The Official Publication of ITACCS - International Trauma ...
The Official Publication of ITACCS - International Trauma ...
The Official Publication of ITACCS - International Trauma ...
Create successful ePaper yourself
Turn your PDF publications into a flip-book with our unique Google optimized e-Paper software.
<strong>Trauma</strong>Care<br />
Volume 13 Number 2<br />
Spring 2003<br />
<strong>The</strong> <strong>Official</strong> <strong>Publication</strong> <strong>of</strong> <strong>ITACCS</strong><br />
<strong>International</strong> <strong>Trauma</strong> Care<br />
<strong>Trauma</strong>Care<br />
now available at<br />
www.<strong>ITACCS</strong>.com<br />
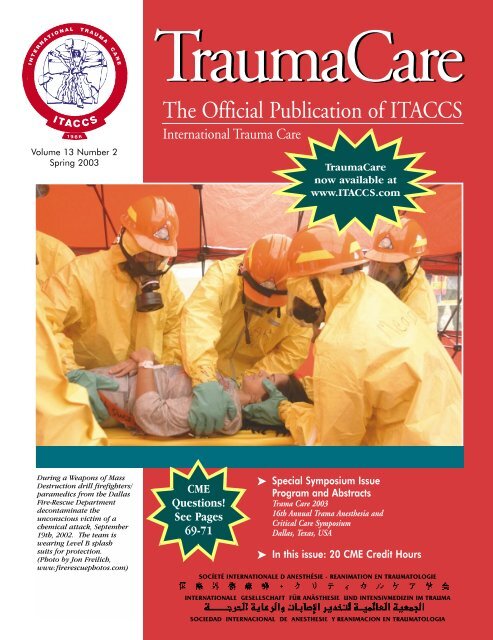
During a Weapons <strong>of</strong> Mass<br />
Destruction drill firefighters/<br />
paramedics from the Dallas<br />
Fire-Rescue Department<br />
decontaminate the<br />
unconscious victim <strong>of</strong> a<br />
chemical attack, September<br />
19th, 2002. <strong>The</strong> team is<br />
wearing Level B splash<br />
suits for protection.<br />
(Photo by Jon Freilich,<br />
www.firerescuephotos.com)<br />
CME<br />
Questions!<br />
See Pages<br />
69-71<br />
➤ Special Symposium Issue<br />
Program and Abstracts<br />
Trama Care 2003<br />
16th Annual Trama Anesthesia and<br />
Critical Care Symposium<br />
Dallas, Texas, USA<br />
➤ In this issue: 20 CME Credit Hours<br />
SOCÍETÉ INTERNATIONALE D ANESTHÉSIE - REANIMATION EN TRAUMATOLOGIE<br />
INTERNATIONALE GESELLSCHAFT FÜR ANÄSTHESIE UND INTENSIVMEDIZIN IM TRAUMA<br />
SOCIEDAD INTERNACIONAL DE ANESTHESIE Y REANIMACION EN TRAUMATOLOGIA
PRESIDENT’S MESSAGE<br />
<strong>Trauma</strong>Care<br />
33 • <strong>Trauma</strong> Care in Times <strong>of</strong> Trouble<br />
Michael J.A. Parr, MB BS MRCP FRCA<br />
FANZCA FJFICM<br />
33 • Special Message From the<br />
U.S. Surgeon General<br />
Richard Carmona, MD, MPH, FACS<br />
PROGRAM<br />
35 • Schedule for 16th ATACCS<br />
ABSTRACTS<br />
39 • Opening Plenary Session<br />
39 • Presidents’ Forum<br />
41 • Thursday Afternoon Sessions<br />
Session A: New Dimensions in <strong>Trauma</strong><br />
and Critical Care<br />
Session B: Disaster Medicine and<br />
Emergency Medicine<br />
Session C: Scientific Free Paper<br />
Presentations<br />
<strong>The</strong> <strong>Official</strong> <strong>Publication</strong> <strong>of</strong> <strong>ITACCS</strong><br />
<strong>International</strong> <strong>Trauma</strong> Care<br />
47 • Friday Morning Sessions<br />
Session A: <strong>Trauma</strong> Airway Management<br />
Session B: Critical Care in the Age<br />
<strong>of</strong> Terrorism<br />
Session C: <strong>Trauma</strong> Education,<br />
Simulation, and Patient Safety<br />
52 • Friday Afternoon Sessions<br />
Session A: Update on New Drugs,<br />
Equipment, and Techniques in<br />
<strong>Trauma</strong> Care<br />
Session B: Ethics: Organ Donation, End<br />
<strong>of</strong> Life Issues<br />
Session C: <strong>Trauma</strong> Airway Management:<br />
Hands-On Skills Station<br />
56 • Saturday Morning Sessions<br />
Session A: Pediatrics<br />
Session B: Prehospital Care<br />
Session C: CRNA Session<br />
65 • Sponsors and Exhibitors<br />
CME QUESTIONS<br />
69 • 35 Questions for 20 Credit Hours in<br />
AMA Category 1<br />
<strong>Publication</strong> Date: May 2003<br />
Credit Expiration Date: May 31, 2004<br />
CONTENTS<br />
Copyright 2003 © by the <strong>International</strong><br />
<strong>Trauma</strong> Anesthesia and Critical Care Society<br />
ISSN 1094-1126<br />
Co-Editors-in-Chief<br />
Adolph H. Giesecke, MD<br />
Department <strong>of</strong> Anesthesiology<br />
UT Southwestern Medical Center<br />
Dallas, TX 75390-9068 USA<br />
Tel: 214-590-7254; Fax: 214-590-6945<br />
e-mail: Adolph.Giesecke@UTSouthwestern.edu<br />
John K. Stene, MD, PhD<br />
Department <strong>of</strong> Anesthesiology<br />
Milton S. Hershey Medical Center<br />
Hershey, PA 17033 USA<br />
Tel: 717-531-8434; Fax: 717-531-4110<br />
e-mail: jstene@psu.edu<br />
Managing Editor<br />
Linda J. Kesselring, MS, ELS<br />
<strong>ITACCS</strong><br />
P.O. Box 4826<br />
Baltimore, MD 21211 USA<br />
Tel: 410-328-7449; Fax: 410-328-3699<br />
e-mail: lkessel112@aol.com<br />
Guidelines for Authors available at<br />
www.itaccs.com<br />
Send address changes and general<br />
inquiries to <strong>Trauma</strong>CareMail@aol.com<br />
<strong>ITACCS</strong> World Headquarters<br />
P.O. Box 4826, Baltimore, MD 21211 USA<br />
Fax: 410-235-8084 • www.<strong>ITACCS</strong>.com<br />
<strong>The</strong> opinions expressed in <strong>Trauma</strong>Care<br />
are those <strong>of</strong> the authors and not necessarily<br />
those <strong>of</strong> <strong>ITACCS</strong>.<br />
<strong>The</strong> drug and dosage information presented<br />
in this publication is believed to be<br />
accurate. However, the reader is urged to<br />
consult the full prescribing information on<br />
any product mentioned in this publication<br />
for recommended dosage, indications,<br />
contraindications, warning, precautions,<br />
and adverse effects. This is particularly<br />
important for drugs that are new or prescribed<br />
infrequently.<br />
Volume 13 Number 2 Spring 2003<br />
BOARD OF DIRECTORS<br />
PRESIDENT<br />
Michael J. A. Parr, MB, BS, MRCP, FRCA, FANZCA, FJFICM<br />
VICE PRESIDENTS<br />
Walter Mauritz, MD, PhD<br />
Jorge G. Plaza, MD<br />
EXECUTIVE DIRECTOR<br />
Christopher M. Grande, MD, MPH<br />
ASSOCIATE EXECUTIVE DIRECTOR<br />
James G. Cain, MD<br />
GENERAL MEMBERS<br />
Jeffrey M. Berman, MD<br />
Pierre A. Carli, MD<br />
Yves Lambert, MD<br />
Freddy Lippert, MD<br />
Jerry P. Nolan, MB, BS FRCA<br />
Eldar Soreide, MD<br />
Keiichi Tanaka, MD, PhD<br />
PAST PRESIDENTS<br />
Enrico M. Camporesi, MD<br />
Elizabeth A.M. Frost, MD<br />
Peter J. F. Baskett, MB, BCh, FRCA, MRCP<br />
John K. Stene, MD, PhD<br />
Adolph H. Giesecke, MD<br />
COMMITTEE CHAIRPERSONS<br />
EDUCATION AND TRAINING<br />
James G. Cain, MD<br />
Christopher M. Grande, MD, MPH<br />
RESEARCH: <strong>Trauma</strong> and Resuscitation <strong>International</strong><br />
Group for Experimentation and Research (TRIGER)<br />
Steering Committee:<br />
James G. Cain, MD<br />
Christopher M. Grande, MD, MPH<br />
Lewis J. Kaplan, MD<br />
Charles E. Smith, MD<br />
JOURNAL: TRAUMACARE<br />
Adolph H. Giesecke, MD (Co-Editor)<br />
John K. Stene, MD, PhD (Co-Editor)<br />
DISASTER/MASS CASUALTY<br />
Andreas Thierbach, MD<br />
PEDIATRIC TRAUMA<br />
Calvin Johnson, MD<br />
PREHOSPITAL/EMS<br />
Charles Deakin, MD<br />
CRITICAL CARE<br />
Maureen McCunn, MD<br />
SPECIAL EQUIPMENT/TECHNIQUES<br />
Charles E. Smith, MD, FRCPC<br />
FINANCE OF TRAUMA CARE<br />
Anne J. Sutcliffe, MB, BCh, FRCA<br />
PAIN MANAGEMENT/REGIONAL ANESTHESIA<br />
Andrew D. Rosenberg, MD<br />
TOXIC TRAUMA/HAZMAT<br />
David J. Baker, M. Phil, DM FRCA<br />
MILITARY TRAUMA<br />
Matthias Helm, MD<br />
TRAUMA SURGERY<br />
Lewis J. Kaplan, MD, FACS<br />
EMERGENCY MEDICINE<br />
Dario Gonzalez, MD, FACEP<br />
CRNA<br />
Charles R. Barton, CRNA, MEd<br />
RESPIRATORY THERAPIST<br />
Rusty Reid, RRT<br />
OPERATIONAL PROJECTS<br />
DEVELOPING NATIONS PROGRAM (DNP)<br />
Christopher M. Grande, MD, MPH<br />
COMPREHENSIVE APPROACH TO TRAUMATOLOGY (CAT)<br />
Peter J. F. Baskett, MB, BCh, FRCA, MRCP<br />
TRAUMA/EMS TERMINOLOGY<br />
Wolfgang F. Dick, MD, PhD<br />
JOURNAL: TRAUMACARE<br />
Linda J. Kesselring, MS, ELS, Managing Editor<br />
REFRESHER COURSES/WORKSHOPS<br />
Paul Hilliard, CRNA, Manager<br />
SPECIAL AD HOC ADVISORS<br />
Bruce F. Cullen, MD<br />
Robert L. Fila, Esq.<br />
Ake N. A. Grenvik, MD, PhD<br />
Douglas G. Hicks, CPA<br />
Irene H. Impellizzeri, PhD<br />
John D. Lupiano, MD, MPH<br />
Peter Safar, MD<br />
31
THE INTERNATIONAL TRAUMA<br />
ANESTHESIA & CRITICAL CARE SOCIETY<br />
PRESENTS<br />
2003-2004 Special CME Courses:<br />
TRAUMA: <strong>The</strong> Team Approach<br />
To <strong>The</strong> Clinical Challenge<br />
While each program title is the same, the content varies.<br />
Request the individual brochure for complete details.<br />
June 15-20, 2003<br />
Grand Tetons National Park, WY<br />
July 21-24, 2003<br />
Hilton Head South Carolina<br />
August 7-10, 2003<br />
Seattle, Washington<br />
August 3-15, 2003<br />
European Cruise: London>Oslo>Arhus<br />
Warnemunde>Gotland > Tallin> St.<br />
Petersburg>Helsinki>Stockholm >Copenhagen<br />
2003<br />
August 23-30, 2003 Alaska Cruise<br />
Seattle>Ketchikan>Juneau>Sitka>Glac<br />
ier Bay>Victoria> Seattle<br />
September 6-10, 2003<br />
Yosemite National Park, California<br />
September 23-26, 2003<br />
Las Vegas, Nevada<br />
October 7-14, 2003 Fall Foliage Cruise<br />
NYC>Newport, RI> Boston, MA>Bar<br />
Harbor, ME>Halifax, NS> Sydney, NS><br />
Charlottetown, PEI >Quebec City><br />
Montreal, Canada<br />
2004<br />
(Preliminary Schedule)<br />
October 19-24, 2003<br />
Bonaire Island<br />
November 2-7, 2003<br />
Puerto Vallarta, MX<br />
November 20-23, 2003<br />
Key West, Florida<br />
December 1-5, 2003<br />
St Thomas, Virgin Islands<br />
February 15-22, 2004<br />
Western Caribbean Cruise<br />
February 22-27, 2004<br />
Punta Cana, Dominican Republic<br />
March 1-4, 2004<br />
Whistler, BC, Canada<br />
April 25-30, 2004<br />
Cozumel, Mexico<br />
June 10-13, 2004<br />
Boston, MA<br />
June 16-20, 2004<br />
Longboat Key, FL<br />
July 12-15, 2004<br />
Cape Cod, MA<br />
August 15-22<br />
Alaska Cruise<br />
September 5-10, 2004<br />
Las Vegas, NV<br />
November 1-11, 2004<br />
Rome to Barcelona Cruise<br />
November 7-12, 2004<br />
Turks & Caicos, BWI<br />
December 5-10, 2004<br />
Aruba<br />
for Additional Information Visit Our Web Site www.nwas.com/itaccs email info@nwas.com<br />
POB 2797, Pasco, WA. USA 99302<br />
PH (509) 547-7065, (800) 222-6927; FAX (509) 547-1265
<strong>ITACCS</strong> Spring 2003<br />
PRESIDENT’S MESSAGE<br />
<strong>Trauma</strong> Care in Times <strong>of</strong> Trouble<br />
Michael J.A. Parr, MB BS MRCP FRCA<br />
FANZCA FJFICM<br />
President, <strong>International</strong> <strong>Trauma</strong> Care<br />
Intensive Care Specialist<br />
University <strong>of</strong> New South Wales<br />
Locked Bag 7103<br />
Sydney NSW 1871<br />
m.parr@unsw.edu.au<br />
Despite a war, threats <strong>of</strong> terrorism, and an epidemic <strong>of</strong> a<br />
new viral severe acute respiratory syndrome (SARS),<br />
<strong>Trauma</strong>Care 2003 will come to fruition in Dallas on May 15th.<br />
Dedicated heathcare workers involved in the management <strong>of</strong><br />
trauma patients in many nations will meet to discuss and hear<br />
<strong>of</strong> advances in the management <strong>of</strong> trauma victims. <strong>The</strong> educational<br />
benefit from these interactions is enormous and translates<br />
to a potential benefit for future patients. <strong>The</strong> value <strong>of</strong> the<br />
multidisciplinary and international input for <strong>Trauma</strong>Care 2003<br />
should not be underestimated. Given the relative lack <strong>of</strong> high<br />
quality scientific research in the field <strong>of</strong> trauma, it is not surprising<br />
that we rely on the consensus <strong>of</strong> the multidisciplinary<br />
approach seen at <strong>Trauma</strong>Care meetings.<br />
So many questions in relation to trauma management<br />
remain to be answered or studied in an objective scientific<br />
manner that allows critical assessment. <strong>The</strong> enthusiasm <strong>of</strong> the<br />
delegates and their commitment to improving trauma care will<br />
continue to drive this area <strong>of</strong> medical science. <strong>ITACCS</strong> is committed<br />
to improved trauma research in the future. <strong>Trauma</strong> has<br />
long been the “poor cousin” in terms <strong>of</strong> attracting research<br />
interest. Perhaps clinicians are too busy looking after patients<br />
to apply time to critical assessment and study <strong>of</strong> what really<br />
makes a difference. Perhaps the healthcare industry has not<br />
seen the potential benefits <strong>of</strong> innovation and advances in trauma<br />
management. This needs to change. Increasingly we recognize<br />
that the end result for a trauma victim may only be as<br />
good as the quality <strong>of</strong> care received at any stage <strong>of</strong> the trauma<br />
management process. <strong>The</strong> complexities and impacts <strong>of</strong> prehospital<br />
resuscitation, in-hospital trauma resuscitation, definitive<br />
care, intensive care, and rehabilitation are only too clear for<br />
those <strong>of</strong> us involved in managing these patients.<br />
During <strong>Trauma</strong>Care 2003 we will hear about innovations<br />
in trauma practice as diverse as alternatives for fluid management,<br />
prehospital ventilation management, control <strong>of</strong> coagulopathy,<br />
and optimizing sedation and minimizing complications<br />
in the ICU. <strong>The</strong>re will be a significant focus on less conventional<br />
forms <strong>of</strong> trauma, including terrorism and weapons <strong>of</strong><br />
mass destruction. <strong>The</strong>re will be interactive hands-on sessions<br />
and ample time to discuss presentations and topics with presenters.<br />
<strong>The</strong> Dallas meeting will pave the way and see the presentation<br />
<strong>of</strong> the plan for <strong>Trauma</strong>Care 2004 in Sydney, Australia,<br />
where we will meet to continue to improve the care <strong>of</strong> trauma<br />
patients across all nations. <strong>The</strong> Sydney meeting will realize<br />
many innovations for <strong>ITACCS</strong> that are currently in preparation.<br />
Details can be found at www.traumacare2004.com and via the<br />
recently updated www.<strong>ITACCS</strong>.com. We will proceed, as<br />
always; through collaboration, good communication, mutual<br />
respect, and dedication to a goal that is realistic. <strong>The</strong>se <strong>ITACCS</strong><br />
meetings and other initiatives will hopefully generate renewed<br />
and revitalized interest in driving improved trauma patient<br />
care. <strong>The</strong> politicians will not drive this and we need to.<br />
Special Message from the Surgeon<br />
General <strong>of</strong> the United States<br />
Richard Carmona, MD, MPH, FACS<br />
On the occasion <strong>of</strong> this educational<br />
meeting, I wish to extend well wishes to this<br />
important gathering <strong>of</strong> trauma care experts,<br />
and indeed to the greater community <strong>of</strong><br />
trauma care providers worldwide.<br />
In the context <strong>of</strong> current events, the care<br />
<strong>of</strong> the injured has assumed even greater importance.<br />
Throughout most <strong>of</strong> my adult life, I have had a close personal<br />
experience with the various dimensions <strong>of</strong> trauma: first, in the<br />
Vietnam War, serving as part <strong>of</strong> the U.S. Army Special Forces,<br />
and then, after returning home, as a paramedic, registered<br />
nurse, physician’s assistant, and police <strong>of</strong>ficer. Subsequently,<br />
after graduating medical school and completing residency<br />
training in surgery and a trauma fellowship, I chose to focus<br />
my practice on the care <strong>of</strong> trauma patients, while maintaining<br />
an active interest in practical field applications as a member <strong>of</strong><br />
the PIMA County Sheriff ’s Department SWAT team (<strong>of</strong> which I<br />
was a team leader). <strong>The</strong>se varied experiences have given me a<br />
unique perspective, having been one <strong>of</strong> the injured in several<br />
instances, and providing care for the wounded in others. In<br />
fact, the topic <strong>of</strong> tactical medicine has been one focus <strong>of</strong> my<br />
medical career and the subject <strong>of</strong> many <strong>of</strong> my published works.<br />
From the standpoint <strong>of</strong> “conventional” trauma, great<br />
strides have been made in the public health aspects <strong>of</strong> care <strong>of</strong><br />
the injured, with improvements in traffic/road safety, automobile<br />
design, and other injury prevention systems, leading to<br />
increased survivability from crashes. At the same time,<br />
upgrades in training, equipment, and emergency medical systems<br />
have enabled more <strong>of</strong> the injured to receive better prehospital<br />
care sooner, and arrive at the trauma center alive.<br />
This, in turn, has presented ever greater challenges to trauma<br />
teams receiving these patients. Thus, from this vantage point,<br />
educational and scientific initiatives such as this are <strong>of</strong> critical<br />
importance in pushing back the barriers to improved trauma<br />
care for all injured patients, and raising the standard <strong>of</strong> care,<br />
not only in the United States, but around the world.<br />
More recently, lesser known “unconventional” types <strong>of</strong><br />
trauma have come to the forefront. <strong>The</strong> concept <strong>of</strong> mass casualty<br />
management has long been a subject <strong>of</strong> discussion and<br />
study, and an area <strong>of</strong> specialization for some trauma care pr<strong>of</strong>essionals;<br />
but previously these incidents dealt with situations<br />
such as war, natural disasters, industrial mishaps, and spectator<br />
events. <strong>The</strong> new realities brought to us by the surge in<br />
international terrorism, and the pr<strong>of</strong>ound threats now represented<br />
by “weapons <strong>of</strong> mass destruction” (WMD), encompassing<br />
various biological and chemical agents, gives new meaning<br />
to the concept. Educational programs that further the understanding<br />
<strong>of</strong> terrorism, weapons <strong>of</strong> mass destruction and prevention,<br />
preparedness, and response are much needed for all<br />
health-related disciplines. Our new world order demands that<br />
we be prepared for “all hazards” we may face.<br />
At the Department <strong>of</strong> Health and Human Services, we are<br />
and have been engaged in numerous clinical and basic science<br />
endeavors to prevent trauma as well as improve care for the<br />
trauma patient.<br />
In closing, I salute trauma care providers and their continued<br />
dedication to the management <strong>of</strong> the injured. I also recognize<br />
the important work <strong>of</strong> many pr<strong>of</strong>essional organizations,<br />
and encourage all <strong>of</strong> you to continue to improve the<br />
care <strong>of</strong> trauma patients across the globe.<br />
33
A joint meeting between THE AUSTRALASIAN TRAUMA SOCIETY<br />
(ATS) AND TRAUMA CARE INTERNATIONAL (<strong>ITACCS</strong>)<br />
SYDNEY CONVENTION & EXHIBITION CENTRE, DARLING HARBOUR, SYDNEY, AUSTRALIA 15-17 OCTOBER, 2004<br />
<strong>The</strong> premier trauma meeting for 2004 for all disciplines involved in trauma care from pre-hospital setting through to rehabilitation.<br />
• Paramedics • Intensive care nurses & physicians • Operating department assistants<br />
• Pre-hospital physicians & nurses • Rehabilitation physicians & nurses • Surgeons, theatre nurses & ward nurses<br />
• Emergency physicians & nurses • Physiotherapists • Hospital administrators<br />
• Anaesthetics & nurse anaesthetists • Medical & nursing students<br />
Plenary sessions on state <strong>of</strong> the art trauma care and concurrent sessions featuring – ‘Update’ and ‘Guideline’ sessions, <strong>Trauma</strong> Master<br />
classes with panel discussions and ‘Pro:Con’ debates. With emphasis on:<br />
• Pre-hospital trauma care • Management <strong>of</strong> biological & chemical • Technological advances in trauma care<br />
• Principles <strong>of</strong> intensive care for weapon injuries • Paediatric trauma<br />
major trauma • Reducing complications for trauma • <strong>Trauma</strong> rehabilitation<br />
• Initial resuscitation for major trauma patients • Blast injuries<br />
• Resuscitative surgery• <strong>International</strong> perspectives<br />
• Resuscitative anaesthesia for major trauma • Neurotrauma<br />
Workshops on:<br />
• <strong>Trauma</strong> simulation • <strong>Trauma</strong> audit as a learning tool • Difficult airway management<br />
• FAST<br />
• Organ donation<br />
Please send me further details on:<br />
■ Abstract submissions<br />
■ Registration document – including provisional program & costs<br />
■ Sponsorship & trade exhibition opportunities<br />
Name: _____________________________________________________________________________________________<br />
Position: ________________________________________ Organisation: __________________________________________<br />
Organisation Address: __________________________________________________________________________________<br />
Suburb: _________________________ State: _________________ Country: ___________________ Postcode: ___________<br />
Telephone: ( ) ____________________________________ Facsimile: ( ) ____________________________________<br />
Email: _____________________________________________________________________________________________<br />
<strong>Trauma</strong>Care 2004 Secretariat, Conference Action Pty Ltd, PO Box 576, Crows Nest, NSW, 1585, AUSTRALIA<br />
Tel: +61 2 9437 9333 Fax: +61 2 9901 4586 Email: confact@conferenceaction.com.au Website: www.traumacare2004.com
<strong>ITACCS</strong> Spring 2003<br />
PROGRAM<br />
<strong>Trauma</strong>Care 2003 16th Annual <strong>Trauma</strong> Anesthesia and Critical Care Symposium<br />
DALLAS, TEXAS, USA<br />
Dallas skyline. (Photo courtesy <strong>of</strong> Dallas Convention and Visitors Bureau.)<br />
Thursday, May 15, 2003<br />
COMMITTEE MEETINGS (by invitation only)<br />
0630–0745 <strong>Trauma</strong>Care Editorial Board Meeting, Bel-Air Room I<br />
Chairs: Adolph H. Giesecke, MD, and John K. Stene, MD, PhD<br />
0700–0745 Disaster/Mass Casualty Committee, Bel-Air Room VI<br />
Chair: Andreas Thierbach, MD<br />
0700–1200 Registration, Garden Court III<br />
0700–0800 Continental Breakfast, Garden Court III<br />
OPENING PLENARY SESSION, Malachite Showroom<br />
0800 Welcome<br />
Christopher Grande, MD, MPH, Executive Director, <strong>ITACCS</strong><br />
Co-Chair, <strong>Trauma</strong>Care 2003 Program<br />
0805 Introductions<br />
James G. Cain, MD, Associate Executive Director, <strong>ITACCS</strong><br />
Co-Chair, <strong>Trauma</strong>Care 2003 Program<br />
0810–0845 JFK in Dallas, A <strong>Trauma</strong> Care Prospective<br />
Adolph H. Giesecke, MD, University <strong>of</strong> Texas Southwestern<br />
Medical Center, Dallas, Texas, USA<br />
PRESIDENTS’ FORUM, Malachite Showroom<br />
0845–0915 President’s Address: What’s New in <strong>Trauma</strong><br />
Michael J.A. Parr, MB BS MRCP FRCA FANZCA FJFICM<br />
University <strong>of</strong> New South Wales, Sydney, NSW<br />
0915–1000 Break, Garden Court III<br />
Exhibits Open<br />
0915–1000 TRAUMA: Resuscitation, Anesthesia, Surgery, &<br />
Critical Care (book edited by W.C. Wilson, C.M. Grande,<br />
D.B. Hoyt). Dr. Wilson will be available to answer<br />
contributors’ questions.<br />
1000–1030 Applications <strong>of</strong> Dexmedetomidine in the <strong>Trauma</strong> Patient<br />
Michael A. E. Ramsay, MD, FRCA<br />
Baylor University Medical Center, Dallas, Texas, USA<br />
1030–1100 Stress Management for Care Providers<br />
in the <strong>Trauma</strong> Setting<br />
Jessie A. Leak, MD, University <strong>of</strong> Texas, MD Anderson<br />
Cancer Center, Houston, Texas<br />
1100–1130 Emergency Ventilatory Management <strong>of</strong> the Trama<br />
Patient: Elemental or Detrimental?<br />
Paul E. Pepe, MD, MPH, UT Southwestern Medical Center,<br />
Dallas, Texas, USA<br />
1130–1200 Fluid Management in <strong>Trauma</strong><br />
Richard P. Dutton, MD, R Adams Cowley Shock <strong>Trauma</strong><br />
Center, Baltimore, Maryland, USA<br />
1200–1315 Lunch (on your own)<br />
Thursday, May 15, 2003<br />
1300–1700 Registration, Garden Court III<br />
SIMULTANEOUS AFTERNOON SESSIONS (1315–1715)<br />
SESSION A<br />
New Dimensions in <strong>Trauma</strong><br />
and Critical Care, Bel-Air Room I-III<br />
Co-Chair: James G. Cain, MD<br />
Co-Chair: Christopher M. Grande, MD, MPH<br />
1315–1345 Sedation for the Critically Injured <strong>Trauma</strong><br />
Patient: Precedex®, a Novel Alternative<br />
James Gordon Cain, MD<br />
Allegheny General Hospital, Pittsburgh, Pennsylvania, USA<br />
West Virginia University, Morgantown, West Virginia, USA<br />
1345–1415 <strong>The</strong> Hazards <strong>of</strong> Nutraceuticals in the<br />
Management <strong>of</strong> the <strong>Trauma</strong> Patient<br />
Jessie A. Leak, MD, University <strong>of</strong> Texas, MD Anderson<br />
Cancer Center, Houston, Texas<br />
1415–1445 Controversies in Blunt Aortic <strong>Trauma</strong><br />
Charles E. Smith, MD, FRCPC<br />
MetroHealth Medical Center, Cleveland, Ohio, USA<br />
1445–1515 Beverage Break, Garden Court III<br />
35
<strong>ITACCS</strong> Spring 2003<br />
1445–1515 TRAUMA: Resuscitation, Anesthesia, Surgery, &<br />
Critical Care (book edited by W.C. Wilson, C.M. Grande,<br />
D.B. Hoyt). Dr. Wilson will be available in the Malachite<br />
Board Room to answer contributors’ questions.<br />
1515–1545 What’s New in Neurotrauma<br />
Anne J. Sutcliffe, MB ChB, FRCA, Queen Elizabeth Hospital<br />
and University <strong>of</strong> Birmingham, Birmingham, UK<br />
1545–1615 Pathophysiological Processes Following Toxic <strong>Trauma</strong><br />
David J. Baker, DM, FRCA, University <strong>of</strong> Paris, Paris, France<br />
1615–1645 End Tidal CO2: From Airway to Cardiac Output<br />
Marvin A. Wayne, MD, FACEP<br />
University <strong>of</strong> Washington and Emergency<br />
Medical Services, Bellingham, Washington, USA<br />
1645–1715 A New Approach to Monitoring Early<br />
Hemodynamic Performance: Transesophageal<br />
Echo Doppler Ultrasound<br />
Yves Lambert, MD<br />
Versailles Hospital, Le Chesnay, France<br />
SESSION B<br />
Disaster Medicine and Emergency Medicine<br />
Bel-Air Room IV-VI<br />
Co-Chair: Dario Gonzalez, MD, New York, New York, USA<br />
Co-Chair: Andreas Thierbach, MD, Mainz, Germany<br />
1315–1345 <strong>International</strong> Chief Emergency<br />
Physician Training Course<br />
Freddy Lippert, MD, Rigshospitalet, Copenhagen<br />
University Hospital, Copenhagen, Denmark<br />
1345–1415 <strong>The</strong> Effect <strong>of</strong> Select Drugs on the<br />
Presentation <strong>of</strong> Shock in the <strong>Trauma</strong> Patient<br />
Joanne Williams, MD, FAAEM, FACFM<br />
Martin Luther King, Jr./Charles R. Drew<br />
Medical Center, Los Angeles, California, USA<br />
1415–1445 Lessons Learned 911<br />
Dario Gonzalez, MD, FACEP, Office <strong>of</strong> Emergency<br />
Management, City <strong>of</strong> New York, and Albert Einstein<br />
College <strong>of</strong> Medicine, New York, New York, USA<br />
1445–1515 Beverage Break, Garden Court III<br />
1445–1515 TRAUMA: Resuscitation, Anesthesia, Surgery, &<br />
Critical Care (book edited by W.C. Wilson, C.M. Grande,<br />
D.B. Hoyt). Dr. Wilson will be available in the Malachite<br />
Board Room to answer contributors’ questions.<br />
1515–1545 Organization <strong>of</strong> Medical Systems Under<br />
Repeat Terror Attacks<br />
Eran Tal-Or, MD, Rambam Medical Center, Haifa, Israel<br />
1545–1615 Triage: Do We Need New Concepts?<br />
Kristi Koenig, MD, FACEP, George Washington University<br />
School <strong>of</strong> Medicine and Health Sciences; National<br />
Director, Emergency Management Strategic Healthcare<br />
Group Department <strong>of</strong> Veterans Affairs, Martinsburg,<br />
West Virginia, USA<br />
1615–1645 Databases for Storing Prehospital and<br />
Intrahospital Data<br />
Dr. Peter A. Oakley, North Staffordshire Hospital,<br />
Stoke-on-Trent, UK<br />
1645–1715 Panel Discussion<br />
SESSION C<br />
Scientific Free Paper Presentations, Le Gala Room<br />
Moderators: Enrico Camporesi, MD, SUNY Health Science<br />
Center, Syracuse, New York, USA; Adolph Giesecke, MD, UT<br />
Southwestern Medical Center, Dallas, Texas, USA; John<br />
Stene, MD, PhD, Hershey Medical Center, Hershey,<br />
Pennsylvania, USA<br />
1315–1445 Scientific Presentations<br />
1445–1515 Beverage Break<br />
1515–1715 Scientific Presentations<br />
1800-2000 Board <strong>of</strong> Directors Meeting and<br />
Faculty Dinner, Mayfair Room<br />
Friday, May 16, 2003<br />
COMMITTEE MEETING (by invitation only)<br />
0630–0745 Critical Care Committee Meeting, Baccarat Room<br />
Chair: Maureen McCunn, MD<br />
0700–0800 Continental Breakfast, Garden View III<br />
0700–1200 Registration, Garden View III<br />
0700–1200 Exhibits Open, Garden View III<br />
SIMULTANEOUS MORNING SESSIONS (0800–1200)<br />
SESSION A<br />
<strong>Trauma</strong> Airway Management, Bel-Air Room I-III<br />
Chair: Andreas Thierbach, MD, Mainz, Germany<br />
0800–0830 <strong>The</strong> ASA Difficult Airway Algorithm as<br />
It Pertains to <strong>Trauma</strong> Patients<br />
William Charles Wilson, MD<br />
University <strong>of</strong> California,<br />
San Diego School <strong>of</strong> Medicine,<br />
San Diego, California, USA<br />
0830–0900 Controversies and Obstacles to Airway Training for<br />
Paramedics: What Are the Options?<br />
Adolph H. Giesecke, MD<br />
University <strong>of</strong> Texas Southwestern Medical School, Dallas,<br />
Texas, USA<br />
0900–0930 Airway Management with Penetrating Neck <strong>Trauma</strong><br />
Vance E. Shearer, MD, University <strong>of</strong> Texas Southwest<br />
Medical Center, Dallas, Texas, USA<br />
0930–1000 Beverage Break, Exhibit Hall, Garden Court III<br />
Exhibits Open<br />
1000–1030 <strong>The</strong> Difficult Airway and Failed Intubation<br />
Jeffrey M. Berman, MD, University <strong>of</strong> North Carolina,<br />
Chapel Hill, North Carolina, USA<br />
1030–1100 <strong>The</strong> Role <strong>of</strong> the Combitube and the EasyTube (EzT)<br />
Andreas R. Thierbach, MD<br />
University <strong>of</strong> Mainz, Mainz, Germany<br />
1100–1130 SLAM Emergency Airway Flowchart<br />
James M. Rich, MA, CRNA<br />
Baylor University Medical Center, Dallas, Texas, USA<br />
1130–1200 Flexible Fiberoptic Intubation<br />
Freddy Lippert, MD, Rigshospitalet, Copenhagen University<br />
Hospital, Copenhagen, Denmark<br />
SESSION B<br />
Critical Care in the Age <strong>of</strong> Terrorism,<br />
Bel-Air Room IV-VI<br />
Chair: Maureen McCunn, MD, R Adams Cowley Shock<br />
<strong>Trauma</strong> Center, Baltimore, Maryland<br />
0800–0830 <strong>Trauma</strong> Care Around the World: How We Are<br />
Different and How We Are the Same<br />
Maureen McCunn, MD, R Adams Cowley Shock <strong>Trauma</strong><br />
Center, Baltimore, Maryland, USA<br />
0830–0900 Wartime Civilian Injuries: An Epidemiological Shift<br />
in Terrorism and Complex Disasters<br />
Michel Badih Aboutanos, MD, MPH<br />
Medical College <strong>of</strong> Virginia, Richmond, Virginia, USA<br />
0900–0930 Suicide Bombings in Israel: Injuries Never Seen Before<br />
Itamar Ashkenazi, MD, and Ricardo Alfici, MD<br />
Hillel Yaffe Medical Center, Hadera, Israel<br />
0930–1000 Beverage Break, Exhibit Hall, Garden Court III<br />
Exhibits Open<br />
36
<strong>ITACCS</strong> Spring 2003<br />
1000–1030 Rapid Evacuation and Transport <strong>of</strong> the<br />
Critically Injured Patient<br />
William Beninati, MD, Air Force Coalition for<br />
Sustainment <strong>of</strong> <strong>Trauma</strong> and Readiness Skills (C-STARS)<br />
University <strong>of</strong> Maryland School <strong>of</strong> Medicine,<br />
Baltimore, Maryland, USA<br />
1030–1100 Organization <strong>of</strong> the Nurses Working with Terror<br />
Victims in the ED and the Wards<br />
Gila Hyams, RN, MA<br />
Rambam Medical Center, Haifa, Israel<br />
1100–1130 Damage Control Surgery: Principles <strong>of</strong> Care<br />
for Critical Injury<br />
Thomas M. Scalea, MD, R Adams Cowley Shock <strong>Trauma</strong><br />
Center, Baltimore, Maryland, USA<br />
1130–1200 Panel Discussion<br />
SESSION C<br />
<strong>Trauma</strong> Education, Simulation, and<br />
Patient Safety, Le Gala Room<br />
Co-Chair: James G. Cain, MD, Pittsburgh,<br />
Pennsylvania, USA<br />
Co-Chair: Michael J.A. Parr, MB BS MRCP FRCA FANZCA<br />
FJFICM, University <strong>of</strong> New South Wales, Sydney, NSW<br />
0800–0830 Human Crisis Simulation for Rural Medical Education<br />
James Gordon Cain, MD<br />
Allegheny General Hospital, Pittsburgh, Pennsylvania, USA<br />
West Virginia University, Morgantown, West Virginia, USA<br />
0830–0930 <strong>The</strong> Role <strong>of</strong> Microsimulators in Training<br />
<strong>Trauma</strong> Pr<strong>of</strong>essionals<br />
Ulrik Juul Christensen, MD<br />
Sophus Medical A/S, Copenhagen, Denmark<br />
0930–1000 Beverage Break, Exhibit Hall, Garden Court III<br />
Exhibits Open<br />
1000–1045 Rapid Preparation <strong>of</strong> Reserve Military Medical Teams<br />
Using Human Patient Simulation<br />
Guy Lin, MD, Israeli Defense Forces, West Galile, Israel<br />
1045–1130 Drills: Are <strong>The</strong>y the Best Way to Prepare for Mass<br />
Casualty Incidents?<br />
Moshe Michaelson, MD<br />
Techjion Haifa, Haife, Israel<br />
1130–1200 <strong>Trauma</strong> Education Through Audit: Simulation<br />
Session (Laerdal Equipment)<br />
Michael J.A. Parr, MRCP FRCA, James G. Cain, MD,<br />
James M. Rich, MA, CRNA<br />
1200–1345 Lunch, Exhibits Open<br />
1200–1245 Pediatric <strong>Trauma</strong> Committee Meeting, Malachite<br />
Board Room (by invitation only)<br />
Chair: Calvin Johnson, MD<br />
1215–1315 Exhibits Open, Garden View III<br />
SPECIAL LUNCHEON PRESENTATION: “Uncontrolled<br />
Hemorrhagic <strong>Trauma</strong>: Progressive Treatments to<br />
Manage Massive Bleeding”<br />
1215–1220 Opening Remarks<br />
W. Keith Hoots, MD<br />
1220–1240 Redefining the Coagulation Cascade<br />
W. Keith Hoots, MD, <strong>The</strong> University <strong>of</strong> Texas, M.D. Anderson<br />
Cancer Center, and the Gulf States Hemophilia and<br />
Thrombophilia Center, Houston, Texas<br />
1240–1300 Catastrophic <strong>Trauma</strong> and Massive Hemorrhage Care<br />
Richard P. Dutton, MD<br />
R Adams Cowley Shock <strong>Trauma</strong> Center, University <strong>of</strong><br />
Maryland Medical Systems, Baltimore, Maryland<br />
1300–1315 Questions and Answers<br />
1315–1345 Desserts and Beverage, Exhibit Hall<br />
Friday, May 16, 2003<br />
SIMULTANEOUS AFTERNOON SESSIONS (1345–1745)<br />
SESSION A<br />
Update on New Drugs, Equipment, and<br />
Techniques in <strong>Trauma</strong> Care, Bel-Air Room I-III<br />
Chair: Charles E. Smith, MD, Cleveland, Ohio, USA<br />
1345–1415 What’s New in Pulse Oximetry<br />
Steven J. Barker, PhD, MD<br />
University <strong>of</strong> Arizona, Tucson, Arizona, USA<br />
1415–1445 Capnography in Trama<br />
Steven J. Barker, PhD, MD<br />
University <strong>of</strong> Arizona, Tucson, Arizona, USA<br />
1445–1515 Neuromuscular Relaxant Pharmacology: An Update<br />
Charles E. Smith, MD<br />
MetroHealth Medical Center, Cleveland, Ohio, USA<br />
1515–1545 Break (Scientific Awards), Garden Court III<br />
Exhibits Open<br />
1545–1615 Acid-Base Balance in <strong>Trauma</strong> Resuscitation<br />
Lewis J. Kaplan, MD, FACS<br />
Yale University School <strong>of</strong> Medicine, New Haven,<br />
Connecticut, USA<br />
1615–1645 <strong>The</strong> Management <strong>of</strong> Massive Bleeds in <strong>Trauma</strong> by an<br />
Injury Site-Specific Agent (Recombinant Activated<br />
Factor VII)<br />
Uri Martinowitz, MD, Pr<strong>of</strong>.<br />
Sackler School <strong>of</strong> Medicine, Tel Aviv University, Tel<br />
Hashomer, Israel<br />
1645–1715 Damage Control Orthopedics<br />
James C. Duke, MD<br />
University <strong>of</strong> Colorado, Denver, Colorado, USA<br />
1715–1745 Emerging Pathogens: Practical and Evidenced-Based<br />
Interventions<br />
Lewis J. Kaplan, MD, FACS, Yale University School <strong>of</strong><br />
Medicine, New Haven, Connecticut, USA<br />
SESSION B<br />
Ethics: Organ Donation, End <strong>of</strong> Life Issues,<br />
Bel-Air Room IV-VI<br />
Chair: Anne J. Sutcliffe, MB ChB, FRCA, Queen Elizabeth<br />
Hospital and the University <strong>of</strong> Birmingham,<br />
Birmingham, UK<br />
1345–1415 Managing Death and Dying<br />
Anne J. Sutcliffe MB ChB, FRCA<br />
Queen Elizabeth Hospital and the University <strong>of</strong><br />
Birmingham, Birmingham, UK<br />
1415–1445 Diagnosing Brain Stem Death: After 30 Years<br />
Couldn’t We Do Better?<br />
Gerlinde Francisca Mandersloot, MB ChB, FRCA<br />
<strong>The</strong> Royal London Hospital, London, UK<br />
1445–1515 Improving Organ Donation Rates<br />
Walter Mauritz, Pr<strong>of</strong>., MD<br />
<strong>Trauma</strong> Hospital Lorenz Boehler, Vienna, Austria<br />
1515–1545 Break (Scientific Awards), Garden Court III<br />
1545–1615 Managing the Donor<br />
Linda E. Pelinka, MD<br />
Lorenz Boehler <strong>Trauma</strong> Center, Vienna, Austria<br />
1615–1645 Non-Heart-Beating Donors<br />
Maureen McCunn, MD<br />
R Adams Cowley Shock <strong>Trauma</strong> Center, Baltimore,<br />
Maryland, USA<br />
1645–1715 Living Donors<br />
Jane McNeill, MB ChB, FRCA<br />
<strong>The</strong> Royal London Hospital, London, UK<br />
1715–1745 Panel Discussion<br />
37
<strong>ITACCS</strong> Spring 2003<br />
SESSION C<br />
<strong>Trauma</strong> Airway Management: Hands-On Skills Station<br />
Le Gala Room<br />
Co-Chair: Andreas Thierbach, MD, Mainz, Germany<br />
Co-Chair: Jeffrey M. Berman, MD, Chapel Hill, North<br />
Carolina, USA<br />
Co-Chair: James M. Rich, MA, CRNA, Dallas, Texas, USA<br />
Co-Chair: Freddy Lippert, MD, Copenhagen, Denmark<br />
Co-Chair: Marvin Wayne, MD, Bellingham,<br />
Washington, USA<br />
Co-Chair: William C. Wilson, MD, San Diego,<br />
California, USA<br />
1345–1745 35 minutes at each station / 5 participants per station<br />
Laryngoscopes, blades, and intubation aids<br />
Bonfils and Bullard<br />
Flexible fiberoptic intubation<br />
Combitube, EasyTube, LT, LMA<br />
Surgical airway: cricothyrotomy<br />
Decision training (Airman, SimMan)<br />
King LT<br />
1745–1900 Glad-You-Joined-Us-in-Texas Reception,<br />
Garden Court III<br />
Saturday, May 17, 2003<br />
0700-0800 Continental Breakfast<br />
SIMULTANEOUS MORNING SESSIONS (0800–1200)<br />
SESSION A<br />
Pediatric <strong>Trauma</strong>, Bel-Air Room I-III<br />
Co-Chair: Gail E. Rasmussen, MD, Meridian, Mississippi, USA<br />
Co-Chair: Jeffrey M. Berman, MD, Chapel Hill, North<br />
Carolina, USA<br />
0800–0830 Emergency Airway Management in the Pediatric<br />
<strong>Trauma</strong> Patient<br />
Gail E. Rasmussen, MD<br />
University <strong>of</strong> Mississippi Medical Center, Meridian,<br />
Mississippi, USA<br />
0830–0900 Sedation/Analgesia/Anesthesia for Diagnostic Studies<br />
and Treatment Outside the Operating Room<br />
James E. Fletcher, MB BS<br />
University <strong>of</strong> North Carolina at Chapel Hill, Chapel Hill,<br />
North Carolina, USA<br />
0900–0930 Pediatric Prehospital Care<br />
Charles D. Deakin, MA MD MRCP FRCA<br />
Southhampton University Hospital, Southampton, UK<br />
0930–1000 Beverage Break<br />
1000–1030 Pediatric Head Injury: Where Have We Been; Where<br />
Are We Going?<br />
Jeffrey M. Berman, MD<br />
University <strong>of</strong> North Carolina, Chapel Hill,<br />
North Carolina, USA<br />
1030–1100 Fluid Management <strong>of</strong> the Injured Child<br />
Calvin Johnson, MD<br />
Charles R. Drew University <strong>of</strong> Medicine, Los Angeles,<br />
California, USA<br />
1100–1130 Early Care <strong>of</strong> the Pediatric Burn Patient<br />
Gary F. Purdue, MD<br />
UT Southwestern Medical Center, Dallas, Texas, USA<br />
1130–1200 Panel Discussion<br />
SESSION B<br />
Prehospital Care, Bel-Air Room IV-VI<br />
Co-Chair: Charles Deakin, MA MD MRCP FRCA,<br />
Southampton, UK<br />
Co-Chair: Marvin Wayne, MD, Bellingham, Washington, USA<br />
0830–0900 Selective Cervical Immobilization<br />
Marvin A. Wayne, MD, FACEP<br />
University <strong>of</strong> Washington and EMS Medical Director,<br />
Bellingham, Washington, USA<br />
0900–0930 Pre-Operative Fluid Resuscitation for <strong>Trauma</strong><br />
Patients: Elemental or Detrimental?<br />
Paul E. Pepe, MD, MPH, FACEP, FACCP, FACP, FCCM<br />
University <strong>of</strong> Texas Southwestern Medical Center at Dallas,<br />
Dallas, Texas, USA<br />
0930–1000 Beverage Break<br />
1000–1030 Prehospital Use <strong>of</strong> Hypertonic Saline Derivatives<br />
Pierre Carli, MD, PhD<br />
Hôpital Necker – Enfants Malades, Paris, France<br />
1030–1100 Prehospital Analgesia and Anesthesia<br />
Caroline Telion, MD, and Pierre Carli, MD, PhD<br />
Hôpital Necker – Enfants Malades, Paris, France<br />
1100–1130 <strong>The</strong> Role <strong>of</strong> the Anesthesiologist in Civil Chemical<br />
and Biological Weapon Attacks<br />
Dr David Baker M Phil DM FRCA<br />
Hôpital Necker – Enfants Malades, Paris, France<br />
1130–1200 Terror-Induced, Multiple Casualty Events: Injury<br />
Patterns and Emergency Department Response<br />
Amir Blumenfeld, MD<br />
Tel Aviv University, Tel Aviv, Israel<br />
SESSION C<br />
CRNA Session, Addison Hospitality Suite<br />
Chair: James M. Rich, MA, CRNA, Dallas, Texas, USA<br />
0800–0815 Vascular Access for <strong>Trauma</strong> Anesthesia: Options,<br />
Risks, Benefits, and Complications<br />
Deborah B. Latham, MHS, CRNA-P<br />
Texas Wesleyan University, Cedar Hill, Texas, USA<br />
0815–0830 Massive Volume Replacement<br />
Charles R. Barton, CRNA, MSN, MEd<br />
Akron, Ohio, USA<br />
0830–0900 Applying ATLS Guidelines to <strong>Trauma</strong> Care<br />
Wendell Dean Spencer, CRNA, MHS<br />
NCAS, O’Neill, Nebraska, USA<br />
0900–0930 Anesthetic Management <strong>of</strong> the Patient Sustaining<br />
Thoracic <strong>Trauma</strong><br />
Charles R. Barton, CRNA, MSN, MEd<br />
Akron, Ohio, USA<br />
0930–1000 Beverage Break<br />
1000–1030 Anesthetic Management <strong>of</strong> the <strong>Trauma</strong> Patient in the<br />
Rural Health Care Setting<br />
Wendell Dean Spencer, CRNA, MHS<br />
NCAS, O’Neill, Nebraska, USA<br />
1030–1100 Airway Management in <strong>Trauma</strong> Patients<br />
James M. Rich, MA, CRNA<br />
Baylor University Medical Center, Dallas, Texas, USA<br />
1100–1130 Anesthesia Management <strong>of</strong> Patients with Abdominal<br />
<strong>Trauma</strong><br />
Deborah B. Latham, MHS, CRNA-P<br />
Texas Wesleyan University, Cedar Hill, Texas, USA<br />
1130–1200 Anesthestic Management <strong>of</strong> the Acute<br />
Spinal-Cord-Injured Patient<br />
Charles R. Barton, CRNA, MSN, MEd<br />
Akron, Ohio, USA<br />
1200 ALL SESSIONS ADJOURN<br />
0800-0830 Use <strong>of</strong> Capnography in Prehospital <strong>Trauma</strong> Care<br />
Charles D. Deakin, MA MD MRCP FRCA<br />
Southhampton University Hospital, Southampton, UK<br />
38
<strong>ITACCS</strong> Spring 2003<br />
ABSTRACTS<br />
Thursday, May 15, 2003<br />
— Opening Plenary Session —<br />
JFK in Dallas, a <strong>Trauma</strong> Care Perspective<br />
Adolph H. Giesecke, MD<br />
Former Jenkins Pr<strong>of</strong>essor <strong>of</strong> Anesthesiology and Chairman<br />
Department <strong>of</strong> Anesthesiology and Pain Management<br />
University <strong>of</strong> Texas Southwestern Medical Center, Dallas, Texas, USA<br />
<strong>The</strong> management <strong>of</strong> patients following injury continues to evolve as our understanding<br />
<strong>of</strong> the physiology <strong>of</strong> injury improves. Technology advances are providing better diagnostic<br />
options, allowing earlier diagnosis and selective intervention. Noninvasive or minimally<br />
invasive techniques are providing new methods <strong>of</strong> intervention, and therapeutic advances<br />
are providing more options for the management <strong>of</strong> difficult cases and complications.<br />
We have a greater understanding <strong>of</strong> the economic consequences <strong>of</strong> trauma care and<br />
this is driving more selective management for specified patients. <strong>Trauma</strong> care dogma is<br />
increasingly challenged in the light <strong>of</strong> sound science, and investigation or review <strong>of</strong> unproven<br />
beliefs that govern treatment decisions should be a priority.<br />
At the time <strong>of</strong> writing, we once again face the potential for major armed conflict and<br />
perhaps never before has the treat <strong>of</strong> nuclear, biological, and chemical weapons been so<br />
great. <strong>The</strong> challenges and concerns these raise affect us all.<br />
We all have potential roles at local, national, and international levels to improve the<br />
management and outcome for the victims <strong>of</strong> trauma. <strong>The</strong>se improvements will be driven by<br />
the enthusiasm and commitment <strong>of</strong> those involved in trauma care.<br />
Applications <strong>of</strong> Dexmedetomidine in the <strong>Trauma</strong> Patient<br />
Michael A.E. Ramsay, MD, FRCA<br />
Baylor University Medical Center<br />
Dallas, Texas, USA<br />
Learning Objectives:<br />
• To understand the pharmacology <strong>of</strong> α2-adrenoceptor agonists.<br />
• To learn how the properties <strong>of</strong> sedation and analgesia without respiratory<br />
depression may be applied to the management <strong>of</strong> the trauma patient.<br />
• To predict the effect on the hemodynamic pr<strong>of</strong>ile <strong>of</strong> the patient.<br />
I was at Parkland Hospital on November 22, 1963, and assisted in the unsuccessful<br />
attempt to resuscitate the president and gave anesthesia to Governor Connally. I shall<br />
describe the events <strong>of</strong> that day, emphasizing the roles <strong>of</strong> doctors at Parkland, the conclusions<br />
<strong>of</strong> the Warren Commission, the controversy surrounding the conspiracy theories, the conclusions<br />
<strong>of</strong> the Select Committee, the movie “JFK,” and the evidence that closed the case in<br />
1992. <strong>The</strong> lecture is dedicated to Pepper Jenkins, Jim Carrico, and Paul Peters, valued colleagues<br />
who were there and who have subsequently died.<br />
JFK came to Texas to try to heal a rift between Lyndon Johnson, his vice president, and<br />
John Connally, the Governor <strong>of</strong> Texas. While riding past the School Book Depository in his<br />
open-topped limousine, he was shot through the neck and head. Governor Connally, who was<br />
riding in front <strong>of</strong> the president, was shot through the chest, wrist, and thigh. JFK was brought<br />
to Parkland Hospital for an attempted resuscitation, which lasted 25 minutes. <strong>The</strong> doctors who<br />
were primarily involved in the resuscitation were Jim Carrico, Pepper Jenkins, Mac Perry, and<br />
Charles Baxter, assisted by Kemp Clark, Paul Peters, Bob McClelland, and myself.<br />
Lyndon Johnson ordered the body removed to Bethesda, took the oath <strong>of</strong> <strong>of</strong>fice aboard<br />
Air Force One, and ordered Chief Justice <strong>of</strong> the Supreme Court Earl Warren to investigate the<br />
crime. <strong>The</strong> Warren Commission concluded that the shots were fired from one rifle held by one<br />
man, Lee Harvey Oswald, who was perched in the sixth floor window <strong>of</strong> the School Book<br />
Depository. <strong>The</strong> public was not satisfied and conspiracy theories flourished. <strong>The</strong><br />
Congressional Select Committee repeated the investigation in 1979 and concluded that<br />
Oswald was not the only gunman, and the conspiracy included figures from organized crime.<br />
Oliver Stone’s movie, “JFK” staring Kevin Costner released in 1991, was based on the discredited<br />
conspiracy theory proposed by Jim Garrison, the District Attorney <strong>of</strong> New Orleans.<br />
Dennis Breo published the evidence, which convinced me that no conspiracy existed.1<br />
He interviewed the pathologists who did the autopsy; reviewed the films, photographs, drawings,<br />
and microscope slides; and interviewed the key players in the resuscitation_Carrico,<br />
Jenkins, Perry, and Baxter. Based on Breo’s article, GD Lundberg,2 editor <strong>of</strong> JAMA, concluded<br />
that we now have “unequivocal forensic evidence, without reservation that JFK was struck by<br />
two bullets fired from behind, from one high velocity rifle…one gunman.” His conclusion was<br />
confirmed in a carefully researched and written book by GL Posner, called Case Closed.3 All participants<br />
in this congress should visit the Sixth Floor Museum, dedicated to the story <strong>of</strong> the<br />
assassination and housed in the old School Book Depository.<br />
References<br />
1. Breo DL. JFK’s death, the plain truth. JAMA 1992; 267:2794–802.<br />
2. Lundberg GD. Closing the case in JAMA on the John F. Kennedy autopsy. JAMA<br />
1992; 268:1736–8.<br />
3. Posner GL. Case Closed. Random House, New York, 1993.<br />
— Presidents’ Forum —<br />
President’s Address: What’s New in <strong>Trauma</strong><br />
Michael J.A. Parr, MB BS MRCP FRCA FANZCA FJFICM<br />
Intensive Care Specialist, University <strong>of</strong> New South Wales, Liverpool Hospital,<br />
Sydney, Australia<br />
Learning Objective: To summarise some recent advances in trauma management<br />
and to identify topics for future initiatives.<br />
<strong>The</strong> α2-adrenoceptors are located in the central nervous system, peripheral nervous system,<br />
vascular smooth muscle, and a variety <strong>of</strong> other organs. Presynaptic activation <strong>of</strong> the α2-<br />
adrenoceptor modulates the release <strong>of</strong> norepinephrine, resulting in a reduction in the stress<br />
response. In many instances, this reduction can be very beneficial and cardioprotective. In a<br />
shock situation, it could be deleterious when the production <strong>of</strong> catecholamines may be essential<br />
to supporting the circulation. <strong>The</strong> activation <strong>of</strong> the α2-adrenoceptor in the spinal cord and<br />
locus ceruleus in the brain produces analgesia and sedation without respiratory depression.<br />
