Drugs Used to Treat Spasticity - UNMC
Drugs Used to Treat Spasticity - UNMC
Drugs Used to Treat Spasticity - UNMC
You also want an ePaper? Increase the reach of your titles
YUMPU automatically turns print PDFs into web optimized ePapers that Google loves.
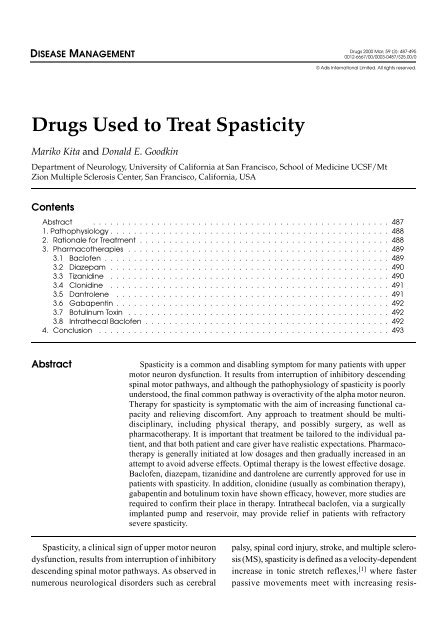
DISEASE MANAGEMENT<br />
<strong>Drugs</strong> 2000 Mar; 59 (3): 487-495<br />
0012-6667/00/0003-0487/$25.00/0<br />
© Adis International Limited. All rights reserved.<br />
<strong>Drugs</strong> <strong>Used</strong> <strong>to</strong> <strong>Treat</strong> <strong>Spasticity</strong><br />
Mariko Kita and Donald E. Goodkin<br />
Department of Neurology, University of California at San Francisco, School of Medicine UCSF/Mt<br />
Zion Multiple Sclerosis Center, San Francisco, California, USA<br />
Contents<br />
Abstract . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 487<br />
1. Pathophysiology . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 488<br />
2. Rationale for <strong>Treat</strong>ment . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 488<br />
3. Pharmacotherapies . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 489<br />
3.1 Baclofen . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 489<br />
3.2 Diazepam . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 490<br />
3.3 Tizanidine . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 490<br />
3.4 Clonidine . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 491<br />
3.5 Dantrolene . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 491<br />
3.6 Gabapentin . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 492<br />
3.7 Botulinum Toxin . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 492<br />
3.8 Intrathecal Baclofen . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 492<br />
4. Conclusion . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 493<br />
Abstract<br />
<strong>Spasticity</strong> is a common and disabling symp<strong>to</strong>m for many patients with upper<br />
mo<strong>to</strong>r neuron dysfunction. It results from interruption of inhibi<strong>to</strong>ry descending<br />
spinal mo<strong>to</strong>r pathways, and although the pathophysiology of spasticity is poorly<br />
unders<strong>to</strong>od, the final common pathway is overactivity of the alpha mo<strong>to</strong>r neuron.<br />
Therapy for spasticity is symp<strong>to</strong>matic with the aim of increasing functional capacity<br />
and relieving discomfort. Any approach <strong>to</strong> treatment should be multidisciplinary,<br />
including physical therapy, and possibly surgery, as well as<br />
pharmacotherapy. It is important that treatment be tailored <strong>to</strong> the individual patient,<br />
and that both patient and care giver have realistic expectations. Pharmacotherapy<br />
is generally initiated at low dosages and then gradually increased in an<br />
attempt <strong>to</strong> avoid adverse effects. Optimal therapy is the lowest effective dosage.<br />
Baclofen, diazepam, tizanidine and dantrolene are currently approved for use in<br />
patients with spasticity. In addition, clonidine (usually as combination therapy),<br />
gabapentin and botulinum <strong>to</strong>xin have shown efficacy, however, more studies are<br />
required <strong>to</strong> confirm their place in therapy. Intrathecal baclofen, via a surgically<br />
implanted pump and reservoir, may provide relief in patients with refrac<strong>to</strong>ry<br />
severe spasticity.<br />
<strong>Spasticity</strong>, a clinical sign of upper mo<strong>to</strong>r neuron<br />
dysfunction, results from interruption of inhibi<strong>to</strong>ry<br />
descending spinal mo<strong>to</strong>r pathways. As observed in<br />
numerous neurological disorders such as cerebral<br />
palsy, spinal cord injury, stroke, and multiple sclerosis<br />
(MS), spasticity is defined as a velocity-dependent<br />
increase in <strong>to</strong>nic stretch reflexes, [1] where faster<br />
passive movements meet with increasing resis-
488 Kita & Goodkin<br />
tance. A clasp-knife phenomenon may be seen with<br />
dissipation of resistance during stretch. Additional<br />
