view PDF - American Association of Neurological Surgeons
view PDF - American Association of Neurological Surgeons
view PDF - American Association of Neurological Surgeons
Create successful ePaper yourself
Turn your PDF publications into a flip-book with our unique Google optimized e-Paper software.
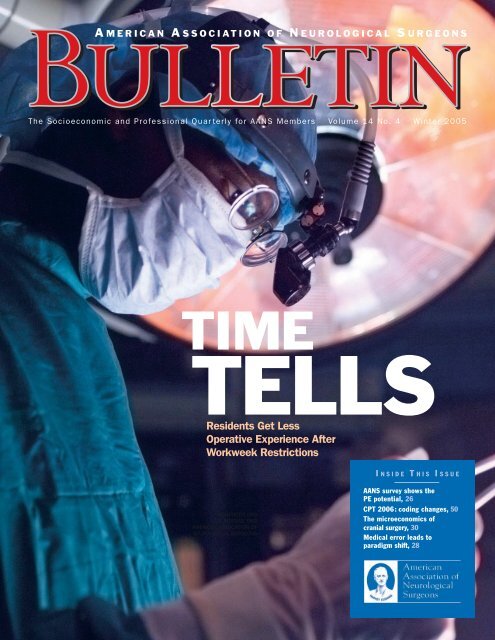
The Socioeconomic and Pr<strong>of</strong>essional Quar terly for AANS Members • Volume 14 No. 4 • Winter 2005<br />
TIME<br />
TELLS<br />
Residents Get Less<br />
Operative Experience After<br />
Workweek Restrictions<br />
I N S I D E T H I S I S S U E<br />
AANS<br />
5550 MEADOWBROOK DRIVE<br />
ROLLING MEADOWS, IL 60008<br />
NON-PROFIT ORG<br />
U.S. POSTAGE PAID<br />
AMERICAN ASSOCIATION OF<br />
NEUROLOGICAL SURGEONS<br />
● AANS survey shows the<br />
PE potential, 26<br />
● CPT 2006: coding changes, 50<br />
● The microeconomics <strong>of</strong><br />
cranial surgery, 30<br />
● Medical error leads to<br />
paradigm shift, 28
C<br />
ONTENT<br />
ONTENTS<br />
VOLUME 14 NO. 4<br />
PRESIDENT’S MESSAGE<br />
5 | Neurosurgery: The Expedition<br />
The AANS is strategically planning for next year—and for<br />
neurosurgery’s next 75 years.<br />
Fremont P. Wirth, MD<br />
FEATURES<br />
26 | The PE Potential<br />
New AANS study supplies a snapshot <strong>of</strong> physician<br />
extenders in neurosurgical practices.<br />
Kathleen T. Craig<br />
30 | When Neurosurgeons Drop Cranial Surgery Privileges<br />
Microeconomics may play a role in these decisions.<br />
Richard N.W. Wohns, MD<br />
ON THE COVER<br />
12 | Time Tells: Residents Get Less Operative<br />
Experience After Workweek Restrictions<br />
Will the newly minted neurosurgeon you hire be as<br />
well-trained as you were For academicians and private<br />
practitioners alike, this is the million-dollar question.<br />
Now, with more than two years <strong>of</strong> data available,<br />
neurosurgery is beginning to apply evidence-based<br />
methodology to determine the actual impact <strong>of</strong> the<br />
restrictions on the medical education <strong>of</strong> its residents.<br />
14 | ACGME-Mandated Work Hours: Implementation<br />
at the University <strong>of</strong> Oklahoma<br />
A peer-re<strong>view</strong>ed study finds that limited work hours<br />
are feasible, but residents operate less.<br />
Michael D. Martin, MD, and<br />
Christopher E. Wolfla, MD<br />
17 | Work Hour Restrictions: Impact on Neurosurgical<br />
Resident Training at the University <strong>of</strong> Utah<br />
A peer-re<strong>view</strong>ed study demonstrates significant decreases<br />
in the operative experience <strong>of</strong> junior residents.<br />
Todd McCall, MD, Ganesh Rao, MD,<br />
and John Kestle, MD<br />
23 | Restrictions Get Reality Check<br />
A neurosurgeon assesses the past, present and future<br />
<strong>of</strong> resident work hour restrictions.<br />
Deborah L. Benzil, MD<br />
46 | MOC Takes Shape<br />
The ABNS begins its Maintenance <strong>of</strong> Certification<br />
program rollout in 2006.<br />
Ralph G. Dacey Jr., MD, M. Sean Grady, MD, Hunt Batjer,<br />
MD, and William Chandler, MD<br />
NEWS AND EVENTS<br />
7 | Newsline: From the Hill<br />
Don’t claim unpaid services for indigents as<br />
charitable deductions.<br />
8 | Newsline: Neuro News<br />
FDA approves titanium implant for treatment <strong>of</strong><br />
lumbar spinal stenosis.<br />
48 | News.org<br />
The AANS endorses NextGen electronic<br />
medical record system.<br />
51 | Calendar <strong>of</strong> Neurosurgical Events<br />
AANS Annual Meeting set for April 22–27 in San Francisco.<br />
OPINION<br />
52 | AANS Answers<br />
The AANS serves up success and prepares for<br />
increased innovation.<br />
Thomas A. Marshall<br />
11 | Personal Perspective<br />
AANS Bulletin delivers data.<br />
William T. Couldwell, MD<br />
Volume 14, Number 4 • AANS Bulletin 3
C<br />
C ONTENTS<br />
S<br />
DEPARTMENTS<br />
41 | Bookshelf 28 | Patient Safety<br />
New Cushing biography fleshes out neurosurgery’s A medical error results in a neurosurgeon’s<br />
founder.<br />
paradigm shift.<br />
Gary Vander Ark, MD<br />
Arnold A. Zeal, MD<br />
50 | Coding Corner 36 | Residents’ Forum<br />
Payers may lag behind Jan. 1 implementation <strong>of</strong> CPT To evaluate a new job, rank your priorities and do<br />
2006 coding changes. your homework.<br />
Gregory J. Przybylski, MD<br />
K. Michael Webb, MD, and Lawrence S. Chin, MD<br />
35 | Computer Ease 39 | Risk Management<br />
Online learning and performance-assessment tools A physician may be liable when a patient delays<br />
are evolving.<br />
surgery with adverse results.<br />
Joel D. MacDonald, MD<br />
Michael A. Chabraja, JD, and Monica Wehby, MD<br />
49 | In Memoriam<br />
Remembering Lyal G. Leibrock, MD<br />
James R. Bean, MD<br />
32 | Medicolegal Update<br />
Can contracts preclude frivolous lawsuits<br />
Jeffrey Segal, MD, and Michael J. Sacopulos, JD<br />
40 | NREF<br />
NREF corporate partner matches donations<br />
100 percent.<br />
Michele S. Gregory<br />
38 | Timeline<br />
When their residence isn’t the hospital, what do you<br />
call physician trainees<br />
Michael Schulder, MD<br />
42 | Washington Update<br />
Contributors to NPHCA support neurosurgery’s<br />
medical liability campaign.<br />
AANS MISSION WRITING GUIDELINES Correspondence is assumed to be for publication unless<br />
The AANS is dedicated to advancing the specialty <strong>of</strong> neuro- www.aans.org/bulletin otherwise specified.<br />
logical surgery in order to provide the highest quality <strong>of</strong><br />
neurosurgical care to the public.<br />
BULLETIN ONLINE<br />
ARTICLE SUBMISSIONS AND IDEAS<br />
The current issue and searchable archives to 1995 are<br />
Articles or article ideas concerning socioeconomic topics<br />
AANS BULLETIN<br />
available at www.aans.org/bulletin.<br />
related to neurosurgery can be submitted to the Bulletin,<br />
The <strong>of</strong>ficial publication <strong>of</strong> the <strong>American</strong> <strong>Association</strong> <strong>of</strong> bulletin@AANS.org. Objective, nonpromotional articles that<br />
<strong>Neurological</strong> <strong>Surgeons</strong>, the Bulletin features news about the are in accordance with the writing guidelines, are original, PUBLICATION INFORMATION<br />
AANS and the field <strong>of</strong> neurosurgery, with a special emphasis and have not been published previously may be considered The AANS Bulletin, ISSN 1072-0456, is published four times<br />
on socioeconomic topics. for publication. a year by the AANS, 5550 Meadowbrook Drive, Rolling<br />
William T. Couldwell, MD, editor<br />
The AANS reserves the right to edit articles for compliance<br />
Meadows, Ill., 60008, and distributed without charge to the<br />
Robert E. Harbaugh, MD, associate editor<br />
with publication standards and available space and to<br />
neurosurgical community. Unless specifically stated otherpublish<br />
them in the vehicle it deems most appropriate.<br />
wise, the opinions expressed and statements made in this<br />
Manda J. Seaver, staff editor<br />
Articles accepted for publication become the property <strong>of</strong> the<br />
publication are the authors’ and do not imply endorsement<br />
AANS unless another written arrangement has been agreed<br />
by the AANS.<br />
BULLETIN ADVISORY BOARD<br />
upon between the author(s) and the AANS.<br />
© 2005–2006 by the <strong>American</strong> <strong>Association</strong> <strong>of</strong> <strong>Neurological</strong><br />
Deborah L. Benzil, MD Mick J. Perez-Cruet, MD <strong>Surgeons</strong>, a 501(c)(6) organization, all rights reserved.<br />
Frederick A. Boop, MD A. John Popp, MD PEER-REVIEWED RESEARCH Contents may not be reproduced, stored in a retrieval system,<br />
Alan S. Boulos, MD Gregory J. Przybylski, MD The Bulletin seeks submissions <strong>of</strong> rigorously researched, or transmitted in any form by any means without prior written<br />
Lawrence S. Chin, MD Michael Schulder, MD hypothesis-driven articles concerning socioeconomic topics permission <strong>of</strong> the publisher.<br />
Fernando G. Diaz, MD Gary D. Vander Ark, MD related to neurosurgery. Selected articles will be re<strong>view</strong>ed by the<br />
David F. Jimenez, MD Monica C. Wehby, MD Peer-Re<strong>view</strong> Panel. Submit articles to the Bulletin,<br />
ADVERTISING SALES<br />
Patrick W. McCormick, MD Richard N. Wohns, MD bulletin@AANS.org.<br />
Bill Scully, Cunningham Associates, (201) 767-4170, or<br />
Katie O. Orrico, JD Peer-Re<strong>view</strong> Panel led by Mick J. Perez-Cruet, MD; bscully@cunnasso.com. Rate card, www.aans.org/bulletin.<br />
Deborah L. Benzil, MD; William E. Bingaman Jr., MD;<br />
Frederick A. Boop, MD; Fernando G. Diaz, MD; David F.<br />
DEPARTMENT EDITORS AND CORRESPONDENTS<br />
Jimenez, MD; Mark E. Linskey, MD; Richard N. Wohns, MD<br />
Deborah L. Benzil, MD (Education); Larry Chin, MD<br />
(Residents' Forum); Fernando Diaz, MD (CSNS Report);<br />
Alan S. Boulos, MD (Computer Ease); William T. Couldwell, LETTERS<br />
MD (NS Innovations); Monica Wehby, MD (Risk<br />
Send your comments on articles you’ve read in these<br />
Management); Katie O. Orrico, JD (Washington Update); pages or on a topic related to the practice <strong>of</strong> neurosurgery<br />
Gregory J. Przybylski, MD (Coding Corner); Michael<br />
to bulletin@AANS.org. Correspondence may be published<br />
Schulder, MD (Timeline); Gary Vander Ark (Bookshelf) in a future issue edited for length, clarity and style.<br />
4 AANS Bulletin • www.AANS.org
P RESIDENT’ S M ESSAGE<br />
F REMONT P .<br />
W IRTH, MD<br />
Neurosurgery: The Expedition<br />
Strategic Planning Guides the Way<br />
“I walked down and joined the<br />
party at their encampment…much<br />
pleased at having arrived at this<br />
long-wished-for spot.”<br />
Meriwether Lewis thus recorded the<br />
arrival <strong>of</strong> the Corps <strong>of</strong> Discovery<br />
expedition at the junction <strong>of</strong> the<br />
Missouri and Yellowstone rivers in<br />
what today is Montana thinking his company<br />
was closing in on its goal <strong>of</strong> finding a<br />
water route to the Pacific Ocean. Though<br />
they would not attain their goal for many<br />
months, Lewis’ journal entry <strong>of</strong> April 26,<br />
1805, describes a point at which to reflect<br />
on the wonders <strong>of</strong> the journey so far and<br />
prepare for the yet unknown challenges<br />
that lay ahead.<br />
As the nation commemorates the bicentennial<br />
<strong>of</strong> Lewis and Clark’s influential<br />
journey, the AANS prepares for celebration<br />
<strong>of</strong> its 75th anniversary, acknowledging an<br />
expedition <strong>of</strong> a different kind. It seems an<br />
appropriate time at which to pause and take<br />
stock <strong>of</strong> what our association has accomplished<br />
and what it seeks to accomplish in<br />
the future.<br />
Numerous wonders in neurosurgery<br />
have come to pass since the association’s<br />
inception in 1931 as the Harvey Cushing<br />
Society in homage to that first “neurosurgeon.”<br />
The venerable icon himself is<br />
explored in a new biography that reveals<br />
fresh insights into Cushing’s progress in<br />
neurological surgery. In many ways, his<br />
pr<strong>of</strong>essional journey is early neurosurgery’s<br />
own.<br />
Initially the association’s primary goal<br />
was to serve as an infrastructure for meetings<br />
that involved “investigation and<br />
advancement in the fields <strong>of</strong> neurosurgery,<br />
with the fundamental needs <strong>of</strong> establishing<br />
methods <strong>of</strong> early diagnosis and postoperative<br />
treatment, directed toward the protection<br />
<strong>of</strong> the patients, and a decrease in<br />
mortality,” according to Temple Fay, a<br />
AANS founder.<br />
Like the Corps <strong>of</strong> Discovery members<br />
who equipped themselves for an arduous<br />
journey and expected the unknown and<br />
unforeseen—wooly mammoths and pure<br />
salt mountains were considered among the<br />
possibilities—the AANS founders prepared<br />
themselves for an expedition into the estab-<br />
Fremont P. Wirth,<br />
MD, is the 2005–2006<br />
AANS president. He is<br />
in private practice at<br />
the <strong>Neurological</strong><br />
Institute <strong>of</strong> Savannah<br />
in Georgia.<br />
lishment and development <strong>of</strong> a new and<br />
demanding surgical specialty. Though<br />
surely they could not have anticipated the<br />
astonishing technological advances available<br />
to us today—functional magnetic resonance<br />
imaging, artificial lumbar discs,<br />
robotic surgery—the mission they articulated<br />
pointed the organization in the right<br />
direction.<br />
Revitalized Mission, Focused but<br />
Flexible Goals<br />
Over the years the AANS has formalized<br />
and expanded upon its founders’ ideas.<br />
The current mission and vision statement<br />
is accessible at www.aans.org/about, and<br />
we anticipate release <strong>of</strong> a revitalized mission<br />
and vision statement during the 75th<br />
anniversary year. However, that the<br />
founders’ concerns remain at the core <strong>of</strong><br />
the AANS today is apparent in the association’s<br />
annual meetings, as the 2006 AANS<br />
Annual Meeting will exemplify.<br />
In April, the AANS will convene in San<br />
Francisco to present its 74th annual neurosurgical<br />
event under the direction <strong>of</strong><br />
James T. Rutka, MD, annual meeting<br />
chair, and Mitchel S. Berger, MD, scientific<br />
program chair. A total <strong>of</strong> 646 abstracts<br />
have been selected for presentation at the<br />
meeting. Over the years the meeting has<br />
grown to encompass plenary and scientific<br />
sessions, AANS/CNS subspecialty section<br />
sessions, breakfast sessions and<br />
special lectures. Hands-on practical clinics<br />
hearken to the AANS founders’ concern<br />
for improved patient outcomes<br />
through refinement <strong>of</strong> surgical technique,<br />
and enjoyable social activities continue to<br />
foster a collegial spirit.<br />
While the meeting itself will focus on<br />
scientific advances that promote quality<br />
patient care and safety, its theme, Challenges<br />
<strong>of</strong> Neurosurgery: Expanding<br />
Resources for a Growing Population, was<br />
chosen to ensure that the meeting also<br />
incorporates valuable information regarding<br />
the impact <strong>of</strong> current societal influences<br />
on the practice <strong>of</strong> neurosurgery. I<br />
selected this theme because issues underlying<br />
workforce and other concerns that are<br />
significantly challenging our pr<strong>of</strong>ession<br />
now and in the next 10 years must be<br />
uncovered and addressed today.<br />
To that end, the AANS Task Force on<br />
Neurosurgical Care and Physician Workforce<br />
Issues met for the first time in November.<br />
I asked several neurosurgeons, chosen<br />
for their seniority and representation <strong>of</strong><br />
various practice situations across the nation,<br />
to join me in this endeavor: Paul J. Camarata,<br />
Mark H. Camel, Martin B. Camins, Stewart<br />
B. Dunsker, Robert Grubb, Hal L.<br />
Hankinson, Julian T. H<strong>of</strong>f, David L. Kelly Jr.,<br />
Lawrence H. Pitts, Donald O. Quest, Robert<br />
A. Ratcheson, Jon H. Robertson, Richard A.<br />
Roski,Alex B.Valadka, and Martin H.Weiss.<br />
Continued on page 6<br />
Volume 14, Number 4 • AANS Bulletin 5
P RESIDENT’ S<br />
M ESSAGE<br />
Continued from page 5<br />
After re<strong>view</strong>ing available information,<br />
the task force identified distribution <strong>of</strong> neurosurgical<br />
services and organization <strong>of</strong> neurosurgical<br />
care as areas in need <strong>of</strong> further<br />
inquiry. Therefore, the AANS is conducting<br />
an online workforce survey in early 2006; if<br />
you are contacted, I encourage you to help<br />
us in this important effort. The task force<br />
plans to report on its findings in April.<br />
Another group, the AANS Physician<br />
Extenders Task Force, spearheaded a survey<br />
conducted last fall to discover how neurosurgeons<br />
are using or would like to use<br />
nurse practitioners and physician assistants<br />
in their practices and to discern how they<br />
are, and should be, trained. Charles Hodge,<br />
MD, led the effort, the results <strong>of</strong> which are<br />
featured in this Bulletin issue.<br />
Workforce was one <strong>of</strong> three issues identified<br />
in my fall column as top AANS concerns;<br />
the other two topics, medical liability<br />
reform and physician reimbursement,<br />
surely are among the forces that are stressing<br />
the neurosurgical workforce. All three<br />
areas remain top priorities, and they will be<br />
addressed in detail in future issues <strong>of</strong> the<br />
Bulletin as well as at the annual meeting.<br />
Progress According to Plan<br />
Provisioned with a clear mission, today’s<br />
AANS leadership employs a detailed document,<br />
the AANS Strategic Plan, which<br />
maps the way to ensuring that our pr<strong>of</strong>ession<br />
maintains excellence in providing our<br />
patients with high quality neurosurgical<br />
care while simultaneously addressing pr<strong>of</strong>essional<br />
issues such as workforce. The<br />
strategic planning process was formalized<br />
in 2003 by A. John Popp, MD, leading the<br />
Long Range Planning Committee. Since<br />
then the successive plans have articulated<br />
goals aligned with the AANS mission, with<br />
specific tasks then assigned to specific committees<br />
and tied to the budget.<br />
For example, in the tradition <strong>of</strong> pr<strong>of</strong>essional<br />
education at the core <strong>of</strong> the<br />
AANS mission, a plan goal <strong>of</strong> developing<br />
member services and benefits specified a<br />
task that called for the AANS to reassess<br />
benefits for young neurosurgeons—our<br />
pr<strong>of</strong>ession’s future workforce. Today residents<br />
in North America not only attend<br />
the annual meeting at no cost to them,<br />
they also receive free AANS membership<br />
and the AANS Journal <strong>of</strong> Neurosurgery.<br />
Another task called for the AANS to establish<br />
a central repository for continuing<br />
medical education and maintenance <strong>of</strong><br />
certification. The AANS has since worked<br />
closely with the <strong>American</strong> Board <strong>of</strong> <strong>Neurological</strong><br />
Surgery to meet this goal and<br />
others in advance <strong>of</strong> the board’s MOC<br />
program launch in January, and today<br />
CME credits for MOC are tracked at<br />
www.MyAANS.org. ABNS directors discuss<br />
MOC implementation in this issue <strong>of</strong><br />
the Bulletin.<br />
Challenges...need not<br />
deter us in pursuing what<br />
we know to be a worthwhile,<br />
stimulating pr<strong>of</strong>ession<br />
that provides essential<br />
services to our patients.<br />
The plan also called for the development<br />
<strong>of</strong> member services and benefits via a<br />
biennial member needs assessment that<br />
would “assure that members’ feedback is<br />
continually factored into leadership decision-making.”<br />
AANS leadership, including<br />
all the committee volunteers who make this<br />
organization work, can attest to the value <strong>of</strong><br />
this data in tailoring an association that<br />
works for you.<br />
The updated AANS Strategic Plan, currently<br />
in development by AANS President-Elect<br />
Don Quest and the Long Range<br />
Planning Committee, will address financial,<br />
organizational, customer service and<br />
advocacy areas <strong>of</strong> the association. The new<br />
plan will be detailed in an upcoming issue<br />
<strong>of</strong> the Bulletin.<br />
By providing a consistent yet flexible<br />
base, the AANS Strategic Plan is an essen-<br />
tial element for meeting the needs <strong>of</strong> our<br />
members and our pr<strong>of</strong>ession today and<br />
anticipating the needs <strong>of</strong> our successors<br />
another 75 years hence. It also serves to<br />
remind us that challenges such as workforce,<br />
medical liability reform and physician<br />
reimbursement—as I write this, we<br />
may or may not have staved <strong>of</strong>f the 4.4 percent<br />
reduction in Medicare physician reimbursement<br />
scheduled to take place in<br />
January—need not deter us in pursuing<br />
what we know to be a worthwhile, stimulating<br />
pr<strong>of</strong>ession that provides essential services<br />
to our patients.<br />
Taking stock <strong>of</strong> the AANS’ first 75 years<br />
inspires great confidence that the organization,<br />
volunteer leaders and members are<br />
equipped with the tools, sense <strong>of</strong> purpose<br />
and fortitude to meet the challenges yet to<br />
be imagined and faced. I believe that our<br />
planning will prove to be as prudent,<br />
responsible and visionary as that <strong>of</strong> our<br />
forebears.<br />
With appreciation for the journey we<br />
have taken together and in anticipation <strong>of</strong><br />
what is to come, I thank you for your<br />
involvement in the AANS and invite your<br />
future participation in our organization.<br />
April 26, 2006, exactly 201 years after<br />
Lewis paused to reflect on his journey at the<br />
confluence <strong>of</strong> two great rivers, coincidentally<br />
will mark the conclusion <strong>of</strong> my<br />
sojourn as AANS president. The entire<br />
AANS leadership team and I are working to<br />
launch the 75th anniversary year memorably<br />
at the 2006 Annual Meeting. I hope<br />
you will join me in San Francisco April<br />
22–27 not only for superlative science and<br />
celebration, but also in feeling much<br />
pleased at having arrived at a long-wishedfor<br />
spot. 3<br />
Related Articles<br />
3 2005 AANS Physician Extender Survey<br />
results reported, page 26<br />
3 ABNS directors discuss Maintenance <strong>of</strong><br />
Certification program launch, page 46<br />
3 New Cushing biography re<strong>view</strong>ed in<br />
Bookshelf, page 41<br />
6 AANS Bulletin • www.AANS.org
N<br />
N EWSLINEE<br />
WSLINE<br />
NewsMembersTrendsLegislation<br />
F R O M T H E H I L L<br />
HHS Opens IT Office<br />
Notice <strong>of</strong> the establishment<br />
<strong>of</strong> the Office <strong>of</strong><br />
Health Information<br />
Technology, a new branch<br />
<strong>of</strong> the U.S. Department<br />
<strong>of</strong> Health and Human<br />
Services, was <strong>of</strong>ficially<br />
given in the Federal<br />
Register on Dec. 27.<br />
The <strong>of</strong>fice’s administrator<br />
sits on the Health<br />
Resources and Services<br />
Administration’s Health<br />
Care Quality Council.<br />
Creation <strong>of</strong> the new<br />
<strong>of</strong>fice is the latest<br />
evidence <strong>of</strong> the Bush<br />
administration’s strong<br />
support for nationwide<br />
adoption <strong>of</strong> health information<br />
technology, an<br />
integral component <strong>of</strong><br />
so-called pay-forperformance<br />
programs.<br />
3 Don’t Claim Unpaid Services for Indigents as Charitable Deductions As a new year begins, taxes are on<br />
the minds <strong>of</strong> many. The AANS Board <strong>of</strong> Directors recently asked AANS legal counsel for an opinion on<br />
whether doctors can claim a charitable deduction for the value <strong>of</strong> uncompensated services performed<br />
for Medicaid patients or otherwise indigent individuals. “The answer is no, primarily because Congress<br />
specifically excluded individuals from the list <strong>of</strong> charitable organizations set forth in the Internal<br />
Revenue Code,” said Russell M. Pelton, JD. “To receive a charitable deduction for services provided to<br />
individuals would require an amendment to the Internal Revenue Code by Congress, an event that is<br />
unlikely to occur in the foreseeable future.” The two main reasons why the value <strong>of</strong> services performed<br />
for Medicaid patients are not deductible are that Medicaid patients do not constitute a charitable organization<br />
within the meaning <strong>of</strong> section 170(c) <strong>of</strong> the tax code and that deductions are not allowed for<br />
the performance <strong>of</strong> services on behalf <strong>of</strong> a charitable organization. According to Pelton, a substantial<br />
number <strong>of</strong> court decisions hold that services do not constitute property for charitable deduction purposes.<br />
The full text <strong>of</strong> the opinion, “Charitable Deduction Issues,” is available at www.AANS.org.<br />
3 CMS Pledges Rapid Implementation <strong>of</strong> New Reimbursement Rates Although Congress adjourned in<br />
December without finalizing budget legislation that would have prevented a 4.4 percent cut to physician<br />
reimbursement from taking effect Jan. 1, the Centers for Medicare and Medicaid Services advised<br />
Congress <strong>of</strong> its readiness to quickly implement the legislation once it is passed. In a letter to Rep. Bill<br />
Thomas, Herb Kuhn, director <strong>of</strong> the Center for Medicare Management, said the CMS would instruct<br />
Medicare contractors to begin paying claims at the revised update <strong>of</strong> 0.0 percent within two business<br />
days <strong>of</strong> the legislation’s passage. Contractors also would be instructed to automatically reprocess claims<br />
received between Jan. 1 and passage <strong>of</strong> legislation, relieving physicians <strong>of</strong> the resubmission process. The<br />
reprocessed claims would be paid in a lump sum to providers by July 1. The CMS also plans to <strong>of</strong>fer<br />
physicians a second enrollment period <strong>of</strong> 45 days following enactment <strong>of</strong> the budget legislation.<br />
Complete text <strong>of</strong> the letter is available at www.aans.org/ltr_to_leadership01_06.pdf.<br />
3 AANS/CNS Prevent a 3 Percent Reimbursement Cut, Proclaim Victory for Neurosurgeons On Nov. 2 the<br />
Centers for Medicare and Medicaid Services announced that it would withdraw its proposal <strong>of</strong> last<br />
August to change the practice expense calculation under the Medicare fee schedule, thus preventing a<br />
nearly 3 percent cut in neurosurgeons’ Medicare reimbursement. The AANS and CNS, along with<br />
numerous other specialty societies, had objected to the proposed changes. The CMS also adopted two<br />
additional policy changes that will result in increased Medicare reimbursement for neurosurgeons. First,<br />
the agency made minor modifications to its formula for calculating malpractice expenses. Second, the<br />
CMS is applying a multiple procedure payment reduction for diagnostic imaging (similar to the multiple<br />
surgery payment reduction policy). Together, these changes result in a modest 0.5 percent increase in<br />
reimbursement for neurosurgeons. Regulation CMS-1502-FC can be found at www.cms.gov.<br />
Frequent updates to<br />
legislative news are<br />
available in the<br />
Legislative Activities<br />
area <strong>of</strong> www.AANS.org.<br />
3 Medical Liability Reform Initiative Progresses In November Doctors for Medical Liability Reform<br />
released a new animated e-mail message calling for reform. The e-mail message from A. John Popp, MD,<br />
president <strong>of</strong> the AANS/CNS advocacy organization Neurosurgeons to Preserve Health Care Access,<br />
encourages recipients to extend the medical liability reform message by forwarding the e-mail to as<br />
many people as possible. The e-mail initiative is one facet <strong>of</strong> the nationwide grassroots education and<br />
advocacy campaign, Protect Patients Now. More information about the DMLR campaign is available at<br />
www.protectpatientsnow.org. A listing <strong>of</strong> donors in 2005 to the NPHCA, an organization that funds the<br />
DMLR Protect Patients Now campaign, is available in this issue’s Washington Update, page 42.<br />
Volume 14, Number 4 • AANS Bulletin 7
N<br />
N EWSLINEE<br />
WSLINE<br />
NewsMembersTrendsLegislation<br />
N E U R O N E W S<br />
.MD DOMAIN<br />
OFFICIALLY LAUNCHES<br />
A domain unique to<br />
members <strong>of</strong> the medical<br />
community, .md, <strong>of</strong>ficially<br />
launched in December.<br />
The .md domain differs<br />
from .com and .net<br />
domains in that it is<br />
dedicated to physicians,<br />
healthcare providers and<br />
medical organizations,<br />
allowing them to be<br />
located quickly by<br />
patients using the<br />
Internet. Additional<br />
information is available<br />
at www.maxmd.md.<br />
3 FDA Approves Device to Treat Lumbar Spinal Stenosis In November the U.S. Food and Drug<br />
Administration announced approval <strong>of</strong> a new titanium implant designed to limit extension <strong>of</strong> the spine<br />
in the area affected by lumbar spinal stenosis, which may relieve the painful symptoms if the disorder. The<br />
X-stop Interspinous Process Decompression System, invented by James Zucherman, MD, fits between the<br />
spinous processes. “By wedging those bones apart, the tube is indirectly opened up,” explained Dr.<br />
Zucherman in an Associated Press story. “The bones don’t collapse on the nerves like they did before [and]<br />
the patient doesn’t have to bend over to protect the nerves.” The X-stop is indicated for treatment <strong>of</strong><br />
patients age 50 or older who have been diagnosed with lumbar spinal stenosis, suffer from pain or cramping<br />
in the legs, and have undergone a regimen <strong>of</strong> at least six months <strong>of</strong> nonoperative treatment. Additional<br />
information is available at www.fda.gov/cdrh/mda/docs/p040001.html.<br />
3 Bone Marrow Stem Cell Approach Tested for Children With TBI A phase I trial underway in early 2006 is<br />
studying the safety and potential <strong>of</strong> treating children who have sustained traumatic brain injury with stem<br />
cells from their own bone marrow. The study at the University <strong>of</strong> Texas Medical School at Houston and<br />
Memorial Hermann Children’s Hospital involves extracting mesenchymal and hematopoietic stem cells<br />
from the bone marrow <strong>of</strong> each <strong>of</strong> 10 patients between the ages <strong>of</strong> 5 and 14, processing a stem cell preparation<br />
and giving it intravenously to the injured child, all within 48 hours <strong>of</strong> injury. “This would be an<br />
absolutely novel treatment, the first ever with potential to repair a traumatically damaged brain,” said neurosurgeon<br />
James Baumgartner, co-principal investigator on the project.<br />
3 Two Studies Explore Benefits and Risks <strong>of</strong> Vertebroplasty In two separate studies published in the<br />
<strong>American</strong> Journal <strong>of</strong> Neuroradiology, Mayo Clinic researchers report that patients with compression fractures<br />
are more functional for up to a year after vertebroplasty, but that the procedure may increase the risk<br />
<strong>of</strong> fracture in adjacent vertebrae. In the November–December issue <strong>of</strong> AJNR, Trout and colleagues report<br />
results <strong>of</strong> their retrospective re<strong>view</strong> <strong>of</strong> patients treated with vertebroplasty who had completed the Roland-<br />
Morris Disability Questionnaire at baseline and at four points during the year following the procedure.<br />
Patients’ pain during rest and activity improved an average <strong>of</strong> seven points one week after treatment and<br />
remained improved one year following treatment. In the January issue <strong>of</strong> AJNR, the researchers found<br />
that following vertebroplasty the risk <strong>of</strong> new fractures in adjacent vertebrae was 4.62 times the risk for<br />