<strong>The</strong> quality <strong>of</strong> sedation produced is different from most other sedatives that act on GABA receptors.<br />
Dexmedetomidine has a sedative pr<strong>of</strong>ile that resembles non-REM sleep, and patients<br />
roused from sedation can be assessed neurologically without evidence <strong>of</strong> being obtunded. 1<br />
Dexmedetomidine is the most selective α2-adrenoceptor agonist available and is an<br />
imidazole compound, but without the steroid suppression action seen with etomidate. It is<br />
metabolized by the liver into inactive metabolites excreted in the urine. <strong>The</strong> redistribution<br />
half-life is approximately 8 minutes, and it has a terminal half-life <strong>of</strong> 3.5 hours; therefore, it is<br />
a readily controlled sedative when administered as an infusion.<br />
<strong>The</strong> dosing is labeled to allow up to 0.7 mcg/kg/h for 24 hours in initially intubated<br />
patients undergoing mechanical ventilation. Venn et al reported dexmedetomidine use in the<br />
medical ICU for up to 7 days without the development <strong>of</strong> tolerance or dependence and without<br />
any rebound hypertension on discontinuing the drug. <strong>The</strong>y also found that doses as high<br />
as 2.5 mcg/kg/h were required to properly control sedation in this patient group. 2<br />
Dexmedetomidine’s analgesic effect has been shown to reduce the need for opioids<br />
by 50% in postoperative cardiac surgery patients. 3<br />
<strong>The</strong> lack <strong>of</strong> respiratory depression has been demonstrated by Hall et al from measurements<br />
<strong>of</strong> end-tidal CO2, by Ebert et al from arterial blood gas analysis, and from CO2<br />
response curves by Ramsay et al. 4–6 This combination <strong>of</strong> sedation and analgesia with no respiratory<br />
depression lends itself to the management <strong>of</strong> the trauma patient. Controlled sedation<br />
can be maintained while facilitating weaning from mechanical ventilation. Sedation and<br />
pain management can be provided for the head injury patient without risk <strong>of</strong> CO2 retention.<br />
<strong>The</strong> effect <strong>of</strong> dexmedetomidine on cerebral blood flow has been examined in human volunteers.<br />
7 It reduces cerebral blood flow, probably as a result <strong>of</strong> reduced cerebral metabolic rate.<br />
This reduction may be an advantage in the management <strong>of</strong> many head injury patients, particularly<br />
if mechanical ventilation can be avoided.<br />
<strong>The</strong> success in using dexmedetomidine in “fast-track” cardiac surgery patients <strong>of</strong>fers<br />
the potential that chest trauma patients may be managed effectively without the need for<br />
mechanical ventilation or thoracic epidural analgesia.<br />
Dexmedetomidine allows us an opportunity to re-evaluate how we provide sedation<br />
and analgesia to the trauma patient.<br />
References<br />
1. Nelson LE, Lu J, Guo T, et al. <strong>The</strong> alpha2-adrenoceptor agonist dexmedetomidine<br />
converges on an endogenous sleep-promoting pathway to exert its sedative effects.<br />
Anesthesiology 2003; 98:428-36.<br />
2. Venn M, Newman J, Grounds M. A phase II study to evaluate the efficacy <strong>of</strong><br />
dexmedetomidine for sedation in the medical intensive care unit. Intensive Care<br />
Med 2003; 29:201–7.<br />
3. Venn RM, Bradshaw CJ, Spencer R, et al. Preliminary UK experience <strong>of</strong> dexmedetomidine,<br />
a novel agent for postoperative sedation in the intensive care unit.<br />
Anaesthesia 1999; 54:1136–42.<br />
4. Hall JE, Uhrich TD, Barney JA, et al. Sedative, amnestic, and analgesic properties <strong>of</strong><br />
small-dose dexmedetomidine infusions. Anesth Analg 2000; 90:699–705.<br />
5. Ebert TJ, Hall JE, Barney JA, et al. <strong>The</strong> effects <strong>of</strong> increasing plasma concentrations<br />
<strong>of</strong> dexmedetomidine in humans. Anesthesiology 2000; 93:382–94.<br />
6. Ramsay MAE, Jones CC, Knorpp HC, et al. Dexmedetomidine does not depress the<br />
CO2 response curve in postoperative patients. Anesthesiology 2002; 96:A1335.<br />
7. Prielipp RC, Wall MH, Tobin JR, et al. Dexmedetomidine-induced sedation in volunteers<br />
decreases regional and global cerebral blood flow. Anesth Analg 2002;<br />
95:1052–9.<br />
39
<strong>ITACCS</strong> Spring 2003<br />
[Dr. Ramsay receives grant/research support from Abbott Laboratories (the manufacturer<br />
<strong>of</strong> Precedex®) and is a consultant and member <strong>of</strong> the speakers bureau for that company.<br />
In regard to “<strong>of</strong>f-label” uses, Dr. Ramsay will present clinical trial data related to the longterm<br />
use <strong>of</strong> dexmedetomidine (Precedex®).]<br />
Stress Management for Care Providers in the <strong>Trauma</strong> Setting<br />
Jessie A. Leak, MD<br />
Associate Pr<strong>of</strong>essor <strong>of</strong> Anesthesiology, University <strong>of</strong> Texas, MD Anderson Cancer Center,<br />
Houston, Texas<br />
What do you want to have? Where do you want to go? Who do you want to go with? How<br />
the hell do you plan to get there? Write it down. Go do it. Enjoy it. Share it. It doesn’t get<br />
much simpler or better than that.<br />
—Lee Iacocca<br />
Stress management is a ubiquitous subject that many think about but few actively practice.<br />
Many <strong>of</strong> us want to reduce stress, particularly in the workplace, but fail to realize that<br />
stress does not occur in a vacuum. If we are feeling stress at work, chances are that we have<br />
stress in other areas <strong>of</strong> our life; these may include personal relationships, anger issues, issues<br />
involving our physical environment at home or at work, financial issues, and, most importantly,<br />
loss <strong>of</strong> opportunities to address our individuality: mind, body, and spirit. Without attention<br />
to all these areas <strong>of</strong> our life, we bring this excess baggage to work and perceive an undesirable<br />
or unpleasant work environment.<br />
What is Stress? Webster’s dictionary describes stress as “any mental or physical tension<br />
or strain.” Russ Hanlin, CFO, Sunkist, says that “it’s always appeared to me that stress is within<br />
the individual and not manufactured by the situation.”<br />
Hans Selye discussed the scientific theory <strong>of</strong> General Adaptation Syndrome that<br />
describes a built-in ability that our bodies have to adapt to situations to a certain extent.<br />
Beyond this point, stress occurs. However, stress can be cumulative and therefore insidiously<br />
destructive when homeostasis is no longer possible because <strong>of</strong> internal resource depletion.<br />
Why am I Feeling Resource Depleted or Experiencing Burnout? Loss <strong>of</strong> control (particularly<br />
in the workplace), the outward manifestation <strong>of</strong> which is stress, can be intensified<br />
for anesthesiologists because <strong>of</strong> the exaggerated loss <strong>of</strong> a doctor-patient reciprocal relationship<br />
that other physician specialists enjoy with their patients. In other words, the loss <strong>of</strong><br />
receiving positive strokes from our patients in conventional doctor-patient relationships may<br />
intensify a chronic depersonalization.<br />
Anesthesiologists may have little or no interaction with their patients, except in the<br />
immediate perioperative period. <strong>The</strong> loss <strong>of</strong> a reciprocal relationship with our patients is<br />
intensified in an oncology or burn ward-type setting (areas with many suffering patients).<br />
Additional factors that can contribute to loss <strong>of</strong> control (stress) may include 1) the constant<br />
need to suppress symptoms <strong>of</strong> fatigue and exhaustion; 2) economic factors that compel<br />
the physician to perform in the dual role <strong>of</strong> physician and business manager/CEO; 3) difficult<br />
relationships with colleagues; 4) increased severity <strong>of</strong> illness <strong>of</strong> patients; 5) liability concerns<br />
(“every patient is a potential law suit” mentality); 6) night call/sleep deprivation; or 7)<br />
compliance issues, e.g., HIPPA, Medicare.<br />
You are not alone. A 1994 study in Anesthesiology reported that nearly half <strong>of</strong> the anesthesiologists<br />
surveyed felt they were under chronic pressure at work. Female physicians<br />
between the ages <strong>of</strong> 45 and 55 without a partner, with full-time hospital work and the attendant<br />
administrative responsibilities in an understaffed area are at greatest risk to experience<br />
chronic pressure or stress. This group also commits suicide at six times the rate <strong>of</strong> the general<br />
population.<br />
Chassot described the triad <strong>of</strong> burnout as emotional exhaustion, depersonalization<br />
(loss <strong>of</strong> empathy), and a lack <strong>of</strong> personal accomplishment. If you are not sure if you are<br />
burned or burning out, see if you recognize any <strong>of</strong> the following burnout symptoms: feeling<br />
tired even with adequate sleep, work dissatisfaction, forgetfulness, sadness, irritability,<br />
increased incidence <strong>of</strong> illness, subpar job performance, substance abuse, decreased concentration,<br />
avoidance <strong>of</strong> interaction with others, increased boredom with work, decreased work<br />
accomplishment despite seeming hard work, dreading going to work, avoiding social activities,<br />
feeling like work is a dead-end (“why bother”), and the perception that what you were<br />
hired to do is not meeting with reality.<br />
Where Do I Go From Here? It is important not to compare yourself to others. What<br />
may drain one individual may be a breeze for another. Simply honor what you know is draining<br />
you and address the issue. You have a right to be the final judge <strong>of</strong> your stress issues and<br />
to accept them as legitimate. Barbara Larrivee tells us in Moving Into Balance that “the journey<br />
toward personal fulfillment and true transformation requires major restructuring that<br />
cannot be prescribed with an intervention formula…<strong>The</strong> pathway cannot be preplanned.<br />
Each <strong>of</strong> us has our own internal gauge for when we are ready to deal with a critical life issue.”<br />
Once you have identified that you are burned out/stressed out, it is imperative to reestablish<br />
some control in your life. Ironically, when we are burned out, the last thing that we<br />
want to do is change because change is work. What we want is less work, but avoidance <strong>of</strong><br />
change can become a fear <strong>of</strong> change (which causes increased stress).<br />
It is not unusual to find that you have stressors in one or more areas in your life: work,<br />
relationships (including issues with anger management or toxic relationships), dysfunction in<br />
your physical environment, financial woes, and most importantly no time or imbalance in<br />
your body, mind, and/or spiritual life. This may include medical issues or a disconnect with<br />
our spiritual life, which may or may not include our religious practices or beliefs.<br />
It is important to take inventory as soon as possible. During this process, it is quite<br />
helpful to establish what your life purpose may be and what makes your life meaningful.<br />
Once you discover what is draining you the most, you have three options: 1) Take care <strong>of</strong> the<br />
issue by yourself and do it! 2) Delegate the task to someone else or hire someone to do it!;<br />
or 3) Throw it out and let it go!<br />
Now is the time which is the borderline between going up and going down; now is the<br />
time when by slipping into laziness even for a moment you will endure constant suffering;<br />
now is the time when by concentrating for an instant you will enjoy constant happiness.<br />
Focus your mind single-mindedly; strive to prolong the results <strong>of</strong> good karma.<br />
—<strong>The</strong> Tibetan Book <strong>of</strong> the Dead<br />
Bibliography<br />
1. Odette Pollar. 365 Ways to Simplify Your Work Life: Ideas That Bring More Time,<br />
Freedom and Satisfaction to Daily Work. Chicago: Dearborn Financial Pub, 1996.<br />
2. Chassot P. Stress in European operating room personnel. World Congress <strong>of</strong><br />
Anesthesiologists, 2000 Proceedings 2000, 63–5.<br />
3. Gaba DM, Howard SK, Jump B. Production pressure in the work environment.<br />
California anesthesiologists’ attitudes and experiences. Anesthesiology 1994;<br />
81:488–500.<br />
4. Heim E. Stressors in health occupations. Do females have a greater health risk? New<br />
Zealand Psychosom Med Psychoanal 1992; 38:207–26.<br />
5. Leak JA. Stress management: communicating with the lion and the lamb. ASA<br />
Newsletter 2002; 66(11): 33–4.<br />
6. Leak JA. Stress management: finding your purpose in the Ark. ASA Newsletter 2001;<br />
65(11):27–8.<br />
7. Leak JA. Stress management: slaying the dragon. ASA Newsletter Part I. 2000;<br />
64(10):27–8.<br />
8. Leak JA. Stress management: slaying the dragon. ASA Newslette. Part II. 2000;<br />
64(11):21–2.<br />
9. Leak JA. Stress management: calming the lion. ASA Newsletter 1999; 63(8):21–2.<br />
Emergency Ventilatory Management <strong>of</strong> the <strong>Trauma</strong> Patient:<br />
Elemental or Detrimental?<br />
Paul E. Pepe, MD, MPH, FACEP, FCCP, FACP, FCCM<br />
Pr<strong>of</strong>essor <strong>of</strong> Surgery, Medicine, and Public Health and Riggs Family Chair in Emergency<br />
Medicine. <strong>The</strong> University <strong>of</strong> Texas Southwestern Medical Center andParkland Health and<br />
Hospital System, Dallas<br />
Medical Director, Dallas Metropolitan Medical Response System (MMRS) and Medical<br />
Director, Dallas Metropolitan Bio Tel (EMS) System<br />
Learning Objectives: 1) To understand the differences in ventilatory techniques<br />
used during normal hemodynamic conditions versus those required during circulatory<br />
arrest/compromise, 2) To appreciate the potential detrimental effects <strong>of</strong> airway and ventilatory<br />
techniques commonly used by emergency care providers for cases <strong>of</strong> cardiac and<br />
trauma resuscitation, 3) To recognize the rationale and appropriate circumstances for recommended<br />
ventilatory strategies/adjuncts, both basic and advanced and 4) to learn<br />
improved strategies for delivering appropriate ventilatory techniques during cardiac and<br />
trauma resuscitations.<br />
Emergency care providers have been trained to make airway management a priority in<br />
cardiac, respiratory, and trauma resuscitation. Nevertheless, most providers <strong>of</strong> emergency<br />
care, both in and out-<strong>of</strong>-hospital, <strong>of</strong>ten lack a fundamental understanding <strong>of</strong> ventilatory physiology<br />
during circulatory arrest/compromise. Furthermore, texts and guidelines for emergency<br />
respiratory care traditionally have been somewhat generic, generally emphasizing<br />
“hyperventilation,” a concept that is also not well understood. <strong>The</strong> purpose <strong>of</strong> this talk is to<br />
review the physiology <strong>of</strong> ventilation in the unusual circumstances <strong>of</strong> circulatory arrest/compromise.<br />
<strong>The</strong> discussion will describe how both basic and advanced airway techniques can be<br />
life-saving if used properly, but can also be detrimental when traditional training techniques<br />
are followed too zealously. <strong>The</strong> lecturer will conclude with updated recommendations for the<br />
management <strong>of</strong> both cardiac and trauma resuscitation and will also review the value <strong>of</strong> each<br />
<strong>of</strong> the various airway adjuncts currently available to emergency care providers.<br />
References<br />
1. American College <strong>of</strong> Surgeons Committee on <strong>Trauma</strong>. Shock. In Advanced <strong>Trauma</strong><br />
Life Support Program for Physicians. Instructor Manual. Chicago: ACS, 1993, pp<br />
75–110.<br />
2. Noc M, Weil MH, Tang W, et al. Mechanical ventilation may not be essential for initial<br />
cardiopulmonary resuscitation. Chest 1995; 108:821–7.<br />
3. Idris AH, Staples ED, O’Brien DJ, et al. Effect <strong>of</strong> ventilation on acid-base balance and<br />
oxygenation in low blood-flow states. Crit Care Med 1994; 22:1827–34.<br />
4. Pepe PE. Acute respiratory insufficiency. In Harwood-Nuss A et al, eds. <strong>The</strong> Clinical<br />
Practice <strong>of</strong> Emergency Medicine. Philadelphia, Lippincott, 1996, chapter 140; pp<br />
636–40.<br />
5. Pepe PE, Marini JJ. Occult positive end-expiratory pressure in mechanically-ventilated<br />
patients with airflow obstruction - the auto-PEEP effect. Am Rev Resp Dis 1982;<br />
126:166–70.<br />
6. Franklin C, Samuel J, Hu TC. Life-threatening hypotension associated with emergency<br />
intubation and the initiation <strong>of</strong> mechanical ventilation. Am J Emerg Med<br />
1994; 12:425–8.<br />
7. Durham LA, Richardson RJ, Wall MJ, Pepe PE, Mattox KL. Emergency center thoracotomy:<br />
impact <strong>of</strong> prehospital resuscitation. J <strong>Trauma</strong> 1992; 32:775–9.<br />
8. Marion DW, Firlik A, McLaughlin MR. Hyperventilation therapy for severe traumatic<br />
brain injury. New Horizons 1995; 3:439–47.<br />
9. Pepe PE. Resuscitation <strong>of</strong> the patient with major trauma. Curr Opin in Crit Care<br />
1995; 1:479–86.<br />
10. Pepe PE. Preoperative fluid resuscitation for post-traumatic hemorrhage: elemental<br />
or detrimental? In Lawin P, Peter K, Prien T, eds. Intensivmedizin. New York,<br />
Stuttgart, Georg Thieme Verlag, 1995, pp 72–7.<br />
11. Pepe PE. Controversies in resuscitation: to infuse or not to infuse (2). Resuscitation<br />
1996; 31:7–10.<br />
12. Bickell WH, Wall MJ, Pepe PE, et al. Immediate versus delayed fluid resuscitation for<br />
hypotensive patients with penetrating torso injury. N Engl J Med Oct. 27, 1994;<br />
331:1105–9.<br />
13. Pepe PE, Mattox KL, Fischer RP, Matsumoto CM. Geographical patterns <strong>of</strong> urban<br />
trauma according to mechanism and severity <strong>of</strong> injury. J <strong>Trauma</strong> 1990; 30:1125–32.<br />
14. Cobb LA, Alvarez H, Copass MK. A rapid response system for out-<strong>of</strong>-hospital cardiac<br />
emergencies. Med Clin North Am 1976; 60:283–90.<br />
15. McManus WF, Tresch DD, Darin JC. An effective prehospital emergency system. J<br />
<strong>Trauma</strong> 1977; 17:304–10.<br />
16. Curka PA, Pepe PE, Ginger VF, et al. Emergency medical services priority dispatch.<br />
Ann Emerg Med 1993; 22:1688–95.<br />
17. Applebaum D. Patient selection for advanced prehospital care in a two-level emergency<br />
medical system. Prehosp Disast Med 1989; 4:36.<br />
18. Sanders AB, Kern KB, Berg RA, et al. Survival and neurologic outcome after cardiopulmonary<br />
resuscitation with four different chest compression-ventilation<br />
ratios. Ann Emerg Med 2002; 40:553–62.<br />
19. Pepe PE, Raedler C, Lurie K, Wigginton J. Emergency ventilatory management in<br />
hemorrhagic states: elemental or detrimental? J <strong>Trauma</strong> 2003 (in press).<br />
20. Pepe PE, Mosesso VN, Falk JL. Prehospital fluid resuscitation <strong>of</strong> the patient with<br />
major trauma. Prehosp Emerg Care 2002; 6(1):81–91.<br />
40
<strong>ITACCS</strong> Spring 2003<br />
Fluid Management in <strong>Trauma</strong><br />
Richard P. Dutton, MD<br />
R Adams Cowley Shock <strong>Trauma</strong> Center, University <strong>of</strong> Maryland, Baltimore, Maryland, USA<br />
Learning Objective: To better understand the anesthesiologist’s role in controlling<br />
life-threatening hemorrhage.<br />
Fluid resuscitation is a rapidly evolving area <strong>of</strong> trauma practice, particularly in early<br />
hemorrhagic shock (while the patient is still actively bleeding). <strong>The</strong> surgeons have brought<br />
new diagnostic and therapeutic options to the table, including FAST, angiography, and damage<br />
control techniques. What has anesthesia contributed?<br />
I will briefly review the history and recent academic literature on early resuscitation,<br />
including the arguments for and against deliberate hypotensive management, early use <strong>of</strong><br />
blood products, hypothermia, hypertonic resuscitation fluids, and pro-coagulants. <strong>The</strong> anesthesiologist<br />
plays a critical role in the application <strong>of</strong> each <strong>of</strong> these therapies and should be<br />
familiar with the evidence that supports their use.<br />
I will conclude with a discussion <strong>of</strong> over-the-horizon approaches to hemorrhagic<br />
shock, including new diagnostic modalities, new treatment options, and new approaches to<br />
long-term resuscitation and prevention <strong>of</strong> organ system failure.<br />
[Editors’ note re “<strong>of</strong>f-label” use: Dr. Dutton will discuss investigational and anecdotal<br />
use <strong>of</strong> dry fibrin sealant bandages, hemoglobin-based oxygen carriers, and recombinant FVIIa.]<br />
Thursday, May 15, 2003<br />
Simultaneous Afternoon Sessions<br />
— Session A —<br />
New Dimensions in <strong>Trauma</strong> and Critical Care<br />
Co-Chair: James G. Cain, MD<br />
Co-Chair: Christopher M. Grande, MD, MPH<br />
Sedation for the Critically Injured <strong>Trauma</strong> Patient: Precedex®, a Novel Alternative<br />
James Gordon Cain, MD<br />
Allegheny General Hospital, Pittsburgh, Pennsylvania, and West Virginia University,<br />
Morgantown, West Virginia, USA<br />
Learning Objective: To provide an introduction to dexmedetomidine, a newly<br />
introduced alpha 2 blocking sedative-analgesic, and its use in critically ill trauma patients.<br />
Dexmedetomidine (Precedex®), a lipophilic imidazole derivative, selective alpha2<br />
agonist (1300:1, a2:a1), is approved for use in initially intubated critically ill patients.<br />
Precedex® <strong>of</strong>fers analgesia, sedation, inhibition <strong>of</strong> shivering, decreased sympathetic outflow,<br />
and decreased catecholamines without significantly decreasing respiratory drive. With this<br />
decrease in sympathetic outflow, mild to moderate hypotension and bradycardia may occur.<br />
Precedex® does not have a direct myocardial effect. A novel aspect <strong>of</strong> Precedex® is that,<br />
compared with an equal level <strong>of</strong> baseline sedation with standard agents, it allows easy arousability.<br />
This would be particularly advantageous in facilitating reproducible, serial neurologic<br />
examinations at will in patients with TBI while avoiding the drastic swings in sedation with<br />
volatile hemodynamics associated with the current prop<strong>of</strong>ol-based technique.<br />
Dexmedetomidine reduced prop<strong>of</strong>ol and morphine requirements and improved hemodynamic<br />
stability during bispectral (BIS) index-guided intensive care unit sedation. Additional<br />
benefits <strong>of</strong> Precedex® may be a modest decrease in cerebral blood flow, along with additional<br />
neuroprotective properties in its own right.<br />
Bibliography<br />
Hall JE, Uhrich TD, Barney JA, et al. Sedative, amnestic, and analgesic properties <strong>of</strong><br />
small-dose dexmedetomidine infusions. Anesth Analg 2000; 90:699–705.<br />
Housmans PR. Effect <strong>of</strong> dexmedetomidine on contractility, relaxation, and intracellular calcium<br />
transients <strong>of</strong> isolated ventricular myocardium. Anesthesiology 1990; 73:919–22.<br />
Jolkkonen J, Puurunen K, Koistinaho J, et al. Neuroprotection by the alpha2-adrenoreceptor<br />
agonist, dexmedetomidine, in rat focal cerebral ischemia. Eur J Pharmacol<br />
1999; 372:31–6.<br />
Kuhmonen J, Pokorny J, Miettinen R, et al. Neuroprotective effects <strong>of</strong> dexmedetomidine<br />
in the gerbil hippocampus after transient global ischemia. Anesthesiology<br />
1997; 87:371–7.<br />
Prielipp RC, Wall MH, Tobin JR, et al. Dexmedetomidine-induced sedation in volunteers<br />
decreases regional and global blood flow. Anesth Analg 2002; 95:1052–9.<br />
Takrouri MS, Seraj MA, Channa AB, et al. Dexmedetomidine in the intensive care unit:<br />
a study <strong>of</strong> hemodynamic changes. Middle East J Anesthesiol 2002;16:587–95.<br />
Talke P, Li J, Jain U, et al. Effects <strong>of</strong> perioperative dexmedetomidine infusion in patients<br />
undergoing vascular surgery. <strong>The</strong> Study <strong>of</strong> Perioperative Ischemia Research Group.<br />
Anesthesiology 1995; 82:620–33.<br />
Triltsch AE, Welte M, von Homeyer P, et al. Bispectral index-guided sedation with<br />
dexmedetomidine in intensive care: a prospective randomized, double blind, placebo-controlled<br />
phase II study. Crit Care Med 2002; 30:1007–14.<br />
Venn RM, Bradshaw CJ, Spencer R, et al. Preliminary UK experience <strong>of</strong> dexmedetomidine,<br />
a novel agent for postoperative sedation in the intensive care unit.<br />
Anaesthesia 1999; 54:1136–42.<br />
Venn RM, Bryant A, Hall GM, Grounds RM. Effects <strong>of</strong> dexmedetomidine on adrenocortical<br />
function, and the cardiovascular, endocrine and inflammatory responses in<br />
post-operative patients needing sedation in the intensive care unit. Br J Anaesth<br />
2001; 86:650–6.<br />
Venn RM, Hell J, Grounds RM. Respiratory effects <strong>of</strong> dexmedetomidine in the surgical<br />
patient requiring intensive care. Crit Care 2000; 4:302–8.<br />
<strong>The</strong> Hazards <strong>of</strong> Nutraceuticals in the Management <strong>of</strong> the <strong>Trauma</strong> Patient<br />
Jessie A. Leak, MD<br />
Associate Pr<strong>of</strong>essor <strong>of</strong> Anesthesiology<br />
University <strong>of</strong> Texas, MD Anderson Cancer Center, Houston, Texas, USA<br />
Learning Objectives: 1) To outline the herbs and dietary supplements (nutraceuticals)<br />
that are most commonly used in the preoperative phase; 2) to discuss the various<br />
preparations in which these products are available; 3) to broadly cover the state <strong>of</strong> government<br />
regulation <strong>of</strong> these products; and 4) most importantly, to target some <strong>of</strong> the more<br />
important potential drug-nutraceutical interactions and hazards, particularly as they<br />
may relate to the care <strong>of</strong> the patient receiving anesthesia.<br />
Because <strong>of</strong> the paucity <strong>of</strong> government regulation regarding purity, contents, manufacturing,<br />
and health claims as well as pharmacologic and physiologic predictability, it is difficult<br />
to fund and perform double-blind, placebo-controlled studies on these products. For this<br />
reason, much <strong>of</strong> the material concerning potential hazards and adverse drug interactions is<br />
based on extrapolation, anecdote, and/or uncontrolled case studies on active ingredients that<br />
are not consistently available in the products that we purchase in our local pharmacies, grocery<br />
stores, and gyms.<br />
SUMMARY OF POTENTIAL INTRAOPERATIVE COMPLICATIONS<br />
Untoward cardiovascular effects Ephedra<br />
Ginseng<br />
Licorice<br />
St. John’s Wort (potential indirect effect)<br />
Vitamin E<br />
Triiodothyroacetic acid<br />
GBL, BD, GHB<br />
Enhanced bleeding potential<br />
Potential for prolongation<br />
<strong>of</strong> anesthesia<br />
Possible renal insufficiency<br />
or hepatotoxicity<br />
Possible abnormal thyroid functions<br />
Potential for electrolyte disturbances<br />
Risk <strong>of</strong> decreased effectiveness <strong>of</strong><br />
HIV protease inhibitors<br />
Ginseng<br />
Ginkgo<br />
Ginger<br />
Garlic<br />
Feverfew<br />
Vitamin E<br />
Valerian<br />
Kava-kava<br />
St. John’s Wort (anecedotal only)<br />
Licorice (renal)<br />
Creatine (renal)<br />
Echinacea (hepatic)<br />
Kava-kava (hepatic)<br />
Triiodothyroacetic acid<br />
Vitamin E<br />
Goldenseal<br />
Licorice<br />
St. John’s Wort<br />
SUMMARY OF INDIVIDUAL HERBS AND SUPPLEMENTS<br />
Name Common Uses Potential Side Effects<br />
Echinacea Common cold, bronchitis Possibly hepatotoxic. May decrease<br />
effectiveness <strong>of</strong> corticosteroids<br />
Ephedra Diet aid; antitussive Death. Cardiovascular instability. Multiple<br />
drug interactions<br />
Feverfew Migraine prophylactic May inhibit platelet activity and increase<br />
bleeding. Avoid use in pts on anticoagulants.<br />
Garlic Lipid & BP lowering; May potentiate warfarin and increase<br />
Antiplatelet, antioxidant, bleeding; affects platelet aggregation.<br />
anithrombolytic qualities<br />
Ginger Antinauseant May be a potent inhibitor <strong>of</strong> thromboxane<br />
synthetase and may increase bleeding time.<br />
Use with caution with warfarin.<br />
Ginkgo Circulatory stimulant May enhance bleeding in pts on<br />
anticoagulant or antithrombotic therapy.<br />
Ginseng “Adaptogenic” Avoid use with other stimulants—may<br />
Energy level enhancer experience tachycardia or hypertension.<br />
Antioxidant<br />
May increase bleeding, especially in patients<br />
on anticoagulant or antithrombotic therapies.<br />
Known to have anti-platelet properties.<br />
Goldenseal Diuretic; anti-inflammatory Functions as aquaretic, not as diuretic; see<br />
no sodium excretion, just free water<br />
excretion. May worsen edema or<br />
hypertension.<br />
Kava-kava Anxiolytic May potentiate barbiturates and prolong<br />
anesthesia.<br />
Licorice Gastric and duodenal ulcers Glycyrrhizic acid in licorice may cause high<br />
blood pressure, low potassium, and edema.<br />
Contraindicated in renal insufficiency, liver<br />
conditions, hypertonia.<br />
St. John’s Wort Mild to moderate depression May prolong effects <strong>of</strong> anesthesia (anecdotal<br />
Anxiety<br />
only). May decrease effectiveness <strong>of</strong> all HIV<br />
protease inhibitors as well as all nonnucleo<br />
side reverse transcriptase inhibitors. May<br />
decrease blood levels <strong>of</strong> digoxin.<br />
Valerian Sedative May potentiate barbiturates.<br />
41
<strong>ITACCS</strong> Spring 2003<br />
Triiodothy- Diet aid May cause heart attacks or strokes due to its<br />
roacetic acid<br />
potent thyroid hormone content. May also<br />
see abnormal thyroid function tests along<br />
with severe diarrhea, fatigue, lethargy,<br />
weight loss.<br />
GHB, BD, GBL Body building, Coma, seizures, vomiting, slowed breathing<br />
weight loss aid,<br />
requiring intubation, slowed heart rate, or<br />
sleep inducement<br />
death. Being investigated as a treatment for<br />
narcolepsy. Implicated as a “date-rape” drug.<br />
Vitamin E Slow aging process May increase bleeding, especially when used<br />
Prevention <strong>of</strong> stroke and PE with anticoagulant and/or anti-thrombotic<br />
Promotes wound healing drugs. May affect thyroid function in<br />
Effective against fibrocystic otherwise healthy patients. May enhance<br />
breast syndrome<br />
HTN in predisposed patients in doses<br />
greater than or equal to 400 IU/day.<br />
Bibliography<br />
1. McLeskey C, Meyer TA, Baisden CE, Gloyna DF, Roberson R. <strong>The</strong> incidence <strong>of</strong><br />
herbal and seleted nutraceutical use in surgical patients. Anesthesiology 1999;<br />
91(34):A1168.<br />
2. Tsen LC, Segal S, Pothier M, Bader A. Alternative medicine use in presurgical<br />
patients. Anesthesiology 2000; 93(1):148–51.<br />
3. Leak JA, Hogervorst SL, Roach P, Arbuckle R, Palmer L. Anesthesiology 2002; A-1129.<br />
4. Eisenberg D, Davis RB, Ettner SL, Appel S, Wilkey S, Rompay M, Kessler RC. Trends<br />
in alternative medicine use in the United States, 1990-1997: results <strong>of</strong> a follow-up<br />
national survey. JAMA 1998; 280:1569–75.<br />
5. Leak JA. Herbal medicines: what do we need to know? ASA Newsletter 2000;<br />
5(2):5–7,11.<br />
6. Eisenberg DM, Kessler RC, Van Rompay M, Kaptchuk TJ, Wilkey SA, Appel S, Davis<br />
RB. Perceptions about complementary therapies relative to conventional therapies<br />
among adults who use both: results from a national survey. Ann Intern Med 2001;<br />
135(5):344–51.<br />
7. O’Hara MA, Kiefer D, Farrell K, Kemper K. A review <strong>of</strong> 12 commonly used medicinal<br />
herbs. Arch Fam Med 1998; 7:523–36.<br />
8. Leak JA. Perioperative considerations in the management <strong>of</strong> the patient taking<br />
herbal medicines. Current Opinion in Anaesthesiology 2000; 13:321–5.<br />
9. Miller HI, Longtin D. Death by dietary supplement. Policy Review 2000; 102:15–25.<br />
10. American Society <strong>of</strong> Anesthesiologists. What you should know about your patients’<br />
use <strong>of</strong> herbal medicines. Pamphlet, American Society <strong>of</strong> Anesthesiologists, 520 N.<br />
Northwest Highway, Park Ridge, Illinois, 60068; 1999.<br />
11. Gruenwald J, Brendler T, Jaenicke C. PDR for Herbal Medicines, ed. 2. Montvale:<br />
New Medical Economics Company; 2000, pp 469–74.<br />
12. Leak JA. Herbal medicine: is it an alternative or an unknown? A brief review <strong>of</strong> popular<br />
herbs used by patients in a pain and symptom management practice setting.<br />
Current Review <strong>of</strong> Pain 1999; 226–36.<br />
13. Durr D, Stieger B, Kullak, Ublick GA, Rentsch KM, Steinert HC, Meier PJ, Fattinger<br />
K. St. John’s wort induces intestinal P-glycoprotein/MDR1 and intestinal and hepatic<br />
CYP3A4. Clin Pharmacol <strong>The</strong>r 2000; 68:598–604.<br />
14. US Food and Drug Administration, Medwatch, Important Message for Health<br />
Pr<strong>of</strong>essionals. Report serious adverse events associated with dietary supplements<br />
containing GBL, GHB, BD. August 25, 1999.<br />
15. Leak JA, Feather SM, DeMonte F. A case <strong>of</strong> multiple and significant postoperative<br />
bleeds in a single patient felt to be attributable to chronic preoperative Panax ginseng<br />
use. Anesthesiology 2001; 95(3):A-1134.<br />
Controversies in Blunt Aortic <strong>Trauma</strong><br />
Charles E. Smith, MD, FRCPC<br />
Pr<strong>of</strong>essor <strong>of</strong> Anesthesia, MetroHealth Medical Center, Case Western Reserve University,<br />
Cleveland, Ohio, USA<br />
Learning Objectives: 1) to review the incidence, pathophysiology, and diagnosis <strong>of</strong><br />
blunt aortic injury and 2) to discuss the anesthetic considerations for patients with blunt<br />
aortic trauma.<br />
Cardiothoracic trauma includes injury to the chest wall, trachea, bronchus, lungs,<br />
pleura, thoracic great vessels, diaphragm, heart, and esophagus. <strong>The</strong> practical points <strong>of</strong> providing<br />
safe and efficient anesthesia for patients with blunt aortic trauma will be stressed.<br />
<strong>The</strong> diagnosis <strong>of</strong> blunt aortic trauma should be suspected based on mechanism <strong>of</strong><br />
injury and widened mediastinum on chest radiograph. .Aortic angiogram is the gold standard<br />
<strong>of</strong> diagnosis <strong>of</strong> aortic injury, although TEE may be an excellent alternative according to the<br />
experience in each institution, especially for the unstable patient. Chest computed tomography<br />
is rapid and noninvasive and may be the test <strong>of</strong> choice to confirm or rule out the existence<br />
<strong>of</strong> mediastinal widening.<br />
<strong>The</strong> spectrum <strong>of</strong> blunt cardiac trauma ranges from asymptomatic myocardial contusion<br />
to cardiogenic shock, arrhythmias, free wall or septal wall rupture, valvular tears, and coronary<br />
artery thrombosis. Echocardiography is the diagnostic method <strong>of</strong> choice in patients with ECG<br />
abnormalities or unexplained cardiovascular instability following blunt chest trauma.<br />
Major considerations for anesthetic management <strong>of</strong> patients undergoing aortic surgery<br />
include location and extent <strong>of</strong> aortic injury and timing <strong>of</strong> surgery. Delaying surgery is recommended<br />
in many instances for stabilization and workup <strong>of</strong> other injuries. Strict control <strong>of</strong><br />
blood pressure with beta blockers and/or vasodilators is essential. Hemodynamic monitoring<br />
is recommended to optimize blood pressure, cardiac output, and tissue perfusion.<br />
Ascending aorta and aortic arch tears require cardiopulmonary bypass and single lung<br />
anesthesia. Deep hypothermic circulatory arrest is <strong>of</strong>ten employed. Proximal descending aortic<br />
tears are usually done with clamp and sew techniques and one-lung anesthesia. Partial left<br />
heart bypass may be utilized. Maintenance <strong>of</strong> normoglycemia improves wound healing and<br />
reduces wound infection and death. Cerebrospinal fluid drainage is not routinely done. Risk<br />
factors for developing paraplegia after aortic surgery include duration <strong>of</strong> aortic cross clamping,<br />
intraoperative hypotension, and surgical technique.<br />
A left-sided double-lumen tube is preferred for one-lung ventilation because <strong>of</strong> the<br />
high margin <strong>of</strong> safety and relative ease <strong>of</strong> deflating the left lung and providing CPAP to the<br />
atelectatic lung. Alternatively, a bronchial blocker technique may be employed. Fiberoptic<br />
bronchoscopy is routinely done to confirm proper position.<br />
Postoperative complications after aortic repair include respiratory failure, stroke,<br />
pneumonia, renal failure, suture line failure, and paraplegia.<br />
References<br />
1. Duan Y, Smith CE. Anesthesia for major cardiothoracic trauma. In Wilson WC,<br />
Grande CM, Hoyt DB, eds. <strong>Trauma</strong>: Resuscitation, Anesthesia, and Critical Care,<br />
chapter 25, 2003, in press.<br />
2. Van den Berghe G. Intensive insulin therapy in the critically ill patients. N Engl J<br />
Med 2001; 345(19):1359–67.<br />
3. Orliaguet G, Ferjani M, Riou B. <strong>The</strong> heart in blunt trauma. Anesthesiology 2001;<br />
95:544–8.<br />
Web-Based Resources<br />
1. Devitt JH. Blunt thoracic trauma: assessment, management, and anaesthesia.<br />
www.anesthesia.org/winterlude/wl95/wl95_4.html.<br />
2. EAST guidelines for blunt aortic trauma management. www.east.org/tpg/chap8.pdf.<br />
3. Pulmonary artery educational project:<br />
www.pacep.org/pages/start/ref.html?xin=accp.<br />
4. ASA guidelines for PA catheters:<br />
www.asahq.org/publicationsandservices/pulm_artery.pdf.<br />
What’s New in Neurotrauma<br />
Dr Anne Sutcliffe MB ChB, FRCA<br />
Consultant in Anaesthesia and Critical Care, Queen Elizabeth Hospital, Birmingham B15<br />
2TH, UK and Honorary Senior Lecturer, University <strong>of</strong> Birmingham<br />
Learning Objectives:<br />
• To review the scientific basis <strong>of</strong> interesting developments<br />
• To put these developments in clinical perspective<br />
<strong>The</strong>se days, all <strong>of</strong> us are trying to practice evidence-based medicine. Unfortunately,<br />
there is a dearth <strong>of</strong> high quality research in the field <strong>of</strong> head injury management. This is<br />
unfortunate because mortality is still high. However, hospital outcome measurement following<br />
head injury is still crude compared to rehabilitation outcome measures. Attempts to link<br />
existing outcome registries have not been practical. Now is the time to reconsider how we<br />
assess outcome.<br />
It is well known that hypoxia, hypotension, and combined hypoxia and hypertension<br />
are associated with poor outcome. <strong>The</strong> original data clearly demonstrate that perfusion is the<br />
crucial factor. But there is debate about how cerebral swelling should be managed. Many<br />
believe that protocol-driven management, which includes fluid and inotropes to raise mean<br />
arterial pressure, is useful. In Lund, an alternative approach is equally successful and treatment<br />
is directed mainly to reducing vasogenic oedema. Hypertonic saline has yet to find a<br />
clear role in the management <strong>of</strong> head injury.<br />
Recent work has shown that blood glucose level in the first 24 hours after injury correlates<br />
more closely with outcome than even hypotension. Most doctors control blood sugar<br />
after head injury, but the evidence for benefit has been shown only in the general ICU population.<br />
Hypothermia following head injury has failed to live up to its early promise. <strong>The</strong> reasons<br />
for this may include delays in inducing hypothermia, practical difficulties in measuring<br />
brain temperature, and faults in study design.<br />
<strong>The</strong> successful management <strong>of</strong> spinal cord injury also depends on maintaining adequate<br />
perfusion. Much attention is still directed to preventing mechanical cord damage but<br />
there is a body <strong>of</strong> evidence suggesting that it would be better if more attention was given to<br />
perfusion. <strong>The</strong> value <strong>of</strong> steroids has been questioned. <strong>The</strong>re is animal evidence to suggest<br />
that uncontrolled oxygen therapy may also be detrimental to the under-perfused spinal cord.<br />
In order to improve outcome after neurotrauma, it is essential that high quality<br />
research is done. An example <strong>of</strong> this is the European CRASH trial. Many questions remain<br />
unanswered but better use <strong>of</strong> existing knowledge should be our current goal.<br />
Further reading<br />
1. Copes WS, Stark MM, Lanwick MM, et al. Linking data from national trauma and<br />
rehabilitation registry. J <strong>Trauma</strong> 1996; 40:428–36.<br />
2. Rosner MJ, Rosner SD, Johnson AH. Cerebral perfusion pressure: management<br />
protocol and clinical results. J Neurosurg 1995; 83:949–62.<br />
3. Eker C, Asgeirsson B, Grande P-O, et al. Improved outcome after severe head injury<br />
with a new therapy based on principles for brain volume regulation and preserved<br />
microcirculation. Crit Care Med 1998; 26:1881–86.<br />
4. Walia S, Sutcliffe AJ. <strong>The</strong> relationship between blood glucose, mean arterial pressure<br />
and outcome after severe head injury. Injury 2002; 33:339–44.<br />
5. Van den Berghe G, Wouters P, Weekers F, et al. Intensive insulin therapy in critically<br />
ill patients. N Engl J Med 2001; 345:1359–67.<br />
6. Qureshi AI, Suarez JI, Castro A, Bhardwaj A. Use <strong>of</strong> hypertonic saline/acetate infusion<br />
in treatment <strong>of</strong> cerebral edema in patients with head trauma: experience at a<br />
single center. J <strong>Trauma</strong> 1999; 47:659–65.<br />
7. Clifton GL, Miller ER, Choi SC, et al. Lack <strong>of</strong> effect <strong>of</strong> induction <strong>of</strong> hypothermia after<br />
acute brain injury. N Engl J Med 2001; 344:556–63.<br />
8. Perez-Pinzon MA, Alonso O, Kraydieh S, Dietrich WD. Induction <strong>of</strong> tolerance against<br />
traumatic brain injury by ischemic preconditioning. Neuroreport 1999; 10:2951–4.<br />
Pathophysiological Processes Following Toxic <strong>Trauma</strong><br />
Dr David Baker M Phil DM FRCA<br />
Department <strong>of</strong> Anaesthesia and SAMU de Paris<br />
Hopital Necker – Enfants Malades, Paris<br />
Learning Objectives: To present an approach toward the management <strong>of</strong> chemical<br />
and biological agent injuries, which is injury rather than agent specific.<br />
Toxic trauma is a term used to describe the injury caused by mass release <strong>of</strong> a variety<br />
<strong>of</strong> toxic agents. <strong>The</strong>se may be drawn from the spectrum <strong>of</strong> chemical and biological warfare<br />
(CBW) agents or from the many industrial hazardous materials (HAZMAT). <strong>The</strong> term may also<br />
be used to include the longer-term organ failure consequences <strong>of</strong> serious infection.<br />
Traditionally, the approach to the management <strong>of</strong> casualties from chemical agents has<br />
been antidote based, an approach that rests upon early identification <strong>of</strong> the noxious agent.<br />
While this is <strong>of</strong>ten possible in the military sphere, where sophisticated detection and monitoring<br />
systems are available, in civil life, such information may not be possible and treatment<br />
must then respond to presenting signs and symptoms. <strong>The</strong> concept <strong>of</strong> early life support in a<br />
42
<strong>ITACCS</strong> Spring 2003<br />
toxic zone (TOXALS) introduced by <strong>ITACCS</strong> in 1996 has now been widely accepted and the<br />
new approach to CBW agent management is based upon life support coupled with appropriate<br />
antidote therapy where possible.<br />
Consideration <strong>of</strong> the pathophysiological processes following toxic agent exposure provides<br />
a rational platform for prehospital and hospital clinical management. CBW agents can<br />
attack all systems <strong>of</strong> the body, including the central and peripheral nervous systems, the skin<br />
and epithelia, and particularly the respiratory system. <strong>The</strong> latter is vulnerable to attack from<br />
blockage <strong>of</strong> the airways through vesication and excess secretions, from failure <strong>of</strong> central control<br />
and peripheral neuromuscular transmission due to disruption <strong>of</strong> the cholinergic transmission<br />
system, and from the development <strong>of</strong> toxic pulmonary oedema. Certain classes <strong>of</strong><br />
agent are clearly associated with different processes: nerve agents and neurotoxins have a<br />
direct effect on synaptic and neural transmission while the classic war gases such as phosgene<br />
and industrial agents such as methyl isocyanate have been demonstrated to cause mass toxic<br />
pulmonary edema. Vesicant agents such as mustard gas are now known to have effects at all<br />
levels <strong>of</strong> the respiratory tree apart from causing vesication <strong>of</strong> the dermis.<br />
<strong>The</strong> explosion in research into the cholinergic transmission system that followed<br />
World War II led to a good understanding <strong>of</strong> the pathophysiology <strong>of</strong> acetylcholinesterase inhibition<br />
and the development <strong>of</strong> a range <strong>of</strong> antidotes that can be used in both military or civil<br />
exposure. <strong>The</strong>re are valuable lessons to be learned from the management <strong>of</strong> pesticide poisoning,<br />
and the rational use <strong>of</strong> oximes has been reappraised. <strong>The</strong> interest in cholinergic<br />
mechanisms has been matched in recent years by work on the pathogenesis <strong>of</strong> toxic pulmonary<br />
edema and new treatment strategies have resulted. Work has focused on increasing<br />
cellular glutathione (GSH) levels as a means <strong>of</strong> preventing lipid–peroxidation induced pulmonary<br />
edema. <strong>The</strong>re are suggestions that N-acetyl cysteine may provide protection by maintaining<br />
GSH levels and inhibiting production <strong>of</strong> inflammatory leukotrienes.<br />
Further application <strong>of</strong> knowledge gained from normal clinical research into disease<br />
mechanisms is likely to have a continued beneficial effect on the management <strong>of</strong> the rarer circumstances<br />
<strong>of</strong> mass toxic trauma.<br />
End Tidal CO2: From Airway to Cardiac Output<br />
Marvin A. Wayne, MD, FACEP<br />
Associate Clinical Pr<strong>of</strong>essor, University <strong>of</strong> Washington<br />
Assistant Clinical Pr<strong>of</strong>essor, Yale University<br />
Emergency Medical Services, Bellingham, Washington, USA<br />
Learning Objectives: 1) to review the physiology <strong>of</strong> CO2 production and excretion<br />
and 2) to describe the use <strong>of</strong> ETCO2 to monitor ventilation, tube placement, and indirect<br />
cardiac output.<br />
Principles. A capnometer projects filtered infrared light at a wavelength <strong>of</strong> 4.28 um<br />
across a sample chamber to a semiconductor detector. <strong>The</strong> detector generates an electrical<br />
signal inversely proportional to the light absorbed by CO2 in the sample chamber, which ultimately<br />
is translated into a capnometer value (CO2 concentration). Capnography is the realtime<br />
graphic depiction <strong>of</strong> CO2 concentration throughout the respiratory cycle.<br />
Gas sampling may be by “sidestream” or “mainstream” technique. Mainstream technique<br />
incorporates the sensor into the ventilation circuit. Sidestream technique samples<br />
exchanged gases through a small branch tube from the ventilation circuit or breathing<br />
patient. Sidestream sampling is more susceptible to clogging with water or mucus and results<br />
in a slower response time compared with mainstream capnometry.<br />
Applications. Carbon dioxide is a by-product <strong>of</strong> cellular metabolism, constantly produced<br />
in proportion to the cellular metabolic rate. Because CO2 is transported via the bloodstream<br />
for elimination by the lungs, measurement <strong>of</strong> end-tidal CO2 (ET CO2) may reflect the<br />
cellular metabolic rate, vascular system intactness, cardiac function, and ventilation.<br />
Capnometry and capnography enjoy widespread use in anesthesia and the ICU. Similar technology<br />
appears transferable to the emergency department and prehospital setting.<br />
Decreased CO2 concentrations, detected by capnometry or capnography, are indicative<br />
<strong>of</strong> endotracheal tube disconnection, extubation, obstruction, or misplacement. ETCO2<br />
was found more reliable than direct visualization, auscultation, or observation <strong>of</strong> chest wall<br />
motion. Capnometry/capnography can confirm esophageal intubation within one respiratory<br />
cycle, whereas pulse oximetry may not detect desaturation for several minutes in the preoxygenated<br />
patient. For these important reasons, capnometry is strongly advocated in the<br />
emergency department and prehospital arena, where physical diagnosis is difficult at best<br />