signs associated with spasticity include weakness,<br />
increased muscle <strong>to</strong>ne, impaired dexterity and coordination,<br />
hyper-reflexia, extensor plantar responses,<br />
spontaneous muscle spasms, and contractures.<br />
[2] <strong>Spasticity</strong> worsens in the setting of<br />
noxious stimuli such as infection, urolithiasis, urinary<br />
or faecal retention, decubitus ulcers, tight or<br />
misfitting clothing or misfitting orthotics. The<br />
symp<strong>to</strong>ms of spasticity can greatly interfere with a<br />
patient’s functional capacity.<br />
1. Pathophysiology<br />
The pathophysiology of spasticity is poorly unders<strong>to</strong>od<br />
but the final common pathway underlying<br />
the mechanism is overactivity of the alpha mo<strong>to</strong>r<br />
neuron. Descending spinal pathways (corticospinal,<br />
reticulospinal, vestibulospinal) exert control over<br />
alpha mo<strong>to</strong>r neurons via mono- and poly-synaptic<br />
pathways.<br />
The muscle spindle is the complex sensory structure<br />
of the muscle conveying information about<br />
muscle length. Spindles lie in parallel with extrafusal<br />
fibres (large muscle fibres that effect gross<br />
movement), so when the muscle is lengthened, the<br />
spindle is stretched causing Ia afferent fibres <strong>to</strong><br />
send impulses <strong>to</strong> the spinal cord. Shortening of the<br />
extrafusal muscle results in shortening of the spindle<br />
and silencing of the Ia afferents. The intrafusal<br />
muscle fibres of the spindle complex are innervated<br />
by gamma mo<strong>to</strong>r neurons in the anterior<br />
horns of the spinal cord, which act <strong>to</strong> increase the<br />
tension of the intrafusal fibre when it is shortened.<br />
This resets the spindle after shortening so it is again<br />
sensitive <strong>to</strong> changes in muscle length.<br />
When the muscle is lengthened by tendon tap or<br />
stretch, Ia afferents produce excita<strong>to</strong>ry postsynaptic<br />
potentials (EPSPs) on agonist mo<strong>to</strong>neurons. Although<br />
this monosynaptic connection plays a role<br />
in the reflex, most excita<strong>to</strong>ry activity in the stretch<br />
reflex is mediated by oligosynaptic and polysynaptic<br />
pathways. [2] Interneurons play a major role in<br />
the reflex arc. Antagonist muscle spindles also send<br />
Ia afferents <strong>to</strong> produce EPSPs on agonist interneurons<br />
which subsequently produce inhibi<strong>to</strong>ry postsynaptic<br />
potentials (IPSPs) on mo<strong>to</strong>neurons. The<br />
firing of the mo<strong>to</strong>neuron depends on the summation<br />
of EPSPs and IPSPs. Additional inhibi<strong>to</strong>ry interneurons<br />
act on Ia afferents <strong>to</strong> produce a presynaptic<br />
inhibition of the afferent signal. γ-Aminobutyric<br />
acid (GABA) is the neurotransmitter involved in<br />
this selective presynaptic inhibition.<br />
Thus, the spinal segmental reflexes require the<br />
participation of muscle spindles, fusimo<strong>to</strong>r innervation<br />
(gamma mo<strong>to</strong>r neurons), Ia primary afferents,<br />
and alpha mo<strong>to</strong>r neurons, as well as Renshaw<br />
recurrent inhibition, disynaptic reciprocal inhibition,<br />
nonreciprocal au<strong>to</strong>genic Ib inhibition, presynaptic<br />
inhibition and remote inhibition/excitation of alpha<br />
mo<strong>to</strong>r neurons. [2] <strong>Spasticity</strong> results from a prolonged<br />
disinhibition of components of this system<br />
but the exact mechanism remains unclear.<br />
2. Rationale for <strong>Treat</strong>ment<br />
The goal of therapy is <strong>to</strong> increase functional capacity<br />
and relieve discomfort. Before initiating treatment<br />
one must first evaluate the functional consequences<br />
of reducing spasticity. For some patients<br />
with proximal leg weakness, increased extensor<br />
<strong>to</strong>ne in the legs offers necessary stability and support<br />
during transferring and walking. For other patients,<br />
hyper-reflexia and clonus interfere with normal<br />
ambulation. In non-ambula<strong>to</strong>ry patients, flexor<br />
