pharmacology of an emulsion formulation<br />
of ICI 35 868. Br J Anaesth 1984;56:617–626.<br />
5. Carr S, Waterman S, Rutherford G, et al. Postsurgical infections<br />
associated with an extrinsically contaminated intravenous<br />
anesthetic agent: California, Illinois, Maine, and<br />
Michigan, 1990. MMWR Morb Mortal Wkly Rep 1990;39:<br />
426–427.<br />
6. Bennett SN, McNeil MM, Bland LA, et al. Postoperative<br />
infections traced to contamination of an intravenous anesthetic,<br />
propofol. N Engl J Med 1995;333:147–154.<br />
7. Ludbrook GL, Visco E, Lam AM. Propofol: relation<br />
between brain concentrations, electro-encephalogram,<br />
middle cerebral artery blood flow velocity, and cerebral<br />
oxygen extraction during induction of anesthesia. <strong>Anesthesiology</strong><br />
2002;97(6):1363–1370.<br />
8. van der Starre PJA, Guta C. Choice of anesthetics. Anesthesiol<br />
Clin North Am 2004;22(2):251–264.<br />
9. Kuizenga K, Wierda JM, Kalkman CJ . Biphasic EEG<br />
changes in relation to loss of consciousness during induction<br />
with thiopental, propofol, etomidate, midazolam or<br />
sevoflurane. Br J Anaesth 2001;86(3):354–360.<br />
10. Schultz A, Grouven U, Zander I, Beger FA, Siedenberg M,<br />
Schultz B. Age-related effects in the EEG during propofol<br />
anaesthesia. Acta Anaesthesiol Scand 2004;48(1):27–34.<br />
11. Ding Z, White PF. <strong>Anesthesia</strong> for electroconvulsive therapy.<br />
Anesth Analg 2002;94(5):1351–1364.<br />
12. Schnider TW, Minto CF, Shafer SL, et al. <strong>The</strong> influence of<br />
age on propofol pharmacodynamics. <strong>Anesthesiology</strong><br />
1999;90(6):1502–1516.<br />
13. Brown RH, Greenberg RS, Wagner EM. Efficacy of propofol<br />
to prevent bronchoconstriction: effects of preservative<br />
. <strong>Anesthesiology</strong> 2001;94:851–855; discussion 6A.<br />
14. Conti G, Dell’Utri D, Vilardi V, et al. Propofol induces<br />
bronchodilation in mechanically ventilated chronic<br />
obstructive pulmonary disease (COPD) patients . Acta<br />
Anaesthesiol Scand 1993;37:105–109.<br />
15. Streisand JB, Nelson P, Bubbers S, et al. <strong>The</strong> respiratory<br />
effects of propofol with and without fentanyl. Anest Analg<br />
1987;66:S171.<br />
16. Bluoin RT, Conrad PF, Gross JB. Time course of ventilatory<br />
depression following induction doses of propofol and<br />
thiopental. <strong>Anesthesiology</strong> 1991;75:940–944.<br />
17. Tagaito Y, Isono S, Nishino T. Upper airway reflexes during<br />
a combination of propofol and fentanyl anesthesia. <strong>Anesthesiology</strong><br />
1998;88(6):1459–1466.<br />
18. Van Keer L, Van Aken H, et al. Propofol does not inhibit<br />
hypoxic pulmonary vasoconstriction in humans. J Clin<br />
Anesth 1989;1:284–288.<br />
19. Abe K, Shimizu T, Takashina M, Shiozaki H, Yoshiya I,<br />
et al. <strong>The</strong> effects of propofol, isoflurane, and sevoflurane<br />
on oxygenation and shunt fraction during one-lung ventilation.<br />
Anesth Analg 1998;87(5):1164–1169.<br />
20. Blouin RT, Seifert HA, Babenco HD, Conard PF, Gross<br />
JB. Propofol depresses the hypoxic ventilatory response<br />
during conscious sedation and isohypercapnia. <strong>Anesthesiology</strong><br />
1993;79:1177–1182.<br />
21. Chan ED, Welsh CH. <strong>Geriatric</strong> respiratory medicine. Chest<br />
1998;114(6):1704–1733.<br />
22. Zaugg M, Lucchinetti E. Respiratory function in the<br />
elderly. Anesthesiol Clin North Am 2000;18(1):47–58, vi.<br />
23. Kirkbride DA, Parker JL, Williams GD, Buggy DJ. Induction<br />
of anesthesia in the elderly ambulatory patient: a<br />
double-blinded comparison of propofol and sevoflurane.<br />
Anesth Analg 2001;93(5):1185–1187.<br />
24. John AD, Sieber FE. Age associated issues: geriatrics.<br />
Anesthesiol Clin North Am 2004;22(1):45–58.<br />
25. Rooke GA. Autonomic and cardiovascular function in the<br />
geriatric patient. Anesthesiol Clin North Am 2000;18(1):<br />
31–46, v–vi.<br />
26. Kazama T, Ikeda K, Morita K, et al. Comparison of the<br />
effect-site k(eO)s of propofol for blood pressure and EEG<br />
bispectral index in elderly and younger patients. <strong>Anesthesiology</strong><br />
1999;90(6):1517–1527.<br />
27. Tramèr M, Moore A, McQuay H. Propofol anaesthesia and<br />
postoperative nausea and vomiting: quantitative systematic<br />
review of randomized controlled studies. Br J Anaesth<br />
1997;78(3):247–255.<br />
28. Borgeat A, Wilder-Smith OH, Saiah M, Rifat K. Subhypnotic<br />
doses of propofol relieve pruritus induced by<br />
epidural and intrathecal morphine. <strong>Anesthesiology</strong><br />
1992;76(4):510–512.<br />
29. Schüttler J, Ihmsen H. Population pharmacokinetics of<br />
propofol: a multicenter study. <strong>Anesthesiology</strong> 2000;92:<br />
727–738.<br />
30. Shafer A, Doze VA, Shafer SL, White PF. Pharmacokinetics<br />
and pharmacodynamics of propofol infusions
16. Intravenous Hypnotic Anesthetics 243<br />
during general anesthesia. <strong>Anesthesiology</strong> 1988;69:<br />
348–356.<br />
31. Schnider TW, Minto CF, Gumbus PL, et al. <strong>The</strong> influence<br />
of method of administration and covariates on the pharmacokinetics<br />
of propofol in adult volunteers. <strong>Anesthesiology</strong><br />
1998;88(5):1170–1182.<br />
32. Shafer SL. <strong>The</strong> pharmacology of anesthetic drugs in elderly<br />
patients. Anesthesiol Clin North Am 2000;18(1):1–29, v.<br />
33. Takaono M, Yogosawa T, Okawa-Takatsuji M, Aotsuka S.<br />
Effects of intravenous anesthetics on interleukin (IL)-6<br />
and IL-10 production by lipopolysaccharide-stimulated<br />
mononuclear cells from healthy volunteers. Acta Anaesthesiol<br />
Scand 2002;46(2):176–179.<br />
34. Alvarez-Ayuso L, Calero P, Granado F, et al. Antioxidant<br />
effect of gamma-tocopherol supplied by propofol preparations<br />
(Diprivan) during ischemia-reperfusion in experimental<br />
lung transplantation. Transpl Int 2004;17(2):71–77.<br />
35. Lombardo A. Inflammation as a possible link between<br />
coronary and carotid plaque instability. Circulation 2004;<br />
109(25):3158–3163.<br />
36. Willerson JT. Inflammation as a cardiovascular risk factor.<br />
Circulation 2004;109(21 Suppl 1):II2–10.<br />
37. Dundee JW, Hassard TH, McGowan WAW, et al. <strong>The</strong><br />
“induction” dose of thiopentone: a method of study and<br />
preliminary illustrative results. Anaesthesia 1982;37:1176.<br />
38. Ball C, Westhorpe R. <strong>The</strong> history of intravenous anaesthesia:<br />
the barbiturates. Part 1. Anaesth Intensive Care 2001;<br />
29(2):97.<br />
39. Ball C, Westhorpe R. <strong>The</strong> history of intravenous anaesthesia:<br />
the barbiturates. Part 2. Anaesth Intensive Care 2001;<br />
29(3):219.<br />
40. Ball C, Westhorpe R. <strong>The</strong> history of intravenous anaesthesia:<br />
the barbiturates. Part 3. Anaesth Intensive Care 2001;<br />
29(4):323.<br />
41. Dundee JW. Fifty years of thiopentone. Br J Anaesth<br />
1984;56:211.<br />
42. Tanelian DL, Kosek P, Mody I, et al. <strong>The</strong> role of the<br />
GABAA receptor/chloride channel complex in anesthesia.<br />
<strong>Anesthesiology</strong> 1993;78:757.<br />
43. Dundee JW. Molecular structure-activity relationships of<br />
barbiturates. In: Halsey MJ, Millar RA, Sutton JA, eds.<br />
Molecular Mechanisms in General <strong>Anesthesia</strong>. New York:<br />
Churchill Livingstone; 1974:16.<br />
44. Archer DP, Ewen A, Froelich J, Roth SH, Samanani N.<br />
Thiopentone induced enhancement of somatic motor<br />
responses to noxious stimulation: influence of GABAA<br />
receptor modulation. Can J Anaesth 1996;43(5 Pt 1):503–<br />
510.<br />
45. Veselis RA, Reinsel RA, Feshchenko VA, Wroński M.<br />
<strong>The</strong> comparative amnestic effects of midazolam, propofol,<br />
thiopental, and fentanyl at equisedative concentrations.<br />
<strong>Anesthesiology</strong> 1997;87(4):749–764.<br />
46. Stulken EH Jr, Milde JH, Michenfelder JD, et al. <strong>The</strong><br />
nonlinear response of cerebral metabolism to low concentrations<br />
of halothane, enflurane, isoflurane and thiopental.<br />
<strong>Anesthesiology</strong> 1977;46:28.<br />
47. Smith AL. Barbiturate protection in cerebral hypoxia.<br />
<strong>Anesthesiology</strong> 1977;47:285.<br />
48. Baughman VL. Brain protection during neurosurgery.<br />
Anesthesiol Clin North Am 2002;20(2):315–327, vi.<br />
49. Albrecht RF, Miletich DJ, Rosenberg R, et al. Cerebral<br />
blood flow and metabolic changes from induction to onset<br />
of anesthesia with halothane or pentobarbital. <strong>Anesthesiology</strong><br />
1977;47:252.<br />
50. Cheng MA, <strong>The</strong>ard MA, Tempelhoff R. Intravenous agents<br />
and intraoperative neuroprotection. Beyond barbiturates.<br />
Crit Care Clin 1997;13(1):185–199.<br />
51. Stanski DR, Maitre PO. Population pharmacokinetics and<br />
pharmacodynamics of thiopental: the effect of age revisited.<br />
<strong>Anesthesiology</strong> 1990;72:412–422.<br />
52. Russo H, Bressolle E. Pharmacodynamics and pharmacokinetics<br />
of thiopental. Clin Pharmacokinet 1998;35:95–134.<br />
53. Sonntag H, Hellberg K, Schenk HD, et al. Effects of thiopental<br />
(Trapanal) on coronary blood flow and myocardial<br />
metabolism in man. Acta Anaesthesiol Scand 1975;19(1):<br />
69–78.<br />
54. Choi SD, Spaulding BC, Gross JB, Apfelbaum JL.<br />
Comparison of the ventilatory effects of etomidate and<br />
methohexital. <strong>Anesthesiology</strong> 1985;62(4):442–447.<br />
55. Hung OR, Varvel JR, Shafer SL, Stanski DR. Thiopental<br />
pharmacodynamics. II. Quantitation of clinical and electroencephalographic<br />
depth of anesthesia. <strong>Anesthesiology</strong><br />
1992;77(2):237–244.<br />
56. Gross JB, Zebrowski ME, Carel WD, Gardner S, Smith TC.<br />
Time course of ventilatory depression after thiopental<br />
and midazolam in normal subjects and in patients with<br />
chronic obstructive pulmonary disease. <strong>Anesthesiology</strong><br />
1983;58(6):540–544.<br />
57. Wada DR, Bjorkman S, Ebling WF, et al. Computer simulation<br />
of the effects of alterations in blood flows and body<br />
composition on thiopental pharmacokinetics in humans.<br />
<strong>Anesthesiology</strong> 1997;87:884.<br />
58. Homer TD, Stanski DR. <strong>The</strong> effect of increasing age on<br />
thiopental disposition and anesthetic requirement. <strong>Anesthesiology</strong><br />
1985;62:714–724.<br />
59. Avram MJ, Krejcie TC, Henthorn TK. <strong>The</strong> relationship of<br />
age to the pharmacokinetics of early drug distribution:<br />
the concurrent disposition of thiopental and indocyanine<br />
green. <strong>Anesthesiology</strong> 1990;72:403–411.<br />
60. Mortier E, Struys M, De Smet T, Versichelen L, Rolly G.<br />
Closed-loop controlled administration of propofol using<br />
bispectral analysis. Anaesthesia 1998;53(8):749–754.<br />
61. Dundee JW, Wyant GM. Intravenous Anaesthesia. 2nd ed.<br />
Edinburgh: Churchill Livingstone; 1988.<br />
62. Reves JG, Glass PSA, Lubarsky DA. Nonbarbiturate intravenous<br />
anesthetics. In: Miller RD, ed. <strong>Anesthesia</strong>. 5th ed.<br />
New York: Churchill Livingstone; 2000:228–272.<br />
63. Kawar P, Dundee JW. Frequency of pain on injection<br />
and venous sequelae following the I.V. administration<br />
of certain anaesthetics and sedatives. Br J Anaesth 1982;<br />
54(9):935–939.<br />
64. Haefely W, Hunkeler W. <strong>The</strong> story of flumazenil. Eur J<br />
Anaesthesiol 1988;2:3.<br />
65. Squires RF, Braestrup C. Benzodiazepine receptors in rat<br />
brain. Nature 1977;266:732.<br />
66. Walser A, Benjamin LES, Flynn T, et al. Quinazolines and<br />
1,4-benzodiazepines. 84. Synthesis and reactions of imidazo<br />
(1,5)(1,4)-benzodiazepines. J Org Chem 1978;43:936.<br />
67. Reves JG, Fragen RJ, Vinik HR, et al. Midazolam: pharmacology<br />
and uses. <strong>Anesthesiology</strong> 1985;62:310.
244 M.D. McEvoy and J.G. Reves<br />
68. Greenblatt DJ, Shader RI, Abernethy DR. Medical intelligence<br />
drug therapy: current status of benzodiazepines.<br />
N Engl J Med 1983;309:354.<br />
69. Arendt RM, Greenblatt DJ, DeJong RH, et al. In vitro<br />
correlates of benzodiazepine cerebrospinal fluid uptake,<br />
pharmacodynamic action and peripheral distribution.<br />
J Pharmacol Exp <strong>The</strong>r 1983;227:98.<br />
70. Mould DR, DeFeo TM, Reele S, et al. Simultaneous<br />
modeling of the pharmacokinetics and pharmacodynamics<br />
of midazolam and diazepam. Clin Pharmacol <strong>The</strong>r 1995;<br />
58:35.<br />
71. Mohler H, Richards JG. <strong>The</strong> benzodiazepine receptor: a<br />
pharmacological control element of brain function. Eur J<br />
Anaesthesiol 1988;2:15.<br />
72. Amrein R, Hetzel W. Pharmacology of Dormicum<br />
(midazolam) and Anexate (flumazenil). Acta Anaesthsiol<br />
Scand 1990;92:6.<br />
73. Mohler H, Fritschy JM, Rudolph U. A new benzodiazepine<br />
pharmacology. J Pharmacol Exp <strong>The</strong>r 2002;300:2.<br />
74. Amrein R, Hetzel W, Harmann D, et al. Clinical pharmacology<br />
of flumazenil. Eur J Anaesthesiol 1988;2:65.<br />
75. Haefely W. <strong>The</strong> preclinical pharmacology of flumazenil.<br />
Eur J Anaesthesiol 1988;2:25.<br />
76. Breimer LTM, Burm AGL, Danhof M, et al. Pharmacokinetic-pharmacodynamic<br />
modelling on the interaction<br />
between flumazenil and midazolam in volunteers by aperiodic<br />
EEG analysis. Clin Pharmacokinet 1991;20:497.<br />
77. White PF, Negus JB. Sedative infusions during local and<br />
regional anesthesia: a comparison of midazolam and propofol.<br />
J Clin Anesth 1991;3(1):32–39.<br />
78. Burnakis TG, Berman DE. Hostility and hallucinations as<br />
a consequence of midazolam administration. DICP 1989;<br />
23(9):671–672.<br />
79. Christe C, Janssens JP, Armenian B, Herrmann F, Vogt N.<br />
Midazolam sedation for upper gastrointestinal endoscopy<br />
in older persons: a randomized, double-blind, placebocontrolled<br />
study. J Am Geriatr Soc 2000;48(11):1398–<br />
1403.<br />
80. Forster A, Gardaz JP, Suter PM, et al. Respiratory depression<br />
by midazolam and diazepam. <strong>Anesthesiology</strong> 1980;<br />
53:494.<br />
81. Brodgen RN, Goa KL. Flumazenil. Drugs 1991;42:1061.<br />
82. Lebowitz PW, Core ME, Daniels AL, et al. Comparative<br />
cardiovascular effects of midazolam and thiopental in<br />
healthy patients. Anesth Analg 1982;61:771.<br />
83. Sunzel M, Paalzow L, Berggren L, et al. Respiratory<br />
and cardiovascular effects in relations to plasma levels of<br />
midazolam and diazepam. Br J Clin Pharmacol 1988;25:<br />
561.<br />
84. Samuelson PN, Reves JG, Kouchoukos NT, et al. Hemodynamic<br />
responses to anesthetic induction with midazolam<br />
or diazepam in patients with ischemic heart disease. Anesth<br />
Analg 1981;60:802.<br />
85. Ruff R, Reves JG. Hemodynamic effects of a lorazepamfentanyl<br />
anesthetic induction for coronary artery bypass<br />
surgery. J Cardiothorac Anesth 1990;4:314.<br />
86. Heikkila H, Jalonen J, Arola M, et al. Midazolam as adjunct<br />
to high-dose fentanyl anaesthesia for coronary artery<br />
bypass grafting operation. Acta Anaesthesiol Scand 1984;<br />
28:683.<br />
87. Benson KT, Tomlinson DL, Goto H, et al. Cardiovascular<br />
effects of lorazepam during sufentanil anesthesia. Anesth<br />
Analg 1988;67:966.<br />
88. Windsor JW, Sherry K, Feneck RO, et al. Sufentanil and<br />
nitrous oxide anaesthesia for cardiac surgery. Br J Anaesth<br />
1988;61:662.<br />
89. Reves JG, Croughwell N. Valium-fentanyl interaction. In:<br />
Reves JG, Hall K, eds. Common Problems in Cardiac<br />
Anaesthesia. Chicago: Year Book; 1987:356.<br />
90. Greenblatt DL, Shader RI. Benzodiazepines in Clinical<br />
Practice. New York: Raven Press; 1974.<br />
91. Elliott HW. Metabolism of lorazepam. Br J Anaesth 1976;<br />
48:1017.<br />
92. Blitt CD. Clinical pharmacology of lorazepam. In: Brown<br />
BRJ, ed. New Pharmacologic Vistas in <strong>Anesthesia</strong>. Philadelphia:<br />
FA Davis; 1983:135.<br />
93. Kronbach T, Mathys D, Umeno M, Gonzalez FJ, Meyer UA.<br />
Oxidation of midazolam and triazolam by human liver<br />
cytochrome P450IIIA4. Mol Pharmacol 1989;36:89–96.<br />
94. Reves JG. Benzodiazepines. In: Prys-Roberts C, Hugg CC,<br />
eds. Pharmacokinetics of <strong>Anesthesia</strong>. Boston: Blackwell<br />
Scientific Publications; 1984:157.<br />
95. Kassai A, Eichelbaum M, Klotz U. No evidence of a genetic<br />
polymorphism in the oxidative metabolism of midazolam.<br />
Clin Pharmacokinet 1988;15:319.<br />
96. Barr J, Donner A. Optimal intravenous dosing strategies<br />
for sedatives and analgesics in the intensive care unit. Crit<br />
Care Clin 1995;11:827.<br />
97. Mandema JW, Tuk B, van Steveninck AL, et al.<br />
Pharmacokinetic-pharmacodynamic modeling of the<br />
central nervous system effects of midazolam and its main<br />
metabolite α-hydroxymidazolam in healthy volunteers.<br />
Clin Pharmacol <strong>The</strong>r 1992;51:715.<br />
98. Bauer TM, Ritz R, Haberthur C, et al. Prolonged sedation<br />
due to accumulation of conjugated metabolites of<br />
midazolam. Lancet 1995;346:145.<br />
99. Greenblatt DJ, Abernethy DR, Loeniskar A, et al. Effect<br />
of age, gender, and obesity on midazolam kinetics. <strong>Anesthesiology</strong><br />
1984;61:27.<br />
100. Weese H, Scharpf W. Evipanein neuartiges Einschlafmittel.<br />
Dtsch Med Wochenschr 1932;58:1205.<br />
101. Tabern TW, Volwiler EH. Sulfur-containing barbiturate<br />
hypnotics. J Am Chem Soc 1935;57:1961.<br />
102. Halford FJ. A critique of intravenous anaesthesia in war<br />
surgery. Anaesthesiology 1943;4:67–69.<br />
103. Sanchez-Izquierdo-Riera JA, Caballero-Cubedo RE,<br />
Perez-Vela JL, Ambros-Checa A, Cantalapiedra-Santiago<br />
JA, Alted-Lopez E. Propofol versus midazolam: safety and<br />
efficacy for sedating the severe trauma patient. Anesth<br />
Analg 1998;86:1219.<br />
104. Vargo JJ, Zuccaro G Jr, Dumot JA, et al. Gastroenterologistadministered<br />
propofol versus meperidine and midazolam<br />
for advanced upper endoscopy: a prospective, randomized<br />
trial. Gastroenterology 2002;123:8.<br />
105. Gauthier RA, Dyck B, Chung R, et al. Respiratory interaction<br />
after spinal anesthesia sedation with midazolam.<br />
<strong>Anesthesiology</strong> 1992;77:909.<br />
106. Kanto J, Sjoval S, Vuori A. Effect of different kinds of<br />
premedication on the induction properties of midazolam.<br />
Br J Anaesth 1982;54:507.
16. Intravenous Hypnotic Anesthetics 245<br />
107. Norton AC, Dundas CR. Induction agents for day-case<br />
anaesthesia. Anaesthesia 1990;45:198.<br />
108. Liu J, Singh H, White PF. Electroencephalogram bispectral<br />
analysis predicts the depth of midazolam-induced sedation.<br />
<strong>Anesthesiology</strong> 1996;84:64–69.<br />
109. Melvin MA, Johnson BH, Quasha AL, et al. Induction of<br />
anesthesia with midazolam decreases halothane MAC in<br />
humans. <strong>Anesthesiology</strong> 1982;57:238.<br />
110. <strong>The</strong>il DR, Stanley TE, White WD, et al. Continuous<br />
intravenous anesthesia for cardiac surgery: a comparison<br />
of two infusion systems. J Thorac Cardiovasc Anesth 1993;<br />
7:300.<br />
111. Gamble JAS, Kawar P, Dundee JW, et al. Evaluation of<br />
midazolam as an intravenous induction agent. Anaesthesia<br />
1981;36:868.<br />
112. Jacobs JR, Reves JG, Marty J, et al. Aging increases pharmacodynamic<br />
sensitivity to the hypnotic effects of midazolam.<br />
Anesth Analg 1995;80:143.<br />
113. Brown CR, Sarnquist FH, Canup CA, et al. Clinical<br />
electroencephalographic and pharmacokinetic studies of<br />
water-soluble benzodiazepine, midazolam maleate. <strong>Anesthesiology</strong><br />
1979;50:467.<br />
114. Nilsson A, Persson MP, Hartvig P, et al. Effect of<br />
total intravenous anaesthesia with midazolam/alfentanil<br />
on the adrenocortical and hyperglycaemic response to<br />
abdominal surgery. Acta Anaesthesiol Scand 1988;32:<br />
379.<br />
115. Doenicke AW, Roizen MF, Kugler J, Kroll H, Foss J,<br />
Ostwald P. Reducing myoclonus after etomidate. <strong>Anesthesiology</strong><br />
1999;90(1):113–119.<br />
116. Watcha MF, White PF. Postoperative nausea and vomiting.<br />
Its etiology, treatment, and prevention. <strong>Anesthesiology</strong><br />
1992;77:162–184.<br />
117. Kettler D, Sonntag H, Donath U, Regensburger D. Schenk<br />
HD. Haemodynamics, myocardial mechanics, oxygen<br />
requirement and oxygenation of the human heart during<br />
induction of anaesthesia with etomidate. Anaesthesist<br />
1974;23:116.<br />
118. Choi SD, Spaulding BC, et al. Comparison of the ventilatory<br />
effects of etomidate and methohexital. <strong>Anesthesiology</strong><br />
1985;62:442.<br />
119. Allolio B, Dörr H, Stuttmann R, Knorr D, Engelhardt D,<br />
Winkelmann W. Effect of a single bolus dose of etomidate<br />
upon eight major corticosteroid hormones and plasma<br />
ACTH. Clin Endocrinol (Oxf) 1985;22:281.<br />
120. Wagner RL, White PF. Etomidate inhibits adrenocortical<br />
function in surgical patients. <strong>Anesthesiology</strong> 1984;61:<br />
647–651.<br />
121. Arden JR, Holley OF, Stanski DR. Increased sensitivity to<br />
etomidate in the elderly: initial distribution versus altered<br />
brain response. <strong>Anesthesiology</strong> 1986;65:19–27.<br />
122. Korttila K, Aromaa U. Venous complications after intravenous<br />
injection of diazepam, flunitrazepam, thiopentone<br />
and etomidate. Acta Anaesthesiol Scand 1980;24:227.
17<br />
Inhalational Anesthetics<br />
Gary R. Haynes<br />
General anesthesia with inhalational anesthetic agents is<br />
the most common method of surgical anesthesia. Although<br />
regional and neuroaxial anesthetics are preferred in some<br />
circumstances, the use of general anesthesia with in -<br />
halational agents remains widespread. Total intravenous<br />
anesthesia has greater acceptance in Europe where it<br />
accounts for approximately 40% of general anesthesia<br />
cases. However, only a small portion of general anesthesia<br />
cases in the United States use this technique.<br />
General anesthesia in older adults with inhalational<br />
agents compares favorably to intravenous anesthesia. 1<br />
However, there are many gaps in our knowledge of volatile<br />
anesthetic drug effects in the elderly. Many of the<br />
most comprehensive studies on inhalational anesthetics<br />
were done in young adults. Clinical drug trials demonstrating<br />
their safety, dosing, and efficacy frequently involve<br />
younger patients. When clinical trials enroll subjects over<br />
a range of ages, they frequently do not stratify patients<br />
into age groups. Consequently, it is often impossible to<br />
make statements describing any differences between<br />
younger and older patients.<br />
<strong>The</strong> focus of past clinical studies investigating inhalational<br />
anesthetic agents was their immediate effects and<br />
short-term outcomes. <strong>The</strong> control of cardiovascular<br />
responses and time for emergence from general anesthesia<br />
are typical examples. <strong>The</strong>re is only limited information<br />
on the immediate perioperative outcome of elderly<br />
patients and even fewer reports regarding their long-term<br />
outcomes. When the concern is the elderly patient, there<br />
are often more questions than answers.<br />
<strong>The</strong> Pharmacokinetics of Inhalational<br />
Agents in the Elderly<br />
<strong>The</strong> pharmacokinetic aspects of inhalational anesthetic<br />
agents include the absorption, distribution, and metabolism<br />
of these drugs. Profound age-related changes occur<br />
in the pharmacokinetics of intravenous drugs, so it is<br />
anticipated that age will also change inhalational anesthetic<br />
behavior. However, there are few studies describing<br />
how their pharmacokinetics change with age.<br />
Advancing age modifies every aspect of systems controlling<br />
the movement of these drugs. Consequently, the<br />
assumptions based on the behavior of inhaled anesthetics<br />
in younger patients may not hold when administered to<br />
older individuals. Some insight comes from the results of<br />
studies in middle-aged adults or from studies in the<br />
elderly conducted for some purpose other than examining<br />
pharmacokinetics.<br />
<strong>The</strong> pharmacokinetics of volatile anesthetics can be<br />
studied in one of two ways. Under laboratory conditions,<br />
subanesthetic doses of several agents can be administered<br />
in combination to a single subject. This approach<br />
has the advantage of limiting the variability between individuals<br />
while measuring the kinetics of each drug. <strong>The</strong><br />
drawback of this method is the inability to measure the<br />
pharmacologic effect specific to each drug. 2,3 <strong>The</strong> other<br />
method is to administer a single agent and track it in an<br />
individual subject. <strong>The</strong>se studies require validation in<br />
many subjects. Frequently, the design of such studies does<br />
not address the issue of age.<br />
Influence of the Aging Pulmonary System<br />
Uptake of anesthetics begins when the fresh gas inflow<br />
from the anesthesia machines carries a volatile agent into<br />
the patient. <strong>The</strong> uptake of an inhalational agent is simply<br />
the difference between the inspired and expired concentrations<br />
multiplied by the alveolar ventilation.<br />
<strong>The</strong> total gas flow passing through the vaporizer determines<br />
the rate of inhalational agent consumption. 4 In<br />
young subjects, saturation is most rapid with desflurane.<br />
Saturation is next most rapid with sevoflurane. High fresh<br />
gas flow (>3 L/min) will consume volatile agents more<br />
rapidly than when using low flows, and anesthetic drug<br />
cost can be reduced by using a low-flow technique.<br />
246
17. Inhalational Anesthetics 247<br />
With the low-flow technique, fresh gas flow rate is reduced<br />
to less than half the patient’s minute ventilation, usually<br />
to less than 3.0 L/min. Monitoring of inspired and expired<br />
gas concentrations is mandatory. At a low flow rate,<br />
consumption of an insoluble agent, such as desflurane,<br />
depends on fresh gas flow whereas halothane does not.<br />
Consumption of isoflurane and enflurane vary with<br />
minimal and low fresh gas flow rates. 5<br />
Do anesthetic agents control the response to surgical<br />
stimulation in the same manner at low flows? <strong>The</strong> partial<br />
pressure of agents in pulmonary arterial blood that have<br />
a low blood/gas solubility should change rapidly with<br />
changes in vaporizer settings. Desflurane provides faster<br />
control of hemodynamic responses at 1 and 3 L/min flows,<br />
and its use requires fewer incremental increases to control<br />
acute responses to surgical stimulation. At fresh gas flow<br />
rates of 1 L/min, more interventions are necessary to<br />
control blood pressure in older patients receiving isoflurane<br />
compared with desflurane. 6<br />
<strong>The</strong> respiratory changes characterizing advanced<br />
age have been thoroughly reviewed by others. 7–11 <strong>The</strong><br />
principal anatomic changes include lung atrophy and a<br />
loss of pulmonary elasticity. <strong>The</strong>re is a loss of alveolar<br />
walls, a depletion of the connective tissue elastin, and an<br />
increase in interstitial fibrous tissue. <strong>The</strong> histopathologic<br />
change in the senescent lung is sometimes termed “senile<br />
emphysema,” and it refers to the atrophic changes and<br />
dilatation of the alveoli that mimic mild emphysema<br />
(Figure 17-1).<br />
<strong>The</strong> destruction of alveolar walls results in small alveoli<br />
coalescing to form larger sacs. Consequently, the lungs<br />
have less elasticity and less natural recoil to hold small<br />
airways open as lung volumes change with respiration. 12,13<br />
Airways from the level of bronchioles to the alveolar<br />
ducts lack a cartilaginous support. Without a semirigid<br />
structure to keep them open during passive exhalation,<br />
these airways depend on the elastic recoil of the lung<br />
parenchyma to prevent collapse at low lung volumes<br />
(Figure 17-2). <strong>The</strong>re is an age-related decrease in the<br />
diameter of small bronchioles from the fourth decade<br />
that is consistent with decreased compliance. 14 In the<br />
older patient, these dependent airways close at a higher<br />
lung volume than in younger subjects. <strong>The</strong> physiologic<br />
consequence of these changes is increasing ventilationperfusion<br />
(V/Q) mismatching with advancing age.<br />
A progressive hypoxemia develops as the number of<br />
alveoli gradually decreases and anatomic dead space<br />
increases. 15<br />
<strong>The</strong> increased closing volume makes it more likely an<br />
older patient will experience hypoxia at some time in the<br />
perioperative period. Older patients experience hemoglobin<br />
desaturation at a faster rate because of greater<br />
V/Q mismatching. In the operating room, the transfer of<br />
oxygen is not as efficient when using positive pressure<br />
ventilation in the supine position as it is when breathing<br />
spontaneously. <strong>The</strong> combination of altered ventilatory<br />
response to hypoxia, sedation from residual inhalational<br />
agents, and analgesics increases the risk of hypoxia after<br />
general anesthesia. <strong>The</strong> likelihood of hypoxia is further<br />
compounded if pulmonary disease is superimposed on<br />
age-related changes.<br />
An age-related mismatching of pulmonary ventilation<br />
and perfusion may influence the uptake of volatile anesthetic<br />
agents. Areas of the lung that are well ventilated<br />
but with less perfusion will contribute more anesthetic<br />
gas and can be expected to cause a more rapid increase<br />
in the ratio of alveolar (F A ) to inspired (F I ) agent concentrations.<br />
However, there is little evidence to confirm this.<br />
A<br />
B<br />
Figure 17-1. Histologic sections of normal lung from a nonsmoking (A) 22-year-old homicide victim, and (B) a 75-year-old individual<br />
(hematoxylin and eosin stain, 2×).
248 G.R. Haynes<br />
14<br />
12<br />
A<br />
110<br />
100<br />
B<br />
Pst(I), H 2 O<br />
10<br />
8<br />
6<br />
4<br />
Arterial PaO2 (mmHg)<br />
90<br />
80<br />
70<br />
2<br />
Age vs Pst(I)<br />
95% C.I.<br />
60<br />
0<br />
0 10 20 30 40 50 60 70<br />
Age, years<br />
Figure 17-2. (A) <strong>The</strong> change in static recoil of the lung measured<br />
at 60% of total lung capacity. <strong>The</strong> decrease in recoil with<br />
age is apparent. Atrophy of pulmonary parenchyma results in<br />
less elastic recoil to hold open small airways at low tidal volumes.<br />
(Data from Turner et al. 13 ) (B) Increasing ventilation-perfusion<br />
50<br />
0 20 30 40 50 60 70 80<br />
Age, years<br />
mismatching occurring with age leads to lower resting PaO 2 .<br />
<strong>The</strong> resting arterial tension was determined by the equation<br />
PaO 2 (mm Hg) = 143.6 − (0.39 × age) − (0.56 × BMI) − (0.57 ×<br />
Paco 2 ), assuming a BMI of 25 and Paco 2 of 40 mm Hg.<br />
(Data from Cerveri et al. 15 )<br />
In the absence of grossly abnormal pulmonary function,<br />
the small increase in the F A /F I ratio caused by a progressive<br />
V/Q mismatch is probably offset by a lower metabolic<br />
rate, and hence lower ventilation and perfusion per<br />
kilogram body weight in the elderly. It is difficult to demonstrate<br />
any difference in anesthetic uptake attributable<br />
to age alone in normal patients (Edmond Eger, personal<br />
communication, 2005). However, patients with chronic<br />
pulmonary obstructive disease from emphysema, chronic<br />
bronchitis, or asthma will have a slower increase in the<br />
alveolar concentration (F A ) of volatile anesthetic agents<br />
(Figure 17-3).<br />
<strong>The</strong>re is no evidence that an obstruction to diffusion<br />
of anesthetic agents develops with age. Alveolar thickening<br />
from unusual disorders such as idiopathic pulmonary<br />
fibrosis or common problems such as lung congestion<br />
from cardiac failure should slow diffusion of anesthetic<br />
gases, but it is not likely that this results in a slower<br />
increase in the partial pressure of the inhalational agent<br />
in pulmonary venous blood.<br />
Any change in V/Q mismatching has a more pronounced<br />
effect on inhalational agents with low blood/gas<br />
partition (B/G) coefficients. 16 This includes sevoflurane,<br />
desflurane, and the inorganic compound nitrous oxide<br />
(Table 17-1). Lu et al. 17 measured sevoflurane concentration<br />
in arterial and jugular venous blood samples in<br />
patients during cardiac surgery. <strong>The</strong>ir study population<br />
consisted of 10 patients between the ages of 51 and 73<br />
years who received a constant 3.5% inspired sevoflurane<br />
concentration for 1 hour. It took 40 minutes before the<br />
concentration of sevoflurane in venous blood became<br />
equal to the arterial blood. <strong>The</strong> arterial sevoflurane concentration<br />
was also approximately 40% less than the endtidal<br />
expired sevoflurane. Thus, the end-tidal sevoflurane<br />
concentration did not reliably reflect the parallel concentration<br />
of sevoflurane in the brain. <strong>The</strong> equilibration<br />
between arterial blood and brain tissues takes four times<br />
longer than predicted and sevoflurane uptake in the brain<br />
takes approximately 1 hour. 17 As a result of the changes<br />
showing slower uptake, it should also be anticipated there<br />
F A /F I<br />
1.0<br />
0.8<br />
0.6<br />
0.4<br />
0.2<br />
Normal<br />
Obstructive pulmonary disease<br />
0.0<br />
0 5 10 15 20 25 30 35<br />
Time (min)<br />
Figure 17-3. <strong>The</strong> effect of pulmonary disease on the increase<br />
of alveolar concentration (F A ) compared with inspired concentration<br />
(F I ) versus time. <strong>The</strong> increase in F A /F I is slower in subjects<br />
with pulmonary disease. (Adapted with permission from<br />
Gloyna DF. Effects of inhalation agents. In: McLeskey CH, ed.<br />
<strong>Geriatric</strong> <strong>Anesthesiology</strong>. Baltimore: Williams & Wilkins;<br />
1997.)
17. Inhalational Anesthetics 249<br />
Table 17-1. Physical properties of inhalational agents including nitrous oxide.<br />
Molecular Boiling* Vapor<br />
Partition coefficient<br />
Recovered as<br />
Agent weight*† (g) point (°C) pressure*‡ Oil/gas* Blood/gas* Fat/blood§ metabolites (%)<br />
Halothane 197.4 50 243 224 2.3 51 11–25<br />
F CI<br />
Br<br />
F<br />
F<br />
Enflurane 184.5 57 172 98.5 1.91 36 2.4<br />
F<br />
F F<br />
F<br />
F O<br />
CI<br />
Isoflurane 184.5 49 238 90.8 1.4 45 0.2<br />
CI F<br />
F<br />
O<br />
F F<br />
F<br />
Desflurane 168 24 669 19 0.45 27 0.02<br />
F<br />
F O<br />
F<br />
F<br />
F F<br />
Sevoflurane 200 59 157 53.4 0.60 48 5.0<br />
F<br />
F<br />
F<br />
F O<br />
F<br />
F F<br />
Nitrous oxide 44 −88 38,770 1.4 0.47 2.3 0<br />
O<br />
I N<br />
N<br />
Note: Values are based on measurement at 37°C unless otherwise noted.<br />
*Data from Stevens WC, Kingston HGG. Inhalational <strong>Anesthesia</strong>. In: Barash PG, ed. Clinical <strong>Anesthesia</strong>. Philadelphia: JB Lippincott; 1989:295.<br />
†Data from Eger EI, Weiskopf RB, Eisenkraft JB. <strong>The</strong> Pharmacology of Inhaled Anesthetics. <strong>The</strong> Dannemiller Memorial Educational Foundation;<br />
2002.<br />
‡At 20°C, in mm Hg.<br />
§Data from Eger EI. Uptate and Distribution. In: Miller RD, ed. <strong>Anesthesia</strong>. Philadelphia: Elsevier Churchill Livingstone; 2005:132.<br />
Data from Carpenter et al. 73<br />
For individuals aged 30–60 years.<br />
will be slower elimination of inhalational anesthetics<br />
from altered pulmonary function. 18<br />
Alveolar ventilation does not change with age. However,<br />
there are changes that lead to degrees of V/Q mismatching<br />
and changes in the control of minute ventilation in<br />
response to hypoxia and hypercarbia. <strong>The</strong> normal partial<br />
pressure of carbon dioxide in arterial blood is 4.6–5.3 kPa<br />
(34.5–39.8 mm Hg) in older patients. 19,20 With advancing<br />
age, the control of ventilation is less sensitive. <strong>The</strong> normal<br />
response to hypercarbia is an increase in the minute ventilation.<br />
In young individuals, there is a profound response,<br />
about 2–5 L/min per torr carbon dioxide. 21,22 Where the<br />
response to rebreathing carbon dioxide is 3.4 L/min in<br />
men whose average age is 26 years, the response is only<br />
1.8 L/min in men who are about 70 years of age. 23 <strong>The</strong><br />
likelihood of respiratory acidosis from impaired ventilation<br />
after general anesthesia is therefore greater but it is<br />
not documented.<br />
<strong>The</strong> ventilatory response to hypoxia greatly diminishes<br />
with advanced age. 23 When combined with the sedative<br />
effect of inhalational anesthetics, the profoundly impaired<br />
drive to increase minute ventilation in response to hypoxia<br />
leaves the elderly patient at risk for hypoxia. This may<br />
contribute to the numerous instances of respiratory complications<br />
in the recovery period including hypoxia<br />
hypoventilation, and atelectasis. 24 <strong>The</strong>refore, less-soluble<br />
inhalational anesthetic drugs for elderly patients are reasonable<br />
choices. Transporting elderly patients with supplemental<br />
oxygen from the operating room to the<br />
postanesthesia care unit (PACU) is prudent. Generous<br />
use of supplemental oxygen and close monitoring while<br />
in the PACU are imperative.
250 G.R. Haynes<br />
Influence of the Aging Cardiovascular System<br />
<strong>The</strong> major cardiovascular changes occurring with age<br />
include impaired pump function and atherosclerotic<br />
changes in the vasculature. <strong>The</strong>se changes occur independently<br />
of diseases that can affect the heart and peripheral<br />
vasculature. <strong>The</strong> most common cardiovascular problems<br />
are hypertension, arteriosclerosis, atherosclerotic vascular,<br />
and coronary disease. Angina pectoris and myocardial<br />
ischemia leading to myocardial infarction are frequent<br />
myocardial events. 25 Heart failure is a common problem<br />
in the elderly. <strong>The</strong> incidence of heart failure in the elderly<br />
is 20–30 cases per 1000 persons older than 80 years of<br />
age. 26 Approximately half of congestive heart failure<br />
cases occur in patients with preserved systolic function, a<br />
problem now recognized as diastolic dysfunction. 27<br />
Aside from being the frequent target of disease, the<br />
cardiovascular system experiences a decline in function<br />
with age. One general measure of cardiac function, the<br />
maximum oxygen transport or VO 2-max , decreases at the<br />
rate of approximately 1% per year after age 30. 28–30 It is<br />
tempting to rely on cardiac output as a way of assessing<br />
the effect of age. However, changes in cardiovascular<br />
function are variable and not easily attributed to a single<br />
cause. Cardiac output has several determinants, and, as a<br />
single index, it is not an adequate measure to understand<br />
anesthetic effects in the elderly.<br />
In healthy older subjects, the peripheral flow of blood<br />
decreases and peripheral vascular resistance increases in<br />
comparison to younger counterparts. Physical conditioning<br />
does not alter these changes 31 (Figure 17-4). Increasing<br />
vascular resistance may explain some decrease in<br />
A<br />
Femoral Blood Flow (ml/min)<br />
600<br />
500<br />
400<br />
300<br />
200<br />
r = –0.40<br />
P < 0.001<br />
B<br />
Femoral Vascular<br />
Resistance (U)<br />
0.7<br />
0.6<br />
0.5<br />
0.4<br />
0.3<br />
0.2<br />
r = 0.47<br />
P < 0.001<br />
C<br />
100<br />
10 20 30 40 50 60 70 80<br />
8<br />
Young (20–35 years)<br />
Older (55–75 years)<br />
0.1<br />
10 20 30 40 50 60 70 80<br />
Age (years)<br />
6<br />
Cardiac output (L/min)<br />
4<br />
2<br />
0<br />
Sedentary<br />
Physically active<br />
Endurance trained<br />
Figure 17-4. Cardiovascular changes<br />
occurring with age in healthy male<br />
subjects. Femoral blood flow decreases<br />
(A) and peripheral vascular resistance<br />
increases (B) with age. <strong>The</strong> effect of age<br />
on these variables is not influenced by<br />
exercise conditioning. (C) Age-related<br />
changes in cardiac output are minor.<br />
(A and B reprinted with permission,<br />
and C data from Dienno FA, Seals DR,<br />
DeSouza CA, Tanaka H. Age-related<br />
decreases in basal limb blood flow in<br />
humans: time course, determinants<br />
and habitual exercise effects. J Physiol<br />
2001;531:573–579.)
17. Inhalational Anesthetics 251<br />
cardiac output, but decreases in cardiac output may also<br />
result from decrement in the chronotropic response, systolic,<br />
and diastolic function. <strong>The</strong>re is general agreement<br />
that the maximum heart rate response decreases with age.<br />
<strong>The</strong> maximum cardiac stroke volume does not change<br />
very much as a result of age alone, but it may decrease<br />
for several reasons, such as ventricular hypertrophy, stiffening<br />
of the ventricular wall, lower preload, and higher<br />
afterload. By carefully matching the physical abilities of<br />
older master athletes with younger competitive runners,<br />
Hagberg et al. 32 demonstrated that the decrease in<br />
VO 2-max occurring with age is attributable only to a<br />
decreased maximal heart rate. <strong>The</strong>re was no change in the<br />
stroke volume and arterial-venous oxygen difference to<br />
account for lower cardiac output. 32 <strong>The</strong> influence of age<br />
on cardiac function is seen when normal subjects are<br />
stressed. <strong>The</strong> cardiac output is maintained by increasing<br />
the end-diastolic volume, and thus the stroke volume, to<br />
compensate for less ability to increase the heart rate<br />
(Figure 17-5).<br />
SLOPE COEFFICIENT OF AGE REGRESSION<br />
1.0<br />
.80<br />
.60<br />
.40<br />
.20<br />
0<br />
–.20<br />
–.40<br />
–.60<br />
EDV<br />
ESV<br />
SBP<br />
CD<br />
EF<br />
Figure 17-5. <strong>The</strong> action of increasing workload on cardiac function<br />
as a function of advancing age. Each point is the slope of<br />
a coefficient for each physiologic parameter measured in a<br />
group of normal subjects ranging in age from 25 to 79 years. <strong>The</strong><br />
subjects performed stationary bicycle work while hemodynamic<br />
measurements were taken and worked to the point of exhaustion.<br />
An increase or decrease in the slope coefficient with<br />
increasing workload indicates an increasing or decreasing effect<br />
of age. CO = cardiac output, EDV = end-diastolic volume,<br />
ESV = end-systolic volume, SBP = systolic blood pressure,<br />
EF = ejection fraction, HR = heart rate. (Reprinted with permission<br />
from Rodeheffer RJ, Gerstenblith G, Becker LC, Fleg JL,<br />
Weisfeldt ML, Lakatta EG. Exercise cardiac output is maintained<br />
with advancing age in healthy human subjects, cardiac<br />
dilatation and increased stroke volume compensate for a diminished<br />
heart rate. Circulation 1984;69:203–213.)<br />
HR<br />
REST 25 50 75 100<br />
WATTS<br />
Cardiac output is determined by the heart rate and<br />
stroke volume. Altered uptake and distribution of inhalational<br />
anesthetic agents result when cardiac pump function<br />
decreases. Patients with decreased cardiac output<br />
have a slower systemic circulation time that is matched<br />
with a slower circulation through the pulmonary circuit.<br />
During general anesthesia, slower pulmonary circulation<br />
provides more time for volatile anesthetic agents to<br />
diffuse into the blood. Pulmonary venous blood can attain<br />
a higher partial pressure of anesthetic gas under these<br />
circumstances than anticipated. Thus, the effect of lower<br />
cardiac output is greater delivery of anesthetic drug to<br />
the myocardium and the central nervous system. Generally,<br />
this effect occurs with the more soluble anesthetics<br />
such as halothane and enflurane. <strong>The</strong> action of low cardiac<br />
output increasing uptake is attenuated by anesthetics<br />
with a lower B/G solubility. This favors the use of lowsolubility<br />
agents such as desflurane and sevoflurane.<br />
A slower systemic circulation also slows delivery of<br />
anesthetic agents to target tissues including the central<br />
nervous system (Figure 17-6). <strong>The</strong> clinical result is a slower<br />
onset of anesthesia. However, with the most soluble inhalational<br />
agents, a lower cardiac output means arterial blood<br />
will convey a higher partial pressure of anesthetic agent to<br />
the central nervous system, and, consequently, with greater<br />
drug delivery, the anesthetic effect may be more profound.<br />
Low cardiac output in patients with cardiac disease exaggerates<br />
this effect. Volatile anesthetic agents can cause a<br />
cycle of myocardial depression leading to increased uptake,<br />
increased alveolar concentration, and further depression<br />
of cardiac output. <strong>The</strong>refore, the potential cardiac depressant<br />
effect of volatile anesthetics is significant.<br />
Anesthetics may decrease stroke volume by depressing<br />
contractility or slowing the rate. Bradycardia is encountered<br />
in many clinical situations and it is often a simple<br />
problem to treat. An advantage of newer volatile anesthetics<br />
is that they generally cause little change in heart<br />
rate or they tend to increase it slightly at higher concentrations<br />
(Figure 17-7). In younger patients, tachycardia results<br />
from abrupt increases in desflurane administration above<br />
1 minimal alveolar concentration (MAC) (Figure 17-8). A<br />
similar but less-pronounced response also occurs with isoflurane.<br />
33 Suddenly increasing the administration of this<br />
agent has no advantage because the drug’s low solubility<br />
will result in a rapid change of its partial pressure in blood.<br />
<strong>The</strong> depression of myocardial contractility by anesthetic<br />
agents is a more important consideration. <strong>Global</strong> cardiac<br />
depression is most likely with halothane, enflurane, and to<br />
some extent, isoflurane. <strong>The</strong>se drugs are more soluble in<br />
blood than either desflurane or sevoflurane, and can have<br />
a greater effect for this reason (Table 17-2).<br />
Predicting how patients with combined pulmonary and<br />
cardiac disease will respond during general anesthesia<br />
with volatile anesthetics is difficult. Clinicians can expect<br />
slower induction and longer emergence from inhalational
252 G.R. Haynes<br />
Reduced cardiac output<br />
CNS<br />
Anesthetic<br />
concentration<br />
Normal cardiac output<br />
Time<br />
Figure 17-6. Reduced cardiac output results in slower pulmonary<br />
circulation and allows for the diffusion of more anesthetic<br />
agent into the blood. This results in a more rapid increase in the<br />
partial pressure of agent in the blood, greater delivery to the<br />
central nervous system, and a more profound onset of anesthesia.<br />
This is more likely with the very soluble anesthetic agents.<br />
However, the onset of action may be delayed compared with<br />
patients with normal cardiac output. (Reprinted with permission<br />
from Gloyna DF. Effects of inhalation agents. In: McLeskey<br />
CH, ed. <strong>Geriatric</strong> <strong>Anesthesiology</strong>. Baltimore: Williams &<br />
Wilkins; 1997. Data from Musnon ES, Eger EI II, Bowers DL.<br />
<strong>The</strong> effects of changes in cardiac output and distribution on the<br />
rate of cerebral anesthetic equilibration. Calculations using a<br />
mathematical model. <strong>Anesthesiology</strong> 1968;29(3):533–537.)<br />
anesthesia. It is also likely these patients will have greater<br />
hemodynamic instability during anesthesia.<br />
Influence of Body Composition Changes<br />
A primary factor influencing inhalational agent pharmacokinetics<br />
is the change in body composition. <strong>The</strong>se<br />
include a reduction in the skeletal muscle mass and an<br />
increase in the total body fat content. 34 Although there is<br />
considerable variation, the general trend is for an increase<br />
in the percentage of body fat (Figure 17-9). <strong>The</strong> change<br />
in body composition is greater for men, with about 25%<br />
of their total body mass being fat. For older women, the<br />
total body fat content averages 35%. 35 As total body fat<br />
increases with age, the proportion of total body water<br />
also decreases.<br />
A 140<br />
B 140<br />
Heart Rate (beats/min)<br />
120<br />
100<br />
80<br />
DES - O 2<br />
DES - N 2 O<br />
Heart Rate (beats/min)<br />
120<br />
100<br />
80<br />
Isoflurane-O 2 1st hour<br />
Isoflurane-O 2 5th hour<br />
60<br />
0.0 0.2 0.4 0.6 0.8 1.0 1.2 1.4 1.6 1.8<br />
Total MAC equivalent<br />
60<br />
0.8 1.0 1.2 1.4 1.6 1.8 2.0 2.8<br />
Total MAC equivalent<br />
Figure 17-7. (A) Hemodynamic effects of desflurane (DES)<br />
during controlled ventilation in young volunteer subjects. <strong>The</strong><br />
subjects received no other drugs. MAC = minimal alveolar concentration.<br />
(Data from Cahalan MK, Weiskopf RB, Eger EI II,<br />
et al. Hemodynamic effects of desflurane/nitrous oxide anesthesia<br />
in volunteers. Anesth Analg 1991;73:157–164.) (B) Hemodynamic<br />
effects of isoflurane during controlled ventilation in<br />
young volunteer subjects. Measurements were made during the<br />
first and fifth hours of continuous anesthesia and demonstrate<br />
small changes occurring in the heart rate response with prolonged<br />
anesthesia. (Data from Stevens et al. 38 )
17. Inhalational Anesthetics 253<br />
Figure 17-8. A transient increase in heart rate, blood pressure,<br />
and sympathetic activity occurs with isoflurane and desflurane<br />
when the concentrations are increased rapidly to more than 1<br />
minimal alveolar concentration. Several interventions have<br />
been described to effectively counter this occurrence, including<br />
avoiding the “over pressuring” technique. HR = heart rate,<br />
MAP = mean arterial pressure. (Reprinted with permission<br />
from Weiskopf et al. 33 )<br />
Fat tissue has a great capacity to retain lipid-soluble<br />
drugs. For those inhalational agents with greater lipid<br />
solubility, the volume of distribution increases (Tables<br />
17-1 and 17-3). Fat acts as a reservoir for volatile agents,<br />
resulting in the accumulation of inhalational agents<br />
during maintenance and delaying emergence. Depending<br />
on many variables, including the lipid solubility of the<br />
agent, less blood flow to fat tissue than other tissues, and<br />
the duration of anesthesia, an increase in the proportion<br />
of body fat may prolong emergence. Although the changes<br />
in body fat composition are greater in men, and women<br />
have a greater percent body fat at all ages, there is no<br />
indication of a gender difference with the pharmacokinetics<br />
of inhalational anesthetic agents.<br />
<strong>The</strong> lipid-soluble drugs redistribute slowly from<br />
fat tissue so their effect may be prolonged. <strong>The</strong> loss of<br />
skeletal muscle mass has a significant impact on drug<br />
pharmacokinetics because this tissue receives a large<br />
portion of the blood supply. As the body fat content<br />
increases, a smaller part of each circulating blood volume<br />
perfuses this tissue and it diminishes the volume of distribution<br />
for the agents that are not very lipid soluble.<br />
Most body fat resides in subcutaneous and abdominal<br />
areas. However, body fat may be heterogeneous and<br />
various anatomic fat stores may differ in their capacity to<br />
act as a reservoir for lipid-soluble drugs. 36 Subcutaneous<br />
fat that develops from excessive eating may function differently<br />
from the epicardial or mesenteric fat that is<br />
present even in very lean individuals. How this might<br />
affect the uptake and retention of lipid-soluble inhalational<br />
agents is yet to be determined.<br />
<strong>The</strong> steady-state volume of distribution, V dss , is greatest<br />
for isoflurane and least with desflurane 37 (Table 17-3). <strong>The</strong><br />
movement of volatile agent from the central to peripheral<br />
compartments is fastest for desflurane and intermediate<br />
for sevoflurane, whereas isoflurane is the slowest.<br />
Table 17-2. <strong>The</strong> influence of halothane or enflurane on myocardial contractility, E ES ,<br />
in a canine model and during coronary artery bypass surgery.<br />
Canine model<br />
Halothane (n = 7) Enflurane (n = 7) CABG surgery<br />
Control 10.1 ± 0.6 15.2 ± 0.4 Control 11.5 ± 2.0<br />
1% 6.7 ± 0.4 12.3 ± 0.6 60% N 2 O 9.0 ± 2.2<br />
2% 4.2 ± 0.5 9.3 ± 0.5 0.5% halothane 8.1 ± 2.4<br />
Source: Data from Van Trigt P, Christian CC, Fagraeus L, et al. Myocardial depression by anesthetic<br />
agents (halothane, enflurane, and nitrous oxide): quantitation based on end-systolic<br />
pressure-dimension relations. Am J Cardiol 1984;53:243–247.<br />
E ES (mm Hg/mm) = slope of the end-systolic pressure-diameter relation, a sensitive index of contractility<br />
unaffected by volume loading; CABG = coronary artery bypass graft.
254 G.R. Haynes<br />
A<br />
Figure 17-9. <strong>The</strong> change in body composition occurring<br />
with age. Data from the Fels Longitudinal Study including<br />
men (A) (n = 102) and women (B) (n = 108) for<br />
subjects not selected because of any known criteria<br />
related to body composition. Women have a greater<br />
percent of body fat than men at all ages. Men have an<br />
increasing trend in body weight and percent body fat.<br />
Women tend to lose fat-free mass as they become older.<br />
(Data from Guo et al. 34 )<br />
B<br />
It is not just the greater solubility of isoflurane that<br />
accounts for its V d being six times that of desflurane. Isoflurane<br />
increases blood flow to tissues such as skeletal<br />
muscle, a tissue with large storage capacity. 37,38<br />
<strong>The</strong> partial pressure of anesthetic permitting wakefulness,<br />
the MAC-awake value, determines the emergence<br />
from general anesthesia. <strong>The</strong> MAC-awake value for all<br />
volatile anesthetics is about one third the MAC value. A<br />
slow, continued release of volatile agent from fat tissue<br />
can maintain a partial pressure of agent in the blood<br />
causing excessive sedation, respiratory depression, and<br />
contribute to postanesthesia delirium. This action may<br />
Table 17-3. Pharmacokinetics of newer volatile anesthetic agents.<br />
Agent MAC B/G* FGF† k 3 12 (min −1 ) Cl 12 ‡ (mL vapor kg −1 min −1 ) V dss ‡ (mL vap /kg bw )<br />
Sevoflurane 2.1 0.69 2 0.117 (0.070–0.344) 13.0 (9.8–22.4) 1748 (819–8997)<br />
Isoflurane 1.2 1.4
17. Inhalational Anesthetics 255<br />
contribute to a greater incidence of postoperative complications<br />
and prolonged stays in the PACU.<br />
<strong>The</strong> increasing proportion of body fat suggests an<br />
advantage with the less-soluble volatile anesthetic drugs.<br />
Emergence from general anesthesia has been studied by<br />
comparing desflurane and isoflurane anesthesia in elderly<br />
patients. Compared with isoflurane anesthesia, signs of<br />
early recovery and endotracheal tube removal occurred<br />
in approximately half the time with desflurane. Emergence<br />
was also faster than with intravenous anesthesia. 39<br />
For short procedures (less than 2 hours), patients reached<br />
signs of early recovery and experienced endotracheal<br />
tube removal sooner with desflurane compared with<br />
sevoflurane. 40<br />
Influence of Renal Changes<br />
Renal atrophy occurs with age, mainly through the loss<br />
of cortical nephrons. <strong>The</strong> kidney loses about 20% of its<br />
mass by age 80, and functional changes accompany renal<br />
atrophy. <strong>The</strong> majority of subjects experience a decrease<br />
in renal blood flow, glomerular filtration rate (GFR), and<br />
creatinine clearance. <strong>The</strong> reduction in renal blood flow<br />
probably results from cardiovascular changes in addition<br />
to renal changes. 41 However, the Baltimore Longitudinal<br />
Study of Aging showed that a decline in the GFR is not<br />
inevitable because 30% of healthy individuals have no<br />
decrease in GFR with age. 42 <strong>The</strong> plasma creatinine level<br />
varies with the muscle mass and with age-related changes<br />
in body composition accompanying the aging process.<br />
Thus, it is better to evaluate renal function in the elderly<br />
using the Cockroft-Gault formula [(140 − age) × weight<br />
(kg)/Cr × 72] than simply using the plasma creatinine<br />
value 43 (Figure 17-10).<br />
All volatile anesthetic agents in clinical use are fluorinated<br />
ether compounds. <strong>The</strong> constellation of renal<br />
changes may place the older patient at greater risk for<br />
fluoride toxicity 44 (Table 17-1). Inorganic free fluoride<br />
ions form during metabolism of these agents by the<br />
hepatic cytochrome P-450 enzyme system. Toxic levels of<br />
free fluoride produce a high output, vasopressin-resistant<br />
form of acute renal failure. 45 This disorder was first<br />
reported with methoxyflurane in 1966.<br />
<strong>The</strong> only inhalation agents used today that can produce<br />
enough fluoride to be of concern are enflurane, isoflurane,<br />
and sevoflurane. 46–48 <strong>The</strong> threshold fluoride level for<br />
causing mild defects in renal concentrating ability is<br />
50 µmol/L. 49 Experiments with cultured collecting duct<br />
cells indicate mitochondria may be the target of the free<br />
fluoride ion. 50<br />
Whether fluoride toxicity results from the use of<br />
modern inhalational anesthetics is in doubt. Concern surrounded<br />
the use of sevoflurane because about 5% of it is<br />
metabolized by the cytochrome P-450 2E1 isoform. 51 Of<br />
that, 3.5% appears in the urine as free fluoride ion. 52 This<br />
is less than the fluoride production from methoxyflurane<br />
metabolism but more than that seen with either enflurane<br />
or isoflurane.<br />
<strong>The</strong> likelihood of fluoride toxicity has been questioned<br />
because fluoride levels in excess of 50 µg/L were reached<br />
in studies comparing sevoflurane and enflurane administration<br />
in humans, yet they did not demonstrate nephrotoxicity.<br />
53 <strong>The</strong> mean fluoride level in patients receiving<br />
sevoflurane was 47 µmol/L, twice the 23 µmol/L level in<br />
Figure 17-10. <strong>The</strong> relationship between serum creatinine and<br />
creatinine clearance by age. <strong>The</strong> glomerular filtration rate<br />
(GFR) decreases in the majority of individuals after age 30 but<br />
a decline in GFR is not inevitable. <strong>The</strong> graphs are standardized<br />
for a 70-kg male with values calculated using the Cockroft-<br />
Gault formula. (Data from Hughes et al. 35 )
256 G.R. Haynes<br />
patients that received prolonged enflurane anesthesia.<br />
More than 40% of subjects having prolonged sevoflurane<br />
anesthesia had plasma fluoride levels greater than<br />
50 µmol/L, with no impairment of renal concentrating<br />
ability. <strong>The</strong> results of this study should be cautiously<br />
extrapolated to the elderly because it included only young<br />
volunteers in their mid-twenties. 54 Neither enflurane nor<br />
halothane produced a further decrease of renal function<br />
in patients with moderate renal insufficiency. 55 At this<br />
time, enflurane is infrequently used for general anesthesia.<br />
<strong>The</strong>re are no clinical reports that actively assert that<br />
enflurane should be avoided in elderly patients with renal<br />
insufficiency.<br />
A toxic fluoride threshold more likely will be met with<br />
prolonged exposure to isoflurane than halothane. <strong>The</strong><br />
peak plasma level of fluoride occurs 24 hours after an<br />
average 10-hour administration of isoflurane. This is<br />
equivalent to 19.2 MAC hours of isoflurane exposure.<br />
With this level of exposure, 40% of patients studied had<br />
fluoride levels slightly greater than 50 µmol/L. In contrast,<br />
similar exposure to halothane produced lower fluoride<br />
levels with the highest plasma levels occurring at the end<br />
of the surgical cases. Among elderly patients with renal<br />
insufficiency, no further deterioration of renal function<br />
resulted with the use of isoflurane, enflurane, or sevoflurane<br />
anesthesia. 56 Desflurane poses very little risk to<br />
patients with renal insufficiency because so very little of<br />
it is metabolized. 57<br />
Sevoflurane breaks down in the alkaline environment<br />
of the carbon dioxide absorber to form fluoromethyl-2,2-<br />
difluoro-1-(trifluoromethyl)vinyl ether, or Compound A.<br />
This happens particularly at low total gas flows. Similar to<br />
free fluoride ion, compound A is also nephrotoxic. <strong>The</strong><br />
production of Compound A is increased with greater production<br />
and absorption of carbon dioxide because<br />
the degradation of sevoflurane increases with absorber<br />
temperature. 58–60 <strong>The</strong> combination favoring production of<br />
Compound A includes not only increased CO 2 absorption<br />
but also absorber temperature, decreased CO 2 washout,<br />
and high levels of sevoflurane. 23,61,62 Compound A is clearly<br />
nephrotoxic in the laboratory, but it is not certain whether<br />
any instances of renal failure occurred from using sevoflurane.<br />
In patients with normal renal function and ranging<br />
in age from 30 to 69 years, Compound A accumulated<br />
during anesthesia with 1 LPM gas flows. Yet, there was no<br />
difference detected in clinical or biochemical markers of<br />
renal function when those patients were compared with<br />
subjects receiving isoflurane anesthesia. 63 Compound A<br />
does not accumulate in breathing circuits or carbon<br />
dioxide absorbers when gas flows are 5 L/min, but because<br />
of the potential for Compound A formation, sevoflurane<br />
is not recommended for use at less than 2 LPM fresh gas<br />
flow. 64 Nevertheless, no differences in biochemical markers<br />
were noted among patients receiving sevoflurane at lowflow<br />
(1 L/min), high-flow (5–6 L/min), or low-flow isoflurane<br />
anesthesia, and no evidence of renal toxicity exists. 65<br />
Furthermore, in older patients with moderately impaired<br />
renal function, sevoflurane anesthesia does not cause<br />
apparent injury to the renal tubules, 66 and low-flow anesthesia<br />
with sevoflurane does not result in any greater<br />
change in blood urea nitrogen, creatinine, or creatinine<br />
clearance than isoflurane. 67<br />
Influence of Hepatic Changes<br />
<strong>The</strong>re is a similar atrophy of the liver that is accompanied<br />
by a reduction in hepatic blood flow. 68–70 Decreased<br />
hepatic blood flow results in diminished metabolism of<br />
drugs that rely on hepatic clearance. <strong>The</strong> decrease in<br />
hepatic blood flow seems responsible for the decreased<br />
hepatic metabolism of drugs and not changes in hepatic<br />
enzyme activity. 71<br />
<strong>The</strong> newer inhalational agents are not extensively<br />
metabolized. Of all the volatile agents, halothane is the<br />
most extensively transformed with approximately 20% of<br />
it metabolized in the liver. 72 <strong>The</strong> other agents in common<br />
use are metabolized to a much lesser extent. Approximately<br />
5% of sevoflurane, 2.4% of enflurane, 0.2% of<br />
isoflurane, and 0.02% of desflurane are metabolized 16,73–75<br />
(Table 17-1). Metabolism of halothane, isoflurane, and<br />
desflurane produces trifluoroacetic acid. <strong>The</strong> amount of<br />
this metabolite produced is lowest with desflurane. 72,76–79<br />
<strong>The</strong> hepatic-function changes associated with aging<br />
are probably important only for halothane and sevoflurane<br />
because the other agents undergo only minimal<br />
transformation. <strong>The</strong> loss of hepatic tissue with age may<br />
be associated with decreased metabolism of the volatile<br />
agents, but this is not documented. If decreased metabolism<br />
of these drugs occurs, it is probably not clinically<br />
significant.<br />
Volatile anesthetic agents have a variable effect on<br />
liver function. Sevoflurane decreases production of fibrinogen,<br />
transferrin, and albumin in cultured hepatocytes<br />
more than exposure to halothane, isoflurane, or enflurane<br />
does. 80 However, enflurane causes greater depression of<br />
albumin synthesis than sevoflurane. <strong>The</strong> effects of desflurane<br />
on hepatic synthesis are not known. It is not anticipated<br />
that it would have much effect because so little of<br />
it is metabolized. 81<br />
Many drugs bind to plasma proteins, and several intravenous<br />
anesthetic drugs are carried in the blood bound<br />
to plasma proteins. Albumin is a carrier for many drugs,<br />
and low blood concentrations of albumin are frequently<br />
encountered in elderly patients. This probably contributes<br />
to the exaggerated effects of many drugs in older<br />
subjects because of the greater fraction of unbound free<br />
drug. <strong>The</strong>re is no evidence suggesting that volatile agents<br />
rely on protein binding for transport or that the increased<br />
sensitivity to volatile anesthetics works through this<br />
mechanism.
17. Inhalational Anesthetics 257<br />
<strong>The</strong> Pharmacodynamics of Inhalational<br />
Agents in the Elderly<br />
<strong>The</strong> introduction of halogenated ethers with progressively<br />
lower solubility characterizes the era of modern<br />
agents. As the solubility of newer agents approaches that<br />
of nitrous oxide, the result is a more rapid uptake and<br />
faster elimination of the drug. <strong>The</strong>oretically, low solubility<br />
and faster uptake also allow greater control of anesthetic<br />
blood levels during the maintenance phase of anesthesia.<br />
Faster elimination with low-solubility agents should<br />
provide for a rapid emergence from anesthesia. Inhalational<br />
agents used for general anesthesia include isoflurane,<br />
sevoflurane, desflurane, halothane, and enflurane.<br />
For practical purposes, the first three warrant most consideration<br />
because they represent the majority of volatile<br />
agents used. <strong>The</strong> properties of the inhalational agents are<br />
found in Table 17-1.<br />
Aging and the Minimal Alveolar<br />
Concentration<br />
<strong>The</strong> classic expression of pharmacodynamic effect for volatile<br />
anesthetic agents is the MAC. MAC is the minimal<br />
alveolar concentration of a volatile drug at 1 atm that prevents<br />
movement in 50% of subjects following surgical incision.<br />
82 <strong>The</strong> concentrations of volatile agents defined by<br />
MAC values are usually not enough for adequate anesthesia<br />
during surgical cases. Frequently, about 1.3 times MAC,<br />
or essentially an ED 95 dose of anesthetic, is needed. 83<br />
For adult subjects, the MAC is 1.15% for isoflurane, 6%<br />
for desflurane, and 1.85% for sevoflurane. As patients<br />
age, MAC decreases for all the volatile drugs, generally<br />
occurring at approximately 6% per decade. 84 <strong>The</strong> decrease<br />
in drug requirement does not follow a linear relationship<br />
but accelerates after 40–50 years of age. This phenomenon<br />
also applies to intravenous anesthetic drugs in which<br />
the pharmacokinetics of injected drugs changes substantially<br />
with age. 85 Guedel 86 was the first to note that inhalational<br />
anesthetic requirements decrease with age. This<br />
has subsequently been documented for halothane, 87 isoflurane,<br />
88 enflurane, desflurane, 89,90 and sevoflurane. 91 <strong>The</strong><br />
mathematic relationship of MAC, age, end-expired concentration<br />
of anesthetic agent, and the contribution by<br />
nitrous oxide has been determined. 92 A nomogram for<br />
estimating age-related changes in MAC is available<br />
(Figure 17-11).<br />
Martin et al. 93 reviewed the use of the most common<br />
anesthetic drug combinations for general anesthesia.<br />
Age (yr)<br />
100<br />
90<br />
80<br />
70<br />
60<br />
50<br />
40<br />
30<br />
20<br />
10<br />
1<br />
Sevoflurane in 87% nitrous oxide for a 3-yr-old<br />
© JGC lerou, 2003<br />
Total MAC<br />
(MAC units)<br />
1.8<br />
1.6<br />
1.4<br />
1.2<br />
1.0<br />
0.8<br />
Turning axis<br />
0.6<br />
0.4<br />
0.2<br />
Sevoflurane<br />
Enflurane<br />
Desflurane<br />
Isoflurane<br />
Halothane<br />
0% 50% 67% nitrous oxide<br />
End-expired concentration (% atm)<br />
Desflurane Other agents<br />
0.0<br />
20 19 18 17 16 15 14 13 12 11 10 9 8 7 6 5 4 3 2 1 0<br />
0.2<br />
0.4<br />
0.6<br />
0.8<br />
1.0<br />
1.2<br />
1.4<br />
1.6<br />
1.8<br />
2.0<br />
2.2<br />
2.4<br />
2.6<br />
2.8<br />
3.0<br />
3.2<br />
3.4<br />
3.6<br />
3.8<br />
4.0<br />
End-expired concentration of halothane, isoflurane,<br />
enflurane or sevoflurane<br />
Figure 17-11. Nomogram relating age, total minimal alveolar<br />
concentration (MAC) expressed in MAC units, and end-expiratory<br />
concentrations of volatile agent and nitrous oxide. A result<br />
is found by drawing two straight lines. Example (dotted lines):<br />
if the measured end-expired concentrations of sevoflurane and<br />
nitrous oxide are 1.8% and 67% (at 1 atm), respectively, then<br />
the total age-related MAC is 1.3 in a 3-year-old. Reverse<br />
example: a total MAC of 1.3 in a 3-year-old, when using sevoflurane<br />
and nitrous oxide 67% in oxygen, requires an endexpired<br />
sevoflurane concentration of 1.8%. (Reprinted with<br />
permission from Lerou. 92 )
258 G.R. Haynes<br />
Isoflurane<br />
Residual<br />
0.02<br />
0.00<br />
–0.02<br />
–0.04<br />
–0.06<br />
–0.08<br />
–0.10<br />
–0.12<br />
30 40 50 60 70 80<br />
Age<br />
Group<br />
IFNPM<br />
IFNT<br />
IFNTM<br />
Figure 17-12. <strong>The</strong> trend in reduction of isoflurane concentration<br />
with age. Compared with maximum values at age 30, there<br />
is an 11%–16% reduction in isoflurane requirement by age 80.<br />
IFNTM, isoflurane, fentanyl, nitrous oxide, thiopental, midazolam;<br />
IFNPM, isoflurane, fentanyl, nitrous oxide, propofol,<br />
midazolam; IFNT, isoflurane, fentanyl, nitrous oxide, thiopental.<br />
(Reprinted with permission from Martin et al. 93 )<br />
When controlling for the synergistic interaction of intravenous<br />
and inhalational agents, the authors demonstrated<br />
a decrease in drug requirements for 80-year-old patients.<br />
<strong>The</strong> decrease was not the same for drugs of different<br />
classes. <strong>The</strong> utilization of intravenous drugs decreased<br />
30%–50%, whereas the requirement for isoflurane<br />
decreased only 11%–26% (Figure 17-12). Although older<br />
patients do not require as much anesthetic drug, there is<br />
little known that explains the decreased requirement of<br />
inhalational anesthetics.<br />
MAC is a value that provides a way to compare<br />
the potency of inhalational anesthetic agents on a specific<br />
endpoint. Depth of anesthesia is one endpoint of interest.<br />
Other endpoints have received less attention in the aged<br />
patient. This is generally one third the MAC value except<br />
in the case of halothane, for which MAC awake is 0.55 MAC.<br />
MAC awake decreases with age. 94 <strong>The</strong> MAC-BAR is the<br />
MAC of agent that inhibits a sympathetic nervous system<br />
response such as tachycardia or hypertension when subjects<br />
are stimulated. It is expressed as a multiple of the<br />
MAC (Table 17-4). However, there is no information on<br />
the concentration of volatile agent needed to attenuate<br />
autonomic reflexes (MAC-BAR) with increasing age.<br />
<strong>The</strong>re are several possible explanations of how<br />
age decreases the inhalational anesthetic requirements.<br />
Several changes contribute to this change: an increase in<br />
body fat; reductions in metabolism, reduced cardiac<br />
output, decreased drug clearance; and atrophy of organ<br />
systems, particularly the central nervous system. 95 A combination<br />
of factors probably accounts for the decreased<br />
dose of hypnotic drugs needed for loss of consciousness<br />
and shifting the electroencephalogram pattern. 96–98 Several<br />
factors associated with increasing and decreasing MAC<br />
are listed in Tables 17-5 and 17-6. Factors not associated<br />
with a change in MAC are listed in Table 17-7.<br />
Drugs frequently used in the elderly influence the<br />
effective dose of volatile agents. <strong>The</strong>se include calcium<br />
channel blockers 99 and clonidine. 100 Some drugs may<br />
affect MAC by depletion of neurotransmitters. 101,102 Benzodiazepines<br />
and opioids have an additive effect with<br />
volatile anesthetic agents. 43<br />
Slow emergence and prolonged sedation in the recovery<br />
room are usually regarded as detrimental for elderly<br />
patients. Postoperative sedation occurs in approximately<br />
10% of elderly general surgery patients. Among elderly<br />
patients, the incidence of postoperative sedation after<br />
general anesthesia can be as high as 61% for those having<br />
emergency surgery. Intraoperative hypotension and anesthetic<br />
drugs contribute to postoperative sedation and<br />
longer hospitalization. 103<br />
<strong>The</strong> physical properties of the inhalational anesthetics<br />
contribute to the speed of action and resolution of these<br />
Table 17-4. Clinical properties of volatile anesthetic agents in routine use.<br />
MAC [atm, (%)] at various ages*<br />
MAC‡§<br />
2–5 years† 36–49 years† 65 years† MAC awake MAC awake /MAC MAC-BAR<br />
N 2 O 1.04 0.68 0.64 —<br />
Halothane 0.0041 0.55 1.3<br />
Isoflurane 0.0160 (1.6) 0.0115 (1.15) 0.0105 (1.05) 0.0049 0.38 1.3<br />
Desflurane 0.0854 (8.54) 0.0600 (6) 0.0517 (5.17) 0.025 0.34 1.45<br />
Sevoflurane 0.0250 (2.5) 0.0185 (1.85) 0.0177 (1.77) 0.0062 0.34 2.24<br />
MAC = minimal alveolar concentration.<br />
*Data from Eger EI II, Eisenkraft JB, Weiskopf RB. <strong>The</strong> Pharmacology of Inhaled Anesthetics. Dannemiller Memorial Educational Foundation;<br />
2002:7–19.<br />
†Volatile agent delivered in oxygen without nitrous oxide.<br />
‡Values for subjects aged 20–60 years.<br />
§Data from Stevens WC, Kingston HCG. Inhalation anesthesia. In: Barash PG, et al. Clinical <strong>Anesthesia</strong>. 3rd ed. Philadelphia: Lippincott-Raven;<br />
1997:359–383.
17. Inhalational Anesthetics 259<br />
Table 17-5. Factors that increase minimal alveolar concentr -<br />
ation.<br />
Increased central neurotransmitters<br />
• Monoamine oxidase inhibitors<br />
• Acute dextroamphetamine use<br />
• Cocaine ingestion<br />
• Ephedrine<br />
• Levodopa<br />
Hyperthermia<br />
Chronic ethanol abuse<br />
Hypernatremia<br />
Source: Modified with permission from Ebert TJ, Schmid PG. Inhalation<br />
anesthesia. In: Barash PG, Cullen BF, Stoelting RK, eds. Clinical<br />
<strong>Anesthesia</strong>. 4th ed. Philadelphia: Lippincott Williams & Wilkins;<br />
1997:389.<br />
drugs. <strong>The</strong> blood level of agents with low blood/gas<br />
and blood/lipid solubility changes rapidly in response to<br />
varying the administered dose. At the conclusion of<br />
general anesthesia, the resolution of the hypnotic effect<br />
resolves faster with these agents. Faster emergence from<br />
general anesthesia is an important way to minimize postoperative<br />
complications in the elderly. Reports indicate<br />
faster emergence from anesthesia and shorter time spent<br />
in the PACU with desflurane. 29<br />
Table 17-6. Factors that decrease minimal alveolar<br />
concentration.<br />
Metabolic acidosis<br />
Hypoxia (PaO 2 < 38 mm Hg)<br />
Hypotension (mean arterial pressure < 50 mm Hg)<br />
Decreased central neurotransmitters (alpha methyldopa, reserpine,<br />
chronic dextroamphetamine use, levodopa)<br />
Clonidine<br />
Hypothermia<br />
Hyponatremia<br />
Lithium<br />
Hypoosmolality<br />
Pregnancy<br />
Acute ethanol use<br />
Ketamine<br />
Pancuronium<br />
Physostigmine (10 times clinical doses)<br />
Neostigmine (10 times clinical doses)<br />
Lidocaine<br />
Opioids<br />
Opioid agonist-antagonist analgesics<br />
Barbiturates<br />
Chlorpromazine<br />
Diazepam<br />
Hydroxyzine<br />
∆-9-Tetrahydrocannabinol<br />
Verapamil<br />
Source: Modified with permission from Ebert TJ, Schmid PG. Inhalation<br />
anesthesia. In: Barash PG, Cullen BF, Stoelting RK, eds. Clinical<br />
<strong>Anesthesia</strong>. 4th ed. Philadelphia: Lippincott Williams & Wilkins;<br />
1997:389.<br />
Table 17-7. Factors that do not reduce minimal alveolar<br />
concentration.<br />
Duration of anesthesia<br />
Type of stimulation<br />
Gender<br />
Hypocarbia (Paco 2 to 21 mm Hg)<br />
Hypercarbia (Paco 2 to 95 mm Hg)<br />
Metabolic alkalosis<br />
Hyperoxia<br />
Isovolemic anemia (hematocrit to 10%)<br />
Arterial hypertension<br />
Thyroid function<br />
Magnesium<br />
Hyperkalemia<br />
Hyperosmolality<br />
Propranolol<br />
Isoproterenol<br />
Promethazine<br />
Naloxone<br />
Aminophylline<br />
Source: Modified with permission from Stevens WC, Kingston HG.<br />
Inhalational anesthesia. In: Barash PG, ed. Clinical <strong>Anesthesia</strong>.<br />
Philadelphia: JB Lippincott; 1992:443.)<br />
Cardiovascular Actions of Inhalational Agents<br />
in the Elderly<br />
<strong>The</strong> elderly patient’s heart and vascular system are<br />
anatomically and functionally different from younger<br />
patients. <strong>The</strong> most striking are a decrease in the maximum<br />
heart rate response to exercise, decreased sensitivity<br />
to catecholamines, increased pulmonary artery, and left<br />
ventricular diastolic filling pressures. 104–107 Determining<br />
whether these changes are a direct result of aging and if<br />
they can be modified are current issues. Both mechanisms<br />
of aging in the cardiovascular system and lifestyle<br />
undoubtedly have a role in these changes. 108<br />
<strong>The</strong> physiologic response of elderly patients during<br />
anesthesia must be evaluated carefully because impressions<br />
about how elderly patients will respond may be<br />
incorrect. For example, Joris et al. 109 found that cardiac<br />
index decreases significantly in young patients when<br />
abdominal insufflation impairs venous return to the right<br />
side of the heart. Because cardiovascular changes inevitably<br />
occur with age, it is reasonable to expect greater<br />
hemodynamic changes in elderly patients. However, the<br />
response of elderly patients may be better than expected.<br />
In patients over age 75 years, the cardiac function<br />
decreased with induction of general anesthesia with<br />
isoflurane and nitrous oxide. But during laparoscopic<br />
cholecystectomy, the cardiac performance increased and<br />
blood pressure returned to preanesthetic levels with the<br />
onset of surgery. Surprisingly, elderly patients tolerated<br />
the decreased preload and increased afterload from<br />
abdominal insufflation rather well. 110<br />
Hemodynamic changes during general anesthesia in<br />
sicker American Society of Anesthesiologists (ASA)
260 G.R. Haynes<br />
physical status 3 and 4 patients are similar to changes<br />
in healthier ASA 1 and 2 patients. 111–117 Inhalation<br />
anesthesia produces a dose-dependent decrease in<br />
blood pressure and depression of the cardiovascular<br />
system. 118–121 Volatile anesthetics reduce blood pressure<br />
by reducing cardiac output and vasodilatation.<br />
Inhalation anesthetics affect cardiac systolic function.<br />
Depression of myocardial contractility in the elderly<br />
varies with the inhalational agent. Isoflurane does<br />
not maintain the cardiac output in older patients as<br />
it does in younger individuals during anesthesia. 120<br />
<strong>The</strong> addition of nitrous oxide to isoflurane helps maintain<br />
the cardiac index; however, its ability to maintain<br />
myocardial contractility is inconsistent. <strong>The</strong>re are reports<br />
suggesting nitrous oxide both helps maintain 122 and<br />
depresses 123 myocardial contractility when combined with<br />
halothane.<br />
Inhalational anesthetics also affect diastolic function.<br />
Myocardial relaxation has two components: an energydependent<br />
active component and a passive component,<br />
influenced by myocardial stiffness. In patients over the<br />
age of 60, halothane and isoflurane decrease the early,<br />
energy-dependent component of left ventricle relaxation,<br />
and the effect is greater with isoflurane. 124<br />
<strong>The</strong> cardiac status of the elderly patient is a significant<br />
factor in determining the response to inhalational anesthetics.<br />
For instance, healthy elderly surgical patients with<br />
well-controlled hypertension tolerate inhalational induction<br />
of general anesthesia with sevoflurane. Whether<br />
receiving sevoflurane as a rapidly delivered bolus (8% for<br />
3 minutes) or in a graded manner (8% initially with 2%<br />
incremental decreases until reaching 2%), patients with<br />
good pump function tolerate the induction with no change<br />
in heart rate, no electrocardiographic evidence of ischemia,<br />
and moderate decreases in blood pressure. <strong>The</strong><br />
decrease in blood pressure when using incremental<br />
decreases of sevoflurane compared with maintaining the<br />
same concentration throughout the induction was less<br />
than that encountered when using low-dose sevoflurane<br />
and propofol in combination. 125<br />
Blood pressure decreases significantly with the ad -<br />
ministration of inhalational anesthetics to patients with<br />
diminished cardiac function. 126 In patients with congestive<br />
heart failure, blood pressure and cardiac index<br />
decrease during isoflurane anesthesia. <strong>The</strong> decrease is<br />
greater with halothane in those patients with poor left<br />
ventricle function. 127 <strong>The</strong> catecholamine blocking effect<br />
of the inhalational agents may have a role in the hypotension<br />
encountered in these settings.<br />
<strong>The</strong> inhalational anesthetics have a variable effect on<br />
heart rate. Isoflurane decreases systemic blood pressure<br />
in both young and old subjects. However, isoflurane<br />
decreases the cardiac index and heart rate in elderly subjects<br />
whereas it increases the heart rate and leaves the<br />
cardiac index unchanged in young individuals. Thus, isoflurane<br />
seems to maintain the cardiac index in younger<br />
patients through increases in heart rate whereas this does<br />
not happen in older patients. Sevoflurane produces a<br />
dose-dependent increase in heart rate when given to<br />
normal, healthy volunteers. 128 In contrast, the heart rate<br />
shows no significant change during induction with either<br />
4% or 8% sevoflurane. 129 Halothane and enflurane have<br />
little effect on heart rate in elderly patients. 130 <strong>The</strong>re is no<br />
difference in the heart rate during the initial period after<br />
induction of anesthesia when using halothane. With isoflurane<br />
anesthesia, elderly patients have a lower heart<br />
rate compared with younger subjects. 120,131<br />
Inhalational anesthetics also influence the cardiovascular<br />
system indirectly through actions on the autonomic<br />
nervous system. Rapid increases above 1 MAC in<br />
the inspired concentration of isoflurane and desflurane<br />
trigger transient sympathetic stimulation. <strong>The</strong>re is a<br />
brief period of hypertension and tachycardia that is more<br />
pronounced with desflurane. 33 This action is apparently<br />
mediated through rapidly adapting airway receptors.<br />
Fentanyl and alpha- and beta-adrenergic blocking drugs<br />
easily block the effect. 132,133 Although this phenomenon<br />
was studied in subjects in their early twenties, elderly<br />
patients have a higher state of sympathetic nervous<br />
system activity and it is likely this action may be more<br />
pronounced.<br />
Inhalational anesthetics may have a delayed inhibition<br />
of hemodynamic control. Patients having a carotid endarterectomy<br />
with isoflurane anesthesia required more<br />
phenylephrine for blood pressure support and needed<br />
more labetalol during emergence to manage hypertension<br />
than did patients receiving propofol for general<br />
anesthesia. More significantly, although there was no difference<br />
in hemodynamic stability between patients anesthetized<br />
with isoflurane or propofol, patients anesthetized<br />
with isoflurane experienced significantly more frequent<br />
myocardial ischemia. 134<br />
Volatile anesthetics typically cause peripheral vasodilatation.<br />
<strong>The</strong> expected consequence is greater blood<br />
flow if cardiac output can be maintained or increased.<br />
However, there is a distinct, age-related difference in<br />
peripheral blood flow between young (18–34 years)<br />
and healthy elderly (60–79 years) subjects during the<br />
induction of general anesthesia. When receiving either<br />
isoflurane or halothane in combination with 66% nitrous<br />
oxide, there is a slight difference in changes of heart rate<br />
or mean blood pressure between the age groups. <strong>The</strong><br />
perfusion of skin and muscle, assessed by forearm<br />
blood flow, decreases along with the mean arterial blood<br />
pressure during anesthesia with halothane, and there<br />
is no age-related difference. However, with isoflurane<br />
anesthesia, the peripheral perfusion is maintained in<br />
young patients even though the blood pressure de -<br />
creases whereas the perfusion decreases in the elderly<br />
(Figure 17-13). 135
17. Inhalational Anesthetics 261<br />
Heart rate during induction of anesthesia, isoflurane<br />
plus 66% nitrous oxide<br />
120<br />
Heart rate during induction of anesthesia, halothane<br />
plus 66% nitrous oxide<br />
120<br />
Heart rate (beats/min)<br />
100<br />
80<br />
60<br />
40<br />
20<br />
Heart rate (beats/min)<br />
100<br />
80<br />
60<br />
40<br />
20<br />
0<br />
Awake Ind + 1 Intub +<br />
1<br />
Agnt +<br />
5<br />
Agnt +<br />
10<br />
Agnt +<br />
15<br />
Agnt +<br />
20<br />
0<br />
Awake Ind + 1 Intub +<br />
1<br />
Agnt +<br />
5<br />
Agnt +<br />
10<br />
Agnt +<br />
15<br />
Agnt +<br />
20<br />
Mean arterial blood pressure during induction of<br />
anesthesia, isoflurane plus 66% nitrous oxide<br />
Mean arterial blood pressure during induction of<br />
anesthesia, halothane plus 66% nitrous oxide<br />
160<br />
160<br />
Mean arterial BP (mm Hg)<br />
140<br />
120<br />
100<br />
80<br />
60<br />
40<br />
20<br />
Mean arterial BP (mm Hg)<br />
140<br />
120<br />
100<br />
80<br />
60<br />
40<br />
20<br />
0<br />
Awake Ind + 1 Intub + Agnt + Agnt +<br />
1 5 10<br />
Agnt +<br />
15<br />
Agnt +<br />
20<br />
0<br />
Awake Ind + 1 Intub +<br />
1<br />
Agnt + Agnt +<br />
5 10<br />
Agnt +<br />
15<br />
Agnt +<br />
20<br />
Forearm blood flow during induction of anesthesia,<br />
isoflurane plus 66% nitrous oxide<br />
Forearm blood flow during induction of<br />
anesthesia, halothane plus 66% nitrous oxide<br />
6<br />
6<br />
FBF (ml blood/100 ml tissue/min)<br />
5<br />
4<br />
3<br />
2<br />
1<br />
FBF (ml blood/ 100 ml tissue/min)<br />
5<br />
4<br />
3<br />
2<br />
1<br />
0<br />
Awake Ind + 1 Intub +<br />
1<br />
Agnt +<br />
5<br />
Agnt +<br />
10<br />
Agnt +<br />
15<br />
Agnt +<br />
20<br />
0<br />
Awake Ind + 1 Intub + Agnt + 5 Agnt +<br />
1<br />
10<br />
Agnt +<br />
15<br />
Agnt +<br />
20<br />
Figure 17-13. Heart rate, mean arterial blood pressure, and<br />
forearm blood flow measured following the induction of general<br />
anesthesia in healthy young and elderly subjects. Patients<br />
received isoflurane (0.8%–1.2%) or halothane (0.7%–1.0%) and<br />
nitrous oxide (66%) after induction with etomidate and endotracheal<br />
intubation. Little difference in the change of heart rate<br />
or blood pressure was found between subject groups. Forearm<br />
blood flow decreased in older and younger patients receiving<br />
halothane whereas it was much greater in young patients receiving<br />
iso flurane. Mean values are shown. Light gray bars = young<br />
(18–34 years), dark gray bars = elderly (60–79 years). Time units<br />
are in minutes. (Data from Dwyer and Howe. 135 )
262 G.R. Haynes<br />
Summary<br />
Much of the clinical literature on inhalational anesthetic<br />
agents during the past decade focused on trying to demonstrate<br />
the superiority of one agent over another. <strong>The</strong><br />
clinical issue is not that one agent is clearly better than<br />
another in all instances. Each agent can control the<br />
response to surgical stimulation during general anesthesia.<br />
<strong>The</strong> issues that matter are which drug is best, given<br />
the particular disease or pathophysiology of the patient,<br />
and to what degree do we suppress consciousness<br />
and autonomic responses. <strong>The</strong> growing interest in the<br />
relationship of depth of anesthesia to long-term survival<br />
raises the possibility that we should use cardiovascular<br />
drugs as adjuncts to control heart rate and blood<br />
pressure.<br />
Because of the limited number of publications describing<br />
how age affects anesthesia, extracting age-related<br />
data from studies that compare intravenous and in -<br />
halational agents is useful. In reviewing the anesthesia<br />
literature of the past decade, it is apparent there is a<br />
growing interest in the relationship between aging and<br />
general anesthesia. However, the limited knowledge<br />
regarding the influence age has on anesthesia is a cause<br />
for concern.<br />
References<br />
1. Luntz SP, Janitz E, Motsch J, Bach A, Martin E, Böttiger<br />
BW. Cost effectiveness and high patient satisfaction in the<br />
elderly: sevoflurane versus propofol anesthesia. Eur J<br />
Anesthesiol 2004;21:115–122.<br />
2. Carpenter RL, Eger EI II, Johnson BH, et al. A new<br />
concept in inhaled anesthetic pharmacokinetics [abstract].<br />
Anesth Analg 1984;64:197.<br />
3. Carpenter RL, Eger EI II, Johnson BH, et al. Pharmacokinetics<br />
of inhaled anesthetics in humans: measurements<br />
during and after simultaneous administration of enflurane,<br />
halothane, isoflurane, methoxyflurane, and nitrous oxide.<br />
Anesth Analg 1984;65:575–582.<br />
4. Weiskopf RB, Eger EI II. Comparing the costs of inhaled<br />
anesthetics. <strong>Anesthesiology</strong> 1993;79:1413–1418.<br />
5. Coetzee JF, Stewart LJ. Fresh gas flow is not the only<br />
determinant of volatile agent consumption: a multi-centre<br />
study of low-flow anesthesia. Br J Anaesth 2002;88:46–55.<br />
6. Avramov MN, Griffin JD, White PF. <strong>The</strong> effect of fresh gas<br />
flow and anesthetic technique on the ability to control acute<br />
hemodynamic responses during surgery. Anesth Analg 1998;<br />
87:666–670.<br />
7. Pump KK. Emphysema and its relation to age. Am Rev<br />
Resp Dis 1976;114:5–13.<br />
8. Kitamura H, Sawa T, Ikezono E. Postoperative<br />
hypoxemia—the contribution of age to the maldistribution<br />
of ventilation. <strong>Anesthesiology</strong> 1973;36:244–252.<br />
9. Ward RJ, Tolas AG, Benveniste RJ, Hansen JM, Bonica JJ.<br />
Effect of posture on normal arterial blood gas tensions in<br />
the aged. <strong>Geriatric</strong>s 1966;21:139–143.<br />
10. Wahba WM. Influence of aging on lung function—clinical<br />
significance of changes from age twenty. Anesth Analg<br />
1983;62:764–776.<br />
11. Pontoppdan H, Geffin B, Lowenstein E. Acute respiratory<br />
failure in the adult. N Engl J Med 1972;287:690–698.<br />
12. Crapo RO, Morris AH, Clayton PD, Nixon CR. Lung<br />
volumes in healthy nonsmoking adults. Bull Eur Physiopathol<br />
Respir 1982;18:419–425.<br />
13. Turner J, Mead J, Wohl M. Elasticity of human lungs in<br />
relation to age. J Appl Physiol 1968;25:644–671.<br />
14. Niewoehner DE, Kleinerman J. Morphologic basis of pulmonary<br />
resistance in the human lung and effects of aging.<br />
J Appl Physiol 1974;36:412–418.<br />
15. Cerveri I, Zoia MC, Fanfulla F, et al. Reference values<br />
of arterial oxygen tension in the middle-aged and elderly.<br />
Am J Respir Crit Care Med 1995;152:934–941.<br />
16. Eger EI II. Uptake and distribution. In: Miller RD, ed.<br />
<strong>Anesthesia</strong>. New York: Churchill Livingstone; 1990:85–<br />
104.<br />
17. Lu CC, Tsai CS, Ho ST, et al. Pharmacokinetics of sevoflurane<br />
uptake into the brain and body. Anaesthesia 2003;58:<br />
951–956.<br />
18. Muravchick S. <strong>Anesthesia</strong> for the elderly. In: Miller RE, ed.<br />
<strong>Anesthesia</strong>. New York: Churchill Livingstone; 1990:1977–<br />
1978.<br />
19. Guénard H, Marthan R. Pulmonary gas exchange in elderly<br />
subjects. Eur Respir J 1996;9:2573–2577.<br />
20. Sorbini CAA, Grassi V, Solinas SE, et al. Arterial oxygen<br />
tension in relation to age in healthy subjects. Respiration<br />
1968;25:3–13.<br />
21. Kronenberg R, Hamilton FN, Gabel R, et al. Comparison<br />
of three methods for quantitating respiratory response to<br />
hypoxia in man. Respir Physiol 1972;16:109–125.<br />
22. Eger EI II, Kellogg RH, Mines AH, et al. Influence of CO 2<br />
on ventilatory acclimatization to altitude. J Appl Physiol<br />
1968;24:607–615.<br />
23. Kronenberg RS, Drage CW. Attenuation of the ventilatory<br />
and heart rate responses to hypoxia and hypercapnia with<br />
aging in normal men. J Clin Invest 1973;52:1812–1819.<br />
24. Pedersen T, Eliasen K, Henriksen E. A prospective study<br />
of mortality associated with anaesthesia and surgery: risk<br />
indicators of mortality in hospital. Acta Anaesthesiol<br />
Scand 1990;34:176–182.<br />
25. McLeskey CH. <strong>Anesthesia</strong> for the geriatric patient. In:<br />
Barash PG, ed. Clinical <strong>Anesthesia</strong>. Philadelphia: JB<br />
Lippincott; 1992:1353–1387.<br />
26. Schocken DD. Epidemiology and risk factors for<br />
heart failure in the elderly. Clin Geriatr Med 2000;16:<br />
407–418.<br />
27. Senni M, Redfield MM. Heart failure with preserved<br />
systolic function. A different natural history? J Am Coll<br />
Cardiol 2001;38:1277–1282.<br />
28. Evans TI. <strong>The</strong> physiological basis of geriatric general anesthesia.<br />
Anaesth Intensive Care 1973;1:319–322.<br />
29. Hurley B, Roth S. Strength training in the elderly: effects<br />
on risk factors for age-related diseases. Sports Med 2000;<br />
30:244–268.<br />
30. Robergs R, Roberts S. Exercise Physiology: Exercise,<br />
Performance, and Clinical Applications. 1st ed. St. Louis:<br />
Mosby-Yearbook; 1997.
17. Inhalational Anesthetics 263<br />
31. Dinenno FA, Seals DR, DeSouza CA, Tanaka H. Agerelated<br />
decreases in basal limb blood flow in humans: time<br />
course, determinants and habitual exercise effects. J Physiol<br />
2001;531:573–579.<br />
32. Hagberg JM, Allen WK, Seals DR, Hurley BF, Ehsani AA,<br />
Holloszy JO. A hemodynamic comparison of young and<br />
older endurance athletes during exercise. J Appl Physiol<br />
1985;58:2041–2046.<br />
33. Weiskopf RB, Moore MA, Eger EI II, et al. Rapid increase<br />
in desflurane concentration is associated with greater transient<br />
cardiovascular stimulation than with rapid increase<br />
in isoflurane concentration in humans. <strong>Anesthesiology</strong><br />
1994;80:1035–1045.<br />
34. Guo SS, Zeller C, Chumlea WC, Siervogel RM. Aging,<br />
body composition, and lifestyle: the Fels Longitudinal<br />
Study. Am J Clin Nutr 1999;79:405–411.<br />
35. Hughes VA, Frontera WR, Roubenoff R, et al. Longitudinal<br />
changes in body composition in older men and women:<br />
role of body weight change and physical activity. Am J Clin<br />
Nutr 2002;76:473–481.<br />
36. Arner P. Not all fat is alike. Lancet 1998;351:1301–1302.<br />
37. Wissing H, Kulin I, Riebrock, Fuhr U. Pharmacokinetics<br />
of inhaled anesthetics in a clinical setting: comparison of<br />
desflurane, isoflurane and sevoflurane. Br J Anaesth<br />
2000;84:443–449.<br />
38. Stevens WC, Cromwell TH, Halsey MJ, et al. <strong>The</strong> cardiovascular<br />
effects of a new inhalational anesthetic, Forane,<br />
in human volunteers at a constant arterial carbon dioxide<br />
tension. <strong>Anesthesiology</strong> 1971;35:8–16.<br />
39. Juvin P, Servin F, Giraud O, Desmonts JM. Emergence of<br />
elderly patients from prolonged desflurane, isoflurane, or<br />
propofol anesthesia. Anesth Analg 1997;85:647–651.<br />
40. Haevner JE, Kaye AE, Lin B-K, King T. Recovery of<br />
elderly patients from two or more hours of desflurane or<br />
sevoflurane anaesthesia. Br J Anaesth 2003;91:502–506.<br />
41. Hollenberg NK, Adams DF, Solomon HS, Rashid A,<br />
Abrams HL, Merrill JP. Senescence and the renal vasculature<br />
in normal man. Circ Res 1974;34:309–316.<br />
42. Lindeman RD, Tobin J, Shock NW. Longitudinal studies on<br />
the rate of decline in renal function with age. J Am Geriatr<br />
Soc 1985;33:278–285.<br />
43. Beck LH. <strong>The</strong> aging kidney: defending a delicate balance<br />
of fluid and electrolytes. <strong>Geriatric</strong>s 2000;55:26–28, 31–32.<br />
44. Mazze RJ, Trudell JR, Cousins MJ. Methoxyflurane metabolism<br />
and renal dysfunction: clinical correlation in man.<br />
<strong>Anesthesiology</strong> 1971;35:247–260.<br />
45. Aronson S. Renal function monitoring. In: Miller RD, ed.<br />
<strong>Anesthesia</strong>. Philadelphia: Churchill Livingstone; 2005:1489.<br />
46. Crandell WB, Pappas SC, MacDonald A. Nephrotoxicity<br />
associated with methoxyflurane anesthesia. <strong>Anesthesiology</strong><br />
1966;27:591–607.<br />
47. Baden JM, Rice SA. Metabolism and toxicity. In: Miller<br />
RD, ed. <strong>Anesthesia</strong>. New York: Churchill Livingstone;<br />
1990:155–170.<br />
48. FDA Prescribing Information: Sevoflurane. North Chicago,<br />
IL: Abbott Laboratories; Ref. 06–9230-RZ. Rev. June,<br />
1995.<br />
49. Cousins MJ, Mazze RI. Methoxyflurane nephrotoxicity:<br />
a study of the dose response in man. JAMA 1973;225:<br />
1611–1616.<br />
50. Cittanova ML, Lelongt B, Verpont MC, et al. Fluoride ion<br />
toxicity in human kidney collecting duct cells. <strong>Anesthesiology</strong><br />
1996;84:428–435.<br />
51. Kharasch ED, Armstrong AS, Gunn K, Artru A, Cox K,<br />
Karol MD. Clinical sevoflurane metabolism and disposition.<br />
II. <strong>The</strong> role of cytochrome P450 2E1 in fluoride and<br />
hexafluoroisopropanol formation. <strong>Anesthesiology</strong> 1995;<br />
82(6):1379–1388.<br />
52. Kharason ED, Karol MD, Lanni C, Sawchuk R. Clinical<br />
sevoflurane metabolism and disposition. I. Sevoflurane<br />
and metabolite pharmacokinetics. <strong>Anesthesiology</strong> 1995;82:<br />
1369–1378.<br />
53. Gentz BA, Malan TPJ. Renal toxicity with sevoflurane: a<br />
storm in a teacup? Drugs 2001;61:2155–2162.<br />
54. Frink EJ, Malan TP, Isner J, et al. Renal concentrating function<br />
with prolonged sevoflurane or enflurane anesthesia in<br />
volunteers. <strong>Anesthesiology</strong> 1994;80:1019–1025.<br />
55. Mazze RI, Sievenpiper TS, Stevenson J. Renal effects of<br />
enflurane and halothane in patients with abnormal renal<br />
function. <strong>Anesthesiology</strong> 1984;60:161–163.<br />
56. Conzen PF, Nuscheler M, Melotte A, et al. Renal function<br />
and serum fluoride concentrations in patients with stable<br />
renal insufficiency after anesthesia with sevoflurane or<br />
enflurane. Anesth Analg 1995;81:569–575.<br />
57. Koblin DD, Eger EI II, Johnson BH, et al. I-653 resists<br />
degradation in rats. Anesth Analg 1988;67:534–538.<br />
58. Frink EJ Jr, Malan T, Morgan S, et al. Quantification of the<br />
degradation products of sevoflurane in two CO 2 absorbents<br />
during low-flow anesthesia in surgical patients.<br />
<strong>Anesthesiology</strong> 1992;77:1064–1069.<br />
59. Eger EI II, Sturm DP. <strong>The</strong> absorption and degradation of<br />
isoflurane and I653 by dry soda lime at various temperatures.<br />
Anesth Analg 1987;66:1312–1315.<br />
60. Munday I, Foden N, Ward P, et al. Sevoflurane degradation<br />
in a circle system at two different fresh gas flows. <strong>Anesthesiology</strong><br />
1994;81:A433.<br />
61. Bito H, Ikede K. Closed-circuit anesthesia with sevoflurane<br />
in humans. Effects on renal and hepatic function and<br />
concentrations of breakdown products with soda lime in<br />
the circuit. <strong>Anesthesiology</strong> 1994;80:71–76.<br />
62. Bito H, Ikeda K. Degradation products of sevoflurane<br />
during low-flow anaesthesia. Br J Anaesth 1995;74:56–<br />
59.<br />
63. Kharasch ED, Frink EJ, Zager R, Bowdle TA, Artru A,<br />
Nogami WM. Assessment of low-flow sevoflurane and isoflurane<br />
effects on renal function using sensitive markers of<br />
tubular toxicity. <strong>Anesthesiology</strong> 1997;86:1238–1253.<br />
64. Frink EJ Jr, Isner RJ, Malan TP Jr, Morgan SE, Brown EA,<br />
Brown BR Jr. Sevoflurane degradation product concentrations<br />
with soda lime during prolonged anesthesia. J Clin<br />
Anaesth 1994;6:239–242.<br />
65. Bito H, Ikeda K. Renal and hepatic function in surgical<br />
patients after low-flow sevoflurane or isoflurane anesthesia.<br />
Anesth Analg 1996;82:173–176.<br />
66. Tsukamoto N, Hirabayashi Y, Shimizu R, Mitsuhata H. <strong>The</strong><br />
effects of sevoflurane and isoflurane anesthesia on renal<br />
tubular function in patients with moderately impaired<br />
renal function. Anesth Analg 1996;82:909–913.<br />
67. Higuchi H, Adachi Y, Wada H, Kanno M, Satoh T. <strong>The</strong><br />
effects of low-flow sevoflurane and isoflurane anesthesia
264 G.R. Haynes<br />
on renal function in patients with stable moderate renal<br />
insufficiency. Anesth Analg 2001;92:650–655.<br />
68. Vestal RE. Drug use in the elderly: a review of problems and<br />
special considerations [review]. Drugs 1978;16:358–382.<br />
69. Muravchick S. <strong>The</strong> aging patient and age related disease.<br />
ASA Annual Refresher Course Lecture #151. Park Ridge,<br />
IL: American Society of Anesthesiologists; 1987.<br />
70. Carleden CM, Kaye CM, Parsons RL. <strong>The</strong> effect of age on<br />
plasma levels of propranolol and practolol in man. Br J<br />
Clin Pharmacol 1975;2:303–306.<br />
71. Woodhouse KW, Mutch E, Williams FM, Rawlins MD,<br />
James OE. <strong>The</strong> effect of age on pathways of drug metabolism<br />
in human liver. Age Ageing 1984;13:328–334.<br />
72. Rehder K, Forbes J, Alter H, et al. Halothane biotransformation<br />
in man: a quantitative study. <strong>Anesthesiology</strong> 1967;<br />
28:711–715.<br />
73. Carpenter RL, Eger EI II, Johnson BH, et al. <strong>The</strong> extent<br />
of metabolism of inhaled anesthetics in humans. <strong>Anesthesiology</strong><br />
1986;65:201–205.<br />
74. Koblin D, Weiskopf R, Holmes MA, et al. Metabolism of<br />
I-653 and isoflurane in swine. Anesth Analg 1989;68:147–<br />
149.<br />
75. Yasuda N, Lockhart S, Eger EI II, et al. Kinetics of desflurane,<br />
isoflurane, and halothane in humans. <strong>Anesthesiology</strong><br />
1991;74:489–498.<br />
76. Cascorbi HF, Blake DA, Helrish M. Differences in biotransformation<br />
of halothane in man. <strong>Anesthesiology</strong> 1970;<br />
32:119–123.<br />
77. Holaday DA, Fiserova-Bergerova V, Latto IP, et al. Resistance<br />
of isoflurane to biotransformation in man. <strong>Anesthesiology</strong><br />
1975;43:325–332.<br />
78. Koblin DD. Characteristics and implications of desflurane<br />
metabolism and toxicity. Anesth Analg 1992;75(4 Suppl):<br />
S10–S16.<br />
79. Sutton TS, Koblin DD, Fuenke LD, et al. Fluoride metabolites<br />
after prolonged exposure of volunteers and patients<br />
to desflurane. Anesth Analg 1991;73:180–185.<br />
80. Franks JJ, Kruskal JB, Holaday DA. Immediate depression<br />
of fibrinogen, albumin, and transferrin synthesis by halothane,<br />
isoflurane, sevoflurane and enflurane. <strong>Anesthesiology</strong><br />
1989;71:A238.<br />
81. Johnes RM. Desflurane and sevoflurane: inhalation anaesthetics<br />
for this decade? Br J Anaesth 1990;65:527–536.<br />
82. Saidman LJ, Eger EI II. Effect of nitrous oxide and of<br />
narcotic premedication on the alveolar concentration of<br />
halothane required for anesthesia. <strong>Anesthesiology</strong> 1964;25:<br />
302–306.<br />
83. deJong R, Eger EI II. MAC explained: AD 50 and AD 95<br />
values of common inhalational anesthetics in man.<br />
<strong>Anesthesiology</strong> 1975;42:384–389.<br />
84. Mapleson WW. Effect of age on MAC in humans: a metaanalysis.<br />
Br J Anaesth 1996;76:179–185.<br />
85. Shüttler J, Ihmsen H. Population pharmacokinetics of propofol.<br />
A multicenter study. <strong>Anesthesiology</strong> 2000;92:727–<br />
738.<br />
86. Guedel AE. Inhalation anesthesia: a fundamental guide.<br />
New York: Macmillan; 1937:61–62.<br />
87. Gregory GA, Eger EI II, Munson ES. <strong>The</strong> relationship<br />
between age and halothane requirement in man. <strong>Anesthesiology</strong><br />
1969;30:488–491.<br />
88. Stevens WC, Nolan WM, Gibbons RT, et al. Minimum<br />
alveolar concentrations (MAC) of isoflurane with and<br />
without nitrous oxide in patients of various ages. <strong>Anesthesiology</strong><br />
1975;42:197–200.<br />
89. Gold MI, Abello D, Herrington C. Minimum alveolar concentration<br />
of desflurane in patients older than 65 years.<br />
<strong>Anesthesiology</strong> 1993;79:710–714.<br />
90. Rampil J, Lockart S, Zwass M, et al. Clinical characteristics<br />
of desflurane in surgical patients: minimum alveolar concentration.<br />
<strong>Anesthesiology</strong> 1991;74:429–433.<br />
91. Nakajima R, Nakajima Y, Ikeda A. Minimum alveolar concentration<br />
of sevoflurane in elderly patients. Br J Anesth<br />
1993;70:273–275.<br />
92. Lerou JGC. Nomogram to estimate age-related MAC. Br<br />
J Anaesth 2004;93:288–291.<br />
93. Martin G, Glass PSA, Breslin DS, et al. A study of anesthetic<br />
drug utilization in different age groups. J Clin Anesth<br />
2003;15:194–200.<br />
94. Katoh T, Suguro Y, Kimura T, Ikeda K. Cerebral awakening<br />
concentration of sevoflurane and isoflurane predicted<br />
during slow and fast alveolar washout. Anesth Analg<br />
1993;77:1012–1017.<br />
95. Jones AG, Hunter JM. Anaesthesia in the elderly. Special<br />
considerations. Drugs Aging 1996;9:319–331.<br />
96. Avram MJ, Krejcie TC, Henthorn TK. <strong>The</strong> relationship of<br />
age to disposition of thiopental and indocyanine green.<br />
<strong>Anesthesiology</strong> 1990;72:403–411.<br />
97. Avram MJ, Sanghvi R, Henthorn TK, et al. Determinants<br />
of thiopental induction dose requirements. Anesth Analg<br />
1993;76:10–17.<br />
98. Kirkpatrick T, Cockshodt ID, Douglas EH, Nimmo WS.<br />
Pharmacokinetics of propofol (Diprivan) in elderly<br />
women. Br J Anaesth 1988;60:146–150.<br />
99. Schwartz AE, Maustisho FE, Bachus WW, et al. Nimodipine<br />
decreases the minimum alveolar concentration of isoflurane<br />
in dogs. Can J Anesth 1991;38:239–242.<br />
100. Nagasaka H, Yaksh TL. Pharmacology of intrathecal<br />
adrenergic agonists: cardiovascular and nociceptive<br />
reflexes in halothane-anesthetized rats. <strong>Anesthesiology</strong><br />
1990;73:1198–1207.<br />
101. Johnston RR, White PF, Way WL, et al. <strong>The</strong> effect of<br />
levodopa on halothane anesthetic requirements. Anesth<br />
Analg 1975;54:178–181.<br />
102. Miller RD, Way WL, Eger EI II. <strong>The</strong> effects of alphamethyl-dopa,<br />
reserpine, guanethidine, and iproniazid<br />
on minimum alveolar anesthetic requirement (MAC).<br />
<strong>Anesthesiology</strong> 1968;29:1153–1158.<br />
103. Gustafson Y, Berggren D, Brannstrom B, et al. Acute confusional<br />
states in elderly patients treated for femoral neck<br />
fracture. J Am Geriatr Soc 1988;36:525–530.<br />
104. Lakatta EG. Diminished beta-adrenergic modulation of<br />
cardiovascular function in advanced age. Cardiol Clin<br />
1986;4:185–200.<br />
105. Virtanen K, Janne J, Frick MH. Response of blood pressure<br />
and plasma norepinephrine to propranolol, metoprolol<br />
and clonidine during isometric and dynamic exercise in<br />
hypertensive patients. Eur J Clin Pharmacol 1982;21:<br />
275–279.<br />
106. Duncan AK, Vittone J, Fleming KC, Smith HC. Cardiovascular<br />
disease in elderly patients. 1996;71:184–196.
17. Inhalational Anesthetics 265<br />
107. Elliott HL, Sumner DJ, McLean K, Reid JL. Effect of age<br />
on the responsiveness of vascular alpha-adrenoceptors in<br />
man. 1982;4:388–392.<br />
108. Rodeheffer RJ, Gersten Glith G, Brecker LC, et al. Exercise<br />
cardiac output is maintained with advancing age in<br />
healthy human subjects: cardiac dilation and increased<br />
stroke volume compensate for diminished heart rate.<br />
Circulation 1984;69:203–213.<br />
109. Joris J, Honore P, Lamy M. Changes in oxygen transport<br />
and ventilation during laparoscopic cholecystectomy.<br />
Anesth Analg 1993;76:1067–1071.<br />
110. Dhoste K, Lacoste L, Karayan J, et al. Haemodynamic<br />
and ventilatory changes during laparoscopic cholecystectomy<br />
in elderly ASA III patients. Can J Anaesth 1996;8:<br />
783–788.<br />
111. Fox LG, Hein HAT, Gawey BJ, et al. Physiologic alterations<br />
during laparoscopic cholecystectomy in ASA III and<br />
IV patients. <strong>Anesthesiology</strong> 1993;79:A55.<br />
112. Feig BW, Berger DH, Dupuis JF, et al. Hemodynamic<br />
effects of CO 2 abdominal insufflation (CAI) during laparoscopy<br />
in high-risk patients. Anesth Analg 1994;78:S109.<br />
113. Safran D, Sgambati S, Orlando R III. Laparoscopy in highrisk<br />
cardiac patients. Surg Gynecol Obstet 1993;176:548–<br />
554.<br />
114. Critchley LAH, Critchley JAJH, Gin T. Haemodynamic<br />
changes in patients undergoing laparoscopic cholecystectomy:<br />
measurement by transthoracic electrical bioimpedance.<br />
Br J Anaesth 1993;70:681–683.<br />
115. Cunningham AJ, Turner J, Rosenbaum S, et al. Transoesophageal<br />
echocardiographic assessment of haemodynamic<br />
function during laparoscopic cholecystectomy. Br J<br />
Anaesth 1993;70:621–625.<br />
116. Joris JL, Noirot DP, Legrand MJ, et al. Hemodynamic<br />
changes during laparoscopic cholecystectomy. Anesth<br />
Analg 1993;76:1067–1071.<br />
117. McLaughlin JG, Bonnell BW, Scheeres DE, et al. <strong>The</strong><br />
adverse hemodynamic effects of laparoscopic cholecystectomy.<br />
Surg Endosc 1995;9:121–124.<br />
118. Roizen MF, Lampe GH, Sheiner LB, et al. Aging increase<br />
hemodynamic responses to induction and incision<br />
[abstract]. Anesth Analg 1985;64:275.<br />
119. Hoffman WE, Miletich DJ, Albrecht RF. Cardiovascular<br />
and regional blood flow changes during halothane anesthesia<br />
in the aged rat. <strong>Anesthesiology</strong> 1982;56:444–448.<br />
120. McKinney MS, Fee JP, Clarke RS. Cardiovascular effects<br />
of isoflurane and halothane in young and elderly patients.<br />
Br J Anaesth 1993;71:696–701.<br />
121. Haldermann G, Schmid E, Frey P, et al. Wirkung von<br />
ethrane auf die kreislaufgrossen geriatrischer patienten.<br />
Anaesthesist 1975;24:343–346.<br />
122. Martin WE, Freund FG, Hornbein RF, et al. Cardiovascular<br />
effects of halothane and halothane-nitrous oxide anesthesia<br />
during controlled ventilation. <strong>Anesthesiology</strong> 1969;<br />
30:346.<br />
123. McKinney MS, Fee JPH. Cardiovascular effects of<br />
50% nitrous oxide in older adult patients anesthetized<br />
with isoflurane or halothane. Br J Anaesth 1998;80:169–<br />
173.<br />
124. Houltz E, Caidahl K, Adin C, et al. Effects of halothane<br />
and isoflurane on left ventricular diastolic function during<br />
surgical stress in patients with coronary artery disease.<br />
Acta Anaesthesiol Scand 1997;41:931–938.<br />
125. Yamaguchi S, Ikeda T, Wake K, et al. A sevoflurane induction<br />
of anesthesia with gradual reduction of concentration<br />
is well tolerated in elderly patients. Can J Anesth 2003;<br />
50:26–31.<br />
126. Kemmotsu O, Hashimoto Y, Shimosato S. Inotropic effects<br />
of isoflurane on mechanics of contraction in isolated cat<br />
papillary muscles from normal and failing hearts. <strong>Anesthesiology</strong><br />
1973;39:470–477.<br />
127. Urzua J, Serra M, Lema G, et al. Comparison of isoflurane,<br />
halothane and fentanyl in patients with decreased ejection<br />
fraction undergoing coronary surgery. Anaesth Intensive<br />
Care 1996;24:579–584.<br />
128. Malan TP, DiNardo JA, Isner RJ, et al. Cardiovascular<br />
effects of sevoflurane compared with those of isoflurane in<br />
volunteers. <strong>Anesthesiology</strong> 1995;83:918–928.<br />
129. Walpole R, Logan M. Effect of sevoflurane concentration<br />
on inhalational induction of anesthesia in the elderly. Br J<br />
Anaesth 1999;82:20–24.<br />
130. Hilgenberg JC. Inhalation and intravenous drugs in the<br />
elderly. Semin Anesth 1986;5:44–53.<br />
131. Linde HW, Oh SO, Homi J, et al. Cardiovascular effects of<br />
isoflurane and halothane during controlled ventilation in<br />
older patients. Anesth Analg 1975;54:70–104.<br />
132. Weiskopf RB, Eger EI II, Noorani M, Daniel M. Repetitive<br />
rapid increases in desflurane concentration blunt transient<br />
cardiovascular stimulation in humans. <strong>Anesthesiology</strong><br />
1994;81:843–849.<br />
133. Weiskopf RB, Eger EI II, Noorani M, Daniel M. Fentanyl,<br />
esmolol, and clonidine blunt the transient cardiovascular<br />
stimulation induced by desflurane in humans. <strong>Anesthesiology</strong><br />
1994;81:1350–1355.<br />
134. Mutch WAC, White IWC, Donen N, et al. Haemodynamic<br />
instability and myocardial ischaemia during carotid endarterectomy:<br />
a comparison of propofol and isoflurane. Can J<br />
Anaesth 1995;42:577–587.<br />
135. Dwyer R, Howe J. Peripheral blood flow in the elderly<br />
during inhalational anesthesia. Acta Anesthesiol Scand<br />
1995;39:939–944.