nonadjacent vertebrae and that vertebrae adjacent to those treated with vertebroplasty fracture significantly<br />
sooner than more distant vertebrae. “This is not definitive evidence, but [it] should be considered<br />
when discussing risks with patients before embarking on vertebroplasty,” said David<br />
Kallmes, MD, senior study investigator.<br />
Send Neuro News briefs<br />
to the Bulletin,<br />
bulletin@AANS.org.<br />
3 Door Opens for Drugs That Turn Off Stroke-Induced Brain Damage A new study indicates that the EP1<br />
receptor on the surface <strong>of</strong> nerve cells is the switch that triggers brain damage caused by lack <strong>of</strong> oxygen during<br />
a stroke or seizure and that ONO-8713 is the compound that can turn the switch <strong>of</strong>f. The study, published<br />
in the January issue <strong>of</strong> Toxicological Sciences, found significant differences among mice whose ventricles<br />
were injected with EP1 stimulator ONO-DI-004, EP1 blocker ONO-8713, or the solvent used to<br />
carry the drugs. The volume <strong>of</strong> damage in mice treated first with ONO-8713 was only about 71 percent<br />
that <strong>of</strong> the control group injected with only the solvent. The researchers at Johns Hopkins University also<br />
showed that ONO-8713 can exert its influence only by binding to the EP1 receptor and that the stimulation<br />
<strong>of</strong> the EP1 receptors triggers the damage caused when blood flow is restored after a stroke. Researchers<br />
concluded that future efforts should focus on development <strong>of</strong> drugs that block the EP1 receptor.<br />
8 AANS Bulletin • www.AANS.org
P ERSONAL P ERSPECTIVE<br />
W ILLIAM T .<br />
C OULDWELL, MD<br />
Considering the Evidence<br />
AANS Bulletin Delivers Data<br />
On July 1, 2003, resident work-hour<br />
restrictions were imposed by the<br />
Accreditation Council for Graduate<br />
Medical Education. In this issue <strong>of</strong><br />
the Bulletin, we highlight two studies that<br />
examine the effects <strong>of</strong> the 80-hour workweek<br />
on neurosurgical resident education.<br />
At the University <strong>of</strong> Oklahoma, both junior<br />
and chief residents were exposed to less volume<br />
<strong>of</strong> surgery following introduction <strong>of</strong><br />
the restrictions. In the University <strong>of</strong> Utah<br />
study, the number <strong>of</strong> cases in which the<br />
junior residents were involved decreased 45<br />
percent after the implementation <strong>of</strong> the<br />
work hour restrictions.<br />
The reduced work hour rules were<br />
imposed without neurosurgical program<br />
directors’ input, and many do not agree<br />
with the changes implemented. Many residents,<br />
on the other hand, have welcomed<br />
the work hour limitations. What will be the<br />
impact <strong>of</strong> these changes on the practicing<br />
neurosurgical graduate As noted by Martin<br />
and Wolfla, while it is apparent that many in<br />
our field do not agree with these rules, it is<br />
imperative that further study be carried out<br />
to ensure that trainees graduating from<br />
neurosurgical residency are competent.<br />
Further, while the issue <strong>of</strong> competency<br />
has been a concern for many program<br />
directors, no studies to date have objectively<br />
assessed the effect <strong>of</strong> such work<br />
restrictions on trainee technical competency.<br />
Will this limitation <strong>of</strong> experience<br />
affect competency, or will extra nonwork-hour<br />
time be compensated by<br />
increased reading and hence knowledge <strong>of</strong><br />
the resident These questions should be<br />
the focus for careful analysis over the next<br />
few years. If the residency training will<br />
limit technical involvement and competency,<br />
then we must consider other alternative<br />
means for education, such as<br />
surgical simulation training. Alternatively,<br />
fellowship training will continue to propagate<br />
as a mechanism to develop competency<br />
in focused areas <strong>of</strong> practice.<br />
As many neurosurgeons are contemplating<br />
practice restrictions, Richard N.W.<br />
Wohns, MD, has compiled a thoughtful<br />
analysis <strong>of</strong> the microeconomics <strong>of</strong> per-<br />
William T. Couldwell,<br />
MD, is editor <strong>of</strong> the<br />
AANS Bulletin.<br />
forming cranial surgeries. Individual<br />
neurosurgeons will be able to mirror this<br />
template analysis and consider the implications<br />
<strong>of</strong> ceasing performance <strong>of</strong> these procedures<br />
in the context <strong>of</strong> their own<br />
particular practice demographics, reimbursement<br />
patterns, malpractice premiums,<br />
AANS Bulletin:<br />
A Top Member Benefit and a<br />
Leading Predictor <strong>of</strong> Satisfaction<br />
With AANS Membership<br />
The AANS Bulletin is the primary source<br />
<strong>of</strong> news that affects the practice <strong>of</strong> neurosurgery:<br />
practice management, legislation,<br />
coding and reimbursement, pr<strong>of</strong>essional<br />
development and education, and<br />
more. Readers are invited to participate<br />
in the Bulletin:<br />
Neurosurgical Pr<strong>of</strong>essionals<br />
• Write a letter to the editor.<br />
• Submit an article or article idea.<br />
and on-call responsibilities. These factors<br />
impact the pr<strong>of</strong>itability <strong>of</strong> cranial procedures,<br />
another <strong>of</strong> the many factors that<br />
must be considered when weighing the<br />
decision to restrict one’s practice.<br />
Also in this issue is an over<strong>view</strong> <strong>of</strong> the<br />
Maintenance <strong>of</strong> Certification program put<br />
forth by the <strong>American</strong> Board <strong>of</strong> <strong>Neurological</strong><br />
Surgery for rollout in January 2006.<br />
The key elements are published in the<br />
MOC handbook and are summarized in<br />
this issue <strong>of</strong> the Bulletin. MOC will be a<br />
foremost consideration for many neurosurgeons<br />
in the coming years. Neurosurgery<br />
has been one <strong>of</strong> the last medical<br />
specialties to adopt an MOC initiative, and<br />
we thank the ABNS and the many individuals<br />
involved with the question-writing<br />
committee for their efforts in the development<br />
<strong>of</strong> the MOC program. 3<br />
William T. Couldwell, MD, is pr<strong>of</strong>essor and Joseph J.<br />
Yager Chair <strong>of</strong> the Department <strong>of</strong> Neurosurgery at the<br />
University <strong>of</strong> Utah School <strong>of</strong> Medicine.<br />
• Submit socioeconomic research papers<br />
for peer re<strong>view</strong>.<br />
• Provide news briefs to News.org.<br />
• Submit a neurosurgical meeting to the<br />
online calendar.<br />
Corporations<br />
• Advertise in the Bulletin.<br />
• Sponsor the Bulletin<br />
(an exclusive opportunity).<br />
Learn more at www.aans.org/bulletin.<br />
Volume 14, Number 4 • AANS Bulletin 11
TIME<br />
TELLS<br />
Residents Get Less<br />
Operative Experience<br />
After Workweek<br />
Restrictions<br />
Will the newly minted neurosurgeon you hire be as<br />
well-trained as you were For academicians and<br />
private practitioners alike, this is the million-dollar<br />
question. When the 80-hour workweek for all<br />
medical residents became effective July 1, 2003, the<br />
Summer 2003 issue <strong>of</strong> the AANS Bulletin <strong>of</strong>fered<br />
an over<strong>view</strong> <strong>of</strong> the restrictions that were mandated<br />
by the Accreditation Council for Graduate<br />
Medical Education and explored their anticipated<br />
consequences. An opinion survey by Chang and<br />
Bell reported that the majority <strong>of</strong> respondents, 80<br />
percent <strong>of</strong> neurosurgical residency program directors<br />
and 56 percent <strong>of</strong> residents, said they expected<br />
the restrictions to have a negative impact on<br />
neurosurgical training, among other findings.<br />
Some articles attempted to foresee the future <strong>of</strong><br />
neurosurgical education, exploring workweek<br />
implementation methodologies and associated<br />
costs, while others re<strong>view</strong>ed the cost <strong>of</strong> New York’s<br />
405 Regulations, which preceded the ACGME<br />
restrictions by a decade, and reported the progress<br />
<strong>of</strong> federal legislation that threatened to supersede<br />
the ACGME restrictions.<br />
Now, with more than two years <strong>of</strong> data available,<br />
neurosurgery is beginning to apply evidence-based<br />
methodology to determine the actual impact <strong>of</strong> the<br />
restrictions on the medical education <strong>of</strong> its residents.<br />
Authors <strong>of</strong> the two peer-re<strong>view</strong>ed studies in this<br />
issue analyzed data at their own neurosurgery training<br />
programs to determine the level <strong>of</strong> compliance<br />
with the work hour restrictions as well as the impact<br />
<strong>of</strong> the restrictions on the operative experience <strong>of</strong> residents.<br />
Both studies found compliance with ACGME<br />
restrictions. Both also found that the number <strong>of</strong><br />
operative cases generally and significantly decreased<br />
for all residents. Interestingly, the distribution <strong>of</strong> the<br />
12 AANS Bulletin • www.AANS.org
operative cases between junior and chief residents was<br />
inverted at the two institutions studied: At the University<br />
Okalahoma, chief residents performed significantly<br />
fewer cases compared with data predating<br />
July 2003, and junior residents, more cases. At the<br />
University <strong>of</strong> Utah, junior residents performed<br />
roughly half the cases they had prior to implementation<br />
<strong>of</strong> the restrictions while chief residents’<br />
caseload remained largely unchanged.<br />
Even if the results <strong>of</strong> these two studies were<br />
extrapolated to all <strong>of</strong> neurosurgical education,<br />
would less operative experience necessarily mean<br />
that the neo-neurosurgeon you hire won’t be as well<br />
trained as you were Common sense may suggest an<br />
affirmative response but, as authors suggest in this<br />
issue, the answer is far more complex.<br />
To date, little additional data has been published<br />
regarding the impact <strong>of</strong> work hour restrictions on<br />
neurosurgical education. One study by Cohen-<br />
Gadol and colleagues surveyed neurosurgical program<br />
directors and residents in the three months<br />
immediately following implementation <strong>of</strong> the work<br />
hour restrictions. They found that 79 percent <strong>of</strong> the<br />
program directors and 61 percent <strong>of</strong> the residents<br />
said the ACGME guidelines have had a negative<br />
effect on their training programs, findings similar<br />
to those reported by Chang and Bell. The Cohen-<br />
Gadol study also reported that 93 percent <strong>of</strong> all<br />
respondents said the work hour restrictions have<br />
had a deleterious impact on patient care.<br />
Of course, improving patient care as well as<br />
patient and physician safety was the primary aim <strong>of</strong><br />
the ACGME in instituting the restrictions, and this<br />
also is the focus <strong>of</strong> related nationwide legislation.<br />
Whether the ACGME work hour restrictions are<br />
robust enough to stave <strong>of</strong>f federal legislation<br />
remains to be seen. Federal legislation that restricts<br />
resident work hours and increases resident supervision<br />
has been introduced every year since 2001,<br />
most recently in the 109th Congress as the Patient<br />
and Physician Safety and Protection Act <strong>of</strong> 2005. In<br />
March H.R. 1228 was referred to the House Ways and<br />
Means Subcommittee on Health, and in June S. 1297<br />
was sent to the Senate Committee on Finance. Text <strong>of</strong><br />
each bill is available at http://thomas.loc.gov.<br />
Data on the cost to neurosurgery programs <strong>of</strong><br />
implementing the restrictions also is scarce in the<br />
published literature. The annual cost <strong>of</strong> hiring physician<br />
extenders to replace residents has been reported<br />
in the AANS Bulletin to be $350,000 and $400,000 at<br />
two different training programs. In this issue’s<br />
“Restrictions Get Reality Check,” the total annual<br />
cost <strong>of</strong> implementing work hour restrictions at one<br />
teaching hospital is estimated at nearly $1 million.<br />
At least one study outside <strong>of</strong> neurosurgery<br />
attempted to analyze cost <strong>of</strong> the work hour reforms<br />
in relation to the benefit <strong>of</strong> preventing adverse<br />
events. In the October 2005 issue <strong>of</strong> the Journal <strong>of</strong><br />
Internal Medicine, Nuckols and Escarce concluded<br />
that a decline in adverse events <strong>of</strong> 5.1 percent to 8.5<br />
percent would make the reforms cost-neutral to<br />
society, but that a much larger drop <strong>of</strong> 18.5 percent<br />
to 30.9 percent would be needed to make them costneutral<br />
for teaching hospitals.<br />
The impact <strong>of</strong> the resident work hour restrictions<br />
on neurosurgery is one <strong>of</strong> many areas ripe for<br />
further research. Those interested in pursuing such<br />
research are encouraged to re<strong>view</strong> the writing<br />
guidelines for the AANS Bulletin, available at<br />
www.aans.org/bulletin. 3<br />
SUMMARY OF ACGME RESTRICTIONS<br />
Complete information is available at www.acgme.org > Resident Duty Hours.<br />
3 80 hours per week, averaged over four weeks, inclusive <strong>of</strong> all in-house call<br />
activities, with up to a 10 percent exception possible.<br />
3 One day in seven “<strong>of</strong>f” (one continuous 24-hour period free from all<br />
clinical, educational, and administrative activities) averaged over four weeks,<br />
inclusive <strong>of</strong> call.<br />
3 10 hours <strong>of</strong>f between all daily duty periods and after in-house call.<br />
3 In-house call every third night, averaged over four weeks.<br />
3 24 consecutive hours on-site, including call, with up to six additional hours for<br />
participating in educational activities and maintaining continuity <strong>of</strong> medical<br />
and surgical care.<br />
“Specialty Specific” Language for <strong>Neurological</strong> Surgery<br />
3 Continuous on-site duty, including in-house call, must not exceed 24 consecutive<br />
hours. Residents may remain on duty for up to six additional hours to participate<br />
in didactic activities, transfer care <strong>of</strong> patients, conduct outpatient clinics, and<br />
maintain continuity <strong>of</strong> medical and surgical care. This may include resident participation<br />
in the first surgical case <strong>of</strong> the day.<br />
3 No new patients may be accepted after 24 hours <strong>of</strong> continuous duty. A new<br />
patient is defined as any patient for whom the neurological surgery service or<br />
department has not previously provided care. The resident should evaluate the<br />
patient before participating in surgery.<br />
Volume 14, Number 4 • AANS Bulletin 13
On The Cover: Time Tells<br />
ACGME-Mandated Work Hours:<br />
Implementation at the University <br />
<strong>of</strong> Oklahoma<br />
PEER-REVIEWED<br />
RESEARCH<br />
Michael D. Martin, MD<br />
University <strong>of</strong> Oklahoma<br />
College <strong>of</strong> Medicine,<br />
Department <strong>of</strong><br />
<strong>Neurological</strong> Surgery,<br />
Oklahoma City, Okla.<br />
Christopher E. Wolfla, MD<br />
Medical College <strong>of</strong><br />
Wisconsin, Department <strong>of</strong><br />
<strong>Neurological</strong> Surgery,<br />
Milwaukee, Wis.<br />
Correspondence to:<br />
M. Martin<br />
Michael-Martin@ouhsc.edu<br />
Introduction<br />
Since July 1, 2003, all residents in U.S. training programs<br />
have been required to comply with restrictions<br />
on work hours mandated by the Accreditation<br />
Council for Graduate Medical Education. Residents<br />
may work no more than 80 hours per week averaged<br />
over a four-week period. In addition, specific<br />
restrictions apply to the number <strong>of</strong> continuous<br />
hours that “in-house” and “home call” residents<br />
may spend in the hospital. These restrictions were<br />
widely debated before their implementation, and<br />
the discussion continues today (5,9).<br />
The purpose <strong>of</strong> this study was to quantify the<br />
number <strong>of</strong> times these limits were exceeded at the<br />
University <strong>of</strong> Oklahoma neurosurgery residency program<br />
since the inception <strong>of</strong> the 80-hour workweek.<br />
The study was also designed to characterize the most<br />
common reasons and situations for violations <strong>of</strong> the<br />
work hour rules. Additionally, the impact <strong>of</strong> the new<br />
work restrictions on residents’ ability to participate in<br />
surgical cases was examined.<br />
Materials and Methods<br />
The University <strong>of</strong> Oklahoma accepts one resident per<br />
year, and the program is seven years in length. The<br />
Abstract<br />
All residents in U.S. training programs are required to comply with work hour restrictions<br />
mandated by the Accreditation Council for Graduate Medical Education. The purpose <strong>of</strong><br />
this retrospective study was to quantify the number <strong>of</strong> times this limit was exceeded since<br />
its implementation on July 1, 2003, as well as to gauge the impact <strong>of</strong> restricted work hours<br />
on operative case experience <strong>of</strong> residents. Data from the University <strong>of</strong> Oklahoma resident<br />
work hour database was analyzed and incidents <strong>of</strong> violation were characterized. Operative<br />
attendance was collected from departmental records. During the study period seven violations<br />
were recorded. Further investigation revealed that all supposed violations were<br />
attributable to errors in calculation or data entry and were not truly violations <strong>of</strong><br />
ACGME-mandated rules. Residents were available to assist in more cases the year before<br />
the work hour restrictions took effect compared to the first year after they were in place.<br />
The differences were evaluated by the chi-square test and found to be significant (p <<br />
0.0001). These results suggest that limited duty hours are feasible, albeit with a decrease in<br />
operative cases in which residents take part. The impact on patient care, continuity and<br />
training experience, however, must be studied further to determine if work hour restrictions<br />
are truly in the best interest <strong>of</strong> trainees and patients.<br />
department has six residents in the second through<br />
seventh years <strong>of</strong> the program. Four residents cover<br />
the neurosurgery service, with one on elective and<br />
one in the laboratory at any given time. During the<br />
study period the department had six attending physicians.<br />
The facility, which encompasses a children’s<br />
hospital, veterans hospital, adult hospital and a level<br />
1 trauma center, has the capacity <strong>of</strong> approximately<br />
700 beds. The junior residents take call one night in<br />
four; senior residents alternate taking backup call<br />
from home one week at a time. The resident workday<br />
is 12 hours. Following call, junior residents must<br />
leave by 10 a.m., while senior residents function on a<br />
flextime system and must subtract the number <strong>of</strong><br />
extra hours they worked from the following day’s<br />
time. In other words, a senior resident who comes in<br />
at night and operates for three hours must leave three<br />
hours early the next day.<br />
For this study, a retrospective analysis <strong>of</strong> data<br />
taken from the University <strong>of</strong> Oklahoma resident<br />
work hour database was performed. The university’s<br />
data system tracks the in-hospital hours <strong>of</strong> every<br />
resident on the campus. Hours are entered daily and<br />
averages are calculated every four weeks. When a<br />
resident is found to have exceeded 80 hours, the<br />
incident is forwarded to the program director and a<br />
written explanation must be made for the violation.<br />
The data system also tracks residents by their current<br />
rotation. Our study used this data to analyze<br />
and characterize the incidents in which a violation<br />
occurred.<br />
For the second part <strong>of</strong> the study, departmental<br />
records were re<strong>view</strong>ed to assess the availability <strong>of</strong> neurosurgical<br />
residents to participate in operative cases.<br />
The department keeps these records, and their accuracy<br />
is checked in weekly meetings with all members<br />
<strong>of</strong> the resident and attending staff and then crosschecked<br />
with the online ACGME Resident Case Log<br />
System. For the purpose <strong>of</strong> this study, bedside procedures<br />
and stereotactic radiosurgery procedures were<br />
excluded. Residents are given credit for being present<br />
for part <strong>of</strong> the case, and in our internal reporting sys-<br />
14 AANS Bulletin • www.AANS.org
tem only one resident may be credited for each case.<br />
There is no system in place for measuring the number<br />
<strong>of</strong> cases residents had to leave before completion<br />
due to work hour restrictions or other commitments.<br />
Results<br />
During the period from July 1, 2003, to June 28, 2004,<br />
seven violations were reported by the University <strong>of</strong><br />
Oklahoma resident duty hour database. In two<br />
instances, residents had entered the wrong information.<br />
Four instances were termed “frame <strong>of</strong> reference”<br />
violations. Examination revealed that these<br />
incidents did not violate ACGME or university rules,<br />
but were in fact related to which four-week period<br />
(or “frame”) the program chose to recognize. The<br />
other violation involved switching from at-home call<br />
to in-house call and confusion about the hour calculation<br />
in these different situations.<br />
We calculated that junior residents averaged 71.2<br />
hours per week while on the neurosurgery service,<br />
52.1 hours per week during the research year, and<br />
58.2 hours per week while on electives. Senior residents<br />
averaged 66.8 hours per week, excluding call<br />
taken from home.<br />
From July 2002 through June 2003, 1,601 major<br />
operative procedures were performed in the neurosurgery<br />
department (Table 1). Residents were unable<br />
to assist with 146 <strong>of</strong> these cases, or 9.1 percent. Each<br />
resident performed an average <strong>of</strong> 242.5 cases. From<br />
July 2003 through June 2004, 1,517 major operative<br />
procedures were performed in the neurosurgery<br />
department. The department performed fewer operations<br />
during the second year <strong>of</strong> the study<br />
(2003–2004) in part due to the departure <strong>of</strong> one<br />
attending neurosurgeon near the end <strong>of</strong> the study<br />
period. Residents were unable to be present for 240<br />
cases, or 15.8 percent. Each resident covered an average<br />
<strong>of</strong> 212.8 cases. The difference was evaluated by chisquare<br />
test and found to be significant (p < 0.0001).<br />
We then analyzed the operative experience <strong>of</strong><br />
chief residents (Figure 1). During the year before the<br />
study, chief residents performed 90.2 percent <strong>of</strong> all<br />
operations at which a resident was present, or 81.9<br />
percent <strong>of</strong> the caseload <strong>of</strong> the entire service. In the<br />
year after work hour restrictions were implemented,<br />
however, the chiefs performed only 81.5 percent <strong>of</strong> the<br />
cases that had a resident present, or 68.6 percent <strong>of</strong> the<br />
service’s overall caseload. This data was evaluated via<br />
chi-square testing, and a significant decline was shown<br />
in chief resident operative experience for both percent<br />
TABLE 1<br />
Resident Operative Cases Before and After ACGME<br />
Resident Work Hour Restrictions<br />
2002-2003 2003-2004<br />
Total Cases 1,601 1,517<br />
Cases Covered by Residents 1,455 1,277<br />
Cases Not Covered by Residents 146 240<br />
Junior Resident Cases 143 236<br />
Chief Resident Cases 1,312 1,041<br />
<strong>of</strong> resident-covered cases and percent <strong>of</strong> all cases they<br />
performed (p < 0.0001 in both analyses).<br />
Discussion<br />
Resident work hour restrictions have forced training<br />
programs to monitor the hours <strong>of</strong> their trainees.<br />
Prior investigations have yielded mixed re<strong>view</strong>s <strong>of</strong><br />
the restrictions and their impact on surgical training.<br />
Studies have shown that program directors, practicing<br />
surgeons and senior residents do not generally<br />
believe that training has improved as a result <strong>of</strong> the<br />
limited work hours (4,10,12–14). Evidence suggests<br />
that, on the whole, current surgical trainees believe<br />
that work hour reductions have improved their quality<br />
<strong>of</strong> life (3). In one study <strong>of</strong> otolaryngology program<br />
directors, 45 percent <strong>of</strong> respondents felt that<br />
the restrictions had resulted in increased faculty<br />
workload (8). Still another study showed that signs <strong>of</strong><br />
“burnout” were unaffected by the decreased work<br />
hours (6). Some programs have reported difficulty in<br />
maintaining the new work hour limits due to factors<br />
such as level 1 trauma status (4) and activities<br />
deemed to be “noneducational” (2).<br />
In general, neurosurgery residents and program<br />
directors have reported that ACMGE guidelines have<br />
had a negative impact on training and continuity <strong>of</strong><br />
care (4). On the other hand, in some studies more<br />
residents have reported an improved quality <strong>of</strong> life<br />
without a negative impact on training (7). Two<br />
reports that evaluated general surgery programs<br />
showed that for their specialty the number <strong>of</strong> cases<br />
preformed by chief residents was unaffected by the<br />
work hour restrictions (11,1).<br />
Our study is limited in that the data obtained is<br />
from only one institution and only covers a two-year<br />
period. The aforementioned lack <strong>of</strong> surveillance <strong>of</strong><br />
residents who must leave cases early is another<br />
Continued on page 16<br />
Received: Sept. 16, 2005<br />
Accepted: Oct. 10, 2005<br />
AANS Bulletin<br />
14:14–16, 2005<br />
Key Words:<br />
resident duty hours,<br />
neurosurgical residency,<br />
neurosurgical training<br />
Abbreviations:<br />
ACGME, Accreditation<br />
Council for Graduate<br />
Medical Education<br />
Volume 14, Number 4 • AANS Bulletin 15
On The Cover: Time Tells<br />
FIGURE 1<br />
Chief Resident Operative Cases Before and After ACGME Resident<br />
Work Hour Restrictions<br />
Percent <strong>of</strong><br />
“Resident<br />
Present” Cases<br />
Covered by<br />
Chief Resident<br />
90.2%<br />
2002-2003<br />
Total No. Chief Resident Cases: 1,312<br />
81.5%<br />
2003-2004<br />
Total No. Chief Resident Cases: 1,041<br />
before the critical portion <strong>of</strong> the operation was<br />
accomplished. At this time the long-term effects <strong>of</strong><br />
decreased operative exposure are not known.<br />
Clearly more research must be done, especially<br />
regarding the impact that the work hour restrictions<br />
will have on those currently in neurosurgical training.<br />
The restricted hours simply have not been in<br />
place long enough for their impact on lengthy training<br />
programs such as neurosurgery’s to be fully realized.<br />
While it is apparent that many in our field do<br />
not agree with these rules, it is imperative that further<br />
study be carried out to ensure that trainees graduating<br />
from neurosurgical residency are equipped to<br />
operate in this most challenging specialty. 3<br />
Percent <strong>of</strong><br />
Total Cases<br />
Covered by 81.9%<br />
68.6%<br />
Chief<br />
Resident<br />
2002-2003<br />
Total No. Chief Resident Cases: 1,312<br />
2003-2004<br />
Total No. Chief Resident Cases: 1,041<br />
Continued from page 15<br />
potential piece <strong>of</strong> information that would make the<br />
data more robust. We also have made no attempt to<br />
determine whether the personal preferences <strong>of</strong> the<br />
chief residents for certain cases over others may have<br />
falsely elevated or decreased their numbers. Also,<br />
although every measure was taken to ensure accurate<br />
recording, no guarantee can be made that the systems<br />
used for recording data are without flaws.<br />
Conclusions<br />
This study examined the feasibility <strong>of</strong> working within<br />
the ACGME-mandated guidelines and the effect<br />
that the presumably reduced time at work had on<br />
resident surgical exposure. The results clearly show<br />
that even in a one-resident-per-year program covering<br />
four hospitals, compliance can be achieved. This<br />
compliance, however, was not achieved without significant<br />
changes to the resident operative experience.<br />
The percentage <strong>of</strong> cases not covered by residents<br />
increased, and further examination revealed that the<br />
operative experience <strong>of</strong> the chief residents dropped<br />
significantly. These numbers are conservative estimates.<br />
No account can be made for residents who<br />
may have had to leave the case before completion or<br />
REFERENCES<br />
1. Bland KI, Stoll DA, Richardson JD, Britt LD: Brief communication<br />
<strong>of</strong> the Residency Re<strong>view</strong> Committee-Surgery (RRC-S) on<br />
residents’ surgical volume in general surgery. Am J Surg<br />
190(3):345–350, 2005<br />
2. Brasel KJ, Pierre AL, Weigelt JA: Resident work hours: what they<br />
are really doing. Arch Surg 139(5):490–493; discussion 493–494,<br />
2004<br />
3. Breen E, Irani JL, Mello MM, Whang EE, Zinner MJ, Ashley SW:<br />
The future <strong>of</strong> surgery: today’s residents speak. Curr Surg<br />
62(5):543–546, 2005<br />
4. Cohen-Gadol AA, Piepgras DG, Krishnamurthy S, Fessler RD:<br />
Resident duty hours reform: results <strong>of</strong> a national survey <strong>of</strong> the<br />
program directors and residents in neurosurgery training programs.<br />
Neurosurgery 56(2):398–403; discussion 398–403, 2005<br />
5. Friedman WA: Resident duty hours in <strong>American</strong> neurosurgery.<br />
Neurosurgery 54(4):925–931; discussion 931–933, 2004<br />
6. Gelfand DV, Podnos YD, Carmichael JC, Saltzman DJ, Wilson<br />
SE, Williams RA: Effect <strong>of</strong> the 80-hour workweek on resident<br />
burnout. Arch Surg 139(9):933–938; discussion 938–944, 2004<br />
7. Irani JL, Mello MM, Ashley SW, Whang EE, Zinner MJ, Breen E:<br />
Surgical residents’ perceptions <strong>of</strong> the effects <strong>of</strong> the ACGME duty<br />
hour requirements 1 year after implementation. Surgery<br />
138(2):246–253, 2005<br />
8. Kupferman TA, Lian TS: Implementation <strong>of</strong> duty hour standards<br />
in otolaryngology-head and neck surgery residency training.<br />
Otolaryngol Head Neck Surg 132(6):819–822, 2005<br />
9. Lowenstein J: Where have all the giants gone Reconciling medical<br />
education and the traditions <strong>of</strong> patient care with limitations<br />
on resident work hours. Perspect Biol Med 46(2):273–282, 2003<br />
10. Reiter ER, Wong DR: Impact <strong>of</strong> duty hour limits on resident<br />