spasms may be painful and debilitating. Patients<br />
with spasticity may exhibit further increase in <strong>to</strong>ne<br />
or spontaneous spasm in the setting of an underlying<br />
infection, such as a urinary tract infection, or<br />
other noxious stimulus. These secondary causes<br />
should be ruled out before altering a given therapeutic<br />
regimen. The approach <strong>to</strong> treating spasticity<br />
should be multimodal. Physical therapy is an essential<br />
component of antispasticity regimens and<br />
in the most patients with refrac<strong>to</strong>ry spasticity, surgical<br />
intervention (e.g. posterior rhizo<strong>to</strong>my or tendon<br />
release procedures) may be beneficial. In this<br />
review we will focus on pharmacological treatment<br />
of spasticity.<br />
© Adis International Limited. All rights reserved. <strong>Drugs</strong> 2000 Mar; 59 (3)
Drug <strong>Treat</strong>ment of <strong>Spasticity</strong> 489<br />
3. Pharmacotherapies<br />
Medications frequently used in the treatment of<br />
spasticity include baclofen, benzodiazepines, tizanidine,<br />
clonidine, dantrolene, gabapentin, and botulinum<br />
<strong>to</strong>xin. Of these, only baclofen, diazepam,<br />
tizanidine and dantrolene are approved for the<br />
treatment of spasticity. A general rule is <strong>to</strong> initiate<br />
treatment at low dosages and <strong>to</strong> increase them<br />
gradually <strong>to</strong> avoid adverse effects. The lowest dosage<br />
that proves <strong>to</strong> be effective for an individual<br />
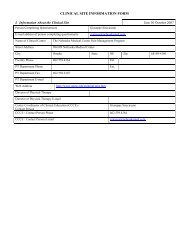
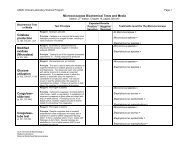
patient is considered optimal. Table I outlines the<br />
use of frequently used oral antispasticity agents.<br />
3.1 Baclofen<br />
Baclofen is a structural analogue of GABA, and<br />
inhibits monosynaptic and polysynaptic spinal reflexes.<br />
It binds <strong>to</strong> the GABA B recep<strong>to</strong>r which is<br />
coupled <strong>to</strong> calcium and potassium channels, and<br />
occurs both pre and postsynaptically. [3] By binding<br />
at the presynaptic site the membrane is hyperpolarised,<br />
and influx of calcium in<strong>to</strong> presynaptic<br />
terminals is restricted resulting in a decrease in<br />
neurotransmitter release in excita<strong>to</strong>ry spinal pathways<br />
and a decrease in alpha mo<strong>to</strong>r neuron activity.<br />
[4] In addition, postsynaptic binding on the Ia<br />
afferent terminal increases potassium conductance,<br />
hyperpolarising the membrane and enhancing the<br />
presynaptic inhibition. Activation of GABA B recep<strong>to</strong>rs<br />
may also result in inhibition of gamma mo<strong>to</strong>r<br />
neuron activity and decreased muscle spindle<br />
sensitivity. [5]<br />
Several trials have examined the efficacy of<br />
baclofen in patients with spasticity secondary <strong>to</strong><br />
MS and spinal cord pathology. [6-14] In the patients<br />
with MS, baclofen has been found <strong>to</strong> be effective<br />
in reducing spasticity, decreasing frequency and<br />
severity of sudden painful spasms, and improving<br />
the range of joint movement. However, increased<br />
weakness was a common complaint. In patients with<br />
spinal cord injuries, baclofen has been reported <strong>to</strong><br />
be particularly helpful in reducing flexor spasms.<br />
In post-stroke patients, it appears <strong>to</strong> be less beneficial.<br />
[15,16] Specifically, patients were found <strong>to</strong> have<br />
amodestdecreaseinmuscle<strong>to</strong>newhichwasinterpreted<br />
subjectively as only a slight improvement<br />
Table I. Oral agents commonly used <strong>to</strong> treat spasticity<br />
Agent Starting dosage Maximum recommended<br />
dosage<br />
Baclofen 5 mg/day<br />
80 mg/day in divided doses Muscle weakness,<br />
increasing<strong>to</strong>15<br />
sedation, fatigue,<br />
mg/day in 3 divided<br />
dizziness, nausea<br />
doses<br />
Diazepam 2 mg/day bid or 5<br />
mg qhs<br />
40-60 mg/day in divided<br />
doses<br />
Adverse effects Moni<strong>to</strong>ring Special attention<br />