and patient motion increases the risk <strong>of</strong> endotracheal tube displacement.<br />
Capnometry and capnography may be useful for assessing the effects <strong>of</strong> cardiopulmonary<br />
resuscitation (CPR). During cardiopulmonary arrest, CO2 is neither efficiently transported<br />
to, nor expired from the lungs, resulting in decreased ETCO2. A rising ETCO2 may be<br />
the first sign <strong>of</strong> improved patient status during CPR. CO2 concentrations as measured by capnometry<br />
have been shown to correlate well with coronary perfusion pressure during CPR.<br />
<strong>The</strong>se data may suggest prognostic application <strong>of</strong> capnometry. Capnogram waveform analysis<br />
enhances the specificity <strong>of</strong> capnometric ETCO2 measurements. Baseline changes may indicate<br />
CO2 rebreathing, while slope changes may indicate resistance that occurs with endotracheal<br />
tube kinking or expiratory obstruction. “Staircase effects” in the capnogram descending limb<br />
may be seen in situations such as pneumothorax. <strong>The</strong>se applications <strong>of</strong> capnography and capnometry<br />
are important in the emergency department and prehospital setting.<br />
Recently a new dimension has been added with the introduction <strong>of</strong> noninvasive cardiac<br />
output. This system utilizes a CO2 Fick principle to simulate the equivalency <strong>of</strong> an O2<br />
Fick application. Initially usable only on intubated patients, this has now been expanded to<br />
those spontaneously breathing. This system combines ETCO2, flow, and differential dead<br />
space rebreathing to non-invasively accomplish this.<br />
Limitations. While highly accurate, in certain clinical situations the ability <strong>of</strong> capnometric<br />
measurement to estimate arterial CO2 tension (PaCO2) is hampered. In healthy<br />
patients with well-matched alveolar ventilation and perfusion, ET CO2 estimates PaCO2 within<br />
2 or 3 mmHg. When expired gas is from poorly or nonperfused alveoli (ventilation-perfusion<br />
ratio, or V/Q, mismatching), ETCO2 underestimates PaCO2. V/Q mismatching has multiple<br />
etiologies, including body position changes, acute and chronic pulmonary disease, and<br />
adult respiratory distress syndrome. While absolute values <strong>of</strong> CO2 concentration may be inaccurate<br />
in these circumstances, trend information may remain valuable. Also, the arterial-alveolar<br />
CO2 difference may be calculated in these patients. <strong>The</strong> arterial-alveolar difference, a-<br />
ADCO2, is the difference between arterial CO2 and end tidal CO2 (ET CO2). Normally this<br />
difference is small (2–3 mmHg) in patients with normal physiology and without cardiovascular<br />
or pulmonary disease. <strong>The</strong> a-ADCO2 difference may be elevated due to incomplete emptying,<br />
shunt perfusion, or dead space ventilation.<br />
In shunt perfusion, a particular lung unit is underventilated relative to the amount <strong>of</strong><br />
perfusion (normal 5L blood flow to 4L ventilation). Here the a-ADCO2 difference will be<br />
slightly elevated in the range <strong>of</strong> 5 to10 mmHg. This small difference is related to the efficiency<br />
<strong>of</strong> the lung and the excellent diffusability <strong>of</strong> CO2.<br />
In dead space ventilation, a particular lung unit is underperfused relative to the<br />
amount <strong>of</strong> ventilation. Dead space ventilation widens the a-ADCO2 much more than does<br />
shunt perfusion alone. This difference may be 10 to 20 mmHg or more. Further, dead space<br />
ventilation and shunt perfusion are not mutually exclusive and may both occur to some<br />
degree in the same patient.<br />
Conclusion. Capnometry/capnography are <strong>of</strong> confirmed value in the hospital setting,<br />
and their applications continue to broaden. Situations unique to the out-<strong>of</strong>-hospital environment<br />
invite their rapid extrapolation to the prehospital setting. <strong>The</strong>ir ultimate value will<br />
depend upon the training, level <strong>of</strong> understanding, and clinical acumen <strong>of</strong> emergency care<br />
providers. New application to allow noninvasive cardiac output will provide a viable alternative<br />
to invasive systems.<br />
A New Approach to Monitoring Early Hemodynamic Performance:<br />
Transesophageal Echo Doppler Ultrasound<br />
Yves Lambert, Olivier Richard, Pascal Renoux<br />
Service d’Aide Médicale Urgente (SAMU 78) & Service Mobile d’Urgence et de<br />
Réanimation<br />
Versailles Hospital, Le Chesnay, France<br />
Early resuscitation <strong>of</strong> severe trauma is first based on physical examination like heart<br />
rate and arterial blood pressure. <strong>The</strong>se parameters are not accurate enough to give a reliable<br />
circulatory status <strong>of</strong> the patient. <strong>The</strong>rapeutic adjustments based on these clinical parameters<br />
are thus difficult to implement and control, even after an initial aggressive therapy. <strong>The</strong> outcoming<br />
<strong>of</strong> the Transesophageal Echo Doppler system, which is a new noninvasive or light<br />
invasive hemodynamic monitor, could lead to an interesting approach in the rapid management<br />
<strong>of</strong> severe trauma patients. Early detection <strong>of</strong> cardiocirculatory disorders and prompt<br />
adequate treatment in order to prevent serious complication like organ failure are required<br />
during the very first hours after trauma.<br />
Transesophageal Echo Doppler monitoring is easy to use and reproducible. On the<br />
trauma field or in the emergency room, the rapid settlement <strong>of</strong> the TEE is a major asset which<br />
allows to obtain a hemodynamic pr<strong>of</strong>ile in just a few minutes. Its logical first use gives the<br />
chance, in clinical practice, to adjust the therapy based on the displayed hemodynamic<br />
parameters: aortic blood flow, stroke volume in the aorta and total systemic vascular resistance<br />
<strong>of</strong> the aortic circuit.<br />
• For severe head trauma patients with no active bleeding, in order to maintain a<br />
mean arterial blood pressure (MABP) <strong>of</strong> 90 mmHg and avoid a secondary cerebral ischemia,<br />
we highly suggest a continuous measurement <strong>of</strong> MABP. Thus, interpreting the arterial blood<br />
pressure data correlated to ABF, Sva and TSVRa, the therapy can be orientated either toward<br />
fluid loading or toward the use <strong>of</strong> catecholamines, i.e., when vascular resistances are low with<br />
a normal flow (neurogenic hypotension). In all cases, continuous monitoring and trends<br />
allow to assess a real time hemodynamic status and help to adjust treatment.<br />
• For polytrauma patients (penetrating or blunt trauma), with an unstable hemodynamic<br />
condition, the arterial blood pressure and heart rate are useless in estimating the right<br />
amount <strong>of</strong> blood loss. Keeping in mind that treatment should not delay surgery, monitoring Sva<br />
and ABF will help guiding the vascular fluid loading. Increase <strong>of</strong> ABF or Sva will reflect more<br />
accurately efficacy <strong>of</strong> initial treatment than any increase <strong>of</strong> arterial blood pressure.<br />
Another challenge provided by Transesophageal Echo Doppler is the possibility to determine<br />
factors able to predict occurrence <strong>of</strong> MOF. Continuous measurement <strong>of</strong> ABF and Sva as<br />
early as possible after the trauma could help to quantify early low flow and poor tissue perfusion<br />
states. Correlation betwin those variation and occurrence <strong>of</strong> MOF have to be determined.<br />
Minimally invasive, hemodynamic monitoring using the Transesophageal Echo<br />
Doppler approach opens very enthusiastic perspectives. Earlier diagnosis and continuous<br />
monitoring <strong>of</strong> circulatory deficiencies must be very useful for the trauma physician to start<br />
adequate resuscitation and minimize tissue ischemia.<br />
— Session B —<br />
Disaster Management and Emergency Medicine<br />
Co-Chair: Dario Gonzalez, MD, New York, New York, USA<br />
Co-Chair: Andreas Thierbach, MD, Mainz, Germany<br />
<strong>The</strong> <strong>International</strong> Chief Emergency Physician Training Course<br />
Freddy Lippert, MD<br />
<strong>Trauma</strong> Center and Major Incident Command Centre,<br />
H:S Rigshospitalet, Copenhagen University Hospital, Denmark<br />
Learning Objectives: To review the development, content, and importance <strong>of</strong> <strong>The</strong><br />
<strong>International</strong> Chief Emergency Physician Training Course.<br />
Education and training are essential in handling major incidents and disasters. It is an<br />
obligation <strong>of</strong> any medical system to meet these challenges. Guidelines for education and<br />
training in disaster medicine have been proposed. 1<br />
<strong>The</strong> <strong>International</strong> Chief Emergency Physician Training course on Command Incident<br />
Management and Mass Casualty Disasters (ICEP) is one <strong>of</strong> the international courses with a<br />
well-established curriculum.<br />
<strong>The</strong> first CEP course was set up in 1998 by <strong>The</strong> <strong>International</strong> <strong>Trauma</strong> Anesthesia and<br />
Critical Care Society (<strong>ITACCS</strong>) in cooperation with a group <strong>of</strong> leading chief emergency physicians<br />
in Mainz and based on experiences from national German CEP courses. 2<br />
<strong>The</strong> international faculty consists <strong>of</strong> experienced chief emergency physicians and<br />
experts in different fields from various parts <strong>of</strong> the world to cover all issues. Participants make<br />
up an international forum <strong>of</strong> physicians with experiences within prehospital care, trauma<br />
care, emergency medicine, and command incident management. This constellation facilitates<br />
international exchange <strong>of</strong> experiences and ideas.<br />
<strong>The</strong> CEP course has an intensive 40 hours curriculum with lectures, discussions <strong>of</strong> case<br />
reports, excursions, and in-field training. Subjects include epidemiology <strong>of</strong> mass casualty incidents<br />
and disasters, responsibilities and duties <strong>of</strong> the CEP, command and control, triage concepts,<br />
personal protection and equipment, communication devices and techniques, evacuation<br />
and long-range transport, planning for mass gatherings, VIP protection, hostage situations,<br />
counter terrorism, HazMat, bio-threats and chemical warfare, medical relief, and media<br />
contact and management.<br />
Lectures are interactive and most are accompanied by practical training sessions or<br />
tabletop discussions. <strong>The</strong>ory and practical training result in full-scale disaster exercises in<br />
cooperation with all local authorities. 3<br />
This international concept facilitates post-course exchange <strong>of</strong> knowledge and experiences<br />
based on the network established during the 5-day intensive curriculum <strong>of</strong> chief emer-<br />
43
<strong>ITACCS</strong> Spring 2003<br />
gency physicians.<br />
<strong>The</strong> ICEP courses are announced at www.<strong>ITACCS</strong>.com.<br />
References<br />
1. Handbook <strong>of</strong> Disaster Medicine <strong>International</strong> Society <strong>of</strong> Disaster Medicine 2000.<br />
Education and Training, pp 481–95.<br />
2. Müller R, Lipp MDW. <strong>The</strong> First <strong>International</strong> Chief Emergency Physician Training<br />
Course. <strong>Trauma</strong>Care 1998; 8:29–30.<br />
3. Thierbach AR, Lippert FK, Grande CM. <strong>The</strong> <strong>International</strong> Chief Emergency<br />
Physician Training Course on Command Incident Management and Mass Casualty<br />
Disasters. <strong>Trauma</strong>Care, in press.<br />
<strong>The</strong> Effect <strong>of</strong> Select Drugs on Shock in the <strong>Trauma</strong> Patient<br />
Joanne (“Dr. J”) Williams, MD, FAAEM, FACFM<br />
Department <strong>of</strong> Emergency Medicine, Martin Luther King, Jr./Charles R. Drew Medical<br />
Center, Charles R. Drew University <strong>of</strong> Medicine & Science, Los Angeles, California, USA<br />
“He takes a little white heart pill in the morning!”<br />
Learning Objectives:<br />
• To understand the effects <strong>of</strong> prescribed medications, herbal supplements, and<br />
illicit drugs on the clinical presentation <strong>of</strong> shock.<br />
• To review the effects <strong>of</strong> prescription medications and their potential influence<br />
on the assessment <strong>of</strong> trauma patients.<br />
• To appreciate the risk <strong>of</strong> adverse drug reactions, especially in elderly patients<br />
with preexisting conditions.<br />
Many prescribed medications, over-the-counter drugs, social “drugs,” and “herbal<br />
medicinals” may camouflage the clinical presentation <strong>of</strong> the shock syndrome in the trauma<br />
patient. For example, beta blockers may blunt the compensatory tachycardia in hypovolemia.<br />
Alcohol is a central nervous system depressant and vasodilator, potentially affecting Glasgow<br />
Coma Scale assessment or potentiating hypotension. A detailed history <strong>of</strong> prescribed medications,<br />
over-the-counter drugs, herbal supplements, and social “drug” activity must be<br />
sought if the “typical” presentation <strong>of</strong> shock is not consistent with the injury pattern or clinical<br />
appearance <strong>of</strong> the patient.<br />
A working knowledge <strong>of</strong> the pharmacokinetics and pharmacodynamics <strong>of</strong> commonly<br />
prescribed medications and other drugs on various organ systems will aid the clinician in the<br />
overall assessment and management <strong>of</strong> the trauma patient.<br />
Drugs used for the management <strong>of</strong> pre-existing disease may be solely or partially<br />
responsible for inciting cause <strong>of</strong> events leading to injury. Chief “culprits” are insulin and/or<br />
oral hypoglycemics, antihypertensives, and antiarrhythmics.<br />
Many adverse drug effects may be treated expeditiously and effectively if it is recognized<br />
that the drug effect exists. For example, naloxone will reverse the effect <strong>of</strong> opiateinduced<br />
respiratory depression, and 50% dextrose in water will reverse hypoglycemia<br />
induced by insulin and oral hypoglycemics.<br />
More than 35 million Americans are 65 years <strong>of</strong> age or older. <strong>The</strong>re is a high incidence<br />
<strong>of</strong> diabetes mellitus and cardiovascular disease in the elderly. Many in this patient population<br />
are dependent on prescribed drugs for maintenance <strong>of</strong> health and, as a result, the elderly are<br />
more at risk for an adverse drug reaction.<br />
Unfortunately, most herbal medications and supplements are not yet regulated by the<br />
Food and Drug Administration and may be purchased readily without prescription.<br />
Consumption <strong>of</strong> these “natural drugs” has increased significantly with the popularity <strong>of</strong><br />
Internet sales and distribution.<br />
Lessons Learned 911<br />
Dario Gonzalez, MD, FACEP<br />
Medical Director, Office <strong>of</strong> Emergency Management, City <strong>of</strong> New York, Brooklyn, New<br />
York, and Albert Einstein College <strong>of</strong> Medicine, Bronx, New York, USA<br />
Learning Objectives:<br />
1. Student will be presented three core issues related to the problems associated<br />
with the 911 disaster.<br />
2. <strong>The</strong> student will be presented with basic lessons learned from the discussed<br />
problems.<br />
3. <strong>The</strong> student will be able to appreciate the need for pre-planning and policy<br />
development for disaster response.<br />
At 0845 on September 11, 2001, hijacked commercial airliners crashed into World<br />
Trade Center (WTC) Complex. This resulted in the collapse <strong>of</strong> the North and South Towers<br />
(each 110 stories). Fire Department City <strong>of</strong> New York (FDNY) and other New York City emergency<br />
responders initiated building evacuation, rescue, and fire suppression activities. <strong>The</strong><br />
collapse <strong>of</strong> the towers killed 450 responders, including much <strong>of</strong> the top leadership <strong>of</strong> the Fire<br />
Department <strong>of</strong> New York City, who were operating within the towers as the on-scene incident<br />
command.<br />
Incident Command Structure. <strong>The</strong> collapse and subsequent death <strong>of</strong> these key<br />
personnel resulted in a command void within the fire department. An effective command<br />
structure is essential to resolve four critical issues: scene control, event mitigation, resource<br />
coordination, and site safety.<br />
<strong>The</strong> command structure did develop with time, but the delays encountered in reestablishing<br />
a command and control structure had significant operational, health, and safety consequences.<br />
<strong>The</strong> development <strong>of</strong> a cohesive incident command structure allowed the transition<br />
from victim rescue operations to body recovery operations and site mitigation.<br />
Lessons Learned:<br />
1. Fire command location must be based on the uniqueness <strong>of</strong> a disaster.<br />
2. Coherent command authority is necessary to coordinate resources.<br />
3. Incident command structure is necessary for the transition and development <strong>of</strong> a<br />
coordinated operational plan.<br />
Hazard Analysis. <strong>The</strong> environment contained hazardous materials, such as jet fuel,<br />
battery acid, asbestos, lead paint, silica, explosives (munitions), radioactive debris, and products<br />
<strong>of</strong> combustion. Traditional site environmental risk-assessment activities had technical<br />
problems. <strong>The</strong> ever-present WTC dust was composed <strong>of</strong> silica (windows), concrete, smoke,<br />
cremated/shredded human remains, and unknown irritants. Its prolonged inhalation ultimately<br />
led to the “World Trade Center cough.” Loss <strong>of</strong> the incident command and the nature<br />
<strong>of</strong> the event resulted in an overall poor personal protective equipment (PPE) compliance rate.<br />
Efforts were made to qualitatively and quantitatively define the Ground Zero atmospheric<br />
environment. <strong>The</strong> environmental readings that were eventually obtained were confusing,<br />
contradictory, and difficult to correlate with human health risk analysis.<br />
Lessons Learned:<br />
1. Environmental data are difficult to interpret and quantify. Numbers in a vacuum<br />
only serve to confuse and alarm the public and emergency responders.<br />
2. Policies for the appropriate use <strong>of</strong> PPE during disaster responses must be enforced.<br />
3. Incident site hazard information must be collected rapidly and accurately.<br />
4. Technologies that can provide rescuers real-time information about their environment<br />
(e.g., sampling and pluming models) are needed.<br />
Volunteerism. Volunteerism after the WTC attack resulted in increased death rate for<br />
FDNY and police, due to the self-assignment by <strong>of</strong>f duty personnel. Civilian volunteers arrived<br />
without appropriate protective equipment and worked in some <strong>of</strong> the most hazardous locations,<br />
outside the direction <strong>of</strong> the incident commander. <strong>The</strong>ir presence added to the confusion<br />
and increased the safety and rescue responsibilities <strong>of</strong> the command structure. <strong>The</strong> massive<br />
outpouring <strong>of</strong> volunteer involvement in the response was heartwarming but became<br />
problematic.<br />
Conclusion. <strong>The</strong> events surrounding September 11 posed unique challenges for the<br />
City <strong>of</strong> New York. Its uniqueness required emergency responders to assume new roles and<br />
responsibilities. <strong>The</strong> events surrounding large-scale disasters have a wide range <strong>of</strong> hazards.<br />
<strong>The</strong> more complicated the event, the greater the potential for multiple complex environmental<br />
threats. <strong>The</strong> World Trade Center incident began as an urgent response (days) and<br />
transitioned into a sustained recovery campaign (18 months).<br />
<strong>The</strong>re should be procedures in place to ensure 1) appropriate use <strong>of</strong> PPE, 2) timely<br />
and accurate hazard assessment, and 3) site management.<br />
Organization <strong>of</strong> Medical Systems Under Repeat Terror Attacks<br />
Eran Tal-Or, MD, 1 Gila Hyams, RN, MA, 1 Guy Lin, MD,2 Amitai Ziv, MD, 3 Zvi Feigenberg,<br />
MD, 4 Moshe Michaelson, MD 1<br />
1<br />
Rambam Medical Center, Haifa, Israel; 2 Medical Corps, Israel Defense Forces; 3 National<br />
Medical Simulation Center, Tel Aviv, Israel; 4 Magen David Adom, Tel Aviv, Israel<br />
From the start <strong>of</strong> the ‘El-Aksa Intifada’ on 29.09.2000 until 13.03.2003, Israel suffered<br />
753 dead and 5,152 injuries from terror attacks. 523 <strong>of</strong> the dead and 3,844 <strong>of</strong> the injured were<br />
civilians. <strong>The</strong> incidents were bomb attacks in buses, hotels, and clubs and shooting at civilians’<br />
cars. After the first few attacks, the Israeli medical system began to change itself to deal<br />
with these terror incidents. <strong>The</strong> prehospital system, Magen David Adom (MDA), changed its<br />
way <strong>of</strong> working by adding on-call ambulances, creating a debriefing protocol after every incident,<br />
and building a feedback system with the hospitals. Emergency wards reviewed the trauma<br />
practice <strong>of</strong> their staff by using smart simulators in the ‘National Medical Simulation<br />
Center’, and the Israeli <strong>Trauma</strong> Association sent volunteers to help community hospitals get<br />
ready to deal with these injuries and to deal with mass casualties situations (MCS). <strong>The</strong><br />
national MCS committee reviewed and updated MCS protocols to match the new situation.<br />
<strong>The</strong> army found new ways to prepare reserve physicians and medics in a short period <strong>of</strong> time<br />
for the new conditions at work. Out <strong>of</strong> all this, we built an international course for managing<br />
trauma systems and MCS.<br />
Triage: Do We Need New Concepts?<br />
Kristi L. Koenig, MD, FACEP<br />
National Director, Emergency Management Strategic Healthcare Group,<br />
Department <strong>of</strong> Veterans Affairs;<br />
Clinical Pr<strong>of</strong>essor <strong>of</strong> Emergency Medicine, George Washington School <strong>of</strong> Medicine and<br />
Health Sciences, Washington, DC, USA<br />
Learning Objectives:<br />
1. Participants will gain an understanding <strong>of</strong> the differences between traditional<br />
triage and triage <strong>of</strong> mass casualties when health care resources are exceeded.<br />
2. Participants will become familiar with the indications for and methodology <strong>of</strong><br />
Simple Triage and Rapid Treatment (START).<br />
<strong>The</strong> goal <strong>of</strong> standard triage is to identify the sickest patients who require the most<br />
immediate care. Clinicians expend the greatest resources on the most critical patients.<br />
However, in a situation in which health care resources are overwhelmed, patients will die if<br />
standard triage methods are applied. <strong>The</strong> focus <strong>of</strong> triage must shift from treating patients<br />
who are gravely ill or injured to “doing the most good for the most people.”<br />
<strong>The</strong>re currently exists no single “correct” method <strong>of</strong> triage. Varying triage methods<br />
should be applied depending on the type or magnitude <strong>of</strong> the event. Is there a scene? Is the<br />
incident static, or are there likely to be additional casualties over time? Is there access to standard<br />
definitive medical care, or must patients be managed under austere field conditions or<br />
triaged to alternate care sites?<br />
A common method for sorting multiple patients at a disaster scene is Simple Triage and<br />
Rapid Treatment (START). All patients who can walk are directed to move to a location away<br />
from the site. Next, patients are divided into green (“walking wounded”), yellow (“delayed”),<br />
red (“immediate”), and black (“deceased”) groups, based on a quick assessment <strong>of</strong> respirations,<br />
pulse, and mental status. Assessment <strong>of</strong> each patient takes only seconds; the sole treatments<br />
performed are opening an airway or placing direct pressure on external hemorrhage.<br />
Under conditions in which immediate transport to definitive care is unavailable,<br />
Secondary Assessment <strong>of</strong> Victim Endpoint (SAVE) triage may be used. SAVE assumes a local<br />
cadre <strong>of</strong> trained health care providers and decentralized equipment. Triage is a dynamic<br />
process and periodic patient reassessment is crucial.<br />
Traditional triage methods presume a static event that occurs at a single point in time.<br />
However, in a catastrophic setting, there may be multiple pockets <strong>of</strong> casualties spread across<br />
a geographic region. Transportation and communication systems may be disrupted, EMS systems<br />
could be nonfunctional, and definitive care facilities could be unavailable. Traditional<br />
triage tags are inadequate for medical documentation during a dynamic event; secondary<br />
examinations and treatment will be necessary.<br />
In non-military settings, mass casualty triage training is limited. Health care providers<br />
are taught to apply resources to the most critically ill or injured patients. It is challenging for<br />
a trained health care pr<strong>of</strong>essional to allow a patient to die, even if this means saving many<br />
other lives. Fortunately, the capacity <strong>of</strong> the U.S. health care system has not been exceeded<br />
since the influenza pandemic <strong>of</strong> 1918. However, many current threats, including a massive<br />
earthquake, pandemic influenza, and some types <strong>of</strong> terrorist attacks would produce more<br />
casualties than could be treated. Surge capacity in the United States is currently lacking for<br />
such a situation; thus, new concepts in triage must be implemented.<br />
44
<strong>ITACCS</strong> Spring 2003<br />
References<br />
1. Koenig KL, Schultz CH. Disaster medicine: advances in local catastrophic disaster<br />
response. Acad Emerg Med 1994; 1:133–6.<br />
2. Schultz CH, Koenig KL, Noji EK. A medical disaster response to reduce immediate<br />
mortality following an earthquake. N Engl J Med 1996; 334(7):438–44.<br />
3. Benson M, Koenig KL, Schultz CH. Disaster triage: START, then SAVE–a new method<br />
<strong>of</strong> dynamic triage for victims <strong>of</strong> a catastrophic earthquake. Prehosp Disaster Med<br />
1996; 11(2):117–24.<br />
4. Koenig KL, Dinerman N, Kuehl AE. Disaster nomenclature–a functional impact<br />
approach: the PICE system. Acad Emerg Med 1996; 3:723–7.<br />
5. Schultz CH, Koenig KL, Noji E. Disaster planning and response. In Marx J,<br />
Hockberger R, Walls R, eds. Rosen’s Emergency Medicine: Concepts and Clinical<br />
Practice, 5th edition. St. Louis, Mosby, 2002.<br />
Databases for Storing Prehospital and Intrahospital Data<br />
Peter A. Oakley, MA, FRCA, MRCGP<br />
Consultant in Anaesthesia and <strong>Trauma</strong>, North Staffordshire Hospital, Stoke-on-Trent,<br />
UK; Senior Research Fellow, Keele University<br />
Databases for Storing Pre-hospital and Intra-hospital Data<br />
Dr. Peter A. Oakley<br />
Consultant in Anaesthesia and <strong>Trauma</strong><br />
University Hospital <strong>of</strong> North Staffordshire<br />
Stoke-on-Trent, Staffordshire, UK<br />
Learning Objectives: To understand the changing requirements for data collection<br />
in trauma care and to appreciate the influences affecting data accuracy.<br />
In a cost-constrained, evidence-based, and digitally competent world, data is precious.<br />
We need it to justify our actions and to point out improvements or pitfalls in care. Its very<br />
necessity creates a tension between unbiased accuracy and the desire to bolster our own<br />
practice. <strong>The</strong> more we are judged on our performance as demonstrated by the data, the higher<br />
the stakes become and the greater the need for transparency. <strong>The</strong>se pressures are further<br />
confounded by the difficulty <strong>of</strong> recording real-time data in an emergency situation and the<br />
inherent uncertainty in the information at the time. Without cost constraints, we would<br />
employ extra scribes to record events while others deliver patient care or we would invest in<br />
labor-intensive media recordings with analytical replay to extract data.<br />
Despite these conflicting constraints, many worthy data systems have been developed<br />
and they have played a pivotal role in trauma care. In its heyday, the Major <strong>Trauma</strong> Outcome<br />
Study (MTOS) allowed an overall comparison <strong>of</strong> mortality in different centres, adjusting for<br />
the variation in anatomical injury and physiological response using the TRISS methodology.<br />
Database development was relatively naïve at the time, leading to data structures that were<br />
somewhat clumsy and were extended ‘by accretion’ as extra variables were added piecemeal<br />
to the whole. In addition, the early focus was on pre-hospital and emergency department<br />
care, neglecting the important contribution <strong>of</strong> definitive care and rehabilitation to outcome<br />
(measured in terms <strong>of</strong> morbidity and disability rather than just mortality).<br />
With the lessons we have learned and the seemingly limitless potential <strong>of</strong> new digital<br />
technology, we are developing new systems. We demand standardization and are keen to<br />
agree on universal data sets. Our greed for completeness haunts us as the list <strong>of</strong> variables<br />
grows ever larger and the problems <strong>of</strong> error, omission, and ‘noise’ remain with us.<br />
Commercial systems such as Collector(, while not inexpensive, have allowed pr<strong>of</strong>essional<br />
s<strong>of</strong>tware developers to enhance the way in which the data is handled. Over 200 centers<br />
worldwide have signed up to Collector’s flexible system. <strong>The</strong> American College <strong>of</strong> Surgeons<br />
has developed its own system, <strong>of</strong>fering the ability to import data from other commercial systems<br />
(including Collector). Its NTRACS( trauma registry, launched in 1992, and the associated<br />
national trauma data bank NTDB( <strong>of</strong>fer national recognition, although only 20-25% <strong>of</strong><br />
Level I-II trauma centers currently subscribe.<br />
In Europe, the demand for unity and standardization is equally strong. After an international<br />
workshop coordinated by the <strong>Trauma</strong> Research and Audit Network (TARN), a<br />
European consensus on the minimum data set for trauma is being established, using the<br />
Delphi technique. TARN, the surviving UK sister <strong>of</strong> MTOS, has commissioned a new webbased<br />
data management system to facilitate remote input <strong>of</strong> and access to data. Although it<br />
incorporates new thinking on the generic nature <strong>of</strong> trauma data as the patient moves from<br />
one location to another (e.g. scene to ER to OR to ICU), other developments await the anticipated<br />
technological surge to allow real-time observations and decision-making to be incorporated<br />
into our trauma data systems.<br />
Bibliography<br />
American College <strong>of</strong> Surgeons <strong>Trauma</strong> Registry: http://www.facs.org/dept/trauma.<br />
Dick WF, Baskett PJ, Grande C, et al. Recommendations for uniform reporting <strong>of</strong> data<br />
following major trauma – the Utstein style. Br J Anaesth 2000; 84:818–9.<br />
<strong>Trauma</strong> Research and Audit Network: http://www.tarn.ac.uk.<br />
Wynn A, Wise M, Wright MJ, et al. Accuracy <strong>of</strong> administrative and trauma registry databases.<br />
J <strong>Trauma</strong> 2001; 51:464–8.<br />
— Session C —<br />
Scientific Free Paper Presentations<br />
Moderators: Enrico M. Camporesi, MD, Syracuse, New York; Adolph H. Giesecke, MD,<br />
Dallas, Texas; John K. Stene, MD, PhD, Hershey, Pennsylvania, USA<br />
Battle Field Anaesthesia: How Different Is It?<br />
Dr. Ankit Sarin and Major Manish Mehrotra<br />
<strong>The</strong> provision <strong>of</strong> anesthesia and critical care is always a big challenge in trauma victims.<br />
It, however, becomes broadly redefined when working in field conditions due to inadequate<br />
logistic support and non-availability <strong>of</strong> optimal working conditions. This is exemplified while<br />
working in a combat zone trauma center.<br />
Military anesthesia has been instrumental in providing care to the wounded since the<br />
discovery <strong>of</strong> anesthesia in 1846 and has made significant progress over the years. Each war<br />
and conflict has required anesthesiologists working in service hospitals to adapt to new challenges<br />
in different environments. This paper provides an insight into the working <strong>of</strong> a forward<br />
military trauma care center located in insurgency-rife Jammu and Kashmir sector. This<br />
part <strong>of</strong> India is at high altitude with extreme cold climate and high wind velocity. Besides the<br />
shelling, altitude, and cold, the area is heavily mined. <strong>The</strong> steep gradient and loose rocky surface<br />
make it prime avalanche territory.<br />
<strong>The</strong> team comprises a single anesthesiologist and a surgeon with necessary ancillary<br />
staff. <strong>The</strong> main operation theatre is inside an underground bunker. We managed 767 casualties<br />
over a period <strong>of</strong> two and a half years (November 1999 to June 2002), out <strong>of</strong> which 587<br />
patients underwent surgery. This included 209 splinter injuries, 191 gunshot wounds, 118<br />
landmine injuries, and 69 grenade injuries.<br />
A standardized protocol using the basics <strong>of</strong> trauma anesthesia was followed. Adequate<br />
wound treatment was given prime importance. Radical primary wound debridement and foreign<br />
body removal accounted for three fourths <strong>of</strong> the procedures. <strong>The</strong> choice <strong>of</strong> anesthesia<br />
was dependent on the site <strong>of</strong> involvement. DA was used for all 23% <strong>of</strong> cases and GA for 19%.<br />
<strong>The</strong> remaining cases were done under regional block anesthesia.<br />
Military experience has shown that the presence <strong>of</strong> expert care in the vicinity <strong>of</strong> a forward<br />
post is a very big moral booster for troops employed in warfare. Prompt optimal care<br />
gives the trauma patient a chance to return to functional life. <strong>The</strong> future challenge for anesthesiologists<br />
involved in trauma care in an advance field surgical unit is to provide tertiary<br />
level care within the available resources and to minimize morbidity and mortality.<br />
Cervical Spine Management in Unconscious Adult <strong>Trauma</strong> Patients: Survey <strong>of</strong><br />
Practice in UK Specialist Centres<br />
Dr. Phil Jones, Mr. John Wadley, Dr. Marie Healy<br />
Royal London Hospital, London, United Kingdom<br />
Learning Objective: To determine how the cervical spine is assessed before discontinuation<br />
<strong>of</strong> immobilisation in unconscious adult trauma patients in UK neurosurgical<br />
centres.<br />
Purpose <strong>of</strong> study: a) to establish if each unit had a written protocol or guidelines to<br />
screen for cervical spine injury, b) to determine the radiological screening tests used routinely<br />
in all unconscious patients, and c) to ascertain whether cervical spine immobilisation<br />
was normally continued until the patient regained consciousness and could be examined<br />
clinically.<br />
Method Used. A postal questionnaire was sent to all neurosurgical centres in the United<br />
Kingdom. Follow-up telephone contact was made if a reply was not received within 6 weeks.<br />
Results. 27 <strong>of</strong> 32 centres responded (84% response rate). <strong>The</strong> following results refer<br />
to the units from whom replies were received: 9% had written guidelines for the radiological<br />
screening tests used routinely in unconscious adults, 6% had a written policy for discontinuing<br />
immobilization, 56% <strong>of</strong> centres used fewer than three plain radiographs (over half <strong>of</strong><br />
these centres did not use computed tomography [CT] routinely). CT scanning was used in<br />
10 centres (37%). Two centres (7%) used dynamic fluoroscopy routinely. One centre used<br />
magnetic resonance imaging (MRI) routinely.<br />
If all radiological investigations were normal, 44% <strong>of</strong> centres discontinued immobilisation<br />
before the patient was awake and could be assessed clinically.<br />
Seven centres (26%) had experience in dynamic flexion-extension fluoroscopy. Three<br />
<strong>of</strong> these believed it was unsafe.<br />
Conclusion. <strong>The</strong>re is little consistency in how the cervical spine is assessed before<br />
the removal <strong>of</strong> immobilisation precautions in UK neurosurgical centres. Although the use <strong>of</strong><br />
plain radiography is ubiquitous, there is wide variation in the number <strong>of</strong> films taken. Routine<br />
use <strong>of</strong> CT is surprisingly low for specialist centres dealing with unconscious trauma victims.<br />
Clinicians in these centres have little experience, and less faith, in the safety <strong>of</strong> dynamic fluoroscopy.<br />
Clinically Relevant Hyperventilation <strong>of</strong> First Aid Providers<br />
Results from Artificial Ventilation<br />
B. Kleine-Weischede, T. Piepho, MD, C. Jaenig, B. B. Wolcke, MD, A. R. Thierbach, MD<br />
Clinic <strong>of</strong> Anesthesiology, Johannes Gutenberg-University, Mainz, Germany<br />
Learning Objective: To investigate the hypothesis that rescuer ventilating an apneic<br />
victim during basic life support (BLS) performing mouth-to-mouth or mouth-to-nose ventilation<br />
suffers from clinically relevant and statistically significant hyperventilation.<br />
Purpose <strong>of</strong> Study. <strong>The</strong> “Guidelines 2000 for Cardiopulmonary Resuscitation and<br />
Emergency Cardiovascular Care–<strong>International</strong> Consensus on Science” recommend a ventilation<br />
volume <strong>of</strong> 10 mL/kg body weight (equivalent to a tidal volume <strong>of</strong> 700 to 1000 mL) without<br />
the use <strong>of</strong> supplemental oxygen in adults during isolated respiratory arrest and two-rescuer<br />
cardiopulmonary resuscitation (CPR). 1 Additionally, a deep breath is recommended<br />
before each ventilation to increase the end-expiratory oxygen concentration <strong>of</strong> the air<br />
exhaled by the first aid provider.<br />
Methods. To investigate the effects <strong>of</strong> these recommendations in healthy volunteers,<br />
test persons were asked to perform isolated artificial ventilation and two-rescuer CPR in a<br />
lung model connected with a BLS mannequin. <strong>The</strong> tidal volume was fixed to 800 mL. <strong>The</strong><br />
breathing rate was set to 12/min for isolated respiratory arrest. In the two-rescuer cardiopulmonary<br />
resuscitation model, it depended primarily on the rate <strong>of</strong> chest compressions (set to<br />
100/min). <strong>The</strong>refore, a breathing rate between 8 and 9/min could be achieved by the test persons.<br />
End-tidal carbon dioxide, oxygen saturation (measured by pulse oximetry), and heart<br />
rate were recorded continuously. Capillary blood gas samples (including capCO 2 ) were collected<br />
before and after the ventilation periods.<br />
Results. Clinically and statistically significant hyperventilation results in first aid<br />
providers performing artificial ventilation during isolated respiratory arrest 2 and two-rescuer<br />
CPR according to the Guidelines 2000. <strong>The</strong> ventilation was associated with a significant<br />
decrease in capillary and end-expiratory carbon dioxide pressure (p
<strong>ITACCS</strong> Spring 2003<br />
with a crash airway.<br />
<strong>The</strong> Statoil Search and Rescue Helicopter Service<br />
Anders Kroken, Flight Nurse, Statoil HNO HMS, Heidrun TLP, Norway<br />
Jørund Resell, MD, Statoil HNO HMS, Stjørdal, Norway<br />
Arne Bere, Flight Nurse, Statoil Tampen HMS, Statfjord B, Norway<br />
Guttorm Brattebø, MD, Anestesi- og intensivavd., Haukeland sykehus, Norway<br />
Eva Shammas, MD, Statoil Tampen HMS, Statfjord B, Norway<br />
Learning Objective: To describe and demonstrate the use <strong>of</strong> <strong>of</strong>fshore stationed SAR<br />
helicopters in emergency situations at <strong>of</strong>fshore oil installations.<br />
Oil companies operating in the North Sea and Norwegian Ocean are obliged to have<br />
their own medical aid and health service on board their platforms, even though a national<br />
coast guard service covers all the coast line. <strong>The</strong> quality <strong>of</strong> the service shall be comparable to<br />
onshore primary health care, and even requires the ability <strong>of</strong> qualified transportation <strong>of</strong><br />
injured or critically ill patients.<br />
Supplying oil installations with competent and immediate medical aid requires a helicopter<br />
based service. <strong>The</strong> low frequency <strong>of</strong> emergencies makes it possible to combine the<br />
service <strong>of</strong> ambulance transportation with tasks concerning surveillance <strong>of</strong> oil spills as well as<br />
search and rescue operations.<br />
<strong>The</strong> crew consists <strong>of</strong> five members. <strong>The</strong> nurse on board is supposed to be able to handle<br />
emergency medical situations with the help <strong>of</strong> the rescue-man.<br />
Statoil commenced the service at the Statfjord B platform in 1982. Since June 2001, the<br />
Statoil SAR operations include a new service based at the Heidrun platform in the Norwegian<br />
Ocean.<br />
<strong>The</strong> method used is retrospective investigation <strong>of</strong> medical files and flight records.<br />
<strong>The</strong> services in the Norwegian Ocean and the North Sea are demonstrated through<br />
pictures and tables. Descriptions <strong>of</strong> personal qualifications and equipment in use will be<br />
given. <strong>The</strong> main categories <strong>of</strong> tasks will be reviewed and discussed.<br />
<strong>The</strong> efficiency <strong>of</strong> the service is demonstrated by referring a medical case, including<br />
serious trauma to extremities. First aid was given at the platform, and treatment was continued<br />
by the SAR nurse arriving at the installation. Scramble time and flight time was half the<br />
time compared with using an onshore based helicopter.<br />
Results. Diagnoses are summarized and counts are reviewed for the year 2002. <strong>The</strong><br />
counts show a total <strong>of</strong> 78 patients treated at Statfjord and 59 at the Heidrun services. <strong>Trauma</strong>s<br />
counted for 22 and 12 <strong>of</strong> the cases, respectively. SAR operations, including hoisting from vessels,<br />
were performed in 6 and 2 cases each. In the other cases, the SAR helicopters where able<br />
to land on the helideck.<br />
Fourteen percent <strong>of</strong> all treated patients were suggested to have an MI. In comparison,<br />
all traumas accounted for 25% <strong>of</strong> total. Major trauma counted for just 3 <strong>of</strong> these 34 cases,<br />
while the major part <strong>of</strong> traumas were distal fractures and s<strong>of</strong>t tissue wounds. Counts show an<br />
increasing number <strong>of</strong> cases with coronary heart disease, while trauma cases are becoming<br />
fewer and less serious than in the early days <strong>of</strong> oil business <strong>of</strong>fshore.<br />
Conclusion. <strong>The</strong> combination <strong>of</strong> helicopter ambulance with a full SAR service in <strong>of</strong>fshore<br />
industry is an appropriate way <strong>of</strong> gaining a high quality medical emergency service.<br />
Sharing the cost with company emergency tasks like sea-rescue and oil spill surveillance<br />
makes it beneficial to the oil companies. Combining these tasks gives an ambulance service<br />
at lower cost, higher quality, and shorter response time.<br />
Stand-By Intra-Aortic Balloon Occlusion in the Prevention <strong>of</strong> Cardiac Arrest Prior<br />
to Definitive Treatment <strong>of</strong> <strong>Trauma</strong>tic Hemorrhage<br />
Kitoji Takuhiro, MD, Hisashi Matsumoto, MD, Toru Mochizuki, MD, Yuji Kamikawa, MD,<br />
Yuichiro Sakamoto, MD, Yoshiaki Hara, MD, Kunihiro Mashiko, MD, Yasuhiro Yamamoto, MD<br />
Department <strong>of</strong> Emergency and Critical Care Medicine, Nippon Medical School, Chiba<br />
Hokuso Hospital, Chiba, Japan<br />
Learning Objective: To understand the strategies <strong>of</strong> initial treatment for the<br />
patients in hemorrhagic shock due to intra-abdominal hemorrhage or retroperitoneal<br />
hemorrhage.<br />
Purpose <strong>of</strong> Study. Hemorrhagic shock due to intra-abdominal hemorrhage or<br />
retroperitoneal hemorrhage caused by severe liver injury or pelvic fracture may cause cardiac<br />
arrest. How can we prevent cardiac arrest prior to adequate blood transfusion or definitive<br />
treatment such as transcutaneous arterial embolization (TAE), external fixation <strong>of</strong> the pelvis,<br />
or laparotomy? In the present study, we show the usefulness <strong>of</strong> the concept <strong>of</strong> stand-by intraaortic<br />
balloon occlusion (IABO).<br />
Methods. In the present study, a retrospective review <strong>of</strong> trauma patients, in whom<br />
IABO was considered appropriate, was conducted over a 3-year period. For the trauma<br />
patient, prior to the use <strong>of</strong> an IABO catheter, a 9Fr introducer or 18G catheter was inserted<br />
percutaneously so that emergency insertion <strong>of</strong> IABO would be possible. We defined this procedure<br />
as “stand-by IABO”.<br />
Results. We reviewed trauma patients with hemorrhagic shock (BP range, 50–94<br />
mmHg) due to intra-abdominal hemorrhage or retroperitoneal hemorrhage at presentation<br />
and who were still fighting for life. Ten patients were considered to need or potentially need<br />
the use <strong>of</strong> IABO and in whom a 9Fr introducer or 18G catheter had been inserted. Among<br />
them, 7 patients were considered to need “stand-by IABO.” Three patients were considered<br />
to need immediate IABO. Three <strong>of</strong> the 7 “stand-by IABO” patients were non-responders or<br />
transient responders to the initial bolus fluid resuscitation and required later inflation <strong>of</strong> the<br />
IABO balloon.<br />
Conclusion. Stand-by intra-aortic balloon occlusion for preventing cardiac arrest<br />
prior to definitive treatment <strong>of</strong> traumatic hemorrhage appears to be a useful adjunct in some<br />
cases. We recommend preparing stand-by IABO for those patients whose initial vital signs are<br />
unstable and who would have intra-abdominal hemorrhage or retroperitoneal hemorrhage<br />
caused by severe liver injury or pelvic fracture, before their vital signs could deteriorate to the<br />
point where the femoral artery could not be palpated.<br />
Mason’s PU-92 Concept: Rapid Recognition and Treatment <strong>of</strong> the Crash Airway<br />
Andrew M. Mason, MB, BS, MRCS, LRCP, Suffolk Accident Rescue Service, Ipswich, Suffolk,<br />
United Kingdom<br />
James M. Rich, MA, CRNA, Staff Nurse Anesthetist, Department <strong>of</strong> Nurse Anesthesia<br />
Baylor University Medical Center, Dallas, TX, USA<br />
Michael A.E. Ramsay, MD, FRCA, Chief <strong>of</strong> Service, Department <strong>of</strong> Anesthesiology and Pain<br />
Management, Baylor University Medical Center, Dallas, TX, USA<br />
Learning Objective: To understand how to rapidly recognize and treat the patient<br />
Mason’s PU-92 concept 1 was designed to assist with the rapid identification <strong>of</strong> the crash<br />
airway 2 by combining an assessment <strong>of</strong> the level <strong>of</strong> consciousness with the patient’s SpO 2<br />
level. <strong>The</strong> AVPU system specifies four levels <strong>of</strong> consciousness: 1) A (Alert) – signifying that the<br />
patient is alert; awake; responsive to voice; and oriented to person, time, and place; 2) V<br />
(responsive to a Voice) – signifying the patient responds to voice but is not fully oriented to<br />
person, time, or place; 3) P (responsive to a Pain) – signifying that the patient does not<br />
respond to voice but does respond to painful stimuli such as pressure to a nail-bed or the<br />
supraorbital nerve; and 4) U (Unresponsive) – signifying that the patient does not respond<br />
to verbal or painful stimuli. An AVPU score <strong>of</strong> ‘P’ or ‘U’ corresponds to a Glasgow Coma Scale<br />
score <strong>of</strong>
<strong>ITACCS</strong> Spring 2003<br />
tions such as airway assessment; oxygenation and ventilation; aspiration prophylaxis; cervical<br />
spine protection; and confirmation <strong>of</strong> tracheal intubation. However, it differs from other algorithms<br />
in the presentation <strong>of</strong> the six limbs, i.e., 1) first responder limb for providers who generally<br />
do not possess tracheal intubation skills and may or may not have rescue ventilation<br />