18<br />
Relaxants and <strong>The</strong>ir Reversal Agents<br />
Cynthia A. Lien and Takahiro Suzuki<br />
Whether or not to maintain neuromuscular block in<br />
patients, young or elderly, is very much a matter of debate 1<br />
and is influenced by the type of anesthesia administered<br />
as well as the planned surgical procedure. Once the decision<br />
is made to administer a nondepolarizing neuromuscular<br />
blocking agent to an elderly patient, special<br />
consideration must be given to the potential for altered<br />
pharmacologic behavior in this patient population.<br />
A number of factors that accompany aging may affect<br />
the effect of nondepolarizing neuromuscular blocking<br />
agents in the geriatric patient. Because of skeletal muscle<br />
denervation, geriatric patients have a decrease in generalized<br />
muscle strength and coordination. Many alterations<br />
in the neuromuscular junction accompany aging. Additionally,<br />
decreased total body fluid and lean body mass,<br />
as well as decreased kidney function, cardiac output, and<br />
splanchnic blood flow may all affect the pharmacodynamics<br />
and kinetics of neuromuscular blocking agents.<br />
An increasing geriatric surgical population, coupled<br />
with constantly changing surgical trends and practices,<br />
mandates that nondepolarizing neuromuscular blocking<br />
agents, as well as anesthetics, are chosen based on<br />
their specific pharmacodynamic characteristics in aged<br />
patients.<br />
Changes in the Structure of the<br />
Neuromuscular Junction<br />
In people over the age of 60 years, the neuromuscular<br />
junction in skeletal muscle undergoes continuous degeneration<br />
and regeneration. <strong>The</strong> reorganization is primarily<br />
mediated through a reduction in the number of motor<br />
neurons in the spinal cord 2 and the ventral root fibers. 3<br />
Moreover, the number of motor units composed of a<br />
motor neuron and the innervated muscle fibers seems to<br />
decrease with aging. Because reinnervation does not<br />
compensate for the progressive neurogenic process,<br />
muscle fibers degenerate and are subsequently replaced<br />
with fat and fibrous tissue. A 25%–35% decrease in<br />
muscle mass is typically seen in the elderly 4 and is considered<br />
to be the result of both a loss of muscle fibers as<br />
well as a reduction in size of primarily type 2, or fasttwitch,<br />
fibers. 5 This is accompanied by a 50%–75%<br />
increase in body fat. 6 <strong>The</strong> loss of motor units is offset by<br />
an increase in the size of the motor unit. Because of this,<br />
an augmented twitch tension is evoked by stimulating a<br />
single motor nerve 7 in the aged.<br />
Aging is accompanied by many structural changes at<br />
the neuromuscular junction. Preterminal axons are<br />
increased in number and a greater number of the axons<br />
enter into a single endplate. <strong>The</strong> distance between the<br />
preterminal axon and the motor endplate is increased.<br />
<strong>The</strong> motor endplate is composed of a greater number of<br />
smaller conglomerates of nicotinic acetylcholine receptors<br />
and is lengthened with increasing age. This is accompanied<br />
by a flattening of the folds of the endplate at the<br />
neuromuscular junction. 8<br />
Alterations in muscle anatomy and physiology extend<br />
beyond the neuromuscular junction in that extrajunctional<br />
acetylcholine receptors are frequently found in<br />
aged muscles. 9 This may be the result of a progressive<br />
denervation that accompanies aging. How these changes<br />
in the neuromuscular junction influence neuromuscular<br />
transmission in the elderly is not known. Proliferation of<br />
acetylcholine receptors, as is observed in disuse atrophy,<br />
leads to a relative resistance to neuromuscular blocking<br />
agents. 10 Elderly patients, however, are not resistant to<br />
the effects of neuromuscular blocking agents.<br />
In animal experiments, age-related changes in acetylcholine<br />
storage and release at the neuromuscular junction<br />
have been found. In the neuromuscular junction of<br />
the diaphragm of aged rats, the acetylcholine content of<br />
a single motor nerve terminal is lower than that found in<br />
young adult rats. However, in these neuromuscular junctions,<br />
increased numbers of nerve terminals per endplate<br />
caused by terminal arborization contribute to the release<br />
266
18. Relaxants and <strong>The</strong>ir Reversal Agents 267<br />
of greater amounts of acetylcholine for each endplate. 11<br />
This alteration in transmitter release is likely responsible<br />
for maintenance of normal neuromuscular transmission<br />
in the aged rats. Overall, however, advanced age is associated<br />
with a decrease in the amount of acetylcholine<br />
released. 8<br />
Despite all of the changes at the neuromuscular junction,<br />
changes in the pharmacodynamic behavior of the<br />
nondepolarizing neuromuscular blocking agents seem to<br />
be the result of alterations in their pharmacokinetics<br />
rather than altered interaction of the nondepolarizing<br />
compound and the motor endplate.<br />
Dose-Response Relationships<br />
in the Elderly<br />
As the elderly become more sedentary and lose muscle<br />
mass, one would expect that there would be an upregulation<br />
of acetylcholine receptors, as is seen with denervation.<br />
12 <strong>The</strong>se physiologic changes would be expected to<br />
contribute to a relative resistance to neuromuscular<br />
blockers. With the decrease in lean body mass 13 and<br />
volume of distribution 14 that accompany aging, one would<br />
also expect that the dose required to establish neuromuscular<br />
block in geriatric patients would be less that that<br />
required in younger patients. Nondepolarizing neuromuscular<br />
blocking compounds are bulky, highly charged<br />
compounds that do not readily leave the central volume.<br />
This has been confirmed in elderly patients receiving<br />
either d-tubocurarine or metocurine. 15 Patients, young<br />
and elderly, received a single intravenous dose of the<br />
study compound and elderly patients were found to have<br />
both a decreased initial volume of distribution and volume<br />
of distribution. Results, with respect to volumes of distribution<br />
of other nondepolarizing compounds, however,<br />
are not consistent. Pharmacokinetic study of the<br />
intermediate-acting agent, vecuronium, in patients over<br />
the age of 70 years demonstrated that both the initial<br />
volume of distribution and the volume of distribution<br />
after a single intravenous dose of 0.1 mg/kg were indistinguishable<br />
from what was found in younger patients. 16<br />
<strong>The</strong> decrease in plasma proteins in the elderly would<br />
argue that bioavailability of drugs would be increased as<br />
less would be bound to proteins. However, nondepolarizing<br />
neuromuscular blocking agents are not highly<br />
protein bound 17 and the available free fractions of long-,<br />
intermediate-, and short-acting compounds have been<br />
shown, in vitro, to be the same in elderly and young<br />
adults. 18<br />
With the structural changes in the neuromuscular junction,<br />
already described in this chapter, it would not be<br />
unreasonable to expect that sensitivity to nondepolarizing<br />
compounds would be increased. This, however, has<br />
Figure 18-1. <strong>The</strong> relationship between plasma metocurine<br />
(o-o) and d-tubocurarine (-) in young and elderly patients<br />
and their depth of neuromuscular block. Values for the young<br />
are represented by the unfilled symbols (o and ) and those for<br />
the elderly by the filled symbols (• and ). Differences between<br />
the young and elderly are not significant for either of the neuromuscular<br />
blocking agents. (Adapted with permission from<br />
Matteo et al. 15 Copyright © Lippincott Williams & Wilkins.)<br />
not been found to be true. Duvaldestin 19 found that, in<br />
the case of the long-acting nondepolarizing compound<br />
pancuronium, there was no difference in the plasma<br />
concentration–response relationships in young and<br />
elderly patients. Similarly, both metocurine and d-<br />
tubocurarine have no difference between the plasma concentration–response<br />
relationships of the elderly and the<br />
young adult patients (Figure 18-1). 15 Similar results have<br />
been documented with the intermediate-acting nondepolarizing<br />
agents. Rupp et al. 20 found that the steady-state<br />
concentration of vecuronium at 50% neuromuscular<br />
block was the same in elderly and young adult patients.<br />
<strong>The</strong>se results indicate that at the same plasma concentration<br />
of relaxant, elderly and young patients have the same<br />
degree of neuromuscular blockade, and sensitivity of the<br />
acetylcholine receptor is, therefore, not increased in geriatric<br />
patients.<br />
Although alterations in pharmacokinetics influence<br />
the onset of effect and duration of action, the dose of re -<br />
laxant that will generally produce 95% neuromuscular<br />
block is the same in elderly and young adults. This<br />
has been shown for the long-acting compounds pancuronium,<br />
19 pipecuronium, 21 and doxacurium 22 as well<br />
as the intermediate-acting compounds vecuronium, 23<br />
rocuronium, 24 and atracurium. 25
268 C.A. Lien and T. Suzuki<br />
Table 18-1. Onset of maximal block in young and elderly patients following administration of nondepolarizing neuromuscular<br />
blocking agents.<br />
Onset (minutes)<br />
Reference Neuromuscular blocking agent Dose (mg ⋅ kg −1 ) Elderly patients Young adult patients<br />
26 Succinylcholine 1 1.58 [0.12] 1.18 [0.13]<br />
Short-acting nondepolarizing neuromuscular blocking agents<br />
52 Mivacurium 0.15 2.03 (0.53) 2.08 (0.82)<br />
Intermediate-acting nondepolarizing neuromuscular blocking agents<br />
26 Vecuronium 0.1 4.92 [0.52] 3.70 [0.23]<br />
59 0.1 3.52 (1.11) 2.57 (0.66)*<br />
42 Rocuronium 0.6 4.5 (2.4) 4.1 (1.5)<br />
43 1.0 1.33 (0.43) 1.04 (0.21)*<br />
26 Cisatracurium 0.1 4.0 3.0*<br />
50 0.1 3.4 (1.0) 2.5 (0.6)*<br />
Long-acting nondepolarizing neuromuscular blocking agents<br />
21 Pipecuronium 0.07 6.9 (2.6) 4.5 (1.5)*<br />
22 Doxacurium 0.025 11.2 (1.1) 7.7 (1.0)*<br />
Note: Data are mean (SD) or [SEM].<br />
*Statistically significant difference when compared with elderly patients.<br />
Onset of Neuromuscular Block<br />
For nondepolarizing neuromuscular blocking agents to<br />
exert their effect, they must be carried to the neuromuscular<br />
junction. <strong>The</strong> rate at which this is done is influenced<br />
by a number of factors including circulation to the muscles,<br />
and cardiac output. Once the nondepolarizing muscle<br />
relaxant arrives at the muscle, it needs to diffuse into the<br />
neuromuscular junction and bind with the acetylcholine<br />
receptor to cause neuromuscular blockade. In geriatric<br />
patients, although there are some differences as to the<br />
extent (Table 18-1), increased age is generally associated<br />
with a slower onset of neuromuscular block when doses<br />
of 2×ED 95 (2 times the dose that causes, on average, 95%<br />
neuromuscular block) or greater are administered. Differences<br />
in onset are more apparent when doses not<br />
causing complete neuromuscular block are examined 26<br />
(Figure 18-2). With administration of these smaller doses<br />
of nondepolarizing compound, the time to the actual<br />
maximal effect can be measured. However, administration<br />
of the larger doses allows only for the determination<br />
of the time required to achieve 100% neuromuscular<br />
block. <strong>The</strong> greater time required for maximal effect may<br />
be attributable to a decreased cardiac output, although<br />
physically active, healthy geriatric patients may not have<br />
a decline in cardiac function. 27<br />
In a study in patients over the age of 65 years, receiving<br />
oxygen-nitrous oxide-isoflurane anesthesia, cisatracurium<br />
(0.1 mg/kg) was administered after induction of<br />
anesthesia and subsequent boluses of 0.025 mg/kg at<br />
recovery of twitch height to 25% in order to maintain<br />
neuromuscular block. 28 <strong>The</strong> authors found that onset of<br />
block after the administration of cisatracurium was slower<br />
in elderly individuals than in young adults (3 versus 4<br />
minutes, respectively). Pharmacodynamic modeling demonstrated<br />
that the biophase equilibration in the elderly<br />
was slower than in young adults (0.06 versus 0.071, respectively).<br />
<strong>The</strong> authors attributed the slower onset of neuromuscular<br />
block to the slower biophase equilibration in<br />
the elderly. <strong>The</strong> relative contributions of decreased cardiac<br />
time (sec)<br />
700<br />
600<br />
500<br />
400<br />
300<br />
200<br />
100<br />
Vecuronium 0.03 mg/kg<br />
1-3 yr<br />
3-10 yr<br />
20-40 yr<br />
60-80 yr<br />
0<br />
0 10 20 30 40 50 60 70 80 90<br />
age (yr)<br />
Figure 18-2. <strong>The</strong> onset of maximal neuromuscular blocking<br />
effect of vecuronium 0.03 mg/kg in four different age groups.<br />
Onset of maximal effect is faster in the children and slowest in<br />
the most aged subjects. p < 0.00001 by linear regression.<br />
(Reprinted with permission from Koscielniak-Nielsen et al. 26<br />
Copyright © Lippincott Williams & Wilkins.)
18. Relaxants and <strong>The</strong>ir Reversal Agents 269<br />
output and slower biophase equilibration remain to be<br />
determined.<br />
<strong>The</strong> slower onset of maximal clinical effect of nondepolarizing<br />
neuromuscular blocking agents in geriatric<br />
patients may result in relative overdosing of the muscle<br />
relaxant. Unwillingness to wait for onset of maximal<br />
effect of a given dose causes clinicians to administer<br />
either additional medication, or a larger dose at the outset<br />
to speed onset of block. This results in an increase in<br />
the duration of action of the drug because a larger<br />
total amount of drug has been administered. Furthermore,<br />
in the case of those compounds that are eliminated<br />
through hepatic and renal mechanisms, these larger doses<br />
and administration of subsequent doses result in cumulation<br />
so that each subsequent dose lasts longer than<br />
the previous one. 29 This occurs because after the initial<br />
dose of nondepolarizing compounds, such as pancuronium<br />
and vecuronium, recovery of neuromuscular function<br />
occurs as a result of distribution to sites other than the<br />
plasma rather than elimination of the relaxant from the<br />
body. With subsequent doses, the first dose is entering<br />
into its elimination phase and reentering the plasma. <strong>The</strong><br />
drug effect, therefore, is a combination not only of the<br />
recently administered relaxant but also of a portion<br />
of the earlier dose as both contribute to plasma concentration.<br />
This effect is more pronounced with the longacting<br />
pancuronium than with the intermediate-acting<br />
vecuronium.<br />
Pharmacokinetics and Duration<br />
of Effect<br />
Aging, even in healthy elderly patients, is accompanied<br />
by decreases in hepatic and renal blood flow and<br />
function. Because the majority of nondepolarizing neuromuscular<br />
blocking agents are eliminated through some<br />
combination of these means, alterations in pharmacokinetics<br />
and duration of effect are to be expected. Alterations<br />
in the pharmacodynamics of nondepolarizing<br />
compounds as a result of changes in the pharmacokinetics<br />
associated with the normal process of aging may<br />
be difficult to distinguish from concomitant disease<br />
processes.<br />
Long-Acting Agents<br />
Although there may be some differences in the actual<br />
percent of drug eliminated through splanchnic and renal<br />
mechanisms, the long-acting nondepolarizing agents<br />
depend largely on the kidney for their elimination from<br />
the plasma (Table 18-2). It is not surprising, therefore,<br />
that these compounds should have a longer duration of<br />
action in geriatric patients. As has been found in the<br />
Table 18-2. Means of elimination of nondepolarizing neuromuscular<br />
blocking agents from the body.<br />
Neuromuscular blocking agent<br />
Means of elimination<br />
Long-acting compounds<br />
Pancuronium Kidney 85%, liver 15%<br />
Pipecuronium Kidney 90%, liver 10%<br />
Doxacurium Kidney 90%, liver 10%<br />
d-Tubocurarine Kidney 80%, liver 20%<br />
Metocurine Kidney 98%, liver 2%<br />
Intermediate-acting compounds<br />
Vecuronium Kidney 40%–50%, liver 50%–60%<br />
Rocuronium Kidney 10%, liver 70%<br />
Atracurium<br />
Kidney 10%–40%, Hofmann<br />
elimination 60%–90%<br />
Cisatracurium<br />
Kidney 16%, Hofmann elimination<br />
>75%<br />
Short-acting compounds<br />
Mivacurium<br />
Kidney 95%<br />
majority of studies with these agents, their prolonged<br />
duration of action can be attributed to a prolonged elimination<br />
half-life and a decreased clearance.<br />
McLeod et al. 30 demonstrated that the clearance of<br />
pancuronium decreased with increasing age. In a later<br />
study, Duvaldestin et al. 19 studied the pharmacokinetics<br />
and dynamics of pancuronium in young adults and those<br />
older than 75 years. He found that the 10%–75% and<br />
25%–75% recovery intervals were prolonged by at least<br />
60% in the elderly. This could be attributed to a slower<br />
elimination of pancuronium from the plasma in elderly<br />
patients (Figure 18-3). Not surprisingly, the clearance of<br />
pancuronium was decreased from 1.8 in young adults to<br />
1.2 mL/min/kg in patients of advanced age. Because the<br />
volume of distribution in the elderly was no different<br />
from that in younger adults, the decrease in clearance<br />
resulted in a doubling of the elimination half-life from<br />
107 to 201 minutes.<br />
Similar results have been found for metocurine and<br />
d-tubocurarine. 15 In this study, elderly patients were<br />
defined as being older than 70 years of age and young<br />
adults were between 29 and 59 years of age. <strong>The</strong> elderly<br />
patients had a significantly prolonged 25%–75% recovery<br />
interval. This could be attributed to a decreased<br />
volume of distribution and clearance as well as a markedly<br />
prolonged elimination half-life for both nondepolarizing<br />
neuromuscular blocking agents. <strong>The</strong> study results<br />
are summarized in Table 18-3.<br />
Doxacurium, similar to the other long-acting neuromuscular<br />
blocking agents, is eliminated through the<br />
kidneys and, in patients with renal failure, its clearance<br />
is significantly decreased 31 and it has a longer duration<br />
of action. 32 Not surprisingly, therefore, the clinical duration<br />
of action 33 and interpatient variability 22 is increased<br />
in elderly patients. In a pharmacokinetic study of the
270 C.A. Lien and T. Suzuki<br />
Figure 18-3. <strong>The</strong> elimination of pancuronium from the plasma<br />
after administration of a bolus dose. Pancuronium disappears<br />
from the plasma significantly more slowly in elderly patients<br />
than in middle-aged adults. (Reprinted with permission<br />
from Duvaldestin et al. 19 Copyright © Lippincott Williams &<br />
Wilkins.)<br />
relaxant in elderly patients, however, the drug was found<br />
to not have a decreased clearance or prolonged elimination<br />
half-life. 22 This negative result may have been the<br />
result of differences in intraoperative fluid management<br />
of the young and elderly patients. <strong>The</strong> elderly patients<br />
received 1750 mL of intravenous fluid at the start of<br />
surgery whereas their younger counterparts received<br />
1063 mL. In addition, the elderly patients sustained, on<br />
average, 5 times more blood loss than did the younger<br />
patients so that total fluid replacement in the elderly was<br />
almost 6 L, whereas in the young it was 2500 mL. <strong>The</strong>se<br />
differences would increase calculated volumes of distribution<br />
and lower the plasma concentration of drug measured<br />
in the elderly.<br />
Similarly, pipecuronium has a prolonged duration of<br />
action and decreased clearance in patients with renal<br />
failure. 34 Despite this, the age-related decreases in renal<br />
function do not seem to cause the drug to have a prolonged<br />
duration of action or a decreased clearance. 21 In<br />
a study of 20 elderly and 10 young adults receiving nitrous<br />
oxide, fentanyl and droperidol anesthesia, patients<br />
received 70 µg/kg pipecuronium as a single intravenous<br />
bolus. <strong>The</strong> elderly patients developed, on average, a lesser<br />
degree of neuromuscular block with this dose than did<br />
the younger patients (95% versus 100%, respectively).<br />
Clearance of pipecuronium was the same in both groups<br />
and differences in elimination half-life (181 versus 154<br />
minutes in the elderly and young, respectively) were not<br />
statistically different.<br />
Intermediate-Acting Agents<br />
In contrast to the dependence of the long-acting nondepolarizing<br />
compounds on the kidneys for their elimination,<br />
the intermediate-acting compounds are eliminated<br />
from the body primarily through other mechanisms<br />
(Table 18-2). <strong>The</strong>se include hepatic elimination and<br />
Hofmann degradation. In addition to decreases in renal<br />
function and blood flow, aging is associated with decreases<br />
in hepatic blood flow and hepatocellular function. 35–37<br />
One would, therefore, expect that compounds relying on<br />
this means for elimination from the body would have<br />
Table 18-3. Pharmacokinetics of nondepolarizing neuromuscular blocking agents in geriatric patients.<br />
Neuromuscular blocking agent Patient age t 1/2 β (minutes) Cl (mL ⋅ kg −1 ⋅ min −1 ) V d (L ⋅ kg −1 ) Reference<br />
Vecuronium Young 78 ± 21 5.6 ± 3.2 0.49 ± 0.02 16<br />
Elderly 125 ± 55* 2.6 ± 0.6* 0.44 ± 0.01<br />
Young 70 ± 20 5.2 ± 0.8 0.24 ± 0.04 20<br />
Elderly 58 ± 10 3.7 ± 1.0* 0.18 ± 0.03*<br />
Atracurium Young 15.7 ± 2.5 5.3 ± 0.9 0.10 ± 0.01 46<br />
Elderly 21.8 ± 3.3* 6.5 ± 1.1 0.19 ± 0.06*<br />
Cisatracurium Young 21.5 ± 2.4 4.6 ± 0.8 0.11 ± 0.01 50<br />
Elderly 25.5 ± 3.7* 5.0 ± 0.9 0.13 ± 0.02*<br />
Pancuronium Young 107 ± 24 1.81 ± 0.36 0.27 ± 0.06 19<br />
Elderly 201 ± 69* 1.18 ± 0.39* 0.32 ± 0.10<br />
Pipecuronium Young 154 ± 61 2.5 ± 0.7 0.31 ± 0.07 21<br />
Elderly 181 ± 68 2.4 ± 1.0 0.39 ± 0.13<br />
d-Tubocurarine Young 173 ± 38 1.71 ± 0.32 0.42 ± 0.06 15<br />
Elderly 268 ± 51* 0.79 ± 0.18* 0.28 ± 0.04*<br />
Metocurine Young 269 ± 56 1.1 ± 0.16 0.45 ± 0.04 15<br />
Elderly 530 ± 83* 0.36 ± 0.08* 0.23 ± 0.03*<br />
Doxacurium Young 86 ± 50 2.22 ± 1.09 0.15 ± 0.04 22<br />
Elderly 96 ± 20 2.47 ± 0.69 0.22 ± 0.08*<br />
t 1/2 β = half-life of elimination, Cl = plasma clearance, V d = volume of distribution.<br />
*<strong>The</strong>re is a statistically significant difference compared with younger adults.
18. Relaxants and <strong>The</strong>ir Reversal Agents 271<br />
altered pharmacokinetics. In contrast, clearance by<br />
Hofmann elimination is independent of end-organ function<br />
and aging should have little impact on the pharmacokinetics<br />
of compounds eliminated primarily by this<br />
means.<br />
Vecuronium was the first of the intermediate-acting<br />
nondepolarizing relaxants to be introduced into clinical<br />
practice. Although it is eliminated primarily in the bile, 38,39<br />
20%–25% of the relaxant is eliminated unchanged in the<br />
urine. Whether or not aging affects the pharmacokinetics<br />
of vecuronium has been much debated. <strong>The</strong> action of<br />
vecuronium in the elderly has been studied by four<br />
different groups of investigators. 16,20,39,40 d’Hollander<br />
and colleagues examined the rate of recovery from<br />
vecuronium-induced neuromuscular blockade in patients<br />
over the age of 60 years. <strong>The</strong>se recovery rates were compared<br />
with those in patients under the age of 40 and those<br />
between 40 and 60 years of age. <strong>The</strong> 10%–25% and<br />
25%–75% recovery intervals were significantly prolonged<br />
in the elderly patients compared with recovery intervals<br />
in younger patients. Additionally, less vecuronium was<br />
required to maintain 90% neuromuscular block for a<br />
period of 90 minutes in the elderly patients than it was in<br />
the younger controls. 39 McCarthy et al. 40 reported very<br />
similar results. <strong>The</strong>y found that the duration of action was<br />
significantly prolonged in the elderly (39 versus 28<br />
minutes) and the clinical duration of action was prolonged<br />
as well (69 and 45 minutes, respectively) after a<br />
bolus of 0.08 mg/kg vecuronium.<br />
Rupp et al. 20 studied the pharmacokinetics and dynamics<br />
of vecuronium in elderly patients in whom an infusion<br />
had been discontinued once 70%–80% neuromuscular<br />
block had been achieved. In this study, patients older than<br />
70 years had clearance and volume of distribution for<br />
vecuronium that were approximately 30% less than was<br />
found in younger adults. Elimination half-life and the<br />
25%–75% recovery interval were not, in contrast, different<br />
from what was found in young adult controls. Lien<br />
et al. 16 used a different study design to determine the<br />
kinetics and dynamics of vecuronium in elderly patients.<br />
In this study, patients received a single intravenous bolus<br />
dose of vecuronium. Recovery was monitored and venous<br />
blood taken for determination of pharmacokinetics.<br />
Elderly patients (between 72 and 86 years of age) had<br />
5%–25% and 25%–75% recovery intervals that were<br />
approximately 3 times longer than those in young adults.<br />
Clearance of vecuronium was half as fast in the elderly<br />
as it was in young adult patients (2.6 versus 5.6 mL⋅kg −1 ,<br />
respectively) and elimination of the compound was<br />
slower in geriatric patients (78 and 125 minutes for young<br />
adult and elderly patients, respectively). <strong>The</strong> authors’<br />
conclusion that the prolonged duration of action of<br />
vecuronium in elderly patients is attributable to its<br />
decreased clearance in this patient population supports<br />
the findings of d’Hollander and colleagues 39 and is<br />
not inconsistent with the decreased clearance found by<br />
Rupp et al. 20<br />
Rocuronium is the other intermediate-acting nondepolarizing<br />
neuromuscular blocking agent that has a steroidal<br />
structure. Similar to vecuronium, it does not depend<br />
on the kidney for its primary means of elimination from<br />
the body. However, although it does not depend on the<br />
kidney solely for its elimination, clearance of rocuronium<br />
is decreased and its mean residence time is prolonged in<br />
patients with renal failure. 41 As with vecuronium, the<br />
behavior of this compound in aged patients has been<br />
studied by different groups of investigators. 24,42,43 In the<br />
case of rocuronium, however, the results are more similar<br />
across the studies. Baykara et al. 43 reported that the first<br />
response in the train-of-four response after administration<br />
of rocuronium, 1 mg/kg, was slower in the elderly<br />
than in young adults. Bevan et al. 24 found, in a study of<br />
repeat bolus doses of rocuronium, that the clinical duration<br />
of action and the 25%–75% recovery intervals were<br />
prolonged in elderly patients. With repeated doses of<br />
0.1 mg/kg rocuronium administered at 25% recovery<br />
of twitch height, the duration of action became longer in<br />
the elderly patients but did not in the young adult control<br />
patients. Matteo et al. 42 studied the pharmacokinetics<br />
and pharmacodynamics of rocuronium in geriatric<br />
patients following a 0.6 mg/kg dose and found that in<br />
patients between the ages of 70 to 78 years, clearance was<br />
decreased by 27%. Not unexpectedly, the 25%–75%<br />
recovery interval was increased from 13 minutes in the<br />
young adults to 22 minutes in the elderly patients.<br />
Atracurium depends on neither the kidney nor the<br />
liver as its primary means of elimination. Rather, it undergoes<br />
the base and temperature catalyzed process of<br />
Hofmann elimination (Table 18-2). This spontaneous<br />
degradation of the relaxant is not end-organ dependent.<br />
<strong>The</strong>refore, the physiologic changes associated with aging<br />
should not affect the pharmacokinetics of atracurium and<br />
its duration of action should be unaffected by advanced<br />
age. As they had done with vecuronium, d’Hollander and<br />
colleagues 44 studied atracurium in patients over the age<br />
of 60 years. In this study, patients received an infusion of<br />
atracurium to maintain 90% depression of neuromuscular<br />
function for 90 minutes. <strong>The</strong> dose of relaxant required<br />
to maintain this depth of paralysis was calculated in the<br />
age groups studied (older than 60 years, 40–60 years, and<br />
younger than 40 years of age). <strong>The</strong>re were no differences<br />
among the groups in terms of their 10%–25% and 25%–<br />
75% recovery intervals or the amount of relaxant necessary<br />
to maintain 90% twitch suppression.<br />
Slight changes in the pharmacokinetics of atracurium<br />
in elderly patients, however, have been reported. Kent<br />
et al. 45 administered 0.6 mg/kg atracurium to elderly<br />
and young adult patients and found no difference in<br />
clearance and the volume of distribution between the two<br />
patient groups. <strong>The</strong>re was, however, a small but significant
272 C.A. Lien and T. Suzuki<br />
difference in the elimination half-life. <strong>The</strong> elimination<br />
half-life of atracurium was prolonged by 15% in elderly<br />
patients, from 20 to 23 minutes. Kitts et al. 46 administered<br />
an infusion of atracurium to achieve 70% neuromuscular<br />
block. As described by Kent et al., 45 elimination half-life<br />
was prolonged in the elderly. Because clearance was not<br />
affected by advanced age, the increase in elimination<br />
half-life was attributable to a larger volume of distribution<br />
in elderly patients. Most recently, Parker et al. 47<br />
found that elimination half-life was prolonged and clearance<br />
decreased in elderly patients. <strong>The</strong> results of Kitts,<br />
Kent, and Parker support the finding by Fisher et al. 48 that<br />
in addition to Hofmann elimination, renal and hepatic<br />
mechanisms contribute to the elimination of the compound.<br />
Despite these pharmacokinetic differences in<br />
elderly patients, however, the dynamics of neuromuscular<br />
blockade with atracurium are not different in the young<br />
and elderly. 44,46<br />
Cisatracurium is one of the 10 isomers that comprise<br />
atracurium. Similar to atracurium, it is eliminated primarily<br />
through Hofmann elimination. Renal clearance<br />
accounts for 16% of its elimination from the body. 49 As<br />
with atracurium, small changes have been found in the<br />
pharmacokinetics of this compound in elderly patients.<br />
Ornstein et al. 50 described a prolongation of the half-life<br />
of 4 minutes (21.5 versus 25.5 minutes in young and<br />
elderly patients, respectively) and an increase in the<br />
volume of distribution (108 versus 126 mL⋅kg −1 in young<br />
and elderly patients, respectively) of cisatracurium in<br />
elderly patients. Clearance was unchanged by advanced<br />
age. Sorooshian et al. 28 also found that clearance was<br />
unaffected by advanced age, whereas volume of distribution<br />
in the elderly was larger. Both studies found no difference<br />
in recovery of neuromuscular function after<br />
administration of 0.1 mg/kg cisatracurium. In a later study,<br />
Pűhringer et al. 51 also noted the lack of effect of small<br />
changes in pharmacokinetics of cisatracurium on the<br />
duration of action of the compound in the elderly. Patients<br />
received 0.15 mg/kg cisatracurium to induce neuromuscular<br />
blockade and 0.03 mg/kg boluses to maintain neuromuscular<br />
blockade. <strong>The</strong> clinical duration of action after<br />
the initial dose and the time to return to a train-of-four<br />
ratio of 0.8 following the last dose of cisatracurium were<br />
recorded. <strong>The</strong> recovery parameters were the same in<br />
young adults and those older than 65 years of age.<br />
Short Duration of Action<br />
Mivacurium is the only available nondepolarizing neuromuscular<br />
blocking agent with a short duration of action.<br />
Similar to succinylcholine, it is metabolized by plasma<br />
cholinesterase and is dependent on neither hepatic<br />
nor renal function for its elimination. Mivacurium has<br />
been shown to have a prolonged recovery in elderly<br />
patients. 52 In this study, patients received either a bolus<br />
of 0.15 mg/kg mivacurium and were allowed to recover<br />
or, following the bolus, were given an infusion to maintain<br />
90% suppression of neuromuscular response to stimulation.<br />
All recovery parameters were prolonged by approximately<br />
30% in elderly patients. <strong>The</strong> amount of mivacurium<br />
required to maintain neuromuscular blockade was also<br />
reduced (3.7 versus 5.5 µg/kg/min in the elderly and<br />
young, respectively). Goudsouzian et al. 53 also found that<br />
elderly patients required a lower infusion rate to maintain<br />
a stable depth of block. <strong>The</strong>se results suggest that the<br />
pharmacokinetics of mivacurium are altered in elderly<br />
patients. <strong>The</strong> results of Østergaard et al. in a study of the<br />
kinetics of the compound do not explain the prolongation<br />
in recovery observed in the elderly. 54 <strong>The</strong>y found that the<br />
half-life and clearances of the three isomers of mivacurium,<br />
cis-trans, trans-trans, and cis-cis, were not different<br />
in elderly patients. <strong>The</strong> volume of distribution of the<br />
relaxant, however, was larger in the elderly.<br />
Plasma cholinesterase activity is reduced in the elderly 55<br />
and mivacurium requirements are inversely related to<br />
plasma cholinesterase activity 56 in that patients with<br />
higher plasma cholinesterase activity require higher<br />
mivacurium infusion rates to maintain the desired depth<br />
of block than those patients with lower plasma cholinesterase<br />
activity. If mivacurium is to be used in geriatric<br />
patients, one can anticipate that lower infusion rates will<br />
be required to maintain a stable depth of neuromuscular<br />
block and, if administered with repeated boluses, longer<br />
dosing intervals would be appropriate.<br />
Anticholinesterases<br />
Because the duration of action of many nondepolarizing<br />
neuromuscular blocking agents is prolonged in the elderly,<br />
the impact of aging on the pharmacokinetics and pharmacodynamics<br />
of their antagonists is of interest. <strong>The</strong><br />
three typically used anticholinesterases, edrophonium,<br />
neostigmine, and pyridostigmine, have prolonged durations<br />
of action and decreased clearances in the elderly<br />
(Table 18-4). <strong>The</strong> kinetics and dynamics of each in the<br />
elderly have been studied with vecuronium and many of<br />
the long-acting neuromuscular blocking agents.<br />
Edrophonium<br />
<strong>The</strong> clearance of edrophonium from the plasma depends<br />
primarily on the kidneys. Decreases in renal blood flow<br />
and glomerular filtration rate likely account for the<br />
altered pharmacokinetics of this compound in the elderly.<br />
As would be anticipated based on its means of elimination,<br />
the clearance of edrophonium (1 mg/kg) is decreased<br />
and its elimination half-life prolonged in the elderly. 57 In<br />
the study by Matteo et al., 57 edrophonium was administered<br />
during an ongoing infusion of metocurine that was
18. Relaxants and <strong>The</strong>ir Reversal Agents 273<br />
Table 18-4. Pharmacokinetics of edrophonium, neostigmine, and pyridostigmine in the elderly and young adults.<br />
Anticholinesterase Patient group t 1/2 β (minutes) Cl (mL ⋅ kg −1 ⋅ min −1 ) V i (L ⋅ kg −1 ) V d (L ⋅ kg −1 )<br />
Edrophonium (1 mg ⋅ kg −1 ) 59 Elderly 84.2 (17)* 5.9 (2)* 0.05 (0.02) 0.72 (0.3)<br />
Young 56.6 (16) 12.1 (4) 0.2 (0.2) 0.81 (0.3)<br />
Neostigmine (0.07 mg ⋅ kg −1 ) 60 Elderly 16.7 (0.8) 23.4 (5) 0.068 (0.018)* 0.566 (0.13)<br />
Young 18.5 (7) 33.5 (4) 0.1 (0.04) 0.549 (0.12)<br />
Pyridostigmine (0.25 mg ⋅ kg −1 ) 68 Elderly 157 (56) 6.7 (2.2)* 0.085 (0.06) 1.4 (0.4)<br />
Young 140 (60) 9.5 (2.7) 0.095 (0.046) 1.8 (0.7)<br />
Note: Data are shown as mean (SD).<br />
t 1/2 β = half-life of elimination, Cl = plasma clearance, V i = initial volume of distribution, V d = volume of distribution.<br />
*<strong>The</strong>re is a statistically significant difference compared with younger adults.<br />
dosed to maintain 90% neuromuscular block before the<br />
administration of the anticholinesterase. Despite its<br />
altered pharmacokinetics, dosing adjustments are not<br />
required for antagonism of residual neuromuscular block.<br />
This has been demonstrated in two different dosing<br />
models. McCarthy et al. 58 demonstrated in a doseresponse<br />
study that the dose of edrophonium required<br />
to antagonize 90% vecuronium-induced neuromuscular<br />
block, after a bolus administration of 0.08 mg/kg<br />
vecuronium, did not differ between the elderly and young<br />
adult patients. Similarly, Kitajima et al. 59 administered<br />
edrophonium, 0.75 mg/kg, to antagonize neuromuscular<br />
block that had been induced with vecuronium, 0.1 mg/kg.<br />
Edrophonium was administered when the train-of-four<br />
ratio had returned to 25%. <strong>The</strong> authors found that there<br />
was no difference in the time required for the train-offour<br />
ratio to recover to 75% in elderly patients (over the<br />
age of 70 years) and young adults. Matteo et al. 57 evaluated<br />
the ability of 1 mg⋅kg −1 edrophonium to reverse a<br />
deep, steady-state block produced by continuous infusion<br />
of metocurine in the elderly and younger adult patients.<br />
<strong>The</strong>y found that there was no significant difference in the<br />
time to the maximum effect of the anticholinesterase<br />
in the two study groups (elderly 2.1 versus younger<br />
1.7 minutes). In this model, the plasma concentration of<br />
edrophonium at any given point in recovery was greater<br />
in the elderly patients than in the young adults.<br />
<strong>The</strong>refore, the change in the pharmacokinetic parameters<br />
of edrophonium in the elderly has no influence on its<br />
efficacy in antagonizing residual neuromuscular block in<br />
this patient population. Because the volume of distribution<br />
tends to be smaller and the clearance slower, the dose of<br />
edrophonium does not need to be adjusted to obtain the<br />
same degree of recovery as in younger adults.<br />
Neostigmine<br />
In a study designed similar to the kinetic studies of edrophonium<br />
in the elderly, 57 Young et al. 60 studied the pharmacokinetics<br />
and dynamics of neostigmine in this patient<br />
population. Neostigmine was administered to patients<br />
receiving a metocurine infusion to maintain 90% neuromuscular<br />
block. <strong>The</strong> authors found that there was a slight,<br />
but not statistically significant, decrease in clearance of<br />
the anticholinesterase in the elderly and a decreased<br />
initial volume of distribution.<br />
Dose-response studies of neostigmine are not as<br />
consistent as those involving edrophonium. <strong>The</strong>y have<br />
demonstrated that the dose of neostigmine required for<br />
antagonism of residual neuromuscular block in elderly<br />
patients is either similar to, 33 or greater 61 than, that<br />
required in younger adults. When neostigmine is used to<br />
antagonize doxacurium-induced block, there is no significant<br />
difference in the dose of neostigmine required to<br />
achieve recovery, within 10 minutes, to a train-of-four<br />
ratio of 0.7 from 25% spontaneous recovery of muscle<br />
strength (41.6 ± 5.8 in the elderly and 53.6 ± 7.5 µg⋅kg −1 in<br />
younger adults). 33 Furthermore, in a different study, neostigmine,<br />
50 µg⋅kg −1 , administered as a bolus at 25%<br />
recovery of muscle strength after administration of doxacurium,<br />
accelerated recovery to a train-of-four ratio of<br />
0.7 to the same degree in both patient populations (12.6<br />
± 7.3 in the elderly and 12.0 ± 6.7 minutes in younger<br />
adults). 62 It has also been reported, however, that the<br />
dose of neostigmine required to antagonize 90%<br />
vecuronium-induced block is greater in the elderly<br />
(31 µg⋅kg −1 ) than in younger adults (19 µg⋅kg −1 ). 61 Slower<br />
spontaneous recovery from vecuronium-induced block in<br />
geriatric patients during neostigmine-antagonized recovery<br />
may be a cause of their apparent greater requirement<br />
for neostigmine. That being said, because of its own<br />
decreased clearance in the elderly, the duration of action<br />
of neostigmine is prolonged in elderly patients. 63 In addition,<br />
the decreased initial volume of distribution of<br />
neostigmine 60 (Table 18-4) results in a greater plasma<br />
concentration of the anticholinesterase after bolus administration<br />
and may contribute to its prolonged duration<br />
of action. This is potentially advantageous because the
274 C.A. Lien and T. Suzuki<br />
duration of action of many nondepolarizing neuromuscular<br />
blocking agents is prolonged in the elderly.<br />
Of note, the values reported for times to recovery to a<br />
train-of-four ratio of 0.7 are average values. As demonstrated<br />
by Kirkegaard et al., 64 there is a substantial degree<br />
of interpatient variability in the time required for neostigmine<br />
antagonism cisatracurium-induced neuromuscular<br />
block. This interpatient variability in young adults<br />
becomes even more pronounced when attempting to<br />
achieve recovery to a train-of-four ratio of 0.9, which has<br />
been recommended as the new standard for adequacy of<br />
recovery. 65<br />
Pyridostigmine<br />
Similar to neostigmine, pyridostigmine exhibits a prolonged<br />
duration of action in the elderly. 63,66 Approximately<br />
75% of administered pyridostigmine is eliminated<br />
by the kidney 63 and its clearance is slower in patients with<br />
renal failure. 67 <strong>The</strong> reduced plasma clearance of pyridostigmine<br />
(Table 18-4) caused by age-related deterioration<br />
in renal function likely accounts for its prolongation<br />
of action.<br />
Adverse Effects of Anticholinesterases in<br />
<strong>Geriatric</strong> Patients<br />
<strong>The</strong> cardiac muscarinic effects of anticholinesterases<br />
include dysrhythmias, such as bradycardia and conduction<br />
defects. Especially in the geriatric patient population,<br />
a large percentage of which has preexisting cardiovascular<br />
disease, anticholinesterase administration creates a<br />
greater risk of cardiac dysrhythmias. 68 Of the anticholinesterases,<br />
neostigmine is more likely to cause dysrhythmias<br />
than pyridostigmine (35% versus 14%, respectively). 69<br />
In any patient, antimuscarinic agents, such as atropine or<br />
glycopyrrolate, are administered with the anticholinesterase<br />
to counteract the bradycardic effects of the anticholinesterase.<br />
Depending on the dosing regimen, tachycardia,<br />
rather than bradycardia, is frequently observed. In<br />
patients with cardiovascular disease, the resultant increase<br />
in myocardial oxygen consumption may not be well tolerated<br />
and may lead to myocardial ischemia.<br />
In addition, atropine is a tertiary amine and can, therefore,<br />
cross the blood–brain barrier. In the central nervous<br />
system, anticholinergic drugs are known to affect the<br />
central cholinergic pathway where they are a cause of<br />
deterioration in postoperative cognitive function. 70 Atropine<br />
has been shown to produce disorientation, hallucinations,<br />
and memory loss. Glycopyrrolate, which is a<br />
quaternary amine, does not readily cross the blood–brain<br />
barrier and postanesthetic arousal times after its administration<br />
with neostigmine are shorter than those after<br />
the administration of atropine and neostigmine. 71<br />
Outcome Studies<br />
Reports of adverse outcome from residual neuromuscular<br />
blockade exist. 72–75 One prospective trial of patient<br />
outcome after general anesthesia and nondepolarizing<br />
relaxants has been done. 72 In this study, patients undergoing<br />
gynecologic, general, or orthopedic surgical procedures<br />
were randomly assigned to receive vecuronium,<br />
atracurium, or pancuronium. Muscle strength was determined<br />
in the postanesthesia care unit and patients were<br />
followed for several days for evidence of postoperative<br />
pulmonary complications. Elderly patients who received<br />
pancuronium were more likely to enter the postanesthesia<br />
care unit with a train-of-four ratio less than 0.7 than<br />
those receiving either of the intermediate-acting relaxants<br />
and the younger adult patients, regardless of the<br />
neuromuscular blocking agent they received. In addition,<br />
these patients were more likely to develop postoperative<br />
pulmonary complications than patients who had arrived<br />
to the postanesthesia care unit with a train-of-four ratio<br />
≥0.7. This is not unexpected because residual neuromuscular<br />
block has been found to interfere with the coordination<br />
of swallowing 76,77 and the response of the carotid<br />
body chemoreceptor to hypoxia. 78<br />
Summary<br />
Although age-related changes in hepatic, renal, and<br />
cardiac function slow the onset and clearance of many<br />
nondepolarizing neuromuscular blocking agents in geriatric<br />
patients, extensive changes at the neuromuscular<br />
junction do not increase sensitivity to these compounds.<br />
Decreased clearance mandates that neuromuscular block<br />
be maintained and subsequent doses administered only<br />
after documentation of return of muscle strength with a<br />
monitor of neuromuscular blockade. Except in rare cases,<br />
the clinician should anticipate having to pharmacologically<br />
antagonize residual neuromuscular block.<br />
As the surgical population ages and surgical trends and<br />
practices evolve, neuromuscular blocking agents, like<br />
anesthetics, must be specifically chosen based not only on<br />
their pharmacokinetic and pharmacodynamic properties,<br />
but also on the basis of patient age.<br />
References<br />
1. Gueret G, Rossignol B, Kiss G, et al. Is muscle relaxant<br />
necessary for cardiac surgery? Anesth Analg 2004;99:1330–<br />
1333.<br />
2. Tomlinson BE, Irving D. <strong>The</strong> numbers of limb motor neurons<br />
in the human lumbosacral cord throughout life. J Neurol Sci<br />
1977;34:213–219.<br />
3. Kawamura Y, Okazaki H, O’Brien PC, et al. Lumbar motoneurons<br />
of man. I. Numbers and diameter histograms of
18. Relaxants and <strong>The</strong>ir Reversal Agents 275<br />
alpha and gamma axons and ventral roots. J Neuropathol<br />
Exp Neurol 1977;36:853–860.<br />
4. Young A, Stokes M, Crowe M. Size, and strength of the<br />
quadriceps muscles of old and young men. Clin Physiol<br />
1985;5:145–154.<br />
5. Lexell J, Taylor CC, Sjöström M. What is the cause of the<br />
ageing atrophy? Total number, size and proportion of different<br />
fiber types studied in whole vastus lateralis muscle from<br />
15- to 83-year-old men. J Neurol Sci 1988;84:275–294.<br />
6. Forbes GB, Reina JC. Adult lean body mass declines with<br />
age: some longitudinal observations. Metabolism 1970;19:<br />
653–663.<br />
7. Doherty TJ, Brown WF. Age-related changes in the twitch<br />
contractile properties of human thenar motor units. J Appl<br />
Physiol 1997;82:93–101.<br />
8. Frolkis VV, Martynenko OA, Zamostan VP. Aging of the<br />
neuromuscular apparatus. Gerontology 1976;22:244–279.<br />
9. Oda K. Age changes of motor innervation and acetylcholine<br />
receptor distribution on human skeletal muscle fibres.<br />
J Neurol Sci 1984;66:327–338.<br />
10. Martyn JA, White DA, Gronert GA, et al. Up-and-down<br />
regulation of skeletal muscle acetylcholine receptors. Effects<br />
on neuromuscular blockers. <strong>Anesthesiology</strong> 1992;76:822–<br />
843.<br />
11. Smith DO. Acetylcholine storage, release and leakage at<br />
the neuromuscular junction of mature adult and aged rats.<br />
J Physiol 1984;347:161–176.<br />
12. Gronert GA. Disuse atrophy with resistance to pancuronium.<br />
<strong>Anesthesiology</strong> 1981;55:547–549.<br />
13. Novak LP. Aging, total body potassium, fat-free mass and<br />
cell mass in males and females between ages of 18–85 years.<br />
J Gerontol 1972;27:438–443.<br />
14. Ritschel WA. Pharmacokinetic approach to drug dosing in<br />
the aged. J Am Geriatr Soc 1976;24:344–354.<br />
15. Matteo RS, Backus WW, McDaniel DD, et al. Pharmacokinetics<br />
and pharmacodynamics of d-tubocurarine and metocurine<br />
in the elderly. Anesth Analg 1985;64:23–29.<br />
16. Lien CA, Matteo RS, Ornstein E, et al. Distribution, elimination<br />
and action of vecuronium in the elderly. Anesth<br />
Analg 1991;73:39–42.<br />
17. Wood M. Plasma drug binding: implications for anesthesiologists.<br />
Anesth Analg 1986;65:786–804.<br />
18. Cameron M, Donati F, Varin F. In vitro plasma protein<br />
binding of neuromuscular blocking agents in different subpopulations<br />
of patients. Anesth Analg 1995;81:1019–1025.<br />
19. Duvaldestin P, Saada J, Berger JL, et al. Pharmacokinetics,<br />
pharmacodynamics, and dose-response relationships of<br />
pancuronium in control and elderly subjects. <strong>Anesthesiology</strong><br />
1982;56:36–40.<br />
20. Rupp SM, Castagnoli KP, Fisher DM, et al. Pancuronium<br />
and vecuronium pharmacokinetics and pharmacodynamics<br />
of vecuronium in younger and elderly adults. <strong>Anesthesiology</strong><br />
1987;67:45–49.<br />
21. Ornstein E, Matteo RS, Schwartz AE, et al. Pharmacokinetics<br />
and pharmacodynamics of pipecuronium (Arduan) in<br />
elderly surgical patients. Anesth Analg 1992;74:841–844.<br />
22. Dresner DL, Basta SJ, Ali HH, et al. Pharmacokinetics and<br />
pharmacodynamics of doxacurium in young and elderly<br />
patients during isoflurane anesthesia. Anesth Analg 1990;71:<br />
498–502.<br />
23. O’Hara DA, Fragen RJ, Shanks CA. <strong>The</strong> effects of age on<br />
the dose response curve of vecuronium in adults. <strong>Anesthesiology</strong><br />
1987;67:45–49.<br />
24. Bevan DR, Fiset P, Balendran P, et al. Pharmacodynamic<br />
behavior of rocuronium in the elderly. Can J Anaesth 1993;<br />
40:127–132.<br />
25. Bell PF, Mirakhur RK, Clarke RSJ. Dose-response studies<br />
of atracurium, vecuronium and pancuronium in the elderly.<br />
Anaesthesia 1989;44:925–927.<br />
26. Koscielniak-Nielsen ZJ, Bevan JC, Popovic V, et al. Onset<br />
of maximum neuromuscular block following succinylcholine<br />
or vecuronium in four age groups. <strong>Anesthesiology</strong> 1993;<br />
79:229–234.<br />
27. Rodeheffer RJ, Gerstenblith G, Becker LC, et al. Exercise<br />
cardiac output is maintained with advancing age in healthy<br />
human subjects: cardiac dilatation and increased stroke<br />
work compensate for a diminished heart rate. Circulation<br />
1984;69:203–213.<br />
28. Sorooshian SS, Stafford MA, Eastwood NB, et al. Pharmacokinetics<br />
and pharmacodynamics of cisatracurium in<br />
young and elderly adult patients. <strong>Anesthesiology</strong> 1996;84:<br />
1083–1091.<br />
29. Fisher DM, Rosen JI. A pharmacokinetic explanation for<br />
increasing recovery time following larger or repeated doses<br />
of nondepolarizing muscle relaxants. <strong>Anesthesiology</strong> 1986;<br />
65:286–291.<br />
30. McLeod K, Hull CJ, Watson MJ. Effects of ageing on the<br />
pharmacokinetics of pancuronium. Br J Anaesth 1979;51:<br />
435–438.<br />
31. Cook RD, Freeman JA, Lai AA, et al. Pharmacokinetics and<br />
pharmacodynamics of doxacurium in normal patients and<br />
in those with hepatic or renal failure. Anesth Analg 1991;<br />
72:143–150.<br />
32. Cashman JN, Luke JJ, Jones RM. Neuromuscular block with<br />
doxacurium (BW A938U) in patients with normal or absent<br />
renal function. Br J Anaesth 1990;64:186–192.<br />
33. Koscielniak-Nielsen ZJ, Law-Min JC, Donati F, et al. Doseresponse<br />
relations of doxacurium and its reversal with neostigmine<br />
in young adults and healthy elderly patients.<br />
Anesth Analg 1992;74:845–850.<br />
34. Caldwell JE, Canfell PC, Castagnoli KP, et al. <strong>The</strong> influence<br />
of renal failure on the pharmacokinetics and duration of<br />
action of pipecuronium bromide in patients anesthetized<br />
with halothane and nitrous oxide. <strong>Anesthesiology</strong> 1989;70:<br />
7–12.<br />
35. Bender AD. <strong>The</strong> effect of increasing age on the distribution<br />
of peripheral blood flow in man. J Am Geriatr Soc 1965;<br />
13:192–198.<br />
36. Leithe ME, Hermiller JB, Magorien RD, et al. <strong>The</strong> effect of<br />
age on central and regional hemodynamics. Gerontology<br />
1984;30:240–246.<br />
37. Kato R, Vassanelli P, Frontino G, et al. Variation in the activity<br />
of liver microsomal drug-metabolizing enzymes in rats<br />
in relation to age. Biochem Pharmacol 1964;13:1037–1051.<br />
38. Bencini AF, Scaf AHJ, Sohn YJ, et al. Hepatobiliary disposition<br />
of vecuronium bromide in man. Br J Anaesth 1986;58:<br />
988–995.<br />
39. d’Hollander AA, Massaux F, Nevelsteen M, et al. Agedependent<br />
dose-response relationship of Org NC45 in<br />
anaesthetized patients. Br J Anaesth 1982;54:653–656.
276 C.A. Lien and T. Suzuki<br />
40. McCarthy G, Elliott P, Mirakhur RK, et al. Onset and duration<br />
of action of vecuronium in the elderly: comparison with<br />
adults. Acta Anaesth Scand 1992;36:383–386.<br />
41. Cooper RA, Maddineni RK, Wierda JMKH, et al. Time<br />
course of neuromuscular effects and pharmacokinetics of<br />
rocuronium bromide (ORG 9426) during isoflurane anaesthesia<br />
in patients with and without renal failure. Br J<br />
Anaesth 1993;71:222–226.<br />
42. Matteo RS, Ornstein E, Schwartz AE, et al. Pharmaco -<br />
kinetics and pharmacodynamics of rocuronium (Org 9426)<br />
in elderly surgical patients. Anesth Analg 1993;77:1193–<br />
1197.<br />
43. Baykara N, Solak M, Toker K. Predicting recovery from<br />
deep neuromuscular block by rocuronium in the elderly.<br />
J Clin Anesth 2003;15:328–333.<br />
44. d’Hollander AA, Luyckx C, Barvais L, et al. Clinical evaluation<br />
of atracurium besylate requirements for a stable<br />
muscle relaxation during surgery: lack of age-related effects.<br />
<strong>Anesthesiology</strong> 1983;59:237–240.<br />
45. Kent AP, Parker CJ, Hunter JM. Pharmacokinetics of atracurium<br />
and laudanosine in the elderly. Br J Anaesth 1989;<br />
63:661–666.<br />
46. Kitts JB, Fisher DM, Canfell PC, et al. Pharmacokinetics<br />
and pharmacodynamics of atracurium in the elderly. <strong>Anesthesiology</strong><br />
1990;72:272–275.<br />
47. Parker CJ, Hunter JM, Snowdon SL. Effect of age, sex and<br />
anesthetic technique on the pharmacokinetics of atracurium.<br />
Br J Anaesth 1992;69:439–443.<br />
48. Fisher DM, Canfell PC, Fahey MR, et al. Elimination of<br />
atracurium in humans: contribution of Hofmann elimination<br />
and ester hydrolysis vs. organ-based elimination. <strong>Anesthesiology</strong><br />
1986;65:6–12.<br />
49. Kisor DF, Schmith VD, Wargin WA, et al. Importance of the<br />
organ-independent elimination of cisatracurium. Anesth<br />
Analg 1996;83:1065–1071.<br />
50. Ornstein E, Lien CA, Matteo RS, et al. Pharmacodynamics<br />
and pharmacokinetics of cisatracurium in geriatric surgical<br />
patients. <strong>Anesthesiology</strong> 1996;84:520–525.<br />
51. Pühringer FK, Heier T, Dodgson M, et al. Double-blind<br />
comparison of the variability in spontaneous recovery of<br />
cisatracurium- and vecuronium-induced neuromuscular<br />
block in adult and elderly patients. Acta Anesthesiol Scand<br />
2002;46:364–371.<br />
52. Maddineni VR, Mirakhur RK, McCoy EP, et al. Neuromuscular<br />
and haemodynamic effects of mivacurium in<br />
elderly and young adult patients. Br J Anaesth 1994;73;<br />
609–612.<br />
53. Goudsouzian N, Charravorti S, Denman W, et al. Prolonged<br />
mivacurium infusion in young and elderly adults. Can J<br />
Anaesth 1997;44:955–962.<br />
54. Østergaard D, Viby-Mogensen J, Pedersen NA, et al. Pharmacokinetics<br />
and pharmacodynamics of mivacurium in<br />
young adult and elderly patients. Acta Anaesthesiol Scand<br />
2002;46:684–691.<br />
55. Maddineni VR, Mirakhur RK, McCoy EP. Plasma cholinesterase<br />
activity in elderly and young adults. Br J Anaesth<br />
1994;72:497.<br />
56. Hart PS, McCarthy GJ, Brown R, Lau M, Fisher DM. <strong>The</strong><br />
effect of plasma cholinesterase activity on mivacurium infusion<br />
rates. Anesth Analg 1995;80:760–763.<br />
57. Matteo RS, Young WL, Ornstein E, et al. Pharmacokinetics<br />
and pharmacodynamics of edrophonium in elderly surgical<br />
patients. Anesth Analg 1990;71:334–339.<br />
58. McCarthy GJ, Mirakhur RK, Maddineni VR, et al.<br />
Dose-responses for edrophonium during antagonism of<br />
vecuronium block in young and older adult patients. Anaesthesia<br />
1995;50:503–506.<br />
59. Kitajima T, Ishii K, Ogata H. Edrophonium as an antagonist<br />
of vecuronium-induced neuromuscular block in the elderly.<br />
Anaesthesia 1995;50:359–361.<br />
60. Young WL, Backus W, Matteo RS, et al. Pharmacokinetics<br />
and pharmacodynamics of neostigmine in the elderly. <strong>Anesthesiology</strong><br />
1984;61:A300.<br />
61. McCarthy GJ, Cooper R, Stanley JC, et al. Dose-response<br />
relationships for neostigmine antagonism of vecuroniuminduced<br />
neuromuscular block in adults and the elderly.<br />
Br J Anaesth 1992;69:281–283.<br />
62. De Mey JC, Rolly G, Blauwen ND. Doxacurium block is not<br />
influenced by age. J Clin Anesth 1995;7:453–456.<br />
63. Young WL, Matteo RS, Ornstein E. Duration of action of<br />
neostigmine and pyridostigmine in the elderly. Anesth<br />
Analg 1988;67:775–778.<br />
64. Kirkegaard H, Heier T, Caldwell JE. Efficacy of tactileguided<br />
reversal from cisatracurium-induced neuromuscular<br />
block. <strong>Anesthesiology</strong> 2002;96:45–50.<br />
65. Kopman AF, Yee PS, Neuman GG. Relationship of the<br />
train-of-four fade ratio to clinical signs and symptoms of<br />
residual paralysis in awake volunteers. <strong>Anesthesiology</strong> 1997;<br />
86:765–771.<br />
66. Stone JG, Matteo RS, Ornstein E, et al. Aging alters the<br />
pharmacokinetics of pyridostigmine. Anesth Analg 1995;<br />
81:773–776.<br />
67. Cronnelly R, Stanski DR, Miller RD, et al. Pyridostigmine<br />
kinetics with and without renal function. Clin Pharmacol<br />
<strong>The</strong>r 1980;28:78–81.<br />
68. Muravchick S, Owens WD, Felts JA. Glycopyrrolate and<br />
cardiac dysrhythmias in geriatric patients after reversal<br />
of neuromuscular blockade. Can Anaesth Soc J 1979;26:<br />
22–25.<br />
69. Owens WD, Waldbaum LS, Stephen CR. Cardiac dysrhythmias<br />
following reversal of neuromuscular blocking agents<br />
in the geriatric patient. Anesth Analg 1978;57:186–190.<br />
70. Simpson KH, Smith RJ, Davies LF. Comparison of the effects<br />
of atropine and glycopyrrolate on cognitive function following<br />
general anesthesia. Br J Anaesth 1987;59:966–969.<br />
71. Baraka A, Yared JP, Karam AM, et al. Glycopyrrolateneostigmine<br />
and atropine-neostigmine mixtures affect postanesthesia<br />
arousal times differently. Anesth Analg 1980;59:<br />
431–434.<br />
72. Berg H, Viby-Mogensen J, Roed Mortensen CR, et al.<br />
Residual neuromuscular block is a risk factor for postoperative<br />
pulmonary complications: a prospective, randomized<br />
and blinded study of postoperative complications after atracurium,<br />
vecuronium and pancuronium. Acta Anaesthesiol<br />
Scand 1997;41:1095–1103.<br />
73. Lunn JN, Hunter AR, Scott DB. Anaesthesia-related surgical<br />
mortality. Anaesthesia 1983;38:1090–1096.<br />
74. Cooper AL, Leigh JM, Tring IC. Admissions to the intensive<br />
care unit after complications of anesthetic techniques over<br />
10 years. Anaesthesia 1989;44:953–958.
18. Relaxants and <strong>The</strong>ir Reversal Agents 277<br />
75. Tiret L, Nivoche Y, Hatton F, Desmonts JM, Vourch G.<br />
Complications related to anesthesia in infants and children:<br />
a prospective survey in 40,240 anaesthetics. Br J Anaesth<br />
1988;61:263–269.<br />
76. Eriksson LI, Sundman E, Olsson R, et al. Functional assessment<br />
of the pharynx at rest and during swallowing in partially<br />
paralyzed humans: simultaneous videomanometry<br />
and mechanomyography of awake human volunteers. <strong>Anesthesiology</strong><br />
1997;87:1035–1043.<br />
77. Sundman E, Witt H, Olsson R, et al. <strong>The</strong> incidence and<br />
mechanisms of pharyngeal and upper esophageal dysfunction<br />
in partially paralyzed humans: pharyngeal videoradi -<br />
ography and simultaneous manometry after atracurium.<br />
<strong>Anesthesiology</strong> 2000;92:977–984.<br />
78. Wyon N, Joensen H, Yamamoto Y, Lindahl SG, Eriksson LI.<br />
Carotid body chemoreceptor function is impaired by<br />
vecuronium during hypoxia. <strong>Anesthesiology</strong> 1998;89:1471–<br />
1479.
19<br />
Management of <strong>Regional</strong> <strong>Anesthesia</strong><br />
Bernadette Veering<br />
<strong>The</strong>re has been a dramatic increase in the elderly population<br />
throughout the past century. In one century, the<br />
number of persons aged 65 years or older has increased<br />
three times. Patients aged 85 and older are the most<br />
rapidly growing age group. By 2030, up to 20% of Western<br />
populations will be more than 65 years of age. 1 This situation<br />
has led to a progressive increase in the number of<br />
surgical interventions in elderly people. It has been estimated<br />
that more than half of the population older than<br />
65 years will require surgical intervention at least once<br />
during the remainder of their lives. 2<br />
<strong>Regional</strong> anesthesia is frequently used in elderly<br />
patients, especially during genitourologic and gynecologic<br />
procedures, orthopedic surgery, cataract extraction,<br />
and inguinal hernia repairs. Knowledge of the age-related<br />
effects is important with respect to the design of an<br />
optimal regional anesthetic regimen in elderly patients.<br />
Age-Related Changes Relevant to<br />
<strong>Regional</strong> <strong>Anesthesia</strong><br />
Anatomic and physiologic changes, associated with<br />
advancing age, may affect the nerve block characteristics<br />
and the pharmacokinetics after administration of local<br />
anesthetics (Figure 19-1). A declining number of neurons,<br />
deterioration in myelin sheaths in the dorsal and ventral<br />
roots, changes in the anatomy of the spine, and intervertebral<br />
foramina may contribute to altered nerve block<br />
characteristics after a regional anesthetic procedure. 3,4<br />
Furthermore, the number of axons in peripheral nerves<br />
decreases with advancing age, and the conduction velocity<br />
diminishes, particularly in motor nerves. 5,6 With<br />
increasing age, changes in the connective tissue ground<br />
substances may result in changes in local distribution,<br />
i.e., in the distribution rate of the local anesthetic from<br />
the site of injection (the epidural space) to the sites<br />
of action. 3<br />
With aging, the dura becomes more permeable to local<br />
anesthetics because of enlarged arachnoid villi. 7 Aging is<br />
possibly associated with a reduction of the total volume<br />
of cerebrospinal fluid (CSF) and with an increase of its<br />
specific gravity. 8,9<br />
Central Neural Blockade<br />
Epidural <strong>Anesthesia</strong><br />
<strong>The</strong> spread of analgesia increases with advancing age<br />
after epidural administration of a fixed dose of a local<br />
anesthetic solution (Figure 19-2). 10–14 Recently, it was<br />
demonstrated that the spread of analgesia was also<br />
greater in elderly patients than in younger patients after<br />
epidural anesthesia with the relatively new long-acting<br />
local anesthetics ropivacaine and levobupivacaine. 15,16<br />
Furthermore, elderly patients have a faster onset of analgesia<br />
in the caudad segments and the rate of regression<br />
of analgesia is prolonged. However, the total time for<br />
recovery from analgesia is not affected by age. <strong>The</strong> motor<br />
block profile associated with epidural anesthesia alters<br />
with age as well. With epidural ropivacaine and bupivacaine,<br />
an enhanced intensity of motor blockade is shown<br />
with advancing age. 15 With bupivacaine, the onset of<br />
motor blockade is faster in the oldest compared with the<br />
youngest patients. 11<br />
Elderly patients exhibit anatomic and physiologic<br />
changes that influence the clinical course during epidural<br />
anesthesia. (See section on age-related changes relevant<br />
to regional anesthesia.) In older patients, the longitudinal<br />
spread of the local anesthetic in the epidural space is<br />
promoted by sclerosis and calcification of the intervertebral<br />
foramina and a reduced fatty tissue content of the<br />
epidural space. A more compliant and less resistant epidural<br />
space with advancing age may also contribute to<br />
this enhanced spread in the elderly. 17 <strong>The</strong> clinical course<br />
of epidural anesthesia may be further influenced by a<br />
278
19. Management of <strong>Regional</strong> <strong>Anesthesia</strong> 279<br />
Figure 19-1. Factors that can modify epidural and spinal anesthesia<br />
in elderly patients.<br />
shift of the site of action from a predominantly paravertebral<br />
site in the young to a subdural or transdural site in<br />
the elderly. Factors causing extensive spread are accelerated<br />
by arteriosclerosis and diabetes, both of which cause<br />
premature aging. 18<br />
Epinephrine is used frequently in the epidural test<br />
dose as a marker of intravascular injection. A given dose<br />
of epinephrine will not be totally reliable in older patients,<br />
because of decreased beta-adrenergic responsiveness. 19<br />
Patient-controlled epidural analgesia has been shown<br />
to be effective in elderly patients in the management<br />
of pain after major surgery. 20 Because elderly patients<br />
exhibit an increased sensitivity to opioids, 21 it has been<br />
suggested to reduce the bolus dose and infusion rate<br />
of opioids up to 50% when administered to the elderly.<br />
Patient-controlled epidural analgesia technique can<br />
be used only in elderly patients who can participate in<br />
self-medication, which excludes those with cognitive<br />
dysfunction. 22<br />
Spinal <strong>Anesthesia</strong><br />
Spinal anesthesia is frequently applied for lower abdominal,<br />
urologic, and lower limb surgery in older patients.<br />
<strong>The</strong> effect of age on the clinical profile of spinal anesthesia<br />
depends on the baricity of the injected solutions. With<br />
isobaric solutions, the effect of age on the maximal height<br />
of spinal analgesia is marginal. 23–25 With glucose-free<br />
0.5% bupivacaine, which acts as a slightly hypobaric solution<br />
at body temperature, the spread of analgesia is unaltered<br />
with age. 23,24 However, with a solution of isobaric<br />
2% mepivacaine, a slightly higher level of sensory analgesia<br />
has been found. 25 <strong>The</strong> caudad spread of analgesia<br />
as well as the development of motor blockade occurs<br />
more rapidly in older patients during spinal anesthesia<br />
with glucose-free bupivacaine. 23,24 <strong>The</strong> effect of age on the<br />
spread of analgesia is more pronounced when hyperbaric<br />
solutions are used. 26–28 With a hyperbaric solution of bupivacaine,<br />
the level of analgesia increases with age, extending<br />
some 3–4 segments higher in elderly as compared to<br />
young adult patients. However, because of profound<br />
interindividual variability, the predictability of the analgesia<br />
levels that will be reached in an individual patient<br />
is low. In addition, a quicker onset time of motor block<br />
has been found in older patients. With both hyperbaric<br />
and glucose-free bupivacaine solutions, the duration of<br />
analgesia of the T12 dermatome is prolonged, which<br />
allows more time for operations on the lower abdominal<br />
or inguinal region in older patients. Addition of adjuvants<br />
to spinal solutions may prolong the duration of neural<br />
blockade. Addition of epinephrine to glucose-free bupivacaine<br />
solutions increases the duration of analgesia in<br />
elderly patients. 29 However, addition of clonidine is associated<br />
with prolongation of motor block. 30<br />
<strong>The</strong> effects of hypobaric spinal anesthetic solutions are<br />
probably less reliable in the elderly because of the higher<br />
average specific gravity and greater individual variation<br />
in the volume of CSF.<br />
Upper level of analgesia<br />
T-1<br />
T-2<br />
T-3<br />
T-4<br />
T-5<br />
T-6<br />
T-7<br />
T-8<br />
T-9<br />
T-10<br />
T-11<br />
T-12<br />
L-1<br />
r = 0.63<br />
p = 0.002<br />
0 20 40 60 80<br />
Age (years)<br />
Figure 19-2. Relationship between the upper level of analgesia<br />
and age after epidural administration of 0.5% bupivacaine.<br />
(Reprinted with permission from Veering et al. 11 Copyright ©<br />
Lippincott Williams & Wilkins.)
280 B. Veering<br />
A<br />
B<br />
Figure 19-3. Duration of complete sensory block (CSB) (A) or motor block (CMB) (B) and age. (Reprinted with permission<br />
from Paqueron et al. 31 Copyright © Lippincott Williams & Wilkins.)<br />
Peripheral Nerve Blockade<br />
For peripheral blocks, the major physiologic changes are<br />
in the response of the nerves themselves to local anesthetics.<br />
By the age of 90 years, one third of the myelinated<br />
fibers have disappeared from peripheral nerves. In addition,<br />
conduction velocity, especially of the motor nerve,<br />
decreases with age. 6<br />
After administration of ropivacaine at a brachial plexus<br />
block, the duration of sensory block and motor block is<br />
greater than in younger patients (Figure 19-3). 31 Onset<br />
time of complete motor block is shorter in elderly patients.<br />
Further study is indicated to investigate the effect of age<br />
on the characteristics of other peripheral blocks.<br />
Pharmacology<br />
<strong>Regional</strong> anesthetic blocks are performed by injecting<br />
local anesthetic agents close to nerve trunks. Two quite<br />
separate processes simultaneously occur after injection.<br />
While there is a vascular uptake of the drug into the systemic<br />
circulation, which removes the drug from the injection<br />
site, the drug also diffuses directly to neural structures,<br />
where the therapeutic action occurs. This is the pharmacodynamic<br />
part. <strong>The</strong> uptake into the systemic circulation<br />
may lead to side effects.<br />
Pharmacokinetics of Local Anesthetics<br />
Changes in body composition and characteristics of<br />
tissues and organs within the body may have an impact<br />
on the rate and extent of systemic absorption, distribution,<br />
and elimination of local anesthetics used for regional<br />
anesthesia. Pharmacokinetic and/or pharmacodynamic<br />
changes, which may occur with increasing age, could alter<br />
the clinical profile of local anesthetics after a regional<br />
anesthetic procedure.<br />
<strong>The</strong> effect of age on the pharmacokinetics of local<br />
anesthetics may be different in females than in males and<br />
may be influenced by concomitant diseases.<br />
Systemic Absorption<br />
Knowledge of the pharmacokinetics of local anesthetics<br />
is of importance in relation to the clinical profile, in particular,<br />
the duration of action, and in relation to the risk<br />
of systemic side effects and toxicity. 32 In this respect, both<br />
the systemic absorption, i.e., the uptake from the perineural<br />
site of administration into the blood, and the systemic<br />
disposition (distribution and elimination) must be considered.<br />
Peak plasma concentrations of lidocaine and bupivacaine<br />
after epidural or caudal administration change<br />
little, if at all, with increasing age. 11,33–35 However, the terminal<br />
half-life of bupivacaine increases after both epidural<br />
and subarachnoid administration, suggesting that the<br />
absorption rate of bupivacaine decreases with advancing<br />
age. 11,24,26<br />
Details on the absorption rate cannot be derived from<br />
the plasma concentration curves, unless a detailed description<br />
of the disposition is available. A stable isotope<br />
method allows simultaneous studies of the absorption<br />
and disposition. 36,37 Local anesthetics exhibit a biphasic<br />
absorption pattern, a fast initial absorption phase followed<br />
by a slower absorption phase after epidural and<br />
subarachnoid administration. 36–38 <strong>The</strong> initial fast absorption<br />
rate is a reflection of the high initial concentration<br />
gradient and the large vascularity of the epidural space.<br />
With spinal anesthesia, the initial absorption is much<br />
slower because the subarachnoid space has a poor perfusion.<br />
<strong>The</strong> slower second absorption phase is believed to<br />
occur from slow uptake of local anesthetics. Whereas a<br />
previous study on the systemic absorption and disposition<br />
kinetics of bupivacaine after epidural administration<br />
did not reveal an effect of age on the absorption kinetics,<br />
12 a recent study demonstrated a significant effect on
19. Management of <strong>Regional</strong> <strong>Anesthesia</strong> 281<br />
the rapid initial absorption kinetics of levobupivacaine<br />
after epidural administration. 16 After subarachnoid<br />
administration, the mean absorption has been shown to<br />
be shorter in elderly patients because of a faster late<br />
absorption rate. 28 Based on the faster absorption, one<br />
might expect a shorter duration of spinal and epidural<br />
anesthesia in older patients; however, this has not been<br />
demonstrated.<br />
<strong>The</strong> epidural absorption studies with bupivacaine and<br />
levobupivacaine and the spinal absorption study with<br />
bupivacaine demonstrate an increased sensitivity in the<br />
elderly that does not seem to be related to the impairment<br />
of vascular absorption. <strong>The</strong>refore, changes in the<br />
clinical profile with epidural and spinal anesthesia are<br />
best explained by anatomic considerations and possibly<br />
pharmacodynamic changes in the elderly rather than by<br />
pharmacokinetic changes in the elderly.<br />
Plasma clearance (mL.min –1 )<br />
1000<br />
800<br />
600<br />
400<br />
200<br />
y = –4.39x + 671.5<br />
r = –0.57<br />
p = 0.001<br />
Systemic Disposition<br />
20<br />
Figure 19-4. Relationship between total plasma clearance<br />
and age. (Reprinted with permission from Veering et al. 11<br />
Copyright © Lippincott Williams & Wilkins.)<br />
Age-related changes in drug distribution may result from<br />
changes in body composition and/or changes in drug<br />
binding and tissue perfusion. As fatty tissue increases, the<br />
volume of distribution of lipophilic local anesthetics<br />
would be expected to increase. 39 Such an increase has<br />
been demonstrated for lidocaine. 40 However, others<br />
observed an unchanged volume of distribution of intravenously<br />
(IV) administered lidocaine. 41,42<br />
A second factor influencing distribution is the plasma<br />
binding of drugs. <strong>The</strong> main binding protein for local anesthetic<br />
agents is α 1 -acid glycoprotein (AAG), an acute<br />
phase reactant protein. 43 <strong>The</strong> plasma protein binding of<br />
lidocaine tends to increase slightly with age. 44 However,<br />
age does not influence the serum protein binding of bupivacaine.<br />
45 This is in keeping with the lack of effect of age<br />
on AAG concentrations. 46 Any effect of age on AAG<br />
concentrations is likely to be relatively small, and therefore<br />
age-related changes in protein binding and in volume<br />
of distribution of local anesthetic agents that bind to<br />
AAG are more likely related to other factors. 47,48<br />
Local anesthetics are predominantly eliminated by<br />
metabolism. 49 <strong>The</strong> effect of age on the metabolism and<br />
excretion of local anesthetics is related to changes in<br />
hepatic function. Decreases in hepatic mass, hepatic blood<br />
flow, and hepatic enzyme activity with advancing age may<br />
result in impairment of metabolism. For local anesthetics<br />
that exhibit a high rate of hepatic extraction (e.g., lidocaine),<br />
the rate-limiting step in metabolism is hepatic<br />
blood flow. 50 Accordingly, the decrease of liver blood flow<br />
is associated with a decline in clearance of lidocaine with<br />
advancing age. 51<br />
<strong>The</strong>re is also a gradual decline in hepatic mass, 52<br />
and, as a consequence, the clearance of local anesthetics<br />
with relatively low hepatic extraction ratios, which are<br />
mostly dependent on metabolizing hepatic enzyme activity,<br />
may decrease with age. Total plasma clearance of<br />
bupivacaine has been found to decrease with increasing<br />
age after epidural and subarachnoid administration<br />
(Figure 19-4). 11,24,26,28<br />
Because bupivacaine has a relatively low hepatic extraction<br />
ratio, the observed age-related decline in clearance is<br />
likely the result of a change in drug-metabolizing hepatic<br />
enzyme activity and/or serum protein binding of bupivacaine,<br />
rather than from an alteration in the liver blood flow.<br />
However, age has not been shown to affect the protein<br />
binding of bupivacaine. 45 <strong>The</strong>refore, the observed agerelated<br />
decline in clearance probably reflects a concomitant<br />
decline in hepatic enzyme activity or capacity.<br />
<strong>The</strong> altered pharmacokinetics in elderly patients<br />
(uncomplicated by disease) seem to be relatively unimportant<br />
with a single epidural injection. <strong>The</strong> local anesthetic<br />
doses need not be modified because of the resulting<br />
plasma concentrations.<br />
However, taking into account the age-related decreased<br />
clearance of lidocaine and bupivacaine, administration of<br />
multiple intermittent injections or continuous epidural<br />
infusion of these local anesthetics for prevention of postoperative<br />
pain might lead to increased accumulation of<br />
these agents. 34 Consequently, the potential of developing<br />
side effects, including toxicity, might be enhanced.<br />
Long-term epidural infusion of bupivacaine for the<br />
relief of postoperative pain has been shown to result in<br />
progressively increasing plasma concentrations. 53,54 This<br />
40<br />
Age (years)<br />
60<br />
80
282 B. Veering<br />
probably reflects a continuous change in the pharmacokinetics,<br />
as a result of changes in the degree of protein<br />
binding. Changes in the protein binding of bupivacaine<br />
are likely to occur in the postoperative phase, because<br />
plasma concentrations of AAG increase progressively<br />
during the first postoperative days. 55 It should be emphasized,<br />
however, that postoperative increases in total<br />
plasma concentrations are not accompanied by similar<br />
increases in the pharmacologically more relevant unbound<br />
(free) plasma concentrations.<br />
However, the concentration of free unbound lidocaine<br />
increases in elderly patients during continuous epidural<br />
infusion of lidocaine for postoperative pain (Figure<br />
Total Lidocaine Concentration (mg/L)<br />
Free-Lidocaine Concentration (mg/L)<br />
4<br />
3<br />
2<br />
1<br />
0<br />
A 0 30 60 90 120 150 180 240 300 min<br />
0.5<br />
0.4<br />
0. 3<br />
0.2<br />
0.1<br />
elder<br />
middle-age<br />
0<br />
B 0 30 60 90 120 150 180 240 300 min<br />
Figure 19-5. Mean plasma concentrations of total (A) and free<br />
(B) lidocaine after epidural administration to elderly or middleaged<br />
male patients. *p < 0.05, compared with the middle-aged<br />
group. Bars represent standard errors. (Reprinted with permission<br />
from Fukuda et al. 56 Copyright © 2003. With permission<br />
from the American Society of <strong>Regional</strong> <strong>Anesthesia</strong> and Pain<br />
Medicine.)<br />
19-5). 56 <strong>The</strong> upward trend of free lidocaine concentration<br />
in elderly patients is not caused by differences in AAG,<br />
but likely reflects a lower metabolic activity. <strong>The</strong> ratios of<br />
the total monoethylglycinexylidide (MEGX)/free lidocaine,<br />
which reflect the ability to metabolize lidocaine,<br />
were lower in the elderly group than in the middle-aged<br />
group. So caution must be exercised during continuous<br />
epidural infusion of lidocaine in geriatric patients.<br />
Problems<br />
Performing epidural and spinal anesthesia may be more<br />
difficult in elderly patients. It is often not easy to position<br />
the elderly patient appropriately because of the anatomic<br />
distortion, particularly curvature or rotation of the spine,<br />
that is found in many older people. <strong>The</strong> inability of the<br />
elderly patient to flex the back as much as the younger<br />
patient makes axial blockade difficult. Aging is frequently<br />
accompanied by an increase in the degree of lumbar lordosis<br />
often attributable to osteoporosis. Calcification of<br />
the interspinous ligaments and ligamentum flavum, the<br />
gradual stenosing of the intervertebral foramina in the<br />
elderly, make needle placement and advancement more<br />
complicated.<br />
<strong>The</strong> most common complication of spinal anesthesia is<br />
postspinal headache. Although the incidence is largely<br />
related to the size of the needle used, the incidence is<br />
decreased with age, possibly because of a decreased elasticity<br />
of the cranial tissues. 57 Consequently, less CSF leaks<br />
away from the subarachnoid space in older patients.<br />
Decreasing pain sensibility with increasing age and a<br />
decrease in distensibility of pain-sensitive structures in<br />
the cranium are also considered to contribute.<br />
Hypotension<br />
Hypotension is the most common cardiovascular disturbance<br />
associated with central neural blockade with a<br />
particularly frequent incidence in the elderly. It occurs<br />
from decreases in systemic vascular resistance and central<br />
venous pressure from sympathetic block with vasodilatation<br />
and redistribution of central blood volume to lower<br />
extremities and splanchnic beds. 58 Hypotension after<br />
spinal anesthesia is a common problem, with an incidence<br />
of 15.3%–33%. 59,60 High levels of analgesia and old<br />
age seem to be the two main factors associated with the<br />
development of hypotension. 60 A greater spread of analgesia<br />
with epidural ropivacaine in elderly patients is<br />
accompanied with a higher incidence of hypotension and<br />
bradycardia (Figure 19-6). 15 This problem is a particularly<br />
important issue in elderly patients with cardiovascular<br />
disease such as hypertension, because the risk for ischemia<br />
secondary to hypotension is increased. 61,62 Moreover,<br />
morbidity and mortality rates in elderly patients
T1<br />
T2<br />
T3<br />
T4<br />
T5<br />
T6<br />
T7<br />
T8<br />
T9<br />
T10<br />
T11<br />
T12<br />
L1<br />
L2<br />
L3<br />
19. Management of <strong>Regional</strong> <strong>Anesthesia</strong> 283<br />
Max. decrease in MAP (mm Hg)<br />
A<br />
70<br />
60<br />
50<br />
40<br />
30<br />
20<br />
10<br />
0<br />
15 25 35 45 55 65 75 85<br />
Age (years)<br />
Figure 19-6. (A) Relationship between the maximum decrease<br />
of the mean arterial blood pressure (MAP; mm Hg) during<br />
the first hour after the induction of epidural anesthesia and age.<br />
(B) Relationship between the maximum decrease of the MAP<br />
during the first hour after the induction of epidural anesthesia<br />
Max. decrease in MAP (mm Hg)<br />
B<br />
70<br />
60<br />
50<br />
40<br />
30<br />
20<br />
10<br />
0<br />
Dermatome<br />
and the highest level of analgesia for the three age groups<br />
(• = group 1, 19–40 years; o = group 2, 41–60 years; = group<br />
3, >61 years). (Adapted with permission from Simon et al. 15<br />
Copyright © Lippincott Williams & Wilkins.)<br />
with hypertension might be more frequent than those in<br />
elderly patients without hypertension because of the<br />
marked intraoperative hemodynamic lability. 63,64<br />
Marked hypotension is especially harmful to elderly<br />
patients with limited cardiac reserve. Structural changes<br />
in the arterioles and changes in the autonomic nervous<br />
system with increasing age may contribute to substantial<br />
hypotension in elderly patients. <strong>The</strong> elderly have increased<br />
resting sympathetic nervous system activity and associated<br />
increased norepinephrine release from nerve terminals.<br />
65,66 In addition, age-related baroreflex dysfunction<br />
may compromise arterial pressure homeostasis. 67 Hemodynamic<br />
instability after spinal anesthesia, therefore,<br />
might be exaggerated in the elderly because of larger<br />
decreases in systemic vascular resistance (Figure 19-7). 68<br />
Transthoracic electrical bioimpedance revealed that<br />
systolic blood pressure decreased by 25% as early as 6–9<br />
minutes after the block, indicating that patients should be<br />
monitored immediately after subarachnoid block. 69<br />
Treatment of Hypotension in the Elderly<br />
Common strategies used to prevent or reduce the incidence<br />
and severity of hypotension include IV fluid bolus<br />
and the use of vasopressors. Both prophylaxis and therapy<br />
should aim primarily at stabilizing or replenishing cardiac<br />
filling. Principally, this can be achieved either by increasing<br />
blood volume or by counteracting vasodilatation in<br />
the sympathicolytic regions with vasoconstrictor agents.<br />
It is common practice to give IV fluids before and during<br />
30<br />
Percentage Change from Control<br />
20<br />
10<br />
0<br />
–10<br />
–20<br />
–30<br />
–40<br />
–50<br />
–60<br />
**<br />
MAP SVR CO HR SV 9 EDV<br />
–0.4<br />
–10<br />
–10 EF<br />
–19<br />
–26 * *<br />
–33<br />
**<br />
**<br />
**<br />
* P < 0.05 vs control<br />
** P < 0.001 vs control<br />
Figure 19-7. Hemodynamic response to high spinal anesthesia<br />
in elderly men with cardiac disease. Decrease in systemic vascular<br />
resistance (SVR) and no decreases in cardiac output (CO)<br />
were primarily responsible for the large decrease in mean arterial<br />
blood pressure (MAP). Heart rate (HR) was unchanged;<br />
therefore, the decrease in cardiac output was attributable to a<br />
decrease in stroke volume (SV). <strong>The</strong> decrease in stroke volume<br />
was less than the decrease in end-diastolic volume (EDV)<br />
because the ejection fraction (EF) increased. (Reprinted with<br />
permission from Rooke et al. 68 Copyright © Lippincott Williams<br />
& Wilkins.)
284 B. Veering<br />
spinal anesthesia to prevent hypotension. In elderly<br />
patients, however, fluid preloading is not always effective.<br />
70,71 Volume loading does not always prevent the<br />
decrease in systemic vascular resistance caused by spinal<br />
anesthesia but, in fact, may cause further decreases. 72<br />
Irrespective of whether crystalloid, colloid, or no prehydration<br />
is used, a high incidence of hypotension follows<br />
spinal anesthesia in normovolemic elderly patients undergoing<br />
elective procedures. Additionally, the attenuated<br />
physiologic reserve in elderly patients seems to make<br />
them less able to increase cardiac output in response to<br />
volume loading.<br />
Administration of a colloid preload during the induction<br />
phase of the block, usually about 7 mL/kg, has been<br />
recommended in elderly patients to compensate for any<br />
decrease in central venous pressure. 73,74 It should be<br />
emphasized, however, that rapid volume preloading constitutes<br />
a potential risk in older patients with limited<br />
cardiac reserve. At the same time, an alpha agonist should<br />
be used to reverse any decrease in vascular resistance.<br />
<strong>The</strong> degree of hypotension correlates with the level of<br />
sympathetic block, which is generally two to four segments<br />
higher than the level of analgesia. 75 From a clinical<br />
point of view, it is, therefore, important to limit the level<br />
of sympathetic block. <strong>The</strong> rationale for combining local<br />
anesthetics with adjuvant drugs is to use lower doses of<br />
each agent and to preserve analgesia with fewer side<br />
effects. A “minidose” of 4 mg of bupivacaine in combination<br />
with 20 µg of fentanyl provided spinal anesthesia for<br />
surgical repair of hip fracture in the elderly. 76 <strong>The</strong> minidose<br />
combination caused dramatically less hypotension<br />
than 10 mg of bupivacaine and nearly eliminated the need<br />
for vasopressor support of blood pressure.<br />
Changes in the technique of hyperbaric bupivacaine<br />
spinal anesthesia by injection of hyperbaric bupivacaine<br />
either at a lower L4-5 interspace than the usual (L3-4)<br />
lumbar interspace 77 or different periods of sitting after<br />
injection had little, if any, influence on final analgesia levels<br />
and on hemodynamic changes in elderly patients. 78<br />
However, unilateral segmental spinal anesthesia may<br />
result in more restricted anesthetic spread with less<br />
hemodynamic variability. Unilaterality can be reliably<br />
produced with small doses of hyperbaric solutions and by<br />
prolonged lateral positioning. 79<br />
Continuous spinal anesthesia (CSA) is a technique that<br />
allows one to titrate local anesthetic solutions and thus<br />
reduce the dosage of local anesthetics, providing a more<br />
adequate analgesia with a lower level of sympathetic<br />
blockade and minimizing arterial hypotension and bradycardia.<br />
80 Also, combined spinal-epidural technique<br />
(CSE) enables smaller intrathecal doses to be used with<br />
the option of topping up the epidural catheter if the block<br />
is inadequate. When hemodynamic stability is critical,<br />
CSE or CSA may be the techniques of choice for lower<br />
limb surgery in the elderly patients.<br />
Hypothermia<br />
As with general anesthesia, advanced age is associated<br />
with hypothermia during epidural and spinal anesthesia.<br />
This should be attributed to a variety of factors such as<br />
a physiologic decrease in basal metabolism, changes in<br />
the thermoregulatory center, and diminished muscular<br />
mass. 81–83 Also, elderly patients may be especially at risk<br />
of hypothermia because low core temperature may not<br />
initiate autonomic protective responses.<br />
Advancing age and high-level spinal blockade are<br />
associated with a significant decrease of thermoregulatory<br />
threshold (Figure 19-8). 83 <strong>The</strong> shivering threshold<br />
is decreased in proportion with the level of spinal blockade<br />
because the vasomotor tone is inhibited below the<br />
A<br />
Figure 19-8. Advanced age (A) and high level of spinal block<br />
(B) were significant predictors of core hypothermia at admission<br />
to the postanesthesia care unit by linear regression.<br />
B<br />
(Reprinted with permission from Frank et al. 81 Copyright ©<br />
Lippincott Williams & Wilkins.)
19. Management of <strong>Regional</strong> <strong>Anesthesia</strong> 285<br />
level of spinal block. 84,85 So the greater the proportion<br />
of the body that is blocked, the greater the level of thermoregulatory<br />
dysfunction that can be expected. Shivering<br />
and increase in oxygen demand further compromise<br />
patients, especially those with known cardiovascular<br />
diseases.<br />
Controlling and monitoring body temperature in older<br />
patients and in those with high spinal blocks could<br />
decrease risk of hypothermia and its complications.<br />
Sedation<br />
Prompt and complete postoperative recovery of mental<br />
function is particularly important in elderly patients if the<br />
mental condition is already compromised by age-related<br />
disease or drug therapy. 22<br />
Elderly people are prone to confusion and are often<br />
sensitive to low doses of sedative drugs. <strong>Geriatric</strong> patients<br />
show an increased responsiveness for benzodiazepine<br />
compounds. 86 <strong>The</strong>refore, smaller doses and more delayed<br />
increments must be used. Also, caution should be used<br />
when benzodiazepines are given as premedication in<br />
geriatric patients.<br />
<strong>The</strong> pharmacokinetics and the pharmacodynamics of<br />
propofol change dramatically with age. 87 Elderly patients<br />
are more sensitive to the hypnotic and electroencephalographic<br />
effects of propofol than younger persons. Older<br />
patients require lower doses for any given effect, in many<br />
cases as little as 30% of the expected “standard” dose.<br />
Propofol infusion for sedation during spinal anesthesia<br />
resulted in a delayed recovery time in elderly patients<br />
compared with younger patients. 88 Elderly patients may<br />
require a more prolonged observation period after cessation<br />
of sedation with propofol.<br />
Postoperative Cognitive Function<br />
A proportion of mostly elderly orthopedic patients<br />
develop early postoperative cognitive dysfunction, confusion,<br />
and delirium, which are all nonspecific symptoms of<br />
central nervous system dysfunction. 89–91 This postoperative<br />
mental condition may persist for several days to<br />
several weeks and can result in increased morbidity,<br />
delayed functional recovery, and prolonged hospital stay.<br />
<strong>The</strong> mechanism of early postoperative confusion after<br />
orthopedic surgery and other operations is probably<br />
multifactorial. 92,93<br />
In most cases, recovery of cognitive function is prompt<br />
and complete within 1 week in elderly patients. Neither<br />
the choice of anesthetic technique nor the modality used<br />
for the management of postoperative pain seems to be<br />
an important determinant of postoperative confusion in<br />
elderly patients. 89,92,93<br />
<strong>The</strong> factors that likely explain the development of<br />
postoperative brain dysfunction are age, hospitalization,<br />
and extension and duration of surgery.<br />
Beneficial Aspects of<br />
<strong>Regional</strong> <strong>Anesthesia</strong><br />
<strong>The</strong> use of both intraoperative and postoperative regional<br />
analgesic techniques provides physiologic benefits and<br />
may attenuate the pathophysiology that occurs after<br />
surgery. 94 Local anesthetic agents have the capability to<br />
block afferent and efferent signals to and from the spinal<br />
cord, thus suppressing the surgical stress response (Table<br />
19-1). 95 <strong>The</strong> cascade of events unleashed during the stress<br />
response to surgical events can be blunted with epidural<br />
anesthesia. 95,96 One such effect is to decrease postoperative<br />
hypercoagulability. Epidural or spinal analgesia<br />
and anesthesia attenuates the hypercoagulable perioperative<br />
state by increasing fibrinolysis and decreasing<br />
coagulability. 97–99<br />
<strong>Regional</strong> anesthesia techniques provide excellent pain<br />
management, thus sparing the sedative effects of opioids<br />
and facilitating early postoperative mobilization for a<br />
faster convalescence. 96,100<br />
When compared with general anesthesia, intraoperative<br />
blood loss is reduced by spinal or epidural anesthesia,<br />
especially in patients undergoing hip replacement<br />
surgery. 101,102 This is attributed to lower venous pressures<br />
Table 19-1. Effects of analgesic techniques on postoperative surgical stress responses.<br />
Type of analgesia Endocrine responses Metabolic responses Inflammatory responses<br />
Systemic opioid (PCA or intermittent)<br />
↓<br />
NSAID ↓ ↓<br />
Epidural opioid<br />
↓<br />
Lumbar epidural local anesthetics<br />
(lower extremity surgery)<br />
↓↓↓<br />
Thoracic epidural local anesthetics<br />
(abdominal surgery)<br />
↓↓<br />
Source: Adapted with permission from Kehlet and Holte. 96 Copyright ® <strong>The</strong> Board of Management and Trustees of the British Journal of<br />
Anaesthesia. Reproduced by permission of Oxford University Press/British Journal of Anaesthesia.<br />
PCA = patient-controlled analgesia, NSAID = nonsteroidal antiinflammatory drug, ↓ = small effect, ↓↓ = moderate effect, ↓↓↓ = major effect.
286 B. Veering<br />
during central neural blockade compared with general<br />
anesthesia.<br />
Compared with general anesthesia, epidural 103 and<br />
spinal anesthesia 104 are not associated with changes in<br />
arterial blood gases either during or after the operation,<br />
indicating a preservation of pulmonary gas exchange. 105<br />
Cardiovascular System<br />
Thoracic epidural anesthesia (TEA) can produce a selective<br />
segmental blockade of the cardiac sympathetic nerves<br />
(T1–T5), with loss of chronotropic and inotropic drive to<br />
the heart. 58 Animal studies have been performed to test<br />
whether sympathetic block lessens ischemia. 106,107 Acute<br />
coronary occlusion during TEA resulted in redistribution<br />
of flow to the epicardium away from the endocardium,<br />
affecting beneficially collateral blood flow during myocardial<br />
ischemia. 106 Under the influence of TEA, the size<br />
of induced myocardial infarcts was smaller after experimental<br />
coronary occlusion in dogs. 107<br />
High TEA in humans improved an ischemia-induced<br />
left ventricular dysfunction; reduced electrocardio -<br />
graphic, echocardiographic, and angiographic signs of<br />
coronary insufficiency decreased the incidence of arrhythmias<br />
and provided relief of ischemic chest pain. 108–111<br />
<strong>The</strong>se results show that TEA with an associated cardiac<br />
sympathetic blockade improves the oxygen supply–<br />
demand ratio. 112<br />
Pulmonary System<br />
Thoracic and lumbar epidural anesthesia are often combined<br />
with general anesthesia in patients undergoing<br />
upper abdominal surgery, vascular surgery, and kidney<br />
surgery. Epidural anesthesia per se has little effect on<br />
respiration in patients with preexisting lung disease. Most<br />
of the respiratory changes associated with epidural anesthesia<br />
are directly attributed to motor block of the muscles<br />
of respiration. 58<br />
Perhaps the most profound effect of major abdominal<br />
and thoracic surgery on pulmonary function is a reduction<br />
in the functional residual capacity as a result of diaphragmatic<br />
dysfunction. This is caused by reflex inhibition<br />
of the phrenic nerve after major surgery, a decreased<br />
chest wall compliance, and pain-limited inspiration. 113<br />
Diaphragmatic activity increases after TEA, possibly<br />
because of the interruption of an inhibitory reflex of<br />
phrenic nerve motor drive, either related to direct deafferentation<br />
of visceral sensory pathways, or because<br />
of a diaphragmatic load reduction caused by increased<br />
abdominal compliance. 114,115<br />
Gastrointestinal System<br />
A TEA over T12 is associated with splanchnic sympathetic<br />
nervous blockade, which results in reduced inhibitory<br />
gastrointestinal tone and increased intestinal blood<br />
flow. 94,116 Blood flow to the bowel is a critical factor for<br />
gastrointestinal motility. Intestinal sympathectomy also<br />
results in a contracted bowel because of vagal predominance.<br />
All these factors result in a faster digestive<br />
transit. 116,117 In addition, TEA improves microvascular<br />
perfusion of the small intestine. 118<br />
Outcome: <strong>Regional</strong> Versus<br />
General <strong>Anesthesia</strong><br />
Generally, geriatric patients have a decreased functional<br />
reserve of organ systems and thus become increasingly<br />
intolerant to surgical stress. Local anesthetics have the<br />
capability to block afferent and efferent signals to and<br />
from the spinal cord, thus suppressing the surgical stress<br />
response and spinal reflex inhibition of diaphragmatic<br />
and gastrointestinal function.<br />
<strong>The</strong> question often asked is whether these men -<br />
tioned beneficial aspects of regional anesthesia make<br />
a difference in the outcome of surgical patients. To<br />
demonstrate superiority of one anesthetic technique<br />
over another technique, one needs to look at outcome<br />
results.<br />
Discrepancies exist between studies that have evaluated<br />
the early mortality, i.e., within 1 month, in elderly<br />
patients, after major orthopedic surgery under either<br />
regional (epidural or spinal) or general anesthesia (Table<br />
19-2). Several studies on elderly patients undergoing hip<br />
Table 19-2. Effect of anesthetic technique on postoperative mortality in elderly patients (age range: 60–90+).<br />
Mortality (%)<br />
Author Number of patients (reg/GA) Method 7 days (reg/GA) 30 days (reg/GA) 1 year (reg/GA)<br />
Sutcliffe 120 383/950 Prospective 9.4/8.8 36.9/32.6<br />
O’Hara et al. 119 3129/6206 Retrospective 1.6/1.3 5.4/4.4<br />
Gilbert et al. 123 430/311 Prospective 19.1/16.6<br />
Urwin et al. 122 1028/1005 Meta-analysis 6.4/9.4* 22.5/21<br />
Reg = regional anesthesia, GA = general anesthesia.<br />
*p < 0.05. Advantage regional anesthesia over general anesthesia.
19. Management of <strong>Regional</strong> <strong>Anesthesia</strong> 287<br />
fracture repair failed to reveal advantages of regional<br />
anesthesia compared with general anaesthesia. 119,120 With<br />
meta-analysis, it is possible to combine relevant data from<br />
several existing investigations in order to study the effect<br />
of specific techniques of anesthesia and to draw conclusions.<br />
121 A systemic review of randomized trials showed<br />
that regional anesthesia for hip fracture surgery was associated<br />
with a reduced early mortality and incidence of<br />
deep vein thrombosis in comparison with general anesthesia.<br />
122 <strong>The</strong> pattern of reduction in early mortality is<br />
possibly related to a decreased incidence of deep venous<br />
thrombosis. Long-term morbidity and mortality (2 months<br />
to 1 year) do not seem to be altered by the anesthetic<br />
type used during hip repair. 120,123<br />
Cardiac Outcome<br />
Cardiac morbidity is the most common cause of death<br />
after major surgical procedures. <strong>The</strong> incidence of cardiovascular<br />
diseases is high in elderly surgical populations<br />
undergoing peripheral vascular surgery of the lower<br />
extremity. Because perioperative sympathetic activation<br />
has a causative role in the development of myocardial<br />
ischemia and infarction, inhibition of this activation<br />
would be expected to reduce cardiac morbidity.<br />
<strong>The</strong>re has been an ongoing discussion as to whether<br />
regional anesthesia is superior to general anesthesia in<br />
patients at cardiac risk. Discrepancies exist between<br />
studies that have evaluated this effect, because most<br />
studies are insufficiently powered to demonstrate clinically<br />
and statistically significant benefits.<br />
<strong>The</strong> impact of anesthetic choice on cardiac outcome<br />
was studied in patients undergoing peripheral vascular<br />
surgery who had a likelihood of associated coronary<br />
artery disease. 124 In this study, patients were randomly<br />
assigned to be given general, epidural, or spinal anesthesia.<br />
<strong>The</strong>re was no significant difference among groups in<br />
cardiovascular morbidity and overall mortality. In another<br />
study, patients were randomized to receive general anesthesia<br />
combined with postoperative epidural analgesia or<br />
general anesthesia with on-demand narcotic analgesia<br />
(PCA). 125 <strong>The</strong> rates of cardiovascular, infectious, and<br />
overall postoperative complications, as well as duration<br />
of intensive care unit (ICU) stay, were significantly<br />
reduced in the general anesthesia–postoperative epidural<br />
analgesia group. In addition, the incidences of graft occlusion<br />
were reduced. However, in a comparable study, no<br />
difference was found in the incidence of cardiac ischemia<br />
in patients scheduled for elective vascular reconstruction<br />
of the lower extremities. 126<br />
However, the need for reoperation for graft failure was<br />
reduced in the epidural group. Park et al. 127 observed in<br />
a large, multiinstitutional clinical trial that epidural plus<br />
general anesthesia and postoperative epidural analgesia<br />
improved the perioperative cardiac outcome of elderly<br />
patients undergoing abdominal aortic operations compared<br />
with that of general anesthesia alone and postoperative<br />
systemic opioid analgesia.<br />
Beattie and colleagues 128 performed a meta-analysis to<br />
determine whether postoperative analgesia continued for<br />
more than 24 hours after surgery reduces postoperative<br />
myocardial infarction or in-hospital death. It seemed that<br />
thoracic epidural analgesia was superior to lumbar epidural<br />
analgesia in reducing postoperative myocardial<br />
infarction. <strong>The</strong>se findings suggest that in high-risk cardiac<br />
patients, thoracic epidural postoperative analgesia is warranted<br />
and should be used more widely.<br />
Early administration of continuous epidural analgesia<br />
was associated with a lower incidence of preoperative<br />
adverse cardiac events in elderly patients with hip fracture<br />
who had or were at risk for coronary artery disease. 129<br />
Although the study group was small, the results war -<br />
rant further study of preoperative analgesia in this<br />
population.<br />
Coagulation<br />
<strong>The</strong> risk and incidence of thromboembolic complications<br />
after lower body complications are lower in patients<br />
operated on under lumbar epidural and spinal anesthesia<br />
as compared with those given general anesthesia. 98,130,131<br />
<strong>The</strong> mechanism is probably a combination of improved<br />
lower extremity blood flow, favorable changes in coagulation<br />
and fibrinolysis, inhibition of thrombocyte aggregation,<br />
and decreasing blood viscosity. 97–99,132 In addition, the<br />
systemic absorption of epidurally administered local<br />
anesthetics, improved pain control, and earlier mobility<br />
likely decrease the incidence of clot formation. 133<br />
Pulmonary Outcome<br />
A major cause of postoperative complications is respiratory<br />
problems during the early postoperative recovery<br />
period.<br />
Decreased intubation times and ICU stays in patients<br />
with epidural anesthesia and analgesia after major<br />
abdominal surgery in elderly patients have been<br />
reported. 129,134 A recent meta-analysis of 48 randomized<br />
controlled clinical trials assessed improvements in pulmonary<br />
outcomes comparing systemic opioids, epidural<br />
opioid, and epidural local anesthetic. 135 Compared with<br />
those who received systemic opioids, patients who<br />
received postoperative epidural analgesia with local<br />
anesthetics had a significant reduction in the incidence<br />
of pulmonary complications, atelectasis, and pneumonia<br />
and increase in the postoperative partial pressure of<br />
oxygen. So continuous epidural local anesthetic or local<br />
anesthetic–opioid mixtures have been demonstrated to<br />
improve outcome by controlling postoperative pain, permitting<br />
earlier extubation, and reducing length of stay.
288 B. Veering<br />
Gastrointestinal Outcome<br />
Postoperative ileus is a major surgical morbidity following<br />
abdominal surgery. As a consequence, the length<br />
of stay of elderly patients may be prolonged in the<br />
hospital. Colonic motility is inhibited for 48–72 hours.<br />
<strong>The</strong> most frequently accepted theory is that abdominal<br />
pain activates a spinal reflex arc that inhibits intestinal<br />
motility. 136–138<br />
Randomized clinical trials that investigated the recovery<br />
of gastrointestinal function after abdominal and other<br />
types of surgery have consistently shown that the use of<br />
postoperative thoracic epidural analgesia with a local<br />
anesthetic-based regimen compared with systemic opioid<br />
analgesia will allow earlier return of gastrointestinal<br />
function and even discharge from the hospital. 96,117,139<br />
Conclusion<br />
This chapter has outlined several aspects of regional<br />
anesthesia in elderly patients. <strong>The</strong> general consensus is<br />
that elderly patients are more sensitive to local anesthetic<br />
agents and show altered clinical profiles. Older patients<br />
experience slightly higher levels of sensory and motor<br />
blockade after epidural and spinal anesthesia and are<br />
also at somewhat greater risk for arterial hypotension<br />
because of the sympathicolytic consequences of acute<br />
peripheral autonomic blockade. Thus, bolus doses of local<br />
anesthetic should be reduced in elderly patients to limit<br />
the side effects.<br />
<strong>Regional</strong> anesthesia offers several beneficial aspects<br />
to elderly patients, including reduced blood loss, better<br />
peripheral vascular circulation, suppression of the surgical<br />
stress response, and better postoperative pain control.<br />
<strong>The</strong> cardiac benefits of regional anesthesia have been<br />
especially attributed to TEA, particularly in patients<br />
with ischemic heart disease. Possibly postoperative thoracic<br />
epidural analgesia reduces cardiac morbidity in<br />
high-risk cardiac patients. Postoperative epidural analgesia<br />
can improve outcome after surgery by reducing<br />
pulmonary complications. Persistent age-related cognitive<br />
dysfunction seems not to be related to the history of<br />
an operation under general or regional anesthesia,<br />
suggesting the existence of other interacting etiologic<br />
factors. <strong>Regional</strong> anesthesia may reduce short-term mortality,<br />
especially in elderly patients undergoing hip fracture<br />
repair by a decrease in thromboembolism because<br />
of maintenance of relatively normal fibrinolysis. However,<br />
no conclusions can be drawn for longer-term mortality.<br />
<strong>The</strong>re is evidence that epidural anesthesia facilitates<br />
earlier recovery by reducing ileus in abdominal surgical<br />
patients.<br />
Nonetheless, large multicenter prospective randomized<br />
studies are required in elderly surgical patients to<br />
more definitively assess the impact of regional anesthesia<br />
on morbidity and mortality, ICU time, length of hospitalization,<br />
and cost of health care.<br />
References<br />
1. US Bureau of Census. Statistical Abstracts of the United<br />
States. 113th ed. Washington, DC: Department of Commerce;<br />
1993.<br />
2. Klopfenstein CE, Herrmann FR, Michel JP, et al. <strong>The</strong><br />
influence of an aging surgical population on the anesthesia<br />
workload: a ten-year survey. Anesth Analg 1998;86:1165–<br />
1170.<br />
3. Bromage PR. Epidural Analgesia. Philadelphia: WB<br />
Saunders; 1978:31–35.<br />
4. Ferrer-Brechner T. Spinal and epidural anaesthesia in the<br />
elderly. Semin Anesth 1986;V:54–61.<br />
5. Jacob JM, Love S. Qualitative and quantitative morphology<br />
of human sural nerve at different ages. Brain 1985;<br />
108:897–924.<br />
6. Dorfman LJ, Bosley TM. Age related changes in peripheral<br />
and central nerve conduction in man. Neurology 1979;29:<br />
38–44.<br />
7. Shanta TR, Evans JA. <strong>The</strong> relationship of epidural anesthesia<br />
to neural membranes and arachnoid villi. <strong>Anesthesiology</strong><br />
1972;37:543–557.<br />
8. May C, Kaye JA, Atack JR, et al. Cerebrospinal fluid production<br />
is reduced in healthy aging. Neurology 1990;40:<br />
500–503.<br />
9. Greene NM. Physiology of Spinal Anaesthesia. 3rd ed.<br />
Baltimore: Williams & Wilkins; 1981:5.<br />
10. Park WY, Balingit PE, MacNamara TE. Age and the epidural<br />
dose response in adult man. <strong>Anesthesiology</strong> 1982;56:<br />
318–332.<br />
11. Veering BT, Burm AGL, Van Kleef JW, et al. Epidural<br />
anesthesia with bupivacaine: effects of age on neural<br />
blockade and pharmacokinetics. Anesth Analg 1987;66:<br />
589–594.<br />
12. Veering BT, Burm AGL, Vletter AA, et al. <strong>The</strong> effect of<br />
age on the systemic absorption and systemic disposition of<br />
bupivacaine after epidural administration. Clin Pharmacokinet<br />
1992;22:75–84.<br />
13. Nydahl PA, Philipson L, Axelsson K, et al. Epidural anesthesia<br />
with 0.5% bupivacaine: influence of age on sensory<br />
and motor blockade. Anesth Analg 1991;73:780–787.<br />
14. Hirabayashi Y, Shimizu R. Effect of age on extradural<br />
dose requirement in thoracic extradural anaesthesia. Br J<br />
Anaesth 1993;71:445–446.<br />
15. Simon MJ, Veering BT, Stienstra R, et al. <strong>The</strong> effects of age<br />
on neural blockade and hemodynamic changes after epidural<br />
anesthesia with ropivacaine. Anesth Analg 2002;94:<br />
1325–1330.<br />
16. Simon MJG, Veering BT, Burm AGL, et al. <strong>The</strong> effect of<br />
age on the clinical profile and the systemic absorption and<br />
disposition of levobupivacaine following epidural anaesthesia.<br />
Br J Anaesth 2004;93:512–520.<br />
17. Hirabayashi Y, Shimizu R, Matsuda J, et al. Effect of extradural<br />
compliance and resistance on spread of extradural<br />
analgesia. Br J Anaesth 1990;65:508–513.
19. Management of <strong>Regional</strong> <strong>Anesthesia</strong> 289<br />
18. Bromage PR. Exaggerated spread of epidural analgesia<br />
in arteriosclerotic patients. Dosage in relation to bio -<br />
logical and chronological ageing. Br Med J 1962;2:1634–<br />
1638.<br />
19. Guinard JP, Mulroy MF, Carpenter RL. Aging reduces the<br />
reliability of epidural epinephrine test doses. Reg Anesth<br />
1995;20:193–198.<br />
20. Mann C, Pouzeratte Y, Boccara G, et al. Comparison of<br />
intravenous or epidural patient-controlled analgesia in the<br />
elderly after major abdominal surgery. <strong>Anesthesiology</strong><br />
2000;92:433–441.<br />
21. Scott JC, Stanski DR. Decreased fentanyl and alfentanil<br />
dose requirements with age. A simultaneous pharmacokinetic<br />
and pharmacodynamic evaluation. J Pharmacol Exp<br />
<strong>The</strong>r 1987;240:159–166.<br />
22. Jin F, Chung F. Minimizing perioperative adverse events in<br />
the elderly. Br J Anaesth 2001;87:608–624.<br />
23. Pitkänen M, Haapaniemi L, Tuominen M, et al. Influence<br />
of age on spinal anaesthesia with isobaric 0.5% bupivacaine.<br />
Br J Anaesth 1984;56:279–284.<br />
24. Veering BT, Burm AGL, Van Kleef JW, et al. Spinal anesthesia<br />
with glucose-free bupivacaine: effects of age on<br />
neural blockade and pharmacokinetics. Anesth Analg<br />
1987;66:965–970.<br />
25. Boss EG, Schuh FT. Der Einfluss des Lebensalters auf die<br />
Ausbreitung der Spinalanasthesie mit isobarem Mepivacain<br />
2%. Anaesthesist 1993;42:162–168.<br />
26. Veering BT, Burm AGL, Spierdijk J. Spinal anaesthesia<br />
with hyperbaric bupivacaine: effects of age on neural<br />
blockade and pharmacokinetics. Br J Anaesth 1988;60:<br />
187–194.<br />
27. Racle JP, Benkhadra A, Poy JY, et al. Spinal analgesia with<br />
hyperbaric bupivacaine: influence of age. Br J Anaesth<br />
1988;60:508–514.<br />
28. Veering BT, Burm AGL, Vletter AA, et al. <strong>The</strong> effect of<br />
age on systemic absorption and systemic disposition of<br />
bupivacaine after subarachnoid administration. <strong>Anesthesiology</strong><br />
1991;74:250–257.<br />
29. Racle JP, Benkhadra A, Poy JY, et al. Prolongation of isobaric<br />
bupivacaine spinal anesthesia with epinephrine and<br />
clonidine for hip surgery in the elderly. Anesth Analg 1987;<br />
66:442–446.<br />
30. Racle JP, Benkhadra A, Poy JY, et al. Effects of increas -<br />
ing amounts of epinephrine during isobaric bupivacaine<br />
spinal anesthesia in elderly patients. Anesth Analg 1987;66:<br />
882–886.<br />
31. Paqueron X, Boccara G, Bendahou M, et al. Brachial<br />
plexus nerve block exhibits prolonged duration in the<br />
elderly. <strong>Anesthesiology</strong> 2002;97:1245–1249.<br />
32. Tucker GT. Pharmacokinetics of local anaesthetics. Br J<br />
Anaesth 1986;58:717–731.<br />
33. Freund PR, Bowdle TA, Slattery JT, et al. Caudal<br />
anesthesia with lidocaine or bupivacaine: plasma local<br />
anaesthetic concentration and extent of sensory spread<br />
in old and young patients. Anesth Analg 1984;63:1017–<br />
1020.<br />
34. Bowdle TA, Freund PR, Slattery JT. Age dependent<br />
lidocaine pharmacokinetics during lumbar peridural anesthesia<br />
with lidocaine hydrocarbonate or lidocaine hydrochloride.<br />
Reg Anesth 1986;11:123–127.<br />
35. Finucane BT, Hammonds WD, Welch MB. Influence of<br />
age on vascular absorption of lidocaine from the epidural<br />
space. Anesth Analg 1987;66:843–846.<br />
36. Burm AGL, Vermeulen NPE, Van Kleef JW, et al. Pharmacokinetics<br />
of lignocaine and bupivacaine in surgical<br />
patients following epidural administration. Simultaneous<br />
investigation of absorption and disposition kinetics using<br />
stable isotopes. Clin Pharmacokinet 1987;13:191–203.<br />
37. Burm AGL, Van Kleef JW, Vermeulen NPE, et al. Pharmacokinetics<br />
of lidocaine and bupivacaine following subarachnoid<br />
administration in surgical patients: simultaneous<br />
investigation of absorption and disposition kinetics using<br />
stable isotopes. <strong>Anesthesiology</strong> 1988;69:584–592.<br />
38. Emanuelsson BMK, Persson J, Alm C, et al. Systemic<br />
absorption and block after epidural injection of ropivacaine<br />
in healthy volunteers. <strong>Anesthesiology</strong> 1997;87:1309–1317.<br />
39. Greenblatt DJ, Sellers EM, Shader RI. Drug disposition in<br />
old age. New Engl J Med 1982;306:1081–1108.<br />
40. Nation RL, Triggs EJ, Selig M. Lignocaine kinetics in<br />
cardiac patients and aged subjects. Br J Clin Pharmacol<br />
1977;4:439–448.<br />
41. Cusson J, Nattel S, Matthews C, et al. Age-dependent lignocaine<br />
disposition in patients with acute myocardial<br />
infarction. Clin Pharmacol <strong>The</strong>r 1985;37:381–386.<br />
42. Cussack B, O’Malley K, Lavan J, et al. Protein binding and<br />
disposition of lignocaine in the elderly. Eur J Clin Pharmacol<br />
1985;29:923–929.<br />
43. Tucker GT, Boyes RN, Bridenbaugh PO, et al. Binding<br />
of anilide-type local anesthetics in human plasma. I.<br />
Relationships between binding, physicochemical properties<br />
and anesthetic activity. <strong>Anesthesiology</strong> 1970;33:287–<br />
303.<br />
44. Davis D, Grossman SH, Kitchell BB, et al. <strong>The</strong> effects of<br />
age and smoking on the plasma binding of lignocaine and<br />
diazepam. Br J Clin Pharmacol 1985;19:261–265.<br />
45. Veering BT, Burm AGL, Gladines MPRR, et al. Age does<br />
not influence the serum protein binding of bupivacaine.<br />
Br J Clin Pharmacol 1991;32:501–503.<br />
46. Veering BT, Burm AGL, Souverijn JHM, et al. <strong>The</strong> effect<br />
of age on serum concentrations of albumin and α 1 -acid<br />
glycoprotein. Br J Clin Pharmacol 1990;29:201–206.<br />
47. Mather LE, Thomas J. Bupivacaine binding to plasma<br />
protein fractions. J Pharm Pharmacol 1978;30:653–654.<br />
48. Tucker GT. Is plasma binding of local anesthetics important?<br />
Acta Anaesthesiol Belg 1988;39:147–150.<br />
49. Tucker GT, Wiklund L, Berlin-Wahlen A, et al. Hepatic<br />
clearance of local anesthetics in man. J Pharmacokinet<br />
Biopharm 1977;5:11–22.<br />
50. Wilkinson GR, Shand DG. A physiological approach<br />
to hepatic drug clearance. Clin Pharmacol <strong>The</strong>r 1975;18:<br />
377–390.<br />
51. Abernethy DR, Greenblatt DJ. Impairment of lidocaine<br />
clearance in elderly male subjects. J Cardiovasc Pharmacol<br />
1983;5:1093–1096.<br />
52. Wynne HA, Cope LH, Mutch E, et al. <strong>The</strong> effect of age<br />
upon liver volume and apparent liver blood flow in healthy<br />
man. Hepatology 1989;9:297–301.<br />
53. Ross RA, Clarke JE, Armitage EN. Postoperative pain<br />
prevention by continuous epidural infusion. Anaesthesia<br />
1980;35:663–668.
290 B. Veering<br />
54. Veering BT, Burm AGL, Feyen MH, et al. Pharmacokinetics<br />
of bupivacaine during postoperative epidural infusion:<br />
enantioselectivity and role of protein binding. <strong>Anesthesiology</strong><br />
2002;96:1062–1069.<br />
55. Aronson KF, Ekelund G, Kindmark CO, et al. Sequential<br />
changes of plasma proteins after surgical trauma. Scand J<br />
Clin Lab Invest 1972;29(Suppl 124):127–136.<br />
56. Fukuda T, Kakiuchi Y, Masayuki M, et al. Free lidocaine<br />
concentrations during continuous epidural anesthesia<br />
in geriatric patients. Reg Anesth Pain Med 2003;28:215–<br />
220.<br />
57. Gielen M. Post dural puncture headache (PDPH): a review.<br />
Reg Anesth 1989;14:101–106.<br />
58. Veering BT, Cousins MJ. Cardiovascular and pulmonary<br />
effects of epidural anaesthesia. Anaesth Intensive Care<br />
2000;28:620–635.<br />
59. Tarkkila P, Isola J. A regression model for identifying<br />
patients at high risk of hypotension, bradycardia and<br />
nausea during spinal anesthesia. Acta Anaesthesiol Scand<br />
1992;36:554–558.<br />
60. Carpenter RL, Caplan RA, Brown DL, et al. Incidence and<br />
risk factors for side effects of spinal anesthesia. <strong>Anesthesiology</strong><br />
1992;76:906–912.<br />
61. Juelsgaard P, Sand NP, Felsby S, et al. Perioperative myocardial<br />
ischaemia in patients undergoing surgery for fractured<br />
hip randomized to incremental spinal, single-dose<br />
spinal or general anaesthesia. Eur J Anaesthesiol 1998;15:<br />
656–663.<br />
62. Racle JP, Poy JY, Haberer JP, et al. A comparison of cardiovascular<br />
responses of normotensive and hypertensive<br />
elderly patients following bupivacaine spinal anesthesia.<br />
Reg Anesth 1989;14:66–71.<br />
63. Priebe HJ. <strong>The</strong> aged cardiovascular risk patient. Br J<br />
Anaesth 2000;85:763–778.<br />
64. Rooke GA. Cardiovascular aging and anesthetic implications.<br />
J Cardiothorac Vasc Anesth 2003;17:512–523.<br />
65. Korkuschko OW, Sarkisow KG, Schatilo WB, et al. Hemodynamic<br />
effects of stimulation of alpha 1-adrenoreceptors<br />
in healthy elderly and aged persons. Z Gerontol 1992;25:<br />
88–93.<br />
66. Veith RC, Featherstone JA, Linares OA, et al. Age differences<br />
in plasma norepinephrine kinetics in humans.<br />
J Gerontol 1986;41:319–324.<br />
67. Ebert TJ, Morgan BJ, Barney JA, et al. Effects of aging on<br />
baroreflex regulation of sympathetic activity in humans.<br />
Am J Physiol 1992;263:H789–803.<br />
68. Rooke GA, Freund PR, Jacobsen AF. Hemodynamic<br />
response and change in organ blood volume during spinal<br />
anesthesia in elderly men with heart disease. Anesth Analg<br />
1997;85:99–105.<br />
69. Critchley LAH, Stuart JC, Short TG, et al. Haemodynamic<br />
effects of subarachnoid block in elderly patients. Br J<br />
Anaesth 1994;73:464–470.<br />
70. Coe AJ, Revanas B. Is crystalloid preloading useful in<br />
spinal anaesthesia in the elderly? Anaesthesia 1990;45:<br />
241–243.<br />
71. Buggy DJ, Power CK, Meeke R, et al. Prevention of spinal<br />
anaesthesia-induced hypotension in the elderly: i.m.<br />
methoxamine or combined hetastarch and crystalloid.<br />
Br J Anaesth 1998;80:199–203.<br />
72. Critchley LAH. Hypotension, subarachnoid block and the<br />
elderly patient. Anaesthesia 1996;51:1139–1143.<br />
73. Critchley LA, Short TG, Gin T. Hypotension during subarachnoid<br />
anaesthesia: haemodynamic analysis of three<br />
treatments. Br J Anaesth 1994;72:151–155.<br />
74. Critchley LA, Conway F. Hypotension during subarachnoid<br />
anaesthesia: haemodynamic effects of colloid and<br />
metaraminol. Br J Anaesth 1996;76:734–736.<br />
75. Chamberlain D, Chamberlain B. Changes in skin temperature<br />
of the trunk and their relationship to sympathetic<br />
block during spinal anesthesia. <strong>Anesthesiology</strong> 1986;65:<br />
139–143.<br />
76. Ben-David B, Frankel R, Arzumonov T, et al. Minidose<br />
bupivacaine-fentanyl spinal anesthesia for surgical repair<br />
of hip fracture in the aged. <strong>Anesthesiology</strong> 2000;92:6–10.<br />
77. Veering BT, Ter Riet PM, Burm AGL, et al. Spinal anaesthesia<br />
with 0.5% hyperbaric bupivacaine in elderly patients:<br />
effect of site of injection on spread of analgesia. Br J<br />
Anaesth 1996;77:343–346.<br />
78. Veering BT, Immink-Speet TTM, Burm AGL, et al. Spinal<br />
anaesthesia with 0.5% hyperbaric bupivacaine in elderly<br />
patients: effects of duration spent in the sitting position.<br />
Br J Anaesth 2001;87:738–742.<br />
79. Sumi M, Sakura S, Koshizaki M, et al. <strong>The</strong> advantages<br />
of the lateral decubitus position after spinal anesthesia<br />
with hyperbaric tetracaine. Anesth Analg 1998;87:879–<br />
884.<br />
80. Favarel-Garrigues JF, Sztark F, Petitjan ME, et al. Hemodynamic<br />
effects of spinal anesthesia in the elderly: single<br />
dose versus titration through a catheter. Anesth Analg<br />
1996;82:312–316.<br />
81. Frank SM, Beattie C, Christopherson R, et al. Epidural<br />
versus general anesthesia, ambient operating room temperature,<br />
and patient age as predictors of inadvertent<br />
hypothermia. <strong>Anesthesiology</strong> 1992;77:252–257.<br />
82. Wagner JA, Robinson S, Marinao RP. Age and temperature<br />
regulation of humans in neutral and cold environments.<br />
J Appl Physiol 1974;37:562–565.<br />
83. Frank SM, El-Rahmany HK, Cattaneo CG, et al. Predictors<br />
of hypothermia during spinal anesthesia. <strong>Anesthesiology</strong><br />
2000;92:1330–1334.<br />
84. Leslie K, Sessler DI. Reduction in the shivering threshold<br />
is proportional to spinal block height. <strong>Anesthesiology</strong><br />
1996;84:1327–1331.<br />
85. Vassilieff N, Rosencher N, Sessler DI, et al. Shivering<br />
threshold during spinal anesthesia is reduced in elderly<br />
patients. <strong>Anesthesiology</strong> 1995;83:1162–1166.<br />
86. Bell GD, Reeve PA, Moshiri M, et al. Intravenous<br />
midazolam for upper gastrointestinal endoscopy: a study<br />
of 800 consecutive cases relating dose to age and sex of<br />
patient. Br J Clin Pharmacol 1987;23:241–243.<br />
87. Schnider TW, Minto CF, Shafer SL, et al. <strong>The</strong> influence of<br />
age on propofol pharmacodynamics. <strong>Anesthesiology</strong> 1999;<br />
90:1502–1516.<br />
88. Shinozaki M, Usui Y, Yamaguchi S, et al. Recovery of psychomotor<br />
function after propofol sedation is prolonged in<br />
the elderly. Can J Anaesth 2002;49:927–931.<br />
89. Wu CL, Hsu W, Richman JM, et al. Postoperative cognitive<br />
function as an outcome of regional anesthesia and analgesia.<br />
Reg Anesth Pain Med 2004;29:257–268.