training in otolaryngology. Laryngoscope 115(5):773–779, 2005<br />
11. Spencer AU, Teitelbaum DH: Impact <strong>of</strong> work-hour restrictions<br />
on residents’ operative volume on a subspecialty surgical service.<br />
J Am Coll Surg 200(5):670–676, 2005<br />
12. Underwood W, Boyd AJ, Fletcher KE, Lypson ML: Viewpoints<br />
from generation X: a survey <strong>of</strong> candidate and associate <strong>view</strong>points<br />
on resident duty-hour regulations. J Am Coll Surg<br />
198(6):989–993, 2004<br />
13. Whang EE, Mello MM, Ashley SW, Zinner MJ: Implementing<br />
resident work hour limitations: lessons from the New York State<br />
experience. Ann Surg 237(4):449–455, 2003<br />
14. Whang EE, Perez A, Ito H, Mello MM, Ashley SW, Zinner MJ:<br />
Work hours reform: perceptions and desires <strong>of</strong> contemporary<br />
surgical residents. J Am Coll Surg 197(4):624–630, 2003<br />
16 AANS Bulletin • www.AANS.org
Work Hour Restrictions: Impact on<br />
Neurosurgical Resident Training at<br />
the University <strong>of</strong> Utah<br />
PEER-REVIEWED<br />
RESEARCH<br />
Introduction<br />
In April 2001, the Committee <strong>of</strong> Interns and Residents,<br />
the <strong>American</strong> Medical Student <strong>Association</strong>,<br />
and Public Citizen sent a petition to the Occupational<br />
Safety and Health Administration requesting<br />
restrictions on resident work hours for all medical<br />
specialties (4,9). As a result, Rep. John Conyers Jr., D-<br />
Mich., and Sen. Jon Corzine, D-N.J., introduced the<br />
Patient and Physician Safety and Protection Act in the<br />
107th Congress (H.R. 3236 and S. 2614) (5,6).<br />
Around the same time, the Accreditation Council for<br />
Graduate Medical Education developed its own<br />
nationwide guidelines that as <strong>of</strong> July 1, 2003, restricted<br />
resident duty hours to 80 averaged over four weeks.<br />
Arguably, <strong>of</strong> all surgical residencies, these work<br />
hour limitations have hit neurosurgical residencies<br />
the hardest. Unlike many other busy medical and<br />
surgical residencies, neurosurgical residencies usually<br />
have only one, and occasionally two or three, residents<br />
per class. The neurosurgical service at a major<br />
hospital <strong>of</strong>ten has a patient census and operative<br />
schedule that is as busy as any surgical service. The<br />
impact <strong>of</strong> the ACGME work hour restrictions on<br />
neurosurgical residencies is sure to be significant.<br />
More than two years after the work hour restrictions<br />
were mandated, little objective information is<br />
available regarding their impact on the surgical<br />
experience and education <strong>of</strong> neurosurgical residents.<br />
Many recent reports in the literature that discuss<br />
perceived effects <strong>of</strong> the 80-hour workweek<br />
reflect the experience <strong>of</strong> general surgery. Most <strong>of</strong><br />
these reports are based on surveys and discuss quality<br />
<strong>of</strong> life, continuity-<strong>of</strong>-care issues, and whether or<br />
not the rules are beneficial to surgical training<br />
(1,2,8,9). Cohen-Gadol et al. recently performed a<br />
survey <strong>of</strong> residents and program directors in neurosurgery<br />
training programs that evaluated the perceived<br />
impact <strong>of</strong> the ACGME regulations (4), but<br />
objective data that assess the effect <strong>of</strong> these regulations<br />
is scarce in the neurosurgical literature.<br />
The University <strong>of</strong> Utah neurosurgery service has<br />
been compliant with the ACGME workweek rules<br />
beginning with the 2003–2004 academic year. We<br />
re<strong>view</strong>ed the impact <strong>of</strong> the work hour restrictions on<br />
the surgical experience at the junior and senior neurosurgical<br />
resident levels.<br />
Continued on page 18<br />
Todd D. McCall, MD,<br />
Ganesh Rao, MD, and<br />
John R.W. Kestle, MD<br />
Department <strong>of</strong><br />
Neurosurgery,<br />
University <strong>of</strong> Utah and<br />
Primary Children’s<br />
Medical Center,<br />
Salt Lake City, Utah<br />
Correspondence to:<br />
J. Kestle<br />
john.kestle@hsc.utah.edu<br />
Received: Nov. 2, 2005<br />
Accepted: Nov. 14, 2005<br />
AANS Bulletin<br />
14:17–22, 2005<br />
Abstract<br />
Resident work hour restrictions imposed by the<br />
Accreditation Council for Graduate Medical Education<br />
became effective on July 1, 2003. To evaluate the effect <strong>of</strong><br />
these regulations on resident operative experience, we<br />
re<strong>view</strong>ed and compared the surgical experience <strong>of</strong><br />
junior and senior neurosurgical residents four years<br />
before and one year after the ACGME restrictions were<br />
implemented. Resident work hours since May 2003 and<br />
operative caseload during the study period were recorded<br />
in commercially available data systems. The mean<br />
number <strong>of</strong> hours worked per week by junior and chief<br />
residents decreased from 104 and 110 hours before the<br />
ACGME work hour restrictions to 81 and 84 hours<br />
afterward, respectively. During the four academic years<br />
before the work hour limitations took effect, the mean<br />
number <strong>of</strong> major cases performed each year was 802.5<br />
for the chief residents and 849.3 for the junior residents.<br />
Following the restrictions, little changed for the chief<br />
residents. However, the junior residents averaged only<br />
467 cases, a 45 percent decrease from the previous years<br />
studied. The mean number <strong>of</strong> cases covered by each<br />
junior resident per month decreased by 30.5 percent<br />
after the work hour restrictions were instituted, and the<br />
mean number <strong>of</strong> cases covered per post-call junior resident<br />
in one month declined 47.8 percent, from 23 to 12.<br />
At our institution, the ACGME work hour restrictions<br />
have resulted in decreased resident work hours for all<br />
residents at the expense <strong>of</strong> the operative experience for<br />
junior residents. The operative caseload for chief residents<br />
has not been affected.<br />
Key Words:<br />
ACGME; resident work<br />
hours<br />
Abbreviations:<br />
ACGME, Accreditation<br />
Council for Graduate<br />
Medical Education<br />
Volume 14, Number 4 • AANS Bulletin 17
On The Cover: Time Tells<br />
FIGURE 1<br />
Work Hours (May 2003-April 2004)<br />
Mean 130 No. <strong>of</strong> Resident Work Hours (May 2003–April 2004)<br />
120<br />
MEAN HOURS PER WEEK<br />
110<br />
100<br />
90<br />
80<br />
CHIEF<br />
JUNIOR<br />
ACGME<br />
70<br />
60<br />
50<br />
May Jun Jul Aug Sep Oct Nov Dec Jan Feb Mar Apr<br />
The work hours <strong>of</strong> residents were recorded beginning in May<br />
2003. The mean number <strong>of</strong> resident work hours per week is<br />
graphed on a monthly basis for both junior and chief residents<br />
over one year. The shaded background represents the maximum<br />
<strong>of</strong> 88 hours averaged over four weeks that residents can work<br />
under the new ACGME guidelines. The 88-hour maximum includes<br />
an eight-hour extension that the ACGME granted to the University<br />
<strong>of</strong> Utah neurosurgical residency program.<br />
Continued from page 17<br />
Methods<br />
Work Hours<br />
Resident work hours were recorded beginning in<br />
May 2003, before implementation <strong>of</strong> the work hour<br />
restrictions. Residents were required to report their<br />
work hours weekly using the s<strong>of</strong>tware TimeClock<br />
Plus (Data Management, Inc., San Angelo, Texas).<br />
On July 1, 2003, the ACGME work hour restrictions<br />
took effect. Briefly, these rules limit the workweek<br />
to 80 hours averaged over a four-week period<br />
and place restrictions on the number <strong>of</strong> hours a resident<br />
may work after on-call service. The University<br />
<strong>of</strong> Utah neurosurgery service was granted the<br />
optional 10 percent exception, which allowed our<br />
residents to work an 88-hour average workweek.<br />
We implemented three changes to the University<br />
<strong>of</strong> Utah neurosurgery service to comply with the<br />
new work hour regulations. First, a senior resident<br />
was moved from service at the veterans hospital to<br />
the University <strong>of</strong> Utah Hospital for coverage <strong>of</strong><br />
junior call responsibilities one day per week and<br />
chief call one weekend each month. Second, the residents<br />
on the research elective were each required to<br />
cover junior call one Friday and one Sunday per<br />
month. Third, the intern no longer took call with a<br />
junior resident and became available every weekday<br />
to help with work on the ward. No physician extenders<br />
were hired.<br />
Operative Case Load<br />
For the duration <strong>of</strong> the reported years (1999–2004),<br />
all neurosurgical operative cases at the University <strong>of</strong><br />
Utah Hospital were recorded in a FileMaker database<br />
(FileMaker Inc., Santa Clara, Calif.). The data for<br />
each case included the attending physician, assisting<br />
residents, date, and description <strong>of</strong> the case. We<br />
re<strong>view</strong>ed the caseload for chief residents and for<br />
junior residents (those in the first or second year <strong>of</strong><br />
neurosurgery residency) in each academic year<br />
18 AANS Bulletin • www.AANS.org
eginning in 1999 and ending in 2004, for a total <strong>of</strong><br />
five academic years. The number <strong>of</strong> major operative<br />
cases performed by junior and chief residents as first<br />
assistant and second assistant was totaled for each<br />
academic year. The number <strong>of</strong> major cases performed<br />
by junior residents per month was totaled.<br />
Minor procedures, as defined on the ACGME institutional<br />
data forms (biopsy, intracranial pressure<br />
monitors, halo tongs, and other), and cases done<br />
with fellows or residents on research or on neurocritical<br />
care rotations were not included. Pediatric<br />
cases, placement <strong>of</strong> lines, and neurosurgical cases<br />
managed nonoperatively were not included.<br />
Before the implementation <strong>of</strong> the work hour<br />
restrictions, the post-call day typically was considered<br />
protected operating time for the junior residents.<br />
However, the new regulations require residents<br />
to leave the hospital within six hours <strong>of</strong> the end <strong>of</strong><br />
their shift. To assess the impact <strong>of</strong> the work hour<br />
rules on the post-call day’s operative experience, we<br />
totaled the number <strong>of</strong> cases in one month (May) that<br />
were performed on the post-call days by the junior<br />
residents before and after the work rules were instituted.<br />
Additionally, to determine differences in<br />
operative experience when taking at-home and<br />
in-hospital call, the total number <strong>of</strong> junior resident<br />
cases in May at the University <strong>of</strong> Utah Hospital was<br />
compared with similar data at the Primary Children’s<br />
Medical Center, where the junior resident takes<br />
home call and therefore is not required to leave the<br />
facility following on-call service.<br />
Results<br />
Work Hours<br />
The mean number <strong>of</strong> hours junior residents and<br />
chief residents worked per week (averaged over four<br />
weeks) from May 2003 to April 2004 is summarized<br />
in Figure 1. Before July 1, 2003, junior residents<br />
averaged 104 hours per week and the chief residents<br />
averaged 110 hours per week. With the implementation<br />
<strong>of</strong> changes to conform to the work hour regulations<br />
after July 1, 2003, the number <strong>of</strong> hours<br />
worked per week decreased to below 88 hours for<br />
both junior residents (80.7 hours) and chief residents<br />
(84.2 hours).<br />
Operative Case Load<br />
The total number <strong>of</strong> major operative cases performed<br />
at the University Hospital has increased steadily over<br />
the last five years (Figure 2). There was a 26.9 percent<br />
increase in cases, from 1,123 during the 1999–2000<br />
academic year to 1,425 during the 2003–2004 academic<br />
year. During the four academic years preceding<br />
implementation <strong>of</strong> the work hour limitations, the<br />
mean number <strong>of</strong> major cases performed by the two<br />
chief residents was 802.5 per year. The mean number<br />
<strong>of</strong> major cases performed by junior residents during<br />
these same four years was 849.3, including 269.5 as<br />
the first assistant and 579.8 as the second assistant. For<br />
the academic year 2003–2004, after the work hour<br />
regulations became effective, the mean number <strong>of</strong><br />
cases performed by the chief residents was 809, but<br />
the mean number <strong>of</strong> junior resident cases during that<br />
same period was 467, including 151 as the first assistant<br />
and 316 as the second assistant. This represents a<br />
45 percent decrease in the number <strong>of</strong> cases performed<br />
by junior residents.<br />
Continued on page 20<br />
FIGURE 2<br />
Total No. <strong>of</strong> Major Operative Cases (July 1999–June 2004)<br />
TOTAL NO.<br />
Major Operative Cases (July 1999-June 2004)<br />
1600<br />
1400<br />
1200<br />
1000<br />
800<br />
600<br />
400<br />
200<br />
0<br />
TOTAL UNIV. CASES<br />
CHIEF<br />
JUNIOR<br />
99-00 00-01 01-02 02-03 03-04<br />
ACADEMIC YEAR<br />
PEER-REVIEWED<br />
RESEARCH<br />
For five consecutive academic years beginning in July 1999, the total number <strong>of</strong> major neurosurgery<br />
cases performed at the University <strong>of</strong> Utah Hospital is reported along with the<br />
number <strong>of</strong> cases with junior resident and chief resident involvement. ACGME guidelines for<br />
resident duty hours took effect at the beginning <strong>of</strong> the 2003–2004 academic year. Junior<br />
resident cases combine both first and second assistant experiences. The sum <strong>of</strong> junior resident<br />
and chief resident cases can be more than the total number <strong>of</strong> cases for a given year<br />
because two residents may be involved with a single case.<br />
Volume 14, Number 4 • AANS Bulletin 19
On The Cover: Time Tells<br />
Continued from page 19<br />
FIGURE 3<br />
Cases Covered by Junior & Chief Residents<br />
Percentage <strong>of</strong> Cases Covered by Junior and Chief Residents<br />
PERCENT OF CASES COVERED<br />
80<br />
70<br />
60<br />
50<br />
40<br />
30<br />
20<br />
10<br />
0<br />
99-00 00-01 01-02 02-03 03-04<br />
ACADEMIC YEAR<br />
CHIEF<br />
JUNIOR<br />
The percentage <strong>of</strong> total neurosurgery cases covered by junior and chief residents was calculated<br />
for each academic year to correct for the variable number <strong>of</strong> total operative cases in each year.<br />
FIGURE 4<br />
Mean No. <strong>of</strong> Operative Cases for Junior Residents in One Month<br />
Number Operative Cases for Junior Residents in One Month<br />
MEAN NO.<br />
30<br />
25<br />
20<br />
15<br />
10<br />
5<br />
0<br />
3<br />
4 5<br />
99-00 00-01 01-02 02-03 03-04<br />
ACADEMIC YEAR<br />
The mean number <strong>of</strong> operative cases for a single junior resident per month was calculated to correct<br />
for the variable number <strong>of</strong> junior residents each year. For each time point, the number <strong>of</strong> junior<br />
residents that year is indicated. In the 2003–2004 academic year the number <strong>of</strong> junior residents<br />
decreased by 50 percent from the previous year. Therefore, even though there were more total<br />
operative cases on the university service per junior resident, the number <strong>of</strong> cases per month that<br />
junior residents operated still declined.<br />
6<br />
3<br />
Both the number <strong>of</strong> operative cases and the number<br />
<strong>of</strong> junior residents varied in each academic year<br />
studied. To correct for the variable number <strong>of</strong> operative<br />
cases in each year, the percentage <strong>of</strong> total neurosurgery<br />
cases covered by junior residents and chief<br />
residents was calculated for each academic year (Figure<br />
3). There was a 52.5 percent decline in the percentage<br />
<strong>of</strong> total neurosurgery cases at the University<br />
<strong>of</strong> Utah Hospital with junior resident involvement.<br />
To correct for the variable number <strong>of</strong> junior residents<br />
each year, the mean number <strong>of</strong> cases per junior resident<br />
per month was calculated (Figure 4). During the<br />
2003–2004 academic year, each junior resident was<br />
involved in an average <strong>of</strong> 18 cases per month, which<br />
represents a 30.5 percent decline from the previous<br />
four academic years, when each junior resident averaged<br />
involvement in 25.9 cases per month.<br />
To evaluate the impact <strong>of</strong> the work hour restrictions<br />
on the post-call operative experience <strong>of</strong> junior<br />
residents, operative data for May 2003 was compared<br />
with data for May 2004. The number <strong>of</strong> cases covered<br />
per post-call junior resident declined from 23 before<br />
the restrictions to 12 after they were instituted (Figure<br />
5). At University Hospital the total number <strong>of</strong><br />
cases performed by all post-call junior residents<br />
declined from 50 before the restrictions to 25 after the<br />
restrictions, compared with a decline from 42 to 36<br />
cases at Primary Children’s Medical Center (Figure 6).<br />
Discussion<br />
Several studies have evaluated the attitudes <strong>of</strong> both<br />
resident and attending general surgeons toward the<br />
work hour limitation (1,2,8-10). Not surprisingly, the<br />
attitudes toward the new rules have been mixed.<br />
Many studies have shown that senior residents and<br />
faculty <strong>view</strong> these new rules as having a negative<br />
impact on surgical training, whereas junior residents<br />
tend to <strong>view</strong> them favorably. However, these studies<br />
do not objectively address the impact that the<br />
restricted work hours have on the technical aspects <strong>of</strong><br />
training a surgeon. The authors <strong>of</strong> one survey-based<br />
study reported that among surgical residents, 44 percent<br />
believed that the work hour restrictions would<br />
negatively impact the surgical experience (1). This<br />
same study showed that the number <strong>of</strong> cases performed<br />
by graduating chief residents actually<br />
increased after the work hour restrictions were in<br />
place. More recently, Cohen-Gadol et al. reported<br />
that the majority <strong>of</strong> residents (61 percent) and program<br />
directors (79 percent) believed that the<br />
20 AANS Bulletin • www.AANS.org
FIGURE 5<br />
No. <strong>of</strong><br />
Operative<br />
Operative<br />
Cases<br />
Cases Covered<br />
Covered<br />
per<br />
by Post-call<br />
Post-Call Junior Junior Residents Resident in In One One Month Month<br />
TOTAL NO.<br />
25<br />
20<br />
15<br />
10<br />
5<br />
0<br />
02-03 03-04<br />
ACADEMIC YEAR<br />
The total number <strong>of</strong> operative cases performed by post-call<br />
junior residents during one month was tallied for the<br />
academic years before (2002–2003) and after (2003–2004)<br />
the ACGME guidelines became effective. There was a<br />
47.8 percent decline in junior residents’ operative experience<br />
after implementation <strong>of</strong> the work hour restrictions.<br />
experience. Residents at the junior levels are those<br />
who take in-hospital call, work 24-hour shifts, are<br />
primarily responsible for patient care, and are the<br />
target <strong>of</strong> the work hour restrictions. These are the<br />
residents who likely will lose out on operative experience.<br />
Our study shows that, indeed, residents at the<br />
junior levels suffer a decrease in operative experience.<br />
Since the implementation <strong>of</strong> the restrictions on<br />
work hours, at our institution the number <strong>of</strong> cases<br />
with junior resident involvement has declined by 45<br />
percent, and the percentage <strong>of</strong> cases covered by<br />
junior residents declined by 52.5 percent. The<br />
absolute number <strong>of</strong> cases performed by junior residents<br />
can be influenced by several factors, such as<br />
the total number <strong>of</strong> available operative cases and<br />
the number <strong>of</strong> junior residents. At our institution,<br />
the total number <strong>of</strong> operative cases has increased<br />
26.9 percent in the past five years, suggesting that<br />
without the new ACGME regulations, the operative<br />
volume <strong>of</strong> the junior residents would have<br />
increased. We corrected for the varying number <strong>of</strong><br />
junior residents each year by calculating the mean<br />
number <strong>of</strong> operative cases for a single junior resident<br />
per month. In the four years before the<br />
ACGME regulations were implemented, each junior<br />
resident averaged 25.9 cases per month and the year<br />
after, 18 cases per month, a 30.5 percent decline.<br />
Therefore, we believe that the decline in the number<br />
<strong>of</strong> cases performed by junior residents in the<br />
2003–2004 academic year most likely is explained<br />
by the ACGME work restrictions.<br />
To be compliant, programs have had to make<br />
drastic changes in the way their resident staff is used.<br />
These changes have included the addition <strong>of</strong> physician<br />
extenders, such as nurse practitioners or<br />
physician assistants, as well as drawing residents from<br />
the previously protected research rotations into the<br />
clinical service (3).<br />
We did not employ physician extenders at our<br />
institution during the period <strong>of</strong> this study. Instead,<br />
residents on their research year took additional<br />
junior call, and a senior resident from the veterans<br />
hospital was added to the University <strong>of</strong> Utah service.<br />
As a result, the added senior resident was able<br />
to provide operative coverage that was lost when<br />
junior residents began going home following their<br />
on-call service. The post-call operative experience<br />
that had been significant at our program for junior<br />
residents decreased 47.8 percent after we became<br />
ACGME guidelines have had a detrimental effect on<br />
their training programs (4).<br />
No study to date has examined the impact <strong>of</strong> the<br />
ACGME regulations on the junior resident operative compliant with the new ACGME guidelines. At Pri<br />
. . . . . .<br />
mary Children’s Medical Center, where the junior<br />
resident takes home call and therefore does not<br />
leave the facility after on-call service, total junior<br />
resident operative cases for one month only<br />
declined 14.3 percent after the new work hour<br />
restrictions were implemented compared with a 50<br />
percent decline at the University <strong>of</strong> Utah Hospital<br />
service. Chief residents generally are not affected by<br />
the post-call restrictions, and therefore their operative<br />
caseload has not diminished.<br />
We considered a number <strong>of</strong> strategies for<br />
improving the operative experience <strong>of</strong> our junior<br />
residents. In one study, 22 percent <strong>of</strong> resident work<br />
hours were unrelated to educational activities (2).<br />
We therefore hired a physician assistant to perform<br />
noneducational duties, freeing the junior residents<br />
for the operating room. Since this change, the<br />
monthly operative caseload for the junior residents<br />
Continued on page 22<br />
PEER-REVIEWED<br />
RESEARCH<br />
Volume 14, Number 4 • AANS Bulletin 21
On The Cover: Time Tells<br />
FIGURE 6<br />
Operative Cases for Junior<br />
Total No. <strong>of</strong> Operative Cases in One Month<br />
Residents in One Month<br />
for Junior Residents<br />
TOTAL NO.<br />
60<br />
50<br />
40<br />
30<br />
20<br />
10<br />
0<br />
Primary Children’s<br />
Medical Center<br />
Univ. <strong>of</strong> Utah Hospital<br />
02-03 03-04<br />
ACADEMIC YEAR<br />
The total number <strong>of</strong> operative cases performed by all post-call<br />
junior residents during one month at Primary Children’s Medical<br />
Center was compared with the number at the University <strong>of</strong> Utah<br />
Hospital for the academic years before (2002–2003) and after<br />
(2003–2004) the ACGME guidelines became effective.<br />
Continued from page 21<br />
cover junior duties and allowing the junior residents<br />
to operate on less complicated cases.<br />
CHIEF<br />
Conclusions<br />
JUNIOR<br />
The ACGME restrictions on resident work hours<br />
represent a paradigm shift in the education <strong>of</strong> surgical<br />
residents in the United States. These new restrictions<br />
are likely to affect several issues, including<br />
patient care, resident training, resident health, and<br />
resident quality <strong>of</strong> life. This study addresses one<br />
aspect <strong>of</strong> resident training: the operative experience.<br />
At our institution, we have managed to comply with<br />
the 80-hour workweek at the expense <strong>of</strong> the operative<br />
experience <strong>of</strong> the junior residents. Any analysis <strong>of</strong><br />
the ACGME work hour restrictions will need to consider<br />
the impact <strong>of</strong> these regulations on several different<br />
aspects <strong>of</strong> resident training, such as number <strong>of</strong><br />
publications, board scores, and serial faculty evaluations,<br />
as well as on patient care. As additional objective<br />
data become available for assessing the impact <strong>of</strong><br />
the ACGME regulations, residency programs will<br />
need to be able to develop strategies to optimize the<br />
residents’ learning experience while maintaining<br />
high standards <strong>of</strong> patient safety. 3<br />
has increased to 21 per month. Less desirable<br />
options, which we have not implemented, include ACKNOWLEDGMENTS<br />
increasing the length <strong>of</strong> residency, decreasing the The authors thank Kristin Kraus for her assistance in preparing<br />
research training period, or having chief residents this manuscript for submission and publication.<br />
. . . . . .<br />
REFERENCES<br />
1. Barden CB, Specht MC, McCarter MD, Daly JM, Fahey TJ 3rd:<br />
Effects <strong>of</strong> limited work hours on surgical training. J Am Coll<br />
Surg 195(4):531–538, 2002<br />
2. Brasel KJ, Pierre AL, Weigelt JA: Resident work hours: what they<br />
are really doing. Arch Surg 139(5):490-493; discussion 493–494,<br />
2004<br />
3. Chandra RK: The resident 80-hour work week: how has it<br />
affected surgical specialties Laryngoscope 114(8):1394–1398;<br />
discussion 1319, 2004<br />
4. Cohen-Gadol AA, Piepgras DG, Krishnamurthy S, Fessler RD:<br />
Resident duty hour reform: results <strong>of</strong> a national survey <strong>of</strong> the<br />
program directors and residents in neurosurgery training programs.<br />
Neurosurgery 56(2):398–402, 2005<br />
5. Conyers JR: Patient and Physician Safety and Protection Act <strong>of</strong><br />
2001. H.R. 3236, 2001<br />
6. Corzine JS: Patient and Physician Safety and Protection Act <strong>of</strong><br />
2002. S. 2614, 2002<br />
7. Friedman WA: Resident duty hours in <strong>American</strong> neurosurgery.<br />
Neurosurgery 54(4):925–931; discussion 931–933, 2004<br />
8. Niederee MJ, Knudtson JL, Byrnes MC, Helmer SD, Smith RS: A<br />
survey <strong>of</strong> residents and faculty regarding work hour limitations<br />
in surgical training programs. Arch Surg 138(6):663-669; discussion<br />
669–671, 2003<br />
9. Underwood W, Boyd AJ, Fletcher KE, Lypson ML: Viewpoints<br />
from generation X: a survey <strong>of</strong> candidate and associate <strong>view</strong>points<br />
on resident duty-hour regulations. J Am Coll Surg<br />
198(6):989–993, 2004<br />
10. Whang EE, Perez A, Ito H, Mello MM, Ashley SW, Zinner MJ:<br />
Work hours reform: perceptions and desires <strong>of</strong> contemporary<br />
surgical residents. J Am Coll Surg 197(4):624–630, 2003<br />
22 AANS Bulletin • www.AANS.org
Restrictions Get Reality Check<br />
Assessing the Past, Present and Future <strong>of</strong> Resident<br />
Work Hour Restrictions<br />
PERSPECTIVE<br />
DEBORAH L. BENZIL,MD<br />
Listening to colleagues across the country discuss<br />
their perceptions <strong>of</strong> the post-July 2003 environment,<br />
I hear hauntingly familiar refrains, the same ones that<br />
echoed throughout New York more than 10 years ago<br />
when the state began to enforce its own resident work<br />
hour restrictions. Because academicians, including<br />
neurosurgeons, learned little from the New York<br />
experience, many will be doomed to repeat the failures<br />
<strong>of</strong> others, perhaps at the expense <strong>of</strong> resident satisfaction,<br />
faculty attrition, and sadly, quality <strong>of</strong> care<br />
for our patients.<br />
Perhaps the most common refrain is that the new<br />
resident work hour restrictions, which were mandated<br />
nationally by the Accreditation Council for Graduate<br />
Medical Education, will debase the pr<strong>of</strong>ession <strong>of</strong><br />
medicine resulting in a “shift-worker mentality”<br />
attended by failure to commit to the best care for our<br />
patients. Anecdotes abound <strong>of</strong> residents leaving in the<br />
middle <strong>of</strong> cardiac arrest codes, showing up late for<br />
rounds because they were entitled to their required<br />
time <strong>of</strong>f, and similar behaviors. But these remain<br />
anecdotes, less valid scientifically than case reports,<br />
and the new reality has yet to be assessed.<br />
It is likely that the full impact <strong>of</strong> the ACGME resident<br />
work hour restrictions will not be understood<br />
for a generation, when the residents training under<br />
this new system gain seniority and assume roles as<br />
program directors and chairs <strong>of</strong> departments. At this<br />
time, two years into national implementation <strong>of</strong> the<br />
80-hour resident workweek, a brief look at the history<br />
<strong>of</strong> this reform and at how the future success or failure<br />
<strong>of</strong> this change will be assessed may be instructive.<br />
Into the Past<br />
Resident work hour restrictions, arguably medical<br />
education’s most sweeping reform in this century,<br />
evolved following the death <strong>of</strong> Libby Zion at a New<br />
York Hospital in March 1984. A junior resident<br />
admitted her with fever, chills and dehydration; by the<br />
next morning, she had died. While the exact cause <strong>of</strong><br />
her death has never been determined, a New York<br />
grand jury investigation in 1986 found that the death<br />
was related to 36-hour<br />
sleepless resident shifts<br />
and inadequate supervision<br />
by attending<br />
physicians.<br />
Sidney Zion, Libby<br />
Zion’s father and also a<br />
newspaper columnist<br />
and attorney, sued New<br />
York Hospital and the<br />
physicians for malpractice.<br />
More than the<br />
malpractice case, he<br />
began a crusade against the system, targeting the long<br />
resident work hours and poor supervision that he felt<br />
had contributed to his daughter’s wrongful death.<br />
The publicity surrounding this case led the New<br />
York Health Commissioner in 1987 to form an ad hoc<br />
advisory committee chaired by Bertrand Bell, a pr<strong>of</strong>essor<br />
<strong>of</strong> medicine at Albert Einstein College <strong>of</strong> Medicine.<br />