skills; 2) nonintubation technique limb, which allows the provider to opt out <strong>of</strong> using tracheal<br />
intubation if the situation dictates and to either continue with a nonrebreathing mask or bagvalve<br />
mask ventilation or proceed with a minimally invasive technique such as Combitube,<br />
COPA, Easy Tube, King LT or LMA; 3) rescue ventilation limb, which provides for rapid insertion<br />
<strong>of</strong> a Combitube or LMA or LMA-Fastrach in the presence <strong>of</strong> a crash airway or failed airway<br />
situation; 4) difficult intubation limb, which provides options for facilitating a difficult<br />
intubation; 5) RSI limb, which focuses on appropriate use <strong>of</strong> rapid sequence intubation; and<br />
6) cricothyrotomy limb for application if rescue ventilation fails.<br />
<strong>The</strong> flowchart assists in improving oxygenation and ventilation regardless <strong>of</strong> the<br />
provider’s skill level. Other contributions include use <strong>of</strong> limiting intubation attempts to avoid<br />
traumatizing the airway or creating a “cannot ventilate–cannot intubate”; 6 “Mason’s PU-92<br />
Concept” for rapid recognition <strong>of</strong> the crash airway 1 ; maxims and special considerations to<br />
facilitate airway safety; technique adjustment if adequate oxygenation is not being attained or<br />
maintained; clear criteria for application <strong>of</strong> rescue ventilation to treat a failed or crash airway;<br />
criteria for application <strong>of</strong> cricothyrotomy; and near-failsafe devices in all locations to confirm<br />
tracheal intubation. Use <strong>of</strong> color to show safe blocks, danger blocks, decision blocks, consideration<br />
blocks, and action blocks aids in instruction and acquisition <strong>of</strong> information.<br />
Conclusions. A flowchart has been developed that can be used by all practitioners<br />
involved in emergency airway management. It provides a platform for teaching critical decisionmaking<br />
skills to diverse practitioners. It is hoped that a tool can be developed to measure its<br />
effect on providers’ ability to apply critical decision-making skills effectively in emergency airway<br />
management. <strong>The</strong> flowchart is germane to that common area <strong>of</strong> emergency airway management<br />
where the diverse fields <strong>of</strong> anesthesiology, emergency medicine, and prehospital care coincide.<br />
References<br />
1. Mason AM. <strong>The</strong> Laryngeal Mask Airway (LMA) & Intubating Laryngeal Mask Airway<br />
(ILMA) in Prehospital <strong>Trauma</strong> Care. Presentation at the Royal College <strong>of</strong><br />
Anaesthetists, London, May 13, 2002.<br />
2. ASA Task Force on Management <strong>of</strong> the Difficult Airway. Anesthesiology 1993; 78:597.<br />
3. Gabbott DA. Management <strong>of</strong> the airway and ventilation during resuscitation. Br J<br />
Anaesth 1997; 79:159–71.<br />
4. Walls RW. <strong>The</strong> emergency airway algorithms. In Walls RW, ed. Manual <strong>of</strong> Emergency<br />
Airway Management. Philadelphia: Lippincott Williams & Wilkins, 2000, pp 16–26.<br />
5. Smith CE, Grande CM, Wayne MA, et al. <strong>ITACCS</strong> Rapid Sequence Intubation (RSI)<br />
in <strong>Trauma</strong> [poster]. 10th ATACCS. Baltimore, May 1997.<br />
6. Benum<strong>of</strong> JL. <strong>The</strong> ASA Difficult Airway Algorithm: new thoughts and considerations.<br />
In Hagberg CA, ed. Handbook <strong>of</strong> Difficult Airway Management. Philadelphia:<br />
Churchill Livingstone, 2000, pp 31–48.<br />
Friday, May 16, 2003<br />
Simultaneous Morning Sessions<br />
— Session A —<br />
<strong>Trauma</strong> Airway Management<br />
Chair: Andreas Thierbach, MD, Mainz, Germany<br />
RECOGNIZED<br />
PROPER<br />
PREPARATION<br />
AWAKE<br />
INTUBATION<br />
CHOICES* +<br />
SUCCEED<br />
SURGICAL<br />
AIRWAY<br />
CANCEL CASE,<br />
REGROUP (e.g.,<br />
different personnel/<br />
equipment)<br />
DIFFICULT AIRWAY<br />
UNCOOPERATIVE<br />
PATIENT<br />
UNRECOGNIZED<br />
MASK VENT<br />
NONPROLEMATIC<br />
FAIL<br />
REGIONAL<br />
ANESTHESIA<br />
(if possible and<br />
surgery reversible)<br />
GENERAL<br />
ANESTHESIA<br />
+ PARALYSIS ++<br />
MASK<br />
VENTILATION<br />
AWAKEN<br />
YES<br />
(non emergency<br />
pathway)<br />
INTUBATION<br />
CHOICES * +<br />
FAIL<br />
+<br />
NO<br />
(emergency<br />
pathway)<br />
SUCCEED<br />
SURGICAL<br />
AIRWAY<br />
++<br />
+<br />
Always consider calling for help (e.g., technical,<br />
medical, surgical etc.) when difficulty with mask<br />
ventilation and/or tracheal intubation is encountered<br />
Consider the need to preserve spontaneous<br />
ventilation<br />
LMA,<br />
COMBITUBE,<br />
TTJV<br />
AWAKEN<br />
INTUBATION<br />
CHOICES* +<br />
SURGICAL<br />
AIRWAY<br />
CONFIRM<br />
when<br />
EXTUBATE<br />
OVER JET<br />
appropriate<br />
STYLET<br />
ANESTHESIA WITH<br />
MASK VENTILATION<br />
Figure 1. <strong>The</strong> ASA Difficult Airway Algorithm from References 1 and 2.<br />
*Non-surgical tracheal intubation choices consist <strong>of</strong> laryngoscopy with a rigid laryngoscope blade (many types), blind<br />
orotracheal or nasotracheal technique, fiberoptic/stylet technique, retrograde technique, illuminating stylet, rigid<br />
bronchoscope, percutaneous dilational tracheal entry. See Reference 2 for a complete discussion <strong>of</strong> these TI choices.<br />
<strong>The</strong> ASA Difficult Airway Algorithm As It Pertains to <strong>Trauma</strong> Patients<br />
William C. Wilson, MD<br />
University <strong>of</strong> California, San Diego School <strong>of</strong> Medicine, San Diego, California, USA<br />
Learning Objectives: 1) to review the ASA difficult airway (DA) algorithm, 2) to recognize<br />
that most <strong>of</strong> the important elements <strong>of</strong> the algorithm apply equally well to the elective<br />
setting and the emergency trauma setting, and 3) to identify special considerations<br />
and solutions related to trauma airway situations.<br />
Pre-induction Airway Evaluation. <strong>The</strong> ASA DA Algorithm (Figure 1) begins with<br />
recognition <strong>of</strong> airway difficulty. Whenever the patient is recognized to have a difficult airway<br />
(and the patient is stable and cooperative), the clinician should secure the airway awake.<br />
Awake Limb <strong>of</strong> the ASA Algorithm. <strong>The</strong> ASA DA algorithm does not endorse any<br />
particular airway technique. However, it does emphasize that the patient must be properly<br />
prepared (both mentally and physically) for an awake technique, and the physician must<br />
ensure continuation <strong>of</strong> spontaneous ventilation and adequacy <strong>of</strong> O 2 saturation.<br />
Stopping to Come Back Another Day (Seldom an Option with <strong>Trauma</strong>). If<br />
awake intubation techniques fail, one can, and should, consider stopping, maintaining spontaneous<br />
ventilation, allowing the patient to recover from topicalization or sedatives and<br />
resume management later with a better plan (other equipment/personnel). However, stopping<br />
is seldom an option when managing the emergency trauma airway.<br />
Anesthetized or Uncooperative Patient Limb <strong>of</strong> ASA Algorithm. <strong>The</strong>re are three<br />
common conditions when the need arises to intubate the trachea <strong>of</strong> an unconscious or anesthetized<br />
patient with a DA: 1) <strong>The</strong> clinician fails to recognize a difficult airway in preoperative<br />
evaluation prior to the induction <strong>of</strong> anesthesia. 2) <strong>The</strong> DA patient who is already unconscious<br />
prior to being assessed by the trauma anesthesiologist. 3) <strong>The</strong> patient has an obvious DA but<br />
is hemodynamically unstable (i.e., following trauma) or absolutely refuses to cooperate with<br />
an awake intubation (child, or mentally retarded, or drugged or head-injured adult). Once<br />
the patient is anesthetized or is rendered apneic or presents comatose and the trachea cannot<br />
be intubated, O 2 -enriched mask ventilation is attempted. If adequate, a number <strong>of</strong> intubation<br />
techniques may be employed. Techniques allowing continuous ventilation during airway<br />
manipulations are favored over those requiring an interruption <strong>of</strong> mask ventilation (e.g.,<br />
fiberoptic bronchoscope, via an LMA or an airway intubating mask, with self-sealing<br />
diaphragm). Alternatively, techniques requiring a cessation <strong>of</strong> ventilation (at least temporarily)<br />
can be employed (these techniques are relatively contraindicated for patients with large<br />
right-to-left transpulmonary shunt or decreased FRC).<br />
Three Emergency Airway Aides (LMA , Combitube, and TTJV) Assist the<br />
Cannot Intubate/Cannot Ventilate Patient. When confronted with this type <strong>of</strong> patient,<br />
three alternative ventilation methods should be considered (Combitube, LMA, TTJV). Once<br />
ventilation is established with one <strong>of</strong> these methods, other more definitive (and time-consuming)<br />
techniques <strong>of</strong> airway management may be considered.<br />
Confirmation <strong>of</strong> Endotracheal Tube Position. Immediately after the patient’s trachea<br />
is intubated, one must confirm endotracheal tube position with end tidal CO 2 measurement.<br />
If end tidal CO 2 measurement is unavailable, the Wee’s esophageal detector device<br />
is reasonably reliable (close to 100% sensitive and specific).<br />
Extubation or Endotracheal Tube Change <strong>of</strong> the Difficult Airway. If the conditions<br />
that caused the airway to be difficult to intubate still exist at the time <strong>of</strong> extubation, or<br />
if new DA conditions exist (e.g., airway edema, Halo), then the trachea should be extubated<br />
over an airway exchange catheter and/or with the assistance <strong>of</strong> a fiberoptic bronchoscope.<br />
References<br />
1. Benum<strong>of</strong> JL. Laryngeal mask airway and the ASA difficult airway algorithm..<br />
Anesthesiology 1996; 84:686-99.<br />
2. Wilson WC, Benum<strong>of</strong> JL. Pathophysiology evaluation and treatment <strong>of</strong> the difficult<br />
airway. Anesthesiol Clin North Am 1998; 16(1):29-75.<br />
Controversies and Obstacles to Airway Training for Paramedics<br />
Adolph H. Giesecke, MD<br />
Retired Jenkins Pr<strong>of</strong>essor and Former Chairman, Anesthesiology and Pain Management<br />
Univeristy <strong>of</strong> Texas Southwestern Medical School, Dallas, Texas, USA<br />
Medical doctors, paramedics, and educators all agree that paramedics should be taught<br />
management <strong>of</strong> the airway. Curriculum should include evaluation <strong>of</strong> the airway and breathing,<br />
airway-clearing maneuvers, bag and mask ventilation, oral and nasal airway insertion, and<br />
endotracheal intubation. Teaching methods should include lectures, teaching movies,<br />
manikin practice, and experience in an operating room supervised by an anesthesiologist or<br />
nurse anesthetist. Most programs require a minimum <strong>of</strong> five supervised intubations before<br />
the course is complete. <strong>The</strong> supervised OR experience improves the successful attempts in<br />
the field from 50% to 95%.<br />
<strong>The</strong> supervised OR experience carries proven benefits to the paramedic and to the<br />
patients, but it is becoming less and less available over the nation. One by one hospitals, anesthesiologists,<br />
and nurse anesthetists have withdrawn from <strong>of</strong>fering this valuable training to<br />
paramedics. <strong>The</strong> reasons <strong>of</strong>fered include fear <strong>of</strong> liability, advice <strong>of</strong> liability insurance carriers,<br />
problems with informed consent and increasing use <strong>of</strong> the LMA in routine surgery.<br />
I don’t have magic bullets to propose to solve the problem, except to strongly repeat the<br />
time honored argument, “When you have your cardiac arrest, what level <strong>of</strong> success will you<br />
accept from your paramedic: 50% or 95%?” Anesthesiologists and nurse anesthetists must continue<br />
to <strong>of</strong>fer this training. Insurance companies must accept the minimal risk associated with<br />
this training, and we must all work on the problem <strong>of</strong> informed consent. We must also carefully<br />
evaluate the use <strong>of</strong> the LMA and Combitube as rescue airways in emergency medical services.<br />
Airway Management with Penetrating Neck <strong>Trauma</strong><br />
Vance E. Shearer, MD<br />
Associate Pr<strong>of</strong>essor, Department <strong>of</strong> Anesthesiology and Pain Management; University <strong>of</strong><br />
Texas Southwestern Medical Center at Dallas; Dallas, Texas, USA<br />
Learning Objectives: 1) To understand the need for an individualized approach<br />
to patients with penetrating neck injuries, 2) to appreciate the indications for and utility <strong>of</strong><br />
fiberoptic bronchoscopy and retrograde intubation in the management <strong>of</strong> penetrating<br />
neck trauma, 3) to understand the need for topical anesthesia during bronchoscopy, 4) to<br />
realize the dangers associated with blind intubation and direct laryngoscopy during the<br />
management <strong>of</strong> penetrating neck trauma, and 5) to recognize the situations in which creation<br />
<strong>of</strong> a surgical airway is warranted.<br />
<strong>The</strong> airway can be distorted significantly by a penetrating neck injury. Standard management<br />
algorithms do not adequately cover the establishment <strong>of</strong> a secure airway in patients<br />
with this type <strong>of</strong> injury. Until prospective studies are completed, the best technique for intubation<br />
remains controversial; meanwhile, each patient’s airway must be approached on an<br />
individual basis.<br />
47
<strong>ITACCS</strong> Spring 2003<br />
Fiberoptic Bronchoscopy. Awake and spontaneously breathing patients can usually<br />
maintain a patent airway. Spontaneous ventilation avoids the potential complications <strong>of</strong> positive<br />
pressure ventilation, e.g., barotrauma or disruption <strong>of</strong> an injured trachea. Intubation<br />
over a fiberoptic bronchoscope (FOB) has the advantages <strong>of</strong> both an awake, spontaneously<br />
breathing patient and the ability to examine the airway distal to the glottis. In the absence <strong>of</strong><br />
significant bleeding, a tracheal wound can be identified and the ETT cuff placed distal to the<br />
injury. If the wound is sufficiently large or is at the level <strong>of</strong> the cricoid ring, then the intubation<br />
can be aborted and a tracheostomy with local anesthesia performed. Few anesthesia<br />
providers possess pr<strong>of</strong>iciency in awake bronchoscopy under emergency conditions; therefore,<br />
alternative methods <strong>of</strong> securing an airway may be necessary.<br />
For an awake FOB technique, the airway must be anesthetized to avoid coughing, gagging,<br />
and vomiting. Transtracheal injection <strong>of</strong> local anesthetic is probably best avoided in the<br />
management <strong>of</strong> penetrating neck injuries, because it tends to cause significant coughing.<br />
Administration <strong>of</strong> a mixture <strong>of</strong> 4% lidocaine with sterile water through a nebulizer appears to<br />
decrease coughing and gagging during subsequent topicalization <strong>of</strong> the airway and provides adequate<br />
tolerance <strong>of</strong> the ETT. Others have reported that gargling with viscous lidocaine followed<br />
by spraying 4% lidocaine through the suction port <strong>of</strong> an advancing FOB is effective and efficient.<br />
However, we refrain from the use <strong>of</strong> viscous lidocaine for fear <strong>of</strong> dislodging tamponaded hemorrhage.<br />
Whatever technique <strong>of</strong> topicalization is utilized, it is important that the airway is anesthetized<br />
adequately. Topicalization <strong>of</strong> the airway can take 5 to 20 minutes, which may be too long<br />
for some patients, and will not be effective in patients with significant bleeding or secretions.<br />
Blind Intubation. Blind attempts at endotracheal intubation are contraindicated<br />
because they may worsen existing injury, leading to airway obstruction or passage <strong>of</strong> the ETT into<br />
a false passage. An awake patient may cough, buck, or vomit during the attempt, causing loss <strong>of</strong><br />
the airway. <strong>The</strong> sympathetic response in an awake patient may increase heart rate and blood<br />
pressure, overcoming hemostasis and causing an expanding hematoma to distort the airway.<br />
Direct Laryngoscopy. Direct laryngoscopy after rapid sequence induction (RSI) has<br />
a high success rate. However, it is a blind procedure after the ETT passes the glottic opening.<br />
Since there is a small potential for blindly placing the ETT through a tracheal wound, initial<br />
breaths should be administered s<strong>of</strong>tly until the ETT is confirmed to be in the trachea by continuously<br />
expired end-tidal CO 2 .<br />
Fiberoptic-Assisted Direct Laryngoscopy. Although direct laryngoscopy has a high<br />
success rate, the author suggests combining FOB or the Shikani Seeing Stylet with direct<br />
laryngoscopy to decrease the possibility <strong>of</strong> blindly placing the ETT through a tracheal wound.<br />
This technique involves RSI, with placement <strong>of</strong> the FOB (preloaded with an ETT) through the<br />
vocal cords under direct laryngoscopy. <strong>The</strong> addition <strong>of</strong> the FOB allows intubation and inspection<br />
<strong>of</strong> the trachea and helps ensure the ETT cuff is distal to a tracheal injury. <strong>The</strong> FOB may<br />
also stent the airway during ETT passage, thereby avoiding additional trauma to the trachea.<br />
<strong>The</strong> Shikani Seeing Stylet is also ideal for visualizing the airway during intubation. Oxygen can<br />
be insufflated through the FOB’s suction port or the stylet’s side port.<br />
Although the author recommends direct laryngoscopy, especially combined with<br />
fiberoptics, the problem is to identify and predict those patients who will be impossible to<br />
intubate and will require a surgical airway as the primary choice. <strong>The</strong>refore, each patient’s<br />
injuries must be evaluated and managed on an individual basis.<br />
Retrograde Intubation. Retrograde intubation has been successful in patients with<br />
severe maxill<strong>of</strong>acial injuries and therefore may be especially useful with a Zone III pharyngeal<br />
injury. In experienced hands, this technique can be performed rapidly and is especially useful<br />
with airway hemorrhage. However, excessive upper airway tissue destruction and edema<br />
may prevent passage <strong>of</strong> the ETT into the trachea. Much <strong>of</strong> this procedure is blind and may<br />
dislodge a previously tamponaded hematoma, causing massive bleeding.<br />
Surgical Airway. Creation <strong>of</strong> a surgical airway is the best first choice in some situations:<br />
• Failure to intubate<br />
• Cricoid ring injury<br />
• Significant laryngeal injury<br />
• Excessive hemorrhage<br />
• Significant tracheal deviation<br />
• <strong>Trauma</strong>-induced airway obstruction<br />
• Quadriplegia<br />
• Significant upper airway tissue edema and destruction<br />
Expectations. As anesthesia providers, we are called upon to provide airway management<br />
in any area <strong>of</strong> our hospital where the need arises, including critical care units and<br />
the emergency department. Often the circumstances are chaotic and the environment difficult.<br />
Moreover, we can be confronted with an obviously difficult airway–facial trauma, airway<br />
edema or hemorrhage, hematoma <strong>of</strong> the neck, or other anatomic abnormality. Nevertheless,<br />
the expectation is that we will secure the airway in a timely manner while simultaneously<br />
maintaining oxygenation. Though this should always be our goal, it ought be recognized that<br />
it is sometimes an unrealistic expectation.<br />
Airway Evaluation. <strong>The</strong> need and value <strong>of</strong> an adequate and accurate airway exam<br />
cannot be overstated. Predicting a difficult airway can and <strong>of</strong>ten averts catastrophic loss <strong>of</strong><br />
airway control. Careful attention should be paid to predictors <strong>of</strong> difficult bag-valve mask ventilation<br />
as well as those stigmata that might predict difficulty for tracheal intubation.<br />
<strong>The</strong> Emergency Difficult Airway Algorithm. Developed by Murphy, Hagberg,<br />
Walls, et al, it specifically deals with the emergent difficult setting. It is a binary decision tree<br />
specifically designed for use in emergency situations outside the elective anesthesia setting.<br />
It seamlessly couples with the Failed Airway Algorithm.<br />
Predicted Difficult Airway. It is universally held that the best approach is to secure the<br />
airway with the patient awake. In the stable and cooperative trauma patient, this may not be<br />
problematic. However, in the unconscious and/or unstable patient, management becomes far<br />
more urgent and difficult <strong>of</strong>ten because <strong>of</strong> declining cardiovascular and/or respiratory status.<br />
Unpredicted Difficult Airway. This situation can easily degenerate very quickly,<br />
especially if bag-valve mask ventilation is impossible or difficult. If SPO 2 can be maintained<br />
above 90%, more options are available. However, if SPO 2 falls below 90%, time to assure adequate<br />
oxygenation becomes critical and the options for doing so become fewer. In this situation,<br />
one must have the confidence and ability to perform a needle cricothyrotomy or<br />
employ a commercial cricothyrotomy kit in short order.<br />
<strong>The</strong> Failed Airway. Recognition that the situation has become extremely time critical<br />
and preparations for a surgical airway must be made. Initiation <strong>of</strong> this algorithm is triggered<br />
by inability to maintain SPO 2 greater than 90% by bag-valve ventilation after attempt(s)<br />
at tracheal intubation.<br />
<strong>The</strong> Difficult and Failed Airway in the <strong>Trauma</strong> Patient<br />
Jeffrey M. Berman, MD<br />
University <strong>of</strong> North Carolina, Chapel Hill, North Carolina, USA<br />
Learning Objectives: 1) To identify the difficult airway in the trauma patient, 2)<br />
recognize when an intubation failure has occurred, 3) to utilize specific algorithms, 4) to<br />
develop personal strategies for emergency airway management.<br />
<strong>The</strong> Role <strong>of</strong> the Combitube (ETC) and the EasyTube (EzT)<br />
Andreas R. Thierbach, MD<br />
Consultant Anesthesiologist, University <strong>of</strong> Mainz, Mainz, Germany<br />
Learning Objectives: To discuss the function, uses, advantages, and disadvantages<br />
<strong>of</strong> the Combitube and to introduce an enhancement <strong>of</strong> the ETC, the EasyTube.<br />
<strong>The</strong> ETC is a double-lumen tube that is introduced blindly into the mouth, combining<br />
the functions <strong>of</strong> an esophageal obturator airway (EOA) and a conventional endotracheal airway.<br />
It is manufactured in two sizes: Combitube 37 F SA (=small adult) and Combitube 41 F.<br />
<strong>The</strong> device is designed to ventilate the lungs, whether the distal end enters the esophagus<br />
or the trachea. <strong>The</strong> longer channel has an open distal end, and the other channel has a<br />
blind end with multiple small openings at supraglottic level. <strong>The</strong>re is a small-volume distal cuff<br />
and a large-volume proximal cuff designed to obliterate the hypopharynx. If the long tube<br />
enters the esophagus (as it does in the majority <strong>of</strong> cases), the patient is ventilated through the<br />
small openings above the glottic level. <strong>The</strong> tidal volume is directed toward the glottis and is<br />
prevented from passing elsewhere by the inflated distal and hypopharyngeal cuffs. If the tube<br />
enters the trachea, ventilation is performed via the open distal channel.<br />
<strong>The</strong> ETC has been used successfully as an artificial airway during cardiorespiratory<br />
arrest. <strong>The</strong> device has also been evaluated for use by ICU nurses and by paramedics in the<br />
prehospital setting. <strong>The</strong> ETC is an effective substitute for tracheal intubation in cases where<br />
there is a lack <strong>of</strong> expertise or familiarity in endotracheal intubation, or there is an inability to<br />
intubate caused by difficult anatomy, or when patients are trapped in unusual positions.<br />
A disadvantage <strong>of</strong> the ETC is that suctioning <strong>of</strong> the trachea is impossible in the<br />
esophageal position. Complications <strong>of</strong> the device include lacerations <strong>of</strong> the pharynx and<br />
hypopharynx, esophageal or tracheal perforation, and the inability to provide adequate ventilation.<br />
<strong>The</strong> Combitube is, however, contraindicated in the following circumstances: patients<br />
shorter than 4 feet; patients with intact gag reflexes irrespective <strong>of</strong> their level <strong>of</strong> consciousness;<br />
patients with known esophageal pathology; patients who have ingested caustic substances;<br />
and patients with obstruction <strong>of</strong> the upper airways, e.g., foreign bodies and tumors.<br />
Since May 2003, the so-called EasyTube (EzT) has been available on the European market.<br />
<strong>The</strong> device will be available on the U.S. market in 2003. It represents a further development<br />
<strong>of</strong> the ETC. Major advantages <strong>of</strong> the EasyTube include a special double-lumen design,<br />
including a tip resembling a standard endotracheal tube. This tip facilitates tracheal intubation,<br />
but still enables ventilation when positioned in the esophagus. Furthermore, the trachea<br />
is accessible in the esophageal and endotracheal position <strong>of</strong> the tip <strong>of</strong> the tube. <strong>The</strong><br />
48
<strong>ITACCS</strong> Spring 2003<br />
large volume proximal cuff is made <strong>of</strong> Neoprene; therefore, the device is suitable for patients<br />
allergic to latex.<br />
<strong>The</strong> EzT is available in two sizes (41 and 27 Fr), making the device applicable for<br />
patients from a height <strong>of</strong> 90 cm on.<br />
SLAM Emergency Airway Flowchart: Universal Considerations<br />
for the Emergency Airway<br />
James M. Rich, MA, CRNA<br />
Baylor University Medical Center, Dallas, TX, USA<br />
Learning Objective: To understand the need for acquisition <strong>of</strong> critical decisionmaking<br />
skills to effectively deal with a wide range <strong>of</strong> emergency airway situations.<br />
Purpose <strong>of</strong> Work. <strong>The</strong> purpose <strong>of</strong> the work was 1) to collate and organize current<br />
information on emergency airway management in a single flowchart that provides a clear<br />
strategy for effectively dealing with emergency airway situations that occur in and out <strong>of</strong> the<br />
hospital; 2) to teach rapid recognition and treatment <strong>of</strong> a “crash” or “failed” airway; 3) to<br />
assist practitioners in developing critical decision making skills for emergency airway management.<br />
Although it can be applied in the operating room, it was primarily developed for<br />
providers outside the operating room and hospital.<br />
Method Used. A literature review was used to collect current peer-reviewed information<br />
on emergency airway management.<br />
Results. Material was drawn from peer reviewed sources 1–5 to develop a single “all-inone”<br />
flowchart that provides a clear strategy for dealing with a wide array <strong>of</strong> emergency airway<br />
situations. It is similar to other flowcharts in its coverage <strong>of</strong> common airway considerations<br />
such as airway assessment; oxygenation and ventilation; aspiration prophylaxis; cervical<br />
spine protection; and confirmation <strong>of</strong> tracheal intubation. However, it differs from other algorithms<br />
in the presentation <strong>of</strong> the six limbs, i.e., 1) first responder limb for providers who generally<br />
do not possess tracheal intubation skills and may or may not have rescue ventilation<br />
skills; 2) nonintubation technique limb, which allows the provider to opt out <strong>of</strong> using tracheal<br />
intubation if the situation dictates and to either continue with a nonrebreathing mask or bagvalve<br />
mask ventilation or proceed with a minimally invasive technique such as Combitube,<br />
COPA, Easy Tube, King LT or LMA; 3) rescue ventilation limb, which provides for rapid insertion<br />
<strong>of</strong> a Combitube or LMA or LMA-Fastrach in the presence <strong>of</strong> a crash airway or failed airway<br />
situation; 4) difficult intubation limb, which provides options for facilitating a difficult<br />
intubation; 5) RSI limb, which focuses on appropriate use <strong>of</strong> rapid sequence intubation; and<br />
6) cricothyrotomy limb for application if rescue ventilation fails.<br />
<strong>The</strong> flowchart assists in improving oxygenation and ventilation regardless <strong>of</strong> the<br />
provider’s skill level. Other contributions include use <strong>of</strong> limiting intubation attempts to avoid<br />
traumatizing the airway or creating a “cannot ventilate–cannot intubate”; 6 “Mason’s PU-92<br />
Concept” for rapid recognition <strong>of</strong> the crash airway 1 ; maxims and special considerations to<br />
facilitate airway safety; technique adjustment if adequate oxygenation is not being attained or<br />
maintained; clear criteria for application <strong>of</strong> rescue ventilation to treat a failed or crash airway;<br />
criteria for application <strong>of</strong> cricothyrotomy; and near-failsafe devices in all locations to confirm<br />
tracheal intubation. Use <strong>of</strong> color to show safe blocks, danger blocks, decision blocks, consideration<br />
blocks, and action blocks aids in instruction and acquisition <strong>of</strong> information.<br />
Conclusions. A flowchart has been developed that can be used by all practitioners<br />
involved in emergency airway management. It provides a platform for teaching critical decision-making<br />
skills to diverse practitioners. It is hoped that a tool can be developed to measure<br />
its effect on providers’ ability to apply critical decision-making skills effectively in emergency<br />
airway management. <strong>The</strong> flowchart is germane to that common area <strong>of</strong> emergency airway<br />
management where the diverse fields <strong>of</strong> anesthesiology, emergency medicine, and prehospital<br />
care coincide.<br />
References<br />
1. Mason AM. <strong>The</strong> Laryngeal Mask Airway (LMA) & Intubating Laryngeal Mask Airway<br />
(ILMA) in Prehospital <strong>Trauma</strong> Care. Presentation at the Royal College <strong>of</strong><br />
Anaesthetists, London, May 13, 2002.<br />
2. ASA Task Force on Management <strong>of</strong> the Difficult Airway. Anesthesiology 1993; 78:597.<br />
3. Gabbott DA. Management <strong>of</strong> the airway and ventilation during resuscitation. Br J<br />
Anaesth 1997; 79:159–71.<br />
4. Walls RW. <strong>The</strong> emergency airway algorithms. In Walls RW, ed. Manual <strong>of</strong> Emergency<br />
Airway Management. Philadelphia: Lippincott Williams & Wilkins, 2000, pp 16–26.<br />
5. Smith CE, Grande CM, Wayne MA, et al. <strong>ITACCS</strong> Rapid Sequence Intubation (RSI)<br />
in <strong>Trauma</strong> [poster]. 10th ATACCS. Baltimore, May 1997.<br />
6. Benum<strong>of</strong> JL. <strong>The</strong> ASA Difficult Airway Algorithm: new thoughts and considerations.<br />
In Hagberg CA, ed. Handbook <strong>of</strong> Difficult Airway Management. Philadelphia:<br />
Churchill Livingstone, 2000, pp 31–48.<br />
Flexible Fiberoptic Intubation<br />
Freddy Lippert, MD<br />
<strong>Trauma</strong> Center and Major Incident Command Centre, H:S Rigshospitalet, Copenhagen<br />
University Hospital, Copenhagen, Denmark<br />
Learning Objectives. To understand 1) the need for a more prominent role <strong>of</strong><br />
fiberoptic endotracheal intubation (FOI) in difficult airway management, 2) to know the<br />
indications and limitations for the use <strong>of</strong> FOI, and 3) to realize the need for acquiring the<br />
necessary skills and experience during daily practice <strong>of</strong> non-emergency situations.<br />
Difficult Airway Management. Airway management <strong>of</strong> the severely traumatized patient<br />
is <strong>of</strong>ten a challenge. <strong>The</strong> aim is to establish a secure airway. <strong>The</strong> ASA difficult airway algorithm<br />
provides various proposals for safe and simple procedures for solving difficult airway management.<br />
However, the flexible fiberoptic facilitated endotracheal intubation is down the line<br />
in the ASA algorithm, and the surgical airway is an early consideration in the advanced trauma<br />
life support (ATLS) airway algorithm.<br />
Fiberoptic Intubation. Various techniques have being developed. For a safe, awake FOI<br />
technique, the airway must be anesthetized sufficiently to avoid coughing, gagging, and vomiting.<br />
Various techniques have been described but time consumption might be a limitation.<br />
In the conscious patient, transtracheal injection <strong>of</strong> local anesthetic is easy, simple, and effective.<br />
Subsequent topicalization <strong>of</strong> the airway provides further tolerance <strong>of</strong> the fiberoptic<br />
scope, and additional spraying <strong>of</strong> lignocaine through the suction port <strong>of</strong> an advancing<br />
fiberoptic scope is effective and efficient.<br />
Advantages. <strong>The</strong> FOI is a simple, non-traumatic technique, superb to most other technique<br />
in the hands <strong>of</strong> the experienced person. <strong>The</strong> FOI can be used for solving most <strong>of</strong> the<br />
challenges presented in difficult airway management <strong>of</strong> trauma patients. In case <strong>of</strong> a suspected<br />
difficult airway in a spontaneously breathing patient, the fiberoptic approach reveals<br />
the problem, thereby avoiding an emergency “cannot intubate situation”. <strong>The</strong> cervical spine<br />
can be protected and movements <strong>of</strong> the C-spine minimized in case <strong>of</strong> suspected C-spine<br />
injuries. Injury to the airway and penetrating neck injuries can be handled with care and<br />
diagnosed early. Hemodynamic stability is preserved during FOI with topical anesthesia. FOI<br />
provides an immediate and precise confirmation <strong>of</strong> endotracheal tube position.<br />
Disadvantages. <strong>The</strong> major disadvantage <strong>of</strong> FOI is that, like all other emergency techniques,<br />
proper use requires skills and prior experience with the equipment and the procedure.<br />
FOI is more time consuming than successful first-time conventional direct laryngoscopy.<br />
Interruption <strong>of</strong> mask ventilation might be necessary in the apneic patient. Bleeding<br />
in the upper airway is another problem making FOI more difficult or impossible. Other limitations<br />
include the relatively high costs and vulnerability <strong>of</strong> fiberoptic scopes, the immediate<br />
availability <strong>of</strong> equipment, and cleaning and maintenance <strong>of</strong> equipment.<br />
Conclusion. Direct laryngoscopy after rapid sequence induction is usually the first<br />
approach. However, the recognition <strong>of</strong> a possible difficult airway is the main issue. If possible,<br />
keep the patient awake and spontaneously breathing. FOI should be considered early if<br />
skills are available. Nasotracheal intubation is <strong>of</strong>ten easier and permitted even in trauma<br />
patients, however, with the risk <strong>of</strong> bleeding making visualization difficult. Establishing a surgical<br />
airway is not always simple and easy; the FOI is a qualified alternative. Skills end experiences<br />
should be obtained during non-emergency situations<br />
<strong>The</strong> challenge is to predict and identify the patients in whom conventional intubation<br />
is not possible or very difficult and those who will require a surgical airway as the primary<br />
choice. Prospective studies need to demonstrate the future role <strong>of</strong> FOI in emergency care.<br />
Recommended Literature<br />
Ovassapian A. Fiberoptic Endoscopy and the Difficult Airway, 2nd edition. Philadelphia,<br />
Lippincott-Raven, 1996.<br />
— Session B —<br />
Critical Care in the Age <strong>of</strong> Terrorism<br />
Chair: Maureen McCunn, MD, Baltimore, Maryland<br />
<strong>Trauma</strong> Care Around the World:<br />
How We Are Different and How We Are the Same<br />
Maureen McCunn, MD<br />
Medical Director, Neurotrauma Critical Care; Physician Director, Continuous Renal<br />
Replacement <strong>The</strong>rapies; R Adams Cowley Shock <strong>Trauma</strong> Center<br />
University <strong>of</strong> Maryland, Baltimore, Maryland, and<br />
Graduate Candidate, Johns Hopkins University, School <strong>of</strong> Advanced <strong>International</strong><br />
Studies, Washington, DC, USA<br />
<strong>Trauma</strong> . . . “the neglected disease <strong>of</strong> modern society” . . .<br />
Learning Objective: To review differences in trauma care in various countries and<br />
to highlight cultural differences.<br />
Injury is a major public health problem in the United States, developed countries, and<br />
developing nations. Blunt trauma due to vehicular craches, industrial equipment, and falls<br />
occurs across all economic strata, in addition to blast and crush injuries that may be seen in<br />
war-ravaged environments. Penetrating injuries from gunshot wounds, stabs, or landmines<br />
occur not only in combatants but more and more commonly in civilians. All populations are<br />
affected by this growing burden <strong>of</strong> injury.<br />
While published data garnered from studies <strong>of</strong> the epidemiology <strong>of</strong> injury and violence<br />
around the world are increasing, there are few to no data concerning how we can effectively<br />
intervene to implement policies or to change ineffective practices surrounding these issues.<br />
What is acceptable in any given society may not be effective in another due to social, cultural,<br />
or religious differences. <strong>Trauma</strong> care in various cultures may demand multiple paradigms<br />
as a result <strong>of</strong> these differences.<br />
Background and Significance. <strong>The</strong> World Health Organization (WHO) estimates<br />
that injury accounts for 16% <strong>of</strong> all disease worldwide. 1 <strong>The</strong> leading causes <strong>of</strong> death for both<br />
men and women between the ages <strong>of</strong> 15 and 44 years are injury related, and by 2020, injuries<br />
will be the third leading cause <strong>of</strong> death and disability in the world. 2 Interpersonal violence and<br />
war-related mortality account for approximately 5 million deaths. Based on 2000 data, 91% <strong>of</strong><br />
homicides occur in low- and middle-income countries. 3<br />
One <strong>of</strong> every ten Americans was treated for an injury in an emergency department in<br />
2000. 4 Injury is also an increasingly significant health problem in most low-income countries.<br />
However, few studies have investigated the epidemiology <strong>of</strong> injury patterns and even fewer<br />
address strategies for injury prevention. Furthermore, there are no published data that investigate<br />
the impact that social customs, religion, or cultural differences may have on trauma care.<br />
In today’s less-developed countries, infectious diseases remain the leading cause <strong>of</strong><br />
death, but this trend is decreasing and trauma is causing more and more deaths. According<br />
to the WHO report concerning the global burden <strong>of</strong> disease, road traffic craches are predicted<br />
to be the leading cause <strong>of</strong> death in the world by 2020. 5 Fifty percent <strong>of</strong> injured victims die<br />
at the scene in some countries. <strong>The</strong> preventable death rate (PDR) is about 25% in Poland,<br />
30% in Greece, 37% in Italy, and 43% to 62% in the United Kingdom. In the United States, the<br />
PDR dropped from 13% to 7% due to better and more efficient systems <strong>of</strong> trauma care. 6<br />
Unfortunately, there are very little data with regard to traumatic injury in developing nations.<br />
Recent Developments. Progress in the organization and the delivery <strong>of</strong> trauma care<br />
has resulted in decreased mortality. <strong>The</strong>se improvements include the following:<br />
• More rapid prehospital transport<br />
• Increased capabilities for prehospital care/training<br />
• Growth <strong>of</strong> emergency medicine as a specialty<br />
• Development <strong>of</strong> trauma surgery as a specialty<br />
• Advanced <strong>Trauma</strong> Life Support (ATLS) course<br />
• Development/certification <strong>of</strong> trauma centers<br />
Unfortunately, many <strong>of</strong> these changes have not reached developing nations.<br />
Differences in <strong>Trauma</strong> Care. Previous queries into trauma system effectiveness in<br />
the United States and Canada concluded that studies assessing efficacy <strong>of</strong> care rely on hospital<br />
deaths as the primary indicator <strong>of</strong> success or failure. 7 But many patients in developing<br />
nations are not even treated for their injuries ,8,9 so hospital deaths may not be an indication<br />
<strong>of</strong> true morbidity or mortality from traumatic injury. A cluster survey <strong>of</strong> household interviews<br />
has shown that many injuries and deaths in poor nations are not captured by hospital data. 10<br />
Mortality from trauma may be directly correlated with gross national product, 11 such<br />
that mortality declines with increasing economic level. Implementation <strong>of</strong> low-cost improve-<br />
49
<strong>ITACCS</strong> Spring 2003<br />
ments in prehospital trauma care in a developing nation has been shown to decrease mortality<br />
during transport by 50%, with only a 16% required increase in the ambulance service<br />
budget. 12 Another difference in patterns <strong>of</strong> injury in developing nations involves urban versus<br />
rural trauma. 13 Prevention strategies need to differ from those in developed countries and<br />
may need to target nonmedical providers (private citizens) to show a difference.<br />
Despite these recently published statistics, and an increasing recognition <strong>of</strong> injury as a<br />
major public health problem worldwide, limited attention and resources have been paid to<br />
this topic. This lack <strong>of</strong> attention is most notable in low-income countries. <strong>International</strong><br />
forums to define the global burden <strong>of</strong> injury and to make recommendations regarding specific<br />
actions required <strong>of</strong> governments, individual researchers, and donor agencies are only<br />
lately forthcoming. 14,15<br />
This dilemma is made more difficult when injuries resulting from conflict are taken into<br />
account. <strong>The</strong> face <strong>of</strong> modern wars has changed dramatically; the target is no longer the destruction<br />
<strong>of</strong> the opposing army, but rather the destabilization <strong>of</strong> the opponent’s political, social, cultural,<br />
and psychological infrastructure. 16 Civilians have been the major targets in recent wars<br />
(Afghanistan, Lebanon, Kosovo, the Persian Gulf) and account for more than 80% <strong>of</strong> those killed<br />
and wounded. This represents a further burden on the effective delivery <strong>of</strong> trauma care and<br />
resources utilized. Today, warfare is the leading cause <strong>of</strong> traumatic deaths in the world.<br />
Cultural Sensitivity. Problems identified in the chain <strong>of</strong> trauma care (from injury<br />
through hospital discharge and rehabilitation) do not include weak links associated with ethnic<br />
prejudices, religious differences, cultural norms, or gender issues. It is known that there<br />
are social and cultural disparities in substance abuse, 17,18 in decisions regarding end-<strong>of</strong>-life<br />
care, 19 and in functional status measurements <strong>of</strong> health-related outcomes. 20 Studies documenting<br />
the presence <strong>of</strong> racial, ethnic, and socioeconomic disparities in health care have outpaced<br />
articles that describe effective strategies to eliminate disparities. 21 Education in the area<br />
<strong>of</strong> cultural competence, defined as a set <strong>of</strong> skills that allows an individual to increase his/her<br />
understanding <strong>of</strong> cultural differences and similarities within, among, and between groups, is<br />
virtually nil. 22,23<br />
Jean Jacques Rosseau makes the all-important point, in <strong>The</strong> Social Contract (1762),<br />
that “the history, character, habits, religion, economic base and education <strong>of</strong> each people<br />
must be taken into account before setting up machinery.”<br />
Eye to the Future. While technological advances and a more precise understanding<br />
<strong>of</strong> the pathophysiology <strong>of</strong> trauma have led to significant improvements in trauma care in<br />
many developed nations, there has been little attention paid to the majority <strong>of</strong> civilization.<br />
<strong>Trauma</strong> systems are only as effective as their ability to be accessed/utilized. We must focus on<br />
developing effectual programs to improve care and quality <strong>of</strong> life throughout the world.<br />
References<br />
1. World Health Organization. Injury: A Leading Cause <strong>of</strong> the Global Burden <strong>of</strong><br />
Disease. Geneva: World Health Organization, 1999.<br />
2. Murray CJL, Lopez AD. <strong>The</strong> Global Burden <strong>of</strong> Disease. Cambridge, Massachusetts:<br />
Harvard University Press, 1996.<br />
3. Krug EG, Dahlberg LL, Mercy JA, et al (eds). World Report on Violence and Health.<br />
Geneva, World Heath Organization, 2002.<br />
4. Centers for Disease Control Data.<br />
5. Krug EG, Sharma GK, Lozano R: <strong>The</strong> global burden <strong>of</strong> injuries. Am J Public Health<br />
2000; 90(4): 523–6.<br />
6. Bielecki K. <strong>Trauma</strong> care for the year 2000. Przegiad Ledarski 2000; 57:S127–8.<br />
7. Mann NC, Mullins RJ, MacKenzie EJ, et al. Systematic review <strong>of</strong> published evidence<br />
regarding trauma system effectiveness. J <strong>Trauma</strong> 1999; 47:S25–33.<br />
8. Mock CN, nii-Amon-Kotei D, Maier RV. Low utilization <strong>of</strong> formal medical services by<br />
injured persons in a developing nation: health service data underestimate the<br />
importance <strong>of</strong> trauma. J <strong>Trauma</strong> 1997; 42:504–511.<br />
9. Mock CN, Forjuoh SN, Rivara FP. Epidemiology <strong>of</strong> transport-related injuries in<br />
Ghana. Accid Anal and Prev 1999; 31:359–370.<br />
10. Mock CN, Abantanga F, Cummings P, et al. Incidence and outcome <strong>of</strong> injury in<br />
Ghana: a community-based survey. Bull World Health Organ 1999; 77:955–64.<br />
11. Mock CN, Jurkovich GJ, nii-Amon-Kotei D, et al. <strong>Trauma</strong> mortality patterns in three<br />
nations are different economic levels: implications for global trauma system development.<br />
J <strong>Trauma</strong> 1998; 44:804–12.<br />
12. Arreola-Risa C, Mock CN, Lojero-Wheatly L, et al. Low-cost improvements in prehospital<br />
trauma care in a Latin American city. J <strong>Trauma</strong> 2000; 48:119–24.<br />
13. Mock CN, Forjuoh SN, Rivara FP. Epidemiology <strong>of</strong> transport-related injuries in<br />
Ghana. Accid Anal Prev 1999; 31:359–70.<br />
14. Forjuoh SN, Zwi AB, Mock CN. Injury control in Africa: getting governments to do<br />
more. Trop Med Int Health 1998; 3:349–56.<br />
15. World Health Organization and <strong>The</strong> Bone and Joint Decade. <strong>The</strong> burden <strong>of</strong> musculoskeletal<br />
conditions at the start <strong>of</strong> the new millennium: Scientific Group<br />
Meeting, Geneva, January 2000.<br />
16. Aboutanos MB, Baker SP. Wartime civilian injuries: epidemiology and intervention<br />
strategies. J <strong>Trauma</strong> 1997; 43:719–25.<br />
17. Leischow SJ, Ranger-Moore J, Lawrence D. Addressing social and cultural disparities<br />
in tobacco use. Addic Behav 2000; 25:821–31.<br />
18. Rossow I. Alcohol and homicide: a cross-cultural comparison <strong>of</strong> the relationship in<br />
14 European countries. Addic 2001; 96:S77–9.<br />
19. Vincent JL. Cultural differences in end-<strong>of</strong>-life care. Crit Care Med 2001; 29:S52–5.<br />
20. Custers JW, Hoijtink H, van der Net J, et al. Cultural differences in functional status<br />
measurement: analyses <strong>of</strong> person fit according to the Rasch model. Qual Lif Res<br />
2000; 9:571–8.<br />
21. Horowitz CR, Davis MH, Palermo AS, et al. Approaches to eliminating sociocultural<br />
disparities in health. Min Heal Today 2001; 2:33–43.<br />
22.Nunez AE: Transforming cultural competence into cross-cultural efficacy in<br />
women’s health education. Acad Med 2000; 75:1071–80.<br />
23. Mesquita B: Emotions in collectivist and individualist contexts. J Pers Soc Psychol<br />
2001; 80:68–74.<br />
Wartime Civilian Injuries. An Epidemiological Shift in<br />
Terrorism and Complex Disasters<br />