Sedation, cognitive<br />
impairment, depression<br />
Tizanidine 2-4 mg/day 36 mg/day in divided doses Drowsiness, dry mouth,<br />
dizziness, reversible<br />
dose-related elevated<br />
liver transaminases<br />
Clonidine 0.1 mg/day Not approved for spasticity;<br />
in patients with hypertension,<br />
doses as high as 2.4mg in<br />
divided doses have been<br />
studied but rarely employed;<br />
Usual dose in hypertension<br />
0.2-0.6 mg/day<br />
Bradycardia, hypotension,<br />
dry mouth, drowsiness,<br />
constipation, dizziness,<br />
depression<br />
Dantrolene 25 mg/day 400 mg/day in divided doses Hepa<strong>to</strong><strong>to</strong>xicity (potentially<br />
irreversible), weakness,<br />
sedation, diarrhoea<br />
Gabapentin 100mg tid 3600 mg/day in divided doses S<strong>to</strong>mach upset<br />
bid = twice daily; qhs = at bedtime; tid = three times daily.<br />
Periodic liver<br />
function tests<br />
Dependence<br />
potential<br />
Periodic liver<br />
function tests<br />
Periodic liver<br />
function tests<br />
Abrupt cessation<br />
associated with<br />
seizures<br />
Withdrawal<br />
syndrome<br />
Not<strong>to</strong>beusedwith<br />
antihypertensives<br />
or clonidine<br />
Add-on agent<br />
Hypotension may<br />
result<br />
Not<strong>to</strong>beusedwith<br />
tizanidine<br />
Hepa<strong>to</strong><strong>to</strong>xicity<br />
© Adis International Limited. All rights reserved. <strong>Drugs</strong> 2000 Mar; 59 (3)
490 Kita & Goodkin<br />
in the feeling of stiffness. No effect was noted on<br />
hyper-reflexia or clonus. [16]<br />
Baclofen is rapidly absorbed after oral administration<br />
but CNS penetration is relatively limited.<br />
The mean half-life is fairly short with an average<br />
of approximately 3.5 hours. Because it is partially<br />
metabolised by the liver (15%) and excreted by the<br />
kidney, the dosage should be decreased in patients<br />
with known hepatic or renal impairment. There<br />
have been reports of elevated liver enzyme levels<br />
in patients receiving baclofen. As such, screening<br />
liver function tests should be performed when initiating<br />
treatment with baclofen and every 6 months<br />
thereafter. <strong>Treat</strong>ment is often initiated at 5mg once<br />
daily increasing <strong>to</strong> 3 times daily as <strong>to</strong>lerated. Thereafter,<br />
the dosage can be increased slowly at increments<br />
of 5mg/day as needed. It may be helpful <strong>to</strong><br />
initiate treatment and increments at night <strong>to</strong> minimise<br />
adverse effects. The highest recommended dosage<br />
is 80mg daily in divided doses, but for some<br />
patients, this dosage may not be sufficient <strong>to</strong> relieve<br />
symp<strong>to</strong>ms. Higher dosages should be prescribed<br />
with caution as adverse effects are likely <strong>to</strong><br />
be more prominent.<br />
Typical adverse effects are related <strong>to</strong> CNS depression<br />
and include drowsiness, fatigue, weakness,<br />
nausea, and dizziness. Abrupt cessation of sustained<br />
treatment should be avoided because sudden<br />
withdrawal of baclofen has been associated with<br />
hallucinations and seizures.<br />
3.2 Diazepam<br />
The action of the benzodiazepines is mediated<br />
by the coupling of the benzodiazepine-GABA A<br />
recep<strong>to</strong>r-chloride ionophore complex. [17] Binding<br />
of benzodiazepine <strong>to</strong> the GABA A recep<strong>to</strong>r increases<br />
chloride conductance resulting in presynaptic<br />
inhibition in the spinal cord. [18,19] Diazepam<br />
is the most commonly used benzodiazepine in the<br />
treatment of spasticity. Early trials have demonstrated<br />
efficacy in treating spasticity in patients<br />
with spinal cord injury, hemiplegia, and MS. [20-23]<br />
From and Heltberg [24] studied 17 patients with MS<br />
in a double-blind, crossover trial with baclofen and<br />
diazepam. Each patient received 4 weeks therapy<br />
with each drug. No differences were seen in efficacy<br />
of reducing spasticity, clonus, flexor spasms,<br />
or improvement in gait or bladder function. The<br />