19. Management of <strong>Regional</strong> <strong>Anesthesia</strong> 291<br />
90. Gustafson Y, Beggren D, Banstöm B, et al. Acute confusional<br />
states in elderly patients treated for femoral neck<br />
fracture. J Am Geriatr Soc 1988;36:525–530.<br />
91. Williams-Russo P, Urquhart RN, Sharrock NE, et al. Postoperative<br />
delirium: predictors and prognosis in elderly<br />
orthopedic patients. J Am Geriatr Soc 1992;40:759–767.<br />
92. Moller JT, Cluitmans P, Rasmussen LS, et al. Long-term<br />
postoperative cognitive dysfunction in the elderly.<br />
ISPOCD1 study. IOPOCD investigators. International<br />
Study of Post Operative Cognitive Dysfunction. Lancet<br />
1998;351:857–861.<br />
93. Canet J, Raeder J, Rasmussen LS, et al. Cognitive dysfunction<br />
after minor surgery in the elderly. Acta Anaesthesiol<br />
Scand 2003;47:1204–1210.<br />
94. Liu S, Carpenter RL, Neal JM. Epidural anesthesia and<br />
analgesia. <strong>The</strong>ir role in postoperative outcome. <strong>Anesthesiology</strong><br />
1995;82:1474–1506.<br />
95. Kehlet H. Surgical stress: the role of pain and analgesia.<br />
Br J Anaesth 1989;63:189–195.<br />
96. Kehlet H, Holte K. Effect of postoperative analgesia on<br />
surgical outcome. Br J Anaesth 2001;87:62–72.<br />
97. Rosenfeld BA. Benefits of regional anaesthesia on<br />
thrombo-embolic complications following surgery. Reg<br />
Anesth 1996;21:S9–S12.<br />
98. Donadoni R, Baele G, Devulder J, et al. Coagulation<br />
and fibrinolytic parameters in patients undergoing total<br />
hip replacement: influence of anaesthesia technique. Acta<br />
Anaesthesiol Scand 1989;33:588–592.<br />
99. Rosenfeld BA, Beattie C, Christopherson R, et al. <strong>The</strong><br />
Perioperative Ischaemia Randomized <strong>Anesthesia</strong> Trial<br />
Study Group: the effects of different anesthetic regimens<br />
on fibrinolysis and the development of postoperative arterial<br />
thrombosis. <strong>Anesthesiology</strong> 1993;79:435–443.<br />
100. Wu CL, Caldwell MD. Effect of post-operative analgesia<br />
on patient morbidity. Best Pract Res Clin Anaesthesiol<br />
2002;16:549–563.<br />
101. Davis FM, McDermott E, Hickton C, et al. Influence of<br />
spinal and general anaesthesia on haemostasis during total<br />
hip arthroplasty. Br J Anaesth 1987;59:561–571.<br />
102. Valentin N, Lomholt B, Jensen JS, et al. Spinal or general<br />
anaesthesia for surgery of the fractured hip? Br J Anaesth<br />
1986;58:284–291.<br />
103. Lundh R, Hedenstierna G, Johansson H. Ventilationperfusion<br />
relationships during epidural analgesia. Acta<br />
Anaesthesiol Scand 1983;27:410–416.<br />
104. McKenzie PJ, Wishart HY, Dewar KMS, et al. Comparison<br />
of the effects of spinal anaesthesia and general anaesthesia<br />
on postoperative oxygenation and perioperative mortality.<br />
Br J Anaesth 1980;52:49–55.<br />
105. Catley D, Thornton C, Jordan C, et al. Pronounced, episodic<br />
oxygen desaturation in the postoperative period: its<br />
association with ventilatory pattern and analgesic regimen.<br />
<strong>Anesthesiology</strong> 1985;63:20–28.<br />
106. Klassen GA, Bramwell RS, Bromage PR, et al. <strong>The</strong><br />
effect of acute sympathectomy by epidural anesthesia on<br />
the canine coronary circulation. <strong>Anesthesiology</strong> 1980;52:<br />
8–15.<br />
107. Davis RF, De Boer LWV, Maroko PR. Thoracic epidural<br />
anesthesia reduces myocardial infarct size after coronary<br />
artery occlusion in dogs. Anesth Analg 1986;65:711–717.<br />
108. Blomberg S, Curelaru J, Emanuelsson H, et al. Thoracic<br />
epidural anaesthesia in patients with unstable angina pectoris.<br />
Eur Heart J 1989;10:437–444.<br />
109. Blomberg S, Emanuelsson H, Kvirst H, et al. Effects of<br />
thoracic epidural anesthesia on coronary arteries and arterioles<br />
in patients with coronary artery disease. <strong>Anesthesiology</strong><br />
1990;73:840–847.<br />
110. Blomberg S, Emanuelsson H, Ricksten SE. Thoracic epidural<br />
anesthesia and central hemodynamics in patients with<br />
unstable angina pectoris. Anesth Analg 1989;69:558–562.<br />
111. Kock M, Blomberg S, Emanuelsson H, et al. Thoracic epidural<br />
anesthesia improves global and regional left ventricular<br />
function during stress-induced myocardial ischemia<br />
in patients with coronary artery disease. Anesth Analg<br />
1990;71:625–630.<br />
112. Meissner A, Rolf N, Van Aken H. Thoracic epidural anesthesia<br />
and the patient with heart disease: benefits, risks and<br />
controversies. Anesth Analg 1997;85:517–528.<br />
113. Ford G, Whitelaw W, Rosenal T, et al. Diaphragm function<br />
after upper abdominal surgery in humans. Am Rev Respir<br />
Dis 1987;127:431–436.<br />
114. Pansard JL, Mankikian B, Bertrand M, et al. Effects of<br />
thoracic extradural block on diaphragmatic electrical<br />
activity and contractility after upper abdominal surgery.<br />
<strong>Anesthesiology</strong> 1993;78:63–71.<br />
115. Polaner DM, Kimball WR, Fratacci M, et al. Thoracic<br />
epidural anesthesia increases diaphragmatic shortening<br />
after thoracotomy in the awake lamb. <strong>Anesthesiology</strong><br />
1993;79:808–816.<br />
116. Steinbrook RA. Epidural anesthesia and gastrointestinal<br />
motility. Anesth Analg 1998;86:837–844.<br />
117. Lehman JF, Wiseman JS. <strong>The</strong> effect of epidural analgesia<br />
on the return of peristalsis and the length of stay after<br />
elective colonic surgery. Am Surg 1995;61:1009–1012.<br />
118. Adolphs J, Schmidt DK, Mousa SA, et al. Thoracic epidural<br />
anesthesia attenuates hemorrhage-induced impairment of<br />
intestinal perfusion in rats. <strong>Anesthesiology</strong> 2003;99:685–692.<br />
119. O’Hara DA, Duff A, Berlin JA, et al. <strong>The</strong> effect of anesthetic<br />
technique on postoperative outcomes of hip fracture<br />
repair. <strong>Anesthesiology</strong> 2000;92:947–957.<br />
120. Sutcliffe AJ. Mortality after spinal and general anaesthesia<br />
for surgical fixation of hip fractures. Anaesthesia 1994;<br />
49:237–240.<br />
121. Pedersen T, Moller A, Cracknell J. <strong>The</strong> mission of the<br />
Cochrane <strong>Anesthesia</strong> Review Group: preparing and disseminating<br />
systematic reviews of the effect of health care<br />
in anesthesiology. Anesth Analg 2002;95:1012–1018.<br />
122. Urwin SC, Parker MJ, Griffiths R. General versus regional<br />
anaesthesia for hip-fracture surgery: meta-analysis of randomized<br />
trials. Br J Anaesth 2000;84:450–455.<br />
123. Gilbert TB, Hawkes WG, Hebel JR, et al. Spinal anesthesia<br />
versus general anesthesia for hip fracture repair: a longitudinal<br />
observation of 741 elderly patients during 2-year<br />
follow-up. Am J Orthop 2000;29:25–35.<br />
124. Bode RH, Lewis PL, Zarich SW, et al. Cardiac outcome<br />
after peripheral vascular surgery. Comparison of general<br />
and regional anesthesia. <strong>Anesthesiology</strong> 1996;84:3–13.<br />
125. Tuman KJ, McCarthy RJ, Marck RJ, et al. Effects of epidural<br />
anesthesia and analgesia on coagulation and outcome after<br />
major vascular surgery. Anesth Analg 1991;73:696–704.
292 B. Veering<br />
126. Christopherson R, Beattie C, Meinert CL, et al. Perioperative<br />
Ischemia Randomized <strong>Anesthesia</strong> Trial Study Group.<br />
Perioperative morbidity in patients randomized to epidural<br />
or general anesthesia for lower extremity vascular<br />
surgery. <strong>Anesthesiology</strong> 1993;79:422–434.<br />
127. Park WY, Thompson JS, Lee KK. Effect on epidural<br />
anesthesia and analgesia on perioperative outcome. A<br />
randomized, controlled veterans affairs cooperative study.<br />
Ann Surg 2001;234(4):560–571.<br />
128. Beattie SW, Badner NH, Choi P. Epidural analgesia re -<br />
duces postoperative myocardial infarction: a metaanalysis.<br />
Anesth Analg 2001;93:853–858.<br />
129. Matot I, Oppenheim-Eden A, Ratrot R, et al. Preoperative<br />
cardiac events in elderly patients with hip fracture randomized<br />
to epidural or conventional analgesia. <strong>Anesthesiology</strong><br />
2003;98:156–163.<br />
130. Modig J, Borg T, Karlström G, et al. Thromboembolism<br />
after total hip replacement: role of epidural and general<br />
anesthesia. Anesth Analg 1983;62:174–180.<br />
131. Modig J, Borg T, Bagge L, et al. Role of extradural<br />
and of general anaesthesia in fibrinolysis and coagulation<br />
after total hip replacement. Br J Anaesth 1983;55:625–<br />
629.<br />
132. Modig J, Borg T, Karlström G, et al. Effect of epidural<br />
versus general anaesthesia on calf blood flow. Acta Anaesthesiol<br />
Scand 1980;24:305–309.<br />
133. Borg T, Modig J. Potential anti-thrombotic effects of local<br />
anaesthetics due to their inhibition of platelet aggregation.<br />
Acta Anaesthesiol Scand 1985;29:739–742.<br />
134. de Leon-Casasola OA, Parker BM, et al. Epidural analgesia<br />
versus intravenous patient-controlled analgesia: differences<br />
in the postoperative course of cancer patients. Reg<br />
Anesth 1994;19:307–315.<br />
135. Ballantyne JC, Carr DB, deFerranti S, et al. <strong>The</strong> comparative<br />
effects of postoperative analgesic therapies on<br />
pulmonary outcome: cumulative meta-analyses of randomized,<br />
controlled trials. Anesth Analg 1998;86:598–612.<br />
136. Smith J, Kelly K. Pathophysiology of postoperative ileus.<br />
Arch Surg 1977;112:203–209.<br />
137. Holte K, Kehlet H. Postoperative ileus—a preventable<br />
event? Br J Surg 2000;87:1480–1493.<br />
138. Kehlet H, Holte K. Review of postoperative ileus. Am J<br />
Surg 2001;182:3S–10S.<br />
139. Lui SS, Carpenter RL, Mackey DC, et al. Effects of perioperative<br />
analgesic technique on rate of recovery after<br />
colon surgery. <strong>Anesthesiology</strong> 1995;83:757–765.
20<br />
Fluid Management<br />
Jessica Miller, Lee A. Fleisher, and Jeffrey L. Carson<br />
It is imperative that anesthesiologists are well versed in<br />
modifications to fluid management for the elderly patient. 1<br />
This chapter discusses the guiding principles in fluid management<br />
and the important alterations in kidney function<br />
and fluid homeostasis in the elderly patient. <strong>The</strong>se concepts<br />
are built upon to provide recommendations for the<br />
perioperative period. Preoperative evaluation, assessment,<br />
and decision making in the intraoperative period<br />
are discussed below, including methods of monitoring<br />
intraoperatively, types of fluids to administer, and the<br />
use of blood transfusions. Special anesthetic challenges<br />
such as spinal anesthesia and fluid management are also<br />
included.<br />
Fluid and Electrolyte Homeostasis<br />
Understanding changes in fluid and electrolyte balance<br />
requires examining the major determinants of fluid<br />
regulation. Total body water decreases with age from<br />
60%–65% in a young man to 50% by age 80. 2 Total<br />
body water is distributed as 67% extracellular fluid<br />
volume and 33% intracellular fluid volume. <strong>The</strong> cell wall<br />
separates extracellular fluid from intracellular fluid.<br />
Extracellular fluid volume is further divided into 75%<br />
interstitial fluid and 25% plasma. <strong>The</strong> cells making up the<br />
walls of arteries and veins and the capillary endothelium<br />
separate the extracellular compartment into interstitial<br />
and intravascular fluid. Water moves freely through cell<br />
walls and vessels. Ions such as sodium can pass freely<br />
across capillary endothelium, but sodium pumps driven<br />
by adenosine 5′-triphosphate maintain a concentration<br />
gradient across cells. Larger molecules such as albumin<br />
and colloids are unable to move across intact capillary<br />
endothelium, thus creating a colloid oncotic pressure.<br />
Movement of fluids between the extracellular and<br />
intracellular compartment is governed by the Starling<br />
equilibrium. Starling forces are composed of hydrostatic<br />
pressure, colloid oncotic pressure, and specific permeability<br />
coefficients:<br />
J = K[Pc − Pt − r(C − T)]<br />
where J = filtration rate out of capillary, K = filtration<br />
coefficient, Pc = capillary pressure, Pt = tissue fluid pressure,<br />
C = plasma colloid oncotic pressure, T = tissue<br />
colloid oncotic pressure, r = reflection coefficient.<br />
Hydrostatic pressure in the capillaries drives movement<br />
of fluid from the capillary to the interstitial space.<br />
Elevated colloid oncotic pressure in intravascular fluid<br />
opposes hydrostatic pressure to maintain intravascular<br />
volume and a relatively dry interstitial compartment.<br />
During surgery, capillary membrane permeability<br />
increases at the surgical site. Proteins move down<br />
their concentration gradient into the interstitial fluid,<br />
thus decreasing colloid oncotic pressure in the intravascular<br />
space. Administration of fluid in the perioperative<br />
period also decreases colloid oncotic pressure due to<br />
hemodilution.<br />
Perioperative fluid distribution can be understood with<br />
the Starling equilibrium; however, alterations in endocrine<br />
and inflammatory mediators also affect fluid homeostasis.<br />
Surgical trauma results in an increased activity of<br />
antidiuretic hormone (ADH), aldosterone, and the reninangiotensin<br />
system. Increased ADH secretion enhances<br />
water reabsorption in the kidney resulting in lowered<br />
plasma sodium concentration and a decrease in diuresis.<br />
Increased aldosterone and renin release results in sodium<br />
conservation and potassium excretion (Figure 20-1). 3<br />
Further aspects of the stress response lead to increased<br />
cortisol secretion. Cortisol may be beneficial in counteracting<br />
inflammatory mediators and helping to maintain<br />
capillary integrity. Inflammatory mediators such as interleukin-6,<br />
tumor necrosis factor, substance P, and bradykinin<br />
may act as vasodilators and cause further increases in<br />
capillary permeability. 4<br />
293
294 J. Miller, L.A. Fleisher, and J.L. Carson<br />
Figure 20-1. Pathways by which decreased plasma volume leads,<br />
via the renin-angiotensin system and aldosterone, to increased<br />
sodium reabsorption and hence decreased sodium excretion.<br />
GFR = glomerular filtration rate. (Reprinted from Vander et al. 3<br />
with permission of <strong>The</strong> McGraw-Hill Companies.)<br />
<strong>The</strong>se concepts can be applied to perioperative management<br />
of the elderly patient by understanding the evolution<br />
of these mechanisms with age. As mentioned, total body<br />
water decreases in the elderly to approximately 50% of<br />
body weight by the age of 80 years. Muscle mass is decreased<br />
by as much as 30% in the 80-year-old patient. <strong>The</strong> effect<br />
of a deceased total body water and decreased lean body<br />
mass results in a larger volume of distribution. Elderly<br />
patients have subtle alterations in the dynamic renal,<br />
endocrine, and hormonal elements that work to maintain<br />
homeostatic balance. <strong>The</strong>se will be discussed in more detail<br />
below. <strong>The</strong>se alterations in fluid homeostasis are magnified<br />
by the decrease in arterial distensibility, decreased baroceptor<br />
reflexes, and more sluggish homeostatic response to<br />
result in larger alterations in hemodynamic stability. 5<br />
Aging and Renal Function<br />
An understanding of changes in renal sodium and water<br />
excretion is central to understanding fluid and electrolyte<br />
balance. <strong>The</strong> aged kidney is able to maintain stable
20. Fluid Management 295<br />
volume and electrolyte status. Age has been shown<br />
to have no effect on basal plasma sodium and potassium<br />
concentrations, or maintenance of normal extracel -<br />
lular fluid volume. However, the aged kidney has less<br />
functional reserve and is slower to adapt to acute<br />
changes.<br />
Changes in structure and function of the kidney with<br />
age affect fluid management, electrolyte homeostasis,<br />
drug metabolism, and pharmacokinetics. <strong>The</strong>se changes<br />
have been well described; however, the methods of assessment<br />
of kidney function in aging individuals have received<br />
more attention recently. Early analysis of aging kidney<br />
function utilized cross-sectional studies. Attempts were<br />
made to exclude patients with overt renal disease;<br />
however, limitations in testing inevitably overlook subclinical<br />
renal disease. Comparison studies between active<br />
young individuals were frequently matched with institutionalized<br />
elderly individuals, thus not representing<br />
the segments of the elderly population that are residing<br />
and functioning in the community. 6,7 More recent studies<br />
have used longitudinal comparison of kidney function in<br />
carefully selected patients who lacked renal diseases,<br />
specifically patients who were deemed suitable for kidney<br />
donation. 8–10 Predictably, these studies showed less<br />
marked changes in kidney function than previous studies.<br />
<strong>The</strong> availability of this more accurate representation of<br />
changing kidney function is beneficial to overall understanding<br />
of clinical management; however, the frequent<br />
presence of comorbid diseases that affect kidney function<br />
cannot be overlooked in applying these principles to individual<br />
patient management.<br />
Alterations in the kidney associated with aging include<br />
both structural and functional changes. Studies have indicated<br />
total and cortical renal mass decreases with age.<br />
Between the ages of 30 and 85 years, renal mass decreases<br />
by 20%–25%. 2 <strong>The</strong> decline in renal mass is relatively<br />
sparing of the medulla, with most loss occurring in the<br />
cortical area. <strong>The</strong> number of functioning glomeruli<br />
decreases proportionally with change in mass; however,<br />
the size of each remaining glomeruli increases. <strong>Global</strong> sclerosis<br />
of the glomeruli increases the proportion of sclerotic<br />
glomeruli from 5% in middle age to 10%–30% by the<br />
eighth decade. <strong>The</strong> length of the proximal convoluted<br />
tubule decreases in size with age, thus matching the decline<br />
in glomerular and tubular function seen in aging. 6<br />
Multiple studies have demonstrated that renal blood<br />
flow decreases with age. 11–13 Renal blood flow begins to<br />
decline after the fourth decade of life by approximately<br />
10% per decade. 14 Further studies also showed a decrease<br />
in mean blood flow per unit mass with advancing age.<br />
When correlated with changes in flow rates, it has been<br />
deduced that the largest decreases in renal perfusion<br />
occur in the cortex, with relative sparing of flow to the<br />
deeper regions of the kidney. As flow decreases from the<br />
cortex, the juxtaglomedullary glomeruli receive more<br />
perfusion. <strong>The</strong>ir preexisting increased filtration fraction<br />
compared with the cortex glomeruli may explain the<br />
increase in filtration fraction with aging. 6<br />
Glomerular filtration rate (GFR) is the predominant<br />
measure of renal function. Initial studies assessing nursing<br />
home residents resoundingly found that GFR decreased<br />
with age. GFR can be estimated to decrease approximately<br />
1 mL/min/y. 15 Assessment of GFR in the elderly<br />
has been repeated using community-dwelling elderly<br />
in both cross-sectional and longitudinal studies. <strong>The</strong>se<br />
studies also found a general decline in GFR, but also<br />
revealed more variations in GFR. Up to 30% of the<br />
elderly subjects had a stable GFR over a 20-year longitudinal<br />
study, suggesting that declining GFR is not<br />
inevitable. 11,15 Only explicit measurement of creatinine<br />
clearance could identify these patients, thus it should not<br />
be assumed the elderly patient has a decreased GFR.<br />
Serum creatinine is relatively constant with age, reflecting<br />
the decrease in muscle mass with age that parallels<br />
the decrease in GFR. In clinical practice, a method of<br />
estimating GFR from creatinine clearance is helpful.<br />
<strong>The</strong> most frequently used formula is the Crockroft-Gault<br />
equation 16 :<br />
Creatinine clearance = [K (140 − age) (weight in kg)]/<br />
[(72) (serum creatinine concentration)]<br />
K = 1.23 for men, 1.03 for women,<br />
creatinine clearance in µmoL/min.<br />
<strong>The</strong> development of this formula may have been skewed<br />
by the use of validation on a small number of subjects,<br />
subjects of only one gender, and institutionalized individuals.<br />
A recent reevaluation of the accuracy of the<br />
Crockroft-Gault equation in comparison to a measured<br />
24-hour creatinine clearance showed only a moderate<br />
correlation in the equation’s estimates with the measured<br />
clearance in the elderly subgroup. 17,18 A more comprehensive<br />
study comparing the validity of several methods<br />
of estimating GFR found most equations underestimated<br />
creatinine clearance. In general, it is recommended that<br />
if an accurate measure of GFR is required, a 24-hour<br />
creatinine clearance should be measured. <strong>The</strong>re is no one<br />
estimation method that accurately predicts GFR. For<br />
purposes needing less accuracy, the Crockroft-Gault<br />
equation is a reasonable guide. Clinical drug dosing in the<br />
elderly should maintain careful consideration of drugs<br />
cleared mainly by renal mechanisms.<br />
Sodium Handling<br />
Less is known about the ability of the aged kidney to<br />
process sodium (Tables 20-1 and 20-2). Studies have concluded<br />
that age significantly decreases the kidney’s ability<br />
to conserve sodium. <strong>The</strong> aged kidney takes a longer<br />
period of time to reduce urinary excretion of sodium in<br />
response to a low-sodium diet when compared with a<br />
young person’s kidney. 8 <strong>The</strong> decrease in renal blood flow
296 J. Miller, L.A. Fleisher, and J.L. Carson<br />
and GFR does not explain this sluggish response. Other<br />
elements of the sodium conservation axis, such as the<br />
renin aldosterone system and atrial natriuretic peptide<br />
may be responsible. Several studies have shown that the<br />
renin aldosterone response to acute stimuli is slower with<br />
advancing age. 14,19,20<br />
<strong>The</strong> aged kidney seems to have impaired sodium excretion<br />
mechanisms. Mechanisms responsible for reduced<br />
sodium excretion may include a decrease in pressuresensitive<br />
natriuresis, which may lead to salt-sensitive<br />
hypertension. An altered response to angiotensin II has<br />
also been investigated. <strong>The</strong> administration of sodium-rich<br />
fluids, dietary indiscretion, and radiocontrast dye must be<br />
considered with forethought into the possible negative<br />
effects of the resultant volume load.<br />
<strong>The</strong> aged kidney’s ability to alter its response to total<br />
body sodium is especially critical in the elderly. Older<br />
patients are more likely to experience confusion and loss<br />
of thirst sensation in periods of acute illness, which further<br />
aggravates the body’s sluggish response to altered plasma<br />
sodium. Other studies have suggested that sodium losses<br />
have magnified effects on hemodynamic stability. A study<br />
by Shannon et al. 21 showed that a diuresis of 2 kg resulted<br />
in a 24 mm Hg decrease in systolic blood pressure upon<br />
changing from the supine to a standing position, a much<br />
larger effect than seen in younger patients.<br />
Investigations into other aspects of fluid homeostasis<br />
have also been conducted. Studies have concluded that<br />
substantial declines in plasma renin activity occur with<br />
aging. 20 Plasma renin is decreased in the resting state,<br />
and ranges from a 40% to 60% decrease in stimulated<br />
conditions. Significant and consistent declines in plasma<br />
renin are found after the sixth decade. <strong>The</strong> effect of renin<br />
on angiotensin II release is technically difficult to study.<br />
Aldosterone is also depleted in elderly patients in the<br />
stimulated and basal states. 19 Atrial natriuretic peptide<br />
has shown to be increased in elderly patients with possible<br />
decreased end-organ responsiveness; at this time its<br />
full effect is not understood.<br />
Renal diluting capacity is also shown to be affected by<br />
aging. A mild defect in renal diluting capacity occurs with<br />
age, which seems to be related to the decline in GFR. This<br />
puts the elderly patient at increased risk for dilutional<br />
hyponatremia in settings of stress, such as surgery, fever,<br />
Table 20-1. Symptoms of hyponatremia.<br />
Malaise<br />
Nausea<br />
Headache<br />
Lethargy<br />
Confusion<br />
Obtundation<br />
Stupor<br />
Seizures<br />
Coma<br />
Table 20-2. Symptoms of hypernatremia.<br />
Polyuria<br />
Thirst<br />
Altered mental status<br />
Weakness<br />
Neuromuscular irritability<br />
Focal neurologic deficits<br />
Seizures<br />
Coma<br />
or acute illness. Studies have found the decrease in plasma<br />
sodium level to be approximately 1 mEq/L per decade<br />
from a mean of 141 mEq/L in youth. 22 Hyponatremia in<br />
the inpatient is frequently iatrogenic, because of either<br />
fluid therapy or medications. Possibilities for medications—such<br />
as antidepressants, carbamazepine, clofibrate,<br />
and neuroleptics—to increase the secretion of ADH or<br />
enhancing the action of ADH at the tubule must also be<br />
considered. Hyponatremia is not a benign diagnosis<br />
because some studies have shown a twofold increase in<br />
mortality over age-matched control subjects. 2,22<br />
Hypernatremia developing in hospitalized elderly<br />
patients is most often attributable to surgery or febrile<br />
illness. Hypernatremia also has implications for mortality<br />
with a sevenfold increase in mortality compared with<br />
age-matched controls. 23<br />
Potassium Management<br />
Maintaining proper kidney function is crucial to potassium<br />
homeostasis, because the kidney is the primary<br />
organ for potassium excretion. Elderly patients are more<br />
susceptible to hyperkalemia, given the decrease in aldosterone<br />
and reduction in GFR. Undergoing surgery, tissue<br />
breakdown, or trauma also increases the risk of hyperkalemia<br />
especially if acute renal failure is present. Elderly<br />
patients are at increased risk of gastrointestinal bleeding,<br />
causing increased potassium levels as a result of red blood<br />
cell breakdown. Comorbid conditions may be present<br />
that affect flow to distal tubular sites, thus decreasing the<br />
amount of sodium available to enable potassium secretion.<br />
Examples of tubular flow-reducing diseases include<br />
hypovolemia, postsurgical or gastrointestinal losses, and<br />
congestive heart failure. 24<br />
Other risk factors present in elderly patients that<br />
may contribute to the risk of hyperkalemia include use<br />
of medications that increase potassium. Many elderly<br />
patients are prescribed diuretics, which may include the<br />
potassium-sparing diuretics spironolactone, triamterene,<br />
and amiloride. Prescription of thiazide diuretics may<br />
prompt the physician to include potassium supplementation<br />
as well. Patients may also be managing hypertension<br />
with salt-lowering diets, which are frequently high in
20. Fluid Management 297<br />
potassium salts. Angiotensin-converting enzyme inhibitors<br />
may cause hyperkalemia, because of reductions in<br />
aldosterone. Similarly, nonsteroidal antiinflammatory<br />
drugs can also result in a hyporeninemic hypoaldosterone<br />
state. Beta-blockers inhibit renin release in the kidney to<br />
cause hyperkalemia. Heparin blocks aldosterone synthesis<br />
in the adrenal gland, which may rarely cause elevated<br />
potassium. Trimethoprim-sulfamethazine acts similar to<br />
amiloride and inhibits the sodium channel in the apical<br />
membrane of the late distal tubule and collecting duct.<br />
This leads to a reduction of sodium and hydrogen transport<br />
into the urine. 24<br />
Regulation of Urinary Concentration<br />
Closely related to the kidney’s ability to process sodium<br />
is the kidney’s ability to alter the concentration of the<br />
urine produced. A well-designed study by Rowe et al. 25<br />
demonstrated that elderly patients were less able to significantly<br />
alter urine flow or urine osmolarity after 12<br />
hours of dehydration. This study also detailed that the<br />
differences were not attributable to differences in solute<br />
intake or correlated to a decreased GFR in the elderly.<br />
Other contributing factors may include a decrease in the<br />
efficacy of the countercurrent exchange system resulting<br />
from a relative increase in the medullary blood flow, or a<br />
possible defect in solute transport from the tubule to the<br />
medulla. <strong>The</strong> role of vasopressin has been investigated<br />
more recently. 26,27 <strong>The</strong>se studies have shown that the<br />
osmoreceptor sensitivity is increased with increasing<br />
age to result in a great amount of vasopressin released<br />
per increase in osmolarity. This would seem to be compensatory<br />
for the reduced ability of the kidney to concentrate<br />
urine. However, the osmoreceptor does not seem<br />
to have increased sensitivity to changes in volume and<br />
pressure, such as those induced with orthostatic changes.<br />
More recent studies have produced conflicting results<br />
and failed to find a difference in overall ability to excrete<br />
a water load. 28–30<br />
Another aspect of water handling is thirst. A study by<br />
Phillips et al. 31 found that the elderly had less sensation<br />
of thirst and exhibited less water intake after a 24-hour<br />
period of dehydration compared with younger individuals,<br />
despite increases in plasma osmolarity and greater<br />
decreases in body mass. This defect is attributed to a<br />
defect in an opioid-mediated thirst center in the central<br />
nervous system.<br />
<strong>The</strong>se altered physiologic responses are insignificant in<br />
maintaining daily homeostasis, but become increasingly<br />
important when access to free water is controlled. Treatment<br />
of electrolyte abnormalities is similar, regardless of<br />
age, but balancing comorbid conditions may complicate<br />
management. For instance, it has been shown that patients<br />
with Alzheimer’s disease have a decreased ADH sensitivity.<br />
Patients treated with thiazide diuretics have impaired<br />
ability to increase free water clearance during water<br />
diuresis. It is worth noting that elderly persons may have<br />
a lag in return to normal mentation after severe electrolyte<br />
abnormalities, despite clinical normalization of lab<br />
indicators.<br />
Acid-Base Abnormalities<br />
Acid-base balance is well maintained in the elderly<br />
patient under normal conditions. However, acute illness<br />
often results in acidosis that may become exaggerated in<br />
the elderly. <strong>The</strong> aged kidney has a decrease in ammonia<br />
generation which acts to buffer about half of the acid<br />
excreted in the kidney. This increases the frequency of<br />
severe metabolic acidosis. Coexisting pulmonary disease<br />
may also limit the ability to excrete carbon dioxide.<br />
Calcium, Phosphate, Magnesium<br />
Studies have shown that, at any given plasma level of<br />
calcium, concentration of parathormone is increased.<br />
Poor dietary intake, medications, and coexisting disease<br />
may result in calcium, magnesium, and phosphorus deficiencies.<br />
<strong>The</strong> existence of renal disease and impaired<br />
ability to excrete electrolytes must be considered when<br />
initiating therapy.<br />
Nutrition<br />
Perioperative nutrition affects fluid and electrolyte management<br />
in the elderly patient. It is also well known that<br />
a malnourished patient has a much higher likelihood for<br />
postoperative morbidity and mortality, also increasing<br />
the chance that the anesthesiologist will be further<br />
involved in their postoperative critical care management.<br />
Nutrition strongly affects surgical recovery by delaying<br />
wound healing, increasing risk of anastomotic breakdown,<br />
infection, and even possible development of multi–<br />
organ system failure. Hypoalbuminemia affects plasma<br />
oncotic pressure, thus altering the distribution of intravascular<br />
fluids. Electrolyte abnormalities are common in<br />
the malnourished patient.<br />
Debate exists about how best to identify and correct<br />
malnutrition. In theory, elective intervention can be preceded<br />
by preoperative supplemental nutrition. Parenteral<br />
nutrition carries the risk of infection, whereas enteral<br />
nutrition has the risk of aspiration pneumonia and invasive<br />
surgical placement. In a thorough meta-analysis<br />
of studies addressing preoperative parenteral nutrition,<br />
only severely malnourished patients demonstrated fewer<br />
noninfectious complications. Benefit was demonstrated<br />
if preoperative parenteral nutrition was provided for<br />
7 days or more. 32
298 J. Miller, L.A. Fleisher, and J.L. Carson<br />
Preoperative enteral nutrition studies demonstrate<br />
reduced postoperative mortality and decreased incidence<br />
of wound infections. 33–36 Difficulties encountered in<br />
implementing these therapies include the need to place<br />
nasogastric tubes or feeding tubes. Oral supplementation<br />
is less predictable in increasing calorie intake because of<br />
poor appetite, taste barriers, and limitations because of<br />
cost.<br />
Postoperative nutrition is more practical because many<br />
surgeries cannot be delayed. Studies have shown a significant<br />
increase in morbidity and mortality if a patient<br />
receives only hypocaloric feeding for more than 14 days. 37<br />
However, postoperative parenteral nutrition has been<br />
shown to increase morbidity in some studies mainly<br />
because of septic complications. Postoperative enteral<br />
nutrition supplementation has been shown to have very<br />
positive effects. Two studies of hip fracture repair in<br />
elderly women showed reduced length of hospital<br />
stay, shortened time to weight bearing, and more rapid<br />
return to independent mobility with the use of enteral<br />
supplementation. 38,39<br />
Clinical Implications<br />
<strong>The</strong> renal response to surgery and anesthesia does not<br />
seem to significantly alter with age. GFR is known to be<br />
directly depressed by general anesthesia; however, this<br />
is not usually clinically significant. Decreases in cardiac<br />
output and blood pressure, frequently attributable to<br />
intravascular losses and hypothermia in surgery, will<br />
decrease renal blood flow. Appropriately assessing and<br />
maintaining intravascular volume has the most impact on<br />
renal function in the perioperative period. Recognition<br />
and treatment of hypovolemia has the potential to reduce<br />
incidence of organ dysfunction, postoperative morbidity,<br />
and death. <strong>The</strong> elderly patient is at much higher risk of<br />
developing acute renal failure because of the lack of functional<br />
reserve of the kidney. Incidence of developing<br />
postoperative renal failure can range from 0.1% to 50%<br />
after high-risk surgeries such as trauma, thoracic, or cardiovascular<br />
interventions, depending on the site of<br />
surgery. Acute tubular necrosis is the most common cause<br />
of acute perioperative renal failure (Table 20-3).<br />
Mortality in patients with acute renal failure can<br />
be greater than 50%, and at least one fifth of all perioperative<br />
deaths in elderly surgical patients are attributable<br />
to acute renal failure. Patients with perioperative<br />
renal failure account for up to 50% of the patients needing<br />
acute dialysis. 40 Acute renal failure in the elderly increases<br />
morbidity and mortality, and also burdens the health<br />
care system with additional costs. Avoidance of complications<br />
resulting from inappropriate fluid management<br />
involves intervention at all stages of perioperative<br />
medicine.<br />
Table 20-3. Risk factors of acute tubular necrosis.<br />
Ischemic acute tubular necrosis<br />
Major surgery<br />
Trauma<br />
Severe hypovolemia<br />
Sepsis<br />
Extensive burns<br />
Toxic acute tubular necrosis<br />
Exogenous: radiocontrast, cyclosporine, antibiotics<br />
(aminoglycosides), chemotherapy (cisplatin), organic solvents<br />
(ethylene glycol), acetaminophen, illegal abortifacients.<br />
Endogenous: rhabdomyolysis, hemolysis, uric acid, oxalate, plasma<br />
cell dyscrasia (myeloma)<br />
Preoperative Evaluation<br />
<strong>The</strong>re are several clinical conditions that merit additional<br />
attention to fluid balance. Preexisting azotemia prompts<br />
the clinician to look for correctable conditions before the<br />
perioperative period. Classification of renal dysfunction<br />
perioperatively is frequently delineated as prerenal, intrarenal,<br />
and postrenal. Chronic disorders such as enterocutaneous<br />
fistulas and chronic diarrhea can produce fluid and<br />
electrolyte depletion. Patients with chronic fluid imbalances<br />
may not have the typical signs and symptoms such<br />
as postural hypotension and tachycardia, making them<br />
more difficult to diagnose. Other important risk factors for<br />
elderly patients to develop hypovolemia include female<br />
sex, age older than 85 years, diagnosis of more than four<br />
chronic medical conditions, taking more than four medications,<br />
and being confined to bed 39 (Table 20-4).<br />
Physical examination remains important in diagnosing<br />
volume status. <strong>The</strong> most reliable clinical signs of hypovolemia<br />
are postural pulse increment and postural hypotension.<br />
A postural pulse increment of 30 beats/min or more<br />
has a specificity of 96%. 41 Postural hypotension is defined<br />
as a decrease in systolic blood pressure of more than<br />
20 mm Hg after rising from supine to standing position.<br />
With age, the increment in pulse can be less than 30 in a<br />
hypovolemic individual; however, there is no absolute<br />
cutoff level to indicate hypovolemia. Postural hypotension<br />
can also be found in 11%–30% of normovolemic<br />
patients older than 65 years. Mild postural dizziness is not<br />
definitive for hypovolemia; however, inability to stand for<br />
vital signs because of severe dizziness is a reliable predictor<br />
of hypovolemia. Skin turgor is less sensitive in elderly<br />
patients because of a reduction in skin elastin with age.<br />
Decreased axillary sweating can indicate hypovolemia.<br />
Invasive measurements of filling pressure and cardiac<br />
output may also be useful, but must be balanced with the<br />
inherent risk of invasive monitoring.<br />
Intraoperative Management<br />
Intrinsic renal failure is common perioperatively with the<br />
use of aminoglycosides, contrast dyes, and postoperative
20. Fluid Management 299<br />
Table 20-4. Adjusted odds ratios and 95% confidence intervals for significant risk factors among severe cases of dehydration.<br />
Strata<br />
Sex*<br />
Mobility*<br />
Age (years)* >85/4 chronic diseases 42.4 (16.8–106.4)‡ 53.6 (21.1–140.2)‡ (7.2–67.6) (3.8–18.6)<br />
>4 medications 30.7 (12.7–74.0)‡ 26.1 (11.3–61.6)‡ 65.0 (10.3–410.1)‡<br />
Mobility:<br />
Assistance 11.5† 36.0†<br />
(2.9–45.2) (7.4–174.7) 22.6 (7.5–68.1)‡ —<br />
Bedridden 1.3 (3.9–17.9)‡ 7.6 (3.6–16.1)‡ —<br />
Feeding status: 19.0† 10.0†<br />
Assistance 30.0 (11.9–74.3)‡ 28.8 (11.5–71.6)‡ (3–122.0) (2.7–37)<br />
Tube 79.00† 17.01†<br />
(10.4–601.6) (5.4–52.9) 24.8 (9.3–67.1)‡ —<br />
45.0† 3.0†<br />
Skilled care level 4.2 (1.9–9.8)‡ 4.3 (1.9–9.4)‡ (6.5–310.9) (1.3–7.2)<br />
25.8† 5.9†<br />
Winter 14.8 (6.4–34.9)‡ 12.8 (5.5–28.8)‡ (8.3–74.4) (2.7–13.3)<br />
*Pooled where appropriate using χ 2 heterogeneity test. All are statistically significant at p = 0.05. Confidence intervals calculated using test-based<br />
interval estimation.<br />
†Not pooled based on heterogeneity score.<br />
‡Pooled, signifi cant with 95% confidence intervals.<br />
Source: Reprinted with permission from Lavizzo-Mourey et al. 39 Published by Blackwell Publishers Ltd.<br />
effects of cardiac bypass. Certain surgeries have increased<br />
risk of postoperative renal failure, such as cardiac or<br />
aortic surgery, as well as any surgery involving large fluid<br />
shifts, trauma patients, or the biliary tract. <strong>The</strong> risk of<br />
postoperative renal dysfunction in open abdominal aortic<br />
aneurysm repair is increased in emergency surgery<br />
and in incidences of increased length of cross-clamp<br />
duration and sustained hypotension. Dislodgement of<br />
atheromatous emboli may also occur in aortic repair.<br />
<strong>The</strong> mechanism of renal dysfunction after biliary tract<br />
surgery is unknown, but associated risk factors include<br />
postoperative sepsis, prior renal insufficiency, and height<br />
of preoperative bilirubin concentration. Preventing<br />
muscle compression and breakdown must also be considered<br />
in lengthy surgeries to decrease myoglobinuria.<br />
Postrenal azotemia should also be suspected, because<br />
elderly patients may have prostatic hypertrophy or<br />
nephrolithiasis. 24,42<br />
Several papers have addressed the best methods for<br />
determining the need for fluid administration in perioperative<br />
patients. <strong>The</strong>se studies link fluid balance with<br />
its effect on hemodynamic stability. <strong>The</strong> Starling curve<br />
describes the effect of volume loading on myocardial<br />
performance. Starling curves (Figure 20-2) illustrate the<br />
relationship between preload and cardiac output. Administration<br />
of a volume of fluid can increase preload and<br />
thus increase cardiac output. Beyond a certain amount of<br />
fluid administration, further increases in end-diastolic<br />
volume can decrease ventricular function and cardiac<br />
output.<br />
From a physiologic standpoint, fluid management can<br />
be guided by physical signs and symptoms of hemodynamic<br />
stability, or more quantitative methods such as<br />
information from esophageal Doppler monitors, central<br />
venous catheters, or pulmonary artery catheters. <strong>The</strong><br />
standard measures of volume status in the anesthetized<br />
patient are blood pressure, heart rate, oxygen saturation,<br />
Cardiac output<br />
Fluid administration<br />
improves myocardial<br />
performance<br />
Fluid volume administered<br />
Fluid administration<br />
impairs myocardial<br />
performance<br />
Figure 20-2. Effects of perioperative fluid therapy on the<br />
Starling myocardial performance curve. (Reprinted from Holte<br />
et al. 3 Copyright © <strong>The</strong> Board of Management and Trustees of<br />
the British Journal of Anaesthesia. Reproduced by permission<br />
of Oxford University Press/British Journal of Anaesthesia.)
300 J. Miller, L.A. Fleisher, and J.L. Carson<br />
and urine output. Interpretation of blood pressure<br />
and heart rate is frequently altered by many different<br />
variables in the perioperative patient, including sympathetic<br />
responses to surgical stimulus, anxiety and pain<br />
responses, and side effects of medications and anesthetic<br />
agents. Urine output is unreliable as well. Because of the<br />
depressive effects of general anesthesia, the common goal<br />
of 0.5 mL/kg/h of urine production is typically attained<br />
only with a fluid load. Meanwhile, studies have demonstrated<br />
that a low intraoperative urinary output did not<br />
correlate with development of renal failure, as long as<br />
hypovolemia was avoided. 43 Furthermore, excretion of<br />
a fluid excess of 1.5–2 L can take up to 2 days in healthy<br />
volunteers, which is an approximate indicator of the<br />
increased workload on the kidney with excessive fluid<br />
administration. 3<br />
A 2002 study 44 focused on the use of esophageal<br />
Doppler monitoring to guide fluid administration during<br />
the intraoperative period for moderate-risk surgical<br />
patients. <strong>The</strong> authors hypothesized that appropriate fluid<br />
resuscitation may decrease the extent of postoperative<br />
gastrointestinal dysfunction, reduce time to ability to tolerate<br />
oral intake, and ultimately reduce length of hospital<br />
stay. This prospective, single-blinded study compared<br />
fluid administration guided by esophageal Doppler, to<br />
administration guided by standard cardiovascular variables<br />
(blood pressure, heart rate, oxygen saturation),<br />
with significantly more hetastarch in the protocol group<br />
(847 ± 373 mL) compared with the control group<br />
(282 ± 470 mL). <strong>The</strong> study demonstrated a reduction in<br />
hospital stay in the Doppler-guided protocol group.<br />
Several studies of perioperative fluid optimization<br />
targeted repair of proximal femoral fractures. This is a<br />
common procedure for elderly and frail patients, typically<br />
straightforward surgically, with outcome determined by<br />
medical comorbidities. Avoidance of hypovolemia is<br />
important; however, fluid overload is also of particular<br />
concern in this patient population with cardiac and pulmonary<br />
comorbidities. Sinclair et al. 45 conducted a<br />
randomized controlled trial of proximal femoral fracture<br />
repairs with fluid administration guided by an esophageal<br />
Doppler monitor that demonstrated reduction of hospital<br />
stay. Because of the data obtained from Doppler monitoring,<br />
the intervention group received a larger volume<br />
of colloid, with approximately equal amounts of crystalloid<br />
received in both groups. Venn et al. 46 concluded a<br />
similar study with fluid management guided by central<br />
venous pressure (CVP) or esophageal Doppler, also<br />
demonstrating a reduction in duration of hospital stay<br />
in patients with fluid optimization guided by quantitative<br />
strategies. <strong>The</strong> drawback of both of these studies is the<br />
small number of participants, only 130 total, which is<br />
inadequate to detect changes in early mortality or to<br />
detect particular subgroups that might especially benefit<br />
from guided fluid administration. 47<br />
<strong>The</strong> studies above describe guided fluid administration<br />
via goals for stroke volume or CVP, and assessment of<br />
changes in these variables in response to additional fluid<br />
boluses. Additional studies focused on using quantitative<br />
data to produce supranormal physiologic parameters and<br />
assess the effects on outcomes. Shoemaker et al. 48 in 1988<br />
observed that survivors of high-risk surgery had increased<br />
hemodynamic and oxygen transport variables. <strong>The</strong>y conducted<br />
a prospective randomized trial to determine if<br />
optimization of hemodynamic and oxygen transport<br />
variables to supranormal values would affect outcome.<br />
This study demonstrated that optimization to supranormal<br />
values with the use of pulmonary artery catheter<br />
data reduced complications, duration of hospitalization,<br />
decreased time in the intensive care unit (ICU), decreased<br />
duration of mechanical ventilation, and reduced hospital<br />
cost. <strong>The</strong> authors caution that use of supranormal physiologic<br />
parameters may be inappropriate for the elderly<br />
patient because of a possible limited capacity for physiologic<br />
compensation. Scalea et al. 49 showed an improvement<br />
in survival rate in patients older than 65 years when<br />
early hemodynamic monitoring was instituted within 2.2<br />
hours from sustaining diffuse blunt trauma, and using this<br />
information to augment cardiac output. Although these<br />
approaches may be appropriate in younger patients with<br />
sepsis, they may lead to increased morbidity and mortality<br />
in the presence of multiple comorbidities. <strong>The</strong>refore,<br />
more studies are needed in the elderly before such an<br />
approach is routinely adopted.<br />
Discussion about the appropriate fluid to use in volume<br />
resuscitation continues for all perioperative patients. Use<br />
of crystalloid is supported by many practitioners for its<br />
economy. <strong>The</strong>y cite colloid use as having potential alterations<br />
in coagulation factors and risk of adverse drug reactions.<br />
Colloid supporters cite the benefit of using a smaller<br />
amount of fluid to resuscitate a patient, which may lead<br />
to less tissue edema and fewer adverse consequences,<br />
such as pulmonary edema and bowel dysfunction. Re -<br />
cently there have been three meta-analyses focusing on<br />
the use of colloid versus crystalloid in patients requiring<br />
volume resuscitation and the effect on mortality (Tables<br />
20-5 and 20-6). None of these studies has demonstrated<br />
a mortality benefit with the use of colloid. <strong>The</strong>se conclusions<br />
have been criticized for their combination of heterogeneous<br />
populations, use of many types of solutions,<br />
and varying indications for use. 50–52 <strong>The</strong> SAFE study,<br />
which is the largest trial of its kind as of this writing,<br />
demonstrated no appreciable difference in outcomes<br />
with the use of either 4% albumin or normal saline for<br />
intravascular volume resuscitation. 53 <strong>The</strong> multicenter,<br />
randomized, double-blind 28-day study included a diverse<br />
cohort of 6997 ICU patients with analogous baseline<br />
characteristics. <strong>The</strong>se results demonstrate that albumin<br />
and saline can be considered clinically comparable<br />
treatments. <strong>The</strong> choice of fluid for intravascular volume
Table 20-5. Summary of results of studies comparing colloid versus crystalloid for resuscitation in critically ill patients.<br />
Review: Colloids versus crystalloids for fluid resuscitation in critically ill patients<br />
Comparison: 01 colloid vs crystalloid (add-on colloid)<br />
Outcome: 01 deaths<br />
Study Colloid n/N Crystalloid n/N Relative risk (fixed) 95% CI Weight (%) Relative risk (fixed) 95% CI<br />
01 Albumin or PPF<br />
x Boldt 1986 0/1 0/1 0.0 Not estimable<br />
x Boldt 1993 0/15 0/15 0.0 Not estimable<br />
Boutros 1979 0/7 2/17 0.2 0.45 [0.02, 8.34]<br />
x Gallagher 1985 0/5 0/5 0.0 Not estimable<br />
Goodwin 1983 11/40 3/39 0.4 3.57 [1.08, 11.85]<br />
Grundmann 1982 1/14 0/6 0.1 1.40 [0.06, 30.23]<br />
Jelenko 1978 1/7 1/5 0.2 0.71 [0.06, 8.91]<br />
Lowe 1977 3/77 4/94 0.5 0.92 [0.21, 3.97]<br />
Lucas 1978 7/27 0/27 0.1 15.00 [0.90, 250.25]<br />
Metildi 1984 12/20 12/26 1.4 1.30 [0.75, 2.25]<br />
x Prien 1990 0/6 0/6 0.0 Not estimable<br />
Rackow 1983 6/9 6/8 0.8 0.89 [0.48, 1.64]<br />
SAFE 2004 726/3473 729/3460 95.0 0.99 [0.91, 1.09]<br />
Shah 1977 2/9 3/11 0.4 0.81 [0.17, 3.87]<br />
x Shires 1983 0/9 0/9 0.0 Not estimable<br />
Tollofsrud 1995 0/10 1/10 0.2 0.33 [0.02, 7.32]<br />
Virgilio 1979 1/15 1/14 0.1 0.93 [0.06, 13.54]<br />
Woittiez 1997 8/15 4/16 0.5 2.13 [0.81, 5.64]<br />
Zetterstrom 1981a 0/15 1/15 0.2 0.33 [0.01, 7.58]<br />
Zetterstrom 1981b 2/9 0/9 0.1 5.00 [0.27, 91.52]<br />
Subtotal (95% CI) 780/3783 767/3793 100.0 1.02 [0.93, 1.11]<br />
Test for heterogeneity chi-square = 13.88 df = 14 p = 0.4584<br />
Test for overall effect = 0.41 p = 0.7<br />
02 Hydroxyethylstarch<br />
x Boldt 1993 0/30 0/15 0.0 Not estimable<br />
x Boldt 2001 0/50 0/25 0.0 Not estimable<br />
x Dehne 2001 0/45 0/15 0.0 Not estimable<br />
x Lang 2001 0/21 0/21 0.0 Not estimable<br />
Nagy 1993 2/21 2/20 12.0 0.95 [0.15, 6.13]<br />
Prien 1990 1/6 0/6 2.9 3.00 [0.15, 61.74]<br />
Rackow 1983 5/9 6/8 37.2 0.74 [0.36, 1.50]<br />
x Sirieix 1999 0/8 0/8 0.0 Not estimable<br />
Woittiez 1997 13/27 4/16 29.5 1.93 [0.76, 4.90]<br />
Younes 1998 2/12 3/11 18.4 0.61 [0.12, 3.00]<br />
Subtotal (95% CI) 23/229 15/145 100.0 1.16 [0.68, 1.96]<br />
Test for heterogeneity chi-square = 3.71 df = 4 p = 0.4468<br />
Test for overall effect = 0.55 p = 0.6<br />
03 Modified gelatin<br />
x Boldt 1993 0/15 0/15 0.0 Not estimable<br />
x Boldt 2001 0/25 0/25 0.0 Not estimable<br />
Evans 1996 1/11 2/14 27.3 0.64 [0.07, 6.14]<br />
x Ngo 2001 0/56 0/111 0.0 Not estimable<br />
Tollofsrud 1995 0/10 1/10 23.3 0.33 [0.02, 7.32]<br />
x Wahba 1996 0/10 0/10 0.0 Not estimable<br />
Wu 2001 2/18 3/16 49.4 0.59 [0.11, 3.11]<br />
Subtotal (95% CI) 3/145 6/201 100.0 0.54 [0.16, 1.85]<br />
Test for heterogeneity chi-square = 0.13 df = 2 p = 0.9393<br />
Test for overall effect = 0.98 p = 0.3<br />
04 Dextran<br />
Dawidson 1991 1/10 1/10 1.5 1.00 [0.07, 13.87]<br />
Hall 1978 18/86 16/86 24.7 1.13 [0.62, 2.06]<br />
Karanko 1987 0/14 1/18 2.0 0.42 [0.02, 9.64]<br />
x Modig 1983 0/14 0/17 0.0 Not estimable<br />
x Ngo 2001 0/55 0/111 0.0 Not estimable<br />
Tollofsrud 1995 0/10 1/10 2.3 0.33 [0.02, 7.32]<br />
Vassar 1993a 21/89 11/85 17.4 1.82 [0.94, 3.55]<br />
Vassar 1993b 49/99 20/50 41.1 1.24 [0.83, 1.83]<br />
Younes 1992 7/35 7/35 10.8 1.00 [0.39, 2.55]<br />
Subtotal (95% CI) 96/412 57/422 100.0 1.24 [0.94, 1.65]<br />
Test for heterogeneity chi-square = 2.76 df = 6 p = 0.8379<br />
Test for overall effect = 1.53 p = 0.13<br />
0.01 0.1 1 10 100<br />
favors colloid favors crystalloid<br />
Source: Reprinted with permission from Alderson. 51 Copyright Cochrane Library.<br />
CI = confidence interval, PPF = plasma protein fraction, df = degrees of freedom; x = relative risk not estimable.
302 J. Miller, L.A. Fleisher, and J.L. Carson<br />
Table 20-6. Summary of results of studies comparing colloid versus crystalloid for resuscitation in critically ill patients.<br />
Review: Colloids versus crystalloids for fluid resuscitation in critically ill patients<br />
Comparison: 02 colloid and hypertonic crystalloid versus isotonic crystalloid<br />
Outcome: 01 deaths<br />
Treatment Control Relative risk (fixed) Weight Relative risk (fixed)<br />
Study n/N n/N 95% CI (%) [95% CI]<br />
01 Albumin or PPF<br />
Jelenko 1978 1/7 2/7 100.0 0.50 [0.06, 4.33]<br />
Subtotal (95% CI) 1/7 2/7 100.0 0.50 [0.06, 4.33]<br />
Test for heterogeneity chi-square = 0.00 df = 0<br />
Test for overall effect = 0.63 p = 0.5<br />
02 Hydroxyethylstarch<br />
Subtotal (95% CI) 0/0 0/0 0.0 Not estimable<br />
Test for heterogeneity chi-square = 0.00 df = 0<br />
Test for overall effect = 0.0 p = 1.0<br />
03 Modified gelatin<br />
Subtotal (95% CI) 0/0 0/0 0.0 Not estimable<br />
Test for heterogeneity chi-square = 0.00 df = 0<br />
Test for overall effect = 0.0 p = 1.0<br />
04 Dextran<br />
Chavez-Negrete 1991 1/26 5/23 2.9 0.18 [0.02, 1.41]<br />
Mattox 1991 35/211 42/211 22.6 0.83 [0.56, 1.25]<br />
Vassar 1990 12/23 13/24 6.8 0.96 [0.56, 1.65]<br />
Vassar 1991 30/83 34/83 18.3 0.88 [0.60, 1.30]<br />
Vassar 1993a 21/89 14/84 7.7 1.42 [0.77, 2.60]<br />
Vassar 1993b 49/99 23/45 17.0 0.97 [0.68, 1.37]<br />
Younes 1992 7/35 8/35 4.3 0.88 [0.36, 2.15]<br />
Younes 1994 27/101 40/111 20.5 0.74 [0.49, 1.11]<br />
Subtotal (95% CI) 182/667 179/616 100.0 0.88 [0.74, 1.05]<br />
Test for heterogeneity chi-square = 5.79 df = 7 p = 0.565<br />
Test for overall effect = 1.41 p = 0.16<br />
Source: Reprinted with permission from Alderson. 51 Copyright Cochrane Library.<br />
CI = confidence interval, PPF = plasma protein fraction, df = degrees of freedom.<br />
0.01 0.1 1 10 100<br />
resuscitation is ultimately governed by the clinician’s<br />
preference and the patient’s ability to tolerate the treatment.<br />
Specific studies addressing the use of colloid versus<br />
crystalloid exclusively in the elderly population have not<br />
been performed.<br />
Postoperative Management<br />
Postoperative management must include continued vigilance<br />
in fluid balance. Early resumption of oral intake<br />
should be encouraged. Fluid losses from all sites must be<br />
accurately accounted and carefully replaced. Insensible<br />
losses should be replaced, typically in the range of 500–<br />
1000 mL/day in afebrile patients. Free water replacement<br />
is guided by serum sodium concentration. Third space<br />
losses, such as postoperative ileus, are deposits for extracellular<br />
fluids. Continued attention to the use of nephrotoxic<br />
drugs is imperative in maintaining renal function.<br />
Good urine output postoperatively is a good indication<br />
of renal function and fluid balance. Creatinine measurements<br />
and creatinine clearance measurements are useful<br />
in patients with higher risk of postoperative acute tubular<br />
necrosis.<br />
Special Situations: <strong>Regional</strong> <strong>Anesthesia</strong><br />
<strong>Regional</strong> anesthesia merits additional consideration when<br />
attempting appropriate fluid management in the perioperative<br />
period. Spinal anesthesia inhibits the release of<br />
norepinephrine of sympathetic efferent nerves at the vascular<br />
smooth muscle cells, the sinoatrial node, the atrioventricular<br />
node, and the muscle cells of the heart. <strong>The</strong><br />
degree of sympathetic blockade is determined by the<br />
spread of local anesthetics in the intrathecal fluid. Studies<br />
have shown that sympathetic blockade extends several<br />
dermatomes above the level of sensory blockade, thus<br />
producing hypotension with even a modest degree of<br />
sensory inhibition. 54 <strong>The</strong> response to the effects of sympathetic<br />
blockade is sensed by the vagus nerve input to the<br />
baroreflex receptor; however, the subsequent response of
20. Fluid Management 303<br />
the baroreflex is limited by the amount of vascular bed<br />
remaining for vasoconstriction.<br />
Management of fluids during spinal anesthesia in the<br />
elderly can pose a conflict between competing physiologic<br />
concerns. <strong>The</strong> need to avoid hypotension is apparent, but<br />
the desire to limit fluid overload must also be considered.<br />
Additionally, it should be considered if the elderly have<br />
exaggerated responses to spinal anesthesia compared with<br />
younger patients. Elderly patients have increased sympathetic<br />
tone at rest, which may cause more dramatic changes<br />
in hemodynamics if vascular resistance is abruptly altered<br />
by spinal anesthesia. <strong>The</strong> aged heart is also less responsive<br />
to beta receptor stimulation triggered by the baroreflex to<br />
increase contractility and heart rate. In addition, this population<br />
may be especially sensitive to acute intravascular<br />
volume changes, because of a more preload-dependent<br />
aged ventricle with possible diastolic dysfunction.<br />
Studies are limited that directly compare young and<br />
elderly patients. Young patients have an average of 10%<br />
decreases in vascular resistance and cardiac output.<br />
Elderly patients with a median block of T4 have an<br />
average 10% decrease in cardiac output, but a larger 26%<br />
decrease in systemic vascular resistance. 55 Hypotension<br />
with spinal anesthesia is prevalent, occurring in up to<br />
60% of patients with sympathetic blockade higher than<br />
T7. 56 <strong>The</strong> appropriate treatment for this hypotension has<br />
been examined. Crystalloid preloading has been shown<br />
to have no effect on the incidence of hypotension in<br />
spinal anesthesia. Treatment with a vasopressor is appropriate<br />
if systolic blood pressure decreases by more than<br />
25% of baseline, or below 90 mm Hg. Ephedrine is often<br />
used; however, it may be less effective in the elderly<br />
patient. A pure vasoconstrictor may seem appropriate<br />
because the primary mechanism of hypotension is<br />
decreased systemic vascular resistance. This may have<br />
adverse effects on coronary vascular resistance and afterload.<br />
Epinephrine can also be considered in small doses<br />
to provide some vasoconstriction, with minimal effect on<br />
blood pressure. Excessive tachycardia should be avoided.<br />
Fluid overload should also be avoided to reduce risk of<br />
adverse outcomes such as pulmonary edema, congestive<br />
heart failure, bowel dysfunction, and prolonged fluid<br />
retention. If hypotension is minimized, cardiac performance<br />
is minimally affected by spinal anesthesia and safe<br />
for patients with preexisting cardiac disease as well. 55<br />
Currently, there is no best way to approach fluid management<br />
with regional anesthesia, and either additional fluid<br />
administration or use of vasopressors is appropriate.<br />
Perioperative Transfusion in the Elderly<br />
A discussion of fluid management should also take into<br />
account the need for repletion of blood products and<br />
the effect on fluid requirements. Blood transfusion is an<br />
extensively studied and discussed topic of medical care.<br />
Approximately 12 million units of red blood cells are<br />
transfused each year. Each unit of blood costs about $217<br />
per patient, for a total cost of more than $2 billion a year.<br />
A large majority, 60%–70% of transfusions, occur in the<br />
perioperative period. 57 <strong>The</strong> need for rational decision<br />
making concerning blood transfusion is obvious. <strong>The</strong><br />
following discussion will focus on transfusion of red<br />
blood cells.<br />
Administration of blood-component therapy in a<br />
patient of any age must take into account the indications<br />
for the treatment, the risks, and the benefits of treatment.<br />
<strong>The</strong> objective of red blood cell transfusion is improvement<br />
of inadequate oxygen delivery. <strong>The</strong> use of perioperative<br />
transfusion assumes that surgical patients<br />
experience adverse outcomes as a result of diminished<br />
oxygen-carrying capacity, and that transfusion can prevent<br />
these adverse outcomes. <strong>The</strong> most serious effect of anemia<br />
and reduction of oxygen-carrying capacity is myocardial<br />
ischemia. Younger patients with less comorbidity may<br />
tolerate altered perfusion to less vessel-rich organs well;<br />
however, the elderly patient may have more significant<br />
long-term morbidity.<br />
<strong>The</strong> decision to transfuse a patient in the periopera -<br />
tive period requires consideration of several factors. <strong>The</strong><br />
National Heart, Lung, and Blood Institute Consensus<br />
Conference recommends considering the following: duration<br />
of anemia, intravascular volume, hemodynamic stability,<br />
extent of operation, probability for massive blood<br />
loss, and comorbidities such as impaired pulmonary<br />
function, decreased cardiac output, myocardial ischemia,<br />
cerebrovascular or peripheral vascular disease. 58<br />
Correlations between acute changes in intravascular<br />
volume and hemodynamic stability have been defined<br />
previously. <strong>The</strong> American College of Surgeons has classified<br />
hypovolemia caused by blood loss according to signs<br />
and symptoms. 59 Class I hemorrhage is a loss of up to<br />
15% of blood volume and usually causes vasoconstriction<br />
and mild tachycardia. Class II hemorrhage is attributable<br />
to a loss of 15%–30% of blood volume, and produces<br />
tachycardia and decreased pulse pressure. Patients who<br />
are awake may exhibit anxiety or restlessness. Class III<br />
hemorrhage is attributable to 30%–40% of blood volume<br />
loss, and causes marked tachycardia, tachypnea, hypotension,<br />
and altered mental status. Class IV hemorrhage,<br />
occurring after loss of more than 40% of blood volume,<br />
results in marked tachycardia, hypotension, narrow pulse<br />
pressure, decreased urine output, and markedly depressed<br />
mental status.<br />
Use of physical signs may be helpful perioperatively,<br />
but may not be as reliable for the anesthetized patient.<br />
Measurements of vital signs that typically indicate anemia<br />
or hypovolemia may be altered by the depressant effects<br />
of general anesthetics. Signs of organ ischemia under<br />
anesthesia can be subtle. Intraoperative myocardial
304 J. Miller, L.A. Fleisher, and J.L. Carson<br />
ischemia is associated with tachycardia in only 26% of<br />
patients, and hypotension in less than 10%. Perioperative<br />
cardiac ischemia is often silent. Ischemic events may<br />
occur during a period of decreased monitoring in the<br />
postoperative period because of pain, fever, shivering,<br />
or physical activity. Invasive monitoring can provide<br />
additional parameters to measure blood volume, but<br />
introduce other risk factors. Blood pressure measurement,<br />
oxygen delivery, and oxygen extraction are global<br />
indicators, but are not representative of organ-specific<br />
oxygen delivery.<br />
Estimation of surgical blood loss is routinely recorded<br />
by the anesthesiologist. Intraoperative blood loss is typically<br />
estimated by examining the surgical field, collected<br />
blood in suction containers, and the presence of sponges<br />
saturated with blood. <strong>The</strong>se estimates are notoriously<br />
inaccurate. Laboratory evidence of hemorrhage is used<br />
to supplement decision making in the operative period.<br />
However, intercompartmental fluid shifts during surgery<br />
and the dilutional effects of crystalloid therapy can make<br />
intraoperative hemoglobin concentrations unreliable<br />
representations of clinical status.<br />
<strong>The</strong> patient’s ability to tolerate acute anemia is altered<br />
by general anesthesia as well. Most anesthetics decrease<br />
myocardial function, resulting in decreased blood pressure,<br />
cardiac output, stroke volume, peripheral vascular<br />
resistance, and oxygen consumption. Depression of the<br />
central nervous system also decreases cerebral metabolic<br />
demands. Hypothermia also reduces metabolic rate.<br />
Anesthetics may affect the body’s ability to compensate<br />
for anemia by reducing the ability to augment cardiac<br />
output in response to hypovolemia. Decreased hepatic<br />
blood flow may inhibit the ability to metabolize lactic<br />
acid, thus worsening an acid-base abnormality due to<br />
decreased perfusion. Compensatory factors such as<br />
augmenting cardiac output may be inhibited by pharmacologic<br />
interventions, such as beta-blockade or use of<br />
calcium channel blockers. <strong>The</strong> complexity of these alterations<br />
defies simple prediction for the need for blood<br />
transfusion therapy. Evidence-based evaluation of bloodcomponent<br />
therapy and established guidelines are most<br />
helpful in making these difficult clinical decisions. <strong>The</strong><br />
additional confounding factors of increased age and<br />
comorbidity make the issue increasingly complex.<br />
<strong>The</strong> consideration of the risks of blood transfusion<br />
must also be balanced in the decision to transfuse. Frequently<br />
cited risks include nonhemolytic transfusion<br />
reaction, transfusion reactions, transmission of infectious<br />
disease, and possible effects of immunosuppression.<br />
<strong>The</strong> initial recommendations concerning transfusion<br />
focused on calculations, stating that oxygen availability<br />
to tissues may be decreased when hemoglobin decreases<br />
below 10 g/dL. Clinical experience has repeatedly demonstrated<br />
that hemoglobin values less than 10 g/dL are<br />
well tolerated in the perioperative period. Other studies<br />
have demonstrated that cardiac output begins to increase<br />
dramatically as hemoglobin decreases below 7 g/dL. A<br />
recent study illustrates the effect of hemoglobin levels<br />
on mortality and morbidity in the perioperative period.<br />
A retrospective study by Carson et al. 60 examining 1958<br />
patients, aged 18 and older, that declined blood prod -<br />
ucts during the perioperative period found that overall<br />
mortality increased with decreasing hemoglobin. Also,<br />
patients with underlying cardiovascular disease defined<br />
as congestive heart failure, angina pectoris, or peripheral<br />
vascular disease, had a greater risk of death at any given<br />
hemoglobin concentration, compared with patients<br />
without cardiovascular disease (Table 20-7).<br />
<strong>The</strong> mortality risk greatly increased when hemoglobin<br />
concentration decreased to below 10 g/dL. Risk of death<br />
was extremely high when hemoglobin concentration<br />
decreased below 5–6 g/dL. 60 This information is helpful in<br />
demonstrating the effect of anemia, but does not address<br />
a decrease in risk of death as a result of receiving transfusions.<br />
<strong>The</strong> most important randomized study in assessing<br />
blood transfusion therapy was the Transfusion Require-<br />
Table 20-7. Adjusted odds ratio (95% confidence interval) for mortality and preoperative hemoglobin and decline in hemoglobin<br />
stratified by cardiovascular disease.<br />
Decline
20. Fluid Management 305<br />
ments in Critical Care (TRICC) study. 61 This was the only<br />
randomized trial with adequate power to evaluate clinical<br />
outcomes of anemia and transfusion practices. A group<br />
of 833 volume-resuscitated patients in the ICU were randomized<br />
to a liberal or restrictive transfusion threshold<br />
level. <strong>The</strong> restrictive group received transfusions at a<br />
hemoglobin concentration less than 7g/dL and was maintained<br />
at a hemoglobin between 7 and 9 g/dL. <strong>The</strong> liberal<br />
transfusion threshold group was transfused for hemoglobin<br />
concentrations less than 10 g/dL and maintained<br />
between 10–12 g/dL. <strong>The</strong> findings were not statistically<br />
significant; however, 30-day mortality was lower in the<br />
restrictive transfusion group. <strong>The</strong> restrictive transfusion<br />
group had a relative reduction in transfusion of 55%,<br />
which could result in significant cost savings. Further<br />
analysis identified a subgroup of patients that were<br />
younger than 55 years and less severely ill (as defined by<br />
APACHE II scores less than 20) in the restrictive transfusion<br />
strategy who were half as likely to die (p < 0.02)<br />
within the 30-day period, compared with the liberal transfusion<br />
strategy. 62 Another subgroup in this study consisted<br />
of 257 patients with ischemic heart disease. This<br />
group had a nonsignificant (p = 0.3) decrease in overall<br />
survival among those patients treated with the restrictive<br />
therapy regimen. Further investigation is required to<br />
determine groups that may benefit from a higher transfusion<br />
threshold, such as patients with cardiac disease,<br />
emphysema, more severe illness, cerebrovascular disease,<br />
trauma, and older patients. Patients with cardiac disease<br />
may be unable to tolerate compensatory responses to<br />
hypovolemia and anemia, such as increasing cardiac<br />
output and heart rate. Increasing chronotropy decreases<br />
coronary artery filling time and reduces blood flow to<br />
the endocardium at a time when metabolic demands are<br />
increased. As a result, myocardial ischemia may result at<br />
higher hemoglobin values of 20–30 g/dL.<br />
As yet, there are no randomized clinical trials that<br />
evaluated transfusion thresholds in patients with cardiovascular<br />
disease. Several observational studies have provided<br />
some insight but have come to different conclusions.<br />
In a group of 190 elderly patients undergoing radical<br />
retropubic prostatectomy, patients with a hematocrit of<br />
less than 28 were at a significantly higher risk of myocardial<br />
ischemia intraoperatively and postoperatively.<br />
Hematocrit levels also correlated with the duration of<br />
myocardial ischemic episodes. 63 Similarly, a group of 27<br />
high-risk patients undergoing infrainguinal arterial<br />
bypass procedures, who were monitored for 80 hours<br />
postoperatively, were determined to have a higher risk of<br />
morbid cardiac events when hematocrit decreased to less<br />
than 28%. 64 A retrospective study of more than 78,000<br />
Medicare patients older than 65 years admitted with<br />
acute myocardial infarction who received a blood transfusion<br />
had a decrease in short-term mortality when the<br />
patient’s admission hematocrit was less than 33%. Lower<br />
hemoglobin values correlated with more frequent in-hospital<br />
events, such as heart failure, shock, and death and<br />
with increased length of hospital stay. 65 However, a recent<br />
analysis in 24,112 patients enrolled in three clinical trials<br />
with acute coronary syndrome came to the opposite conclusion.<br />
66 Patients receiving blood transfusion had about<br />
a three- to fourfold higher risk of death and myocardial<br />
infarction than patients not receiving transfusion. Finally,<br />
a retrospective cohort study of 3783 patients with cardiovascular<br />
disease undergoing hip fracture repair found<br />
that postoperative transfusion at a hemoglobin of 8 g/dL<br />
or higher did not influence mortality. 67 Thus, large clin -<br />
ical trials are needed to provide high-quality evidence to<br />
guide transfusion decisions in patients with cardiovascular<br />
disease.<br />
<strong>The</strong>re are few high-quality studies that establish the<br />
critical transfusion thresholds. <strong>The</strong> best evidence comes<br />
from the TRICC trial, which found a 7 g/dL threshold<br />
was at least as safe, and may be preferable, to a 10 g/dL<br />
threshold in critical care patients. Whether these results<br />
are applicable to geriatric patients undergoing surgery is<br />
unknown. Pending additional clinical trials, the best<br />
data suggest that a restrictive transfusion trigger (7 g/dL)<br />
should be used in most patients. It is unclear whether a<br />
higher transfusion threshold, 9–10 g/dL, should be used in<br />
patients with cardiovascular disease.<br />
<strong>The</strong> American Society of Anesthesiologists evidencebased<br />
guidelines for transfusion therapy from 1994 are<br />
still relevant today. Selected recommendations as related<br />
to red blood cell transfusion are summarized below 57 :<br />
1. Transfusion is rarely indicated at hemoglobin levels<br />
greater than 10 g/dL, and is almost always indicated when<br />
hemoglobin is less than 6 g/dL.<br />
2. Transfusion of a patient with a hemoglobin concentration<br />
between 6–10 g/dL is based on the patient’s risk<br />
for complications as a result of inadequate oxygenation.<br />
3. Use of a single hemoglobin “trigger” or other<br />
approaches that do not consider physiologic and surgical<br />
factors regarding oxygen delivery requirements is not<br />
recommended.<br />
4. Preoperative autologous blood donation, intra -<br />
operative blood recovery, acute normovolemic hemodilution,<br />
and physiologic or pharmacologic measures to<br />
decrease blood loss may be beneficial. However, in our<br />
opinion, these methods have not been established to<br />
work, and their application is at least very limited. <strong>The</strong>se<br />
methodologies result in cell salvage with significant blood<br />
loss, and normovolemic hemodilution has not been established<br />
to be effective, because it results in a need to make<br />
patients more anemic than can be tolerated.<br />
5. Indications to transfuse autologous red blood cells<br />
may be more liberal than allogeneic red blood cells. We<br />
do not agree with this recommendation, because the risk<br />
of mislabeling may still lead to risks at transfusion.
306 J. Miller, L.A. Fleisher, and J.L. Carson<br />
Conclusion<br />
<strong>The</strong> elderly patient is a challenge to the anesthesiologist<br />
because of the tremendous variability of their physiologic<br />
conditions. This is often combined with a limited ability<br />
to provide accurate clinical history. <strong>The</strong> goal of this discussion<br />
of fluid management in the elderly is to provide<br />
a summary of the known data concerning fluid management<br />
and patients in the perioperative period. <strong>The</strong>se data<br />
can be combined with knowledge of a patient’s comorbidities<br />
and used as a basis to inform clinical decision<br />
making for specific patients. Perhaps the most important<br />
and difficult concept for clinicians to grasp is that few<br />
generalizations will hold for all elderly patients, and<br />
careful observation and adaptability in treatment may<br />
prove most beneficial for the patient.<br />
References<br />
1. Liu LL, Leung JM. Perioperative complications in the<br />
elderly patient. Available at: http://www.asahq.org/clinical/<br />
geriatrics/perio_comp.htm. Accessed May, 2003.<br />
2. Luckey A, Parsa C. Fluid and electrolytes in the aged. Arch<br />
Surg 2003;138:1055–1060.<br />
3. Vander AJ, Sherman JH, Luciano DS. Human Physiology:<br />
<strong>The</strong> Mechanisms of Body Function. 6th ed. New York:<br />
McGraw-Hill; 1994:539.<br />
4. Holte K, Sharrock NE, Kehlet H. Pathophysiology and<br />
clinical implications of perioperative fluid excess. Br J<br />
Anesth 2002;89(4):622–632.<br />
5. Wei JY. Age and cardiovascular system. N Engl J Med<br />
1992;327:1735–1739.<br />
6. Epstein M. Aging and the kidney. J Am Soc Nephrol<br />
1996;7:1106–1122.<br />
7. Rowe JW. Clinical research on aging; strategies and directions.<br />
N Engl J Med 1977;297:1332–1336.<br />
8. Epstein M, Hollenberg NK. Age as a determinant of renal<br />
sodium conservation in normal man. J Lab Clin Med 1976;<br />
87:411–417.<br />
9. Hollenberg NK, Adams DF, Solomon HS, Rashid A, Abrams<br />
HL, Merrill JP. Senescence and the renal vasculature in<br />
normal man. Circ Res 1974;34:309–316.<br />
10. Rowe JW, Andres R, Tobin JD, Norris AH, Shock NW. <strong>The</strong><br />
effect of age on creatinine clearance in man: a cross sectional<br />
and longitudinal study. J Gerontol 1976;31:155–163.<br />
11. Fliser D, Aeier M, Nowack R, Ritz E. Renal functional<br />
reserve in healthy elderly subjects. J Am Soc Nephrol 1993;<br />
3:1371–1377.<br />
12. Faulstick D, Yeingst MJ, Oussler DA, Shock NW. Glomerular<br />
permeability in young and old subjects. J Gerontol 1962;<br />
17:40–44.<br />
13. McDonald RK, Solomon DH, Shock NW. Aging is a factor<br />
in the renal hemodynamic changes induced by a standard<br />
pyrogen. J Clin Invest 1951;30:457–462.<br />
14. Wesson LG. Renal hemodynamics in physiological states.<br />
In: Physiology of the Human Kidney. New York: Grune and<br />
Stratton; 1969:96–108.<br />
15. Lindeman RD, Tobin JD, Shock NW. Longitudinal studies<br />
on the rate of decline in renal function with age. J Am<br />
Geriatr Soc 1985;33:278–285.<br />
16. Crockroft DW, Gault MH. Prediction of creatinine clearance<br />
from serum creatinine. Nephron 1976;16:31–41.<br />
17. Goldberg TH, Finkelstein MS. Difficulties in estimating<br />
glomerular filtration rate in the elderly. Arch Intern Med<br />
1987;147:1430–1433.<br />
18. Malmrose LC, Gray SL, Peiper CF, et al. Measured versus<br />
estimated creatinine clearance in a high functioning elderly<br />
sample: MacArthur Foundation study of successful aging.<br />
J Am Geriatr Soc 1988;36:437–441.<br />
19. Crane MG, Harris JJ. Effect of aging on renin activity and<br />
aldosterone excretion. J Lab Clin Med 1976;87:947–959.<br />
20. Weidmann P, Demyttenaere-Bursztein S, Maxwell MH,<br />
DeLima J. Effect of aging on plasma renin and aldosterone<br />
in normal man. Kidney Int 1975;8:325–333.<br />
21. Shannon RP, Wei JY, Rosa RM, Epstein FH, Rowe JH.<br />
<strong>The</strong> effect of age and sodium depletion on cardiovascular<br />
response to orthostasis. Hypertension 1986;8:438–443.<br />
22. Sunderam SG, Mankikar GD. Hyponatremia in the elderly.<br />
Age Aging 1983;12:77–80.<br />
23. Snyder NA, Feigal DW, Ariff AI. Hypernatremia in elderly<br />
patients: a heterogenous, morbid and iatrogenic entity. Ann<br />
Intern Med 1987;107:309–319.<br />
24. Beck LH. Changes in renal function with aging. Clin Geriatr<br />
Med 1998;14(2):199–209.<br />
25. Rowe JW, Shock NW, DeFronzo RA. <strong>The</strong> influence of age<br />
on the renal response to water deprivation in man. Nephron<br />
1976;17:270–278.<br />
26. Helderman JH, Vestal RE, Rowe JW, Tobin JD, Andres R,<br />
Robertson GL. <strong>The</strong> response of arginine vasopressin to<br />
intravenous ethanol and hypertonic saline in man: the<br />
impact of aging. J Gerontol 1978;33:39–47.<br />
27. Rowe JW, Minaker KL, Sparrow D, Robertson GL. Agerelated<br />
failure of volume–pressure-mediated vasopressin<br />
release. J Clin Endocrinol Metab 1982;54:661–664.<br />
28. Duggan J, Kilfeather S, Lightman SL. <strong>The</strong> association of age<br />
with plasma arginine vasopressin and plasma osmolality.<br />
Age Ageing 1993;22:332–336.<br />
29. Frolkis VV, Golovchenko SF, Medved VI, Frolkis RA. Vasopressin<br />
and cardiovascular system in aging. Gerontology<br />
1982;28:290–302.<br />
30. Kirkland J, Lye M, Goddard C, Vargas E, Davies I. Plasma<br />
arginine vasopressin in dehydrated elderly patients. Clin<br />
Endocrinol 1984;20:451–456.<br />
31. Phillips PA, Rolls BY, Ledingham JG, Forsling ML, Morton<br />
JJ, Crowe MJ. Reduced thirst after water deprivation in<br />
healthy elderly men. N Engl J Med 1984;311:753–759.<br />
32. Howard L, Ashley C. Nutrition in the perioperative patient.<br />
Ann Rev Nutr 2003;23:263–282.<br />
33. Flynn MB, Leightty FF. Preoperative outpatient nutritional<br />
support of patients with squamous cancer of the upper<br />
aerodigestive tract. Am J Surg 1987;154(4):359–362.<br />
34. Foschi D, Cavagna G, Callioni F, Morandi E, Rovati V. Hyperalimentation<br />
of jaundiced patients on percutaneous trans<br />
hepatic biliary drainage. Br J Surg 196;73(9):716–719.<br />
35. Shukla HS, Rao RR, Banu N, Gupta RM, Yaday RC. Enteral<br />
hyperalimentation in malnourished surgical patients. Ind J<br />
Med Res 1984;80:339–346.
20. Fluid Management 307<br />
36. Von Meyenfeldt MF, Meijerink WJHJ, Rouflart MMJ,<br />
Builmaassen MTHJ, Soeters PB. Perioperative nutritional<br />
support: a randomized clinical trial. Clin Nutr 1992;11:180–<br />
\186.<br />
37. Sandstom R, Drott C, Hytlander A, et al. <strong>The</strong> effect of<br />
postoperative intravenous feeding (TPN) on outcome<br />
following major surgery evaluated in a randomized study.<br />
Ann Surg 1993;217:185–195.<br />
38. Delmi M, Rapin CH, Bengoa JM, et al. Dietary supplementation<br />
in elderly patients with fractured neck of femur.<br />
Lancet 1990;335(8698):1013–1016.<br />
39. Lavizzo-Mourey R, Johnson J, Stolley P. Risk factors for<br />
dehydration among elderly nursing home residents. J Am<br />
Geriatr Soc 1988;36:213–218.<br />
40. Barlow I. Perioperative renal insufficiency and failure<br />
in elderly patients. Available at: www.asahq.org/clinical/<br />
geriatrics. Accessed 5/2003.<br />
41. Mcgee S, Abernethy WB, Simel DL. Is this patient hypovolemic?<br />
JAMA 1999;281(11):1022–1029.<br />
42. Beck LH. Perioperative renal, fluid, and electrolyte management.<br />
Clin Geriatr Med 1990;6(3):557–569.<br />
43. Alpert RA, Roizen MF, Hamilton WK, et al. Intraoperative<br />
urinary output does not predict postoperative renal function<br />
in patients undergoing abdominal aortic revascularization.<br />
Surgery 1984;95:707–711.<br />
44. Gan TJ, Soppitt A, Maroof M, et al. Goal-directed intraoperative<br />
fluid administration reduced length of hospital stay<br />
after major surgery. <strong>Anesthesiology</strong> 2002;97(4):820–826.<br />
45. Sinclair S, James S, Singer M. Intraoperative intravascular<br />
volume optimisation and length of hospital stay after repair<br />
of proximal femoral fracture. Br Med J 1997;315(7113):<br />
909–912.<br />
46. Venn R, Steele A, Richardson P, Poloniecki J, Grounds M,<br />
Newman P. Randomized controlled trial to investigate the<br />
influence of the fluid challenge on duration of hospital stay<br />
and perioperative morbidity in patients with hip fractures.<br />
Br J Anesth 2002;88:65–71.<br />
47. Price JD, Sear JW, Venn RM. Perioperative fluid volume<br />
optimization following proximal femoral fracture. Cochrane<br />
Database Syst Rev 2004;(1):CD003004.<br />
48. Shoemaker WC, Appel PL, Kram HB, Waxman K, Lee TS.<br />
Prospective trial of supranormal values of survivors as therapeutic<br />
goals in high risk surgical patients. Chest 1988;<br />
94:1176–1186.<br />
49. Scalea TM, Simon HM, Duncan AO, et al. <strong>Geriatric</strong> blunt<br />
multiple trauma: improved survival with early invasive<br />
monitoring. J Trauma 1990;30(2):129–134.<br />
50. Velanovich V. Crystalloid versus colloid fluid resuscitation:<br />
a meta-analysis of mortality. Surgery 1989;105(1):65–71.<br />
51. Alderson P, Schierhout G, Roberts I, Bunn F. Colloids versus<br />
crystalloids for fluid resuscitation in critically ill patients.<br />
Cochrane Database Syst Rev 2000;(2):CD000567.<br />
52. Bunn F, Alderson P, Hawkins V. Colloid solutions for<br />
fluid resuscitation. Cochrane Database Syst Rev 2003;(1):<br />
CD001319.<br />
53. Finfer S, Bellomo R, Boyce N, et al. A comparison of albumin<br />
and saline for fluid resuscitation in the intensive care unit.<br />
NEJM 2004;350:2247–2256.<br />
54. Rooke GA. Cardiovascular response to spinal anesthesia<br />
in the elderly. Available at: www.asahq.org/clinical/<br />
geriatrics. Accessed May 2003.<br />
55. Rooke GA, Freund PR, Jacobson AF. Hemodynamic<br />
response and change in organ blood volume during spinal<br />
anesthesia in elderly men with cardiac disease. Anesth<br />
Analg 1997;85:99–105.<br />
56. Coe AJ, Revanas B. Is crystalloid preloading useful in<br />
spinal anesthesia in the elderly? Anaesthesia 1990;45:241–<br />
243.<br />
57. Nutall GA, Brost BC, Connis RT, et al. Practice Guidelines<br />
for Blood Com ponent <strong>The</strong>rapy: a report by the American<br />
Society of Anesthesiologist Task Force on Blood Component<br />
<strong>The</strong>rapy. <strong>Anesthesiology</strong> 1996;84(3):732–747.<br />
58. Perioperative red cell transfusion. Natl Inst Health Consens<br />
Dev Conf Consens Statement 1988;7(4):1–19.<br />
59. American College of Surgeons, Committee on Trauma.<br />
Advanced Trauma Life Support Course Manual. Chicago:<br />
American College of Surgeons; 1989.<br />
60. Carson JL, Duff A, Poses RM, et al. Effect of anemia and<br />
cardiovascular disease on surgical mortality and morbidity.<br />
Lancet 1996;348:1055–1060.<br />
61. Herbert PC, Wells G, Blajchman MA, et al. A multicenter,<br />
randomized, controlled clinical trial of transfusion requirements<br />
in critical care. N Engl J Med 1999;340(6):409–<br />
417.<br />
62. Ely EW, Bernard GR. Transfusions in critically ill patients.<br />
N Engl J Med 1999;340(6):467–468.<br />
63. Hogue CW, Goudnough LR, Monk TG. Perioperative myocardial<br />
ischemic episodes are related to hematocrit level<br />
in patients undergoing radical prostatectomy. Transfusion<br />
1998;38:924–931.<br />
64. Nelson AH, Fleisher LA, Rosenbaum SH. Relationship<br />
between postoperative anemia and cardiac morbidity in<br />
high-risk vascular patients in the intensive care unit. Crit<br />
Care Med 1993;21:860–866.<br />
65. Wei-Chih W, Rathore S, Wang Y, Radford M, Krumholz H.<br />
Blood transfusions in elderly patients with acute myocardial<br />
infarction. N Engl J Med 2001;345(17):1230–1236.<br />
66. Rao SV, Jollis JG, Harrington RA, et al. Relationship of<br />
blood transfusion and clinical outcomes in patients with<br />
acute coronary syndromes. JAMA 2004;292(13):1555–<br />
1562.<br />
67. Carson JL, Duff A, Berlin JA, et al. Perioperative blood<br />
transfusion and postoperative mortality. JAMA 1998;<br />
279(3):199–205.
21<br />
Pain Management<br />
Jack M. Berger<br />
<strong>The</strong> United States senior population is expected to double<br />
over the next 30 years (www.agingstats.gov). According<br />
to the latest data from the National Center for Health<br />
Statistics, 40.3 million inpatient surgical procedures were<br />
performed in the United States in 1996, followed closely<br />
by 31.5 million outpatient surgeries. <strong>The</strong>se statistics are<br />
from 1996 and although the ratio of outpatient to inpatient<br />
procedures may have changed in the past 10 years,<br />
the total number of surgical procedures per year has not<br />
diminished. And certainly, the elderly undergo a disproportionate<br />
number of surgical procedures compared with<br />
younger age groups. <strong>The</strong>refore, acute pain secondary to<br />
surgery will continue to be a significant problem for<br />
physicians.<br />
In addition, estimates are that 80%–85% of individuals<br />
over 65 years old have at least one significant health<br />
problem that predisposes them to pain. Epidemiologists<br />
at Brown University (reporting in JAMA, June 17, 1998)<br />
found that between 25%–40% of older cancer patients<br />
studied had daily pain. Among these patients, 21%<br />
between the ages of 65 and 74 received no pain medication<br />
at all. Of those 75–84 years old, 26% received no pain<br />
medication, and for those older than 85, 30% were left<br />
untreated. 1<br />
In northern California, Jury Verdict No. H205732–1 of<br />
the California Superior Court awarded $1.5 million to the<br />
family of an elderly lung cancer patient in a civil suit in<br />
which the physician was found liable for recklessness and<br />
elder abuse for failure to prescribe adequate pain medication.<br />
This resulted in California Assembly Bill 487 that<br />
now requires every physician in California to obtain 12<br />
continuing medical education credits in pain management<br />
and palliative care in the next 3 years in order to<br />
renew their license. And so as much as providing adequate<br />
pain management is a moral obligation, inadequate<br />
pain management has become a liability.<br />
<strong>The</strong>re are about 1.5 million frail elderly residing in<br />
20,000 nursing homes in the United States. Forty percent<br />
are over the age of 85 years. Forty-five percent to 85%<br />
may have pain as compared with 25%–50% of community-dwelling<br />
elderly. 2,3 A telephone poll conducted by<br />
Cooner and Amorosi from Louis Harris and Associates<br />
of New York City in 1997, revealed that more than half of<br />
older adults had taken prescription pain medications for<br />
longer than 6 months, and 45% had visited at least three<br />
physicians for their pain in the last 5 years. 4 New pain<br />
visits to physicians are most common in the 15- to 44-yearold<br />
group, whereas the lowest are in the elderly. Persistent<br />
pain complaints, however, are most common in the elderly,<br />
and pain is the most common symptom noted by the consulting<br />
physician. 5 Yet elderly people and young children<br />
are often perceived by the health care delivery system as<br />
being insensitive to pain. And therefore those who are<br />
most dependent on the health care system are most likely<br />
to receive the least optimal care for pain.<br />
Pain is a highly subjective, variable sensory and emotional<br />
experience, with a pathophysiology composed of<br />
complex neuroanatomic and neurochemical processes. 6<br />
Everyone has an intuitive idea of what pain is. Pain is<br />
always something that “hurts.” But many things hurt. A<br />
broken arm hurts. This is an example of acute somatic<br />
pain. A heart attack hurts. This is ischemic pain. A kidney<br />
stone and appendicitis hurt, which are examples of visceral<br />
pain. An amputated leg may hurt; this is phantom<br />
limb pain. An individual may hurt in the arm or leg on<br />
the side affected by a stroke. Both of these are examples<br />
of central neuropathic pain. <strong>The</strong> death of a loved one<br />
“hurts.” It is a “painful emotional experience” for which<br />
we use the same words of description as for physical<br />
injury. It is clear then that the perception of “pain” is<br />
always subjective and takes place in the brain. Tissue<br />
injury is perceived as nociception. But the site of the<br />
nociception does not necessarily correspond to the area<br />
of the body in which “the pain” is felt. Furthermore, the<br />
tissue injury may have actually healed while the perception<br />
of pain persists.<br />
308
21. Pain Management 309<br />
Three Pain Scenarios<br />
It is quite clear from the above introduction that pain in<br />
the elderly follows one of three scenarios:<br />
1. Acute pain results from surgery, cancer, fractures,<br />
medical conditions such as vascular ischemia, herpes<br />
zoster.<br />
2. Chronic pain results from various persistent medical<br />
and physical conditions. Specific chronic pain syndromes<br />
that are known to affect the geriatric population disproportionately<br />
include: arthritis which may affect 80% of<br />
patients over 65, cancer, herpes zoster and postherpetic<br />
neuralgia, temporal arteritis, polymyalgia rheumatica,<br />
atherosclerotic peripheral vascular disease, diabetic neuropathy,<br />
and back pain syndromes. 6 In chronic pain states,<br />
there is often the absence of the “normal” physiologic<br />
indicators of acute pain such as tachycardia, hypertension,<br />
and diaphoresis. Yet, there may be hyperpathia, allodynia,<br />
and hyperalgesia in the absence of any physical<br />
findings of tissue injury:<br />
• Allodynia is pain elicited by a nonnoxious stimulus<br />
(clothing, air movement, touch), mechanical (induced<br />
by light pressure), thermal (induced by a nonpainful<br />
cold or warm stimulus).<br />
• Hyperalgesia is exaggerated pain response to a<br />
mildly noxious (mechanical or thermal) stimulus.<br />
• Hyperpathia is delayed and explosive pain response<br />
to a noxious stimulus.<br />
3. Finally, there are those who are suffering from persistent<br />
pain who then experience a new acute injury or<br />
exacerbation of their primary condition that is superimposed<br />
on their primary pain state.<br />
Elderly patients present special problems with respect<br />
to treating pain in each of these three scenarios.<br />
Depression, Anxiety, and Pain<br />
Associations between pain and depression are well documented<br />
in elderly patients. 7,8 Studies show that elderly<br />
subjects who are anxious and/or depressed voice more<br />
localized pain complaints than their nonanxious and nondepressed<br />
counterparts. Furthermore, anxious and/or<br />
depressed individuals report more intense pain. 9 Clinical<br />
evidence suggests that cognitive impairment may be<br />
exacerbated by pain and/or its treatment, especially in the<br />
elderly. <strong>The</strong>se patients may benefit dramatically from psychologic<br />
or psychiatric interventions. Common missed<br />
diagnoses or underdiagnosed diseases in the elderly that<br />
can cause pain are: endocrine disorders, neurologic disorders,<br />
major medical disorders including electrolyte imbalances,<br />
polypharmacy, dysphoria, sleep disturbances, and<br />
loss of appetite, etc. 6<br />
Assessment<br />
Many older adults are afraid to report pain. 10,11 <strong>The</strong>re is<br />
often fear of losing independence because of chronic<br />
illness. If an older adult fears that reporting pain will lead<br />
to a debilitating diagnosis that may cause nursing home<br />
placement or further loss of physical independence, he or<br />
she may be less likely to report it. Or the patient may fear<br />
additional procedures, diagnostic tests, or medication prescriptions<br />
that may result from reporting pain. For acute<br />
postoperative pain, this is less of a problem unless the<br />
patient has dementia or other condition that prevents<br />
direct communication.<br />
Elderly patients may present special problems in<br />
obtaining an accurate pain history. Failures in memory,<br />
depression, and sensory impairments may hinder historytaking.<br />
<strong>The</strong>y may tend to underreport symptoms because<br />
they expect pain associated with aging and their diseases,<br />
or because they just do not want to be a bother to anyone.<br />
<strong>The</strong> inability to be aware of, and to verbalize, one’s emotional<br />
state is called alexithymia. Patients with chronic<br />
pain have been found to have a significant incidence<br />
(33%) of alexithymia. This may be a factor in causing<br />
geriatric patients to express emotional distress more<br />
often through somatic complaints because they have<br />
been found to be more alexithymic. 12<br />
Nociception Is Not Pain<br />
Activity induced in the nociceptor and nociceptive pathways<br />
by a noxious stimulus is not pain, which is always a<br />
psychologic state. Although we appreciate that pain most<br />
often has a proximate physical cause, especially acute<br />
pain, activity in nociceptor systems is not equivalent to<br />
the experience of pain. <strong>The</strong> recognition that pain serves<br />
an important biologic function related to survival, raises<br />
the important question: To what extent do age-related<br />
changes in nociception affect the capacity of the pain<br />
experience to fulfill an “enteroceptive” function (such as<br />
thirst, hunger, and thermoception that constitute sensory<br />
indexes of the health of the body)? 13<br />
Age does not seem to affect success of traditional interventions<br />
for the treatment of pain. Assessment and intervention<br />
for pain in the elderly should begin with the<br />
assumption that all neurophysiologic processes subserving<br />
nociception are intact. That is to say, tissue injury<br />
produces the same intensity of stimulus in an elderly<br />
person as in a young person. <strong>The</strong>re are data to suggest<br />
that there is impairment of Aδ fibers with aging and<br />
therefore of the early warning of tissue injury. 13 <strong>The</strong>re are<br />
also data that suggest that widespread and substantial<br />
changes in structure, neurochemistry, and function occur<br />
in the dorsal horn of the spinal cord and central nervous<br />
system (CNS) with aging. 13
310 J.M. Berger<br />
Multiple studies report reductions in the descending<br />
inhibitory modulating systems for nociception in the<br />
elderly. Gibson and Ferrell 13 conclude that the reduced<br />
efficacy of endogenous analgesic systems might be ex -<br />
pected to result in a more severe pain after prolonged<br />
noxious stimulation. It is also possible that documented<br />
decline in afferent transmission pathways could be offset<br />
by a commensurate reduction in the endogenous inhibitory<br />
mechanisms of older persons, with a net result of<br />
little or no change in the perceptual pain experience. 13<br />
<strong>The</strong>y further conclude that any deficit in endogenous<br />
analgesic response (which is stimulus intensity dependent)<br />
will become critical, thereby making it more difficult<br />
for persons of advanced age to cope with severe or<br />
persistent clinical pain conditions. 13<br />
Although there is controversy over whether the<br />
number and integrity of nociceptors decreases with age,<br />
the position that age dulls the sense of pain is untenable. 13<br />
It is the processing of the nociceptive information that<br />
may be altered in the elderly, and the elderly may be<br />
more sensitive to the side effects of medications that are<br />
used to treat pain. <strong>The</strong>se observations thereby give the<br />
impression that the elderly are less sensitive to pain. But<br />
no physiologic changes in pain perception in the elderly<br />
have been demonstrated according to a recent five-state<br />
study. 1 One would not assume that a surgical incision in<br />
an elderly patient will “hurt” less and therefore does not<br />
need to be treated. Likewise, anyone who has observed<br />
an elderly patient with acute herpes zoster certainly can<br />
attest to the excruciating pain that these unfortunate<br />
patients report.<br />
Pathophysiology of Types of Pain<br />
Somatic Pain<br />
A noxious stimulus in the periphery activates nociceptors.<br />
This results in a release of pain-producing subs -<br />
tances, e.g., prostaglandins, leukotrienes, and substance<br />
P. Impulses travel via Aδ and C fibers to the dorsal horn<br />
of the spinal cord. Somatic pain is well localized and<br />
gnawing. <strong>The</strong>re is often associated tenderness and swelling.<br />
Examples include fractures, bone metastasis, and<br />
postoperative pain. This type of pain is usually opioid<br />
responsive.<br />
Visceral Pain<br />
When viscera are stretched, compressed, invaded, or<br />
distended, pain will result. <strong>The</strong> pain is poorly localized<br />
and may be referred. It is described as deep, squeezing,<br />
cramp like, or colicky. It is frequently associated with<br />
sympathetic and parasympathetic symptoms: nausea, diaphoresis,<br />
and hypotension. Examples include bowel<br />
obstruction and pancreatic cancer. This type of pain is<br />
also usually opioid responsive.<br />
Neuropathic Pain<br />
Injury to neural tissues or dysfunctional changes of the<br />
nervous system from trauma, compression, tumor invasion,<br />
or cancer therapies result in this form of pain. <strong>The</strong><br />
pain may be associated with sensory and motor deficits,<br />
but not always. <strong>The</strong> quality of the pain is often described<br />
as burning, squeezing, lancinating, or electrical. <strong>The</strong>re can<br />
be associated sleep and eating disturbances, and significant<br />
patient emotional suffering. Examples include brachial<br />
and lumbosacral plexopathy, postherpetic neuralgia,<br />
neuromas, complex regional pain syndrome, diabetic neuropathy,<br />
and radiculopathies. Neuropathic pain is associated<br />
with opioid tolerance, termed “apparent opioid<br />
resistance.” That is, patients with neuropathic pain often<br />
require higher than expected doses of opioids to obtain<br />
pain relief and the pain relief is usually not complete.<br />
Neuropathic Pain and Visceral Hypersensitivity<br />
Injury of nerves innervating somatic structures enhances<br />
nociception from stimulation of viscera with convergent<br />
input from nearby dermatomes, suggesting that somatic<br />
neuropathic pain could be accompanied by an increased<br />
likelihood of visceral pain. 14 This raises the possibility<br />
that pain disorders such as fibromyalgia, chronic fatigue<br />
syndrome, chronic pelvic pain, and chronic interstitial<br />
cystitis all represent visceral hypersensitivity pain syndromes<br />
of neuropathic origin.<br />
Medication Management<br />
Little is known of the neurophysiologic relationships<br />
between pain and age-related degenerative brain diseases.<br />
However, Fine 15 has recently reviewed the issues of<br />
pharmacologic management of persistent pain in older<br />
patients. In general, pharmacodynamics (what the drug<br />
does to the patient) are unaffected in the normal aging<br />
process. <strong>The</strong> molecular action of morphine is the same in<br />
all animals, although dose requirements to produce the<br />
same effect may change with age. However, because centrally<br />
acting drugs may interact with a preexisting disease<br />
state, care must be taken when treating pain in patients<br />
with CNS disease such as parkinsonism, Alzheimer<br />
dementia, or stroke.<br />
Pharmacokinetics (what the patient does to the drug)<br />
are frequently affected by aging processes, and disease<br />
states. Pharmacokinetic changes attributable to physical<br />
aging may complicate medication management. (See<br />
Chapter 15, <strong>The</strong> Pharmacology of Opioids.) <strong>The</strong>re is<br />
decreased liver mass and blood flow, which prolongs
21. Pain Management 311<br />
opioid and acetaminophen metabolism. This is of concern,<br />
particularly with fixed combination drugs, such as hydrocodone<br />
or codeine with acetaminophen (Vicodin or<br />
Tylenol #3) and opioids with active metabolites (e.g.,<br />
morphine to morphine-3-glucuronide or meperidine to<br />
normeperidine).<br />
<strong>The</strong>re is decreased renal function which increases the<br />
risk of nonsteroidal antiinflammatory drug (NSAID)<br />
nephrotoxicity and accumulation of metabolites of drugs<br />
such as meperidine. <strong>The</strong>re is decreased plasma binding,<br />
which increases blood levels of active drugs, opioids, and<br />
NSAIDs [even the cyclooxygenase (COX)-2 specifi c<br />
inhibitors, such as Celebrex].<br />
In the elderly, there is increased CNS sensitivity to<br />
opioids leading to enhanced sedation, analgesia, and side<br />
effects including delirium. But the experience of pain<br />
tends to counteract the sedative effects of opioids. <strong>The</strong>refore,<br />
patients who have not received adequate doses of<br />
opioid analgesics and who are still experiencing pain do<br />
not suffer respiratory depression. 16<br />
In acute pain situations or in a “pain crisis,” rapid<br />
titration of opioids in elderly patients is safe. In a study<br />
of 175 elderly patients versus 875 younger patients<br />
who were treated with intravenous (IV) morphine for<br />
postoperative pain in the postanesthesia care unit, there<br />
was no increased incidence of adverse side effects noted<br />
when a strict titration to pain level protocol was followed.<br />
It was not necessary to change the protocol according<br />
to age. 17<br />
<strong>The</strong> use of an opioid is the strategy of choice for rapid<br />
titration to pain relief in most clinical situations. Opioid<br />
side effects are usually manageable if frequent assessments<br />
are made. <strong>The</strong> elderly, of course, may require more<br />
frequent assessments and smaller incremental doses in<br />
order to manage side effects. <strong>The</strong> exact timing of interval<br />
assessments must be dictated by the needs of the individual<br />
case.<br />
<strong>The</strong> management of an acute pain crisis involves immediate<br />
control of the pain, maintenance of analgesia, and<br />
long-term management. During the initial titration to<br />
pain relief, there is ample opportunity to evaluate the<br />
patient for the causes of the pain. <strong>The</strong> best way to gain<br />
control is to get the syringe and titrate to effect. <strong>The</strong> dose<br />
depends on the history of current use or whether the<br />
patient is opioid naïve. <strong>The</strong> choice of drug, e.g., 1–4 mg of<br />
morphine, 0.2–1 mg of hydromorphone (Dilaudid), 10–<br />
50 mg of meperidine (Demerol), or the equianalgesic IV<br />
dose based on the patient’s P.O. breakthrough medication,<br />
is not as important.<br />
Opioids reach maximum plasma levels in 10–15 minutes<br />
after IV bolus (excluding fentanyl and its congeners), so<br />
bolus doses every 10–15 minutes until the patient is comfortable,<br />
begins to become sedated, or has decreasing<br />
respiratory rate is the most effective method of opioid<br />
analgesic loading. An alternative method involves starting<br />
low, then doubling the dose every 30 minutes, until<br />
comfort is obtained, e.g., morphine 2, 4, 8, 16 mg, etc., with<br />
the effect being obtained in less than 90 minutes (range<br />
4–215 minutes). 18 This second method may be more<br />
appropriate for the “younger elderly” as opposed to the<br />
“old elderly.”<br />
After loading the patient and obtaining comfort, maintenance<br />
dosing must be ordered. Intramuscular or IV<br />
bolus dosing by the nursing staff on a PRN basis is a poor<br />
choice. <strong>The</strong> dose required to make the patient com -<br />
fortable can be used as an estimate of the 3-hour dose<br />
requirement for maintenance, e.g., when converting to IV<br />
patient-controlled analgesia (PCA).<br />
Contraindications for IV PCA include patients<br />
who are unable to operate the device because of impaired<br />
mental status or physical limitations, and patients who<br />
are unwilling to use the technique, i.e., some patients do<br />
not want to push the button and want to be given<br />
their medication by the nurse. Patients with sleep apnea<br />
disorders pose a relative contraindication. Failure to<br />
achieve adequate analgesia without side effects after an<br />
appropriate trial is also a contraindication. If the patient<br />
chooses to have the nurse administer analgesia, it would<br />
still be advantageous to have a PCA set up, which would<br />
eliminate intramuscular injections that hurt and produce<br />
tissue injury in the elderly. Also, the medications can<br />
be titrated in small doses by the nurse to adequate<br />
analgesia.<br />
Postsurgical Analgesia<br />
Elderly patients undergo a high number of surgical interventions.<br />
<strong>The</strong> importance of adequate postoperative<br />
analgesia for reducing morbidity and mortality in the<br />
elderly is undisputed. 19 Epidural analgesia and IV PCA<br />
are both excellent postoperative techniques. Physicians<br />
are often reluctant to use PCA in older patients. 20,21 PCA<br />
was found to be effective in this population with the<br />
caveat that the patient is physically or mentally able to<br />
operate the machine. 22 <strong>Regional</strong> anesthetic techniques<br />
are excellent for the elderly. Although a fair amount of<br />
research has been published, data proving long-term<br />
benefit are lacking. 19<br />
In a study of elderly patients after abdominal surgery,<br />
IV PCA versus patient-controlled epidural analgesia<br />
(PCEA), the IV PCA group had general anesthesia with<br />
sufentanil, isoflurane, nitrous oxide, and atracurium for<br />
muscle relaxation. Postoperative loading was 5 mg of<br />
morphine followed by a morphine PCA of 1.5 mg, lockout<br />
8 minutes. <strong>The</strong> epidural group had a T7–T11 catheter<br />
placed, depending on surgery level, which was activated<br />
with 2% lidocaine with epinephrine 5 µg/mL, dosed to T4<br />
sensory level before induction of general anesthesia.<br />
A solution of 0.25% bupivacaine plus 1 µg/mL Sufenta
312 J.M. Berger<br />
was infused continuously throughout the surgery<br />
and continued postoperatively with a solution of<br />
0.125% bupivacaine plus 0.5 µg/mL Sufenta at 3–5 mL/h<br />
with a 2- to 3-mL PCEA bolus and a lockout of 12<br />
minutes. 23<br />
<strong>The</strong> authors concluded that PCEA with local anesthetic<br />
and opioid provided better pain control, improved<br />
mental status, and better bowel function return than did<br />
traditional IV PCA morphine after general anesthesia.<br />
Orthostatic and mobility deficits were not a problem with<br />
the PCEA adjustments.<br />
Carli et al., 24 in their study of 64 patients for elective<br />
colon surgery randomized to an IV PCA group or epidural<br />
group, found that epidural analgesia enhanced functional<br />
exercise capacity and health-related quality of life<br />
indicators after colonic surgery. In their study, the PCA<br />
group had anesthetics consisting of 250 µg of fentanyl,<br />
adjusted isoflurane, nitrous oxide, oxygen, and PCA morphine<br />
with no basal rate but a dose of 1–2 mg every 5<br />
minutes. It was discontinued on day 3–4 if the verbal<br />
analog score was
21. Pain Management 313<br />
management a priority to allow earlier discharge.<br />
However, if this is to be accomplished successfully, physicians<br />
must have knowledge of equianalgesic equivalents.<br />
Equivalency charts can be found in many different texts.<br />
An excellent revised chart can be obtained from the<br />
Southern California Cancer Pain Initiative (sccpi@coh.<br />
org), and found in a relevant article by Gammaitoni<br />
and associates. 28 In the author’s experience, some simple<br />
conversions for chronic administration include the<br />
following:<br />
• IV morphine 10 mg = 30 mg orally.<br />
• IV morphine 1 mg = hydromorphone 0.2 mg.<br />
• Oral morphine 30 mg = hydromorphone 6 mg orally.<br />
• Oral morphine 30 mg = oxycodone 15–20 mg orally.<br />
• IV morphine 60 mg/day = morphine orally 180 mg/day<br />
= fentanyl transdermal patch of 100 µg/h.<br />
• IV morphine 10 mg = hydrocodone 30 mg orally.<br />
An example of a common mistake is the patient<br />
who is obtaining excellent pain relief from an IV PCA<br />
of 10 mg of morphine every 3 hours. <strong>The</strong> time for discharge<br />
arrives, and the PCA is discontinued; the substitution<br />
is hydrocodone/acetaminophen (Vicodin) 5 mg/<br />
500 mg tablets. <strong>The</strong> equivalency for analgesic effect for<br />
10 mg of morphine IV is 30 mg of hydrocodone orally. Ten<br />
milligrams of morphine IV every 3 hours would be eight<br />
doses per day of 30 mg of hydrocodone or 48 tablets of<br />
hydrocodone/acetaminophen per day. Of course, this<br />
would be a lethal dose of acetaminophen. It is unlikely<br />
that any patient would actually take 48 tablets per day,<br />
but the normal prescription of 1 to 2 tablets every 6 hours<br />
PRN for pain might certainly be inadequate for someone<br />
requiring 10 mg of morphine IV every 3 hours.<br />
It therefore behooves the physician managing the<br />
patient to convert the patient to an acceptable oral medication<br />
several days before discharge to ensure adequate<br />
pain control and lack of side effects. In converting from<br />
IV morphine to transdermal fentanyl, this author has<br />
found that 60 mg per day of IV morphine would require<br />
a 100 µg/h transdermal fentanyl patch, which would be<br />
changed every 72 hours. Because hydromorphone is<br />
approximately 5 times more potent than morphine, 60 mg<br />
per day of IV morphine would convert to 12 mg per 24<br />
hours of hydromorphone and again equate to a transdermal<br />
fentanyl patch of 100 µg/h dose.<br />
CYP 2D6 Enzyme and the Efficacy of<br />
Codeine and Codeine-Like Drugs<br />
Codeine, dihydrocodeine (Synalgos DC), and hydrocodone<br />
(Vicodin, Lortab, etc.) are not active opioids. <strong>The</strong>se<br />
opiates must be converted to morphine by the enzyme<br />
Table 21-1. Medications that inhibit the enzyme CYP 2D6.<br />
Amiodarone (Cordarone)<br />
Fluoxetine (Prozac)<br />
Haloperidol (Haldol)<br />
Paroxetine (Paxil)<br />
Propafenone (Rythmol)<br />
Propoxyphene (Darvon)<br />
Quinidine<br />
Ritonavir (Norvir)<br />
Terbinafine (Lamisil)<br />
Thioridazine (Mellaril)<br />
Source: Data from Supernaw. 29<br />
CYP 2D6 to become effective. 29,30 Approximately 20% of<br />
the population is genetically deficient in this enzyme and<br />
so would report a poor analgesic response when prescribed<br />
these medications. Furthermore, many medications<br />
also inhibit the action of CYP 2D6 that are<br />
frequently used by elderly patients; some of these are<br />
shown in Table 21-1.<br />
Oxycodone is metabolized by CYP 2D6; therefore,<br />
patients who are deficient in this enzyme will have a<br />
greater effect from oxycodone medications.<br />
Opioids for Neuropathic Pain and<br />
Broad-Spectrum Opioids<br />
Many elderly patients suffer from neuropathic pain which<br />
is poorly responsive to opioid analgesics that act primarily<br />
at the µ opioid receptor (Table 21-2). 31 While affinity<br />
for µ, δ, and κ receptors of opiates are steric dependent,<br />
the affinity of “l” and “d” forms are nearly equal with<br />
respect to nonopiate receptor actions such as N-methyl-<br />
D-aspartate (NMDA) antagonist and blockage of reuptake<br />
of serotonin and noradrenaline. Multiple actions of<br />
the broad-spectrum opiates seem to be synergistic with<br />
respect to analgesic action, similar to using narrowspectrum<br />
opiates in combination with an NMDA receptor<br />
antagonist and a tricyclic antidepressant. As listed<br />
in Table 21-3, the opioids that have dual actions both<br />
for opioid receptors and for NMDA receptors will be<br />
more effective for neuropathic pain than the narrowspectrum<br />
opioids. <strong>The</strong> opioids in the gray-screened area<br />
Table 21-2. Narrow-spectrum opioids acting only at opioid<br />
receptors.<br />
Morphine<br />
Hydromorphone<br />
Codeine<br />
Fentanyl<br />
Sufentanil<br />
Oxycodone<br />
Buprenorphine
314 J.M. Berger<br />
Table 21-3. Other actions of broad-spectrum opioids not at the<br />
opioid receptors.<br />
Broad-spectrum opioids acting also<br />
as antagonists to N-methyl-Daspartate<br />
receptors<br />
Methadone<br />
Ketobemidone<br />
Dextropropoxyphene<br />
Dextromethorphan<br />
Meperidine (pethidine)<br />
are common to the effects of NMDA receptor antagonism<br />
and inhibition of reuptake of serotonin and<br />
norepinephrine.<br />
Because dextropropoxyphene and meperidine both<br />
have metabolites that act in the brain of elderly patients<br />
and lead to confusion and even seizures, the only<br />
true broad-spectrum opioid analgesic available is<br />
methadone.<br />
End-of-Life Care<br />
Broad-spectrum opioids<br />
acting also as inhibitors of<br />
reuptake of serotonin and<br />
norepinephrine (similar to the<br />
tricyclic antidepressants)<br />
Methadone<br />
Levorphanol<br />
Dextromethorphan<br />
Dextropropoxyphene<br />
Tramadol<br />
Meperidine (pethidine)<br />
For 67% of patients, the last place of care was an institution,<br />
with 38.4% dying in a hospital and 30.5% in a nursing<br />
home. Only 33% died at home; 49.3% of these were on<br />
home hospice care; 38.2% received no formal services;<br />
and 12.5% had home health care nursing services without<br />
hospice participation. 32<br />
Reporting on the degree of satisfaction of bereaved<br />
family members with the care their loved ones received,<br />
hospice care at home received the highest level of overall<br />
satisfaction with 71% of respondents. Twenty-five percent<br />
of all patients with pain or dyspnea did not receive “any”<br />
or “enough” treatment. Inadequate pain management<br />
was 1.6 times more likely in a nursing home setting or<br />
with home health services and 1.2 times more likely in a<br />
hospital than with home hospice. 33<br />
End-of-life pain management for patients who are<br />
being managed at home presents problems of assessment<br />
and administration of medication. Patients who are still<br />
able to swallow can be managed with oral medications.<br />
Rectal suppositories, transdermal medications, and transmucosal<br />
medications are available.<br />
Kadian and Avinza are every-24-hour, single-dose<br />
sustained-release morphine preparations. Although their<br />
uptake properties differ, they both have the property<br />
of being packaged in a capsule that can be sprinkled<br />
as pellets onto applesauce or added to slurry for administration<br />
down an NG- or G-tube, while retaining the<br />
sustained-release characteristic. MS Contin is an every-<br />
12-hour sustained-release morphine preparation that<br />
cannot be broken open. Doing so destroys the integrity<br />
of the sustained-release capsule; the patient receives the<br />
entire dose as an immediate-release preparation. Oxy-<br />
Contin is a 12-hour sustained-release preparation of oxycodone<br />
that also cannot be opened or it too becomes an<br />
immediate-release preparation. <strong>The</strong>re is currently no<br />
sustained-release preparation of hydromorphone or<br />
methadone. Fentanyl and buprenorphine are the only<br />
commercially available transdermal opioids.<br />
It is important to remember that sustained-release<br />
medications are encouraged for patients who have continuous<br />
pain. But it must be remembered that activity will<br />
often increase the level of pain; patients must be prescribed<br />
rapid-onset, short-acting medications to be used<br />
for such breakthrough pain. Because patients vary tremendously<br />
in their requirements for pain medication,<br />
particularly in the senior population in which the margin<br />
for error is smaller, it is important to titrate patients<br />
with immediate-release medication to determine how to<br />
convert to sustained-release medication. Although sustained-release<br />
morphine is available in capsules that are<br />
recommended for every-12-hour dosing and every-24-<br />
hour dosing, the absorption characteristics will determine<br />
whether a particular patient experiences adverse effects<br />
such as nausea or sedation, or end of dose failure. It is<br />
sometimes necessary to lower the dose and change to<br />
every-8-hour or every-12-hour dosing.<br />
Rarely in acute pain situations and more often in endof-life<br />
care, patients’ pain cannot be brought under<br />
control with opioid infusions alone. In such situations,<br />
optimum pain control with minimal side effects could be<br />
obtained with a combination solution of 1 mg/mL morphine<br />
and 1 mg/mL ketamine, with a lockout period of 8<br />
minutes with an IV PCA. 34 <strong>The</strong>se agents can both be<br />
given orally as well in the same ratio, e.g., 30 mg of immediate<br />
release morphine sulfate with 30 mg of ketamine<br />
every 3–4 hours.<br />
Sedation of Terminally Ill<br />
When patients are terminally ill and traditional analgesic<br />
regimens are unsuccessful at providing adequate analgesia<br />
and relief from suffering, the following solution can<br />
provide benefit 35 :<br />
Ketamine (dissociative anesthetic, NMDA blocker)<br />
2 mg/mL<br />
Midazolam (benzodiazepine, reduces incidence of hallucinations,<br />
sedative effects, antianxiety) 0.1 mg/mL<br />
Fentanyl (potent opioid, less nausea, less pruritus, less<br />
constipation, enhanced effect combined with ketamine/<br />
midazolam) 5 µg/mL<br />
IV infusion should begin at 3–5 mL/h titrating to effect.<br />
Doubling the concentrations will allow reduction of the<br />
volume infused if needed. High concentrations can be
21. Pain Management 315<br />
used as subcutaneous infusion as long as the volume<br />
infused per hour remains less than 2 mL.<br />
Nonsteroidal Antiinflammatory<br />
Analgesics<br />
<strong>The</strong> antiprostaglandin effect of NSAIDs can be beneficial<br />
during the acute phase of soft tissue injury. This biochemical<br />
effect may control the inflammatory response to injury<br />
and provide pain relief. <strong>The</strong> duration of an NSAID’s analgesic<br />
effect may be different from its antiinflammatory<br />
effect. <strong>The</strong> antiinflammatory effect may last longer than<br />
the analgesic effect.<br />
Chronic inflammatory disease pain such as arthritis<br />
may warrant chronic NSAID therapy. But some authors<br />
have expressed concern that NSAIDs may actually interfere<br />
with the later stages of tissue repair and remodeling,<br />
where prostaglandins still help mediate debris cleanup.<br />
(This does not seem to be true for the COX-2 specific<br />
inhibitors.) <strong>The</strong>refore, dosage, timing, and potential side<br />
effects of NSAIDs should be evaluated. It is not possible<br />
to predict patient response to a particular NSAID by<br />
chemical class or pharmacokinetics. 36<br />
Remember that COX-2 specific inhibitors do not affect<br />
platelet aggregation and therefore may pose a risk for<br />
myocardial infarction if a patient is taken off aspirin<br />
therapy. For the same reason, it is safe to continue COX-2<br />
specific inhibitors with daily low-dose aspirin. COX-2<br />
inhibitors also have a safer profile from the standpoint of<br />
gastrointestinal irritation, but care should still be taken<br />
in patients with borderline renal function. Baseline renal<br />
function tests should probably be obtained for elderly<br />
patients who are beginning a course of chronic coxib<br />
therapy or NSAID therapy. Drug holidays of 30–60 days<br />
every 4–6 months may also be advisable.<br />
Tricyclic Antidepressants and Specific<br />
Serotonin Reuptake Inhibitors<br />
Tricyclic antidepressants are often used as adjuvants in<br />
treating neuropathic pain because of their inhibition of<br />
reuptake of serotonin and norepinephrine. <strong>The</strong>re is fear<br />
that antidepressants will cause cardiac arrhythmias.<br />
Tricyclic antidepressants are safe for cardiac patients,<br />
except for several months after a myocardial infarction<br />
or if a conduction defect or persistent dangerous arrhythmia<br />
is already present. 37<br />
Specific serotonin reuptake inhibitors (SSRIs) have<br />
safer cardiac profiles than tricyclic antidepressants. SSRIs<br />
are effective for depression. SSRIs do not have analgesic<br />
effects like the tricyclics because they are only serotonin<br />
reuptake inhibitors and not norepinephrine reuptake<br />
inhibitors. Both are necessary to modulate neuropathic<br />
pain. Tricyclics are more effective for pain and for<br />
sleep but may also cause sedation, cognitive changes,<br />
and dizziness. Elderly patients taking tricyclic antidepressants<br />
are at risk for falling, resulting in hip or other fractures.<br />
Again, titration and frequent reassessment are the<br />
key to successful treatment. In addition, many newer<br />
classes of antidepressants provide inhibition of reuptake<br />
of norepinephrine and serotonin without the associated<br />
sedation.<br />
Anticonvulsants for Neuropathic Pain<br />
Gabapentin (Neurontin) is probably the most effective<br />
agent with the fewest side effects for the treatment of<br />
neuropathic pain. It is absorbed in the duodenum, not<br />
metabolized by the liver, not protein bound, excreted<br />
unchanged by the kidneys, and has no ceiling dose. It is<br />
nontoxic to the liver and kidney. <strong>The</strong> only significant side<br />
effects are sedation and cognitive impairment. Starting low<br />
and titrating to response again is the recommendation, but<br />
rapid titration upward is possible as tolerated. Oxcarbazepine<br />
(Trileptal), lamotrigine (Lamictal), and Topamax are<br />
also effective substitutes. And now pregabalin (Lyrica) is<br />
also available and FDA approved for use in treating both<br />
postherpetic neuralgic and diabetic neuralgia.<br />
Evaluation by a psychiatrist may yield information<br />
about clinical depression resulting in emotional suffer -<br />
ing perceived as pain versus sadness, frustration, and<br />
isolation in response to inadequately treated pain. This<br />
would be valuable information in making a choice of<br />
treating with an SSRI versus a tricyclic or other agent<br />
with both serotonin and norepinephrine reuptake inhibition<br />
effects.<br />
With any of these medications, tricyclic or other antidepressants,<br />
anticonvulsants, etc., cognitive impairment<br />
caused by the medication must frequently be accepted or<br />
tolerated in the elderly in order to obtain pain relief.<br />
Pain and Insulin Resistance<br />
Acute, severe pain decreases insulin sensitivity. This<br />
would indicate that relief for acute pain is important for<br />
maintenance of normal glucose metabolism. Many elderly<br />
patients are diabetic, emphasizing the need for good<br />
pain relief. 38<br />
<strong>Regional</strong> Analgesia<br />
Upper extremity surgeries are amenable to brachial<br />
plexus anesthesia and analgesia. Brachial plexus nerve<br />
blocks have a prolonged duration of action in the elderly,<br />
approximately 2.5 times longer. This would lead to a
316 J.M. Berger<br />
slower return of pain and therefore easier titration of<br />
postoperative medications. 39 However, elderly patients<br />
are frequently at risk for falls before surgery, so greater<br />
care must be taken in discharge criteria after a regional<br />
anesthetic to make sure they can maintain balance and<br />
that the caregiver with whom they will be discharged<br />
home is capable of protecting them from falls.<br />
Common Pain Syndromes<br />
Chronic lumbar pain as a result of degenerative arthritis<br />
is very common. Osteoarthritis is the most common cause<br />
of nociceptive pain in the elderly. Inflammatory pain does<br />
respond well to analgesics such as antiinflammatory medications<br />
and opioids. Cancer pain, myofascial pain syndromes,<br />
postherpetic neuralgia, diabetic polyneuropathy,<br />
radiculopathy or amyotrophy, trigeminal neuralgia, and<br />
central post-stroke pain (CPSP) syndrome are all common<br />
in the elderly. Furthermore, arthritis of the knee, hip, or<br />
shoulder are all common problems in the senior population,<br />
and surgical replacement is very advanced and<br />
highly successful. Diagnosis is easy and fairly certain to<br />
be correct.<br />
CPSP is a neuropathic pain syndrome characterized<br />
by constant or intermittent pain in a body part occurring<br />
after stroke. It is associated with sensory abnormalities<br />
in the painful body part. <strong>The</strong> incidence of CPSP is<br />
8% within the first year, but pain may appear up to 3<br />
years after the stroke. Sixty-three percent of those who<br />
develop pain had onset within the first month. 40 Two<br />
thirds of those who develop pain experience moderate to<br />
severe pain. This 8% incidence of pain with 5% expressing<br />
moderate to severe pain is similar to other neuropathic<br />
pain syndromes such as phantom limb pain, 41<br />
central pain in spinal cord injury, 42 and pain in diabetic<br />
neuropathy. 43<br />
Back Pain<br />
About two thirds of adults have low back pain at<br />
some time. Of the 65 million people in the United<br />
States with low back pain, approximately 151,000 undergo<br />
fusion of the lumbar spine each year. 44 <strong>The</strong> number of<br />
spinal fusion surgeries is increasing annually, in part,<br />
according to Deyo and associates, because of widening<br />
indications, including the diagnosis of back pain made by<br />
discography. 45,46<br />
Because of the high rate of unsatisfactory results<br />
with open spinal surgery and the more tenuous physical<br />
condition of elderly patients to undergo and tolerate<br />
open spinal surgery, less-invasive techniques for treat -<br />
ing discogenic pain have been developed. One such<br />
procedure is percutaneous diskectomy using coablation<br />
technology. This is a percutaneous technique to reduce<br />
the volume of internally disrupted disk material. 47<br />
Intrathecal drug delivery has also been effective for<br />
control of pain in unremitting low back pain and radicular<br />
pain. 48<br />
For chronic zygapophyseal joint (spinal facet joint)<br />
pain, radiofrequency neurotomy of the medial branch of<br />
the posterior spinal nerve ramus has been found to be<br />
effective in both the cervical and lumbar regions. 49,50<br />
Although low back pain is a fact of life for a substantial<br />
proportion of the population at all ages, the aged have a<br />
greater prevalence and experience greater impact on<br />
their quality of life than the remainder of the population.<br />
At the same time, they are underrepresented in research. 51<br />
Treatment protocols are poorly defined in the elderly.<br />
History and a comprehensive evaluation are necessary<br />
for an appropriate strategy. 52<br />
Thoracic and Lumbar Compression Fractures<br />
Epidural injections can be helpful for acute vertebral<br />
compression fractures, which are common in the elderly.<br />
Continuous epidural infusion of local anesthetic is also<br />
an option but requires hospitalization. Vertebroplasty<br />
is also an option. This involves a technique designed<br />
to consolidate pathologic vertebral bodies through the<br />
injection of orthopedic cement under fluoroscopic guidance.<br />
53–55 This procedure has been shown to be safe in frail<br />
elderly patients and can improve quality of life. 56<br />
Spinal Stenosis<br />
Neurogenic claudication is frequently a presenting<br />
symptom of lumbar spinal stenosis. <strong>The</strong> patient complains<br />
of pain in the legs with walking which is relieved with<br />
rest. Epidural injections can sometimes be helpful in<br />
early disease. In advanced disease if surgery is not an<br />
option, spinal infusion therapy may be helpful as an<br />
alternative. 57<br />
Herpes Zoster (AHZ, Shingles)<br />
<strong>The</strong> word herpes stems from the Greek herpein which<br />
means “to creep,” whereas zoster means “girdle.” <strong>The</strong><br />
disease infects 800,000 people in the United States each<br />
year, and the incidence increases with advancing age. <strong>The</strong><br />
etiopathogenesis of herpes begins after chicken pox,<br />
when the varicella virus becomes dormant in a spinal<br />
nerve. When reduced cell-mediated immunity occurs,<br />
AHZ reactivates. Reactivation leads to infection down<br />
the nerve to the skin with the eruption of skin lesions.<br />
<strong>The</strong> inflammation can also travel to reach the spinal cord<br />
or the trigeminal brainstem complex. 58<br />
<strong>The</strong> first sign of shingles is intense pain or itching, even<br />
before the lesions erupt on the skin. It is only along one
21. Pain Management 317<br />
nerve on one side of the body. Treatment should start as<br />
soon as possible with antiviral medication, pain medication,<br />
and steroids. Steroids are safe in acute herpes zoster<br />
because it is an immunoglobulin G–mediated immune<br />
response. 58 Epidural injections usually are helpful only in<br />
the first 3 days after eruption. Subcutaneous infiltration<br />
of local anesthetic and long-acting steroid can provide<br />
relief and accelerate healing. Stellate ganglion sympathetic<br />
and superior cervical sympathetic ganglion local<br />
anesthetic blocks can be helpful for zoster of the face in<br />
the trigeminal distribution. Manabe and associates 59<br />
demonstrated that continuous epidural infusion of local<br />
anesthetic can shorten the duration of zoster-associated<br />
pain.<br />
Postherpetic Neuralgia<br />
Usually this disease is defined as pain that extends beyond<br />
the normal healing period of 6 weeks to 2 months.<br />
<strong>The</strong> pain takes on the characteristics of neuropathic pain<br />
with allodynia, and hyperalgesia. <strong>The</strong> frequency of persistent<br />
pain is given in Table 21-4. 60 Aggressive therapy for<br />
acute herpes zoster will not prevent the development of<br />
postherpetic neuralgia. However, it will change the quality<br />
of the pain from the intense unsupportable pain syndrome<br />
to a more diffuse, deep aching pain that can be<br />
supported. 61<br />
Treatment options for postherpetic neuralgia have<br />
not significantly improved over the years. Analgesics,<br />
even traditional opioid analgesics, offer little relief.<br />
Methadone can be helpful if the patient can tolerate it.<br />
It is a difficult medication to titrate in the elderly. Spinal<br />
cord stimulation can be beneficial in about 50% of cases<br />
of postherpetic neuralgia if the virus has not affected<br />
the dorsal horn of the spinal cord. Lidocaine 5% topical<br />
patches have been found to reduce the symptoms of<br />
postherpetic neuralgia about 30%–40%. Kotani et al. 62<br />
did report on the use of intrathecal methylprednisolone<br />
60 mg administered with 3 mL of 3% lidocaine once<br />
per week for up to 4 weeks as being 70% effective in<br />
reducing pain.<br />
Table 21-4. Persistent pain in postherpetic neuralgia as a function<br />
of age.<br />
Age group<br />
Percentage of patients<br />
with pain for 1 year<br />
0–19 4 4<br />
20–29 2 2<br />
30–39 15 10<br />
40–49 33 7<br />
50–59 49 18<br />
60–69 65 37<br />
>70 74 48<br />
Source: Reprinted with permission from de Moragas and Kierland. 60<br />
Case Examples<br />
When assessing pain problems and making clinical decisions<br />
for therapy in the elderly, the situation is not always<br />
what it seems, and care must be taken to not go down the<br />
wrong path. Following are two cases that illustrate this<br />
problem.<br />
Case 21-1. Lumbar Radiculopathy<br />
A 67-year-old male physician presented with a sudden<br />
onset of back and leg pain, with a foot drop. A magnetic<br />
resonance imaging (MRI) scan showed a protruding<br />
disk with nerve root impingement corresponding to<br />
the side of the foot drop. <strong>The</strong> patient chose not go to a<br />
surgeon but instead requested that this author treat him<br />
with epidural steroid injection therapy. He received an<br />
initial lumbar epidural steroid injection followed by two<br />
caudal steroid injections over a 3-week interval. He experienced<br />
rapid resolution of all symptoms, including the<br />
foot drop, and returned to playing golf again with no<br />
return of the foot drop at 3 years after epidural injections.<br />
<strong>The</strong> MRI image is shown in Figure 21-1A (December 10,<br />
2001). Figure 21-1B is a comparison MRI image (January<br />
1, 1995) taken when the patient volunteered to have<br />
a scan done for a new scanner that needed calibration.<br />
<strong>The</strong> disk protrusion was present in 1995 but was asymptomatic<br />
until 2001. It is also clear that faced with the<br />
MRI image of 2001 along with pain and a foot drop,<br />
most neurosurgeons would have considered this a surgical<br />
emergency (Figure 21-2). It is clear that epidural<br />
steroid injections cannot dissolve away a disk protrusion.<br />
In this case, however, the problem was an acute nerve<br />
root irritation in the presence of a longstanding asymptomatic<br />
disk protrusion that did respond to epidural<br />
steroid injections.<br />
Steroid injections are efficacious for different spine<br />
problems. Epidural steroid injections are being performed<br />
under image intensifier needle guidance both by the<br />
translaminar approach as well as the transforaminal<br />
approach to treat radiculitis and radiculopathy of the<br />
cervical as well as the lumbar nerve. 63–65<br />
Case 21-2. Excessive Treatment in<br />
a Missed Diagnosis<br />
An 85-year-old woman who was healthy, ambulatory, and<br />
living independently, upon getting out of bed one morning,<br />
experienced a sudden onset of right hip pain radiating<br />
down her leg. Nothing was done for a week, but she was<br />
not able to bear weight on that leg. After a week, she went<br />
to her primary doctor who immediately ordered an MRI<br />
scan of her lumbar spine. Based on the results of<br />
that scan, she was referred to a pain clinic where she
318 J.M. Berger<br />
A<br />
B<br />
Figure 21-1. A: MRI from December 10, 2001. <strong>The</strong> patient was symptomatic of the disk protrusion at L4–5 (arrow). B: MRI from<br />
January 1, 1995. <strong>The</strong> patient was asymptomatic of the disk protrusion at L4–5 (arrow).<br />
Figure 21-2. Significant disk protrusion noted (arrow).