Michel B. Aboutanos, MD, MPH<br />
Medical College <strong>of</strong> Virginia Hospitals, Virginia Commonwealth University. Richmond,<br />
Virginia, USA<br />
Learning Objectives:<br />
1. <strong>The</strong> audience should understand the recent trends in world violence in terms <strong>of</strong><br />
terrorist activities and armed conflicts.<br />
2. <strong>The</strong> audience should understand the risk factors leading to increase morbidity<br />
and mortality in armed conflicts and terrorist events<br />
3. <strong>The</strong> audience should understand the implication <strong>of</strong> blast injuries in terms <strong>of</strong> prevention,<br />
response, and trauma and critical care management.<br />
Background. Two forms <strong>of</strong> world violence, international terrorism and major armed<br />
conflicts, have escalated exponentially in the post-world wars era. Since 1945, 160 wars and<br />
armed conflicts resulted in an estimated 22 millions deaths and over 60 million injuries.<br />
Between 1990 and 2000, 56 different major armed conflicts in 44 different locations were<br />
recorded, with 25 conflicts still active in 2000. 1,2 Similarly, since 1968 over 14,000 international<br />
terrorist attacks have taken place throughout the world. 3,4<br />
Purpose. To delineate the characteristics <strong>of</strong> the recent armed conflicts and the significant<br />
terrorist incidents in terms <strong>of</strong> demographics, method <strong>of</strong> wounding, causes <strong>of</strong> injury, risk<br />
factors, and the implications for the trauma and critical care communities.<br />
Methods. An extensive review <strong>of</strong> governmental documents and published experiences<br />
dealing with wartime injuries and prominent international terrorist incidents from<br />
1961 to 2001. Specific trends in demographics, etiologies, and methods <strong>of</strong> wounding were<br />
delineated along with the contributing risk factors.<br />
Results. A total <strong>of</strong> 392 terrorist incidents were reviewed, accounting for 27,312 casualties<br />
and 5,682 deaths. Seventy percent <strong>of</strong> all terrorist incidents were against civilian targets,<br />
which constituted 92% <strong>of</strong> all casualties. Bombings were the most frequent terrorist events<br />
(44%) and accounted for 74% (20,221) <strong>of</strong> all casualties and over 90% <strong>of</strong> all deaths. Similar<br />
results were observed in recent wars. Civilians were the major targets in recent armed conflicts<br />
and accounted for most <strong>of</strong> the killed and wounded (80%–90%). A shift toward more<br />
powerful explosive devices (artillery shells and mines) was also noted. Whereas noncivilian<br />
victims (army, paramilitary, government agents) were mainly male and restricted to the 21- to<br />
40-year-old age group in both armed conflicts and terrorist incidents, civilian victims were <strong>of</strong><br />
all ages and both genders. <strong>The</strong> risk factors for lethal injuries identified in both wartime and<br />
terrorist incidents were similar and included 1) the intentional targeting <strong>of</strong> civilians, 2) the<br />
confinement <strong>of</strong> a large number <strong>of</strong> people in a single area (bomb shelters and hospitals in the<br />
armed conflicts, transportation vehicles such as buses and commercial airplanes in the terrorist<br />
incidents), 3) personal and environmental vulnerability <strong>of</strong> the targeted victims, and 4)<br />
the exponential increase in firepower and lethality <strong>of</strong> modern explosives. <strong>The</strong>se factors also<br />
lead to higher mortality rates among critically injured survivors due to the enormous number<br />
<strong>of</strong> wounded from secondary blast injuries that can overwhelm triage, treatment, and<br />
resource/personnel allocation.<br />
Conclusion. In both wartime and terrorist incidents, civilians are now the primary targets.<br />
An epidemiological shift in the demographics <strong>of</strong> the victims and lethality <strong>of</strong> injuries corresponds<br />
to the shift in targeting <strong>of</strong> civilians and the methods <strong>of</strong> fatal wounding. <strong>The</strong> implications<br />
to international aid agencies and to the trauma and critical care communities in terms<br />
<strong>of</strong> prevention strategies, targeted preparation, and medical response are highly significant.<br />
References<br />
1. Seybolt TB. Major armed conflicts. SIPRI Yearbook 2001. Armaments,<br />
Disarmaments and <strong>International</strong> Security. Oxford: Oxford University Press, 2001.<br />
2. Wallensteen P, Sollenberg M. Armed Conflict, 1989–98. Journal <strong>of</strong> Peace Research<br />
36(5):593, 1999.<br />
3. Federal Bureau <strong>of</strong> Investigation. Terrorism in the United States. Washington, DC:<br />
FBI, 1999.<br />
4. U.S. Department <strong>of</strong> State. Patterns <strong>of</strong> Global Terrorism, 1999.<br />
Suicide Bombings in Israel: Injuries Never Seen Before<br />
Itamar Ashkenazi, MD, and Ricardo Alfici, MD<br />
Surgery B, Hillel Yaffe Medical Center PO Box 169, Hadera, Israel 38100<br />
In the past two years, victims from 38 terrorist incidents were treated in Hillel Yaffe<br />
Medical Center. Of these, 16 were bomb attacks that resulted in mass casualties. Our experience<br />
will be presented. Special emphasis will be given to injuries never reported before in the<br />
medical literature. <strong>The</strong> diagnostic and therapeutic challenge, together with the implications<br />
upon treatment, will be discussed. <strong>The</strong>se new presentations <strong>of</strong> injury represent an introduction<br />
to a new phase in the ingenuity <strong>of</strong> perpetrating injury in suicide bombings.<br />
Rapid Evacuation and Transport <strong>of</strong> the Critically Injured Patient<br />
William Beninati, MD, Air Force Coalition for Sustainment <strong>of</strong> <strong>Trauma</strong> and Readiness<br />
Skills/R Adams Cowley Shock <strong>Trauma</strong> Center, Baltimore, Maryland, USA<br />
Todd Carter, MD, Office <strong>of</strong> the Air Force Surgeon General, Washington, DC, USA<br />
Gregory Rupert, RN, Wilford Hall Medical Center, San Antonio, Texas, USA<br />
James H. Henderson, MD, Wilford Hall Medical Center, San Antonio, Texas, USA<br />
Learning Objectives<br />
1. To describe the US Air Force Aeromedical Evacuation System for transporting<br />
casualties.<br />
2. To comprehend the clinical capabilities that can be reasonably be provided during<br />
long-range air transport.<br />
3. To explain the technological limitations to care during long-range air transport.<br />
4. To explain the USAF Critical Care Air Transport Team experience with evacuation<br />
<strong>of</strong> casualties across a spectrum <strong>of</strong> settings from peacetime healthcare to combat.<br />
<strong>The</strong> United States Air Force (USAF) maintains an Aeromedical Evacuation System<br />
(AES) designed to operate across a broad spectrum <strong>of</strong> activities from peacetime healthcare<br />
to combat support. This system is flexible and scalable, and can accommodate a range from<br />
single-patient to mass casualty evacuation. To provide for the care <strong>of</strong> casualties who have<br />
been stabilized by ground-based medical teams, but who remain critically ill or injured, the<br />
USAF developed Critical Care Air Transport Teams (CCATT). <strong>The</strong> CCATT capability permits<br />
the use <strong>of</strong> small, highly capable, ground-based resuscitative teams without imbedded postresuscitative<br />
care. Such teams can be rapidly inserted with minimal impact on limited airlift<br />
resources, relying on the AES to provide post-resuscitation/post-surgical care.<br />
Methods. <strong>The</strong> AES uses opportune cargo aircraft staffed by dedicated aeromedical<br />
evacuation (AE) crews consisting <strong>of</strong> flight nurses and technicians. Patients with imminent loss<br />
<strong>of</strong> life, limb, or vision are designated urgent or priority for rapid evacuation; a subset <strong>of</strong> these<br />
casualties are critically ill. For transport <strong>of</strong> critically ill patients, the AE crews oversee the conduct<br />
<strong>of</strong> the mission to include flight safety, loading and unloading, and access to oxygen and<br />
electricity. Direct care <strong>of</strong> critical patients is provided by CCATT. A CCATT consists <strong>of</strong> a critical<br />
care physician, critical care nurse, and respiratory therapist equipped with appropriate supplies<br />
and portable, battery-operated medical equipment. This equipment includes mechanical<br />
ventilators, physiologic monitors, a pacemaker/defibrillator, multi-channel infusion<br />
pumps, and a laboratory analyzer. This personnel and equipment package provides the<br />
majority <strong>of</strong> capability available in a hospital-based intensive care unit. A training pipeline has<br />
50
<strong>ITACCS</strong> Spring 2003<br />
been developed for team members, which includes clinical qualification, basic aeromedical<br />
training, evacuation exercises, as well as operational and clinical sustainment training.<br />
Results. <strong>The</strong> USAF CCATTs have safely transported critically ill and injured patients in<br />
settings that include peacetime health care, disaster response, terrorist attacks, peacekeeping<br />
operations, and combat. Transport times have been as long as 20 hours. Specific missions<br />
will be discussed to demonstrate the flexibility, clinical capabilities, and limitations <strong>of</strong> this system.<br />
In the early phase <strong>of</strong> Operation Enduring Freedom in Afghanistan, initial casualty care<br />
was provided by forward surgical teams with limited capacity for sustained critical care postdamage<br />
control. This care was provided in the air by the AES. In the first 17 months <strong>of</strong> this<br />
operation, CCATTs transported 172 critical casualties (see graph), representing 12% <strong>of</strong> total<br />
casualties moved. <strong>The</strong>re was no peri-transport morbidity or mortality.<br />
for re-exploration. <strong>The</strong> patient is unpacked and residual bleeding dealt with. Careful inspection<br />
should be made for injuries missed at initial laparotomy. Gastrointestinal integrity can be<br />
reconstituted.<br />
Occasionally, it is possible to close the fascia primarily at this point. Temporary closure<br />
can be effected in a number <strong>of</strong> ways, such as mobilization <strong>of</strong> skin flaps or bridging the fascial<br />
defect with absorbable mesh. If mesh is used, this can be skin grafted in about 2 weeks.<br />
Delayed abdominal wall reconstruction can be accomplished at 6 months when all intraabdominal<br />
inflammation has subsided.<br />
Damage control can also be utilized elsewhere in the body, especially in polytrauma<br />
patients with long-bone fractures. While the advantages <strong>of</strong> early fracture fixation are clear,<br />
definitive fixation can be time consuming and risks considerable blood loss. Temporary<br />
external fixation provides the advantages <strong>of</strong> fracture stabilization without blood loss or time<br />
in the operating room. When the patient is stable, the intra-medullary techniques can be used<br />
to gain final fracture stabilization.<br />
Damage control involves utilizing standard trauma principles in a slightly different way<br />
when dealing with the most critically ill patients. It is a philosophy <strong>of</strong> care, not a technique,<br />
and is applicable to a large number <strong>of</strong> critically ill patients.<br />
— Session C—<br />
<strong>Trauma</strong> Education, Simulation, and Patient Safety<br />
Co-Chair: James G. Cain, MD Pittsburgh, Pennsylvania, and West Virginia University,<br />
Morgantown, West Virginia, USA<br />
Co-Chair: Michael J.A. Parr, MB BS MRCP FRCA FANZCA, FJFICM, University <strong>of</strong> New South<br />
Wales, Sydney, NSW<br />
Discussion. <strong>The</strong> CCATT model demonstrates a highly successful balance <strong>of</strong> small size,<br />
portability, and robust clinical capability. This model has proven flexible across a broad range<br />
<strong>of</strong> settings. This model for rapid evacuation <strong>of</strong> stabilized casualties can be adapted to civilian<br />
disaster response and to novel situations that may arise.<br />
Organization <strong>of</strong> Nurses Working with Terror Victims in the Emergency<br />
Department and on the Wards<br />
Gila Hyams, RN, MA<br />
Rambam Medical Center, Haifa, Israel<br />
Over the past two years, Israel has been hit by a wave <strong>of</strong> terror attacks, mostly bomb<br />
explosions, amidst the civilian population. <strong>The</strong> large number <strong>of</strong> events has brought about an<br />
improvement in the organization <strong>of</strong> every link in the chain <strong>of</strong> survival.<br />
Organizing a hospital to deal with a mass casualty situation (MCS) is a very complicated<br />
affair. It includes organizing the physical space, the equipment, and the manpower. In<br />
manpower, the largest group is the nurses. A variety <strong>of</strong> subjects must be dealt with: 1) knowledge/medical<br />
skills, 2) recruiting <strong>of</strong> nursing staff, 3) organization in the admitting sites, and<br />
4) preparation <strong>of</strong> wards.<br />
This means that every nurse in an MCS should know what to do, where to do it, and<br />
how to do it. To achieve this end, a complex process <strong>of</strong> preparedness must occur in a continuing<br />
fashion. <strong>The</strong> tools to achieve this goal are lectures, computer lessons, drills, and,<br />
above all, writing detailed standing orders for each and every situation. With our experience<br />
in recent terror attacks, we will describe the benefits and drawbacks <strong>of</strong> each tool in preparing<br />
the nursing staff to deal successfully with an MCS.<br />
In addition, we will discuss new protocols that we have adopted for a ‘limited’ MCS,<br />
with training <strong>of</strong> teams, nurses and physicians together, at a medical simulation center and<br />
debriefing <strong>of</strong> teams after every event.<br />
Damage Control Surgery: Principles <strong>of</strong> Care for Critical Injury<br />
Thomas Scalea, MD, FACS<br />
Physician in Chief, R Adams Cowley Shock <strong>Trauma</strong> Center, University <strong>of</strong> Maryland School<br />
<strong>of</strong> Medicine, Baltimore, Maryland, USA<br />
Learning Objectives: To understand the conditions that warrant damage control<br />
surgery and the procedures associated with this approach to the stabilization <strong>of</strong> severely<br />
injured patients.<br />
Damage control applies standard principles differently in critically injured patients.<br />
Damage control is divided into phases. Phase 1 occurs in the emergency department. Patients<br />
who present in extremis should undergo rapid evaluation with limited radiographs ascertaining<br />
the location <strong>of</strong> cavitary blood loss. This should take less than 15 minutes and the<br />
patient taken directly to the operating room. <strong>The</strong> damage control operation should be tailored<br />
to stop named bleeding and control gross contamination. Expendable organs (the<br />
spleen) should be resected. Major vascular injuries should be repaired, or temporarized by<br />
intraluminal shunting. Non-expendable organs (the liver) should have major bleeding controlled<br />
and non-surgical bleeding packed. Gastrointestinal injuries should be ligated or<br />
resected without anastamosis. Once major blood loss is controlled, the patient should be<br />
packed and temporarily closed.<br />
Exsanguinating hemorrhage <strong>of</strong>ten leads to hypothermia acidosis and coagulopathy.<br />
Further operation perpetuates this cycle. Thus, early selection is important. This may be<br />
based on either anatomic criteria (multiple visceral injuries, major vascular injury) or physiologic<br />
criteria (acidosis, blood product requirements).<br />
<strong>The</strong> patient should then be taken to the ICU. Cardiovascular function is optimized generally<br />
using invasively derived hemodynamic parameters. Respiratory function should be<br />
optimized, <strong>of</strong>ten using pressure limited ventilatory strategies. Most importantly, coagulopathy<br />
must be reversed and normal temperature restored.<br />
Adjunctive hemostasis can be obtained using angiographic embolization. This technique<br />
is most helpful with central liver injuries, bleeding deep in the pelvis or adjacent to the<br />
great vessels. Strong consideration for re-operation should be given for ongoing transfusion<br />
requirements or inability to normalize lactate.<br />
When homeostasis is restored, the patient should be returned to the operating room<br />
Human Crisis Simulation for Rural Medical Education<br />
James Gordon Cain, MD<br />
Allegheny General Hospital, Pittsburgh, Pennsylvania, USA, and West Virginia University,<br />
Morgantown, West Virginia, USA<br />
Learning Objective: To provide an introduction to simulation as a means to<br />
extend resources in providing trauma education in a rural setting.<br />
Rural areas present unique challenges in providing trauma services and educating<br />
practitioners in acute care. Rural populations have experienced unique patterns <strong>of</strong> trauma<br />
since medieval times. Thirty percent <strong>of</strong> the United States’ population is rural, yet 70% <strong>of</strong> all<br />
trauma fatalities occur in that population. <strong>The</strong> reasons for increased risk are multifactorial.<br />
Poverty and unemployment are higher. Hazardous occupations are more common. More<br />
than half <strong>of</strong> all fatal motor vehicle collisions occur on rural roads and involve local residents.<br />
Rural patients are more frequently aged, chronically ill, or disabled (congenital or acquired),<br />
increasing the likelihood <strong>of</strong> death from less severe injuries. <strong>Trauma</strong> is the number one cause<br />
<strong>of</strong> childhood death. Mortality from rural pediatric trauma is approximately twice that <strong>of</strong> urban<br />
pediatric trauma.<br />
A major impediment for the rural trauma patient is access to adequate health care. It<br />
is difficult to attract and retain physicians <strong>of</strong> any description to rural areas. Economic pressures<br />
limit physician staffing <strong>of</strong> rural emergency departments. Rural settings benefit from<br />
innovations improving acute care management, such as medical simulation.<br />
Medical simulation’s roots are vested in aviation, a standard, accepted tool for pilot<br />
education, evaluation, and reproduction <strong>of</strong> critical events. Similar to flying, anesthesiology<br />
requires vigilance while multitasking in the face <strong>of</strong> distracters. In 1986, the VA Palo Alto<br />
HSC/Stanford University Center for Crisis Management Training in Health Care extrapolated<br />
technology from aviation to medicine and anesthesia. Medical simulation now includes critical<br />
care, trauma, and emergency medicine and may decrease morbidity related to critical<br />
events. Most major simulation centers worldwide have developed simulation programs focusing<br />
on the dynamics <strong>of</strong> Crisis Resource Management (CRM). CRM is resource intensive and<br />
requires expenditures for the simulator, physical plant, personnel, and support staff required<br />
to produce complete operating room, emergency department, or critical care simulations.<br />
Institutions unable to muster such resources may feel unable to participate.<br />
<strong>The</strong> West Virginia University Human Crisis Simulation Program developed a successful,<br />
heavily utilized center with a modicum <strong>of</strong> resources in a rural setting. Simulation allows<br />
stretching <strong>of</strong> educational resources. Simulation <strong>of</strong>fers rural medical trainees and practitioners<br />
a safe and effective environment in which to learn appropriate actions and procedures in<br />
acute care situations. <strong>The</strong> West Virginia Human Crisis Simulation Program is located in a<br />
recently renovated 700-square-foot facility near clinical areas and includes a simulator room,<br />
control room, and physician <strong>of</strong>fice. <strong>The</strong> simulator is used extensively to introduce anesthesia<br />
residents to anesthesia and acute care medicine and for multidisciplinary education, medical<br />
student education, and continuing medical education. Videotaped simulations may be used<br />
to educate juries, judges, and attorneys in medical malpractice trials. Media coverage<br />
expounding the benefits <strong>of</strong> simulation in medicine and its potential to decrease the likelihood<br />
for serious errors provided welcome favorable publicity and enhanced public relations.<br />
Future uses for the simulator include multidisciplinary research, modeling work environment<br />
for new technologies, videoconferencing with statewide CME capability, and pr<strong>of</strong>essional<br />
evaluations and certifications. <strong>The</strong> curriculum is unique in its application <strong>of</strong> tertiary care and<br />
Level 1 trauma skills to a rural population.<br />
<strong>The</strong> Role <strong>of</strong> Microsimulators in Training <strong>Trauma</strong> Pr<strong>of</strong>essionals<br />
Ulrik Juul Christensen, MD<br />
Sophus Medical A/S, Copenhagen, Denmark<br />
Learning Objective: To provide an overview <strong>of</strong> the background for the use <strong>of</strong><br />
microsimulators (PC-based simulators) in medical education in general and in trauma<br />
education in particular.<br />
Background. Medical microsimulators are PC-based simulators that can be used for<br />
training the cognitive aspects <strong>of</strong> handling patients in a low-risk, instructor-less, and easily accessible<br />
environment. <strong>The</strong> debriefing after simulation sessions is just as important for microsimulation<br />
as in full-scale (also known as macrosimulation) simulation with manikins and instructors<br />
involved. In order to use microsimulators for self-directed learning and optimally for distance<br />
learning, the simulators should have as advanced technology for debriefing as possible in order<br />
to provide qualified feedback on the performance in the virtual simulators.<br />
Most microsimulators are designed to supplement the existing education based on lec-<br />
51
<strong>ITACCS</strong> Spring 2003<br />
tures, reading, classroom teaching, and optimally large numbers <strong>of</strong> hands-on practice in safe<br />
environments such as full-scale simulators, task trainers, and simulated patients (actors). <strong>The</strong><br />
philosophy is that microsimulators in the same way as chess computers (i.e., microsimulators<br />
for chess playing) can provide the learning access to a vast amount <strong>of</strong> more or less seldom cases<br />
that can be dealt with dynamically. This aspect becomes particularly more important if the learners<br />
have limited access to “real” cases where they can be taught in an apprenticeship manner.<br />
<strong>The</strong> issue <strong>of</strong> access to only a very limited number <strong>of</strong> clinically challenging problems<br />
(and consequently the lack <strong>of</strong> cognitive and psychomotor practice) is evident in the case <strong>of</strong><br />
the training <strong>of</strong> the US Army Combat Medics (the so-called 91W program). <strong>The</strong> 91W program<br />
is a condensed 16-week course, with the first part being a standard EMT-B education. Due to<br />
a variety <strong>of</strong> reasons, with some being quite obvious during peacetime, the equivalent <strong>of</strong> clinical<br />
encounters, bedside learning, and clinical sessions is very limited. <strong>The</strong>refore, the US<br />
Army decided to train to up to 8000 each year with extensive use <strong>of</strong> full-scale human patient<br />
simulators, a variety <strong>of</strong> task trainers such as IV arms and CPR manikins, and finally days in a<br />
simulated battlefield with both portable simulators and humans with wound make up.<br />
<strong>The</strong> US Army is now introducing microsimulation as a integrated part <strong>of</strong> the training<br />
<strong>of</strong> the army combat medics in order to achieve a number <strong>of</strong> benefits: a) to strengthen the<br />
cognitive training by focusing more on deep learning (by doing!) rather than more superficial<br />
learning types that can be the result <strong>of</strong> classroom teaching only, b) to use less intensive<br />
time during practical exercises for more self-directed learning, and c) to free resources during<br />
the practical exercises in order to increase the instructor-to-student ratio during psychomotor<br />
and field training exercises. <strong>The</strong> military microsimulators are based on systems<br />
used in prehospital and inhospital care as well as by the Red Cross in many countries for training<br />
in First Aid (in the military environment the target for the latter technology is the equivalent<br />
<strong>of</strong> First Aid – called Self Aid and Buddy Aid). <strong>The</strong> immediate implementation <strong>of</strong> the military<br />
microsimulators will be at the combat medic level, but the technology has been developed<br />
to be scaled up and down to be used for all group <strong>of</strong> personnel from emergency physicians<br />
to EMT-Bs, combat medics, and nurses. <strong>The</strong> majority <strong>of</strong> the cases will focus on trauma<br />
care, but a large number <strong>of</strong> cases will also be aimed at the EMT-B education, including ALS<br />
and other aspects <strong>of</strong> acute medicine as well as several cases aimed at CBRNE (chemical, biological,<br />
radiation, nuclear, explosions) related patients.<br />
Rapid Preparation <strong>of</strong> Reserve Military Medical Teams<br />
Using Advanced Patient Simulators<br />
Guy Lin,1 Yahav Oron, 1 Ron Ben-Abraham,1 Dafna Barsuk, 2 Haim Berkenstadt, 2 Amitai<br />
Ziv, 2 Amir Blumenfeld1<br />
1<br />
IDF-Medical Corps <strong>Trauma</strong> Branch and the 2 National Medical Simulation Center<br />
(M.S.R.), Chaim Sheba Medical Center, Tel-Hashomer, Israel<br />
Learning Objectives: To discuss the advantages <strong>of</strong> the use <strong>of</strong> advanced patient simulators<br />
in the training <strong>of</strong> reserve medical personnal.<br />
Primary prehospital medical treatment for trauma casualties has unique features in the<br />
military setting. <strong>The</strong> environment is sometimes hostile, and tactical situations together with<br />
the feasibility <strong>of</strong> evacuation are major considerations. Most <strong>of</strong> our reserve medical teams are<br />
not working routinely in this environment. In many debriefings, we recognize gaps in<br />
patients’ evaluation, diagnosis <strong>of</strong> deterioration in the patient respiratory or hemodynamic<br />
condition after the initial treatment, and need for rapid evacuation. We believed that training<br />
with advanced patient simulators could improve these tasks.<br />
Many reserve medical teams were recruited for the medical support <strong>of</strong> the “Defensive<br />
Shield” operation (April 2002). <strong>The</strong> reserve teams were composed <strong>of</strong> physicians having all<br />
kinds <strong>of</strong> expertise and medics having various non-medical pr<strong>of</strong>essions. A questionnaire<br />
revealed that 72% <strong>of</strong> reserve staff rarely treat trauma patients. Forty-seven percent define<br />
themselves as not good enough in trauma management. Moreover, reserve forces are usually<br />
trained for a high-intensity conflict, being prepared for prolonged evacuation time, and are<br />
not accustomed to the nearness <strong>of</strong> trauma centers to the battle zone.<br />
Every military physician has ATLS certification. Complementary training is usually done<br />
by traditional methods such as simple manikins and living animal models. <strong>The</strong>se models fit for<br />
technical skills and familiarity with the equipment, and less for diagnosis and decision-making.<br />
Team training is usually done by “fake” patients with less attention to individual performance.<br />
Advanced patient simulators give the opportunity to integrate all these skills.<br />
Recruitment <strong>of</strong> reserve medical teams for medical support <strong>of</strong> battle zones adjacent to<br />
medical centers creates a need to assimilate rapid diagnosis and decision making (which<br />
interventions are more important than time?), together with refreshment <strong>of</strong> the critical skills<br />
<strong>of</strong> airway management and chest decompression.<br />
During a 3-week period, 75 teams (90 physicians and 352 medics) were trained by<br />
advanced patient simulators in the Israeli Center for Medical Simulation (a collaboration <strong>of</strong><br />
military and civilian systems).<br />
We developed a scenario-based training adapted to specific missions. <strong>The</strong> basic program<br />
included an airway station (Airman manikin), head injury with difficulties in endotracheal<br />
inbtubation (Sim Man manikin), penetrating chest injury causing tension pneumothorax<br />
and hemorrhagic shock (Meti manikin), a multi-trauma pediatric patient (Pediasim Meti<br />
manikin), and a multi-casualty event. Video-screened debriefing was conducted by experienced<br />
ATLS instructors.<br />
Feedback <strong>of</strong> trainees revealed overwhelming satisfaction. Reality <strong>of</strong> scenarios was evaluated<br />
as high by 95% <strong>of</strong> trainees. Eighty-seven percent said they are more ready for decision<br />
making in the care <strong>of</strong> combat casualties. Seventy-three percent felt they increased their<br />
knowledge and improved their skills.<br />
Twelve trained medical teams have treated major trauma patients during the operation.<br />
<strong>The</strong>y reported great contribution <strong>of</strong> advanced simulators training to the care <strong>of</strong> their<br />
patients: improved individual performance, self-confidence, and staff coordination.<br />
Conclusion. Scenario-based training using HPS should be a leading system in the<br />
qualification <strong>of</strong> military medical teams. Rapid preparation for combat casualties care is feasible.<br />
This method <strong>of</strong> treatment should be developed, and the next step will be constructing a<br />
study for objective validation.<br />
Selected References<br />
Ali J, Adam R, Josa D, et al. Effects <strong>of</strong> basic pre-hospital trauma life support program on<br />
cognitive and trauma management skills. World J Surg 1998; 1192–6.<br />
Ali J, Adam R, Pierre I, et al. Comparison <strong>of</strong> performance two years after the old and<br />
new (interactive) ATLS courses. J Surg Res 2001; 97:71–5.<br />
Ali J, Cohen RJ, Gana TJ, Al-Bedah KF. Effects <strong>of</strong> ATLS program on medical students’<br />
performance in simulated trauma patient management. J <strong>Trauma</strong> 1998; 44:588–91.<br />
Ali J, Gana TJ, Howard N. <strong>Trauma</strong> mannequin assessment <strong>of</strong> management skills <strong>of</strong> surgical<br />
residents after ATLS training. J Surg Res 2000; 93:197–200.<br />
Bond FB, Kostenbader M, McCarthy JF. Pre-hospital and hospital-based health care<br />
providers experience with a human patient simulator. Prehospital Emerg Care<br />
2001; 5:284–7.<br />
Blumenfeld A, Abraham RB, Stein M, et al. Cognitive knowledge decline after ATLS<br />
courses. J <strong>Trauma</strong> 1998; 44:513–6.<br />
Devitt JH, Kurrek MM, Cohen MM, Cleave-Hogg D. <strong>The</strong> validity <strong>of</strong> performance assessment<br />
using simulation. Anesthesiology 2001; 95:36–42.<br />
Issenberg SB, Megaghic WC, Hart IR, et al. Simulation technology for health care pr<strong>of</strong>essional<br />
skills training and assessment. JAMA 1999; 282:861–6.<br />
Ziv A, Small S, Wolpe P, Patient safety and simulation based medical education. Med<br />
Tech 2000; 22:489–95.<br />
Drills: Are <strong>The</strong>y the Best Way to Prepare for a Mass Casualty Situation?<br />
Moshe Michaelson, MD<br />
<strong>Trauma</strong> Unit, Rambam Medical Center, Haifa, Israel<br />
Learning Objective: To compare the types <strong>of</strong> drills available for training participants<br />
to respond to a mass casualty situation.<br />
<strong>The</strong> key to success in a mass casualty situation (MCS) is to be prepared. <strong>The</strong> first step<br />
in preparedness is writing detailed standing orders. Standing orders should provide answers<br />
to all the problems that may arise during this difficult situation. However, writing standing<br />
orders is only part <strong>of</strong> the solution. A bigger task is to disseminate the information to all participants.<br />
<strong>The</strong>re are a few tools to help us in this undertaking, and drills are one <strong>of</strong> the best.<br />
We discuss the types <strong>of</strong> drills available, with emphasis on the role each drill plays in achieving<br />
the goal <strong>of</strong> preparing the system to deal with an MCS. Attention is paid to cost-benefits and<br />
the ability <strong>of</strong> a single hospital to organize drills without outside help. At the end <strong>of</strong> the presentation,<br />
it will be clear whether drills are the best way to prepare for an MCS.<br />
Friday, May 16, 2003<br />
Simultaneous Afternoon Sessions<br />
— Session A —<br />
Update on New Drugs, Equipment, and Techniques in <strong>Trauma</strong> Care<br />
Chair: Charles E. Smith, MD, FRCPC, Cleveland, Ohio, USA<br />
What’s New in Pulse Oximetry<br />
Steven J. Barker, PhD, MD<br />
Pr<strong>of</strong>essor and Head, Department <strong>of</strong> Anesthesiology<br />
University <strong>of</strong> Arizona, Tucson, Arizona, USA<br />
Learning Objectives: This lecture will promote a better understanding <strong>of</strong> 1) how<br />
pulse oximeters work, 2) what they can and cannot measure, 3) the application <strong>of</strong> pulse<br />
oximetry to care <strong>of</strong> the trauma patient, and 4) current and expected new developments in<br />
the technology.<br />
This lecture will review the theoretical background and recent developments in pulse<br />
oximetry, with emphasis on its use in trauma patients. <strong>The</strong> relationship <strong>of</strong> pulse oximetry to<br />
other monitors <strong>of</strong> patient oxygenation will be explored through a review <strong>of</strong> the physiology <strong>of</strong><br />
oxygen transport. Clinical applications will be used to show both the value and the limitations<br />
<strong>of</strong> saturation monitoring.<br />
Recent developments in pulse oximetry have been aimed chiefly at improving accuracy<br />
and reliability in the presence <strong>of</strong> various signal artifacts. <strong>The</strong>se sources <strong>of</strong> error include patient<br />
motion, hypovolemia, shock, dyshemoglobinemias, and venous pulsations. Each <strong>of</strong> these artifacts<br />
and their potential remedies will be discussed in the context <strong>of</strong> the trauma patient.<br />
Capnography in <strong>Trauma</strong><br />
Steven J. Barker, PhD, MD<br />
Pr<strong>of</strong>essor and Head, Department <strong>of</strong> Anesthesiology<br />
University <strong>of</strong> Arizona, Tucson, Arizona, USA<br />
Learning Objectives: This lecture will provide a better understanding <strong>of</strong> the mechanisms<br />
<strong>of</strong> CO 2 transport from the body, the relationship between arterial and end-tidal CO 2<br />
tensions, and the use <strong>of</strong> the capnogram as a diagnostic tool. <strong>The</strong> attendee will be able to identify<br />
various abnormal capnogram shapes and use these to initiate and monitor treatment.<br />
Capnography, the measurement <strong>of</strong> respiratory carbon dioxide, is effectively a minimum<br />
standard <strong>of</strong> care for general anesthesia. It is particularly important in the trauma<br />
patient, because the capnogram provides information not only about ventilation, but also<br />
about circulation and metabolism. This lecture will review the physiology <strong>of</strong> carbon dioxide<br />
transport, using this background as a guide to the interpretation <strong>of</strong> expired CO 2 . <strong>The</strong> reasons<br />
for the difference between end-tidal and arterial carbon dioxide tensions will be discussed in<br />
detail, to show how this difference can be used as an important diagnostic tool.<br />
We shall also review some basic capnogram waveforms and their clinical interpretation.<br />
This waveform can provide valuable diagnostic information, and it can also be used to monitor<br />
the progress <strong>of</strong> therapeutic interventions. We will see how the capnograph can even be<br />
used to measure the effectiveness <strong>of</strong> chest compressions during CPR. Unlike the pulse<br />
oximeter, which provides data on only one patient variable (arterial oxygenation), the capnograph<br />
provides an indication <strong>of</strong> metabolism, circulation, and ventilation simultaneously.<br />
Neuromuscular Relaxant Pharmacology: An Update<br />
Charles E. Smith, MD, FRCPC<br />
Department <strong>of</strong> Anesthesia, MetroHealth Medical Center, Case Western Reserve University,<br />
Cleveland, Ohio, USA<br />
Learning Objective: To discuss the scientific basis for choosing a neuromuscular<br />
relaxant for trauma patients.<br />
Non-depolarizing relaxants bind to the acetylcholine (Ach) receptor at the post junctional nicotinic<br />
receptor and competitively prevent binding <strong>of</strong> Ach to the receptor. <strong>The</strong> ion channel is closed and no<br />
52
<strong>ITACCS</strong> Spring 2003<br />
current can flow. Depolarizers such as succinylcholine mimic the action <strong>of</strong> Ach and result in excitation <strong>of</strong><br />
muscle contraction followed by blockade <strong>of</strong> neuromuscular transmission. Nonclassical mechanisms<br />
include prejunctional block, ion channel block, desensitization <strong>of</strong> receptors, perijunctional block, and<br />
tonic block <strong>of</strong> extraocular muscles.<br />
Relaxants are used to facilitate tracheal intubation and provide skeletal muscle relaxation<br />
for surgery and mechanical ventilation. Other reasons are to reduce oxygen demand<br />
and intracranial pressure, abolish shivering, and as adjuncts to the treatment <strong>of</strong> tetanus, and<br />
status epilepticus.<br />
Non-depolarizers are polar molecules. Potency is described by dose-response relationships.<br />
<strong>The</strong> ED90 is the dose that produces 90% block (± SD). In practice, larger doses such<br />
as 3 x ED90 are given to produce pr<strong>of</strong>ound block initially. Smaller “repeat” doses or continuous<br />
infusions are then used to maintain block. Some muscle groups are more resistant than<br />
others with the dose-response curve shifted to right: e.g., diaphragm, larynx, eye muscles.<br />
Other muscle groups are more sensitive with the dose-response curve shifted to left: e.g.,<br />
pharyngeal musculature that maintains upper airway patency. Monitoring <strong>of</strong> neuromuscular<br />
function is crucial in order to avoid complications from giving too much or too little relaxant.<br />
Various factors influence the choice <strong>of</strong> relaxant such as onset, duration, side effects,<br />
histamine release, biliary or liver disease, renal function, hypothermia, age, and altered pharmacology<br />
due to drug–drug and drug–disease interactions (e.g., volatile agents, magnesium,<br />
muscular dystrophies, burns, motor neuron disease, myasthenia gravis, and sepsis). <strong>The</strong> table<br />
summarizes some important clinical information on neuromuscular relaxants for trauma.<br />
Selected Neuromuscular Relaxants for <strong>Trauma</strong><br />
Agent Intubating Intubating Duration Comments<br />
dose, mg/kg time (min)^ (min)*<br />
Succinylcholine 0.6-1.1 1 4-6 Side effects may<br />
contraindicate its use, e.g.,<br />
hyperkalemia<br />
Rocuronium 0.6-1.2 0.7-1.1 31-67 Nondepolarizer <strong>of</strong> choice<br />
for rapid sequence<br />
intubation. Mild vagolysis<br />
Mivacurium 0.15-0.25 1.5-2.5 16-23 Metabolized by plasma<br />
cholinesterase. Histamine<br />
release<br />
Vecuronium 0.08-0.10 2.5-3 25-40 Onset time delayed unless<br />
high doses (0.3-0.4 mg/kg)<br />
used. Cardiovascular<br />
effects unlikely<br />
Cisatracurium 0.15-0.2 1.5-2 55-65 Potent stereoisomer <strong>of</strong><br />
atracurium with organ<br />
independent elimination.<br />
Cardiovascular<br />
effects unlikely<br />
Atracurium 0.4-0.5 2-2.5 35-45 Organ independent<br />
elimination.<br />
Histamine release<br />
Pancuronium 0.06-0.10 2-3 65-100 Long acting. Associated<br />
with tachycardia and<br />
activation <strong>of</strong> the sympathetic<br />
nervous system<br />
^ Average time to good-excellent intubating conditions ((80% block).<br />
* Average time to 25% first twitch recovery.<br />
References<br />
1. Bevan DR. Complications <strong>of</strong> muscle relaxants. Semin Anesth 1995; 14:663.<br />
2. Smith CE, Grande CM, Wayne MA, <strong>ITACCS</strong> Consensus Panel, and <strong>International</strong><br />
Review Committee. Rapid Sequence Intubation in <strong>Trauma</strong>. <strong>ITACCS</strong>, Baltimore, 1998.<br />
3. Grande CM, Smith CE, Stene JK. <strong>Trauma</strong> anesthesia. In Longnecker DE, Tinker JH,<br />
Morgan GE, eds. Principles and Practice <strong>of</strong> Anesthesiology, 2nd edition. St. Louis,<br />
Mosby, chapter 81, 1997, pp 2138–64.<br />
Acid-Base Balance in <strong>Trauma</strong> Resuscitation<br />
Lewis J. Kaplan, MD, FACS<br />
Associate Pr<strong>of</strong>essor <strong>of</strong> Surgery, Director Emergency General Surgery, Yale University<br />
School <strong>of</strong> Medicine, Department <strong>of</strong> Surgery, Section <strong>of</strong> <strong>Trauma</strong>, Surgical Critical Care,<br />
and Emergency General Surgery, New Haven, Connecticut, USA<br />
Learning Objectives: 1) To articulate the recent advances in trauma care over the<br />
past 3 years, 2) to enumerate the directly applicable changes in the trauma care paradigm,<br />
and 3) to construct an integrated plan to minimize iatrogenic acidosis and minimize<br />
transfusion needs in severely traumatized patients.<br />
Military realities as well as civilian trauma (e.g., terrorist attacks <strong>of</strong> 9/11/01) have<br />
prompted a reexamination <strong>of</strong> trauma resuscitation tools and strategies. Traditional resuscitation<br />
strategies focused on hemorrhage control in conjunction with intense fluid resuscitation,<br />
including massive transfusion <strong>of</strong> blood and blood products as needed to clear lactate as<br />
an arbiter <strong>of</strong> hypoperfusion. 1 Recognition <strong>of</strong> the potential deleterious effects <strong>of</strong> this strategy<br />
prior to definitive hemorrhage control, limitation <strong>of</strong> the US blood banking system to meet<br />
demands, and heightened public and medical desires to avoid allogeneic exposures also promoted<br />
reevaluating the traditional resuscitation paradigm.<br />
Several key factors have influenced the reshaped perspective in trauma resuscitation:<br />
1) equivalent survivorship with low pressure resuscitation, 2 2) laboratory evidence <strong>of</strong> reduced<br />
survivorship with high volume resuscitation, 3 3) acknowledgement <strong>of</strong> the presence and<br />
importance <strong>of</strong> hyperchloremic acidosis following massive resuscitation, 4 4)recognition <strong>of</strong> the<br />
interplay between metabolic acidosis and coagulopathy independent <strong>of</strong> hypothermia, 5,6 5)<br />
improved understanding <strong>of</strong> the relationship between starch-based resuscitation and coagulopathy,<br />
7,8 6) accelerated interest in prehospital and military evaluation <strong>of</strong> hemoglobin-based<br />
oxygen carrier driven resuscitation, 7) the development and looming implementation <strong>of</strong> procoagulants<br />
such as recombinant factor VIIa 9 and a durable hemostatic dressing, and 10 ) elucidation<br />
<strong>of</strong> the key role <strong>of</strong> maintaining microcirculatory flow as a means <strong>of</strong> ameliorating regional<br />
hypoperfusion.<br />
As a result, increases in starch-based resuscitation, including during the current war in<br />
Iraq, and reduced prehospital volume resuscitation are becoming more widely accepted.<br />
Multiple trials are being initiated to explore the benefits <strong>of</strong> procoagulant agents as well as the<br />
efficacy <strong>of</strong> HBOC resuscitation. However, the clear benefit from these changes is an altered<br />
acid-base pr<strong>of</strong>ile from reduced chloride loading. Further data evaluation will allow us to<br />
understand the impact such a strategy will have on ICU length <strong>of</strong> stay, minute ventilation<br />
needs, and blood product transfusion. 10<br />
References<br />
1. Cinat ME, Wallace WC, Nastanski F, et al. Improved survivorship following massive<br />
transfusion in patients who have undergone trauma. Arch Surg 1999; 134(9):964–8.<br />
2. Dutton RP, Mackenzie CF, Scalea TM. Hypotensive resuscitation during active hemorrhage:<br />
impact on in-hospital mortality. J <strong>Trauma</strong> 2002; 52(6):1141–6.<br />
3. Solomonov E, Hirsh M, Yahiya A, et al. <strong>The</strong> effect <strong>of</strong> vigorous fluid resuscitation in<br />
uncontrolled hemorrhagic shock after massive splenic injury. Crit Care Med 2000;<br />
28(3):749–54.<br />
4. Kaplan LJ, Bailey H, Kellum J. <strong>The</strong> etiology and significance <strong>of</strong> metabolic acidosis in<br />
trauma patients. Curr Op Crit Care 1999; 5(6):458–63.<br />
5. Roche AM, James MF, Grocott MP, Mythen MG. Coagulation effects <strong>of</strong> in vitro serial<br />
haemodilution with a balanced electrolyte hetastarch solution compared with a<br />
saline-based hetastarch solution and lactated Ringer’s solution. Anaesthesia 2002;<br />
57(10):950–5.<br />
6. Patterson T, Bailey H, Kaplan LJ. Hyperchloremia induces acidosis, increases the<br />
strong ion gap, and impairs coagulation. Crit Care Med 2000; 28(12):A118.<br />
7. Martin G, Bennett-Guerrero E, Wakeling H, et al. A prospective, randomized comparison<br />
<strong>of</strong> thromboelastographic coagulation pr<strong>of</strong>ile in patients receiving lactated<br />
Ringer’s solution, 6% hetastarch in a balanced-saline vehicle, or 6% hetastarch in<br />
saline during major surgery. J Cardiothorac Vasc Anesth 2002; 16(4):441–6.<br />
8. Kaplan LJ, Bailey H, Walters W. Large volume resuscitation with hydroxyethyl starch<br />
in lactated ringers solution restores perfusion and minimally induces hyperchloremia<br />
without impairing coagulation. Crit Care 2001; 5(Suppl 1):S53.<br />
9. Martinowitz U, Kenet G, Segal E, et al. Recombinant factor VII for adjunctive hemorrhage<br />
control in trauma. J <strong>Trauma</strong> 51(3):431–9.<br />
10. Claridge JA, Schulman AM, Young JS. Improved resuscitation minimizes respiratory<br />
dysfunction and blunts interleukin-6 and nuclear factor-kappa B activation after<br />
traumatic hemorrhage. Crit Care Med 2002; 30(8):1815–9.<br />
<strong>The</strong> Management <strong>of</strong> Massive Bleeds in <strong>Trauma</strong> by an Injury Site-Specific Agent<br />
(Recombinant Activated Factor VII)<br />
U. Martinowitz, 1 L. Aharonson-Daniel, 2 G. Kenet,1 B. Savitsky, 2 , A. Lubezki,1 G.<br />
Martonowits, 3 G. Lin, 3 A. Blumenfeld, 3 and K. Peleg 2<br />
1<br />
<strong>The</strong> National Hemophilia Center, 2 <strong>The</strong> National Center for <strong>Trauma</strong> and Emergency<br />
Medicine Research, <strong>The</strong> Gertner Institute, Sheba Medical Center, Tel Hashomer, Ministry <strong>of</strong><br />
Health and Sackler School <strong>of</strong> Medicine, Tel Aviv University, and 3 Medical Corp, Israel<br />
Defense Forces (G.M. is the Surgeon General), Israel<br />
Learning Objective: To discuss the use <strong>of</strong> recombinant activated factor VII as a<br />
hemostatic agent in trauma patients with massive hemorrhage.<br />
Uncontrolled hemorrhage is a major cause <strong>of</strong> death in trauma patients, accounting for<br />
about 40-50% <strong>of</strong> the mortality in both military and civilian trauma. Most critically ill trauma<br />
patients develop pr<strong>of</strong>ound multifactorial coagulopathy due to activation <strong>of</strong> coagulation with<br />
consumption <strong>of</strong> coagulation factors and platelets, activation <strong>of</strong> fibrinolysis (with fibrinogenolysis<br />
and hyperfibrinolysis in massive trauma), hemodilution, massive transfusions,<br />
hypothermia, and metabolic changes (acidosis, hypocalcemia, etc.). Introduction <strong>of</strong> a “sitespecific”<br />
agent enhancing hemostasis only at the site <strong>of</strong> injury may decrease hemorrhagic<br />
mortality and morbidity in trauma patients. Such an agent, rFVIIa, has been used successfully<br />
for almost a decade in patients with hemophilia developing inhibitors to factor VIII or IX.<br />
rFVIIa activates the coagulation system on the membrane <strong>of</strong> activated platelets, adhered to<br />
the site <strong>of</strong> injury, upon complex formation with tissue factor that is exposed at that site.<br />
Hence, its action is compartmentalized, limited to the site <strong>of</strong> injury, without a systemic effect.<br />
<strong>The</strong> use <strong>of</strong> rFVIIa in trauma patients was avoided due to the theoretical risk <strong>of</strong> thromboembolic<br />
complications. We performed a pig trauma study that supported the safety and efficacy<br />