The committee’s strong recommendation to<br />
restrict resident work hours led to New York State<br />
health code legislation enacted July 1, 1989, commonly<br />
known as the 405 Regulations. Sidney Zion,<br />
however, continued to campaign, claiming that many<br />
hospitals were wantonly ignoring the code. In 1998,<br />
stiff hospital penalties were added. Initial violations<br />
could be fined up to $6,000 per violation with followup<br />
violations escalating to $25,000 and then $50,000.<br />
While New York hospitals were struggling with the<br />
405 Regulations, the push to implement national<br />
work hour restrictions began. In 2002 the ACGME<br />
announced its intention to impose national duty<br />
hour regulations effective July 1, 2003.<br />
A Look at the Present<br />
Assessment <strong>of</strong> the effect <strong>of</strong> the 80-hour resident<br />
workweek within much <strong>of</strong> surgery has emphasized<br />
the loss <strong>of</strong> surgical case volume and the dilution <strong>of</strong> the<br />
surgical training experience (3,11,13). The two studies<br />
published in this issue <strong>of</strong> the AANS Bulletin<br />
demonstrate the reduced number <strong>of</strong> cases in which<br />
Continued on page 24<br />
Volume 14, Number 4 • AANS Bulletin 23
On The Cover: Time Tells<br />
Continued from page 23<br />
neurosurgical residents are participating following<br />
implementation <strong>of</strong> the work hour restrictions. Unfortunately,<br />
little is known about how many procedures<br />
a resident must do to achieve competence or to attain<br />
the necessary balance <strong>of</strong> didactics, patient care, and<br />
technical training. Clearly individual residents follow<br />
very different learning curves. Surgical simulators,<br />
which increasingly are being used for both training<br />
and assessment <strong>of</strong> technical skills (6,7,9,15), may at<br />
least partially fill the gap in operative experience<br />
opened by the restrictions and also provide additional<br />
exposure to particular techniques. Some have even<br />
suggested applying the model <strong>of</strong> flight training to resident<br />
education, requiring residents to have simulation<br />
experience before they are awarded any patient<br />
responsibility (12).<br />
While volume <strong>of</strong> surgical cases always will be an<br />
important factor in technical training, many other<br />
factors may also be crucial to achieving technical<br />
pr<strong>of</strong>iciency. At the same time, fatigue, the technical<br />
and supervisory skill <strong>of</strong> the attending surgeon and<br />
the resident’s own preparation all may affect the<br />
ability to learn surgical technique. Increasing evidence<br />
has emerged about the effect <strong>of</strong> fatigue on<br />
medical errors (4,16), resident safety (1), and resident<br />
burnout (14). The impact <strong>of</strong> this research on<br />
the public is far greater than the multitude <strong>of</strong> more<br />
descriptive studies on attitudes and perceptions. To<br />
date, few studies have even tried to assess the impact<br />
<strong>of</strong> resident work hour restrictions on quality <strong>of</strong><br />
patient care (2). Several studies have raised the concern<br />
<strong>of</strong> continuity <strong>of</strong> care but without clear evidence<br />
that it has been compromised by the<br />
restrictions (10,17). Just one study has addressed<br />
the issue <strong>of</strong> patient satisfaction and physician<br />
fatigue, finding that rested residents received consistently<br />
higher ratings from patients (8).<br />
Attention also has been given to resident attitudes<br />
and the increasing time and responsibility on attending<br />
physicians (5,14,20). At least one study failed to<br />
document increased faculty hours (19). Most studies<br />
<strong>of</strong> resident attitudes and perceptions are most notable<br />
for the differences expressed by senior and junior residents,<br />
with junior residents generally more likely to<br />
<strong>view</strong> the 80-hour workweek positively (10,17,18).<br />
This may be a reflection <strong>of</strong> the longer hours junior<br />
residents typically work or <strong>of</strong> a wider acceptance <strong>of</strong><br />
the new paradigm <strong>of</strong> training permeating medical<br />
schools. This dichotomy <strong>of</strong> attitudes supports the idea<br />
that assessing the full impact <strong>of</strong> these changes may<br />
take many years, perhaps a “training generation.”<br />
A Note on Cost<br />
To date, little public consideration has been given to<br />
the cost <strong>of</strong> this mandate. When penalties were instituted<br />
for violation <strong>of</strong> New York’s 405 Regulations,<br />
the state provided significant funding to hospitals to<br />
balance the new costs. Unfortunately, over time<br />
these added monies were withdrawn, though the<br />
higher costs remain in place and new funding was<br />
not appropriated with the institution <strong>of</strong> the national<br />
ACGME regulations.<br />
At my own institution, three full-time nurse<br />
practitioners were hired in the neurosurgery<br />
department at a cost <strong>of</strong> $375,000 per year to cover<br />
120 hours <strong>of</strong> “lost” resident time, and conference<br />
time for neurosurgery residents declined by 25 percent.<br />
To compensate for its own loss <strong>of</strong> 120 hours <strong>of</strong><br />
resident time, the orthopedics department hired<br />
five physician extenders at an annual cost <strong>of</strong><br />
$520,000 and recalled two “away” residents to the<br />
primary institution. The hospital also hired a compliance<br />
<strong>of</strong>ficer, initially half time, then full time at a<br />
cost <strong>of</strong> $80,000 per year, as well as ancillary staff at<br />
an estimated cost <strong>of</strong> $250,000 per year. These hospital-wide<br />
costs were shared by the neurosurgery<br />
and orthopedics departments, bringing the annual<br />
cost <strong>of</strong> the work hour restrictions for just two surgical<br />
specialties at one hospital to nearly $1 million.<br />
Implementation <strong>of</strong> the work hour restrictions<br />
also has coincided with that <strong>of</strong> several other<br />
unfunded mandates: maintenance <strong>of</strong> certification,<br />
ACGME Core Competency Assessments, and the<br />
Health Insurance Portability and Accountability<br />
Act—all hitting at a time when most medical institutions<br />
have little operating surplus. While few in<br />
organized medicine argue with the concepts <strong>of</strong><br />
maintaining patient confidentiality, error reduction,<br />
provision <strong>of</strong> quality care, and developing<br />
sound resident education and evaluation, the<br />
accompanying cost makes embracing these programs<br />
more difficult. At least some <strong>of</strong> the funding<br />
for these mandates has negatively impacted physician<br />
salaries. How this will impact retention and<br />
recruitment <strong>of</strong> faculty into academic programs<br />
remains to be seen.<br />
The Prospective Reality<br />
In the future, will expectation <strong>of</strong> a more reasonable<br />
24 AANS Bulletin • www.AANS.org
workweek make entering medical school more<br />
appealing to a wider range <strong>of</strong> applicants Will traditionally<br />
time-demanding subspecialties like neurosurgery<br />
become more appealing by leveling the time<br />
component <strong>of</strong> the playing field Medical students<br />
entering new residencies in 2006 will have started<br />
medical school knowing <strong>of</strong> the 80-hour restriction.<br />
Soon after, we can more fully understand how the<br />
new landscape will be shaped.<br />
It has always been surprising to me that once<br />
neurosurgeons leave residency, they have the magical<br />
ability not only to forget the physical and mental<br />
stress <strong>of</strong> those years but to look back on them as the<br />
best years <strong>of</strong> their lives! Many who then enter academic<br />
medicine find it difficult to fathom another system<br />
that could successfully train competent neurosurgeons.<br />
However, rather than resisting the restrictions<br />
that already are in place, perhaps neurosurgery<br />
would be better served by participating in a concerted<br />
effort to assess the success or failure <strong>of</strong> this major<br />
paradigm shift on the quality <strong>of</strong> resident education<br />
and patient care. By understanding the critical factors<br />
that contribute to successful resident education and<br />
technical training, including work schedules, we will<br />
meet the goals <strong>of</strong> medical education. 3<br />
Deborah L. Benzil, MD, is associate pr<strong>of</strong>essor at New York<br />
Medical College, Valhalla, N.Y., and a neurosurgeon at<br />
Westchester Spine and Brain Surgery PLLC, Hartsdale, N.Y.<br />
Avinash Mohan, MD, a resident at New York Medical College,<br />
contributed to this article.<br />
REFERENCES<br />
1. Arnedt JT, Owens J, Crouch M, Stahl J, Carskadon MA: Neurobehavioral<br />
performance <strong>of</strong> residents after heavy night call vs.<br />
after alcohol ingestion. JAMA 294(9):1025-33, 2005<br />
2. Bailit JL, Blanchard MH: The effect <strong>of</strong> house staff working<br />
hours on the quality <strong>of</strong> obstetric and gynecologic care. Obstet<br />
Gynecol 103(4):613-6, 2004<br />
3. Blanchard MH, Amini SB, Frank TM: Impact <strong>of</strong> work hour<br />
restrictions on resident case experience in an obstetrics and<br />
gynecology residency program. Am J Obstet Gynecol<br />
191(5):1746-51, 2004<br />
4. Boult M: Patient safety. The fatigue factor. Health Serv J<br />
115(5962):34-5, 2005<br />
5. Cohen-Gadol AA, Piepgras DG, Krishnamurthy S, Fessler RD:<br />
Resident duty hours reform: results <strong>of</strong> a national survey <strong>of</strong> the<br />
program directors and residents in neurosurgery training programs.<br />
Neurosurgery 56(2):398-403; discussion 398-403, 2005<br />
6. Dupuis O, Silveira R, Zentner A, Dittmar A, Gaucherand P,<br />
Cucherat M, et al.: Birth simulator: reliability <strong>of</strong> transvaginal<br />
assessment <strong>of</strong> fetal head station as defined by the <strong>American</strong> College<br />
<strong>of</strong> Obstetricians and Gynecologists classification. Am J<br />
Obstet Gynecol 192(3):868-74, 2005<br />
7. Fichera A, Prachand V, Kives S, Levine R, Hasson H: Physical<br />
reality simulation for training <strong>of</strong> laparoscopists in the 21st century.<br />
A multispecialty, multi-institutional study. JSLS 9(2):125-9,<br />
2005<br />
8. Hoellein AR, Feddock CA, Griffith CH 3rd, Wilson JF, Barnett<br />
DR, Bass PF 3rd, Caudill ST: Are continuity clinic patients less<br />
satisfied when the resident is postcall J Gen Intern Med 19(5 Pt<br />
2):562-5, 2004<br />
9. Korndorffer JR Jr, Dunne JB, Sierra R, Stefanidis D, Touchard<br />
CL, Scott DJ: Simulator training for laparoscopic suturing using<br />
performance goals translates to the operating room. J Am Coll<br />
Surg 201(1):23-9, 2005<br />
10. Kort KC, Pavone LA, Jensen E, Haque E, Newman N, Kittur D: Resident<br />
perceptions <strong>of</strong> the impact <strong>of</strong> work-hour restrictions on health<br />
care delivery and surgical education: time for transformational<br />
change. Surgery 136(4):861-71, 2004<br />
11. McElearney ST, Saalwachter AR, Hedrick TL, Pruett TL, Sanfey HA,<br />
Sawyer RG: Effect <strong>of</strong> the 80-hour work week on cases performed by<br />
general surgery residents. Am Surg 71(7):552-5; discussion 555-6,<br />
2005<br />
12. Sexton JB, Thomas EJ, Helmreich RL: Error, stress, and teamwork in<br />
medicine and aviation: cross sectional surveys. BMJ 320(7237):745<br />
9, 2000<br />
13. Spencer AU, Teitelbaum DH: Impact <strong>of</strong> work-hour restrictions on<br />
residents’ operative volume on a subspecialty surgical service. J Am<br />
Coll Surg 200(5):670-6, 2005<br />
14. Stamp T, Termuhlen P, Miller S, Nolan D, Hutzel P, Gilchrist J, Johnson<br />
RM: Before and after resident work hour limitations: an objective<br />
assessment <strong>of</strong> the well-being <strong>of</strong> surgical residents. Curr Surg<br />
62(1):117-21, 2005<br />
15. Stefanidis D, Korndorffer JR Jr, Sierra R, Touchard C, Dunne JB,<br />
Scott DJ: Skill retention following pr<strong>of</strong>iciency-based laparoscopic<br />
simulator training. Surgery 138(2):165-70, 2005<br />
16. Veasey S, Rosen R, Barzansky B, Rosen I, Owens J: Sleep loss and<br />
fatigue in residency training: a reappraisal. JAMA 288(9):1116-24,<br />
2002<br />
17. Whang EE, Mello MM, Ashley SW, Zinner MJ: Implementing resident<br />
work hour limitations: lessons from the New York State experience.<br />
Ann Surg 237(4):449-55, 2003<br />
18. Whang EE, Perez A, Ito H, Mello MM, Ashley SW, Zinner MJ: Work<br />
hours reform: perceptions and desires <strong>of</strong> contemporary surgical residents.<br />
J Am Coll Surg 197(4):624-30, 2003<br />
19. Winslow ER, Berger L, Klingensmith ME: Has the 80-hour work<br />
week increased faculty hours Curr Surg 61(6):602-8, 2004<br />
20. Zuckerman JD, Kubiak EN, Immerman I, Dicesare P: The early<br />
effects <strong>of</strong> code 405 work rules on attitudes <strong>of</strong> orthopaedic residents<br />
and attending surgeons. J Bone Joint Surg Am 87(4):903-8, 2005<br />
Volume 14, Number 4 • AANS Bulletin 25
The PE Potential<br />
New AANS Study Shows Snapshot <strong>of</strong> Physician Extenders in Neurosurgical Practices<br />
KATHLEEN T. CRAIG<br />
Neurosurgeons recently have expressed great concern over<br />
workforce issues. While the need for neurosurgical care<br />
has increased, the supply <strong>of</strong> neurosurgeons to deliver<br />
that care has remained the same or declined, particularly<br />
in areas <strong>of</strong> the country outside urban centers and in<br />
states experiencing a medical liability crisis.<br />
“The growth <strong>of</strong> America’s population and the increasing<br />
longevity <strong>of</strong> its citizens are being met with a decreasing number <strong>of</strong><br />
neurosurgeons to provide care for them,” said AANS President Fremont<br />
P. Wirth, MD.“Recently, there has been significant discussion<br />
regarding the use <strong>of</strong> physician extenders in neurosurgery, and how<br />
they could be used to alleviate the current strain.”<br />
Physician extenders, a collective term for nurse practitioners and<br />
physician assistants, also have become increasingly important to<br />
training programs in order to help compensate for lost resident<br />
time related to work hour restrictions. Similarly, physician extenders<br />
appear to be playing an increasingly important role in the practice<br />
<strong>of</strong> neurosurgery by helping to facilitate the efficient use <strong>of</strong><br />
neurosurgeons’ time.<br />
In fall 2005 the AANS surveyed members in the Active and<br />
Active Provisional categories, specifically addressing:<br />
WHY EMPLOY PHYSICIAN EXTENDERS<br />
26.3%<br />
Other<br />
29.2%<br />
Ease demands <strong>of</strong><br />
ER coverage<br />
28.6%<br />
Satisfy resident<br />
work hours rules<br />
34.9%<br />
Help residents<br />
manage their<br />
responsibilities<br />
74.2%<br />
Increase<br />
patient volume<br />
in the <strong>of</strong>fice<br />
69.5%<br />
Assist in the OR<br />
In the 2005 AANS Physician Extender Survey, respondents who currently employ physician<br />
extenders were asked how they are using PEs, and those not currently employing<br />
PEs were asked how their practices would like to use them. Because respondents<br />
could check any option that applied, results do not sum to 100 percent.<br />
3 how members use or would like to use, physician extenders in<br />
their practices;<br />
3 which neurosurgical procedures physician extenders should be<br />
trained to perform;<br />
3 how physician extenders currently are trained in neurosurgical<br />
procedures and how members would like them to be trained in the<br />
future; and<br />
3 which educational resources the AANS currently <strong>of</strong>fers that<br />
might meet physician extender needs, and what should be developed<br />
in the future.<br />
Charles J. Hodge Jr., MD, the AANS vice president during fiscal<br />
2005 and the head <strong>of</strong> the Physician Extenders Task Force, led the<br />
survey project, which ultimately was administered by a contracted<br />
research firm. The online survey garnered 524 responses and a<br />
robust sample size <strong>of</strong> 380 or more for most questions. Therefore,<br />
researchers are 95 percent confident that results presented in the<br />
survey report have accuracy <strong>of</strong> plus-or-minus 5 percent or better,<br />
which essentially means that if the survey was implemented one<br />
hundred times, the results would be the same 95 times.<br />
The survey results are being used by the AANS Long Range<br />
Planning Committee and the AANS Physician Extenders Task Force<br />
in their planning. The first <strong>of</strong> the resulting initiatives will be<br />
launched during the 2006 AANS Annual Meeting in San Francisco.<br />
Respondent Pr<strong>of</strong>ile<br />
About half <strong>of</strong> the respondents were from private practices. Another<br />
28 percent were full-time academicians. Forty percent <strong>of</strong> respondents<br />
indicated that their practice settings were small (two-to-five<br />
neurosurgeons), and 24 percent selected medium (six-to-20 neurosurgeons<br />
and neurosurgical groups). These figures are consistent<br />
with the AANS Member Needs survey taken in 2004, and demonstrate<br />
a representative sample <strong>of</strong> membership.<br />
Use <strong>of</strong> Physician Extenders<br />
Seventy-four percent <strong>of</strong> respondents indicated that they employ<br />
physician extenders. Of these, just over half have been using physician<br />
extenders for more than five years. Another 40 percent have<br />
been using them for two-to-five years. When physicians in university<br />
settings were asked with whom extenders primarily work, 76<br />
percent responded “attendings,” and 18 percent, “residents.”<br />
The AANS also asked members if they felt their practices were<br />
26 AANS Bulletin • www.AANS.org
in need <strong>of</strong> physician extenders (regardless <strong>of</strong> whether they currently<br />
employ them). A slight majority <strong>of</strong> respondents, 53 percent,<br />
said that their practices are in need <strong>of</strong> physician extender assistance<br />
compared with 47 percent who did not.<br />
Survey respondents who currently employ physician extenders<br />
were asked how they are using PEs, and those not currently<br />
employing PEs were asked how their practices would like to use<br />
them. Respondents could check any option that applied (multiple<br />
options).<br />
Most respondents identified “hospital based patient evaluation<br />
and management” (74 percent) and “<strong>of</strong>fice patient evaluation and<br />
management” (73 percent) as among the duties for physician extenders.<br />
The selection “phone call returns/administrative duties (letters<br />
<strong>of</strong> appeals)” generated 70 percent <strong>of</strong> responses, and 64 percent<br />
selected “first assist in the operating room.”When asked specifically<br />
about which invasive procedures they would like physician extenders<br />
to perform, top choices were suturing (58 percent) and lumbar<br />
punctures (36 percent).<br />
The pie chart on page 26 illustrates reasons for employing physician<br />
extenders. As shown, most respondents selected to “increase<br />
patient volume in the <strong>of</strong>fice” (74 percent) and to “assist in the operating<br />
room” (70 percent).<br />
Long range plans under consideration<br />
include developing a physician<br />
extender curriculum for competency<br />
in neurosurgery, developing advanced<br />
curriculum for continued education,<br />
and investigating Web-based modules<br />
for a formal training program.<br />
Neurosurgical Training for Physician Extenders<br />
The majority <strong>of</strong> respondents, 81 percent, indicated that “on the job<br />
training” best describes the method <strong>of</strong> physician extenders’ neurosurgical<br />
training. Sixteen percent reported that extenders were<br />
trained in a formal training program. Only 2 percent indicated they<br />
were trained in the military. The majority <strong>of</strong> respondents (60 percent)<br />
also indicated that their physician extenders received training<br />
at a university hospital.<br />
When asked how long the neurosurgical training period was,<br />
the majority <strong>of</strong> respondents, 57 percent, indicated that their physician<br />
extenders received training for six months or less and 21 percent<br />
indicated one year.<br />
More than 77 percent <strong>of</strong> respondents reported that the establishment<br />
<strong>of</strong> formal training programs for physician extenders in neurosurgery<br />
would be useful. When asked how long this training period<br />
should be to gain competence in the tasks that neurosurgeons expect<br />
a physician extender to accomplish, over half, 52 percent, selected six<br />
months <strong>of</strong> neurosurgical training. Thirty-seven percent selected one<br />
year. The participants were equally divided on who should be paying<br />
for the training: 40 percent said the physician extender, and 40 percent<br />
said the future or current employer. About 57 percent indicated<br />
that they expect the physician extender to receive a salary while<br />
attending an extended training program in neurosurgery.<br />
Working With the AANS<br />
When asked: “which <strong>of</strong> the following AANS <strong>of</strong>ferings would best<br />
help meet the educational needs <strong>of</strong> physician extenders,” 62 percent<br />
selected “AANS annual meeting practical clinics or breakfast seminars.”<br />
Fifty-three percent <strong>of</strong> respondents selected “AANS instructional<br />
DVDs, publications or online <strong>of</strong>ferings,” and 36 percent<br />
selected the “AANS Master Series courses taught in educational/<br />
research facilities <strong>of</strong>fering lab work using cadaver material.” (Multiple<br />
selections were allowed.)<br />
“Survey participants also identified many topics and types <strong>of</strong><br />
educational experiences they would like extenders to receive from<br />
the AANS,” said Dr. Hodge. “Leadership re<strong>view</strong>ed a summary <strong>of</strong><br />
write-in recommendations.”<br />
Moving Forward<br />
With survey results in hand as well as input from the task force, the<br />
Long Range Planning Committee began to address the issue <strong>of</strong><br />
using <strong>of</strong> physician extenders as one <strong>of</strong> many solutions to workforce<br />
shortages.<br />
“Initially, training courses for physician extenders will be <strong>of</strong>fered<br />
during the 2006 AANS Annual Meeting in San Francisco,” said Dr.<br />
Hodge. “Short-range plans focus on identifying funding for additional<br />
physician extender neurosurgical training and expanding<br />
AANS <strong>of</strong>ferings for physician extenders. Long range plans under<br />
consideration include developing a physician extender curriculum<br />
for competency in neurosurgery, developing advanced curriculum<br />
for continued education, and investigating Web-based modules for<br />
a formal training program.”<br />
Addressing workforce issues has been a priority for Dr. Wirth<br />
during his presidential year.<br />
“It is clear that there is tremendous potential for physician<br />
extenders to help alleviate neurosurgical workforce shortages,” said<br />
Dr. Wirth.“We are considering all the recommendations <strong>of</strong> the task<br />
force and are working closely with nurse practitioner and physician<br />
assistant organizations to investigate which avenues will result in<br />
optimal benefit to our patients.” 3<br />
Kathleen T. Craig is AANS director <strong>of</strong> marketing.<br />
Volume 14, Number 4 • AANS Bulletin 27
P ATIENTS AFETY A RNOLD A. ZEAL, M D<br />
Error Results in Doctor’s Paradigm Shift<br />
Protocols, Team Approach and Site Marking Increase Patient Safety<br />
As a board-certified neurosurgeon in<br />
practice for nearly 30 years, I have<br />
served as chair <strong>of</strong> the neurosurgery<br />
section at a major medical center<br />
and as vice chair <strong>of</strong> the entire surgery<br />
department for a number <strong>of</strong> years. As vice<br />
chair <strong>of</strong> the surgery department, I was also<br />
chair <strong>of</strong> the department’s Quality Assurance<br />
Committee, and I additionally served<br />
as a sitting member <strong>of</strong> that committee for<br />
eight years.<br />
During my tenure in these positions, I<br />
was faced with several instances <strong>of</strong> medical<br />
errors involving colleagues, including<br />
wrong-site surgery. I listened to surgeons<br />
describe how their errors occurred and<br />
always found myself very unsympathetic. I<br />
could not imagine how conscientious surgeons<br />
could make such errors and could<br />
not, in my wildest dreams, imagine it happening<br />
to me. I am one <strong>of</strong> those compulsive<br />
surgeons who checks, double-checks, and<br />
even sometimes triple-checks things during<br />
surgery to the extent that my partner and<br />
operating room staff <strong>of</strong>ten tease me about<br />
being so obsessive-compulsive.<br />
Then it happened to me. I learned that<br />
we all make mistakes. It is easy. We are<br />
human. In fact, when I was forced to<br />
re<strong>view</strong> the literature to produce a lecture<br />
on this topic, I discovered that the numbers<br />
<strong>of</strong> medical errors and wrong-site<br />
surgeries and the injuries they cause are<br />
unbelievable.<br />
I became a convert, and in 2003 I was<br />
one <strong>of</strong> the surgeons and other health pr<strong>of</strong>essionals<br />
and organizations standing with<br />
the Joint Commission on Accreditation <strong>of</strong><br />
Healthcare Organizations strongly advocating<br />
and promoting the Universal Protocol<br />
for Preventing Wrong Site, Wrong Procedure,<br />
Wrong Person Surgery. The following<br />
account describes how I came to be there<br />
and what I learned along the way.<br />
Anatomy <strong>of</strong> a Medical Mistake<br />
In December 2000, a former partner <strong>of</strong><br />
mine referred his best friend to me for<br />
treatment <strong>of</strong> an L3–4 disc herniation. The<br />
patient, an internist, was well known to me.<br />
Examination revealed a mild right footdrop.<br />
A magnetic resonance image demonstrated<br />
a moderately large, very central<br />
herniated nucleus pulposus at L3–4, plus a<br />
very small extruded fragment on the right.<br />
The patient was scheduled for surgery a few<br />
days later, on a Monday.<br />
The weekend before the surgery was<br />
particularly memorable for me, with several<br />
exciting events transpiring. When I came<br />
to the OR, I enjoyed telling everyone the<br />
weekend’s exciting details during the case.<br />
In addition, to accommodate the patient, I<br />
had elected to perform the surgery in the<br />
hospital where he practices, an excellent<br />
institution where I rarely perform elective<br />
surgery, although I do assist my colleagues<br />
in covering this facility. At my usual hospital,<br />
the rooms are rectangular and the<br />
operating table is always set up parallel to<br />
the long axis <strong>of</strong> the room in a grid-like<br />
fashion, whereas in this hospital, the operating<br />
table is frequently on a diagonal.<br />
My usual routine<br />
is to scrub my hands,<br />
enter the room,<br />
check the X-rays and<br />
magnetic resonance<br />
images, then go to<br />
the side <strong>of</strong> the patient<br />
on which I intend to<br />
operate and finish<br />
prepping the skin<br />
with the antiseptic.<br />
At this hospital, the<br />
doctors are not permitted<br />
to prep the<br />
skin, so I had to<br />
enter, mark the site<br />
and help drape from the most accessible<br />
side <strong>of</strong> the patient. Aside from having a<br />
minimal acquaintance with the anesthesiologist,<br />
I knew no one else in the room, and<br />
as the case proceeded, I realized they also<br />
were inexperienced regarding my particular<br />
techniques.<br />
I started the case standing on the<br />
patient’s left side because, as I entered the<br />
room with the table somewhat askew, I<br />
stood there to help drape. I took an X-ray<br />
to confirm my level, L3–4, as I exposed the<br />
lamina. I then proceeded with the laminotomy.<br />
I was easily able to identify a large<br />
central disc herniation, but no free fragment.<br />
A second X-ray was taken to confirm<br />
the level, and then I extended the small<br />
laminotomy cranially and caudally looking<br />
for the free fragment. A third X-ray confirmed<br />
that I was at the L3–4 level as<br />
intended. Eventually I incised into the large<br />
herniated disc and performed a discectomy.<br />
The small extruded fragment was not<br />
located, but I had long since learned that<br />
sometimes findings are not exactly as<br />
expected. I did detect and remove a large<br />
herniation, decompressing the thecal sac<br />
and nerve roots.<br />
28 AANS Bulletin • www.AANS.org
Exiting the OR, I discussed the case with<br />
my former partner, the referring physician,<br />
including my concern regarding not finding<br />
the extruded fragment. When dictating<br />
the operative report, as soon as I stated the<br />
preoperative diagnosis <strong>of</strong> “large central disc<br />
herniation with small right extruded fragment,”<br />
I realized that I had been on the<br />
patient’s left side. When I explained my<br />
concerns to the OR technicians, they reassured<br />
me that I must have been in the correct<br />
place because I had uncovered and<br />
removed a large disc herniation and had<br />
checked and rechecked the X-rays. I debated<br />
the pros and cons <strong>of</strong> returning to<br />
surgery, with the thought that the significant<br />
decompression and excision <strong>of</strong> the<br />
large central disc probably would accomplish<br />
the desired goal <strong>of</strong> alleviating his<br />
radiculopathy. However, compelled by my<br />
conscience to return to the OR, eventually<br />
I convinced everyone that we needed to<br />
return to explore the patient’s right side. I<br />
discussed the situation with the patient’s<br />
wife as well as with the awakening patient<br />
himself; this was incredibly uncomfortable.<br />
Back in the OR, I explored the right side<br />
at L3–4 through the same incision and<br />
located and removed the extruded fragment.<br />
My former partner called me a few<br />
hours later to advise me that the patient’s<br />
foot-drop had already significantly improved<br />
and he was doing great. The next<br />
morning the patient had no residual footdrop,<br />
was comfortable, and was discharged.<br />
Two weeks after the operation he<br />
covered call for his colleagues during the<br />
holidays and was playing tennis within a<br />
few months. He greeted me as a friend<br />
whenever I saw him in the hospital, but I<br />
always felt too embarrassed to talk with<br />
him, other than simply to say hello.<br />
Despite those facts, the patient did file<br />
a malpractice suit and the case was referred<br />
to the state board <strong>of</strong> medicine, as is appropriate<br />
for such cases. Those issues were a<br />
concern, but my greatest concern was simply<br />
the fact that I could make such a mistake.<br />
I was devastated. I started searching<br />