adverse effect profiles differed slightly, with more<br />
patients reporting sedation while receiving diazepam,<br />
but the severity of adverse effects was similar<br />
in both groups. When patients, still masked <strong>to</strong> treatment<br />
assignment, were asked which agent they preferred,<br />
baclofen was significantly favoured. [24] Other<br />
studies have confirmed comparable antispasticity<br />
effects of baclofen and diazepam in reducing muscle<br />
<strong>to</strong>ne and frequency of spasms. However, baclofen<br />
was not necessarily favoured by patients over<br />
diazepam. [25,26] In clinical practice, diazepam is<br />
frequently used as an adjunct <strong>to</strong> baclofen in treating<br />
spasticity, [27] andislesscommonlyusedasasingle<br />
agent.<br />
Diazepam is well absorbed after oral administration<br />
and reaches a peak concentration after approximately<br />
1 hour. It is 98% protein-bound and is<br />
metabolised by the liver <strong>to</strong> active compounds nordazepam<br />
and oxazepam. In patients with hepatic<br />
dysfunction, initial dosages should be titrated carefully.<br />
Total half-life can range between 20 and 80<br />
hours. <strong>Treat</strong>ment may be initiated at 2mg twice<br />
daily increasing as needed <strong>to</strong> obtain a desired effect.<br />
Alternatively, single 5mg doses at night may be<br />
effective for nocturnal symp<strong>to</strong>ms. Adverse effects<br />
include sedation and cognitive impairment, and<br />
there is a potential for dependence. A withdrawal<br />
syndrome is associated with the benzodiazepines<br />
and abrupt cessation of diazepam has been associated<br />
with seizures.<br />
3.3 Tizanidine<br />
Tizanidine is an imidazole derivative and is a<br />
centrally acting α 2 -adrenergic agonist which inhibits<br />
the release of excita<strong>to</strong>ry amino acids in spinal<br />
interneurons. It may also act by facilitating the action<br />
of glycine. Tizanidine has demonstrated potent<br />
muscle relaxing properties in animal models of<br />
spasticity, [28] anditwasfound<strong>to</strong>suppressthepolysynaptic<br />
reflex in the spinal-transected cat. [29,30] In<br />
addition, tizanidine has been shown <strong>to</strong> enhance<br />
vibra<strong>to</strong>ry inhibition of the H-reflex in humans and<br />
© Adis International Limited. All rights reserved. <strong>Drugs</strong> 2000 Mar; 59 (3)
Drug <strong>Treat</strong>ment of <strong>Spasticity</strong> 491<br />
reduces abnormal co-contraction which may also,<br />
in part, contribute <strong>to</strong> antispasticity effects. [31] In<br />
placebo-controlled trials, tizanidine has been shown<br />
<strong>to</strong> reduce muscle <strong>to</strong>ne and frequency of muscle<br />
spasms in both patients with MS and spinal cord<br />
injury. [32-34] Similar efficacy was noted when tizanidine<br />
open-label was tested in patients who had<br />
experienced a stroke. [35] Although tizanidine was<br />
found <strong>to</strong> reduce spasticity without altering muscle<br />
strength, it has shown no consistent positive effect<br />
on functional measures, such as timed ambulation,<br />
upper extremity function or activities necessary in<br />
activities of daily living (ADLs). [32] When compared<br />
with baclofen or diazepam in early trials,<br />
tizanidine demonstrated similar efficacy and better<br />
<strong>to</strong>lerability. [30,33,36-43] When compared with baclofen,<br />
night-time insomnia was reported more frequently<br />
with tizanidine, and weakness was also reported<br />
but less frequently than with baclofen. [36]<br />
There have been no controlled trials investigating<br />
the use of tizanidine in combination with baclofen.<br />
Tizanidine undergoes first-pass hepatic metabolism<br />
and is subsequently eliminated by the kidney.<br />
Its half-life is approximately 2.5 hours and the peak<br />
effect is seen 1 <strong>to</strong> 2 hours after administration. Liver<br />
function tests should be checked at baseline, months<br />
1, 3 and 6 of treatment, and periodically thereafter.<br />
<strong>Treat</strong>ment is initiated at 2 <strong>to</strong> 4 mg/day, increasing<br />