<strong>of</strong> rFVIIa in this animal trauma model and, immediately after, a few exsanguinating trauma<br />
patients were treated successfully with rFVIIa, which led to ethical committee approval <strong>of</strong> this<br />
agent in patients suffering uncontrolled bleeding.<br />
Patients. Since mid-1999, more than 105 trauma, surgical, and medical patients suffering<br />
massive life-threatening bleeding have been treated with rFVIIa in Israel. We describe<br />
here the data <strong>of</strong> 36 trauma patients treated in 14 <strong>of</strong> the 22 hospitals in Israel. Patients were<br />
critically ill (ISS 25-75 in 86%), multi-transfused (see below), hypothermic, and acidotic and<br />
suffered pr<strong>of</strong>ound coagulopathy (see below). Median age was 20 (range 14-65). Most were<br />
victims <strong>of</strong> terror (40%) and other violence (32%), which reflected the type <strong>of</strong> injury (46% penetrating,<br />
11% blast, and the rest, blunt).<br />
Results. <strong>The</strong> abnormal coagulation tests improved significantly within 15-20 minutes<br />
after administration <strong>of</strong> rFVIIa (PT shortened from 20.7±8.4 to 13.3±6.3 seconds [P
<strong>ITACCS</strong> Spring 2003<br />
Damage Control Orthopedics<br />
James C. Duke, MD<br />
Associate Director, Department <strong>of</strong> Anesthesiology, Denver Health Medical Center;<br />
Associate Pr<strong>of</strong>essor <strong>of</strong> Anesthesiology, University <strong>of</strong> Colorado Health Sciences Center,<br />
Denver, Colorado, USA<br />
Learning Objective: To gain some understanding <strong>of</strong> the evolution in management<br />
<strong>of</strong> long-bone fractures in the multiply injured patient.<br />
“Damage control” surgery began with packing <strong>of</strong> significant hepatic injuries when it<br />
was recognized that prolonged operative time resulted in exsanguinating, cold, acidotic,<br />
coagulopathic patients who <strong>of</strong>ten went on to die. 1 When hemorrhage was controlled, the<br />
patient was transferred to the ICU for further correction <strong>of</strong> these metabolic problems. <strong>The</strong><br />
patient then received a planned reoperation once physiologic stabilization was achieved.<br />
Since that time, the techniques <strong>of</strong> damage control have evolved and been applied to other<br />
surgical disciplines, including orthopedic trauma.<br />
<strong>The</strong> timing <strong>of</strong> long-bone fracture fixation has long been a topic <strong>of</strong> controversy. In<br />
selected patients, early total fracture care has benefits, including less pain, earlier mobilization,<br />
ease in nursing care, less fat embolization, fewer decubitus ulcers, as well as reduced<br />
pulmonary sequelae. However, controversy exists as to whether early total care may place<br />
certain patients with associated pulmonary or head injuries at risk for clinical deterioration.<br />
No randomized clinical trials exist with which to make the best clinical recommendations or<br />
to support a “standard <strong>of</strong> care.” <strong>The</strong> best clinical data tend to be prospective and noncomparative,<br />
and recommendations are very general in nature.<br />
“Damage control orthopedic” care has been adopted by many trauma centers as the<br />
preferred method <strong>of</strong> managing long-bone fractures in the multiply injured patient. 2–4<br />
Generally speaking, these patients are hemodynamically unstable and have multisystem<br />
injuries, and, in particular, pulmonary injuries. Damage control is practiced by employing<br />
temporary external fixation as a bridge to definitive operative repair. <strong>The</strong> orthopedic complication<br />
rate for delayed definitive fixation compares favorably with that <strong>of</strong> patients receiving<br />
early definitive fixation.<br />
In conclusion, there is a clear benefit to early stabilization <strong>of</strong> long-bone fractures. Early<br />
intramedullary fracture fixation remains a desirable goal in the patient with only isolated<br />
femur fractures. However, certain multiply injured “borderline” patients with long-bone fractures<br />
should receive temporary external fixation. Many <strong>of</strong> the benefits <strong>of</strong> definitive<br />
intramedullary fixation, such as decrease in pain and requirement for analgesics, less fat<br />
embolization, and ease in nursing care will be conferred while limiting surgical trauma, fluid<br />
and blood resuscitation, and hypothermia in a vulnerable period.<br />
References<br />
1. Johnson JW, Gracias VH, Schwab CW, et al. Evolution in damage control for exsanguinating<br />
abdominal injury. J <strong>Trauma</strong> 2001; 51:261–71.<br />
2. Scalea TM, Boswell SA, Scott JD, et al. External fixation as a bridge to intramedullary<br />
nailing for patients with multiple injuries and with femur fractures: damage control<br />
orthopedics. J <strong>Trauma</strong> 2000; 48:613–23.<br />
3. Pape H-C, Giannoudis P, Krettek C. <strong>The</strong> timing <strong>of</strong> fracture treatment in polytrauma<br />
patients: relevance <strong>of</strong> damage control orthopedic surgery. Am J Surg 2002;<br />
183:622–9.<br />
4. Pape H-C, Hildebrand F, Pertschy S, et al. Changes in the management <strong>of</strong> femoral<br />
shaft fractures in polytrauma patients: from early total care to damage control<br />
orthopedic surgery. J <strong>Trauma</strong> 2002; 53:452–62.<br />
— Session B —<br />
Ethics: Organ Donation, End <strong>of</strong> Life Issues<br />
Chair: Anne J. Sutcliffe, MB ChB, FRCA, Birmingham, UK<br />
Managing Death and Dying<br />
Anne Sutcliffe MB ChB, FRCA<br />
Consultant in Anaesthesia and Critical Care, Queen Elizabeth Hospital, Birmingham B15<br />
2TH, UK, and Honorary Senior Lecturer, University <strong>of</strong> Birmingham<br />
Learning Objectives:<br />
• To demonstrate that death is easier to accept if it is explained in terms that<br />
include not only medical but also religious and cultural concepts.<br />
• To illustrate that traditional and brain stem death are more similar that commonly<br />
believed.<br />
Death <strong>of</strong> a loved one is never easy to accept. This is particularly true following head<br />
injury, because the severity <strong>of</strong> external injury is <strong>of</strong>ten minimal in comparison to internal, invisible<br />
injury. <strong>The</strong> difficulty is even greater when the diagnosis <strong>of</strong> brain stem death is made in a<br />
warm, pink, “breathing” patient.<br />
Unlike other medical diagnoses, death is final and is not amenable to further treatment.<br />
Treatment occurring at the time <strong>of</strong> death is stopped rather than withdrawn. Decisions<br />
to withdraw or withhold treatment imply that although treatment may have short-term physiological<br />
benefit, this benefit will not alter the underlying disease process and death is<br />
inevitable in days or weeks. In the case <strong>of</strong> brain stem death, treatment is neither possible nor<br />
<strong>of</strong> benefit.<br />
Recommendations for end-<strong>of</strong>-life care in the intensive care unit deal mainly with<br />
patients in whom treatment is withdrawn. 1 Nevertheless, they contain useful guidance for<br />
management <strong>of</strong> the brain-dead patient. Communication with families is essential. It may help<br />
them to accept death if they are able to understand the similarities between traditional and<br />
brain stem death. This implies that the staff supporting them must also be clear about how<br />
its current medical concepts fit into religious, societal, and cultural concepts <strong>of</strong> death.<br />
Brain stem death has been an accepted diagnosis for approximately 20 years but is still<br />
challenged by some doctors 2 and religious groups. 3 Others see it as a means to the end <strong>of</strong><br />
developing the organ transplantation programme. In Japan, it is possible to choose how the<br />
declaration <strong>of</strong> death is made. 4<br />
For the following reasons, I believe traditional death and brain stem death are more<br />
closely related than many people appreciate:<br />
• Traditional death depends on recognisable features such as absence <strong>of</strong> respiration and<br />
a pulse. Some religions, e.g., Judaism, require that breath has left the body, based on<br />
medicine as it was practiced in ancient times. In fact, unsuccessful cardiopulmonary<br />
resuscitation is always associated with brain stem death and this is the reason the<br />
patient does not breathe and the heart does not beat.<br />
• Life and death are a continuum marked by the acquisition <strong>of</strong> mandatory certificates at<br />
given points <strong>of</strong> time. Death in all its forms is a process, not an event, as suggested by<br />
the legal requirement to state a time <strong>of</strong> death. This time describes the time the diagnosis<br />
is made, not the time when the process reached a point where medical death can<br />
be diagnosed.<br />
• <strong>The</strong> diagnosis <strong>of</strong> death has always described the death <strong>of</strong> the organism as a whole, not<br />
the whole organism.<br />
• All diagnoses <strong>of</strong> death require that preconditions are met. Hypothermia is an exclusion<br />
criterion for both traditional and brain stem death.<br />
Further Reading<br />
1. Truog RD, Cist AFM, Brackett SE, et al. Recommendations for end-<strong>of</strong> life care in the<br />
intensive care unit: <strong>The</strong> Ethic Committee <strong>of</strong> the Society <strong>of</strong> Critical Care Medicine.<br />
Crit Care Med 2001; 29:2332–48.<br />
2. Taylor RM. Reexamining the definition and criteria <strong>of</strong> death. Semin Neurol 1997;<br />
17:265–70.<br />
3. Lazar NM, Shemia S, Webster GC, et al. Bioethics for clinicians: 24. Brain Death.<br />
CMJA 2001; 164:833–6.<br />
4. Morioka M. Reconsidering brain death. A lesson from Japan’s fifteen years <strong>of</strong> experience.<br />
Hastings Center Report 2001; 31:41–6 (www.lifestudies.org/reconsidering.html).<br />
Diagnosing Brain Stem Death: After 30 Years, Couldn’t We Do Better?<br />
Dr. Gerlinde Mandersloot<br />
Royal London Hospital, London, United Kingdom<br />
Learning Objectives: To assess the changes and progress in medical technology, philosophy,<br />
and ethics relating to brainstem death.<br />
<strong>The</strong> development <strong>of</strong> medical technology in intensive care medicine dramatically<br />
increased the complexity <strong>of</strong> cases over the past 30 to 40 years. <strong>The</strong> ability to maintain ventilation<br />
and circulation artificially, and the advances made in organ transplantation, showed<br />
that meaningful life could be maintained even though these organs had failed. <strong>The</strong>refore, the<br />
concept <strong>of</strong> cessation <strong>of</strong> cardiorespiratory function as the defining criteria for death had to be<br />
revised.<br />
<strong>The</strong> (re)definition <strong>of</strong> death–‘irreversible loss <strong>of</strong> the capacity for consciousness, combined<br />
with the irreversible loss <strong>of</strong> the capacity to breathe’–has largely been accepted throughout<br />
the western world, since its inception in the 1960s. <strong>The</strong> debate surrounding brain (stem)<br />
death initially involved mainly clinicians, lawyers, philosophers, and religious leaders. This<br />
concept <strong>of</strong> death has been accepted in the United Kingdom and United Sates without much<br />
public debate, but in the last 20 years it has seen extensive public debate in Denmark,<br />
Germany, and also Japan. It remains interesting to note that worldwide the public voice was<br />
not heard as much in this debate as in the one on when ‘life’ begins.<br />
Although clinical diagnosis remains at the heart <strong>of</strong> the diagnosis <strong>of</strong> brain stem death,<br />
some countries specify additional special tests. <strong>The</strong>se may be required by law as an essential<br />
component <strong>of</strong> the diagnosis, or left to the discretion <strong>of</strong> the clinicians to be used as an additional<br />
decision-making tool. <strong>The</strong> special investigations also vary from country to country and<br />
include EEG, vascular flow studies, CT scanning, and MRI. Little work has been done to objectively<br />
assess the contribution and validity <strong>of</strong> these investigations.<br />
Also, the point <strong>of</strong> death remains a varying one. For example, in the United Kingdom,<br />
the time <strong>of</strong> death is recorded as the time when the first set <strong>of</strong> clinical tests confirm brain stem<br />
death, in Denmark it is recorded as the time when the heart stops.<br />
Although brain stem death has gained increasing acceptance over the last 30 years,<br />
many questions surrounding the philosophical concept <strong>of</strong> what death is and when it occurs,<br />
the diagnostic criteria, and confirmatory tests required still remain.<br />
Bibliography<br />
Beecher HK. A definition <strong>of</strong> irreversible coma. Report <strong>of</strong> the ad hoc committee <strong>of</strong> the<br />
Harvard Medical School to examine the definition <strong>of</strong> brain death.” JAMA 1968;<br />
205:337–40.<br />
Working Group <strong>of</strong> Conference <strong>of</strong> Medical Royal Colleges and their Faculties in the<br />
United Kingdom. <strong>The</strong> criteria for diagnosing brainstem death. J R Coll Phys<br />
(Lond) 1995; 29:281–2.<br />
Pallis C, Harley DH. ABC <strong>of</strong> brainstem death, second edition. London, BMJ Publishing<br />
Group, 1996.<br />
Improving Organ Donation Rates<br />
Walter Mauritz 1 , MD, Paul Sporn 2 , MD, Emanuel Sporn, MD 3<br />
1<br />
Department <strong>of</strong> Anesthesia and CCM, <strong>Trauma</strong> Center „Lorenz Boehler”, 2 Department <strong>of</strong><br />
Anesthesia and CCM, KA „Rudolfstiftung“, 3 Department <strong>of</strong> Surgery, University <strong>of</strong> Vienna,<br />
Vienna, Austria, EU<br />
Learning Objectives: To describe the current state <strong>of</strong> organ donation, as well as<br />
medical, organizational, financial, and legal approaches to improve donation rates.<br />
Methods. Medline searches for “organ donation rates”, “organ transplantation” (by<br />
organs), and “donation rate improvement” from 1994 – 2003. Internet search for “transplant<br />
statistics”. With a few exceptions, only data from the US and the EU were used.<br />
Results. <strong>The</strong>re is a serious worldwide shortage <strong>of</strong> transplantable organs. <strong>The</strong> maximum<br />
donation rate is estimated to be 50/mill.pop./yr; 35/mill.pop/yr is considered optimal.<br />
Most centers achieve only a fraction <strong>of</strong> this value, and many patients die on the lists. Different<br />
strategies have been employed to improve donation rates:<br />
• Medical: “Expanded donor criteria”: kidneys from elderly donors, non-heart-beating<br />
donors, donors with renal disease; livers from hepatitis C-positive donors, from aged donors<br />
(>70 yr!!); lungs from older donors (>55 yr), from smokers with >20 “pack yrs” (!), hearts<br />
from poisoned donors, and various organs from donors with a history <strong>of</strong> cancer have been<br />
used with good results. “New techniques”: split liver transplantation, xenotransplantation (?).<br />
All these options increase the rate <strong>of</strong> available organs by a considerable margin.<br />
• Organizational: Increasing awareness <strong>of</strong> medical staff that organ donation is an<br />
option, improving the request process, and improving donation logistics have all resulted in<br />
increased donation rates.<br />
• Financial: In some countries (e.g. Turkey, India), organs may be bought, which gives<br />
acceptable long-term results but higher rates <strong>of</strong> HIV- and hepatitis B-infected recipients. This<br />
is illegal in the EU and US, yet some ethically acceptable financial incentives (e.g., reim-<br />
54
<strong>ITACCS</strong> Spring 2003<br />
bursement for funeral expenses) are discussed.<br />
• Legal: <strong>The</strong> “Final Rule” was introduced in Hawaii in 1998; it states that “all hospitals<br />
are required to notify organ procurement organizations <strong>of</strong> all deaths and imminent deaths”<br />
in order to remain eligible for Medicare and Medicaid reimbursement. Donor referrals<br />
increased by 50%. Some EU countries use a “Presumed Consent” policy, thus avoiding the<br />
<strong>of</strong>ten difficult request process. This results in heart and lung transplantation rates that are at<br />
least twice as high as those from comparable EU countries.<br />
Conclusions. Many different strategies have been developed and tested. Each transplant<br />
center or organ procurement organization has to find the best way to deal with the local<br />
situation. With the right combination <strong>of</strong> techniques, an optimal donation rate should be<br />
possible to achieve.<br />
Managing the Donor<br />
Linda E. Pelinka, MD,1 and Emanuel Sporn, MD2<br />
1<br />
Department <strong>of</strong> Anesthesia and Critical Care Medicine, Lorenz Boehler <strong>Trauma</strong> Center,<br />
and 2 Clinical Department <strong>of</strong> Transplantation, Surgical University Clinic <strong>of</strong> Vienna,<br />
Vienna, Austria, European Union<br />
Learning Objectives: To review the pathophysiologic changes that occur after brain<br />
death and the clinical actions necessary to maintain the brain-dead, heart-beating donor.<br />
<strong>The</strong> most important limitation in organ transplantation is donor availability. For many<br />
patients with end-stage organ disease, the brain-dead, heart-beating donor is the only potential<br />
source from which to gain a healthy organ. Many available organs are lost to transplantation<br />
because <strong>of</strong> insufficient knowledge <strong>of</strong> the pathophysiology <strong>of</strong> brain death and because <strong>of</strong><br />
inadequate management <strong>of</strong> the potential donor.<br />
Pathophysiologic Changes. A brief parasympathetic phase is followed by intense<br />
catecholamine release, associated with increased systemic vascular resistance, myocardial<br />
work, and oxygen consumption. Subsequently, cardiac output and blood pressure drop and<br />
ischemic tissue injury is enhanced because the inotropic and chronotropic condition <strong>of</strong> the<br />
heart is impaired. Loss <strong>of</strong> antidiuretic hormone secretion causes diabetes insipidus, which is<br />
associated with hypernatremia, hypokalemia, hypocalcemia, and hypomagnesemia. Damage<br />
to the hypothalamus causes hypothermia. Plasminogen activator release causes disseminated<br />
intravascular coagulopathy.<br />
Aims <strong>of</strong> <strong>The</strong>rapy<br />
Ventilatory management: Lower FiO 2 as much as possible while keeping pO 2 >100<br />
mmHg and keep peak end-expiratory pressure 30% in multiple organ donors and >24% in<br />
other donors. Replace clotting factors with fresh frozen plasma and platelets. INR should be<br />
50.000.<br />
Electrolytes: Replace 0.9% saline with 0.45% saline and 5% dextrose water when sodium<br />
>136 mEq/L. Treat diabetes insipidus with a 4 µg bolus <strong>of</strong> desmopressin acetate; repeat<br />
every 4 hours if necessary. Urinary output should be approximately 1 ml kg –1 hr –1 .<br />
Kidney function: Administer furosemide if urinary output
<strong>ITACCS</strong> Spring 2003<br />
donation and recovery process, including the time frame/limit for death to occur. A<br />
written informed consent is obtained for organ and tissue donation, according to<br />
established TRC policies. <strong>The</strong> consent must be witnessed and signed by a hospital<br />
staff member. <strong>The</strong> TRC coordinator writes a detailed note in the patient’s hospital<br />
record regarding the consent process.<br />
9. All necessary laboratory and diagnostic testing is performed according to established<br />
TRC policies.<br />
10. <strong>The</strong> operating room staff is notified <strong>of</strong> the pending NHBD recovery. Space and OR<br />
nursing staff availability will be determined. Anesthesia services will not be required<br />
for the customary withdrawal <strong>of</strong> care. Arrangements for continuous palliative care<br />
should be made should donation be precluded.<br />
11. Once all necessary evaluation, organ placement arrangements, and recovery<br />
arrangements have been completed, and all members <strong>of</strong> the organ recovery team<br />
are in place, withdrawal <strong>of</strong> care will take place in accordance with individual hospital<br />
policies. <strong>The</strong> physician may order, as part <strong>of</strong> his/her usual and customary practice,<br />
ongoing pain relief, if in the physician’s belief it is medically and ethically necessary.<br />
No member <strong>of</strong> the TRC or the transplant team/center is present for or<br />
involved with this portion <strong>of</strong> the process.<br />
12. <strong>The</strong> patient’s vital signs are closely monitored and recorded every 5 minutes from<br />
the time the ventilator/pressor support is discontinued. <strong>The</strong> patient will be pronounced<br />
dead by the physician <strong>of</strong> record or intensivist designee after 5 minutes <strong>of</strong><br />
asystole as measured by 1) the absence <strong>of</strong> electrical activity, and 2) the absence <strong>of</strong><br />
an arterial pulse waveform, and 3) the absence <strong>of</strong> ventilatory efforts. Should death<br />
not occur within 60 minutes after discontinuing life support, the patient is returned<br />
to the intensive care unit or a private room for ongoing palliative care. After declaration<br />
<strong>of</strong> death, surgical recovery <strong>of</strong> organs occurs according to standard procedures<br />
as directed by the transplant recovery surgeons.<br />
Thank you to Charlie Alexander, RN, BSN, CPTC, Director, Development and Donor<br />
Services Center, TRC <strong>of</strong> Maryland, for the use <strong>of</strong> the above prepared information<br />
Living Donors<br />
Jane McNeill, MB ChB, FRCA<br />
<strong>The</strong> Royal London Hospital, London, UK<br />
— Session C —<br />
<strong>Trauma</strong> Airway Management: Hands-On Skills Station<br />
Andreas Thierbach, MD Mainz, Germany<br />
Jeffrey Berman, MD, Chapel Hill, North Carolina, USA<br />
James M. Rich, MA, CRNA, Dallas, Texas, USA<br />
Freddy Lippert, MD, Copenhagen, Denmark<br />
Marvin A. Wayne, MD, FACEP, Bellingham, Washington, USA<br />
William C. Wilson, MD, San Diego, California, USA<br />
Saturday, May 17, 2003<br />
Simultaneous Morning Sessions<br />
— Session A —<br />
Pediatrics<br />
Co-Chair: Gail E. Rasmussen, MD, Meridian, Mississippi, USA<br />
Co-Chair: Jeffrey M. Berman, MD, Chapel Hill, North Carolina, USA<br />
Emergency Airway Management in the Pediatric <strong>Trauma</strong> Patient<br />
Gail E. Rasmussen, MD<br />
Adjunct Clinical Faculty, Department <strong>of</strong> Anesthesiology, University <strong>of</strong> Mississippi Medical<br />
Center, Jackson, Mississippi, USA<br />
Learning Objectives: To review emergency airway management in the pediatric<br />
trauma patient. <strong>The</strong> lecture will include discussion <strong>of</strong> the difficult airway algorithm and<br />
alternative airway devices and cervical spine immobilization.<br />
<strong>The</strong> most immediate concern in the management <strong>of</strong> the pediatric trauma patient begins<br />
with the ABCs <strong>of</strong> resuscitation with airway assessment and assurance <strong>of</strong> adequate oxygenation.<br />
Without adequate oxygenation and effective ventilation, all other resuscitative efforts will be<br />
ineffective. Pediatric patients also force our hands more quickly than adults because the apneato-hypoxia<br />
interval is so much shorter and we are forced to intervene more quickly. Airway<br />
management in the trauma setting differs from other scenarios because <strong>of</strong> the need for cervical<br />
spine stabilization and immobilization, which may restrict options for intubation. <strong>The</strong> differences<br />
between adult and pediatric cervical spine injury will be delineated. One must recognize<br />
the need for airway intervention in the setting <strong>of</strong> respiratory distress and impending<br />
respiratory failure. This is <strong>of</strong>ten overlooked in the initial resuscitation, where there may be<br />
more concern for establishment <strong>of</strong> IV access than airway control.<br />
After initial assessment and relief <strong>of</strong> anatomic obstruction, patients who do not resume<br />
spontaneous ventilation and those with altered levels <strong>of</strong> consciousness (Glasgow Coma Scale<br />
score <strong>of</strong> 8 or less) will need more definitive airway protection and probably intubation. One<br />
must have the proper airway equipment available and checked before this is undertaken.<br />
Also, alternative airway adjuncts should be available should intubation prove difficult (including<br />
LMAs, jet ventilation equipment, and equipment for cricothyroidotomy).<br />
<strong>The</strong> trauma patient also poses an increased risk for aspiration <strong>of</strong> stomach contents<br />
because they are considered to be full stomachs. GI prophylaxis is optimal if time allows<br />
before undertaking a rapid sequence induction with cricoid pressure. <strong>The</strong> use <strong>of</strong> succinylcholine<br />
and its relative contraindications in the pediatric patient will be discussed. In the trauma<br />
setting, regardless <strong>of</strong> the age <strong>of</strong> the patient an anticholinergic agent is recommended (i.e.,<br />
atropine, 5-10 mcg/kg, up to a maximum <strong>of</strong> 0.4 mg, or glycopyrrolate, 0.1 mg/kg) prior to<br />
induction. <strong>The</strong>re has also been the recommendation, particularly in head trauma, to pretreat<br />
with 2 mg/kg <strong>of</strong> intravenous lidocaine prior to intubation. <strong>The</strong> sedative-hypnotic selected<br />
depends on the hemodynamic stability <strong>of</strong> the patient and the presence or absence <strong>of</strong> raised<br />
intracranial pressure (ICP). <strong>The</strong> top three choices include prop<strong>of</strong>ol, thiopentothal, and etomidate,<br />
depending on the particular circumstance <strong>of</strong> the patient.<br />
Once endotracheal intubation has been accomplished, confirmation <strong>of</strong> correct placement<br />
is essential, via auscultation. Tracheal rings can be visualized via bronchoscopy and the<br />
presence <strong>of</strong> carbon dioxide determined on capnogram or with an attachable CO2 detector.<br />
<strong>The</strong> pediatric trauma patient has several unique aspects in clinical practice that must<br />
be taken into consideration in the successful management <strong>of</strong> the emergency airway and ultimately<br />
the resuscitation.<br />
References<br />
McAllister JD, Gnauck KA. Rapid sequence intubation <strong>of</strong> the pediatric patient: fundamentals<br />
<strong>of</strong> practice. Ped Clin North Am 1999; 46:1249–84.<br />
Gausche M, Lewis RJ, Stratton SJ, et al. A prospective randomized study <strong>of</strong> the effect <strong>of</strong><br />
out-<strong>of</strong>-hospital pediatric endotracheal intubation on survival and neurological outcome.<br />
JAMA 2000; 283:783–90.<br />
O’Kelly SW, Reynolds PI, Collito M. <strong>The</strong> use <strong>of</strong> fiberoptic endoscopy and laryngeal mask<br />
airway in securing the traumatized airway in the pediatric patient. Am J Anesth<br />
1995; 22:152–3.<br />
Sedation/Analgesia/Anesthesia for Diagnostic Studies and Treatment<br />
Outside the Operating Room<br />
James E. Fletcher, MD<br />
Department <strong>of</strong> Anesthesia, University <strong>of</strong> North Carolina, Chapel Hill, North Carolina<br />
Learning Objectives: 1) To review pain management strategies for children with<br />
trauma-induced pain and 2) to consider various sedatives, analgesics, and anesthetic<br />
agents and the implications <strong>of</strong> their use on assessment procedures.<br />
In addition to experiencing the pain directly caused by trauma, children who have suffered<br />
injury may have to undergo procedures that provoke anxiety and pain as part <strong>of</strong> their<br />
diagnostic workup or treatment. <strong>The</strong> nature <strong>of</strong> the injury, ranging from an isolated fractured<br />
long bone to a semiconscious head injury with chest contusion, will affect the strategy chosen<br />
to manage the patient’s comfort and cooperation. Similarly, the proposed intervention<br />
will determine the use <strong>of</strong> anxiolytics, analgesics, sedatives, and anesthetics.<br />
Diagnostic studies may involve painful procedures such as tapping <strong>of</strong> the peritoneal<br />
cavity or invasive radiology such as angiography. Immobility is important for noninvasive radiology<br />
such as CT or MRI, particularly in the latter instance. Alternatively, a therapeutic intervention<br />
such as placement <strong>of</strong> a chest drain or fixation <strong>of</strong> a broken limb will require analgesia<br />
to facilitate cooperation.<br />
Central to any such intervention is an assessment <strong>of</strong> the patient’s cardiorespiratory system,<br />
including keen attention to either pre-existing or trauma-induced compromise <strong>of</strong> the<br />
airway or circulating blood volume.<br />
Pain should be assessed frequently in the pediatric population, as children are reluctant<br />
to report pain. <strong>The</strong> pain experience includes sensory qualities–where, when, how<br />
much–and motivational-affective qualities–emotional, aversive (‘hurt’), and pain-reducing<br />
behavior. Parental guidance is useful in understanding the child’s pain and distress behaviors.<br />
Children who have difficulty communicating, such as those with cognitive deficits or who do<br />
not speak English, are particularly difficult to assess. Age-specific methods <strong>of</strong> assessment are<br />
available. <strong>The</strong> pain language used by the child should be determined (e.g. ‘hurt’, ‘booboo’).<br />
Self-reporting is preferred in most children over 4 years <strong>of</strong> age; for those above age 7 years,<br />
a numerical pain scale may be used. Observation <strong>of</strong> body posture, activity, and facial expression<br />
may also help, although some apparently “normal” behavior may represent a coping<br />
mechanism for pain.<br />
Sedation, anesthesia, and systemic analgesia represent a spectrum <strong>of</strong> CNS depression,<br />
which has the potential to compromise the airway and cardiovascular system, while also providing<br />
humanitarian relief <strong>of</strong> suffering and facilitating successful diagnostic studies and treatment.<br />
“Conscious sedation” involves the use <strong>of</strong> CNS depressants to produce inattention, anxiolysis,<br />
and analgesia. <strong>The</strong> essential feature <strong>of</strong> this technique is that the patient remains conscious<br />
and able to respond to a mild stimulus–ideally, a voice. Once consciousness is lost, the<br />
child has lapsed into a state <strong>of</strong> light anesthesia, with its accompanying risks. As it is not possible<br />
to predict the effect <strong>of</strong> medication and the interaction <strong>of</strong> the medication with the<br />
patient’s medical state, full resuscitative equipment and expertise must be available at all<br />
times when sedation is administered.<br />
Often, sedative/analgesic drugs can be combined usefully with local anesthetic techniques.<br />
Options include IV (PCA) opioids, oral analgesics/sedatives, inhalation <strong>of</strong> nitrous oxide,<br />
ketamine, behavioral techniques, epidural local anesthetics and opioids, NSAIDs. Each drug has<br />
a specific pr<strong>of</strong>ile <strong>of</strong> anxiolysis, analgesia, and sedation, as well as specific pharmacological features<br />
such as speed <strong>of</strong> onset and duration <strong>of</strong> action, which affect selection. Because <strong>of</strong> this, the<br />
non-analgesic, slow onset/<strong>of</strong>fset sedative chloral hydrate is relatively unhelpful in comparison<br />
to morphine or fentanyl, combined with midazolam. Often, behavioral techniques can be combined<br />
with pharmacological methods. However, opioid analgesics and local anesthetics remain<br />
the cornerstone <strong>of</strong> procedural pain management. Sedative/anxiolytics should be reserved for<br />
non-painful procedures, as they will not relieve pain, while making assessment more difficult.<br />
All drugs should be given incrementally to effect.<br />
Pediatric Prehospital Care<br />
Dr. Charles D. Deakin<br />
Consultant Anaesthetist, Southampton University Hospital, Southampton, UK<br />
Learning Objectives:<br />
• To understand injury patterns in children.<br />
• To understand how differences in paediatric anatomy and physiology relate<br />
to injury patterns.<br />
• To understand the principles <strong>of</strong> prehospital trauma care in children.<br />
56
<strong>ITACCS</strong> Spring 2003<br />
• To understand splinting, packaging, and transport <strong>of</strong> injured children.<br />
Injury Patterns in Children. <strong>The</strong> commonest cause <strong>of</strong> death and injury in infants<br />
and children is trauma. In urban settings, 35% <strong>of</strong> accidents are due to pedestrian injury from<br />
motor vehicles, and a similar percent from falls from heights. Drowning and choking also<br />
contribute significantly to pediatric mortality, although the incidence <strong>of</strong> both is gradually<br />
decreasing. In Europe, blunt trauma accounts for 98% <strong>of</strong> injuries, whereas the pattern is very<br />
different in the USA, with penetrating trauma approaching 50% <strong>of</strong> all serious injuries. Child<br />
abuse is an under-reported cause <strong>of</strong> pediatric injury.<br />
Paediatric Anatomy and Pathophysiology. Anatomical and physiological differences<br />
in children result in increased risk for specific injuries. <strong>The</strong> head is disproportionately<br />
large, which, combined with weak neck muscles and underdeveloped protective arm reflexes,<br />
predisposes children to head injury. Raised intracranial pressure is more common than in<br />
adults and occurs more rapidly following head injury. Respiratory muscles are also underdeveloped,<br />
making respiratory failure more common and worsening secondary brain injury from<br />
ischemia and hypercapnia. Bone requires more energy than adults to cause fractures, and in<br />
chest trauma, lung contusion without overlying rib fracture is common. Abdominal organs are<br />
disproportionately large, and the liver and spleen are particularly susceptible to rupture following<br />
abdominal trauma. <strong>The</strong> large surface area:volume ratio predisposes to hypothermia.<br />
Principles <strong>of</strong> Prehospital <strong>Trauma</strong> Care in Children. Unlike adults, primary cardiac<br />
arrest is rare, and cardiac arrest in children is usually due to hypoxia where bradycardia<br />
rapidly progresses to asystole. Ventricular fibrillation is rare and <strong>of</strong>ten due to hyperkalaemia,<br />
tricyclic overdose, solvents, or hypothermia. Treatable causes <strong>of</strong> pulseless electrical activity<br />
must be excluded rapidly (hypovolaemia, tension pneumothorax, cardiac tamponade).<br />
Airway management in the traumatised child is a priority. A short neck, large tongue,<br />
large tonsils, large epiglottis, and high anterior larynx make endotracheal intubation more difficult.<br />
Attempts at pediatric intubation in obtunded children are likely to fail without the use<br />
<strong>of</strong> appropriate sedative and neuromuscular blocking drugs. <strong>The</strong> laryngeal mask airway is now<br />
being introduced to prehospital care in Europe for the management <strong>of</strong> difficult paediatric airways.<br />
Prehospital surgical airways are particularly challenging. Gastric decompression with an<br />
orogastric tube may improve tidal volumes and lower airway pressures. Cardiovascular compensation<br />
to acute hypovolaemia is more marked in children than adults and a hypotensive<br />
child will be severely hypovolaemic. Bleeding into body cavities must be carefully excluded.<br />
Venous access is difficult because <strong>of</strong> small size, overlying adipose tissue, and venous collapse.<br />
Intraosseous access should be gained early. Effective analgesia is particularly important in<br />
children, and requires opioids and local or even general anaesthesia.<br />
Splinting, Packaging, and Transport <strong>of</strong> Injured Children. Careful splinting and<br />
packaging <strong>of</strong> children is vital for successful and safe transfer, particularly by air. Parents are<br />
generally a better alternative to sedation during transfer <strong>of</strong> the injured child.<br />
Reference<br />
Mazurek AJ, Meyer PG, Rasmussen GE. Prehospital trauma management <strong>of</strong> the pediatric<br />
patient. In Soreide E, Grande CM, eds. Prehospital <strong>Trauma</strong> Care. New York,<br />
Marcel Dekker, 2001, pp 421–40.<br />
Pediatric Head Injury: Where Have We Been; Where Are We Going?<br />
Jeffrey M. Berman, MD<br />
University <strong>of</strong> North Carolina, Chapel Hill, North Carolina<br />
Learning Objectives: 1) To appreciate changes in morbidity and mortality statistics,<br />
2) to appreciate the evolution <strong>of</strong> clinical management <strong>of</strong> pediatric head injury, 3) to<br />
appreciate evolving management strategies, and 4) to understand current guidelines.<br />
Mortality. <strong>The</strong> December 6, 2002, MMWR reported an 11.4% decline in mortality<br />
related to traumatic brain injury (TBI). <strong>The</strong>se statistics, which cover the decade from January<br />
1989 to December 1998, also document the changes in the etiology <strong>of</strong> injury among patient<br />
groups, including children. <strong>The</strong> three leading causes <strong>of</strong> TBI death are motor vehicles,<br />
firearms, and falls. Motor vehicle crashes persist as the leading cause <strong>of</strong> TBI and subsequent<br />
deaths amongst children (1–19 years <strong>of</strong> age).<br />
Evolution <strong>of</strong> Clinical Management. In the past, clinical management <strong>of</strong> head injury<br />
focused on control <strong>of</strong> ICP. <strong>The</strong> modalities used to accomplish that goal were hyperventilation<br />
(to PaCO 2 into the mid 20s), barbiturates (including barbiturate coma), steroids, fluid restriction,<br />
osmolar and diuretic therapy (mannitol, furosimide), and nursing care delivered in the<br />
head-up position (~30˚). Simultaneous with a shift in focus to prevention <strong>of</strong> secondary brain<br />
injury, more sophisticated means to measure cerebral hemodynamics became available.<br />
<strong>The</strong>se technologies made it apparent that in order to avoid secondary injury the therapeutic<br />
focus ought be on brain perfusion, especially in the penumbra <strong>of</strong> primary injury. To achieve<br />
this endpoint, a variety <strong>of</strong> modalities coupling brain monitoring with pharmacological and/or<br />
mechanical interventions are being employed (e.g., measurement <strong>of</strong> jugular venous saturation,<br />
drainage <strong>of</strong> CSF, osmotic therapy using hypertonic saline, induced mild hypothermia,<br />
and maintaining normocapnia).<br />
Current Guidelines. Current recommendations are based on the aforementioned<br />
principle <strong>of</strong> maintaining cerebral perfusion. At a minimum, ICP monitoring ought be<br />
employed in every child who has sustained a severe TBI (GCS score 40 mmHg in younger children and >50 in older children and<br />
adolescents. PaCO 2 ought range from 35-38 unless treating impending intracranial herniation.<br />
Osmolar therapy using mannitol or hypertonic saline may be <strong>of</strong> use but lacks definitive<br />
evidence, as does the use <strong>of</strong> barbiturates.<br />
Conclusion. Though much progress has been made in the identification <strong>of</strong> cellular<br />
mechanisms and likely triggers <strong>of</strong> pathophysiology, we have yet to produce unequivocal<br />
definitive therapies for TBI. Nevertheless, prevention efforts and aggressive neurointensive<br />
care focused on prevention <strong>of</strong> secondary brain injury have yielded very gratifying reductions<br />
in morbidity and mortality. As every year, we are hoping that discovery <strong>of</strong> the “silver bullet”<br />
is just days or months away. We are closer but have not yet achieved that goal.<br />
Fluid Management <strong>of</strong> the Injured Child<br />
Calvin Johnson, MD<br />
Charles R. Drew University <strong>of</strong> Medicine, Martin Luther King Jr. Medical Center, Los<br />
Angeles, California, USA<br />
Learning Objective: To educate the participant about assessing volume status,<br />
recent advances in fluid management, and a rational therapeutic approach for fluid<br />
administration in the injured child.<br />
<strong>The</strong> leading cause <strong>of</strong> death in children age 1 to 14 years in the developed world is<br />
trauma. <strong>The</strong> major cause <strong>of</strong> disability in children is trauma. It has been reported that inadequate<br />
evaluation and inappropriate treatment contributes to 30% <strong>of</strong> early deaths in children<br />
with severe trauma. 1<br />
Prompt and accurate assessment and treatment are critical in the prevention <strong>of</strong> unnecessary<br />
pediatric morbidity and mortality from trauma. <strong>The</strong> most crucial first step in providing<br />
for the injured child is the establishment <strong>of</strong> adequate oxygenation and ventilation. Once oxygenation<br />
has been established, intravenous access and the administration <strong>of</strong> appropriate<br />
intravenous fluids are essential.<br />
Assessment <strong>of</strong> the pediatric circulatory system must take into account the following.<br />
Shock in children may exist with a normal blood pressure. In children, cardiac output<br />
decreases in a linear fashion as blood volume decreases; however, blood pressure may<br />
remain unchanged. In the pediatric patient, stroke volume is fixed; thus, cardiac output in<br />
the face <strong>of</strong> hypovolemia is maintained by increasing the heart rate and peripheral vascular<br />
resistance. When cardiac reserve is exhausted, bradycardia indicates significantly decreased<br />
blood volume.<br />
Intravenous access must be obtained while assessing the severity <strong>of</strong> injuries. With significant<br />
blood loss, the child’s compensatory vasoconstriction can make IV access difficult.<br />
Attempts at IV access should be limited to 60-90 seconds, and if unsuccessful, the clinician<br />
should proceed to insertion <strong>of</strong> an intra-osseous needle. Be sure to avoid the leg with a suspected<br />
tibial/femoral fracture or vascular injury. All IV fluids should be warmed to 37˚C.<br />
Children have small blood volumes and cannot afford to lose large amounts <strong>of</strong> blood.<br />
Occult blood losses from the head (especially scalp) and neck region can result in significant<br />
hemodynamic instability. Aggressive control <strong>of</strong> bleeding is indicated. Remember, a hemodynamically<br />
unstable child should never be sent to CT scan to determine the site <strong>of</strong> bleeding.<br />
That child must be taken to the OR for surgical exploration. <strong>The</strong> choice <strong>of</strong> colloid over crystalloid<br />
for the initial resuscitation has been reported to increase the mortality by 4%.<br />
Crystalloids 20 ml/kg times 2 doses should be given and if no improvement in hemodynamics<br />
occurs, then administer blood 10ml/kg. Colloids should be given only as a temporizing<br />
measure while you are waiting for blood products. 2 Dextrose-containing fluids should be<br />
given only when there is laboratory evidence <strong>of</strong> hypoglycemia.<br />
In the management <strong>of</strong> traumatic brain injury, the goal is maximizing cerebral perfusion<br />
pressure and reducing ICP. <strong>The</strong> early introduction <strong>of</strong> inotropes maintaining MAP <strong>of</strong> 70mmHg<br />
is recommended to avoid fluid overload.<br />
References<br />
1. Delayed diagnosis <strong>of</strong> injury in pediatric trauma. Pediatrics 1996; 98:56–62.<br />
2. Fluid resuscitation with colloid or crystalloid solutions in critically ill patients: a systematic<br />
review <strong>of</strong> randomized trials. BMJ 1998; 316:961–4.<br />
Early Care <strong>of</strong> the Pediatric Burn Patient<br />
Gary F. Purdue, MD<br />
Pr<strong>of</strong>essor, Department <strong>of</strong> Surgery, UT Southwestern Medical Center, Dallas, Texas, USA<br />
Learning Objectives: 1) to learn to recognize the elements <strong>of</strong> burn severity and<br />
understand the components <strong>of</strong> a major pediatric burn, 2) to recognize the different types<br />
<strong>of</strong> inhalation injury, and 3) to appreciate the special aspects <strong>of</strong> burn treatment, including<br />
thermal maintenance, airway protection, and fluid resuscitation.<br />
Children are at special risk <strong>of</strong> burn injury, comprising one third <strong>of</strong> burn center admissions.<br />
A plan <strong>of</strong> initial burn assessment and therapy includes the care essential for all cases,<br />
specific treatments for minor burns, and the special requirements <strong>of</strong> major thermal trauma.<br />
Rapid estimation <strong>of</strong> body surface area burned permits planning <strong>of</strong> immediate management<br />
and fluid therapy and dictates the needs for definitive care. Only second- and thirddegree<br />
burns are tabulated with Lund-Browder or Berkow charts providing correction for<br />
age. <strong>The</strong> “Rule <strong>of</strong> Nine’s” is not appropriate for children.<br />
While depth <strong>of</strong> injury is important in determining the choice <strong>of</strong> care and ultimate outcome,<br />
initial evaluation is difficult. Characteristics will be discussed.<br />
Burns <strong>of</strong> the face, hands, feet, and perineum/genitalia present special problems, while<br />
burned children
<strong>ITACCS</strong> Spring 2003<br />
— Session B —<br />
Prehospital Care<br />
Co-Chair: Charles D. Deakin, MA MD MRCP FRCA, Southampton, UK<br />
Co-Chair: Marvin A. Wayne, MD, FACEP, Bellingham, Washington, USA<br />
Isolated ext injuries<br />
Mechanism<br />
GLF<br />
Moderate speed MVA<br />
High speed MVA<br />
Falls >20 feet<br />
GSW's<br />
Negative<br />
Uncertain<br />
Positive<br />
Use <strong>of</strong> Capnography in Pre-Hospital <strong>Trauma</strong> Care<br />
Dr. Charles D. Deakin<br />
Consultant Anaesthetist, Southampton University Hospital, Southampton, UK<br />
Learning Objectives:<br />
• To understand the physiology <strong>of</strong> CO2 production and excretion.<br />
• To understand the techniques <strong>of</strong> measuring end-tidal CO2.<br />
• To understand changes in end-tidal CO2 in relation to pathophysiology.<br />
• To understand predictive value <strong>of</strong> end-tidal CO2 in relation to outcome.<br />
What is End-Tidal Carbon Dioxide? Cellular metabolism results in carbon dioxide<br />
(CO2) formation as a by-product <strong>of</strong> adenosine triphosphate (ATP) production. CO2 is excreted<br />
by the cell, and ultimately by the body, to maintain normal homeostasis. CO2 diffuses out<br />
<strong>of</strong> the cell to enter the blood stream, where it is carried in the plasma or in erythrocytes. As<br />
blood flows through the lungs and the alveolar capillaries, a diffusion gradient causes CO2 to<br />
diffuse from the blood into alveolar air spaces. <strong>The</strong> CO2 is then excreted from the alveolar air<br />
spaces in expired air. <strong>The</strong> CO2 in expired air can be measured using capnography. <strong>The</strong> peak<br />
CO2 in expired air is maximal at end-expiration (end-tidal CO2; PetCO2) and equates approximately<br />
to arterial CO2 (PaCO2).<br />
How is end-tidal carbon dioxide measured? End-tidal CO2 is measured directly<br />
from respiratory gases. <strong>The</strong>re are two methods by which it can be measured:<br />
• Colorimetric CO2 detectors change colour when exposed to CO2.<br />
• Electronic measurement. Uses spectrophotometry to give a real-time value <strong>of</strong><br />
CO2.<br />
End-Tidal Carbon Dioxide and Cardiac Output. In low cardiac output states,<br />
blood flow to the lungs is low, so that relatively few alveoli are perfused. Since tidal volumes<br />
delivered with a resuscitation bag tend to be large, many alveoli are ventilated that are not<br />
perfused and consequently the PetCO2 is low. If the blood flow to the lungs improves, more<br />
alveoli are perfused and PetCO2 will increase. Providing the lungs are ventilated at a fixed<br />
minute volume (rate x tidal volume), changes in PetCO2 are proportional to changes in cardiac<br />
output.<br />
Use <strong>of</strong> Capnography in Pre-Hospital Care<br />
1. Confirmation <strong>of</strong> endotracheal intubation. In a patient with a spontaneous cardiac<br />
output, correct endotracheal intubation will immediately show the presence<br />
<strong>of</strong> CO 2 , whereas oesophageal intubation results in absence <strong>of</strong> PetCO 2 . In<br />
the absence <strong>of</strong> cardiac output, PetCO 2 is minimal and correct endotracheal<br />
placement should be confirmed by other means.<br />
2. Operator fatigue. Because PetCO 2 is proportional to cardiac output, PetCO 2 is<br />