for answers to how this mistake could happen<br />
and how similar incidents can be prevented<br />
from ever occurring. Literature<br />
re<strong>view</strong>s revealed that many other instances<br />
<strong>of</strong> surgical errors have the same or very<br />
similar factors contributing to the errors.<br />
In almost all cases, there is a “systems<br />
breakdown” in which everyone participating<br />
in the case holds some responsibility.<br />
Several factors contributed to my error.<br />
First, the case was not performed at my<br />
usual hospital. Second, the room setup was<br />
unfamiliar to me. Third, the OR staff was<br />
unfamiliar to me. Fourth, I was not able to<br />
prep the skin myself, which disrupted my<br />
usual routine. Fifth, I was distracted by the<br />
exciting events <strong>of</strong> the preceding weekend.<br />
Lastly, I knew something was wrong and<br />
felt I was in the wrong place but could not<br />
recognize that I had exposed the unintended<br />
side—what I call “oblivious to the<br />
obvious.” Later, recognizing these factors<br />
made me even more distressed at how easily<br />
such errors happen, and searching the<br />
literature and recognizing the frequency <strong>of</strong><br />
these errors was an absolute eye-opener.<br />
Despite the fact that my patient made a<br />
rapid and excellent recovery, I still have<br />
nightmares about this case.<br />
Toward a New Ideology and Culture<br />
I decided that we must develop a new ideology<br />
and culture to recognize how such<br />
errors occur and to prevent them from<br />
happening again. This was further reinforced<br />
by listening, in horror, to some <strong>of</strong><br />
the disastrous cases <strong>of</strong> wrong-site and even<br />
wrong-patient surgery presented at the<br />
board <strong>of</strong> medicine meeting I attended.<br />
My recommendations, as presented at<br />
two national JCAHO conferences, are the<br />
following:<br />
1. We must do a better job <strong>of</strong> communicating<br />
between members <strong>of</strong> the OR team,<br />
and should involve the patients.<br />
2. The surgeon is no longer autonomous.<br />
3. We must emphasize teamwork and<br />
“systems” to succeed safely.<br />
4. There must be protocols and checklists.<br />
5. The surgeon must participate in development<br />
<strong>of</strong> new ideas to promote teamwork<br />
and safety.<br />
6. The OR staff is there to protect the<br />
patient.<br />
7. Our culture must change, and the goal<br />
and expectation must be perfection.<br />
The protocols and checklists should<br />
include:<br />
1. Cases stating site and side should be<br />
posted in the OR and listed on the OR<br />
schedule.<br />
2. Consent forms should identify site and<br />
side specifics.<br />
3. The surgeon should visit the patient<br />
immediately before the surgery to reconfirm<br />
site and side and note it in the chart.<br />
4. When possible, the surgeon should mark<br />
the site and side (in the surgical field).<br />
5. OR staff should reconfirm the intended<br />
procedure and site and side immediately<br />
before surgery.<br />
6. Appropriate studies—X-rays, scans and<br />
data—must be available in the OR, plus<br />
confirmed by the OR staff to represent the<br />
appropriate patient.<br />
Everyone in the OR is a part <strong>of</strong> a team.<br />
The individual team members are important,<br />
responsible parties who must communicate<br />
and interrelate in the OR in the<br />
interest <strong>of</strong> the patient. This must be a “systems<br />
approach.” We must focus on quality<br />
and accountability. Safety represents quality,<br />
and freedom from errors equates with<br />
good results.<br />
Humans are fallible, but mistakes are<br />
preventable. We must devote more time<br />
and resources to developing teams <strong>of</strong> varying<br />
expertise within the operating room<br />
environment to work together toward the<br />
common goal <strong>of</strong> error-free surgery. Surgical<br />
errors are devastating for the surgeon<br />
just as they are for the patient and must be<br />
prevented. 3<br />
Arnold A. Zeal, MD, FACS, FAHA, is chief <strong>of</strong> neurosurgery<br />
at Baptist Health System in Jacksonville, Fla.<br />
Volume 14, Number 4 • AANS Bulletin 29
When Neurosurgeons Drop<br />
What Role Might Microeconomics Play in Their Decision<br />
RICHARD N.W. WOHNS,MD,MBA<br />
Although neurosurgeons are popularly known as “brain”<br />
surgeons, anecdotal evidence and some studies suggest that<br />
at least a small number <strong>of</strong> neurosurgeons are relinquishing<br />
cranial surgery privileges. A result <strong>of</strong> taking such action is<br />
that the neurosurgeon involved no longer can cover emergency<br />
call. While cranial surgery and emergency call long have been<br />
accepted tenets <strong>of</strong> the neurosurgical pr<strong>of</strong>ession, relinquishing cranial<br />
surgery privileges is commonly thought to limit liability and<br />
help control rising medical liability insurance costs, as well as ease<br />
the surgeon’s demanding schedule.<br />
However, the underlying reason why a neurosurgeon might<br />
relinquish cranial surgery privileges may be because the microeconomics<br />
<strong>of</strong> neurosurgical practice has changed. Diminished reimbursement,<br />
particularly in the face <strong>of</strong> escalating overhead affected<br />
by high medical liability insurance premiums, means that cranial<br />
procedures now may consume more practice dollars than they generate.<br />
To illuminate the issues underlying the contentious topic <strong>of</strong><br />
dropping cranial surgery privileges, a business perspective and<br />
analysis can be applied.<br />
Devaluation and Decline <strong>of</strong> Neurosurgical Reimbursement<br />
Reimbursement for neurosurgical procedures has experienced an<br />
overall decline in recent years. After reimbursement values reached<br />
their maximum in 1997, cranial surgery values fell about 25 percent<br />
and spinal surgery values, about 30 percent. The reimbursement<br />
reductions primarily were due to Medicare’s transition to the<br />
resource-based relative value scale between 1999 and 2002.<br />
Since 1992, reimbursement for spinal procedures fell more than<br />
for cranial procedures in most cases. An example <strong>of</strong> the reimbursement<br />
decline for spinal procedures is the 30 percent reduction for<br />
code 63047 (lumbar laminectomy) from $1,408 in 1992 to $1,010<br />
in 2003. (Code 22612 for posterolateral fusion is an exception.<br />
Reimbursement for this code increased from $1,255 in 1992 to<br />
$1,372 in 2004.) Cranial surgery reimbursement remained<br />
unchanged or even increased slightly from 1992 to 2004, but there<br />
was a significant reduction in the real dollar value. This is due to<br />
lack <strong>of</strong> any adjustment for inflation, cost <strong>of</strong> living or practice overhead<br />
increase. Several examples <strong>of</strong> reimbursement for cranial procedures<br />
per Current Procedural Terminology Code are: code 61313<br />
(craniotomy for intracranial hemorrhage)—$1,600 in 1992, and<br />
$1,662 in 2003; code 61312 (craniotomy for subdural hematoma)—<br />
$1,605 in 1992, and $1,654 in 2004; and code 61512 (craniotomy for<br />
meningioma)—$1,913 in 1992, and $2,315 in 2003.<br />
The Cost <strong>of</strong> Lost Opportunity<br />
In addition to the rate <strong>of</strong> reimbursement, the time and expense<br />
involved in performing each surgical procedure must be assessed.<br />
The time and expense spent in the total provision <strong>of</strong> cranial surgery<br />
exceeds that spent in spinal surgery. Therefore, when neurosurgeons<br />
forego the revenues generated from spinal surgeries to perform cranial<br />
surgeries, they are experiencing the phenomenon <strong>of</strong> “opportunity<br />
cost.” This particularly is the experience when emergency<br />
cranial surgeries cause cancellation <strong>of</strong> elective spinal surgeries.<br />
A neurosurgical practice that primarily focuses on spinal surgery<br />
not only is efficient, but there also is very little adverse impact on<br />
the pr<strong>of</strong>itability <strong>of</strong> a practice that does not include brain surgery<br />
and emergency coverage. An analysis <strong>of</strong> the opportunity cost and<br />
microeconomics <strong>of</strong> neurosurgical practice illustrates the contrast in<br />
pr<strong>of</strong>itability between cranial and spinal surgery.<br />
Marginal Revenue, Marginal Cost, and Pr<strong>of</strong>it Maximization<br />
When businesses have a product with diminishing pr<strong>of</strong>itability and<br />
other products with greater pr<strong>of</strong>itability, the decision <strong>of</strong>ten is made<br />
to drop the less pr<strong>of</strong>itable product. The decision hinges on the marginal<br />
revenue <strong>of</strong> the product, whether the business is running at<br />
capacity, and the supply and demand for products. If the business<br />
is not running at capacity and the devalued product helps to cover<br />
fixed expenses, then good business practice supports continuing<br />
with that product line. However, if the business is running at capacity<br />
and there is strong demand for the products, then good business<br />
practice supports dropping the less pr<strong>of</strong>itable product.<br />
As the business increases its level <strong>of</strong> output, each additional unit<br />
adds to the total revenue <strong>of</strong> the business. The additional revenue<br />
attributable to producing one more unit <strong>of</strong> output is called marginal<br />
revenue. As the business increases its level <strong>of</strong> output, each unit<br />
increase in output increases the business’s total cost. The additional<br />
cost <strong>of</strong> producing one more unit <strong>of</strong> output is called marginal cost.<br />
In the special case in which the price <strong>of</strong> the commodity is given to<br />
the business by the market, marginal revenue equals price. For<br />
example, if the business produces plywood, and the market price <strong>of</strong><br />
plywood is $300 per 1,000 square feet, the marginal revenue from<br />
each additional thousand square feet is $300. The business would<br />
increase plywood production—and maximize pr<strong>of</strong>it—as long as<br />
the marginal cost <strong>of</strong> each additional thousand square feet is less<br />
than $300. The business would not increase production if cost <strong>of</strong><br />
each additional thousand square feet is more than $300 to produce.<br />
The principle <strong>of</strong> pr<strong>of</strong>it maximization is germane to a neurosurgical<br />
practice. The reasoning used by businesses that choose<br />
30 AANS Bulletin • www.AANS.org
Cranial Surgery Privileges<br />
output to maximize pr<strong>of</strong>it, described by Maurice and Thomas in<br />
their 1995 book Managerial Economics, can be applied to neurosurgical<br />
practice thusly: If neurosurgeons consider surgery as their<br />
product, the means to maximizing pr<strong>of</strong>it is to choose the level <strong>of</strong><br />
the activity, or surgery, at which the additional revenue just equals<br />
the additional cost.<br />
If a neurosurgical practice produces craniotomies and the market<br />
price <strong>of</strong> craniotomies is $1,500, the marginal revenue from each<br />
additional craniotomy is $1,500. The neurosurgeon would increase<br />
craniotomy production as long as the marginal cost <strong>of</strong> each additional<br />
craniotomy is less than $1,500. The neurosurgeon would not<br />
increase production if the cost <strong>of</strong> each additional craniotomy is<br />
more than $1,500 to produce.<br />
The marginal cost <strong>of</strong> producing craniotomies has steadily<br />
increased due to escalating practice overhead, including the cost<br />
<strong>of</strong> medical liability insurance. The marginal revenue has steadily<br />
decreased due to diminishing insurance reimbursements. In<br />
addition, there is the previously discussed phenomenon <strong>of</strong> opportunity<br />
cost wherein neurosurgeons forego the revenues generated<br />
from additional spinal surgeries by performing craniotomies,<br />
particularly in emergency cases.<br />
Purely from an economic perspective, a neurosurgeon would<br />
decrease the output <strong>of</strong> craniotomies when marginal cost is greater<br />
than marginal revenue. A neurosurgeon would increase the number<br />
<strong>of</strong> craniotomies when the added revenue from the expansion<br />
(marginal revenue) is greater than the added cost <strong>of</strong> the expansion<br />
(marginal cost). In order to maximize pr<strong>of</strong>it, the neurosurgeon<br />
would choose to produce the level <strong>of</strong> output for which marginal<br />
revenue equals marginal cost.<br />
Neurosurgery, <strong>of</strong> course, is not solely an economic enterprise.<br />
Some services are <strong>of</strong>fered which, while less pr<strong>of</strong>itable, are considered<br />
part <strong>of</strong> the full array <strong>of</strong> neurosurgical services, and these services<br />
are subsidized by other more pr<strong>of</strong>itable services. However,<br />
when margins run thin and subsidies disappear, the less pr<strong>of</strong>itable<br />
services such as cranial surgery may be dropped.<br />
When deciding on the value <strong>of</strong> neurosurgical services <strong>of</strong>fered,<br />
neurosurgeons might heed the wisdom <strong>of</strong> Jim Collins, author <strong>of</strong><br />
business books Built to Last and Good to Great:<br />
Our study clearly shows that a company does not need to be in a<br />
great industry to become a great company. Each good-to-great company<br />
built a fabulous economic engine, regardless <strong>of</strong> the industry.<br />
They were able to do this because they attained pr<strong>of</strong>ound insights<br />
into their economics.<br />
Neurosurgical practices are, at least in part, economic enterprises,<br />
and neurosurgeons undoubtedly can benefit from the<br />
insights that economic analysis can yield. 3<br />
Richard N.W. Wohns, MD, MBA, is chair <strong>of</strong> the AANS Pr<strong>of</strong>essional Liability<br />
Committee and chair <strong>of</strong> the CSNS Northwest Quadrant. He is president and founder<br />
<strong>of</strong> South Sound Neurosurgery, PLLC, in the Puget Sound region <strong>of</strong> Washington.<br />
<strong>Surgeons</strong> Link Ad<br />
PU Fall 2005<br />
The Benefit <strong>of</strong> Economic Insight<br />
The phenomenon <strong>of</strong> decreasing the output <strong>of</strong> craniotomies,<br />
that is, giving up cranial surgery privileges, may actually be an<br />
attempt by neurosurgeons, with or without formal economic<br />
analysis, to establish at least a short-term microeconomic competitive<br />
equilibrium. Whether this will become a more prevalent<br />
long-term strategy for neurosurgeons, for whatever reason, is yet<br />
to be determined.<br />
Volume 14, Number 4 • AANS Bulletin 31
M EDICOLEGALU PDATE J EFFREY S EGAL, MD, AND M ICHAEL J . S A COPULOS, JD<br />
Can Contracts Preclude Frivolous Lawsuits<br />
Precedent Suggests Yes, When Carefully Crafted and Introduced<br />
Frivolous malpractice claims are expensive<br />
and time-consuming. What<br />
remedies are available to physicians<br />
who fall prey to such lawsuits<br />
One remedy is to file a suit against the<br />
plaintiff and his or her attorney using the<br />
tort <strong>of</strong> malicious prosecution. However, a<br />
key element for prevailing is proving that<br />
the attorney filed the case with malice,<br />
which is difficult to do. In addition, courts<br />
generally grant plaintiffs and attorneys<br />
wide latitude in pursuing claims <strong>of</strong> malpractice.<br />
Hence, malicious prosecution is a<br />
remedy rarely used.<br />
Contract law, which is separate from<br />
tort law, is another avenue <strong>of</strong> redress for<br />
physicians to investigate. This article will<br />
explore the ability <strong>of</strong> contract law to protect<br />
physicians from frivolous lawsuits.<br />
Making Contracts Enforceable<br />
To help explain what should work, it is first<br />
useful to describe what will not work. Asking<br />
a patient to forego all remedies is not a<br />
workable solution. For example, demanding<br />
that a patient not sue for any reason will<br />
not be enforceable. Public policy dictates<br />
that patients must have some remedy for<br />
negligence. That remedy is usually through<br />
the courts, although arbitration is another<br />
viable option. Having a patient sign a blanket<br />
release would be considered an “abuse<br />
<strong>of</strong> power,” and courts routinely have dismissed<br />
such agreements.<br />
If, however, the demands <strong>of</strong> a contract<br />
are narrower, the contract should withstand<br />
challenges to enforceability. The<br />
contract defines expectations regarding<br />
resolution <strong>of</strong> concerns, specifically that<br />
the physician cannot be sued for a frivolous<br />
reason and that should there be a dispute,<br />
each side will use experts who follow<br />
the code <strong>of</strong> ethics <strong>of</strong> the physician’s specialty<br />
society.<br />
The following considerations for the<br />
patient-physician contract are suggested:<br />
3 Be clear on the mutuality <strong>of</strong> agreement.<br />
3 Do not make any attempt to change the<br />
physician’s duty to the patient within the<br />
agreement.<br />
3 Call the patient’s attention to contractual<br />
provisions.<br />
3 Allow the patient the opportunity to<br />
think about the contract and its consequences<br />
and to ask questions.<br />
3 Do not seek the patient’s agreement<br />
when care is needed urgently or emergently.<br />
A better approach is to obtain agreement<br />
later (for example, in a post-hospitalization<br />
<strong>of</strong>fice visit) and to make the agreement<br />
retroactive—as long as the effective date <strong>of</strong><br />
the agreement is clearly reflected.<br />
3 Do not condition the patient’s treatment<br />
on signing the agreement.<br />
Tests <strong>of</strong> Enforceability Under<br />
Case Law<br />
One test determining enforceability is<br />
whether the document is a contract <strong>of</strong><br />
adhesion. An adhesion contract, as defined<br />
in Sanford v. Castleton Health Care<br />
Center, is “a standardized contract, which,<br />
imposed and drafted by the party <strong>of</strong> superior<br />
bargaining strength, relegates to the<br />
subscribing party only the opportunity to<br />
adhere to the contract or reject it.” While<br />
“adhesion contract” is usually <strong>view</strong>ed as a<br />
pejorative label, one court, in Ingles v.<br />
State Farm Mutual Insurance, has recognized<br />
the basic truth that most contracts<br />
fit that description. As the Ingles court<br />
noted, however, the important task is to<br />
distinguish which adhesion contracts are<br />
appropriate and therefore enforceable,<br />
and which are not.<br />
The usual term to describe the unenforceable<br />
adhesion contract is “unconscionable.”<br />
The court in Sanford v.<br />
Castleton wrote that “a contract is unconscionable<br />
if a great disparity in bargaining<br />
power exists between the parties, such that<br />
the weaker party is made to sign a contract<br />
unwillingly or without being aware <strong>of</strong> its<br />
terms.” The court proceeded to cite the<br />
definition <strong>of</strong> “unconscionable” according<br />
to a 1989 Indiana appellate court opinion:<br />
“The contract must be such as no sensible<br />
man not under delusion, duress, or in distress<br />
would make, and such as no honest<br />
and fair man would accept.”<br />
Unconscionability is a fact-sensitive,<br />
case-by-case issue. As addressed by the<br />
court in Sosa v. Paulos, there are two aspects<br />
to unconscionability: procedural and substantive.<br />
The procedural aspect addresses<br />
the way the contract is reached. The substantive<br />
aspect refers to the actual terms.<br />
Two provisions <strong>of</strong> agreement that likely<br />
would not be considered unconscionable<br />
32 AANS Bulletin • www.AANS.org
are first the promise not to bring a frivolous<br />
lawsuit and second the mutual promise to<br />
use only experts who follow the code <strong>of</strong><br />
ethics for the physician’s specialty society.<br />
The first promise could be “unconscionable”<br />
only if the court concludes that<br />
it is intended to have a chilling effect on<br />
bringing lawsuits, which, the argument<br />
would state, is against public policy. Such a<br />
promise, however, is nothing more than an<br />
obligation already imposed on litigants.<br />
People are not supposed to file frivolous<br />
lawsuits. This principle is reflected in<br />
numerous statutes. For example, an Indiana<br />
statute permits the winning party to<br />
recover attorney fees if the losing party’s<br />
lawsuit was frivolous.<br />
The second promise focuses on how<br />
evidence may be brought forward. The<br />
well-reputed treatise on contract law,<br />
Williston on Contracts, Fourth Edition,<br />
states: “There is a growing tendency for<br />
courts to uphold the right <strong>of</strong> parties to prescribe<br />
certain rules <strong>of</strong> evidence should a<br />
lawsuit arise out <strong>of</strong> the bargain between<br />
them, so long as it does not unduly interfere<br />
with the inherent power and right <strong>of</strong><br />
the court to consider relevant evidence.”<br />
As to the option <strong>of</strong> arbitration, it is<br />
well established that patients and physicians<br />
can contractually use arbitration.<br />
Arbitration asks the plaintiffs to forego<br />
their right to trial by judge or jury. Yet<br />
imposing reasonable conditions on expert<br />
witness behavior is clearly less restrictive<br />
than arbitration. Agreements to arbitrate<br />
are a far greater intrusion into the traditional<br />
judicial system.<br />
Recent cases on arbitration are split<br />
among jurisdictions. However, close analysis<br />
suggests that the cases in which arbitration<br />
was not enforced were so decided<br />
because the way the contract was reached<br />
was unconscionable, not because arbitration<br />
was unconscionable in and <strong>of</strong> itself. In<br />
Sosa v. Paulos, an agreement to arbitrate<br />
was presented to the patient immediately<br />
before knee surgery, after the plaintiff was<br />
in his surgical gown, and the agreement<br />
was presented for signature without explanation.<br />
Neither was there any explanation<br />
<strong>of</strong> the documents at any postoperative visits.<br />
The Utah Supreme Court found this<br />
agreement unconscionable because <strong>of</strong> the<br />
way the patient was asked to make the<br />
agreement. When, however, the troublesome<br />
facts reflected in Sosa v. Paulos have<br />
not been present, agreements to arbitrate<br />
have been held to be not unconscionable<br />
and, therefore, enforceable.<br />
In the Buraczynsky v. Eyring and Sanford<br />
v. Castleton cases, the courts relied on<br />
several factors to find that the contracts<br />
were not unconscionable and therefore<br />
were enforceable. Those factors included:<br />
3 Contractual provisions were not hidden,<br />
but highlighted.<br />
3 There was opportunity to read the contract<br />
unrushed and to ask questions.<br />
3 The language was easy to read and<br />
understand.<br />
3 The language did not change the physician’s<br />
duty to use reasonable care.<br />
3 The contract did not limit liability <strong>of</strong> the<br />
provider to the patient.<br />
Contract Enforceability for Nonsignatory<br />
Parties<br />
A contract can mandate that any attorney a<br />
patient-plaintiff hires follows the same<br />
rules. Further, falling back on the arbitration<br />
analogy, there are precedents for holding<br />
nonsignatory parties to agreements.<br />
A minor child can be bound by the<br />
mother in an agreement to arbitrate made<br />
during the prenatal period. The court in<br />
Wilson v. Kaiser Foundation Hospitals<br />
interpreted the arbitration clause to apply<br />
to any claim arising from services under the<br />
agreement, even though the plaintiff had<br />
not been born when the agreement was<br />
signed. In Gross v. Recabaren, the spouse <strong>of</strong><br />
a contract signatory filed a lawsuit for loss<br />
<strong>of</strong> consortium because <strong>of</strong> a physician’s<br />
negligence. The court found that when a<br />
patient contracts to arbitrate claims <strong>of</strong> negligence,<br />
all claims arising from the alleged<br />
malpractice must be arbitrated. Similarly,<br />
in Herbert v. Superior Court, heirs in a<br />
wrongful death action were found to be<br />
bound by the decedent’s agreement to<br />
arbitrate because the contract required<br />
claims by the “member’s heir or personal<br />
representative” to be arbitrated.<br />
A note on retroactive enforcement:<br />
Physicians <strong>of</strong>ten have long-term relationships<br />
with patients. Is it possible to script<br />
a new contract to address past actions<br />
The answer is maybe. In California the<br />
Coon v. Nicola ruling provided precedent<br />
for retroactive activation <strong>of</strong> an arbitration<br />
agreement.<br />
What Is “Frivolous”<br />
The fact remains that what is frivolous to<br />
one person might be entirely legitimate to<br />
another. How can the definition be tightened<br />
to make a contract to avoid pursuing<br />
a frivolous case meaningful<br />
One solution is to focus on frivolous<br />
testimony as a determinant <strong>of</strong> breach. For<br />
example, a conclusion by the pr<strong>of</strong>essional<br />
conduct committee <strong>of</strong> an organization<br />
such as the AANS might serve as the basis<br />
that the expert testimony was indeed frivolous.<br />
Labeling definitions and rules <strong>of</strong><br />
procedure are <strong>of</strong>ten embedded in contracts.<br />
Hence, the definition <strong>of</strong> frivolous or<br />
the process for determining if testimony is<br />
frivolous could likewise be incorporated<br />
into a contract.<br />
In summary, contracts can be used with<br />
patients to decrease the likelihood that the<br />
physician will be sued for a frivolous reason.<br />
There is ample precedent with arbitration<br />
contracts to believe that such<br />
contracts can be enforced. However, proper<br />
attention must be paid to the content<br />
and the procedure used for obtaining<br />
agreement. Given that tort reform may not<br />
be the best tool to deal specifically with<br />
frivolous lawsuits, contract law should help<br />
to fill the gaps. 3<br />
Jeffrey Segal, MD, FACS, is a neurosurgeon and<br />
founder and chief executive <strong>of</strong>ficer <strong>of</strong> Medical Justice<br />
Services Inc. Michael J. Sacopulos, JD, is a partner<br />
<strong>of</strong> Sacopulos, Johnson and Sacopulos.<br />
Volume 14, Number 4 • AANS Bulletin 33
Wisconsin<br />
St. Vincent<br />
COUNSEL AND EDUCATE PATIENTS AND THEIR FAMILIES<br />
A PATIENT’S GUIDE<br />
Often patients see you when they are in pain, frustrated by a prolonged condition, or<br />
overwhelmed with information they’ve received from friends, the Internet or other physicians.<br />
No matter how much time you spend with a patient, inevitably they feel better having<br />
something from you to take home.<br />
AANS Patient Education Brochure Series<br />
Visit the AANS Online Marketplace at www.AANS.org.<br />
34 AANS Bulletin • www.AANS.org
C OMPUTERE ASE J OEL D. MACD ONALD, M D<br />
Computers in Neurosurgical Education<br />
Online Learning and Performance-Assessment Tools Are Evolving<br />
Throughout a physician’s career,<br />
computer-assisted learning <strong>of</strong>fers<br />
several advantages over traditional<br />
educational vehicles. Search and retrieval<br />
<strong>of</strong> information is more rapid and comprehensive.<br />
Content is dynamic and can<br />
be quickly and easily updated. Digital<br />
documents can incorporate multimedia<br />
elements. Resource information can be<br />
stored more efficiently and economically<br />
in digital format. From a cost standpoint,<br />
computers require a high initial investment<br />
but that expense would ultimately<br />
be exceeded by the alternative <strong>of</strong> accumulating<br />
an extensive hardbound library.<br />
Neurosurgery is highly dependent on<br />
computer technology. Diagnostic imaging<br />
and surgical navigation demand substantial<br />
computer facility. Neurosurgeons’<br />
familiarity with computers enables the<br />
specialty as a whole to take advantage <strong>of</strong><br />
the numerous opportunities that computers<br />
<strong>of</strong>fer for medical education—opportunities<br />
that will continue to evolve.<br />
Computers can be used for education in<br />
two main ways. The first involves directed<br />
learning via computers, whereas the second<br />
involves learning through the day-to-day<br />
use <strong>of</strong> computers. As time passes, the latter<br />
model will gradually supersede the first,<br />
allowing surgeons to take care <strong>of</strong> patients<br />
and simultaneously learn through selfevaluation<br />
and competency maintenance.<br />
Under the older model, computers are<br />
used to deliver educational content and<br />
assess performance. Most <strong>of</strong> the educational<br />
content currently available online follows<br />
this paradigm. The most common example<br />
<strong>of</strong> this type <strong>of</strong> computer-assisted learning is<br />
online continuing medical education. A<br />
wide variety <strong>of</strong> CME activities covering the<br />
spectrum <strong>of</strong> clinical topics are now available<br />
online. These activities have many<br />
advantages for busy clinicians. First and<br />
foremost, they can be conducted at the<br />
convenience <strong>of</strong> the learner. They usually<br />
provide immediate feedback and a selfevaluation<br />
process, as well as immediate<br />
validation <strong>of</strong> earned credit. Typically, the<br />
materials are updated frequently and cost<br />
per credit is low.<br />
The self-assessment test for neurological<br />
surgery, known as SANS Wired, is a<br />
good example <strong>of</strong> a computer-based tool<br />
that provides a mechanism for periodic<br />
knowledge assessment and learner-driven<br />
study. Each SANS question provides immediate<br />
feedback, with a detailed critique and<br />
hyperlinks to additional content on the<br />
Internet. Users can explore a given topic<br />
through the SANS examination using only<br />
a Web browser to broaden their reach to<br />
study materials. Learning occurs primarily<br />
through the process <strong>of</strong> investigating incorrect<br />
responses to practice test questions.<br />
The user can study entirely from the SANS<br />
Wired system without the need for textbooks.<br />
The system tracks the user’s<br />
progress and also permits the user to interrupt<br />
the study process at any time. Yet even<br />
though the SANS experience is flexible and<br />
“termless,” the content is structured and<br />
based on defined learning objectives.<br />
The second way that computers can be<br />
used for education involves learning<br />
through the routine use <strong>of</strong> computers. By<br />
incorporating computers into clinical<br />
activity on a day-to-day basis, the learning<br />
process becomes perpetual and less well<br />
defined. For example, clinical expert systems<br />
and clinical decision support systems<br />
provide a vast potential for learning in a<br />
relatively unstructured fashion. Knowledge<br />
acquisition tends to be driven by the interest<br />