21. Pain Management 319<br />
A<br />
Figure 21-3. A: A-P X-ray of the lower lumber spine and pelvis<br />
showing extensive discogenic and vertebral body degeneration<br />
with scoliosis to the left, osteophytes and endplate abnormalities<br />
on the left. B: Magnified view of the right acetabulum<br />
showing the small fracture (circled in black). <strong>The</strong> patient never<br />
complained of back pain.<br />
B<br />
underwent a series of three translaminar lumbar epidural<br />
steroid injections and a left-sided L3 and S1 transforaminal<br />
epidural steroid injection without benefit. She continued<br />
to be unable to walk. Surgery was recommended for<br />
her back, but fortunately the patient declined. After 6<br />
months, she was referred to this author. Upon taking the<br />
history and performing an examination, it was clear that<br />
the most likely diagnosis was a fracture of the right hip.<br />
<strong>The</strong> patient never complained of back pain and never<br />
complained of left-sided leg pain. Her pain was always<br />
emanating from her right hip. A plain X-ray was ordered<br />
by this author that revealed a fracture of the pelvis close<br />
to the acetabulum on the right side. It is a wonder in<br />
looking at the X-ray, however, that the patient never did<br />
suffer from back pain (Figure 21-3).<br />
Conclusions<br />
<strong>The</strong> major goal of geriatric care is often comfort and<br />
control of the symptoms of chronic disease. 3 <strong>The</strong> following<br />
guidelines are useful in approaching pain management<br />
in the elderly:<br />
1. Always ask elderly patients about pain.<br />
2. Accept the patient’s word about pain and its<br />
intensity.<br />
3. Never underestimate the potential effects of chronic<br />
pain on a patient’s overall condition and quality of<br />
life.<br />
4. Be compulsive in the assessment of pain. An accurate<br />
diagnosis will lead to the most effective treatment.<br />
5. Treat pain to facilitate diagnostic procedures. Do not<br />
wait for a diagnosis to relieve suffering.<br />
6. Use a combined approach of drug and nondrug strategies<br />
when possible.<br />
7. Mobilize patients physically and psychosocially.<br />
Involve patients in their therapy.<br />
8. Use analgesic drugs correctly. Start doses low and<br />
increase slowly. Achieve adequate doses and anticipate<br />
side effects.<br />
9. Anticipate and attend to anxiety and depression.<br />
10. Reassess responses to treatment. Alter therapy to<br />
maximize functional status and quality of life.<br />
References<br />
1. Cleeland C. Undertreatment of cancer pain in elderly<br />
patients. JAMA 1998;279(23):1914–1915.<br />
2. Ferrell BA, Ferrell BR, Osterweil D. Pain in the nursing<br />
home. J Am Geriatr Soc 1990;38:409–414.<br />
3. Ferrell BA. Pain management in elderly people. J Am<br />
Geriatr Soc 1991;39:64–73.<br />
4. Chevlen E. Optimizing the use of opioids in the elderly<br />
population. Am J Pain Manage Suppl 2004;14(2):19S–24S.<br />
5. Otis J, McGeeney B. Managing pain in the elderly. Clin<br />
Geriatr 2001;9:82–88.<br />
6. Fine P. Difficulties and challenges in the treatment of<br />
chronic pain in the older adult. Am J Pain Manage<br />
2004;14(2):2S–8S.<br />
7. Parmelee PA, Katz IR, Lawton MP. <strong>The</strong> relation of pain to<br />
depression among institutionalized aged. J Gerontol 1991;<br />
46:15–21.<br />
8. Williamson G, Schulz RL. Pain, activity restriction, and<br />
symptoms of depression among community-residing elderly<br />
adults. J Gerontol 1992;47:367–372.<br />
9. Casten R, Parmelee P, Kleban M, et al. <strong>The</strong> relationships<br />
among anxiety, depression, and pain in a geriatric institutionalized<br />
sample. Pain 1995;61:271–276.
320 J.M. Berger<br />
10. Gaston-Johansson F, Johansson F, Johansson C. Pain in the<br />
elderly: prevalence, attitudes and assessment. Nurs Home<br />
Manage 1996;4(11):325–331.<br />
11. Gaston-Johansson F, Johansson F, Johansson N. Undertreatment<br />
of pain in the elderly: causes and prevention. Ann<br />
Long-Term Care 1999;7(5):190–196.<br />
12. Postone N. Alexithymia in chronic pain patients. Gen Hosp<br />
Psychiatry 1986;8:163–167.<br />
13. Gibson S, Ferrell M. A review of age differences in the<br />
neurophysiology of nociception and the perceptual experience<br />
of pain. Clin J Pain 2004;20(4):227–239.<br />
14. Shin S, Eisenach J. Peripheral nerve injury sensitizes the<br />
response to visceral distension but not its inhibition by<br />
the antidepressant Milnacipran. <strong>Anesthesiology</strong> 2004;100(3):<br />
671–675.<br />
15. Fine P. Pharmacological management of persistent pain in<br />
older patients. Clin J Pain 2004;20(4):220–226.<br />
16. Zukerman LA, Ferrante FM. Nonopioid and opioid<br />
analgesics. In: Ashburn MA, Rice LJ, eds. <strong>The</strong> Manage -<br />
ment of Pain. New York: Churchill-Livingstone; 1998:<br />
111–140.<br />
17. Auburn F, Monsel S, Langeron O, et al. Postoperative titration<br />
of intravenous morphine in the elderly patient. <strong>Anesthesiology</strong><br />
2002;96(1):17–23.<br />
18. Hagen NA, Elwood T, Ernst S. Cancer pain emergencies: a<br />
protocol for management. J Pain Symptom Manage 1997;<br />
14(1):45–50.<br />
19. Cook D, Rooke A. Priorities in perioperative geriatrics.<br />
Anesth Analg 2003;96:1823–1836.<br />
20. Dyer C, Ashton C. Postoperative delirium: a review of<br />
80 primary data-collection studies. Arch Intern Med<br />
1995;155(5):461–465.<br />
21. Gustafson Y, Berggren D, Brännström B, et al. Acute confusional<br />
states in elderly patients treated for femoral neck<br />
fracture. J Am Geriatr Soc 1988;36:525–530.<br />
22. Gagliese L, Jackson M, Ritvo P, et al. Age is not an impediment<br />
to effective use of patient controlled analgesia by<br />
surgical patients. <strong>Anesthesiology</strong> 2000;93(3):601–610.<br />
23. Mann C, Pouzeratte Y, Bocarra G, et al. Comparison of<br />
intravenous or epidural patient-controlled analgesia in the<br />
elderly after major abdominal surgery. <strong>Anesthesiology</strong><br />
2000;92(2):433–441.<br />
24. Carli F, Phil M, Mayo N, et al. Epidural analgesia enhances<br />
functional exercise capacity and health related quality of<br />
life after colonic surgery. Results of a randomized trial.<br />
<strong>Anesthesiology</strong> 2002;97(3):540–549.<br />
25. Jacox A, Carr DB, Payne R, et al. Management of cancer<br />
pain. Clinical practice guideline no. 9. AHCPR Publication<br />
No. 94–0592. Rockville, MD: Agency for Health Care Policy<br />
and Research, U.S. Department of Health and Human Services,<br />
Public Health Service; 1994.<br />
26. Weissman DE, Haddox JD. Opioid pseudoaddiction—an<br />
iatrogenic syndrome. Pain 1989;36:363–366.<br />
27. Lasagna L, Beecher H. Optimal dose of morphine. J Am<br />
Med Assoc 1954;156(3):230–234.<br />
28. Gammaitoni A, Fine P, Alvarez N, et al. Clinical application<br />
of opioid equianalgesic data. Clin J Pain 2003;19(5):286–<br />
297.<br />
29. Supernaw J. CYP2D6 and the efficacy of codeine-like drugs.<br />
Am J Pain Manage 2001;11(1):30–31.<br />
30. Fishbain DA, Fishbain D, Lewis J, et al. Genetic testing for<br />
enzymes of drug metabolism: does it have clinical utility for<br />
pain medicine at the present time? A structured Review.<br />
Pain Med 2004;5(1):81–93.<br />
31. Morley J. New perspectives in our use of opioids. Pain<br />
Forum 1999;8(4):200–205.<br />
32. Quality of Life Matters Bulletin 2004;6(1). Published by<br />
Quality of Life Publishing Co. Tel: 1–877–513–0099.<br />
33. Teno J, Clarridge B, Casey V, et al. Family perspectives<br />
on end-of-life care at the last place of care. JAMA 2004;<br />
291(1):88–93.<br />
34. Sveticic G, Gentilini A, Eichenberger U, et al. Combinations<br />
of morphine with ketamine for patient-controlled analgesia.<br />
A new optimization method. <strong>Anesthesiology</strong> 2003;98(5):<br />
1195–1205.<br />
35. Berger JM, Ryan A, Vadivelu N, et al. Use of ketaminefentanyl-midazolam<br />
infusion for the control of symptoms<br />
in terminal life care. Am J Hosp Palliat Care 2000;17(2):<br />
127–136.<br />
36. Kellett J. Acute soft tissue injuries—a review of the literature.<br />
Med Sci Sports Exerc 1986;18:489–500.<br />
37. Vieth R, Raskind M, Caldwell J, et al. Cardiovascular effects<br />
of tricyclic antidepressants in depressed patients with<br />
chronic heart disease. N Engl J Med 1982;306:954–959.<br />
38. Greisen J, Juhl C, Grofte T, et al. Acute pain induces insulin<br />
resistance in humans. <strong>Anesthesiology</strong> 2001;95(3):578–584.<br />
39. Paqueron X, Boccara G, Bendahou M, et al. Brachial plexus<br />
nerve block exhibits prolonged duration in the elderly.<br />
<strong>Anesthesiology</strong> 2002;97(5):1245–1249.<br />
40. Andersen G, Vestergaard K, Ingeman-Nielsen M, et al. Incidence<br />
of central post-stroke pain. Pain 1995;61:187–193.<br />
41. Jensen TS, Rasmussen P. Phantom pain. In: Wall PD, Melzack<br />
R, eds. Textbook of Pain. Edinburgh: Churchill-Livingstone;<br />
1994:651–665.<br />
42. Beri’c A, Dimitrijevi’c MA, Lindblom U. Central dysesthesia<br />
syndrome in spinal cord injury patients. Pain 1988;34:<br />
109–116.<br />
43. Melton LJ, Dyck PJ. Epidemiology. In: Dyck PJ, Thomas PK,<br />
Asbury AK, et al., eds. Diabetic Neuropathy. Philadelphia:<br />
Saunders; 1987:27–35.<br />
44. Lipson S. Spinal-fusion surgery—advances and concerns. N<br />
Engl J Med 2004;350(7):643–644.<br />
45. Deyo RA, Nachemson A, Mirza SK. Spinal-fusion surgery—<br />
the case for restraint. N Engl J Med 2004;350(7):722–726.<br />
46. Cohen SP, Larkin TM, Barna SA, et al. Lumbar discography: a<br />
comprehensive review of outcomes studies, diagnostic accuracy,<br />
and principles. Reg Anesth Pain Med 2005;30(2):163–183.<br />
47. Singh V, Piryani C, Liao K. Role of percutaneous disc<br />
decompression using coblation in managing chronic discogenic<br />
low back pain: a prospective, observational study.<br />
Pain Phys 2004;7:419–425.<br />
48. Deer T, Chapple I, Classen A, et al. Intrathecal drug delivery<br />
for treatment of chronic low back pain: report from the<br />
national outcomes registry for low back pain. Pain Med<br />
2004;5(1):6–13.<br />
49. Faclier G, Kay J. Cervical facet radiofrequency neurotomy.<br />
Tech Reg Anesth Pain Manage 2000;4(3):120–125.<br />
50. Dreyfuss P, Halbrook B, Pauza K, et al. Efficacy and validity<br />
of radiofrequency neurotomy for chronic lumbar zygapophysial<br />
joint pain. Spine 2000;25:1270–1277.
21. Pain Management 321<br />
51. Manchikanti L. Chronic low back pain in the elderly: Part<br />
I. Am J Pain Manage 1997;7(3):104–117.<br />
52. Manchikanti L. Chronic low back pain in the elderly: Part<br />
II. Am J Pain Manage 1997;7(4):133–145.<br />
53. Mathis JM, Barr JD, Belkoff SM, et al. Percutaneous<br />
vertebroplasty: a developing standard of care for vertebral<br />
compression fractures. AJNR Am J Neuroradiol 2001;22:<br />
373–381.<br />
54. Sesay M, Dousset V, Liguoro D, et al. Intraosseous lidocaine<br />
provides effective analgesia for percutaneous vertebroplasty<br />
of osteoporotic fractures. Can J Anesth 2002;49:137–143.<br />
55. Jensen ME, Evans AJ, Mathis JM, et al. Percutaneous<br />
polymethylmethacrylate vertebroplasty in the treatment of<br />
osteoporotic vertebral body compression fractures: technical<br />
aspects. Am J Neuroradiol 1997;18:1897–1904.<br />
56. McKiernan F, Faciszewski T, Jensen R. Quality of life<br />
following vertebroplasty. J Bone Joint Surg 2004;86(12):<br />
2600–2606.<br />
57. Dougherty P, Staats P. Intrathecal drug therapy for chronic<br />
pain: from basic science to clinical practice. <strong>Anesthesiology</strong><br />
1999;91(6):1891–2003.<br />
58. Toliver KT, Berger JM, Pardo ES. Review of herpes zoster.<br />
Semin Anesth 1997;16(2):127–131.<br />
59. Manabe H, Dan K, Hirata K, et al. Optimum pain relief with<br />
continuous epidural infusion of local anesthetic shortens<br />
the duration of zoster-associated pain. Clin J Pain 2004;<br />
20(5):302–308.<br />
60. de Moragas JM, Kierland RR. <strong>The</strong> outcome of patients with<br />
herpes zoster. AMA Arch Derm 1957;75:193–196.<br />
61. Pardo ES, Berger JM, Toliver KT. Post herpetic neuralgia.<br />
Semin Anesth 1997;16(2):132–135.<br />
62. Kotani N, Kushikata T, Hashimoto H, et al. Intrathecal<br />
methylprednisolone for intractable postherpetic neuralgia.<br />
N Engl J Med 2000;343(21):1514–1519.<br />
63. Abram S. Treatment of lumbosacral radiculopathy with<br />
epidural steroids: clinical concepts and commentary.<br />
<strong>Anesthesiology</strong> 1999;91(6):1937–1941.<br />
64. Rowlingson J. Epidural steroids in treating failed back<br />
surgery syndrome. Anesth Analg 1999;88:240–242.<br />
65. Fredman B, Nun M, Zohar E, et al. Epidural steroids for<br />
treating “failed-back surgery syndrome.” Is fluoroscopy<br />
really necessary? Anesth Analg 1999;88:367–372.
22<br />
<strong>Anesthesia</strong> Considerations for<br />
<strong>Geriatric</strong> Outpatients<br />
Kathryn E. McGoldrick<br />
During the past two decades, ambulatory anesthesia has<br />
matured and expanded. With ambulatory surgery currently<br />
accounting for almost 80% of all surgical procedures<br />
performed in the United States, it has become<br />
undisputedly the dominant mode of surgical practice in<br />
North America, as well as in many of the world’s other<br />
developed nations. Several factors have contributed to<br />
the phenomenal growth of outpatient surgery, including<br />
economic pressures; technologic advances that allow<br />
minimally invasive surgery; and new, short-acting drugs<br />
and anesthetic agents that have dramatically improved<br />
our ability to prevent and treat postoperative nausea and<br />
vomiting (PONV) 1 and to manage postoperative pain.<br />
Nonetheless, ambulatory anesthesiologists cannot afford<br />
the luxury of resting on our laurels. To paraphrase the<br />
gifted poet, Robert Frost, we still have miles to go before<br />
we sleep. . . .<br />
<strong>The</strong> elderly (≥65 years old) population is the fastest<br />
growing demographic segment in the United States as<br />
well as in many parts of the developed world. According<br />
to the 2000 census, there are 4.2 million Americans age<br />
85 years or older, an increase of 30% since 1990. Those<br />
75–84 years of age number 12.4 million, an increase of<br />
>20% since 1990. <strong>The</strong>se realities have profound implications<br />
for clinicians, including anesthesiologists and surgeons.<br />
Aging, for example, increases the probability that<br />
an individual will require surgery. Whereas approximately<br />
12% of those aged 45–60 years undergo surgery annually,<br />
this number increases to >21% in those aged ≥65 years. 2<br />
Unfortunately, however, morbidity and mortality are<br />
increased in the geriatric population, with steep increases<br />
observed after age 75 years. Thus, an aging population has<br />
multifaceted implications for the practice of anesthesiology<br />
that are evident in the preoperative, intraoperative,<br />
and postoperative periods.<br />
In 2000, Dr. Lee A. Fleisher, as the recipient of the first<br />
Society for Ambulatory <strong>Anesthesia</strong> (SAMBA) Outcomes<br />
Research Award, began an investigation of the impact of<br />
location of care and patient factors on the rate of complications<br />
and readmission after outpatient surgery. 3 Not<br />
surprisingly, the study determined that age in excess of<br />
85 years, prior inpatient hospital admission within 6<br />
months, invasive surgery, and surgical venue were predictive<br />
of unanticipated admission and other adverse outcomes,<br />
including death. <strong>The</strong>se findings are suggestive<br />
that not all ambulatory facilities—i.e., hospitals, freestanding<br />
surgicenters, or office-based operating rooms—<br />
are created equal in terms of their ability to successfully<br />
manage complicated patients having lengthy, relatively<br />
invasive procedures. Clearly, this important work by Dr.<br />
Fleisher highlights two major challenges confronting<br />
anesthesiologists today: the exigencies and nuances of<br />
gerontologic anesthesia and the safety of office-based<br />
surgery.<br />
In this context, it is important to appreciate that 15%<br />
of all elective surgeries performed in the United States<br />
in 2002 were conducted in offices. Indeed, office-based<br />
anesthesia is currently the fastest growing segment of<br />
anesthesia practice in our country. However, startling<br />
death rates associated with office-based anesthesia and<br />
surgery have been reported. <strong>The</strong> death rate for officebased<br />
surgery in Florida a few years ago was estimated<br />
at 1 : 8500, and it has been disclosed that the mortality for<br />
liposuction may be as high as 1:5000 procedures. 4 Vila and<br />
colleagues 5 reviewed all adverse incidents reported to the<br />
Florida Board of Medicine from April 2000 until April<br />
2002. Despite the implementation of corrective-action<br />
measures by the Board of Medicine for office-based<br />
surgery in 2000, the investigators found a more than<br />
tenfold increase in rates of adverse incidents (66 : 100,000<br />
versus 5.3 : 100,000) and death (9.2 : 100,000 versus<br />
0.78 : 100,000) when comparing offices and ambulatory<br />
surgery centers, respectively. <strong>The</strong>re are multiple reasons<br />
for these alarming findings, and most of them pertain to<br />
the lack of regulatory control that is characteristic of<br />
private offices, where it is not uncommon to have clerical<br />
staff administer sedative-hypnotics and opioids under the<br />
“guidance” of the operating physician (who often may be<br />
322
22. <strong>Anesthesia</strong> Considerations for <strong>Geriatric</strong> Outpatients 323<br />
a dermatologist rather than a surgeon). Indeed, only a<br />
small minority of states have regulations pertaining to<br />
office-based surgery. <strong>The</strong>refore, SAMBA and the American<br />
Society of Anesthesiologists (ASA) have joined<br />
together to ensure the same level of safety in offices as<br />
in hospitals or accredited surgicenters. To accomplish this<br />
goal, patients and procedures must be appropriately<br />
matched to venue, and anesthesia care must be delivered<br />
only by those with expertise in the specialty. Frail, complex<br />
elderly patients are inappropriate candidates for lengthy,<br />
relatively invasive surgical procedures performed in<br />
private offices.<br />
Preoperative Evaluation<br />
<strong>The</strong> preoperative evaluation of the geriatric patient characteristically<br />
is more complex than that of the younger<br />
patient because of the heterogeneity of seniors and the<br />
increased frequency and severity of comorbid conditions<br />
associated with aging. <strong>The</strong> process of aging is highly individualized.<br />
Different people age at varying rates and<br />
often in different ways. Typically, however, virtually all<br />
physiologic systems decline with advancing chronologic<br />
age. Nevertheless, chronologic age is a poor surrogate for<br />
capturing information about fitness or frailty. 6 Moreover,<br />
perioperative functional status can be difficult to quantitate<br />
because many elderly patients have reduced preoperative<br />
function related to deconditioning, age-associated<br />
disease, or cognitive impairment. Thus, it is challenging to<br />
satisfactorily evaluate the patient’s capacity to respond<br />
to the specific stresses associated with anesthesia and<br />
surgery. How, for example, does one determine cardiopulmonary<br />
reserve in a patient severely limited by osteoarthritis<br />
and dementia? Even “normal” aging results in<br />
alterations in cardiac, respiratory, neurologic, and renal<br />
physiology that are linked to reduced functional reserve<br />
and ability to compensate for physiologic stress. Moreover,<br />
the consumption of multiple medications so typical<br />
of the elderly can alter homeostatic mechanisms.<br />
Preoperative Testing<br />
In the general population, there is strong consensus that<br />
most routine tests are not indicated. In the subset of<br />
geriatric patients, our knowledge is somewhat more<br />
limited. Nonetheless, a recent study on routine preoperative<br />
testing in more than 18,000 patients undergoing<br />
cataract surgery is worthy of comment. Patients were<br />
randomly assigned to undergo or not undergo routine<br />
testing (electrocardiogram, complete blood cell count,<br />
electrolytes, blood urea nitrogen, creatinine, and<br />
glucose). 7 <strong>The</strong> analysis was stratified by age and disclosed<br />
no benefit to routine testing for any group of patients.<br />
Similar conclusions were drawn in a smaller study of<br />
elderly noncardiac surgical patients by Dzankic and colleagues.<br />
8 Some physicians and lay people, however, misinterpreted<br />
the results of the study by Schein et al., 7<br />
believing that patients having cataract surgery need no<br />
preoperative evaluation. It is vital to note that all patients<br />
in this trial received regular medical care and were evaluated<br />
by a physician preoperatively. Patients whose<br />
medical status indicated a need for preoperative laboratory<br />
tests were excluded from the study. Because “routine”<br />
testing for the more than 1.5 million cataract patients in<br />
the United States is estimated to cost $150 million annually,<br />
the favorable economic impact of this “targeted”<br />
approach is obvious.<br />
From these investigations and others, a few concepts<br />
emerge. First, routine screening in a general population<br />
of elderly patients does not significantly augment information<br />
obtained from the patient’s history. Second, the<br />
positive predictive value of abnormal findings on routine<br />
screening is limited. Third, positive results on screening<br />
tests have modest impact on patient care.<br />
<strong>The</strong> dearth of population studies of perioperative risk<br />
and outcomes specifically addressing the geriatric population<br />
can make selecting the most appropriate course of<br />
care challenging. Because age itself adds very modest<br />
incremental risk in the absence of comorbid disease,<br />
most risk-factor identification and risk-predictive indices<br />
have focused on specific diseases. 9–11 It is well known,<br />
for example, that normal aging produces structural<br />
changes in the cardiovascular system, as well as changes<br />
in autonomic responsiveness/control, that can compromise<br />
hemodynamic stability. <strong>The</strong> superimposition of such<br />
comorbid conditions as angina pectoris or valvular heart<br />
disease can further impair cardiovascular performance,<br />
especially in the perioperative period.<br />
According to the guidelines of the American College<br />
of Cardiology and the American Heart Association for<br />
preoperative cardiac evaluation, the patient’s activity<br />
level, expressed in metabolic units, is a primary determinant<br />
of the necessity for further evaluation, along with<br />
the results obtained from history and physical examination.<br />
9 <strong>The</strong>se findings are then evaluated in conjunction<br />
with due consideration for the invasiveness of the<br />
planned surgical procedure. Clearly, the goal of the preoperative<br />
evaluation should be the identification of major<br />
predictors of cardiac risk such as unstable coronary syndromes<br />
[for example, unstable angina or myocardial<br />
infarction (MI) 30 days ago, compensated or prior<br />
congestive heart failure, diabetes mellitus, or renal<br />
insufficiency), the invasiveness of the surgery and the
324 K.E. McGoldrick<br />
functional status of the patient will have major roles in<br />
determining the nature and extent of preoperative testing<br />
or intervention. Importantly, no preoperative cardiovascular<br />
testing should be performed if the results will not<br />
change perioperative management. For those in whom<br />
further testing is warranted, there are several options<br />
including pharmacologic stress testing and dobutamine<br />
stress echocardiography. <strong>The</strong> use of perioperative betablockade<br />
in intermediate- or high-risk patients undergoing<br />
vascular surgery can be beneficial and may obviate<br />
the need for more invasive interventions. 12 However,<br />
there is a dearth of data pertaining to the use of perioperative<br />
betablockade in patients undergoing less-invasive<br />
outpatient surgery.<br />
Given the heterogeneity of the elderly population, it is<br />
reasonable to examine more domains than just cardiopulmonary<br />
capacity. A multidimensional approach seems<br />
indicated and should include screening for mental status,<br />
depression, and alcohol abuse. We have recently come to<br />
appreciate that subtle forms of cognitive impairment can<br />
predispose to worsened cognitive outcome postoperatively.<br />
It is mandatory to appreciate that the elderly<br />
patient is at much greater risk for long-term functional<br />
compromise after the stress of surgery than is the younger<br />
patient. <strong>The</strong>se potential complications include, but are<br />
not limited to, aspiration, postoperative delirium and cognitive<br />
dysfunction, adverse drug interactions, malnutrition,<br />
pressure ulcers, urosepsis, falls, and failure to return<br />
to ambulation or to home. Appropriate preoperative<br />
optimization may well pay dividends in terms of improving<br />
functional status after discharge.<br />
Sleep Apnea<br />
<strong>The</strong> prevalence of sleep disorders among the general<br />
American population is high. Sleep apnea has received<br />
increasing attention during the past few decades in<br />
tandem with the pandemic of obesity in the United States,<br />
as well as the accumulation of research linking obstructive<br />
sleep apnea (OSA) to cognitive, behavioral, cardiovascular,<br />
and cerebrovascular disease. OSA is defined as<br />
the cessation of airflow for >10 seconds during sleep<br />
despite persistent respiratory effort by the abdomen and<br />
rib cage. OSA is usually associated with a decrease in<br />
arterial oxygen saturation of >4%. Although there is no<br />
uniform definition of hypopnea, it is characterized by<br />
decreased airflow for 10 seconds during sleep and is associated<br />
with an oxyhemoglobin desaturation of 3% from<br />
baseline. It should be noted for the sake of completeness<br />
that the three types of sleep apnea are obstructive, central,<br />
and mixed. Central sleep apnea, a much rarer entity than<br />
OSA, is also known as Ondine’s curse, an allusion to the<br />
mythologic man who was condemned by his rejected<br />
lover, a mermaid, to stay awake in order to breathe.<br />
Unlike OSA, respiratory efforts temporarily stop in<br />
central sleep apnea. Diagnosis is established during<br />
polysomnography.<br />
Conservative estimates suggest that 2% of middleaged<br />
women and 4% of middle-aged men are afflicted<br />
with this disorder. 13 Growing evidence points to a much<br />
higher incidence in the elderly. 14,15 Indeed, the prevalence<br />
of OSA is two- to threefold greater in older persons (>65<br />
years) compared with those in middle age. 16 Some data<br />
actually suggest that OSA in elders is a condition distinct<br />
from that of middle age. Bixler and colleagues 17 reported<br />
that OSA is less severe in older compared with middleaged<br />
persons, and suggested that central sleep apnea is<br />
more common than in younger counterparts. Interestingly,<br />
other data suggest that the associations of OSA<br />
with hypertension, sleepiness, and cognitive dysfunction<br />
are weaker in older versus middle-aged persons. 18<br />
Obesity is a critical independent causative/risk factor.<br />
<strong>The</strong> majority of people who have OSA are obese and the<br />
severity of the condition seems to correlate with the<br />
patient’s neck circumference. 13 In the minority of patients<br />
who are nonobese, causative risk factors are craniofacial<br />
and orofacial bony abnormalities, nasal obstruction, and<br />
hypertrophied tonsils. 19,20<br />
<strong>The</strong> apnea/hypopneic index (AHI) is obtained by performing<br />
polysomnography. <strong>The</strong> number of apneic and<br />
hypopneic episodes per hour is recorded, and the patient<br />
is assigned a corresponding number. An AHI value<br />
between 5 and 14 is associated with mild OSA, 15–30<br />
moderate, and >30 severe OSA. 21<br />
It is generally accepted that many patients with OSA<br />
have resultant daytime sleepiness associated with performance<br />
decrements and an increased incidence of workand<br />
driving-related accidents. It has also been well<br />
established that patients with severe apnea suffer major<br />
health consequences, including premature death, as a<br />
result of their condition. Few absolute conclusions can be<br />
drawn at this time about the long-term consequences of<br />
mild to moderate OSA. However, recently published<br />
findings from the Sleep Heart Health Study, 22 the Copenhagen<br />
City Heart Study, 23 and others 24 demonstrate a firm<br />
association between sleep apnea and systemic hypertension,<br />
even after other important patient characteristics,<br />
such as age, gender, race, consumption of alcohol, and use<br />
of tobacco products are controlled for. Additionally,<br />
patients with OSA have been found to have disturbances<br />
in inflammatory and coagulation profiles as well as altered<br />
vascular responsiveness. Increased sympathetic tone and<br />
enhanced platelet aggregation may contribute to the<br />
greater incidence of MI and stroke noted in these<br />
patients. 25,26 A preoperative assessment of comorbid conditions<br />
should be undertaken to detect hypertension, dysrhythmias,<br />
previous MI, cerebrovascular disease, and<br />
biventricular failure. Polycythemia, electrocardiogram<br />
abnormalities including right and left ventricular hypertrophy,<br />
and cor pulmonale may be present secondary to
22. <strong>Anesthesia</strong> Considerations for <strong>Geriatric</strong> Outpatients 325<br />
Table 22-1. Conditions often associated with sleep apnea.<br />
• Obesity<br />
• Cor pulmonale<br />
• Systemic hypertension<br />
• Dysrhythmias<br />
• Pulmonary hypertension<br />
• ↑ Platelet aggregation<br />
• Right and/or left ventricular hypertrophy<br />
• Inflammatory disturbances<br />
• Polycythemia<br />
pulmonary or systemic hypertension (Table 22-1). <strong>The</strong><br />
physical examination of a patient with known or suspected<br />
OSA should include particular attention to neck<br />
circumference, Mallampati class, and signs of redundant<br />
oropharyngeal tissue.<br />
In terms of pathophysiology, sleep apnea occurs when<br />
the negative airway pressure that develops during inspiration<br />
is greater than the muscular distending pressure,<br />
causing collapse of the airway. Obstruction can occur<br />
throughout the upper airway, above, below, or at the level<br />
of the uvula. 27,28 Because there is an inverse relationship<br />
between obesity and pharyngeal area, the smaller size of<br />
the upper airway in the obese patient causes a more negative<br />
pressure to develop for the same inspiratory flow. 28,29<br />
Kuna and Sant’Ambrogio 28 have also postulated that<br />
there may be a neurologic basis for the disease in that the<br />
neural drive to the airway dilator muscles is insufficient<br />
or not coordinated appropriately with the drive to the<br />
diaphragm. Obstruction can occur during any sleep state,<br />
but is often noted during rapid eye movement sleep.<br />
Nasal continuous positive airway pressure (CPAP) can<br />
ameliorate the situation by keeping the pressure in the<br />
upper airway positive, thus acting as a “splint” to maintain<br />
airway patency.<br />
<strong>The</strong> site(s) of obstruction can be determined preoperatively<br />
by such techniques as magnetic resonance imaging,<br />
computed tomography studies, and intraluminal pressure<br />
measurements during sleep. 30 Some studies suggest that<br />
the major site of obstruction in most patients is at the<br />
oropharynx, but obstruction can also occur at the nasopharynx,<br />
the hypopharynx, and the epiglottis. 31<br />
CPAP devices, at least in the recent past, were often<br />
not well tolerated by patients. However, many technologic<br />
advances have been made with positive airway pressure<br />
devices, making these gadgets more easily tolerated.<br />
Additionally, weight loss may improve OSA, and avoidance<br />
of alcohol and sedatives may have beneficial effects.<br />
Recently, atrial overdrive pacing has shown promising<br />
results in patients with central or OSA. 32 Interestingly,<br />
French investigators serendipitously observed that some<br />
patients who had received a pacemaker with atrial overdrive<br />
pacing to reduce the incidence of atrial dysrhythmias<br />
reported a reduction in breathing disorders after<br />
pacemaker implantation. <strong>The</strong>se cardiologists, therefore,<br />
initiated a study to investigate the efficacy of atrial overdrive<br />
pacing in the treatment of sleep apnea symptoms<br />
in consecutive patients who required a pacemaker for<br />
conventional indications. <strong>The</strong>y found that atrial pacing at<br />
a rate 15 beats per minute faster than the mean nocturnal<br />
heart rate resulted in a significant reduction in the number<br />
of episodes of both central and obstructive apnea. 32 Postulating<br />
that enhanced vagal tone may be associated with<br />
(central) sleep apnea, the investigators acknowledged,<br />
however, that the mechanism of the amelioration of OSA<br />
by atrial overdrive pacing is unclear. Moreover, whether<br />
these unexpected findings are germane to the sleep apnea<br />
patient with normal cardiac function is uncertain. Gottlieb<br />
33 has tantalizingly suggested that a central mechanism<br />
affecting both respiratory rhythm and pharyngeal<br />
motor neuron activity would offer the most plausible<br />
explanation for the reported equivalence in the improvement<br />
of central and OSA during atrial overdrive pacing.<br />
Do cardiac vagal afferents also inhibit respiration?<br />
Perhaps identification of specific neural pathways might<br />
also advance efforts to develop pharmacologic treatment<br />
for sleep apnea.<br />
A variety of surgical approaches to treating sleeprelated<br />
airway obstruction are available. <strong>The</strong>y include<br />
classic procedures, such as tonsillectomy, that directly<br />
enlarge the upper airway, or tracheotomy to bypass the<br />
pharyngeal part of the airway, as well as more specialized<br />
procedures to accomplish the former objective. Examples<br />
include uvulopalatopharyngoplasty, lingualplasty, and<br />
maxillomandibular osteotomy and advancement. Many<br />
OSA patients can be managed effectively with one or a<br />
combination of therapies.<br />
Few definitive data exist to guide perioperative management<br />
of patients with OSA. <strong>The</strong>refore, it is not surprising<br />
that many anesthesiologists question whether<br />
OSA patients are appropriate candidates for ambulatory<br />
surgery. <strong>The</strong> risks of caring for these challenging patients<br />
in the ambulatory venue are further amplified by the<br />
unfortunate fact that 80%–95% of people with OSA are<br />
undiagnosed 34 ; they have neither a presumptive clinical<br />
and/or a sleep study diagnosis of OSA. This is disconcerting<br />
because these patients may suffer perioperatively<br />
from life-threatening desaturation and postoperative<br />
airway obstruction.<br />
Recently, the ASA Task Force on Perioperative<br />
Management of Patients with Obstructive Sleep Apnea<br />
published practice guidelines intended to assist in the<br />
perioperative management of these challenging patients. 35<br />
<strong>The</strong> task force members commented that the literature is<br />
insufficient to offer guidance regarding which patients<br />
with OSA can be safely managed on an outpatient basis,<br />
as well as the appropriate time for discharge of OSA<br />
patients from the surgical facility. <strong>The</strong> consultants agreed,<br />
however, that procedures typically performed on an<br />
outpatient basis in non-OSA patients may also be safely
326 K.E. McGoldrick<br />
performed on an outpatient basis in patients at increased<br />
risk for perioperative OSA when local or regional anesthesia<br />
is administered. <strong>The</strong> consultants were equivocal<br />
concerning whether superficial procedures may be safely<br />
performed during general anesthesia in outpatients with<br />
OSA, and they believe that airway surgery should not be<br />
performed on an outpatient basis in patients with OSA.<br />
Moreover, the capabilities of the outpatient facility are<br />
critical, and the availability of emergency difficult airway<br />
equipment, respiratory care equipment, radiology and<br />
clinical laboratory facilities, and a transfer agreement<br />
with an inpatient facility should be in place if an outpatient<br />
facility assumes responsibility for outpatient surgery<br />
in OSA patients. 35<br />
<strong>The</strong> serious and thoughtful ongoing debate about<br />
whether OSA patients should undergo surgery as outpatients<br />
suggests there is no one-size-fits-all solution. 34 In<br />
deciding a management strategy, it is important to consider<br />
the patient’s body mass index and neck circumference,<br />
the severity of the OSA, the presence or absence of<br />
associated cardiopulmonary disease, the nature of the<br />
surgery, and the anticipated postoperative opioid requirement<br />
(Table 22-2). It seems reasonable to expect that<br />
OSA patients without multiple risk factors who are<br />
having relatively noninvasive procedures under local or<br />
regional anesthesia (carpal tunnel repair, breast biopsy,<br />
knee arthroscopy, etc.) typically associated with minimal<br />
postoperative pain may be candidates for ambulatory<br />
status. However, those individuals with multiple risk<br />
factors, those with severe OSA, or those OSA patients<br />
having airway surgery, most probably will benefit from a<br />
more conservative approach that includes postoperative<br />
admission and careful monitoring. It is imperative to<br />
appreciate that these patients are exquisitely sensitive to<br />
the respiratory depressant effects of opioids and other<br />
central nervous system (CNS) depressants. Additionally,<br />
the risk of prolonged apnea is increased for as long as 1<br />
week postoperatively.<br />
It is important not to be lulled into a false sense of<br />
security simply because general anesthesia is not involved.<br />
Certainly, the use of regional anesthesia may not necessarily<br />
obviate the need for securing the airway, and may<br />
even require emergency airway intervention if excess<br />
sedative-hypnotics or opioids are administered. Regardless<br />
of the type of anesthesia selected, sedation should be<br />
administered judiciously. <strong>The</strong>se patients frequently have<br />
Table 22-2. Factors affecting perioperative management of<br />
obstructive sleep apnea.<br />
• Severity of obstructive sleep apnea (apnea/hypopnea index)<br />
• Body mass index and neck circumference<br />
• Comorbid conditions<br />
• Surgical invasiveness<br />
• Anticipated postoperative opioid requirement<br />
a difficult airway, and often it is more difficult to ventilate<br />
them via a mask than it is to intubate them, although the<br />
latter may also prove challenging. Moreover, it is important<br />
to be aware that the American Sleep Apnea Association<br />
36 notes that “It may be fitting to monitor sleep apnea<br />
patients for several hours after the last doses of anesthesia,<br />
longer than non-sleep apnea patients require and<br />
possibly through one full natural sleep period.” Notably,<br />
the ASA guidelines indicate that patients with OSA<br />
should be monitored for a median of 3 hours longer than<br />
their non-OSA counterparts before discharge from the<br />
facility. Additionally, they indicated that monitoring of<br />
patients with OSA should continue for a median of 7<br />
hours after the last episode of airway obstruction or<br />
hypoxemia while breathing room air in an unstimulating<br />
environment. 35<br />
When confronted with an especially challenging OSA<br />
patient requiring general anesthesia, a judicious approach<br />
may include awake fiberoptic intubation, administering<br />
very low-dose, short-acting narcotics, short-acting muscle<br />
relaxants, and a low solubility inhalational agent, and<br />
infiltrating the surgical site with a long-acting local anesthetic.<br />
Extubation should be performed only when the<br />
patient is without residual neuromuscular blockade and<br />
fully awake, using a tube changer or catheter, and CPAP<br />
should be available postoperatively. Elevation of the<br />
head of the bed to 30 degrees may facilitate pulmonary<br />
excursion. In the postanesthesia care unit (PACU), it is<br />
prudent to have a more prolonged period of observation<br />
and monitoring in patients with OSA, and it is, therefore,<br />
helpful to schedule the procedure early in the day. If no<br />
problems occur in the PACU, and the patient has returned<br />
to baseline with satisfactory analgesia, the patient is discharged<br />
to home. However, if episodes of desaturation or<br />
obtundation have occurred, or if analgesia is problematic,<br />
it is prudent to admit these high-risk patients to a telemetry<br />
ward or intensive care unit because the challenge of<br />
maintaining the airway will extend well into the postoperative<br />
period. Respiratory events after surgery in OSA<br />
patients may occur at any time.<br />
General Principles of<br />
Intraoperative Management<br />
General <strong>Anesthesia</strong><br />
Because of pulmonary changes (discussed elsewhere in<br />
this book) (Table 22-3), it is imperative to appreciate that<br />
desaturation occurs faster in older adults. Additionally,<br />
elderly patients are more vulnerable to desaturationrelated<br />
cardiac events. <strong>The</strong>refore, proper preoxygenation<br />
is critical. Benumof 37 points out that maximal preoxygenation<br />
is achieved with 8 breaths of 100% O 2 within 60<br />
seconds with an oxygen flow of 10 L/min.
22. <strong>Anesthesia</strong> Considerations for <strong>Geriatric</strong> Outpatients 327<br />
Table 22-3. Pulmonary changes associated with aging.<br />
• Reduced chest wall compliance, elastic recoil, and maximal minute<br />
ventilation<br />
• Increased work of breathing<br />
• Increased closing volume<br />
• Reduced forced expiratory volume in 1 second<br />
• Increased ventilation-perfusion mismatch, diffusion block, and<br />
anatomic shunt<br />
• Progressive decline in arterial oxygen tension<br />
• Disproportionately high incidence of postoperative respiratory<br />
complications<br />
Table 22-4. Recommendations for geriatric outpatients having<br />
general anesthesia.<br />
• Appropriate preoxygenation<br />
• ↓↓ Dose of anesthetic agents<br />
• Prevent hypotension by maintaining euvolemia and carefully<br />
titrating appropriate agents<br />
• Select shorter-acting drugs, including neuromuscular blockers<br />
• ? Role of bispectral index monitoring<br />
• Transport to postanesthesia care unit with oxygen<br />
• Maintain normothermia and provide adequate analgesia<br />
Advanced age is clearly associated with a reduction in<br />
median effective dose requirements for all agents that act<br />
within the CNS regardless of whether these drugs are<br />
administered via the oral, parenteral, or inhalational<br />
route. Indeed, the median effective dose equivalent for<br />
inhalation anesthetics decreases linearly with age, such<br />
that the “typical” 80-year-old will require only about two<br />
thirds of the anesthetic concentration required to produce<br />
comparable effects in a young adult. This reduction in<br />
anesthetic requirement is agent-independent and probably<br />
reflects fundamental neurophysiologic changes in the<br />
brain, such as reduced neuron density or altered concentrations<br />
of neurotransmitters.<br />
Elderly patients require less propofol (and other<br />
agents) for induction, and it is also important to appreciate<br />
that the concurrent use of midazolam, ketamine,<br />
and/or opioids with propofol synergistically increases the<br />
depth of anesthesia. Moreover, even with an appropriate<br />
dose reduction of propofol, hypotension is common. Less<br />
hypotension has been reported with appropriately titrated<br />
administration of mask sevoflurane for induction compared<br />
with a propofol infusion. 38 Interestingly, gender<br />
differences have been described in the pharmacokinetics<br />
of propofol given by continuous infusion in elderly<br />
patients, 39 but data in this area have been inconsistent.<br />
<strong>The</strong> time required for clinical recovery from neuromuscular<br />
blockade is markedly increased in older adults<br />
for nondepolarizing agents that undergo organ-based<br />
clearance from plasma, but is minimally different for<br />
atracurium, cisatracurium, or mivacurium because they<br />
undergo hydrolysis in plasma. <strong>The</strong> likelihood of postoperative<br />
pulmonary complications after long-acting muscle<br />
relaxants increases with advanced age, and it is not<br />
unusual for patients who meet rigorous extubation criteria<br />
in the operating room to deteriorate in the PACU.<br />
<strong>The</strong>refore, it seems advisable to administer a short- or<br />
intermediate-acting muscle relaxant to any elderly patient<br />
for whom extubation is planned at the end of the surgical<br />
procedure (Table 22-4).<br />
In planning an expeditious emergence, the anesthesiologist<br />
should be aware that end-tidal gas monitoring<br />
significantly underestimates the brain concentration of<br />
the more soluble agents. Failure to appreciate this hysteresis<br />
effect leads to prolonged emergence. Moreover,<br />
MAC awake is more favorable if the vaporizer is turned<br />
down gradually rather than turned off abruptly. 40 Not<br />
surprisingly, it has been reported that use of shorteracting<br />
drugs (propofol, desflurane, sevoflurane), in conjunction<br />
with bispectral index (BIS) monitoring, can<br />
provide more rapid emergence in geriatric patients and<br />
facilitate PACU bypass. 41 Whether this approach will<br />
have a favorable effect on longer-term outcomes remains<br />
to be determined. Interestingly, a recent study reported<br />
that advancing age and deeper intraoperative anesthetic<br />
levels are associated with higher first-year death rates,<br />
and the authors recommended keeping the BIS level<br />
under general anesthesia close to 60 rather than in the 40<br />
range. 42 Additionally, because of the abnormalities in gas<br />
exchange characteristic of the elderly, it is recommended<br />
that they be transported to the PACU with 2–4 L/min of<br />
oxygen via nasal cannula, even after relatively minor<br />
ambulatory surgery. 43<br />
<strong>Regional</strong> <strong>Anesthesia</strong><br />
When one considers selection of anesthetic technique, it<br />
is important to appreciate that there are no controlled,<br />
randomized studies in elderly patients to show that<br />
regional anesthesia is superior to general anesthesia for<br />
ambulatory surgery. Indeed, neuraxial, plexus, or nerve<br />
blocks in the elderly may be associated with an increased<br />
risk of persistent numbness, nerve palsies, and other neurologic<br />
complications. Additionally, it has recently been<br />
demonstrated that age is a major determinant of duration<br />
of complete motor and sensory blockade with peripheral<br />
nerve block, perhaps reflecting increased sensitivity to<br />
conduction failure from local anesthetic agents in peripheral<br />
nerves in the elderly population. 44 That said, peripheral<br />
nerve blocks offer some appealing features, especially<br />
in terms of postoperative pain control. Clonidine is a<br />
valuable adjunct because it enhances both local anesthetic<br />
and narcotic efficacy, and its addition to the local<br />
anesthetic mixture may afford some hemodynamic advantages<br />
compared with epinephrine. However, one should<br />
select a dose of clonidine that will not produce postoperative<br />
sedation or hypotension. When administering central
328 K.E. McGoldrick<br />
neuraxial blockade to elderly patients, it is important to<br />
remember that a given dose will produce a higher level<br />
of block in seniors and is typically accompanied by a<br />
greater incidence and degree of hypotension and<br />
bradycardia as well as a longer duration of anesthesia. 45<br />
Sedation requirements are dramatically reduced under<br />
conditions of central neuraxial block. 46 Sensory input to<br />
the brain is attenuated and the BIS 50 is shifted to a higher<br />
index. Although recent data have supported a relaxation<br />
of the requirements for voiding before discharge after<br />
outpatient neuraxial blockade with short-acting drugs for<br />
low-risk surgical procedures in low-risk patients, it is<br />
important to appreciate that elderly patients do not meet<br />
these criteria. 47 Currently, it seems that elderly (≥70 years)<br />
patients who received neuraxial block, regardless of the<br />
duration of the block, should be required to demonstrate<br />
ability to void before discharge.<br />
Monitored <strong>Anesthesia</strong> Care<br />
Monitored anesthesia care with intravenous sedation has<br />
become increasingly important in the ambulatory venue<br />
for a variety of cogent reasons. Advances in surgical technology<br />
have enabled many procedures to be performed<br />
through an endoscope rather than a surgical incision, and<br />
these procedures that previously required general or<br />
major regional anesthesia can now be accomplished with<br />
local anesthesia plus sedation. Similarly, technologic<br />
advances in the expanding area of diagnostics have<br />
created an augmented demand for monitored anesthesia<br />
care. Additionally, demographic shifts have seen a steady<br />
growth in the proportion of geriatric patients with coexisting<br />
medical conditions that benefit from minimally<br />
invasive surgical and anesthetic techniques. Finally, as<br />
patients become more knowledgeable “consumers,” they<br />
frequently request anesthetic techniques that will obviate<br />
the side effects associated with general or neuraxial anesthesia<br />
and that will facilitate the most rapid return to<br />
their normal activities. Monitored anesthesia care nicely<br />
dovetails with these exigencies.<br />
Monitored anesthesia care is typically selected for<br />
patients who require supervision of vital signs and administration<br />
of sedative/anxiolytic drugs to supplement local<br />
infiltration or regional anesthesia, or to provide sedation<br />
during uncomfortable or unpleasant diagnostic procedures.<br />
In everyday clinical practice, monitored anesthesia<br />
care usually connotes an anesthetic state ranging from<br />
conscious sedation to deep sedation. However, it is<br />
imperative to appreciate that sedation is a continuum,<br />
and it is not always possible to predict how an individual<br />
patient will respond to a given dose of drug.<br />
<strong>The</strong> major objective of outpatient anesthesia is to<br />
provide a balance between patient comfort and patient<br />
safety while preventing hemodynamic or respiratory<br />
instability, or delay in recovery. Sedation techniques<br />
encompass the use of sedatives, hypnotics, analgesics, and<br />
subanesthetic concentrations of inhalational anesthetics<br />
alone or in combination to supplement local or regional<br />
anesthesia. <strong>The</strong>se classes of drug, when combined, confer<br />
three important components of sedation: amnesia, anxiolysis,<br />
and analgesia.<br />
It is essential to appreciate that the technique of sedation<br />
is as much an art as a science, and facility is gained<br />
best through experience, sensitivity, and proper patient<br />
and surgeon selection. Monitored anesthesia care is recommended<br />
for patients who fear or reject general anesthesia<br />
or who are at increased risk because of age or<br />
certain coexisting medical conditions. Monitored anesthesia<br />
care must be used with caution, however, for<br />
extremely anxious, impaired, or uncooperative patients.<br />
Similarly, monitored anesthesia care is not a panacea for<br />
certain types of medical problems. For example, patients<br />
with severe coronary artery disease or certain morbidly<br />
obese patients might be managed with a greater degree<br />
of control under general anesthesia. Additionally, the<br />
surgeon must be comfortable operating on an awake<br />
patient and must be capable of working gently and with<br />
alacrity. <strong>The</strong> outpatient procedures that lend themselves<br />
to management with monitored anesthesia care include<br />
arthroscopy, biopsies, blepharoplasty and other types of<br />
superficial skin procedures, bronchoscopy, carpal tunnel<br />
repair and other types of upper extremity surgery, cataract<br />
extraction as well as retina and vitrectomy surgery,<br />
cystoscopy, dilatation and curettage, dental surgery, gastrointestinal<br />
endoscopy, insertion of lines and shunts,<br />
herniorrhaphy, rhinoplasty, and rhytidectomy. Similarly,<br />
many diagnostic cardiologic and radiologic procedures<br />
are conducted smoothly and expeditiously under monitored<br />
anesthesia care.<br />
Agents frequently used for monitored anesthesia care,<br />
either alone or in combination, include midazolam, propofol,<br />
fentanyl, and remifentanil. Interpatient variability<br />
is marked with midazolam, and it is important to appreciate<br />
that some patients may be exquisitely sensitive to its<br />
pharmacologic effects. Indeed, when midazolam initially<br />
was introduced to clinicians, reports soon began to circulate<br />
of deaths from unrecognized airway obstruction,<br />
apnea, and hypoxia predominantly in older patients with<br />
concomitant respiratory or cardiovascular disease. <strong>The</strong><br />
package insert was appropriately revised to include warnings<br />
about the necessity of careful monitoring, ability to<br />
manage the airway, and immediate availability of emergency<br />
resuscitation equipment. It is imperative to appreciate<br />
that midazolam depresses the slope of the carbon<br />
dioxide response curve, and attenuates the ventilatory<br />
response to hypoxia. Apnea is not uncommonly encountered.<br />
<strong>The</strong> apparent steepness of the dose-response curve<br />
seen with midazolam underscores the necessity for meticulous<br />
titration and careful monitoring. In geriatric or<br />
debilitated patients, elimination is slower and the dose
22. <strong>Anesthesia</strong> Considerations for <strong>Geriatric</strong> Outpatients 329<br />
should be adjusted downward. Moreover, effects are synergistic<br />
with narcotics. Indeed, when combined with barbiturates,<br />
narcotics, or propofol, the dose of midazolam<br />
should be reduced by at least 25% in young, healthy<br />
patients. This dose reduction should be much more<br />
marked (i.e., ≥50%) initially in elderly and frail individuals.<br />
Although flumazenil may have limited ability to<br />
reverse benzodiazepine-induced respiratory depression, 48<br />
it is thought to have efficacy in reversing the benzodiazepine<br />
component of apnea associated with administration<br />
of midazolam-opioid combinations. 49 Because the<br />
half-life of flumazenil is approximately only 1 hour, the<br />
potential for resedation exists and has been reported.<br />
<strong>The</strong>refore, it is incumbent upon clinicians to monitor<br />
patients carefully for at least 2 hours after administration<br />
of flumazenil.<br />
Propofol possesses a short context-sensitive half-life<br />
and a high plasma clearance that produce a rapid, clearheaded<br />
awakening when used as the sole agent even after<br />
a prolonged continuous infusion. Propofol does, however,<br />
cause a dose-dependent reduction in arterial blood pressure<br />
and it should be used with caution, if at all, in hypovolemic<br />
patients. <strong>The</strong> respiratory effects of low-dose<br />
propofol are moderate. To avoid the unwanted hemodynamic<br />
side effects associated with relative overdosage, it<br />
is critical to reduce initial doses by approximately 40%<br />
in the elderly, even for conscious sedation. 50 Additionally,<br />
it is important to appreciate that recovery of psychomotor<br />
function after propofol sedation is prolonged in geriatric<br />
patients. 51<br />
Remifentanil, the most recently introduced opioid and<br />
an ultrashort-acting fentanyl analog, has a truncated<br />
onset, resembling that of alfentanil, and a high metabolic<br />
clearance. Its most relevant advantage, however, is its<br />
brief context-sensitive half-life (approximately 3 minutes)<br />
that is independent of the duration of the infusion. Remifentanil’s<br />
high lipid solubility and relatively high unbound<br />
un-ionized fraction at physiologic pH result in peak effect<br />
compartment concentration within 1–2 minutes after<br />
bolus administration. 52,53 Likewise, distribution and widespread<br />
esterase metabolism of remifentanil allow for<br />
early offset and return of spontaneous ventilation. 54<br />
Although remifentanil is unique among the opioids in<br />
terms of its metabolism and brief context-sensitive halflife,<br />
remifentanil shares the typical opioid-related side<br />
effects of bradycardia and potential to produce chest wall<br />
rigidity and nausea/vomiting.<br />
Nuances pertaining to dosing of remifentanil merit discussion.<br />
Elderly patients require less remifentanil because<br />
of altered pharmacokinetics and pharmacodynamics that<br />
involve a substantial reduction in central compartment<br />
volume and clearance, and reduction in median effective<br />
concentration and the equilibration between plasma and<br />
its effect compartment. 55 It has also been reported that<br />
adjusting pharmacokinetic models to lean body mass<br />
improve model performance. 55,56 <strong>The</strong>se results suggest<br />
that the dosing of remifentanil should be adjusted to the<br />
lean body mass and that geriatric patients require as<br />
much as 50%–70% dosage reduction.<br />
Remifentanil has been used effectively by bolus injection<br />
for intensely stimulating procedures of brief duration,<br />
such as awake laryngoscopy. 57 Because of the relative<br />
absence of residual opioid effect, prudent use of remifentanil<br />
requires adjunctive analgesics to maintain satisfactory<br />
postoperative analgesia after painful procedures.<br />
This is often accomplished with a combination of nonopioid<br />
analgesics given well in advance of remifentanil<br />
discontinuation, often at or before induction or toward<br />
the completion of surgery. Examples of this multimodal<br />
approach to analgesia include preoperative oral administration<br />
of an appropriate nonsteroidal antiinflammatory<br />
drug followed by infiltration of the wound with local<br />
anesthetic.<br />
It is, perhaps, easy to be lulled into a false sense of<br />
security when one is involved in “only” a monitored anesthesia<br />
care anesthetic for a healthy patient. This misperception,<br />
combined with the production pressures inherent<br />
in contemporary clinical practice, can lead to tragic outcomes.<br />
Unfortunately, the literature is replete with reports<br />
of adverse events associated with sedation techniques. 58–60<br />
Some of these catastrophes reflect performance in remote<br />
locations with inadequate monitoring and sedation<br />
administered by individuals not thoroughly trained in<br />
monitoring, pharmacology, airway management, and<br />
resuscitation.<br />
Even in the skilled hands of an experienced anesthesiologist,<br />
monitored anesthesia care can be challenging.<br />
Patients expected to be most susceptible to the effects of<br />
these medications are those at the extremes of age, the<br />
obese, those given additive or synergistic drug combinations,<br />
and those with cardiopulmonary, renal, or hepatic<br />
disease.<br />
According to data from the Food and Drug Administration,<br />
midazolam was implicated in at least 80 deaths<br />
during gastrointestinal endoscopy, which occurred mainly<br />
in the absence of monitoring by an anesthesiologist. 58<br />
Respiratory events were responsible for the majority<br />
of the incidents, and most patients had also received<br />
an opioid.<br />
In a study by Cohen of 100,000 anesthetics, monitored<br />
anesthesia care morbidity was 208/10,000, higher<br />
than that associated with either general anesthesia or<br />
regional techniques. 61 In fact, during the 1990s, monitored<br />
anesthesia care medicolegal claims became more com -<br />
mon, accounting for 6% of the cases in the Closed Claims<br />
database. 62 Sixty-five percent of the monitored anes -<br />
thesia care patients involved were older, sicker (ASA<br />
physical status 3–5) outpatients. In contradistinction to<br />
most ambulatory claims that tend to involve rather minor<br />
types of injuries in healthier patients, 63 the monitored
330 K.E. McGoldrick<br />
anesthesia care claims reflected more severe injuries, with<br />
death (39%) and brain damage (15%) common. Moreover,<br />
payments were high (similar to that for general<br />
anesthesia), and the mechanism of injury was often respiratory<br />
(25%) or cardiovascular (14%). It is troubling that<br />
litigation from monitored anesthesia care–related injury<br />
increased during the 1990s, despite the use of pulse oximetry<br />
and other respiratory monitoring. <strong>The</strong> sine qua non<br />
of safety is that the provider must have a profound respect<br />
for the continuum from anxiolysis to unconsciousness.<br />
Adherence to uniform standards is critical. Patients re -<br />
ceiving monitored anesthesia care should benefit from<br />
the same level of preoperative, intraoperative, and postoperative<br />
vigilance as patients receiving general or<br />
regional anesthesia. <strong>The</strong>refore, it is imperative that<br />
patients be monitored appropriately by qualified personnel<br />
who are knowledgeable about pharmacokinetics and<br />
pharmacodynamics, especially in the gerontologic population,<br />
and who are experienced in airway management<br />
and resuscitation. <strong>The</strong> recent development of ultrashortacting<br />
drugs such as remifentanil, new techniques of<br />
administration (e.g., patient-controlled sedation and<br />
target-controlled infusions), and monitoring devices such<br />
as the BIS may further optimize intraoperative conditions<br />
and expedite recovery, thereby enhancing the safety,<br />
efficiency, and cost-effectiveness of ambulatory surgery.<br />
Pain Management Pitfalls<br />
Many elderly individuals suffer from acute or chronic<br />
pain and increasingly seek treatment for their condition.<br />
Depression is common in the elderly and is especially<br />
likely to be encountered in the geriatric patient with<br />
chronic pain. Given the increased prevalence of pain<br />
management options and facilities that became available<br />
in the 1990s, it is not surprising that the overall percentage<br />
of chronic pain management claims in the Closed<br />
Claims increased from 2%–3% in the 1970s and 1980s to<br />
10% in the 1990s. <strong>The</strong> overwhelming majority (97%) of<br />
pain litigation in the claims database involved invasive<br />
procedures such as blocks, injections, ablative procedures,<br />
and insertion and/or removal of implantable pumps or<br />
stimulators. 64 Although nerve injury and pneumothorax<br />
were the most common adverse outcomes in pain management<br />
claims, devastatingly serious injuries involving<br />
brain damage occurred also.<br />
Nerve injury was the most common complication of<br />
invasive pain management procedures; tragically, half of<br />
the 63 nerve injury claims involved spinal cord injury.<br />
Epidural hematoma was a common mechanism of spinal<br />
cord injury. <strong>The</strong>refore, the anesthesiologist should have a<br />
high index of suspicion concerning any unexpected motor<br />
or sensory findings after performance of neuraxial blockade,<br />
and should carefully monitor patients for an extended<br />
time after performance of the procedure.<br />
Twenty-one percent of pain management claims were<br />
related to pneumothorax, which was associated primarily<br />
with intercostal nerve blocks, trigger point injections, and<br />
stellate ganglion blocks. Interestingly, in nearly two thirds<br />
(64%) of chronic pain management claims, the injury<br />
became apparent only after discharge from the treatment<br />
facility. Because this temporal association was noted in<br />
some of the cases of pneumothorax, it is important to<br />
instruct patients about the signs and symptoms of pneumothorax<br />
after intercostal nerve blocks, stellate ganglion<br />
blocks, trigger point injections, and brachial plexus blocks.<br />
Additionally, it is critical to be vigilant with implantable<br />
device procedures in which pump programming errors,<br />
drug overdose, and concomitant use of other CNS depressants<br />
can result in death or brain damage.<br />
Postoperative Management<br />
Most surgical morbidity and mortality occur in the postoperative<br />
period. 65 This incontrovertible fact has multifaceted<br />
implications for management of the geriatric<br />
outpatient.<br />
Postoperative Respiratory Insufficiency<br />
Postoperative hypoxemia may occur in 20%–60% of<br />
elderly surgical patients. 66 As highlighted previously,<br />
gerontologic patients have an increased alveolar-arterial<br />
gradient, reduced respiratory muscle strength, and<br />
blunted hypoxic and hypercarbic drives at baseline. Additionally,<br />
there is progressive loss of airway reflexes with<br />
age, and apnea and periodic breathing after administration<br />
of narcotics are more common. 67,68 Postoperative<br />
pain, atelectasis, and shivering further increase the likelihood<br />
of respiratory complications. <strong>The</strong> supine position<br />
during recovery increases the transpulmonary shunt,<br />
making hypoxemia more likely. Finally, orthopedic, upper<br />
abdominal, and intrathoracic procedures, which are<br />
common in elderly persons, have an independent effect<br />
in exacerbating postoperative hypoxemia and other<br />
respiratory complications. 69,70 Fortunately, these types of<br />
procedures—with the possible exception of laparoscopic<br />
cholecystectomy and minor orthopedic interventions—<br />
are not performed on patients in the ambulatory setting.<br />
Nonetheless, as ambulatory surgical centers become<br />
increasingly more inundated with patients, continued<br />
pressure is applied to truncate the time to discharge.<br />
Clearly, such tactics may not be in the best interests of<br />
our geriatric patients who should be observed carefully<br />
for signs of hypoxemia or apnea.<br />
<strong>The</strong> anesthesiologist must be mindful of the risk of<br />
postoperative aspiration in the elderly surgical patient.<br />
Because of alterations in pharyngeal function, diminished<br />
cough, and a higher incidence of gastroesophageal reflux,
22. <strong>Anesthesia</strong> Considerations for <strong>Geriatric</strong> Outpatients 331<br />
elderly patients have an accentuated risk of aspiration. 71,72<br />
This risk is compounded by the effects of anesthesia,<br />
sedatives, and narcotics, as well as by such interventions<br />
as endotracheal intubation, nasogastric tube placement,<br />
and upper abdominal or neck surgery. 73–75 Most probably,<br />
pharyngeal manipulation alters sensation, motor function,<br />
and the protective reflexes that prevent aspiration.<br />
<strong>The</strong> duration of this effect after extubation is often presumed<br />
to be a function of the duration of endotracheal<br />
intubation or other forms of pharyngeal trespass. If so,<br />
this may offer some reassurance to the ambulatory anesthesiologist.<br />
Nonetheless, although the incidence of perioperative<br />
aspiration is low and is rarely associated with<br />
clinically important pneumonitis or pneumonia, 76 the risk<br />
for aspiration extends well beyond the immediate postoperative<br />
period. Clearly, additional research is needed<br />
in the areas of restoration of pharyngeal and tracheal<br />
reflexes, as well as the advancement of feeding after<br />
surgery in the elderly. 77 It seems prudent for the ambulatory<br />
anesthesiologist to alert the geriatric patient and<br />
family members to this potential hazard and to adjust<br />
oral intake accordingly for 24–48 hours postoperatively.<br />
Hypothermia<br />
Because of altered autonomic function, perioperative<br />
hypothermia is prevalent in both young and elderly surgical<br />
patients, but it is more frequent, pronounced, and<br />
prolonged in the elderly who have compromised ability<br />
to regain thermoregulatory control quickly. 78 Adverse<br />
consequences of postoperative hypothermia include<br />
cardiac ischemia, arrhythmias, increased blood loss,<br />
wound infection, decreased drug metabolism, and prolonged<br />
hospitalization. 79 Indeed, it has been shown that<br />
maintaining normothermia decreases cardiac morbidity<br />
by 55%. 80<br />
Postoperative Pain<br />
Postoperative pain increases the risk of adverse outcome<br />
in elderly patients by contributing to cardiac ischemia,<br />
tachycardia, hypertension, and hypoxemia. Effective<br />
analgesia can decrease the incidence of myocardial ischemia<br />
and pulmonary complications, accelerate recovery,<br />
promote early mobilization, shorten hospital stay, and<br />
reduce medical care costs. However, postoperative pain<br />
control often is inadequate in the elderly 81 because of<br />
concerns about drug overdose, adverse response, drug<br />
interactions, and other issues. Pain control is further complicated<br />
by the fact that the patient’s perception and<br />
expression of pain often are affected by changes in mental<br />
status. Current postoperative analgesic techniques include<br />
the use of opioids by various routes, nonsteroidal antiinflammatory<br />
drugs, local anesthetic techniques (neuroaxial,<br />
intraarticular, peripheral nerve block, etc.), and<br />
nonpharmacologic (transcutaneous or percutaneous<br />
electrical nerve stimulation, acupuncture, acupressure,<br />
etc.) methods. Preemptive, multimodal approaches are<br />
favored to minimize the risk of such opioid-related side<br />
effects as hypoxemia, constipation, and pruritus. A balanced<br />
analgesic technique combining opioids, nonopioids,<br />
and local anesthetic agents is recommended.<br />
Clearly, the elderly person is extremely vulnerable to<br />
drug interactions and has an enhanced probability of<br />
respiratory depression, urinary retention, ileus, constipation,<br />
and postoperative falls. <strong>The</strong> likelihood of these complications<br />
can be influenced by the selection of analgesics<br />
and, possibly, the route of administration. 82–85 Drugs such<br />
as clonidine, dexmedetomidine, or the nonsteroidal antiinflammatory<br />
agents may have a valuable role in reducing<br />
side effects attributable to opioids. It is imperative to<br />
be cognizant of the investigation by Bates and colleagues 86<br />
demonstrating that analgesics are the class of drugs associated<br />
not only with the highest number of adverse events,<br />
but also with the greatest number of preventable adverse<br />
events. Other significant offenders are sedatives and<br />
antibiotics.<br />
Postoperative Atrial Fibrillation<br />
In terms of cardiac function, it is well known that geriatric<br />
patients have decreased beta-adrenergic responsiveness,<br />
and they experience an increased incidence of conduction<br />
abnormalities, bradyarrhythmias, and hypertension.<br />
Fibrotic infiltration of cardiac conduction pathways and<br />
replacement of myocardial elastic fibers render the<br />
elderly individual vulnerable to conduction delay and to<br />
atrial and ventricular ectopy. Indeed, it is well known that<br />
postoperative atrial arrhythmias, and atrial fibrillation<br />
(AF) and flutter specifically, are seen in 6.1% of elderly<br />
patients undergoing noncardiothoracic surgery and in<br />
10%–40% of patients after cardiothoracic operations. 87–90<br />
Although it has been firmly established that older age<br />
(>60 years) is the strongest predictor of postoperative AF,<br />
a recent investigation found that a greater preoperative<br />
heart rate (≥74 beats per minute) is also independently<br />
associated with postoperative AF. 91 This suggests that a<br />
lower vagal tone before surgery may be a contributing<br />
trigger of this arrhythmia. Interestingly, AF occurred at a<br />
median of 69 hours after surgery. Because reliance on<br />
atrial “kick” is critically important for older adults, should<br />
we prophylactically treat high-risk patients to prevent<br />
postoperative AF? If so, should we use rate control or<br />
rhythm control drugs? <strong>The</strong>se are unanswered questions<br />
and offer inviting opportunities for important research.<br />
However, given the types of procedures that are typically<br />
conducted on an ambulatory basis, geriatric outpatients<br />
may be at less risk for this complication than their inpatient<br />
counterparts.
332 K.E. McGoldrick<br />
Postoperative Cognitive Impairment<br />
Reports of postoperative cognitive deterioration in<br />
elderly patients surfaced more than a century ago, and<br />
anesthesia had often been implicated as a possible cause<br />
or contributing factor. Although improvements in surgical<br />
techniques and anesthetic agents and methods have<br />
led to improved outcomes in the elderly, a troubling<br />
proportion of these patients experience postoperative<br />
cognitive impairment. 92–95 <strong>The</strong> implications of this abrupt<br />
cognitive decline are devastating because affected individuals<br />
often become dependent and withdraw from<br />
society. Sadly, our knowledge about the CNS effects<br />
of anesthetics on the aging brain is rather primitive.<br />
However, the previously described age-associated changes<br />
imply that the aging CNS has reduced functional reserve,<br />
similar to the heart, lungs, and kidneys. Perhaps this putative<br />
reduction in brain functional reserve renders the<br />
elderly more likely to develop postoperative cognitive<br />
disturbances.<br />
<strong>The</strong> syndromes of postoperative cognitive impairment<br />
can be classified into two main categories: postoperative<br />
delirium and postoperative cognitive dysfunction<br />
(POCD). 96 Although postoperative delirium and POCD<br />
may have similar predisposing factors, they are not equivalent<br />
syndromes. Delirium is defined as an acute change<br />
in cognitive function that develops over a brief period of<br />
time, often lasting for a few days to a few weeks, and frequently<br />
has a fluctuating course. Onset is typically on the<br />
first to third postoperative day, and the patient’s confusion<br />
tends to wax and wane. Prospective studies have<br />
cited an incidence of delirium that ranges from 3% to<br />
>50% and is dependent on the type of surgery, the<br />
patient’s preoperative physical and cognitive status, and<br />
the age of the patient. 96 <strong>The</strong> etiology of delirium is probably<br />
multifactorial and may include drug intoxication or<br />
withdrawal, drug interaction, anticholinergic agents, metabolic<br />
disturbances, hypoxia, abnormal carbon dioxide<br />
levels, sepsis, inadequate analgesia, and organic brain<br />
disease. 97 Curiously, the incidence of postoperative confusion<br />
is similar regardless of whether spinal, epidural, or<br />
general anesthesia is used. 93 It has been postulated that<br />
postoperative delirium may be associated with failure of<br />
CNS cholinergic transmission. 98 It has also been suggested<br />
that pain, sleep deprivation, sensory deprivation<br />
or overload, and an unfamiliar environment may contribute<br />
to delirium. Recently, the use of melatonin to treat<br />
delirium has produced some benefit, presumably by resetting<br />
the circadian sleep–awake cycle of older surgical<br />
patients. 99 Postoperative delirium is common in the<br />
elderly and its incidence may be reduced by protocoldriven<br />
perioperative treatment. Marcantonio and colleagues,<br />
100 in a study of orthopedic inpatients, reported a<br />
reduction in postoperative delirium by one third, and of<br />
severe delirium by half, by adherence to multifaceted<br />
recommendations that included elimination or minimization<br />
of benzodiazepines, anticholinergics, antihistaminics,<br />
and meperidine. Additionally, systolic blood pressure was<br />
kept more than two thirds of baseline or >90 mm Hg,<br />
oxygen saturation was maintained at >90% (preferably<br />
>95%), hematocrit was maintained at >30%, early mobilization<br />
was encouraged, and appropriate environmental<br />
stimuli were provided. Because ambulatory patients<br />
return home to a familiar environment postoperatively<br />
where appropriate stimuli and support are available, one<br />
suspects that the incidence of delirium may be less in<br />
outpatients than in their hospitalized counterparts.<br />
POCD is defined as a “deterioration of intellectual<br />
function presenting as impaired memory or concentration.”<br />
101 <strong>The</strong> clinical features of this disorder range from<br />
mild forgetfulness to permanent cognitive impairment.<br />
We have much to learn about the pathogenesis and<br />
prevention of POCD. A current hypothesis is that the<br />
etiology is multifactorial and may include impaired preoperative<br />
cognitive status, as well as intraoperative events<br />
related to the surgery itself (e.g., microemboli), and anesthetic<br />
agents/depth. Additionally, physiologic and sociologic<br />
consequences of hospitalization and surgery may<br />
have a role.<br />
Moller and colleagues 92 in a multinational study evaluated<br />
cognitive function in patients aged 60 years or older<br />
after major abdominal and orthopedic surgery. <strong>The</strong>se<br />
investigators found that approximately 25% of the<br />
patients had measurable cognitive dysfunction a week<br />
after their surgery and 10% had cognitive changes 3<br />
months postoperatively. This finding contrasted with a<br />
3% incidence of cognitive deterioration 3 months later in<br />
healthy control subjects in the same age range who did<br />
not undergo anesthesia and surgery. Interestingly, despite<br />
extensive monitoring, neither hypoxemia nor hypotension<br />
correlated with the occurrence of prolonged cognitive<br />
dysfunction. <strong>The</strong> identified risk factors for early<br />
POCD were increasing age and duration of anesthesia,<br />
low education level, a need for a second operation, postoperative<br />
infection, and respiratory complications. <strong>The</strong><br />
only risk factor for late POCD was age. Although the<br />
incidence of late POCD was 14% for patients ≥70 years,<br />
this rate decreased to only 7% for patients between the<br />
ages of 60 to 70 years.<br />
An additional large, prospective study conducted by<br />
Monk and colleagues 95 evaluated the relationship of age<br />
to POCD. Using the same methodology as the first multinational<br />
study, 92 Monk and colleagues reported that<br />
cognitive decline occurred in 16% of patients aged 60<br />
years or older at 3 months after major noncardiac surgery,<br />
but was present in only 3%–5% of younger patients. 94<br />
This study also determined that rates of cognitive decline<br />
were higher in those ≥70 years compared with younger<br />
elderly patients. Interestingly, anesthetic technique does<br />
not seem to matter; there is no difference between
22. <strong>Anesthesia</strong> Considerations for <strong>Geriatric</strong> Outpatients 333<br />
regional and general anesthesia in the incidence of<br />
cognitive impairment 3–6 months postoperatively even<br />
though short-term recovery may be better with regional<br />
anesthesia. 93,102<br />
<strong>The</strong>re are few prospective studies on long-term cognitive<br />
outcomes after outpatient surgery, but an analysis of<br />
cognitive recovery after major and minimally invasive<br />
surgery exists. Monk classified the type of surgical procedure<br />
as minimally invasive (laparoscopic or superficial<br />
surgery), major intraabdominal surgery, or orthopedic<br />
surgery. 95 <strong>The</strong> incidence of POCD was significantly greater<br />
for patients undergoing major or orthopedic procedures<br />
compared with minimally invasive surgery. Because outpatient<br />
surgery is usually minimally invasive, these results<br />
suggest that outpatients may have a better cognitive<br />
outcome than patients who require hospitalization. <strong>The</strong><br />
International Study of Postoperative Cognitive Dysfunction<br />
group recently conducted a longitudinal study comparing<br />
the incidence of POCD after inpatient versus<br />
outpatient surgery in patients older than 60 years. 103 At 7<br />
days after surgery, the incidence of POCD was significantly<br />
lower in the outpatient group, but this difference<br />
was not detected 3 months later. <strong>The</strong>se results suggest<br />
that elderly outpatients have better cognitive outcomes<br />
at discharge than elderly inpatients, but we currently have<br />
no explanation for the difference. Possible explanations<br />
for the improved early outcome in outpatients include<br />
the healthier status of patients who qualify for outpatient<br />
surgery, the briefer surgical and anesthesia times, the<br />
minimally invasive nature of most outpatient procedures,<br />
or avoidance of hospitalization.<br />
Although we have much to learn about postoper -<br />
ative delirium and cognitive decline, it is clear that subclinical<br />
decrements in functional status may become<br />
evident during the perioperative period. Indeed, if a cognitive<br />
deficit is noted preoperatively, it may be a harbinger<br />
of further postoperative decline. <strong>The</strong> data on the predictive<br />
value of preoperative cognitive status 104 and the ability<br />
of that assessment to result in successful intervention (as<br />
may be the case with delirium) 100,105 offer compelling<br />
reasons to conduct a simple, brief mental status examination<br />
as part of the preoperative interview.<br />
It is important to understand that full return of cognitive<br />
function to preoperative levels may require several<br />
days, even after ambulatory surgery in young, healthy<br />
patients. 97,106 Indeed, Lichtor et al. 107 have suggested that<br />
even young adults may be sleepy for 8 hours after receiving<br />
intravenous sedation with midazolam and fentanyl,<br />
and the elderly outpatient with balance disturbances or<br />
age-related gait impairment may be at high risk of falling<br />
because of residual drowsiness. Moreover, Monk et al. 95<br />
have reported that POCD is detected with psychometric<br />
testing in 34% of young (aged 18–39 years), 35%<br />
of middle-aged (40–59 years), and 40% of elderly (aged<br />
≥60 years) patients 1 week postoperatively. Similarly,<br />
Johnson 108 has reported a 19.6% incidence of POCD at 1<br />
week postoperatively in patients aged 40–60 years. This<br />
rate decreased to 6.2% at 3 months.<br />
Nonetheless, it remains unclear which patient populations<br />
are most vulnerable and what the causative factors<br />
might be for the serious problem of POCD. As mentioned,<br />
there seems to be no difference in the incidence<br />
of POCD whether regional or general anesthesia is<br />
administered. 93,102,109 Hopefully, future studies will lead to<br />
a clearer definition of the incidence, mechanisms, and<br />
prevention of POCD.<br />
Other Postdischarge Concerns<br />
Although the Aldrete guidelines offer a satisfactory paradigm<br />
to determine when an inpatient is fit for discharge<br />
from the PACU to an overnight bed, or when an outpatient<br />
is able to bypass phase I recovery and go directly to<br />
a step-down unit, the Aldrete criteria are inadequate<br />
to assess fitness for discharge to home in an ambulatory<br />
patient. To that end, Chung 110 has developed a modified<br />
postanesthesia discharge scoring system (PADSS) that<br />
addresses this need. Whereas the Aldrete score focuses<br />
on activity (ability to move the extremities), respiration,<br />
blood pressure, level of consciousness, and color, the<br />
modified PADSS assesses such additional and germane<br />
parameters as ability to ambulate without dizziness,<br />
nausea and vomiting, pain, and surgical bleeding (Table<br />
22-5).<br />
Typically, PONV and pain are two of the most common<br />
reasons for unanticipated admission after planned outpatient<br />
surgery. 111 Apfel and colleagues 112 have shown that<br />
the four most relevant risk factors for predicting PONV<br />
are female gender, previous PONV or motion sickness,<br />
nonsmoking status, and postoperative opioid use. <strong>The</strong><br />
Table 22-5. Modified postanesthesia discharge scoring system.<br />
Vital signs<br />
Ambulation and mental status<br />
Nausea and vomiting<br />
Pain<br />
Surgical bleeding<br />
2 = within 20% of baseline<br />
1 = 20%–40% of baseline<br />
0 = 40% of baseline<br />
2 = steady gait, no dizziness<br />
1 = walks with assistance<br />
0 = none/dizziness<br />
2 = minimal<br />
1 = moderate<br />
0 = severe<br />
2 = minimal<br />
1 = moderate<br />
0 = severe<br />
2 = minimal<br />
1 = moderate<br />
0 = severe<br />
Source: Reprinted from Chung, 110 with permission from Elsevier.<br />
Note: Total postanesthesia discharge scoring system score is 10; score<br />
≥9 considered fit for discharge.
334 K.E. McGoldrick<br />
Sinclair score requires a probability calculation based on<br />
the same first three factors as well as the age of the<br />
patient and the duration and type of surgery. 113 Fortunately,<br />
the risk of PONV is said to decrease 17% with<br />
each decade after age 50.<br />
Transient, subclinical hearing loss is not uncommon<br />
after spinal anesthesia. 114,115 <strong>The</strong> pathophysiology is<br />
thought to involve movement of perilymph from the ear<br />
into the subarachnoid space as cerebrospinal fluid leaks<br />
out. <strong>The</strong> perilymph enters the subarachnoid space via<br />
the cochlear aqueduct; the resultant increase in endolymphatic<br />
pressure in the ear is thought to contribute to<br />
the diminished hearing. It has been demonstrated that<br />
the rate of mild hearing loss after spinal anesthesia<br />
varies inversely with the patient’s age. A recent investigation<br />
disclosed that both the incidence and degree of<br />
hearing loss were increased in patients aged ≤30 years. 115<br />
Perhaps cerebrospinal fluid leakage after dural puncture<br />
occurs more frequently and more extensively in the<br />
young, and possibly this phenomenon also accounts for<br />
the much greater incidence of postdural puncture headache<br />
in the young.<br />
It is imperative that elderly outpatients be discharged<br />
from an outpatient surgery facility only if accompanied by<br />
an escort, and a competent individual should remain with<br />
the patient for at least 24 hours postoperatively. <strong>Geriatric</strong><br />
patients are at higher risk for drowsiness, confusion,<br />
falls, urinary retention, and adverse drug interactions than<br />
their younger counterparts. Clinicians should provide the<br />
patient and his or her caregiver with clear, written postoperative<br />
instructions about administration of medications,<br />
activities to be avoided, and the phone number to<br />
be called should problems or questions arise.<br />
Summary<br />
Elderly patients are uniquely vulnerable and particularly<br />
sensitive to the stresses of hospitalization and surgery/<br />
anesthesia in ways that are only partially understood. Preoperatively<br />
a thoughtful assessment of organ function and<br />
reserve is required. Efforts to identify the “best” intraoperative<br />
anesthetic agent or technique or approach for the<br />
elderly continue, but it seems that no anesthetic agent or<br />
technique is unequivocally superior for all conditions<br />
or circumstances. <strong>The</strong>refore, clinicians should strive to<br />
maintain homeostasis, to avoid drug cocktails—especially<br />
long-acting benzodiazepines and anticholinergics—to<br />
administer short-acting drugs, maintain normothermia<br />
and euvolemia, and provide adequate postoperative analgesia.<br />
When possible, a case might be made for encouraging<br />
ambulatory surgery because of its typically brief<br />
duration, relatively noninvasive approach, and its ability<br />
to allow elderly patients to recover in their familiar, supportive<br />
home environment.<br />
References<br />
1. McGoldrick KE. Postoperative nausea and vomiting. In:<br />
Afifi A, Rosenbaum S, eds. Problems in <strong>Anesthesia</strong>. Vol 12,<br />
No. 3. PACU and Anesthetic Management. Philadelphia:<br />
Lippincott Williams & Wilkins; 2000:274–286.<br />
2. Ergina P, Gold S, Meakins J. Perioperative care of the<br />
elderly patient. World J Surg 1993;17:192–198.<br />
3. Fleisher LA, Pasternak LR, Herbert R, Anderson GF.<br />
Inpatient hospital admissions and death after outpatient<br />
surgery in elderly patients. Arch Surg 2004;139:67–72.<br />
4. Rao RB, Ely SF, Hoffman RS. Deaths related to liposuction.<br />
N Engl J Med 1999;340:1471–1475.<br />
5. Vila H, Soto R, Cantor AB, Mackey D. Comparative outcomes<br />
analysis of procedures performed in physician<br />
offices and ambulatory surgery centers. Arch Surg 2003;<br />
138:991–995.<br />
6. Silverstein JH. <strong>Geriatric</strong> anesthesia enters a new age. ASA<br />
Newslett 2004;68:6, 22.<br />
7. Schein OD, Katz J, Bass EB, et al. <strong>The</strong> value of routine<br />
preoperative medical testing before cataract surgery. N<br />
Engl J Med 2000;342:168–175.<br />
8. Dzankic S, Pastor D, Gonzalez C, Leung JM. <strong>The</strong> prevalence<br />
and predictive value of abnormal preoperative<br />
laboratory tests in elderly surgical patients. Anesth Analg<br />
2001;93:301–308.<br />
9. Eagle KA, Berger PB, Calkins H, et al. ACC/AHA guideline<br />
update for perioperative cardiovascular evaluation for<br />
noncardiac surgery. J Am Coll Cardiol 2002;39:542–553.<br />
10. Goldman L. Cardiac risks and complications of noncardiac<br />
surgery. Ann Intern Med 1983;98:504–513.<br />
11. Liu LL, Leung JM. Predicting adverse postoperative<br />
outcomes in patients aged 80 years or older. J Am Geriatr<br />
Soc 2000;48:405–412.<br />
12. Poldermans D, Boersma E, Bax JJ, et al. <strong>The</strong> effect of<br />
bisoprolol on perioperative mortality and myocardial<br />
infarction in high-risk patients undergoing vascular surgery.<br />
N Engl J Med 1999;341:1789–1794.<br />
13. Young T, Palta M, Dempsey J, et al. <strong>The</strong> occurrence<br />
of sleep-disordered breathing among middle-aged adults.<br />
N Engl J Med 1993;328:1230–1235.<br />
14. Carskadon MA, Dement WC. Respiration during sleep<br />
in the aged human. J Gerontol 1981;36:420–423.<br />
15. Strollo PJ Jr, Rogers RM. Obstructive sleep apnea. N Engl<br />
J Med 1996;334:99–104.<br />
16. Young T, Skatrud J, Peppard PE. Risk factors for obstructive<br />
sleep apnea in adults. JAMA 2004;219:2013–2016.<br />
17. Bixler EO, Vgontzas AN, Ten Have T, et al. Effects of age<br />
on sleep apnea in men: prevalence and severity. Am J<br />
Respir Crit Care Med 1998;157:144–148.<br />
18. Young T, Peppard PE, Gottlieb DJ. Epidemiology of<br />
obstructive sleep apnea. Am J Respir Crit Care Med 2002;<br />
165:1217–1239.<br />
19. Helfaer MA, Wilson MD. Obstructive sleep apnea, control<br />
of ventilation, and anesthesia in children. Pediatr Clin<br />
North Am 1994;41:131–151.<br />
20. Loadsman JA, Hllman DR. Anaesthesia and sleep apnoea.<br />
Br J Anaesth 2001;86:254–256.<br />
21. American Academy of Sleep Medicine Task Force. Sleeprelated<br />
breathing disorders in adults: recommendations for
22. <strong>Anesthesia</strong> Considerations for <strong>Geriatric</strong> Outpatients 335<br />
syndrome definition and measurement techniques in clinical<br />
research. Report of the American Academy of Sleep<br />
Medicine Task Force. Sleep 1999;22:667.<br />
22. Nieto FJ, Young TB, Lind BK et, al. Association of sleepdisordered<br />
breathing, sleep apnea, and hypertension in a<br />
large community-based study: Sleep Heart Health Study.<br />
JAMA 2000;283:1829–1836.<br />
23. Nymann P, Backer V, Dirksen A, Lange P. Increased diastolic<br />
blood pressure associated with obstructive sleep<br />
apnea independently of overweight [abstract]. Sleep 2000;<br />
23:A61.<br />
24. Bixler EO, Vgontzas AN, Lucas T, et al. <strong>The</strong> association<br />
between sleep-disordered breathing and cardiovascular<br />
abnormalities [abstract]. Sleep 2000;23:A59.<br />
25. Grote L, Kraiczi H, Hedner J. Reduced alpha- and beta 2 -<br />
adrenergic vascular response in patients with obstructive<br />
sleep apnea. Am J Respir Crit Care Med 2000;162:1480–<br />
1487.<br />
26. Shamsuzzaman AS, Somers VK. Fibrinogen, stroke, and<br />
obstructive sleep apnea: an evolving paradigm of cardiovascular<br />
risk. Am J Crit Care Med 2000;162:2018–2020.<br />
27. Hudgel DW. Mechanisms of obstructive sleep apnea. Chest<br />
1992;101:541–549.<br />
28. Kuna ST, Sant’Ambrogio G. Pathophysiology of upper<br />
airway closure during sleep. JAMA 1991;266:1384–1389.<br />
29. Beydon L, Hassapopoulos J, Quera MA, et al. Risk factors<br />
for oxygen desaturation during sleep after abdominal<br />
surgery. Br J Anaesth 1992;69:137–142.<br />
30. Boudewyns AN, DeBacker WA, Van de Heyning PH.<br />
Pattern of upper airway obstruction during sleep before<br />
and after uvulopalatopharyngoplasty in patients with<br />
obstructive sleep apnea. Sleep Med 2001;2:309–315.<br />
31. Catalfumo FJ, Golz A, Westerman ST, et al. <strong>The</strong> epiglottis<br />
and obstructive sleep apnoea syndrome. J Laryngol Otol<br />
1998;112:940–943.<br />
32. Garrigue S, Bordier P, Jais P, et al. Benefit of atrial<br />
pacing in sleep apnea syndrome. N Engl J Med 2002;346:<br />
404–412.<br />
33. Gottlieb DJ. Cardiac pacing—a novel therapy for sleep<br />
apnea? [editorial]. N Engl J Med 2002;346:444–445.<br />
34. Benumof JL. Obstructive sleep apnea in the adult obese<br />
patient: implications for airway management. J Clin Anesth<br />
2001;13:144–156.<br />
35. ASA Task Force on Perioperative Management of Patients<br />
with Obstructive Sleep Apnea. Practice guidelines for the<br />
perioperative management of patients with obstructive<br />
sleep apnea. <strong>Anesthesiology</strong> 2006;104:1081–1093.<br />
36. American Sleep Apnea Association: sleep apnea and same<br />
day surgery. Washington, DC: American Sleep Apnea<br />
Association; 1999. www.sleepapnea.org/sameday/html.<br />
37. Benumof J. Preoxygenation: best method for both efficacy<br />
and efficiency [editorial]. <strong>Anesthesiology</strong> 1999;91:603–605.<br />
38. Kirkbride DA, Parker JL, Williams GD, Buggy DJ. Induction<br />
of anesthesia in the elderly ambulatory patient: a<br />
double-blind comparison of propofol and sevoflurane.<br />
Anesth Analg 2001;93:1185–1187.<br />
39. Vuyk J, Oostwouder CJ, Vletter AA, Burm AGL, Bovill JG.<br />
Gender differences in the pharmacokinetics of propofol in<br />
elderly patients during and after continuous infusion. Br J<br />
Anaesth 2001;86:183–188.<br />
40. Katoh T, Suguro Y, Kimura T, Ikeda K. Cerebral awakening<br />
concentration of sevoflurane and isoflurane predicted<br />
during slow and fast alveolar washout. Anesth Analg 1993;<br />
77:1012–1017.<br />
41. Fredman B, Sheffer O, Zohar E, et al. Fast-track eligibility<br />
of geriatric patients undergoing short urologic procedures.<br />
Anesth Analg 2002;94:560–564.<br />
42. Weldon BC, Mahla ME, van der Aa MT, Monk TG. Advancing<br />
age and deeper intraoperative anesthetic levels are<br />
associated with higher first year death rates [abstract].<br />
<strong>Anesthesiology</strong> 2002;96:A1097.<br />
43. Mathes DD, Conaway MR, Ross WT. Ambulatory<br />
surgery: room air versus nasal cannula oxygen during<br />
transport after general anesthesia. Anesth Analg 2001;93:<br />
917–921.<br />
44. Pagueron X, Boccara G, Bendahou M, Coriat P, Riou B.<br />
Brachial plexus nerve block exhibits prolonged duration<br />
in the elderly. <strong>Anesthesiology</strong> 2002;97:1245–1249.<br />
45. Simon MJG, Veering BT, Stienstra R, van Kleek JW, Burm<br />
AGL. <strong>The</strong> effects of age on neural blockade and hemodynamic<br />
changes after epidural anesthesia with ropivacaine.<br />
Anesth Analg 2002;94:1325–1330.<br />
46. Pollock JE, Neal JM, Liu SS, et al. Sedation during spinal<br />
anesthesia. <strong>Anesthesiology</strong> 2000;93:728–734.<br />
47. Mulroy MF, Salinas FV, Larkin KL, Polissar NL. Ambulatory<br />
surgery patients may be discharged before voiding<br />
after short-acting spinal and epidural anesthesia. <strong>Anesthesiology</strong><br />
2002;97:315–319.<br />
48. Mora CT, Torjman M, White PF. Sedative and ventilatory<br />
effects of midazolam infusion: effect of flumazenil reversal.<br />
Can J Anaesth 1995;42:677–684.<br />
49. Rouiller M, Forster A, Gemperle M. Evaluation de<br />
l’efficacité et de la tolerance d’un antagoniste des benzodiazepines<br />
(Ro 15–1788). Ann Fr Anesth Reanim 1987;<br />
6:1–6.<br />
50. Kazema T, Takeuchi K, Ikeda K, et al. Optimal propofol<br />
plasma concentration during upper gastrointestinal endoscopy<br />
in young, middle-aged, and elderly patients. <strong>Anesthesiology</strong><br />
2000;93:662–669.<br />
51. Shinozaki M, Usui Y, Yamaguchi S, et al. Recovery of psychomotor<br />
function after propofol sedation is prolonged in<br />
the elderly. Can J Anaesth 2002;49:927–931.<br />
52. Egan TD. <strong>The</strong> clinical pharmacology of the new fentanyl<br />
congeners. Anesth Analg 1997;84(Suppl):31–38.<br />
53. Bailey PL, Egan TD, Stanley TH. Intravenous opioid anesthesia.<br />
In: Miller RD, ed. <strong>Anesthesia</strong>. 5th ed. Philadelphia:<br />
Churchill Livingstone; 2000:273–376.<br />
54. Egan TD. Remifentanil pharmacokinetics and pharmacodynamics:<br />
a preliminary appraisal. Clin Pharmacokinet<br />
1995;29:80–94.<br />
55. Minto CF, Schnider TW, Egan TD, et al. Influence of age<br />
and gender on the pharmacokinetics and pharmacodynamics<br />
of remifentanil. <strong>Anesthesiology</strong> 1997;86:10–23.<br />
56. Egan TD, Huizinga B, Gupta SK, et al. Remifentanil pharmacokinetics<br />
in obese versus lean patients. <strong>Anesthesiology</strong><br />
1998;89:562–573.<br />
57. Johnson KB, Swenson JD, Egan TD, et al. Midazolam and<br />
remifentanil by bolus injection for intensely stimulating<br />
procedures of brief duration: experience with awake laryngoscopy.<br />
Anesth Analg 2002;94:1241–1243.
336 K.E. McGoldrick<br />
58. Food and Drug Administration. Warning re-emphasized in<br />
midazolam labeling. FDA Drug Bull 1986;27:5.<br />
59. Coté CJ, Notterman DA, Karl HW, et al. Adverse sedation<br />
events in pediatrics: a critical incident analysis of contributing<br />
factors. Pediatrics 2000;105:805–814.<br />
60. Coté CJ, Karl HW, Notterman DA, et al. Adverse sedation<br />
events in pediatrics: analysis of medications used for sedation.<br />
Pediatrics 2000;106:633–644.<br />
61. Cohen MM, Duncan PG, Tate RB. Does anesthesia<br />
contribute to operative mortality? JAMA 1988;260:2859–<br />
2863.<br />
62. Domino KB. Trends in litigation in the 1990s: MAC claims.<br />
ASA Newslett 1997;61:15–17.<br />
63. Posner KL. Liability profile of ambulatory anesthesia.<br />
ASA Newslett 2000;64(6):10–12.<br />
64. Fitzgibbon DR, Posner KL, Domino KB, Caplan RA,<br />
Lee LA, Cheney FW. Chronic pain management:<br />
American Society of Anesthesiologists closed claims<br />
project. <strong>Anesthesiology</strong> 2004;100:98–105.<br />
65. Pedersen T, Eliasen K, Henriksen E. A prospective study<br />
of risk factors and cardiopulmonary complications associated<br />
with anaesthesia and surgery: risk indicators of cardiopulmonary<br />
morbidity. Acta Anaesthesiol Scand 1990;34:<br />
144–155.<br />
66. Moller JT, Wittrup M, Johansen SH. Hypoxemia in the<br />
postanesthesia care unit: an observer study. <strong>Anesthesiology</strong><br />
1990;73:890–895.<br />
67. Arunasalam K, Davenport HT, Painter S, Jones JG. Ventilatory<br />
response to morphine in young and old subjects.<br />
Anaesthesia 1983;38:529–533.<br />
68. Pontoppidan H, Beecher HK. Progressive loss of protective<br />
reflexes in the airway with advance of age. JAMA<br />
1960;174:2209–2213.<br />
69. Seymour DG, Vaz FG. A prospective study of elderly<br />
general surgical patients. II. Postoperative complications.<br />
Age Ageing 1989;18:316–326.<br />
70. Pedersen T, Viby-Mogensen J, Ringsted C. Anaesthetic<br />
practice and postoperative pulmonary complications. Acta<br />
Anaesthesiol Scand 1992;36:812–818.<br />
71. Aviv JE. Effects of aging on sensitivity of the pharyngeal<br />
and supraglottic areas. Am J Med 1997;103:74S–76S.<br />
72. Marik PE. Aspiration pneumonitis and aspiration pneumonia.<br />
N Engl J Med 2001;344:665–671.<br />
73. de Larminat V, Montravers P, Dureuil B, Desmonts JM.<br />
Alteration in swallowing reflex after extubation in intensive<br />
care unit patients. Crit Care Med 1995;23:486–490.<br />
74. Hogue CW Jr, Lappas GD, Creswell LL, et al. Swallowing<br />
dysfunction after cardiac operations. Associated adverse<br />
outcomes and risk factors including intraoperative transesophageal<br />
echocardiography. J Thorac Cardiovasc Surg<br />
1995;110:517–522.<br />
75. Mitchell CK, Smoger SH, Pfeifer MP, et al. Multivariate<br />
analysis of factors associated with postoperative pulmonary<br />
complications following general elective surgery.<br />
Arch Surg 1998;133:194–198.<br />
76. Warner MA, Warner ME, Weber JG. Clinical significance<br />
of pulmonary aspiration during the perioperative period.<br />
<strong>Anesthesiology</strong> 1993;78:56–62.<br />
77. Cook DJ. <strong>Geriatric</strong> anesthesia. In: Solomon DH, LoCicero<br />
J III, Rosenthal RA, eds. New Frontiers in <strong>Geriatric</strong><br />
Research. New York: American <strong>Geriatric</strong>s Society; 2004:<br />
9–52.<br />
78. Vaughan MS, Vaughan RW, Cork RC. Postoperative hypothermia<br />
in adults: relationship of age, anesthesia, and shivering<br />
to rewarming. Anesth Analg 1981;60:746–751.<br />
79. Leslie K, Sessler DI, Bjorksten AR, Moayeri A. Mild hypothermia<br />
alters propofol pharmacokinetics and increases<br />
the duration of action of atracurium. Anesth Analg 1995;<br />
80:1007–1014.<br />
80. Frank SM, Higgins MS, Breslow MJ, et al. <strong>The</strong> catecholamine,<br />
cortisol, and hemodynamic responses to mild<br />
perioperative hypothermia: a randomized clinical trial.<br />
<strong>Anesthesiology</strong> 1995;82:83–93.<br />
81. Jones JS, Johnson K, McNinch M. Age as a risk factor for<br />
inadequate emergency department analgesia. Am J Emerg<br />
Med 1996;14:157–160.<br />
82. Petros JG, Alameddine F, Testa E, et al. Patient-controlled<br />
analgesia and postoperative urinary retention after hysterectomy<br />
for benign disease. J Am Coll Surg 1994;179:<br />
663–667.<br />
83. Petros JG, Mallen JK, Howe K, et al. Patient-controlled<br />
analgesia and postoperative urinary retention after open<br />
appendectomy. Surg Gynecol Obstet 1993;177:172–175.<br />
84. Carpenter RL, Abram SE, Bromage PR, Rauck RL. Consensus<br />
statement on acute pain management. Reg Anesth<br />
1996;21:152–156.<br />
85. Carpenter RL. Gastrointestinal benefits of regional anesthesia/analgesia.<br />
Reg Anesth 1996;21:13–17.<br />
86. Bates DW, Cullen DJ, Laird N, et al. Incidence of adverse<br />
drug events and potential adverse drug events: implications<br />
for prevention. ADE Prevention Study Group. JAMA<br />
1995;274:29–34.<br />
87. Polanczyk CA, Goldman L, Marcantonio ER, et al. Supraventricular<br />
arrhythmias in patients having noncardiac<br />
surgery: clinical correlates and effect on length of stay. Ann<br />
Intern Med 1998;129:279–285.<br />
88. Amar D, Roistacher N, Burt M, et al. Clinical and echocardiographic<br />
correlates of symptomatic tachydysrhythmias<br />
after noncardiac thoracic surgery. Chest 1995;108:349–354.<br />
89. Aranki SF, Shaw DP, Adams DH, et al. Predictors of atrial<br />
fibrillation following coronary artery bypass graft surgery:<br />
current trends and impact on hospital resources. Circulation<br />
1996;94:390–397.<br />
90. Mathew JP, Parks R, Savino JS, et al. Atrial fibrillation<br />
following coronary artery bypass graft surgery: predictors,<br />
outcomes, and resource utilization. JAMA 1996;276:300–<br />
306.<br />
91. Amar D, Zhang H, Leung DHY, et al. Older age is the<br />
strongest predictor of postoperative atrial fibrillation.<br />
<strong>Anesthesiology</strong> 2002;96:352–356.<br />
92. Moller JT, Cluitmans P, Rasmussen LS, et al. Long-term<br />
postoperative cognitive dysfunction in the elderly:<br />
ISPOCD1 study. Lancet 1998;351:857–861.<br />
93. Williams-Russo P, Sharrock NE, Mattis S, Szatowski TP,<br />
Charlson ME. Cognitive effects after epidural vs. general<br />
anesthesia in older adults. JAMA 1995;274:44–50.<br />
94. Dodds C, Allison J. Postoperative cognitive deficit in the<br />
elderly surgical patient. Br J Anaesth 1998;81:449–462.<br />
95. Monk TG, Garvin CW, Dede DE, van der Aa MT,<br />
Gravenstein JS. Predictors of postoperative cognitive
22. <strong>Anesthesia</strong> Considerations for <strong>Geriatric</strong> Outpatients 337<br />
dysfunction following major surgery [abstract]. <strong>Anesthesiology</strong><br />
2001;95:A50.<br />
96. Moller JT. Cerebral dysfunction after anaesthesia. Acta<br />
Anaesthesiol Scand 1997;110(Suppl):13–16.<br />
97. O’Keefe ST, Chonchubhair AN. Postoperative delirium in<br />
the elderly. Br J Anaesth 1994;73:673–687.<br />
98. Marcantonio ER, Juaraz G, Goldman L, et al. <strong>The</strong> relationship<br />
of postoperative delirium with psychoactive medication.<br />
JAMA 1994;272:1518–1522.<br />
99. Hanania M, Kitain E. Melatonin for the treatment and<br />
prevention of postoperative delirium. Anesth Analg 2002;<br />
94:338–339.<br />
100. Marcantonio ER, Flacker JM, Wright RJ, Resnick NM.<br />
Reducing delirium after hip fracture: a randomized trial. J<br />
Am Geriatr Soc 2001;49:516–522.<br />
101. Rasmussen LS, Larssen K, Houx P, et al. <strong>The</strong> assessment<br />
of postoperative cognitive dysfunction. Acta Anaesthesiol<br />
Scand 2001;45:275–289.<br />
102. Rasmussen LS, Johnson T, Kuipers HM, et al. Does<br />
anaesthesia cause postoperative cognitive dysfunction? A<br />
randomized study of regional versus general anaesthesia<br />
in 438 elderly patients. Acta Anaesthesiol Scand 2003;47:<br />
260–266.<br />
103. Canet J, Raeder J, Rasmussen LS, et al. for the ISPOCD2<br />
group. Cognitive dysfunction after minor surgery in<br />
the elderly. Acta Anaesthesiol Scand 2003;47:1204–<br />
1210.<br />
104. Inouye SK. Predisposing and precipitating factors for<br />
delirium in hospitalized older patients. Dement Geriatr<br />
Cogn Disord 1999;10:393–400.<br />
105. Inouye SK, Bogardus ST Jr, Charpentier PA, et al. A multicomponent<br />
intervention to prevent delirium in hospitalized<br />
older patients. N Engl J Med 1999;340:669–676.<br />
106. Tzabar Y, Asbury AJ, Millar K. Cognitive failure after<br />
general anaesthesia for day-case surgery. Br J Anaesth<br />
1996;76:194–197.<br />
107. Lichtor JL, Alessi R, Lane BS. Sleep tendency as a measure<br />
of recovery after drugs used for ambulatory surgery. <strong>Anesthesiology</strong><br />
2002;96:878–883.<br />
108. Johnson T. Postoperative cognitive dysfunction in middleaged<br />
patients. <strong>Anesthesiology</strong> 2002;96:1351–1357.<br />
109. Wu CL, Hsu W, Richman JM, Raja SN. Postoperative cognitive<br />
function as an outcome of regional anesthesia and<br />
analgesia. Reg Anesth Pain Med 2004;29:257–268.<br />
110. Chung F. Are discharge criteria changing? J Clin Anesth<br />
1993;5(Suppl):66S.<br />
111. Gold BS, Kitz DS, Lecky JH, Neuhaus JM. Unanticipated<br />
admission to the hospital following ambulatory surgery.<br />
JAMA 1989;262:3008–3010.<br />
112. Apfel CC, Läärä E, Koivuranta M et al. A simplified risk<br />
score for predicting postoperative nausea and vomiting:<br />
Conclusions from cross-validations between two centers.<br />
<strong>Anesthesiology</strong> 1999;91:693–700.<br />
113. Sinclair DR, Chung F, Mezei G. Can postoperative nausea<br />
and vomiting be predicted? <strong>Anesthesiology</strong> 1999;91:109–118.<br />
114. Wang LP, Fog J, Boe M. Transient hearing loss following<br />
spinal anaesthesia. Anaesthesia 1987;42:1258–1263.<br />
115. Gultekin S, Ozcan S. Does hearing loss after spinal anesthesia<br />
differ between young and elderly patients? Anesth<br />
Analg 2002;94:1318–1320.
Part IV<br />
<strong>Anesthesia</strong> for Common Surgical<br />
Procedures in the Aged
23<br />
Sedation and Monitoring<br />
Sheila R. Barnett<br />
Sedation is often required for patients undergoing minor<br />
procedures. <strong>The</strong> increased availability of newer medications<br />
with short duration, rapid onset, and minimal side<br />
effects has led patients and physicians to expect comfort,<br />
amnesia, and good “operating” conditions for a multitude<br />
of minimally invasive procedures. Given the increase in<br />
the elderly population, it is not surprising that there has<br />
also been a marked increase in procedures performed in<br />
extremely old patients. <strong>The</strong> skillful administration of<br />
sedation and analgesia for interventional procedures may<br />
allow these very elderly patients to avoid more invasive<br />
surgery and the consequent associated morbidity of<br />
surgery and prolonged hospitalization. 1<br />
What Is Meant by the Term Sedation?<br />
Both the American Society of Anesthesiologists (ASA)<br />
and the Joint Commission on Accreditation of Healthcare<br />
Organization describe four levels of sedation,<br />
from minimal or anxiolysis to general anesthesia 2,3<br />
(Table 23-1).<br />
Minimal sedation or anxiolysis refers to a controlled<br />
state of diminished consciousness wherein the ability to<br />
respond to moderate verbal stimuli and the ability to<br />
maintain a patent airway are retained. 4,5 <strong>The</strong>re is little<br />
impact on the cardiopulmonary status. Although this is<br />
popularly referred to as conscious sedation by many nonanesthesia<br />
specialties, the ASA task force recommends<br />
the use of sedation and analgesia rather than conscious<br />
sedation. 2<br />
Moderate sedation or analgesia is a drug-induced state<br />
during which a patient may be less responsive than with<br />
anxiolysis but still respond to verbal commands appropriately,<br />
although sometimes requiring simultaneous light<br />
tactile stimulation. Spontaneous respiration is maintained<br />
and cardiovascular parameters are unchanged.<br />
Deep sedation or analgesia is a drug-induced condition<br />
whereby the patient may be difficult to awaken but will<br />
respond purposefully to painful stimuli. With deep sedation,<br />
spontaneous respiration may not be adequate, and<br />
the patient may not be able to maintain a patent airway<br />
without assistance. Although controversial, in general,<br />
the ASA and many hospitals recommend the presence<br />
of anesthesia-trained personnel if deep sedation is<br />
anticipated or required to complete a procedure. 2 At<br />
a minimum, deep sedation requires the immediate availability<br />
of an individual trained in cardiopulmonary resuscitation<br />
and airway management.<br />
Sedation is a continuum of consciousness, and the<br />
practitioner providing sedation should be ready to<br />
respond appropriately to the next-higher level of sedation<br />
in addition to being comfortable at the current sedation<br />
level. This is particularly relevant when sedation is<br />
administered by nonanesthesiologists such as dental<br />
practitioners, radiologists, dermatologists, cardiologists,<br />
and gastroenterologists. 4,6–10<br />
Why Is Sedation a Particular Concern<br />
in Elderly Patients?<br />
<strong>The</strong> geriatric population is a heterogeneous group, and<br />
chronologic age does not always parallel physiologic age.<br />
Older patients present with multiple comorbidities,<br />
numerous medications, and less physiologic reserve. 5,11<br />
<strong>The</strong>y can be more sensitive to the sedative and depressant<br />
effects of the drugs used for sedation and are at<br />
increased risk from additive side effects when combinations<br />
of medications are administered. Although brief<br />
episodes of hypotension or desaturation may be insignificant<br />
in a young patient, the same episodes in an elderly<br />
frail patient may result in serious consequences, such as<br />
cardiac ischemia and arrhythmias 12 (Table 23-2).<br />
341
342 S.R. Barnett<br />
Table 23-1. Sedation depth.<br />
Minimal<br />
Moderate<br />
Deep<br />
Patient responds appropriately to normal-volume verbal<br />
cues, through voice or action. <strong>The</strong> response is<br />
immediate.<br />
Patient responds purposefully to verbal or light tactile<br />
stimulus. <strong>The</strong> response is either verbal or physical. For<br />
example, opening eyes, turning head in a given<br />
direction, appropriate change in position.<br />
<strong>The</strong> patient does not respond to either verbal or tactile<br />
stimulus, but responds appropriately to painful stimuli.<br />
Comorbid Conditions<br />
Elderly patients carry a large burden of disease: In a<br />
recent study examining preoperative health status in<br />
elderly patients, more than 84% of 544 patients had at<br />
least one comorbid condition, with 30% of patients having<br />
three or more preoperative health conditions and 27%<br />
with two. 11 Disability restricting mobility is also prevalent:<br />
73% of people older than 80 years have at least<br />
one disability. <strong>The</strong>se conditions have an impact on the<br />
delivery of sedation and may limit the options available<br />
for sedation.<br />
Cardiac conditions such as angina, hypertension, and<br />
congestive heart failure are all prevalent among elderly<br />
patients. 13–15 <strong>The</strong> high incidence of coronary artery disease<br />
places older patients at high risk for myocardial ischemia<br />
during awake procedures, especially if the procedure is<br />
painful and/or anxiety provoking and it proves difficult<br />
to relieve the pain/anxiety without resorting to unacceptable<br />
levels of sedation. Similarly, hemodynamic instability,<br />
particularly hypotension, is more likely in older<br />
patients because of their sensitivity to hypovolemia and<br />
the increased sympathetic tone that could be reduced by<br />
sedation. However, hypotension is not a likely result if<br />
stage II sedation is not exceeded. 2,16<br />
Age-related pulmonary changes 17 also affect the administration<br />
of sedation; changes in lung and chest wall compliance<br />
predispose the older patient to atelectasis with<br />
associated hypoxia that may not be amenable to treatment<br />
with supplemental oxygen. Hypercarbia may also<br />
develop and produce hypoxia (if not on supplemental<br />
oxygen) and may produce undesired hypertension and<br />
tachycardia.<br />
Table 23-2. Considerations for sedation in the elderly.<br />
1. Presence of multiple comorbidities: coronary disease, arrhythmias;<br />
prior cerebrovascular accidents<br />
2. Positioning challenges<br />
3. Chronic pain especially of the back and spine<br />
4. Prevalence of chronic hypoxia and the need for home oxygen<br />
5. Hearing and vision impairments that interfere with communication<br />
6. Dementia and cognitive dysfunction<br />
Renal disease may require alternations in medication<br />
dosing, and uremia can render patients very sensitive to<br />
the effects of sedation, especially the apneic side effects<br />
of narcotics. With the obesity epidemic in the United<br />
States, diabetes is becoming more prevalent and is very<br />
common in older patients. Glucose control can be problematic,<br />
and associated diabetic gastroparesis may result<br />
in a full stomach, even after 8 hours of fasting.<br />
Central nervous system aging renders older patients<br />
more sensitive to sedatives and analgesics, and patients<br />
with mild cognitive dysfunction are at particular risk for<br />
agitation and confusion with even small amounts of<br />
sedatives.<br />
Challenges Encountered During<br />
Administration of Sedation<br />
<strong>The</strong>re are certain issues that are uniquely relevant to<br />
elderly patients that may impinge on the sedation plan 5,18,19<br />
(Table 23-3).<br />
Positioning<br />
<strong>The</strong> accelerated loss of subcutaneous and intramuscular<br />
fat observed with aging may result in bony prominences<br />
that are at risk from skin breakdown and predispose<br />
elderly patients to accidental injury from seemingly<br />
benign positions. <strong>The</strong> loss of skin elasticity and slow<br />
healing further contribute to complex skin wounds<br />
and shearing injuries. Chronic pain, especially back pain,<br />
may limit the ability of an elderly patient to attain or<br />
maintain certain positions for long periods of time.<br />
Vertebrobasilar insufficiency may predispose an older<br />
patient to unexpected cerebral ischemia with neck extension;<br />
this may be particularly important if manipulation<br />
of the airway or neck is required. Cardiopulmonary<br />
compromise may occur secondary to positioning. For<br />
instance, the prone position or Trendelenburg may be less<br />
well tolerated in the elderly patient with significant<br />
cardiac disease.<br />
Table 23-3. Practical considerations for the administration of<br />
sedation in elderly patients.<br />
• Allow extra time to explore the preoperative history including<br />
medications and comorbidities.<br />
• Provide written instructions in large type.<br />
• Provide extra copy of instructions to caretaker if applicable.<br />
• Allow extra time for changing clothes at the beginning and end of<br />
the procedure.<br />
• Be prepared to provide additional assistance transferring to and<br />
from procedure table.<br />
• Postoperative recovery facilities with monitoring should be<br />
available in the event of a slow postoperative recovery.