an indicator <strong>of</strong> the effectiveness <strong>of</strong> cardiac massage. Decreased PetCO 2 during<br />
cardiac massage may indicate operator fatigue. 1<br />
3. Indication <strong>of</strong> the return <strong>of</strong> spontaneous cardiac activity. An increase in PetCO 2 is<br />
<strong>of</strong>ten the first indicator <strong>of</strong> the return <strong>of</strong> spontaneous circulation. 1,2<br />
4. Indication <strong>of</strong> adequate ventilation. PetCO 2 is a marker <strong>of</strong> adequate ventilation<br />
because it approximates to arterial CO 2 . Ventilation <strong>of</strong> trauma patients using<br />
capnography results in more optimal PaCO 2 values. 3<br />
5. Prediction <strong>of</strong> outcome. Patients suffering primary cardiac arrest in whom<br />
PetCO 2 has failed to rise above 1. 4 kPa after 20 minutes <strong>of</strong> advanced life support<br />
are extremely unlikely to survive. 4 Only 5% trauma patients with PetCO 2
<strong>ITACCS</strong> Spring 2003<br />
IVF resuscitation in certain uncontrolled hemorrhage models and one major clinical study<br />
has even shown the efficacy <strong>of</strong> withholding IVF infusions preoperatively in those patients<br />
with penetrating torso injuries (versus the standard rapid infusions <strong>of</strong> IVF in both the prehospital<br />
and emergency department settings). It is therefore speculated that BP elevation,<br />
prior to achievement <strong>of</strong> hemostasis, may actually increase mortality in certain subgroups <strong>of</strong><br />
injury patients. <strong>The</strong> rationale, experimental evidence, scientific design, and limitations <strong>of</strong><br />
these studies will be examined and qualified in this discussion. In addition, the concept <strong>of</strong><br />
using hypertonic solutions and new hemoglobin-based oxygen carriers in such circumstances<br />
will be analyzed as well.<br />
Bibliography<br />
Bickell W, Wall M, Pepe P, et al. Immediate versus delayed fluid resuscitation for<br />
hypotensive patients with penetrating torso injuries. Resuscitation 1995;<br />
29(2):183–4.<br />
Dutton R, Mackenzie C, Scalea T. Hypotensive resuscitation during active hemorrhage:<br />
impact on in-hospital mortality. J <strong>Trauma</strong> 2002; 52:1141–6.<br />
Fowler RL, Pepe PE. Prehospital care <strong>of</strong> the patient with major trauma. Emerg Med Clin<br />
North Am 2002; 20:953–74.<br />
Manning JE, Katz LM, Brownstein MR, et al Bovine hemoglobin-based oxygen carrier<br />
(HVOC-291) for resuscitation <strong>of</strong> uncontrolled, exsanguinating liver injury in swine.<br />
Shock 2000; 13:152–9.<br />
Pepe PE, Lurie K, Raedler C. Emergency ventilatory management in hemorrhagic<br />
states: elemental or detrimental? J <strong>Trauma</strong> June 2003; 54(6), in press.<br />
Pepe PE, Mosseso V, Falk JL. Prehospital fluid resuscitation <strong>of</strong> the patient with major<br />
trauma. Prehosp Emerg Care 2002; 6(1):81–91.<br />
Stern SA. Low-volume fluid resuscitation for presumed hemorrhagic shock: helpful or<br />
harmful. Curr Opin Crit Care 2001; 7:422–30.<br />
Stern SA, Wang X, Mertz M, et al. Effect <strong>of</strong> initially limited resuscitation in a combined<br />
model <strong>of</strong> fluid percussion brain injury and severe uncontrolled hemorrhagic shock.<br />
J Neurosurg 2000; 93:305–14.<br />
Stern SA, Zink BJ, Mertz M, et al. Under resuscitation <strong>of</strong> near-lethal uncontrolled hemorrhage:<br />
effects on mortality and end-organ function at 72 hours. Shock 2001;<br />
15:16–23.<br />
Prehospital Use <strong>of</strong> Hypertonic Saline Derivatives<br />
Pr<strong>of</strong>essor Pierre Carli, MD, PhD<br />
Department <strong>of</strong> Anesthesiology, Hôpital Necker–Enfants Malades, Paris, France<br />
Learning Objectives: 1) To understand the importance <strong>of</strong> correct assessment <strong>of</strong> the<br />
status <strong>of</strong> trauma cases in the prehospital setting and 2) to learn the use <strong>of</strong> small-volume<br />
hypertonic solutions in penetrating trauma for rapid fluid replacement, providing a modified<br />
systemic arterial pressure capable <strong>of</strong> maintaining vital functions while limiting the<br />
possibility <strong>of</strong> further hemorrhage.<br />
Hypertonic saline solutions associated with colloids are particularly suitable for prehospital<br />
use in major trauma.<br />
In European EMS systems, where physicians are involved in prehospital care, three<br />
steps <strong>of</strong> management are closely linked. First, the on-site evaluation <strong>of</strong> the patient is essential<br />
to assess the mechanism <strong>of</strong> the injuries and the respiratory and ventilatory status. Special<br />
care must be taken with penetrating trauma with hypotension or multiple blunt trauma with<br />
severe brain injury because the management <strong>of</strong> these patients is different.<br />
Second, on-site respiratory management in order to provide efficient airway ventilation<br />
and oxygenation is the first priority <strong>of</strong> treatment. Stabilisation <strong>of</strong> respiratory status improves<br />
patient survival. Prehospital intubation is indicated in severe trauma patients who are unconscious<br />
(GCS
<strong>ITACCS</strong> Spring 2003<br />
ble range <strong>of</strong> chemical and biological agents regarded as hazards is wide, the number that pose<br />
real threats is limited, particularly when being deployed by terrorists. A study <strong>of</strong> agents that<br />
have been used such as sarin and anthrax, together with experience gained from civil accidental<br />
releases, provides a basis for anesthesiological training to provide an effective response.<br />
Terror-Induced, Multiple Casualty Events: Injury Patterns and Emergency<br />
Department Response<br />
Amir Blumenfeld, Yahav Oron, Oleg Zaslavsky, Eitan Melamed, Ron Ben-Avraham, Guy Lin<br />
IDF Medical Corps <strong>Trauma</strong> Branch<br />
Learning Objectives: To review and discuss the types <strong>of</strong> injuries caused by suicidal<br />
terrorist attacks and to consider the implications <strong>of</strong> these injury patterns on emergency<br />
medical systems.<br />
By September 2000, the Israeli-Palestinian conflict escalated by what was later known<br />
as the “Al-Aksa Intifada.” It was a combination <strong>of</strong> civilian population riots and low-intensity<br />
military conflict between the Israeli army (IDF) and the Palestinian armed forces. Soon after<br />
these riots, which started in the west bank and Gaza strip, got into the hearts <strong>of</strong> the Israeli<br />
cities and towns and, by changing its nature to suicidal terrorist attacks, caused severe<br />
injuries and death among children, women, and men.<br />
Up to December 2002, more than 5,000 civilians and security force personnel had been<br />
injured. About 700 people were killed, 370 <strong>of</strong> them in multiple casualty events (MCE) caused<br />
by explosives carried on suiciders’ bodies or hidden in cars.<br />
In order to define injury patterns and estimate the needs <strong>of</strong> the injured, we conducted<br />
a retrospective survey. Data were collected from EMS (operational and medical) records,<br />
police reports, ED records, trauma registry files, and specially designed questionnaires run<br />
among ED personnel.<br />
MCE victims were divided into three groups by location <strong>of</strong> occurrence: open spaces<br />
(N=316), closed spaces (N=280), and buses (N=260). Injury severity as well as EMS and hospital<br />
resource utilization and patients’ immediate outcomes were analyzed according to this<br />
division.<br />
As a rule, an indoor blast magnifies both casualty generation and injury severity.<br />
Mortality rate, which ranged between 8% and 22%, was the highest among bus explosion victims.<br />
Severe injuries (ISS>16) rate ranges between 7% and 11.4%, while acute stress reaction<br />
is a common consequence (37% to 52%), especially among people injured in open spaces.<br />
Emergency interventions such as endotracheal intubation, chest drain insertion, and ED thoracotomy<br />
as well as operative procedures and ICU admission were needed much more frequently<br />
by victims injured in confined-space explosions. Though gathered experience<br />
improved hospitals’ performance, there was still an “over-recruitment” phenomena <strong>of</strong> medical<br />
resources on both the prehospital and ED level.<br />
<strong>The</strong> results and conclusions drawn from this study may serve as a basis for future planning<br />
<strong>of</strong> national emergency medical systems.<br />
— Session C —<br />
CRNA Session<br />
Chair: James M. Rich, MA, CRNA, Dallas, Texas, USA<br />
Vascular Access for <strong>Trauma</strong> Anesthesia:<br />
Options, Risks, Benefits, and Complications<br />
Deborah B. Latham, MHS, CRNA-P<br />
Department <strong>of</strong> Nurse Anesthesia, Baylor University Medical Center, Dallas, Texas<br />
Learning Objectives: 1) To compare and contrast the classifications <strong>of</strong> shock, 2) to<br />
discuss the number, size, and location necessary for vascular access in trauma, 3) to<br />
understand the acute and chronic complications associated with vascular access, and 4)<br />
to discuss the options for vascular access for children younger than 5.<br />
Multiple trauma patients with hemorrhagic shock require rapid intravenous access<br />
after airway patency and ventilation are established. Timely restoration <strong>of</strong> intravascular volume<br />
improves systemic perfusion, alleviates tissue hypoxia and acidosis, and arrests cell<br />
death and progression to irreversible shock. <strong>The</strong>rapeutic goals include restoring volume<br />
deficits and preventing further loss. 1 <strong>The</strong> type and location <strong>of</strong> injury, duration and rate <strong>of</strong><br />
blood loss, and classification <strong>of</strong> hemorrhagic shock (Table 1) will mandate the size, number,<br />
and location <strong>of</strong> intravenous catheters.<br />
Table 1. Classes <strong>of</strong> Shock 2<br />
Class Blood Heart Rate Blood Pulse Respirations/min<br />
loss (mL)/% Pressure Pressure<br />
Total Blood<br />
Volume<br />
Class 1 2000<br />
>40% >140 Decreased Decreased >35<br />
ATLS protocol recommends insertion <strong>of</strong> two large-bore (16g or larger) IV catheters<br />
before insertion <strong>of</strong> a central venous catheter or venous cutdown in patients with severe<br />
injuries and hemorrhagic shock. 3 Classes 2, 3, and 4 shock warrant central venous access for<br />
fluid replacement and monitoring.<br />
When considering a location for IV access, several factors are considered. Injuries<br />
below the diaphragm require one IV placed in a tributary <strong>of</strong> the superior vena cava because<br />
<strong>of</strong> possible disruption <strong>of</strong> the inferior vena cava. Patients with upper chest and neck injuries<br />
require access in lower extremities because superior vena cava disruption may be present. In<br />
multisystem trauma, large-bore IV access above and below the diaphragm is necessary.<br />
Patients in hypovolemic shock need rapid administration <strong>of</strong> IV fluids through short<br />
large-bore catheters. Doubling internal diameter <strong>of</strong> the catheter increases flow 16-fold. Eight<br />
and nine French large-bore catheter introducers deliver flow rates nearly twice as fast as short<br />
14g catheters and can be used in subclavian, internal and external jugular, femoral, and antecubital<br />
sites. 4<br />
Catheterization <strong>of</strong> large central veins provides access for rapid infusion and measurement<br />
<strong>of</strong> central venous pressure. Table 2 summarizes acute and chronic complications <strong>of</strong> subclavian<br />
and internal jugular catheters. Anesthesia providers must be aware <strong>of</strong> these complications,<br />
especially if the patient’s condition does not improve or deteriorates during anesthesia.<br />
Table 2. Acute and Chronic Complications <strong>of</strong><br />
Subclavian and Internal Jugular Catheters<br />
Acute Complications 5,6 Late Complications 5,6<br />
Cardiac arrhythmias<br />
Infection<br />
Arterial puncture<br />
Sepsis<br />
Pneumothorax<br />
Intravascular thrombosis<br />
Hydrothorax<br />
Pseudoaneurysm<br />
Air embolism<br />
Arteriovenous fisula formation<br />
Horner’s Syndrome<br />
Thoracic duct injury<br />
Guidewire or catheter fragment embolization<br />
Cardiac tamponade<br />
Vessel perforation with hemorrhage<br />
Cerebral infarction<br />
Phrenic nerve injury<br />
Brachial plexopathy<br />
Intraosseous catheters can be used in children younger than 5 years <strong>of</strong> age because the<br />
cortical bone is s<strong>of</strong>ter. Specifically designed intraosseous needles are available and flow rates<br />
<strong>of</strong> 40 mL/min with crystalloids using pressure bags have been achieved. 7 Complications<br />
include disruption <strong>of</strong> the growth plate, cellulitis, osteomyelitis, fat embolism, and extravasation<br />
<strong>of</strong> fluids into the surrounding tissue.<br />
Anesthesia providers must be skilled in each catheterization technique and utilize the<br />
technique with which they are most experienced. However, they should have the expertise<br />
to perform as many techniques as warranted by the situation. Diligent observation for possible<br />
complications should be an ongoing process during anesthesia. Successful vascular access<br />
is <strong>of</strong> prime importance in preventing morbidity and mortality in trauma.<br />
References<br />
1. Sweeney MN. Vascular access in trauma: options, risks, benefits, and complications.<br />
Anesthesiol Clin North Am 1999; 17(1):97–106.<br />
2. Abraham E, Shapiro M, Podolsky S. Central venous catheterization in the emergency<br />
setting. Crit Care Med 1983; 11:515–7.<br />
3. Millikan JS, Cain TL, Hansbrough J, et al. Rapid volume replacement for hypovolemic<br />
shock: a comparison <strong>of</strong> techniques and equipment. J <strong>Trauma</strong> 1984;<br />
24:428–31.<br />
4. Bickell V, Pepe PE, Mattox KL. Complications <strong>of</strong> resuscitation. In Mattox KL, ed.<br />
Complications <strong>of</strong> <strong>Trauma</strong>. New York, Churchill Livingstone, 1994.<br />
5. Eckhard WF, Iaconetti J, Kwon JS, et al. Inadvertent carotid artery cannulations during<br />
pulmonary artery catheter insertion. J Cardiothorac Vasc Anesth 1996;<br />
10:283–90.<br />
6. Shoor PM, Berryhill RE, Benum<strong>of</strong> JL. Intraosseous infusion: pressure-flow relationship<br />
and pharmacokinetics. J <strong>Trauma</strong> 1979; 19:722–4.<br />
7. Alexander HA, Proctor HJ. Advanced <strong>Trauma</strong> Life Support, 5th edition. Chicago,<br />
American College <strong>of</strong> Surgeons, 1993.<br />
Massive Volume Replacement in the <strong>Trauma</strong> Patient<br />
Charles R. Barton, CRNA, MSN, M.Ed.<br />
Director, Graduate Anesthesia Program, <strong>The</strong> University <strong>of</strong> Akron<br />
College <strong>of</strong> Nursing, Akron, Ohio, USA<br />
Learning Objective: To discuss the means <strong>of</strong> evaluating hemorrhagic blood loss<br />
and the appropriate replacement fluids in the trauma patient sustaining severe injuries.<br />
Hemorrhagic blood loss in the trauma patient leads to shock and increased mortality<br />
unless treated promptly and appropriately at the earliest possible time following initial injury.<br />
With an adequate understanding <strong>of</strong> the mechanism <strong>of</strong> injury, the anesthetist develops a high<br />
index <strong>of</strong> suspicion for potential high volume <strong>of</strong> blood loss in patients with significant thoracic,<br />
abdominal, and pelvic injuries. Additionally, conditions such as bilateral femoral fractures and<br />
major vascular injuries are also associated with substantial hemorrhage.<br />
Initial Assessment and Management. In an ideal trauma system, intravenous fluids are<br />
initiated at the scene. Volume resuscitation is administered vigorously until the patient<br />
appears to normalize physiological parameters. Desirable endpoints include an adequate<br />
blood pressure, reasonable pulse rate, appropriate capillary refill, and 1-2 ml/kg urinary output<br />
per hour.<br />
In the trauma center resuscitation area, several large-bore intravenous catheters are<br />
placed and blood is drawn for determination <strong>of</strong> a CBC, SMAC, coagulation panel, and toxicology<br />
screen. <strong>The</strong> establishment <strong>of</strong> venous access facilitates volume restoration and provides a<br />
route for intravenous drug administration. During CPR, peripheral lines are placed. Following<br />
restoration <strong>of</strong> spontaneous circulation, central venous lines are placed as indicated.<br />
In life-threatening situations, type O-negative (or alternatively O-positive) blood is<br />
transfused without type and cross-matching. If time permits, generous volumes <strong>of</strong> crystalloid<br />
and colloid fluids are given with continuous evaluation <strong>of</strong> the patient’s clinical presentation.<br />
Concurrently, hemogloblin and hematocrit values are determined to guide progress <strong>of</strong> resuscitation<br />
and the need for additional blood.<br />
Management <strong>of</strong> major blood loss will include the placement <strong>of</strong> several large-bore intravenous<br />
catheters and placement <strong>of</strong> appropriate invasive physiological monitors. Liberal<br />
administration <strong>of</strong> balanced salt solution is used. Colloids are used to rapidly increase intravascular<br />
volume to aid in restoration <strong>of</strong> adequate blood pressure and appropriate pulse rate.<br />
During surgery, red blood cell salvaging is helpful in reducing the need for additional bank<br />
blood. Efficient fluid warming and adequate capacity to pump fluids at high flow rates are<br />
used to prevent hypothermia and to provide rapid fluid replacement. Initial comprehensive<br />
assessment and aggressive fluid resuscitation will <strong>of</strong>ten allow the anesthetist to avoid the<br />
need for ACLS drug interventions.<br />
Conclusions. Fluid resuscitation <strong>of</strong> the trauma patient is a critical element in the over-<br />
60
<strong>ITACCS</strong> Spring 2003<br />
all anesthetic management. Early establishment <strong>of</strong> adequate venous access and administration<br />
<strong>of</strong> warmed crystalloid and colloid fluids and blood products are essential to initial resuscitation.<br />
Fluid management is based on careful assessment and monitoring <strong>of</strong> physiological and<br />
laboratory values. <strong>The</strong> principles <strong>of</strong> successful management <strong>of</strong> the trauma patient are based on<br />
organization and preparation, assessment <strong>of</strong> the patient’s injuries, proper priority for therapeutic<br />
interventions, achievement and maintenance <strong>of</strong> a patent airway, fluid resuscitation,<br />
application <strong>of</strong> appropriate continuous invasive and noninvasive monitoring, correction <strong>of</strong> acidbase<br />
and electrolyte disturbances, and careful titration <strong>of</strong> anesthetic and adjunctive agents.<br />
<strong>The</strong> degree <strong>of</strong> functional outcome <strong>of</strong> trauma patients is largely dependent on the early involvement<br />
<strong>of</strong> sound principles <strong>of</strong> anesthesia care in the resuscitation and overall anesthetic management<br />
during the perioperative period. In a well-managed team approach, assessment and<br />
treatment are carried out in rapid succession or even simultaneously.<br />
Suggested Readings<br />
Barton CR. <strong>Trauma</strong> anesthesia. In Nagelhout J, Zaglaniczny K, eds. Nurse Anesthesia,<br />
2nd edition. Philadelphia, WB Saunders, 2001, pp 824–47.<br />
Barton CR, Beeson M, Campbell J. Anesthesia for the trauma patient. Curr Rev Nurse<br />
Anesth 1998; 20:241–52.<br />
Barton CR. Anesthesia for the trauma patient. In McIntosh LW, ed. Essentials <strong>of</strong> Nurse<br />
Anesthesia. New York, McGraw-Hill, 1997, pp 477–97.<br />
Grande CM. Mechanisms and patterns <strong>of</strong> injury: the key to anticipation in trauma management.<br />
Crit Care Clin 1990; 6:25–35.<br />
to percussion <strong>of</strong> one hemithorax, distended neck veins, or tracheal shift. An upright expirational<br />
chest radiograph provides definite information if the problem is significant. However,<br />
if the trauma patient is unstable, a large-bore intravenous catheter is inserted into the superior<br />
portion <strong>of</strong> the second intercostal space along the midclavicular line.<br />
Many thoracic injuries can be life threatening. Massive hemothorax, which can be<br />
caused by bleeding from the heart and great vessels, must be treated immediately. Adequate<br />
fluid resuscitation is accomplished before placement <strong>of</strong> chest tubes. Chest tubes allow<br />
drainage <strong>of</strong> blood from the pleural cavity but can lead to more extensive bleeding and<br />
hypotension. Pericardial tamponade that restricts filling <strong>of</strong> the cardiac chambers during diastole<br />
and produces a fixed low cardiac output is also a life-threatening emergency that requires<br />
immediate correction with pericardiocentesis. Patients with cardiac rupture without pericardial<br />
tamponade seldom survive because exsanguination is extremely rapid in this situation.<br />
<strong>Trauma</strong>tic aortic rupture, if complete, is usually fatal, but with an intimal tear with a dissecting<br />
aneurysm, the patient can be saved if the diagnosis and repair are performed promptly<br />
during well-managed fluid resuscitation and anesthesia care. Management <strong>of</strong> these cases<br />
requires rapid and accurate assessment and appropriate surgical and anesthesia intervention.<br />
Partial disruption <strong>of</strong> the trachea or major bronchi can be handled in many cases through<br />
securing <strong>of</strong> the airway (by intubation or tracheostomy) and surgical correction. Total disruption<br />
<strong>of</strong> the trachea is commonly fatal unless rapid surgical retrieval <strong>of</strong> the distal disrupted airway<br />
segment is accomplished; this measure allows life-saving mechanical ventilation.<br />
Diagnosis <strong>of</strong> stable chest injuries is frequently enhanced by computed tomography<br />
(CT), angiography, and other radiologic studies.<br />
Applying ATLS Guidelines to <strong>Trauma</strong> Care<br />
Wendell Spencer, CRNA, MHS<br />
President <strong>of</strong> North Central Anesthesia Services, LLC<br />
O’Neill, Nebraska, USA<br />
Learning Objective: To apply ATLS guidelines to management <strong>of</strong> the trauma<br />
patient in the critical care setting by CRNAs.<br />
Assessment <strong>of</strong> the patient should begin with the airway. 1 Decisions should be made in<br />
the opening minutes <strong>of</strong> assessment to recognize pitfalls in establishing the airway, recognition<br />
<strong>of</strong> the incorrectly established airway, displacement <strong>of</strong> an ongoing airway, and the possibility<br />
<strong>of</strong> aspiration.<br />
Problems that can occur early in assessment include several types <strong>of</strong> trauma: head<br />
trauma, neck trauma, and maxill<strong>of</strong>acial trauma that may influence the type <strong>of</strong> airway control<br />
used. <strong>The</strong> goal should be to provide airway support and deliver oxygen without causing further<br />
harm to patients (i.e., aspiration, further trauma).<br />
Maxill<strong>of</strong>acial trauma patients should be assessed for their ability to breath in supine<br />
position and for fractures to the trachea or oropharynx. Neck trauma patients may have penetrating<br />
injuries that cause displacement <strong>of</strong> the trachea and require tracheostomies.<br />
Associated laryngeal trauma may include a triad in the fracture <strong>of</strong> the larynx, including hoarseness,<br />
subcutaneous emphysema, and a palpable fracture.<br />
In the initial assessment <strong>of</strong> the airway, look, listen, and feel for any abnormalities.<br />
Looking at the airway should include observation <strong>of</strong> obstruction, decreased air movement,<br />
retraction, deformity, and debris. Listening to the airway may reveal noisy speech, gurgle or<br />
stridor, or hoarseness requiring further intervention. Feeling the airway may reveal the location<br />
<strong>of</strong> the trachea, hematoma formation, or fracture locations.<br />
Ventilation capabilities must be assessed for factors <strong>of</strong> the central nervous system that<br />
may impede the airway. <strong>The</strong>se factors may include CNS depression, blunt chest trauma, spinal<br />
cord injury, and other problems.<br />
Management <strong>of</strong> patients must always include immobilization <strong>of</strong> the neck at all times<br />
with traction on the head in a neutral position and care to avoid complicated fractures <strong>of</strong> the<br />
face and nasal area. Needs for definitive airways include the following types <strong>of</strong> patients:<br />
unconscious, severe maxill<strong>of</strong>acial trauma, and those at risk for obstruction or aspiration.<br />
Nasal tracheal intubation should be used only when clearly indicated. Airway algorithms<br />
should be followed to minimize poor decision making in choosing the next step in assisting<br />
the patient to ventilate. Jet ventilators or surgical cricothyrotomies may be used as a last<br />
resort in rescuing the airway. 2,3<br />
References<br />
1. Wheeler M, Ovassapian A. Prediction and evaluation <strong>of</strong> the difficult airway. In<br />
Hagberg CA, ed. Handbook <strong>of</strong> Difficult Airway Management. Philadelphia:<br />
Churchill Livingstone, 2000, pp 15–30.<br />
2. Bowman-Howard M. Management <strong>of</strong> the traumatized airway. In Hagberg CA, ed.<br />
Handbook <strong>of</strong> Difficult Airway Management. Philadelphia: Churchill Livingstone,<br />
2000, pp 319–45.<br />
3. Melker RJ, Florete OG. Cricothyrotomy: review and debate. In Doyle DJ, Sandler<br />
AN, eds. <strong>The</strong> Difficult Airway II. Anesthesiol Clin North Am 1995; 13: 565–83.<br />
Anesthetic Management <strong>of</strong> the Patient Sustaining Thoracic <strong>Trauma</strong><br />
Charles R. Barton, CRNA, MSN, M.Ed.<br />
Director, Graduate Anesthesia Program, <strong>The</strong> University <strong>of</strong> Akron<br />
College <strong>of</strong> Nursing, Akron, Ohio, USA<br />
Learning Objectives: To understand manifestations and management <strong>of</strong> the lifethreatening<br />
conditions that can result from blunt thoracic trauma.<br />
Blunt thoracic trauma <strong>of</strong>ten results from the impact <strong>of</strong> drivers who are not wearing<br />
safety belts into the steering wheel during a motor vehicle crash. Penetrating and blunt trauma<br />
to the chest may injure several structures and thus compromise optimal resuscitation.<br />
<strong>The</strong>se structures include the chest wall, the lungs and airways, the heart and pericardium,<br />
and the great vessels <strong>of</strong> the thorax. Injuries to these structures also compromise anesthesia<br />
care by affecting gas exchange and cardiac output.<br />
Several life-threatening conditions require immediate interventions in patients with<br />
chest injuries. A tension pneumothorax develops when the pleural cavity is punctured, creating<br />
a one-way valve that controls the flow <strong>of</strong> air into this cavity. With each breath, more air<br />
becomes trapped in this space, increasing intrapleural pressure to the point that it eventually<br />
exceeds all other intrathoracic pressures. <strong>The</strong> enlarging pleural cavity then collapses the<br />
ipsilateral lung and shifts structures <strong>of</strong> the mediastinum (e.g., trachea, great vessels, heart)<br />
into the opposite hemithorax, thereby compressing the contralateral lung. <strong>The</strong> size <strong>of</strong> a<br />
pneumothorax rapidly increases during positive-pressure ventilation, especially if nitrous<br />
oxide is used in the field for analgesia or during anesthesia in the trauma facility. Patients with<br />
a pneumothorax <strong>of</strong>ten present with hypotension, subcutaneous emphysema <strong>of</strong> the neck or<br />
chest, unilateral decrease in breath sounds, diminished chest wall motion, hyper-resonance<br />
Anesthetic Management <strong>of</strong> the <strong>Trauma</strong> Patient in the Rural Health Care Setting<br />
Wendell Spencer, CRNA, MHS<br />
President <strong>of</strong> North Central Anesthesia Services, LLC<br />
O’Neill, Nebraska, USA<br />
Learning Objective: To discuss the anesthetic considerations unique to the rural<br />
health care trauma patient as they relate to the area <strong>of</strong> shock.<br />
<strong>The</strong> rural health patient presents many challenges to the anesthetic care provider in<br />
resources and in the management and treatment <strong>of</strong> shock. Recognition <strong>of</strong> the signs and<br />
symptoms <strong>of</strong> shock is the key to successful intervention and treatment <strong>of</strong> trauma patients.<br />
Shock is defined as both inadequate tissue/organ perfusion and a lack <strong>of</strong> tissue oxygenation.<br />
Knowledge <strong>of</strong> cardiac output and stroke volume is necessary to evaluate the patient<br />
who presents in shock. Cardiac output is the volume <strong>of</strong> blood pumped per minute as a result<br />
<strong>of</strong> heart rate and stroke volume. Stroke volume is the amount <strong>of</strong> blood pumped by the heart<br />
as determined by preload, myocardial contractility, and afterload. 1<br />
Early changes <strong>of</strong> blood loss include tachycardia, progressive vasoconstriction, release<br />
<strong>of</strong> histamine, and bradykinin. Initial goals include restoring cardiac output via volume repletion<br />
with isotonic solutions. 1 Vasopressors may be contraindicated at this time due to the<br />
need for volume replacement and the additional stress placed on the heart muscle.<br />
Recognition <strong>of</strong> shock includes tachycardia, vasoconstriction, decreased cardiac output,<br />
a narrowing pulse pressure, decreasing mean arterial pressures, and decreased blood flow.<br />
Tachycardia varies by patient age group, and normal values should be taken into consideration<br />
while assessing the patient. 1<br />
Pitfalls in assessment <strong>of</strong> the shock patient include extremes <strong>of</strong> age, athletes, pregnant<br />
patients, medications ingested by the patient prior to arrival, and misleading hemoglobin and<br />
hematocrit values resulting from fluid resuscitation.<br />
Types <strong>of</strong> shock include hemorrhagic, cardiogenic, neurogenic, and some types <strong>of</strong> septic<br />
shock. Class I, II, III, and IV types <strong>of</strong> hemorrhagic shock can start as “minor” emergencies<br />
and quickly turn into the loss <strong>of</strong> patient life. Initial assessment <strong>of</strong> the patient and rapid allocation<br />
<strong>of</strong> equipment and personnel may yield the difference in outcome to the patient in the<br />
rural health setting. 1<br />
Equipment such as a large-volume rapid infusion system, forced-air warmer, intravenous<br />
fluid warmer may be utilized to reverse hypothermia and <strong>of</strong>fset blood loss quickly. 2<br />
Lab personnel and nursing staff are essential to respond rapidly to the patient’s changing condition.<br />
ATLS( guidelines and practice trauma drills are helpful in training the trauma team to<br />
respond successfully to trauma patients and assist practitioners in the “rules <strong>of</strong> engagement”<br />
for highly successful outcomes.<br />
References<br />
1. Dutton RP. Shock and trauma anesthesia. In Grande CM, Smith CE, eds. <strong>Trauma</strong>.<br />
Anesthesiol Clin North Am 1999; 17:83–96.<br />
2. McCunn M, Karlin A. Nonblood fluid resuscitation. In Grande CM, Smith, eds.<br />
<strong>Trauma</strong>. Anesthesiol Clin North Am 1999; 17:107–24.<br />
Airway Management in <strong>Trauma</strong> Patients<br />
James M. Rich, MA, CRNA<br />
Baylor University Medical Center, Dallas, Texas, USA<br />
Learning Objective: Upon completion <strong>of</strong> this lecture, the participant will be able to<br />
list the four anatomic variants associated with a potential difficult airway.<br />
Airway management and fluid resuscitation are the two most important priorities <strong>of</strong><br />
the trauma patient, if there is to be any chance <strong>of</strong> viable survival without significant disability.<br />
This lecture will cover important aspects <strong>of</strong> airway management for the trauma patient.<br />
Airway anatomy, evaluation, and assessment <strong>of</strong> the airway with recognition <strong>of</strong> airway<br />
distortion caused by either blunt or penetrating trauma are crucial to develop an appropriate<br />
plan <strong>of</strong> care. Remembering the “four Ds” will aid in airway assessment, i.e., disproportion, distortion,<br />
decreased range <strong>of</strong> motion, and dental overbite. 1<br />
In order to provide rapid correction <strong>of</strong> the “Crash Airway” patient, a quick method for<br />
recognizing this situation is crucial. Application <strong>of</strong> Mason’s PU-92 concept accomplishes<br />
this. 2,3 Rational selection <strong>of</strong> an appropriate airway technique to include aspiration prophylaxis<br />
and protection <strong>of</strong> suspected or evident cervical spine injuries is paramount. Populations<br />
that require special consideration in trauma include obstetrical patients, pediatric patients,<br />
patients with a traumatized airway, and patients with suspected or evident cervical spine<br />
injuries. Methods to secure the airway in these populations will be discussed. 4<br />
When airway difficulty is suspected, the practitioner must decide to either to temporarily<br />
avoid tracheal intubation through use <strong>of</strong> a non-intubation airway technique with or<br />
without application <strong>of</strong> a minimally invasive airway option. It is also crucial in the face <strong>of</strong><br />
potential intubation difficulty that consideration be given to a technique that allows spontaneous<br />
ventilation versus apnea secondary to use <strong>of</strong> neuromuscular blocks.<br />
<strong>The</strong> choice <strong>of</strong> rapid-sequence intubation (RSI) should be reserved for patients with no<br />
61
<strong>ITACCS</strong> Spring 2003<br />
signs <strong>of</strong> predicted difficulty. RSI should be avoided if rescue ventilation options are not available<br />
to treat a failed airway. 5<br />
A failed intubation strategy should include use <strong>of</strong> bag-valve-mask ventilation (BVMV)<br />
with cricoid pressure as well as the use <strong>of</strong> a Combitube, LMA, or LMA-Fastrach (ILMA) to provide<br />
life-saving ventilation and oxygenation as well as the potential for tracheal intubation<br />
(i.e., LMA-Fastrach [ILMA]). <strong>The</strong> Combitube <strong>of</strong>fers aspiration prophylaxis similar to that <strong>of</strong> an<br />
endotracheal tube. <strong>The</strong> LMA protects from aspiration much better than BVMV. 2 , 6–8<br />
If rescue ventilation does not attain or maintain an acceptable SpO 2 (≥ 92%), then a<br />
cricothyrotomy option should be immediately applied; however, the use <strong>of</strong> rescue ventilation<br />
will greatly decrease the need for transtracheal jet ventilation, percutaneous dilational<br />
cricothyrtomy, or surgical cricothyrotomy. 9<br />
Confirmation <strong>of</strong> tracheal intubation is a central aspect <strong>of</strong> airway management. <strong>The</strong> best<br />
method to confirm endotracheal intubation is to use capnography in a patient with a beating<br />
heart and good pulmonary vascular blood flow and to use an esophageal detector device in<br />
patients with cardiac arrest or severe low flow states. 10 In addition to the use <strong>of</strong> a near-fail-safe<br />
device, the patient’s chest should also be auscultated along the mid-axillary lines and over the<br />
abdomen.<br />
References<br />
1. Wheeler M, Ovassapian A. Prediction and evaluation <strong>of</strong> the difficult airway. In<br />
Hagberg CA, ed. Handbook <strong>of</strong> Difficult Airway Management. Philadelphia:<br />
Churchill Livingstone, 2000, pp 15–30.<br />
2. Mason AM. <strong>The</strong> Laryngeal Mask Airway (LMA) & Intubating Laryngeal Mask Airway<br />
(ILMA) in Prehospital <strong>Trauma</strong> Care. Presentation at the Royal College <strong>of</strong><br />
Anaesthetists, London, May 13, 2002.<br />
3. Mackay CA et al. Association between the assessment <strong>of</strong> conscious level using the<br />
AVPU system and the Glasgow coma scale. Pre-hospital Immediate Care 2000;<br />
4:17–9.<br />
4. Smith C, DeJoy S. New equipment and techniques for airway management in trauma.<br />
Current Opinion in Anaesthesiology 2001; 14:197–209.<br />
5. Smith C. Rapid-sequence intubation in adults: indications and concerns. Clinical<br />
Pulmonary Medicine 2001; 8; 47–65.<br />
6. Agro F, Frass M, Benum<strong>of</strong> JL, Krafft P. Current status <strong>of</strong> the CombitubeTM: a review<br />
<strong>of</strong> the literature. J Clin Anesth 2002; 14:307–17.<br />
7. Benum<strong>of</strong> JL. <strong>The</strong> ASA Difficult Airway Algorithm: new thoughts and considerations.<br />
In Hagberg CA, ed. Handbook <strong>of</strong> Difficult Airway Management. Philadelphia:<br />
Churchill Livingstone, 2000, pp 31–48.<br />
8. Baskett PJF (coordinator). <strong>The</strong> use <strong>of</strong> the laryngeal mask airway by nurses during<br />
cardiopulmonary resuscitation: multicentre trial. Anaesthesia 1994; 49:3–7.<br />
9. Melker RJ, Florete OG. Cricothyrotomy: review and debate. In Doyle DJ, Sandler<br />
AN, eds. <strong>The</strong> Difficult Airway II. Anesthesiol Clin North Am 1995; 13:565–83.<br />
10. Salem MR, Baraka A. Confirmation <strong>of</strong> tracheal intubation. In Benum<strong>of</strong> JL, ed. Airway<br />
Management: Principles and Practice. St. Louis: Mosby, 1996, pp 531–60.<br />
Anesthetic Management <strong>of</strong> Patients with Abdominal <strong>Trauma</strong><br />
Deborah B. Latham, MHS, CRNA-P<br />
Department <strong>of</strong> Nurse Anesthesia, Baylor University Medical Center, Dallas, Texas<br />
Learning Objectives: 1) To state the indications for emergency exploratory laparotomy,<br />
2) to determine appropriate intraoperative monitoring, 3) to determine “safe” drugs,<br />
4) to recognize transfusion complications, and 5) to determine when abbreviated damage<br />
control surgery is appropriate.<br />
Exsanguinating hemorrhage is the major acute cause <strong>of</strong> death following abdominal<br />
trauma. 1–3 Initial focus is on controlling hemorrhage, limiting contamination, rapid assessment,<br />
and treatment <strong>of</strong> blunt and penetrating abdominal trauma.<br />
First priority is securing the airway, then IV access, resuscitation, and identification and<br />
stabilization <strong>of</strong> life-threatening injuries. A decision is then made to proceed with surgical<br />
intervention or perform more diagnostic evaluation.<br />
Initial laboratory and diagnostic studies are based on the patient’s stability. Indications<br />
for emergency exploratory laparotomy 4 are listed below:<br />
1. Penetrating or blunt trauma with hypotension<br />
2. Uncontrolled hemorrhage<br />
3. Signs <strong>of</strong> peritonitis<br />
4. GSW to abdomen<br />
5. Positive objective study (CT, Sonogram, DPL)<br />
6. Ruptured diaphragm<br />
7. Pneumoperitoneum on admission chest film<br />
8. Evisceration <strong>of</strong> bowel or omentum<br />
9. Herniation <strong>of</strong> abdominal contents<br />
10. Significant bleeding from NG tube, rectum<br />
11. Ongoing bleeding from unknown source<br />
12. Stab wounds with known vascular, biliary, or colonic injury<br />
Minimum noninvasive monitors include EKG, automated B/P, pulse oximetry, core<br />
temperature probe with stethoscope, and capnography. A Foley catheter with urometer, radial<br />
or brachial arterial catheter for monitoring and frequent lab analysis during trauma laparotomy.<br />
Two large-bore peripheral catheters must be established with central venous access in<br />
cases involving large blood loss or transfusion. Blood must be available, <strong>of</strong>ten infusing prior<br />
to opening the abdomen in severely hypotensive patients.<br />
Early goals include re-establishment and maintenance <strong>of</strong> normal hemodynamics.<br />
Correct size and number <strong>of</strong> IV lines is accomplished before incision. Hypotension from drug<br />
effect, suppression <strong>of</strong> endogenous catecholamines, and initiation <strong>of</strong> positive-pressure ventilation<br />
will dictate the need for immediate surgical incision upon induction. Following incision,<br />
tamponade <strong>of</strong> abdominal bleeding is lost, and copious blood loss may precipitate.<br />
Etomidate (0.2 mg/kg), normally cardiac neutral, is well tolerated in awake traumatized<br />
patients. Ketamine can promote greater hypotension in a patient with poor sympathetic<br />
tone. In unstable hypotension, oxygen with a muscle relaxant is required until return <strong>of</strong><br />
hemodynamics allow additional anesthetic drugs. When anesthesia needs to be withheld,<br />
scopolamine may be given for amnesia.<br />
Periodic measurement <strong>of</strong> laboratory values is essential. Central venous pressure, urine<br />
output and hemodynamics aid in calculation <strong>of</strong> fluid volumes. Cell saver blood should be<br />
given for noncontaminated intra-abdominal blood loss.<br />
<strong>The</strong> following complications can arise from massive transfusions 5,6 : coagulopathy,<br />
hypothermia, hypocalcemia, hyperkalemia, and hemolysis.<br />
With a pH
*<br />
*For infections due to susceptible strains<br />
<strong>of</strong> indicated organisms.<br />
Careful inquiry should be made<br />
concerning previous hypersensitivity<br />
reaction, as serious and occasionally<br />
fatal anaphylactic reactions have been<br />
reported in patients receiving therapy<br />
with penicillins. ZOSYN is contraindicated<br />
in patients with a history <strong>of</strong> these<br />
reactions to any <strong>of</strong> the penicillins,<br />
cephalosporins, or ß-lactamase inhibitors.<br />
While ZOSYN possesses the characteristic<br />
low toxicity <strong>of</strong> the penicillin group <strong>of</strong><br />
antibiotics, periodic assessment <strong>of</strong> organ<br />
system functions, including renal, hepatic,<br />
and hematopoietic, during prolonged<br />
therapy is advisable.<br />
During clinical trials, pseudomembranous<br />
colitis has been rarely reported (
ZOSYN ® (Piperacillin and Tazobactam for Injection) Brief Summary<br />
See package insert for full prescribing information.<br />
INDICATIONS AND USAGE For the treatment <strong>of</strong> patients with moderate to severe infections caused by<br />
piperacillin-resistant, piperacillin/tazobactam-susceptible, β-lactamase producing strains <strong>of</strong> the designated<br />
microorganisms in the specified conditions listed below:<br />
Appendicitis (complicated by rupture or abscess) and peritonitis caused by Escherichia coli or the following<br />
members <strong>of</strong> the Bacteroides fragilis group: B. fragilis, B. ovatus, B. thetaiotaomicron, or B. vulgatus.<br />
<strong>The</strong> individual members <strong>of</strong> this group were studied in less than 10 cases.<br />
Uncomplicated and complicated skin and skin structure infections, including cellulitis, cutaneous<br />
abscesses, and ischemic/diabetic foot infections caused by Staphylococcus aureus.<br />
Postpartum endometritis or pelvic inflammatory disease caused by Escherichia coli.<br />
Community-acquired pneumonia (moderate severity only) caused by Haemophilus influenzae.<br />
Nosocomial pneumonia (moderate to severe) caused by Staphylococcus aureus. (See Full Prescribing<br />
Information—DOSAGE AND ADMINISTRATION.)<br />
Infections caused by piperacillin-susceptible organisms, for which piperacillin has been shown to be<br />
effective, are also amenable to ZOSYN treatment due to its piperacillin content. Treatment <strong>of</strong> mixed<br />
infections caused by piperacillin-susceptible organisms and piperacillin-resistant, β-lactamase producing<br />
organisms susceptible to ZOSYN should not require the addition <strong>of</strong> another antibiotic.<br />
ZOSYN is useful as presumptive therapy in the indicated conditions prior to the identification <strong>of</strong> causative<br />
organisms because <strong>of</strong> its broad spectrum <strong>of</strong> bactericidal activity against gram-positive and gram-negative<br />
aerobic and anaerobic organisms. Appropriate cultures should usually be performed before initiating<br />
antimicrobial treatment in order to isolate and identify the organisms causing infection and to determine<br />
their susceptibility to ZOSYN.<br />
CONTRAINDICATIONS ZOSYN is contraindicated in patients with a history <strong>of</strong> allergic reactions to any <strong>of</strong> the<br />
penicillins, cephalosporins, or β-lactamase inhibitors.<br />
WARNINGS SERIOUS AND OCCASIONALLY FATAL HYPERSENSITIVITY (ANAPHYLACTIC/ANAPHYLACTOID)<br />
REACTIONS (INCLUDING SHOCK) HAVE BEEN REPORTED IN PATIENTS RECEIVING THERAPY WITH<br />
PENICILLINS INCLUDING ZOSYN. THESE REACTIONS ARE MORE LIKELY TO OCCUR IN INDIVIDUALS<br />
WITH A HISTORY OF PENICILLIN HYPERSENSITIVITY OR A HISTORY OF SENSITIVITY TO MULTIPLE<br />
ALLERGENS. THERE HAVE BEEN REPORTS OF INDIVIDUALS WITH A HISTORY OF PENICILLIN<br />
HYPERSENSITIVITY WHO HAVE EXPERIENCED SEVERE REACTIONS WHEN TREATED WITH<br />
CEPHALOSPORINS. BEFORE INITIATING THERAPY WITH ZOSYN, CAREFUL INQUIRY SHOULD BE MADE<br />
CONCERNING PREVIOUS HYPERSENSITIVITY REACTIONS TO PENICILLINS, CEPHALOSPORINS, OR<br />
OTHER ALLERGENS. IF AN ALLERGIC REACTION OCCURS, ZOSYN SHOULD BE DISCONTINUED AND<br />
APPROPRIATE THERAPY INSTITUTED. SERIOUS ANAPHYLACTIC/ANAPHYLACTOID REACTIONS<br />
(INCLUDING SHOCK) REQUIRE IMMEDIATE EMERGENCY TREATMENT WITH EPINEPHRINE. OXYGEN,<br />
INTRAVENOUS STEROIDS, AND AIRWAY MANAGEMENT, INCLUDING INTUBATION, SHOULD ALSO BE<br />
ADMINISTERED AS INDICATED.<br />
Pseudomembranous colitis has been reported with nearly all antibacterial agents, including ZOSYN,<br />
and may range in severity from mild to life-threatening. Consider this diagnosis in patients who<br />
present with diarrhea after antibacterial agent administration. Treatment with antibacterial agents alters<br />
the normal flora <strong>of</strong> the colon and may permit overgrowth <strong>of</strong> clostridia. Studies indicate that a toxin<br />
produced by Clostridium difficile is one primary cause <strong>of</strong> “antibiotic-associated colitis.”<br />
After the diagnosis <strong>of</strong> pseudomembranous colitis has been established, initiate therapeutic measures. Mild<br />
cases usually respond to drug discontinuation alone. In moderate to severe cases, fluids and electrolytes,<br />
protein supplementation, and treatment with an antibacterial drug clinically effective against Clostridium<br />
difficile colitis may be necessary.<br />
PRECAUTIONS General: Bleeding manifestations have occurred in some patients receiving β-lactam<br />
antibiotics, including piperacillin. <strong>The</strong>se reactions have sometimes been associated with coagulation test<br />
abnormalities such as clotting time, platelet aggregation, and prothrombin time and are more likely to<br />
occur in renal failure patients. If bleeding manifestations occur, discontinue ZOSYN and institute<br />
appropriate therapy.<br />
<strong>The</strong> possibility <strong>of</strong> the emergence <strong>of</strong> resistant organisms that might cause superinfections should be kept in<br />
mind. If this occurs, appropriate measures should be taken.<br />
As with other penicillins, patients may experience neuromuscular excitability or convulsions if higher than<br />
recommended doses are given intravenously (particularly in the presence <strong>of</strong> renal failure).<br />
ZOSYN is a monosodium salt <strong>of</strong> piperacillin and a monosodium salt <strong>of</strong> tazobactam, containing 2.35 mEq<br />
(54 mg) <strong>of</strong> Na+ per gram <strong>of</strong> piperacillin; consider this when treating patients requiring restricted salt intake.<br />
Perform periodic electrolyte determinations in patients with low potassium reserves; the possibility <strong>of</strong><br />
hypokalemia should be kept in mind with patients who have potentially low potassium reserves and who<br />
are receiving cytotoxic therapy or diuretics.<br />
As with other semisynthetic penicillins, piperacillin has been associated with an increased incidence <strong>of</strong><br />
fever and rash in cystic fibrosis patients.<br />
In patients with renal insufficiency or in hemodialysis patients, the intravenous dose should be adjusted to<br />
the degree <strong>of</strong> renal function impairment.<br />
Laboratory Tests: Perform periodic assessment <strong>of</strong> hematopoietic function, especially with prolonged<br />
therapy, ie, ≥21 days. (See ADVERSE REACTIONS—Adverse Laboratory Events.)<br />
Drug Interactions: Aminoglycosides —<strong>The</strong> mixing <strong>of</strong> ZOSYN with an aminoglycoside in vitro can result in<br />
substantial inactivation <strong>of</strong> the aminoglycoside. (See Full Prescribing Information—DOSAGE AND<br />
ADMINISTRATION—Compatible Intravenous Diluent Solutions.)<br />
When ZOSYN was co-administered with tobramycin, the area under the curve, renal clearance, and urinary<br />
recovery <strong>of</strong> tobramycin were decreased by 11%, 32%, and 38%, respectively. Pharmacokinetic alterations<br />