<strong>of</strong> the user or the need to solve a particular<br />
clinical problem. Under these<br />
circumstances, performance evaluation is<br />
more difficult because the learning objectives<br />
are not defined in advance. Furthermore,<br />
since not everyone is studying the<br />
same thing, cohort performance comparison<br />
is not possible. As computer-based clinical<br />
tools evolve, however, the routine-use<br />
realm will <strong>of</strong>fer the most opportunity for<br />
expansion <strong>of</strong> educational activities.<br />
One specific type <strong>of</strong> learning that is <strong>of</strong><br />
paramount importance to neurosurgeons,<br />
the mastery <strong>of</strong> technical skills, cannot be<br />
easily accomplished using computers. Virtual<br />
reality and simulation platforms for<br />
surgery are only in their infancy. There are<br />
a few simulators for exercises such as ventricular<br />
endoscopy and temporal bone<br />
drilling, but they are expensive and rudimentary<br />
and currently are not in widespread<br />
use. Ideally, the sophistication <strong>of</strong><br />
these platforms will improve so that clinicians<br />
can use actual patient data for both<br />
surgical rehearsal and training. This would<br />
not only promote competency with technical<br />
skills but also improve safety for<br />
patients in future.<br />
As the capabilities <strong>of</strong> handheld computers<br />
expand and as data transfer<br />
improves, too, additional educational<br />
applications that work in conjunction with<br />
clinical tools will likely emerge. Indeed,<br />
young physicians routinely “Google”<br />
everything from drug doses to treatment<br />
recommendations, <strong>of</strong>ten using their cell<br />
phones or personal digital assistants.<br />
Computer-assisted learning is clearly an<br />
integral part <strong>of</strong> medical education<br />
throughout a physician’s clinical career.<br />
The body <strong>of</strong> knowledge has now expanded<br />
well beyond the ordinary physician’s<br />
capacity to carry adequate reference materials<br />
physically or to memorize information—and<br />
it will only expand more,<br />
necessitating further development <strong>of</strong><br />
everyday opportunities for computerassisted<br />
education. 3<br />
Joel D. MacDonald, MD, is associate pr<strong>of</strong>essor<br />
<strong>of</strong> neurosurgery at the University <strong>of</strong> Utah<br />
Medical Center.<br />
Volume 14, Number 4 • AANS Bulletin 35
R ESIDENTS’ F ORUM K. MICHAEL W EBB, M D, AND L AWRENCE S. CHIN, M D<br />
Evaluating a New Job<br />
Rank Your Priorities and Do Your Homework<br />
After many years <strong>of</strong> residency, the<br />
prospect <strong>of</strong> getting a job is very<br />
exciting. Unfortunately, that excitement<br />
can make it difficult to evaluate<br />
a potential practice rationally. During<br />
residency one learns little about the business<br />
side <strong>of</strong> neurosurgery, and there is no<br />
chapter in Greenberg to help you out.<br />
Guidance for evaluating job opportunities<br />
in both academic and private settings is the<br />
subject <strong>of</strong> this Residents’ Forum.<br />
The first step in looking for a job is to<br />
determine what is most important to you<br />
and your family. The main factors to consider<br />
are the practice’s location, income<br />
potential and financial strength, as well as<br />
your interest in a subspecialty and<br />
research opportunities. Rank these factors<br />
in order <strong>of</strong> importance, but remember<br />
that every job requires some compromise.<br />
To decide what is negotiable, you must<br />
know your priorities.<br />
Location<br />
Location may be <strong>of</strong> primary importance,<br />
particularly if you have a family. Most<br />
hospitals, <strong>of</strong>fices and operating rooms<br />
look the same, and you will spend most <strong>of</strong><br />
your time there. Your family, however,<br />
will need to deal with jobs elsewhere as<br />
well as with schools, new neighbors and<br />
friends, and the like. Talk to people who<br />
know the area well, and make sure that<br />
you spend at least a few days exploring<br />
the area on your own to examine commute<br />
times, access to shopping and recreation,<br />
and other things that are important<br />
to your life outside <strong>of</strong> work.<br />
Income Potential<br />
Of the 800 neurosurgical job openings<br />
each year, approximately 5 percent to 10<br />
percent are academic jobs. Of approximately<br />
150 residents graduating each<br />
year, about 50 go on to fellowships,<br />
research or military positions, leaving 100<br />
residents entering the job market. At an 8<br />
1 ratio <strong>of</strong> jobs to graduates, the odds favor<br />
you heavily. Regardless <strong>of</strong> your academic<br />
interests and research prowess, remember<br />
that your income will largely be determined<br />
by your clinical activity. Additional<br />
training such as an endovascular or<br />
spine fellowship will allow you to command<br />
a premium salary.<br />
Because it is a job-seeker’s market, academic<br />
practices have increased their starting<br />
salaries to be more competitive with<br />
private practices. However, this relative<br />
equality ends after a few years, as private<br />
practitioners become partners in their<br />
practices. Compensation <strong>of</strong> private practitioners<br />
is on average 20 percent to 50<br />
percent higher than that <strong>of</strong> their academic<br />
counterparts. So if you are considering<br />
joining a private practice, ask about the<br />
path toward partner status (for example,<br />
time frame and board certification), but<br />
remember, everything is negotiable. Practices<br />
with large assets such as <strong>of</strong>fice buildings<br />
or surgery centers may require a<br />
buy-in—but be wary if the assets are not<br />
easily valued.<br />
Academic compensation is frequently<br />
tied to rank. Be aware that the salary differential<br />
between a full pr<strong>of</strong>essor and a partner<br />
in private practice may be less than anticipated,<br />
particularly when you factor in benefits<br />
such as travel compensation, insurance<br />
benefits and malpractice coverage.<br />
Financial Strength<br />
Most academic practices associated with a<br />
medical school are either a department,<br />
which indicates more financial responsibility<br />
and direct reporting to the dean, or a<br />
division <strong>of</strong> general surgery where financial<br />
decisions are made in conjunction with the<br />
chair <strong>of</strong> surgery—though financial independence<br />
for divisions <strong>of</strong> neurosurgery is<br />
not uncommon. Obviously, a private practice<br />
is completely responsible for its<br />
finances. In addition to paying salaries, a<br />
practice must pay employee benefits, <strong>of</strong>fice<br />
rental, supplies, resident expenses and pr<strong>of</strong>essional<br />
liability insurance. Any remaining<br />
money may be paid as a bonus or used for<br />
practice development.<br />
You should meet with the business manager<br />
to evaluate the practice’s financial condition.<br />
Let the manager know in advance<br />
what you want to learn, so this person can<br />
be prepared with the right information. On<br />
the income side, look for the amounts billed<br />
and collected, as well as income from alternate<br />
sources such as pain clinics, ambulatory<br />
surgical centers, <strong>of</strong>fice building rents and<br />
other sources. On the expense side, look at<br />
the “dean’s tax,” salaries and overhead. Also,<br />
ask if bonuses have been based on case<br />
numbers or relative value units and whether<br />
Continued on page 38<br />
36 AANS Bulletin • www.AANS.org
T IMELINE: N eurosurgery Through History<br />
When Their Residence Isn’t the Hospital<br />
What Do You Call Physician Trainees<br />
MICHAEL SCHULDER,MD<br />
Odd label, “residents,” for medical doctors who are preparing<br />
to be fully-trained surgical specialists charged with caring for<br />
patients who may be very ill, and who sometimes can do surgical<br />
procedures that their presumed teachers and supervisors<br />
cannot. The origin <strong>of</strong> this term sheds light on the long hours<br />
that residents have “traditionally” worked such that an 88-hour<br />
workweek is <strong>view</strong>ed as a veritable sinecure.<br />
Through the late 19th century, medical and surgical education<br />
followed a haphazard apprenticeship model. No formal education<br />
was required. Didactic learning was obtained through courses<br />
given by voluntary faculty lecturing in medical schools. Students<br />
bought tickets to attend, and when the time was right they<br />
attached themselves to a practitioner from whom they learned the<br />
art <strong>of</strong> medicine and/or surgery. When Harvey Cushing entered<br />
Harvard Medical School in 1891, he was nearly the only member<br />
<strong>of</strong> his class who had attended college.<br />
At about this time a movement was underway to improve the<br />
level <strong>of</strong> <strong>American</strong> medical education. William Osler, in particular<br />
fervently promoted the importance <strong>of</strong> formal bedside teaching for<br />
medical students and postgraduate trainees. To learn the most pos-<br />
Residents training to be<br />
neurosurgeons started<br />
out working in essence<br />
around the clock for<br />
almost no money.<br />
sible (and to do the<br />
work <strong>of</strong> caring for<br />
patients, much more<br />
<strong>of</strong> a burden in the<br />
developing world <strong>of</strong><br />
scientific medicine<br />
and surgery—and<br />
still following an<br />
apprentice model),<br />
the young doctors<br />
were required to live in the hospital. Hence, they became known as<br />
resident physicians.<br />
Residents training to be neurosurgeons started out working in<br />
essence around the clock for almost no money. Over time they<br />
came to work incredibly hard, by most standards, for a living wage.<br />
Now organized neurosurgery has accepted the concept <strong>of</strong> strictly<br />
defined limitations on work hours. Residents still work long and<br />
hard but no longer have to fear that a sleepless night will be followed<br />
by a day without end. Some people may consider this a<br />
needless accommodation. Others might call it progress. 3<br />
Michael Schulder, MD, is associate pr<strong>of</strong>essor in the Department <strong>of</strong> <strong>Neurological</strong><br />
Surgery and director <strong>of</strong> image-guided neurosurgery at UMDNJ-New Jersey Medical<br />
School in Newark.<br />
Continued from page 36<br />
teaching and research have been considered.<br />
Is there a business plan for increasing<br />
income and decreasing expenses Does the<br />
practice have certified coders Is it looking at<br />
alternative revenue sources Does it have a<br />
plan for expansion Don’t be shy in asking<br />
questions—a good practice will have nothing<br />
to hide.<br />
Subspecialization<br />
When considering your subspecialty interest,<br />
determine what cases you will be<br />
expected to do and what you will need to<br />
give up. More importantly, make sure the<br />
practice’s expectations are not at odds with<br />
the financial incentives. For example, there<br />
will be very little incentive to give up highbilling<br />
cases such as those with spinal<br />
instrumentation if the salary and bonus are<br />
determined by relative value units. If you<br />
are interested in subspecializing, will you be<br />
given the opportunity and resources for<br />
developing a new practice<br />
Research<br />
Starting a laboratory requires space, equipment,<br />
money, collaborators, a mentor and<br />
a lab technician. Meet with the neuroscience<br />
chair and other faculty who share<br />
your research interests. Determine if<br />
resources can be shared and if they are<br />
open to collaboration. Ask for a list <strong>of</strong> faculty<br />
members and their research support.<br />
Protected research time, start-up funds<br />
and a grace period in which your research<br />
will be supported by department funds are<br />
critical for the young investigator. Having<br />
an experienced mentor (preferably a<br />
neurosurgeon who will understand the<br />
unique demands on your time) is a common<br />
factor for clinician-investigators who<br />
become successful.<br />
The Bottom Line<br />
The most important piece <strong>of</strong> advice before<br />
signing with a new practice is to get the<br />
specifics in writing. A key corollary is that<br />
everything is negotiable. Be open and<br />
polite, but do not be afraid to ask the<br />
tough questions. In the end, you will be<br />
respected for your acumen and attention<br />
to detail. 3<br />
K. Michael Webb, MD, is a spine fellow at Barrow<br />
Neurosurgical Associates in Phoenix, Ariz. Lawrence<br />
S. Chin, MD, is pr<strong>of</strong>essor <strong>of</strong> neurosurgery at the<br />
University <strong>of</strong> Maryland Medical Center in Baltimore.<br />
38 AANS Bulletin • www.AANS.org
R ISKM ANAGEMENT M ICHAEL A. CHABRAJA, J D, AND M ONICA W EHBY, M D<br />
Surgeon’s Error or Jury’s Sympathy<br />
Patient Delays Surgery With Adverse Results<br />
When treating high-risk patients,<br />
the uncomfortable reality is that<br />
regardless <strong>of</strong> whether error is<br />
involved, juries <strong>of</strong>ten are swayed<br />
by severe outcomes.<br />
In this case, the defendant neurosurgeon<br />
had recommended surgery in June<br />
1994. Despite having received this recommendation,<br />
the patient elected to postpone<br />
the surgery until after his son’s<br />
wedding in October. The patient’s condition<br />
deteriorated rapidly after the wedding<br />
and somatosensory evoked potential<br />
monitoring performed prior to surgery<br />
failed to pick up any signals from his legs.<br />
The defendant neurosurgeon performed<br />
anterior cervical discectomy and fusion at<br />
C5–6 and C6–7 on the 57-year-old patient<br />
in October 1994 to remove two herniated<br />
discs and treat spinal stenosis caused by<br />
degenerative disc disease. Following surgery,<br />
the patient was paralyzed from the chest<br />
down. He remained a paraplegic with weakness<br />
<strong>of</strong> his arms and hands until he died<br />
from unrelated cancer approximately eight<br />
years later.<br />
The patient’s estate and his spouse sued<br />
the neurosurgeon and the hospital for malpractice.<br />
In addition to recovery <strong>of</strong> medical<br />
expenses, the estate sought damages for loss<br />
<strong>of</strong> normal life, pain and suffering and disfigurement.<br />
The spouse sought damages<br />
for loss <strong>of</strong> consortium and loss <strong>of</strong> services.<br />
The patient’s expert opined at trial that<br />
the postoperative films showed a disc fragment<br />
remaining in the spinal canal and<br />
pressing on the spinal cord, causing worse<br />
compression than the preoperative magnetic<br />
resonance images had revealed. The<br />
defense countered that the postoperative<br />
MR images showed that the spinal canal had<br />
been decompressed successfully. The<br />
defense further maintained that the patient’s<br />
spinal cord was so severely compromised<br />
prior to surgery that the cord could not<br />
withstand the normal trauma <strong>of</strong> surgery<br />
and the simple act <strong>of</strong> decompressing the<br />
stenotic spinal cord caused a spinal stroke.<br />
The evidence presented at trial demonstrated<br />
that in the weeks immediately preceding<br />
the surgery, the patient became<br />
numb from the waist down and had to use<br />
a wheelchair to get around. With regard to<br />
the issue <strong>of</strong> when the surgery took place,<br />
the defense introduced the neurosurgeon’s<br />
notes in the medical record documenting<br />
his discussion with the patient concerning<br />
the risks associated with delaying surgery.<br />
After deliberating for two days and<br />
twice reporting that it was deadlocked, the<br />
jury returned a verdict against the defendant<br />
neurosurgeon and in favor <strong>of</strong> the<br />
patient’s estate and his spouse in the<br />
amount <strong>of</strong> $2,269,034. The bulk <strong>of</strong> this<br />
sum, 1.5 million, was awarded to the estate<br />
and apportioned as $750,000 for loss <strong>of</strong><br />
normal life, $500,000 for pain and suffering,<br />
and $250,000 for disfigurement. The<br />
remainder <strong>of</strong> $769,034 was awarded to the<br />
patient’s spouse, with $517,034 allotted for<br />
medical expenses, $150,000 for loss <strong>of</strong> consortium<br />
and $102,000 for loss <strong>of</strong> services.<br />
Notably, the defendant hospital had settled<br />
out prior to trial for $400,000.<br />
Outcome’s Severity<br />
The fact that the jury twice reported that it<br />
was deadlocked is evidence <strong>of</strong> its struggle to<br />
reach a decision on liability. Although the<br />
patient’s decision to delay his surgery may<br />
well have resulted in further compromising<br />
his spinal cord, the jury ultimately concluded<br />
that this was insufficient to relieve<br />
the defendant neurosurgeon <strong>of</strong> liability.<br />
An argument can be made that the<br />
defendant neurosurgeon should have documented<br />
more clearly in his notes that he had<br />
explained the risks <strong>of</strong> paralysis as well as the<br />
risk <strong>of</strong> delaying surgery with the patient.<br />
However, it is far from clear that this action<br />
would have been outcome determinative.<br />
The result in this case illustrates that the<br />
risk <strong>of</strong> an adverse verdict is sometimes<br />
directly related to the severity <strong>of</strong> the outcome<br />
rather than to the actions taken by a<br />
surgeon. A 2002 study conducted by<br />
Kessler and McClellan underscores this<br />
conclusion and demonstrates its frequency.<br />
The study revealed that evidence <strong>of</strong> medical<br />
negligence was found in less than 20<br />
percent <strong>of</strong> cases in which a patient received<br />
some form <strong>of</strong> compensation from a medical<br />
provider and further that only one in<br />
every 15 patients who were found to have<br />
sustained an injury due to medical negligence<br />
received any sort <strong>of</strong> compensation.<br />
This evident lack <strong>of</strong> relationship<br />
between medical liability award and medical<br />
negligence compounds the risk <strong>of</strong> liability<br />
for specialists treating high-risk<br />
patients. Data maintained by medical liability<br />
insurance provider The Doctors<br />
Company shows that neurosurgeons frequently<br />
sustain claims, averaging a claim<br />
every 18 months. Thus, high-risk specialists<br />
such as neurosurgeons are sued more <strong>of</strong>ten,<br />
not because <strong>of</strong> medical negligence, but<br />
because <strong>of</strong> the risk <strong>of</strong> the medical condition<br />
and the severity <strong>of</strong> the adverse outcome. 3<br />
Michael A. Chabraja, JD, is a partner with<br />
McGuireWoods LLP in Chicago, Ill. Monica Wehby,<br />
MD, is a neurosurgeon with Microneurosurgical<br />
Consultants P.C. in Portland, Ore.<br />
Suggestions By exploring closed<br />
medical liability cases, Risk Management<br />
aims to help neurosurgeons identify<br />
and avoid areas <strong>of</strong> legal peril. If you<br />
would like to see a particular topic<br />
covered, please send your idea to<br />
Monica Wehby, MD, Risk Management<br />
editor, mcwehby@yahoo.com.<br />
Volume 14, Number 4 • AANS Bulletin 39
NREF<br />
M ICHELE S. G REGORY<br />
A Match Made in Science<br />
NREF Gives and Receives in Name <strong>of</strong> Medical Research<br />
It is easy to understand why a relationship<br />
works between the Neurosurgery<br />
Research and Education Foundation<br />
and Kyphon Inc., a medical device company<br />
that develops and markets minimally<br />
invasive technology designed to restore<br />
spinal anatomy. Both organizations are<br />
trying to do the same thing: improve<br />
patient care and quality <strong>of</strong> life through<br />
research and the development <strong>of</strong> advanced<br />
medical technology.<br />
The AANS founded the NREF, its<br />
research division, in 1981 in response to a<br />
rapid decline in federal and private funding<br />
for medical research. The membership<br />
was supportive; however, the annual contributions<br />
were not enough to sustain the<br />
level <strong>of</strong> funding necessary to pursue quality<br />
research into neurosurgical diseases.<br />
Consequently, to enhance the much needed<br />
grant support, in the 1990s the NREF<br />
began partnering with pharmaceutical<br />
and medical device companies such as<br />
Kyphon Inc.<br />
Founded in 1994, Kyphon utilizes a<br />
proprietary balloon technology to repair<br />
spinal fractures with minimally invasive<br />
surgery. The company strives to remain<br />
true to its core values <strong>of</strong> loyalty, trust and<br />
respect for others, and to operate an organization<br />
based on honesty, integrity and<br />
commitment.<br />
Since 2003, Kyphon has been one <strong>of</strong><br />
the many corporations investing in spine<br />
research through NREF research fellowships<br />
and young clinician investigator<br />
awards. Kyphon’s annual support <strong>of</strong> a oneor<br />
two-year grant has made a difference in<br />
the research careers <strong>of</strong> three clinicianscientists<br />
funded by these grants.<br />
“We are pleased to continue our support<br />
<strong>of</strong> the NREF and its research activities,”<br />
said Karen Talmadge, PhD, Kyphon’s<br />
executive vice president and chief science<br />
Pictured at the 2005 AANS Annual Meeting, NREF<br />
Chair Martin H. Weiss, MD, at right, presents Kyphon<br />
representative Karen Talmadge, PhD, with a token <strong>of</strong><br />
appreciation for Kyphon’s 2004–2005 support <strong>of</strong> the<br />
AANS’ neurosurgical research and educational goals.<br />
Dr. Talmadge is Kyphon’s executive vice president<br />
and chief science <strong>of</strong>ficer. For more NREF information,<br />
visit www.AANS.org/research. For more about<br />
Kyphon, visit www.kyphon.com.<br />
<strong>of</strong>ficer. “Through our corporate sponsorship,<br />
we can support the foundation’s<br />
activities to realize our common mission<br />
<strong>of</strong> improving patient care and quality <strong>of</strong><br />
life by advancing worthwhile neurosciences<br />
research.”<br />
Kyphon Matches Donations<br />
100 Percent<br />
Kyphon recently took its relationship with<br />
the NREF to yet another level, issuing a<br />
matching grant and a challenge to all<br />
AANS members. Kyphon generously<br />
agreed to match 100 percent <strong>of</strong> all donations<br />
to the NREF up to $25,000. Hence<br />
the donations made to NREF, either firsttime<br />
or renewed gifts, were doubled, thus<br />
enabling each contribution to have a<br />
greater impact on the overall research<br />
grant program.<br />
“We are proud to partner with Kyphon<br />
in this way,” commented NREF Chair Martin<br />
H. Weiss, MD, FACS. “Neurosurgery’s<br />
growth and expansion is dependent upon<br />
both technical evolution and the expansion<br />
<strong>of</strong> our understanding <strong>of</strong> the disease<br />
processes that confront us. Corporations<br />
like Kyphon are assisting us with this<br />
growth and expansion through their dedicated<br />
support <strong>of</strong> research.”<br />
It is a true match made in the name <strong>of</strong><br />
science and medical research. Kyphon and<br />
the NREF are organizations working<br />
together toward a common good—making<br />
a difference in neurosurgery, one day and<br />
one dollar at a time.<br />
Silent Auction Donations<br />
Support Research<br />
In addition to corporate support, another<br />
avenue <strong>of</strong> NREF support will be evidenced<br />
at the 2006 AANS Annual Meeting<br />
April 22–27, when the Young Neurosurgeons<br />
Committee hosts the 2006 Annual<br />
Silent Auction benefiting the NREF.<br />
The committee, led by Edward Vates,<br />
MD, began procuring items for the eighth<br />
silent auction immediately following the<br />
2005 event, securing popular items such as<br />
vacation packages, electronic gadgets,<br />
sports memorabilia and medical books.<br />
Also welcomed are monetary donations,<br />
which will be used to purchase items in the<br />
name <strong>of</strong> the contributor or contributing<br />
company. This year’s fundraising goal for<br />
the auction is $30,000.<br />
Proceeds from the YNC-sponsored auction<br />
assist the NREF in its efforts to fund<br />
scientific investigations through research<br />
fellowships and young clinician awards.<br />
For more information about the 2006<br />
Annual Silent Auction, to make a donation<br />
or to learn more about the NREF grants<br />
program, visit www.AANS.org/research. 3<br />
Michele S. Gregory is AANS director <strong>of</strong> development.<br />
40 AANS Bulletin • www.AANS.org
B OOKSHELF G ARY V ANDER A RK, M D<br />
A Tale <strong>of</strong> Neurosurgery’s Founder<br />
A Compelling Cushing Inspired a Specialty<br />
Harvey Cushing:<br />
A Life in Surgery,<br />
by Michael Bliss,<br />
2005, Oxford<br />
University Press,<br />
591 pp., $40<br />
($26.40 for AANS<br />
members).<br />
Canadian historian Michael Bliss,<br />
MD, author <strong>of</strong> William Osler: A Life<br />
in Medicine, has written a new book<br />
about neurosurgery’s founder, Harvey<br />
Cushing. It is a book that everyone<br />
should read.<br />
Bliss based this book on a host <strong>of</strong> Cushing<br />
family papers unavailable to earlier<br />
biographers. As a result, this is a less constrained<br />
and more personal biography.<br />
Cushing still comes through as a daring<br />
innovator and icon, but he is also revealed<br />
as a real person with many foibles.<br />
Born in Cleveland in 1869, Cushing<br />
graduated from Yale in 1891 and Harvard<br />
Medical School in 1895, staying in Boston<br />
for an internship at Massachusetts General<br />
Hospital. Then Baltimore beckoned with<br />
its new, graciously endowed Johns Hopkins<br />
Hospital and Medical School. Halsted,<br />
Welch, Kelly and Osler all influenced Cushing,<br />
although during his training Cushing<br />
had limited contact with Halsted, but it was<br />
Osler who quickly became a surrogate<br />
father figure for the young surgical pioneer.<br />
A most significant part <strong>of</strong> Cushing’s<br />
development then followed in his “Wanderjahr”<br />
<strong>of</strong> 1900–01, when he visited Europe.<br />
There, Cushing was shocked by the lack <strong>of</strong><br />
surgical asepsis, concern for the feelings <strong>of</strong><br />
the patients and consistency <strong>of</strong> surgical<br />
techniques. He also did the research that led<br />
to elucidation <strong>of</strong> the “Cushing reflex.”<br />
The next year, Cushing married Kate<br />
Crowell and they moved into the house next to<br />
the Oslers in Baltimore. Cushing was declared<br />
the neurosurgical specialist among the Hopkins<br />
surgeons. His interest in brain surgery<br />
resulted from his ability to successfully treat<br />
trigeminal neuralgia by gasserian ganglionectomy.<br />
As a result, he began to do brain tumor<br />
operations, and in 1902 performed a successful<br />
nerve anastamosis.<br />
Before 1900 more than 500 general surgeons<br />
in the United States had done operations<br />
on the brain. Cushing, however,<br />
brought to the then-dismal field a highly<br />
developed set <strong>of</strong> techniques to control<br />
bleeding, crucial knowledge <strong>of</strong> and sensitivity<br />
to the problem <strong>of</strong> intracranial pressure,<br />
an awesome dexterity, and an equally<br />
He was the kind <strong>of</strong> man<br />
you would work with,<br />
admire and respect, but<br />
not one you would like.<br />
awesome combination <strong>of</strong> enthusiasm and<br />
determination to succeed.<br />
During the first decade <strong>of</strong> the 20th century,<br />
Cushing established neurosurgery as a<br />
specialty. He developed subtemporal decompression<br />
as his basic intracranial operation. It<br />
was his all-purpose response to any cerebral<br />
symptomology. Halsted is said to have commented<br />
during these years that he didn’t<br />
know whether to refer to “poor Cushing’s<br />
patients or Cushing’s poor patients.”<br />
But he also increasingly dedicated himself<br />
to the pituitary toward the end <strong>of</strong> that<br />
decade. By 1912 he had data on 48 patients<br />
and wrote The Pituitary Body and Its Disorders.<br />
It was not until many years later that he<br />
described the syndrome <strong>of</strong> hypersecretion<br />
due to a basophilic adenoma that came to be<br />
known as Cushing’s syndrome.<br />
Cushing is not presented in this book as the<br />
well-rounded person we would like our residents<br />
to become. He was not a good husband;<br />
he was an absentee father, and in the operating<br />
room he could be peevish and mean. One<br />
Hopkins resident said, “He was the kind <strong>of</strong><br />
man you would work with, admire and<br />
respect, but not one you would like.”<br />
World War I, in which Cushing served<br />
two tours <strong>of</strong> duty, definitely took its toll.<br />
While in France he probably had the dreadful<br />
influenza and then post-flu Guillain-<br />
Barre syndrome. This, combined with<br />
Berger’s disease made worse by his smoking,<br />
resulted in significant pain and lower extremity<br />
disability. He also learned something<br />
from the war, however—how to operate<br />
more rapidly. By the time the war ended, he<br />
was able to do eight major cases in a day.<br />
I particularly enjoyed the portions <strong>of</strong><br />
this book that deal with the relationship<br />
between Cushing and Osler. The book’s<br />
most moving scene is the death <strong>of</strong> Osler’s<br />
son, Revere, on the operating table in Flanders.<br />
William Osler himself died in December<br />
1919, and within a few months his<br />
widow asked Cushing to write his biography.<br />
Cushing responded by doubling his<br />
workload to write more than a million<br />
words about his mentor. The final work was<br />
edited down to the two-volume The Life <strong>of</strong><br />
Sir William Osler, published in 1925. One<br />
year later Cushing was awarded the Pulitzer<br />
Prize in biography for this work.<br />
Bliss refers to Cushing as “the Babe Ruth<br />
<strong>of</strong> his game.” Interestingly, his subject<br />
enjoyed the athletic analogy, too. Cushing<br />
wrote to his oldest son, who was struggling<br />
with his studies, “Life all round is a kind <strong>of</strong><br />
sporting event and the best any <strong>of</strong> us can do<br />
is to try continually to improve our game.”<br />
Reading this book will help you improve<br />
your own game. 3<br />
Gary Vander Ark, MD, is director <strong>of</strong> the Neurosurgery<br />
Residency Program at the University <strong>of</strong> Colorado. He is<br />
the 2001 recipient <strong>of</strong> the AANS Humanitarian Award.<br />
Volume 14, Number 4 • AANS Bulletin 41
W ASHINGTONU PDATE<br />
2005 NPHCA Contributors<br />
Special Thanks to Neurosurgery’s Medical<br />
Liability Campaign Supporters<br />
This listing <strong>of</strong> 2005 contributors to Neurosurgeons to Preserve Health Care Access<br />
reflects donations at press time. The NPHCA is the AANS/CNS advocacy organization<br />
that funds Doctors for Medical Liability Reform, which in October<br />
launched a new interactive, nationwide grassroots education and advocacy campaign<br />