23. Sedation and Monitoring 343<br />
Communication<br />
Diminished visual acuity, blindness, deafness, or impaired<br />
hearing make it more difficult to communicate during a<br />
procedure. Furthermore, many common procedures such<br />
as colonoscopies and endoscopies take place in a darkened<br />
endoscopy suite, further reducing the sensory input<br />
to the older patient. Any written information should be<br />
easy to read, and extra copies should be available for<br />
patient’s family, especially if the patient has any cognitive<br />
or communication issues.<br />
Table 23-5. General anesthesia recommendations.<br />
General anesthesia is recommended in patients who are:<br />
• Obtunded<br />
• Intoxicated<br />
• Septic<br />
• Have active hematemesis<br />
• Have significant cognitive impairment—e.g., dementia or are<br />
unable to cooperate secondary to confusion or anxiety<br />
• At high risk from aspiration—e.g., obesity, reflux, or ascites<br />
• Unable to lie still secondary to pain, confusion, or other medical<br />
conditions<br />
Administering Sedation<br />
More than 10 million gastrointestinal procedures are<br />
performed in the United States and Canada annually, 20<br />
and the volume of procedures conducted by gastroenterologists<br />
in the United States has increased almost twofold<br />
in the past 15 years. Individual endoscopists may perform<br />
between 9 and 15 esophagogastroduodenoscopies and 22<br />
colonoscopies per week. Colonoscopy is generally an<br />
unpleasant procedure associated with considerable<br />
discomfort. It is possible to perform colonoscopies with<br />
no sedation, but widespread use of sedation is well known<br />
to many patients, and most expect the option of safe<br />
sedation. 21,22 Endoscopic management of biliary disease<br />
in the elderly may be particularly advantageous, 23 and<br />
skillful administration of sedation is a vital component<br />
for these procedures, which may be complex and at times<br />
uncomfortable. 24,25<br />
Results from a survey of sedation practices among<br />
1500 gastroenterologists demonstrated that 98% of<br />
gastroenterologists routinely used sedation of some<br />
type, more than 70% routinely administered oxygen,<br />
almost 99% monitored blood pressure and saturation,<br />
whereas capnography remained relatively infrequent and<br />
was monitored in only 3% of respondents. With respect<br />
to drug administration, the endoscopist was responsible<br />
for making decisions regarding sedation doses in 78% of<br />
cases unless propofol was used, in which case anesthesia<br />
personnel were responsible in almost 70% of the<br />
cases. 20<br />
This section particularly addresses the issues of sedation<br />
with respect to gastroenterology procedures. 24,25 <strong>The</strong><br />
administration of sedation to an elderly patient involves<br />
Table 23-4. Predictors of difficult sedation.<br />
History of:<br />
Substance abuse<br />
Heavy alcohol use<br />
Chronic narcotic use<br />
Difficulty with previous sedation case<br />
Anticipated prolonged or complex procedure<br />
a preprocedure assessment and formulation of a plan,<br />
including monitoring, ensuring availability of resuscitative<br />
equipment, and an appropriate choice of drugs. 5,26,27<br />
Preprocedure Evaluation<br />
Before administering sedation, an assessment of the<br />
patient’s overall health including an estimate of the<br />
patient’s reserve function of major organ systems is<br />
needed. At a minimum, this should include a medical<br />
history, a comprehensive list of medications, and a brief<br />
physical examination including an airway assessment.<br />
One of the guiding principles for the successful administration<br />
of sedation is cooperation; preprocedure assessment<br />
should include an evaluation of the patient’s ability<br />
to cooperate at baseline. Patients who cannot cooperate<br />
because of dementia, sensory issues such as hearing or<br />
visual loss, or who are in extreme pain or disabled from<br />
arthritis and prior strokes and so on may not be suitable<br />
sedation candidates, and a deep sedation or a general<br />
anesthetic may be required. 2,5,24,25<br />
Sedation History<br />
A history of sedation and anesthesia is invaluable. Difficulties<br />
with prior procedures under sedation, substance<br />
and alcohol abuse, and extensive pain medication use<br />
have been shown to predict difficulty in sedation administration.<br />
In addition, technically difficult or lengthy procedures<br />
also predict difficulty with sedation. In these<br />
instances, it may be preferable to schedule elective procedures<br />
for deep sedation or general anesthesia 2,5,24,25<br />
(Tables 23-4 and 23-5).<br />
Consent<br />
<strong>The</strong> patient should understand and agree with the specific<br />
plan for sedation and the risks involved. When the patient<br />
is significantly disabled or dependent, it is important<br />
to involve caregivers early. Aside from consent issues<br />
in these patients, caregivers are likely to be needed in<br />
the postprocedure care of the patient. Frequently, the
344 S.R. Barnett<br />
surgical consent will include permission for sedation<br />
during the procedure, and separate consent for sedation<br />
is not always needed; however, specifics will depend on<br />
local administration and regulations within the hospital<br />
or facility.<br />
Preoperative Fasting Guidelines<br />
Both the ASA and the American Society for Gastrointestinal<br />
Endoscopy (ASGE) recommend restricting solid<br />
foods for 6–8 hours and allowing only clear liquids until<br />
2–3 hours before the procedures. In the elderly person,<br />
it is useful to establish who is receiving these instructions<br />
and who is responsible to enforce them. In the more<br />
frail or demented patient, adherence with fasting guidelines<br />
is particularly important because it can be difficult<br />
to predict the reaction to sedation and there may be a<br />
need for conversion to a deeper sedation or a general<br />
anesthesia. 24,25<br />
Monitoring<br />
Guidelines for monitoring have been developed by the<br />
ASA and ASGE. 28 At a minimum, all sedated patients<br />
must be monitored throughout the procedure for level of<br />
consciousness. Standard monitoring includes heart rate<br />
monitoring via pulse oximetry, noninvasive blood pressure<br />
at regular intervals, respiratory rate, and oxygen<br />
saturation, and in the elderly population, electrocardiography<br />
is also recommended. Postprocedure vital signs<br />
should also be monitored periodically during the recovery<br />
period until the effects of all medications have worn<br />
off and the patient is ready for discharge.<br />
<strong>The</strong> presence of a pacemaker requires the availability<br />
of a magnet if cautery is contemplated. Patients with a<br />
significant cardiac history, ongoing angina, congestive<br />
heart failure, or oxygen-dependent lung disease have<br />
almost no reserve function. <strong>The</strong>se patients may not be<br />
suitable candidates for sedation because they may require<br />
additional monitoring.<br />
Patients may maintain normal oxygen saturation<br />
despite significant hypoventilation and hypercapnia, and<br />
monitoring of ventilation is advisable whenever deep<br />
sedation is contemplated, especially during long procedures.<br />
Capnography 28 can be used to monitor ventilation<br />
and to detect early increases in carbon dioxide. However,<br />
the role for routine capnography is not clear and probably<br />
unnecessary in most instances of routine (nonpropofol)<br />
conscious sedation. Similarly, the bispectral index<br />
monitor has been used to assess the level of sedation in<br />
patients receiving propofol for sedation; however, the<br />
utility has yet to be determined. 29<br />
It should be recognized that clinical monitoring of the<br />
elderly patient may be more demanding than that of the<br />
younger patient. During the procedure, a dedicated individual<br />
should be able to supervise the patient. This individual<br />
should not be performing the procedure but rather<br />
should be continuously monitoring the patient for responsiveness,<br />
cooperation, and vital signs. Because by definition<br />
a sedated patient should be responsive at all times,<br />
communication with the patient is one of the most valuable<br />
monitoring methods.<br />
Emergency Resuscitation<br />
When administering sedation, emergency resuscitative<br />
equipment should be available, and those providing sedation<br />
should ideally be trained in basic and advanced life<br />
support. Minimal emergency equipment should include<br />
dedicated oral suction, oxygen, a bag-valve-mask device,<br />
an oral airway, and reversal agents. 30,31<br />
Oxygen<br />
Elderly patients with limited reserve function are predisposed<br />
to hypoventilation and hypoxemia; this may<br />
be exacerbated by cardiopulmonary and other diseases.<br />
Studies in gastroenterology have described episodes<br />
of desaturation during endoscopic and colonoscopic procedures<br />
in both sedated and nonsedated patients 32,33<br />
emphasizing the vulnerability of these patients. Supplemental<br />
oxygen provided via nasal cannula at 4 L/min has<br />
been successful in abolishing or attenuating episodes of<br />
desaturation. As stated, monitoring of ventilation is indicated<br />
because oxygen may mask the development of<br />
hypercapnia in sedated patients, especially those receiving<br />
supplemental narcotics. 2,24,28<br />
Medications<br />
Intravenous administration of medications is preferable<br />
to oral or intramuscular administration because it provides<br />
a more immediate effect and allows for more precise<br />
dosing. In addition, the presence of an intravenous line<br />
can be used to administer reversal or resuscitative drugs<br />
if needed. <strong>The</strong> time taken for the effect of a drug to peak<br />
can be slower in the elderly patient, and lengthening the<br />
interval between incremental doses in the older patient<br />
is recommended. Combinations of medications can allow<br />
a reduction in individual doses needed to produce the<br />
effect. However, in the older person, there is a potential<br />
for exaggerated effects; this can be minimized through<br />
dose reduction and interval extension. Some of the drugs<br />
used most frequently are combinations of midazolam,<br />
fentanyl, and meperidine. 3,20,24,25,30<br />
Midazolam is the preferred benzodiazepine: it has a<br />
fast onset, is short acting, and has few residual effects.<br />
In contrast, the longer-acting benzodiazepines such as<br />
diazepam and lorazepam may provide equally good sedative<br />
effects, but may result in prolonged sedation. 22,34,35
23. Sedation and Monitoring 345<br />
Advanced age is associated with an increased central<br />
sensitivity to midazolam, 36 and the doses recommended<br />
are an initial bolus of 0.5–1 mg followed by incremental<br />
doses of 0.25–0.5 mg during the procedure.<br />
<strong>The</strong> narcotics remifentanil, fentanyl, and meperidine<br />
are popular choices for sedation and are frequently combined<br />
with midazolam. Fentanyl is a relatively shortacting<br />
opioid that has been used for many years to provide<br />
sedation. As with all opioids, postoperative nausea is a<br />
risk, and this may preclude its use in certain instances.<br />
<strong>The</strong> respiratory depressant effects of fentanyl may be<br />
exaggerated by midazolam, and doses should be reduced<br />
when the combination is used. In the elderly, fentanyl<br />
doses range from 12.5 to 50 µg, titrating to effect and<br />
closely monitoring for respiratory depression. <strong>The</strong><br />
extreme short duration of remifentanil is particularly<br />
advantageous for infusions, although, as with other<br />
opioids, the risk of postoperative nausea may limit its<br />
value. 37 <strong>The</strong> combination of remifentanil and propofol<br />
may provide better sedation, pain relief, and toleration<br />
of colonoscopies compared with the administration<br />
of midazolam, fentanyl, and propofol. 35 However, the<br />
overall benefits of these and other combinations have not<br />
been adequately investigated at this point to make a<br />
single recommendation, and there are clearly multiple<br />
approaches to sedation that are acceptable. 37–39<br />
Meperidine is also popular for sedation in the younger<br />
generation, but in older patients it is best avoided because<br />
of its relatively long action, toxic metabolites, and the<br />
potential for central nervous system side effects.<br />
Dexmedetomidine is an alpha2 receptor agonist that<br />
has some significant advantages over the classic sedative<br />
choices. It is a relatively new agent currently approved<br />
for administration in the intensive care unit for sedation.<br />
A major advantage is the lack of respiratory depression<br />
with significant sedation and analgesia; however, it can<br />
cause significant hypotension. When compared with a<br />
propofol infusion, dexmedetomidine may cause slightly<br />
more hypotension and sedation, but it does have narcotic-sparing<br />
qualities that may be of value in frail elderly<br />
patients. <strong>The</strong> role of dexmedetomidine continues to be<br />
explored. 40,41<br />
Propofol<br />
Although in general the ASA discourages the use of propofol<br />
by nonanesthesia personnel, 2,30,35 propofol is clearly<br />
gaining popularity for sedation by nonanesthesiologists 23<br />
(Table 23-6). Advantages of propofol are its rapid action<br />
and fast clearance that make it an attractive choice for<br />
sedation. However, caution is required in elderly patients<br />
in whom administration may also result in abrupt hypotension<br />
and severe respiratory depression. One study<br />
investigated the recovery of psychomotor function in<br />
elderly compared with young patients after propofol<br />
Table 23-6. Administration of propofol for sedation: general<br />
recommendations.<br />
• <strong>Anesthesiology</strong>-trained personnel recommended for deep-sedation<br />
administration<br />
• Provision for a dedicated individual for the administration of<br />
sedating medication<br />
• Individuals administering propofol should:<br />
Be trained in advanced cardiac life support<br />
Have experience in airway management<br />
• Monitoring of vital signs is required<br />
• Emergency resuscitation equipment should be immediately<br />
available<br />
infusions. <strong>The</strong> authors compared 15 elderly patients,<br />
mean age 72 years, with 15 young patients, mean age 38.<br />
Both groups received continuous propofol infusions for<br />
approximately 140 minutes. Immediate recovery time to<br />
opening eyes was similar in each group, but the elderly<br />
patients had a much prolonged complete recovery of psychomotor<br />
function as tested using the Tieger’s dot test. 42<br />
Although the study numbers are small, this study emphasizes<br />
the potential for prolonged effects of medications<br />
in the elderly patient, even when the agent is regarded as<br />
of very short duration.<br />
Several protocols using propofol delivery have been<br />
developed by gastroenterology services with success. In<br />
these trials, low-dose propofol given by endoscopists provided<br />
a good level of low sedation and optimal operating<br />
environments for the procedure. It is important to note<br />
that in these studies individuals received specific training<br />
in propofol administration, and emergency equipment<br />
was extensive. 23,39<br />
In a survey conducted on gastroenterologists, propofol<br />
was used by about 25% of endoscopists, anesthesia providers<br />
were involved in 28% of endoscopies, and only<br />
7.7% of endoscopists reported using propofol themselves<br />
in their practices. In contrast, European studies suggest<br />
the use of propofol by endoscopists may be as high as<br />
34%. Interestingly, when questioned, more than 40% of<br />
endoscopists would choose propofol for their own procedure.<br />
<strong>The</strong> reasons they stated for preferring propofol was<br />
speed of onset and recovery, and satisfaction. 20<br />
Propofol for sedation is also popular among emergency<br />
room physicians where it is often the drug of choice for<br />
brief procedures such as cardioversions, fracture reductions,<br />
and dislocations. Overall, the role of propofol by<br />
nonanesthesiologists is still unresolved and varies substantially<br />
across the nation. 43–46<br />
Another new trend emerging in endoscopy studies is<br />
patient-controlled sedation (PCS). Lee et al. 47 randomized<br />
patients to receive either PCS or intravenous sedation.<br />
<strong>The</strong>y found that in general the incidence of<br />
hypotension was lower in the PCS group and the patients<br />
recovered faster. Although this is obviously not feasible<br />
in the demented or cognitively fragile elderly patient,
346 S.R. Barnett<br />
patient autonomy may lead to less medication usage and<br />
high satisfaction.<br />
Reversal Agents<br />
Although reversal issues are not unique to the elderly,<br />
it is advisable to have naloxone, a selective opioid reversal<br />
agent, and flumazenil, a benzodiazepine antagonist,<br />
immediately available if narcotics and benzodiazepines<br />
are being administered. Many elderly patients take<br />
chronic opioid therapy for pain, 5,15 and administration of<br />
naloxone should be done cautiously because it may result<br />
in a catecholamine surge and subsequent hypertension<br />
and tachycardia. <strong>The</strong> initial dose to reverse narcotic respiratory<br />
depression is frequently less than a full dose of<br />
0.4 mg; in the elderly patient, an even smaller initial dose<br />
may be sufficient. Flumazenil will reverse the sedative<br />
and psychomotor effects of midazolam but not any<br />
narcotic respiratory depression. Usually naloxone should<br />
be administered first if respiratory depression is the<br />
primary issue after combination therapy. Sedative protocols<br />
using routine reversal of benzodiazepines have<br />
been described but these have not been popular in the<br />
United States. 48,49<br />
Scheduling and Information<br />
<strong>The</strong> geriatric patient may have limited mobility and other<br />
issues that may result in the need for extra time to change<br />
and transfer from a chair to a stretcher. <strong>The</strong>refore, additional<br />
time in between cases and arrangements to help<br />
with dressing and so on should be allotted.<br />
All instructions should be written avoiding medical<br />
jargon and available in large easy-to-read print. In addition<br />
to preoperative instructions, written information<br />
should be given to patients and/or caregivers before discharge<br />
that clearly states what to expect postoperatively,<br />
whom to contact with questions, and how to arrange for<br />
emergency help if needed.<br />
Adverse Events<br />
Aspiration<br />
With advanced age, the pharyngeal reflexes are diminished,<br />
and elderly patients are at increased risk from<br />
aspiration. For this reason, fasting guidelines should be<br />
adhered to and the level of sedation kept to a minimum<br />
when possible. <strong>The</strong> age-related reduction in pharyngeal<br />
sensitivity compared with younger patients is an advantage<br />
when performing a simple upper endoscopy, and<br />
the elderly patient may not require any sedation. When<br />
sedation is required, aspiration risk is increased, and<br />
in the frail elderly patient aspiration can be a morbid<br />
event. 18,21<br />
Cardiopulmonary Events<br />
<strong>The</strong>se are the most serious of all adverse events and<br />
include hypoxemia, hypoventilation, arrhythmias, airway<br />
obstruction, and hypotension. Fortunately, the incidence<br />
of serious complications is uncommon: results from two<br />
large studies looking at more than 30,000 patients<br />
reported complication rates of 2–5 per 1000 patients. 19,20,50<br />
<strong>The</strong> complications ranged from mild hypoxemia to cardiac<br />
ischemia. More recently, Rodriguez-Gonzzalez et al. 1<br />
looked retrospectively at 159 ERCPs (range 1–5 per<br />
patient) performed in patients over the age of 90 years<br />
at their institution. This included 126 very elderly patients<br />
with a mean age of 92 years, ranging from 90 to 101 years;<br />
some had more than one procedure. Forty-two percent<br />
of patients had significant chronic conditions—mostly<br />
diabetes mellitus and coronary artery disease. All<br />
patients underwent a procedure performed under local<br />
pharyngeal anesthesia, and 99% received supplemental<br />
intravenous sedation. <strong>The</strong> most frequently administered<br />
medication was midazolam, which was given in 96% of<br />
patients; meperidine was administered in 4%. In addition,<br />
hyoscine-N-butylbromide was given in 75% and glucagon<br />
in 25% of patients. Overall, the procedures were well<br />
tolerated in 92% of patients, and no patient experienced<br />
a direct complication from the sedation. <strong>The</strong> procedure<br />
was suspended for anatomic reasons in only nine or<br />
5.7% of cases. Four patients went to surgery subsequently<br />
because of inadequate endoscopic interventions and<br />
all four died postoperatively. Although this was an unusually<br />
healthy group of 90-year-olds, this study supports<br />
the importance of skillful sedation. It is evident from the<br />
data that the mortality with biliary surgery can be high<br />
in very elderly patients, and avoidance of a surgery may<br />
be beneficial. 1,23<br />
Elderly patients can become significantly dehydrated<br />
easily, especially in hot climates or if they are taking<br />
diuretic and antihypertensive medications. Patients that<br />
have had fluid restricted or received bowel preparations<br />
may demonstrate significant orthostatic hypotension<br />
when standing up for the first time after a procedure, so<br />
care should be taken when getting these patients up to<br />
ambulate. A careful plan for postoperative hydration<br />
should be discussed with the patient and the caretaker.<br />
Hypoxemia<br />
Hypoxia is more common in individuals receiving a combination<br />
of medications such as midazolam and fentanyl<br />
or midazolam and meperidine. Longer procedures such<br />
as endoscopic retrograde cholangiopancreatographies<br />
(ERCPs) are also more likely to be associated with<br />
hypoxic episodes, and supplemental oxygen is recommended.<br />
As discussed above, hypoventilation may be<br />
underappreciated, especially in long procedures in<br />
patients with chronic obstructive pulmonary disease,
23. Sedation and Monitoring 347<br />
dementia, and in patients receiving combined sedation<br />
with benzodiazepines and narcotics. In these instances,<br />
monitoring of end-tidal carbon dioxide may be merited,<br />
but this is not universally available or clearly stated in<br />
any guidelines. 5,24,25<br />
Summary<br />
In general, administration of sedation to elderly patients<br />
undergoing minimally invasive procedures is safe.<br />
Eye Surgeries in the Elderly<br />
Cataract extraction is a classic example of an invaluable<br />
surgery performed with minimal sedation. One and a half<br />
million cataract surgeries are performed annually in the<br />
United States, and the annual Medicare expenditure is in<br />
excess of $3.4 billion. 51,52 In general, these are very lowrisk<br />
outpatient surgeries, 53 but the complications related<br />
to the procedure can be devastating and may result in<br />
significant visual disability and even blindness. 54 An anesthesia<br />
care provider is frequently involved in the sedation<br />
and monitoring of these cases. 55<br />
Cataracts<br />
More than 20 million people (17.5%) over age 40 years<br />
have a cataract in at least one eye, and 6.1 million (5%)<br />
have pseudoaphakia/aphakia (prior cataract surgery) in<br />
the United States. By 2020, it is estimated that 30 million<br />
Americans will have a cataract and 9.5 million pseudophakia/aphakia.<br />
56,57 <strong>The</strong> majority of cataracts in the<br />
United States are senile or age-related cataracts and a<br />
major cause of blindness. <strong>The</strong> exact pathogenesis of cataracts<br />
is not completely understood; however, the current<br />
evidence suggests that a photoxidative mechanism has a<br />
major role. <strong>The</strong> normal crystalline lens is composed of a<br />
very complex structure consisting of specialized cells<br />
arranged in a highly ordered manner; the high content of<br />
the cytoplasmic protein provides the transparency critical<br />
to the functioning lens. During aging, the epithelial cells<br />
are not shed as they are in other structures, and there is<br />
a gradual buildup of protein and pigment, forming the<br />
basis of the cataract. Risk factors include aging, smoking,<br />
alcohol consumption, sunlight, low education, and diabetes<br />
mellitus. 58<br />
Table 23-7. Most common causes of blindness.<br />
1. Cataract<br />
2. Macular degeneration<br />
3. Glaucoma<br />
4. Diabetes mellitus<br />
Table 23-8. Causes of cataracts.<br />
1. Aging<br />
2. Smoking<br />
3. Alcohol<br />
4. Sunlight exposure<br />
5. Diabetes mellitus<br />
6. Steroids<br />
Nuclear cataracts are the type that usually occurs<br />
with aging and may themselves cause further eye problems<br />
such as glaucoma. Phacolytic glaucoma occurs when<br />
a mature cataract liquefies and leaks out of the capsule<br />
into the anterior chamber, resulting in inflammation and<br />
clogging of the trabecular network with subsequent<br />
increased intraocular pressure. Phacomorphic glaucoma<br />
occurs when large cataracts push forward resulting in a<br />
narrowing of the angle and subsequent narrow-angle<br />
glaucoma. 55,58<br />
<strong>The</strong> only known treatment for cataracts at this time<br />
is surgery, and fortunately, 90% of patients undergoing<br />
first-time cataract surgery have improved visual acuity<br />
and satisfaction at 4-month follow-up 59–61 (Tables 23-7<br />
and 23-8).<br />
Modern Cataract Surgery<br />
All cataract surgery involves removal of the cataract;<br />
key advances in the field have been the development of<br />
small foldable implantable lenses and the development<br />
of phacoemulsification techniques. Nowadays, patients<br />
can be in and out of the hospital within a few hours<br />
and experience immediate improvement of sight 59,60,62–65<br />
(Table 23-9).<br />
Intracapsular cataract extraction (ICCE) refers to the<br />
total extraction of the opacified lens and the capsule; a<br />
new lens is then inserted into the anterior chamber. This<br />
technique is less common nowadays, although it may still<br />
be used for selected complex cases. Extracapsular cataract<br />
extraction (ECCE) refers to the procedure during<br />
which the lens is removed but the capsule is left intact.<br />
This procedure is more technically challenging but advantageous<br />
because the capsule supplies support for the<br />
implantable lens. Both ICCE and ECCE procedures<br />
require relatively large incisions. 62–64<br />
Table 23-9. Complications of cataract surgery.<br />
1. Astigmatism<br />
2. Wound leak or dehiscence<br />
3. Prolapsed iris<br />
4. Flat anterior chamber<br />
5. Expulsive rupture of choroidal vessels<br />
6. Strabismus
348 S.R. Barnett<br />
Today, the most popular approach to cataract extraction<br />
in the United States is phacoemulsification. 62 Under<br />
an operating microscope, ultrasonically driven oscillating<br />
needles are inserted through a tiny incision and used to<br />
emulsify the lens. At the same time, a continuous irrigation/aspiration<br />
system is used to remove the tiny pieces<br />
of shattered opacified lens. Foldable implantable lenses<br />
are inserted through the small incision. <strong>The</strong>se tiny incisions<br />
frequently do not require sutures for closure, allowing<br />
for a rapid surgery and recovery. Occasionally, mature<br />
cataracts are extremely hard and difficult to break<br />
up using standard phacoemulsification techniques; in<br />
these instances, the procedure may be prolonged or<br />
alternative techniques such as ICCE or ECCE may be<br />
required. 53,62,65,66<br />
Indications for Surgery<br />
Not all cataracts require immediate surgery. <strong>The</strong> key indication<br />
for surgery is visual impairment accompanied by<br />
deterioration in general function secondary to failing<br />
eyesight, and a promising surgical prognosis for recovery<br />
of vision. Generally, prognosis depends on the presence<br />
or absence of other ocular comorbidities, such as glaucoma<br />
or retinopathy. Phacomorphic glaucoma and followup<br />
of diabetic retinopathy through regular funduscopic<br />
examinations are other indications for cataract extraction.<br />
In older patients, even those with dementia, correction<br />
of vision may improve quality of life and allow for<br />
more independence. 67,68<br />
Preoperative Evaluation for Cataract Surgery<br />
As stated, cataract surgery is very low risk, especially as<br />
many surgeons are now performing these surgeries using<br />
phacoemulsification techniques under topical anesthesia<br />
with minimal sedation. Unfortunately, the preoperative<br />
assessment in these patients can still be problematic<br />
because patients have complicated histories and multiple<br />
illnesses. <strong>The</strong> preoperative assessment will need to identify<br />
patients that may need additional anesthesia, such as<br />
those with unstable medical conditions or conditions that<br />
may prohibit the patient from lying still during the procedure<br />
such as severe cardiopulmonary disease. 69,70<br />
<strong>The</strong> value of preoperative laboratory testing has been<br />
questioned, and a recent prospective trial evaluated more<br />
than 18,000 cataract patients who were randomly assigned<br />
to either the preoperative routine testing group or the<br />
no-testing group. 69 At the time of the preoperative assessment,<br />
the testing group received routine tests including<br />
blood count and chemistries. In contrast, the no-testing<br />
group only underwent testing if there was a change in<br />
their medical history or physical examination that suggested<br />
the need for testing at the time of the visit. After<br />
the procedure, there was no difference in the surgical<br />
complications and the postoperative or intraoperative<br />
events in either group, which was approximately 31.3<br />
events per 1000 patients. <strong>The</strong> authors suggested that<br />
routine laboratory testing was not indicated; however, it<br />
is important to recognize that all patients did receive a<br />
preoperative history and physical examination. In general,<br />
a history and physical examination before cataract<br />
surgery, possibly as part of a routine physical visit, are<br />
beneficial because these patients have complex medical<br />
histories. In most instances, a baseline electrocardiogram<br />
within 6–12 months is also recommended in the event of<br />
a dysrhythmia or other cardiac event during the case.<br />
Anticoagulation and Cataract Surgery<br />
Controversy surrounds the relative risks of discontinuing<br />
anticoagulant or antiplatelet medications for cataract<br />
surgery versus continuing these medications. Several<br />
studies have not found any increase in hemorrhagic complications<br />
when aspirin or warfarin are continued during<br />
cataract surgery. 71–75 A more recent, large cohort study 33<br />
in 2003 examined the impact of continuing or discontinuing<br />
aspirin or warfarin in patients undergoing cataract<br />
surgery in the United States and Canada. 74 Data on more<br />
than 19,000 patients undergoing cataract surgery were<br />
included. Twenty-four percent (4517) of patients took<br />
aspirin, and 4% were taking warfarin or warfarin and<br />
aspirin. A small percentage of patients (22.5%) discontinued<br />
aspirin for 2 weeks, and 28% had stopped warfarin<br />
4 days before surgery. <strong>The</strong> incidence of adverse events<br />
was extremely low in all cases. <strong>The</strong>re was no difference<br />
in the incidence of thrombotic events in individuals who<br />
continued aspirin (1.49/1000 surgeries) versus those who<br />
discontinued aspirin (1/1000 surgeries). Similarly, there<br />
was no increase in ocular hemorrhage between patients<br />
who continued or discontinued warfarin.<br />
It is likely from the available evidence that anticoagulant<br />
and antiplatelet medication can be continued safely<br />
during the perioperative period. <strong>The</strong> decision to withhold<br />
the medication should take into account the reason the<br />
patient is taking the medication, the type of anesthesia<br />
planned (local versus regional), and whether the patient<br />
is monocular or not. <strong>The</strong> decision should be made in<br />
conjunction with the patient’s primary physician. If a<br />
decision to stop the anticoagulants is agreed upon, there<br />
should be a clear timeline for the postoperative reinstatement<br />
of the medications, including who is responsible for<br />
follow-up.<br />
<strong>Anesthesia</strong> for Cataract Surgery<br />
Recent surveys suggest that local and intracameral anesthesia<br />
are the preferred anesthetic techniques, although<br />
there are areas in this country and the world where<br />
regional techniques are still routinely used 65,76–78 (Table<br />
23-10). This section describes the different types of anesthesia<br />
as well as the relative merits of each approach.
23. Sedation and Monitoring 349<br />
Table 23-10. Common anesthetic options for cataract surgery.<br />
1. Retrobulbar block<br />
2. Peribulbar block<br />
3. Sub-Tenon’s block<br />
4. Topical anesthesia<br />
5. Topical anesthesia with intracameral injection<br />
<strong>Regional</strong> Orbital <strong>Anesthesia</strong><br />
<strong>Regional</strong> anesthesia for eye surgery provides dense ocular<br />
anesthesia and akinesia; this may be advantageous in<br />
complex or prolonged cases. Retrobulbar and peribulbar<br />
blocks are the most common regional techniques de -<br />
scribed. 79 <strong>The</strong> successful regional block requires a block<br />
of the optic nerve and the ciliary ganglion. Blockade of<br />
the ciliary ganglion results in a fixed, mid-position pupil.<br />
<strong>The</strong> surgery may also require paralysis of the orbicularis<br />
oculi muscle to prevent blinking; this muscle is innervated<br />
by the seventh fascial nerve.<br />
Retrobulbar and Peribulbar <strong>Anesthesia</strong><br />
<strong>The</strong> retrobulbar and peribulbar blocks are similar. <strong>The</strong><br />
retrobulbar block involves the injection of local anesthetic<br />
agent behind the orbit within the muscular cone.<br />
<strong>The</strong> needle is introduced at the junction of the lateral and<br />
middle two thirds of the lower lid above the inferior<br />
orbital rim. As the needle pierces the orbital septum, it<br />
remains parallel to the orbit floor; after reaching the<br />
globe equator, the needle is redirected upward to the<br />
apex of the orbit. <strong>The</strong> operator may feel a pop as the<br />
needle traverses the bulbar fascia, entering the muscle<br />
cone. Between 2 to 4 mL of local anesthetic is injected<br />
inside the cone of muscles, close to the optic nerve. During<br />
the injection, an awake patient is instructed to look<br />
straight ahead (a primary gaze), minimizing the chance<br />
of an intraneural injection. <strong>The</strong> peribulbar block is very<br />
similar; the needle is introduced as described for the retrobulbar<br />
block. However, the needle is kept parallel and<br />
lateral to the rectus muscle, and no effort is made to enter<br />
the bulbar fascia. As the needle reaches the equator, the<br />
local anesthetic is injected, i.e., around the muscle cone,<br />
not inside. For the peribulbar block, a larger volume of<br />
anesthetic is required to allow diffusion—generally 4–<br />
6 mL. Additionally, it may take closer to 20 minutes to<br />
achieve the desired anesthesia. <strong>The</strong> peribulbar block may<br />
be accompanied by a second injection of 3–5 mL of local<br />
anesthetic injected medially in the superomedial orbit. A<br />
blunt-tipped needle of less than 31 mm in length is recommended<br />
to reduce the chance of a globe or neural<br />
puncture. 76–79<br />
Sub-Tenon’s block is a combination block. Topical<br />
anesthesia is applied to the conjunctiva, and one quadrant<br />
of the sclera is exposed to reveal Tenon’s capsule<br />
surrounding the sclera. A blunt catheter or needle is<br />
inserted into the sub-Tenon’s space, and local anesthetic<br />
is infused. This provides excellent anterior anesthesia, but<br />
topical anesthesia is required for the cornea and conjunctiva.<br />
<strong>The</strong>re is a small risk of global puncture with this type<br />
of injection, but in general, complications are lower than<br />
those described for retrobulbar blocks. 76,79<br />
Monitoring and Sedation<br />
During the placement of the orbital block, the patient’s<br />
electrocardiogram, blood pressure, and oxygen saturation<br />
should be monitored. 80 It is important that the patient<br />
remains still during the injection, and this may be achieved<br />
by the administration of short-acting sedative medication<br />
accompanied by supplemental oxygen. Multiple drug<br />
regimens have been described, and low-dose propofol<br />
(30–50 mg) is probably the medication of choice, offering<br />
excellent conditions with few side effects and a short<br />
duration. 81–83 Midazolam is also frequently used, but, as a<br />
solo agent, may not provide a deep enough plane of sedation<br />
to prevent movement during the injection. Shortacting<br />
narcotics can be used but most prefer to avoid<br />
narcotics because of an increased risk of postoperative<br />
nausea and vomiting. 84 Combinations of a benzodiazepine,<br />
such as midazolam, and ketamine may result in<br />
improved patient cooperation, 85 but it is not clear if there<br />
are true advantages over low-dose propofol. <strong>The</strong> role for<br />
dexmedetomidine in cataract surgery has yet to be established.<br />
A recent double-blind study comparing the use of<br />
midazolam to dexmedetomidine for sedation in cataract<br />
surgery under peribulbar block found that patient satisfaction<br />
was slightly higher with dexmedetomidine. This<br />
advantage was offset by greater reductions in blood pressure<br />
and longer recovery time with delayed discharge<br />
compared with the midazolam group. 40<br />
In contrast to the requirements for block place -<br />
ment, minimal sedation during the case is generally<br />
sufficient, and short-acting anxiolysis with midazolam is<br />
the most popular choice. Various protocols have been<br />
described including patient-controlled administration<br />
of propofol. 86,87 However, the data so far do not show<br />
any particular advantage, and indeed the combination of<br />
midazolam and propofol often resulted in undesirable<br />
head movement. Furthermore, any sedation must be<br />
balanced against the potential downside of disorienta -<br />
tion and lack of cooperation in the patient during the<br />
procedure.<br />
Side Effects and Complications of<br />
Intraorbital <strong>Anesthesia</strong><br />
Complications from intraorbital anesthesia are uncommon<br />
but the effects may be devastating, resulting in<br />
permanent visual damage or blindness (Table 23-11).<br />
Although the overall complication rate is less than 0.5%,<br />
this still has the potential to affect thousands of patients
350 S.R. Barnett<br />
Table 23-11. Complications of retrobulbar anesthesia.<br />
1. Retrobulbar hemorrhage<br />
2. Globe perforation<br />
3. Neural injection of optic nerve<br />
4. Vascular injection<br />
5. Central retinal artery or vein occlusion<br />
6. Brainstem anesthesia<br />
because of the huge number of patients undergoing<br />
cataract surgery. <strong>The</strong> most significant adverse events are<br />
described below.<br />
Orbital hemorrhage occurs in 0.1%–1.7% of retrobulbar<br />
and 0.072% of peribulbar blocks. Hemorrhage occurs<br />
as a result of the inadvertent puncture of the ophthalmic<br />
artery as it crosses the optic nerve. Immediate signs of<br />
hemorrhage include proptosis, subconjunctival hemorrhage,<br />
and increased orbital pressure. Initial treatment is<br />
direct intermittent pressure to the eye. If the globe relaxes<br />
back (retropulsion) and intraocular pressure is normal,<br />
cataract surgery may be continued. If increased intraocular<br />
pressure or proptosis persists, then a lateral canthotomy<br />
is performed. Retinal perfusion should be confirmed<br />
using the ophthalmoscope. If the intraocular pressure<br />
remains increased despite a patent canthotomy, then<br />
aqueous suppressants may be added.<br />
Globe perforation is most common with a retrobulbar<br />
block, but may also occur during a peribulbar or sub-<br />
Tenon’s block; the incidence varies from 0% to 0.75% of<br />
blocks performed. Major risk factors for perforation<br />
include inexperience by the operator and staphyloma of<br />
the eye. <strong>The</strong> visual damage after a globe perforation will<br />
depend on the presence or absence of a retinal detachment<br />
and vitreous hemorrhage 58,76 (Table 23-12).<br />
Optic nerve damage is very rare after a retrobulbar<br />
injection.<br />
Central Nervous System Complications<br />
<strong>The</strong> optic nerve sheath communicates directly with cerebrospinal<br />
fluid, and inadvertent injection of local anesthesia<br />
into the sheath may result in immediate brainstem<br />
anesthesia. Similarly, intraarterial injection of local anesthesia<br />
may cause central nervous system toxicity and seizures.<br />
Acute vascular injury may result from damage to<br />
the central retinal artery or vein; this may lead to significant<br />
injury.<br />
Topical <strong>Anesthesia</strong> for Ocular Surgery<br />
Topical anesthesia, mostly with lidocaine or tetracaine<br />
eye drops, has become very popular with surgeons<br />
and patients. 53,88 In a survey from 1999, the American<br />
Society of Cataract and Refractive Surgery found that<br />
topical anesthesia was used by 45% of respondents.<br />
Caseload was a factor contributing to choice. Surgeons<br />
performing five or fewer cases per month favored regional<br />
anesthesia, whereas surgeons performing more than<br />
50 cases per month preferred topical anesthesia. Eightyone<br />
percent of surgeons using local anesthesia used<br />
a combination of topical and intracameral injection, 82<br />
which involves a small incision and installation of local<br />
anesthesia into the anterior chamber. <strong>The</strong> intracameral<br />
injection reduces the discomfort during manipulation<br />
of the lens. Some patients may still require small<br />
amounts of midazolam or similar medications during the<br />
surgery. 80,89,90<br />
Advantages of Topical <strong>Anesthesia</strong><br />
<strong>The</strong>re are several advantages to topical anesthesia (Table<br />
23-13). <strong>The</strong> patient avoids the risk of retrobulbar hemorrhage<br />
and other complications, is able to see immediately,<br />
and the postoperative recovery is very speedy. Even<br />
complex cataract surgery may be performed under topical<br />
anesthesia. Jacobi et al. 88 found that surgical complications<br />
in complex surgeries were not different between<br />
patients receiving topical versus retrobulbar anesthesia.<br />
Patient satisfaction with the different techniques has<br />
been questioned. In the study on complex surgeries,<br />
Jacobi et al. found greater patient satisfaction for topical<br />
over retrobulbar anesthesia (p = 0.01). However, Boezaart<br />
et al. 78 questioned elderly patients (mean age 71 years)<br />
having cataract surgery and found that 70% of patients<br />
preferred the block over the local anesthetic. Interestingly,<br />
98% did not remember the insertion of the block,<br />
a positive benefit of sedation with the block. In general,<br />
patient satisfaction is high with both techniques; how -<br />
ever, the rapid postoperative recovery ultimately makes<br />
the topical approach very appealing to patients and<br />
physicians.<br />
<strong>The</strong> Role of the Anesthesiologist<br />
Several surveys have provided conflicting data on the<br />
need for an anesthesiologist during cataract surgeries.<br />
Table 23-12. Factors increasing risk of globe rupture.<br />
• Uncooperative patient<br />
• Long eye axial length >26 mm<br />
• Staphyloma<br />
• Long needle used for the block<br />
Table 23-13. Advantages of topical versus regional block.<br />
1. Eliminates risk of retrobulbar hemorrhage<br />
2. Reduces risk to the optic nerve and other structures<br />
3. Minimizes risk of strabismus postoperatively<br />
4. Very short recovery time with immediate sight
23. Sedation and Monitoring 351<br />
Rosenfield et al., 80 in a study of 1006 patients, found that<br />
in one third of cases an intervention by an anesthesia<br />
team was required and that the need for an intervention<br />
was unpredictable. <strong>The</strong> lack of predictability is perhaps<br />
one of the strongest arguments for anesthesia involvement.<br />
<strong>The</strong> International Cataract Surgery Outcomes<br />
Study surveyed ophthalmologists in the United States,<br />
Canada, Denmark, and Spain from 1993 to 1994. 90 <strong>The</strong>y<br />
found that in the United States 78% of surgeons used<br />
phacoemulsification for the cataract removal. In this<br />
survey, they found only 14% used topical for the anesthesia,<br />
46% used retrobulbar, and 38% used peribulbar<br />
blocks. Most blocks (79%) were performed by the surgeon,<br />
although in 78% of cases an anesthesiologist was<br />
present. All patients were monitored: 97% with electrocardiogram,<br />
blood pressure, and oxygen saturation. <strong>The</strong><br />
low rate of topical anesthesia may reflect the sampling<br />
era because more recent results support topical anesthesia.<br />
Furthermore, the international study had a high rate<br />
of anesthesia involvement. In an in-depth analysis of<br />
anesthesia management during cataract surgery, Reeves<br />
et al. 91 found preferences for an anesthesiologist, sedation,<br />
and a block for the surgery. However, these results<br />
were highly dependent on the selection of a relatively<br />
small expert panel. In contrast, the results of more recent<br />
surveys of ophthalmologists favor topical anesthesia.<br />
Thus, although not universal, anesthesiologists are still<br />
frequently involved in monitoring the patient during the<br />
cataract surgery.<br />
Special Situations<br />
<strong>The</strong>re are some special circumstances in the elderly<br />
patient that may require alternative approaches. For<br />
instance, demented or uncooperative patients may require<br />
more sedation or even general anesthesia. Chronic pain<br />
patients may be unable to lie flat and be tolerant of medications.<br />
Occipital pain has been described during the procedure<br />
necessitating additional medications. In patients<br />
with significant cardiopulmonary disease, supplemental<br />
oxygen may be required during the case, and several<br />
instances of hypercapnia have been described. 92,93 <strong>The</strong><br />
anesthesiologist should be prepared to respond to the<br />
variable needs of this population.<br />
Postoperative<br />
A cataract extraction is an outpatient procedure. Patients<br />
generally follow up with the ophthalmologist the next<br />
day. All patients should receive instructions from the<br />
ophthalmologist’s office before discharge. In patients<br />
receiving blocks, an eye patch is common, and vision will<br />
take longer to return. 94 <strong>The</strong>se patients may require additional<br />
help at home during convalescence.<br />
Conclusions<br />
Elderly patients should be offered the opportunity to<br />
undergo procedures and simple surgeries under sedation<br />
with minimal risk. Skillful administration of sedation may<br />
help avoid more morbid and complex surgeries and<br />
improve outcomes. Sedation in the older patient is safe,<br />
but requires additional vigilance and patience.<br />
References<br />
1. Rodriguez-Gonzzalez FJ, Naranjo-Rodriguez A, Mata-<br />
Tapia I, Chicano-Gallardo M, Puente-Gutierrez JJ, López-<br />
Vallejos P. ERCP in patients 90 years of age and older.<br />
Gastrointest Endosc 2003;58:220–225.<br />
2. Practice Guidelines for Sedation and Analgesia by Non<br />
Anesthesiologists. Task force on sedation and analgesia.<br />
<strong>Anesthesiology</strong> 1996;84:459–471.<br />
3. Gullo A. Sedation and anesthesia outside the operating<br />
room: definitions, principles, critical points and recommendations.<br />
Minerva Anestesiol 2005;71:1–9.<br />
4. Arepally A, Oechsle D, Kirkwood S, Savader SJ. Safety of<br />
conscious sedation in interventional radiology. Cardiovasc<br />
Intervent Radiol 2001;24:185–190.<br />
5. Modifications in endoscopic practice for the elderly. Gastrointest<br />
Endosc 2000;52(6):849–851.<br />
6. Calderini E. Recommendation for anesthesia and sedation<br />
in non-operating room locations. Minerva Anestesiol 2005;<br />
71:11–20.<br />
7. Manninen PH, Chan ASH, Papworh D. Conscious sedation<br />
for interventional neuroradiology: a comparison of midazolam<br />
and propofol infusion. Can J Anaesth 1997;44:<br />
26–30.<br />
8. Otley CC, Nguyen TH. Safe and effective conscious<br />
sedation administered by dermatologic surgeons. Arch<br />
Dermatol 2000;136:1333–1335.<br />
9. Parlak M, Parlak I, Erdur B, Ergin A, Sagiroglu E. Age<br />
effect on efficacy and side effects of two sedation and analgesia<br />
protocols on patients going through cardioversion:<br />
a randomized clinical trial. Acad Emerg Med 2006;13:<br />
493–499.<br />
10. Jackson DL, Johnson BS. Conscious sedation for dentistry:<br />
risk management and patient selection. Dent Clin North<br />
Am 2002;46:767–780.<br />
11. Leung JM, Dzankic S. Relative importance of preoperative<br />
health status versus intraoperative factors in predicting<br />
postoperative adverse outcomes in surgical patients. J Am<br />
Geriatr Soc 2001;49:1080–1085.<br />
12. Oei-Lim VL, Kalkman CJ, Bartelsman JF, Res JC,<br />
van Wezel HB. Cardiovascular responses, arterial saturation<br />
and plasma catecholamines concentration during upper<br />
gastrointestinal; endoscopy using conscious sedation with<br />
midazolam or propofol. Eur J Anaesthesiol 1998;15:<br />
535–543.<br />
13. Elveback LR, Connolly DC, Melton LJ. Coronary heart<br />
disease in residents of Rochester, Minnesota. VII. Incidence<br />
1950–1982. Mayo Clin Proc 1986;61:896–900.<br />
14. Gerstenblith G, Fleg JL, Van Tosh A, Weisfeldt M, Lakatta<br />
EG. Stress testing redefines the prevalence of coronary
352 S.R. Barnett<br />
artery disease in epidemiologic studies. Circulation 1980;<br />
62:111–308.<br />
15. Muravchik S. Geroanesthesia: Principles for Management<br />
of the Elderly Patient. St. Louis, MO: Mosby-Year Book;<br />
1997.<br />
16. Christe C, Janssens JP, Armenian B, Herrmann F, Vogt N.<br />
Midazolam sedation for upper gastrointestinal endoscopy<br />
in older persons: a randomized, double blind, placebocontrolled<br />
study. J Am Geriatr Soc 2000;48:1398–<br />
1403.<br />
17. Smetana G. Preoperative pulmonary evaluation. N Engl<br />
J Med 1999;340:937–944.<br />
18. Clarke GA, Jacobson BC, Hammett RJ, Carr-Locke DL.<br />
<strong>The</strong> indications, utilization and safety of gastrointestinal<br />
endoscopy in an extremely elderly patient cohort. Endoscopy<br />
2001;33(7):580–584.<br />
19. Waring J, Baron T, Hirota W, Goldstein J, Jacobson B, Leighton<br />
J, et al. Guidelines for conscious sedation and monitoring<br />
during gastrointestinal endoscopy. American Society<br />
for Gastrointestinal Endoscopy. Gastrointest Endosc 2003;<br />
58(3):317–322.<br />
20. Cohen LB, Wecsler JS, Gaetano JN, Benson AA, Miller KM,<br />
Durkalski V, et al. Endoscopic sedation in the United States:<br />
results form a nationwide survey. Am J Gastroenterol<br />
2006;101:967–974.<br />
21. Lukens FJ, Loeb DS, Machicao VI, Achem SR, Picco MF.<br />
Colonoscopy in octogenarians: a prospective outpatient<br />
study. Am J Gastroenterol 2002;97:1722–1725.<br />
22. Morrow JB, Zuccaro G, Conwell DL, Vargo JJ, Dumot JA,<br />
Karafa M, et al. Sedation for colonoscopy using a<br />
single bolus is safe, effective and efficient: a prospective,<br />
randomized double blind trial. Am J Gastroenterol<br />
2000;95:2242–2247.<br />
23. Heuss LT, Schnieper P, Drewe J, Pflimlin E, Beglinger C.<br />
Safety of propofol for conscious sedation during endoscopic<br />
procedures in high risk patients—a prospective controlled<br />
study. Am J Gastroenterol 2003;98:1751–1757.<br />
24. Sedation and monitoring of patients undergoing gastrointestinal<br />
endoscopic procedures. Gastrointest Endosc 1995;<br />
42(6):626–629.<br />
25. Faigel DO, Baron TH, Goldstein JL, Hirota WK, Jacobson<br />
BC, Johanson JF. Guidelines for the use of deep sedation<br />
and anesthesia for GI endoscopy. American Society of<br />
Gastrointestinal Endoscopy. Gastrointest Endosc 2002;<br />
56(5):613–617.<br />
26. Abraham N, Wieczorek P, Huang J, Mayrand S, Fallone CA,<br />
Barkun AN. Assessing clinical generalizability in sedation<br />
studies of upper GI endoscopy. Gastrointest Endosc 2004;<br />
60:28–33.<br />
27. Abraham N, Barkun A, Larocque M, Fallone C, Mayrand S,<br />
Baffis, V. Predicting which patients can undergo upper<br />
endoscopy comfortably without conscious sedation. Gastrointest<br />
Endosc 2002;56:180–189.<br />
28. Silverman W, Chotiprasidhi P, Chuttani R, Liu J, Petersen B,<br />
Taitelbaum G. Monitoring equipment for endoscopy.<br />
Gastrointest Endosc 2004;59:761–765.<br />
29. Chen SC, Rex DK. An initial investigation of bispectral<br />
monitoring as an adjunct to nurse-administered propofol<br />
sedation for colonoscopy. Am J Gastroenterol 2004;99:<br />
1081–1086.<br />
30. Heuss LT, Schnieper P, Drewe J, Pflimlin E, Beglinger C.<br />
Conscious sedation with propofol in elderly patients: a<br />
prospective evaluation. Aliment Pharmacol <strong>The</strong>r 2003;17:<br />
1493–1501.<br />
31. Bhardwaj G, Conlon S, Bowles J, Baralt J. Use of midazolam<br />
and propofol during colonoscopy: 7 years of experience.<br />
Letter Am J Gastroenterol 2002;97:495–496.<br />
32. Wang CY, Ling LC, Cardosa MS, Wong AKH, Wong NW.<br />
Hypoxia during upper gastrointestinal endoscopy with and<br />
without sedation and the effect of pre-oxygenation on<br />
oxygen saturation. Anaesthesia 2000;55:654–658.<br />
33. Yano H, Iishi H, Tatsuta M, Sakai N, Narahara H, Omori M.<br />
Oxygen desaturation during sedation for colonoscopy in<br />
elderly patients. Hepatogastroenterology 1998;45:2138–<br />
2141.<br />
34. Erb T, Sluga M, Hampl KF, Ummenhofer W, Schneider MC.<br />
Preoperative anxiolysis with minimal sedation in elderly<br />
patients: bromazepam or clorazepate-dipotassium? Acta<br />
Anaethesiol Scand 1998;42:97–101.<br />
35. Rudner R, Jalowoecki P, Kawecki P, Gonciarz M, Mularczyk<br />
A, Patelenz M. Conscious sedation analgesia/sedation with<br />
remifentanil and propofol versus total intravenous anesthesia<br />
with fentanyl, midazolam, and propofol for outpatient<br />
colonoscopy. Gastrointest Endosc 2003;57:667–673.<br />
36. Jacobs JR, Reves JG, Marty J, White WD, Bai SA, Smith LR.<br />
Aging increases pharmacodynamic sensitivity to the<br />
hypnotic effects of midazolam. Anesth Analg 1995;80:<br />
143–148.<br />
37. Akcaboy ZN, Akcaboy EY, Albayrak D, Altinoren B,<br />
Dikmen B, Gogus N. Can remifentanil be a better choice<br />
than propofol for colonoscopy during monitored anesthesia<br />
care? Acta Anaesthesiol Scand 2006;50:736–741.<br />
38. Koshy G, Nair S, Norkus EP, Hertan HI, Pitchumoni CS.<br />
Propofol versus midazolam and meperidine for conscious<br />
sedation in GI endoscopy. Am J Gastroenterol 2000;95:<br />
1476–1479.<br />
39. Cohen LB, Hightower CD, Wood DA, Miller KM, Aisenberg<br />
J. Moderate level sedation during endoscopy: a prospective<br />
study using propofol. Meperidine/fentanyl and<br />
midazolam. Gastrointest Endosc 2004;58:795–803.<br />
40. Alhashemi JA. Dexmedetomidine vs. midazolam for monitored<br />
anaesthesia care during cataract surgery. Br J Anaesth<br />
206;96:722–726.<br />
41. Arain SR, Ebert JE. <strong>The</strong> efficacy, side effects, and recovery<br />
characteristics of dexmedetomidine versus propofol when<br />
used for intraoperative sedation. Anesth Analg 2002;95:<br />
461–465.<br />
42. Shinozaki M, Usui Y, Yamaguchi S, Okuda Y, Kitajima T.<br />
Recovery of psychomotor function after propofol<br />
sedation is prolonged in the elderly. Can J Anaesth<br />
2002;49:927–931.<br />
43. Frank LR, Strote J, Hauff SR, Bigelow SK, Fay K. Propofol<br />
by infusion protocol for ED procedural sedation. Am J<br />
Emerg Med 2006;24:599–602.<br />
44. Burton JH, Miner JR, Shipley ER, Strout TD, Becker C,<br />
Thode HC. Propofol for emergency department procedural<br />
sedation and analgesia: a tale of three centers. Acad Emerg<br />
Med 2006;13:24–30.<br />
45. Heuss LT, Drewe J, Schnieper P, Tapparelli CB, Pflimlin E,<br />
Beglinger C. Patient controlled versus nurse administered
23. Sedation and Monitoring 353<br />
sedation with propofol during colonoscopy. A prospective<br />
randomized trial. Am J Gastroenterol 2004;99:511–518.<br />
46. Heuss LT, Schnieper P, Drewe J, Pflimlin E, Beglinger C.<br />
Risk stratification and safe administration of propofol by<br />
registered nurses supervised by gastroenterologist: a prospective<br />
observational study of more than 2000 cases. Gastrointest<br />
Endosc 2003;57:664–671.<br />
47. Lee DW, Chan AC, Sze TS, Ko CW, Poon CM, Chan KC.<br />
Patient controlled sedation versus intravenous sedation for<br />
colonoscopy in elderly patients: a prospective randomized<br />
controlled trial. Gastrointest Endosc 2002;56:629–632.<br />
48. Mazzon D, Germanà B, Poole D, Celato M, Bernardi L,<br />
Calleri G. Conscious sedation during endoscopic<br />
retrograde cholangiopancreatography: implementation of<br />
SIED-SIAARTI-ANOTE guidelines in Belluno Hospital.<br />
Minerva Anestesiol 2005;71:101–109.<br />
49. Harrison SJ, Mayet J. Cardioversion and the use of sedation.<br />
Heart 2004;90:1374–1376.<br />
50. Walker JA, McIntyre RD, Schleinitz PF, Jacobson KN, Haulk<br />
AA, Adesman P. Nurse administered propofol sedation<br />
without anesthesia specialists in 9152 endoscopic cases in<br />
an ambulatory surgery center. Am J Gastroenterol 2003;<br />
98:1744–1750.<br />
51. Busbee BG, Brown MM, Brown GC, Sharma S. Incremental<br />
cost-effectiveness of initial cataract surgery. Ophthalmology<br />
2002;109:606–613.<br />
52. Steinberg EP, Javitt JC, Sharkey PD, Zuckerman A,<br />
Legro MW, Anderson GF, et al. <strong>The</strong> content and cost of<br />
cataract surgery. Arch Ophthalmol 1993;111:1041–1049.<br />
53. Hutchisson B, Nicoladis CB. Topical anesthesia—a new<br />
approach to cataract surgery. AORN J 2001;74:340–350.<br />
54. Powe NR, Schein OD, Gieser SC, Tielsch JM, Luthra R,<br />
Javitt J, et al. Synthesis of the literature on visual acuity<br />
and complications following cataract extraction with intraocular<br />
lens implantation. Arch Ophthalmol 1994;112:<br />
239–252.<br />
55. Woodcock M, Shah S, Smith RJ. Clinical review: recent ad -<br />
vances in customizing cataract surgery. BMJ 2004;328:92–96.<br />
56. Eye Diseases Prevalence Research Group. Prevalence of<br />
cataract and pseudophakia/aphakia among adults in the<br />
United States. Arch Ophthalmol 2004;122:487–494.<br />
57. Solomon DH, Locicero J, Rosenthal RA. New Frontiers in<br />
<strong>Geriatric</strong> Research. New York: Americas <strong>Geriatric</strong>s Society;<br />
2004:177–202.<br />
58. Kohnen T, Koch DD, eds. Cataract and Refractive Surgery.<br />
Essentials in Ophthalmology (Series). Berlin: Springer-<br />
Verlag; 2005:1–36, 123–132.<br />
59. Steinberg EP, Tielsch JM, Schein OD, Javitt JC, Sharkey P,<br />
Cassard SD, et al. National study of cataract surgery outcomes.<br />
Ophthalmology 2004;101:1131–1141.<br />
60. Tielsch JM, Steinberg EP, Cassard SD, Schein OD, Javitt JC,<br />
Legro MW, et al. Preoperative Functional Expectations<br />
and Postoperative Outcomes among Patients Undergoing<br />
First Eye Cataract Surgery. Arch Ophthalmol 1995;113:<br />
1312–1318.<br />
61. Schein OD, Steinberg EP, Cassard SD. Predictors of<br />
outcome in patients who underwent cardiac surgery.<br />
Ophthalmology 1995;102:817–823.<br />
62. Minassian DC, Rosen P, Dart JK, Reidy A, Desai P, Sidhu<br />
M, et al. Extracapsular cataract extraction compared with<br />
small incision surgery by phacoemulsification: a randomized<br />
trial. Br J Ophthalmol 2001;85:822–829.<br />
63. Schein OD, Bass EB, Sharkey P, Luthra R, Tielsch JM,<br />
Javitt JC, et al. Cataract Surgical Techniques. Arch Ophthalmol<br />
1995;113:1108–1112.<br />
64. Powe NR, Tielsch JM, Schein OD, Luthra R, Steinberg EP.<br />
Rigor of research methods in studies of the effectiveness<br />
and safety of cataract extraction with intraocular lens<br />
implantation. Arch Ophthalmol 1944;112:228–238.<br />
65. Vander JF, Gault JA. Ophthalmology Secrets. 2nd ed.<br />
Philadelphia: Hanley and Belfus; 2002:1–7, 8–11, 189–<br />
204.<br />
66. Jaffe NS. History of cataract surgery. Ophthalmology 1996;<br />
103(8):S5–S16.<br />
67. Appollonio I, Carabellese C, Magni E, Frattola L,<br />
Trabucchi M. Sensory impairments and mortality in an<br />
elderly community population: a six-year follow-up study.<br />
Age Ageing 1995;24:30–36.<br />
68. Keller BK, Morton JL, Thomas VS, Potter JF. <strong>The</strong> effect<br />
of visual and hearing impairments on functional status.<br />
J Am Geriatr Soc 1999;47:1319–1325.<br />
69. Schein OD, Katz J, Bass EB, Tielsch JM, Lubomski LH,<br />
Feldman MA, et al. <strong>The</strong> value of routine preoperative<br />
medical testing before cataract surgery. N Engl J Med<br />
2000;342:168–175.<br />
70. Bass EB, Steinberg EP, Luthra R, Schein OD, Tielsch JM,<br />
Javitt, JC, et al. Do ophthalmologists, anesthesiologist, and<br />
internists agree about preoperative testing in healthy<br />
patients undergoing cataract surgery? Arch Ophthalmol<br />
1995;113:1248–1256.<br />
71. Gainey SP, Robertson DM, Fay W, Ilstrup D. Ocular surgery<br />
on patients receiving long-term warfarin therapy. Am J<br />
Ophthalmol 1989;108:142–146.<br />
72. McMahan LB. Anticoagulants and cataract surgery. J<br />
Cataract Refract Surg 1988;14:569–571.<br />
73. Hall DL, Steen WH, Drummond JW, Byrd WA. Brief notes:<br />
anticoagulants and cataract surgery. Ophthalmic Surg 1988;<br />
19:221–222.<br />
74. Katz J, Feldman MA, Bass EB, Lubomski LH, Tielsch JM,<br />
Petty, BG, et al. Risks and benefits of anticoagulant and<br />
antiplatelet medication use before cataract surgery. Ophthalmology<br />
2003;110:1748–1788.<br />
75. Fry RA. Anticoagulants and local anaesthesia for eye<br />
surgery. Anaesth Intensive Care 2000;28:709.<br />
76. Dutton JJ. Anatomic considerations in ophthalmic anesthesia.<br />
Surv Ophthalmol 2001;46:172–178.<br />
77. Roman S, Auclin F, Ullern M. Topical versus peribulbar<br />
anesthesia in cataract surgery. J Cataract Refract Surg 1996;<br />
22:1121–1124.<br />
78. Boezaart A, Berry R, Nell M. Topical anesthesia versus<br />
retrobulbar for cataract surgery: the patients’ perspective.<br />
J Clin Anesth 2000;12:58–60.<br />
79. Ripart JR, Lefrant JY, de La Coussaye JE, Prat-Pradal D,<br />
Vivien B, Eledjam JJ. Peribulbar versus retrobulbar<br />
anesthesia for ophthalmic surgery. <strong>Anesthesiology</strong> 2001;<br />
94:56–62.<br />
80. Rosenfeld SI, Litinsky SM, Snyder DA, Plosker H, Astrove<br />
AW, Schiffman J. Effectiveness of monitored anesthesia<br />
care in cataract surgery. Ophthalmology 1999;106:1256–<br />
1261.
354 S.R. Barnett<br />
81. Habib NE, Balmer HG, Hockind G. Efficacy and safety of<br />
sedation with propofol in peribulbar anaesthesia. Eye 2002;<br />
16:60–62.<br />
82. Bosman YK, Krige SJ, Edge KR, Newstead J, DuToit PW.<br />
Comfort and safety in eye surgery under local anesthesia.<br />
Anaesth Intensive Care 1998;26:173–177.<br />
83. Malhoutra SK, Dutta A, Gupta A. Monitored anesthesia in<br />
elderly ophthalmic elderly patients. Lancet 2002;359:532.<br />
84. Mandelcorn M, Taback N, Mandelcorn E, Ananthanarayan C.<br />
Risk factors for pain and nausea following retinal and vitreous<br />
surgery under conscious sedation. Can J Ophthalmol<br />
1999;34:281–285.<br />
85. Rosenberg JK, Raymond C, Bridge PD. Comparison of<br />
midazolam/ketamine with methohexital for sedation during<br />
peribulbar block. Anesth Analg 1995;81:173–174.<br />
86. Janzen PRM, Hall WJ, Hopkins PM. Setting targets for<br />
sedation with a target controlled propofol infusion. Anaesthesia<br />
2000;55:666–669.<br />
87. Pac-Soo CK, Deacock S, Lockwood G, Carr C, Whitwam<br />
JG. Patient-controlled sedation for cataract surgery using<br />
peribulbar block. Br J Anaesth 1996;77:370–374.<br />
88. Jacobi PC, Dietlein TS, Jacobi FK. Comparative study of<br />
topical vs. retrobulbar anesthesia in complicated cataract<br />
surgery. Arch Ophthalmol 2000;118:1037–1043.<br />
89. Harman DM. Combined sedation and topical anesthesia for<br />
cataract surgery. J Cataract Refract Surg 2000;26:109–113.<br />
90. Nørregaard JC, Schein OD, Bellan L, Black C, Alonso J,<br />
Bernth-Petersen P, et al. International variation in anesthesia<br />
care during cataract surgery. Arch Ophthalmol 1997;<br />
115:1304–1308.<br />
91. Reeves SW, Friedman DS, Fleisher LA, Lubomski LH,<br />
Schein OD, Bass EB. A decision analysis of anesthesia<br />
management for cataract surgery. Am J Ophthalmol 2001;<br />
132:528–536.<br />
92. Risdall JE, Geraghty EF. Oxygenation of patients undergoing<br />
ophthalmic surgery under local anaesthesia. Anaesthesia<br />
1997;52:489–500.<br />
93. Schlager A. Accumulation of carbon dioxide under ophthalmic<br />
drapes during eye surgery: a comparison of three different<br />
drapes. Anaesthesia 1999;54:683–702.<br />
94. Shelswell NL. Perioperative patient education for retinal<br />
surgery. AORN J 2002;75:801–807.
24<br />
Total Hip Replacement, Joint Replacement,<br />
and Hip Fracture<br />
Idit Matot and Shaul Beyth<br />
Surgical treatment of hip fracture is a well-known medical<br />
emergency in the elderly. Similar to arthroplasty, this<br />
operation is performed to acutely restore function<br />
and decrease pain. Although the anatomic approach,<br />
instrumentation, and final mechanical results of hip fracture<br />
repair are similar to what occurs with hip arthroplasty,<br />
major differences between the two patient<br />
populations exist and create differences in perioperative<br />
management.<br />
Background<br />
Total Hip and Knee Arthroplasty<br />
Joint replacement is one of the most rewarding procedures<br />
in the field of orthopedic surgery in general. It is<br />
indicated in individuals with a painful, disabling arthritic<br />
joint that is no longer responsive to conservative treatment.<br />
For these patients, it may provide improvement in<br />
the quality of life. Focusing on the frequently replaced<br />
weight-bearing joints, i.e., hip and knee, it should be noted<br />
that in addition to complete primary joint replacement, a<br />
whole new field of reconstructive surgery has evolved<br />
around the implantation of prostheses that includes, but<br />
is not limited to, partial arthroplasty, revision procedures<br />
for failed implants, computer-assisted surgery, and minimally<br />
invasive surgery.<br />
Patients coming for elective joint replacement surgery<br />
are highly motivated and in most cases mentally prepared<br />
to undergo major surgery in order to regain daily functions.<br />
<strong>The</strong>se patients undergo a thorough preoperative<br />
evaluation and preparation including relevant specialist<br />
evaluation, revision of medications, autologous blood<br />
donation, and preparation from a rehabilitation facility<br />
for the postoperative period.<br />
Elective total hip or knee arthroplasty (THA/TKA) is<br />
considered a relatively safe orthopedic procedure. Known<br />
complications after these procedures, not related to the<br />
implants used, include thromboembolism, postoperative<br />
anemia, infection, fractures, and death. However, despite<br />
the low incidence of mortality after total joint arthroplasty,<br />
a significant number of deaths occur given<br />
the extensive number of procedures being performed.<br />
<strong>The</strong> specific risk has been reported to be as low as 0.1%<br />
and as high as 3%. 1 Compared with THA, the risk of<br />
perioperative death after TKA is considerably lower. Preexisting<br />
comorbidities and the American Society of Anesthesiologists<br />
physical status classification are significantly<br />
related to the incidence of postoperative death in patients<br />
undergoing elective hip or knee arthroplasty. 2 Also, total<br />
joint arthroplasty performed for fracture or malignancy<br />
has a higher risk of mortality. 3,4 Other patient healthindependent<br />
factors that are associated with a significantly<br />
increased mortality include: age more than 70<br />
years, revision (as compared with primary) surgery, use<br />
of a cemented prosthesis, and simultaneous bilateral<br />
arthroplasty. 4 Recognition of these risk factors and implementation<br />
of appropriate measures may enable the<br />
orthopedic team to reduce perioperative mortality after<br />
major lower extremity surgery.<br />
<strong>The</strong> preoperative medical status of the patient may be<br />
even more important to outcome than the risks of the<br />
surgical procedure. Patients with preexisting cardiac or<br />
respiratory disease have decreased physiologic reserve<br />
and are at greater risk of morbidity and mortality, specifically<br />
cardiorespiratory collapse after an embolic load,<br />
hypoxemia as a result of ventilation/perfusion mismatch<br />
during lateral decubitus position, and myocardial ischemia<br />
or infarct, which may be prompted by intra- or<br />
postoperative blood loss, hypotension, and/or tachycardia.<br />
Measures to consider include optimizing medical<br />
therapy of patients who have a history of cardiac or pulmonary<br />
problems; avoiding bilateral one-stage TKA in<br />
patients who are ill or elderly; vigilant anesthetic monitoring,<br />
especially around the times of surgical interventions<br />
that are known to be associated with marrow and<br />
fat embolization; and the use of vasopressor agents during<br />
355
356 I. Matot and S. Beyth<br />
episodes of hypotension. Modifications in surgical technique<br />
and implant choice to reduce marrow and fat<br />
embolization may also be appropriate in some high-risk<br />
patients. <strong>The</strong> use of prophylactic antibiotics decreases<br />
infection rate to less than 1%. Administration of antibiotics<br />
30 minutes before skin incision or, during revision<br />
arthroplasty, after samples for bacterial culture are<br />
obtained, is recommended.<br />
Hip Fracture Surgery<br />
Fractures of the hip, which most frequently occur in the<br />
elderly, are associated with a very high mortality. With<br />
increasing life expectancy, these injuries are on the<br />
increase and will thus continue to be a substantial workload<br />
for trauma departments. Impaired balance and coordination,<br />
leading to frequent falls, paired with a high<br />
prevalence of osteoporosis make the elderly particularly<br />
prone to incur this fracture. Operative treatment of hip<br />
fractures is usually straightforward, but postoperative<br />
recovery and rehabilitation are fraught with complications.<br />
One-year mortality after hip fracture surgery is<br />
remarkably high, around 26%, with a range of 14%–36%<br />
reported in the literature. It is highest during the first 6<br />
months after injury, and after the first year it approaches<br />
that of unoperated patients of matching age and sex. 5<br />
<strong>The</strong> reported in-hospital mortality rates range from<br />
1.4% to 12%. 6–8 <strong>The</strong> principal causes of in-hospital death<br />
after hip fracture are cardiac failure and myocardial<br />
infarction, which occur early after the fracture, peaking at<br />
2 days, bronchopneumonia, which accounts for the majority<br />
of late deaths, and pulmonary embolism, which peaks<br />
in the second week after injury. <strong>The</strong> overall incidence of<br />
perioperative myocardial ischemia in elderly patients<br />
undergoing hip fracture surgery has been reported to be<br />
35%–42%. 9,10 Preoperative placement of an epidural<br />
catheter with provision of effective analgesia has recently<br />
been shown to reduce the preoperative incidence of<br />
adverse cardiac outcomes in high-risk patients with neck<br />
of femur fracture. 9,10 Mortality from bronchopneumonia<br />
and pulmonary embolism after hip fracture may be<br />
reduced by early surgical intervention, early mobilization,<br />
antibiotics, and prophylactic anticoagulation. 5,8,11<br />
Unlike patients scheduled for joint arthroplasty,<br />
patients with hip fracture are routinely admitted to the<br />
emergency room without prior preparation or evaluation.<br />
<strong>The</strong>se patients should be considered as requiring urgent<br />
treatment. Thus, perioperative management should be<br />
oriented toward adequate pain control, multidisciplinary<br />
consultation, if needed, and optimal monitoring and riskreduction<br />
within a given time frame. <strong>The</strong> issue that the<br />
anesthesiologist must consider in the preoperative evaluation<br />
and clearance for urgent surgical treatment of a hip<br />
fracture is the timing of surgery. In most studies, patients<br />
wait on average 1.5–3.5 days between admission and<br />
surgery. 5,11–16 Results of studies of the optimal timing of<br />
surgery are contradictory. Whereas some studies reported<br />
an increased mortality if patients had surgery within 24<br />
hours, the majority have demonstrated a clear advantage<br />
of early surgical intervention. <strong>The</strong> current prevailing recommendation<br />
is that patients who are medically fit for<br />
surgery should be operated on the day of admission 16<br />
because delays serve to increase morbidity, mortality,<br />
and resource utilization. 14–16 In two recent studies, longer<br />
waiting time increased the risk for developing deep<br />
vein thrombosis and pulmonary embolism, atelectasis,<br />
pneumonia, 11 and decubitus ulcer formation. 16 Nevertheless,<br />
sufficient time should be taken to study and prepare<br />
patients with significant comorbidities. For these patients,<br />
preoperative epidural analgesia may prove to be most<br />
helpful. 10<br />
It is important to note that, although the two categories<br />
of hip fracture surgeries (THA and hip fracture stabilization)<br />
aim to improve ambulation, they differ in both<br />
patient characteristics (as noted above) and in the expected<br />
end result. For arthroplasty, the expected surgical outcome<br />
is functioning “better than before,” whereas the anticipated<br />
result of procedures for hip fractures is functioning<br />
“as close to before (the fracture)” as possible.<br />
Surgical Procedure<br />
Total Hip and Knee Arthroplasty<br />
Arthroplasty of both hip and knee joints is a procedure<br />
aimed to improve patients’ ambulation by means of<br />
replacing damaged and worn-out joint components with<br />
prosthetic devices. Inherently, these procedures involve<br />
surgical removal of articulating surfaces together with the<br />
subchondral bone, implantation of the substitute parts,<br />
and fixation of those components.<br />
Hip<br />
<strong>The</strong>re are several prosthetic devices available, most of<br />
which share a few basic characteristics:<br />
1. After surgical dislocation from the acetabulum, the<br />
arthritic femoral head and a portion of the femoral neck<br />
are resected and replaced with an intramedullary stemmed<br />
component, anchored to its place using a premade space<br />
reamed through the soft spongious bone (“press-fit”)<br />
and/or cement surrounding the stem.<br />
2. If the acetabulum needs replacement, the damaged<br />
articulating cartilage is reamed and the prosthetic acetabular<br />
component is attached to its place, using the same<br />
techniques as above. It can then be further supported by<br />
screws and/or bone graft.<br />
3. No matter which surgical approach to the joint has<br />
been used (anterior, posterior, or lateral), the two artifi-
24. Total Hip Replacement, Joint Replacement, and Hip Fracture 357<br />
cial joint components are fit together (“reduction” of a<br />
“dislocated joint”) at the very last stages of the operation.<br />
This step is best assisted by muscle relaxation. Dislocation<br />
may occur shortly after surgery if the muscle tone<br />
that keeps the joint in place is not restored.<br />
Knee<br />
This procedure begins with a knee joint arthrotomy. <strong>The</strong><br />
distal femur and the proximal tibia are shaped using measured<br />
templates to fit the size of the available prosthetic<br />
parts. <strong>The</strong>se parts are later attached to the bones, covering<br />
the exposed surfaces. Shaping of the bony ends is<br />
accompanied by bleeding, especially from the trabecular<br />
bone. Although fitting of the prosthesis leads to hemostasis,<br />
the bleeding from trabecular bone is not always fully<br />
controlled. Blood loss from trabecular bone may therefore<br />
proceed after surgery and is halted because of clot<br />
formation and/or tamponade effect of the hematoma.<br />
Close monitoring of hematocrit and hemoglobin levels is<br />
thus essential in the postoperative period.<br />
<strong>The</strong> patella may be replaced either completely or<br />
partially, or may not be replaced at all. Also, the new<br />
prosthetic components may be either cemented or uncemented,<br />
depending on the findings and the surgeons’<br />
preferences.<br />
Hip Fractures<br />
Several procedures are accepted today in the management<br />
of hip fractures, depending primarily on the type of fracture<br />
and the patient’s concurrent diseases (Figure 24-1).<br />
A<br />
B<br />
Extracapsular Fractures<br />
<strong>The</strong> vast majority of these fractures will unite after proper<br />
reduction and fixation. Both extra- and intramedullary<br />
systems are used to treat pertrochanteric and subtrochanteric<br />
fractures. <strong>The</strong> newest devices are introduced through<br />
minor skin incisions from a lateral aspect approach to<br />
the thigh and require not more than an hour for a skilled<br />
team.<br />
Intracapsular Fractures<br />
Because the retrograde blood supply to the head of the<br />
femur is often compromised after displaced femoral neck<br />
fractures, the degree of displacement dictates the nature<br />
of surgical procedure:<br />
• Minimally and nondisplaced intracapsular fractures are<br />
usually stabilized in their position by percutaneous introduction<br />
of cannulated screws into the femoral neck and<br />
head through the fracture line. This is a minimally invasive<br />
procedure that results in minor systemic effect.<br />
• Displaced intracapsular fractures, often termed “subcapital”<br />
or “femoral neck” fractures, are often treated<br />
Figure 24-1. (A) Intertrochanteric femoral fracture. Fracture<br />
line extends from greater to lesser trochanters, external to hip<br />
joint capsule. (B) Femoral neck fracture. Fracture line extends<br />
from medial to lateral cortex of the proximal femur, within the<br />
hip joint capsule (“sub-capital” fracture).<br />
by prosthetic replacement of the femoral side of the<br />
hip joint (hemiarthroplasty), because of the abovementioned<br />
risk of femoral head necrosis after compromise<br />
of its blood supply. From the anesthesiologist’s<br />
point of view, the surgical procedure itself is almost<br />
identical to that of complete hip joint replacement.<br />
Anesthetic Management<br />
Anesthetic Technique<br />
<strong>The</strong> choice of anesthetic technique is a complex medical<br />
decision that depends on many factors, including patient<br />
characteristics (e.g., comorbidity, age), type of surgery performed,<br />
and risks of the anesthetic techniques. Assessment
358 I. Matot and S. Beyth<br />
of the risks of the anesthetic technique should include<br />
consideration of technical factors (airway, establishment<br />
of regional blocks, invasive monitoring), anesthetic agent<br />
toxicities, incidence of critical intraoperative and postoperative<br />
events, and postoperative treatment of pain. 6<br />
<strong>Anesthesia</strong> for Hip Fracture Repair<br />
In recent years, regional anesthesia has been used more<br />
frequently in hip fracture patients. In 1981–1982, general<br />
anesthesia was used in 94.8% of patients, whereas in<br />
1993–1994, general anesthesia was used in only 49.6% of<br />
patients. 6<br />
Few studies have compared the outcome of patients<br />
administered general versus regional anesthesia for hip<br />
fracture surgery. <strong>The</strong> largest retrospective analysis that<br />
included 9425 hip fracture patients reported that the type<br />
of anesthesia did not seem to influence morbidity or<br />
overall mortality. 6 This finding suggests that unadjusted<br />
differences in outcome between general anesthesia and<br />
regional anesthesia are mainly a result of concomitant<br />
disease and not of any protective effect of one anesthetic<br />
technique versus another. As might be predicted from<br />
clinical practice, the authors found that older patients and<br />
those who were sicker were more likely to be receiving<br />
a regional anesthetic. Intraoperative hypotension and the<br />
use of vasopressors were more frequent in the regional<br />
anesthesia group than in the general anesthesia group.<br />
<strong>The</strong> results of this study are in agreement with two earlier<br />
meta-analyses 13,17 that included randomized controlled<br />
trials that evaluated the outcome of hip fracture surgery<br />
up to 1 month postoperatively. <strong>The</strong> authors were unable<br />
to identify any difference in long-term mortality or blood<br />
loss attributable to the use of either regional or general<br />
anesthesia. However, there was a clearly reduced incidence<br />
of deep vein thrombosis in the regional anesthesia<br />
group. Subsequent large, single-center observational<br />
studies 12,18 also did not identify meaningful differences in<br />
cardiopulmonary morbidity or mortality attributable to<br />
the choice of the anesthetic technique in hip surgery<br />
patients. A similar conclusion was reached in the 2002<br />
Cochrane Library review. 19,20<br />
In the past few years, there has been a growing interest<br />
in peripheral nerve blockade in orthopedic patients. Such<br />
techniques are used more and more often not only to<br />
provide anesthesia but also for postoperative analgesia<br />
after limb surgery. Various nerve blocks have been used<br />
to reduce pain after hip fracture. <strong>The</strong> 2002 Cochrane<br />
Library review 21 summarized the data from eight randomized<br />
trials involving 328 patients. Three trials related<br />
to placement of a nerve block (lateral cutaneous, femoral,<br />
triple, psoas) preoperatively and the remaining five to<br />
perioperative insertion. Nerve blocks resulted in lower<br />
reported pain levels and reduced consumption of pain<br />
medications (parenteral and oral) during the perioperative<br />
period. No clinical benefits beyond these reductions<br />
could be demonstrated.<br />
Neuraxial <strong>Anesthesia</strong> for Total Knee or<br />
Hip Arthroplasty<br />
<strong>Regional</strong> anesthesia may be of benefit to patients undergoing<br />
major joint surgery. A retrospective study found that<br />
the use of neuraxial anesthesia compared with general<br />
anesthesia in patients having elective total knee or hip<br />
replacements was associated with a lower rate of intensive<br />
care unit admission postoperatively. 22 In addition, intraoperative<br />
blood loss and transfusion requirements were<br />
significantly lower in patients who received neuraxial anesthesia<br />
or lumbar plexus block. 23–26 Neuraxial anesthesia<br />
and analgesia were associated with a reduction in thromboembolic<br />
complications. 27–29 Also, postoperative confusional<br />
state was reported to be less frequent in a group of<br />
patients who had epidural anesthesia compared with those<br />
patients who had surgery under general anesthesia. 30<br />
Others 31,32 have failed to find an advantage of general<br />
versus regional anesthesia in all outcome measurements<br />
(magnitude or pattern of postoperative cognitive dysfunction<br />
and incidence of major cardiovascular complications)<br />
except that epidural anesthesia was associated with more<br />
rapid achievement of postoperative in-hospital rehabilitation<br />
goals. <strong>The</strong> largest benefit of regional anesthesia and<br />
analgesia is its role in providing adequate pain control for<br />
rehabilitation. This topic is discussed in depth in the section<br />
on postoperative analgesia.<br />
Intraoperative Monitoring<br />
With advances in both anesthetic and surgical techniques,<br />
the need for invasive intraoperative monitoring in medically<br />
fit patients has diminished. Nevertheless, several<br />
stages in the intraoperative period can cause significant<br />
hemodynamic and respiratory alterations. <strong>The</strong>refore, in<br />
high-risk patients or procedures (complex or revision<br />
surgery), the use of an arterial line for continuous hemodynamic<br />
and blood gas monitoring may be useful. Intraoperative<br />
transesophageal echocardiography may detect<br />
fat embolization and monitor intraoperative volume status<br />
and cardiac function. 33 In high-risk patients undergoing<br />
bilateral procedures, pulmonary artery pressure monitoring<br />
may also be of benefit, both as a diagnostic and a<br />
prognostic tool. 34 Although more invasive monitoring<br />
improves detection of pulmonary embolization and its<br />
sequelae, there is no evidence to suggest that these interventions<br />
improve outcome in fat emboli syndrome.<br />
Positioning<br />
<strong>The</strong> lateral decubitus positioning, which is frequently<br />
used for THA and displaced intracapsular fractures
24. Total Hip Replacement, Joint Replacement, and Hip Fracture 359<br />
Figure 24-2. Positioning of the patient on the fracture table for fracture of hip surgery (A) or in the lateral decubitus position<br />
for total hip arthroplasty (B) should be performed carefully because of potential morbidities.<br />
(Figure 24-2), requires special attention to pressure points,<br />
hemodynamic stability, and oxygenation. A low axillary<br />
roll is placed under the chest and lower shoulder to<br />
prevent brachial plexus stretching and axillary artery<br />
occlusion of the dependent side. Padding of the nonoperated<br />
(dependent) hip and leg is important, as well as<br />
padding of the nondependent leg and hand to prevent<br />
injury to the femoral, popliteal, and pudendal nerve, the<br />
brachial plexus, and the ulnar nerve. <strong>The</strong> head and neck<br />
should be aligned properly and supported to avoid injury<br />
to the cervical spine, ears, and eyes. Positioning into the<br />
lateral decubitus may cause brief hypotension, especially<br />
if the patient is hypovolemic. It may also result in hypoxemia,<br />
which results from increased degree of ventilation/<br />
perfusion mismatch: the nondependent lung is well ventilated<br />
but poorly perfused and the dependent lung is<br />
poorly ventilated but well perfused. 35<br />
Cement<br />
Polymethylmethacrylate bone cement prepared in a liquid<br />
methylmethacrylate monomer is widely used to anchor<br />
prostheses in joint replacement surgery. Multiple adverse<br />
effects have been associated with the use of polymethylmethacrylate<br />
cement. 36,37 Hypoxemia, pulmonary hypertension,<br />
right ventricle failure, cardiac arrest, and sudden<br />
death are well-recognized complications during THA and<br />
to a lesser degree after TKA. Although incompletely<br />
understood, these complications have been in part attributed<br />
to formation of microemboli and activation of the<br />
complement system, resulting in triggering of the inflammatory<br />
cascade, which in turn leads to increased vascular<br />
endothelial permeability. 38,39 <strong>The</strong> increase of intramedullary<br />
pressure caused by the mechanical compression of the<br />
femoral canal during the insertion of the prosthetic stem<br />
is the most decisive pathogenic factor for the development<br />
of embolism. <strong>The</strong> thin-walled vessels in the medullary<br />
cavity are easily disrupted by focal application of compressive<br />
loads, allowing the intravasation of bone marrow, fat,<br />
and bone debris and the embolization through the venous<br />
system located along the linea aspera and through the<br />
metaphyseal vessels. Migration of bone marrow into the<br />
draining veins activates the coagulation system. Occlusion<br />
of lung capillaries by these emboli causes an increased<br />
arteriovenous shunt and alveolar hypoperfusion. 40–44 In<br />
addition, the methylmethacrylate cement causes direct<br />
vasodilatation leading to transient hypotension.<br />
<strong>The</strong> progressive decrease of serious intraoperative cardiorespiratory<br />
complications in the past few decades has<br />
been attributed to the constant improvement of anesthesiologic<br />
and surgical techniques. To prevent hypoxemia<br />
intraoperatively, 100% oxygen administration during<br />
cementing and prosthesis insertion in patients at risk has<br />
been recommended anecdotally although there are<br />
no prospective studies confirming the usefulness of this<br />
maneuver. 34 Fluid therapy to prevent hypovolemia is<br />
also recommended, because canine studies have shown<br />
that acute hemodynamic changes during prosthesis insertion<br />
and fat embolism may be aggravated in hypovolemic<br />
states. 45 Maintenance of perfusion pressure with vasoconstrictors<br />
to preserve right heart perfusion and function<br />
and to avoid fluid loading may be preferable in patients<br />
with preexisting heart disease with congestive symptoms.<br />
Modifications of surgical techniques aimed at prevention<br />
of embolism, e.g., by venting of the femoral shaft and<br />
lavage of the medullary canal (to minimize increases<br />
in intramedullary pressure and the amount of fatty<br />
bone marrow present), and increased use of total condylar<br />
components from long-stemmed prostheses (that<br />
obviate the need for extensive intramedullary manipulation)<br />
may be most effective at reducing the incidence of<br />
these complications.
360 I. Matot and S. Beyth<br />
Blood Management<br />
<strong>The</strong> likelihood of major intra- and postoperative blood<br />
loss and resultant transfusion of blood components is<br />
high in lower extremity joint replacement and hip fracture<br />
surgery. TKA, for example, can be associated with<br />
major blood loss. Lotke et al. 46 concluded in their study<br />
that the mean calculated total blood loss in TKA was<br />
approximately 1.5 L. In TKA the total blood loss is composed<br />
of “visible” blood loss (from the surgical field<br />
and wound drainage) and “hidden” blood loss (into the<br />
tissues). <strong>The</strong> latter can account for up to 50% of total<br />
blood loss. 47 Blood management should be aimed at<br />
addressing the total blood loss and underestimation ought<br />
to be avoided.<br />
In several series over the past decade, 48–51 32%–85% of<br />
the operated patients received allogeneic blood. <strong>The</strong> frequency<br />
of allogeneic blood transfusion varied with respect<br />
to the type of operative procedure (revision THA and<br />
bilateral TKA were associated with the highest prev -<br />
alence of such transfusions) and with a baseline hemoglobin<br />
level of 130 g/L or less. Concerns about the risks<br />
associated with allogeneic blood transfusion led to the<br />
development of a variety of blood conservation techniques<br />
intended to minimize the need for allogeneic<br />
transfusion. <strong>The</strong>se include preoperative donation of<br />
autologous blood, acute normovolemic hemodilution,<br />
blood salvage, hypotensive anesthesia, improvements in<br />
tissue hemostasis, and pharmacologic agents such as preoperative<br />
use of erythropoietin and intraoperative use of<br />
antifibrinolytics. 52 Several studies have confirmed the use<br />
of these techniques to reduce allogeneic blood transfusion;<br />
however, their use is based on hospital resources<br />
and on the anesthesiologist and surgeon preferences. In<br />
addition to reducing the need for and exposure to allogeneic<br />
blood, the potential for less blood loss may translate<br />
into less swelling, improved range of motion, and<br />
earlier return to function. <strong>The</strong> anesthesiologist should be<br />
thoroughly acquainted with these blood conservation<br />
techniques and remember that all methods come with<br />
varying amounts of risk and cost. Also, the use of regional<br />
anesthesia may reduce the risk of transfusion in lower<br />
extremity arthroplasties. 23–26<br />
Postoperative Analgesia<br />
For lower limb orthopedic surgery, postoperative pain is<br />
a major problem. Peripheral nerve blocks with or without<br />
a catheter are the techniques of the new millennium. 53<br />
For acute pain management after major lower limb<br />
surgery, continuous femoral nerve blockade has been<br />
advocated as an alternative to epidural analgesia or intravenous<br />
opiate administered by patient-controlled analgesia<br />
(PCA). 54–62 Both epidural analgesia and continuous<br />
femoral nerve blockade are more effective than intravenous<br />
PCA in patients undergoing THA. Both provide<br />
effective postoperative pain control, reduce opiate<br />
requirements and associated side effects, and improve<br />
functional recovery. <strong>The</strong> advantage of a femoral nerve<br />
block in this major joint surgery seems to be the analgesic<br />
effect on pain during mobilization. Similar results have<br />
been obtained after TKA. 55–58 Moreover, as was confirmed<br />
by Ganapathy et al. 59 and Chelly et al., 57 compared<br />
with intravenous PCA, continuous femoral nerve blockade<br />
reduced the length of hospital stay and the frequency<br />
of serious complications while conveniently avoiding the<br />
risk of epidural hematoma associated with the use of<br />
anticoagulant. Thus, a continuous femoral nerve block<br />
should be considered after proximal lower limb surgery.<br />
<strong>The</strong> use of PCA boluses (for femoral nerve block), with<br />
or without low basal infusion rate after TKA or THR, 60,61<br />
significantly reduces the local anesthetic consumption<br />
and therefore the risk of local anesthetic toxicity and<br />
increases patient satisfaction. It has been argued that<br />
femoral nerve block does not consistently produce anesthesia<br />
of the obturator nerve. <strong>The</strong> addition of an obturator<br />
nerve block has been therefore recommended to<br />
improve the quality of postoperative analgesia after total<br />
knee replacement. 62 <strong>The</strong> need for addition of a sciatic<br />
nerve block to a femoral nerve block is controversial.<br />
Whereas Allen et al. 58 reported that it does not further<br />
improve analgesic efficacy, Davies et al. 63 showed that<br />
combined femoral and sciatic blocks offer a practical<br />
alternative to epidural analgesia for unilateral knee<br />
replacements. Others suggested posterior lumbar plexus<br />
block for postoperative analgesia after TNA. 64,65<br />
Both clonidine and opioids have been used to supplement<br />
the analgesic effect of local anesthetics in peripheral<br />
nerve blocks. <strong>The</strong> addition of opioids to local anesthetic<br />
solution to maintain continuous nerve blockade has been<br />
debated because Picard et al. 66 failed to show any positive<br />
effect of opioids. A detailed discussion of the different<br />
peripheral nerve block techniques is beyond the scope of<br />
this chapter. For further discussion, the reader is referred<br />
to Internet resources, including the New York Society for<br />
<strong>Regional</strong> <strong>Anesthesia</strong> Web site (http://www.nysora.com),<br />
the Peripheral <strong>Regional</strong> <strong>Anesthesia</strong> Web site (http://www.<br />
nerveblocks.net), or the <strong>Regional</strong>Block.com Web site<br />
(http://www.regionalblock.com).<br />
Specific Considerations<br />
Venous Thromboembolism, Anticoagulation,<br />
and Neuraxial <strong>Anesthesia</strong><br />
Patients who undergo major lower extremity orthopedic<br />
surgery are among those considered to be at greatest risk<br />
for venous thromboembolism. Data suggest a deep vein<br />
thrombosis rate as high as 40%–84% when prophylaxis
24. Total Hip Replacement, Joint Replacement, and Hip Fracture 361<br />
is not administered to patients undergoing TKA, a rate<br />
of 45%–57% after THA, and a rate of 36%–60% in<br />
patients receiving hip fracture surgery. 67 Clinically<br />
detected pulmonary embolism occurs in 2%–10% of<br />
patients with deep vein thrombosis who have had knee<br />
or hip arthroplasty. <strong>The</strong> incidence of fatal pulmonary<br />
embolism is 1%–2%. Thromboembolism can occur in<br />
vessels in the pelvis, thigh, and calf. Most thrombi probably<br />
develop in the deep veins of the calf and subsequently<br />
extend into the thigh, but isolated thrombi in the pelvis<br />
or deep femoral veins can also develop. Unfortunately,<br />
after knee or hip arthroplasty, deep vein thrombosis is<br />
clinically asymptomatic in 70%–80% of patients who<br />
experience clinically significant pulmonary emboli. 68<br />
<strong>The</strong>refore, thromboprophylaxis has become a worldwide<br />
standard practice for preventing complications during<br />
and after major lower extremity orthopedic surgery.<br />
Recently, the American College of Chest Physicians<br />
(ACCP) published its recommendation for prophylaxis<br />
for patients undergoing TKA, THA, and hip fracture<br />
surgery. 69 Either a low-molecular-weight heparin or an<br />
adjusted-dose warfarin is recommended for prophylaxis<br />
in THA and TKA (grade IA) and hip fracture surgery<br />
(grade IB). <strong>The</strong> ACCP also suggested that low-molecularweight<br />
heparin is significantly more effective than warfarin<br />
in preventing asymptomatic and symptomatic<br />
in-hospital venous thromboembolism because of the<br />
more rapid onset of anticoagulant activity with lowmolecular-weight<br />
heparin than with warfarin. Nevertheless,<br />
regimens for deep vein thrombosis prophylaxis are<br />
frequently institution- and surgeon-specific. Anesthetic<br />
techniques that enhance lower extremity blood flow and<br />
minimize the hypercoagulable state may be advantageous<br />
in the management of patients undergoing lower extremity<br />
surgery. Clearly, the incidence of intraoperative thrombosis<br />
formation is reduced with the use of central neuraxis<br />
techniques when compared with general endotracheal<br />
anesthesia without other active interventions. 27–29,70 Epidural<br />
anesthesia may prevent the development of the<br />
hypercoagulable state without impairing the coagulation<br />
process as measured by the platelet-mediated hemostasis<br />
time and the clotting time. Possible explanations include:<br />
central neuraxial blockade-induced sympathectomy, prolonged<br />
exposure to high systemic blood levels of local<br />
anesthetic, and the antiinflammatory effects of local<br />
anesthetics. 70<br />
<strong>The</strong> introduction of new anticoagulants and antiplatelet<br />
agents, the complexity of balancing thromboembolic<br />
with hemorrhagic complications, and the evolving indications<br />
for regional anesthesia/analgesia have raised<br />
concern over the issue of neuraxial anesthesia in caring<br />
for surgical orthopedic patients. Spinal/epidural hematoma<br />
is a rare but potentially catastrophic complication<br />
of spinal or epidural anesthesia, the incidence of which<br />
was estimated to be less than 1 in 150,000 epidural and<br />
less than 1 in 220,000 spinal anesthetics. 71 Risk factors<br />
include the intensity of the anticoagulant effect, epidural<br />
(versus spinal) technique, traumatic needle/catheter<br />
placement, sustained anticoagulation in an indwelling<br />
neuraxial catheter, catheter removal during therapeutic<br />
levels of anticoagulation, increased age, female gender,<br />
concomitant use of anticoagulant or antiplatelet medications,<br />
length of therapy, and twice-daily low-molecularweight<br />
heparin administration. 72 Decreased weight and<br />
concomitant hepatic or renal disease may also exaggerate<br />
the anticoagulant response and theoretically increase the<br />
risk. <strong>The</strong> onset of symptoms immediately postoperatively<br />
is uncommon. Immediate diagnosis of spinal hematoma<br />
is critical because the reported time to progress from new<br />
neurologic deficits to complete paralysis was approximately<br />
15 hours, and complete neurologic recovery was<br />
unlikely if more than 8 hours elapsed between the development<br />
of paralysis and surgical intervention. 73 <strong>The</strong>refore,<br />
any new or progressive neurologic symptoms<br />
occurring in the presence of epidural analgesia warrant<br />
immediate discontinuation of the infusion (with the catheter<br />
left in situ) to rule out any contribution from the<br />
local anesthetic or volume effect. 71 Radiographic imaging,<br />
preferably magnetic resonance imaging, should be<br />
obtained as soon as possible as well as consultation with<br />
a neurosurgeon to determine the urgency of surgery.<br />
When the American Society of <strong>Regional</strong> <strong>Anesthesia</strong><br />
convened for the first Consensus Conference on Neuraxial<br />
<strong>Anesthesia</strong> and Anticoagulation in April 1998,<br />
45 cases of spinal hematoma were associated with<br />
low-molecular-weight heparins, 40 of which involved a<br />
neuraxial anesthetic. Recently, recommendations for<br />
perioperative management of patients receiving lowmolecular-weight<br />
heparin thromboprophylaxis were published<br />
74 based on the consensus statements developed<br />
during the Second American Society of <strong>Regional</strong> <strong>Anesthesia</strong><br />
Consensus Conference on Neuraxial <strong>Anesthesia</strong><br />
and Anticoagulation. 72 Perioperative management of<br />
patients receiving low-molecular-weight heparins requires<br />
coordination and communication. Time intervals between<br />
neuraxial needle placement and administration of<br />
low-molecular-weight heparins must be maintained 74 ;<br />
preoperatively, 10–12 hours should elapse after the<br />
last thromboprophylaxis dose of low-molecular-weight<br />
heparin (enoxaparin 40 mg or dalteparin 5000 U/kg every<br />
24 hours), whereas higher doses require delays of at least<br />
24 hours. Postoperatively, indwelling neuraxial catheters<br />
should be removed at least 10–12 hours after the last dose<br />
of low-molecular-weight heparin, and subsequent dosing<br />
of the drug should take place at least 2 hours after catheter<br />
removal. Other anticoagulants or antiplatelet medications<br />
should be avoided when low-molecular-weight<br />
heparins are used. In contrast to nonsteroidal antiinflammatory<br />
drugs and aspirin, which in and of themselves<br />
do not seem to present significant risk to patients for
362 I. Matot and S. Beyth<br />
developing spinal-epidural hematomas, current practice<br />
is to have patients discontinue clopidogrel for a week and<br />
14 days for ticlopidine before performing a neuroaxial<br />
block. 72,74 Platelet GP IIb/IIIa inhibitors exert a profound<br />
effect on platelet aggregation. After administration, the<br />
time to normal platelet aggregation is 24–48 hours for<br />
abciximab and 4–8 hours for eptifibatide and tirofiban.<br />
Neuraxial techniques should be avoided until platelet<br />
function has recovered. As experience grows with the<br />
newer antithrombotic and/or antiplatelet agents, guidelines<br />
will be revised. Herbal drugs, by themselves, seem<br />
to represent no added significant risk for the development<br />
of spinal hematoma in patients having epidural or<br />
spinal anesthesia.<br />
<strong>The</strong> decision to perform neuraxial blockade on patients<br />
receiving thromboprophylaxis must be made on an individual<br />
basis, while weighing the risk of spinal hematoma<br />
from needle or catheter placement against the benefits<br />
gained. <strong>The</strong> anesthesiologists taking care of these patients<br />
are expected to be familiar with the updated recommendations<br />
for management of this patient population.<br />
Tourniquet-Related Complications<br />
<strong>The</strong> arterial tourniquet is widely used in lower extremity<br />
surgery to reduce blood loss and provide good operating<br />
conditions. <strong>The</strong> local and systemic physiologic effects and<br />
the anesthetic implications were recently reviewed. 75 Use<br />
of arterial tourniquet can be associated with complications<br />
ranging from the minor and self-limiting to the<br />
debilitating and even fatal. Localized complications result<br />
from either tissue compression beneath the cuff or tissue<br />
ischemia distal to the tourniquet. Pressure-related injuries<br />
to the underlying skin, nerve, muscle, and blood<br />
vessels are dependent on both the duration and pressure<br />
of tourniquet inflation. Systemic effects are related to the<br />
inflation or deflation of the tourniquet. Most tourniquetrelated<br />
complications occur as a result of equipment<br />
failure or improper use and are thus easily avoided with<br />
good clinical practice. Tourniquet failure can result in<br />
over-pressurization, causing tissue injury, or underpressurization,<br />
causing loss of hemostasis. Improper cuff<br />
application can result in bruising, blistering, friction burns<br />
to skin, and chemical burns from spirit solutions leaking<br />
under the tourniquet. 76 Results are conflicting from<br />
studies comparing postoperatively measured blood loss,<br />
operating time, need for blood transfusion, postoperative<br />
pain, analgesia requirement, and knee flexion in patients<br />
undergoing TKA with or without the use of tourniquet.<br />
Whereas some authors reported that operations without<br />
the use of a tourniquet cause a greater blood loss and<br />
need for blood transfusion, 77 others show no difference<br />
in operating time or total blood loss and/or blood transfusion.<br />
Furthermore, not using a tourniquet seems to be<br />
associated with significantly less postoperative pain,<br />
earlier knee flexion, fewer superficial wound infections,<br />
and fewer deep vein thromboses. 78–80 <strong>The</strong>se latter studies<br />
question the routine use of a tourniquet during TKA.<br />
Local Effects<br />
High tourniquet pressures directly under the cuff and<br />
prolonged ischemia are implicated in many cases of nerve<br />
and muscle damage, respectively. Arterial injury and skin<br />
damage are uncommon complications but may occur in<br />
patients with peripheral vascular disease and frail skin.<br />
Nerve compression causes intraneural microvascular<br />
abnormalities and edema formation, and these subsequently<br />
compromise local tissue nutrition, resulting in<br />
axonal degeneration. 81 Intracellular creatine phosphate<br />
and adenosine 5′-triphosphate are depleted in muscles<br />
after 2 and 3.5 hours of ischemia, respectively, resulting<br />
in prolonged metabolic recovery of the muscle. 81,82 After<br />
tourniquet release, reperfusion injury of the limb ensues,<br />
with edema and microvascular congestion that lead to the<br />
“post-tourniquet syndrome,” the most common and least<br />
appreciated morbidity associated with tourniquet use. 83<br />
This syndrome is characterized by stiffness, pallor, weakness<br />
without paralysis, and subjective numbness of the<br />
extremity without objective anesthesia. Nerve injuries<br />
associated with the use of tourniquets range from paresthesia<br />
to complete paralysis, but most nerve lesions heal<br />
spontaneously in
24. Total Hip Replacement, Joint Replacement, and Hip Fracture 363<br />
the tourniquet. 88,89 <strong>The</strong>se changes are often resistant to<br />
analgesic drugs and increased depth of anesthesia, and<br />
are described in detail below.<br />
After deflation of the tourniquet and reperfusion<br />
of the ischemic limb, central venous pressure and arterial<br />
blood pressure decrease as a result of a shift of intravascular<br />
volume back into the limb, aggravated by postischemic<br />
reactive hyperemia and the acute effects of ischemic<br />
metabolites released into the systemic circulation.<br />
In selected cases, acute blood loss complicates the<br />
picture. 90<br />
Because of the efflux of hypercapnic venous blood<br />
from an ischemic area into the systemic circulation and<br />
increase in cardiac output, deflation of the tourniquet is<br />
associated with a transient increase in end-tidal carbon<br />
dioxide tension. <strong>The</strong> increase in carbon dioxide tension is<br />
associated with an increase in cerebral blood volume.<br />
Precautions should therefore be taken in treating patients<br />
with increased intracranial pressures (e.g., polytrauma<br />
patients with head injury), and hyperventilation to normocapnia<br />
immediately after tourniquet deflation can<br />
help prevent increased cerebral blood flow velocity and<br />
intracranial pressure. 91–93 Modest increases in arterial<br />
plasma potassium and lactate concentrations, together<br />
with metabolic and respiratory acidosis, are observed<br />
for up to half an hour after tourniquet release, but are of<br />
minor clinical significance. 94<br />
Embolic phenomena (showers of fat, marrow, and<br />
thrombovascular emboli reaching the heart and lungs)<br />
after tourniquet release during TKA have been very well<br />
described. According to Berman et al., 95 immediately<br />
after tourniquet release, echogenic material is seen in the<br />
hearts of all patients. Although well tolerated by most,<br />
this phenomenon may lead to cardiac arrest or fat embolism<br />
syndrome (discussed in the next section) in some<br />
patients. 95–98<br />
<strong>The</strong> pharmacokinetics of anesthetic drugs may be modified<br />
by the use of an arterial tourniquet. Drugs administered<br />
before inflation of the tourniquet cuff may be<br />
sequestered in the isolated limb, then redistributed systemically<br />
after tourniquet deflation; drugs administered<br />
after tourniquet inflation may have altered pharmacokinetics<br />
because of a reduced volume of distribution.<br />
However, except for antibiotics, which should be administered<br />
before tourniquet inflation, the effect of tourniquet<br />
inflation or deflation on pharmacokinetics of drugs<br />
is of limited clinical importance. 99<br />
Recommendations in the literature for both safe tourniquet<br />
time and reperfusion intervals vary. Most authors<br />
suggest that tourniquet inflation should be for the shortest<br />
period possible, with an upper limit of 2 hours in<br />
healthy patients. 75 <strong>The</strong> elderly, trauma patients, and those<br />
with peripheral vascular disease are probably more susceptible<br />
to muscle injury. For surgical procedures longer<br />
than 2 hours, the tourniquet should be deflated every 2<br />
hours to allow 10 minutes of reperfusion of the muscles<br />
beneath and distal to the tourniquet cuff. 81 Because nerve<br />
damage results primarily from direct pressure beneath<br />
the cuff, use of the lowest pressure that causes arterial<br />
occlusion is recommended. Tourniquet pressures more<br />
than 40.0–46.7 kPa (300–350 mm Hg) should rarely be<br />
necessary to produce a bloodless field in normotensive<br />
patients with compliant vessels. However, in patients with<br />
atherosclerosis and the morbidly obese or hypertensive<br />
patients, higher pressures may be required. Common<br />
sense suggests that tourniquet pressure should be based<br />
on the patient’s systolic blood pressure, with the tourniquet<br />
inflated to a pressure of approximately 150 mm Hg<br />
above the systolic pressure. 100,101<br />
Fat Embolism<br />
Fat embolism occurs in almost all lower extremity trauma<br />
and intramedullary surgery, in particular, intramedullary<br />
nailing of long bones, hip arthroplasty, and knee arthroplasty.<br />
Fat emboli syndrome, however, is a severe multisystem<br />
manifestation of embolization that develops in<br />
10%–20% of these patients. 102–106 Overall mortality varies<br />
between 7%–20%, 107,108 and long-term morbidity is<br />
usually attributable to neurologic dysfunction. 109<br />
<strong>The</strong> diagnosis of fat emboli syndrome is clinical, usually<br />
one of exclusion. A high index of suspicion is required for<br />
early clinical diagnosis in at-risk patients. Patients may<br />
present with intraoperative cardiorespiratory collapse<br />
after femoral reaming, 107 insertion of intramedullary<br />
alignment guide 107 or cemented prosthesis, 108 or after<br />
tourniquet release. 103 Hypotension, respiratory dysfunction<br />
with hypoxia, tachycardia, neurologic changes that<br />
may present as diffuse encephalopathy and/or focal<br />
abnormalities, petechiae that are distributed on the upper<br />
body (chest, neck, and conjunctivae), lipuria, and even<br />
electromechanical dissociation may also be presenting<br />
signs. <strong>The</strong>se may develop in the postoperative period.<br />
Laboratory tests should include arterial blood gas,<br />
complete blood count to identify anemia or thrombocytopenia,<br />
and a coagulation profile. 109 Any other treatable<br />
causes of neurologic dysfunction, e.g., toxic, metabolic, or<br />
infectious, must be excluded. 110 Urinalysis may reveal fat<br />
globules, but this is nonspecific. <strong>The</strong> electrocardiogram<br />
may be normal, reflect right heart strain, or may reveal<br />
ischemia. <strong>The</strong> chest radiograph is nonspecific, with diffuse<br />
fluffy bilateral infiltrates and opacities consistent with<br />
increased capillary permeability and edema. 33<br />
Treatment is essentially supportive, consisting of<br />
cardiovascular and respiratory resuscitation and stabilization.<br />
33 No specific drug therapy is currently recommended.<br />
Small prospective randomized controlled studies<br />
of steroid prophylaxis in patients with long bone fractures<br />
have indicated both a decrease in the development<br />
of fat emboli syndrome and a decreased incidence of
364 I. Matot and S. Beyth<br />
hypoxemia in steroid-treated groups compared with<br />
controls. 103,104<br />
Summary<br />
1. Elective THA/TKA is a relatively safe orthopedic procedure.<br />
Known complications include thromboembolism,<br />
postoperative anemia, infection, fractures, and death. Fat<br />
emboli syndrome is an uncommon but devastating complication<br />
with relatively high mortality rate and longterm<br />
morbidity, which is usually attributable to neurologic<br />
dysfunction. Preexisting comorbidities and the American<br />
Society of Anesthesiologists physical status classification<br />
are significantly related to the incidence of postoperative<br />
death. In contrast, fractures of the hip, which most frequently<br />
occur in elderly women, are associated with a<br />
very high mortality. Major causes are cardiac morbidity,<br />
bronchopneumonia, and pulmonary embolism. Patients<br />
who are medically fit for surgery should be operated on<br />
the day of admission. Perioperative management should<br />
be oriented toward adequate pain control and multidisciplinary<br />
consultation, if needed. Patients undergoing<br />
major lower extremity orthopedic surgery should receive<br />
prophylaxis with antibiotics and anticoagulants to reduce<br />
the risk of infection and deep vein thrombosis. <strong>The</strong> decision<br />
to perform neuraxial blockade on patients receiving<br />
thromboprophylaxis should therefore take into account<br />
recent recommendations for management of this patient<br />
population.<br />
2. <strong>The</strong> choice of anesthetic technique is a complex<br />
medical decision that depends on many factors. For hip<br />
fracture patients, the type of anesthesia does not seem to<br />
influence significantly morbidity or overall mortality. For<br />
THA/TKA, there is evidence to suggest that regional<br />
anesthesia may be of benefit because it was associated<br />
with a lower rate of intensive care unit admission postoperatively,<br />
reduced intraoperative blood loss and transfusion<br />
requirements, and was associated with a lower<br />
incidence of thromboembolic events. For all lower extremity<br />
operations, regional analgesia and anesthesia provide<br />
better pain control for the rehabilitation period.<br />
3. Special attention during the operation should be<br />
given to positioning of the patient, blood loss and transfusion<br />
requirements, blood pressure control, fluid management,<br />
careful monitoring and management during cement<br />
insertion and possible associated complications, and to<br />
tourniquet-related complications.<br />
4. For lower limb orthopedic surgery, postoperative<br />
pain is a major problem. Peripheral nerve blocks with or<br />
without a catheter are the techniques of choice.<br />
References<br />
1. Harris WH, Sledge CB. Total hip and total knee replacement.<br />
N Engl J Med 1990;323:725–731.<br />
2. Rauh MA, Krackow KA. In-hospital deaths following<br />
elective total joint arthroplasty. Orthopedics 2004;27(4):<br />
407–411.<br />
3. Dearborn JT, Harris WH. Postoperative mortality after<br />
total hip arthroplasty. An analysis of deaths after two thousand<br />
seven hundred and thirty-six procedures. J Bone Joint<br />
Surg Am 1998;80:1291–1294.<br />
4. Parvizi J, Sullivan TA, Trousdale RT, et al. Thirty-day<br />
mortality after total knee arthroplasty. J Bone Joint Surg<br />
Am 2001;83:1157–1161.<br />
5. Morrison RS, Chassin MR, Siu AL. <strong>The</strong> medical consultant’s<br />
role in caring for patients with hip fracture. Ann<br />
Intern Med 1998;128:1010–1020.<br />
6. O’Hara D, Duff A, Berlin JA, et al. <strong>The</strong> effect of anesthetic<br />
technique on postoperative outcomes on hip fracture<br />
repair. <strong>Anesthesiology</strong> 2000;92:947–957.<br />
7. Myers AH, Robinson EG, Van Natta ML, et al. Hip<br />
fracture among the elderly: factors associated with<br />
inhospital mortality. Am J Epidemiol 1991;134:1128–<br />
1137.<br />
8. Perez JV, Warwick CP, Case CP, et al. Death after proximal<br />
femoral fracture—an autopsy study. Injury 1995;26(4):237–<br />
240.<br />
9. Scheinin H, Virtanen T, Kentala E, et al. Epidural infusion<br />
of bupivacaine and fentanyl reduces perioperative myocardial<br />
ischaemia in elderly patients with hip fracture—a<br />
randomized controlled trial. Acta Anaesthesiol Scand<br />
2000;44:1061–1070.<br />
10. Matot I, Oppenheim-Eden A, Ratrot R, et al. Preoperative<br />
cardiac events in elderly patients with hip fracture<br />
randomized to epidural or conventional analgesia. <strong>Anesthesiology</strong><br />
2003;98(1):156–163.<br />
11. Casaletto JA, Gatt R. Post-operative mortality related to<br />
waiting time for hip fracture surgery. Injury 2004;35(2):114–<br />
120.<br />
12. Sutcliffe AJ, Parker M. Mortality after spinal and general<br />
anaesthesia for surgical fixation of hip fracture. Anaesthesia<br />
1994;49:237–240.<br />
13. Sorenson RM, Pace NL. Anesthetic techniques during<br />
surgical repair of femoral neck fractures. A meta-analysis.<br />
<strong>Anesthesiology</strong> 1992;77:1095–1104.<br />
14. Zuckerman JD, Skovron ML, Koval KJ, et al. Postoperative<br />
complications and mortality associated with operative<br />
delay in older patients who have a fracture of the hip.<br />
J Bone Joint Surg Am 1995;77(10):1551–1556.<br />
15. Rogers FB, Shackford SR, Keller MS. Early fixation<br />
reduces morbidity and mortality in elderly patients with<br />
hip fractures from low impact falls. J Trauma 1995;39(2):<br />
261–265.<br />
16. Grimes JP, Gregory PM, Noveck H, et al. <strong>The</strong> effect of<br />
time-to-surgery on mortality and morbidity in patients<br />
following hip fracture. Am J Med 2002;112:702–709.<br />
17. Urwin SC, Parker MJ, Griffiths R. General versus<br />
regional anaesthesia for hip fracture surgery: a metaanalysis<br />
of randomized trials. Br J Anaesth 2000;84:450–<br />
455.<br />
18. Gilbert TB, Hawkes WG, Hebel JR, et al. Spinal anesthesia<br />
versus general anesthesia for hip fracture repair: a longitudinal<br />
observation of 741 elderly patients during 2-year<br />
follow-up. Am J Orthop 2000;29:25–35.
24. Total Hip Replacement, Joint Replacement, and Hip Fracture 365<br />
19. Lien CA. <strong>Regional</strong> versus general anesthesia for hip<br />
surgery in older patients: does the choice affect patient<br />
outcome? J Am Geriatr Soc 2002;50:191–194.<br />
20. Parker MJ, Handoll HH, Griffiths R. Anaesthesia for hip<br />
fracture surgery in adults. Cochrane Database Syst Rev<br />
2001(4):CD000521.<br />
21. Parker MJ, Griffiths R, Appadu BN. Nerve blocks<br />
(subcostal, lateral cutaneous, femoral, triple, psoas) for<br />
hip fractures. Cochrane Database Syst Rev 2002(1):<br />
CD001159.<br />
22. Kaufmann SC, Wu CL, Pronovost PJ, et al. <strong>The</strong> associa -<br />
tion of intraoperative neuroaxial anesthesia on anticipated<br />
admission to the intensive care unit. J Clin Anesth 2002;<br />
14:432–436.<br />
23. McQueen DA, Kelly HK, Wright TF. A comparison of<br />
epidural and non-epidural anesthesia and analgesia in<br />
total hip or knee arthroplasty patients. Orthopedics 1992;<br />
15:169–173.<br />
24. Modig J, Karistrom G. Intra- and post-operative blood loss<br />
and haemodynamics in total hip replacement when performed<br />
under lumbar epidural versus general anaesthesia.<br />
Eur J Anaesthesiol 1987;4:345–355.<br />
25. Twyman R, Kirwan T, Fennelly M. Blood loss reduced<br />
during hip arthroplasty by lumbar plexus block. J Bone<br />
Joint Surg Br 1990;72:770–771.<br />
26. Stevens RD, Van Gessel E, Flory N, et al. Lumber plexus<br />
block reduces pain and blood loss associated with total hip<br />
arthroplasty. <strong>Anesthesiology</strong> 2000;93:115–121.<br />
27. Mitchell D, Friedman RJ, Baker JD, et al. Prevention of<br />
thromboembolic disease following total knee arthroplasty.<br />
Epidural versus general anesthesia. Clin Orthop Relat Res<br />
1991;(269):109–112.<br />
28. Modig J, Borg T, Karistrom G, et al. Thromboembolism<br />
after total hip replacement: role of epidural and general<br />
anesthesia. Anesth Analg 1983;62:174–180.<br />
29. Hollmann MW, Wieczorek KS, Smart M, et al. Epidural<br />
anesthesia prevents hypercoagulation in patients undergoing<br />
major orthopedic surgery. Reg Anesth Pain Med 2001;<br />
26(3):215–222.<br />
30. Laskin RS. Total knee replacement in patients older than<br />
85 years. Clin Orthop 1999;367:43–49.<br />
31. Williams-Russo P, Sharrock NE, Haas SB, et al. Randomized<br />
trial of epidural versus general anesthesia: outcomes<br />
after primary total knee replacement. Clin Orthop 1996;<br />
331:199–208.<br />
32. Williams-Russo P, Sharrock NE, Mattis S, et al. Cognitive<br />
effects after epidural vs general anesthesia in older adults.<br />
A randomized trial. JAMA 1995;274(1):44–50.<br />
33. Jenkins K, Chung F, Wennberg R, et al. Fat embolism<br />
syndrome and elective knee arthroplasty. Can J Anaesth<br />
2002;49:19–24.<br />
34. Enneking FK. Cardiac arrest during total knee replacement<br />
using a long-stem prosthesis. J Clin Anesth 1995;<br />
7:253–263.<br />
35. Hedenstierna G, Mebius C, Bygdeman S. Ventilationperfusion<br />
relationship during hip arthroplasty. Acta<br />
Anaesthesiol Scand 1983;27:56–61.<br />
36. Fallon KM, Fuller JG, Morley-Forster P. Fat embolization<br />
and fatal cardiac arrest during hip arthroplasty with methylmethacrylate.<br />
Can J Anaesth 2001;48:626–629.<br />
37. Ereth MH, Weber JG, Abel MD, et al. Cemented vs. noncemented<br />
total hip arthroplasty: embolism, hemodynamics,<br />
and intrapulmonary shunting. Mayo Clin Proc 1992;<br />
67:1066–1074.<br />
38. Bengtson A, Larsson M, Gammer W, et al. Anaphylatoxin<br />
release in association with methylmethacrylate fixation of<br />
hip prostheses. J Bone Joint Surg Am 1987;69A:46–49.<br />
39. Dahl OE, Garvik LJ, Lyberg T. Toxic effects of methylmethacrylate<br />
monomer on leucocytes and endothelial cells<br />
in vitro. Acta Orthop Scand 1994;65:147–153.<br />
40. Breed AL. Experimental production of vascular hypotension,<br />
and bone marrow and fat embolism with methylmethacrylate<br />
cement. Traumatic hypertension of bone.<br />
Clin Orthop 1974;102:227–244.<br />
41. Tronzo RG, Kallos T, Wyche MQ. Elevation of intramedullary<br />
pressure when methylmethacrylate is inserted in total<br />
hip arthroplasty. J Bone Joint Surg 1974;56A:714–718.<br />
42. Pitto RP, Kößler M. <strong>The</strong> relevance of the drainage along<br />
the linea aspera for the reduction of fat embolism in<br />
cemented total hip replacement. J Bone Joint Surg 1997;<br />
79B(Suppl II):169–170.<br />
43. Wenda K, Runkel M, Degreif J, et al. Pathogenesis and<br />
clinical relevance of bone marrow embolism in medullary<br />
nailing. Injury 1993;24(Suppl 3):73–81.<br />
44. Woo R, Minster GJ, Fitzgerald RH Jr, et al. Pulmonary fat<br />
embolism in revision hip arthroplasty. Clin Orthop 1995;<br />
319:41–53.<br />
45. Berman AT, Price HL, Hahn JF. <strong>The</strong> cardiovascular<br />
effects of methylmethacrylate in dogs. Clin Orthop 1974;<br />
100:265–269.<br />
46. Lotke PA, Faralli VJ, Orenstein EM, et al. Blood loss after<br />
total knee replacement. J Bone Joint Surg Am 1999;73A:<br />
1037–1040.<br />
47. Sehat KR, Evans R, Newman JH. How much blood is<br />
really lost in total knee arthroplasty? Correct blood loss<br />
management should take hidden loss into account. Knee<br />
2000;7(3):151–155.<br />
48. Toy PT, Kaplan EB, McVay PA, et al. Blood loss and<br />
replacement in total hip arthroplasty: a multicenter study.<br />
<strong>The</strong> Preoperative Autologous Blood Donation Study<br />
Group. Transfusion 1992;32(1):63–67.<br />
49. Bierbaum BE, Callaghan JJ, Galante JO, et al. An analysis<br />
of blood management in patients having a total hip or knee<br />
arthroplasty. J Bone Joint Surg Am 1999;81(1):2–10.<br />
50. Churchill WH, McGurk S, Chapman RH, et al. <strong>The</strong> Collaborative<br />
Hospital Transfusion Study: variations in use of<br />
autologous blood account for hospital differences in red<br />
cell use during primary hip and knee surgery. Transfusion<br />
1998;38(6):530–539.<br />
51. Halm EA, Wang JJ, Boockvar K, et al. Effects of blood<br />
transfusion on clinical and functional outcomes in patients<br />
with hip fracture. Transfusion 2003;43(10):1358–1367.<br />
52. Tenholder M, Cushner FD. Intraoperative blood management<br />
in joint replacement surgery. Orthopedics 2004;27(6<br />
Suppl):S663–668.<br />
53. Singelyn FJ, Capdevila X. <strong>Regional</strong> anaesthesia for orthopaedic<br />
surgery. Curr Opin Anaesthesiol 2001;14:733–740.<br />
54. Singelyn F, Gouverneur JM. Postoperative analgesia after<br />
total hip arthroplasty: IV PCA with morphine, patientcontrolled<br />
epidural analgesia, or continuous “3-in-1 block”:
366 I. Matot and S. Beyth<br />
a prospective evaluation by our acute pain service in more<br />
than 1300 patients. J Clin Anesth 1999;11:550–554.<br />
55. Capdevila X, Barthelet Y, Biboulet P, et al. Effects of perioperative<br />
analgesic technique on the surgical outcome and<br />
duration of rehabilitation after major knee surgery. <strong>Anesthesiology</strong><br />
1999;91:8–15.<br />
56. Singelyn F, Deyaert M, Joris D, et al. Effects of intravenous<br />
patient-controlled analgesia with morphine, continuous<br />
epidural analgesia, and continuous three-in-one block on<br />
postoperative pain and knee rehabilitation after unilateral<br />
total knee arthroplasty. Anesth Analg 1998;87:88–92.<br />
57. Chelly J, Greger J, Gebhard R, et al. Continuous femoral<br />
blocks improve recovery and outcome of patients undergoing<br />
total knee arthroplasty. J Arthroplasty 2001;16:436–<br />
445.<br />
58. Allen H, Liu S, Ware P, et al. Peripheral nerve blocks<br />
improve analgesia after total knee replacement surgery.<br />
Anesth Analg 1998;87:93–97.<br />
59. Ganapathy S, Wasserman R, Watson J, et al. Modified continuous<br />
femoral three-in-one block for postoperative pain<br />
after total knee arthroplasty. Anesth Analg 1999;88:1197–<br />
1202.<br />
60. Singelyn F, Gouverneur JM. Extended ‘three-in-one’’<br />
block after total knee arthroplasty: continuous versus<br />
patient-controlled techniques. Anesth Analg 2000;91:176–<br />
180.<br />
61. Singelyn F, Vanderelst P, Gouverneur JM. Extended<br />
femoral nerve sheath block after total hip arthroplasty:<br />
continuous versus patient-controlled techniques. Anesth<br />
Analg 2001;92:455–459.<br />
62. Macalou D, Trueck S, Meuret P, et al. Postoperative analgesia<br />
after total knee replacement: the effect of an obturator<br />
nerve block added to the femoral 3-in-1 nerve block.<br />
Anesth Analg 2004;99:251–254.<br />
63. Davies AF, Segar EP, Murdoch J, et al. Epidural infusion<br />
or combined femoral and sciatic nerve blocks as perioperative<br />
analgesia for knee arthroplasty. Br J Anaesth<br />
2004;93(3):368–374.<br />
64. Kaloul I, Guay J, Cote C, et al. <strong>The</strong> posterior lumbar plexus<br />
(psoas compartment) block and the three-in-one femoral<br />
nerve block provide similar postoperative analgesia after<br />
total knee replacement. Can J Anaesth 2004;51:45–51.<br />
65. Mansour N, Bennetts F. An observational study of combined<br />
continuous lumbar plexus and single-shot sciatic<br />
nerve blocks for post-knee surgery analgesia. Reg Anesth<br />
Pain Med 1996;21:287–291.<br />
66. Picard P, Tramer M, McQuay H, et al. Analgesic efficacy of<br />
peripheral opioids (all except intra-articular): a qualitative<br />
systematic review of randomized controlled trials. Pain<br />
1997;72:309–318.<br />
67. Geerts WH, Heit JA, Clagett GP, et al. Prevention of<br />
venous thromboembolism. Chest 2001;119:132–175.<br />
68. Haas S. Deep vein thrombosis: beyond the operating table.<br />
Orthopedics 2000;23(Suppl 6):S629–S632.<br />
69. Sixth American College of Chest Physicians (ACCP)<br />
Consensus Conference on Antithrombotic <strong>The</strong>rapy. Chest<br />
2004;126(3 Suppl).<br />
70. Hollman MW, Durieux ME. Local anesthetics and the<br />
inflammatory response: a new therapeutic indication?<br />
<strong>Anesthesiology</strong> 2000;93:858–875.<br />
71. Horlocker TT. What’s a nice patient like you doing with<br />
a complication like this? Diagnosis, prognosis and prevention<br />
of spinal hematoma. Can J Anaesth 2004;51:<br />
527–534.<br />
72. Horlocker TT, Wedel DJ, Benzon H, et al. <strong>Regional</strong> anesthesia<br />
in the anticoagulated patient: defining the risks (<strong>The</strong><br />
Second ASRA Consensus Conference on Neuraxial <strong>Anesthesia</strong><br />
and Anticoagulation). Reg Anesth Pain Med 2003;<br />
28(3):172–197.<br />
73. Vandermeulen EP, Van Aken H, Vermylen J. Anticoagulants<br />
and spinal-epidural anesthesia. Anesth Analg 1994;<br />
79:1165–1177.<br />
74. Horlocker TT. Thromboprophylaxis and neuroaxial anesthesia.<br />
Orthopedics 2003;26(2):243–248.<br />
75. Kam PC, Kavanagh R, Yoong FF. <strong>The</strong> arterial tourniquet:<br />
pathophysiological consequences and anaesthetic implications.<br />
Anaesthesia 2001;56(6):534–545.<br />
76. Carter K, Shaw A, Telfer ABM. Tourniquets for surgery:<br />
safety aspects. J Med Eng Technol 1983;7:136–139.<br />
77. Vandenbussche E, Duranthon LD, Couturier M, et al. <strong>The</strong><br />
effect of tourniquet use in total knee arthroplasty. Int<br />
Orthop 2002;26(5):306–309.<br />
78. Tetro AM, Rudan JF. <strong>The</strong> effects of a pneumatic tourniquet<br />
on blood loss in total knee arthroplasty. Can J Surg 2001;<br />
44(1):33–38.<br />
79. Abdel-Salam A, Eyres KS. Effects of tourniquet during<br />
total knee arthroplasty. A prospective randomised study.<br />
J Bone Joint Surg Br 1995;77(2):250–253.<br />
80. Jarolem KL, Scott DF, Jaffe WL, et al. A comparison of<br />
blood loss and transfusion requirements in total knee<br />
arthroplasty with and without arterial tourniquet. Am<br />
J Orthop 1995;24(12):906–909.<br />
81. Newman RJ. Metabolic effects of tourniquet ischaemia<br />
studied by nuclear magnetic resonance spectroscopy.<br />
J Bone Joint Surg Br 1984;66:434–440.<br />
82. Wilgis EFS. Observations on the effects of tourniquet ischaemia.<br />
J Bone Joint Surg Am 1971;53:1343–1346.<br />
83. Mohler LR, Pedowitz RA, Lopez MA, et al. Effect of<br />
tourniquet compression of neuromuscular function. Clin<br />
Orthop 1999;359:213–220.<br />
84. Hodgson AJ. A proposed etiology for tourniquet-induced<br />
neuropathies. J Biomech Eng 1994;116:224–227.<br />
85. Palmer SH, Graham G. Tourniquet-induced rhabdomyolysis<br />
after total knee replacement. Ann R Coll Surg Engl<br />
1994;76:416–417.<br />
86. Kaufman RD, Walts LF. Tourniquet induced hypertension.<br />
Br J Anaesth 1982;54:333–336.<br />
87. Bradford EMW. Haemodynamic changes associated with<br />
the application of lower limb tourniquets. Anaesthesia<br />
1969;24:190–197.<br />
88. Valli H, Rosenberg PH, Kytta J, et al. Arterial hypertension<br />
associated with the use of a tourniquet with either general<br />
or regional anaesthesia. Acta Anaesthesiol Scand 1987;31:<br />
279–283.<br />
89. Gielen MJ, Stienstra R. Tourniquet hypertension and<br />
its prevention: a review. Reg Anesth 1991;16:191–<br />
194.<br />
90. Townsend HS, Goodman SB, Schurman DJ, et al. Tourniquet<br />
release: systemic and metabolic effects. Acta Anaesthesiol<br />
Scand 1996;40:1234–1237.