every 3 days by 2 <strong>to</strong> 4 mg/day. The <strong>to</strong>tal dosage<br />
shouldnotexceed36mg/dayin3divideddoses.<br />
There is little experience with single doses greater<br />
than 8mg. Adverse effects include dry mouth (45%),<br />
drowsiness (54%) and dizziness, and were seen<br />
primarily when dosages exceeded 24 mg/day. Visual<br />
hallucinations (3%) and elevated liver function<br />
tests (5%) were reversible with dosage reduction.<br />
[32] Tizanidine has not been found <strong>to</strong> have<br />
consistent effects on blood pressure, but because<br />
of its central α 2 -adrenergic activity and risk of potential<br />
hypotension, concomitant use of antihypertensives,<br />
especially clonidine, should be avoided.<br />
3.4 Clonidine<br />
Clonidine is a centrally acting α 2 -adrenergic agonist<br />
that is frequently used <strong>to</strong> treat hypertension<br />
as well as opiate withdrawal. The central α-adrenergic<br />
activation is thought <strong>to</strong> decrease sympathetic<br />
outflow. Clonidine has been shown <strong>to</strong> decrease the<br />
vibra<strong>to</strong>ry inhibition index in patients with spinal<br />
cord injury, [44] <strong>to</strong> reduce muscle <strong>to</strong>ne in patients with<br />
brain injuries (stroke, trauma, haema<strong>to</strong>ma, cerebral<br />
palsy), [45] and has shown modest benefit as a<br />
supplement <strong>to</strong> baclofen. [46] Clonidine is rarely used<br />
as a single agent in the treatment of spasticity. It is<br />
available in 0.1mg tablets, but the patch formulation<br />
(0.1mg and 0.2mg) is designed <strong>to</strong> deliver the<br />
specified dose daily and must be changed every 7<br />
days. Adverse effects include bradycardia, hypotension,<br />
dry mouth, drowsiness, constipation, dizziness,<br />
and depression.<br />
3.5 Dantrolene<br />
Dantrolene is a hydan<strong>to</strong>in derivative. It acts directly<br />
on muscle contractile elements decreasing<br />
the release of Ca 2+ from skeletal muscle sarcoplasmic<br />
reticulum, which interferes with excitationcontraction<br />
coupling that is necessary <strong>to</strong> produce<br />
muscle contraction. [47-49] Theeffectismostpronounced<br />
on extrafusal fibres, but there is a minor<br />
effect on intrafusal fibres as well. Whether this effect<br />
may alter spindle sensitivity is unclear. [50]<br />
Dantrolene has a greater effect on fast-twitch fibres<br />
(those that produce rapid contraction and high tension,<br />
but fatigue relatively easily) than on slowtwitch<br />
fibres (those that contract <strong>to</strong>nically, producing<br />
less tension, but are more resistant <strong>to</strong> fatigue). [51]<br />
Placebo-controlled trials of dantrolene have<br />
demonstrated effective reduction of muscle <strong>to</strong>ne and<br />
hyper-reflexia. [49,52-54] When dantrolene was compared<br />
with diazepam in a double-blind, crossover<br />
designed trial in 42 patients with MS, both drugs<br />
were found <strong>to</strong> decrease spasticity, clonus and hyperreflexia,<br />
as well as diminish muscle stiffness and<br />
cramping. [55] Similar trials have been performed in<br />
children with cerebral palsy [56] and in patients with<br />
spasticity secondary <strong>to</strong> varying causes of cerebral<br />
and spinal disorders. [57] <strong>Spasticity</strong> was slightly better<br />
controlled with dantrolene than with diazepam<br />
and adverse effects were reported <strong>to</strong> be more <strong>to</strong>lerable<br />
with dantrolene.<br />
© Adis International Limited. All rights reserved. <strong>Drugs</strong> 2000 Mar; 59 (3)
492 Kita & Goodkin<br />
The half-life for oral dantrolene is approximately<br />
15 hours, with peak concentrations occurring<br />
within 3 <strong>to</strong> 6 hours. It is metabolised largely by the<br />
liver. Dantrolene therapy is initiated at 25 mg/day<br />
and slowly titrated upwards by increments of 25<br />
mg/day every 5 <strong>to</strong> 7 days, with a recommended<br />
maximum of 400 mg/day in divided doses. Because<br />
its site of action is peripheral, the most common<br />