known as Protect Patients Now (www.protectpatientsnow.org). Additional<br />
NPHCA information is located at www.neuros2preservecare.org. Questions or concerns<br />
can be directed to Katie Orrico, NPHCA director, at (202) 628-2883.<br />
Alabama<br />
Neurosurgical Society <strong>of</strong> Alabama<br />
Robert H. Bradley Jr., MD<br />
Thomas L. Francavilla, MD<br />
Paul G. Matz, MD<br />
Richard B. Morawetz, MD<br />
Thomas W. Rigsby, MD<br />
Patrick G. Ryan, MD<br />
Nicholas F. Voss, MD<br />
Thomas A. S. Wilson Jr., MD<br />
D. Bruce Woodham, MD<br />
H. Evan Zeiger, MD<br />
Alaska<br />
None<br />
Arizona<br />
Hillel Baldwin, MD<br />
L. Philip Carter, MD<br />
Curtis A. Dickman, MD<br />
Paul M. Francis, MD<br />
Gabriel A. Gonzales-Portillo, MD<br />
Barry A. Kriegsfeld, MD<br />
Paul W. LaPrade Jr., MD<br />
Bradley R. Nicol, MD<br />
Stephen M. Papadopoulos, MD<br />
Randall W. Porter, MD<br />
Abhay Sanan, MD<br />
Thomas B. Scully, MD<br />
Kris A. Smith, MD<br />
Volker K. H. Sonntag, MD<br />
Robert F. Spetzler, MD<br />
Harvey G. Thomas, MD<br />
Carrie L. Walters, MD<br />
Arkansas<br />
Rebecca J. Barret-Tuck<br />
James Blair Blankenship, MD<br />
George T. Burson, MD<br />
Arthur M. Johnson, MD<br />
Ali F. Krisht, MD<br />
Jeffrey Alan Kornblum, MD<br />
Gregory F. Ricca, MD<br />
Tresa Sauthier<br />
Pervie Simpson Jr., MD<br />
Kenneth Tonymon, MD<br />
California<br />
Moustapha Abou-Samra, MD<br />
Laurie Lynn Ackerman, MD<br />
Mark E. Anderson, MD<br />
Brian T. Andrews, MD<br />
James I. Ausman, MD, PhD<br />
Mitchel S. Berger, MD<br />
David B. Bybee, MD<br />
Steven D. Chang, MD<br />
E. Thomas Chappell, MD<br />
SooHo Choi, MD<br />
Tony F. Feuerman, MD<br />
Igor Fineman, MD<br />
Sanjay Ghosh, MD<br />
William Hitselberger, MD<br />
Robert John Jackson, MD<br />
J. Patrick Johnson, MD<br />
John A. Kusske, MD<br />
David I. Levy, MD<br />
Mark A. Liker, MD<br />
Mark E. Linskey, MD<br />
Amir S. Makoui, MD<br />
Michael W. McDermott, MD<br />
Jenny Jasbir Multani, MD<br />
Kimberly A. Page, MD<br />
Mahmoud Rashidi, MD<br />
Benjamin J. Remington, MD<br />
Roderick G. Sanden, MD<br />
Marc S. Schwartz, MD<br />
Randal W. Smith, MD<br />
Melvin Snyder, MD<br />
Philip A. Starr, MD, PhD<br />
Peter P. Sun, MD<br />
Asher H. Taban, MD<br />
Peyman R. Tabrizi, MD<br />
Scott Patrick Wachhorst, MD<br />
Daniel Vernon White, MD<br />
Daniel Won, MD<br />
Kevin Yoo, MD<br />
Colorado<br />
Giancarlo Barolat, MD<br />
Hans C. Coester, MD<br />
Andrew T. Dailey, MD<br />
John Diaz Day, MD<br />
J. Paul Elliott, MD<br />
Timothy M. Fullagar, MD<br />
David Hall, MD<br />
John H. McVicker, MD<br />
Lloyd W. Mobley III, MD<br />
J. Adair Prall, MD<br />
Chad J. Prusmack, MD<br />
Carson J. Thompson, MD<br />
Larry D. Tice, MD<br />
Donn Martin Turner, MD<br />
Brian H. Wieder, MD<br />
Timothy C. Wirt, MD<br />
Connecticut<br />
Gary M. Bloomgarden, MD<br />
Abraham Mintz, MD<br />
Patrick R Tomak, MD<br />
Stephen A. Torrey, MD<br />
Andrew E. Wakefield, MD<br />
Delaware<br />
Magdy I. Boulos, MD<br />
Michael G. Sugarman, MD<br />
District <strong>of</strong> Columbia<br />
Bruce J. Ammerman, MD<br />
Katie Orrico, JD<br />
Florida<br />
John K. B. Afshar, MD<br />
Anthony M. Alberico, MD<br />
Christopher J. Baker, MD<br />
Kaveh Barami, MD, PhD<br />
John Scott Boggs, MD<br />
Kevin L. Boyer, MD<br />
Joseph C. Cauthen, MD<br />
Harold J. Colbassani Jr., MD<br />
Gary P. Colon, MD<br />
Gary J. Correnti, MD<br />
Mark James Cuffe, MD<br />
Paul D. Dernbach, MD<br />
William O. DeWeese, MD<br />
Antonio DiSclafani II, MD<br />
Andrew D. Fine, MD<br />
Duane B. Gainsburg, MD<br />
Mark B. Gerber, MD<br />
F. Gary Gieseke, MD<br />
Jordan C. Grabel, MD<br />
Cesar Guerrero, MD<br />
Philip Henkin, MD<br />
Roberto C. Heros, MD<br />
Hector E. James, MD<br />
Dale K. Johns, MD<br />
I. Basil Keller, MD<br />
Rakesh Kumar, MD<br />
Albert S. Lee, MD<br />
Dean C. Lohse, MD<br />
Lucy Carole Love, MD<br />
Lloyd I. Maliner, MD<br />
Fairuz Matuk, MD<br />
Peter L. Mayer, MD<br />
Christie M. McMorrow, MD<br />
Muhammed Y. Memon, MD<br />
Paulo Monteiro, MD<br />
Brett A. Osborn, DO<br />
Guillermo A. Pasarin, MD<br />
Antonio R. Prats, MD<br />
Christopher S. Rumana, MD<br />
John S. Sarzier, MD<br />
Douglas F. Savage, MD<br />
Andrew E. Sloan, MD<br />
Mark A. Spatola, MD<br />
John C. Stevenson, MD<br />
Amos Stoll, MD<br />
Philip W. Tally, MD<br />
Troy M. Tippett, MD<br />
Jed P. Weber, MD<br />
Aizik L. Wolf, MD<br />
Georgia<br />
Michael A. Amaral, MD<br />
Roy Powell Baker, MD<br />
Kimberly S. Brown, MD<br />
Cliff Cannon Jr., MD<br />
C. Michael Cawley, MD<br />
Marc S. Goldman, MD<br />
Regis W. Haid Jr., MD<br />
Peter Osborne Holliday III, MD<br />
Timothy B. Mapstone, MD<br />
Praveen V. Mummaneni, MD<br />
Bruce J. Nixon, MD, PhD<br />
Gregory M. Oetting, MD<br />
Jeffrey J. Olson, MD<br />
Nelson M. Oyesiku, MD, PhD<br />
Gerald E. Rodts Jr., MD<br />
Karl D. Schultz Jr., MD<br />
David Louis Semen<strong>of</strong>f, MD<br />
John M. Shutack, MD<br />
Ildemaro J. Volcan, MD<br />
Fremont P. Wirth, MD<br />
Hawaii<br />
Jon F. Graham, MD<br />
Warren Y. Ishida, MD<br />
Leon K. Liem, MD<br />
Michon Morita, MD<br />
Idaho<br />
Roy Tyler Frizzell, MD<br />
William F. Ganz, MD<br />
Douglas E. Smith, MD<br />
42 AANS Bulletin • www.AANS.org
Illinois<br />
Todd D. Alexander, MD<br />
Nesher G. Asner, MD<br />
H. Hunt Batjer, MD<br />
Jerry Bauer, MD<br />
Central Illinois Neuro<br />
Health Science<br />
Byong Uk Uk Chung, MD<br />
Jeffrey Warren Cozzens, MD<br />
Oliver N. R. Dold, MD<br />
Jose A. Espinosa, MD<br />
Richard G. Fessler, MD, PhD<br />
Aruna Ganju, MD<br />
Kenneth S. Heiferman, MD<br />
Thomas Richard Hurley, MD<br />
Russ P. Nockels, MD<br />
Vikram C. Prabhu, MD<br />
John Kevin Ratliff, MD<br />
Arden F. Reynolds Jr., MD<br />
Robert Richardson, MD<br />
Gail L. Rosseau, MD<br />
Sean A. Salehi, MD<br />
James L. Stone, MD, SC<br />
Dennis Yung K. Wen, MD<br />
Indiana<br />
Jose M. Arias, MD<br />
Michael R. Burt, MD<br />
Henry Feuer, MD<br />
Peter G. Gianaris, MD<br />
Julius M. Goodman, MD<br />
Terry Horner, MD<br />
Steven M. James, MD<br />
Wayel Kaakaji, MD<br />
Jeffrey K. Kachmann, MD<br />
Saad Abul Khairi, MD<br />
Thomas J. Leipzig, MD<br />
Jean-Pierre Mobasser, MD<br />
Troy D. Payner, MD<br />
Eric A. Potts, MD<br />
M. Hytham Rifai, MD<br />
J. Sartorius, MD<br />
Daria D. Schooler, MD<br />
Mitesh V. Shah, MD<br />
Erick Stephanian, MD<br />
Michael S. Turner, MD<br />
Ronald LeRoy Young, MD<br />
Iowa<br />
David W. Beck, MD<br />
Thomas A. Carlstrom, MD<br />
Matthew A. Howard III, MD<br />
Darren S. Lovick, MD<br />
Todd R. Ridenour, MD<br />
Vincent C. Traynelis, MD<br />
Sabrina M. Walski-Easton, MD<br />
Kansas<br />
Paul M. Arnold, MD<br />
John D. Ebeling, MD<br />
Clifford M. Gall, MD<br />
Raymond W. Grundmeyer III, MD<br />
Kentucky<br />
Steven C. Bailey, MD<br />
James R. Bean, MD<br />
William H. Brooks, MD<br />
Steven P. Kiefer, MD<br />
Bradley G. Mullen, MD<br />
Srinivasan Periyanayagam, MD<br />
David A. Petruska, MD<br />
Steven J. Reiss, MD<br />
Andrew Scott, MD<br />
Bradbury A. Skidmore, MD<br />
Karin R. Swartz, MD<br />
Wayne G. Villanueva, MD<br />
Louisiana<br />
David Cavanaugh, MD<br />
John Robert Clifford, MD<br />
Lawrence Drerup, MD<br />
Thomas B. Flynn, MD<br />
David G. Kline, MD<br />
Ricardo R. Leoni, MD<br />
Horace L. Mitchell, MD<br />
Stefan G. Pribil, MD<br />
Troy M. Vaughn, MD<br />
Rand M. Voorhies, MD<br />
Erich W. Wolf II, MD, PhD<br />
Maine<br />
Konrad (Max) N. M. Barth, MD<br />
Joel I. Franck, MD, PA<br />
Patricio Hernan Mujica, MD<br />
Lee L. Thibodeau, MD<br />
Maryland<br />
Bizhan Aarabi, MD<br />
Kheder Ashker, MD<br />
Hugo E. Benalcazar, MD<br />
Henry Brem, MD<br />
John R. Caruso, MD<br />
Lawrence S. Chin, MD<br />
Gary A. Dix, MD<br />
Howard M. Eisenberg, MD<br />
Augusto F. Figueroa Jr., MD<br />
Raymond I. Haroun, MD<br />
Jeff Jacobson, MD<br />
Saied Jamshidi, MD<br />
Jacek Marian Malik, MD, PhD<br />
William T. Monacci, MD<br />
Swami Nathan, MD<br />
Daniele Rigamonti, MD<br />
Henry M. Shuey Jr., MD<br />
J. Sullivan, MD<br />
Dennis D. Winters, MD<br />
Ravi Yalamanchili, MD<br />
Massachusetts<br />
Christopher H. Comey, MD<br />
Arthur L. Day, MD<br />
Peter K. Dempsey, MD<br />
Michael H. Freed, MD<br />
Marc H. Friedberg, MD, PhD<br />
Howard M. Gardner, MD<br />
Carl Barnes Heilman, MD<br />
Kamal K. Kalia, MD<br />
Michael Dean Medlock, MD<br />
Savvas Papazoglou, MD<br />
Ronald K. Warren, MD<br />
Michigan<br />
Christopher J. Abood, MD<br />
Charles H. Bill II, MD, PhD<br />
Paul D. Croissant, MD<br />
Fernando G. Diaz, MD, PhD<br />
Alain Y. Fabi, MD<br />
Phillip Friedman, MD<br />
David A. Herz, MD<br />
Julian T. H<strong>of</strong>f, MD<br />
Vivekanand Palavali, MD<br />
Miguel Lis-Planells, MD<br />
Mick J. Perez-Cruet, MD<br />
Norbert Roosen, MD<br />
Donald M. Seyfried, MD<br />
John E. Stevenson, MD<br />
Sherry L. Taylor, MD<br />
Ge<strong>of</strong>frey M. Thomas, MD<br />
Minnesota<br />
Hector W. Ho, MD<br />
Cornelius H. Lam, MD<br />
David George Piepgras, MD<br />
Corey Raffel, MD, PhD<br />
Mississippi<br />
W. Craig Clark, MD, PhD<br />
E. Thomas Cullom III, MD<br />
John J. McCloskey, MD<br />
Andrew D. Parent, MD<br />
Missouri<br />
Robert J. Backer, MD<br />
Charles Palmer Bondurant, MD<br />
Arthur Steven Daus, MD<br />
Thomas R. Forget Jr., MD<br />
Robert L. Grubb Jr., MD<br />
J. Alexander Marchosky, MD<br />
Midwest Neurosurgery Associates<br />
M. Ellen Nichols, MD<br />
Nebraska<br />
Kenneth A. Follett, MD, PhD<br />
Benjamin R. Gelber, MD<br />
Leslie C. Hellbusch, MD<br />
Lyal G. Leibrock, MD<br />
Douglas J. Long, MD<br />
A. Angelo Patil, MD<br />
William E. Thorell, MD<br />
Nevada<br />
John A. Anson, MD<br />
Gary Flangas, MD<br />
Randal Peoples, MD<br />
Dante F. Vacca, MD<br />
New Hampshire<br />
Jonathan A. Friedman, MD<br />
Nigel Ross Jenkins, MD<br />
New Jersey<br />
Peter W. Carmel, MD<br />
Duncan B. Carpenter, MD<br />
Jeffrey E. Catrambone, MD<br />
James M. Chimenti, MD<br />
Roderick J. Clemente, MD<br />
Michael P. Feely, MD<br />
Allan L. Gardner, MD<br />
Robert F. Heary, MD<br />
Frank M. Moore, MD<br />
Jay More, MD<br />
Francis J. Pizzi, MD<br />
Elisabeth M. Post, MD<br />
Bruce R. Rosenblum, MD<br />
Catherine A. Ruebenacker-<br />
Mazzola, MD<br />
Michael Schulder, MD<br />
Richard C. Strauss, MD<br />
New Mexico<br />
Hal L. Hankinson, MD<br />
Andrew K. Metzger, MD<br />
New York<br />
Rick Abbott, MD<br />
Rafael Allende, MD<br />
Ron L. Alterman, MD<br />
Ashok Anant, MD<br />
Marc S. Arginteanu, MD<br />
Saeed Bajwa, MD<br />
Ethan A. Benardete, MD, PhD<br />
Alan S. Boulos, MD<br />
Jeffrey N. Bruce, MD<br />
Michael H. C. Cho, MD<br />
Paul R. Cooper, MD<br />
Kaushik Das, MD<br />
Anthony K. Frempong-Boadu, MD<br />
Daniel D. Galyon, MD<br />
Francis W. Gamache Jr., MD<br />
Isabelle M. Germano, MD<br />
John G. Golfinos, MD<br />
Robert Goodman, MD<br />
Alan D. Hirschfeld, MD<br />
L. N. Hopkins III, MD<br />
Paul P. Huang, MD<br />
Jafar Jewad Jafar, MD<br />
Patrick J. Kelly, MD<br />
Ezriel Edward Kornel, MD<br />
David C. Y. Kung, MD<br />
Ranjit Kumar Laha, MD<br />
Michael K. Landi, MD<br />
Michael H. Lavyne, MD<br />
Steven P. Leon, MD<br />
P. Jeffrey Lewis, MD<br />
Veetai Li, MD<br />
Paul C. McCormick, MD<br />
Raj Murali, MD<br />
Stephen T. Onesti, MD<br />
Robert J. Plunkett, MD<br />
A. John Popp, MD<br />
Kalmon D. Post, MD<br />
Donald O. Quest, MD<br />
Sumeer Sathi, MD<br />
Steven J. Schneider, MD<br />
Theodore H. Schwartz, MD<br />
Daniel E. Spitzer, MD<br />
Jack Stern, MD, PhD<br />
Loubert Steven Suddaby, MD<br />
Jeffrey H. Wis<strong>of</strong>f, MD<br />
Seth M. Zeidman, MD<br />
North Carolina<br />
Tim E. Adamson, MD<br />
Anthony Asher, MD<br />
Joe D. Bernard Jr., MD<br />
Adam P. Brown, MD<br />
Domagoj Coric, MD<br />
Vinay Deshmukh, MD<br />
Continued on page 44<br />
Volume 14, Number 4 • AANS Bulletin 43
W ASHINGTONU PDATE<br />
Continued from page 43<br />
E. Hunter Dyer, MD<br />
Frederick E. Finger III, MD<br />
Michael D. Heafner, MD<br />
Martin M. Henegar, MD<br />
Stephen W. Hipp, MD<br />
Bruce P. Jaufmann, MD<br />
F. Douglas Jones, MD<br />
Barry Katz, MD<br />
Robin Koeleveld, MD<br />
Kim Eng Koo, MD<br />
Robert Lacin, MD<br />
Clinton Edward Massey, MD<br />
C. Scott McLanahan, MD<br />
Henry Moyle, MD<br />
Victoria Neave, MD<br />
Richard K. Osenbach, MD<br />
Christopher G. Paramore, MD<br />
Mark P. Redding, MD<br />
Eric Loren Rhoton, MD<br />
Malcolm Shupeck, MD<br />
Pat Smith, MD<br />
Victor G. Sonnino, MD<br />
Craig Andrew Van Der Veer, MD<br />
Carol M. Wadon, MD<br />
North Dakota<br />
John W. Hutchison, MD<br />
Ohio<br />
Cynthia Zane Africk, MD<br />
Arthur G. Arand, MD<br />
Janet W. Bay, MD<br />
William E. Bingaman Jr., MD<br />
Robert J. Bohinski, MD, PhD<br />
Louis P. Caragine Jr., MD, PhD<br />
A. Lee Greiner, MD<br />
Edward J. Kosnik, MD<br />
Charles Kuntz IV, MD<br />
George T. Mandybur, MD<br />
Dennis E. McClure, MD<br />
John M. McGregor, MD<br />
Azedine Medhkour, MD<br />
Raj K. Narayan, MD<br />
Morris Wade Pulliam, MD<br />
Robert Ratcheson, MD<br />
Andrew J. Ringer, MD<br />
E. Salinas, MD<br />
Thomas G. Saul, MD<br />
P. Robert Schwetschenau, MD<br />
Mario M. Sertich, MD<br />
Michael B. Shannon, MD<br />
Joel D. Siegal, MD<br />
Lawrence M. Spetka, MD<br />
Jean-Claude M. Tabet, MD<br />
John M. Tew Jr., MD<br />
Philip V. Theodosopoulos, MD<br />
William D. Tobler, MD<br />
Ronald E. Warnick, MD<br />
Hwa-shain Yeh, MD<br />
Bo H. Yoo, MD<br />
Ahmad Zakeri, MD<br />
Mario Zuccarello, MD<br />
Oklahoma<br />
Christopher Covington, MD<br />
Karl N. Detwiler, MD<br />
Charles F. Engles, MD<br />
Douglas R. Koontz, MD, PC<br />
Jeffrey Paul Nees, MD<br />
Neuroscience Specialists<br />
Don F. Rhinehart, MD<br />
James A. Rodgers, MD<br />
Oklahoma Spine Hospital<br />
Stan Pel<strong>of</strong>sky, MD<br />
Bruce Pendleton, MD<br />
Stewart C. Smith, MD<br />
Oregon<br />
Mark G. Belza, MD<br />
Kim J. Burchiel, MD<br />
Maurice Collada Jr., MD<br />
Michael Dorsen, MD<br />
Jerry L. Hubbard, MD<br />
Andrew J. Kokkino, MD<br />
Michael W. Potter, MD<br />
Donald A. Ross, MD<br />
Nathan R. Selden, PhD, MD<br />
Francisco X. Soldevilla, MD<br />
Pennsylvania<br />
P. David Adelson, MD<br />
Perry Argires, MD<br />
Kimberly S. Harbaugh, MD<br />
Robert E. Harbaugh, MD<br />
James S. Harrop, MD<br />
Philip J. Hlavac, MD<br />
Christopher D. Kager, MD<br />
James A. Kenning, MD<br />
Douglas S. Kondziolka, MD<br />
Keith R. Kuhlengel, MD<br />
Daniel V. Loesch, MD<br />
L. Dade Lunsford, MD<br />
Joseph Charles Maroon, MD<br />
Mark R. McLaughlin, MD<br />
David R. Oliver-Smith, MD<br />
Carroll Prentis Osgood, MD<br />
Roger H. Ostdahl, MD<br />
Robert H. Rosenwasser, MD<br />
Frederick Anthony Simeone, MD<br />
Richard M. Spiro, MD<br />
Michael I. Stanley, MD<br />
Hani J. Tuffaha, MD<br />
Kevin Walter, MD<br />
William C. Welch, MD<br />
Joel W. Winer, MD<br />
Rhode Island<br />
Curtis E. Doberstein, MD<br />
J. Frederick Harrington Jr., MD<br />
South Carolina<br />
Michael A. Cowan, MD<br />
Brian G. Cuddy, MD<br />
David B. Kee Jr., MD<br />
Aaron Curtis MacDonald, MD<br />
William M. Rambo Jr., MD<br />
Andrew Rhea, MD<br />
South Dakota<br />
Quentin John Durward, MD<br />
Marc E. Eichler, MD<br />
Mark W. Fox, MD, PC<br />
Michael J. Giordano, MD<br />
Thorir S. Ragnarsson, MD<br />
Tennessee<br />
Tennessee Neurosurgical Society<br />
Kenan Arnautovic, MD<br />
H. Glenn Barnett II, MD<br />
Frederick A. Boop, MD<br />
Allen S. Boyd Jr., MD<br />
John A. Campbell, MD<br />
Gregory Corradino, MD<br />
David L. Cunningham, MD<br />
Sanat Dixit, MD<br />
Stephanie L. Einhaus, MD<br />
Jerry Engelberg, MD<br />
Claudio Andres Feler, MD<br />
Kevin T. Foley, MD<br />
Thomas Duane Fulbright, MD<br />
John J. Kruse, DMD, MD<br />
Michael S. Muhlbauer, MD<br />
John W. Neblett, MD<br />
Rodney Glen Olinger, MD<br />
Morris William Ray, MD<br />
Jon H. Robertson, MD<br />
Allen K. Sills Jr., MD<br />
Maurice M. Smith, MD<br />
Jeffrey M. Sorenson, MD<br />
Shelly D. Timmons, MD, PhD<br />
Eugenio F. Vargas, MD<br />
Clarence B. Watridge, MD<br />
Texas<br />
Alfonso Aldama-Luebbert, MD<br />
David W. Barnett, MD<br />
Jay M. Barrash, MD<br />
Michael James Burke, MD<br />
Tamerla D. Chavis, MD<br />
Jeffrey D. Cone, MD, FACS<br />
John S. Crutchfield, MD<br />
David J. Donahue, MD<br />
Luis E. Duarte, MD<br />
Bruce L. Ehni, MD<br />
Richard E. George Jr., MD<br />
Michael Gieger, MD<br />
Jeffrey Heitkamp, MD<br />
W. Robert Hudgins, MD<br />
Matthew K. Hummell, MD<br />
Richard Henry Jackson, MD<br />
Thomas A. Kingman, MD<br />
Mark J. Kubala, MD<br />
Martin L. Lazar, MD<br />
James J. Leech, MD<br />
Erwin Lo, MD<br />
Thomas S. L<strong>of</strong>tus, MD, PA<br />
Christopher B. Michael, MD<br />
Luis A. Mignucci, MD<br />
James A. Moody, MD<br />
Mahmood Moradi, MD<br />
Richard C. Naftalis, MD<br />
Warren Neely, MD<br />
Ibrahim Muftah El Nihum, MD<br />
Stig E. Peitersen, MD<br />
James Michael Randle, MD<br />
Raymond Sawaya, MD<br />
Abdolreza Siadati, MD<br />
Alex B. Valadka, MD<br />
Utah<br />
Ronald I. Apfelbaum, MD<br />
William T. Couldwell, MD, PhD<br />
Joel D. MacDonald, MD<br />
Virginia<br />
Charles Azzam, MD<br />
Nasrollah Fatehi, MD<br />
Robert M. Gorsen, MD<br />
Donald G. Hope, MD<br />
Peter M. Klara, MD, PhD<br />
Bothwell Graves Lee, MD<br />
Charles L. Levy, MD<br />
Jonathan P. Partington, MD<br />
Nicholas Poulos, MD<br />
Eric B. Schubert, MD<br />
Crystl D. Willison, MD<br />
Washington<br />
W. Ben Blackett, MD, JD<br />
Richard G. Ellenbogen, MD<br />
Steven Lewis Klein, MD<br />
Barry J. Landau, MD<br />
Jae Y. Lim, MD<br />
Benjamin C. Ling, MD<br />
Daniel G. Nehls, MD<br />
Norman C. Rokosz, MD<br />
Richard N. Wohns, MD<br />
Jacob N. Young, MD<br />
West Virginia<br />
Frederick H. Armbrust, MD<br />
Julian Bailes, MD<br />
Warren W. Boling, MD<br />
Larry Carson, MD<br />
Robert J. Crow, MD<br />
Jeffrey Allen Greenberg, MD<br />
Charles L. Rosen, MD, PhD<br />
John H. Schmidt III, MD<br />
Wisconsin<br />
Robert Dempsey, MD<br />
Walter J. Faillace, MD<br />
Richard L. Harrison, MD<br />
Dennis Jay Maiman, MD, PhD<br />
Jeffrey E. Masciopinto, MD<br />
John H. Neal, MD<br />
Phillip J. Porter, MD<br />
Sanjay C. Rao, MD<br />
Mark K. Stevens, MD, PhD<br />
Wyoming<br />
Steven Joseph Beer, MD<br />
Joseph Sramek, MD<br />
National Organizations<br />
<strong>American</strong> <strong>Association</strong> <strong>of</strong><br />
<strong>Neurological</strong> <strong>Surgeons</strong><br />
Congress <strong>of</strong> <strong>Neurological</strong> <strong>Surgeons</strong><br />
Canada<br />
James T. Rutka, MD, PhD, FRC<br />
Puerto Rico<br />
Ricardo H. Brau, MD<br />
Juan M. Padilla, MD<br />
44 AANS Bulletin • www.AANS.org
MOC Takes Shape<br />
ABNS Begins Maintenance <strong>of</strong> Certification Rollout in 2006<br />
RALPH G. DACEY JR., MD, M. SEAN GRADY,MD,HUNT BATJER,MD, AND WILLIAM CHANDLER,MD<br />
In 2006 the <strong>American</strong> Board <strong>of</strong> <strong>Neurological</strong> Surgery<br />
begins rollout <strong>of</strong> its Maintenance <strong>of</strong> Certification, or<br />
MOC®, program. The ABNS was founded in 1940 to provide<br />
initial certification to practitioners <strong>of</strong> neurosurgery<br />
who meet specific training and practice requirements. In<br />
recent years the public, payers, other healthcare organizations<br />
and governmental agencies have called for periodic<br />
recertification <strong>of</strong> specialists.<br />
In March 2000 all member boards <strong>of</strong> the <strong>American</strong> Board <strong>of</strong><br />
Medical Specialties, including the ABNS, adopted a commitment<br />
to modify their current or planned programs for recertification<br />
into programs for MOC. After analyzing the arguments for the<br />
establishment <strong>of</strong> an MOC program, ABNS directors concluded<br />
that regulatory bodies will very soon require neurosurgeons to<br />
participate in the process. ABNS directors are committed to making<br />
available to all diplomates a meaningful and practical MOC<br />
program, one that takes into account the concerns <strong>of</strong> diplomates<br />
and meets the standards <strong>of</strong> the ABNS, as well as those established<br />
by the ABMS.<br />
Through its MOC program, the ABNS supports its diplomates’<br />
dedication to lifelong learning. The guiding principle in this<br />
endeavor is to foster excellence in patient care.<br />
The ABNS MOC program is designed to reflect the realities <strong>of</strong><br />
today’s neurosurgical practice. Emphasis is placed on core neurosurgical<br />
knowledge and practice common to all neurosurgeons.<br />
The process is designed to permit diplomates to include the areas<br />
<strong>of</strong> their individual expertise when devoting time to continuing<br />
medical education activities, selecting a module for the cognitive<br />
examination and submitting key cases from their practice.<br />
Diplomates are enrolled in the program upon issuance <strong>of</strong> timelimited<br />
ABNS certificates and submission <strong>of</strong> a completed MOC<br />
application. Time-limited certificates, current for 10 years, were first<br />
issued to new ABNS diplomates in 1999. In order to maintain their<br />
certification, diplomates certified during or after 1999 must participate<br />
in the MOC program. Each individual’s progress through the<br />
MOC program requirements will be tracked online.<br />
Non-time-limited certificate holders may participate in the<br />
program at any time. Current for the life <strong>of</strong> the individual, nontime-limited<br />
certificates were issued to all ABNS diplomates certified<br />
before 1999. A non-time-limited, original certificate will not<br />
expire regardless <strong>of</strong> the individual’s participation in the MOC program.<br />
Individuals in this group, however, are strongly encouraged<br />
to participate in the MOC program.<br />
Program Requirements<br />
There are four basic components <strong>of</strong> all specialty MOC programs:<br />
evidence <strong>of</strong> pr<strong>of</strong>essional standing; evidence <strong>of</strong> lifelong learning and<br />
self-assessment; evidence <strong>of</strong> cognitive knowledge; and evidence <strong>of</strong><br />
performance in practice.<br />
Into this framework, the ABNS MOC program has integrated<br />
seven requirements: chief <strong>of</strong> staff questionnaire; CME hours, both<br />
category 1 and category 2; cognitive examination; communication<br />
assessment tool (the CAHPS); key case analysis; Self-Assessment in<br />
<strong>Neurological</strong> Surgery Examination (the SANS); and unrestricted<br />
license to practice medicine.<br />
The four basic components and the individual ABNS requirements,<br />
plus the frequency with which they must be updated, have<br />
been integrated as follows.<br />
1. Evidence <strong>of</strong> Pr<strong>of</strong>essional Standing<br />
A. Full unrestricted license to practice medicine in all jurisdictions in which<br />
the diplomate practices will be verified every three years.<br />
B. Unencumbered hospital admitting privileges to practice neurosurgery<br />
will be verified every three years.<br />
C. Questionnaires will be completed by the chief <strong>of</strong> the medical staff <strong>of</strong><br />
the diplomate’s primary hospital every three years.<br />
2. Evidence <strong>of</strong> Lifelong Learning<br />
and Self-Assessment<br />
A. Lifelong Learning: At least 150 CME hours must be accumulated<br />
every three years and must include a minimum <strong>of</strong> 60 category 1 neurosurgical<br />
hours with the remainder in either category 1 or category 2.<br />
At least 80 percent <strong>of</strong> the 150 hours must be specific to neurosurgery.<br />
The ABNS reserves the right to establish the activities that qualify for<br />
CME categories 1 and 2; a list <strong>of</strong> accepted activities will be available<br />
on the ABNS Web site. Self-assessment exercises and examinations<br />
can be used to satisfy portions <strong>of</strong> the requirement. Accrual <strong>of</strong> CME<br />
hours will be tracked in conjunction with the <strong>American</strong> <strong>Association</strong> <strong>of</strong><br />
<strong>Neurological</strong> <strong>Surgeons</strong>, and the information may be verified online.<br />
B. Self-Assessment: The diplomate must participate in a Web-based educational<br />
program. For this the ABNS has selected the SANS examination.<br />
Its development and administration is done by the Congress <strong>of</strong> <strong>Neurological</strong><br />
<strong>Surgeons</strong>. Participation in the examination will be verified electronically<br />
and forwarded to the ABNS data repository every three years.<br />
46 AANS Bulletin • www.AANS.org
3. Evidence <strong>of</strong> Performance in Practice<br />
A. Key Cases: Every three years diplomates must submit the details <strong>of</strong><br />
10 consecutive cases <strong>of</strong> one procedure selected from a list <strong>of</strong> procedures<br />
that cover the subspecialties. If the diplomate practices general neurosurgery<br />
or a subspecialty not represented, he or she may send in 10 consecutive<br />
cases <strong>of</strong> the most frequent procedure. Questionnaires must be<br />
filled out by the diplomate regarding each reported consecutive case. The<br />
list <strong>of</strong> cases so far consists <strong>of</strong> the following: (1) Anterior Cervical Discectomy;<br />
(2) Chiari Decompression; (3) Clipping <strong>of</strong> Anterior Circulation<br />
Aneurysm; (4) Craniotomy for Cerebral Glioma; (5) Craniotomy for Temporal<br />
Lobectomy; (6) Endovascular Embolization <strong>of</strong> an Anterior Circulation<br />
Aneurysm; (7) Lumbar Discectomy; (8) Radiosurgery <strong>of</strong> a Metastatic Brain<br />
Tumor; (9) Release <strong>of</strong> Tethered Cord; (10) Removal <strong>of</strong> Intracranial<br />
Hematoma; (11) Surgical Treatment <strong>of</strong> Pituitary Tumor; (12) Surgical Treatment<br />
<strong>of</strong> Trigeminal Neuralgia; (13) Ulnar Nerve Transposition; (14) Nonsurgical<br />
Treatment <strong>of</strong> Back Pain. Key case participation will be validated<br />
and feedback given to diplomates for analysis.<br />
B. Communication Assessment Tool: Practice assessment <strong>of</strong> physicianpatient<br />
communication must be submitted every three years. Patient perception<br />
<strong>of</strong> physician performance in the areas <strong>of</strong> interpersonal and<br />
communication skills will be measured using a survey given to 20 patients<br />
who respond via telephone or the Internet. Participation in the communication<br />
assessment survey is validated and feedback given to the participant<br />
for analysis.<br />
C. Chief <strong>of</strong> Staff Questionnaire: Every three years a chief <strong>of</strong> staff questionnaire<br />
must be submitted by the diplomate. The questionnaire will allow<br />
the ABNS to verify the diplomate’s standing at his or her primary hospital<br />
and will cover the MOC areas <strong>of</strong> pr<strong>of</strong>essionalism, communication skills<br />
and participation in systems-based practice.<br />
D. SANS: Content is developed by the SANS CNS editorial board to assess<br />
the competencies <strong>of</strong> interpersonal skills, pr<strong>of</strong>essionalism, practice-based<br />
learning and improvement, and systems-based practice. Items are then<br />
refined to meet the standards <strong>of</strong> the ABNS and the National Board <strong>of</strong> Medical<br />
Examiners for cognitive knowledge examinations.<br />
E. Additional Modules: Other modules, including one on patient safety, will<br />
be added as developed. Participation is expected to be every three years.<br />
4. Evidence <strong>of</strong> Cognitive Knowledge<br />
A cognitive examination must be taken and passed in the eighth, ninth or<br />
10th year <strong>of</strong> each 10-year MOC cycle. Prior to taking the examination, the<br />
applicant must have met these criteria:<br />
3 Active continuous participation in the MOC program (all three-year<br />
cycles—i.e., CME hours, key cases, SANS, communications assessment<br />
tool, unrestricted license and chief <strong>of</strong> staff questionnaires) or<br />
successful reinstatement in the process if there was a period <strong>of</strong> nonparticipation.<br />
3 No fees outstanding to the ABNS.<br />
This secure computer-based examination will be given at regional testing<br />
centers. It will consist <strong>of</strong> 200 questions and will be entirely clinically<br />
based. The pass rate is anticipated to be very high. A significant portion<br />
<strong>of</strong> the content <strong>of</strong> the MOC cognitive examination will be similar in style<br />
and content to the material presented in previous SANS examinations.<br />
Three different modules will be <strong>of</strong>fered:<br />
(1) General Examination: Consists <strong>of</strong> 200 basic clinical neurosurgery<br />
questions.<br />
(2) Spine Examination: Consists <strong>of</strong> 150 <strong>of</strong> the basic clinical neurosurgery<br />
questions, plus 50 complex spine questions.<br />
(3) Pediatric Examination: Consists <strong>of</strong> 150 <strong>of</strong> the basic clinical neurosurgery<br />
questions, plus 50 pediatric questions.<br />
As soon as the results become available, participants will receive their<br />
examination score reports and notification <strong>of</strong> their passage or failure. Participants<br />
who do not receive their results within 16 weeks should call the<br />
ABNS <strong>of</strong>fice and request a report. Examination results will be communicated<br />
to the diplomate via a written report mailed to the diplomate’s postal<br />
address; no results will be communicated via telephone, fax or e-mail.<br />
Most diplomates who participate in the MOC cognitive examination will<br />
be successful. Those who do not pass will be encouraged to continue the<br />
MOC process and retake it at the earliest possible time, as long as they<br />
are within their 10-year cycle. An examination fee must be paid each time<br />
the examination is taken. Diplomates may retake the examination as long<br />
as they continue to meet the program requirements expected <strong>of</strong> active<br />
participants.<br />
3 For Time-Limited Certificates: Diplomates with time-limited certificates<br />
are required to pass the MOC cognitive examination. The examination may<br />
be taken during the eighth, ninth or 10th year <strong>of</strong> the MOC process. Individuals<br />
who have not passed it by the end <strong>of</strong> the 10-year period may reinstate<br />
their diplomate status only by repeating all the requirements for<br />
initial ABNS certification, including passing the primary and oral examinations<br />
and thereby earning a new, valid, time-limited certificate. Consequently,<br />
diplomates are encouraged to take the MOC examination in the<br />
eighth or ninth year <strong>of</strong> their 10-year cycle so that, in the event they do not<br />
pass, they can retake it prior to the expiration <strong>of</strong> the 10-year period.<br />
3 For Non-Time-Limited Certificates: Diplomates with non-time-limited certificates<br />
who wish to satisfy the requirements <strong>of</strong> the MOC process but do<br />
not pass the cognitive examination by the end <strong>of</strong> their 10-year period will<br />
not lose their certification; however, they will no longer be considered<br />
active in the MOC process unless granted an exemption by the ABNS.<br />
Ralph G. Dacey Jr., MD, M. Sean Grady, MD, Hunt Batjer, MD, and William Chandler,<br />
MD, are directors <strong>of</strong> the <strong>American</strong> Board <strong>of</strong> <strong>Neurological</strong> <strong>Surgeons</strong>, www.ABNS.org.<br />
Volume 14, Number 4 • AANS Bulletin 47
N EWS. ORG<br />
AANS/CNS SectionsCommittees<strong>Association</strong>sSocieties<br />
“Lost” AANS Members<br />
Year Joined,<br />
Last Known Location<br />
Hugh W. Barr, MD<br />
1969, Ontario<br />
Wesley A. Cook Jr., MD<br />