<strong>of</strong> tobramycin when administered with ZOSYN may be due to in vivo and in vitro inactivation <strong>of</strong> tobramycin<br />
in the presence <strong>of</strong> piperacillin/tazobactam. <strong>The</strong> inactivation <strong>of</strong> aminoglycosides in the presence <strong>of</strong> penicillinclass<br />
drugs has been recognized. It has been postulated that microbiologically inactive penicillinaminoglycoside<br />
complexes <strong>of</strong> unknown toxicity form. In patients with severe renal dysfunction (ie, chronic<br />
hemodialysis patients), tobramycin pharmacokinetics are significantly altered when administered with<br />
piperacillin. <strong>The</strong> alteration <strong>of</strong> tobramycin pharmacokinetics and the potential toxicity <strong>of</strong> the penicillinaminoglycoside<br />
complexes in patients with mild to moderate renal dysfunction who are administered an<br />
aminoglycoside with ZOSYN are unknown.<br />
Probenecid—Probenecid administered with ZOSYN prolongs the half-life <strong>of</strong> piperacillin by 21% and <strong>of</strong><br />
tazobactam by 71%.<br />
Vancomycin—No pharmacokinetic interactions with ZOSYN have been noted.<br />
Heparin—Coagulation parameters should be tested more frequently and monitored regularly during<br />
simultaneous administration <strong>of</strong> high doses <strong>of</strong> heparin, oral anticoagulants, or other drugs that may affect<br />
the blood coagulation system or the thrombocyte function.<br />
Vecuronium—Piperacillin used with vecuronium has been implicated in the prolongation <strong>of</strong> the neuromuscular<br />
blockade <strong>of</strong> vecuronium. ZOSYN could produce the same phenomenon if given with vecuronium. Due to their<br />
similar mechanism <strong>of</strong> action, the neuromuscular blockade produced by any <strong>of</strong> the non-depolarizing muscle<br />
relaxants could be prolonged in the presence <strong>of</strong> piperacillin. (See package insert for vecuronium bromide.)<br />
Methotrexate—Piperacillin may reduce the excretion <strong>of</strong> methotrexate; therefore, serum levels <strong>of</strong> methotrexate<br />
should be monitored in patients to avoid drug toxicity.<br />
Drug/Laboratory Test Interactions: As with other penicillins, ZOSYN may result in a false-positive reaction<br />
for glucose in the urine using a copper-reduction method (CLINITEST ®§ ). Glucose tests based on enzymatic<br />
glucose oxidase reactions (such as DIASTIX ®§ or TES-TAPE ®§ ) are recommended.<br />
Carcinogenesis, Mutagenesis, Impairment <strong>of</strong> Fertility: Long term carcinogenicity studies in animals have<br />
not been conducted with piperacillin/tazobactam, piperacillin, or tazobactam. Piperacillin/tazobactam was<br />
negative in the following mutagenicity tests/assays up to the concentrations noted: microbial mutagenicity<br />
assay (14.84/1.86 µg/plate), unscheduled DNA synthesis (UDS) test (5689/711 µg/mL), mammalian point<br />
mutation (Chinese hamster ovary cell HPRT) assay (8000/1000 µg/mL), and a mammalian cell<br />
(BALB/c-3T3) transformation assay (8/1 µg/mL). In vivo, piperacillin/tazobactam did not induce<br />
chromosomal aberrations in rats dosed I.V. with 1500/187.5 mg/kg; this dose is similar to the maximum<br />
recommended human daily (MRHD) dose on a body-surface-area basis (BSA) (mg/m 2 ).<br />
Piperacillin was negative in the following mutagenicity tests/assays up to the concentrations noted:<br />
microbial mutagenicity assays (50 µg/plate), UDS test (10,000 µg/mL), and a cell (BALB/c-3T3)<br />
transformation assay (3000 µg/mL). <strong>The</strong>re was no DNA damage in bacteria (Rec assay) exposed to<br />
piperacillin at concentrations up to 200 µg/disk. In a mammalian point mutation (mouse lymphoma cells)<br />
assay, piperacillin was positive at concentrations ≥2500 µg/mL. In vivo, piperacillin did not induce<br />
chromosomal aberrations in mice at I.V. doses up to 2000 mg/kg/day or rats at I.V. doses up to<br />
1500 mg/kg/day. <strong>The</strong>se doses are half (mice) or similar to (rats) the MRHD dose based on BSA (mg/m 2 ).<br />
In another in vivo test, there was no dominant lethal effect when piperacillin was administered to rats at I.V.<br />
doses up to 2000 mg/kg/day, which is similar to the MRHD dose based on BSA (mg/m 2 ). When mice were<br />
administered piperacillin at I.V. doses up to 2000 mg/kg/day, which is half the MRHD dose based on BSA<br />
(mg/m 2 ), urine from these animals was not mutagenic when tested in a microbial mutagenicity assay.<br />
Bacteria injected into the peritoneal cavity <strong>of</strong> mice administered piperacillin at I.V. doses up to<br />
2000 mg/kg/day did not show increased mutation frequencies.<br />
Tazobactam was negative in the following mutagenicity assays up to the concentrations noted: microbial<br />
mutagenicity assays (333 µg/plate), UDS test (2000 µg/mL), mammalian point mutation (Chinese hamster<br />
ovary cell HPRT) (5000 µg/mL), a cell (BALB/c-3T3) transformation assay (900 µg/mL). In another<br />
mammalian point mutation (mouse lymphoma cells) assay, tazobactam was positive at concentrations<br />
≥3000 µg/mL. In an in vitro cytogenetics (Chinese hamster lung cells) assay, tazobactam was negative at<br />
concentrations up to 3000 µg/mL. In vivo, tazobactam did not induce chromosomal aberrations in rats at<br />
I.V. doses up to 5000 mg/kg, which is 23 times the MRHD dose based on BSA (mg/m 2 ).<br />
Pregnancy: Teratogenic effects—Pregnancy Category B: Piperacillin/tazobactam: Reproduction studies in<br />
rats have revealed no evidence <strong>of</strong> impaired fertility due to piperacillin/tazobactam administered up to a dose<br />
which is similar to the MRHD dose based on BSA (mg/m 2 ).<br />
Teratology studies in mice and rats have revealed no evidence <strong>of</strong> harm to the fetus due to<br />
piperacillin/tazobactam administered up to a dose which is 1 to 2 times and 2 to 3 times the human dose<br />
<strong>of</strong> piperacillin and tazobactam, respectively, based on BSA (mg/m 2 ). Piperacillin and tazobactam<br />
cross the placenta.<br />
Piperacillin: Reproduction and teratology studies in mice and rats have revealed no evidence <strong>of</strong> impaired<br />
fertility or fetal harm due to piperacillin administered up to a dose which is half (mice) or similar to (rats)<br />
the MRHD dose based on BSA (mg/m 2 ).<br />
Tazobactam: Reproduction studies in rats have revealed no evidence <strong>of</strong> impaired fertility due to tazobactam<br />
administered at doses up to 3 times the MRHD dose based on BSA (mg/m 2 ).<br />
Teratology studies in mice and rats have revealed no evidence <strong>of</strong> fetal harm due to tazobactam administered at<br />
doses up to 6 and 14 times, respectively, the human dose based on BSA (mg/m 2 ). In rats, tazobactam crosses<br />
the placenta. Concentrations in the fetus are less than or equal to 10% <strong>of</strong> those found in maternal plasma.<br />
<strong>The</strong>re are no adequate and well-controlled studies with the piperacillin/tazobactam combination or with<br />
piperacillin or tazobactam alone in pregnant women. Use this drug during pregnancy only if clearly needed.<br />
Nursing Mothers: Piperacillin is excreted in low concentrations in human milk; tazobactam concentrations<br />
in human milk have not been studied. Exercise caution when ZOSYN is administered to a nursing woman.<br />
Pediatric Use: Safety and efficacy in pediatric patients have not been established.<br />
Geriatric Use: Patients over 65 years are not at an increased risk <strong>of</strong> developing adverse effects solely<br />
because <strong>of</strong> age. However, dosage should be adjusted in the presence <strong>of</strong> renal insufficiency.<br />
ADVERSE REACTIONS During the initial clinical investigations, 2621 patients worldwide were treated with<br />
ZOSYN in phase 3 trials. In the key North American clinical trials (n=830 patients), 90% <strong>of</strong> the adverse<br />
events reported were mild to moderate in severity and transient in nature. However, in 3.2% <strong>of</strong> the patients<br />
treated worldwide, ZOSYN was discontinued because <strong>of</strong> adverse events primarily involving the skin (1.3%),<br />
including rash and pruritus; the gastrointestinal system (0.9%), including diarrhea, nausea, and vomiting;<br />
and allergic reactions (0.5%).<br />
Adverse local reactions that were reported, irrespective <strong>of</strong> relationship to ZOSYN therapy, were phlebitis (1.3%),<br />
injection site reaction (0.5%), pain (0.2%), inflammation (0.2%), thrombophlebitis (0.2%), and edema (0.1%).<br />
In the completed study <strong>of</strong> nosocomial lower respiratory tract infections, 155 patients received ZOSYN<br />
3.375 g every 4 hours in combination with an aminoglycoside. In this trial, 88.5% <strong>of</strong> the adverse experiences<br />
reported were mild to moderate in severity and transient in nature. In this trial, ZOSYN was discontinued in<br />
four patients (2.6%) due to adverse experiences: thrombocytopenia and pancreatitis in one patient; fever in one<br />
patient; fever and eosinophilia in another patient; and diarrhea and elevated liver enzymes in the fourth patient.<br />
Adverse Clinical Events: Based on patients from the North American trials (n=1063), the events with the<br />
highest incidence in patients, irrespective <strong>of</strong> relationship to ZOSYN therapy, were diarrhea (11.3%); headache<br />
(7.7%); constipation (7.7%); nausea (6.9%); insomnia (6.6%); rash (4.2%), including maculopapular, bullous,<br />
urticarial, and eczematoid; vomiting (3.3%); dyspepsia (3.3%); pruritus (3.1%); stool changes (2.4%); fever<br />
(2.4%); agitation (2.1%); pain (1.7%); moniliasis (1.6%); hypertension (1.6%); dizziness (1.4%); abdominal<br />
pain (1.3%); chest pain (1.3%); edema (1.2%); anxiety (1.2%); rhinitis (1.2%); and dyspnea (1.1%).<br />
Based on patients in the completed study <strong>of</strong> nosocomial lower respiratory tract infections (n=155), using<br />
every-4-hour dosing and aminoglycoside therapy, the events with the highest incidence in patients,<br />
irrespective <strong>of</strong> relationship to ZOSYN and aminoglycoside therapy, were diarrhea (20%); constipation<br />
(8.4%); agitation (7.1%); nausea (5.8%); headache (4.5%); insomnia (4.5%); oral thrush (3.9%);<br />
erythematous rash (3.9%); anxiety (3.2%); fever (3.2%); pain (3.2%); pruritus (3.2%); hiccough (2.6%);<br />
vomiting (2.6%); dyspepsia (1.9%); edema (1.9%); fluid overload (1.9%); stool changes (1.9%); anorexia<br />
(1.3%); cardiac arrest (1.3%); confusion (1.3%); diaphoresis (1.3%); duodenal ulcer (1.3%); flatulence<br />
(1.3%); hypertension (1.3%); hypotension (1.3%); inflammation at injection site (1.3%); pleural effusion<br />
(1.3%); pneumothorax (1.3%); rash, not otherwise specified (1.3%); supraventricular tachycardia (1.3%);<br />
thrombophlebitis (1.3%); and urinary incontinence (1.3%).<br />
Additional adverse systemic clinical events reported in 1.0% or less <strong>of</strong> the patients in the initial North<br />
American trials and/or in the patients administered ZOSYN 3.375 g every 4 hours plus an aminoglycoside<br />
in the nosocomial lower respiratory tract study are listed below within each body system (bracketed events<br />
occurred only in the nosocomial pneumonia trial): Autonomic nervous system: hypotension, ileus,<br />
syncope. Body as a whole: rigors, back pain, malaise, [asthenia, chest pain]. Cardiovascular: tachycardia,<br />
including supraventricular and ventricular; bradycardia; arrhythmia, including atrial fibrillation, ventricular<br />
fibrillation, cardiac arrest, cardiac failure, circulatory failure, myocardial infarction, [angina]. Central<br />
nervous system: tremor, convulsions, vertigo, [aggressive reaction (combative)]. Gastrointestinal: melena,<br />
flatulence, hemorrhage, gastritis, hiccough, ulcerative stomatitis, [fecal incontinence, gastric ulcer,<br />
pancreatitis]. Pseudomembranous colitis was reported in one patient during the clinical trials. <strong>The</strong> onset <strong>of</strong><br />
pseudomembranous colitis symptoms may occur during or after antibacterial treatment. (See WARNINGS.)<br />
Hearing and vestibular system: tinnitus, [deafness, earache]. Hypersensitivity: anaphylaxis. Metabolic and<br />
Nutritional: symptomatic hypoglycemia, thirst, [gout, vitamin B12 deficiency anemia]. Musculoskeletal:<br />
myalgia, arthralgia. Platelets, Bleeding, Clotting: mesenteric embolism, purpura, epistaxis, pulmonary<br />
embolism, [ecchymosis, hemoptysis]. (See PRECAUTIONS—General.) Psychiatric: confusion,<br />
hallucination, depression. Reproductive, Female: leukorrhea, vaginitis, [perineal irritation/pain].<br />
Reproductive, Male: [balanoposthitis]. Respiratory: pharyngitis, pulmonary edema, bronchospasm,<br />
coughing, [atelectasis, dyspnea, hypoxia]. Skin and Appendages: genital pruritus, diaphoresis,<br />
[conjunctivitis, xerosis]. Special senses: taste perversion. Urinary: retention, dysuria, oliguria, hematuria,<br />
incontinence, [urinary tract infection with trichomonas, yeast in urine]. Vision: photophobia. Vascular<br />
(extracardiac): flushing, [cerebrovascular accident].<br />
Additional adverse events reported from worldwide marketing experience with ZOSYN, where causal<br />
relationship to ZOSYN is uncertain: Gastrointestinal: hepatitis, cholestatic jaundice. Hematologic: hemolytic<br />
anemia, anemia, thrombocytosis, agranulocytosis, pancytopenia. Immune: hypersensitivity reactions,<br />
anaphylactic/anaphylactoid reactions (including shock). Infections and Infestations: candidal superinfections.<br />
Renal: rarely, interstitial nephritis, renal failure. Skin and Appendages: erythema multiforme and Stevens-<br />
Johnson syndrome, rarely reported; toxic epidermal necrolysis.<br />
Adverse Laboratory Events (Seen During Clinical Trials): Of the studies reported, including that <strong>of</strong><br />
nosocomial lower respiratory tract infections in which a higher dose <strong>of</strong> ZOSYN was used in combination<br />
with an aminoglycoside, changes in laboratory parameters, without regard to drug relationship, include:<br />
Hematologic: decreases in hemoglobin and hematocrit, thrombocytopenia, increases in platelet count,<br />
eosinophilia, leukopenia, neutropenia. <strong>The</strong> leukopenia/neutropenia appears to be reversible and most<br />
frequently associated with prolonged administration, ie, ≥21 days <strong>of</strong> therapy. <strong>The</strong>se patients were<br />
withdrawn from therapy; some had accompanying systemic symptoms (eg, fever, rigors, chills).<br />
Coagulation: positive direct Coombs’ test, prolonged prothrombin time, prolonged partial thromboplastin<br />
time. Hepatic: transient elevations <strong>of</strong> AST (SGOT), ALT (SGPT), alkaline phosphatase, bilirubin. Renal:<br />
increases in serum creatinine, blood urea nitrogen. Urinalysis: proteinuria, hematuria, pyuria.<br />
Additional laboratory events include abnormalities in electrolytes (ie, increases and decreases in sodium,<br />
potassium, and calcium), hyperglycemia, decreases in total protein or albumin, blood glucose decreased,<br />
gamma-glutamyltransferase increased, hypokalemia, and bleeding time prolonged.<br />
<strong>The</strong> following adverse reaction has also been reported for PIPRACIL ® (sterile piperacillin sodium): Skeletal:<br />
prolonged muscle relaxation. (See PRECAUTIONS—Drug Interactions.)<br />
Piperacillin therapy has been associated with an increased incidence <strong>of</strong> fever and rash in cystic fibrosis patients.<br />
OVERDOSAGE <strong>The</strong>re have been post-marketing reports <strong>of</strong> overdose with piperacillin/tazobactam. <strong>The</strong><br />
majority <strong>of</strong> those events experienced including nausea, vomiting, and diarrhea have also been reported with<br />
the usual recommended dosages. Patients may experience neuromuscular excitability or convulsions if<br />
higher than recommended doses are given intravenously (particularly in the presence <strong>of</strong> renal failure).<br />
Treatment should be supportive and symptomatic according to the patient's clinical presentation. Excessive<br />
serum concentrations <strong>of</strong> either piperacillin or tazobactam may be reduced by hemodialysis. (See Full<br />
Prescribing Information—CLINICAL PHARMACOLOGY.)<br />
§<br />
CLINITEST ® and DIASTIX ® are registered trademarks <strong>of</strong> Ames Division, Miles Laboratories, Inc.<br />
§<br />
TES-TAPE ® is a registered trademark <strong>of</strong> Eli Lilly and Company.<br />
This Brief Summary is based on ZOSYN direction circulars CI 4630-5 and CI 4813-4 (Revised November 2002).<br />
© 2003, Wyeth Pharmaceuticals, Philadelphia, PA 19101 102682-01
<strong>ITACCS</strong> Spring 2003<br />
SPONSORS & EXHIBITORS<br />
We wish to recognize and thank the following sponsors<br />
and exhibitors for their gracious support:<br />
— Platinum Sponsor —<br />
Abbott Pharmaceuticals<br />
— Gold Sponsor —<br />
Novo Nordisk Pharmaceuticals<br />
— Grand Sponsors —<br />
Organon Pharmaceuticals<br />
Smiths/Level 1<br />
Wyeth Pharmaceuticals<br />
— Elite Sponsor —<br />
Laerdal Medical Corporation<br />
— Special Sponsor —<br />
Lodox Systems<br />
— Exhibitors —<br />
Belmont Instrument Corporation<br />
Elsevier: W.B. Saunders/Mosby/Churchill Medical Publishers<br />
Financial Planners <strong>of</strong> the South<br />
First Care Products/Z Medica<br />
Great Plains Ballistics<br />
Pneu-Pac<br />
King Systems Corporation<br />
<strong>The</strong> Exhibit Hall will be open on Friday, May 16, at 0700;<br />
during the morning break at 0915; during lunch (1200–1315);<br />
during the afternoon break at 1445; and during the<br />
evening reception (1715–1830).<br />
•••<br />
Editorial Board for <strong>Trauma</strong>Care<br />
Editors-in-Chief<br />
Adolph H. Giesecke, MD (USA) • John K. Stene, MD, PhD (USA)<br />
Prehospital Care<br />
Dario Gonzalez, MD, FACEP (USA) • Herbert Kuhnigk, MD (Germany)<br />
David Lacombe, NREMT-P (USA) • Hans Morten Lossius, MD (Norway)<br />
Eldar Søreide, MD, PhD (Norway)<br />
Emergency Department Care<br />
Bruce Adams, MD (USA) • Dale M. Carrison, DO, FACEP (USA)<br />
Ludi Jagminas, MD (USA) • Marvin Wayne, MD, FACEP (USA)<br />
OR and Intensive Care<br />
James G. Cain, MD (USA) • Richard P. Dutton, MD (USA)<br />
William F. Fallon, Jr., MD, FACS (USA) • Maureen McCunn, MD (USA)<br />
Pediatric <strong>Trauma</strong><br />
Gail E. Rasmussen, MD (USA) • James E. Fletcher, MD, MBBS (USA)<br />
Calvin Johnson, MD (USA)<br />
Thomas J. Long, MD (USA)<br />
CRNA Section<br />
Charles R. Barton, MEd, CRNA (USA) • James M. Rich, MA, CRNA (USA)<br />
<strong>International</strong> Advisory Board<br />
Wolfgang F. Dick, MD, PhD (Germany) • Christopher M. Grande, MD, MPH (USA)<br />
Louis M. Guzzi, MD (USA) • Yves Lambert, MD (France)<br />
Walter Mauritz, MD, PhD (Austria) • Jerry Nolan, MB, ChB, FFARCS (England)<br />
Michael J.A. Parr, MB, BS, MRCP(UK), FRCA (Australia)<br />
Anne J. Sutcliffe, FRCA (England) • Keiichi Tanaka, MD (Japan)<br />
<strong>ITACCS</strong> thanks the following for their<br />
support <strong>of</strong> and contributions to the <strong>Trauma</strong> Airway<br />
Management workshop:<br />
Airway Education & Research Foundation<br />
AMBU, Inc. - Ambu Intubation Trainers<br />
Clarus Medical - Shikani Optical Stylet<br />
Cook Critical Care - Melker Kits, ENK TTJV Kits, Retrograde<br />
Intubation Kits<br />
Glide Scope - glide scope video scope system<br />
Karl Storz - Bon Fils Scope<br />
King Systems Corporation - <strong>The</strong> KING LT<br />
Laerdal/MPL - 7 AirMan Simulators, 1 SimMan Simulator, 4<br />
Difficult Airway Trainers<br />
LMA North America - LMA Classics and LMA-Fastrachs<br />
Nonin Medical - Electronic Carbon Dioxide Detector<br />
Olympus - Flexible fiberoptic intubation stations with manikins<br />
Sunmed - Laryngoscope sets<br />
Tyco Kendall - Combitubes<br />
Educational Objectives<br />
This publication/activity is designed to provide trauma<br />
care pr<strong>of</strong>essionals interested in the treatment <strong>of</strong> critically ill<br />
trauma patients with a regular overview and critical analysis <strong>of</strong><br />
the most current, clinically useful information available, covering<br />
strategies and advances in the diagnosis <strong>of</strong> traumatic<br />
injuries and the treatment <strong>of</strong> trauma patients. Controversies,<br />
advantages, and disadvantages <strong>of</strong> diagnosis and treatment plans<br />
are emphasized. <strong>The</strong>re are no prerequisites for participation in<br />
this activity.<br />
After reading each issue, participants should have a working<br />
familiarity with the most significant information and perspectives<br />
presented and apply what they have learned promptly<br />
in clinical practice. Specific learning objectives are printed at<br />
the opening <strong>of</strong> each abstract.<br />
65
After high blood loss surgeries,<br />
patient outcomes can hang<br />
in the balance.<br />
<strong>The</strong> carrier in your plasma volume expander can<br />
affect outcomes such as:<br />
• Coagulation difficulties.<br />
• Pain, including chest pain.<br />
• Use <strong>of</strong> anti-emetics.<br />
• Reduced renal output.<br />
Find out more with a call to your Abbott representative<br />
or to 1-866-464-4261, extension HEXTEND (439-8363).<br />
®<br />
6% HETASTARCH IN LACTATED ELECTROLYTE INJECTION<br />
3-013-Mar., 03
• HEXTEND (6% Hetastarch in Lactated Electrolyte injection) is indicated in the treatment <strong>of</strong> hypovolemia<br />
when plasma volume expansion is desired. It is not a substitute for blood or plasma.<br />
• Solutions containing hetastarch are contraindicated in patients with known sensitivity to hydroxyethyl<br />
starch, bleeding disorders or with congestive heart failure where volume overload is a potential problem.<br />
• Solutions containing hetastarch should not be used in renal disease with oliguria or anuria not related<br />
to hypovolemia.<br />
Please see brief summary <strong>of</strong> Prescribing Information on following page.
BRIEF SUMMARY<br />
a HEXTEND ®<br />
6% Hetastarch in Lactated Electrolyte Injection<br />
Flexible Plastic Container<br />
INDICATIONS AND USAGE<br />
HEXTEND (6% Hetastarch in Lactated Electrolyte Injection) is indicated in the treatment <strong>of</strong> hypovolemia<br />
when plasma volume expansion is desired. It is not a substitute for blood or plasma.<br />
CONTRAINDICATIONS<br />
Solutions containing hetastarch are contraindicated in patients with known hypersensitivity to<br />
hydroxyethyl starch or with bleeding disorders or with congestive heart failure where volume overload<br />
is a potential problem. Solutions containing hetastarch should not be used in renal disease with oliguria<br />
or anuria not related to hypovolemia.<br />
Solutions containing lactate are NOT FOR USE IN THE TREATMENT OF LACTIC ACIDOSIS.<br />
WARNINGS<br />
Solutions containing calcium should not be administered simultaneously with blood through the same<br />
administration set because <strong>of</strong> the likelihood <strong>of</strong> coagulation.<br />
Life threatening anaphylactic/anaphylactoid reactions have been rarely reported with solutions<br />
containing hetastarch; death has occurred, but a causal relationship has not been established.<br />
Patients who develop severe anaphylactic/anaphylactoid reactions may need continued supportive<br />
care until symptoms have resolved.<br />
Hypersensitivity reactions can occur even after solutions containing hetastarch have been<br />
discontinued.<br />
Solutions which contain potassium should be used with great care, if at all, in patients with<br />
hyperkalemia and severe renal failure and in situations in which potassium retention is present.<br />
Solutions containing sodium ions should be used with great care, if at all, in patients with congestive<br />
heart failure and severe renal insufficiency and in clinical states in which edema with sodium retention<br />
occurs.<br />
In patients with diminished renal function,<br />
administration <strong>of</strong> solutions containing sodium or<br />
potassium ions may result in sodium or potassium<br />
retention.<br />
Solutions containing lactate ions should be used with<br />
great care in patients with metabolic or respiratory<br />
alkalosis. <strong>The</strong> administration <strong>of</strong> lactate ions should be<br />
performed with great care when dealing with conditions in<br />
which an increased level or an impaired utilization <strong>of</strong><br />
these ions occurs, such as severe hepatic insufficiency.<br />
DO NOT USE IN LEUKAPHERESIS.<br />
Usage in Plasma Volume Expansion<br />
Large volumes <strong>of</strong> isotonic solutions containing 6%<br />
hetastarch (HEXTEND or Hetastarch Injection) may<br />
transiently alter the coagulation mechanism due to<br />
hemodilution and a mild direct inhibitory action on Factor<br />
VIII. Hemodilution by isotonic solutions containing 6%<br />
hetastarch may also result in a 24 hour decline <strong>of</strong> total<br />
protein, albumin, and fibrinogen levels and in transient<br />
prolongation <strong>of</strong> prothrombin, activated partial<br />
thromboplastin, clotting, and bleeding times.<br />
Hematocrit may be decreased and plasma proteins<br />
diluted excessively by administration <strong>of</strong> large volumes <strong>of</strong><br />
isotonic solutions containing 6% hetastarch.<br />
Administration <strong>of</strong> packed red cells, platelets, and fresh<br />
frozen plasma should be considered if excessive dilution<br />
occurs.<br />
In randomized, controlled, comparative studies <strong>of</strong> Hetastarch Injection (n = 92) and Albumin (n = 85)<br />
in surgical patients, no patient in either treatment group had a bleeding complication and no significant<br />
difference was found in the amount <strong>of</strong> blood loss between the treatment groups.<br />
HEXTEND has not been adequately evaluated to establish its safety in situations other than treatment<br />
<strong>of</strong> hypovolemia in elective surgery. In some cases, the use <strong>of</strong> isotonic solutions containing 6%<br />
hetastarch has been associated with coagulation abnormalities in conjunction with an acquired,<br />
reversible von Willebrand’s-like syndrome and/or Factor VIII deficiency when used over a period <strong>of</strong><br />
days. Replacement therapy should be considered if a severe Factor VIII or von Willebrand deficiency is<br />
identified. If a coagulopathy develops, it may take several days to resolve. Certain conditions may affect<br />
the safe use <strong>of</strong> isotonic solutions containing 6% hetastarch on a chronic basis. For example, in patients<br />
with subarachnoid hemorrhage where an isotonic solution containing 6% hetastarch is used repeatedly<br />
over a period <strong>of</strong> days for the prevention <strong>of</strong> cerebral vasospasm, significant clinical bleeding may occur.<br />
Intracranial bleeding resulting in death has been reported with the use <strong>of</strong> Hetastarch Injection.<br />
PRECAUTIONS<br />
General<br />
<strong>The</strong> possibility <strong>of</strong> circulatory overload should be kept in mind. Caution should be used when the risk <strong>of</strong><br />
pulmonary edema and/or congestive heart failure is increased. Special care should be exercised in<br />
patients who have impaired renal clearance since this is the principal way in which hetastarch is<br />
eliminated and in clinical states in which edema with sodium retention occurs.<br />
Indirect bilirubin levels <strong>of</strong> 8.3 mg/L (normal 0.0-7.0 mg/L) have been reported in 2 out <strong>of</strong> 20 normal<br />
subjects who received multiple infusions <strong>of</strong> Hetastarch Injection. Total bilirubin was within normal<br />
limits at all times; indirect bilirubin returned to normal by 96 hours following the final infusion. <strong>The</strong><br />
significance, if any, <strong>of</strong> these elevations is not known; however, caution should be observed before<br />
administering isotonic solutions containing 6% hetastarch to patients with a history <strong>of</strong> liver disease.<br />
If a hypersensitivity effect occurs, administration <strong>of</strong> the drug should be discontinued and appropriate<br />
treatment and supportive measures should be undertaken (see WARNINGS).<br />
Caution should be used when administering solutions containing hetastarch to patients allergic to<br />
corn because such patients can also be allergic to hetastarch.<br />
Clinical evaluation and periodic laboratory determinations are necessary to monitor changes in fluid<br />
balance, electrolyte concentrations, acid-base balance, and coagulation parameters during prolonged<br />
parenteral therapy or whenever the condition <strong>of</strong> the patient warrants such evaluation.<br />
Solutions containing dextrose should be used with caution in patients with known subclinical or<br />
overt diabetes mellitus.<br />
Caution must be exercised in the administration <strong>of</strong> parenteral fluids, especially those containing<br />
6% HETASTARCH IN LACTATED ELECTROLYTE INJECTION<br />
sodium ions, to patients receiving corticosteroids or corticotropin.<br />
Potassium containing solutions should be used with caution in the presence <strong>of</strong> cardiac disease,<br />
particularly in digitalized patients or in the presence <strong>of</strong> renal disease.<br />
Solutions containing lactate ions should be used with caution as excess administration may result in<br />
metabolic alkalosis.<br />
Elevated serum amylase levels may be observed temporarily following administration <strong>of</strong><br />
solutions containing hetastarch although no association with pancreatitis has been<br />
demonstrated. Serum amylase levels cannot be used to assess or to evaluate for pancreatitis<br />
for 3-5 days after administration <strong>of</strong> solutions containing hetastarch. Elevated serum amylase<br />
levels persist for longer periods <strong>of</strong> time in patients with renal impairment. Solutions containing<br />
hetastarch have not been shown to increase serum lipase.<br />
One report suggests that in the presence <strong>of</strong> renal glomerular damage, larger molecules <strong>of</strong> hetastarch<br />
can leak into the urine and elevate the specific gravity. <strong>The</strong> elevation <strong>of</strong> specific gravity can obscure<br />
the diagnosis <strong>of</strong> renal failure.<br />
Hetastarch is not eliminated by hemodialysis. <strong>The</strong> utility <strong>of</strong> other extracorporeal elimination<br />
techniques has not been evaluated.<br />
If administration is by pressure infusion, all air should be withdrawn or expelled from the bag through<br />
the medication port prior to infusion.<br />
Carcinogenesis, Mutagenesis, Impairment <strong>of</strong> Fertility<br />
Long-term studies <strong>of</strong> animals have not been performed to evaluate the carcinogenic potential <strong>of</strong><br />
hetastarch.<br />
Teratogenic Effects: Pregnancy Category C.<br />
Hetastarch Injection has been shown to have an embryocidal effect on New Zealand rabbits when<br />
given intravenously over the entire organogenesis period in a daily dose 1/2 times the maximum<br />
recommended therapeutic human dose (1500 mL) and on BD rats when given intraperitoneally, from the<br />
16th to the 21st day <strong>of</strong> pregnancy, in a daily dose 2.3 times the maximum recommended therapeutic<br />
human dose. When Hetastarch Injection was administered to New Zealand rabbits, BD rats, and Swiss<br />
mice with intravenous daily doses <strong>of</strong> 2 times, 1/3 times, and 1 times the maximum recommended<br />
therapeutic human dose, respectively, over several days during the period <strong>of</strong> gestation, no evidence <strong>of</strong><br />
teratogenicity was evident. <strong>The</strong>re are no adequate and well controlled studies in pregnant women.<br />
HEXTEND should be used during pregnancy only if the potential benefit justifies the potential risk to the<br />
fetus.<br />
Nursing Mothers<br />
It is not known whether hetastarch is excreted in human milk. Because many drugs are excreted in<br />
human milk, caution should be exercised when HEXTEND is administered to a nursing woman.<br />
Pediatric Use<br />
<strong>The</strong> safety and effectiveness <strong>of</strong> HEXTEND in pediatric<br />
patients have not been established. Adequate, wellcontrolled<br />
clinical trials to establish the safety and<br />
effectiveness <strong>of</strong> HEXTEND in pediatric patients have not<br />
been conducted. However, in one small double-blind<br />
study, 47 infants, children, and adolescents (ages 1 year<br />
to 15.5 years) scheduled for repair <strong>of</strong> congenital heart<br />
disease with moderate hypothermia were randomized to<br />
receive either Hetastarch Injection or Albumin as a<br />
postoperative volume expander during the first 24 hours<br />
after surgery. Thirty-eight children required colloid<br />
replacement therapy, <strong>of</strong> which 20 children received<br />
Hetastarch Injection. No differences were found in the<br />
coagulation parameters or in the amount <strong>of</strong> replacement<br />
fluids required in the children receiving 20 mL/kg or less<br />
<strong>of</strong> either colloid replacement therapy. In children who<br />
received greater than 20 mL/kg <strong>of</strong> Hetastarch Injection,<br />
®<br />
an increase in prothrombin time was demonstrated (p =<br />
0.006). <strong>The</strong>re were no neonates included in this study.<br />
Geriatric Use<br />
Of the total number <strong>of</strong> patients in clinical trials <strong>of</strong><br />
HEXTEND (n=119), 30% were 65 or older while 12% were<br />
70 or older. Other reported experience with Hetastarch<br />
Injection has not identified differences in responses<br />
between elderly and younger patients, but greater<br />
sensitivity <strong>of</strong> some older individuals cannot be ruled out.<br />
This drug is known to be substantially excreted by the<br />
kidney, and the risk <strong>of</strong> toxic reactions to this drug may be greater in patients with impaired renal<br />
function. Because elderly patients are more likely to have decreased renal function, care should be<br />
taken in dose selection, and it may be useful to monitor renal function.<br />
ADVERSE REACTIONS<br />
In clinical trials comparing the plasma volume expanding properties <strong>of</strong> HEXTEND (n=60) with those <strong>of</strong><br />
Hetastarch Injection (n=59), there were no significant differences in the number <strong>of</strong> adverse or serious<br />
adverse events between the two groups.<br />
Reported adverse reactions with isotonic solutions containing 6% hetastarch include:<br />
General<br />
Hypersensitivity (see WARNINGS).<br />
Death, life-threatening anaphylactic/anaphylactoid reactions, cardiac arrest, ventricular fibrillation,<br />
severe hypotension, non-cardiac pulmonary edema, laryngeal edema, bronchospasm, angioedema,<br />
wheezing, restlessness, tachypnea, stridor, fever, chest pain, bradycardia, tachycardia, shortness <strong>of</strong><br />
breath, chills, urticaria, pruritus, facial and periorbital edema, coughing, sneezing, flushing, erythema<br />
multiforme, and rash.<br />
Cardiovascular<br />
Circulatory overload, congestive heart failure, and pulmonary edema (see PRECAUTIONS).<br />
Hematologic<br />
Intracranial bleeding, bleeding and/or anemia due to hemodilution (see WARNINGS) and/or Factor VIII<br />
deficiency, acquired von Willebrand’s-like syndrome, and coagulopathy including rare cases <strong>of</strong><br />
disseminated intravascular coagulopathy and hemolysis. With extensive clinical use <strong>of</strong> Hetastarch<br />
Injection, rare cases <strong>of</strong> disseminated intravascular coagulopathy and hemolysis have been observed.<br />
Metabolic<br />
Metabolic acidosis.<br />
Other<br />
Vomiting, peripheral edema <strong>of</strong> the lower extremities, submaxillary and parotid glandular enlargement,<br />
mild influenza-like symptoms, headaches, and muscle pains. Hydroxyethyl starch-associated pruritus<br />
has been reported in some patients with deposits <strong>of</strong> hydroxyethyl starch in peripheral nerves.<br />
Caution: Federal (USA) law prohibits dispensing without prescription.<br />
©Abbott 1999 Reference 58-0851-R2-Rev. September, 1999 Printed in USA<br />
Manufactured and Distributed by: Abbott Laboratories, North Chicago, IL 60064, USA<br />
Under license from BioTime, Inc., Berkeley, CA 94710, USA<br />
68
<strong>ITACCS</strong> Spring 2003<br />
CME QUESTIONS<br />
This issue <strong>of</strong> <strong>Trauma</strong>Care can be used to earn 20 CME credit hours.<br />
Accreditation Statement<br />
This activity has been planned and produced in accordance with the Essential Areas and Policies <strong>of</strong> the Accreditation Council for Continuing Medical Education (ACCME) through the sponsorship<br />
<strong>of</strong> the <strong>International</strong> <strong>Trauma</strong> Anesthesia and Critical Care Society (<strong>ITACCS</strong>). <strong>ITACCS</strong> is accredited by the ACCME to sponsor continuing medical education (CME) for physicians and<br />
takes responsibility for the content, quality, and scientific integrity <strong>of</strong> this CME activity.<br />
Credit Designation Statement: <strong>ITACCS</strong> designates this educational activity for a maximum <strong>of</strong> 20 hours per issue in category 1 credit toward the<br />
AMA Physician’s Recognition Award.<br />
Nurse Anesthetists/CRNAs: Please apply to AANA for post-activity continuing education credits. Certificates <strong>of</strong> completion will be provided.<br />
Faculty Disclosure Statement<br />
It is the policy <strong>of</strong> <strong>ITACCS</strong> that faculty members disclose real or apparent conflict <strong>of</strong> interest relating to the topics <strong>of</strong> this educational activity and also disclose discussions <strong>of</strong> unlabeled/unapproved<br />
uses <strong>of</strong> drugs or devices in their presentations. <strong>The</strong> authors’ completed disclosure forms are on file in the managing editor’s <strong>of</strong>fice.<br />
INSTRUCTIONS<br />
• On the answer form at the bottom <strong>of</strong> page 71, circle only one response next to each number.<br />
• Complete the evaluation form.<br />
• Cut out or copy your completed answer form and evaluation form.<br />
• Write a check for $200 (or $100 accompanied by verification <strong>of</strong> current <strong>ITACCS</strong> membership), payable to the <strong>International</strong> <strong>Trauma</strong> Anesthesia and Critical Care Society.<br />
• Mail the forms and your check (and membership verification, if applicable) to <strong>ITACCS</strong>, Department <strong>of</strong> CME Credit, PO Box 4826, Baltimore, MD 21211.<br />
• <strong>The</strong> completed test will be accepted for grading if received by May 31, 2004.<br />
• Please allow 4 to 6 weeks for processing.<br />
CME QUESTIONS<br />
1. Which <strong>of</strong> the following therapies is appropriate for early resuscitation <strong>of</strong> the patient with active hemorrhagic shock?<br />
a. Pressor therapy with norepinephrine<br />
b. Rapid crystalloid administration to maintain SBP > 120<br />
c. Bicarbonate infusion to maintain pH > 7.30<br />
d. Administration <strong>of</strong> O-positive PRBC<br />
2. Dexmedetomidine is a potent respiratory depressant.<br />
a. True b. False<br />
3. Concerning traumatic thoracic aortic tears, which <strong>of</strong> the following statements is true?<br />
a. Paraplegia and death are less common after surgical repair in the presence <strong>of</strong> preoperative hemodynamic instability.<br />
b. Medical control <strong>of</strong> blood pressure with beta blockers (e.g., esmolol, metoprolol, labetalol) is <strong>of</strong> doubtful clinical importance.<br />
c. One-lung ventilation is contraindicated for descending thoracic aorta surgery because <strong>of</strong> the risk <strong>of</strong> hypoxemia.<br />
d. Delayed repair is <strong>of</strong>ten indicated in the presence <strong>of</strong> major co-morbidity (e.g, head injury, pulmonary contusion, coagulopathy).<br />
e. None <strong>of</strong> the above.<br />
4. <strong>The</strong> main goal <strong>of</strong> triage in a mass casualty setting in which health care resources are exceeded is to rapidly treat the most critically ill patients.<br />
a. True b. False<br />
5. Chemical warfare agents can act upon<br />
a. the central nervous system<br />
b. the alveoli<br />
c. the gastrointestinal system<br />
d. the bone marrow<br />
e. all <strong>of</strong> the above<br />
6. <strong>Trauma</strong> simulation is possible only in major centers with extensive resources.<br />
a. True b. False<br />
7. What is the unique contribution <strong>of</strong> the advanced patient simulators for trauma management training?<br />
a. Team training<br />
b. Acquiring technical skills<br />
c. Learning algorithms and protocols<br />
d. Diagnosis-making capability<br />
8. <strong>The</strong> difference between end-tidal and arterial carbon dioxide tension can be increased by:<br />
a. Pulmonary embolism.<br />
b. Is<strong>of</strong>lurane.<br />
c. Hypovolemia.<br />
d. Atropine.<br />
e. All <strong>of</strong> the above<br />
69
<strong>ITACCS</strong> Spring 2003<br />
9. Most pulse oximeters that are commercially available today will provide erroneous SpO2 values in the presence <strong>of</strong> all the following EXCEPT:<br />
a. Venous blood pulsations. c. Carboxyhemoglobin.<br />
b. Mal-positioned sensor on the finger. d. Anemia.<br />
10. Concerning monitoring <strong>of</strong> neuromuscular block, which <strong>of</strong> the following statements is true?<br />
a. <strong>The</strong>re is a narrow margin <strong>of</strong> safety <strong>of</strong> neuromuscular transmission.<br />
b. Loss <strong>of</strong> all 4 twitches in response to supramaximal train-<strong>of</strong>-four indicates mild block.<br />
c. <strong>The</strong> diaphragm, larynx, and eye muscles are more sensitive to non-depolarizing agents compared with muscles <strong>of</strong> the thumb.<br />
d. Compared with muscles <strong>of</strong> the eye (orbicularis oculi, superciliary), muscles that maintain patency <strong>of</strong> the upper airway are more<br />
sensitive to non-depolarizing agents.<br />
e. None <strong>of</strong> the above.<br />
11. Which <strong>of</strong> the following resuscitation solutions is not associated with the development <strong>of</strong> hyperchloremic metabolic acidosis?<br />
a. 0.9% NSS d. Albumin<br />
b. Lactated Ringers e. Hydroxyethyl starch in balanced salt solution<br />
c. Hypertonic saline<br />
12. Low-pressure, high-volume resuscitation strategies are associated with hypoperfusion and reduced survival.<br />
a. True b. False<br />
13. Mortality and morbidity after head injury are significantly reduced by<br />
a. Maintaining a PaO2 at greater than normal c. Steroids<br />
b. Preventing hypotension (true) d. Hypothermia within 6 hours <strong>of</strong> injury<br />
14. Strict pre-conditions have to be met before the diagnosis <strong>of</strong> brain stem death can be considered.<br />
a. True b. False<br />
15. CO2 is excreted from the body only via the lungs?<br />
a. True b. False<br />
16. Differences in trauma care around the world are associated with<br />
a. economic disparities c. lack <strong>of</strong> education<br />
b. cultural variances d. all <strong>of</strong> above<br />
17. <strong>The</strong> large number <strong>of</strong> civilian deaths caused by explosive wounds can be attributed to<br />
a. <strong>The</strong> aggregation <strong>of</strong> large numbers <strong>of</strong> people in a single confined area.<br />
b. <strong>The</strong> exponential increase in firepower <strong>of</strong> modern explosives.<br />
c. Deliberate targeting.<br />
d. Personal and environmental/structural vulnerability.<br />
e. All <strong>of</strong> the above.<br />
18. <strong>The</strong> USAF has adopted physician-based crews to conduct critical care air transport <strong>of</strong> stabilized casualties.<br />
a. True b. False<br />
19. Brain death<br />
a. is diagnosed only if the patient is a potential organ donor.<br />
b. is a process, not an event.<br />
c. is an acceptable diagnosis to all races and religions.<br />
d. is always present if brain stem reflexes and respiration are absent.<br />
20. <strong>The</strong> inotrope <strong>of</strong> choice for the management <strong>of</strong> the brain-dead, heart-beating donor is<br />
a. Dopamine b. Norepinephrine c. Vasopressin<br />
21. End-tidal CO2 is the peak value <strong>of</strong> exhaled CO2 at end-expiration.<br />
a. True b. False<br />
22. <strong>The</strong> absence <strong>of</strong> end-tidal CO2 following attempted intubation confirms oesophageal placement <strong>of</strong> the tube.<br />
a. True b. False.<br />
23. Decreasing end-tidal CO2 during cardiac massage may indicate operator fatigue.<br />
a. True b. False<br />
24. Low end-tidal CO2 values in trauma patients are positively associated with survival.<br />
a. True b. False.<br />
25. A patient suffering primary cardiac arrest with an end-tidal CO2 <strong>of</strong> 1.0 kPa after 20 minutes <strong>of</strong> resuscitation is unlikely to survive.<br />
a. True. b. False<br />
26. <strong>The</strong> use <strong>of</strong> hypertonic saline combined with a dextran instead <strong>of</strong> crystalloid in the prehospital care <strong>of</strong> patients with severe head injury with hypotension<br />
improves survival by a factor <strong>of</strong> two.<br />
a. True b. False<br />
70
<strong>ITACCS</strong> Spring 2003<br />
27. In physician-operated EMS care in France, all <strong>of</strong> the techniques listed below have a place in the provision <strong>of</strong> prehospital analgesia EXCEPT:<br />
a. use <strong>of</strong> opioids<br />
b. use <strong>of</strong> paracetamol<br />
c. rewarming<br />
d. spinal block<br />
e. peripheral nerve blocks<br />
28. Anesthesiologists have no immediate role to play in the management casualties from terrorist chemical and biological attacks.<br />
a. True b. False<br />
29. Road traffic incidents and falls from height are the commonest causes <strong>of</strong> paediatric trauma.<br />
a. True b. False<br />
30. <strong>The</strong> most common paediatric arrhythmia at cardiac arrest is pulseless electrical activity.<br />
a. True b. False<br />
31. A cause <strong>of</strong> ventricular fibrillation that should be excluded is hypothermia.<br />
a. True b. False<br />
32. A low larynx in children makes visualisation <strong>of</strong> the vocal cords more difficult.<br />
a. True b. False<br />
33. Intraosseous access is contraindicated distal to a limb fracture.<br />
a. True b. False<br />
34. <strong>The</strong> recommended fluid for initial resuscitation <strong>of</strong> the pediatric trauma patient is:<br />
a. Crystalloid solutions b. Colloid solutions c. Dextrose solutions<br />
35. <strong>The</strong> two most important determinants <strong>of</strong> burn severity are burn size and location.<br />
a. True b. False<br />
Evaluation Form: Please rate this self-study activity by marking one response for each statement.<br />
Did the articles meet their stated objectives? ___Yes ___No<br />
How do you rank the quality <strong>of</strong> this educational activity? ___5 (high) ____4 ___3 ___2 ___1 (low)<br />
Comments: _________________________________________________________________________________________________________________<br />
Did you perceive any evidence <strong>of</strong> bias for or against any commercial products? ___Yes ___No If yes, please explain.<br />
Comments: _________________________________________________________________________________________________________________<br />
How do you rank the effectiveness <strong>of</strong> this activity as it pertains to your practice? ___5 (high) ____4 ___3 ___2 ___1 (low)<br />
Did this material stimulate your intellectual curiosity? ___5 (high) ____4 ___3 ___2 ___1 (low)<br />
Additional comments about this activity:<br />
__________________________________________________________________________________________________________________________<br />
__________________________________________________________________________________________________________________________<br />
Answer Form: Please circle the one best answer for each question.<br />
<strong>Trauma</strong>Care Spring 2003 issue<br />
Name:<br />
Address:<br />
City:<br />
__________________________________________________________________<br />
__________________________________________________________________<br />
__________________________________________________________________<br />
__________________________________________________________________<br />
State: _________________ Zip: _________ Phone:_____________________________<br />
I certify that I have completed the “<strong>Trauma</strong>Care/Spring 2003” activity as designed and claim 20 credit hours in<br />
Category 1 <strong>of</strong> the Physicians Recognition Award <strong>of</strong> the American Medical Association.<br />
____________________________________________________________________________<br />
Signature<br />
Date<br />
Mail answer form and check ($100, members; $200, nonmembers) to <strong>ITACCS</strong> Department <strong>of</strong><br />
CME Credit, P.O. Box 4826, Baltimore, MD 21211. Allow 4 to 6 weeks for processing.<br />
Credit for this activity is <strong>of</strong>fered until May 31, 2004.<br />
71<br />
1. a b c d<br />
2. a b<br />
3. a b c d e<br />
4. a b<br />
5. a b c d e<br />
6. a b<br />
7. a b c d<br />
8. a b c d e<br />
9. a b c d<br />
10. a b c d e<br />
11. a b c d e<br />
12. a b<br />
13. a b c d<br />
14. a b<br />
15. a b<br />
16. a b c d<br />
17. a b c d e<br />
18. a b<br />
19. a b c d<br />
20. a b c<br />
21. a b<br />
22. a b<br />
23. a b<br />
24. a b<br />
25. a b<br />
26. a b<br />
27. a b c d e<br />
28. a b<br />
29. a b<br />
30. a b<br />
31. a b<br />
32. a b<br />
33. a b<br />
34. a b c<br />
35. a b