24. Total Hip Replacement, Joint Replacement, and Hip Fracture 367<br />
91. Kadoi Y, Ide M, Saito S, et al. Hyperventilation after tourniquet<br />
deflation prevents an increase in cerebral flow<br />
velocity. Can J Anaesth 1999;46:259–264.<br />
92. Lam AM, Slee T, Hirst R, et al. Cerebral blood flow velocity<br />
following tourniquet release in humans. Can J Anaesth<br />
1990;37:S29.<br />
93. Sparling RJ, Murray AW, Choksey M. Raised intracranial<br />
pressure associated with hypercarbia after tourniquet<br />
release. Br J Neurosurg 1993;7:75–78.<br />
94. Kokki H, Vaatainen U, Pantila J. Metabolic effects of a low<br />
pressure tourniquet system compared with a high pressure<br />
tourniquet system in arthroscopic anterior crucial ligament<br />
reconstruction. Acta Anaesthesiol Scand 1998;42:<br />
418–424.<br />
95. Berman AT, Parmet JL, Harding SP, et al. Emboli observed<br />
with use of transesophageal echocardiography immediately<br />
after tourniquet release during total knee arthroplasty with<br />
cement. J Bone Joint Surg Am 1998;80:389–396.<br />
96. Parmet JL, Berman AT, Horrow JC, et al. Thromboembolism<br />
coincident with tourniquet deflation during total knee<br />
arthroplasty. Lancet 1993;341:1057–1058.<br />
97. McGrath BJ, Hsia J, Boyd A, et al. Venous embolization<br />
after deflation of lower extremity tourniquets. Anesth<br />
Analg 1994;78:349–353.<br />
98. Morawa LG, Manley MT, Edidin AA, et al. Transesophageal<br />
echocardiographic monitored events during total<br />
knee arthroplasty. Clin Orthop 1996;331:192–198.<br />
99. Barnette RE, Eriksson LI, Cooney GF, et al. Sequestration<br />
of vecuronium bromide during extremity surgery involving<br />
use of a pneumatic tourniquet. Acta Anaesthesiol<br />
Scand 1997;41:49–54.<br />
100. Shaw JA, Murray DG. <strong>The</strong> relationship between tourniquet<br />
pressure and underlying soft-tissue pressure in the<br />
thigh. J Bone Joint Surg Am 1982;64:1148–1152.<br />
101. Van Roekel HE, Thurston AJ. Tourniquet pressure: the<br />
effect of limb circumference and systolic blood pressure.<br />
J Hand Surg (Br) 1985;10:142–144.<br />
102. Fabian TC, Hoots AV, Stanford DS, et al. Fat embolism<br />
syndrome: prospective evaluation in 92 fracture patients.<br />
Crit Care Med 1990;18:42–46.<br />
103. Kallenbach J, Lewis M, Zaltzman M, et al. “Low-dose”<br />
corticosteroid prophylaxis against fat embolism. J Trauma<br />
1987;27:1173–1176.<br />
104. Lindeque BGP, Schoeman HS, Dommisse GF, et al.<br />
Fat embolism and the fat embolism syndrome. A doubleblind<br />
therapeutic study. J Bone Joint Surg Br 1987;69:<br />
128–131.<br />
105. Schonfeld SA, Ploysongsang Y, DiLisio R, et al. Fat<br />
embolism prophylaxis with corticosteroids. A prospective<br />
study in high-risk patients. Ann Intern Med 1983;99:438–<br />
443.<br />
106. Bulger EM, Smith DG, Maier RV, et al. Fat embolism syndrome.<br />
A 10-year review. Arch Surg 1997;132:435–439.<br />
107. Robert JH, Hoffmeyer P, Broquet PE, et al. Fat embolism<br />
syndrome. Orthop Rev 1993;22:567–571.<br />
108. Johnson MJ, Lucas GL. Fat embolism syndrome. Orthopedics<br />
1996;19:41–50.<br />
109. Byrick RJ. Fat embolism and postoperative coagulopathy<br />
[editorial]. Can J Anaesth 2001;48:618–621.<br />
110. Jacobsen DM, Terrance CF, Reinmuth OM. <strong>The</strong> neurologic<br />
manifestations of fat embolism. Neurology 1986;36:847–<br />
851.
25<br />
Transurethral Prostatectomy Syndrome and<br />
Other Complications of Urologic Procedures<br />
Daniel M. Gainsburg<br />
Elderly patients undergo numerous urologic procedures.<br />
This chapter presents some of the more common<br />
concerns and complications associated with these<br />
procedures.<br />
<strong>The</strong> Transurethral Prostatectomy<br />
Syndrome<br />
Transurethral prostatectomy (TURP) is considered the<br />
gold standard for the surgical treatment of benign prostatic<br />
hyperplasia (BPH). 1 During the past decade, the<br />
annual number of TURPs performed in the United States<br />
has declined from 400,000 to 100,000 because of advances<br />
in medical management, the introduction of minimally<br />
invasive thermal therapies (laser, radiofrequency, and<br />
microwave), 2 and the development of patient-care guidelines<br />
for patients with BPH. 3<br />
BPH is the most common nonmalignant tumor of the<br />
prostate, causing urinary symptoms in more than 50% of<br />
the aging male population. 4 TURP patients, who are often<br />
elderly, tend to have coexisting problems of which the<br />
most common are pulmonary (14.5%), gastrointestinal<br />
(13.2%), myocardial infarction (12.5%), arrhythmia<br />
(12.4%), and renal insufficiency (4.5%). 5 <strong>The</strong>refore, these<br />
patients should be carefully evaluated preoperatively to<br />
determine the status of any coexisting diseases.<br />
Complications of TURP include (1) absorption of irrigating<br />
solution; (2) circulatory overload, hyponatremia,<br />
and hypoosmolality; (3) glycine and ammonia toxicity; (4)<br />
bladder perforation; (5) transient bacteremia and septicemia;<br />
(6) hypothermia; (7) bleeding and coagulopathy;<br />
and 8) TURP syndrome. 6 <strong>The</strong> 30-day mortality rate of<br />
TURP is reported to be between 0.2% and 0.8%. 5<br />
Common causes of death include myocardial infarction,<br />
pulmonary edema, and renal failure. 7 <strong>The</strong> postoperative<br />
morbidity rate was noted to be 18% and increased morbidity<br />
was found in patients with resection times exceeding<br />
90 minutes, gland size greater than 45 g, acute urinary<br />
retention, and age older than 80 years. 5 TURP syndrome<br />
is a general term used to describe a collection of signs<br />
and symptoms caused primarily by excessive absorption<br />
of irrigating fluid through the opened venous sinuses of<br />
the prostate.<br />
<strong>The</strong> Surgical Procedure<br />
TURP is performed by inserting a resectoscope through<br />
the urethra and resecting prostatic tissue in an orderly<br />
manner with an electrically powered cutting-coagulating<br />
metal loop. Prostatic tissue is then resected without perforating<br />
the prostatic capsule. If the capsule is violated,<br />
large amounts of irrigation solution may be absorbed into<br />
the circulation, and the periprostatic and retroperitoneal<br />
spaces. 6,8 It is this rapid absorption of irrigation solution<br />
into the circulation that differentiates this complication<br />
from that of bladder perforation. (See also the section on<br />
Bladder Perforation.) Prostatic capsular perforation<br />
occurs in about 2% of patients and presents with symptoms<br />
of restlessness, nausea, vomiting, and abdominal<br />
pain—even under spinal anesthesia. 1 If perforation is suspected,<br />
the operation should be terminated as quickly as<br />
possible and hemostasis obtained. 1<br />
Bleeding often occurs during TURP, but is usually controllable.<br />
Arterial bleeding is controlled by electrocoagulation.<br />
1 However, when large venous sinuses are opened,<br />
hemostasis becomes difficult. If this venous bleeding<br />
becomes uncontrollable, the procedure should be terminated<br />
as quickly as possible, and a Foley catheter should<br />
be inserted into the bladder and traction applied. 6,8<br />
Attempts at estimating blood loss during TURP are<br />
usually extremely inaccurate, because the shed blood is<br />
mixed with ample amounts of irrigating solution. Intraoperative<br />
blood loss has been estimated to range from 2<br />
to 4 mL/min of resection time and 20 to 50 mL/g of prostate<br />
tissue. 9 Bleeding requiring transfusion occurs in 2.5%<br />
of patients undergoing TURP. 5<br />
368
25. Transurethral Prostatectomy Syndrome 369<br />
Even though they cause no significant hemolysis, ex -<br />
Table 25-1. Osmolality of various irrigation solutions used for<br />
transparency. 2,8 ventricular ectopy are often observed. 9,20<br />
transurethral prostatectomy.<br />
cessive absorption of modern irrigation solutions can<br />
Solution Concentration (%) Osmolality (mOsm/kg) be associated with numerous perioperative complications,<br />
including circulatory overload, hyponatremia, and<br />
Glycine 1.2 175<br />
Glycine 1.5 220 hypoosmolality. Additionally, the solutes in the solutions<br />
Cytal 178 may cause adverse effects: glycine may cause cardiac,<br />
Mannitol 5 275 neurologic, and retinal effects 8,12,13 ; mannitol rapidly<br />
Sorbitol 3.5 165 expands intravascular volume and might lead to pulmonary<br />
edema in cardiac patients 6 ; sorbitol is converted to<br />
Glucose 2.5 139<br />
Urea 1 167<br />
Water 0 fructose and lactate, which may cause hyperglycemia and/<br />
or lactic acidosis 14 ; and glucose may cause severe hyperglycemia<br />
in the diabetic patient. 15<br />
Irrigation Solutions<br />
<strong>The</strong> ideal irrigating solution for use during TURP would<br />
be isotonic, nonhemolytic, electrically inert, transparent,<br />
nonmetabolized, nontoxic, rapidly excreted, and inexpensive.<br />
Originally, distilled water was the fluid of choice<br />
because it was nonconductive and transparent. However,<br />
its absorption into the circulation caused massive hemolysis,<br />
dilutional hyponatremia, rare renal failure, and central<br />
nervous system (CNS) symptoms. 6,11<br />
<strong>The</strong>se complications eventually led to abandonment of<br />
distilled water and to the use of isosmotic or nearly isosmotic<br />
solutions for TURP. Solutions such as normal saline<br />
and Ringer’s lactate are isosmotic and would be well<br />
tolerated if absorbed intravascularly; however, they are<br />
highly ionized and cause dispersion of the high-frequency<br />
current from the resectoscope. Recently, in a small study,<br />
normal saline was used as the irrigating solution in which<br />
a bipolar electrocautery resectoscope replaced the customary<br />
monopolar resectoscope. None of the patients<br />
developed hyponatremia or TURP syndrome. 2<br />
<strong>The</strong> introduction of nonconductive and also nonhemolytic<br />
solutions, such as glycine, Cytal (a mixture of sorbitol<br />
2.7% and mannitol 0.54%), sorbitol, mannitol, glucose,<br />
and urea, have replaced distilled water (Table 25-1). 6,8<br />
Glycine and Cytal are currently the two most frequently<br />
used solutions. 6 Although all are nonconductive solu -<br />
tions that allow for electrocautery resection, they are<br />
purposely prepared moderately hypotonic to maintain<br />
Signs and Symptoms<br />
TURP syndrome may occur anytime intraoperatively or<br />
postoperatively. It has been observed as early as a few<br />
minutes after the start of surgery 16 and as late as several<br />
hours after completion of surgery. 17 Recent reports noted<br />
that TURP syndrome occurs in 2% of patients. 5,18<br />
Clinical manifestations of TURP syndrome include<br />
neurologic, cardiovascular, and respiratory effects (Table<br />
25-2). <strong>The</strong> effects on the CNS include headache, dizziness,<br />
restlessness, agitation, confusion, seizures, and eventually<br />
coma. <strong>The</strong> clinical picture may be further compounded<br />
by the neurotoxic effects of glycine and ammonia. 6 TURP<br />
syndrome is usually described as being caused by hyponatremia<br />
and water intoxication. It is now thought that<br />
the classic CNS effects of TURP syndrome are not caused<br />
by hyponatremia, in itself, but are caused by the acute<br />
decrease in serum osmolality that results in the development<br />
of cerebral edema. 19,20<br />
Cardiovascular and respiratory effects occur from<br />
volume overload and hyponatremia. Acute hypervolemia<br />
will initially cause hypertension and bradycardia, which<br />
may progress to congestive heart failure, pulmonary<br />
edema, and cardiac arrest. 21 Rapidly decreasing serum<br />
sodium levels are associated with negative inotropic<br />
effects on the heart manifesting in hypotension, pulmonary<br />
edema, and congestive heart failure. 9,20 Electrocardiogram<br />
changes, such as widened QRS complexes and<br />
Table 25-2. Signs and symptoms of transurethral prostatectomy syndrome.<br />
Cardiovascular and respiratory Central nervous system Metabolic Other<br />
Hypertension Restlessness Hyponatremia Hypoosmolality<br />
Pulmonary edema Agitation Hyperglycinemia Hemolysis<br />
Congestive heart failure Confusion Hyperammonemia<br />
Hypotension<br />
Seizures<br />
Arrhythmias<br />
Coma<br />
Respiratory arrest<br />
Blindness<br />
Cardiac arrest
370 D.M. Gainsburg<br />
Absorption of Irrigating Solution<br />
Excessive absorption of irrigating solution through<br />
opened venous sinuses of the prostate is the primary<br />
cause of TURP syndrome. <strong>The</strong> amount of absorption correlates<br />
with (1) the height of the irrigating fluid above the<br />
patient which determines hydrostatic pressure, (2) amount<br />
of distention of the bladder by the surgeon, (3) extent of<br />
opened venous sinuses, and (4) the length of time of<br />
resection. 22 <strong>The</strong> average rate of fluid absorption is 10–30<br />
mL/min of resection time and as much as 8 L may be<br />
absorbed during a procedure. 6 A quick estimation of fluid<br />
volume absorbed, which compares serum sodium levels<br />
before and after the procedure, can be made by using the<br />
following equation:<br />
Volume absorbed<br />
= {(preoperative [Na + ]/postoperative [Na + ]) × ECF} − ECF<br />
where extracellular fluid (ECF) volume comprises<br />
20%–30% of body weight. 8,23<br />
Circulatory Overload, Hyponatremia,<br />
and Hypoosmolality<br />
<strong>The</strong> replacement of distilled water with the present generation<br />
of irrigating solutions has eliminated hemolysis<br />
as a complication of TURP. At the same time, there has<br />
been a decrease in the incidence of severe CNS complications<br />
associated with hyponatremia. 20 However, excessive<br />
absorption of irrigating solution still occurs and leads to<br />
circulatory overload. Initially, hypertension and bradycardia<br />
are seen with acute volume overload, which may<br />
progress to congestive heart failure, pulmonary edema,<br />
and eventually cardiac arrest. 21<br />
<strong>The</strong> classic CNS signs of TURP syndrome are now<br />
thought to be caused by acute serum hypoosmolality,<br />
movement of water into the cells, and consequent cerebral<br />
edema. 19,20 With the use of solute-based nearly isosmotic<br />
solutions, the incidence of severe CNS symptoms<br />
has been reduced because acute serum hypoosmolality<br />
does not occur; however, CNS symptoms can still occur<br />
secondary to hyponatremia. 19,20<br />
Sodium is an electrolyte that is essential for the ability<br />
of excitable cells, particularly those of the heart and brain,<br />
to depolarize and produce an action potential. 6,8 With<br />
acute decreases in serum sodium levels to 120 mEq/L,<br />
CNS symptoms and cardiovascular effects are observed<br />
(Table 25-3). 8,14 Initially, confusion and restlessness are<br />
noted, and with decreasing serum sodium levels, may<br />
progress to loss of consciousness and seizures. 24 Rapidly<br />
decreasing serum sodium levels are associated with hypotension,<br />
pulmonary edema, congestive heart failure, and<br />
electrocardiogram changes. At levels near 100 mEq/L,<br />
respiratory and cardiac arrest may occur. 24,25 Acute changes<br />
in serum sodium levels are more harmful than chronic<br />
hyponatremia. 26 Also, it is often impossible to separate<br />
these symptoms of cardiovascular compromise secondary<br />
to hyponatremia from those caused by fluid overload.<br />
Glycine and Ammonia Toxicity<br />
Glycine is a nonessential amino acid. When absorbed in<br />
significant amounts, glycine may cause cardiac and neurologic<br />
effects. 8,12,13 It is metabolized in the liver into<br />
ammonia and glyoxylic acid. 12 <strong>The</strong> cardiac effect of glycine<br />
is myocardial depression; the mechanism is unknown. 27<br />
Glycine has been implicated as the cause of transient<br />
blindness in TURP patients. It acts as an inhibitory neurotransmitter<br />
in the brain, spinal cord, and retina. Centrally<br />
acting mechanisms, such as cerebral edema, may<br />
cause visual impairment, but these patients have normal<br />
papillary light reflexes. In contrast, TURP patients with<br />
transient blindness have sluggish or nonreactive pupils,<br />
suggesting a retinal effect. <strong>The</strong>refore, TURP blindness<br />
may be caused by increased glycine levels exerting an<br />
inhibitory effect on the retina. 28,29<br />
Signs of ammonia toxicity, nausea and vomiting, usually<br />
occur within 1 hour after surgery. With increasing<br />
ammonia levels, the patient lapses into a coma lasting<br />
about 10–12 hours, and then awakens as the ammonia<br />
levels decrease below 150 µmol/L. 8 A possible explanation<br />
for hyperammonemia in TURP patients is arginine<br />
deficiency. Ammonia is metabolized to urea in the liver,<br />
in a reaction that requires arginine. Patients who are<br />
Table 25-3. Signs and symptoms associated with acute hyponatremia.<br />
Serum Na + (mEq/L) Central nervous system changes Cardiovascular effects Electrocardiogram changes<br />
25. Transurethral Prostatectomy Syndrome 371<br />
arginine deficient are unable to convert the excess<br />
ammonia created in the body when glycine solutions are<br />
absorbed, therefore leading to hyperammonemia. 30,31<br />
Bladder Perforation<br />
Accidental perforation of the bladder is another common<br />
complication of TURP with an incidence of approximately<br />
1% and most perforations occurring retroperitoneally.<br />
(See also the section on Transurethral Resection<br />
of Bladder Tumors.) It usually results from surgical instrumentation<br />
or overdistension of the bladder with irrigating<br />
fluid. An early sign of perforation, often unnoticed, is<br />
a decrease in return of irrigating solution from the<br />
bladder. Eventually, a significant volume of fluid will<br />
accumulate in the abdomen causing abdominal distention:<br />
patients under regional anesthesia may start to complain<br />
of abdominal pain and/or experience nausea and<br />
vomiting. Other clinical signs are hypotension followed<br />
by hypertension. Symptoms of intraperitoneal perforation<br />
are similar, develop sooner, and include severe<br />
shoulder pain secondary to diaphragmatic irritation.<br />
Diagnosis of bladder perforation is made by cystourethrography<br />
and treated with a suprapubic cystotomy. 8<br />
Transient Bacteremia and Septicemia<br />
<strong>The</strong> prostate harbors a variety of bacteria, which can be<br />
the source of perioperative bacteremia through open<br />
prostatic venous sinuses. <strong>The</strong> presence of an indwelling<br />
urinary catheter will increase the risk. <strong>The</strong>refore, the prophylactic<br />
administration of antibiotics is recommended in<br />
TURP patients. <strong>The</strong> bacteremia is usually transient and<br />
symptomless, and easily treated with frequently used<br />
antibiotic combinations. Nevertheless, 6%–7% of these<br />
patients will develop septicemia. 5 Common signs are<br />
fever, chills, hypotension, tachycardia, and/or bradycardia.<br />
In severe cases, cardiovascular collapse may occur,<br />
with mortality rates from 25% to 75%. 32<br />
Hypothermia<br />
<strong>The</strong> use of room temperature irrigating solutions during<br />
TURP may cause shivering and hypothermia in many<br />
patients, especially in the elderly, who have a reduced<br />
thermoregulatory capacity. 14 Using warmed irrigating<br />
solutions will decrease heat loss and shivering. 33 <strong>The</strong><br />
concern that warmed irrigating solutions may cause<br />
increased bleeding because of vasodilation has not been<br />
shown to be of clinical importance. 34<br />
Coagulopathy<br />
Abnormal bleeding after TURP occurs in fewer than 1%<br />
of cases. 9 Possible causes include dilutional thrombocytopenia<br />
and systemic coagulopathy. <strong>The</strong> absorption of large<br />
volumes of irrigating solution might result in dilution of<br />
platelets and coagulation factors. Systemic coagulopathy<br />
in TURP patients is probably caused by either primary<br />
fibrinolysis or disseminated intravascular coagulopathy.<br />
In primary fibrinolysis, a plasminogen activator, which<br />
converts plasminogen into plasmin, is released from the<br />
prostate. Plasmin then causes fibrinolysis with the resultant<br />
increase in bleeding. Suggested treatment for primary<br />
fibrinolysis is epsilon aminocaproic acid. 9 Fibrinolysis<br />
that is secondary to disseminated intravascular coagulopathy<br />
is triggered by the systemic absorption of prostate<br />
tissue, which is rich in thromboplastin. 35 This will, in<br />
turn, cause a depletion of coagulation factors and platelets.<br />
Treatment is supportive with fluid and blood products<br />
administered as needed. 14<br />
Anesthetic Considerations for<br />
Transurethral Prostatectomy<br />
<strong>Regional</strong> anesthesia, particularly spinal anesthesia, has<br />
long been considered the anesthetic technique of choice<br />
for TURP. 5 By allowing the patient to remain awake, this<br />
anesthetic technique allows early detection of mental<br />
status changes caused by TURP syndrome or the extravasation<br />
of irrigating solution. Restlessness and confusion<br />
are early signs of hyponatremia and/or serum hyperosmolality<br />
and should not be assumed to be signs of inadequate<br />
anesthesia. <strong>The</strong> administration of sedatives or the<br />
induction of general anesthesia in the presence of TURP<br />
syndrome can lead to severe complications and even<br />
death. 36 As discussed above, extravasation of irrigating<br />
solution secondary to either the perforation of the prostatic<br />
capsule or the bladder will cause the awake patient<br />
to complain of abdominal pain and/or experience nausea<br />
and vomiting.<br />
<strong>The</strong>re is controversy concerning whether anes -<br />
thetic technique influences blood loss during TURP surgery.<br />
Some studies have reported less bleeding under<br />
regional anesthesia, 37–39 whereas others found no significant<br />
difference in blood loss between regional and<br />
general anesthesia. 40–43 In those studies that demonstrated<br />
decreased bleeding with regional anesthesia, the authors<br />
postulated that regional anesthesia reduces blood<br />
loss not only by decreasing systemic blood pressure,<br />
but also by decreasing central and peripheral venous<br />
pressures. 6,37–39<br />
Numerous comparative studies using neuropsychologic<br />
testing have been conducted to test whether the incidence<br />
of postoperative cognitive dysfunction would be<br />
less with regional anesthesia than general anesthesia.<br />
One small prospective study comparing spinal anesthesia<br />
with intravenous sedation versus general anesthesia on<br />
elderly TURP patients found a significant decrease in
372 D.M. Gainsburg<br />
mental status in both groups at 6 hours after surgery, but<br />
there were no differences in perioperative mental function<br />
at any time between the groups during the first 30<br />
days after surgery. 44 In a recent study of 438 elderly<br />
patients undergoing various types of surgical procedures,<br />
it was found that the incidence of postoperative cognitive<br />
dysfunction after 1 week was significantly greater after<br />
general than regional anesthesia, but no difference was<br />
found after 3 months. 45 Incidentally, this study found significantly<br />
greater mortality after general than regional<br />
anesthesia, noting that postoperative respiratory complications<br />
and need for prolonged intensive care occurred<br />
only after general anesthesia. 45<br />
If regional anesthesia is chosen for TURP, a T10 sensory<br />
level is needed to block the pain of bladder distention.<br />
Sensory levels above T9 are undesirable because the<br />
patient will not feel abdominal pain caused by perforation<br />
of the prostatic capsule. 6 Spinal anesthesia is often<br />
preferred over epidural anesthesia, because of the need<br />
to block sacral segments, which provide sensory innervations<br />
to the prostate, bladder neck, and penis. 14 Another<br />
advantage of regional anesthesia for TURP is improved<br />
postoperative pain control and decreased requirement<br />
for postoperative analgesics. 46<br />
Treatment of Transurethral<br />
Prostatectomy Syndrome<br />
Prompt treatment is essential when the signs and symptoms<br />
of TURP syndrome are recognized. Initially, oxygenation,<br />
ventilation, and cardiovascular support should<br />
be provided based on the patient’s symptomatology,<br />
while, at the same time, considering other treatable conditions<br />
such as diabetic coma, hypercarbia, or drug interactions.<br />
10 <strong>The</strong> surgeon should be asked to terminate the<br />
procedure as rapidly as possible. Blood samples should<br />
be rapidly analyzed for electrolytes, creatinine, glucose,<br />
and arterial blood gases. A 12-lead electrocardiogram<br />
recording should be obtained. 8,14<br />
Treatment of hyponatremia and volume overload<br />
is dictated by the severity of the patient’s symptoms.<br />
If the symptoms are mild and the serum sodium level<br />
is greater than 120 mEq/L, then fluid restriction and<br />
the administration of a loop diuretic, usually furosemide,<br />
are all that is necessary in returning serum sodium to<br />
normal levels. In severe cases, serum sodium less than<br />
120 mEq/L, the recommended treatment is intravenous<br />
administration of hypertonic saline. A 3% sodium chloride<br />
solution should be infused at a rate no greater than<br />
100 mL/h and the patient’s hyponatremia should be corrected<br />
at a rate no greater than 0.5 mEq/L/h. 8,47 Rapid<br />
correction of hyponatremia with hypertonic saline has<br />
been associated with cerebral edema and central pontine<br />
myelinolysis. 20,48<br />
<strong>The</strong> Future of Transurethral<br />
Prostatectomy Syndrome<br />
With advances in medical treatment and the introduction<br />
of new surgical techniques for the treatment of symptomatic<br />
BPH, TURP syndrome will become a rare complication<br />
of prostate surgery. In the near future, it seems<br />
that the new gold standard for the surgical treatment of<br />
BPH will be holmium laser enucleation of the prostate<br />
(HoLEP). 49 Advantages of HoLEP over TURP are its<br />
ability to be used on any size of prostate gland, decreased<br />
blood loss, can be performed as an ambulatory procedure,<br />
decreased absorption of irrigating solution, and the elimination<br />
of TURP syndrome. 49 Long-term complications of<br />
HoLEP are urethral stricture, bladder neck contracture,<br />
and reoperation rate higher than TURP. However, in a<br />
recent retrospective study of 552 patients, these complications<br />
were less than reported elsewhere for TURP and<br />
open prostatectomy. 5,18,49 Because of these advantages,<br />
HoLEP is becoming the preferred surgical procedure<br />
for BPH, especially in elderly patients with significant<br />
comorbidities.<br />
Complications of Other<br />
Urologic Procedures<br />
Transurethral Resection of Bladder Tumors<br />
Bladder cancer is the second most common urologic<br />
malignancy and these tumors occur with a male to female<br />
ratio of approximately 3 : 1. 14 Most patients undergo<br />
an endoscopic procedure of transurethral resection of<br />
bladder tumor (TURBT). This procedure can be performed<br />
with either general or regional anesthesia. If a<br />
regional anesthesia is chosen, then a T10 sensory level is<br />
required to block the pain of bladder distention. As in<br />
TURP, bladder perforation can occur during TURBT<br />
with the same signs and symptoms that have been previously<br />
discussed. Bladder perforation can also occur if the<br />
bladder tumor lies near the obturator nerve. As the obturator<br />
nerve courses through the pelvis, it passes near the<br />
lateral bladder wall, bladder neck, and prostatic urethra.<br />
Inadvertent bladder perforation may occur if stimulation<br />
of the obturator nerve by electrocautery during the procedure<br />
causes the thigh muscles to contract forcefully. In<br />
this situation, general anesthesia with muscle relaxation<br />
would be the preferred technique. 50,51<br />
Extracorporeal Shock Wave Lithotripsy<br />
In the United States, the annual incidence of urolithiasis<br />
is 16–24 cases per 10,000 persons and accounts for 7–10<br />
of every 1000 hospital admissions. 52 Traditionally, renal<br />
stones were treated with open surgical procedures that
25. Transurethral Prostatectomy Syndrome 373<br />
required general anesthesia; however, in the late 1970s, a<br />
minimally invasive procedure, percutaneous nephrolithotomy,<br />
was introduced. Percutaneous nephrolithotomy<br />
also required general anesthesia, but had the advantage<br />
of shorter convalescence for patients. In 1980, a major<br />
noninvasive advance was made with the introduction of<br />
extracorporeal shock wave lithotripsy (ESWL), which<br />
has become the initial treatment modality for most<br />
patients with urinary tract stones. 53 Basically, the lithotripter<br />
generates repetitive high-energy shock waves that<br />
are focused on the stone and cause it to eventually fragment.<br />
<strong>The</strong> fragments are then excreted down the urinary<br />
tract over several weeks. 53<br />
First-generation lithotripters required immersion of<br />
the patient into a water bath and could cause physiolo -<br />
gic effects in patients. Immersion causes compression of<br />
peripheral veins, resulting in an increase in cardiac<br />
preload, along with an increase in central venous, right<br />
atrial, and pulmonary pressures. As central venous pressure<br />
increases, arterial pressure and cardiac output will<br />
typically increase. This may lead to congestive heart<br />
failure and decreased systemic blood pressure in patients<br />
who have limited cardiac reserve. 54 Immersion of a patient<br />
to the level of their clavicles increases the work of breathing<br />
and respirations often become shallow and rapid. 55<br />
<strong>The</strong> temperature of the water bath is of concern, especially<br />
in the elderly who have impaired thermoregulatory<br />
capacity. Cold water may induce vasoconstriction and<br />
shivering, whereas warm water may cause vasodilatation<br />
and hypotension. 54<br />
Cardiac arrhythmias have been observed in patients<br />
treated with first-generation lithotripters. It is thought<br />
that these arrhythmias are caused by the mechanical<br />
effects of the shock waves on the myocardium during the<br />
repolarization phase of the heart. By using electrocardiographic<br />
gating, the shock waves can be delivered milliseconds<br />
after the R wave during the refractory period of the<br />
heart. Newer generation lithotripters use a nonsynchronized<br />
mode in order to improve treatment times, but if<br />
induced arrhythmias are detected, a return to a gated<br />
mode will eliminate them. 53,56<br />
Because of the intense pain associated with firstgeneration<br />
lithotripters, general or regional anesthesia<br />
was required. Newer generations of lithotripters use a<br />
lower working voltage and have eliminated the water<br />
bath. Although they cause less pain, most patients still<br />
require intravenous sedation during treatments. Because<br />
the newer lithotripters use less power, the efficiency of<br />
stone fragmentation has decreased, causing the rate of<br />
re-treatment to increase. 53<br />
Absolute contraindications to ESWL are pregnancy,<br />
coagulopathy, and an active urinary tract infection. Relative<br />
contraindications include distal urethral stricture or<br />
obstruction, large stones, calcification or aneurysm of the<br />
renal artery or aorta, and/or renal insufficiency. 14,53 Surgical<br />
complications from ESWL include urinary obstruction<br />
from stone fragments; subcapsular, parenchymal,<br />
and perinephric hematomas of the kidney; transient renal<br />
failure; and damage to adjacent organs, such as the liver,<br />
pancreas, spleen, and lung. 14,53<br />
Laparoscopic Surgery in Urology<br />
Just as other surgical specialists have adapted to laparoscopic<br />
techniques, so have urologists. Initially, pelvic<br />
lymph node dissection was the most common urologic<br />
laparoscopic procedure performed; however, in recent<br />
years, the complexity of surgeries performed laparoscopically<br />
has become greater to include radical or donor<br />
nephrectomies, adrenalectomy, and radical prostatectomy.<br />
<strong>The</strong> advantages of this minimally invasive technique,<br />
although often taking longer to perform, are<br />
decreased postoperative pain, decreased blood loss,<br />
shorter hospital stays, and quicker return to normal function<br />
compared with open surgery. 14,57<br />
In addition to all the conventional complications<br />
and concerns associated with laparoscopic surgery, urologic<br />
laparoscopic procedures have their own unique set<br />
of problems. Because many urogenital structures are<br />
retroperitoneal, urologists often prefer insufflating the<br />
retroperitoneal space during laparoscopic surgery.<br />
Several studies have shown that CO 2 absorption is<br />
greater with retroperitoneal than intraperitoneal insufflation.<br />
58–60 Because the large retroperitoneal space and its<br />
connections with the thorax and subcutaneous tissue are<br />
exposed to insufflated CO 2 , subcutaneous emphysema is<br />
a common complication. Subcutaneous emphysema is<br />
observed late in the procedure, is preceded by an increase<br />
in end-tidal CO 2 , may extend all the way up to the head<br />
and neck, and is confirmed by palpation for crepitus. 57,61<br />
In severe cases, the upper airway may be compromised<br />
secondary to pharyngeal swelling caused by submucous<br />
CO 2 ; therefore, extubation may have to be delayed and<br />
ventilation adjusted in these patients. 6,57<br />
General anesthesia with controlled ventilation is<br />
preferred because insufflation of CO 2 and use of the<br />
steep Trendelenburg position causes increased intraabdominal<br />
and intrathoracic pressures. Some urologic laparoscopic<br />
procedures tend to be lengthy, thereby allowing<br />
sufficient absorption of CO 2 to cause hypercapnia and<br />
acidosis. 6,61 Oliguria may occur intraoperatively during<br />
prolonged periods of gas insufflation and then be followed<br />
by diuresis in the postoperative period. 6 Two possible<br />
mechanisms for the cause of this oliguria have been<br />
postulated: the first being that insufflation causes<br />
decreased renal cortical blood flow and renal vein obstruction<br />
62 ; and the second is an increase in stress hormone<br />
levels, such as antidiuretic hormone. 63 Because intraoperative<br />
oliguria during prolonged laparoscopic procedures<br />
may not truly reflect intravascular volume depletion,
374 D.M. Gainsburg<br />
treatment with fluid administration may lead to circulatory<br />
overload. 14<br />
Radical Prostatectomy<br />
Prostate cancer is the most frequently diagnosed cancer<br />
in men. 64 Radical prostatectomy involves the removal of<br />
the entire prostate gland, the ejaculatory ducts, the<br />
seminal vesicles, and a portion of the bladder neck. 57 <strong>The</strong><br />
procedure can be performed with either a retropubic or<br />
perineal approach; however, in the United States, most<br />
urologists use the retropubic approach. 57 Prostate cancer<br />
is a disease of older men with an incidence estimated<br />
at 75% for patients over 75 years old. 65 Preoperative<br />
evaluation should therefore focus on other coexisting<br />
conditions that are prevalent in elderly patients. 57<br />
<strong>The</strong> perioperative mortality rate has been reported to be<br />
approximately 0.2%. 66<br />
<strong>The</strong> most common intraoperative complication is hemorrhage<br />
with reported blood loss ranging from less than<br />
500 mL to greater than 1500 mL. 57 Because of the potential<br />
for rapid blood loss, the use of invasive arterial pressure<br />
monitoring as well as adequate venous access are<br />
recommended. 14,57 Patients undergoing radical prostatectomy<br />
are often placed in a hyperextended supine position<br />
along with Trendelenburg, 57 which places the pubis above<br />
the head. 6 Significant venous air embolism from the<br />
prostatic fossa may occur as a result of a gravitational<br />
gradient between the prostatic veins and head. 67 <strong>The</strong><br />
Trendelenburg position can also produce edema of the<br />
upper airway. 14 Early postoperative complications, which<br />
occur in 0.5%–2% of cases, include deep vein thrombosis,<br />
pulmonary embolism, hematoma, seroma, and wound<br />
infection, 66 whereas late surgical complications are incontinence,<br />
impotence, and bladder neck contracture. 68<br />
General or regional anesthesia with sedation may be<br />
used for this procedure. If regional anesthesia is chosen,<br />
then a sensory level of T6 is recommended. 57 Because<br />
many patients may not tolerate lengthy surgery in the<br />
Trendelenburg position, one needs to be prepared for<br />
conversion to general anesthesia. 57 <strong>The</strong> choice of anesthetic<br />
technique does not seem to influence postoperative<br />
morbidity 69 or quality of life. 70<br />
Radical Cystectomy<br />
<strong>The</strong> treatment of muscle-invasive bladder cancer is a<br />
radical cystectomy. <strong>The</strong> patient is usually male, a cigarette<br />
smoker, and/or had occupational chemical exposure who<br />
presents with painless, gross hematuria. 57 In men,<br />
it involves the removal of the bladder, prostate gland,<br />
seminal vesicles, and proximal urethra; in women, the<br />
bladder, uterus, fallopian tubes, ovaries, and the anterior<br />
vaginal wall are removed. After the bladder is removed,<br />
a urinary diversion is performed; an ileal conduit, bowel<br />
segments for continent reservoirs, or ureterostomies are<br />
frequently used. 57,71<br />
<strong>The</strong> intraoperative problems that may occur during<br />
radical retropubic prostatectomy may also arise in this<br />
procedure. However, radical cystectomy is an intraperitoneal<br />
procedure with increased fluid requirements. In<br />
addition to adequate venous access, the use of invasive<br />
arterial pressure monitoring and/or central venous monitoring<br />
to guide intravenous fluid therapy may be helpful<br />
because urinary output cannot be assessed. 57 Because of<br />
the length and extent of surgery, general or a combined<br />
general-epidural anesthetic technique is mandated. 14,57<br />
A recent study of 50 patients undergoing radical cystectomy<br />
comparing combined epidural-general anesthesia<br />
(CEGA) to general anesthesia concluded that the CEGA<br />
group had significantly less blood loss than the general<br />
anesthesia group. <strong>The</strong>re were no significant differences in<br />
intraoperative hemodynamics or postoperative complications,<br />
and the CEGA group had better postoperative pain<br />
control. 72<br />
Radical Nephrectomy<br />
Renal cell carcinoma is the most common malignancy of<br />
the kidney. Because it is refractory to chemotherapy and<br />
radiation therapy, radical nephrectomy is the treatment<br />
of choice. Radical nephrectomy involves the excision of<br />
the kidney, surrounding fascia, the ipsilateral adrenal<br />
gland, and the upper ureter. 14,57 Partial nephrectomy is<br />
considered in those patients with small lesions or bilateral<br />
tumors or those at risk because of other diseases such<br />
as diabetes and hypertension. 73 This malignancy has a<br />
peak age of incidence of 60 years, and cigarette smoking<br />
has been identified as a risk factor. 57 <strong>The</strong>refore, coronary<br />
artery disease as well as chronic obstructive pulmonary<br />
disease is common in these patients. 57<br />
Frequently used approaches for radical nephrectomy<br />
are the flank, subcostal, or thoracoabdominal. Potential<br />
complications of these approaches include significant<br />
pneumothorax with possible insertion of a chest tube;<br />
pulmonary contusion, caused by lung retraction, necessitating<br />
prolonged postoperative ventilation; and injuries<br />
to adjacent organs, in particular, splenic injury, which has<br />
a 10% incidence in association with a left nephrectomy. 57<br />
<strong>The</strong>se tumors tend to be very vascular and extensive<br />
blood loss may occur. 57 General anesthesia with invasive<br />
arterial pressure monitoring and adequate intravenous<br />
access is recommended. 57<br />
In 5%–10% of patients, the tumor extends into the<br />
renal vein and vena cava; therefore, the extent of the<br />
lesion must be defined preoperatively. Several potential<br />
problems can occur in these patients, ranging from circulatory<br />
failure as a result of total occlusion by tumor of<br />
the vena cava, to acute pulmonary embolization of tumor<br />
fragments. 6 Cardiopulmonary bypass is necessary when
25. Transurethral Prostatectomy Syndrome 375<br />
control of the vena cava above the tumor thrombus<br />
cannot be obtained. 57 If the tumor thrombus extends into<br />
the right atrium, then right heart catheterization is contraindicated.<br />
57 <strong>The</strong> use of transesophageal echocardiography<br />
during resection of renal cell carcinoma with vena<br />
cava involvement has been shown to be helpful in the<br />
management of these complex cases. 74,75<br />
Summary<br />
With the continuing decline in the annual number of<br />
TURPs being performed and the introduction of HoLEP,<br />
anesthesiologists will rarely, if at all, experience a patient<br />
with TURP syndrome. Because of its advantages over<br />
TURP, HoLEP will become the new gold standard for<br />
the surgical treatment of BPH in the elderly patient. As<br />
urologists become more proficient at laparoscopic techniques,<br />
the number of laparoscopic procedures performed<br />
on the elderly will increase. Because of their age and<br />
increased prevalence of comorbid disease, elderly patients<br />
are at higher risk for perioperative morbidity and mortality<br />
than their younger counterparts, especially during<br />
major surgery. Elderly patients may therefore benefit the<br />
most if current and future advances in urologic surgical<br />
techniques continue to improve outcomes.<br />
References<br />
1. Fitzpatrick JM, Mebust WK. Minimally invasive and endoscopic<br />
management of benign prostatic hyperplasia. In:<br />
Walsh PC, ed. Campbell’s Urology. 8th ed. Philadelphia:<br />
WB Saunders; 2002:1379–1422.<br />
2. Issa MM, Young MR, Bullock AR, et al. Dilutional hyponatremia<br />
of TURP syndrome: A historical event in the 21st<br />
century. Urology 2004; 64:298–301.<br />
3. McConnell JD, Barry MD, Bruskewitz RC, et al. Benign<br />
prostatic hyperplasia: diagnosis and treatment. Clinical<br />
practice guideline. Rockville, MD: Agency for Health Care<br />
Policy and Research; 1994. Publication No. 94-0582.<br />
4. Issa MM, Marshall FF. Contemporary diagnosis and management<br />
of diseases of the prostate. 2nd ed. Newton, PA:<br />
Handbook in Health Care Co.; 2004:13–14.<br />
5. Mebust WK, Holtgrewe HL, Cockett ATK, et al. Transurethral<br />
prostatectomy: immediate and postoperative complications—cooperative<br />
study of 13 participating institutions<br />
evaluating 3885 patients. J Urol 1989;141:243–247.<br />
6. Malhota V, Sudheendra V, Diwan S. <strong>Anesthesia</strong> and the<br />
renal and genitourinary systems. In: Miller RD, ed. Miller’s<br />
<strong>Anesthesia</strong>. 6th ed. Philadelphia: Elsevier; 2005:2175–2207.<br />
7. Melchior J, Valk WL, Foret JD, et al. Transurethral prostatectomy:<br />
computerized analysis of 2223 consecutive cases.<br />
J Urol 1974;112:634–642.<br />
8. Azar I. Transurethral prostatectomy syndrome and other<br />
complications of urological procedures. In: McLeskey CH,<br />
ed. <strong>Geriatric</strong> <strong>Anesthesia</strong>. 1st ed. Baltimore: Williams &<br />
Wilkins; 1997:595–607.<br />
9. Hatch PD. Surgical and anaesthetic considerations in transurethral<br />
resection of the prostate. Anaesth Intensive Care<br />
1987;15:203–211.<br />
10. Jensen V. <strong>The</strong> TURP syndrome. Can J Anaesth 1991;38:<br />
90–96.<br />
11. Marx GF, Orkin LR. Complications associated with transurethral<br />
surgery. <strong>Anesthesiology</strong> 1962;23:802–813.<br />
12. Roesch RP, Stoelting RK, Lingeman JE, et al. Ammonia<br />
toxicity resulting from glycine absorption during a transurethral<br />
resection of the prostate. <strong>Anesthesiology</strong> 1983;58:<br />
577–579.<br />
13. Hoekstra PT, Kahnoski R, McMamish MA, et al. Transurethral<br />
prostatic resection syndrome—a new perspective:<br />
encephalopathy with associated hyperammonemia. J Urol<br />
1983;130:704–707.<br />
14. Monk TG, Weldon BC. <strong>The</strong> renal system and anesthesia for<br />
urologic surgery. In: Barash PG, Cullen BF, Stoeling RK,<br />
eds. Clinical <strong>Anesthesia</strong>. 4th ed. Philadelphia: Lippincott<br />
Williams & Wilkins; 2001:1005–1033.<br />
15. Creevy CD. Reactions peculiar to transurethral resection of<br />
the prostate. Surg Clin North Am 1967;47:1471–1472.<br />
16. Hurlbert BJ, Wingard DW. Water intoxication after 15<br />
minutes of transurethral resection of the prostate. <strong>Anesthesiology</strong><br />
1979;50:355–356.<br />
17. Still AJ, Modell JA. Acute water intoxication during transurethral<br />
resection of the prostate using glycine solution for<br />
irrigation. <strong>Anesthesiology</strong> 1973;38:98–99.<br />
18. Borboroglu PG, Kane CJ, Ward JF, et al. Immediate and<br />
postoperative complications of transurethral prostatectomy<br />
in the 1990s. J Urol 1999;162:1307–1310.<br />
19. Hahn RG. <strong>The</strong> transurethral resection syndrome—not<br />
yet a finished story [editorial]. Reg Anesth Pain Med 1998;<br />
23:115.<br />
20. Gravenstein D. Transurethral resection of prostate (TURP)<br />
syndrome: a review of pathophysiology and management.<br />
Anesth Analg 1997;84:438–446.<br />
21. Hahn RG. <strong>The</strong> transurethral resection syndrome. Acta<br />
Anaesthesiol Scand 1991;35:557–567.<br />
22. Rao PN. Fluid absorption during urological endoscopy.<br />
Br J Urol 1987;60:93–99.<br />
23. Agin C. <strong>Anesthesia</strong> for transurethral prostate surgery.<br />
Int Anesthesiol Clin 1993;31:25–46.<br />
24. Henderson DJ, Middleton RG. Coma from hyponatremia<br />
following transurethral resection of the prostate. Urology<br />
1980;15:267–271.<br />
25. Narins RG. <strong>The</strong>rapy of hyponatremia: does haste make<br />
waste? N Engl J Med 1986;314:1573–1575.<br />
26. Osborn DE, Rao PN, Green MJ, et al. Fluid absorption<br />
during transurethral resection. Br Med J 1980;281:1549–<br />
1550.<br />
27. Mebust WK, Brady TW, Valk WL. Observations on cardiac<br />
output, blood volume, central venous pressure, fluid and<br />
electrolyte changes in patients undergoing transurethral<br />
prostatectomy. J Urol 1970;103:632–636.<br />
28. Rose FC. Transient blindness. Br Med J 1964;3:763–764.<br />
29. Barletta JP, Fanous MM, Hamed LM. Temporary blindness<br />
in the TUR syndrome. J Neuroophthalmol 1994;14:6–8.<br />
30. Fahey JL. Toxicity and blood ammonia rise resulting from<br />
intravenous amino acid administration in man: the protective<br />
effect of L-arginine. J Clin Invest 1957;36:1647–1655.
376 D.M. Gainsburg<br />
31. Nathans D, Fahey JL, Ship AG. Sites of origin and removal<br />
of blood ammonia formed during glycine infusion: effect of<br />
L-arginine. J Lab Clin Med 1958;51:124–133.<br />
32. Murphy DM, Falkiner FR, Carr M, et al. Septicemia after<br />
transurethral prostatectomy. Urology 1983;22:133–135.<br />
33. Allen TD. Body temperature changes during prostatic<br />
resection as related to the temperature of the irrigating<br />
solution. J Urol 1973;110:433–435.<br />
34. Heathcote PS, Dyer PM. <strong>The</strong> effect of warm irrigation on<br />
blood loss during transurethral prostatectomy under spinal<br />
anesthesia. Br J Urol 1986;58:669–671.<br />
35. Ladehoff AA, Rasmussen J. Fibrinolysis and thromboplastic<br />
activities in relation to hemorrhage in transvesical prostatectomy.<br />
Scand J Clin Lab Invest 1961;13:231–244.<br />
36. Aasheim GM. Hyponatremia during transurethral surgery.<br />
Can Anaesth Soc J 1973;20:274–280.<br />
37. Abrams PH, Shah PJR, Bryning K, et al. Blood loss during<br />
transurethral resection of the prostate. Anaesthesia 1982;37:<br />
71–73.<br />
38. Mackenzie AR. Influence of anesthesia on blood loss in<br />
transurethral prostatectomy. Scott Med J 1990;35:14–16.<br />
39. Madsen RE, Madsen PO. Influence of anesthesia form on<br />
blood loss in transurethral prostatectomy. Anesth Analg<br />
1967;46:330–332.<br />
40. McGowan SW, Smith GFN. Anaesthesia for transurethral<br />
prostatectomy. Anaesthesia 1980;35:847–853.<br />
41. Nielsen KK, Andersen K, Asbjorn J, et al. Blood loss in<br />
transurethral prostatectomy: epidural versus general anesthesia.<br />
Int Urol Nephrol 1987;19:287–292.<br />
42. Fraser I, Scott M, Campbell I, et al. Routine cross-matching<br />
is not necessary for a transurethral resection of the prostate.<br />
Br J Urol 1964;56:399–405.<br />
43. Slade N, Andrews GL, Tovey GH, et al. Blood loss in prostatic<br />
surgery. Br J Urol 1964;36:399–405.<br />
44. Chung FF, Chung A, Meier RH, et al. Comparison of perioperative<br />
mental function after general anaesthesia and<br />
spinal anaesthesia with intravenous sedation. Can J Anaesth<br />
1989;36:382–387.<br />
45. Rasmussen LS, Johnson T, Kuipers HM, et al. Does<br />
anaesthesia cause post-operative cognitive dysfunction? A<br />
randomized study of regional versus general anaesthesia<br />
in 438 elderly patients. Acta Anaesthesiol Scand 2003;47:<br />
260–266.<br />
46. Bowman GW, Hoerth JW, McGlothlen JS, et al. <strong>Anesthesia</strong><br />
for transurethral resection of the prostate: spinal or general?<br />
AANA J 1981;49:63–68.<br />
47. Sterns RH, Riggs JE, Schochet SS Jr. Osmotic demyelinization<br />
syndrome following correction of hyponatremia.<br />
N Engl J Med 1986;314:1535–1542.<br />
48. Malhotra V. Transurethral resection of the prostate. Anesthesiol<br />
Clin North Am 2000;18:883–897.<br />
49. Elzayat EA, Habib EI, Elhilahi MM. Holmium laser enucleation<br />
of the prostate: a size-independent new “gold standard.”<br />
Urology 2005;66(Suppl 5A):108–113.<br />
50. Hobika JH, Clarke BG. Use of neuromuscular blocking<br />
drugs to counteract thigh-adductor spasm induced by electrical<br />
shocks of obturator nerve during transurethral resection<br />
of bladder tumors. J Urol 1961;85:295–296.<br />
51. Prentiss RJ, Harvey GW, Bethard WF, et al. Massive adductor<br />
muscle contraction in transurethral surgery: cause and<br />
prevention; development of new electrical circuitry. J Urol<br />
1965;93:263–271.<br />
52. Pahira JJ, Razack AA. In: Hanno PM, Malkowitz SB, Wein<br />
AJ, eds. Nephrolithiasis: Clinical Manual of Urology. 3rd ed.<br />
New York: McGraw Hill; 2001:231–252.<br />
53. Gravenstein D. Extracorporeal shock wave lithotripsy and<br />
percutaneous nephrolithotomy. Anesthesiol Clin North Am<br />
2000;18:953–971.<br />
54. Weber W, Madler C, Keil B, et al. Cardiovascular effects of<br />
extracorporeal shock wave lithotripsy. In: Gravenstein D,<br />
Peter K, eds. Extracorporeal Shock Wave Lithotripsy for<br />
Renal Stone Disease: Technical and Clinical Aspects. Stoneham,<br />
MA: Butterworth; 1986:101–112.<br />
55. Bromage PR, Bonsu AK, el-Faqih S, et al. Influence of<br />
Dornier HM3 system on respiration during extracorporeal<br />
shock wave lithotripsy. Anesth Analg 1989;68:363–367.<br />
56. Greenstein A, Kaver I, Lechtman V, et al. Cardiac arrhythmias<br />
during non-synchronized extracorporeal shock wave<br />
lithotripsy. J Urol 1995;154:1321–1322.<br />
57. Whalley DG, Berrigan MJ. <strong>Anesthesia</strong> for radical prostatectomy,<br />
cystectomy, nephrectomy, pheochromocytoma, and<br />
laparoscopic procedures. Anesthesiol Clin North Am 2000;<br />
18:889–917.<br />
58. Mullett CE, Viale JP, Sagnard PE, et al. Pulmonary CO 2<br />
elimination during surgical procedures using intra- or extraperitoneal<br />
CO 2 insulation. Anesth Analg 1993;76:622–626.<br />
59. Wolf JS Jr, Monk TG, McDougall EM, et al. <strong>The</strong> extraperitoneal<br />
approach and subcutaneous emphysema are associated<br />
with greater absorption of carbon dioxide during<br />
laparoscopic renal surgery. J Urol 1995;154:959–963.<br />
60. Wolf JS Jr, Clayman RV, Monk TG, et al. Carbon dioxide<br />
absorption during laparoscopic pelvic operation. J Am Coll<br />
Surg 1995;180:555–560.<br />
61. Weingram J, Sosa RE, Stein B, et al. Subcutaneous emphysema<br />
(SCE) during laparoscopic pelvic lymph node dissection<br />
(LPLND). Anesth Analg 1993;S460:76.<br />
62. McDougall EM, Monk TG, Hicks M, et al. <strong>The</strong> effect of<br />
prolonged pneumo-peritoneum on renal function in an<br />
animal model. J Am Coll Surg 1996;182:317–328.<br />
63. Ortega AE, Peters JH, Incarbone R, et al. A prospective<br />
randomized comparison of the metabolic and stress hormonal<br />
responses of laparoscopic and open cholecystectomy.<br />
J Am Coll Surg 1996;183:249–256.<br />
64. Brawer MK. How to use prostate-specific antigen in the<br />
early detection or screening for prostatic carcinoma. Cancer<br />
J Clin 1995;45:148–164.<br />
65. Morgan GE Jr, Mikhail MS, Murray MJ. <strong>Anesthesia</strong> for<br />
genitourinary surgery. In: Clinical <strong>Anesthesia</strong>. 4th ed. New<br />
York: Lange Medical Books; 2006:757–772.<br />
66. Monk TG. Cancer of the prostate and radical prostatectomy.<br />
In: Malhotra V, ed. <strong>Anesthesia</strong> for Renal and Genitourinary<br />
Surgery. New York: McGraw Hill; 1996:177–195.<br />
67. Albin MS, Ritter RR, Reinhart R, et al. Venous air embolism<br />
during radical retropubic prostatectomy. Anesth Analg<br />
1992;74:151–153.<br />
68. Catalona WJ. Surgical management of prostate cancer. Contemporary<br />
results with anatomic surgical prostatectomy.<br />
Cancer 1995;75:1903–1908.<br />
69. Shir Y, Frank SM, Brendler CB, et al. Postoperative morbidity<br />
is similar in patients anesthetized with epidural and
25. Transurethral Prostatectomy Syndrome 377<br />
general anesthesia for radical prostatectomy. Urology 1994;<br />
44:232–236.<br />
70. Haythornthwaite JA, Raja SN, Fisher B, et al. Pain and<br />
quality of life following radical retropubic prostatectomy.<br />
J Urol 1998;160:1761–1764.<br />
71. Maffezzini M, Gerbi G, Campodonico F, et al. Peri-operative<br />
management of ablative and reconstructive surgery for<br />
invasive bladder cancer in the elderly. Surg Oncol 2004;13:<br />
197–200.<br />
72. Ozyuvaci E, Altran A, Karadeniz T, et al. General anesthesia<br />
verus epidural and general anesthesia in radical cystectomy.<br />
Urol Int 2005;74:62–67.<br />
73. Shah N. Radical cystectomy, radical nephrectomy and<br />
retroperitoneal lymph node dissection. In: Malhotra V, ed.<br />
<strong>Anesthesia</strong> for Renal and Genitourinary Surgery.<br />
New York: McGraw Hill; 1996:197–226.<br />
74. Hasnain JU, Watson RJN. Transesophageal echocardiography<br />
during resection of renal cell carcinoma<br />
involving the inferior vena cava. South Med J 1994;87:<br />
273–275.<br />
75. Mizoguchi T, Koide Y, Ohara M, et al. Multiplane transesophageal<br />
echocardiographic guidance during resection of<br />
renal cell carcinoma extending into the inferior vena cava.<br />
Anesth Analg 1995;81:1102–1105.
26<br />
Thoracic Procedures<br />
Steven M. Neustein and James B. Eisenkraft<br />
From 1900 to 1990, the fraction of the population aged<br />
65 years and older tripled to 13%. 1 Persons aged 80 years<br />
and older now constitute the fastest-growing elderly<br />
group in the United States. 2 Between 2000 and 2020, this<br />
segment of the United States population is expected to<br />
increase by approximately 35%.<br />
Aging increases the susceptibility to pulmonary<br />
disease. 3 Lung cancer is the leading cause of cancer death<br />
in persons older than 70 years. 4 More than half of all lung<br />
cancers occur in people who are older than 65 years.<br />
From 1955 to 1992, worldwide mortality from lung cancer<br />
has increased by 180% and 580% in 65- to 82-year-old<br />
men and women, respectively. 5<br />
Most lung cancers become manifest in the geriatric<br />
population because they are associated with a long latency<br />
period after prolonged exposure to tobacco smoke or<br />
other predisposing factors. Surgical resection is currently<br />
the only available means for curing lung cancer. Those<br />
patients with unresectable tumors often receive chemotherapy<br />
and radiation treatment. Surgery is also the treatment<br />
of choice for localized non–small cell carcinomas,<br />
because often they can be excised completely.<br />
Lung resection for tumor is a common procedure in the<br />
elderly. Resection is often preceded by bronchoscopy to<br />
evaluate tumor involvement of the airway and to determine<br />
the resectability. If there is mediastinal adenopathy<br />
on computed tomography scan of the chest, a mediastinoscopy<br />
is performed to determine if this enlargement is<br />
the result of malignant spread of the tumor, which, if<br />
present, would contraindicate surgical resection.<br />
Although surgery is necessary to cure most lung cancers,<br />
the risk of operating on the elderly is increased. 6 Patients<br />
in this segment of the population are offered surgery less<br />
often than younger counterparts. 7 Elderly patients who<br />
are not treated survive an average 1–5 years. 8 Overall, the<br />
5-year survival rate for patients with lung cancer is 18.5%<br />
for those younger than 65 and 13.8% for those 65 years<br />
or older. 9 This may be attributable to a lower rate of<br />
surgery in elderly patients with lung cancer.<br />
Morbidity and Mortality of Thoracic<br />
Surgical Procedures in the Elderly<br />
Among elderly patients undergoing pneumonectomy and<br />
lobectomy, the associated mortality has been twice that of<br />
patients younger than 65 years. 10 A series of 476 patients<br />
were studied by Kohman et al. 11 to identify predictors of<br />
mortality after thoracotomy for lung cancer. Hospital<br />
mortality for patients undergoing pulmonary resection<br />
was 5.6%. <strong>The</strong> only statistically significant risk factors for<br />
mortality were age 60 years or older, the presence of premature<br />
ventricular contractions on the admission electrocardiogram<br />
(EKG), and the need for pneumonectomy<br />
(versus lobectomy). Patients younger than 60 years had a<br />
mortality rate of 2.4%, as compared with 7.4% in patients<br />
aged 60 years or older. Hospital mortality after pneumonectomy<br />
and lobectomy was 11.7% and 3.7%, respectively.<br />
More recently, a 30-day mortality rate of 22% in<br />
patients older than 70 years has been reported after pneumonectomy.<br />
12 In another report of patients more than 80<br />
years undergoing thoracic surgery for lung cancer, there<br />
was a mortality rate of only 3%. 13 In a study of 296 patients<br />
who were 65–89 years of age, and underwent resection<br />
with video-assisted thoracoscopy (VAT) for stage 1 lung<br />
cancer, there was a 15% incidence of morbidity, and only<br />
a 1% mortality rate. 14<br />
Gerson et al. 15 studied 177 patients who were 65 years<br />
of age or older and scheduled for major elective abdominal<br />
or noncardiac thoracic surgery. <strong>The</strong> inability to exercise,<br />
defined as the inability to perform supine bicycle<br />
pedaling for 2 minutes or to increase the heart rate to at<br />
least 100 beats per minute, was the best predictor of<br />
postoperative cardiopulmonary complications. Patients<br />
capable of this exercise had a perioperative cardiac or<br />
pulmonary complication rate of 9.3%, as compared with<br />
42% for those who could not perform the exercise. <strong>The</strong><br />
comparative mortality rates were 0.9% and 7.2%, respectively.<br />
Perioperative pulmonary complications occurred<br />
378
26. Thoracic Procedures 379<br />
in 24 patients (14%). Twenty-three of these patients had<br />
pneumonia, and one patient had a pulmonary embolism.<br />
Arterial blood gases were not predictive of the incidence<br />
of perioperative pulmonary complications in this study,<br />
but this may have been caused by the paucity of patients<br />
with increased carbon dioxide levels. A history of congestive<br />
heart failure or neurologic disease has been associated<br />
with an increased risk of postoperative pulmonary<br />
dysfunction in the elderly. 16<br />
Perioperative chest physical therapy in the elderly,<br />
when combined with postoperative chest physical therapy,<br />
can further decrease the incidence of atelectasis. 17 In this<br />
study of elderly patients who underwent cardiac and<br />
other thoracic surgical procedures, none of the 67 patients<br />
with chronic obstructive pulmonary disease (COPD) who<br />
received both preoperative and postoperative chest physical<br />
therapy developed pulmonary complications, as compared<br />
with all 34 patients with COPD who only received<br />
postoperative chest physical therapy (p < 0.02). 17 In a<br />
more recent study, patients with COPD who had a perioperative<br />
chest physical therapy program that was begun<br />
preoperatively also had a reduction in postoperative pulmonary<br />
complications. 18 Elderly patients have decreased<br />
pulmonary function because of aging and increased duration<br />
of exposure to cigarette smoke, and are less likely to<br />
tolerate removal of lung tissue.<br />
In the study by Gerson et al., 15 perioperative cardiac<br />
complications occurred in 25 of 177 patients (14%).<br />
Ninety-two percent of patients who had a perioperative<br />
pulmonary complication, and 88% of patients who had<br />
a perioperative cardiac complication, were unable to<br />
perform 2 minutes of exercise and increase their heart<br />
rates to at least 100 beats per minute. A previous study<br />
also demonstrated this test to be a predictor of perioperative<br />
cardiac complications in noncardiac thoracic geriatric<br />
surgery. 19<br />
Cardiorespiratory Physiology<br />
in the Elderly<br />
A thorough preoperative assessment is essential for any<br />
patient scheduled to undergo thoracic surgery. It is particularly<br />
important for the geriatric patient, because with<br />
advancing age comes a decline in cardiopulmonary function.<br />
<strong>The</strong>re is decreased elastic tissue in both peripheral<br />
and coronary arteries, leading to systolic hypertension,<br />
left ventricular hypertrophy, and decreased coronary<br />
reserve. <strong>The</strong>re is also a decrease in the maximum achievable<br />
stroke volume and heart rate, and thus in maximum<br />
cardiac output.<br />
A decrease in elastic tissue occurs in the lungs with age,<br />
leading to an increase in lung compliance. However, the<br />
thorax is more rigid because of calcification so that total<br />
thoracic compliance may be unchanged. <strong>The</strong> decrease in<br />
the amount of elastic tissue leads to airway closure, and<br />
there is an increase in both anatomic and alveolar dead<br />
space. <strong>The</strong> closing capacity, closing volume, and residual<br />
volume increase. In addition to a decreased ventilatory<br />
response to hypoxia and hypercarbia, elderly patients<br />
may have periodic breathing during sleep, putting them<br />
at increased risk of apnea in the postanesthesia care<br />
unit. 20 <strong>The</strong> vital capacity and PaO 2 decrease with increasing<br />
age. 21 A frequently used formula for estimating the<br />
PaO 2 according to age is, PaO 2 = 100 − age (in years)/3.<br />
With aging, there is a decrease in both immune function,<br />
and ciliary function, which accounts for an increased rate<br />
of respiratory infections in the elderly. 22<br />
<strong>The</strong> patient with a preoperative forced vital capacity<br />
(FVC) of less than 20 mL/kg or postbronchodilator forced<br />
expiratory volume in 1 second (FEV 1 )/FVC of less than<br />
50% is at increased risk for pulmonary complications.<br />
Preoperative teaching of breathing exercises and planned<br />
bronchial therapy can decrease postoperative pulmonary<br />
complications. 23<br />
<strong>The</strong> elderly have decreased anesthetic requirements.<br />
<strong>The</strong>re is an increase in sensitivity to anesthetic agents,<br />
which parallels the loss of cortical neurons and decrease<br />
in brain neurotransmitters that occur with aging. Premedication<br />
of the elderly patient for thoracic surgery<br />
should be light, because of the decreased pulmonary<br />
reserve and increased sensitivity to anesthetics. In many<br />
cases, premedication is best omitted. Anticholinergics to<br />
decrease secretions may be helpful, especially if bronchoscopy<br />
is planned.<br />
Preoperative Evaluation<br />
Postoperative pulmonary complications are a major<br />
source of morbidity and mortality after thoracic surgery. 24<br />
<strong>The</strong> best evaluation of pulmonary function is a careful<br />
history. <strong>The</strong> information to be collected includes history<br />
of smoking, presence of respiratory systems, and functional<br />
status.<br />
As described by Slinger and Johnston, 25 pulmonary<br />
function can be evaluated by assessing three aspects:<br />
mechanics, gas exchange, and cardiopulmonary function.<br />
<strong>The</strong> single most important test of respiratory mechanics<br />
is the FEV 1 . Patients with an FEV 1 40% are at decreased risk, whereas those<br />
with values
380 S.M. Neustein and J.B. Eisenkraft<br />
A predicted postoperative DLCO 15 mL/kg/min is associated with reduced risk, 30<br />
and
26. Thoracic Procedures 381<br />
at rates greater than 100 breaths per minute. A highpressure<br />
air-oxygen supply is modulated by a solenoid<br />
valve, producing frequent jet pulses that result in forward<br />
motion of airway gas. HFPPV at rates of up to 150 breaths<br />
per minute has produced similar blood gas values to<br />
those obtained with the Sanders injector system. 35 <strong>The</strong><br />
tracheobronchial wall is immobile during HFPPV, which<br />
may be an important advantage during laser surgery. 35<br />
Complications of rigid bronchoscopy include damage<br />
to teeth, hemorrhage, bronchial or tracheal perforation,<br />
airway edema, and barotrauma. <strong>The</strong>se risks are greater if<br />
the patient moves while the rigid bronchoscopy is in<br />
place. Flexible fiberoptic bronchoscopy is associated with<br />
fewer complications.<br />
Flexible Fiberoptic Bronchoscopy<br />
An examination of the airway with the flexible fiberoptic<br />
bronchoscope is typically performed before a lung resection.<br />
Preoperatively, an antisialagogue should be administered<br />
to decrease secretions that would otherwise<br />
interfere with visualization. Although scopolamine is the<br />
most potent drying agent, it may cause confusion in the<br />
elderly and should therefore be avoided. Glycopyrrolate<br />
is the drying agent of choice. It has a longer duration<br />
of action than atropine, and does not cross the blood–<br />
brain barrier.<br />
Flexible fiberoptic bronchoscopy can be performed<br />
using either local or general anesthesia. Local anesthetic<br />
solution can be sprayed onto the base of the tongue, or<br />
the patient can gargle with viscous lidocaine (2%). Bilateral<br />
superior laryngeal nerve blocks can be performed<br />
either percutaneously or by using Krause forceps to hold<br />
local anesthetic-soaked pledgets in each piriform fossa.<br />
<strong>The</strong> trachea and vocal cords are anesthetized by direct<br />
injection of local anesthetic into the trachea through the<br />
cricothyroid membrane, by spraying of local anesthetic<br />
under direct vision, or by injection via the working<br />
channel of the fiberscope.<br />
Instead of using the blocks described above, a nebulizer<br />
can be used to topically anesthetize the whole airway.<br />
A disposable (“acorn”) nebulizer filled with lidocaine<br />
(4 mL of 4%) is attached to a closely fitting face mask.<br />
<strong>The</strong> flow of oxygen to the nebulizer creates a mist of<br />
lidocaine that is inhaled by the patient, who is instructed<br />
to hold the mist in the airway for as long as possible. <strong>The</strong><br />
nasal mucosa should also be anesthetized if the fiberoptic<br />
bronchoscope is to be passed nasally. This can be accomplished<br />
with cocaine, or a mixture of lidocaine (3 mL of<br />
4%) and phenylephrine (1 mL of 1%).<br />
<strong>The</strong> technique of flexible fiberoptic bronchoscopy in<br />
an awake patient requires considerable cooperation<br />
from the patient. <strong>The</strong> elderly patient with lung disease<br />
may not tolerate much sedation; therefore, good topical<br />
anesthesia of the airway with local anesthetic is<br />
important.<br />
Fiberoptic bronchoscopy can also be performed with<br />
the patient under general anesthesia. <strong>The</strong> trachea is first<br />
intubated, and then the fiberscope is inserted through an<br />
adapter that will create a gas-tight seal around the instrument<br />
such that the patient’s lungs may be ventilated<br />
around the fiberscope. <strong>The</strong> passage of a fiberscope through<br />
an endotracheal tube during IPPV may cause a positive<br />
end-expiratory pressure (PEEP) effect. If PEEP is already<br />
being applied via the anesthesia circuit, it should be discontinued<br />
while the fiberscope is in place. 33 A smallerdiameter<br />
fiberscope should be used if the endotracheal<br />
tube being used is less than 8.0 mm in internal diameter.<br />
Problems associated with fiberoptic bronchoscopy<br />
include local anesthetic toxicity, bleeding, and airway<br />
obstruction because of passage of the fiberscope<br />
through a stenosed portion of the trachea, or bleeding<br />
into an already narrowed airway, hypoxemia, and<br />
bronchospasm. 32<br />
Mediastinoscopy<br />
Mediastinoscopy was initially described by Carlens 36 as a<br />
method for assessing spread of bronchial carcinoma. <strong>The</strong><br />
procedure enables examination of the superior mediastinal<br />
lymph nodes lying posterior to the aortic arch. <strong>The</strong><br />
lymphatic drainage of the lungs is first to the subcarinal<br />
and paratracheal nodes and then to the supraclavicular<br />
nodes and thoracic duct. Through biopsy of these nodes,<br />
a diagnosis can be established, and suitability for thoracotomy<br />
and tumor resection can be determined. Proximal<br />
bronchial lesions often metastasize to the mediastinum,<br />
whereas peripheral lesions do not. Mediastinoscopy is less<br />
useful in patients with left lung tumors because these<br />
tumors usually spread to the subaortic lymph nodes that<br />
are not accessible via the mediastinoscope. <strong>The</strong>se subaortic<br />
nodes are approached by an anterior thoracotomy<br />
through the second or third intercostal space (Chamberlain<br />
operation). Malignant spread of the tumor to the<br />
contralateral mediastinal nodes is an absolute contraindication<br />
to surgical resection of the tumor, whereas metastasis<br />
to the ipsilateral nodes does not rule out resection.<br />
Traditional mediastinoscopy is performed via a transverse<br />
incision just above the suprasternal notch.<br />
Following anteriorly to the trachea, the tip of the mediastinoscope<br />
is passed behind the innominate (brachiocephalic)<br />
vessels and the aortic arch. Mediastinoscopy is<br />
usually not performed if the patient has had a previous<br />
mediastinoscopy. This is because of scarring and loss of<br />
usual tissue planes.<br />
Mediastinoscopy can be performed under local anesthesia,<br />
but an awake patient breathing spontaneously<br />
would be at increased risk for venous air embolism
382 S.M. Neustein and J.B. Eisenkraft<br />
because of negative intrathoracic inspiratory pressure<br />
and for mediastinal trauma if the patient moves. It has<br />
been claimed that performing mediastinoscopy under<br />
local anesthesia is safer in those patients with limited<br />
pulmonary reserve and cerebrovascular disease, both of<br />
which are more common in the elderly. 37 However,<br />
general anesthesia is usually preferred for mediastinoscopy<br />
and should include paralysis to prevent patient<br />
movement and coughing that could lead to intrathoracic<br />
venous congestion and possible intrathoracic trauma.<br />
Mediastinoscopy is performed with the patient in the<br />
supine position and the neck hyperextended. <strong>The</strong> elderly<br />
patient may not be able to tolerate this position as well<br />
as the younger individual, and it is advisable to test the<br />
patient’s range of neck motion before induction of general<br />
anesthesia.<br />
<strong>The</strong> most common complication of mediastinoscopy is<br />
hemorrhage, which can be sudden and massive. Blood<br />
should therefore be available before starting the procedure.<br />
Emergency thoracotomy or sternotomy may be<br />
required to stop the bleeding, although surgical tamponade<br />
via the mediastinoscope may be done as a temporizing<br />
measure. Needle aspiration of any structure before its<br />
biopsy is done so that a major vessel will not be accidentally<br />
biopsied. If the bleeding is venous, a large-bore<br />
intravenous catheter should be placed in a vein in a lower<br />
extremity, because fluid and medications given into an<br />
upper extremity vein in this situation will drain into the<br />
mediastinum. 38 A torn mediastinal vein may also lead to<br />
an air embolus, especially if the patient is breathing spontaneously.<br />
<strong>The</strong> reverse Trendelenburg position can<br />
decrease venous pressure and therefore bleeding, but this<br />
also increases the potential for venous air embolism.<br />
A pneumothorax may occur during mediastinoscopy,<br />
which may necessitate placement of a chest tube. <strong>The</strong><br />
recurrent laryngeal nerve may be injured. <strong>The</strong> nerve<br />
may be damaged by the mediastinoscope or compressed<br />
by the tumor. Bilateral recurrent laryngeal nerve injury<br />
may lead to airway obstruction after tracheal extubation<br />
and spontaneous ventilation by the patient. An additional<br />
potential complication is arrhythmias that may occur<br />
because of stimulation of pressor receptors in the<br />
aortic arch.<br />
<strong>The</strong> mediastinoscope may compress the innominate<br />
(brachiocephalic) artery, leading to a decrease in blood<br />
flow in the common carotid and right subclavian arteries.<br />
This has been misdiagnosed as a cardiac arrest. 39 Transient<br />
left hemiparesis has also been reported after mediastinoscopy.<br />
40 <strong>The</strong> elderly patient is more likely to have a<br />
history of neurovascular insufficiency and be at risk for<br />
this complication. <strong>The</strong> blood pressure can be measured<br />
in the left arm, but the pulse in the right arm should be<br />
monitored continuously. <strong>The</strong> pulse is monitored most<br />
sensitively by an arterial catheter and pressure transducer<br />
system and less sensitively by a pulse oximeter.<br />
A damped right radial pulse pressure is an indication<br />
for repositioning of the mediastinoscope, relieving compression<br />
of the innominate artery. Other complications<br />
of mediastinoscopy include tracheal collapse, tension<br />
pneumomediastinum, hemothorax, and chylothorax. A<br />
chest radiograph should be obtained in the immediate<br />
postoperative period if a pneumothorax is suspected,<br />
and is taken routinely in many centers.<br />
Thoracotomy<br />
Pulmonary resection (pneumonectomy or lobectomy) is<br />
the most frequently performed thoracic surgical procedure.<br />
Whenever possible, a lobectomy rather than a pneumonectomy<br />
is done for a primary tumor, because this<br />
procedure is associated with a lower morbidity and mortality<br />
but offers a similar prognosis to the more extensive<br />
procedure. 11<br />
<strong>The</strong> elderly have a higher mortality rate than younger<br />
patients undergoing thoracotomy. 1 In one series, the<br />
operative mortality in elderly patients undergoing pneumonectomy<br />
was 22%, compared with 3.2% in younger<br />
patients. 41<br />
Cardiovascular Complications<br />
Arrhythmias are a common perioperative complication<br />
after pulmonary resection and may not be as well tolerated<br />
in the elderly. <strong>The</strong> older patient is more likely<br />
to have diastolic dysfunction and the less compliant ventricle<br />
is more dependent on the atrial contraction<br />
for proper filling. Atrial arrhythmias are more likely to<br />
cause hypotension in the geriatric patient. Arrhythmias<br />
are more common in patients older than 50 years undergoing<br />
pulmonary resection and are more frequently<br />
related to right pneumonectomy as compared with left<br />
pneumonectomy.<br />
In a retrospective study of 236 patients, a 22% incidence<br />
of perioperative arrhythmias has been reported in<br />
the perioperative period of pneumonectomies. 42 Atrial<br />
fibrillation, which made up 64% of all arrhythmias, was<br />
the most common. In 55%, the arrhythmias persisted, and<br />
there was a 31% in-hospital mortality rate in this group.<br />
Prophylactic perioperative digitalization can reduce the<br />
incidence of arrhythmias 43,44 but has the potential for<br />
toxicity and contributing to arrhythmias. A prospective,<br />
controlled, randomized clinical study in 140 consecutive<br />
patients reevaluated the role of prophylactic digoxin<br />
in relation to thoracic surgical procedures. 45 Patients were<br />
randomly allocated to receive no digoxin or digoxin<br />
0.5 mg twice on the night before surgery, followed by<br />
0.25 mg with premedication. Postoperatively, patients<br />
received digoxin 0.25 mg per day for 9 days. <strong>The</strong> dose of
26. Thoracic Procedures 383<br />
digoxin was adjusted according to serum level, and<br />
patients were monitored by EKG. <strong>The</strong> overall mortality<br />
was 5.7%. <strong>The</strong> investigators found no significant difference<br />
in the incidence of arrhythmias between the two<br />
groups and concluded that prophylactic digitalization in<br />
elective thoracic operations is not justified.<br />
<strong>The</strong> use of perioperative metoprolol can reduce the<br />
incidence of atrial fibrillation after thoracotomy for lung<br />
resection. 46 In this prospective, randomized, double-blind<br />
study, the incidence of arrhythmias was 6.7% after metoprolol<br />
versus 40% in the control group.<br />
Monitoring<br />
Hypoxemia is likely during one-lung ventilation, and continuous<br />
monitoring using pulse oximetry is the standard<br />
of care. Patients undergoing pulmonary resection should<br />
have an indwelling arterial catheter for continuous blood<br />
pressure monitoring and arterial blood sampling. Central<br />
venous access allows for central delivery of drugs for<br />
treatment of arrhythmias, hypotension, measurement of<br />
pressure, and can guide the anesthesia provider in fluid<br />
therapy management.<br />
Elderly patients are more likely to have cardiovascular<br />
disease, and their management may be facilitated by the<br />
use of a pulmonary artery catheter. Patients are at greater<br />
risk for pulmonary edema after pneumonectomy because<br />
of a decreased pulmonary vasculature cross-sectional<br />
area (increased pulmonary vascular resistance); thus,<br />
a pulmonary artery catheter may be of even more value<br />
in these cases. If a pulmonary artery catheter is placed<br />
for pneumonectomy, it is imperative that its tip not be in<br />
the pulmonary artery of the lung to be resected at the<br />
time of ligation. It may be necessary to withdraw the<br />
catheter at the time of pulmonary artery ligation and to<br />
then re-advance the catheter after the ligation.<br />
Transesophageal echocardiography (TEE) may be<br />
useful during thoracic surgery. It may help to delineate<br />
the anatomy if a tumor is invading or compressing the<br />
heart. 47 It can provide real-time estimation of myocardial<br />
function and ventricular filling. <strong>The</strong> elderly patient is<br />
more likely to have a decrease in cardiac function and<br />
therefore is more likely to require central venous monitoring<br />
and/or TEE monitoring.<br />
Airway Management<br />
<strong>The</strong> placement of a double-lumen endobronchial tube<br />
allows collapse of the operated lung, making the surgical<br />
resection easier. It also facilitates suctioning and application<br />
of continuous positive airway pressure to the nonventilated<br />
lung. <strong>The</strong> most common approach to lung<br />
separation is the use of a left-sided double-lumen tube,<br />
except when the left mainstem bronchus is diseased. <strong>The</strong><br />
left mainstem bronchus, being longer than the right mainstem<br />
bronchus, permits placement of a left-sided endobronchial<br />
tube with a smaller chance of upper lobe<br />
obstruction. In the case of a left pneumonectomy, the<br />
tube must be withdrawn into the trachea before ligation<br />
of the bronchus.<br />
Another alternative is placement of an endobronchial<br />
tube into the nonoperative side, so as to avoid disruption<br />
of a potentially diseased bronchus and to avoid repositioning<br />
in the case of a pneumonectomy. A disadvantage<br />
of this method is that upper lobe obstruction is likely to<br />
cause hypoxemia during one-lung ventilation, because<br />
this is the lung to be ventilated during surgery of the<br />
contralateral lung.<br />
A third method is placement of the endobronchial tube<br />
into the operated side. <strong>The</strong> advantage of this method is<br />
that upper lobe obstruction during one-lung ventilation<br />
is not more likely to lead to hypoxemia, because this lung<br />
will be collapsed during one-lung anesthesia. However, in<br />
the case of a right thoracotomy, the presence of the tube<br />
in this short bronchus may interfere with the surgeon’s<br />
ligation of the bronchus.<br />
Intubation is more likely to be difficult in the elderly<br />
if there is arthritis of the neck, with consequent limitation<br />
of mobility. Arthritis of the temporomandibular joint<br />
may cause limitation of mouth opening. However, if the<br />
patient is edentulous, which is also more likely in the<br />
elderly, the intubation may be easier. Thus, increased age<br />
may have the effect of making intubation easier or more<br />
difficult. Each patient must therefore be evaluated<br />
individually.<br />
In the case of a difficult intubation, it may be preferable<br />
to begin by placing a single-lumen tube. A tube exchanger<br />
can then be used to replace the single-lumen tube with<br />
a double-lumen tube. Alternatively, one-lung ventilation<br />
could be facilitated with a bronchial blocker placed<br />
through the single-lumen tube into the bronchus of the<br />
lung to be deflated. Two blockers that are now available<br />
are the Arndt and the Cohen tip-deflecting blocker. <strong>The</strong><br />
Arndt blocker (Cook Critical Care, Bloomington, IN) has<br />
a lumen with a wire extending through it, ending in a<br />
loop. A fiberscope is passed through the loop and is used<br />
to guide the blocker into place. More recently, the Cohen<br />
tip-deflecting blocker (Cook Critical Care) has been<br />
introduced. This blocker has an internal wire, which<br />
allows the tip to be angled and directed into either bronchus.<br />
<strong>The</strong>re is a wheel at the proximal end that, when<br />
turned, bends (flexes) the tip of the blocker.<br />
Intraoperative Anesthetic Management<br />
Most pulmonary resections are performed with the<br />
patient in the lateral decubitus position and via a posterolateral<br />
incision. After transection of the chest wall muscles,
384 S.M. Neustein and J.B. Eisenkraft<br />
the pleural space is entered either by rib resection or via<br />
an intercostal space. <strong>The</strong> lung should be collapsed before<br />
this entry to prevent injury. <strong>The</strong> lung resection is accomplished<br />
with ligation of the arterial and venous vessels,<br />
and the bronchus of the diseased lobe or lung.<br />
Blood loss is usually not severe enough to require<br />
transfusion during lobectomy or pneumonectomy, but<br />
blood should be available. Blood loss is likely to be<br />
greater during pleuropneumonectomy, pleurectomy, or<br />
decortication, and the patient is more likely to require<br />
blood transfusion. Measurement of central venous pressure<br />
and hematocrit, and estimation of blood loss assist<br />
in guiding fluid administration. A fluid warmer is important<br />
because heat loss may occur during thoracotomy, and<br />
hypothermia will delay extubation and increase the likelihood<br />
of arrhythmias.<br />
After lung resection, there is a reduction in the pulmonary<br />
vascular bed and an increased risk of pulmonary<br />
edema, especially after a pneumonectomy. 48 Fluids should<br />
therefore be given cautiously during and after pneumonectomy.<br />
Fluid overload in this situation may also cause<br />
right atrial distention and arrhythmias. <strong>The</strong> elderly have<br />
a decreased ability to tolerate these hemodynamic aberrations<br />
and, with a reduced cardiac function, would be<br />
more likely to develop pulmonary edema. Hypotension<br />
could lead to inadequate coronary artery perfusion, myocardial<br />
ischemia, and possibly infarction.<br />
Maintenance of general anesthesia can be accomplished<br />
using a potent inhaled anesthetic agent and neuromuscular<br />
blocking drug to prevent movement of the<br />
diaphragm. <strong>The</strong> elderly patient with limited cardiac<br />
reserve may not tolerate a potent inhaled agent and may<br />
require a high-dose opioid technique in which case ventilation<br />
must be continued postoperatively. 49 However, in<br />
contrast to high-dose fentanyl, an infusion of remifentanil<br />
can decrease the requirement for a potent inhaled agent<br />
and still allow the patient to awaken promptly after the<br />
surgery. A high Fio 2 is needed during one-lung anesthesia,<br />
but, after this, the addition of nitrous oxide can also facilitate<br />
an earlier extubation by allowing use of lesser<br />
amounts of potent inhaled anesthetic agent.<br />
After lung resection and before reinflation of remaining<br />
lung tissue, the endobronchial tube should be suctioned.<br />
<strong>The</strong> bronchial suture line is tested by applying<br />
20–40 cm H 2 O pressure using manual compression of the<br />
anesthesia circuit reservoir bag. Before closure of the<br />
chest, complete reexpansion of remaining lung tissue<br />
should be visually confirmed. Thoracostomy tubes are<br />
placed for drainage of air and fluid after a lobectomy.<br />
<strong>The</strong>se tubes are not placed if a pneumonectomy has been<br />
performed, because there is no remaining lung tissue to<br />
reexpand. In this case, the use of nitrous oxide can lead<br />
to a tension pneumothorax once the chest is closed,<br />
because there is no tube to vent the space. After skin<br />
closure and return of the patient to the supine position,<br />
pressure in the postpneumonectomy thoracic cavity space<br />
is relieved by needle aspiration. <strong>The</strong> trachea may be<br />
extubated immediately after surgery, depending on the<br />
preoperative condition of the patient, temperature,<br />
hemodynamic stability, and extent of surgery and technique<br />
used (e.g., opioid versus potent inhaled agent).<br />
Early return to spontaneous ventilation is advantageous,<br />
because it can decrease an air leak from the lung and<br />
reduce stress on bronchial sutures. <strong>The</strong> double-lumen<br />
tube is generally replaced with a single-lumen endotracheal<br />
tube if the trachea is to remain intubated postoperatively.<br />
However, the airway may be edematous, and if<br />
intubation before the procedure was difficult, it may be<br />
prudent to change the tube over a guide or perhaps even<br />
not change the tube at all. <strong>The</strong> surgeon may request that<br />
the double-lumen tube be changed to a single-lumen tube<br />
after the resection in order to perform bronchoscopy.<br />
Postoperative Complications<br />
Several life-threatening complications may occur after<br />
thoracic surgery, and individual outcome is related to the<br />
underlying condition of the patient, which may be further<br />
impaired by aging. Outcome is also related to the extent<br />
of surgery.<br />
Cardiopulmonary complications include arrhythmias,<br />
which are more frequent after pneumonectomy. Factors<br />
predisposing to arrhythmias include sympathetic stimulation<br />
from pain, intraoperative cardiac manipulation, and<br />
a reduced vascular bed from the pulmonary resection. 50<br />
Arrhythmias that frequently occur after pneumonectomy<br />
include atrial tachycardia, atrial flutter, and atrial fibrillation.<br />
Multifocal atrial tachycardia is common in patients<br />
with obstructive pulmonary disease and right-sided heart<br />
strain. <strong>The</strong> elderly in particular are prone to circulatory<br />
compromise from these arrhythmias. 51 Right-sided heart<br />
failure may present in the postoperative period from a<br />
reduction in the pulmonary vascular bed.<br />
Other postoperative pulmonary complications include<br />
atelectasis, which may be related to intraoperative lung<br />
retraction and manipulation, impaired clearance of secretions,<br />
splinting from pain, or incomplete reexpansion<br />
of the remaining lung tissue after one-lung anesthesia.<br />
Atelectasis may lead to pneumonia, which can be fatal in<br />
the setting of the reduced lung tissue postthoracotomy. 50<br />
<strong>The</strong> elderly patient is more likely to have limited pulmonary<br />
reserve and be more affected by a pneumonia. <strong>The</strong><br />
removal of lung tissue, especially a right-sided pneumonectomy,<br />
puts the patient at risk for pulmonary edema<br />
because of a reduced vascular bed and increased pulmonary<br />
arterial pressures. Fluid is therefore more likely to<br />
move into the lung interstitium according to the Starling<br />
forces. Pulmonary embolism may occur in the postoperative<br />
period, possibly originating from the remaining
26. Thoracic Procedures 385<br />
pulmonary artery stump or tumor tissue. An elderly<br />
patient with limited cardiopulmonary reserve may require<br />
a longer period of postoperative ventilatory support than<br />
a younger person undergoing a similar procedure.<br />
Potential structural complications requiring rapid<br />
surgical treatment include cardiac herniation, tension<br />
pneumothorax, and hemorrhage. Cardiac herniation is a<br />
rare but catastrophic complication. It may occur after<br />
pneumonectomy, in which the heart herniates through a<br />
pericardial defect. To help avoid this complication, the<br />
patient should not be turned lateral, with the operative side<br />
dependent.<br />
A tension pneumothorax can occur, even if chest tubes<br />
are placed, if they are not functioning properly or become<br />
occluded. A pneumothorax created by the placement of<br />
a central venous catheter into the nonoperative side of<br />
the chest is particularly hazardous both intraoperatively<br />
and postoperatively, because this is the only lung to be<br />
ventilated during one-lung anesthesia, and takes on an<br />
even greater role after resection of the other lung.<br />
Hemorrhage may be caused by slipped sutures or<br />
ligatures, bleeding from raw lung surfaces, or damaged<br />
bronchial or intercostal arteries. Postoperative neurologic<br />
complications may be related to the surgery or to<br />
positioning. Surgical injuries can affect the phrenic nerve,<br />
recurrent laryngeal nerve, and spinal cord. <strong>The</strong> lateral<br />
decubitus position can lead to damage to the brachial<br />
plexus, radial nerve, ulnar nerve, sciatic nerve, and<br />
common peroneal nerve.<br />
A bronchopleural fistula may develop after pulmonary<br />
resection, either immediately or even years later. 52 It<br />
carries a mortality rate of >20%. It may result from dehiscence<br />
of the bronchial stump after lung resection. Treatment<br />
includes reduction of the air leak and prevention of<br />
infection. Surgical intervention may be required. Placement<br />
of a double-lumen endobronchial tube into the<br />
contralateral mainstem bronchus can allow exclusive<br />
contralateral ventilation and isolation of the contralateral<br />
lung. An alternative is the use of high-frequency jet<br />
ventilation, which allows ventilation with lower airway<br />
pressures. 32<br />
Postthoracotomy Pain Management<br />
Thoracic surgery is often followed by pain and pulmonary<br />
dysfunction because of the thoracic incision. <strong>The</strong>re<br />
is a decreased functional residual capacity and vital<br />
capacity, which in association with pain produces atelectasis,<br />
hypoxia, and CO 2 retention. 53 Traditionally, opioids<br />
have been administered intravenously or intramuscularly<br />
to treat postthoracotomy pain. <strong>The</strong> disadvantage of these<br />
methods is that administering an amount of opioid adequate<br />
to relieve pain is likely to cause sedation and respiratory<br />
depression. <strong>The</strong> elderly patient is more likely<br />
to have pulmonary dysfunction and decreased central<br />
nervous system activity and is even more likely to have<br />
postoperative impairment of pulmonary function.<br />
Patient-controlled analgesia (PCA) is preferred over<br />
the intermittent administration of pain medications. A<br />
basal continuous delivery of medication can be programmed<br />
in addition to boluses. Patients have been<br />
reported to have less pain and sedation with PCA as<br />
compared with intramuscular opioids. 54,55 Patients who<br />
receive PCA after thoracotomy have been reported to<br />
require less pain medication and have a lower incidence<br />
of pulmonary complications. 56 PCA also allows patients<br />
to feel less dependent and helpless, and it is generally well<br />
accepted. <strong>The</strong> elderly patient is also more sensitive to the<br />
respiratory depressant effects of systemically administered<br />
opioids. It may be preferable to not use a basal<br />
infusion rate, but rather to use only demand dosing in<br />
the interest of safety.<br />
Ketorolac, a nonsteroidal antiinflammatory agent, does<br />
not cause respiratory depression and therefore may be<br />
a useful adjunct in the elderly. Ketorolac should not<br />
be used if there has been significant bleeding because<br />
it inhibits platelet function and can lead to further<br />
bleeding.<br />
Cryoanalgesia can be accomplished by the direct application<br />
of a cryoprobe intraoperatively by the surgeon to<br />
the intercostal nerves, which reduces but does not eliminate<br />
postthoracotomy pain; it is usually used together<br />
with other analgesic treatments. Disadvantages include<br />
prolonged anesthesia, possible permanent nerve trauma,<br />
and the loss of intercostal muscle tone. 57<br />
Spinal opioids administered into either the epidural or<br />
subarachnoid space provide excellent analgesia for<br />
patients after thoracotomy. Spinal opioids work by<br />
binding to opioid receptors in the substantia gelatinosa<br />
of the spinal cord. Intrathecal (subarachnoid) opioids can<br />
bind directly to the spinal cord, whereas those administered<br />
into the epidural space travel to the spinal cord<br />
by either passing through the dura 58 or by being absorbed<br />
into blood vessels that supply the spinal cord. 59 <strong>The</strong><br />
analgesia provided by spinal opioids is attributable to<br />
the effect on the spinal cord, as opposed to a systemic<br />
effect.<br />
<strong>The</strong> subarachnoid injection of morphine can produce<br />
analgesia with a much smaller dose (10–15 µg/kg) than<br />
produced by the intravenous, intramuscular, or oral<br />
routes. 60,61 Patients are more comfortable postoperatively,<br />
and less sedated when given subarachnoid opioids. 62,63 If<br />
given before the surgical incision, subarachnoid opioids<br />
have been reported to decrease the intraoperative general<br />
anesthetic requirement. 64 This technique would limit the<br />
amount of opioids required for analgesia. <strong>The</strong> use of<br />
intrathecal morphine carries with it the risk of delayed<br />
respiratory depression. <strong>The</strong> rostral spread of intrathecal<br />
morphine is greater than that of other opioids that are
386 S.M. Neustein and J.B. Eisenkraft<br />
lipophilic and therefore bind to spinal opioid receptors<br />
rapidly and are reabsorbed into blood vessels.<br />
<strong>The</strong> placement of an epidural catheter allows for<br />
repeated doses and therefore provides a longer duration<br />
of analgesia than the “one-shot” injection of subarachnoid<br />
morphine. Epidural fentanyl has been administered<br />
as a continuous infusion to provide postoperative<br />
analgesia. If given through a lumbar epidural catheter,<br />
the fentanyl should be diluted to a volume of at least<br />
20 mL so that the fentanyl can reach the thoracic levels<br />
of the spinal cord. 65,66 Patient-controlled epidural analgesia<br />
may allow for improved pain treatment, compared<br />
with intravenous PCA. 67,68 In a large series of patients,<br />
epidural analgesia resulted in less intravenous morphine<br />
usage. 69 This would be an important consideration in<br />
the elderly.<br />
<strong>The</strong> intravenous administration of ketorolac may be<br />
helpful, even in the presence of an epidural, to treat<br />
shoulder pain that may occur from being in the lateral<br />
position for an extended period of time. Epidurally<br />
administered local anesthetic is not effective in treating<br />
shoulder pain of this origin.<br />
In a recent review of 165 studies, which included almost<br />
20,000 patients, the results of three methods of postoperative<br />
analgesia after major surgery were reported. 70<br />
<strong>The</strong> three different routes of treatment studied were<br />
intramuscular, PCA, and epidural. <strong>The</strong> highest degree<br />
of oxygen hemoglobin desaturation was associated<br />
with intramuscular analgesia (37%). <strong>The</strong> incidence of<br />
respiratory depression, as reflected by usage of nalox -<br />
one, was highest with intramuscular PCA (1.9%).<br />
Hypotension was most often associated with the epidural<br />
route (5.6%).<br />
<strong>The</strong> technique of interpleural analgesia was first<br />
described in 1986. 71 <strong>The</strong> injection of local anesthetic<br />
between the visceral and parietal layers of pleura may<br />
either block multiple intercostal nerves or the thoracic<br />
sympathetic chain. For patients undergoing thoracotomy,<br />
the catheter can be placed through an epidural needle<br />
under direct vision while the chest is open. This method<br />
of placement can avoid the risk of pneumothorax and<br />
aberrant placement of the catheter when performed<br />
percutaneously.<br />
<strong>The</strong> results of interpleural block for postoperative pain<br />
relief after thoracotomy have been mixed, ranging from<br />
poor 72,73 to excellent analgesia. 74–76 Chest tubes should not<br />
be placed on suction for approximately 15 minutes after<br />
the injection of local anesthetic, because this would lead<br />
to removal of local anesthetic and a decrease in analgesic<br />
effect of the block. 72 Systemic toxicity is more likely<br />
in the presence of pleural abnormality. 73 This technique<br />
may be an option when neuraxial analgesia is contraindicated.<br />
<strong>The</strong> elderly patient is more likely to have kyphoscoliosis,<br />
which may make placement of an epidural more<br />
difficult.<br />
Videothoracoscopy<br />
VAT is now being used for a variety of thoracic procedures,<br />
including pleural biopsy, lung biopsy and resection,<br />
closure of bronchopleural fistulas, pericardial biopsy,<br />
pleurodesis, and laser ablation of emphysematous<br />
bullae. 77–80 Even lobectomy can be performed by VAT.<br />
VAT uses small incisions to accommodate the video<br />
camera for on-screen visualization, and working instruments.<br />
This technique does not involve spreading of the<br />
ribs, and there is no need for the large incision that is<br />
required for open thoracotomy. <strong>The</strong>re generally is less<br />
postoperative pain and respiratory impairment than after<br />
a conventional thoracotomy. Postthoracotomy pain can<br />
otherwise cause splinting and limit deep breathing, coughing,<br />
and clearing of secretions. <strong>The</strong>re is a lower incidence<br />
of morbidity after thoracoscopy compared with thoracotomy.<br />
Thoracoscopy is better tolerated than thoracotomy<br />
by high-risk patients, which would include the elderly<br />
who have reduced cardiac and pulmonary function.<br />
Arrhythmias may still occur after VAT. 81 <strong>The</strong> use of epidural<br />
analgesia may help to reduce the incidence of<br />
arrhythmias. 81,82 Ketorolac may be a useful adjunct, especially<br />
if an epidural has not been placed.<br />
A procedure such as diagnostic VAT and pleural biopsy<br />
can be performed under general anesthesia, thoracic epidural<br />
anesthesia, or intercostal block. For procedures in<br />
which there is a high likelihood that thoracoscopy may<br />
not be adequate and a conventional thoracotomy may be<br />
required, unless it is expected that the patient can be<br />
easily tracheally intubated in the lateral position, general<br />
anesthesia is the best option. A double- or single-lumen<br />
tube with a bronchial blocker is required during general<br />
anesthesia to provide adequate surgical exposure. Insufflation<br />
of gas is usually not needed for visualization under<br />
these conditions.<br />
Videoscopic surgery, which carries a lower risk of morbidity<br />
and mortality, may be preferable in the elderly<br />
patient, who is at increased risk. 1 Patients undergoing<br />
either wedge resection or lobectomy for stage I lung<br />
cancer, which are tumors that have not spread to lymph<br />
nodes, have been reported to have similar 5-year survival<br />
rates. 83,84 Patients undergoing video-assisted lobectomies<br />
have been reported to have a lower incidence of complications<br />
than patients undergoing lobectomy with thoracotomy.<br />
85 Although long-term survival may be a less<br />
important consideration for the elderly than short-term<br />
results and complications, the long-term survival after<br />
video-assisted lobectomy seems to be similar to lobectomy<br />
via thoracotomy. A limited resection in the elderly<br />
may be preferable, because of a possible reduction in risk,<br />
and an increased incidence of diagnosis of stage I tumors. 1<br />
Age is a risk factor for mortality after thoracotomy;<br />
therefore, the increased usage of VAT is particularly<br />
advantageous in the elderly. 86
26. Thoracic Procedures 387<br />
Conclusion<br />
<strong>The</strong> anesthesia considerations for the elderly patient<br />
undergoing the most frequently performed thoracic<br />
surgical procedures have been briefly reviewed. Optimum<br />
anesthesia care of the elderly patient undergoing thoracic<br />
surgery requires an understanding of the principles<br />
of anesthesia for thoracic surgery coupled with an appreciation<br />
of the changes associated with aging. Most<br />
lung cancers occur in people older than 65 years of age,<br />
and surgical treatment should not be withheld based on<br />
age alone. 1<br />
References<br />
1. Jaklitsch MJ, Mery CM, Audisio RA. <strong>The</strong> use of surgery<br />
to treat lung cancer in elderly patients. Lancet 2003;4:<br />
463–471.<br />
2. Etzioni DA, Liu JH, O’Connell JB, Maggard MA, Ko CY.<br />
Elderly patients in surgical workloads: a population-based<br />
analysis. Am Surg 2003;69:901–905.<br />
3. Hurria A, Kris MG. Management of lung cancer in older<br />
adults. CA Cancer J Clin 2003;53:325–341.<br />
4. Cangemi V, Volpino P, D’Andrea N, et al. Lung cancer<br />
surgery in elderly patients. Tumori 1996;82:237–241.<br />
5. Levi F, La Vecchia C, Lucchini F, Negri E. Worldwide trends<br />
in cancer mortality in the elderly, 1955–1992. Eur J Cancer<br />
1996;32:652–672.<br />
6. Smetana GW. Preoperative pulmonary assessment of the<br />
older adult. Clin Geriatr Med 2003;19:35–55.<br />
7. Mery CM, Pappas AN, Lukanich JM, et al. Long-term<br />
survival of patients with early stage non-small cell lung<br />
cancer as a function of age and treatment modality. Chest<br />
2001;120:176.<br />
8. Damhuis RA, Schutte PR. Resection rates and perioperative<br />
mortality in 7899 patients with lung cancer. Eur Respir<br />
J 1996;9:7–10.<br />
9. National Cancer Institute. SEER Cancer Statistics Review<br />
1973–1997. Bethesda, MD: National Cancer Institute;<br />
2000.<br />
10. Hall SW. Cancer: special considerations in older patients.<br />
<strong>Geriatric</strong>s 1984;39:74–78.<br />
11. Kohman, LJ, Meyer JA, Ilkins PM, Oates RP. Random<br />
versus predictable risks of mortality after thoracotomy for<br />
lung cancer. Thorac Cardiovasc Surg 1986;91:551–554.<br />
12. Mizushima Y, Noto H, Sugiyama S, et al. Survival and prognosis<br />
after pneumonectomy in the elderly. Ann Thorac Surg<br />
1997;64:193–198.<br />
13. Osaki T, Shirakura T, Kodte M, et al. Surgical treatment of<br />
lung cancer in the octogenarian. Ann Thorac Surg 1994;<br />
57:188–193.<br />
14. Jaklitsch MT, DeCamp MM Jr, Liptay MJ, et al. Video<br />
assisted thoracic surgery in the elderly: a review of 307 cases.<br />
Chest 1996;110:751–758.<br />
15. Gerson MC, Hurst JM, Hertzberg VS, Baughman R, Rouan<br />
GS, Ellis K. Prediction of cardiac and pulmonary complications<br />
related to elective abdominal and non-cardiac thoracic<br />
surgery in geriatric patients. Am J Med 1990;88:101–107.<br />
16. Liu LL, Leung JM. Predicting adverse postoperative<br />
outcomes in patients aged 80 years or older. J Am Geriatr<br />
Soc 2000;48:405–412.<br />
17. Castillo R, Haas A. Chest physical therapy: comparative<br />
efficacy of preoperative and postoperative in the elderly.<br />
Arch Phys Med Rehabil 1985;66:376–379.<br />
18. Warner DO. Preventing postoperative pulmonary complications.<br />
<strong>Anesthesiology</strong> 2000;92:1467–1471.<br />
19. Gerson MC, Hurst JM, Hertzber VS, et al. Cardiac prognosis<br />
in non-cardiac geriatric surgery. Ann Intern Med 1985;<br />
103:832–837.<br />
20. Shore ET, Millman RD, Silage DA, et al. Ventilatory and<br />
arousal patterns during sleep in normal young and elderly<br />
subjects. J Appl Physiol 1985;59:1607.<br />
21. Rossi A, Ganassini A, Tantucci C, Grassi V. Aging and the<br />
respiratory system. Aging (Milano) 1996;8:143–161.<br />
22. Ganguly R, Craig CP, Waldman RH. Respiratory tract<br />
immunity in the aged. Z Erkr Atmungsorgane 1984;163:<br />
112–120.<br />
23. Van Dewater JM. Preoperative and postoperative techniques<br />
in the prevention of pulmonary complications. Surg<br />
Clin North Am 1980;60:1339–1348.<br />
24. Naunheim KS, Kesler KA, D’Orazio SA, et al. Lung cancer<br />
surgery in the octogenarian. Eur J Cardiothorac Surg 1994;<br />
8:453–456.<br />
25. Slinger P, Johnston MR. Preoperative assessment for pulmonary<br />
function. J Cardiothorac Vasc Anesth 2000;14:<br />
202–211.<br />
26. Ploeg AJ, Kappefeim P, van Tangeren, et al. Factors associated<br />
with perioperative complications and long-term results<br />
after pulmonary resection for primary carcinoma of the<br />
lung. Eur J Cardiothorac Surg 2003;23:26–29.<br />
27. Bernard L, Ferrand O, Benoit L. Identification of prognostic<br />
factors determining risk groups for lung resection. Ann<br />
Thorac Surg 2000;70:1161–1167.<br />
28. Nakahara K, Ohno K, Hashimoto J, et al. Prediction<br />
of postoperative respiratory failure in patients undergoing<br />
lung resection for cancer. Ann Thorac Surg 1988;46:549–<br />
552.<br />
29. Ferguson MK, Reeder LB, Mick R. Optimizing selection<br />
of patients for major lung resection. J Thorac Cardiovasc<br />
Surg 1995;109:275–283.<br />
30. Walsh GL, Morice RC, Putnam JB, et al. Resection of lung<br />
cancer is justified in high risk patients selected by oxygen<br />
consumption. Ann Thorac Surg 1994;58:704.<br />
31. Bollinger CT, Wyser C, Roser H, et al. Lung scanning and<br />
exercise testing for the prediction of postoperative performance<br />
in lung resection candidates at increased risk for<br />
complications. Chest 1995;108:341–348.<br />
32. Eisenkraft JB, Neustein SM. <strong>Anesthesia</strong> for special problems<br />
in thoracic surgery. Probl Anesth 1990;4:326–354.<br />
33. Frumin MJ, Epstein R, Cohen G. Apneic oxygenation in<br />
man. <strong>Anesthesiology</strong> 1959;20:789.<br />
34. Sanders RD. Two ventilating attachments for bronchoscopes.<br />
Del Med J 1967;39:1270.<br />
35. Vourc’h G, Fishler M, Michon F, et al. Manual jet ventilation<br />
vs. high frequency jet ventilation during laser resection of<br />
tracheobronchial stenosis. Br J Anaesth 1983;55:973.<br />
36. Carlens E. Mediastinoscopy: a method for inspection and<br />
tissue biopsy stenosis. Br J Anaesth 1983;55:973.
388 S.M. Neustein and J.B. Eisenkraft<br />
37. Morton JR, Guinn GA. Mediastinoscopy using local anesthesia.<br />
Am J Surg 1971;122:696.<br />
38. Roberts JT, Gissen AJ. Management of complications<br />
encountered during anesthesia for mediastinoscopy. Anesthesiol<br />
Rev 1979;6:31.<br />
39. Lee J, Salvatore AJ. Innominate artery compression simulating<br />
cardiac arrest during mediastinoscopy. Anesth Analg<br />
1976;55:748.<br />
40. Ashbaugh DG. Mediastinoscopy. Arch Surg 1970;100:568.<br />
41. Morandi U, Stefani A, Golinelli M, et al. Results of surgical<br />
resection in patients over the age of 70 years with non smallcell<br />
lung cancer. Eur J Cardiothorac Surg 1997;11:432–439.<br />
42. Krowke MJ, Pairolero PC, Trustek F, Payne WS, Bernatz PE.<br />
Cardiac dysrhythmia following pneumonectomy: clinical<br />
correlates and prognostic significance. Chest 1987;91:490–<br />
495.<br />
43. Burman SO. <strong>The</strong> prophylactic use of digitalis before thoracotomy.<br />
Ann Thorac Surg 1972;14:359–368.<br />
44. Shields TW, Unik GT. Digitalization for prevention of<br />
arrhythmias following pulmonary surgery. Surg Gynecol<br />
Obstet 1968;126:743–746.<br />
45. Ritchie AJ, Bowe P, Gibbons JRP. Prophylactic digitalization<br />
for thoracotomy: a reassessment. Ann Thorac Surg<br />
1990;50:86–88.<br />
46. Jakobsen CJ, Billie S, Ahlburg P. Perioperative metoprolol<br />
reduces the frequency of atrial fibrillation after thoracotomy<br />
for lung resection. J Cardiothorac Vasc Anesth 1997;11:<br />
746–751.<br />
47. Neustein SM, Cohen E, Reich D, et al. Transesophageal<br />
echocardiography and the intraoperative diagnosis of left<br />
atrial invasion by carcinoid tumor. Can J Anaesth 1993;40:<br />
664–666.<br />
48. Licker M, de Perrot M, Spiliopoulos A. Risk factor for acute<br />
lung injury after thoracic surgery for lung cancer. Anesth<br />
Analg 2003;97:1558–1565.<br />
49. Eisenkraft JB. Effects of anaesthetics on the pulmonary<br />
circulation. Br J Anaesth 1990;65:63–78.<br />
50. Gallagher C, Sladen RN, Lubarsky D. Thoracotomy. Postoperative<br />
complications. Probl Anesth 1990;4:393–415.<br />
51. Breyer RH, Sippe C, Pharr WF, et al. Thoracotomy<br />
in patients over age seventy years: ten year experience.<br />
J Thorac Cardiovasc Surg 1981;81:187.<br />
52. Hankins JR, Miller JE, Atlar S, et al. Bronchopleural fistula:<br />
thirteen-year experience with 77 cases. J Thorac Cardiovasc<br />
Surg 1978;76:755–762.<br />
53. Craig DB. Postoperative recovery of pulmonary function.<br />
Anesth Analg 1981;60:46–52.<br />
54. Bennett RL, Battenhorst RL, Graves D, et al. Patientcontrolled<br />
analgesia—a new concept of postoperative relief.<br />
Ann Surg 1982;195:700–705.<br />
55. Bennett RL, Baumann TJ, Graves DA, Griffen WD Jr.<br />
Patient controlled analgesia and analgesic outcome, nocturnal<br />
sleep, and spontaneous activity. Surg Forum 1987;35:<br />
57–59.<br />
56. Lange MP, Dahn MS, Jacobs LA. Patient-controlled analgesia<br />
versus intermittent analgesia dosing. Heart Lung 1988;17:<br />
495–498.<br />
57. Maiwand O, Makey AR, Rees A. Cryoanalgesia after thoracotomy.<br />
Improvement of technique and review of 600<br />
cases. J Thorac Cardiovasc Surg 1986;92:291–295.<br />
58. Nordberg G, Hedner T, Mellstrand T, et al. Pharmacokinetic<br />
aspect of epidural morphine analgesia. <strong>Anesthesiology</strong><br />
1983;58:545–551.<br />
59. Cousins MJ, Mather LE. Intrathecal and epidural administration<br />
of opioids. <strong>Anesthesiology</strong> 1984;61:276–310.<br />
60. Gray JR, Fromme GA, Nauss LA, Wang JK, Istrup DM.<br />
Intrathecal morphine for post-thoracotomy pain. Anesth<br />
Analg 1986;65:873–876.<br />
61. Kotob HIM, Hand CV, Moore RA, et al. Intrathecal morphine<br />
and heroin in humans: six-hour drug levels in spinal<br />
fluid and plasma. Anesth Analg 1986;65:718–722.<br />
62. Shulman M, Sandler AN, Bradley JW, Young PS, Brobrer J.<br />
Post-thoracotomy pain and pulmonary function following<br />
epidural and systemic morphine. <strong>Anesthesiology</strong> 1984;61:<br />
509–575.<br />
63. Samii J, Chavim M, Viars P. Postoperative spinal analgesia<br />
with morphine. Br J Anaesth 1981;53:817–820.<br />
64. Neustein SM, Cohen E. Intrathecal morphine during thoracotomy.<br />
Part II. Effect on postoperative meperidine requirements<br />
and pulmonary function tests. J Cardiothorac Vasc<br />
Anesth 1993;7:157–159.<br />
65. Whiting WG, Sandler AN, Lau LC, Chovaz PM. Analgesic<br />
and respiratory effects of epidural sufentanil in postthoracotomy<br />
patients. <strong>Anesthesiology</strong> 1988;609:36–42.<br />
66. Melendez J, Cirella VN, Delphin ES. Lumbar epidural fentanyl<br />
analgesia after thoracic surgery. J Cardiothorac Anesth<br />
1989;3:150–153.<br />
67. Mann C, Pouzeratte J, Eledjam JJ. Postoperative patientcontrolled<br />
analgesia in the elderly: risks and benefits of<br />
epidural versus intravenous administration. Drugs Aging<br />
2003;20:337–345.<br />
68. Alon E, Jaquenod M, Schaepp B. Post-operative epidural<br />
versus intravenous patient-controlled analgesia. Minerva<br />
Anestesiol 2003;69:473–476.<br />
69. Flisberg P, Rudin A, Linne R, et al. Pain relief and safety<br />
after major surgery. A prospective study of epidural and<br />
intravenous analgesia in 2696 patients. Acta Anaesthesiol<br />
Scand 2003;47:457–465.<br />
70. Cashman JN, Dolin SJ. Respiratory and hemodynamic<br />
effects of acute postoperative pain management: evidence<br />
from published data. Br J Anaesth 2004;93:212–223.<br />
71. Reiestad F, Stromskag KE. Interpleural catheter in the<br />
management of postoperative pain: a preliminary report.<br />
Reg Anaesth 1986;11:89–91.<br />
72. el-Baz N, Faber LP, Ivankovic AD, et al. Intrapleural infusion<br />
of local anesthetic: a word of caution. <strong>Anesthesiology</strong><br />
1988;68:809–810.<br />
73. Rosenberg PH, Scheinin BWA, Lepantalo MJ, et al. Continuous<br />
intrapleural infusion of bupivacaine for analgesia<br />
after thoracotomy. <strong>Anesthesiology</strong> 1987;67:811–813.<br />
74. Reddy Kanbam J, Hammon J, Parris WC, et al. Intrapleural<br />
analgesia for postthoracotomy pain and blood levels of<br />
bupivacaine following intrapleural injection. Can J Anaesth<br />
1989;36:106–109.<br />
75. Symreng T, Gomez MN, Rossi N. Intrapleural bupivacaine<br />
and saline after thoracotomy: effects on pain and lung function—a<br />
double blind study. J Cardiothorac Anaesth 1989;<br />
3:144–149.<br />
76. Tetik O, Islamoglu F, Ayan E, et al. Intermittent infusion<br />
of 0.25% bupivacaine through an intrapleural catheter for
26. Thoracic Procedures 389<br />
post-thoracotomy pain relief. Ann Thorac Surg 2004;77:<br />
284–288.<br />
77. Hasnin JU, Krasna MJ, Barker SJ, Weiman DS, Whitman<br />
GJR. Anesthetic consideration for thoracoscopic procedures.<br />
J Cardiothorac Vasc Anesth 1992;6:624–627.<br />
78. Wakabayashi A. Thoracoscopic ablation of blebs in the<br />
treatment of recurrent or persistent spontaneous pneumothorax.<br />
Ann Thorac Surg 1989;48:651–653.<br />
79. Torre M, Belloni P. Nd:YAG laser pleurodesis through thoracoscopy:<br />
new curative therapy in spontaneous pneumothorax.<br />
Ann Thorac Surg 1989;47:887–889.<br />
80. Barker SJ, Clarke C, Hyatt J, Le N, Bhakta C. Thoracoscopic<br />
laser ablation of bullous emphysema: an anesthetic case<br />
study. Anesth Analg 1991;72:S11.<br />
81. Neustein SM, Kahn P, Krellenstein D, et al. Incidence of<br />
arrhythmias after thoracic surgery: thoracotomy vs video-assist<br />
thoracoscopy. J Cardiothorac Vasc Anesth 1998;12:659–661.<br />
82. Oka T, Ozawa Y, Ohkubo Y. Thoracic epidural bupiv -<br />
acaine attenuates supraventricular tachyarrhythmias<br />
after pulmonary resection. Anesth Analg 2001;93:253–<br />
259.<br />
83. Faulkner SI. Is lobectomy the gold standard for stage I lung<br />
cancer in year 2000? Chest 2000;118:119S.<br />
84. Swanson SJ, Bueno R, Jaklitsch MT, et al. Subcentimeter<br />
non-small cell lung cancer: a program for detection and<br />
resection is warranted. Proceedings of the 80th Annual<br />
Meeting of the American Association of Thoracic Surgery,<br />
Toronto, Canada; 2000:70.<br />
85. Roberts JR, DeCamp MM, Mentzer SJ, Sugarbaker DJ. Prospective<br />
comparison of open and video assisted lobectomy.<br />
Chest 1996;110:45S.<br />
86. Jaklitsch MT, Pappas-Estocin A, Bueno R. Thoracoscopic<br />
surgery in elderly lung patients. Crit Rev Oncol Hematol<br />
2004;49:165–171.