1974, North Carolina<br />
Giuseppe Dalle Ore, MD<br />
1970, Italy<br />
Jeremy W. Denning, MD<br />
2000, Texas<br />
Stefanie Ann DiCea, PA-C<br />
2005, Michigan<br />
Robert A. Evans, MD<br />
1970, California<br />
William S. Fields, MD<br />
1960, Georgia<br />
Adolphe Y. Gerol, MD<br />
1963, Wisconsin<br />
H. Stephen Goldberg, MD<br />
1977, Texas<br />
Daniel Charles Good, MD<br />
1978, Pennsylvania<br />
John Hankinson, MD<br />
1973, England<br />
Thomas J. Holbrook, MD<br />
1950, West Virginia<br />
Henry L. Hood, MD<br />
1961, Pennsylvania<br />
William S. Huestis, MD<br />
1965, Nova Scotia<br />
Kenneth I. Kiluk, MD<br />
1978, North Carolina<br />
Stephen Francis<br />
Kornyey, MD<br />
1958, Hungary<br />
Joyce A. Kunkel, RN,<br />
CNRN<br />
1994, North Carolina<br />
Warren H. Leimbach II, MD<br />
1992, Ohio<br />
Nills G. Lundberg, MD<br />
1969, Sweden<br />
Ignacio A. Magana, MD<br />
1993, Florida<br />
Richard Malmros, MD<br />
1969, Denmark<br />
Help Find “Lost” AANS Members The AANS seeks<br />
readers’ help in locating the members listed at left. In<br />
an effort to locate them, the AANS has contacted<br />
their medical schools, residency programs, institutions<br />
where they practiced medicine and state neurosurgical<br />
societies, and has conducted Web<br />
searches. Those with contact or other information<br />
that may help to locate an individual are asked to<br />
contact AANS Member Services at (888) 566-2267,<br />
ext. 538, or kal@aans.org.<br />
AANS Endorses NextGen EMR System AANS members<br />
now can receive a discount on NextGen electronic<br />
medical record systems, available through a new<br />
alliance agreement. EMR systems can help physician<br />
practices improve quality, reduce risk, cut costs and<br />
increase revenues. NextGen’s EMR system is appropriate<br />
for any size <strong>of</strong> medical practice—solo or small<br />
practice or large, multiprovider, multilocation<br />
group. Providers that want to share and manage<br />
clinical and administrative patient information<br />
through a comprehensive, single-source application<br />
can visit www.nextgen.com or call (215) 657-7010 to<br />
learn more. Neurosurgical templates are available.<br />
For information on other AANS partner programs,<br />
visit the AANS Web site at www.aans.org/membership/mem_services.asp<br />
AANS Achieves ACCME Accreditation Through 2009<br />
Following a routine re<strong>view</strong> <strong>of</strong> AANS continuing<br />
medical education activities, the Accreditation<br />
Council for Continuing Medical Education accredited<br />
the AANS until the next re<strong>view</strong> in November<br />
2009. The ACCME notified the AANS in<br />
November <strong>of</strong> accreditation, finding compliance in<br />
all areas and exemplary compliance in two areas.<br />
As an ACCME-accredited provider, the AANS<br />
takes full responsibility for its certified activities<br />
including planning, implementing and evaluating<br />
them. Accreditation by the ACCME allows the<br />
AANS to directly sponsor CME programs such as<br />
AANS coding courses, practice management<br />
courses, clinical courses and oral boards courses. It<br />
also allows the AANS to jointly sponsor CME programs<br />
with unaccredited providers and to cosponsor<br />
CME programs with accredited providers.<br />
Additional information on joint sponsorship,<br />
cosponsorship and all AANS CME activities is<br />
available at www.AANS.org/education.<br />
ACS/AANS Health Policy Scholarship The 2006 Health<br />
Policy Scholarship, <strong>of</strong>fered by the <strong>American</strong> College<br />
<strong>of</strong> <strong>Surgeons</strong> and the AANS, supports attendance at<br />
the Leadership Program in Health Policy and<br />
Management at Brandeis University from May 29<br />
to June 3, 2006. The goal <strong>of</strong> the leadership program<br />
is to provide clinical leaders with the policy and<br />
management skills essential for creating innovative<br />
and sustainable solutions that improve the quality,<br />
cost-effectiveness, and efficiency <strong>of</strong> healthcare service<br />
delivery. The awardee must be between the<br />
ages <strong>of</strong> 30 and 55 and a member <strong>of</strong> both the ACS<br />
and the AANS. The application deadline is Feb. 1.<br />
Additional information is available at www.aans<br />
.org/ACS_AANS_Scholarship.pdf.<br />
“Contemporary Neurosurgery” Now Counts Toward<br />
AANS CME Requirements Each issue <strong>of</strong> Contemporary<br />
Neurosurgery, a biweekly newsletter, has been recognized<br />
as a cosponsored activity for which 1.5 category<br />
1 credits are awarded toward the AANS Continuing<br />
Education Award in Neurosurgery. A description <strong>of</strong><br />
the newsletter is available at www.lww.com/product/<br />
0163-2108. Subscribers to Contemporary Neurosurgery<br />
may submit CME certificates to the AANS<br />
retroactive to January 2005. AANS members are eligible<br />
to receive a one-time 10 percent discount on<br />
their subscriptions by calling (800) 638-3030 and referencing<br />
the AANS promotional code YNLAANS.<br />
AANS Endorses TotalChart Medical S<strong>of</strong>tware System<br />
TotalChart, a complete and portable electronic chart<br />
and medical record, allows access to up-to-date<br />
coding information, patient information, schedules<br />
and clinical notes. “One <strong>of</strong> the critical elements to<br />
the success <strong>of</strong> a surgical practice is the efficient<br />
management <strong>of</strong> the coding and billing process,”<br />
said Ronald Warnick, MD, chair <strong>of</strong> the AANS<br />
Member Development Committee. “TotalChart is<br />
one <strong>of</strong> a new breed <strong>of</strong> practice solutions that put<br />
control <strong>of</strong> this process in the hands <strong>of</strong> the surgeon.”<br />
AANS members a receive 10 percent discount <strong>of</strong><br />
the current list price for the TotalChart s<strong>of</strong>tware<br />
license. Additional information is available at<br />
48 AANS Bulletin • www.AANS.org
I N M EMORIAM<br />
Remembering<br />
Lyal G. Leibrock, MD<br />
JAMES R. BEAN,MD<br />
At the passing <strong>of</strong> Lyal G. Leibrock, MD, we all lost<br />
a dear friend, a wise and humorous companion,<br />
and an intrepid and dearly loved fellow-traveler<br />
on the highway <strong>of</strong> neurosurgery.<br />
We will miss him, with his unfeigned modesty,<br />
his too little acknowledged distinction, and his<br />
understated leadership. He devoted his life to his<br />
pr<strong>of</strong>ession, even to this bitter and untimely end.<br />
He was instrumental in bringing the Council<br />
<strong>of</strong> State Neurosurgical Societies to the position <strong>of</strong><br />
influence and respectability in neurosurgery that<br />
it now enjoys. His guidance and enthusiasm are<br />
unmatchable and irreplaceable.<br />
He worked until his will no longer trumped<br />
his illness, enduring his trial without complaint.<br />
This expected news brings unaccustomed sorrow.<br />
We see death <strong>of</strong>ten, but rarely does it touch our<br />
lives so deeply. We mourn his passing.<br />
Dr. Leibrock died Sunday, Nov. 13, <strong>of</strong> metastatic<br />
colon cancer. He is survived by his wife, Judi,<br />
children Michele, Elizabeth and Christopher, and<br />
a granddaughter, Olivia.<br />
Biography<br />
For 27 years, Lyal G. Leibrock, MD, was an active<br />
participant in the Department <strong>of</strong> Surgery at the<br />
University <strong>of</strong> Nebraska Medical Center, most<br />
www.aans.org/membership/totalchart.asp and at<br />
www.TotalChart.com, (888) 220-1050.<br />
AMA Says P4P Programs Must Be Fair and Ethical At its<br />
semiannual policymaking meeting in November, the<br />
<strong>American</strong> Medical <strong>Association</strong> voted to oppose<br />
Medicare pay-for-performance initiatives (such as<br />
“value-based purchasing programs”) that do not<br />
meet the AMA’s Principles and Guidelines for Payfor-Performance.“The<br />
AMA today sends a clear message<br />
that pay-for-performance must be focused on<br />
quality and be patient-centered, fair and ethical,” said<br />
AMA Trustee John Armstrong, MD. The five AMA<br />
principles for fair and ethical pay-for-performance<br />
programs are: ensure quality <strong>of</strong> care; foster the<br />
recently as pr<strong>of</strong>essor and<br />
department chair. When a<br />
neurosurgery training program<br />
was approved at UNMC<br />
in July 1993, Dr. Leibrock<br />
served as its program director.<br />
Dr. Leibrock had an interest<br />
in pain, skull base, and<br />
spinal surgery. He was a visiting<br />
pr<strong>of</strong>essor at many universities in the United States<br />
as well as Shiraz University in Shiraz, Iran, and the<br />
China/Japan Friendship Hospital in Beijing, China. He<br />
was a fellow <strong>of</strong> the <strong>American</strong> College <strong>of</strong> <strong>Surgeons</strong>, a<br />
member <strong>of</strong> the Society for <strong>Neurological</strong> <strong>Surgeons</strong> as<br />
well as the <strong>American</strong> <strong>Association</strong> <strong>of</strong> <strong>Neurological</strong> <strong>Surgeons</strong><br />
and the Congress <strong>of</strong> <strong>Neurological</strong> <strong>Surgeons</strong> for<br />
which he served on numerous committees, and a<br />
founding member <strong>of</strong> the North <strong>American</strong> Skull Base<br />
Society. He participated in the Council <strong>of</strong> State Neurosurgical<br />
Societies for more than a decade, serving as<br />
chair from 1999 to 2001. The CSNS recently honored<br />
him with the Distinguished Service Award.<br />
Dr. Leibrock was born in Alma, Kan., Nov. 20,<br />
1940, and raised in California, where he graduated<br />
from the University <strong>of</strong> Southern California School <strong>of</strong><br />
Medicine. Dr. Leibrock performed a surgical internship<br />
at Los Angeles County USC Medical Center<br />
from 1969 to 1970. He completed his neurosurgical<br />
training at Johns Hopkins Hospital in the summer <strong>of</strong><br />
1976 under the direction <strong>of</strong> A.E. Walker, MD, and<br />
Donlin Long, MD, and he then served two years on<br />
active duty at the Naval Regional Medical Center,<br />
Oakland, Calif. 3<br />
patient-physician relationship; <strong>of</strong>fer voluntary physician<br />
participation; use accurate data and fair reporting;<br />
and provide fair and equitable program incentives.<br />
Additional information is available at<br />
www.ama-assn.org.<br />
2006 NASS Research Grant and Fellowship Applications<br />
Due May 5 The North <strong>American</strong> Spine Society is<br />
<strong>of</strong>fering research grants for investigative research on<br />
the spine, as well as a clinical traveling fellowship and<br />
a research traveling fellowship. The application deadline<br />
is May 5. Additional information and an application<br />
are available at www.spine.org/Research/<br />
ResearchProgram.cfm.<br />
S. Napoleon Martinez, MD<br />
1962, Canada<br />
Luciano M. Modesti, MD<br />
1972, New York<br />
Juan Negrin Jr., MD<br />
1952, New York<br />
Helge Nornes, MD<br />
1976, Norway<br />
Jorge Rene Ordonez, MD<br />
1979, Maryland<br />
Richard G. Perrin, MD<br />
1998, Ontario<br />
Richard Henry Retter, MD<br />
1958, Ohio<br />
Charles W. Rossel, MD<br />
1967, Ohio<br />
William A. Rouady, MD<br />
1978, Virginia<br />
John Albert Savoy, MD<br />
1976, Maine<br />
James F. Sheridan, MD<br />
1973, Ohio<br />
Richard B. Small, MD<br />
1983, California<br />
Donald Leon Stainsby, MD<br />
1960, Washington<br />
Gordon J. Strewler, MD<br />
1957, North Carolina<br />
Fred N. Sugar, MD<br />
1976, Colorado<br />
Jean Talairach, MD<br />
1970, France<br />
John L. K. Tsang, MD<br />
1955, Nevada<br />
Andrew F. Venditti, PA-C<br />
2001, Indiana<br />
Jody M. Wellwood, MSN,<br />
ACNP<br />
2002, Michigan<br />
Walter R. Whitehurst, MD<br />
1967, Florida<br />
Stuart R. Winston, MD<br />
1977, Arizona<br />
Luis Yarzagaray, MD<br />
1975, Columbia<br />
John C. Zahniser, MD<br />
1982, California<br />
David S. Zealear, MD<br />
1955, California<br />
Leonard L. Zinker, MD<br />
1962, Florida<br />
Volume 14, Number 4 • AANS Bulletin 49
C ODING C ORNER<br />
G REGORY J .<br />
P RZYBYLSKI, MD<br />
Coding Changes for CPT 2006<br />
Payers May Lag Behind Jan. 1 Implementation<br />
In the past 18 months, several codes have<br />
moved through the Current Procedural<br />
Terminology process, valuation by the<br />
Relative-value Update Committee and<br />
publication in the 2006 Medicare fee schedule.<br />
These codes include spinal incision and<br />
drainage, vertebral augmentation after cavity<br />
creation (kyphoplasty) and intracranial<br />
stenting. This Coding Corner will examine<br />
the new category I codes for 2006 as well as<br />
their valuation in relative value units, or<br />
RVUs, since Medicare payment is determined<br />
by a code's RVUs multiplied by the<br />
conversion factor. The deletion <strong>of</strong> several<br />
evaluation and management codes also<br />
will be addressed.<br />
The <strong>American</strong> Academy <strong>of</strong> Orthopaedic<br />
<strong>Surgeons</strong> requested the development<br />
<strong>of</strong> spinal incision and drainage codes<br />
to parallel similar codes that exist for<br />
extremity joints. After collaboration with<br />
the AANS, CNS and North <strong>American</strong> Spine<br />
Society, a pair <strong>of</strong> codes was developed to<br />
describe posterior incision and drainage <strong>of</strong><br />
a subfascial infection. Code 22010 (21.69<br />
facility RVUs) reflects posterior drainage <strong>of</strong><br />
a subfascial cervicothoracic abscess, whereas<br />
code 22015 (21.50 facility RVUs)<br />
described the same procedure in the lumbosacral<br />
region. Neither code should be<br />
reported with instrumentation removal<br />
(codes 22850 and 22852) or drainage <strong>of</strong> a<br />
complex postoperative wound (code<br />
10180, 4.59 facility RVUs), which was the<br />
only code available for this procedure<br />
before 2006.<br />
AANS and CNS Call for New<br />
Kyphoplasty Codes<br />
The AANS and CNS requested the development<br />
<strong>of</strong> codes to reflect vertebral augmentation<br />
after cavity creation and/or<br />
fracture reduction (kyphoplasty).<br />
Although similar codes for vertebroplasty<br />
were developed years earlier, the AANS<br />
and CNS requested a new set <strong>of</strong> codes to<br />
reflect the additional work <strong>of</strong> balloon<br />
kyphoplasty. Code 22523 (16.29 facility<br />
RVUs) reflects percutaneous vertebral<br />
augmentation, including cavity creation<br />
and biopsy, using a mechanical device in<br />
the thoracic spine. The code will be used<br />
once in an operative session, even if bilateral<br />
access is obtained. Additional levels <strong>of</strong><br />
kyphoplasty performed in either the thoracic<br />
or lumbar spine would be coded<br />
22525 (7.47 facility RVUs). If only lumbar<br />
vertebrae are treated, then the primary<br />
code used would be 22524 (15.61 facility<br />
RVUs). Although previously reimbursed<br />
at 50 percent more than vertebroplasty by<br />
some payers under the unlisted code<br />
22899, the survey process revealed only an<br />
incremental difference in physician work<br />
when comparing intraoperative work for<br />
vertebroplasty and kyphoplasty.<br />
If the surgeon uses image guidance, the<br />
supervision and interpretation <strong>of</strong> the<br />
imaging is to be separately reported. The<br />
imaging codes for vertebroplasty were<br />
revised to include kyphoplasty as well.<br />
Code 76012–26 (1.88 facility RVUs) would<br />
be used for guidance by fluoroscopy,<br />
whereas code 76013–26 (1.93 facility RVU)<br />
would be used for computed tomographic<br />
guidance. The modifier –26 is appended<br />
when the surgeon does not own the equipment,<br />
but rather is only providing the pr<strong>of</strong>essional<br />
component <strong>of</strong> the service. A<br />
radiology report must be dictated to reflect<br />
the supervision and interpretation <strong>of</strong> the<br />
radiological procedure, but it may be<br />
included in the operative note as a separate<br />
and distinct paragraph. Alternatively, a<br />
completely separate radiology report may<br />
be dictated.<br />
A series <strong>of</strong> five endovascular treatment<br />
codes also was developed to reflect recent<br />
innovations in intracranial endovascular<br />
procedures. Code 61630 describes<br />
intracranial balloon angioplasty, whereas<br />
61635 describes placement <strong>of</strong> an intracranial<br />
stent including balloon angioplasty, if<br />
necessary. Both codes include all selective<br />
vessel catheterization and diagnostic imaging<br />
including supervision and interpretation<br />
<strong>of</strong> the images obtained. For treatment<br />
<strong>of</strong> vasospasm, code 61640 describes balloon<br />
dilatation on the initial vessel in vasospasm,<br />
whereas 61641 reflects each additional vessel<br />
treated in the same vascular family and<br />
61642 each additional vessel in a different<br />
vascular family. Likewise, the selective vessel<br />
catheterization and diagnostic imaging<br />
including supervision and interpretation <strong>of</strong><br />
the images is included. Unfortunately, the<br />
Centers for Medicare and Medicaid Services<br />
have identified these as non-covered<br />
services and did not publish RVU values.<br />
Redundant E&M Codes Eliminated<br />
In addition, several evaluation and management<br />
codes have been eliminated for<br />
2006. Three follow-up inpatient consultation<br />
codes (99261–99263) will now be<br />
reported as subsequent hospital care<br />
(99231–99233). The former codes were<br />
felt to be redundant with the subsequent<br />
hospital care codes, which will now be<br />
used for any subsequent E&M service provided<br />
after an inpatient consultation<br />
(99251– 99255). Similarly, the confirmatory<br />
consultation codes (99271–99275) will<br />
now be reported as an outpatient consultation<br />
(99241–99245). The confirmatory<br />
consultation codes were also deemed<br />
redundant. If a third-party payer requests<br />
the consultation, the –32 mandated services<br />
modifier should be appended to the<br />
outpatient consultation code.<br />
Note that although the codes become<br />
valid on Jan. 1, it can take payers as long as<br />
six months to recognize the new changes. 3<br />
Gregory J. Przybylski, MD, is pr<strong>of</strong>essor and director<br />
<strong>of</strong> neurosurgery at JFK Medical Center in Edison, N.J.<br />
He is co-chair <strong>of</strong> the AANS/CNS Coding and<br />
Reimbursement Committee and a member <strong>of</strong> the<br />
CMS Practicing Physicians Advisory Council, and he<br />
plans and instructs coding courses for the AANS and<br />
the North <strong>American</strong> Spine Society.<br />
50 AANS Bulletin • www.AANS.org
E<br />
E VENTS<br />
S<br />
Calendar <strong>of</strong> Neurosurgical Events<br />
ACI’s 7th National Conference on<br />
Adding, Updating & Expanding<br />
Neuroscience Centers <strong>of</strong> Excellence<br />
Jan. 26–27, 2006<br />
Phoenix, Ariz.<br />
(312) 780-0700<br />
www.acius.net<br />
Update in EEG, EMG and Clinical<br />
Neurophysiology 2006<br />
Jan. 29–Feb. 4, 2006<br />
Scottsdale, Ariz.<br />
(480) 301-4580<br />
www.mayo.edu/cme<br />
Richard Lende Winter Neurosurgery<br />
Conference +<br />
Feb. 3–8, 2006<br />
Snowbird, Utah<br />
(801) 581-6554<br />
www.lendemeeting.com<br />
Neurology Neurosurgery<br />
Interface 2006<br />
Feb. 17–19, 2006<br />
San Juan, Puerto Rico<br />
(215) 898-6400<br />
www.med.upenn.edu/cme<br />
Joint Annual Meeting <strong>of</strong> the AANS/CNS<br />
Cerebrovascular Section and the<br />
<strong>American</strong> Society <strong>of</strong> Interventional &<br />
Therapeutic Neuroradiology +<br />
Feb. 17–20, 2006<br />
Orlando, Fla.<br />
(888) 566-2267<br />
www.neurosurgery.org/cv<br />
44th Annual Dr. Kenneth M. Earle<br />
Memorial Neuropathology<br />
Re<strong>view</strong> Course<br />
Feb. 20–24, 2006<br />
Bethesda, Md.<br />
(202) 782-2637<br />
www.afip.org/Departments/<br />
edu/coursehtm/06neuro<br />
path.htm<br />
22nd Annual Meeting <strong>American</strong><br />
Academy <strong>of</strong> Pain Medicine<br />
Feb. 22–25, 2006<br />
San Diego, Calif.<br />
(847) 375-4731<br />
www.painmed.org/<br />
annualmeeting<br />
Carotid Interventional:<br />
Interactive Seminar and Live<br />
Demonstration +<br />
Feb. 27–28, 2006<br />
Buffalo, N.Y.<br />
(716) 887-5200 x2135<br />
Current Topics in Neurosurgery:<br />
Meet the Experts<br />
Feb. 27–March 5, 2006<br />
San Juan, Puerto Rico<br />
(732) 235-7430<br />
www.umdnj.edu<br />
Southern Neurosurgical Society<br />
Annual Meeting +<br />
March 2–5, 2006<br />
Southampton, Bermuda<br />
www.southernneurosurgery.org<br />
International Spine & Spinal<br />
Injuries Conference<br />
March 3–5, 2006<br />
New Delhi, India<br />
www.scs-isic.com<br />
Interurban Neurosurgical Society<br />
Annual Scientific Meeting +<br />
March 3, 2006<br />
Chicago, Ill.<br />
(715) 542-3201<br />
mrakow@frontiernet.net<br />
2nd Annual Update Symposium<br />
Series on Clinical Neurology<br />
and Neurophysiology<br />
March 6–8, 2006<br />
Jerusalem, Israel<br />
www.isas.co.il/<br />
neurophysiology2006.com<br />
21st Annual Meeting <strong>of</strong> the<br />
AANS/CNS Section on Disorders <strong>of</strong><br />
the Spine and Peripheral Nerves +<br />
March 15–18, 2006<br />
Lake Buena Vista, Fla.<br />
www.spinesection.org/<br />
MeetingsEd.htm<br />
Carotid Intervention:<br />
Interactive Seminar With Live<br />
Demonstration Simulation +<br />
March 27–28, 2006<br />
Buffalo, N.Y.<br />
(716) 887-5200 x2135<br />
58th Annual Meeting <strong>American</strong><br />
Academy <strong>of</strong> Neurology<br />
April 1–8, 2006<br />
San Diego, Calif.<br />
www.aan.com<br />
3rd State <strong>of</strong> the Art in<br />
Chronic Low Back Pain<br />
Symposium<br />
April 9–12, 2006<br />
Bodrum, Turkey<br />
www.vitalmedbodrum.com<br />
2006 AANS/CNS Section on<br />
Pain Surgery Annual Meeting +<br />
April 21, 2006<br />
San Francisco, Calif. <br />
(888) 566-2267<br />
www.neurosurgery.org/pain<br />
2006 AANS Annual Meeting<br />
April 22–27, 2006<br />
San Francisco, Calif.<br />
(888) 566-2267<br />
www.AANS.org<br />
<strong>American</strong> Society <strong>of</strong> Neuroradiology<br />
44th Annual Meeting<br />
April 29–May 5, 2006<br />
San Diego, Calif.<br />
(630) 574-0220<br />
www.asnr.org<br />
Carotid Intervention: Interactive<br />
Seminar with Live Demonstration<br />
and Simulation +<br />
May 1–2, 2006<br />
Buffalo, N.Y.<br />
(716) 887-5200 x2135<br />
The Society <strong>of</strong> <strong>Neurological</strong> <strong>Surgeons</strong><br />
Annual Meeting<br />
May 21–23, 2006<br />
Durham, N.C.<br />
www.societyns.org<br />
18th Annual International Bethesda<br />
Spine & Peripheral Nerve Workshop<br />
May 31–June 6, 2006<br />
www.bethesdaspine.com<br />
<strong>American</strong> Society for Stereotactic and<br />
Functional Neurosurgery<br />
June 1–4, 2006<br />
Boston, Mass.<br />
www.assfn.org<br />
9th International Conference on<br />
Cerebral Vasospasm<br />
June 27–30, 2006<br />
Istanbul, Turkey<br />
www.cerebralvasospasm9.org<br />
Computer Assisted Radiology and<br />
Surgery (CARS 2006)<br />
June 28–July 1, 2006<br />
Osaka, Japan<br />
www.cars-int.org<br />
12th Computed Maxill<strong>of</strong>acial<br />
Imaging Congress<br />
June 28–July 1, 2006<br />
Osaka, Japan<br />
www.cars-int.org<br />
+ These meetings are jointly sponsored or cosponsored by the <strong>American</strong> <strong>Association</strong> <strong>of</strong> <strong>Neurological</strong> <strong>Surgeons</strong>. The frequently<br />
updated online meetings calendar and continuing medical education information are available at www.aans.org/education.<br />
AANS Courses<br />
For information or to register call (888) 566-AANS<br />
or visit www.aans.org/education.<br />
3 Managing Coding & Reimbursement Challenges<br />
in Neurosurgery<br />
*“Coding for Pros” prerequisite: AANS coding course taken<br />
within two years.<br />
Jan. 27–28, 2006 . . . . . . . . .Las Vegas, Nev.<br />
Feb. 17–18, 2006* . . . . .San Antonio, Texas<br />
March 3–4, 2006 .St. Pete Beach/Tampa, Fla.<br />
May 5–6, 2006* . . . . . . . . .Philadelphia, Pa.<br />
Sept. 8–9, 2006 . . . . . . . . . . . . .Chicago, Ill.<br />
Nov. 3–4, 2006* . . . . . . . .Los Angeles, Calif.<br />
3 Neurosurgery Re<strong>view</strong> by Case Management:<br />
Oral Board Preparation<br />
May 7–9, 2006 . . . . . . . . . . .Houston, Texas<br />
Nov. 5–7, 2006 . . . . . . . . . . .Houston, Texas<br />
3 Current Advances in Spinal Fixation:<br />
Advanced Course<br />
Feb. 11–12, 2006 Memphis, Tenn.<br />
3 Minimally Invasive Spinal Techniques<br />
June 10–11, 2006 . . . . . . . . . .St. Louis, Mo.<br />
3 Neurosurgical Practice Management:<br />
Improving the Financial Health <strong>of</strong> Your Practice<br />
May 7, 2006 . . . . . . . . . . . .Philadelphia, Pa.<br />
Sept. 10, 2006 . . . . . . . . . . . . . .Chicago, Ill.<br />
Volume 14, Number 4 • AANS Bulletin<br />
51
AANSA NSWERS<br />
T HOMAS A. MARSHALL<br />
AANS LEADERSHIP 2005–2006<br />
OFFICERS<br />
Fremont P. Wirth, MD, president<br />
Donald O. Quest, MD, president-elect<br />
Robert L. Grubb Jr., MD, vice-president<br />
Jon H. Robertson, MD, secretary<br />
James R. Bean, MD, treasurer<br />
Robert A. Ratcheson, MD, past president<br />
DIRECTORS AT LARGE<br />
Robert E. Harbaugh, MD<br />
Christopher M. L<strong>of</strong>tus, MD<br />
James T. Rutka, MD<br />
Warren R. Selman, MD<br />
Troy M. Tippett, MD<br />
REGIONAL DIRECTORS<br />
Jeffrey W. Cozzens, MD<br />
Paul E. Spurgas, MD<br />
Clarence B. Watridge, MD<br />
Edie E. Zusman, MD<br />
HISTORIAN<br />
Eugene S. Flamm, MD<br />
EX-OFFICIO<br />
Rick Abbott, MD<br />
Lawrence S. Chin, MD<br />
Fernando G. Diaz, MD<br />
Robert F. Heary, MD<br />
Andres M. Lozano, MD<br />
Dennis E. McDonnell, MD<br />
Richard K. Osenbach, MD<br />
Robert H. Rosenwasser, MD<br />
Alex B. Valadka, MD<br />
Ronald E. Warnick, MD<br />
LIAISONS<br />
Isabelle M. Germano, MD<br />
Mark G. Hamilton, MD<br />
Nelson M. Oyesiku, MD<br />
AANS EXECUTIVE OFFICE<br />
5550 Meadowbrook Drive<br />
Rolling Meadows, IL 60008<br />
Phone: (847) 378-0500<br />
(888) 566-AANS<br />
Fax: (847) 378-0600<br />
E-mail: info@AANS.org<br />
Web site: www.AANS.org<br />
Thomas A. Marshall, executive director<br />
Ronald W. Engelbreit, CPA,<br />
deputy executive director<br />
Susan M. Eget, associate executive<br />
director-governance<br />
Joni L. Shulman, associate executive<br />
director-education & meetings<br />
DEPARTMENTS<br />
Communications, Betsy van Die<br />
Development, Michele S. Gregory<br />
Information Services, Anthony P. Macalindong<br />
Marketing, Kathleen T. Craig<br />
Meeting Services, Patty L. Anderson<br />
Member Services, Chris A. Philips<br />
AANS/CNS WASHINGTON OFFICE<br />
725 15th Street, NW, Suite 800<br />
Washington, DC 20005<br />
Phone: (202) 628-2072<br />
Fax: (202) 628-5264<br />
Web site: www.aans.org/legislative/<br />
aans/washington_c.asp<br />
AANS Serves Up Success<br />
Table’s Already Set for Increased Innovation<br />
The fiscal 2004–2005 year-end report was<br />
presented to the AANS Board <strong>of</strong> Directors<br />
at its November 2005 meeting. The<br />
report affirmed that for the fourth consecutive<br />
year, the AANS enjoyed an extremely<br />
favorable cycle <strong>of</strong> financial stability and growth <strong>of</strong><br />
services to its members. In fact, this marks the<br />
first time in the organization’s records that the<br />
AANS has enjoyed four consecutive years “in the<br />
black” since its founding 75 years ago.<br />
What is evident is that the AANS successfully<br />
weathered a series <strong>of</strong> internal and external<br />
upheavals that most organizations rarely must<br />
confront separately, let alone simultaneously, in<br />
the final years <strong>of</strong> the 1990s and the initial years <strong>of</strong><br />
this decade.<br />
In the late 1990s, the budget was losing<br />
between $3 million and $5 million annually, there<br />
was a management revolving door <strong>of</strong> three AANS<br />
executive directors hired successively in 1998,<br />
1999 and 2000, and the Executive Office staff,<br />
while somewhat inflated in number, was turning<br />
over at a rate <strong>of</strong> 117 percent in 2000 and 2001.<br />
Though daunting, these management challenges<br />
were not the real cause for concern. Far<br />
more ominous clouds threatened, not on the horizon,<br />
but directly overhead.<br />
The AANS had become dangerously reliant on<br />
only two very undependable sources <strong>of</strong> income for<br />
its operations: the annual meeting and membership<br />
dues. Not only could earthquake, terrorist<br />
attack, or, as we just saw in New Orleans, devastating<br />
flood wipe out the former, the AANS was not<br />
even systematically and consistently collecting the<br />
latter. The only thing that was consistent about the<br />
dues was that they were raised every year as a budgetary<br />
matter <strong>of</strong> course to reflect a cost-<strong>of</strong>-living<br />
increase. (Dues have not been raised in the last four<br />
consecutive successful fiscal years).<br />
Given what the organization faced at the time,<br />
how the AANS has reached the levels <strong>of</strong> stability<br />
and service that you enjoy today as a member is<br />
worth truly understanding.<br />
While it is true that dramatic restructuring,<br />
downsizing and spending cuts at the front end<br />
Thomas A. Marshall<br />
is AANS<br />
executive director.<br />
paved the road to recovery, those key decisions are<br />
already enjoying too much <strong>of</strong> the focus and credit.<br />
Critical as those strategies were, they were only<br />
the “table setting” for the success that followed.<br />
The reasons behind today’s success can be<br />
attributed to far more than the belt-tightening<br />
tactics <strong>of</strong> five years ago. Crucial to this success is<br />
that simultaneously the AANS augmented a<br />
thoughtfully chosen menu <strong>of</strong> new, and at least for<br />
the AANS, unproven revenue streams: the expansion<br />
<strong>of</strong> educational programming; the development<br />
<strong>of</strong> products and services based upon<br />
accurate assessment <strong>of</strong> what you, the member,<br />
told us you wanted; the revision <strong>of</strong> organizational<br />
policies covering dues, investment revenue, and a<br />
cash reserve; and the measured outreach to a variety<br />
<strong>of</strong> allied publics who had an interest in the<br />
health <strong>of</strong> neurosurgery and its most diversified<br />
membership association.<br />
Five years’ worth <strong>of</strong> AANS leadership and staff<br />
can take pride in the success <strong>of</strong> those basic strategies.<br />
But it was always the AANS members who<br />
were the intended ultimate beneficiaries <strong>of</strong> those<br />
early decisions.<br />
At a time when most organizations would seek<br />
shelter to ride out the fiscal, structural and philosophical<br />
storm, the decisions to propel the AANS<br />
into a proactive production mode were critical to<br />
providing better and expanded services to AANS<br />
members. This proactive mode is the core <strong>of</strong><br />
AANS’ strategic planning for the latter half <strong>of</strong> this<br />
decade and well beyond. The new and improved<br />
AANS is an organization ready to move forward<br />
in the 21st century with innovative programming<br />
for its members, and positioned to launch the specialty<br />
to new heights. 3<br />
52 AANS Bulletin • www.AANS.org