27<br />
Cardiac Procedures<br />
James H. Abernathy III<br />
Our population, both nationally and worldwide, is getting<br />
increasingly older. <strong>The</strong> proportion of people aged 65 and<br />
older in the United States is projected to increase from<br />
35 million (12.4%) to 71 million (19.6%) by 2030 and 82<br />
million by 2050. 1 <strong>Global</strong> trends are similar: people aged<br />
65 and older are expected to make up 12% of the population<br />
by 2030 and 20% of the population by 2050. Considering<br />
that older patients have invasive procedures at<br />
almost four times the frequency of people younger than<br />
65, this will significantly affect our health care system. 2<br />
Because there are a greater number of older patients,<br />
surgery for cardiovascular disease is increasing. Compounding<br />
this, patients are increasingly presenting at an<br />
older age and later in their disease processes. For instance,<br />
in 1983, 12% of coronary artery bypass graft (CABG)<br />
patients were older than 65 years of age. Just 10 years<br />
later, half the patients undergoing CABG were older<br />
than 65 years of age. 3 Today, the average age of CABG<br />
surgery patients is 66 years of age. 4 For cardiac surgery,<br />
the 30-day mortality is estimated to increase by a factor<br />
of 1.55 per decade of age, compared with noncardiac<br />
surgery at 1.35 per decade of age. 5 However, despite<br />
the increasing age of our patients and the increased risk<br />
of morbidity and mortality as the patient population<br />
has aged, operative mortality from cardiac surgery has<br />
not substantially increased. <strong>The</strong> reasons for this are multifactorial<br />
including improved surgical techniques, dedicated<br />
cardiac anesthesiologists, better cardiopulmonary<br />
bypass (CPB) machines, improved pharmacologic interventions,<br />
and better anesthesia techniques and technology<br />
such as transesophageal echocardiography and<br />
epiaortic ultrasound.<br />
This chapter concentrates on the surgical interventions<br />
for elderly patients with heart disease. Surgical frequency,<br />
morbidity, and mortality between the aged population<br />
and younger patients are explored. In addition, strategies<br />
for preventing adverse outcomes in this unique patient<br />
cohort are presented.<br />
<strong>The</strong> Society of Thoracic Surgeons (STS) Cardiac<br />
Surgery Database was initiated in 1986 with the goal of<br />
providing risk-adjusted outcomes compared with the<br />
national experience. <strong>The</strong> data set contains detailed clinical<br />
information on more than 1.5 million registered<br />
patients undergoing cardiac surgical procedures from 541<br />
academic, private, military, and Veterans Affairs hospitals<br />
from 48 of the United States and Canada. It is the single<br />
best place to investigate risk factors and outcomes of<br />
cardiac operations. Most of what has been published<br />
regarding age and cardiac surgery revolves around multiple<br />
series from single institutions. 6–12 We focus mostly on<br />
those few studies that have utilized large databases such<br />
as the STS database.<br />
Coronary Artery Disease<br />
Coronary artery disease (CAD) continues to be a major<br />
contributor to mortality in the elderly. An even larger<br />
proportion of the elderly population experiences morbidity<br />
from their CAD. Approximately 40% of Americans<br />
will reach the age of 80 and, of these, 40% will have<br />
symptomatic heart disease. 13 Eighty-three percent of<br />
all cardiovascular deaths occur in patients older than<br />
65 years of age. 14 As the population ages, it is not surprising,<br />
therefore, that the median age of coronary artery<br />
bypass grafting has steadily increased to 66 years of<br />
age. Despite this increase in age at operation, there<br />
has been a significant decline in overall operative mortality<br />
and risk-adjusted mortality for CABG patients 15<br />
(Figure 27-1).<br />
Anesthesiologists and surgeons are faced with caring<br />
for older and sicker patients to palliate CAD. As previously<br />
discussed in this book, elderly patients present with<br />
multiple organ system disease resulting in less physiologic<br />
reserve than their younger counterparts. <strong>The</strong>y are more<br />
likely to have hypertension, diabetes mellitus, cerebral<br />
390
27. Cardiac Procedures 391<br />
2.00<br />
1.75<br />
O/E Ratio<br />
1.50<br />
1.25<br />
1.00<br />
0.75<br />
0.50<br />
All CABG Patients<br />
Subanalysis CABG Patients<br />
Medicare CABG Pts<br />
1990 1991 1992 1993 1994 1995 1996 1997 1998 1999<br />
Year of Procedure<br />
Figure 27-1. Observed mortality to expected mortality ratio (O/E), 1990–1999. CABG = coronary artery bypass graft. (Reprinted<br />
with permission from Ferguson et al. 15 Copyright © 2002. With permission of <strong>The</strong> Society of Thoracic Surgeons.)<br />
and peripheral vascular disease. Elderly patients presenting<br />
for coronary revascularization are more likely to be<br />
women, in New York Heart Association (NYHA) heart<br />
failure class IV, and have left main CAD. 16 Interestingly,<br />
in reviewing the STS database of more than 1 million<br />
patients, Ferguson et al. 15 found that, when compared<br />
with younger patients, fewer elderly patients are undergoing<br />
reoperative CABG, likely reflecting patient<br />
selection.<br />
Examining the extremes of the elderly population,<br />
Bridges et al. 17 investigated 575,389 nonagenarians and<br />
centenarians undergoing CABG. Patients older than 90<br />
years of age were more likely to be women, undergo<br />
urgent or emergent operations, have left main disease,<br />
unstable angina, and preoperative renal failure, and be in<br />
NYHA class IV. <strong>The</strong> overall operative mortality for these<br />
patients was 11% compared with 2.8% for those younger<br />
than 80 years of age. <strong>The</strong> multivariate analysis for operative<br />
mortality showed an increased risk for emergent or<br />
salvage operation [odds ratio (OR) 2.26], preoperative<br />
intraaortic balloon pump (IABP) (OR 2.79), perioperative<br />
renal failure (OR 2.08), defined as creatinine >2.0 and<br />
also more than twice the baseline value or a new requirement<br />
for dialysis, peripheral or cerebral vascular disease<br />
(OR 1.39), and mitral insufficiency (OR 1.50). This trend<br />
was evident in morbidity measures as well as with patients<br />
older than 90 having an increased risk of perioperative<br />
stroke (2.9%), renal failure (9.2%), prolonged ventilation<br />
(12.2%), and postoperative length of stay (median 7<br />
days). 17 In this population, if the patient did not have the<br />
preoperative risk factors of emergent operation, IABP,<br />
renal failure, peripheral vascular disease, or cerebral vascular<br />
disease, their operative mortality was only 7.2%.<br />
Surprisingly, this subpopulation accounted for 57% of the<br />
nonagenarians and centenarians undergoing CABG.<br />
Valvular Heart Disease<br />
As we age, the fibromuscular skeleton of the heart<br />
changes, including myxomatous degeneration and collagen<br />
infiltration, termed sclerosis. Aortic valve sclerosis is<br />
estimated to occur in 30% of elderly persons. Other agerelated<br />
changes include calcium deposition on the leaflets<br />
of the aortic valve, base of the semilunar cusps, and the<br />
mitral annulus. Fibrosis with valve calcification is the<br />
most common etiology of valvular stenosis in the elderly.<br />
Valvular regurgitation often occurs as a result of ischemia<br />
or hypertensive disease, especially at the mitral valve. 18<br />
<strong>The</strong> age of the patient presenting for a valve operation is<br />
ever increasing (Figure 27-2).<br />
Aortic Valve<br />
Aortic stenosis in patients older than 65 years of age is<br />
estimated to be 2% for severe stenosis, 5% for moderate<br />
stenosis, and 9% for mild stenosis. 18,19 Consequences of<br />
aortic stenosis, left ventricular hypertrophy, decreased<br />
left ventricular compliance, and decreased stroke volume<br />
are independent of etiology. <strong>The</strong> same process that causes
392 J.H. Abernathy III<br />
Mean Age (Years)<br />
72<br />
70<br />
68<br />
66<br />
64<br />
62<br />
60<br />
58<br />
AVR CAB+AVR MVR CAB+MVR<br />
86 87 88 89 90 91 92 93 94 95<br />
Year of Surgery<br />
Figure 27-2. Mean age by year and valve procedure. AVR =<br />
aortic valve replacement, CAB = coronary artery bypass, MVR<br />
= mitral valve replacement. (Reprinted with permission from<br />
Jamieson et al. 21 Copyright © 1999. With permission of <strong>The</strong><br />
Society of Thoracic Surgeons.)<br />
sclerosis of the aortic valve seems to also affect the coronaries<br />
and helps to explain the association between aortic<br />
valve disease and CAD.<br />
Aortic regurgitation also occurs with increasing frequency<br />
in the elderly. In one study, 13% of those older<br />
than 80 had mild aortic regurgitation, and 16% had either<br />
moderate or severe regurgitation. Patients with heart<br />
failure and pulmonary congestion from acute aortic<br />
regurgitation have a 50%–80% mortality. 20<br />
Morbidity and mortality data for elderly patients<br />
undergoing aortic valve replacement (AVR) has mostly<br />
come from small, single institution case series. <strong>The</strong> mortality<br />
rates have been quoted from 5% to 10%, depending<br />
on comorbidities. Using the STS database, Jamieson<br />
et al. 21 better quantified the operative mortality risk for<br />
patients undergoing valve replacements with or without<br />
CABG. Table 27-1 delineates the increased risk of mortality<br />
with increasing age. <strong>The</strong> operative risk for AVR<br />
almost doubles with every decade over 60 years of age.<br />
Independent predictors of mortality have been consistently<br />
shown to include age, emergent procedures,<br />
advanced NYHA class, and renal failure. However, in the<br />
STS analysis by Jamieson et al., 21 age was not an independent<br />
risk factor. Those of statistical significance included<br />
salvage status (OR 7.12), perioperative renal failure (OR<br />
4.32), emergent case (OR 3.46), reoperation (OR 2.27),<br />
cardiogenic shock (OR 1.67), NYHA class IV (OR 1.56),<br />
prior cerebrovascular accident (OR 1.44), previous myocardial<br />
infarction (OR 1.36), female gender (OR 1.25),<br />
and diabetes mellitus (OR 1.23).<br />
Chiappini et al. 22 retrospectively studied 115 patients<br />
with a mean age of 82 years who underwent AVR alone<br />
or in combination with CABG. <strong>The</strong> most common presenting<br />
symptoms were dyspnea in 99%, congestive heart<br />
failure in 15%, and angina in 77%. As expected in an<br />
extreme elderly population presenting for heart surgery,<br />
20% had an ejection fraction lower than 50%, 44% had<br />
significant CAD, and 78% presented in NYHA class III<br />
Table 27-1. Operative mortality rate by age group and valve position and population size (1986–1995, <strong>The</strong> Society of Thoracic<br />
Surgeons database).<br />
Age (years)<br />
Procedure<br />
50–59 60–69 70–79 80–89 90–99<br />
AVR<br />
Mortality rate (%) 2.9 3.2 5.3 8.5 14.5<br />
Population 3,686 7,001 8,468 2,756 69<br />
AVR + CABG<br />
Mortality rate (%) 4.7 5.1 8.6 12.5 18.8<br />
Population 1,709 6,120 10,617 3,717 64<br />
MVR<br />
Mortality rate (%) 4.1 6.1 9.8 13.4 25<br />
Population 2,815 4,062 3,576 621 4<br />
MVR + CABG<br />
Mortality rate (%) 8.6 12.3 18.4 25.1 42.9<br />
Population 1,050 2,889 3,782 730 7<br />
Multiple valves<br />
Mortality rate (%) 5.5 9.9 15.7 23.7 0<br />
Population 803 998 854 177 2<br />
Multiple + CABG<br />
Mortality rate (%) 10.3 16.5 21.4 26.6 100<br />
Population 155 430 612 154 2<br />
Source: Adapted with permission from Jamieson et al. 21 Copyright © 1999, with permission from <strong>The</strong> Society of Thoracic Surgeons.<br />
AVR = aortic valve replacement, CABG = coronary artery bypass graft, MVR = mitral valve replacement.
27. Cardiac Procedures 393<br />
or greater. <strong>The</strong> 30-day mortality rate was 8.5% with an<br />
actuarial survival rate of 86.4% at 1 year and 69% at 5<br />
years. <strong>The</strong>re was no statistically significant difference in<br />
the death rate, either in hospital or out of hospital,<br />
between AVR or AVR-CABG groups. Logistical regression<br />
analysis revealed that reduced preoperative ejection<br />
fraction, perioperative heart failure, and type of implanted<br />
device were predictors of late death. Those patients who<br />
received a bioprosthetic valve did much better than those<br />
who received a mechanical or stentless valve. Having a<br />
patient survive an operation is not the only endpoint<br />
worth discussing. <strong>The</strong> elderly have to do better in life<br />
post-repair than before. In this patient population, 98%<br />
of survivors were satisfied with their choice. <strong>The</strong>re was a<br />
statistically significant improvement in NYHA class, 2.9<br />
± 0.6 versus 1.6 ± 0.6, p < 0.01. 22<br />
Mitral Valve<br />
<strong>The</strong> aging process has a similar effect on the mitral valve<br />
as it does on the aortic valve. <strong>The</strong>se same factors also<br />
predispose patients to worse outcomes after mitral valve<br />
surgery. Left ventricular diastolic function, decreased systemic<br />
vascular compliance, increased left ventricular mass<br />
index, and altered neurohormonal and autonomic influences<br />
have been attributed to adverse outcomes in those<br />
undergoing mitral valve repair.<br />
Mehta et al. 23 analyzed data on all patients undergoing<br />
mitral valve replacements, either alone or in combination<br />
with CABG or tricuspid valve operation between January<br />
1997 to December 2000 who were enrolled in the STS<br />
database. Of the 262,718 patients in the database, 31,688<br />
met the criteria. Mitral valve replacement represents the<br />
only cardiac operation done more frequently in those<br />
patients who are older than 70 years of age than in any<br />
other age group. <strong>The</strong> elderly patients (>60 years of age)<br />
were more likely to undergo an urgent operation, have a<br />
concomitant CABG, and need the assistance of an IABP.<br />
Pump times and cross-clamp times were similar across all<br />
age groups.<br />
All in-hospital adverse events increased with advancing<br />
age including stroke, prolonged ventilation, reoperation<br />
for bleeding, renal failure, atrial fibrillation, and<br />
mortality. Multivariate models show that the risk of operative<br />
mortality increases with age, even after adjusting for<br />
other variables (Figure 27-3). Sadly, this indicates that a<br />
vigorous 80 year old has increased risk of mortality independent<br />
of other comorbidities. Using their multiple<br />
regression model, Mehta et al. proposed a classification<br />
tree for those older than 75 years of age contemplating<br />
mitral valve replacement (shown in Figure 27-4).<br />
–2.5<br />
–3.0<br />
Log Odds<br />
–3.5<br />
–4.0<br />
–4.5<br />
20 40 60 80 100<br />
Patient Age (Years)<br />
Figure 27-3. Plot of log odds of operative mortality for mitral valve replacement versus age, after adjusting for other risk factors.<br />
(Reprinted with permission from Mehta et al. 23 Copyright © 2002. With permission from <strong>The</strong> Society of Thoracic Surgeons.)
394 J.H. Abernathy III<br />
Hemodynamic<br />
Instability?<br />
No<br />
Renal<br />
Failure?<br />
No<br />
NYHA<br />
Class IV?<br />
No<br />
Yes<br />
Yes<br />
Yes<br />
Concomitant<br />
CABG?<br />
No<br />
Yes<br />
N<br />
Mortality<br />
997<br />
31.9<br />
589<br />
25.3<br />
1597<br />
15.7<br />
2207<br />
11.4<br />
2535<br />
7.7<br />
Figure 27-4. Risk classification tree for elderly patients (>75<br />
years) undergoing mitral valve replacement. NYHA = New<br />
York Heart Association, CABG = coronary artery bypass graft.<br />
(Reprinted with permission from Mehta et al. 23 Copyright ©<br />
2002. With permission of <strong>The</strong> Society of Thoracic Surgeons.)<br />
Preventing Adverse Outcomes<br />
Despite the existence of an increase in both morbidity<br />
and mortality for elderly patients undergoing cardiac<br />
surgery, relatively little is known about how to prevent it.<br />
Improvements in anesthesia techniques, medications, surgical<br />
techniques, and perfusion practices have improved<br />
cardiac surgical outcomes despite a population of advancing<br />
age. What little is known is covered in the following<br />
section.<br />
Cardiovascular<br />
Atrial fibrillation is a morbid event occurring in up to<br />
30% of elderly patients after cardiac surgery. Because of<br />
the elderly’s lower physiologic reserve, it is imperative to<br />
avoid beta-blocker and statin withdrawal, two offenders<br />
in postoperative atrial fibrillation. Additionally, their<br />
peripheral vascular system is more calcified and less distendable<br />
than younger patients. This increases their risk<br />
of aortic dissection and embolization with cannulation<br />
and initiation of CPB. Severe aortic disease or lower<br />
extremity vascular disease may increase the risk associated<br />
with IABP. Furthermore, poor coronary vasculature<br />
may predispose patients to incomplete revascularization<br />
and further ischemia after CPB. Ferguson et al. 24 demonstrated<br />
that the internal mammary artery was underutilized<br />
in elderly patients (77% for elderly versus 93% for<br />
younger). Those elderly patients who received an internal<br />
mammary artery bypass had a lower operative and postoperative<br />
mortality, even after controlling for other causative<br />
factors.<br />
Central Nervous System/Neurologic<br />
Neurologic injury remains one of the largest sources of<br />
morbidity and mortality after cardiac surgery. Its risk<br />
clearly increases with age, with quoted stroke risks ranging<br />
from 1% to 30% depending on age and operation. Figure<br />
27-5 demonstrates the increased risk of neurologic insult<br />
with increasing age. Roach et al. 25 studied adverse cerebral<br />
outcomes after CABG surgery in 2108 patients. Type<br />
I injuries were defined as death attributable to stroke or<br />
hypoxic encephalopathy, nonfatal stroke, transient ischemic<br />
attack, or stupor or coma at the time of discharge.<br />
Type II injuries were defined as new deterioration in<br />
intellectual function, confusion, agitation, disorientation,<br />
memory deficit, or seizure without evidence of focal<br />
injury. <strong>The</strong> predominant predictor of both type I and II<br />
injury was age: 6.1% of patients who were older than 70<br />
experienced a type I injury, and 5.8% experienced a type<br />
II compared with 1.9% and 1.8%, respectively, for those<br />
patients younger than 70 years of age. 25
27. Cardiac Procedures 395<br />
PROBABILITY OF MORBID EVENT<br />
0.200<br />
0.175<br />
0.150<br />
0.125<br />
0.100<br />
0.075<br />
0.050<br />
0.025<br />
0.000<br />
NEUROLOGIC DEFICIT<br />
LOW CARDIAC OUTPUT STATE<br />
MYOCARDIAL INFARCTION<br />
35 45 55 65 75 85 95<br />
AGE (YEARS)<br />
Figure 27-5. Probability of incurring a morbid event during<br />
the perioperative cardiac surgical period and its association<br />
with age. Neurologic deficits increase dramatically beginning<br />
at age 65, whereas low cardiac output state and myocardial<br />
infarction remain relatively stable. (Reprinted with permission<br />
from Tuman KJ, McCarthy RJ, Najafi H, Ivankovich AD.<br />
Differential effects of advanced age on neurologic and cardiac<br />
risks of coronary artery operations. J Thorac Cardiovasc Surg<br />
1992;104(6):1510–1517. Copyright © 1992. With permission of<br />
the American Association for Thoracic Surgery.)<br />
Suggested mechanisms of cerebral injury include global<br />
hypoperfusion, focal occlusion of the cerebral vasculature,<br />
or thermal injury on rewarming. It seems that,<br />
despite reductions in cerebral blood flow during CPB in<br />
the elderly, there is a concomitant reduction in cerebral<br />
metabolic rate of oxygen consumption keeping the difference<br />
in arterial-venous oxygen content normal. 26<br />
Embolic phenomena have been blamed as the most likely<br />
culprit in central nervous system damage in the elderly.<br />
It is for this reason that combined carotid endarterectomy<br />
and CABG in the elderly remains a debated topic.<br />
Detecting ascending aortic atheroma either by surgical<br />
palpation or epiaortic ultrasound has been shown to<br />
reduce embolic events and improve post-bypass cerebral<br />
outcomes. 27,28 pH management by either alpha-stat or<br />
pH-stat and the association with cerebral outcomes has<br />
been vigorously studied. pH stat, through increased CO 2 ,<br />
is associated with increased cerebral blood flow, but<br />
alpha-stat preserves cerebral autoregulation 29 (also J.P.<br />
Mathew et al., in press, <strong>Anesthesiology</strong>). Because most<br />
neurologic injuries are secondary to embolic phenomena,<br />
more cerebral blood flow may be detrimental. One prospective,<br />
randomized trial failed to show a difference<br />
between alpha-stat and pH-stat management in adult<br />
patients. 30 Based on preserving autoregulation, alpha-stat<br />
blood gas management would be recommended in the<br />
elderly. No intervention, however, has been studied in a<br />
population exclusive to those aged more than 65.<br />
Renal<br />
<strong>The</strong> prevalence of renal failure after cardiac operation<br />
varies from 2% to 15%, depending on the procedure and<br />
degree of preoperative renal dysfunction. 23 If it occurs,<br />
the mortality rate may be as high as 80%. Because the<br />
elderly have lower baseline glomerular filtration rate, are<br />
likely to have hypertension and an altered renal autoregulatory<br />
curve, and are more likely to have diabetes<br />
mellitus, they are at a higher risk of renal failure than<br />
their younger counterparts. <strong>The</strong> use of preoperative<br />
diuretics for those with depressed ejection fraction and<br />
radiopaque dyes often worsens preoperative renal function.<br />
Unfortunately, there has been no large investigation<br />
regarding the prevention of renal dysfunction in the<br />
elderly patient undergoing CPB. Mannitol as a scavenger<br />
of oxygen free-radicals and Lasix are often used but have<br />
not been specifically studied in the elderly population.<br />
<strong>The</strong> most important principle might be that recovery of<br />
renal function after bypass is directly related to the recovery<br />
of cardiac function.<br />
Cardiopulmonary Bypass Management<br />
CPB provides many alterations to the normal physiologic<br />
milieu. <strong>The</strong> optimal mean arterial pressure, perfusion<br />
flow, mode of perfusion (pulsatile versus nonpulsatile),<br />
pH and CO 2 management, temperature, and hematocrit<br />
have not been established for the elderly patient undergoing<br />
CPB. As previously mentioned, aortic cannula sites<br />
should be carefully chosen with the assistance of epiaortic<br />
ultrasound scanning to minimize embolized atheromatous<br />
debris. Perfusion flows range from 1.2 to 2.4 L/min/m 2 ,<br />
with perfusion pressures varying from 30 to 80 mm Hg.<br />
No difference in outcomes has been demonstrated for<br />
flows within this range or for pulsatile versus nonpulsatile<br />
flows. <strong>The</strong> appropriate temperature management (normothermia<br />
versus hypothermia) for the elderly patient<br />
has not been studied.<br />
<strong>The</strong> optimum hematocrit while on CPB and immediately<br />
after for the elderly patient has not been determined.<br />
<strong>The</strong> absolute safe level will depend on many<br />
variables, including adequacy of myocardial revascularization,<br />
myocardial function, and, possibly, the age of the<br />
patient. <strong>The</strong> adequacy of tissue oxygenation and perfusion<br />
as determined by the mixed venous oxygen saturation<br />
determines transfusion in most centers. Blood-sparing<br />
strategies such as cell salvage techniques and retrograde<br />
autologous prime should routinely be used to conserve<br />
hematocrit and decrease the need for transfusion. <strong>The</strong><br />
elderly might be a group for whom a higher hematocrit<br />
is beneficial; however, transfusion delivers new risks, most<br />
of which are related to the inflammatory response.<br />
Increased sternal wound infection, longer intensive care<br />
unit stays, and increased renal failure associated with
396 J.H. Abernathy III<br />
blood transfusion should be weighed against evidence of<br />
poor tissue oxygen delivery.<br />
With admittedly little scientific evidence to support<br />
their assertions, some authors empirically recommend<br />
the following: (1) alpha-stat blood gas management, (2)<br />
higher perfusion pressures throughout the perioperative<br />
period, (3) higher mean arterial pressures while on CPB,<br />
(4) higher hematocrit before termination of CPB (>24%),<br />
(5) mild hypothermia (32°C) during CPB, and (6) careful<br />
selection of the aortic cannulation site with the assistance<br />
of epiaortic ultrasound scanning. 31<br />
Conclusion<br />
We have demonstrated over the past several decades<br />
that, with continued focus on improving outcomes in<br />
cardiac surgery, we can be successful. Cardiac surgical<br />
patients are older, but their overall outcomes have<br />
improved. As our population ages, so too will our patients,<br />
and we will continue to push the envelope. Despite our<br />
successes, however, there are many unanswered questions.<br />
With continued vigilance, one day our recommendations<br />
will be more than empiric: they will be well-proven<br />
scientific assertions.<br />
References<br />
1. Centers for Disease Control and Prevention. Trends in<br />
aging—United States and worldwide. MMWR Morb Mortal<br />
Wkly Rep 2003;52(6):101.<br />
2. Lichtor J. Sponsored research reveals postoperative mortality<br />
stats. Anesth Patient Safety Found Newslett 1988;3:9–11.<br />
3. Gersh BJ, Kronmal RA, Schaff HV, et al. Long-term<br />
(5 year) results of coronary bypass surgery in patients 65<br />
years old or older: a report from the Coronary Artery<br />
Surgery Study. Circulation 1983;68(3 Pt 2):II190–199.<br />
4. Acinapura AJ, Jacobowitz IJ, Kramer MD, Adkins MS,<br />
Zisbrod Z, Cunningham JN Jr. Demographic changes in<br />
coronary artery bypass surgery and its effect on mortality and<br />
morbidity. Eur J Cardiothorac Surg 1990;4(4):175–181.<br />
5. Khuri SF, Daley J, Henderson W, et al. Risk adjustment of<br />
the postoperative mortality rate for the comparative assessment<br />
of the quality of surgical care: results of the National<br />
Veterans Affairs Surgical Risk Study. J Am Coll Surg 1997;<br />
185(4):315–327.<br />
6. Utley JR, Leyland SA. Coronary artery bypass grafting<br />
in the octogenarian. J Thorac Cardiovasc Surg 1991;101(5):<br />
866–870.<br />
7. Edmunds LH Jr, Stephenson LW, Edie RN, Ratcliffe MB.<br />
Open-heart surgery in octogenarians. N Engl J Med 1988;<br />
319(3):131–136.<br />
8. Samuels LE, Sharma S, Morris RJ, et al. Cardiac surgery in<br />
nonagenarians. J Card Surg 1996;11(2):121–127.<br />
9. Akins CW, Daggett WM, Vlahakes GJ, et al. Cardiac operations<br />
in patients 80 years old and older. Ann Thorac Surg<br />
1997;64(3):606–614; discussion 614–615.<br />
10. Avery GJ 2nd, Ley SJ, Hill JD, Hershon JJ, Dick SE. Cardiac<br />
surgery in the octogenarian: evaluation of risk, cost, and<br />
outcome. Ann Thorac Surg 2001;71(2):591–596.<br />
11. Sundt TM, Bailey MS, Moon MR, et al. Quality of life after<br />
aortic valve replacement at the age of >80 years. Circulation<br />
2000;102(19 Suppl 3):III70–74.<br />
12. Fiore AC, Naunheim KS, Barner HB, et al. Valve replacement<br />
in the octogenarian. Ann Thorac Surg 1989;48(1):<br />
104–108.<br />
13. National health interview survey 1983–1985. Hyattsville,<br />
MD: National Center for Health Statistics; 1986.<br />
14. National Center for Health Statistics: Advance report of<br />
final mortality statistics, 1988. Monthly Vital Stat Rep 1990;<br />
39(7 Suppl):1–48.<br />
15. Ferguson TB Jr, Hammill BG, Peterson ED, DeLong ER,<br />
Grover FL. A decade of change—risk profiles and outcomes<br />
for isolated coronary artery bypass grafting procedures,<br />
1990–1999: a report from the STS National Database<br />
Committee and the Duke Clinical Research Institute.<br />
Society of Thoracic Surgeons. Ann Thorac Surg 2002;73(2):<br />
480–489; discussion 489–490.<br />
16. Khan SS, Kupfer JM, Matloff JM, Tsai TP, Nessim S. Interaction<br />
of age and preoperative risk factors in predicting operative<br />
mortality for coronary bypass surgery. Circulation<br />
1992;86(5 Suppl):II186–190.<br />
17. Bridges CR, Edwards FH, Peterson ED, Coombs LP,<br />
Ferguson TB. Cardiac surgery in nonagenarians and centenarians.<br />
J Am Coll Surg 2003;197(3):347–356; discussion<br />
356–357.<br />
18. Otto CM, Lind BK, Kitzman DW, Gersh BJ, Siscovick DS.<br />
Association of aortic-valve sclerosis with cardiovascular<br />
mortality and morbidity in the elderly. N Engl J Med 1999;<br />
341(3):142–147.<br />
19. Zipes D, Libby P, Bonow R, Braunwald E. Braunwald’s<br />
Heart Disease: A Textbook of Cardiovascular Medicine.<br />
7th ed. Philadelphia: Saunders; 2005.<br />
20. Aronow WS, Ahn C, Kronzon I. Comparison of echocardiographic<br />
abnormalities in African-American, Hispanic, and<br />
white men and women aged >60 years. Am J Cardiol 2001;<br />
87(9):1131–1133, A10.<br />
21. Jamieson WR, Edwards FH, Schwartz M, Bero JW,<br />
Clark RE, Grover FL. Risk stratification for cardiac valve<br />
replacement. National Cardiac Surgery Database. Database<br />
Committee of <strong>The</strong> Society of Thoracic Surgeons. Ann<br />
Thorac Surg 1999;67(4):943–951.<br />
22. Chiappini B, Camurri N, Loforte A, Di Marco L, Di Bartolomeo<br />
R, Marinelli G. Outcome after aortic valve replacement<br />
in octogenarians. Ann Thorac Surg 2004;78(1):85–89.<br />
23. Mehta RH, Eagle KA, Coombs LP, et al. Influence of age<br />
on outcomes in patients undergoing mitral valve replacement.<br />
Ann Thorac Surg 2002;74(5):1459–1467.<br />
24. Ferguson TB Jr, Coombs LP, Peterson ED. Internal thoracic<br />
artery grafting in the elderly patient undergoing coronary<br />
artery bypass grafting: room for process improvement? J<br />
Thorac Cardiovasc Surg 2002;123(5):869–880.<br />
25. Roach GW, Kanchuger M, Mangano CM, et al. Adverse<br />
cerebral outcomes after coronary bypass surgery. Multicenter<br />
Study of Perioperative Ischemia Research Group<br />
and the Ischemia Research and Education Foundation<br />
Investigators. N Engl J Med 1996;335(25):1857–1863.
27. Cardiac Procedures 397<br />
26. Newman MF, Croughwell ND, Blumenthal JA, et al. Effect<br />
of aging on cerebral autoregulation during cardiopulmonary<br />
bypass. Association with postoperative cognitive dysfunction.<br />
Circulation 1994;90(5 Pt 2):II243–249.<br />
27. Gold JP, Torres KE, Maldarelli W, Zhuravlev I, Condit D,<br />
Wasnick J. Improving outcomes in coronary surgery: the<br />
impact of echo-directed aortic cannulation and perioperative<br />
hemodynamic management in 500 patients. Ann Thorac<br />
Surg 2004;78(5):1579–1585.<br />
28. Marshall WG Jr, Barzilai B, Kouchoukos NT, Saffitz J. Intraoperative<br />
ultrasonic imaging of the ascending aorta. Ann<br />
Thorac Surg 1989;48(3):339–344.<br />
29. Murkin JM, Farrar JK, Tweed WA, McKenzie FN, Guiraudon<br />
G. Cerebral autoregulation and flow/metabolism coupling<br />
during cardiopulmonary bypass: the influence of PaCO 2 .<br />
Anesth Analg 1987;66(9):825–832.<br />
30. Bashein G, Townes BD, Nessly ML, et al. A random -<br />
ized study of carbon dioxide management during hypothermic<br />
cardiopulmonary bypass. <strong>Anesthesiology</strong> 1990;<br />
72(1):7–15.<br />
31. Schell RM, Newman M, Reves J. Interventional therapy to<br />
palliate coronary artery disease in the elderly. In: McLeskey<br />
CH, ed. <strong>Geriatric</strong> <strong>Anesthesiology</strong>. Baltimore: Williams &<br />
Wilkins; 1997:609–635.
28<br />
Vascular Procedures<br />
Leanne Groban*and Sylvia Y. Dolinski<br />
<strong>Anesthesia</strong> for vascular surgery is predominantly geriatric<br />
anesthesia. Atherosclerosis, the underlying disease<br />
process in the patient with peripheral vascular disease,<br />
has an insidious onset but typically presents about 10<br />
years after the diagnosis of coronary artery disease. Given<br />
that persons aged 65 years and older comprise the fastestgrowing<br />
segment of the United States population, the<br />
prevalence of vascular interventions, including minimally<br />
invasive angioplasty, endovascular stents, and open reconstructive<br />
procedures, will undoubtedly increase. This<br />
chapter focuses on anesthetic management for the geriatric<br />
patient undergoing aortic and peripheral vascular<br />
surgery. Preoperative preparation is a key feature, because<br />
various comorbidities associated with advanced age, such<br />
as ischemic heart disease, renal insufficiency, and diabetes<br />
are robust predictors of cardiac complications in the vascular<br />
patient. 1 A brief discussion of postoperative care<br />
follows the discussion of surgical procedures.<br />
Preoperative Evaluation<br />
and Preparation<br />
*Partially funded by the Dennis Jahnigen Career Development<br />
Award and Paul Beeson Scholars Award (K08-AG026764-01)<br />
to Dr. Groban.<br />
Fundamental to perioperative management is an understanding<br />
of the specific anesthetic and overall goals for<br />
care of the elderly vascular patient (Table 28-1). A critical<br />
step to achieving these perioperative goals and obtaining<br />
the best possible outcome from the surgical procedure is<br />
a careful preoperative evaluation. Knowledge of the agerelated<br />
structural and functional changes that may have<br />
an impact on anesthesia for the geriatric patient is also<br />
important (Table 28-2). <strong>The</strong> aims of the preoperative<br />
assessment for the older vascular patient are to: (1) estimate<br />
risk; (2) optimize cardiovascular, respiratory, renal,<br />
and endocrinologic status; (3) undertake further investigation<br />
when necessary; (4) plan the anesthetic management;<br />
and (5) arrange appropriate postoperative care.<br />
Given that the elderly patient is at an increased risk for<br />
postoperative complications, because of increased comorbid<br />
illnesses and diminished organ functional reserve, 2 a<br />
detailed evaluation of both cardiac and respiratory<br />
systems reserve is warranted.<br />
Cardiac Risk Assessment<br />
and Intervention<br />
Regardless of age, cardiovascular complications (e.g., myocardial<br />
infarction, pulmonary edema, arrhythmias) are<br />
among the most serious postoperative problems in patients<br />
undergoing noncardiac surgery. 3 Assessment of the perioperative<br />
cardiac risk and its impact on long-term health<br />
should be accomplished during preoperative evaluations<br />
to ascertain potential interventions that may modify the<br />
cardiac risk. However, one must also take particular caution<br />
when applying generalizations about the elderly population<br />
to specific elderly persons, because the aging process<br />
is very heterogeneous. That is, even major vascular procedures<br />
are accompanied by low risk when cardiac functional<br />
status is good, coronary artery disease is absent, and<br />
the multifactorial risk index is low. 4<br />
<strong>The</strong> Revised Cardiac Risk Index (RCRI) is often used<br />
to predict the risk of major cardiac complications among<br />
patients undergoing major, nonemergent, noncardiac<br />
surgery. 1 <strong>The</strong> index was derived from 2893 patients and<br />
validated in 1422 patients, all aged 50 or older. <strong>The</strong> six<br />
independent predictors of cardiac risk identified from the<br />
study that are currently used include high-risk surgery<br />
(Table 28-3), history of ischemic heart disease, history of<br />
congestive heart failure, history of cerebrovascular<br />
disease, insulin therapy, and serum creatinine more than<br />
2.0 mg/dL. <strong>The</strong> presence of zero, one, two, and three or<br />
more predictors has been associated with cardiac complication<br />
rates of nearly 0.5%, 1%, 7%, and 12%, respectively.<br />
1,5 Thus, the higher the score based on the presence<br />
of risk indices, the greater the risk for cardiac morbidity.<br />
398
28. Vascular Procedures 399<br />
Table 28-1. Perioperative goals.<br />
For vascular surgery<br />
• Maintain cardiovascular stability<br />
• Maintain circulating blood volume<br />
• Decrease stress response<br />
• Preserve renal function<br />
For the geriatric surgical patient<br />
• Optimize medical and physical status<br />
• Minimize perioperative starvation and inactivity<br />
• Minimize the stresses of hypothermia, hypoxemia, and pain<br />
• Promote rapid recovery and avoid declines in functional status<br />
• Meticulous perioperative care to avoid complications from:<br />
Fluid and electrolyte perturbations<br />
Impaired cardiorespiratory function<br />
Inappropriate pharmacotherapy<br />
Interestingly, the RCRI does not include advanced age as<br />
an independent predictor of cardiovascular outcome presumably<br />
because ischemic heart disease, insulin-dependent<br />
diabetes, and renal insufficiency are already highly<br />
associated with age.<br />
<strong>The</strong> American College of Cardiology/American Heart<br />
Association guidelines for perioperative cardiovascular<br />
evaluation for noncardiac surgery 6 advocate identification<br />
of functional status in the assessment algorithm. This<br />
can be done by estimating energy demands of daily activities<br />
using the unit of metabolic equivalents (METs). <strong>The</strong><br />
MET is a ratio comparing the energy consumption of an<br />
activity to energy consumption at rest. Usually, healthy<br />
elders can achieve 4.0 METs (e.g., showering while standing,<br />
toweling off, fishing, sweeping floors, playing with<br />
children) without dyspnea or fatigue. 7 Poor functional<br />
status, described as patients’ inability to perform activities<br />
of 5%)<br />
Emergent major operations, particularly in the elderly<br />
Aortic and other major vascular surgery (suprainguinal, abdominal,<br />
or thoracic)<br />
Peripheral vascular surgery<br />
Anticipated prolonged surgical procedures associated with large<br />
fluid shift and/or blood loss<br />
Intermediate (reported cardiac risk generally 75%–85% of<br />
their maximum age-predicted heart rate with a nonischemic<br />
electrocardiogram (ECG) response, are at low risk<br />
for postoperative cardiac events. 8<br />
Except in the case of emergent vascular surgery<br />
(when additional testing is obviated and the patient<br />
Table 28–2. Age-related physiologic changes and anesthetic implications.<br />
Structural and functional changes Physiologic consequences Clinical consequences<br />
Myocyte<br />
Impaired calcium homeostasis<br />
Reduced number (apoptosis) and<br />
increased size<br />
Reduced beta receptor responsiveness<br />
Extracellular matrix<br />
Increased interstitial fibrosis<br />
Amyloid deposition<br />
Conduction system<br />
Apoptosis of pacemaker and Hisbundle<br />
cells<br />
Valvular apparatus<br />
Fibrosis and calcification<br />
Vasculature<br />
Increased diameter of large arteries<br />
Increased medial and intimal thickness<br />
Decreased endothelial nitric oxide<br />
production<br />
LV = left ventricular, LVH = left ventricular hypertrophy.<br />
Impaired LV relaxation<br />
Increased myocardial stiffness<br />
Impaired Ca 2 + homeostasis, reduced LV relaxation,<br />
increased circulating catecholamines<br />
Increased LV stiffness<br />
Conduction block, atrial fibrillation, decreased<br />
contribution of atrial contraction to diastolic<br />
volume<br />
Aortic stenosis leads to LVH, reduced compliance,<br />
impaired relaxation<br />
Increased arterial stiffness, increased vascular<br />
impedance, early reflected waves, increase<br />
pulse wave velocity—decreasing LV<br />
compliance<br />
Greater reliance on ventricular filling and<br />
increases in stroke volume (rather<br />
than ejection fraction) to achieve<br />
increases in cardiac output.<br />
Intolerance to hypovolemia<br />
Intolerance to tachycardia. dysrhythmias,<br />
including atrial fibrillation<br />
Prone to large swings in blood pressure<br />
with clamping and unclamping
400 L. Groban and S.Y. Dolinski<br />
Figure 28-1. Perioperative beta-blockers: patient selection and<br />
preoperative risk stratification. <strong>The</strong> six independent predictors<br />
of complications in the Revised Cardiac Risk Index include:<br />
high-risk surgery, history of ischemic heart disease, congestive<br />
heart failure or cerebral vascular accident, preoperative insulin<br />
therapy, or serum creatinine >2.0 mg/dL. METS = metabolic<br />
equivalents. (Reprinted with permission from Auerbach and<br />
Goldman. 9 Copyright © 2002 American Medical Association.<br />
All rights reserved.)<br />
proceeds directly to the operating room), the decision to<br />
perform noninvasive testing is based on the presence of<br />
clinical risk factors, the patient’s functional status, and the<br />
type of surgery scheduled. Although little evidence exists<br />
showing that noninvasive imaging tests lead to therapeutic<br />
strategies that reduce cardiac risk, they remain a useful<br />
stratification tool for those elderly patients with age-related<br />
musculoskeletal changes that limit their functional status.<br />
For nonemergent vascular surgery, noninvasive testing<br />
(e.g., dobutamine stress echocardiography) may be indicated<br />
for (1) patients with stable angina, (2) patients<br />
scheduled for major aortic surgery who have either poor
28. Vascular Procedures 401<br />
functional status or one clinical predictor, and (3) patients<br />
undergoing intermediate surgery (e.g., carotid endarterectomy),<br />
who have poor functional status and/or two or more<br />
clinical predictors. Given that perioperative beta-blockade<br />
lowers cardiac risk, 9 it should be initiated in all patients<br />
undergoing major aortic surgery who carry, at minimum,<br />
one cardiac risk factor. If beta-blockade is contraindicated,<br />
alpha-adrenergic agonists can be substituted. 10 One clinical<br />
algorithm for preoperative risk stratification and perioperative<br />
beta-blockade is shown in Figure 28-1. 9<br />
Optimization Strategies<br />
Beta-Blocker <strong>The</strong>rapy<br />
Perioperative administration of beta-adrenergic receptor<br />
blockers reduces the incidence of postoperative cardiac<br />
complications and death in high-risk patients undergoing<br />
noncardiac, major vascular procedures, 9,11–15 with beneficial<br />
effects lasting up to 2 years. 11,14,16 Perioperative myocardial<br />
infarctions are not necessarily all caused by<br />
unstable plaque rupture and subsequent thrombosis that<br />
occludes coronary arteries. Many occur in the absence of<br />
plaque rupture and in areas not supplied by known<br />
severely stenosed arteries. 17 Postoperative changes in<br />
sympathetic activity and stress response lead to changes<br />
in heart rate and blood pressure predisposing to myocardial<br />
ischemia perhaps from imbalances in supply and<br />
demand of coronary perfusion. This is where beta-blocker<br />
therapy enters the perioperative therapeutic picture, to<br />
help reduce these changes in heart rate and blood pressure.<br />
<strong>The</strong> strongest evidence to date that beta-blockade<br />
decreases the incidence of postoperative myocardial<br />
infarction and death is from Poldermans et al. 12 <strong>The</strong>se<br />
investigators showed that high-risk patients with positive<br />
dobutamine stress echocardiograms administered bisoprolol<br />
(7 days preoperatively to 30 days postoperatively)<br />
had a tenfold decrease in morbidity and mortality compared<br />
with untreated patients. Despite overwhelming evidence<br />
in support of perioperative beta-blockade, these<br />
agents remain underutilized 18–20 because of classic concerns<br />
from described contraindications of diabetes, chronic<br />
obstructive lung disease, and heart failure. How ever, betablockers<br />
are often well tolerated in these individuals,<br />
especially when carefully titrated. 21,22 <strong>The</strong> reluctance of<br />
some physicians may be attributable to the lack of published<br />
data regarding their beneficial effects in the geriatric<br />
patient. A given trial in the elderly may have insufficient<br />
power to promote evidenced-based therapy, because the<br />
elderly are often excluded from studies, and thus the<br />
results, in fact, may not be generalizable. However, in a<br />
subgroup analysis of those >80 years, the mortality after<br />
myocardial infarction is reduced by 30%. 18–20<br />
In a small prospective study of 63 elderly patients<br />
(>65 years) undergoing noncardiac surgery, Zaugg et al. 23<br />
showed no difference in in-hospital myocardial infarction<br />
rates between patients who received perioperative atenolol<br />
and those who did not receive prophylactic treatment.<br />
However, the perioperative use of beta-blockade in<br />
this study was associated with reduced analgesic requirements,<br />
faster recovery times from anesthesia, and<br />
improved hemodynamic stability, suggesting that perioperative<br />
beta-blockade may be not only safe, but provide<br />
additional beneficial effects in the elderly. Similarly, in the<br />
nonsurgical Metoprolol CR/XL Randomized Intervention<br />
Trial, 24,25 a subgroup of elderly patients ≥65 years<br />
(n = 1920) with chronic systolic heart failure treated with<br />
metoprolol exhibited risk reductions in total mortality<br />
(37%), sudden death (43%), death from worsening heart<br />
failure (36%), and hospitalizations from worsening heart<br />
failure (36%). <strong>The</strong>se results were as favorable as the<br />
benefits observed in younger (75 years of age, 26 beta-blockers<br />
should not be withheld from any surgical, high-risk patient<br />
with evidence of or known risk factors for coronary artery<br />
disease. One must keep in mind that older patients have<br />
decreased beta receptor responsiveness and, thus, may<br />
not exhibit the expected negative chronotropic response.<br />
Also, because of the rapid changes in blood volume that<br />
occur during aortic cross-clamping and unclamping and<br />
the age-related reductions in baroreceptor responsiveness,<br />
27 the authors choose to use an esmolol infusion<br />
during the intraoperative period.<br />
Alpha Agonists<br />
Alpha-2 agonists provide an alternative therapy for prevention<br />
of cardiac morbidity and mortality in patients<br />
with or at risk for coronary artery disease who undergo<br />
vascular surgery. 10,28 In a recent study by Wallace et al., 28<br />
perioperative administration of oral (0.2 mg) or transdermal<br />
clonidine (0.2 mg/day) for 4 days reduced the incidence<br />
of perioperative myocardial ischemia (clonidine<br />
group, 14% versus placebo group, 31%) and also reduced<br />
the incidence of postoperative mortality in patients >60<br />
years of age undergoing noncardiac surgery for up to 2<br />
years. Mivazerol, an alpha-2 agonist administered by continuous<br />
infusion, significantly reduced the incidence of<br />
myocardial infarction in major vascular surgery patients<br />
who had cardiac disease. 29 However, with the potential<br />
for hypotension 30–32 and reductions in coronary perfusion<br />
pressure, the authors prefer using beta-blockers rather<br />
than alpha-2 agonists in the elderly in light of an increased<br />
prevalence of aortic stenosis with advancing age. Clearly,<br />
direct-comparison studies are needed to determine which<br />
class of sympatholytic agents provides the greatest<br />
cardiovascular benefit with the fewest side effects in this<br />
expanding surgical cohort.
402 L. Groban and S.Y. Dolinski<br />
Statins<br />
Statins may also have cardiac protective effects in major<br />
vascular surgery. <strong>The</strong> mechanisms through which statins<br />
confer their beneficial effect include antithrombotic and<br />
antiinflammatory effects, 33 normalization of sympathetic<br />
outflow, 34 improved vasodilation, 35 and attenuation of<br />
cardiac remodeling. 36 In two case-control studies, statins<br />
were associated with lower perioperative 37 and longterm<br />
38 mortality after major noncardiac vascular surgery.<br />
In two retrospective studies, preoperative use of statins<br />
significantly decreased cardiovascular complications<br />
(statin: 9.9% versus nonstatin: 16.5%) 39 and in-hospital<br />
mortality (statin users had a 38% reduction in the odds<br />
of in-hospital mortality). 40 Only the former, an observational<br />
study, 39 was specific to older patients (median age<br />
71; range 63–78). Thus, even though the latter study 40<br />
included 780,591 patients, it is not clear how well the<br />
results apply to older patients. Whether statins should be<br />
given to octogenarians for the prevention of cardiac<br />
disease and perioperative complications remains controversial.<br />
41,42 Interestingly, Alter et al. 43 projected that if a<br />
combined therapy of statins and beta-blockers in acute<br />
coronary syndromes would have a 25% efficacy rate, one<br />
would need to treat 15 elderly patients compared with<br />
175 in the youngest age group to show a benefit (Table<br />
28-4). Findings from the Prospective Study of Pravastatin<br />
in the Elderly at Risk primary prevention trial 44 show that<br />
even though statins reduce death from heart disease, nonfatal<br />
myocardial infarction, and fatal or nonfatal stroke<br />
in the elderly, they may increase risks of myositis, rhabdomyolysis,<br />
and cancer. 42 Thus, until more trials are conducted<br />
in the older high-risk patient, the decision to<br />
prescribe a statin for prophylaxis against perioperative<br />
cardiac complications awaits additional study. Also, the<br />
effect of abrupt discontinuation of statin therapy in the<br />
elderly, high-risk patient remains unclear. 45<br />
Preoperative Assessment<br />
A detailed cardiovascular history and examination with<br />
standard laboratory studies including a hematocrit, platelets,<br />
electrolytes, creatinine, and clotting profile are sufficient.<br />
A relatively recent 12-lead ECG is also indicated.<br />
Cardiovascular symptoms should be carefully determined,<br />
because preoperative ECG abnormalities do not<br />
predict postoperative cardiac complications in the<br />
elderly. 46 Chronic stable angina represents a low risk,<br />
whereas unstable angina has been associated with a high<br />
risk of perioperative ventricular dysfunction, ischemia,<br />
myocardial infarction, and arrhythmias. <strong>The</strong> high-risk<br />
patient should be referred to a cardiologist for additional<br />
testing and coronary therapies, if deemed necessary,<br />
before vascular surgery. Because many elderly patients<br />
have limited exercise capacity (because of arthritis,<br />
osteoporosis, and claudication) and atypical features of<br />
coronary artery disease, the authors recommend dobutamine<br />
stress echocardiography or dipyramidole-thallium<br />
scanning. Patients ultimately having either coronary<br />
stenting or angioplasty should then wait 2–4 weeks before<br />
their vascular procedure. Failure to wait for recovery<br />
after coronary intervention places these patients at high<br />
risk for lethal intraoperative bleeding or myocardial<br />
infarction. 47,48<br />
Patients with congestive heart failure are also at<br />
increased risk for postoperative cardiac complications.<br />
B-type natriuretic peptide (BNP) plasma level is useful<br />
in determining the etiology of pulmonary congestion. 49,50<br />
With BNP levels of ≤100 pg/mL, heart failure is highly<br />
unlikely. However, BNP levels are increased in healthy<br />
elderly 51 and should not be used in isolation from clinical<br />
context. BNP trends in the chronic heart failure patient<br />
may help determine whether medical optimization is<br />
required before surgery. In the elderly hypertensive<br />
patient with concentric left ventricular hypertrophy and<br />
normal systolic function, diastolic dysfunction can lead to<br />
congestive heart failure. <strong>The</strong>se patients are exquisitely<br />
sensitive to factors that alter diastolic filling such as<br />
tachycardia, atrial fibrillation, and hypovolemia. Thus,<br />
identifying these patients preoperatively, with Doppler<br />
echocardiographic indices of diastolic performance, 52<br />
could help to establish the perioperative goals of fluid<br />
and blood pressure management. 53<br />
Because there is a paucity of data on patients >75 years<br />
of age, with normal systolic function and impaired diastolic<br />
function or diastolic heart failure, management of<br />
Table 28-4. <strong>The</strong> relation between baseline risk (1-year mortality) and number needed to treat by various relative efficacies of<br />
treatment.<br />
Age group (years)<br />
1-Year mortality<br />
Number needed to treat assuming<br />
a relative efficacy of 10%<br />
Number needed to treat<br />
assuming a relative efficacy of<br />
25%<br />
Number needed to treat<br />
assuming a relative<br />
efficacy of 50%<br />
28. Vascular Procedures 403<br />
these patients remains largely empiric and should be<br />
weighed on a case-by-case basis. Intraoperative and postoperative<br />
management emphasis should be placed on<br />
control of arterial hypertension (no higher than 130–<br />
140/80–90 mm Hg), maintenance of normal sinus rhythm<br />
and a low, normal heart rate (60–70 bpm), avoidance of<br />
ischemia, and the prevention of volume overload as well<br />
as an insufficient LV preload. In general, control of hypertension<br />
is easily done by anesthesia (to a desirable systolic<br />
blood pressure of 120 mm Hg). <strong>The</strong> authors also use<br />
a combination of low-dose infusions of nitroglycerin and<br />
phenylephrine titrated to maintain systolic blood pressure<br />
within 10% of baseline and to prevent increases in<br />
pulse pressure (e.g., pulse pressure > diastolic blood pressure<br />
≅ increased impedance) and low diastolic blood<br />
pressures (e.g.,
404 L. Groban and S.Y. Dolinski<br />
adjustments of medications. At present, there are no published<br />
guidelines of measures to prevent perioperative<br />
renal failure, although the use of acetylcysteine pre- and<br />
post-IV contrast has appeared in the literature. 73 Indeed,<br />
the use of magnetic resonance angiography as the sole<br />
imaging modality is an acceptable alternative for the preoperative<br />
evaluation of vascular architecture in high-risk<br />
patients, and it does not have harmful renal effects. 73<br />
Nonetheless, the authors strive to maintain circulating<br />
blood volume and cardiac output in an attempt to maintain<br />
renal blood flow and perfusion pressure. <strong>The</strong> two<br />
“renal protective” strategies often used during aortic<br />
surgery include low-dose dopamine (1–3 µg/kg/min) for<br />
its antialdosterone effect and mannitol (12.5–25 mg/70 kg),<br />
given before aortic cross-clamp application, for its potential<br />
free-radical scavenging and osmotic diuretic effects.<br />
Although dopamine has not been shown to have direct<br />
renal protective effects, it can be used to augment cardiac<br />
output, thus improving renal blood flow. 74 Mannitol<br />
increases tubular flow through its osmotic effects and by<br />
reducing renal tubular cellular swelling. Its renal protective<br />
effects were demonstrated in the renal transplant<br />
literature. 75 <strong>The</strong>re are no large randomized controlled<br />
studies of its conclusive benefit in the vascular patient;<br />
however, one small study revealed reduced tubular injury<br />
by measured urinary albumin and N-acetyl glucosaminidase<br />
levels. 76<br />
Some anesthesiologists also advocate the use of loop<br />
diuretics in an attempt to “poison” the energy requiring<br />
Na + /K + -adenosine triphosphatase pump, thereby reducing<br />
renal metabolic O 2 demand. 58,77 However, with the<br />
high prevalence of diastolic dysfunction in geriatric<br />
patients, 78 the authors do not advise the routine use of<br />
loop diuretics for fear of compromising stroke volume<br />
and cardiac output. It has been suggested that low-dose<br />
fenoldopam (0.03 µg/kg/min), a selective dopaminergic-1<br />
receptor agonist, may have renal protective effects. 73,79,80<br />
At this dose, it is unlikely to contribute to the hypotension<br />
one often sees postoperatively in these patients.<br />
Cognitive Function/Delirium<br />
Postoperative delirium is common in elderly patients and<br />
is a predictor of prolonged hospital stay and functional<br />
decline. 81 Risk factors for postoperative delirium include<br />
preexisting dementia, visual impairment, alcohol use,<br />
duration of anesthesia, use of benzodiazepines and narcotics,<br />
and postoperative infection. In an effort to identify<br />
patients at risk, the Mini-Mental State Examination is a<br />
reliable screening tool that is easy to use. (See Chapter 9<br />
for more discussion on delirium.) In those patients considered<br />
to be at risk for postoperative delirium, the<br />
authors recommend a regional technique, if possible with<br />
no sedation. Although there is no evidence that regional<br />
anesthesia decreases the incidence of postoperative delirium,<br />
the authors think this is attributable to the common<br />
use of various sedatives (e.g., midazolam, fentanyl, propofol,<br />
and ketamine) during surgical procedures performed<br />
under regional anesthesia.<br />
Intraoperative Management<br />
General <strong>Anesthesia</strong> for the Vascular Patient<br />
After arrival in the warm operating room, standard noninvasive<br />
monitors are applied. Supplemental oxygen by<br />
nasal cannula is initiated at the time of low-dose premedication<br />
with either midazolam (0.5–1.0 mg) or fentanyl<br />
(25–50 µg). All patients should be attached to an ECG<br />
system capable of monitoring V5 and all limb and augmented<br />
leads. Normally, leads II and V5 are monitored<br />
simultaneously with ST segment trending. <strong>The</strong> only<br />
patients for whom the authors do not routinely place an<br />
arterial line are those presenting for a lower extremity<br />
bypass or amputation procedure. One has access to the<br />
wrists during these surgeries and often they can be<br />
managed without direct arterial pressure monitoring,<br />
unless the procedure is prolonged, the noninvasive blood<br />
pressure monitor cannot detect a regular pulse (e.g.,<br />
chronic atrial fibrillation), or multiple activated clotting<br />
times are requested by the surgeon. Unless peripheral<br />
intravenous access is poor, a 16-gauge peripheral intravenous<br />
is started for induction. Central venous or pulmonary<br />
artery pressure monitoring is performed after<br />
induction in only those patients who are undergoing open<br />
aortic aneurysm/aortobifemoral bypass, because these<br />
surgeries predispose to large volume shifts. Central<br />
venous access allows assessment of right-sided filling<br />
pressure, the administration of vasoactive drugs, if necessary,<br />
and the facilitation of rapid blood transfusion. <strong>The</strong><br />
elderly maintain their cardiac output by increasing stroke<br />
volume and preload. This preload dependency results in<br />
significant hypotension when hypovolemia is encountered.<br />
<strong>The</strong>refore, acute blood loss during surgery is not<br />
well tolerated. 53 <strong>The</strong> noncompliant, older heart is exquisitely<br />
sensitive to volume overload. Thus, the delicate<br />
balance between hypotension and congestive heart failure<br />
warrants the use of central monitoring both intraoperatively<br />
and postoperatively in the geriatric patient undergoing<br />
major aortic surgery under general anesthesia.<br />
Transesophageal echocardiography is frequently used by<br />
one author (L.G.), because it provides real-time information<br />
about filling status, myocardial function, and ischemia.<br />
Monitoring of central and peripheral temperature<br />
is desirable. <strong>The</strong> aim is to maintain normothermia during<br />
surgical procedures using active measures including<br />
forced air, fluid warming devices, and warm ambient temperatures.<br />
<strong>The</strong> geriatric patient has less-efficient mechanisms<br />
of heat conservation, production, and dissipation.
28. Vascular Procedures 405<br />
Maintaining intraoperative normothermia reduces wound<br />
infections, cardiac events, and length of stay. 82,83<br />
Before preoxygenation, esmolol boluses or an esmolol<br />
infusion is titrated to achieve a heart rate 10%–20%<br />
below the patient’s baseline. <strong>The</strong> advantages of esmolol<br />
include its high specificity for the beta 1 receptor, and its<br />
short duration of action. It can be used in severe chronic<br />
obstructive pulmonary disease patients, because it does<br />
not affect forced expiratory volume in 1 second, even at<br />
high infusion rates. 84 Preoxygenation in the geriatric<br />
patient is very important because an increased closing<br />
volume and a delayed onset of neuromuscular blockade<br />
predisposes them to rapid and profound desaturation and<br />
hypoxemia-induced cardiac events. 85 If rushed for time, 8<br />
breaths at 100% oxygen over 1 minute at a 10 L/min flow<br />
rate is recommended. 86<br />
No matter if the approach to anesthesia is opioid-based<br />
supplemented with a volatile agent or a combined general<br />
and regional technique, the goals are the same (Table<br />
28-1). Induction is undertaken with short-acting opioids,<br />
any intravenous induction agent (etomidate 0.2 mg/kg;<br />
propofol 0.5–0.7 mg/kg; thiopental 3 mg/kg), and cisatracurium.<br />
General anesthesia and sedative/hypnotics have<br />
a direct negative effect on sympathetic output, cardiac<br />
contractility, vascular tone, and cardiac filling pressures<br />
predisposing the older patient to a greater risk of hypotension.<br />
After the patient either stops breathing or<br />
becomes obtunded, the inhalational agent is slowly added<br />
to maintain normotension while neuromuscular blockade<br />
takes effect. Long-acting neuromuscular agents such as<br />
pancuronium should be avoided, because even when<br />
reversed these agents are associated with postoperative<br />
pulmonary complications. 87 <strong>The</strong> authors prefer cisatracurium<br />
for its forgiving pharmacodynamic profile. All neuromuscular<br />
blockers, including cisatracurium, have an<br />
increased onset time by about 1 minute in the geriatric<br />
patient. Recovery times for pancuronium, vecuronium,<br />
and rocuronium are also longer, whereas recovery times<br />
with cisatracurium are not altered by advanced age. 88<br />
Heart rate responses to laryngoscopy are prevented by<br />
the use of the esmolol infusion (vide supra beta-blocker<br />
therapy). <strong>Anesthesia</strong> is maintained with any of the<br />
volatile agents, additional fentanyl, and a cisatracurium<br />
infusion at 1–3 µg/kg/min. Because minimal alveolar<br />
concentration (MAC) requirements are reduced in the<br />
elderly, bispectral index (BIS) monitoring may be useful.<br />
Longer-acting opioids (e.g., morphine) may be given<br />
toward the end of surgery to provide postoperative pain<br />
control if an epidural is not in place. However, one must<br />
keep in mind that the volume of distribution of morphine<br />
is smaller in the elderly, plasma and tissue drug levels are<br />
greater for a fixed dose, and the drug disappears more<br />
slowly from cerebral spinal fluid. Taken together, these<br />
effects can account for the more marked respiratory<br />
depression seen in the morphine-treated 80-year-old<br />
versus the morphine-treated 50-year-old. Moreover,<br />
plasma morphine concentration and morphine clearance<br />
also depend on renal function.<br />
Patients are extubated provided they are warm and<br />
have an arterial pH of >7.35. <strong>The</strong> elderly are less able to<br />
mount a respiratory compensation for a metabolic<br />
acidosis, especially in the face of pain or narcotic loads.<br />
<strong>The</strong>y have less muscle strength, and their hypoxic drive<br />
to breathe is also easily blunted with residual 0.1 MAC<br />
inhalational agent on board. Patients with postoperative<br />
epidural analgesia may be more readily extubated.<br />
Patients not extubated at the end of surgery receive infusions<br />
of either low-dose propofol (15 µg/kg/min) or dexmedetomidine<br />
(0.2–0.7 µg/kg/h). Dexmedetomidine has<br />
no respiratory depressant effects and minimal blood<br />
pressure–lowering effects in euvolemic patients. 89,90 Heart<br />
rates are lower with dexmedetomidine than with placebo<br />
during emergence and up to 48 hours after major vascular<br />
surgery, suggesting a cardioprotective benefit as well. 91<br />
Epidural <strong>Anesthesia</strong>/<strong>Regional</strong> Techniques<br />
Neuraxial/regional anesthesia alone, or in combination<br />
with general anesthesia, has several potential benefits<br />
including attenuation of the stress response and the<br />
production of a sympathectomy (Table 28-5). <strong>The</strong>se<br />
effects may reduce the tendency to form clots and<br />
enhance graft patency through improved blood flow. 92,93<br />
Numerous studies, however, have failed to show that<br />
regional anesthesia is superior to general anesthesia for<br />
vascular surgeries for other outcomes such as death. 94<br />
With the emphasis on administration of beta-blockers<br />
and maintenance of normothermia, morbidity and mortality<br />
in patients undergoing general anesthesia may be<br />
reduced, negating any difference one might see between<br />
regional and general anesthesia groups. 95 In addition, an<br />
inadequate or failed regional technique resulting in<br />
untreated tachycardia and hypertension, which leads to<br />
an increased need for supplementation of narcotics and<br />
anxiolytics, may produce hypercarbia or hypotension that<br />
likely will have a more adverse effect on outcome than a<br />
well-executed general.<br />
Elderly patients at risk for postoperative delirium may<br />
benefit from epidural pain control as opposed to systemic<br />
Table 28-5. Potential benefit of epidural anesthesia for vascular<br />
surgery.<br />
Reduce stress response to surgery<br />
Improve myocardial oxygen supply/demand balance<br />
Improve endocardial blood flow<br />
Reduce minimal alveolar concentration<br />
Improve graft patency<br />
Preserve pulmonary function<br />
Reduce postoperative narcotic requirements
406 L. Groban and S.Y. Dolinski<br />
opiates in addition to the possibility of minimal sedation<br />
during the surgery. 95,96 T2 epidural anesthesia reduces<br />
MAC and MAC awake by 50%. 97,98 <strong>The</strong> concentration of<br />
inhalational agent required during combined general/epidural<br />
technique is markedly reduced. In fact, BIS levels<br />
are reduced with the combination technique. 99 Intraoperative<br />
anticoagulation is not a contraindication for a<br />
neuraxial technique as long as the heparin is dosed 1 hour<br />
after the epidural insertion. 100 Lower extremity surgeries<br />
require a T-12 level. Presently, there seems to be little<br />
evidence in the literature that regional anesthesia provides<br />
a benefit in length of hospital stay, mortality, and<br />
cardiac morbidity over general anesthesia. 94 This may<br />
be because in randomized controlled trials both the<br />
study and control groups are closely watched, and it is<br />
close perioperative watching that makes a difference<br />
in outcome.<br />
However, on subgroup analysis of aortic surgery,<br />
Park et al. 96 found that patients who had epidurals had<br />
fewer postoperative complications including less cardiovascular<br />
and respiratory failure. A meta-analysis of randomized<br />
controlled trials addressing the postoperative<br />
effects of epidurals on pulmonary function revealed that<br />
there is a decreased incidence of respiratory infections<br />
and overall pulmonary complications, compared with<br />
systemic opioid administration. 98 Another recent metaanalysis<br />
also showed reductions in the pulmonary complications<br />
of pulmonary embolism, pneumonia, and<br />
respiratory depression. 101<br />
When the authors place epidurals for abdominal aortic<br />
surgeries at T6–8, the patients undergo test dosing with<br />
2% lidocaine. Before incision, morphine (2–3 mg) is<br />
administered epidurally. It is not until after the crossclamp<br />
has been removed and the patient is hemodynamically<br />
stable, that the epidural is redosed with 2% lidocaine,<br />
and a continuous 0.25% bupivacaine infusion through<br />
the epidural catheter is begun at a rate of 3 mL/h. As the<br />
blood pressure increases, the patient is given a 1- to 2-mL<br />
2% lidocaine bolus, and the bupivacaine infusion is<br />
increased by 1 mL/h. This is repeated until the patient is<br />
on an infusion of 4–6 mL/h at the end of the case. In the<br />
postanesthesia care unit, the 0.25% bupivacaine infusion<br />
is stopped once the postoperative infusion of 0.125%<br />
bupivacaine with 0.005% morphine sulfate is available,<br />
thereby continually controlling postoperative pain.<br />
In the postoperative period, if the patient is anticoagulated<br />
with prophylactic low-molecular-weight heparin<br />
(LMWH), the epidural should be removed at least 10–12<br />
hours after the last LMWH dose, and 2 hours before<br />
the next dose, 100 to reduce the risk of epidural or spinal<br />
hematoma associated with anticoagulation. <strong>The</strong> epidural<br />
is continued if the patient receives prophylactic unfractionated<br />
heparin for a few days postoperatively. <strong>The</strong><br />
authors discourage their surgical colleagues from using<br />
fractionated heparin in the elderly despite creatinine<br />
values in the normal range. <strong>The</strong>re is some evidence that<br />
the elderly are at increased risk of bleeding when given<br />
fractionated heparin. 102<br />
Infraaortic Vascular Procedures<br />
<strong>The</strong>se procedures are amenable to either neuraxial techniques<br />
alone or combined with general anesthesia<br />
depending on the length of surgery and/or type of surgery.<br />
An ileofemoral bypass requires abdominal muscle relaxation<br />
better afforded by neuromuscular blockade (and<br />
hence, general anesthesia) than by only a neuraxial technique.<br />
However, patients undergoing such procedures are<br />
frequently already receiving anticoagulants such as intravenous<br />
heparin or have been recently dosed with platelet<br />
inhibitors such as clopidogrel, which preclude any neuraxial<br />
technique. Other regional techniques such as lumbar<br />
plexus/sciatic blocks have been associated with increased<br />
bleeding risks. 103 Below the knee amputations have successfully<br />
been performed by popliteal blocks, and distal<br />
foot amputations are amenable to ankle blocks.<br />
Aortic Surgeries<br />
<strong>The</strong> risk of rupture for aneurysms 6 cm, the annual rupture risk is >25%.<br />
<strong>The</strong> best predictor of rupture risk is an aneurysm that<br />
increases in size more than 1.0 cm/year. Current standard<br />
of care dictates that aneurysms >5.0 cm in size should be<br />
repaired. Advanced age is a risk factor for increased<br />
death and complication rates. Postoperative mortality in<br />
octogenarians for open aortic repair has been reported<br />
to be between 1.4%–9.6% (Table 28-6). Dardik et al. 104<br />
showed that mortality was 2.9% in those in their sixth<br />
decade of life compared with 7.9% in octogenarians<br />
(Table 28-6, Figure 28-2). Increased postoperative<br />
complications have also been reported with advanced<br />
age (Figure 28-3). Octogenarians undergoing endovascular<br />
abdominal aneurysm repair (EVAR), however,<br />
had a mortality rate of 1.9% versus 5.3% for open<br />
surgeries. 105<br />
Before aortic cross-clamp placement, heparin (100 U/<br />
kg) is administered and an activated clotting time is con-<br />
Table 28-6. Perioperative mortality rates after elective open<br />
surgical repair of abdominal aortic aneurysm in octogenarians.<br />
Source Patients (no.) Mortality rate (%)<br />
Treiman (1982) 35 8.6<br />
Paty (1993) 116 3.0<br />
Akkersdijk (1994) 75 8.3<br />
Ohara (1995) 94 9.6<br />
Van Damme (1998) 52 45.7<br />
Kazmers (1998) 206 8.3<br />
Dardik (1999) 246 7.9<br />
Mailapur (2001) 62 1.4
28. Vascular Procedures 407<br />
Figure 28-2. Rate of in-hospital mortality after repair of intact<br />
abdominal aortic aneurysm compared across age groups (p <<br />
0.001). (Reprinted with permission from Vemuri C, Wainess<br />
RM, Dimick JB, et al. Effect of increasing patient age on<br />
complication rates following intact abdominal aortic aneurysm<br />
repair in the United States. J Surg Res 2004;118:26–31.<br />
Copyright © 2004. With permission from Elsevier.)<br />
firmed to be longer than 250 seconds. Depth of anesthesia<br />
is increased and a nitroglycerin drip is also started before<br />
clamp placement. Venodilatation aids in volume loading<br />
of the patient during aortic cross-clamping. <strong>The</strong> physiologic<br />
response to aortic cross-clamping is dependent on<br />
the preoperative myocardial function, site of clamp application,<br />
aortic pathology (e.g., occlusive versus aneurysmal),<br />
and the volume status. A diaphragmatic-level aortic<br />
clamp is associated with increases in central venous, pulmonary<br />
artery end diastolic, and pulmonary artery mean<br />
pressures along with increases in mean arterial pressure.<br />
<strong>The</strong> cardiac output also increases in patients with normal<br />
myocardial function because of a shift in blood volume<br />
proximal to the clamp. In patients with ischemic heart<br />
Figure 28-3. Percentage of patients with one or more complications<br />
after surgery for repair of intact abdominal aortic aneurysm<br />
according to age group (p < 0.001). (Reprinted with<br />
permission from Vemuri C, Wainess RM, Dimick JB, et al. Effect<br />
of increasing patient age on complication rates following intact<br />
abdominal aortic aneurysm repair in the United States. J Surg<br />
Res 2004;118:26–31. Copyright © 2004. With permission from<br />
Elsevier.)
408 L. Groban and S.Y. Dolinski<br />
disease, however, ventricular function can deteriorate<br />
secondary to increased wall tension. If afterload reducing<br />
agents and volume do not restore cardiac output, inotropes<br />
may be required. In the case of an infraceliac<br />
aortic cross-clamp, a shift in blood volume to a dilated<br />
splanchnic bed may in fact result in a decrease in venous<br />
return and preload, prompting the administration of<br />
fluids at the time of cross-clamp. 58 Distal to the clamp,<br />
anaerobic metabolism ensues as blood flow to the gut,<br />
kidney, and legs decrease. Upon removal of the crossclamp<br />
and reperfusion of the lower half of the body, the<br />
patient is subjected to a sudden decrease in afterload and<br />
washout of anaerobic metabolites which can lead to<br />
hypotension if not properly volume loaded. Cell saver<br />
blood and autologous blood units as well as saline are<br />
infused to optimize preload before unclamping. <strong>The</strong><br />
nitroglycerin drip, if used, is now discontinued. <strong>The</strong> concentration<br />
of the inhalational agent is reduced, fractional<br />
inspired oxygen concentration increased, and ventilation<br />
increased to counteract the released acid load. Phenylephrine<br />
is readily available, and the surgeon releases the<br />
cross-clamp slowly while volume is rapidly infused to<br />
counteract the vasodilation and hypotension.<br />
Endovascular Abdominal Aortic<br />
Aneurysm Repair<br />
Since 1991, the number of endovascular graft surgeries<br />
has surged. Three studies looking at EVAR in the elderly<br />
have shown >82%–95% success rate in placement with a<br />
28. Vascular Procedures 409<br />
Table 28-7. Descriptive analyses of in-hospital mortality rates according either to age and significant risk factors or to ASA scoring.<br />
Patients 1.8 mg/dL, and congestive<br />
heart failure. Life expectancy after abdominal aortic<br />
aneurysm repair for individuals aged 70, 75, 80, and 85<br />
years is 10, 8, 6, and 5 years, respectively. 108 <strong>The</strong> 4-year<br />
survival rate was 43% compared with 17% in those octogenarians<br />
deemed too high a risk for surgery in the past,<br />
half of whom died from aneurysm rupture. 107 One study<br />
of ASA 4 patients showed an in-hospital mortality rate<br />
of 4.7% in EVAR patients compared with the open repair<br />
rate of 19.2% (p < 0.02). Patients older than 72 with pulmonary<br />
or renal risk factors had a 21.4% mortality in the<br />
open group compared with the EVAR group of 5.3%. In<br />
the same age group, those without pulmonary or renal<br />
risks had a 4% mortality in the open group compared<br />
with the EVAR of 1.6% 113 (Table 28-7).<br />
Two large-bore IVs and an arterial line are placed. <strong>The</strong><br />
authors do not routinely place central venous catheters<br />
for EVAR. A phenylephrine drip is prepared. Blood is<br />
kept in the room in case of intraoperative aortic rupture.<br />
<strong>The</strong> authors prefer to place a combined spinal-epidural<br />
catheter as the primary anesthetic for the procedure. <strong>The</strong><br />
spinal injection of 12.5 mg plain isobaric 0.5% bupivacaine<br />
typically provides anesthesia/analgesia for the<br />
duration of the procedure. During placement of the neuraxial<br />
catheter, the patient receives minimal amounts of<br />
midazolam. Intraoperatively, the patient is sedated via a<br />
continuous infusion of dexmedetomidine (0.2–0.7 µg/kg/<br />
h) or a propofol/ketamine (190:10 mg) mixture.<br />
Carotid Endarterectomy<br />
Two landmark randomized prospective trials showed that<br />
endarterectomy performed in patients who are symptomatic<br />
and have >70% internal carotid stenosis reduces the<br />
risk of ipsilateral stroke from 26% to 9% over the course<br />
of 2 years. 114,115 During surgery, the patient is at risk for<br />
an intraoperative stroke, and it is thought that placing a<br />
shunt across the clamped artery may improve on the<br />
ischemia. Some surgeons routinely place a shunt in<br />
patients undergoing a general anesthetic, because the<br />
ischemia that leads to a stroke cannot be recognized until<br />
after the operation. Some place a shunt only in patients<br />
at high risk for perioperative stroke, whereas others try<br />
not to place a shunt at all because the majority of patients<br />
do tolerate cross-clamping of the carotid. Shunting has its<br />
inherent risks of dissection or shedding of atheroemboli.<br />
High-risk patients are considered those with a 100% contralateral<br />
carotid occlusion.<br />
This procedure can be performed under regional or<br />
general anesthetic techniques. Sensory blockade in the<br />
C2–C4 dermatome can be achieved with a superficial<br />
cervical or deep cervical plexus block with minimal or no<br />
sedation. Local infiltration of lidocaine by the surgeons<br />
is an alternative option. This allows monitoring for<br />
optimal cerebral blood flow perfusion during the carotid<br />
cross-clamping by conversing with the patient. <strong>The</strong>re is<br />
little need for more invasive or complex cerebral monitoring<br />
and often less need for shunting. However, with<br />
high carotid bifurcations, the regional technique usually<br />
fails to control all the intraoperative mandibular retraction<br />
pain and local anesthetic supplementation by the<br />
surgeon is required.<br />
A recent Cochrane review of nonrandomized trials<br />
suggests that surgery performed under local anesthesia is<br />
associated with a reduction in the odds of death, stroke,<br />
myocardial infarction, and pulmonary complications<br />
within 30 days of the operation. In the seven randomized<br />
controlled trials, there were no differences in the aforementioned<br />
outcomes. <strong>The</strong> ongoing General Anesthetic<br />
versus Local Anesthetic for Carotid Surgery trial is a<br />
randomized controlled trial designed to determine if<br />
regional anesthesia leads to a reduction in postoperative<br />
strokes. 116<br />
<strong>Regional</strong> anesthesia may be associated with occasional<br />
intense pain and anxiety that can lead to myocardial stress.<br />
Not all patients are candidates for regional anesthesia,<br />
particularly those who are claustrophobic, very anxious,<br />
or experience a lot of pain from lying on a hard surface.
410 L. Groban and S.Y. Dolinski<br />
Two intravenous lines are placed. Both phenylephrine<br />
and nitroglycerin drips are attached to a T-port connector<br />
on one of the lines close to the intravenous catheter insertion<br />
site, thereby ensuring little dead space. <strong>The</strong> authors<br />
typically perform a superficial cervical block with 0.25%<br />
ropivacaine because the cardiac safety profile seems to<br />
be better than the other long-acting local anesthetics,<br />
especially if the drug is inadvertently bolused into a large<br />
vessel in the neck. 117 After the block is placed, an arterial<br />
line is inserted in the arm opposite of the surgical site if<br />
both arms are not tucked. Intravenous fluids are kept to<br />
a minimum, blood pressure is kept at or above baseline,<br />
and the patient is monitored by engaging the patient in<br />
conversation. If necessary, the surgeon can supplement<br />
with 1% lidocaine if pain arises from the carotid sheath.<br />
During removal of the plaque, it is useful to warn the<br />
patient that this will feel like a dull toothache. Before<br />
cross-clamping, a 100 mg/kg bolus of heparin is given, and<br />
after the cross-clamping of the carotid, the patient is<br />
monitored for 1–2 minutes by squeezing the patient’s<br />
untucked hand and listening to the patient’s speech. If<br />
any change in the patient’s behavior is noted, the surgeon<br />
is alerted, the cross-clamp removed, the blood pressure<br />
increased by 20% above base line, and the clamp replaced.<br />
If the patient again exhibits signs of decreased cerebral<br />
perfusion, the surgeon places a shunt.<br />
If a general anesthetic is required because of surgeon<br />
or patient preference and cooperation, then induction<br />
proceeds as previously described under General <strong>Anesthesia</strong><br />
for the Vascular Patient. Typically, only 1–2 µg/kg<br />
of fentanyl (or a maximum of 150 µg) is given to maximize<br />
the chances for a rapid emergence. Alternatively,<br />
remifentanil can be used and titrated off as the patient is<br />
allowed to spontaneously breathe; fentanyl is then titrated<br />
to a respiratory rate of 8–12. <strong>The</strong> authors typically hold<br />
pressure over the surgical site dressing until the patient<br />
is extubated. <strong>The</strong> goal is a smooth emergence with minimal<br />
coughing.<br />
Intraoperatively, there are numerous techniques for<br />
the monitoring of cerebral ischemia, and the authors have<br />
typically used cerebral oximetry or spectral edge<br />
frequency. Other techniques include full 16-lead electroencephalography,<br />
jugular venous saturation, stump<br />
pressures, evoked potentials, and transcranial Doppler<br />
monitoring. 118 None is as good as an awake, cooperative,<br />
communicative patient. In fact, when awake patients<br />
were simultaneously monitored by electroencephalography,<br />
there was a 6.7% false-positive and a 4.5% falsenegative<br />
rate in detection of neurologic deficits. 119<br />
Carotid Stents<br />
Of the endovascular techniques used for treating carotid<br />
stenosis, stenting is the preferred technique because it<br />
reduces the restenosis and dissection rates compared<br />
with angioplasty. 120 <strong>The</strong> first randomized controlled trial<br />
comparing carotid stent placement with open surgery in<br />
high-risk patients was conducted in 2002. 121 <strong>The</strong> 30-day<br />
mortality, stroke, or myocardial infarction rate was 5.8%<br />
for the stent group and 12.6% for the carotid endarterectomy<br />
group (p < 0.05). At 1-year follow-up, the differences<br />
were still remarkable for the same endpoints: 11.9%<br />
in the stent group compared with 19.9% in the carotid<br />
endarterectomy group. 122 However, the Cochrane review<br />
of the five trials comparing endovascular with open<br />
carotid endarterectomy showed that there was no significant<br />
difference in the risk of perioperative stroke, myocardial<br />
infarction, or death. It did show a reduction in<br />
cranial neuropathy. 123 This technique allows very highrisk<br />
patients and high, surgically inaccessible cervical<br />
carotid lesions to be treated. However, unlike stents<br />
placed in a coronary vessel or aorta, carotid surgery is<br />
relatively safe, inexpensive, and associated with a short<br />
hospital stay. Atheromatous emboli are devastating, and<br />
neuroprotective devices such as balloon catheter or<br />
microfilter systems are used by surgeons. 120 Local anesthesia<br />
and standard noninvasive monitors are used.<br />
Postoperative Care<br />
Most elderly patients have comorbidities that warrant<br />
their admission to the ICU. <strong>The</strong>se include cardiac,<br />
respiratory, and renal insufficiency. <strong>The</strong> elderly are more<br />
prone to delirium. Bohner et al. 124 documented the<br />
incidence to be 38.9% with longer ICU treatment needed.<br />
Early restoration to preoperative physiologic and cognitive<br />
functioning is most important. Longer-term postoperative<br />
cognitive dysfunction is also not uncommon in<br />
the elderly. A large study revealed that 9.9% of patients<br />
had some postoperative cognitive deficits compared<br />
with their cohort who did not have any anesthesia. 125 Of<br />
those >75 years of age, 14% had a persistent cognitive<br />
deficit. Deeper anesthesia has also been suggested to<br />
affect mortality in the elderly. 126 Patients 60 years and<br />
older who were subjected to deeper BIS values (
28. Vascular Procedures 411<br />
Finally, as pointed out in the beta-blocker therapy<br />
section, it is not enough to write for postoperative betablockers,<br />
but one must titrate to a heart rate effect. Prolonged<br />
increased heart rate (>95 bpm for >12 hours) is<br />
associated with increased myocardial infarctions and<br />
cardiac death. 134<br />
Increased heart rate, especially in the elderly, is associated<br />
with the development of atrial fibrillation. Both<br />
myocardial infarction and atrial fibrillation result in<br />
prolonged ICU stays.<br />
Conclusions<br />
Figure 28-5. Mortality tends to be higher if the bispectral index<br />
(BIS) levels are 28%, whereas it<br />
occurred in 77% of those whose hematocrit was
412 L. Groban and S.Y. Dolinski<br />
predict cardiac morbidity and death after vascular reconstruction.<br />
J Vasc Surg 1991;14:160–169.<br />
9. Auerbach AD, Goldman L. β-Blockers and reduction of<br />
cardiac events in noncardiac surgery: scientific review.<br />
JAMA 2002;287:1435–1444.<br />
10. Wijeysundera DN, Naik JS, Beattie WS. Alpha-2 adrenergic<br />
agonists to prevent perioperative cardiovascular complications:<br />
a meta-analysis. Am J Med 2003;114:742–752.<br />
11. Mangano DT, Layug EL, Wallace A, et al. Effect of atenolol<br />
on mortality and cardiovascular morbidity after<br />
noncardiac surgery. Multicenter Study of Perioperative<br />
Ischemia Research Group. N Engl J Med 1996;335:<br />
1713–1720.<br />
12. Poldermans D, Boersma E, Bax JJ, et al. <strong>The</strong> effect of<br />
bisoprolol on perioperative mortality and myocardial<br />
infarction in high-risk patients undergoing vascular surgery.<br />
Dutch Echocardiographic Cardiac Risk Evaluation Applying<br />
Stress Echocardiography Study Group. N Engl J Med<br />
1999;341:1789–1794.<br />
13. Raby KE, Brull SJ, Timimi F, et al. <strong>The</strong> effect of heart rate<br />
control on myocardial ischemia among high-risk patients<br />
after vascular surgery. Anesth Analg 1999;88:477–482.<br />
14. Wallace A, Layug B, Tateo I, et al. Prophylactic atenolol<br />
reduces postoperative myocardial ischemia. McSPI<br />
Research Group. <strong>Anesthesiology</strong> 1998;88:7–17.<br />
15. Boersma E, Poldermans D, Bax JJ, et al. DECREASE<br />
Study Group (Dutch Echocardiographic Cardiac Risk<br />
Evaluation Applying Stress Echocardiography). Predictors<br />
of cardiac events after major vascular surgery: role of<br />
clinical characteristics, dobutamine echocardiography, and<br />
beta-blocker therapy. JAMA 2001;285:1865–1873.<br />
16. Poldermans D, Boersma E, Bax JJ, et al. Dutch Echocardiographic<br />
Cardiac Risk Evaluation Applying Stress Echocardiography<br />
Study Group. Bisoprolol reduces cardiac<br />
death and myocardial infarction in high-risk patients as<br />
long as 2 years after successful major vascular surgery. Eur<br />
Heart J 2001;22:1353–1358.<br />
17. Landesberg G. <strong>The</strong> pathophysiology of perioperative myocardial<br />
infarction: facts and perspectives. J Cardiothorac<br />
Vasc Anesth 2003;17:90–100.<br />
18. Warltier DC. Beta-adrenergic-blocking drugs: incredibly<br />
useful, incredibly underutilized. <strong>Anesthesiology</strong> 1998;88:<br />
2–5.<br />
19. Mendelson G, Aronow WS. Underutilization of betablockers<br />
in older patients with prior myocardial infarction<br />
or coronary artery disease in an academic, hospital-based<br />
geriatrics practice. J Am Geriatr Soc 1997;45:1360–1361.<br />
20. Soumerai SB, McLaughlin TJ, Spiegelman D, et al. Adverse<br />
outcomes of underuse of beta-blockers in elderly survivors<br />
of acute myocardial infarction. JAMA 1997;277:115–121.<br />
21. Sirak TE, Jelic S, Le Jemtel TH. <strong>The</strong>rapeutic update: nonselective<br />
beta- and alpha-adrenergic blockade in patients<br />
with coexistent chronic obstructive pulmonary disease and<br />
chronic heart failure. J Am Coll Cardiol 2004;44:497–502.<br />
22. Di Bari M, Marchionni N, Pahor M. Beta-blockers after<br />
acute myocardial infarction in elderly patients with diabetes<br />
mellitus: time to reassess. Drugs Aging 2003;20:13–22.<br />
23. Zaugg M, Tagliente T, Lucchinetti E, et al. Beneficial effects<br />
from beta-adrenergic blockade in elderly patients undergoing<br />
noncardiac surgery. <strong>Anesthesiology</strong> 1999;91:1674–1686.<br />
24. [No authors listed.] Effect of metoprolol CR/XL in chronic<br />
heart failure: Metoprolol CR/XL Randomised Intervention<br />
Trial in Congestive Heart Failure (MERIT-HF).<br />
Lancet 1999;353:2001–2007.<br />
25. Hjalmarson A, Goldstein S, Fagerberg B, et al. Effects of<br />
controlled-release metoprolol on total mortality, hospitalizations,<br />
and well-being in patients with heart failure: the<br />
Metoprolol CR/XL Randomized Intervention Trial in<br />
Congestive Heart Failure (MERIT-HF). MERIT-HF Study<br />
Group. JAMA 2000;283:1295–1302.<br />
26. Deedwania PC, Gottlieb S, Ghali JK, et al. MERIT-HF<br />
Study Group. Efficacy, safety and tolerability of betaadrenergic<br />
blockade with metoprolol CR/XL in elderly<br />
patients with heart failure. Eur Heart J 2004;25:<br />
1300–1309.<br />
27. Ebert TJ, Morgan BJ, Barney JA, et al. Effects of aging on<br />
baroreflex regulation of sympathetic activity in humans.<br />
Am J Physiol 1992;263:H798–803.<br />
28. Wallace AW, Galindez D, Salahieh A, et al. Effect of clonidine<br />
on cardiovascular morbidity and mortality after noncardiac<br />
surgery. <strong>Anesthesiology</strong> 2004;101:284–293.<br />
29. Oliver MF, Goldman L, Julian DG, et al. Effect of mivazerol<br />
on perioperative cardiac complications during noncardiac<br />
surgery in patients with coronary heart disease: the<br />
European Mivazerol Trial (EMIT). <strong>Anesthesiology</strong> 1999;<br />
91:951–961.<br />
30. Jalonen J, Hynynen M, Kuitunen A, et al. Dexmedetomidine<br />
as an anesthetic adjunct in coronary artery bypass<br />
grafting. <strong>Anesthesiology</strong> 1997;86:331–345.<br />
31. Boldt J, Rothe G, Schindler E, et al. Can clonidine, enoximone,<br />
and enalaprilat help to protect the myocardium<br />
against ischaemia in cardiac surgery? Heart 1996;76:<br />
207–213.<br />
32. Myles PS, Hunt JO, Holdgaard HO, et al. Clonidine and<br />
cardiac surgery: haemodynamic and metabolic effects,<br />
myocardial ischaemia and recovery. Anaesth Intensive<br />
Care 1999;27:137–147.<br />
33. Undas A, Brozek J, Musial J. Anti-inflammatory and antithrombotic<br />
effects of statins in the management of coronary<br />
artery disease. Clin Lab 2002;48:287–296.<br />
34. Hayashidani S, Tsutsui H, Shiomi T, et al. Fluvastatin, a<br />
3-hydroxy-3-methylglutaryl coenzyme a reductase inhibitor,<br />
attenuates left ventricular remodeling and failure after<br />
experimental myocardial infarction. Circulation 2002;105:<br />
868–873.<br />
35. Laufs U, La Fata V, Plutzky J, et al. Upregulation of endothelial<br />
nitric oxide synthase by HMG CoA reductase<br />
inhibitors. Circulation 1998;97:1129–1135.<br />
36. Hasegawa H, Yamamoto R, Takano H, et al. 3-Hydroxy-3-<br />
methylglutaryl coenzyme A reductase inhibitors prevent<br />
the development of cardiac hypertrophy and heart failure<br />
in rats. J Mol Cell Cardiol 2003;35:953–960.<br />
37. Poldermans D, Bax JJ, Kertai MD, et al. Statins are associated<br />
with a reduced incidence of perioperative mortality<br />
in patients undergoing major noncardiac vascular surgery.<br />
Circulation 2003;107:1848–1851.<br />
38. Kertai MD, Boersma E, Westerhout CM, et al. Association<br />
between long-term statin use and mortality after successful<br />
abdominal aortic aneurysm surgery. Am J Med 2004;116:<br />
96–103.
28. Vascular Procedures 413<br />
39. O’Neil-Callahan K, Katsimaglis G, Tepper MR, et al.<br />
Statins decrease perioperative cardiac complications in<br />
patients undergoing noncardiac vascular surgery: the<br />
Statins for Risk Reduction in Surgery (StaRRS) study.<br />
J Am Coll Cardiol 2005;45:336–342.<br />
40. Lindenauer PK, Pekow P, Wang K, et al. Lipid-lowering<br />
therapy and in-hospital mortality following major noncardiac<br />
surgery. JAMA 2004;291:2092–2099.<br />
41. Stone NJ. Are statins indicated for the primary prevention<br />
of coronary heart disease in octogenarians? Protagonist<br />
viewpoint. Am J Geriatr Cardiol 2003;12:351–356.<br />
42. Foody JM, Krumholz HM. Are statins indicated for the<br />
primary prevention of CAD in octogenarians? Antagonist<br />
viewpoint. Am J Geriatr Cardiol 2003;12:357–360.<br />
43. Alter DA, Manuel DG, Gunraj N, et al. Age, risk-benefit<br />
trade-offs, and the projected effects of evidence-based<br />
therapies. Am J Med 2004;116:540–545.<br />
44. Shepherd J, Blauw GJ, Murphy MB, et al. PROSPER Study<br />
Group. PROspective Study of Pravastatin in the Elderly<br />
at Risk. Pravastatin in elderly individuals at risk of vascular<br />
disease (PROSPER): a randomised controlled trial.<br />
Lancet 2002;360:1623–1630.<br />
45. McGowan MP. Treating to New Target (TNT) Study<br />
Group. <strong>The</strong>re is no evidence for an increase in acute coronary<br />
syndromes after short-term abrupt discontinuation<br />
of statins in stable cardiac patients. Circulation 2004;110:<br />
2333–2335.<br />
46. Liu LL, Dzankic S, Leung JM. Preoperative electrocardiogram<br />
abnormalities do not predict postoperative cardiac<br />
complications in geriatric surgical patients. J Am Geriatr<br />
Soc 2002;50:1186–1191.<br />
47. Kaluza GL, Joseph J, Lee JR, et al. Catastrophic outcomes<br />
of noncardiac surgery soon after coronary stenting. J Am<br />
Coll Cardiol 2000;35:1288–1294.<br />
48. Posner KL, Van Norman GA, Chan V. Adverse cardiac<br />
outcomes after noncardiac surgery in patients with prior<br />
percutaneous transluminal coronary angioplasty. Anesth<br />
Analg 1999;89:553–560.<br />
49. Maisel AS. <strong>The</strong> diagnosis of acute congestive heart<br />
failure: role of BNP measurements. Heart Fail Rev 2003;8:<br />
327–334.<br />
50. Cowie MR, Jourdain P, Maisel A, et al. Clinical applications<br />
of B-type natriuretic peptide (BNP) testing. Eur<br />
Heart J 2003;24:1710–1718.<br />
51. Wallen T, Landahl S, Hedner T, et al. Brain natriuretic<br />
peptide in an elderly population. J Intern Med 1997;242:<br />
307–311.<br />
52. Zile MR, Brutsaert DL. New concepts in diastolic dysfunction<br />
and diastolic heart failure. Part I. Diagnosis, prognosis,<br />
and measurements of diastolic function. Circulation 2002;<br />
105:1387–1393.<br />
53. Groban L. Diastolic dysfunction in the older heart: a<br />
review. J Cardiothorac Vasc Anesth 2005;19:228–236.<br />
54. Somes GW, Pahor M, Shorr RI, et al. <strong>The</strong> role of diastolic<br />
blood pressure when treating isolated systolic hypertension.<br />
Arch Intern Med 1999;159:2004–2009.<br />
55. Mitchell GF, Parise H, Benjamin EJ, et al. Changes in<br />
arterial stiffness and wave reflection with advancing age<br />
in healthy men and women: the Framingham Heart Study.<br />
Hypertension 2004;43:1239–1245.<br />
56. Pauca AL, Kon ND, O’Rourke MF. <strong>The</strong> second peak of the<br />
radial artery pressure wave represents aortic systolic pressure<br />
in hypertensive and elderly patients. Br J Anaesth<br />
2004;92:651–657.<br />
57. London GM. Large artery function and alterations in<br />
hypertension. J Hypertens Suppl 1995;13:S35–38.<br />
58. Gelman S. <strong>The</strong> pathophysiology of aortic cross-clamping<br />
and unclamping. <strong>Anesthesiology</strong> 1995;82:1026–1060.<br />
59. Franklin SS, Jacobs MJ, Wong ND, et al. Predominance<br />
of isolated systolic hypertension among middle-aged and<br />
elderly US hypertensives: analysis based on National<br />
Health and Nutrition Examination Survey (NHANES) III.<br />
Hypertension 2001;37:869–874.<br />
60. Kannel WB. Elevated systolic blood pressure as a cardiovascular<br />
risk factor. Am J Cardiol 2000;85:251–255.<br />
61. Staessen JA, Gasowski J, Wang JG, et al. Risks of untreated<br />
and treated isolated systolic hypertension in the elderly:<br />
meta-analysis of outcome trials. Lancet 2000;355:865–872.<br />
62. Vaccarino V, Berger AK, Abramson J, et al. Pulse pressure<br />
and risk of cardiovascular events in the systolic hypertension<br />
in the elderly program. Am J Cardiol 2001;88:<br />
980–986.<br />
63. Shammash JB, Trost JC, Gold J, et al. Perioperative betablocker<br />
withdrawal and mortality in vascular surgical<br />
patients. Am Heart J 2001;141:148–153.<br />
64. Comfere T, Sprung J, Kumar MM, et al. Angiotensin system<br />
inhibitors in a general surgical population. Anesth Analg<br />
2005;100:636–644.<br />
65. Ryckwaert F, Colson P. Hemodynamic effects of anesthesia<br />
in patients with ischemic heart failure chronically<br />
treated with angiotensin-converting enzyme inhibitors.<br />
Anesth Analg 1997;84:945–949.<br />
66. Coriat P, Richer C, Douraki T, et al. Influence of chronic<br />
angiotensin-converting enzyme inhibition on anesthetic<br />
induction. <strong>Anesthesiology</strong> 1994;81:299–307.<br />
67. Bertrand M, Godet G, Meersschaert K, et al. Should the<br />
angiotensin II antagonists be discontinued before surgery?<br />
Anesth Analg 2001;92:26–30.<br />
68. Prys-Roberts C. Hypertension and anesthesia—fifty years<br />
on. <strong>Anesthesiology</strong> 1979;50:281–284.<br />
69. Goldman L, Caldera DL. Risks of general anesthesia and<br />
elective operation in the hypertensive patient. <strong>Anesthesiology</strong><br />
1979;50:285–292.<br />
70. Howell SJ, Hemming AE, Allman KG, et al. Predictors of<br />
postoperative myocardial ischaemia. <strong>The</strong> role of intercurrent<br />
arterial hypertension and other cardiovascular risk<br />
factors. Anaesthesia 1997;52:107–111.<br />
71. Arozullah AM, Khuri SF, Henderson WG, et al. Development<br />
and validation of a multifactorial risk index for predicting<br />
postoperative pneumonia after major noncardiac<br />
surgery. Ann Intern Med 2001;135:847–857.<br />
72. Hall JC, Tarala RA, Hall JL, et al. A multivariate analysis<br />
of the risk of pulmonary complications after laparotomy.<br />
Chest 1991;99:923–927.<br />
73. Swaminathan M, Stafford-Smith M. Renal dysfunction after<br />
vascular surgery. Curr Opin Anaesthesiol 2003;16:45–51.<br />
74. Sadovnikoff N, Gelman S. Perioperative renal protection.<br />
Curr Opin Anaesthesiol 1999;12:337–341.<br />
75. Tiggeler RG, Berden JH, Hoitsma AJ, et al. Prevention of<br />
acute tubular necrosis in cadaveric kidney transplantation
414 L. Groban and S.Y. Dolinski<br />
by the combined use of mannitol and moderate hydration.<br />
Ann Surg 1985;201:246–251.<br />
76. Nicholson ML, Baker DM, Hopkinson BR, et al. Randomized<br />
controlled trial of the effect of mannitol on renal<br />
reperfusion injury during aortic aneurysm surgery. Br J<br />
Surg 1996;83:1230–1233.<br />
77. Gelman S. Renal protection during surgical stress. Acta<br />
Anaesthesiol Scand Suppl 1997;110:43–45.<br />
78. Phillip B, Pastor D, Bellows W, et al. <strong>The</strong> prevalence of<br />
preoperative diastolic filling abnormalities in geriatric surgical<br />
patients. Anesth Analg 2003;97:1214–1221.<br />
79. Gilbert TB, Hasnain JU, Flinn WR, et al. Fenoldopam infusion<br />
associated with preserving renal function after aortic<br />
cross-clamping for aneurysm repair. J Cardiovasc Pharmacol<br />
<strong>The</strong>r 2001;6:31–36.<br />
80. Halpenny M, Rushe C, Breen P, et al. <strong>The</strong> effects of<br />
fenoldopam on renal function in patients undergoing elective<br />
aortic surgery. Eur J Anaesthesiol 2002;19:32–39.<br />
81. Moller JT, Cluitmans P, Rasmussen LS, et al. Long-term<br />
postoperative cognitive dysfunction in the elderly<br />
ISPOCD1 study. ISPOCD investigators. International<br />
Study of Post-Operative Cognitive Dysfunction. Lancet<br />
1998;351:857–861.<br />
82. Frank SM, Fleisher LA, Breslow MJ, et al. Perioperative<br />
maintenance of normothermia reduces the incidence of<br />
morbid cardiac events. A randomized clinical trial. JAMA<br />
1997;277:1127–1134.<br />
83. Kurz A, Sessler DI, Lenhardt R. Perioperative normothermia<br />
to reduce the incidence of surgical-wound infection<br />
and shorten hospitalization. Study of Wound Infection and<br />
Temperature Group. N Engl J Med 1996;334:1209–1215.<br />
84. Gold MR, Dec GW, Cocca-Spofford D, et al. Esmolol and<br />
ventilatory function in cardiac patients with COPD. Chest<br />
1991;100:1215–1218.<br />
85. Roy RC. What’s New in <strong>Geriatric</strong> <strong>Anesthesia</strong>? 55th Annual<br />
Refresher Course Lectures and Basic Science Reviews.<br />
Park Ridge, IL: American Society of Anesthesiologists;<br />
2004:109.<br />
86. Benumof JL. Preoxygenation: best method for both<br />
efficacy and efficiency. <strong>Anesthesiology</strong> 1999;91:603–605.<br />
87. Berg H, Roed J, Viby-Mogensen J, et al. Residual neuromuscular<br />
block is a risk factor for postoperative pulmonary<br />
complications. A prospective, randomised, and blinded<br />
study of postoperative pulmonary complications after<br />
atracurium, vecuronium and pancuronium. Acta Anaesthesiol<br />
Scand 1997;41:1095–1103.<br />
88. Moore EW, Hunter JM. <strong>The</strong> new neuromuscular blocking<br />
agents: do they offer any advantages? Br J Anaesth 2001;<br />
87:912–925.<br />
89. Arain SR, Ruehlow RM, Uhrich TD, et al. <strong>The</strong> efficacy of<br />
dexmedetomidine versus morphine for postoperative<br />
analgesia after major inpatient surgery. Anesth Analg<br />
2004;98:153–158.<br />
90. Herr DL, Sum-Ping ST, England M. ICU sedation after<br />
coronary artery bypass graft surgery: dexmedetomidinebased<br />
versus propofol-based sedation regimens. J Cardiothorac<br />
Vasc Anesth 2003;17:576–584.<br />
91. Talke P, Chen R, Thomas B, et al. <strong>The</strong> hemodynamic and<br />
adrenergic effects of perioperative dexmedetomidine infusion<br />
after vascular surgery. Anesth Analg 2000;90:834–839.<br />
92. Cook DJ, Rooke GA. Priorities in perioperative geriatrics.<br />
Anesth Analg 2003;96:1823–1836.<br />
93. Rosenfeld BA, Beattie C, Christopherson R, et al. <strong>The</strong><br />
effects of different anesthetic regimens on fibrinolysis and<br />
the development of postoperative arterial thrombosis.<br />
Perioperative Ischemia Randomized <strong>Anesthesia</strong> Trial<br />
Study Group. <strong>Anesthesiology</strong> 1993;79:435–443.<br />
94. Norris EJ, Beattie C, Perler BA, et al. Double-masked randomized<br />
trial comparing alternate combinations of intraoperative<br />
anesthesia and postoperative analgesia in abdominal<br />
aortic surgery. <strong>Anesthesiology</strong> 2001;95:1054–1067.<br />
95. Roy RC. Choosing general versus regional anesthesia<br />
for the elderly. Anesthesiol Clin North Am 2000;18:<br />
91–104.<br />
96. Park WY, Thompson JS, Lee KK. Effect of epidural anesthesia<br />
and analgesia on perioperative outcome: a randomized,<br />
controlled Veterans Affairs cooperative study. Ann<br />
Surg 2001;234:560–569; discussion 569–571.<br />
97. Hodgson PS, Liu SS, Gras TW. Does epidural anesthesia<br />
have general anesthetic effects? A prospective, randomized,<br />
double-blind, placebo-controlled trial. <strong>Anesthesiology</strong><br />
1999;91:1687–1692.<br />
98. Inagaki Y, Mashimo T, Kuzukawa A, et al. Epidural lidocaine<br />
delays arousal from isoflurane anesthesia. Anesth<br />
Analg 1994;79:368–372.<br />
99. Ishiyama T, Kashimoto S, Oguchi T, et al. Epidural ropivacaine<br />
anesthesia decreases the bispectral index during the<br />
awake phase and sevoflurane general anesthesia. Anesth<br />
Analg 2005;100:728–732.<br />
100. Horlocker TT, Wedel DJ, Benzon H, et al. <strong>Regional</strong> anesthesia<br />
in the anticoagulated patient: defining the risks<br />
(the second ASRA Consensus Conference on Neuraxial<br />
<strong>Anesthesia</strong> and Anticoagulation). Reg Anesth Pain Med<br />
2003;28:172–197.<br />
101. Rodgers A, Walker N, Schug S, et al. Reduction of postoperative<br />
mortality and morbidity with epidural or spinal<br />
anaesthesia: results from overview of randomised trials.<br />
BMJ 2000;321:1493.<br />
102. Siguret V, Pautas E, Gouin I. Low molecular weight heparin<br />
treatment in elderly subjects with or without renal insufficiency:<br />
new insights between June 2002 and March 2004.<br />
Curr Opin Pulm Med 2004;10:366–370.<br />
103. Weller RS, Gerancher JC, Crews JC, et al. Extensive retroperitoneal<br />
hematoma without neurologic deficit in two<br />
patients who underwent lumbar plexus block and were<br />
later anticoagulated. <strong>Anesthesiology</strong> 2003;98:581–585.<br />
104. Dardik A, Lin JW, Gordon TA, et al. Results of elective<br />
abdominal aortic aneurysm repair in the 1990s: a population-based<br />
analysis of 2335 cases. J Vasc Surg 1999;30:<br />
985–995.<br />
105. Sicard GA, Rubin BG, Sanchez LA, et al. Endoluminal<br />
graft repair for abdominal aortic aneurysms in high-risk<br />
patients and octogenarians: is it better than open repair?<br />
Ann Surg 2001;234:427–435; discussion 435–437.<br />
106. Lobato AC, Rodriguez-Lopez J, Malik A, et al. Impact of<br />
endovascular repair for abdominal aortic aneurysms in<br />
octogenarians. Ann Vasc Surg 2001;15:525–532.<br />
107. Minor ME, Ellozy S, Carroccio A, et al. Endovascular<br />
aortic aneurysm repair in the octogenarian: is it worthwhile?<br />
Arch Surg 2004;139:308–314.
28. Vascular Procedures 415<br />
108. Al-Omran M, Verma S, Lindsay TF, et al. Clinical decision<br />
making for endovascular repair of abdominal aortic aneurysm.<br />
Circulation 2004;110:e517–523.<br />
109. Brinkman WT, Terramani TT, Najibi S, et al. Endovascular<br />
abdominal aortic aneurysm repair in the octogenarian.<br />
Ann Vasc Surg 2004;18:401–407.<br />
110. Biebl M, Lau LL, Hakaim AG, et al. Midterm outcome of<br />
endovascular abdominal aortic aneurysm repair in octogenarians:<br />
a single institution’s experience. J Vasc Surg<br />
2004;40:435–442.<br />
111. Chaikof EL, Blankensteijn JD, Harris PL, et al. Ad Hoc<br />
Committee for Standardized Reporting Practices in<br />
Vascular Surgery of <strong>The</strong> Society for Vascular Surgery/<br />
American Association for Vascular Surgery. Reporting<br />
standards for endovascular aortic aneurysm repair. J Vasc<br />
Surg 2002;35:1048–1060.<br />
112. Kahn RA, Moskowitz DM, Marin M, et al. Anesthetic<br />
considerations for endovascular aortic repair. Mt Sinai<br />
J Med 2002;69:57–67.<br />
113. Teufelsbauer H, Prusa AM, Wolff K, et al. Endovascular<br />
stent grafting versus open surgical operation in patients<br />
with infrarenal aortic aneurysms: a propensity scoreadjusted<br />
analysis. Circulation 2002;106:782–787.<br />
114. European Carotid Surgery Trialists’ Collaborative Group.<br />
MRC European Carotid Surgery Trial: interim results for<br />
symptomatic patients with severe (70–99%) or with mild<br />
(0–29%) carotid stenosis. Lancet 1991;337:1235–1243.<br />
115. North American Symptomatic Carotid Endarterectomy<br />
Trial Collaborators. Beneficial effect of carotid endarterectomy<br />
in symptomatic patients with high-grade carotid<br />
stenosis. N Engl J Med 1991;325:445–453.<br />
116. Rerkasem K, Bond R, Rothwell PM. Local versus general<br />
anaesthesia for carotid endarterectomy. Cochrane Database<br />
Syst Rev 2004;(2):CD000126.<br />
117. Groban L, Deal DD, Vernon JC, et al. Cardiac resuscitation<br />
after incremental overdosage with lidocaine, bupivacaine,<br />
levobupivacaine, and ropivacaine in anesthetized<br />
dogs. Anesth Analg 2001;92:37–43.<br />
118. Ackerstaff RG, van de Vlasakker CJ. Monitoring of brain<br />
function during carotid endarterectomy: an analysis of<br />
contemporary methods. J Cardiothorac Vasc Anesth 1998;<br />
12:341–347.<br />
119. Stoughton J, Nath RL, Abbott WM. Comparison of simultaneous<br />
electroencephalographic and mental status monitoring<br />
during carotid endarterectomy with regional<br />
anesthesia. J Vasc Surg 1998;28:1014–1021; discussion<br />
1021–1023.<br />
120. Wholey MH, Wholey M. Current status in cervical carotid<br />
artery stent placement. J Cardiovasc Surg (Torino) 2003;44:<br />
331–339.<br />
121. Mozes G, Sullivan TM, Torres-Russotto DR, et al. Carotid<br />
endarterectomy in SAPPHIRE-eligible high-risk patients:<br />
implications for selecting patients for carotid angioplasty<br />
and stenting. J Vasc Surg 2004;39:958–966.<br />
122. Bettmann MA, Dake MD, Hopkins LN, et al. American<br />
Heart Association. Atherosclerotic Vascular Disease Conference:<br />
Writing Group VI: revascularization. Circulation<br />
2004;109:2643–2650.<br />
123. Coward LJ, Featherstone RL, Brown MM. Percutaneous<br />
transluminal angioplasty and stenting for carotid<br />
artery stenosis. Cochrane Database Syst Rev 2004;(2):<br />
CD000515.<br />
124. Bohner H, Friedrichs R, Habel U, et al. Delirium increases<br />
morbidity and length of stay after vascular surgery operations.<br />
Results of a prospective study [German]. Chirurg<br />
2003;74:931–936.<br />
125. Moller JT, Cluitmans P, Rasmussen LS, et al. Longterm<br />
postoperative cognitive dysfunction in the elderly<br />
ISPOCD1 study. ISPOCD Investigators. International<br />
Study of Post-Operative Cognitive Dysfunction. Lancet<br />
1998;351:857–861.<br />
126. Monk TG, Saini V, Weldon BC, et al. Anesthetic management<br />
and one-year mortality after noncardiac surgery.<br />
Anesth Analg 2005;100:4–10.<br />
127. Weldon BC, Mahla ME, van der Aa MT, et al. Advancing<br />
age and deeper intraoperative anesthetic levels are associated<br />
with higher first year death rates. <strong>Anesthesiology</strong><br />
2002;97(Suppl):A1097.<br />
128. Rasmussen LS, Johnson T, Kuipers HM, et al. ISPOCD2<br />
(International Study of Postoperative Cognitive Dysfunction)<br />
Investigators. Does anaesthesia cause postoperative<br />
cognitive dysfunction? A randomised study of regional<br />
versus general anaesthesia in 438 elderly patients. Acta<br />
Anaesthesiol Scand 2003;47:260–266.<br />
129. Hebert PC, Wells G, Blajchman MA, et al. A multicenter,<br />
randomized, controlled clinical trial of transfusion requirements<br />
in critical care. Transfusion Requirements in Critical<br />
Care Investigators, Canadian Critical Care Trials Group. N<br />
Engl J Med 1999;340:409–417.<br />
130. Nelson AH, Fleisher LA, Rosenbaum SH. Relationship<br />
between postoperative anemia and cardiac morbidity in<br />
high-risk vascular patients in the intensive care unit. Crit<br />
Care Med 1993;21:860–866.<br />
131. Wu WC, Rathore SS, Wang Y, et al. Blood transfusion in<br />
elderly patients with acute myocardial infarction. N Engl<br />
J Med 2001;345:1230–1236.<br />
132. Bush RL, Pevec WC, Holcroft JW. A prospective, randomized<br />
trial limiting perioperative red blood cell transfusions<br />
in vascular patients. Am J Surg 1997;174:143–148.<br />
133. van den Berghe G, Wouters P, Weekers F, et al. Intensive<br />
insulin therapy in the critically ill patients. N Engl J Med<br />
2001;345:1359–1367.<br />
134. Sander O, Welters ID, Foex P, et al. Impact of pro -<br />
longed elevated heart rate on incidence of major cardiac<br />
events in critically ill patients with a high risk of cardiac<br />
complications. Crit Care Med 2005;33:81–88; discussion<br />
241–242.
29<br />
Abdominal Procedures<br />
Jeffrey H. Silverstein<br />
Operations on the abdominal viscera are common among<br />
the elderly. Few of the operations are truly elective, with<br />
the majority being either scheduled reasonably shortly<br />
after a diagnostic procedure or truly emergent procedures<br />
necessitated by the presence of an intraabdominal<br />
catastrophe. <strong>The</strong> impact of abdominal surgery on the<br />
elderly is significant and the potential for complications<br />
is high. This chapter synthesizes current thought to<br />
provide an approach to the elderly abdominal surgical<br />
patient including both emergent and elective surgeries. It<br />
should be stated that there are relatively few prospective<br />
trials regarding the perioperative management of abdominal<br />
surgery in the elderly. <strong>The</strong>re is a good amount of<br />
retrospectively acquired information that provides direction<br />
to both current care paradigms as well as ongoing<br />
research. Major vascular surgery may involve an abdominal<br />
approach; however, vascular surgery, particularly in<br />
the elderly, is becoming the province of endovascular<br />
surgery and is not covered in this chapter.<br />
General Principles<br />
Presentation<br />
<strong>The</strong> presentation of abdominal symptoms in the elderly<br />
is frequently diminished, muted, or less specific than in<br />
younger patients. Significant numbers of patients over the<br />
age of 65 do not manifest classic symptoms of cholecystitis.<br />
1 Sixty percent did not have typical upper quadrant<br />
pain and 5% had no pain at all. Less than half were<br />
febrile. Approximately 30% of patients with peptic ulcer<br />
disease do not complain of pain and frequently the first<br />
sign of ulcer disease is perforation. 2 However, pain out of<br />
proportion to all physical findings remains the most<br />
common and prominent symptom of acute mesenteric<br />
ischemia, a frequently fatal disease in older patients. Lyon<br />
and Clark 3 have recently reviewed the general approach<br />
to the diagnosis of abdominal pain in the elderly. Anesthesiologists<br />
do not generally participate in the diagnosis<br />
of abdominal disease; however, they should be aware<br />
that, because symptoms are frequently nonspecific, by the<br />
time the patient arrives in the operating room (OR) they<br />
are potentially sicker than would be the case for younger<br />
patients. It is not uncommon for a patient to be relatively<br />
stable at the beginning of the operation only to become<br />
very unstable as the pathology evolves either in the OR<br />
or not long thereafter.<br />
Outcomes from Abdominal Surgery<br />
As explained in the first chapter, many patients approach<br />
the outcomes from their proposed surgery not in terms<br />
of whether their wound will heal, but on how it will affect<br />
their function and independence. <strong>The</strong> return to preoperative<br />
levels of independent activities of daily living can<br />
take up to 6 months after abdominal surgery. <strong>The</strong> landmark<br />
study by Lawrence et al. 4 indicated that function<br />
returns in a progressive manner with activities of daily<br />
living returning before the independent activities which,<br />
in turn, recover quicker than some measures of physical<br />
strength. It should be noted that the data of Lawrence et<br />
al. were collected before widespread use of laparoscopic<br />
surgical techniques. <strong>The</strong>re have been a number of reports<br />
of a combined multimodal approach to primarily colonic<br />
surgery patients. 5 Included in the program is early ambulation<br />
and discharge home within 2 days of surgery. <strong>The</strong>se<br />
programs have reported some success and seem to indicate<br />
a capacity to recover more rapidly from abdominal<br />
surgery than the cases reported by Lawrence.<br />
<strong>The</strong> risk of surgery in patients older than 90 years was<br />
evaluated by Denney and Denson. 6 <strong>The</strong>ir report on 272<br />
patients undergoing 301 operations at the University of<br />
Southern California Medical Center found that the risk<br />
was more than justified in at least 70% of the nonagenarians.<br />
However, they did find that serious bowel obstruction<br />
was associated with a prohibitive perioperative<br />
mortality rate (63%), even though there is rarely an alter-<br />
416
29. Abdominal Procedures 417<br />
native to surgery. Reviewing their experience many years<br />
ago, Djokovic and Hedley-Whyte 7 reported that mortality<br />
in 500 patients older than 80 years was predicted by<br />
the American Society of Anesthesiologists (ASA) physical<br />
status classification. Fewer than 1% of ASA 2 patients<br />
died whereas 25% of ASA 4 patients died. At the time<br />
(1979), myocardial infarction was the leading cause of<br />
postoperative death. In a cohort of 2291 patients evaluated<br />
between 1982 and 1991, pulmonary complications<br />
were found to be more frequent and associated with<br />
longer hospital stays than cardiac complications. 8 <strong>The</strong><br />
data support the idea that risk is not a function of chronologic<br />
age but rather of coexisting disease and physical<br />
status. <strong>The</strong> ASA physical score does not specifically<br />
include age as a factor, although many clinicians probably<br />
factor their assessment of the impact of age on their<br />
assessment of functional status.<br />
Both the relative risks and potential benefits associated<br />
with anesthesia and major abdominal surgery need to be<br />
individually assessed for each elderly patient. <strong>The</strong> elderly<br />
patient, as described in many of the preceding chapters,<br />
may have relatively intact function of all systems with<br />
limited alterations that limit the ability to respond to<br />
stress, or they may have function that is suboptimal and<br />
limiting even at rest. <strong>The</strong> heterogeneity between patients<br />
and even within a patient is important to keep in mind<br />
as any given patient is assessed. <strong>The</strong> goals of the planned<br />
therapy should be clear to the anesthesia and surgical<br />
teams. Maximization of longevity by means of a definitive<br />
or curative major surgical procedure may be a very<br />
appropriate option for elderly patients, but some patients<br />
may prefer a functional result short of cure. Patients may<br />
have alternative needs based on their perception of risk,<br />
concerns regarding independence and immediate responsibilities<br />
for spouses among myriad issues. Although<br />
the anesthesiologist must carefully assess all systems to<br />
understand the physiologic status of any given patient,<br />
the decision to pursue a surgical procedure has typically<br />
been made by the patient and their surgeon. Emergency<br />
surgery has repeatedly been shown to be an independent<br />
predictor of adverse postoperative outcomes in older surgical<br />
patients undergoing noncardiac surgery. 9,10 It has<br />
long been speculated that poorer preoperative physiology<br />
and preparation have a large influence on these<br />
results. <strong>The</strong> challenge is to prepare the patient expeditiously<br />
and minimize risks where intervention has the<br />
potential to make a difference.<br />
Consent and Health Proxy<br />
<strong>The</strong> care team should have a clear idea of how decisions<br />
will be made should the patient not be able to decide for<br />
themselves for some period of time after surgery. Regulations<br />
regarding health care proxies, next of kin and surrogate<br />
decision making, and the role of physicians in<br />
emergency decision making vary state by state. Particularly<br />
for emergent surgeries on patients with impaired<br />
capacity to consent, how the decision to proceed with<br />
surgery is made should be clear to the anesthesia team.<br />
Some jurisdictions allow physicians to make decisions<br />
regarding the need for emergency treatment, others<br />
do not and, surprisingly, some states do not have clear<br />
regulation for surrogate decision making in the absence<br />
of a formal health proxy. Assessment of the capacity to<br />
consent to a procedure is not clearly standardized. A<br />
reasonable expectation is that an individual consenting<br />
to surgery should be able to reiterate what procedure is<br />
being done and why. Asking a patient to reiterate the<br />
risks of a procedure may indicate understanding, but can<br />
also increase anxiety and is rarely required. Some jurisdictions<br />
require a separate anesthesia consent. It is best<br />
if there is a standard procedure to follow if there is<br />
a disagreement among the perioperative staff as to<br />
the patient’s capacity to consent. <strong>The</strong> appropriate local<br />
approach to “do not resuscitate” orders in place for<br />
patients brought to the OR should be clear to the anesthesia<br />
team. This area remains controversial. 11 If policy<br />
and time permit, the anesthesiologist should have a clear<br />
discussion with the patient and appropriate family<br />
members regarding the appropriate approach to different<br />
circumstances that occur in the immediate perioperative<br />
period. Even if the do not resuscitate order remains in<br />
effect, once intubated for general anesthesia it is not possible<br />
to remove an endotracheal tube in the absence of a<br />
reasonable assessment that the patient will breathe spontaneously.<br />
Patients and families who have indicated that<br />
they do want to “end up intubated on a ventilator” need<br />
to understand how endotracheal intubation will be<br />
managed in a given patient.<br />
Preoperative Care<br />
Preanesthetic Evaluation<br />
For emergency surgery, a comprehensive geriatric<br />
assessment may be difficult. Given the opportunity, the<br />
perioperative team should have a complete understanding<br />
of the physical, psychosocial, and environmental<br />
factors that can affect the health of the patient, with the<br />
goal of optimizing functional outcomes. 12 (See also<br />
Chapter 1.) Although the anesthesiologist might not<br />
be the obvious person to collect this information, there is<br />
no existential reason opposing it. Regardless of how<br />
the preparation of elderly surgical patients is organized,<br />
there must be mechanisms to capture this information,<br />
which will be important to properly design postoperative<br />
care plans.<br />
Frailty is a term used to characterize the weakest and<br />
most vulnerable subset of older adults. Frailty does not
418 J.H. Silverstein<br />
Table 29-1. Changes in cardiovascular parameters in elderly patients at rest and with exercise.<br />
Cardiovascular parameter Aging effect at rest Aging effect with exercise<br />
Heart rate No change or slight decrease Less increase<br />
Systolic blood pressure Increased Greater increase<br />
Diastolic blood pressure No change Slightly greater increase<br />
Cardiac output No change Slightly less increase<br />
Ejection fraction No change Less increase<br />
Stroke volume No change or slight increase Greater increase<br />
fit neatly into a system-based assessment for preanesthetic<br />
evaluation and is almost never the chief complaint<br />
or presenting symptom for a surgical patient. <strong>The</strong> current<br />
clinical model for frailty focuses on muscle loss (sarcopenia)<br />
and diminished strength, 13 although many of those<br />
interested in the field tend to refer to the broader concept<br />
of homeostenosis or decreased ability to respond to a<br />
broad array of stressors. 14 <strong>The</strong> majority of work on this<br />
concept has been applied retrospectively to cohorts of<br />
medical patients and has demonstrated that frailty is<br />
related to increased vulnerability and poor health outcomes.<br />
13 Specific research into the utility of frailty as a<br />
means of assessment and risk stratification or as a target<br />
of perioperative intervention is just beginning. Although<br />
it seems reasonable to be concerned about the frail<br />
elderly, it is not currently possible to make any specific or<br />
general evidence-based recommendations.<br />
Age-related changes in cardiac function have been<br />
described as emanating primarily from alterations in the<br />
stiffness of the aorta, ultimately resulting in systolic<br />
hypertension, concentric left ventricular hypertrophy,<br />
and delayed relaxation of the left ventricle. Nonetheless,<br />
the resting cardiac function of an elderly patient, in the<br />
absence of specific cardiovascular disease, should be fairly<br />
normal (Table 29-1) and the ability to respond to stress<br />
(or exercise) is somewhat, but not seriously, limiting. If<br />
noticeable cardiac functional decline is present, this<br />
should not be attributed to old age, but rather requires a<br />
coherent pathophysiologic explanation.<br />
Diastolic function is currently conceived as an important<br />
aspect of aging and age-related cardiovascular<br />
disease. Phillip et al. 15 reported on 251 patients whose<br />
mean age was 72 ± 7 years to determine the prevalence<br />
of diastolic abnormalities. <strong>The</strong>y found that only 36.5% of<br />
the patients had normal diastolic filling. Mild dysfunction<br />
was most common (48.3%), but 9.6% had mild to moderate<br />
abnormalities, 3.9% had pseudonormal filling properties,<br />
and 1.7% of patients were considered to have severe<br />
abnormalities suggestive of a restrictive pattern. Of<br />
the patients with ejection fractions >50%, 61.5% had<br />
diastolic filling abnormalities.<br />
Pulmonary function gradually declines in the elderly,<br />
even in those who exercise in order to maintain aerobic<br />
capacity. Aging is associated with structural changes such<br />
as decreases in lung static elastic recoil and chest wall<br />
compliance, and functional changes such as impaired<br />
respiratory muscle strength and alterations in responses<br />
to hypoxia. In the absence of pathology, the aging process<br />
does not limit a patient’s respiratory capacity, although<br />
the capacity to markedly increase respiration in response<br />
to a challenge is markedly limited. How these factors<br />
interact with the stress associated with surgery and anesthesia<br />
is of primary importance because postoperative<br />
respiratory complications account for approximately<br />
40% of the perioperative deaths in patients over 65 years<br />
of age. 16 In evaluating a patient, the practitioner should<br />
keep in mind that the breathing pattern of elderly patients<br />
typically involves smaller tidal volumes and an increased<br />
respiratory rate. This can be further exacerbated by<br />
intraabdominal pathology. Between the ages of 40 and 75,<br />
the PaO 2 (mm Hg) decreases, with significant relationship<br />
to changes in both Paco 2 and the body mass index (BMI).<br />
<strong>The</strong> following equation provides a reasonable estimate:<br />
PaO 2 (mm Hg) = 143.6 − (0.39 × age) − (0.56 × BMI) −<br />
(0.57 × Paco 2 ). After 75 years of age, arterial oxygen<br />
tension remains unaffected by BMI and PaO 2 , and<br />
remains relatively stable at around 83 mm Hg. 17 A deterioration<br />
of protective mechanisms of cough and swallowing<br />
in the elderly may lead to ineffective clearance of<br />
secretions and increased susceptibility to aspiration. Loss<br />
of protective upper-airway reflexes has been postulated<br />
to be related to an age-related peripheral deafferentation<br />
together with a decreased central nervous system reflex<br />
activity. 18<br />
Renal Assessment<br />
Multiple alterations in normal renal function and fluid<br />
and electrolyte balance are seen in the aging (Table 29-2).<br />
Assessment of fluid status is problematic in the older<br />
patient. Skin turgor is difficult to interpret because the<br />
loss of elasticity and thinning of the dermis makes skin<br />
appear dehydrated. <strong>The</strong> decrease in thirst sensation<br />
makes a lack of thirst not useful. Even urine output is<br />
suspect because of the possibility of inappropriately<br />
dilute urine being excreted. Estimating the patients glomerular<br />
filtration rate allows the practitioner to develop<br />
an expectation of how quickly administered fluid and<br />
medications may be excreted. Estimating equations<br />
provide some guidance but are often not accurate for
29. Abdominal Procedures 419<br />
Table 29-2. Alteration in fluid balance in the elderly.<br />
Decrease in total body water<br />
Kidney<br />
Decrease in renal cortical<br />
mass<br />
Decline in renal blood flow<br />
Decrease in glomerular<br />
filtration rate<br />
Decrease in urinary<br />
concentrating ability<br />
Increase in antidiuretic<br />
hormone<br />
Increase in atrial natriuretic<br />
peptide<br />
Decrease in aldosterone<br />
Decrease in thirst mechanism<br />
Decrease in free water<br />
clearance<br />
Young body is 65% water, 80-yearold<br />
body 50%<br />
20% loss, primarily cortex by age 85<br />
10% decline/decade<br />
Down 10 mL/decade, 50% by age 80<br />
Less sensitivity to antidiuretic<br />
hormone<br />
Increase relative to osmolality,<br />
decreased in Alzheimer’s<br />
disease<br />
Fivefold over basal levels<br />
a given patient. <strong>The</strong>refore, an actual measurement of<br />
glomerular filtration rate is preferable. 19 When medications<br />
that require careful control of plasma levels are<br />
used, drug levels should be measured. <strong>The</strong> combina -<br />
tion of senescence in fluid management and the current<br />
understanding of cardiovascular aging suggest that the<br />
therapeutic window for intravenous fluid is markedly<br />
narrowed.<br />
Patients presenting for emergent surgery, particularly<br />
those with bowel obstruction, present an important<br />
dilemma regarding preoperative fluid preparation.<br />
Patients who have been vomiting and or undergoing<br />
upper gastrointestinal decompression with a nasogastric<br />
tube may be significantly intravascularly dehydrated.<br />
Ideally, rehydration of these patients should begin immediately<br />
upon their admission to the hospital and continue<br />
through any diagnostic procedures that are undertaken.<br />
If the patient’s rehydration is not accomplished before<br />
surgery, the anesthesiologist is faced with the decision to<br />
delay operation in order to resuscitate the patient and<br />
hopefully ameliorate cardiovascular instability during<br />
induction and maintenance of anesthesia. Most studies of<br />
hemodynamic optimization have involved the use of a<br />
pulmonary artery catheter and have produced extremely<br />
controversial results. A meta-analysis and review in 1996<br />
concluded that achieving supranormal hemodynamic<br />
goals did not reduce mortality in critically ill patients. 20<br />
In subsequent years, the distinction between patients who<br />
had signs of organ failure at the time of resuscitation<br />
compared with those whose organ function was intact<br />
when therapy was instituted suggested that such therapy<br />
applied sufficiently early in the clinical course could be<br />
effective. In a recent review of nearly 2000 patients in 17<br />
randomized controlled trials designed to increase tissue<br />
perfusion in the perioperative period, Boyd 21 concluded<br />
that there was a significant reduction in mortality in the<br />
treatment group [odds ratios 0.45 (95% confidence interval<br />
0.33–0.60)]. A similar review from Kern and Shoemaker<br />
22 essentially agreed, indicating that patients who<br />
achieved an increase in oxygen delivery before the onset<br />
of organ dysfunction had decreased perioperative mortality.<br />
Essentially, all of the published trials of optimization<br />
of oxygen delivery for elderly patients undergoing<br />
either elective or emergent abdominal surgery have been<br />
conducted preoperatively in intensive care units, rather<br />
than in the OR. However, the ability to undertake preoperative<br />
optimization is frequently limited by facilities<br />
and staff. <strong>The</strong>refore, it seems prudent to advise that<br />
patients who are assessed to have a high risk of organ<br />
failure (signs of severe dehydration and particularly those<br />
showing early signs of shock physiology) should undergo<br />
an attempt to improve oxygen delivery, initially using<br />
fluids but potentially including autonomic stimulation as<br />
well, before the induction of anesthesia. If feasible, this<br />
tune-up is probably best done over a number of hours in<br />
an intensive care environment. Preoperative optimization<br />
of elderly patients presenting for most elective surgeries<br />
is generally not necessary. Indeed, as discussed<br />
below, there is a strong argument to be made for the<br />
administration of significantly less intravenous fluid than<br />
is frequently prescribed.<br />
Bowel Preparation<br />
Many patients presenting for bowel surgery have undergone<br />
some type of preparation to clean out their bowel.<br />
<strong>The</strong>se preparations have the potential for altering the<br />
fluid and electrolyte balance of the patient. Although not<br />
the general province of the anesthesiologist, a short overview<br />
of what is used and the associated side effects is<br />
useful. <strong>The</strong> literature for bowel preparation has been<br />
developed primarily by endoscopists and is the subject<br />
of a recent consensus statement and addendum prepared<br />
by a task force from the American Society of Colon<br />
and Rectal Surgeons, the American Society for Gastrointestinal<br />
Endoscopy, and the Society of American<br />
Gastrointestinal and Endoscopic Surgeons. 23 Tolerance<br />
and effectiveness of preparations for bowel surgery vary.<br />
Most preparations use either polyethylene glycol, an<br />
osmotically balanced electrolyte lavage solution or other<br />
osmotic laxatives such as sodium phosphate (NaP) or<br />
magnesium citrate. <strong>The</strong> polyethylene glycol prepara -<br />
tions are effective, but 4 L of fluid can be difficult to tolerate.<br />
NaP preparations may be safe in selected healthy<br />
elderly patients. Elderly patients were found to be at an<br />
increased risk for phosphate intoxication. Administration<br />
of NaP causes a significant increase in serum phosphate,<br />
even in patients with normal creatinine clearance. Hypokalemia<br />
is more prevalent in frail patients. 24 Other adverse<br />
effects on the elderly using oral preparations range from
420 J.H. Silverstein<br />
confusion, dehydration with tongue dryness, and upperbody<br />
muscle weakness to electrolyte disturbances.<br />
<strong>The</strong>re is considerably less agreement on the need<br />
for orthograde bowel preparation for colorectal surgery.<br />
Although this is clearly the standard of care in many<br />
facilities, a recent meta-analysis of 10 randomized<br />
trials comparing cleansing with no bowel preparation<br />
showed a significant increase in anastomotic dehiscences<br />
and a trend toward increased surgical infections<br />
and reoperation even though mortality was unchanged<br />
by orthograde bowel cleansing. 25 <strong>The</strong> anesthesiologist<br />
caring for colorectal surgery patients should inquire<br />
as to whether they underwent some type of bowel<br />
preparation.<br />
Interaction with <strong>Geriatric</strong>ians<br />
Excellent results have been reported for programs specifically<br />
designed to address issues that are uniquely or<br />
primarily geriatric that could be easily integrated into<br />
perioperative care regimens. 26,27 <strong>The</strong> Hospital Elder Life<br />
Program (Table 29-3) is designed to prevent delirium.<br />
Although the results of this and other programs have<br />
been promising in early trials, the ability to implement<br />
such plans varies among institutions 28,29 and much remains<br />
to be learned about the general utility as well as applicability<br />
of these programs to the perioperative period. 30<br />
Much of the care offered by these geriatric-focused programs<br />
are not specifically reimbursable under current<br />
insurance programs, such that funding for these programs<br />
can be difficult to obtain. However, these are the types of<br />
programs you would want in place if your grandmother<br />
needed surgery.<br />
Table 29-3. Contents of the Hospital Elder Life Program.<br />
• Daily Visitor Program: cognitive orientation, communication, and<br />
social support<br />
• <strong>The</strong>rapeutic Activities Program: cognitive stimulation and<br />
socialization<br />
• Early Mobilization Program: daily exercise and walking assistance<br />
• Non-Pharmacologic Sleep Protocol: promotes relaxation and<br />
sufficient sleep<br />
• Hearing and Vision Protocol: hearing and vision adaptations and<br />
equipment<br />
• Oral Volume Repletion and Feeding Assistance Program: assistance<br />
and companionship during meals<br />
• <strong>Geriatric</strong> Interdisciplinary Care: nursing, medicine, rehabilitation<br />
therapies, pharmacy, nutrition and chaplaincy care, and support for<br />
patients and their families<br />
• Provider Education Program: geriatric education for professional<br />
staff<br />
• Links with Community Services: assist with the transition from<br />
hospital to home<br />
Data from Inouye et al., 26 and from McDowell JA, Mion LC, Lydon TJ,<br />
Inouye SK. A nonpharmacologic sleep protocol for hospitalized older<br />
patients. J Am Geriatr Soc 1998;46(6):700–705.<br />
Intraoperative Care<br />
Intravenous Access and Choice of Monitoring<br />
<strong>The</strong>re are no studies that have specifically addressed intravenous<br />
access in the elderly. <strong>The</strong> following suggestions are<br />
based on the author’s personal experience. <strong>The</strong> skin of the<br />
elderly is thin with relatively diminished elasticity. A catheter<br />
size that will easily fit in the vein selected for cannulation<br />
should be chosen. A tight fit will easily disrupt the<br />
vein, causing a potentially large widespread hematoma.<br />
<strong>The</strong> skin surrounding the vein must be stretched and fixed<br />
with the nondominant hand to facilitate entrance of the<br />
intravenous catheter into the vein. This maneuver also<br />
straightens and fixes tortuous veins. <strong>The</strong> vein is usually not<br />
as “deep” as younger patients. Once in the vein, the catheter<br />
itself should be advanced without releasing the<br />
tension on the surrounding skin. This generally requires<br />
advancing the catheter with the index finger of the dominant<br />
hand. Cannulation of a vein, as well as general<br />
comfort for the elderly, can be facilitated by the institution<br />
of a forced-air warming system immediately upon entrance<br />
to the OR. <strong>The</strong> patient does not shiver and the veins dilate<br />
slightly in response to the warmth. At least two intravenous<br />
cannulas should be considered for major surgical<br />
cases. When the arms are not visually accessible to the<br />
anesthesiologists, great concern for vein rupture should<br />
always be considered when an infusion set ceases to flow<br />
easily. <strong>The</strong> arms should be visualized before any pressure<br />
is applied to the infusion system.<br />
Particularly fragile skin on the upper arm or an upper<br />
arm with excess skin relative to muscle mass may predispose<br />
to bruising from the blood pressure cuff. This can be<br />
prevented to a certain extent by a layer or two of cotton<br />
wadding (Webril and others) typically available from the<br />
OR nurses. Oscillometric blood pressure measurement<br />
can be difficult in the presence of substantial arrhythmias.<br />
A decision to place an intraarterial cannula for invasive<br />
blood pressure measurement and frequent blood sampling<br />
is based on the same considerations applied to<br />
younger patients. Age per se is not an indication for intraarterial<br />
blood pressure measurement; however, agerelated<br />
alterations and coexisting disease may easily<br />
persuade the experienced practitioner to institute such<br />
monitoring. Whether such monitoring is instituted before<br />
or after induction of anesthesia is based on experience<br />
and local practice, because no clear evidence exists to<br />
specifically recommend either practice.<br />
<strong>The</strong> evidence regarding measurement of central venous<br />
versus pulmonary artery pressure has not been specifically<br />
addressed regarding elderly patients. To the extent<br />
that central venous pressures or pulmonary artery pressures<br />
reflect intravascular volume, they can be useful.<br />
Multiple recent randomized studies of the pulmonary<br />
artery catheter have failed to demonstrate an advantage
29. Abdominal Procedures 421<br />
over central venous pressure monitoring and have been<br />
associated with increased complication rates. 31,32 Transesophageal<br />
echocardiography has been proposed as a<br />
particularly effective tool for evaluating the geriatric<br />
heart. 15 Echocardiography is the only means currently<br />
available for detecting diastolic dysfunction, which is<br />
present in a significant number of the elderly. Echocardiography<br />
requires expensive equipment and extensive<br />
training, particularly to distinguish findings such as diastolic<br />
dysfunction. In the absence of direct outcome data,<br />
it is not possible to recommend routine echocardiographic<br />
monitoring of elderly abdominal surgery patients. Noninvasive<br />
monitoring of physiologic variables (primarily<br />
cardiac output), which has been successfully used in<br />
elderly trauma patients, should also be helpful in surgical<br />
cardiovascular management. 33<br />
Renna and Venturi 34 found that although age-related<br />
electroencephalogram differences exist in the normal<br />
population, the bispectral index (BIS, Aspect Systems)<br />
still correlates with the depth of sedation independently<br />
of age. Senile dementia may be associated with significantly<br />
lower BIS values.<br />
Urinary catheters provide important information<br />
during longer surgeries but their use may promote urinary<br />
incontinence and urinary tract infections in the elderly.<br />
Studies of elderly patients undergoing orthopedic surgery<br />
tend to favor avoidance of a catheter if the indication is<br />
weak, and removal of the catheter within 24 hours with<br />
the use of intermittent straight catheterization. <strong>The</strong>se<br />
approaches tend to diminish urinary retention, but not<br />
infection rates. 35,36 A more intensive infection prevention<br />
program has recently demonstrated a decrease in the<br />
incidence of urinary tract infection from 10.4 to 3.9<br />
episodes per 100 patients. 37<br />
<strong>The</strong> physiology of thermal stability and the importance<br />
of maintaining normothermia in elderly patients are<br />
described in detail in Chapter 8. Every effort should be<br />
engaged to maintain normal temperatures in abdominal<br />
surgery patients.<br />
Patient positioning can be important. 38 At times, the<br />
patient’s ability to move extremities into certain positions<br />
should be explored with the patient awake in order<br />
to avoid damaging an extremity under anesthesia. Look<br />
for pressure spots, particularly around the sacrum and<br />
heels and provide padding. Patients with severe spine<br />
deformities can represent a challenge to pad appropriately;<br />
however, this should be done with the goal of not<br />
only preventing nerve damage, but also avoiding skin<br />
breakdown and undue stretch on contracted tendons<br />
and ligaments.<br />
Choosing an Epidural Catheter<br />
<strong>The</strong>re is a longstanding debate regarding whether neuraxial<br />
techniques such as epidural analgesia reduces the<br />
frequency of postoperative complications. Pulmonary<br />
and central nervous system complications (delirium<br />
and postoperative cognitive dysfunction) have been the<br />
principal focus. Although there is no doubt that these<br />
techniques provide excellent analgesia and patient satisfaction,<br />
their benefit regarding various outcomes is much<br />
less clear. 39 Epidural anesthesia/analgesia is an integral<br />
part of the multiple modal approach to abdominal surgery<br />
developed by Kehlet and colleagues in Denmark. 40<br />
This approach to anesthesia for abdominal surgery is<br />
described below. Some meta-analyses have concluded<br />
that there is benefit to epidural analgesia; however, many<br />
of the studies used in these analyses are plagued with<br />
several problems.<br />
Jayr et al. 41 studied 153 patients undergoing abdominal<br />
cancer surgery randomized to receive either continuous<br />
epidural bupivacaine and morphine, or subcutaneous<br />
morphine infusion. This carefully designed study found<br />
no difference in pulmonary complications even in patients<br />
with preexisting pulmonary dysfunction. <strong>The</strong> authors did<br />
note that the epidural provided superior postoperative<br />
analgesia. Norris et al. 42 randomized 168 patients undergoing<br />
abdominal aortic aneurysm and found essentially<br />
the same result.<br />
Variations on Anesthetic Plans for the Elderly<br />
Most abdominal surgery is accomplished using general<br />
anesthesia. Lower abdominal procedures can be done<br />
using a primarily regional technique with the addition of<br />
sedation. Adjustments to regional technique for elderly<br />
patients are described in Chapter 19. Despite numerous<br />
attempts to show superiority of regional versus general<br />
anesthesia, substantive reviews of the subject 39,43,44 have<br />
failed to show a substantial difference in outcomes. Because<br />
many, if not most, procedures are currently undertaken<br />
using laparoscopic techniques, the need to create a pneumoperitoneum<br />
and to frequently adjust the position of the<br />
patient makes the use of general endotracheal anesthesia<br />
the preferred technique. Patients presenting for emergency<br />
surgery are typically administered general anesthesia,<br />
although there may be cases that can appropriately be<br />
accomplished with regional techniques.<br />
Laparoscopic surgery has been promoted as being<br />
less stressful, particularly for elderly patients. <strong>The</strong> actual<br />
advantage has yet to be clearly delimited; however, there<br />
is little reason to specifically select an open surgical<br />
technique if a laparoscopic technique is technically<br />
feasible. 45,46<br />
Elderly patients being prepared for general anesthesia<br />
require additional time to successfully achieve proper<br />
denitrogenation (preoxygenation). Patients with severe<br />
abdominal pain or distension can have limited res -<br />
piratory effort. Supplemental oxygen should be considered<br />
early in the treatment plan for such patients and
422 J.H. Silverstein<br />
continued 4–5 days into the postoperative period. 47,48 It<br />
has been suggested that a full 3-minute period for preoxygenation<br />
be used in elderly patients to effectively prevent<br />
hypoxemia during the induction and intubation process. 49<br />
Elderly patients are prone to decreased muscular pharyngeal<br />
support and decreased upper airway reflexes thought<br />
to be secondary to age-related neural deafferentation. 50<br />
<strong>The</strong> general approach to patients with a propensity for<br />
aspiration is to use a rapid sequence induction of general<br />
anesthesia, which incorporates cricothyroid pressure to<br />
occlude the upper esophagus. Occlusion of the esophagus<br />
is purported to prevent passive regurgitation. <strong>The</strong>re have<br />
been no studies that support this beneficial result from<br />
cricoid pressure although there are substantial numbers<br />
of reports indicating that it is ineffective and at times<br />
hampers intubation. 51,52 This procedure is so ingrained in<br />
United States anesthesia practice that it is hard to suggest<br />
that it not be used. Practitioners should at least be willing<br />
to release cricoid pressure should it appear to be impeding<br />
intubation.<br />
<strong>The</strong>re is little to suggest a specific drug choice for<br />
either induction or maintenance of anesthesia based on<br />
aging physiology. Most comparisons of specific agents are<br />
based on recovery times. Regimens are usually found to<br />
be safe and effective without clinically significant advantages.<br />
53–55 It is clear that the doses of most common agents,<br />
with the primary exception of neuromuscular blocking<br />
agents, are decreased in aged patients (Table 29-4). Particular<br />
care should be taken with those patients whose<br />
hemodynamic stability is in question at the beginning of<br />
an anesthetic.<br />
A multimodal approach to perioperative care that<br />
seeks to reduce the stress response and organ dysfunction<br />
leading to earlier recovery has been extensively studied<br />
and promoted by Kehlet. 56 One of the principal endpoints<br />
of this approach, which is also referred to as fasttrack<br />
surgery, is to accelerate the recovery process and<br />
get the patient out of the hospital quickly. This approach<br />
to elective surgery has been used primarily in colon<br />
surgery. <strong>The</strong> approach begins with extensive preoperative<br />
counseling with the patient. <strong>The</strong> patients do not undergo<br />
bowel preparation (except enemas), receive no sedative<br />
premedication, and are not fasted but rather receive carbohydrate-loaded<br />
liquids until 2 hours before surgery.<br />
<strong>The</strong> anesthetic combines a thoracic epidural catheter plus<br />
short-acting inhalational anesthetic agents. Patients are<br />
mobilized and fed early on the first postoperative day<br />
(Table 29-5). Results from fast-track colonic surgery<br />
suggest that postoperative pulmonary, cardiovascular,<br />
and muscle function are improved and body composition<br />
preserved as well as providing the potential to achieve a<br />
normal oral intake of energy and protein. In a recent<br />
controlled study of 160 patients, hospital stay was reduced<br />
from 7.5 days to 3.4 days. 5 In this group, functional re -<br />
covery, as measured by activities of daily living, was not<br />
improved. Despite a higher risk for readmissions, overall<br />
costs and morbidity seem to be reduced. This approach<br />
has been shown clearly to be safe for elderly patients. For<br />
those who recover more rapidly, the program seems to be<br />
beneficial; however, one cannot expect all elderly patients<br />
to recover more rapidly. <strong>The</strong> utility of this approach has<br />
yet to be explored extensively in the United States.<br />
Because the program includes not only specific medical<br />
interventions (e.g., thoracic epidural analgesia) but also<br />
behavioral components that require a different approach<br />
by both the patient as well as doctors and nurses, it is<br />
necessary to reserve judgment as to whether this approach<br />
will effectively save resources in the United States system.<br />
Hopefully, this information will be available in the near<br />
future.<br />
<strong>The</strong>se considerations should not discourage the use of<br />
these valuable techniques in the elderly, but the evidence<br />
does not support their use to minimize pulmonary complications.<br />
<strong>The</strong> use of a full range of adjunctive analgesia<br />
techniques, such as infiltration with local anesthetics,<br />
peripheral nerve blocks, nonsteroidal antiinflammatory<br />
agents, and others as part of a “multimodal” approach is<br />
appropriate.<br />
<strong>The</strong> one study that has evaluated atelectasis formation<br />
in the elderly included 45 patients between the ages of<br />
23 and 69. Although 87% of subjects developed some<br />
atelectasis, the degree of atelectasis was not associated<br />
with age. 57 Nonetheless, in the presence of limited reserve<br />
capacity, the impact of atelectasis can be severe and<br />
is best prevented. <strong>The</strong> application of positive endexpiratory<br />
pressure does not predictably reverse atelectasis<br />
or increase arterial oxygenation unless preceded by<br />
a prolonged vital capacity breath with high inflation pressures,<br />
referred to as a “recruitment maneuver.” 58–60 A<br />
peak opening inspiratory pressure of at least 40 cm H 2 O<br />
is needed to fully reverse anesthesia-induced collapse of<br />
healthy lungs. Blood pressure should be monitored during<br />
a recruitment maneuver because of its potential to induce<br />
hypotension.<br />
Fluid Management in the Elderly<br />
<strong>The</strong>re is a continuing debate about the type and quantity<br />
of fluid that should be administered during elective major<br />
surgery, particularly in the elderly. <strong>The</strong>re is a substantial<br />
collection of publications that describe the adverse effects<br />
of excess fluid. Persistent positive fluid balance in older<br />
surgical patients is associated with prolonged mechanical<br />
ventilation. 61 Itobi et al. 62 found that elderly patients were<br />
more likely to develop edema and that the presence of<br />
edema was associated with a delay in tolerating solid<br />
food, opening bowels, a prolonged hospital stay [median<br />
17 (range 8–59) versus 9 (range 4–27) days], and more<br />
postoperative complications (13 of 20 versus 4 of 18<br />
patients; p = 0.011). Fluid replacement for abdominal
29. Abdominal Procedures 423<br />
Table 29-4. Age-related pharmacologic changes of anesthetics and drugs in anesthesia practice.<br />
Anesthetic/drug Pharmacodynamics Pharmacokinetics Anesthetic management<br />
Inhalational<br />
anesthetics<br />
Sensitivity of the brain↑<br />
(cerebral metabolic<br />
rate)↓<br />
Ventilation/perfusion mismatch<br />
with slow increase of<br />
alveolar/inspired ratio of<br />
inhaled gases; maximal<br />
cardiac output;↓ volume of<br />
distribution↑<br />
Hypnotics<br />
Thiopental No changes Central volume of distribution;↓<br />
intercompartmental<br />
clearance↑<br />
Propofol No changes Central volume of distribution;↓<br />
intercompartmental<br />
clearance↑<br />
Minimal alveolar concentration down 30%; slower<br />
induction and emergence; delayed but more<br />
profound onset of anesthesia<br />
Induction dose reduced by 15% (20-year-old patient:<br />
2.5–5.0 mg/kg IV; 80-year-old patient: 2.1 mg/kg<br />
IV). Maintenance dose: same requirements 60<br />
minutes after starting a continuation infusion.<br />
Emergence: slightly faster<br />
Induction dose reduced by 20% (slower induction<br />
requires lower doses) (20-year-old: 2.0–3.0 mg/kg<br />
IV; 80-year-old: 1.7 mg/kg IV). Maintenance dose:<br />
same requirements 120 minutes after starting a<br />
continuous infusion. Emergence: slightly faster (?)<br />
Midazolam Sensitivity of the brain↑ Clearance↓ Sedation/induction dose reduced by 50% (20-yearold:<br />
0.07–0.15 mg/kg IV; 80-year-old: 0.02–0.03 mg/<br />
kg IV). Maintenance dose reduced by 25%.<br />
Recovery: delayed (hours)<br />
Etomidate No changes Central clearance;↓ volume of<br />
distribution↑<br />
Induction dose reduced by 20% (20-year-old: 0.3 mg/<br />
kg IV; 80-year-old: 0.2 mg/kg IV). Emergence:<br />
slightly faster (?)<br />
Ketamine ? ? Use with caution: hallucinations, seizures, mental<br />
disturbance, release of catecholamines; avoid in<br />
combination with levodopa (tachycardia, arterial<br />
hypertension)<br />
Opioids<br />
Fentanyl, alfentanil,<br />
sufentanil<br />
Sensitivity of the brain↑ No changes Induction dose reduced by 50%. Maintenance doses<br />
reduced by 30%–50%. Emergence: may be delayed<br />
Remifentanil Sensitivity of the brain↑ Central volume of distribution;↓<br />
intercompartmental<br />
clearance↓<br />
Induction dose reduced by 50%. Maintenance dose<br />
reduced by 70%. Emergence: may be delayed<br />
Muscle relaxants<br />
Mivacurium,<br />
succinylcholine<br />
Pancuronium,<br />
doxacuronium,<br />
pipecuronium,<br />
vecuronium,<br />
rocuronium<br />
No changes<br />
No changes<br />
Plasma cholinesterase;↓ muscle<br />
blood flow;↓ cardiac output;↓<br />
intercompartmental<br />
clearance↓<br />
Muscle blood↓ flow; cardiac<br />
output;↓ intercompartmental<br />
clearance;↓ clearance;<br />
(volume of distribution)↓<br />
Atracurium No changes No changes No changes<br />
Reversal agents<br />
Neostigmine,<br />
pyridostigmine<br />
Onset time.↑ Maintenance dose requirements.↓<br />
Duration of action↑ clinically indistinguishable<br />
from mivacurium. Differences: no changes in initial<br />
dose, prolonged block with metoclopramide<br />
Onset time.↑ Maintenance dose requirements.↓<br />
Duration of action.↑ Recommended dose reduced<br />
by 20%<br />
No changes Clearance↓ Duration of action;↑↑ because muscle relaxants have<br />
a markedly prolonged duration of action, larger<br />
doses of reversal agents are needed in elderly<br />
patients<br />
Edrophonium No changes No changes No change<br />
Local anesthetics Sensitivity of the nervous<br />
tissue (?)↑<br />
Hepatic microsomal metabolism<br />
of amide local anesthetics<br />
[lidocaine (lignocaine),<br />
bupivacaine];↓ plasma<br />
protein binding;↓ cephalad<br />
spread↑<br />
Epidural (and spinal) dose requirements.↓ Duration<br />
of spinal and epidural anesthesia seems clinically<br />
independent of age, toxicity↑ (percent free<br />
drug)↑<br />
↑, increase; ↓, decrease.<br />
Source: Modified with permission from Silverstein JH, Zaugg M. <strong>Geriatric</strong>s. In: Hemmings HC, Hopkins PM, eds. Foundations of <strong>Anesthesia</strong>:<br />
Basic and Clinical Science. 2nd ed. London: Elsevier Mosby; 2006.
424 J.H. Silverstein<br />
Table 29-5. Care program in patients undergoing colonic resection<br />
with fast-track care.<br />
Preoperatively<br />
Information of surgical procedure, expected length of stay, and<br />
daily milestones for recovery<br />
Day of surgery<br />
Mobilized 2 hours<br />
Drink 1 L<br />
2 protein-enriched drinks<br />
Solid food<br />
Postoperative day 1<br />
Mobilized >8 hours<br />
Drink >2 L<br />
4 protein-enriched drinks<br />
Solid food<br />
Remove bladder catheter<br />
Plan discharge<br />
Postoperative day 2<br />
Normal activity<br />
Remove epidural catheter<br />
Discharge after lunch<br />
Source: Reprinted with permission from Jakobsen et al. 5<br />
surgery is based on the idea that there is a large amount<br />
of insensible or unmeasurable loss through evaporation<br />
and that a substantial amount of fluid is transudated into<br />
an area often referred to as the third space. In a recent<br />
review, Brandstrup 63 concluded that:<br />
• current standard fluid therapy is not at all<br />
evidence-based;<br />
• the evaporative loss from the abdominal cavity is highly<br />
overestimated;<br />
• the nonanatomic third space loss is based on flawed<br />
methodology and probably does not exist;<br />
• the fluid volume accumulated in traumatized tissue is<br />
very small; and<br />
• volume preloading of neuroaxial blockade is not effective<br />
and may cause postoperative fluid overload.<br />
Many of the trials reviewed by Brandstrup refer<br />
to “restricted” intravenous fluid therapy. In a randomized<br />
controlled study, Brandstrup et al. 64 used two different<br />
fluid regimens in patients undergoing colon surgery.<br />
<strong>The</strong> principal difference was the absence of a preload<br />
and lack of replacement for third space loss (Table 29-6).<br />
<strong>The</strong> administered intravenous fluid volume on the day<br />
of operation was significantly less in the restricted group<br />
[median 2740 mL (range 1100–8050) versus 5388 mL<br />
(range 2700–11083); p < 0.0005]. <strong>The</strong> patients receiving<br />
less fluid had significantly lower complication rates<br />
[28 (33%) versus 44 (51%) in the standard group (p =<br />
0.013)]. In another study, patients receiving on average<br />
5.9 L for colon surgery had a longer duration of ileus,<br />
more complications after surgery, and longer hospital<br />
stays than patients who received about 3.6 L. 65 However,<br />
in the largest study (n = 253), there was no difference<br />
in wound healing or hospital stay between patients randomized<br />
who received approximately 5.7 versus 3.1 L of<br />
crystalloid perioperatively. 66 As compared with major<br />
abdominal surgery, patients undergoing ambulatory<br />
surgery seem to benefit from administration of >1–1.5 L<br />
of fluid, compared with patients who receive 500 mL, additional HAES 6%<br />
Blood-component therapy started at approximate<br />
loss >1500 mL dependent on hematocrit<br />
Blood-component therapy started at approximate<br />
loss >1500 mL dependent on hematocrit<br />
*Hydroxyethyl starch 6% in normal saline.<br />
Reprinted with permission from Brandstrup B, Tonnesen H, Beier-Holgersen R, Hjortso E, Ording H, Lindorff-Larsen K, Rasmussen MS, Lanng<br />
C, Wallin L, Iversen LH, Gramkow CS, Okholm M, Blemmer T, Svendsen PE, Rottensten HH, Thage B, Riis J, Jeppesen IS, Teilum D, Christensen<br />
AM, Graungaard B, Pott F. Effects of intravenous fluid restriction on postoperative complications: comparison of two perioperative fluid regimens:<br />
a randomized assessor-blinded multicenter trial. Ann Surg. 2003 November; 238(5): 641–648.
29. Abdominal Procedures 425<br />
identical manner to younger patients with the dosage<br />
titrated to an effect rather than a specific dose.<br />
Emergence and Extubation of the Elderly<br />
<strong>The</strong> elderly may be particularly prone to the effects of<br />
inadequate reversal of muscle relaxation. 68 In elderly<br />
patients who are overly narcotized, hypoventilation may<br />
lead to respiratory acidosis that potentiates the effects of<br />
residual neuromuscular blockade in the recovery room,<br />
further increasing the rate of postoperative pulmonary<br />
complications. 69 <strong>The</strong>re is little published guidance on<br />
making decisions regarding extubation of elderly patients<br />
after anesthesia. From clinical experience, emergence can<br />
sometimes be prolonged without obvious reason, and<br />
return of active upper airway reflexes can also be delayed.<br />
<strong>The</strong>re are no data to suggest that standard extubation<br />
criteria should not be required in the elderly.<br />
Postoperative Care<br />
<strong>The</strong> postoperative care of the elderly abdominal surgery<br />
patient has been best described by Kehlet and colleagues.<br />
(See discussion of multimodal approach above and Table<br />
29-5.) Apart from those efforts and geriatric programs that<br />
incorporate specific geriatric assessments, postoperative<br />
care for the elderly follows the same plans used for younger<br />
patients. Pain management can be more demanding in the<br />
elderly because the therapeutic ratio of the narcotic analgesics<br />
seems narrowed. Nonetheless, pain control is no less<br />
important for the elderly. (See Chapter 21.)<br />
Postoperative Complications<br />
Elderly patients have higher levels of complications than<br />
younger patients. 70 <strong>The</strong> impact of illness on the elderly is<br />
greater, such that the number of complications associated<br />
with disease is considerably higher in elderly patients with<br />
underlying disease. <strong>The</strong>re are also a number of complications<br />
that are both more common in the elderly and associated<br />
with poor outcomes. <strong>The</strong>se are highlighted here so that<br />
they are clearly in mind as the practitioner develops a perioperative<br />
care plan for a patient. Delirium and postoperative<br />
cognitive dysfunction are mentioned but are explored<br />
in greater detail elsewhere in this book. (See Chapter 9.)<br />
Postoperative ileus is treated somewhat more in depth.<br />
Finally, a predilection for pneumonia represents the most<br />
common complication of elderly surgical patients.<br />
Postoperative Ileus<br />
Ileus is the temporary absence of propulsive bowel function.<br />
Two forms of postoperative ileus can be distinguished:<br />
(1) an uncomplicated form that occurs after<br />
most abdominal surgery, particularly open abdominal<br />
surgery, and spontaneously resolves in 2 or 3 days, and<br />
(2) a paralytic form that lasts more than 3 days and generally<br />
prolongs hospital stay.<br />
<strong>The</strong> list of potential etiologies for postoperative ileus<br />
is large. Contributory mechanisms may include alterations<br />
of autonomic nervous function, gastrointestinal hormones,<br />
inflammatory mediators, and the direct action of<br />
anesthetic agents. Although many factors have been<br />
implicated, no single mechanism or final common pathway<br />
has been identified. 71<br />
Traditional treatment for ileus has been based on nasogastric<br />
decompression and bowel rest. Unfortunately,<br />
these regimens have not been found to hasten the return<br />
of bowel function and seem to increase hospital stays and<br />
prolong recovery. 71 Interesting novel approaches to preventing<br />
or decreasing the duration of ileus include the use<br />
of nonsteroidal antiinflammatory agents, such as ketorolac.<br />
72 <strong>The</strong> most promising therapeutic approach on the<br />
horizon is alvimopan, a selective, competitive mu-opioid<br />
receptor antagonist with limited oral bioavailability that<br />
may be used to reduce length of postoperative ileus. A<br />
recent meta-analysis of five trials including 2195 patients<br />
concluded that alvimopan was effective in restoring gastrointestinal<br />
function and reduced time to discharge after<br />
major abdominal surgery, with acceptable side effects. 73<br />
<strong>The</strong> use of a midthoracic (T6–T8) epidural catheter with<br />
local anesthetic for pain relief is effective; however, lower<br />
thoracic and lumbar catheters are not effective in altering<br />
the duration of ileus. 71,74 In recent years, patients are being<br />
fed earlier, and the traditional marker of waiting for first<br />
flatus is no longer considered a reasonable endpoint. 71<br />
Early small feedings are most appropriate.<br />
Pneumonia<br />
Concomitant pneumonia and influenza constitute the<br />
leading infectious cause of death in the elderly and the<br />
fourth most common cause of death overall. <strong>The</strong> presence<br />
of concomitant illness and delays in diagnosis contribute<br />
to significant mortality from this disease in the elderly.<br />
Senescence of the immune system seems less important<br />
in predisposition to pneumonia than the presence of concomitant<br />
illness. Mortality is generally higher in older<br />
than in younger patients, although outcome in pneumonia<br />
depends primarily on the presence of underlying<br />
illness and the causative organism. 75 Delay in diagnosis is<br />
frequently secondary to the atypical presentations of<br />
pneumonia in the elderly. <strong>The</strong> typical symptoms of sputum<br />
production, fever, chills, and rigors may be absent in the<br />
elderly; confusion may be the only presenting symptom.<br />
Tachypnea is frequent; however, this vital sign is poorly<br />
recorded in many facilities and is not sufficiently sensitive<br />
in making a diagnosis. Leukocytosis is common, but by<br />
no means specific. Chest roentgenograms frequently
426 J.H. Silverstein<br />
show incomplete consolidation, and the findings are difficult<br />
to distinguish from other diseases of the elderly,<br />
such as congestive heart failure, atelectasis, pulmonary<br />
embolism, and malignancy. <strong>The</strong>refore, clinical diagnosis<br />
requires a high index of suspicion despite atypical clinical<br />
manifestations. In a recent review for the American<br />
College of Physicians, Lawrence et al. 76 concluded that<br />
few interventions have been shown to clearly or even<br />
possibly reduce postoperative pneumonia, noting that the<br />
quality of the evidence regarding the prevention of pneumonia<br />
in general was only fair. Thus, prevention of pneumonia<br />
in elderly patients remains a key, yet elusive goal<br />
in improving perioperative care.<br />
Conclusion<br />
<strong>The</strong> elderly patient presenting for abdominal surgery represents<br />
a challenge to the anesthesia practitioner. Patients<br />
may be sicker than one would presume from their clinical<br />
presentation. Given the likelihood of diminished reserve<br />
capacity in one or more organ systems, aggressive management<br />
to prevent organ dysfunction is in order. Fluid<br />
resuscitation remains a controversial issue, and determining<br />
appropriate endpoints for fluid administration is clinically<br />
challenging. In the absence of major preexisting<br />
disease, elderly patients should tolerate surgery and anesthesia<br />
and recover well if complications can be avoided.<br />
Certain postoperative complications, particularly central<br />
nervous system, gastrointestinal, and pulmonary complications,<br />
are most common in the elderly, are particularly<br />
troublesome, and their likelihood is possibly reducible by<br />
techniques that can be used in the perioperative period.<br />
Clinicians can hope to see additional data published in<br />
the next few years that should help to further fine-tune<br />
the perioperative approach to the elderly abdominal<br />
surgical patient.<br />
References<br />
1. Parker LJ, Vukov LF, Wollan PC. Emergency department<br />
evaluation of geriatric patients with acute cholecystitis.<br />
Acad Emerg Med 1997;4:51–55.<br />
2. Hilton D, Iman N, Burke GJ, et al. Absence of abdominal<br />
pain in older persons with endoscopic ulcers: a prospective<br />
study. Am J Gastroenterol 2001;96:380–384.<br />
3. Lyon C, Clark DC. Diagnosis of acute abdominal pain in<br />
older patients. Am Fam Physician 2006;74:1537–1544.<br />
4. Lawrence VA, Hazuda HP, Cornell JE, et al. Functional<br />
independence after major abdominal surgery in the elderly.<br />
J Am Coll Surg 2004;199:762–772.<br />
5. Jakobsen DH, Sonne E, Andreasen J, Kehlet H. Convalescence<br />
after colonic surgery with fast-track vs conventional<br />
care. Colorectal Dis 2006;8:683–687.<br />
6. Denney JL, Denson JS. Risk of surgery in patients over 90.<br />
<strong>Geriatric</strong>s 1972;27:115–118.<br />
7. Djokovic JL, Hedley-Whyte J. Prediction of outcome of<br />
surgery and anesthesia in patients over 80. JAMA 1979;242:<br />
2301–2306.<br />
8. Lawrence VA, Hilsenbeck SG, Mulrow CD, Dhanda R,<br />
Sapp J, Page CP. Incidence and hospital stay for cardiac and<br />
pulmonary complications after abdominal surgery. J Gen<br />
Intern Med 1995;10:671–678.<br />
9. Hosking MP, Warner MA, Lobdell CM, Offord KP, Melton<br />
LJ III. Outcomes of surgery in patients 90 years of age and<br />
older. JAMA 1989;261:1909–1915.<br />
10. Leung JM, Dzankic S. Relative importance of preoperative<br />
health status versus intraoperative factors in predicting<br />
postoperative adverse outcomes in geriatric surgical<br />
patients. J Am Geriatr Soc 2001;49:1080–1085.<br />
11. Ewanchuk M, Brindley PG. Perioperative do-not-resuscitate<br />
orders—doing ‘nothing’ when ‘something’ can be done. Crit<br />
Care 2006;10:219.<br />
12. Palmer RM. <strong>Geriatric</strong> assessment. Med Clin North Am<br />
1999;83:1503–1523, vii–viii.<br />
13. Fried LP, Tangen CM, Walston J, et al. Frailty in older adults:<br />
evidence for a phenotype. J Gerontol A Biol Sci Med Sci<br />
2001;56:M146–M156.<br />
14. Fried LP, Hadley EC, Walston JD, et al. From bedside to<br />
bench: research agenda for frailty. Sci Aging Knowledge<br />
Environ 2005;2005:e24.<br />
15. Phillip B, Pastor D, Bellows W, Leung JM. <strong>The</strong> prevalence<br />
of preoperative diastolic filling abnormalities in geriatric<br />
surgical patients. Anesth Analg 2003;97:1214–1221.<br />
16. Zaugg M, Lucchinetti E. Respiratory function in the elderly.<br />
Anesthesiol Clin North Am 2000;18:47–58, vi.<br />
17. Cerveri I, Zoia MC, Fanfulla F, Spagnolatti L, Berrayah L,<br />
Grassi M, Tinelli C. Reference values of arterial oxygen<br />
tension in the middle-aged and elderly. Am J Respir Crit<br />
Care Med 1995;152:934–941.<br />
18. Marik PE, Kaplan D. Aspiration pneumonia and dysphagia<br />
in the elderly. Chest 2003;124:328–336.<br />
19. Malmrose LC, Gray SL, Pieper CF, et al. Measured versus<br />
estimated creatinine clearance in a high-functioning elderly<br />
sample: MacArthur Foundation Study of Successful Aging.<br />
J Am Geriatr Soc 1993;41:715–721.<br />
20. Heyland DK, Cook DJ, King D, Kernerman P, Brun-Buisson<br />
C. Maximizing oxygen delivery in critically ill patients: a<br />
methodologic appraisal of the evidence. Crit Care Med<br />
1996;24:517–524.<br />
21. Boyd O. Optimisation of oxygenation and tissue perfusion<br />
in surgical patients. Intensive Crit Care Nurs 2003;19:<br />
171–181.<br />
22. Kern JW, Shoemaker WC. Meta-analysis of hemodynamic<br />
optimization in high-risk patients. Crit Care Med 2002;30:<br />
1686–1692.<br />
23. Wexner SD, Beck DE, Baron TH, et al. A consensus document<br />
on bowel preparation before colonoscopy: prepared<br />
by a Task Force from the American Society of Colon and<br />
Rectal Surgeons (ASCRS), the American Society for Gastrointestinal<br />
Endoscopy (ASGE), and the Society of American<br />
Gastrointestinal and Endoscopic Surgeons (SAGES).<br />
Surg Endosc 2006;20:1161.<br />
24. Seinela L, Pehkonen E, Laasanen T, Ahvenainen J. Bowel<br />
preparation for colonoscopy in very old patients: a randomized<br />
prospective trial comparing oral sodium phosphate and
29. Abdominal Procedures 427<br />
polyethylene glycol electrolyte lavage solution. Scand J<br />
Gastroenterol 2003;38:216–220.<br />
25. Muller-Stich BP, Choudhry A, Vetter G, et al. Preoperative<br />
bowel preparation: surgical standard or past? Dig Surg<br />
2006;23:375–380.<br />
26. Inouye SK, Bogardus ST Jr, Baker DI, Leo-Summers L,<br />
Cooney LM Jr. <strong>The</strong> Hospital Elder Life Program: a model<br />
of care to prevent cognitive and functional decline in older<br />
hospitalized patients. Hospital Elder Life Program. J Am<br />
Geriatr Soc 2000;48:1697–1706.<br />
27. Marcantonio ER, Flacker JM, Wright RJ, Resnick NM.<br />
Reducing delirium after hip fracture: a randomized trial.<br />
J Am Geriatr Soc 2001;49:516–522.<br />
28. Bradley EH, Webster TR, Schlesinger M, Baker D, Inouye<br />
SK. Patterns of diffusion of evidence-based clinical programmes:<br />
a case study of the Hospital Elder Life Program.<br />
Qual Saf Health Care 2006;15:334–338.<br />
29. Inouye SK, Baker DI, Fugal P, Bradley EH. Dissemination<br />
of the Hospital Elder Life Program: implementation,<br />
adaptation, and successes. J Am Geriatr Soc 2006;54:<br />
1492–1499.<br />
30. Landefeld CS. Improving health care for older persons. Ann<br />
Intern Med 2003;139:421–424.<br />
31. Sandham JD, Hull RD, Brant RF, et al. A randomized, controlled<br />
trial of the use of pulmonary-artery catheters in<br />
high-risk surgical patients. N Engl J Med 2003;348:5–14.<br />
32. Wheeler AP, Bernard GR, Thompson BT, et al. Pulmonaryartery<br />
versus central venous catheter to guide treatment of<br />
acute lung injury. N Engl J Med 2006;354:2213–2224.<br />
33. Brown CV, Shoemaker WC, Wo CC, Chan L, Demetriades<br />
D. Is noninvasive hemodynamic monitoring appropriate<br />
for the elderly critically injured patient? J Trauma 2005;58:<br />
102–107.<br />
34. Renna M, Venturi R. Bispectral index and anaesthesia in<br />
the elderly. Minerva Anestesiol 2000;66:398–402.<br />
35. Michelson JD, Lotke PA, Steinberg ME. Urinary-bladder<br />
management after total joint-replacement surgery. N Engl<br />
J Med 1988;319:321–326.<br />
36. Skelly JM, Guyatt GH, Kalbfleisch R, Singer J, Winter L.<br />
Management of urinary retention after surgical repair of<br />
hip fracture. CMAJ 1992;146:1185–1189.<br />
37. Stephan F, Sax H, Wachsmuth M, Hoffmeyer P, Clergue F,<br />
Pittet D. Reduction of urinary tract infection and antibiotic<br />
use after surgery: a controlled, prospective, before-after<br />
intervention study. Clin Infect Dis 2006;42:1544–1551.<br />
38. Martin JT. Positioning aged patients. Anesthesiol Clin North<br />
Am 2000;18:105–121.<br />
39. Roy RC. Choosing general versus regional anesthesia for<br />
the elderly. Anesthesiol Clin North Am 2000;18:91–104.<br />
40. Kehlet H. Future perspectives and research initiatives in<br />
fast-track surgery. Langenbecks Arch Surg 2006;391:495–<br />
498.<br />
41. Jayr C, Thomas H, Rey A, Farhat F, Lasser P, Bourgain JL.<br />
Postoperative pulmonary complications. Epidural analgesia<br />
using bupivacaine and opioids versus parenteral opioids.<br />
<strong>Anesthesiology</strong> 1993;78:666–676.<br />
42. Norris EJ, Beattie C, Perler BA, et al. Double-masked randomized<br />
trial comparing alternate combinations of intraoperative<br />
anesthesia and postoperative analgesia in abdominal<br />
aortic surgery. <strong>Anesthesiology</strong> 2001;95:1054–1067.<br />
43. Wu CL, Hsu W, Richman JM, Raja SN. Postoperative<br />
cognitive function as an outcome of regional anesthesia and<br />
analgesia. Reg Anesth Pain Med 2004;29:257–268.<br />
44. Bryson GL, Wyand A. Evidence-based clinical update:<br />
general anesthesia and the risk of delirium and postoperative<br />
cognitive dysfunction. Can J Anaesth 2006;53:669–677.<br />
45. Basse L, Jakobsen DH, Bardram L, et al. Functional recovery<br />
after open versus laparoscopic colonic resection: a randomized,<br />
blinded study. Ann Surg 2005;241:416–423.<br />
46. Kehlet H, Kennedy RH. Laparoscopic colonic surgery—<br />
mission accomplished or work in progress? Colorectal Dis<br />
2006;8:514–517.<br />
47. Reeder MK, Goldman MD, Loh L, et al. Postoperative<br />
hypoxaemia after major abdominal vascular surgery. Br J<br />
Anaesth 1992;68:23–26.<br />
48. Arunasalam K, Davenport HT, Painter S, Jones JG.<br />
Ventilatory response to morphine in young and old<br />
subjects. Anaesthesia 1983;38:529–533.<br />
49. Valentine SJ, Marjot R, Monk CR. Preoxygenation in the<br />
elderly: a comparison of the four-maximal-breath and threeminute<br />
techniques. Anesth Analg 1990;71:516–519.<br />
50. Pontoppidan H, Beecher HK. Progressive loss of protective<br />
reflexes in the airway with the advance of age. JAMA 2006;<br />
174:2209–2213.<br />
51. Brimacombe JR, Berry AM. Cricoid pressure. Can J Anaesth<br />
1997;44:414–425.<br />
52. Butler J, Sen A. Best evidence topic report. Cricoid pressure<br />
in emergency rapid sequence induction. Emerg Med J 2005;<br />
22:815–816.<br />
53. Iannuzzi E, Iannuzzi M, Viola G, Cerulli A, Cirillo V,<br />
Chiefari M. Desflurane and sevoflurane in elderly patients<br />
during general anesthesia: a double blind comparison.<br />
Minerva Anestesiol 2005;71:147–155.<br />
54. Iannuzzi E, Iannuzzi M, Cirillo V, Viola G, Parisi R, Chiefari<br />
M. Small doses of remifentanil and alfentanil in continuous<br />
total intravenous anesthesia in major abdominal surgery.<br />
A double blind comparison. Minerva Anestesiol 2003;69:<br />
127–136.<br />
55. Heavner JE, Kaye AD, Lin BK, King T. Recovery of elderly<br />
patients from two or more hours of desflurane or sevoflurane<br />
anaesthesia. Br J Anaesth 2003;91:502–506.<br />
56. Kehlet H. Fast-track colonic surgery: status and perspectives.<br />
Recent Results Cancer Res 2005;165:8–13.<br />
57. Gunnarsson L, Tokics L, Brismar B, Hedenstierna G. Influence<br />
of age on circulation and arterial blood gases in man.<br />
Acta Anaesthesiol Scand 1996;40:237–243.<br />
58. Hedenstierna G, Rothen HU. Atelectasis formation during<br />
anesthesia: causes and measures to prevent it. J Clin Monit<br />
Comput 2000;16:329–335.<br />
59. Rothen HU, Sporre B, Engberg G, Wegenius G, Hedenstierna<br />
G. Reexpansion of atelectasis during general anaesthesia<br />
may have a prolonged effect. Acta Anaesthesiol Scand<br />
1995;39:118–125.<br />
60. Lachmann B. Open up the lung and keep the lung open.<br />
Intensive Care Med 1992;18:319–321.<br />
61. Epstein CD, Peerless JR. Weaning readiness and fluid<br />
balance in older critically ill surgical patients. Am J Crit<br />
Care 2006;15:54–64.<br />
62. Itobi E, Stroud M, Elia M. Impact of oedema on recovery<br />
after major abdominal surgery and potential value of
428 J.H. Silverstein<br />
multifrequency bioimpedance measurements. Br J Surg<br />
2006;93:354–361.<br />
63. Brandstrup B. Fluid therapy for the surgical patient. Best<br />
Pract Res Clin Anaesthesiol 2006;20:265–283.<br />
64. Brandstrup B, Tonnesen H, Beier-Holgersen R, et al. Effects<br />
of intravenous fluid restriction on postoperative complications:<br />
comparison of two perioperative fluid regimens: a<br />
randomized assessor-blinded multicenter trial. Ann Surg<br />
2003;238:641–648.<br />
65. Nisanevich V, Felsenstein I, Almogy G, Weissman C, Einav<br />
S, Matot I. Effect of intraoperative fluid management on<br />
outcome after intraabdominal surgery. <strong>Anesthesiology</strong> 2005;<br />
103:25–32.<br />
66. Kabon B, Akca O, Taguchi A, et al. Supplemental intravenous<br />
crystalloid administration does not reduce the risk<br />
of surgical wound infection. Anesth Analg 2005;101:<br />
1546–1553.<br />
67. Holte K, Kehlet H. Fluid therapy and surgical outcomes in<br />
elective surgery: a need for reassessment in fast-track<br />
surgery. J Am Coll Surg 2006;202:971–989.<br />
68. Berg H, Roed J, Viby-Mogensen J, et al. Residual neuromuscular<br />
block is a risk factor for postoperative pulmonary<br />
complications. A prospective, randomised, and blinded<br />
study of postoperative pulmonary complications after atracurium,<br />
vecuronium and pancuronium. Acta Anaesthesiol<br />
Scand 1997;41:1095–1103.<br />
69. Debaene B, Plaud B, Dilly MP, Donati F. Residual paralysis<br />
in the PACU after a single intubating dose of nondepolarizing<br />
muscle relaxant with an intermediate duration of<br />
action. <strong>Anesthesiology</strong> 2003;98:1042–1048.<br />
70. Tiret L, Desmonts JM, Hatton F, Vourch G. Complications<br />
associated with anaesthesia—a prospective survey in France.<br />
Can Anaesth Soc J 1986;33:336–344.<br />
71. Mattei P, Rombeau JL. Review of the pathophysiology and<br />
management of postoperative ileus. World J Surg 2006;30:<br />
1382–1391.<br />
72. Kelley MC, Hocking MP, Marchand SD, Sninsky CA. Ketorolac<br />
prevents postoperative small intestinal ileus in rats. Am<br />
J Surg 1993;165:107–111.<br />
73. Tan EK, Cornish J, Darzi AW, Tekkis PP. Meta-analysis:<br />
alvimopan vs. placebo in the treatment of post-operative<br />
ileus. Aliment Pharmacol <strong>The</strong>r 2007;25(1):47–57.<br />
74. Delaney CP. Clinical perspective on postoperative ileus<br />
and the effect of opiates. Neurogastroenterol Motil 2004;16<br />
(Suppl 2):61–66.<br />
75. Fein AM. Pneumonia in the elderly: special diagnostic and<br />
therapeutic considerations. Med Clin North Am 1994;78:<br />
1015–1034.<br />
76. Lawrence VA, Cornell JE, Smetana GW. Strategies to<br />
reduce postoperative pulmonary complications after noncardiothoracic<br />
surgery: systematic review for the American<br />
College of Physicians. Ann Intern Med 2006;144:596–608.
Index<br />
A<br />
AA. See Anesthesiologist Assistant<br />
AARP. See American Association of<br />
Retired Persons<br />
ABA. See American Board of<br />
<strong>Anesthesiology</strong><br />
Abdominal operation, 11<br />
Abdominal procedures, 416–426<br />
general principles, 416–417<br />
consent/health proxy, 417<br />
outcomes from abdominal surgery,<br />
416–417<br />
presentation, 416<br />
intraoperative care, 420–425<br />
anesthetic plans for, 421–422<br />
emergence/extubation of elderly,<br />
425<br />
epidural catheter choice, 421<br />
fluid management in elderly,<br />
422–425<br />
intravenous access/monitoring<br />
choice, 420–421<br />
postoperative care, 425–426<br />
pneumonia, 425–426<br />
postoperative complications, 425<br />
postoperative ileus, 425<br />
preoperative care, 417–420<br />
bowel preparation, 419–420<br />
geriatrician’s interaction, 420<br />
preanesthetic evaluation, 417–418<br />
Abdominal surgery, 416–417<br />
Aberrant oncogene activation, 149<br />
Abnormalities, 297<br />
Academic Health Centers (AHCs),<br />
20<br />
Accreditation Council for Graduate<br />
Medical Education (ACGME),<br />
58<br />
ACE. See Angiotensin-converting<br />
enzyme<br />
Acetabulum, 356<br />
Acetaminophen, 209–210<br />
Acetylcholine receptors, 266<br />
ACGME. See Accreditation Council for<br />
Graduate Medical Education<br />
Acid<br />
barbituric, 234<br />
gammaaminobutryic, 32<br />
Acid-base abnormalities, 297<br />
Acidosis, 154<br />
Active arteriovenous shunt<br />
vasoconstriction, 109<br />
Active precapillary vasodilation, 109<br />
Activities of Daily Living (ADL), 8, 59,<br />
70, 189<br />
Acute onset, 124<br />
Acute pain, 309<br />
Acute pain management, 79<br />
Acute tubular necrosis, 298<br />
Adenosine 5′-diphosphate (ADP), 205<br />
Adequate cardiac preload, 145<br />
ADH. See Antidiuretic hormone<br />
ADL. See Activities of Daily Living<br />
ADP. See Adenosine 5′-diphosphate<br />
Adrenergic receptor activity, 142–143<br />
Advanced glycation end-products<br />
(AGEs), 31, 137<br />
Advance directives, 44–46<br />
Adverse drug reactions, 103<br />
Adverse events, 80<br />
Afferent input, 107–108<br />
AGE. See Advanced glycation<br />
end-products<br />
Age and gender adjusted population, 71<br />
Age-rationing, 50<br />
Age related physiologic changes, 399<br />
Age-related pulmonary changes, 342<br />
AGEs. See Advanced glycation end<br />
products<br />
Aging, 4, 68–69, 151, 211, 294–295<br />
cardiovascular system, 250–252<br />
pulmonary changes associated, 327<br />
central nervous system changes of,<br />
123–124<br />
cholinergic theory of, 31<br />
clinical studies of, 35<br />
concepts of, 29–32<br />
altered receptor systems, 31–32<br />
oxidative stress, 32<br />
programmed aging, 29–30<br />
stochastic aging, 30–31<br />
definitions, 4<br />
effects on gas exchange, 153–154<br />
exercise capacity, 154<br />
general physiology of, 5<br />
human/geriatrics, 34–35<br />
neurobiologic changes, 124<br />
pathologic, 124<br />
physiologic, 5<br />
programmed, 29–30<br />
proposed molecular mechanisms of,<br />
33<br />
reconciling the theories, 32–34<br />
respiratory system, 149–160<br />
social views of, 38–39<br />
stochastic, 30–31<br />
theories, 29–36<br />
Aging lung physiology, 149–155<br />
age-related changes in mechanics of<br />
breathing, 149–153<br />
aging effects on gas exchange,<br />
153–154<br />
aging/exercise capacity, 154<br />
airway closure concept (closing<br />
volume), 152–153<br />
breathing regulation, 154–155<br />
chest wall/respiratory muscles,<br />
149–150<br />
lung parenchyma, 150<br />
spinometry/static/dynamic tests/<br />
underlying physiology, 150–152<br />
upper airway dysfunction, 155<br />
cellular mechanisms, 149<br />
perioperative pulmonary<br />
complications in elderly,<br />
155–160<br />
429
430 Index<br />
Aging lung physiology (cont.)<br />
general health status, 156–157<br />
strategies used to minimize<br />
pulmonary risk in elderly<br />
patients, 157–160<br />
Agonists<br />
alpha, 401<br />
alpha 2 -adrenergic, 200<br />
beta, 203<br />
AGS. See American <strong>Geriatric</strong> Society<br />
AHCs. See Academic Health Centers<br />
AHI. See Apnea/hypopneic index<br />
Airway<br />
closure concept, 152–153<br />
diameter, 153<br />
management, 383<br />
Albumin, 99<br />
Alfentanil, 111, 219<br />
Allodynia, 309<br />
Allogeneic transfusion requirement,<br />
114–115<br />
Alpha 1 acid glycoprotein, 99<br />
Alpha 1 -adrenergic antagonists, 200<br />
Alpha 2 -adrenergic agonists, 200<br />
Alpha agonists, 401<br />
Altered level of consciousness, 124<br />
Altered receptor systems, 31–32<br />
Alveolar concentration, 248<br />
Alveolar gas exchange, 153<br />
Alveolar surface area, 154<br />
Alveolar ventilation, 249<br />
Alveolar walls, 247<br />
Alzheimer’s disease, 124, 310<br />
AMA. See American Medical<br />
Association<br />
Ambient temperature, 116–117<br />
American Association of Retired<br />
Persons (AARP), 17<br />
American Board of <strong>Anesthesiology</strong><br />
(ABA), 58<br />
American College of Cardiology, 70<br />
American <strong>Geriatric</strong> Society (AGS), 61<br />
American Medical Association (AMA),<br />
15<br />
American Society for Gastrointestinal<br />
Endoscopy (ASGE), 344<br />
American Society of Anesthesiologists<br />
(ASA), 5, 21, 58, 165, 259, 323<br />
Amiodarone, 201<br />
Ammonia toxicity, 370–371<br />
Analgesia, 146<br />
cumulative patient-controlled, 223<br />
cyo, 385<br />
deep sedation, 341<br />
neuraxial, 386<br />
patient-controlled, 209–224, 279<br />
patient-controlled epidural, 311<br />
postoperative, 360<br />
postsurgical, 311–312<br />
regional, 315–316<br />
Analgesic efficacy, 210<br />
Analgesics, 315<br />
<strong>Anesthesia</strong>. See also General anesthesia<br />
bronchoscopy, 381<br />
cataracts, 348–350<br />
CSA, 284<br />
epidural, 278–279, 404–405<br />
general, 404–405<br />
geriatric, 3–14, 60<br />
lumbar epidural, 286<br />
Medicare, 21<br />
monitored care, 328–330<br />
neuraxial, 360–362<br />
regional, 302–303, 327–328<br />
SAGA, 14<br />
SAMBA, 322<br />
spinal, 279, 303<br />
thermoregulatory defenses during,<br />
110–111<br />
thoracic epidural, 286<br />
<strong>Anesthesia</strong> care team, 23–24<br />
attending physician relationship, 24<br />
medical direction/supervision of<br />
concurrent procedures, 23–24<br />
<strong>Anesthesia</strong> considerations for geriatric<br />
outpatients, 322–334<br />
general principles of intraoperative<br />
management, 326–330<br />
general anesthesia, 326–327<br />
monitored anesthesia care, 328–330<br />
pain management pitfalls, 330<br />
postdischarge concerns, 333–334<br />
postoperative management, 330–333<br />
hypothermia, 331<br />
postoperative atrial fibrillation, 331<br />
postoperative cognitive impairment,<br />
332–333<br />
postoperative pain, 331<br />
postoperative respiratory<br />
insufficiency, 330–331<br />
preoperative evaluation, 323–326<br />
preoperative testing, 323–324<br />
sleep apnea, 324–326<br />
<strong>Anesthesia</strong> implications, 144–147<br />
<strong>Anesthesia</strong> payment methodology, 22<br />
Anesthesiologist Assistant (AA), 21<br />
<strong>Anesthesiology</strong>, 5, 102–103<br />
adverse drug reactions, 103<br />
practice impact, 102–103<br />
residency, 58<br />
Anesthetic factors, 129–130<br />
Anesthetic implications of chronic<br />
medications, 197–206<br />
cardiovascular drugs, 200–203<br />
alpha 2 -adrenergic agonists, 200<br />
amiodarone, 201<br />
angiotensin-converting enzyme<br />
inhibitors, 203<br />
beta receptor antagonists, 201–202<br />
calcium channel blockers, 202–203<br />
digoxin, 201<br />
disopyramide, 201<br />
gastrointestinal drugs, 204<br />
cimetidine, 204<br />
metoclopramide, 204<br />
H 1 receptor antagonists, 206<br />
diphenhydramine, 206<br />
hydroxyzine/chlor-trimeton, 206<br />
neuropsychiatric/pain-related<br />
medications, 197–200<br />
antidementia drugs, 199–200<br />
Antiparkinson medications, 199<br />
benzodiazepines, 197–198<br />
carbamazepine, 198<br />
gabapentin, 198<br />
MAOIs, 198–199<br />
selective serotonin reuptake<br />
inhibitors, 199<br />
tricyclic antidepressants, 199<br />
nonsteroidal antiinflammatory drugs,<br />
205–206<br />
indomethacin, 205–206<br />
ketorolac, 205<br />
opioids, 206<br />
pentazocine, 206<br />
propoxyphene, 206<br />
oral anticoagulants, 204–206<br />
ticlopidine, 205<br />
warfarin, 204–205<br />
pulmonary drugs, 203–204<br />
beta agonists, 203<br />
theophylline, 203–204<br />
Anesthetic-induced thermoregulatory<br />
impairment in elderly, 111<br />
Anesthetic management, 182<br />
Anesthetics, 68<br />
inhalation, 246–262<br />
intravenous hypnotic, 229–242<br />
spinal, 361<br />
Anesthetic techniques, 158, 182<br />
Angina, 342<br />
Angiogenesis, 168<br />
Angiotensin-converting enzyme (ACE),<br />
203<br />
ANS. See Autonomic nervous system<br />
Antagonists<br />
alpha 1 -adrenergic, 200<br />
beta receptor, 201–202<br />
dopamine, 204<br />
H 1 receptor, 206<br />
Anticholinesterases, 272–274<br />
adverse effects of anticholinesterases<br />
in geriatric patients, 274<br />
edrophonium, 272–273<br />
neostigmine, 273–274<br />
pyridostigmine, 274<br />
Anticoagulant use, 130<br />
Anticoagulation, 360–362<br />
Antidementia drugs, 199–200<br />
Antidiuretic hormone (ADH), 293
Index 431<br />
Antiparkinson medications, 199<br />
Anxiety, 309<br />
Anxiolysis, 341<br />
Aortic valve, 391–393<br />
Apnea/hypopneic index (AHI), 324<br />
Appropriate preoperative fasting, 77<br />
Arrhythmias, 114, 144, 382<br />
Arterial sevoflurane concentration, 248<br />
Arthroplasty<br />
hip, 114, 358<br />
knee, 355–357<br />
total hip, 356–357, 359<br />
total knee, 358<br />
Arthrotomy, 357<br />
Artificial oxygenation, 154<br />
ASA. See American Society of<br />
Anesthesiologists<br />
Aspiration, 346<br />
Atracurium, 271<br />
Atropine, 274<br />
Attending physician relationship, 24<br />
Autonomic influences, 393<br />
Autonomic nervous system (ANS), 137<br />
B<br />
Baby boomer expectations, 17<br />
Back pain, 316<br />
Barbituric acid, 234<br />
Baroceptor response, 67<br />
Baroflex, 142<br />
Baroreflex, 143<br />
Basal metabolic rate (BMR), 97–98<br />
Benign prostatic hyperplasia (BPH),<br />
368<br />
Benzodiazepines, 197–198<br />
Beta-adrenergic blockade, 185<br />
Beta agonists, 203<br />
Beta-blockers, 186, 400<br />
Beta-blocker therapy, 401<br />
Beta receptor antagonists, 201–202<br />
Bilevel positive airway pressure<br />
(BiPAP), 159<br />
BiPAP. See Bilevel positive airway<br />
pressure<br />
BIS. See Bispectral index<br />
Bispectral index (BIS), 327, 405<br />
Bladder perforation, 371<br />
Bladder tumors, 372<br />
Blindness, 347<br />
Blood-brain barrier, 114<br />
Blood-component therapy, 303<br />
Blood flow<br />
cerebral, 123<br />
femoral, 250<br />
hypercapnic venous, 363<br />
in lower extremities, 170<br />
renal, 100, 102<br />
Blood loss, 81, 144, 384<br />
Blood management, 360<br />
Blood pressure, 203, 253<br />
mean arterial, 125, 283<br />
oscillometric, measurement, 420<br />
BMR. See Basal metabolic rate<br />
BNP. See B-type natriuretic peptide<br />
Body compositions, 254<br />
body fat changes, 98<br />
muscle mass, 98<br />
protein loss, 98<br />
transport proteins, 98–99<br />
Body fat, 253<br />
Body heat changes, 113<br />
Body heat content, 113<br />
Bowel preparation, 419–420<br />
BPH. See Benign prostatic hyperplasia<br />
Bradykinnin, 109<br />
Breathing mechanics, 149–153<br />
Breathing regulation, 154–155<br />
Broad-spectrum opioids, 313–314<br />
Broflex dysfunction, 283<br />
Bronchoconstriction, 155<br />
Bronchopleural fistula, 385<br />
B-type natriuretic peptide (BNP), 402<br />
Bupivacaine, 279, 284<br />
Busiprone, 110<br />
C<br />
CABG. See Coronary artery bypass<br />
graft<br />
Calcium channel blockers (CCBs), 198,<br />
202–203<br />
Calcium uptake, 139<br />
Caloric restriction, 34<br />
CAM. See Confusion Assessment<br />
Method<br />
Capillary blood volume, 154<br />
Carbamazepine, 198<br />
Cardiac baroflex, 142<br />
Cardiac muscle hypertrophy, 139<br />
Cardiac output, 251<br />
Cardiac procedures, 390<br />
CAD, 390–391<br />
preventing adverse outcomes, 394–396<br />
cardiopulmonary bypass<br />
management, 395–396<br />
cardiovascular, 394<br />
renal, 394–395<br />
valvular heart disease, 391–393<br />
aortic valve, 391–393<br />
mitral valve, 393<br />
Cardiac risk indexes, 183<br />
Cardiopulmonary bypass (CPB), 390<br />
Cardiopulmonary bypass management,<br />
395–396<br />
Cardiopulmonary complications, 384<br />
Cardiopulmonary events, 346<br />
Cardiorespiratory physiology in elderly,<br />
379<br />
Cardiovascular changes, 66–67<br />
Cardiovascular complications, 183–186,<br />
382–383<br />
predictors of, 184<br />
reducing, 184–186<br />
Cardiovascular disease (CVD), 137<br />
Cardiovascular drugs, 200–203<br />
alpha 2 -adrenergic agonists, 200<br />
amiodarone, 201<br />
angiotensin-converting enzyme<br />
inhibitors, 203<br />
beta receptor antagonists, 201–202<br />
calcium channel blockers, 202–203<br />
digoxin, 201<br />
disopyramide, 201<br />
Cardiovascular effects, 231, 240–241<br />
Cardiovascular parameters, 418<br />
Cardiovascular system, 250–252, 286<br />
Carotid endarterectomy, 409–410<br />
Carotid stents, 410<br />
Cataracts, 12, 347<br />
anesthesia, 348–350<br />
advantages of topical anesthesia,<br />
350<br />
central nervous system<br />
complications, 350<br />
monitoring/sedation, 349<br />
regional orbital anesthesia, 349<br />
retrobulbar/peribulbar anesthesia,<br />
349<br />
side effects/intraorbital anesthesia,<br />
349–350<br />
anesthesiologists role in, 350–351<br />
anticoagulation/cataract surgery, 348<br />
indications for, 348<br />
preoperative evaluation for, 348<br />
Catecholamine concentrations, 68<br />
Catheter, 81, 421<br />
CBF. See Cerebral blood flow<br />
CCBs. See Calcium channel blockers<br />
Cellular mechanisms, 149<br />
Cement, 359<br />
Central control, 108–109<br />
Central nervous system (CNS), 123, 199<br />
changes of aging, normal aging,<br />
123–124<br />
effects, 229–230<br />
Central nervous system dysfunction,<br />
123–132<br />
Central neural blockade<br />
epidural anesthesia, 278–279<br />
spinal anesthesia, 279<br />
Central pontine myelinolysis, 372<br />
Central post-stroke pain (CPSP), 316<br />
Central venous pressure (CVP), 300<br />
Cerebral blood flow (CBF), 123<br />
Cerebrospinal fluid (CSF), 235, 278<br />
Certified Registered Nurse Anesthetists<br />
(CRNAs), 21<br />
Chest wall/respiratory muscles, 149–150<br />
Chest X-rays (CXRs), 190<br />
CHF. See Congestive heart failure<br />
Chlor-trimeton, 206
432 Index<br />
Chronic medications, 197–206<br />
Chronic obstructive pulmonary disease<br />
(COPD), 156, 379<br />
Chronic pain, 81–83, 309<br />
Chronic wounds, 165–174<br />
in elderly resulting in significant<br />
morbidity/mortality, 165–168<br />
diabetic foot ulcers, 165–166<br />
ischemic wounds, 167–168<br />
pressure ulcers, 166<br />
venous ulcers, 166–167<br />
experimental evidence of physiologic<br />
impairments in elderly, 168<br />
angiogenesis in wound healing, 168<br />
decreased immune response, 168<br />
Cimetidine, 204<br />
Circulating-water mattresses, 116<br />
Circulatory function, alterations in,<br />
137–147<br />
adrenergic receptor activity/aging,<br />
142–143<br />
anesthesia implications, 144–147<br />
arrhythmias, 144<br />
heart/vessel structural alterations,<br />
137–141<br />
ischemic preconditioning, 144<br />
reflex control mechanism and aging,<br />
141<br />
renin/vasopressin activity, 143–144<br />
vagal activity/aging, 143<br />
Cisatracurium, 272<br />
CNS. See Central nervous system<br />
Coagulopathy, 114–115, 371<br />
Codeine-like drugs, 313–314<br />
Coexisting disease importance,<br />
181–182<br />
Cognitive dysfunction, 127, 182–183<br />
Cognitive function measurement, 7–8<br />
Cognitive impairment, 73<br />
Cold tolerance, 110<br />
Colloid, 284, 301<br />
Combined spinal-epidural (CSE), 284<br />
Communication skills, 58–59<br />
Comorbid conditions, 342<br />
Comorbid disease, 146<br />
Comorbidities, 172–173<br />
Comparative ethical theory, 39<br />
Complete sensory block (CSB), 280<br />
Complex regional pain syndromes, 82<br />
Compliance issues, 24–26<br />
documentation requirements, 25–26<br />
Medicare fraud/abuse, 25<br />
physicians at teaching hospitals Office<br />
of Inspector General, 25<br />
reassignment of Medicare benefits,<br />
24–25<br />
Component and Mental Component<br />
Scales, 7–8<br />
Comprehensive geriatric assessment<br />
(CGA), 12, 191–192<br />
Confusion Assessment Method (CAM),<br />
124<br />
Congestive heart failure (CHF), 185<br />
Conscious sedation, 341<br />
Context-sensitive half-time, 214<br />
Continuous positive airway pressure<br />
(CPAP), 159, 325<br />
Continuous spinal anesthesia (CSA),<br />
284<br />
COPD. See Chronic obstructive<br />
pulmonary disease<br />
Core competencies, 59<br />
Core temperatures, 117<br />
Coronary artery bypass graft (CABG),<br />
184, 390<br />
Coronary artery disease (CAD),<br />
390–391<br />
CPAP. See Continuous positive airway<br />
pressure<br />
CPB. See Cardiopulmonary bypass<br />
CPSP. See Central post-stroke pain<br />
Creatine<br />
clearance, 101<br />
serum, 216<br />
CRNAs. See Certified Registered Nurse<br />
Anesthetists<br />
Crystalloid, 302<br />
CSA. See Continuous spinal anesthesia<br />
CSB. See Complete sensory block<br />
CSE. See Combined spinal-epidural<br />
CSF. See Cerebrospinal fluid<br />
Cumulative patient-controlled analgesia,<br />
223<br />
Cutaneous warming, 116–117<br />
CVD. See Cardiovascular disease<br />
CVP. See Central venous pressure<br />
CXRs. See Chest X-rays<br />
Cyoanalgesia, 385<br />
Cystectomy, 374<br />
D<br />
Daily living, 8, 189<br />
activities of, 8, 59, 70, 189<br />
IADL, 7<br />
instrumental activities of, 190<br />
Decision making capacity, 41–42<br />
Decreased cardiac output, 146<br />
Decreased immune response, 168<br />
Deep sedation analgesia, 341<br />
Deep vein thrombosis (DVT), 167, 169<br />
Dehydration, 299<br />
Delayed wound treatment, 165<br />
Delirium, 81, 124–126<br />
anesthetic factors, 129–130<br />
delirium/adverse outcomes, 125–126<br />
after noncardiac surgery, 182–183<br />
patient factors, 127–128<br />
physiologic factors, 129<br />
surgery/illness factors, 128–129<br />
treatment/prevention, 126<br />
Dementia, 310<br />
Depression, 309<br />
DES. See Desflurane<br />
Desflurane (DES), 111, 252<br />
Deterioration, 38<br />
Determining program’s needs, 61–62<br />
Diabetes mellitus, 188<br />
Diabetic foot ulcers, 165–166<br />
Diagnostic related groups (DRG), 12<br />
Diastolic dysfunction, 139, 141, 250<br />
Diastolic filling pressures, 259<br />
Digoxin, 201<br />
Diphenhydramine, 206<br />
Disablement process, 7<br />
Diseases<br />
Alzheimer’s, 124, 310<br />
chronic obstructive pulmonary, 156,<br />
379<br />
comorbid, 146<br />
CVD, 137<br />
obstructive lung, 186<br />
venous reflux, 167<br />
Disopyramide, 201<br />
Disorganization, 38<br />
Disorganized thinking, 124<br />
Documentation requirements, 25–26<br />
Dopamine antagonist, 204<br />
Dose-response relationships, 267<br />
Double-lumen tube, 383<br />
Doxacurium, 269<br />
Doxazosin (Cadura), 200<br />
DRG. See Diagnostic related groups<br />
Drosophila, 30<br />
Drosophila melanogaster, 33<br />
Drug reactions, 69, 103<br />
Drugs<br />
antidementia, 199–200<br />
cardiovascular, 200–203<br />
codeine-like, 313–314<br />
gastroesophageal, 204<br />
gastrointestinal, 204<br />
lipid-soluble, 253<br />
water-soluble, 69<br />
Duvaldestin, 267<br />
DVT. See Deep vein thrombosis<br />
E<br />
ECCE. See Extracapsular cataract<br />
extraction<br />
ECG. See Electrocardiogram<br />
Echo-Doppler evaluation, 139<br />
ECT. See Electro-convulsive therapy<br />
Edrophonium, 272–273<br />
EEG. See Electroencephalogram<br />
Effect-site concentration, 213, 221<br />
Effect-site decrement, 221<br />
Efferent responses, 109<br />
Elderly population growth, 4<br />
Electrocardiogram (ECG), 72, 190<br />
Electro-convulsive therapy (ECT), 230
Index 433<br />
Electroencephalogram (EEG), 213<br />
Electrolyte disturbances, 81<br />
Electrolyte homeostasis, 293–294<br />
Embolic phenomena, 363<br />
Emergency resuscitation, 344<br />
Emphysema, 150, 247<br />
Endarterectomy, 409–410<br />
End-of-life care, 48–50, 314–315<br />
sedation of terminally ill, 314–315<br />
fetanyl, 314<br />
ketamine, 314<br />
midazolam, 314<br />
Endoscopic retrograde<br />
cholangiopancreatographies<br />
(ERCPs), 346<br />
Endovascular abdominal aneurysm<br />
repair (EVAR), 406<br />
Endovascular abdominal aortic<br />
aneurysm repair, 408–409<br />
Epidemiologic studies, 73<br />
Epidural absorption, 281<br />
Epidural anesthesia, 278–279, 404–405<br />
Epidural catheter choice, 421<br />
Epinephrine, 279<br />
EPP. See Equal pressure point<br />
Equal pressure point (EPP), 153<br />
ERCPs. See Endoscopic retrograde<br />
cholangiopancreatographies<br />
Erythropoietin, 360<br />
Esophageal Doppler monitors, 299<br />
ESWL. See Extracorporeal shock wave<br />
lithotripsy<br />
Ethanol, 31<br />
Ethical management of elderly patients,<br />
38–53<br />
advance directives, 44–46<br />
consent elements/decision/<br />
autonomous authorization, 44<br />
do-not-attempt resuscitation orders<br />
in operating room, 46–47<br />
end-of-life care, 48–50<br />
ethical principles, 39–40<br />
informed consent in elderly, 40–44<br />
informational elements, 43–44<br />
personal autonomy respect, 40<br />
shared decision making, 41<br />
threshold elements, 41–43<br />
resource allocation/elderly, 50–51<br />
social views of aging, 38–39<br />
treatment futility, 47–48<br />
treatment redirection/palliative care,<br />
48<br />
Ethical principles, 39–40<br />
Etomidate, 240–241<br />
adverse effects/contraindications,<br />
241<br />
dosing in elderly, 241<br />
indications, 241<br />
metabolism/disposition, 241<br />
pharmacodynamics, 240<br />
cardiovascular effects, 240–241<br />
central nervous system effects, 240<br />
endocrine effects, 241<br />
respiratory effects, 241<br />
pharmacology, 240<br />
Euglycemia, 411<br />
EVAR. See Endovascular abdominal<br />
aneurysm repair<br />
Exercise capacity, 154, 189–190<br />
Extracapsular cataract extraction<br />
(ECCE), 347<br />
Extracorporeal shock wave lithotripsy<br />
(ESWL), 372, 373<br />
F<br />
Facilitated conduction, 112<br />
Faculty development, 61<br />
Fat embolism, 363–364<br />
Fels longitudinal study, 254<br />
Femoral blood flow, 250<br />
Femoral fracture, 357<br />
Fetanyl, 215, 217–219, 314<br />
Fetanyl delivery systems, 218–219<br />
Fistula, 385<br />
Flexible fiberoptic bronchoscopy, 381<br />
Flow limitation, 152<br />
Fluid balance, 419<br />
Fluid homeostasis, 293–294<br />
Fluid management, 293–306<br />
aging/renal function, 294–295<br />
clinical implications, 298–302<br />
in elderly, 422–425<br />
fluid/electrolyte homeostasis, 293–294<br />
perioperative transfusion in elderly,<br />
303–305<br />
potassium management, 296–297<br />
sodium handling, 295–296<br />
urinary concentration, 297–298<br />
acid-base abnormalities, 297<br />
calcium/phosphate/magnesium, 297<br />
nutrition, 297–298<br />
Fluid therapy, 359<br />
Fluid warming, 117<br />
Flumazenil, 329<br />
Fluoride toxicity, 255<br />
Folstein Mini-Mental State Exam<br />
(MMSE), 8<br />
Forced vital capacity (FVC), 379<br />
Frailty, 5–6<br />
FRC. See Functional residual capacity<br />
Free plasma concentrations, 282<br />
French paradox, 31<br />
Functional adaptations, 140<br />
Functional assessments, 70–72<br />
Functional recovery, 11<br />
Functional reserve, 67, 98<br />
Functional reserve concepts, 97<br />
Functional residual capacity (FRC), 150,<br />
230<br />
Functional status assessment, 189–190<br />
Functioning, 9<br />
Futility, 47<br />
FVC. See Forced vital capacity<br />
G<br />
GABA. See Gammaaminobutryic acid<br />
Gabapentin, 198, 315<br />
Gammaaminobutryic acid (GABA), 32<br />
GAO. See Government Accounting<br />
Office<br />
Gas exchange<br />
aging and, 153–154<br />
alveolar, 153<br />
Gastroesophageal reflux, 330<br />
Gastrointestinal drugs, 204<br />
cimetidine, 204<br />
metoclopramide, 204<br />
Gastrointestinal system, 286<br />
GDS. See <strong>Geriatric</strong> Depression Scale<br />
General anesthesia, 286–288, 404–405<br />
geriatric outpatient recommendations,<br />
327<br />
intraoperative lung expansion during,<br />
158<br />
intraoperative management, 74–76,<br />
326–327<br />
for vascular patient, 404–405<br />
General health status, 156–157<br />
<strong>Geriatric</strong> anesthesia, 3–14, 60<br />
aging definitions of, 4–5<br />
approach to patient, 8–12<br />
demography, 3–4<br />
frailty, 5–6<br />
general physiology of aging, 5<br />
growth of, 60<br />
organizations/resources in, 13–14<br />
surgical outcomes/functional deadline,<br />
6–7<br />
<strong>Geriatric</strong> anesthesiology, 58–64<br />
geriatric curriculum developing,<br />
61–63<br />
assessment of resources, 61<br />
determining program’s needs, 61–62<br />
faculty development, 61<br />
producing geriatric curriculum,<br />
62–63<br />
geriatrics as part of core<br />
competencies, 58–59<br />
geriatrics in educational program, 58<br />
geriatric training importance, 59–60<br />
growth of geriatric anesthesia, 60<br />
priority research questions of, 84<br />
research priorities, 66–84<br />
physiologic changes relevant to<br />
perioperative care, 66–84<br />
postoperative management, 78–83<br />
preoperative assessment of the<br />
elderly, 69–78<br />
teaching geriatrics, 60<br />
<strong>Geriatric</strong> Depression Scale (GDS), 10
434 Index<br />
<strong>Geriatric</strong> medical care, 3<br />
<strong>Geriatric</strong> patient care<br />
demographics/economics of, 15–27<br />
Medicare demographics/financing<br />
issues, 15–20<br />
Medicare policy issues for geriatric<br />
anesthesiologist, 20–27<br />
focus areas for, 12<br />
<strong>Geriatric</strong>s<br />
in educational program, 58<br />
as part of core competencies, 58–59<br />
communication, 58–59<br />
practice-based learning/<br />
improvement, 59<br />
system-based practice, 59<br />
Gerontology, 29<br />
GFR. See Glomerular filtration rate<br />
Globe perforation, 350<br />
Glomerular filtration rate (GFR), 5, 101,<br />
255, 295<br />
Glucose control, 77<br />
Glycine, 370–371<br />
Glycopyrrolate, 274<br />
GME. See Graduate Medical Education<br />
Government Accounting Office (GAO),<br />
22<br />
Graduate Medical Education (GME),<br />
19<br />
Growth factor therapies, 172<br />
H<br />
H 1 receptor antagonists, 206<br />
Halothane, 260, 261<br />
Hearing loss, 12<br />
Heart block, 144<br />
Heart disease, 391–393<br />
Heart failure, 185<br />
Heart rate, 253<br />
Heart/vessel structural alterations,<br />
137–141<br />
Heat distribution in body, 112–114<br />
Hemodynamic lability, 283<br />
Hemodynamic response, 145<br />
Hemodynamic stability, 294<br />
Hemoglobin, 304<br />
Heparin blocks, 297<br />
Hepatic function, in elderly, 99–100<br />
laboratory tests, 100<br />
morphologic changes, 99–100<br />
physiologic changes, 100<br />
Hepatic mass, 281<br />
Hepatic metabolism, 198<br />
Herbal medications, 191<br />
Hernia repair, 73<br />
Herpes zoster, 316–317<br />
HI. See Hospital Insurance<br />
Hip arthroplasty, 114, 358<br />
Hip fracture, 355–364<br />
extracapsular fractures, 357<br />
intracapsular fractures, 357<br />
Hip fracture repair, 358<br />
Hip fracture surgery, 356<br />
Homeostenosis, 5<br />
Hospital elder life program, 420<br />
Hospital Insurance (HI), 16<br />
HSE. See Human Skin Equivalent<br />
Human Skin Equivalent (HSE), 172<br />
Hydromorphone, 217–218<br />
Hydrostatic pressure, 293<br />
Hydroxyzine, 206<br />
Hyperalgesia, 309<br />
Hyperammonemia, 371<br />
Hyperbaric bupivacaine, 284<br />
Hypercampic ventilatory responses, 230<br />
Hypercapnia, 154<br />
Hypercapnic venous blood flow, 363<br />
Hypercarbia fever, 81<br />
Hypernatremia, 296<br />
Hyperpathia, 309<br />
Hypertension, 103, 141, 146, 185, 202,<br />
342, 403<br />
Hyperthyroidism, 202<br />
Hypertrophy<br />
cardiac muscle, 139<br />
progressive ventricular, 67<br />
Hyperventilation, 129<br />
Hypokalemia, 203<br />
Hypomagnesaemia, 201<br />
Hyponatremia, 296<br />
Hypotension, 131, 144, 282–284, 385,<br />
403<br />
Hypothermia, 109, 114, 115, 284–285,<br />
331, 371<br />
Hypovolemia, 145<br />
Hypovolemic control, 145<br />
Hypoxemia, 152, 346–347<br />
Hypoxia, 67<br />
I<br />
IADL. See Instrumental activities of<br />
daily living<br />
ICCE. See Intracapsular cataract<br />
extraction<br />
ICU. See Intensive care unit<br />
Impaired drug metabolism, 116<br />
Impaired thermoregulation, 109–110<br />
Inattention, 124<br />
Increased ventricular stiffness, 140<br />
Individual cardiac baroflex, 142<br />
Indomethacin, 205–206<br />
Infections<br />
elimination, 170<br />
surgical wound, 115<br />
urinary tract, 72<br />
Informational elements, 43–44<br />
Informed consent, 41<br />
Infraaortic vascular procedures, 406<br />
Infusion duration, 214<br />
Inhalation agents, 249<br />
Inhalation anesthetics, 246–262<br />
pharmacodynamics of inhalation<br />
agents in elderly, 257–261<br />
aging/minimal alveolar<br />
concentration, 257–259<br />
cardiovascular actions of<br />
inhalational agents in elderly,<br />
259–261<br />
pharmacokinetics of, in elderly,<br />
246–256<br />
aging cardiovascular system<br />
influence, 250–252<br />
aging in pulmonary system<br />
influence, 246–249<br />
body composition changes<br />
influence, 252–255<br />
hepatic changes influence, 256<br />
renal changes influence, 255–256<br />
Inhibitors<br />
angiotensin-converting enzyme, 203<br />
monoamine oxidase, 198–199<br />
SSRIs, 199, 315<br />
In-hospital mortality rates, 409<br />
Institutional review boards (IRBs), 52<br />
Instrumental activities of daily living<br />
(IADL), 7<br />
Intensive care unit (ICU), 77, 287, 300,<br />
408<br />
Intercostal muscles, 149<br />
Interdependence, 40<br />
Intermediate-acting agents, 270–272<br />
International Study of Postoperative<br />
Cognitive Dysfunction<br />
(ISPOCD), 126<br />
Intertochanteric femoral fracture, 357<br />
Intracapsular cataract extraction<br />
(ICCE), 347<br />
Intraoperative blood loss, 144<br />
Intraoperative care, 420–425<br />
anesthetic plans for, 421–422<br />
emergence/extubation of elderly, 425<br />
epidural catheter choice, 421<br />
fluid management in elderly, 422–425<br />
intravenous access/monitoring choice,<br />
420–421<br />
Intraoperative glucose control, 77<br />
Intraoperative lung expansion, 158<br />
Intraoperative management, 74–78,<br />
326–330<br />
general anesthesia, 326–327<br />
monitored anesthesia care, 328–330<br />
pain management pitfalls, 330<br />
physiologic management, 76–78<br />
regional/general anesthesia, 74–76<br />
Intraoperative monitoring, 358<br />
Intraoperative myocardial ischemia,<br />
303–304<br />
Intraoperative research agenda items,<br />
77–78<br />
Intravenous access, 420–421<br />
Intravenous hypnotic agents, 230<br />
Intravenous hypnotic anesthetics,<br />
229–242<br />
etomidate, 240–241
Index 435<br />
midazolam, 237–240<br />
propofol, 229–234<br />
pharmacodynamics, 229–231<br />
pharmacology, 229<br />
thiopental, 234–237<br />
Intravenous isoprotenerol infusions,<br />
142<br />
IRBs. See Institutional review boards<br />
Irrigation solutions, 369<br />
Ischemia, 114<br />
Ischemic preconditioning, 144<br />
Ischemic wounds, 167–168<br />
Isoflurane, 129, 254, 255<br />
concentration, 258<br />
nitrous oxide, 129<br />
Isoprotenerol infusions, 142<br />
ISPOCD1. See International Study of<br />
Postoperative Cognitive<br />
Dysfunction<br />
J<br />
Joint arthroplasty, 356<br />
Joint replacement, 355–364<br />
K<br />
Ketamine, 314<br />
Ketorolac, 205, 385<br />
Kidney stone, 309<br />
Knee arthroplasty, 355–357<br />
Knee joint arthrotomy, 357<br />
L<br />
Laboratory and radiologic evaluation,<br />
169–170<br />
Laboratory tests, 100<br />
Laparoscopic surgery, 373–374<br />
Lateral decubitus position, 359<br />
Left ventricular ejection fraction<br />
(LVEF), 201<br />
Lidocaine, 381<br />
Lipid-soluble drugs, 253<br />
Liver function, 256<br />
Living will, 45<br />
LMWH. See Low-molecular weight<br />
heparin<br />
Local effects, 362<br />
Local wound care, 170–171<br />
Long-acting agents, 269–270<br />
Lower esophageal sphincter, 204<br />
Low-molecular weight heparin<br />
(LMWH), 361, 406<br />
Low sodium plasma levels, 101<br />
Lumbar compression fractures, 316<br />
Lumbar epidural anesthesia, 286<br />
Lumbar radiculopathy, 317<br />
Lung<br />
cancer, 378<br />
expansion, 158<br />
parenchyma, 150<br />
physiology, 149–155<br />
volumes, 151<br />
LVEF. See Left ventricular ejection<br />
fraction<br />
M<br />
MAC. See Minimal alveolar<br />
concentration<br />
Major autonomic thermoregulatory<br />
defenses, 109<br />
Major autonomic warm defenses, 108<br />
Mammals, 30<br />
MAOIs. See Monoamine Oxidase<br />
Inhibitors<br />
MAP. See Mean arterial pressure<br />
Maximal minute ventilation, 67<br />
Maximal neuromuscular blocking, 268<br />
Maximum intensity, 107<br />
Mean aortic pressure, 138<br />
Mean arterial blood pressure, 125, 283<br />
Mean arterial pressure (MAP), 229<br />
Mean cutaneous heat, 117<br />
Mean plasma concentrations, 282<br />
Mean skin temperature, 108<br />
Mechanical ventilation, 159–160<br />
Mediastinoscopy, 381–382<br />
Medical direction, 26<br />
Medical fitness, 137<br />
Medical Insurance Trust Fund, 17<br />
Medicare anesthesia, 21<br />
Medicare demographics/financing issues,<br />
15–20<br />
Medicare/Academic Health Center,<br />
19–20<br />
GME payments, 19–20<br />
pay for performance initiatives, 20<br />
Medicare coverage gaps, 17–19<br />
impact on near-poor, 18–19<br />
prescription drug benefit, 18<br />
Medicare program enacted, 15<br />
organization/funding, 15–16<br />
twenty-first century realities/Medicare<br />
future, 16–17<br />
Medicare Fee Schedule (MFS), 21<br />
Medicare fraud/abuse, 25<br />
Medicare payment methodologies for<br />
anesthesia services<br />
Medicare fee schedule for anesthesia<br />
services, 21–22<br />
Medicare’s resource based relative<br />
value system, 21<br />
proposed changes to the anesthesia<br />
payment methodology, 22<br />
sustainable growth rate formula,<br />
22–23<br />
Medicare policy issues, for geriatric<br />
anesthesiologist, 20–27<br />
anesthesia care team, 23–24<br />
anesthesiologist participation in<br />
Medicare Program, 20–21<br />
compliance issues, 24–26<br />
Medicare payment methodologies for<br />
anesthesia services, 21–23<br />
Medication management, 310–311<br />
Medigap, 18<br />
Meperidine, 217, 312, 345<br />
Messenger RNA (mRNA), 31<br />
Metabolic acidosis, 154<br />
Metabolic equivalents (METs), 184, 399<br />
Metabolic functions/electrolytes, 97–107<br />
aims, 97<br />
albumin, 99<br />
alpha 1 acid glycoprotein, 99<br />
anesthesiology practice, 102–103<br />
basal metabolic rate, 97–98<br />
functional reserve concepts, 97<br />
hepatic function in elderly, 99–100<br />
renal function, 100–103<br />
creatine clearence, 101<br />
glomerular filtration rate, 101<br />
renal blood flow, 100, 102<br />
renal mass, 100–101<br />
tubular function, 101–102<br />
Metabolism<br />
etomidate, 241<br />
hepatic, 198<br />
impaired drug, 116<br />
midazolam, 238–239<br />
mild hypothermia, 116<br />
propofol, 231<br />
thiopental, 236<br />
Methadone, 222<br />
Metoclopramide, 204<br />
Metocurine, 267<br />
METs. See Metabolic equivalents<br />
MFS. See Medicare Fee Schedule<br />
Midazolam, 110, 197, 237–240, 314,<br />
344<br />
adverse effects and contraindications,<br />
240<br />
effects of age on pharmacology, 240<br />
indications, 239<br />
induction/maintenance anesthesia,<br />
239<br />
intravenous sedation, 239<br />
metabolism/disposition, 238–239<br />
pharmacodynamics, 237–238<br />
cardiovascular effects, 238<br />
central nervous system effects,<br />
237–238<br />
respiratory effects, 238<br />
pharmacology, 237<br />
Mild emphysema, 247<br />
Mild hypothermia, 114<br />
complications of, 114–116<br />
coagulopathy/allogeneic transfusion<br />
requirement, 114–115<br />
impaired drug metabolism, 116<br />
myocardial ischemia/arrhythmias,<br />
114<br />
postoperative shivering, 115–116<br />
surgical wound infections/during<br />
hospitalization, 115<br />
Mild intraoperative hypothermia, 115
436 Index<br />
Minimal alveolar concentration (MAC),<br />
69, 230, 251, 257, 259, 405<br />
Minimal sedation, 341<br />
Mitral valve, 393<br />
MMSE. See Folstein Mini-Mental State<br />
Exam<br />
Moderate sedation, 341<br />
Modern cataract surgery, 347–350<br />
Modified postanesthesia discharge<br />
scoring system, 333<br />
Monitored anesthesia care, 328–330<br />
Monoamine Oxidase Inhibitors<br />
(MAOIs), 198–199<br />
Morbidity, 5<br />
Morphine, 215–217<br />
Morphine-6-glucuronide, 216<br />
Morphologic changes, 99–100<br />
Mortality, 5, 391<br />
mRNA. See Messenger RNA<br />
mtDNA, 34<br />
Multifocal atrial tachycardia, 384<br />
Muscles<br />
chest wall/respiratory, 149–150<br />
intercostal, 149<br />
MVO 2 . See Myocardial oxygen<br />
consumption<br />
Myocardial contractility, 260<br />
Myocardial ischemia, 114, 303–304<br />
Myocardial oxygen consumption<br />
(MVO 2 ), 235<br />
Mythological foundation, 51<br />
N<br />
Narrow-spectrum opioids, 313<br />
Nasogastric tubes, 78<br />
National Surgical Quality Improvement<br />
Program (NSQIP), 6<br />
National Veterans Administration<br />
Surgical Risk Study, 189<br />
NDMA. See N-methyl-d-aspartate<br />
nDNA. See nuclear DNA<br />
Necrosis, 298<br />
Neostigmine, 273–274<br />
Neo-Synephrine, 403<br />
Nephrectomy, 374–375<br />
Neuraxial analgesia, 386<br />
Neuraxial anesthesia, 360–362<br />
Neuraxial blocks, 158<br />
Neurologic changes, 68<br />
Neurologic consultation, 131<br />
Neuromuscular block, 268–269<br />
Neuromuscular blocker (NMBD), 233<br />
Neuropathic pain, 310, 313–315, 315<br />
Neuropsychiatric/pain-related<br />
medications, 197–200<br />
antidementia drugs, 199–200<br />
Antiparkinson medications, 199<br />
benzodiazepines, 197–198<br />
carbamazepine, 198<br />
gabapentin, 198<br />
MAOIs, 198–199<br />
SSRIs, 199<br />
tricyclic antidepressants, 199<br />
Neurotransmitters, 258<br />
New consumerism, 43<br />
New York Heart Association (NYHA),<br />
391<br />
Nitric oxide, 114<br />
Nitrous oxide, 129, 249<br />
NMBD. See Neuromuscular blocker<br />
N-methyl-d-aspartate (NDMA),<br />
200<br />
Nociception, 309–310<br />
Non-cardiac surgical procedures,<br />
399<br />
Nondepolarizing neuromuscular<br />
blocking agents, 268, 270<br />
Noninvasive positive pressure<br />
ventilation, 159<br />
Nonischemic electrocardiogram, 399<br />
Nonshivering thermogenesis, 107<br />
Nonsteroidal antiinflammatory<br />
analgesics, 315<br />
Nonsteroidal antiinflammatory drugs<br />
(NSAIDs), 203, 205–206, 311<br />
indomethacin, 205–206<br />
ketorolac, 205<br />
Nonviable tissue, 171–172<br />
Normal thermoregulation, 107–109<br />
North American Symptomatic Carotid<br />
Endarectomy Trial, 76<br />
NSAIDs. See Nonsteroidal<br />
antiinflammatory drugs<br />
NSQIP. See National Surgical Quality<br />
Improvement Program<br />
nuclear DNA (nDNA), 30<br />
Nutrition, 297–298<br />
Nutritional assessment, 188–189<br />
NYHA. See New York Heart<br />
Association<br />
O<br />
Observed mortality, 391<br />
Obstructive lung disease, 186<br />
Obstructive sleep apnea (OSA), 155,<br />
324, 326<br />
Obstructive sleep apnea syndrome<br />
(OSAS), 187<br />
Office of the Inspector General (OIG),<br />
24–26, 25<br />
Offloading pressure, 172<br />
OIG. See Office of the Inspector<br />
General<br />
Oncogene activation, 149<br />
Operating room, 165<br />
Operations, 11<br />
Operative debridements, 165–174<br />
for chronic wounds, 165–174<br />
in elderly resulting in significant<br />
morbidity/mortality, 165–168<br />
experimental evidence of<br />
physiologic impairments in<br />
elderly, 168<br />
intraoperative risk and precautions<br />
for development of pressure<br />
ulcers, 173–174<br />
multidisciplinary approach for<br />
treating ulcers, 168–173<br />
operating room, 165<br />
Operative mortality rate, 392<br />
Opioids, 159, 206. See also Specific<br />
opioids<br />
addiction, 312<br />
drug effect, 211–215<br />
offset, 214–216<br />
onset, 211–214<br />
frequently used, 212<br />
narrow-spectrum, 313<br />
pharmacology, 209–224<br />
age/, 211<br />
aging/pain perception, 211<br />
general observations, 209–210<br />
opioid receptor, 210–211<br />
patient controlled anesthesia,<br />
222–224<br />
specific, 215–222<br />
relative potency of, 214<br />
Opioid therapy, 312–313<br />
anticonvulsants for neuropathic pain,<br />
315<br />
case examples, 317–319<br />
excessive treatment in a missed<br />
diagnosis, 317–319<br />
lumbar radiculopathy, 317<br />
common pain syndromes, 316–317<br />
back pain, 316<br />
herpes zoster, 316–317<br />
postherpetic neuralgia, 317<br />
spinal stenosis, 316<br />
thoracic/lumbar compression<br />
fractures, 316<br />
end-of-life care, 314–315<br />
for neuropathic pain/broad-spectrum<br />
opioids, 313–314<br />
nonsteroidal antiinflammatory<br />
analgesics, 315<br />
opioid addiction, 312<br />
opioid conversions, 312–313<br />
pain/insulin resistance, 315–316<br />
titration of, 312<br />
tricyclic antidepressants/specific<br />
serotonin reuptake inhibitors,<br />
315<br />
Optic nerve damage, 350<br />
Oral anticoagulants, 204–206<br />
ticlopidine, 205<br />
warfarin, 204–205<br />
Orbital hemorrhage, 350<br />
Organ function, 97<br />
Organ system functional reserve, 30
Index 437<br />
OSA. See Obstructive sleep apnea<br />
OSAS. See Obstructive sleep apnea<br />
syndrome<br />
Oscillometric blood pressure<br />
measurement, 420<br />
Osmolality, 369<br />
Oxidative phosphorylation, 34<br />
Oxidative stress, 32<br />
Oxygenation, 129, 154, 381<br />
Oxygen supply-demand ratio, 286<br />
Oxyhemoglobin desaturation, 154<br />
P<br />
PACU. See Postanesthesia care unit<br />
PADSS. See Postanesthesia discharge<br />
scoring system<br />
PAHC. See Power of Attorney for<br />
Healthcare<br />
Pain, 79–80<br />
acute, 309<br />
back, 316<br />
central post-stroke, 316<br />
chronic, 81–83, 309<br />
neuropathic, 310, 313–315<br />
opioid therapy and, 315–316<br />
perception, 211<br />
postoperative, 331<br />
somatic, 310<br />
Southern California Cancer Pain<br />
Initiative, 313<br />
subjectivity of, 308<br />
visceral, 310<br />
Pain-controlled analgesia (PCA), 311<br />
Pain management, 173, 308–319<br />
acute, 79<br />
assessment, 309<br />
CYP 2D6 enzyme/efficacy of codeine/<br />
codeine-like drugs, 313–314<br />
depression/anxiety/pain, 309<br />
fear of reporting, 309<br />
medication management, 310–311<br />
neuraxial blocks, 158<br />
nociception and, 309–310<br />
opioid therapy, 312–313<br />
pathophysiology of, 310–311<br />
neuropathic pain, 310<br />
somatic pain, 310<br />
visceral pain, 310<br />
pitfalls, 330<br />
postoperative, 183<br />
postsurgical analgesia, 311–312<br />
postthoracotomy, 385–386<br />
three pain scenarios, 309<br />
Pairwise associations, 6<br />
Palliative care, 48<br />
Pancuronium, 270<br />
Parenchyma, 248<br />
Parkinsonism, 310<br />
Passive insulation, 116–117<br />
Pathologic aging, 124<br />
Pathophysiologic mechanisms, 151<br />
Patient-controlled analgesia (PCA),<br />
209–224, 279<br />
Patient-controlled epidural analgesia<br />
(PCEA), 311<br />
Patient-controlled sedation (PCS),<br />
345<br />
Patient Self-Determination Act (PSDA),<br />
44<br />
PCA. See Pain-controlled analgesia<br />
PCEA. See Patient-controlled epidural<br />
analgesia<br />
PCS. See Patient-controlled sedation<br />
Pedersen study, 183<br />
PEEP. See Positive end-expiratory<br />
pressure<br />
Pentazocine, 206<br />
Perioperative activity level, 138<br />
Perioperative beta-blockers, 400<br />
Perioperative care, physiologic changes<br />
relevant to, 66–69<br />
aging/pharmacokinetics/<br />
pharmodynamics, 68–69<br />
cardiovascular changes, 66–67<br />
implications, 69<br />
neurologic changes, 68<br />
pulmonary changes, 67–68<br />
renal changes, 68<br />
Perioperative clonidine, 76<br />
Perioperative fluid therapy, 299<br />
Perioperative functional assessment,<br />
71<br />
Perioperative geriatrics, 3<br />
Perioperative goals, 399<br />
Perioperative heat balance, 112–114<br />
Perioperative hemodynamic stability,<br />
67<br />
Perioperative optimization, 73–74<br />
Perioperative pulmonary complications<br />
in elderly, 155–160<br />
Perioperative stroke, 130–132<br />
Perioperative testing, 72–73<br />
Perioperative thermoregulation,<br />
107–118<br />
impaired thermoregulation in elderly,<br />
109–110<br />
mild hypothermia, 114<br />
normal thermoregulation, 107–109<br />
afferent input, 107–108<br />
central control, 108–109<br />
efferent responses, 109<br />
thermal management, 116–117<br />
thermoregulation during anesthesia,<br />
110–111<br />
anesthetic-induced<br />
thermoregulatory impairment in<br />
elderly, 111<br />
thermoregulatory defenses during<br />
anesthesia, 110–111<br />
Peripheral nerve blockade, 280–282<br />
pharmacology, 280<br />
pharmacokinetics, 280–282<br />
system absorption, 280–281<br />
systemic disposition, 281–282<br />
Personal autonomy respect, 40<br />
Persuasion, 44<br />
Pharyngeal trespass, 78<br />
Phenylephrine, 408<br />
PHN. See Postherpetic neuralgia<br />
Phosphorylation, 34<br />
Physical therapy, 173<br />
Physiologic aging, 5<br />
Physiologic changes, 100, 399<br />
Physiologic factors, 129<br />
Physiologic management, 76–78<br />
Plasma concentration, 213<br />
Plasma metocurine, 267<br />
Plasma proteins, 256<br />
Pneumonia, 425–426<br />
Pneumothorax, 382<br />
POCD. See Postoperative cognitive<br />
dysfunction<br />
POGOe. See Portal of <strong>Geriatric</strong>s Online<br />
Education<br />
Polycythemia, 324<br />
Polymethylmethacrylate bone cement,<br />
359<br />
PONV. See Postoperative nausea and<br />
vomiting<br />
Portal of <strong>Geriatric</strong>s Online Education<br />
(POGOe), 63<br />
Positioning, 358–359<br />
Positive end-expiratory pressure<br />
(PEEP), 158, 381<br />
Postanesthesia care unit (PACU), 249,<br />
326<br />
Postanesthesia delirium, 254<br />
Postanesthesia discharge scoring system<br />
(PADSS), 333<br />
Postganglionic nerves, 109<br />
Postherpetic neuralgia (PHN), 82, 317<br />
Postoperative analgesia, 360<br />
Postoperative atrial fibrillation, 331<br />
Postoperative care, 425–426<br />
pneumonia, 425–426<br />
postoperative complications, 384–385,<br />
425<br />
postoperative ileus, 425<br />
Postoperative central nervous system<br />
dysfunction, 123–132<br />
central nervous system changes of<br />
aging, 123–124<br />
normal aging, 123–124<br />
pathologic aging, 124<br />
delirium, 124–126<br />
perioperative stroke, 130–132<br />
postoperative cognitive dysfunction,<br />
126–130<br />
Postoperative cognitive dysfunction<br />
(POCD), 123, 126–130, 182
438 Index<br />
Postoperative cognitive function, 285<br />
Postoperative cognitive impairment,<br />
332–333<br />
Postoperative complications, 384–385,<br />
425<br />
Postoperative ileus, 288, 425<br />
Postoperative management, 78–83, 302,<br />
330–333<br />
acute pain management, 79<br />
chronic pain, 81–83<br />
delirium/cognitive decline, 80–81<br />
hypothermia, 331<br />
pain/adverse outcomes, 79–80<br />
postoperative atrial fibrillation, 331<br />
postoperative cognitive impairment,<br />
332–333<br />
postoperative pain, 331<br />
postoperative respiratory insufficiency,<br />
78, 330–331<br />
Postoperative nausea and vomiting<br />
(PONV), 322<br />
Postoperative pain, 331<br />
Postoperative pain management, 183<br />
Postoperative research agenda items,<br />
82–83<br />
Postoperative respiratory assistance,<br />
159<br />
Postoperative respiratory insufficiency,<br />
78, 330–331<br />
Postoperative shivering, 115–116<br />
Postoperative surgical stress responses,<br />
285<br />
Postsurgical analgesia, 311–312<br />
Postthoracotomy pain management,<br />
385–386<br />
Potassium management, 296–297<br />
Power of Attorney for Healthcare<br />
(PAHC), 45<br />
Practice-based learning/improvement,<br />
59<br />
Preanesthetic evaluation, 417–418<br />
Preoperative assessment of the elderly,<br />
11, 69–78<br />
functional asessments, 70–72<br />
intraoperative management, 74–78<br />
perioperative optimization, 73–74<br />
perioperative testing, 72–73<br />
risk stratification, 70<br />
Preoperative care, 417–420<br />
bowel preparation, 419–420<br />
geriatricians interaction, 420<br />
preanesthetic evaluation, 417–418<br />
Preoperative discontinuation, 191<br />
Preoperative evaluation, 323–326,<br />
379–380<br />
preoperative testing, 323–324<br />
sleep apnea, 324–326<br />
Preoperative fasting guidelines, 344<br />
Preoperative research agenda items,<br />
73–74<br />
Preoperative risk stratification, 181–192<br />
cardiovascular complications,<br />
183–186<br />
coexisting disease importance,<br />
181–182<br />
cognitive dysfunction/delirium after<br />
noncardiac surgery, 182–183<br />
comprehensive geriatric assessment,<br />
191–192<br />
diabetes mellitus, 188<br />
exercise capacity/functional status<br />
assessment, 189–190<br />
laboratory values, 190–191<br />
medications, 191<br />
nutritional assessment, 188–189<br />
pulmonary complications, 186–187<br />
renal dysfunction, 187<br />
Preoperative testing, 323–324<br />
Preprocedure evaluation, 343<br />
Pressure ulcers, 166, 173–174<br />
Prewarming, 117<br />
Proactive geriatric consultation, 192<br />
Producing geriatric curriculum, 62–63<br />
computer-based materials, 63<br />
didactics, 62<br />
discussion groups, 62–63<br />
evaluation of curriculum, 63<br />
reference books, 63<br />
sample curriculum, 62<br />
stimulation, 63<br />
Programmed aging, 29–30<br />
Progressive hypoxia, 67<br />
Progressive neurogenic process, 266<br />
Progressive ventricular hypertrophy, 67<br />
Prolonged sedation, 258<br />
Proper hemostatic control, 172<br />
Prophylactic anticoagulation, 356<br />
Propofol, 111, 345<br />
adverse effects/contraindications, 233<br />
context-sensitive half-time, 233<br />
dosing in elderly, 231–233<br />
future considerations, 233–234<br />
indications, 231<br />
infusion rate, 232<br />
metabolism/disposition, 231<br />
pharmacodynamics, 229–231<br />
cardiovascular effects, 231<br />
central nervous system effects,<br />
229–230<br />
other effects, 231<br />
respiratory effects, 230–231<br />
Propoxyphene, 206, 312<br />
Prostatectomy, 374<br />
Proteins<br />
body compositions, 98<br />
plasma, 256<br />
transport, 98–99<br />
PSDA. See Patient Self-Determination<br />
Act<br />
Pulmonary changes, 67–68, 327, 342<br />
Pulmonary complications, 155–160,<br />
186–187, 384<br />
Pulmonary drugs, 203–204<br />
beta agonists, 203<br />
theophylline, 203–204<br />
Pulmonary outcome, 287<br />
Pulmonary parenchyma, 248<br />
Pulmonary risk in elderly patients,<br />
157–160<br />
anesthesia induction, 157–158<br />
anesthesia muscle relaxants, 158<br />
caution regarding perioperative use of<br />
opioids, 158–159<br />
intraoperative lung expansion during<br />
general anesthesia, 158<br />
mechanical ventilation in elderly,<br />
159–160<br />
neuraxial blocks for pain<br />
management, 158<br />
noninvasive positive pressure<br />
ventilation, 159<br />
postoperative respiratory assistance<br />
to maintain lung expansion, 159<br />
preoperative testing, 157<br />
preoperative therapies, 157<br />
regional anesthetic techniques, 158<br />
surgical considerations, 157<br />
Pulmonary system, 286<br />
Pulmonary venous blood, 251<br />
Pupilometry, 216<br />
Pyridostigmine, 273, 274<br />
R<br />
Radical cystectomy, 374<br />
Radical nephrectomy, 374–375<br />
Radical prostatectomy, 374<br />
Radiocontrast dye, 296<br />
Raynaud’s syndrome, 202<br />
RCRI. See Revised Cardiac Risk Index<br />
Reactive oxygen species (ROS), 32<br />
Receptors<br />
acetylcholine, 266<br />
adrenergic activity, 142–143<br />
altered, systems, 31–32<br />
opioids, 210, 211<br />
Reduced cardiac output, 252<br />
Reflex control mechanism, 141<br />
Reflex inhibition, 286<br />
<strong>Regional</strong> analgesia, 315–316<br />
<strong>Regional</strong> anesthesia, 302–303, 327–328<br />
<strong>Regional</strong> anesthesia management,<br />
278–288<br />
age-related changes relevant to, 278<br />
beneficial aspects of regional<br />
anesthesia, 285–286<br />
cardiovascular system, 286<br />
gastrointestinal system, 286<br />
pulmonary system, 286<br />
central neural blockade, 278–279<br />
epidural anesthesia, 278–279<br />
spinal anesthesia, 279<br />
hypotension, 282–284<br />
hypothermia, 284–285
Index 439<br />
outcome/regional/general anesthesia,<br />
286–288<br />
cardiac outcome, 287<br />
coagulation, 287<br />
gastrointestinal outcome, 288<br />
pulmonary outcome, 287<br />
peripheral nerve blockade, 280–282<br />
postoperative cognitive function, 285<br />
problems, 282<br />
sedation, 285<br />
Regression line slopes, 142<br />
Relaxants, 266–274<br />
anticholinesterases, 272–274<br />
changes in structure of neuromuscular<br />
junction, 266–267<br />
dose-response relationships in elderly,<br />
267<br />
neuromuscular block onset, 268–269<br />
outcome studies, 274<br />
pharmacokinetics/duration of effect<br />
intermediate-acting agents, 270–272<br />
long-acting agents, 269–270<br />
short duration of action, 272<br />
Remifentanil, 220–222<br />
Renal blood flow, 100, 102<br />
Renal changes, 68<br />
Renal dysfunction, 187, 395<br />
Renal function, 294–295<br />
Renal impairment, 200<br />
Renin/vasopressin activity, 143–144<br />
Resource allocation, 50–51<br />
Respiratory depression, 198, 209<br />
Respiratory effects, 230–231<br />
Respiratory heat, 113<br />
Retinal effects, 369<br />
Revised Cardiac Risk Index (RCRI),<br />
398<br />
Risk classification tree, 394<br />
Risk stratification, 70<br />
Rocuronium, 271<br />
ROS. See Reactive oxygen species<br />
S<br />
SAGA. See <strong>The</strong> Society for the<br />
Advancement of <strong>Geriatric</strong><br />
<strong>Anesthesia</strong><br />
SAMBA. See Society for Ambulatory<br />
<strong>Anesthesia</strong><br />
Scoliosis, 319<br />
Sedation, 285, 341–351<br />
administering, 343–347<br />
adverse events, 346<br />
consent, 343–344<br />
emergency resuscitation, 344<br />
medications, 344–346<br />
monitoring, 344<br />
oxygen, 344<br />
preoperative fasting guidelines,<br />
344<br />
preprocedure evaluation, 343<br />
reversal agents, 346<br />
scheduling/information, 346<br />
sedation history, 343<br />
administration sedation, 342–343<br />
communication, 343<br />
positioning, 342<br />
comorbid conditions, 342<br />
conscious, 341<br />
eye surgeries in elderly, 347–351<br />
cataracts, 347<br />
modern cataract surgery, 347–350<br />
meaning of, 341<br />
minimal, 341<br />
moderate, 341<br />
as particular concern, 341<br />
patient-controlled, 345<br />
regional anesthesia management, 285<br />
Selective serotonin reuptake inhibitors<br />
(SSRIs), 199, 315<br />
Senescence, 30<br />
Senescent physiology, 12<br />
Senile emphysema, 150<br />
SEP. See Specific entropy production<br />
Septicemia, 371<br />
Sevoflurane, 256<br />
SGR. See Sustainable growth rate<br />
formula<br />
Shared decision making, 41<br />
Short duration of action, 272<br />
Sleep apnea, 155, 187, 324–326<br />
SMI. See Supplementary Medical<br />
Insurance<br />
Society for Ambulatory <strong>Anesthesia</strong><br />
(SAMBA), 322<br />
<strong>The</strong> Society for the Advancement of<br />
<strong>Geriatric</strong> <strong>Anesthesia</strong> (SAGA), 14<br />
Society of Thoracic Surgeons (STS), 390<br />
Sodium conservation, 68<br />
Sodium handling, 295–296<br />
Southern California Cancer Pain<br />
Initiative, 313<br />
Specific entropy production (SEP), 30<br />
Specific opioids<br />
alfentanil, 111, 219<br />
fetanyl, 215, 217–219, 314<br />
hydromorphone, 217–218<br />
meperidine, 217, 312, 345<br />
methadone, 222<br />
morphine, 215–217<br />
remifentanil, 220–222<br />
sufentanil, 219–220<br />
Spinal anesthesia, 279, 303<br />
Spinal anesthetics, 361<br />
Spinal stenosis, 316<br />
SSRIs. See Selective serotonin reuptake<br />
inhibitors<br />
Static elastic recoil, 150<br />
Statins, 402<br />
Steroid-treating groups, 364<br />
St. John’s wort, 191<br />
Stochastic aging, 30–31<br />
Stress, 32, 285<br />
Stroke, 310<br />
Stroke management, 132<br />
Stroke volume (SV), 283<br />
STS. See Society of Thoracic Surgeons<br />
Subarchnoid injection, 385<br />
Substantial hypotension, 144<br />
Substituted judgment, 51<br />
Subtle systolic dysfunction, 141<br />
Sufentanil, 219–220<br />
Supine position, 384<br />
Supplemental insurance, 18<br />
Supplemental Security Income, 18<br />
Supplementary Medical Insurance<br />
(SMI), 16<br />
Surgery<br />
abdominal, 416–417<br />
hip fracture, 356<br />
laparoscopic, 373–374<br />
modern cataract, 347–350<br />
thoracic, 71<br />
Surgical dislocation, 356<br />
Surgical procedure, 368<br />
Surgical wound infections, 115<br />
Sustainable growth rate formula (SGR),<br />
22–23<br />
SV. See Stroke volume<br />
Syndromes<br />
common pain, 316–317<br />
complex regional pain, 82<br />
OSAS, 187<br />
Raynaud’s, 202<br />
transurethral prostatectomy,<br />
368–375<br />
visceral hypersensitivity pain, 310<br />
System-based practice, 59<br />
Systolic function, 140<br />
Systolic hypertension, 403<br />
T<br />
Tachycardia, 146<br />
TBW. See Total body water<br />
TEA. See Thoracic epidural anesthesia<br />
TEE. See Transesophageal<br />
echocardiography<br />
Telomere shortening, 31<br />
Thallium scanning, 73<br />
<strong>The</strong>ophylline, 203–204<br />
<strong>The</strong>ories of Aging, 4<br />
<strong>The</strong>rapeutic misconception, 52<br />
<strong>The</strong>rapy<br />
blood-component, 303<br />
electro-convulsive, 230<br />
fluid, 359<br />
growth factor, 172<br />
perioperative fluid, 299<br />
physical, 173<br />
wound and compression, 172<br />
<strong>The</strong>rmal management, 116–117<br />
ambient temperature/passive<br />
insulation/cutaneous warming,<br />
116–117
440 Index<br />
<strong>The</strong>rmal management (cont.)<br />
fluid warming, 117<br />
prewarming, 117<br />
<strong>The</strong>rmoception, 309<br />
<strong>The</strong>rmoregulatory defenses, 108<br />
Thiopental, 234–237<br />
adverse effects/contraindications,<br />
236–237<br />
dosing in elderly, 236<br />
indications, 236<br />
metabolism/disposition, 236<br />
pharmacodynamics, 234<br />
cardiovascular system, 235<br />
central nervous system effects, 234<br />
onset of central nervous system<br />
effects, 234–235<br />
respiratory system, 235–236<br />
pharmacology, 234<br />
Thirty-day mortality, 6<br />
Thoracic epidural anesthesia (TEA),<br />
286<br />
Thoracic lumbar compression fractures,<br />
316<br />
Thoracic procedures, 378–387<br />
airway management, 383<br />
bronchoscopy, 380–381<br />
anesthesia, 381<br />
ventilation/oxygenation, 381<br />
cardiorespiratory physiology in<br />
elderly, 379<br />
cardiovascular complications, 382–383<br />
flexible fiberoptic bronchoscopy, 381<br />
intraoperative anesthetic<br />
management, 383–384<br />
mediastinoscopy, 381–382<br />
monitoring, 383<br />
morbidity/mortality of thoracic<br />
surgical procedures in elderly,<br />
378–379<br />
postoperative complications, 384–385<br />
postthoracotomy pain management,<br />
385–386<br />
preoperative evaluation, 379–380<br />
thoracotomy, 382<br />
videothorascopy, 386<br />
Thoracic surgery, 71<br />
Threshold elements, 41–43<br />
decision making capacity, 41–42<br />
voluntariness, 42<br />
Thromboprophylaxis, 362<br />
Ticlopidine, 205<br />
Titration, 312<br />
TLC. See Total lung capacity<br />
Total body fat content, 252<br />
Total body water (TBW), 99<br />
Total hip arthroplasty, 356–357, 359<br />
Total hip replacement, 355–364<br />
Total knee arthroplasty, 358<br />
Total lung capacity (TLC), 150<br />
Total plasma clearance, 281<br />
Tourniquet-related complications, 362<br />
Toxic fluoride, 256<br />
Toxicity, 370–371<br />
Transesophageal echocardiography<br />
(TEE), 383<br />
Transfusion Requirements in Critical<br />
Care (TRICC), 305<br />
Transient bacteremia, 371<br />
Transparency, 43<br />
Transport proteins, 98–99<br />
Transpulmonary pressure, 152<br />
Transurethral prostatectomy (TURP),<br />
368<br />
irrigation solutions, 369<br />
surgical procedure, 368<br />
Transurethral prostatectomy syndrome,<br />
368–375<br />
absorption of irrigating solution, 370<br />
anesthetic considerations for, 371–372<br />
bladder perforation, 371<br />
circulatory overload/hypnonatremia/<br />
hypoosmolality, 370<br />
coagulopathy, 371<br />
future of, 372<br />
glycine/ammonia toxicity, 370–371<br />
hypothermia, 371<br />
signs/symptoms of, 369<br />
transient bacteremia/septicemia, 371<br />
treatment of, 372<br />
Transurethral resection, 372<br />
Treatment futility, 47–48<br />
Treatment/prevention, 126<br />
Treatment redirection, 48<br />
TRICC. See Transfusion Requirements<br />
in Critical Care<br />
Tricyclic antidepressants, 199, 315<br />
Trimethoprim-sulfamethazine, 297<br />
Tubular function, 101–102<br />
TURP. See Transurethral prostatectomy<br />
U<br />
Ubiquitin, 114<br />
Ulcers<br />
diabetic foot, 165–166<br />
multidisciplinary approach for<br />
treating, 168–173<br />
summary of current usage, 169<br />
pressure, 166, 173–174<br />
venous, 166–167<br />
Upper airway dysfunction, 155<br />
Urinary concentration, 297–298<br />
Urinary tract infections, 72<br />
Urologic procedures, 368–375<br />
V<br />
Vagal activity, 143<br />
Valvular heart disease, 391–393<br />
Variable elements, 7–8<br />
Vascular procedures, 398–411<br />
cardiac risk assessment/intervention,<br />
398–401<br />
intraoperative management, 404–410<br />
carotid endarterectomy, 409–410<br />
carotid stents, 410<br />
endovascular abdominal aortic<br />
aneurysm repair, 408–409<br />
epidural anesthesia/regional<br />
techniques, 404–405<br />
general anesthesia for vascular<br />
patient, 404–405<br />
infraaortic vascular procedures,<br />
406<br />
postoperative care, 410–411<br />
optimization strategies, 401–404<br />
alpha agonists, 401<br />
beta-blocker therapy, 401<br />
cognitive function/delirium, 404<br />
preoperative assessment, 402–403<br />
renal, 403–404<br />
statins, 402<br />
preoperative evaluation/preparation,<br />
398<br />
Vascular resistance, 250<br />
Vascular stiffening, 141<br />
Vasoconstriction, 109, 110, 111, 143<br />
Vasodilation, 109<br />
Vasomotor tone, 284<br />
VC. See Vital capacity<br />
Vecuronium, 271<br />
Venous reflux disease, 167<br />
Venous thromboembolism, 360–362<br />
Venous ulcers, 166–167<br />
Ventilation<br />
alveolar, 249<br />
maximal minute, 67<br />
mechanical, 159–160<br />
noninvasive positive pressure, 159<br />
Ventilatory response, 67<br />
Video-assisted thoracoscopy (VAT), 378<br />
Virtue ethics, 39<br />
Visceral hypersensitivity, 310<br />
Visceral pain, 310<br />
Visual acuity, 12<br />
Vital capacity (VC), 150<br />
Volatile anesthetic agents, 256<br />
Volume depletion, 187<br />
Voluntariness, 42<br />
W<br />
Warfarin, 204–205<br />
Water-soluble drugs, 69<br />
Wound and compression therapy, 172<br />
Wound bed preparation, 171–172<br />
Wound healing, 170<br />
Z<br />
Zygapophyseal joint, 316