adverse effect of dantrolene is weakness. For<br />
this reason, dantrolene may be most appropriate for<br />
those patients who are non-ambula<strong>to</strong>ry with severe<br />
spasticity. Other adverse effects include drowsiness,<br />
diarrhoea and malaise. Hepa<strong>to</strong><strong>to</strong>xicity, which<br />
can be irreversible, is the major concern with dantrolene<br />
and those patients who are being considered<br />
for therapy should have liver function tests<br />
checked prior <strong>to</strong> initiating therapy and on a regular<br />
basis (every 3 months) thereafter.<br />
3.6 Gabapentin<br />
Gabapentin was first introduced in 1994 as a<br />
new treatment option for patients with partial seizures.<br />
[58] It is structurally similar <strong>to</strong> GABA, exerting<br />
GABAnergic activity by binding recep<strong>to</strong>rs in<br />
the neocortex and hippocampus. However, it does<br />
not bind conventional GABA A , GABA B ,glycine,<br />
glutamate, benzodiazepine or N-methyl aspartate<br />
recep<strong>to</strong>rs. [59,60] It is easily absorbed, reaching peak<br />
plasma concentrations in 2 <strong>to</strong> 3 hours, it is not protein<br />
bound, does not undergo metabolism, and is<br />
excreted unchanged in the urine. It is well <strong>to</strong>lerated<br />
indosagesup<strong>to</strong>3600mg/day. [61] Recent studies<br />
and reports have suggested it might be effective as<br />
another <strong>to</strong>ol in treating spasticity [61,62] but further<br />
studies will be necessary <strong>to</strong> confirm efficacy.<br />
3.7 Botulinum Toxin<br />
Botulinum <strong>to</strong>xin is a product of Clostridium botulinum,<br />
and ingestion of the organism or its spores<br />
results in botulism. Botulinum <strong>to</strong>xin blocks presynaptic<br />
release of acetylcholine from the nerve<br />
terminal. Seven immunologically distinct <strong>to</strong>xins<br />
(type A through G) have been purified. Local intramuscular<br />
injection of botulinum <strong>to</strong>xin A has been<br />
approved for the treatment of strabismus and<br />
blepharospasm associated with dys<strong>to</strong>nia. When injected,<br />
the agent spreads through muscle and fascia<br />
approximately 30mm, binding presynaptic cholinergic<br />
nerve terminals, resulting in a chemical denervation.<br />
Botulinum <strong>to</strong>xin injection has been studied as a<br />
treatment for severe spasticity caused by stroke, traumatic<br />
brain injury and other causes, [63-66] and has<br />
been found <strong>to</strong> be effective in reducing muscle <strong>to</strong>ne<br />
and spasms. Snow et al. [67] studied botulinum <strong>to</strong>xin<br />
A in 9 patients with advanced MS (wheelchair- or<br />
bed-bound) in a randomised, crossover, doubleblind<br />
study. Muscle <strong>to</strong>ne, frequency of spasms and<br />
hygiene/self-care scores were used <strong>to</strong> assess efficacy.<br />
Botulinum <strong>to</strong>xin injection produced a significant<br />
reduction in spasticity and improvement in ease<br />
of nursing care, with no adverse effects. [67] Botulinium<br />
<strong>to</strong>xin injection was found <strong>to</strong> be a promising<br />
therapy for the treatment of spasticity in children<br />
with cerebral palsy. [68,69] Judicious use of botulinum<br />
<strong>to</strong>xin may permit surgery <strong>to</strong> be delayed until children<br />
reach a more suitable age.<br />
Although botulinum <strong>to</strong>xin injection is off-label<br />
for treatment of spasticity, it may be an appropriate<br />
option for selected patients with severe localised<br />
spasms. Physicians using botulinum <strong>to</strong>xin should<br />
be trained in its use with attention <strong>to</strong> relevant <strong>to</strong>pical<br />
ana<strong>to</strong>my and kinesiology. Onset of focal muscle<br />
fibre paralysis begins in 24 <strong>to</strong> 72 hours with a<br />
maximal effect seen at 5 <strong>to</strong> 14 days. The paralysis<br />
is transient lasting 12 <strong>to</strong> 16 weeks. Localising specific<br />
muscles with electromyographic guidance<br />
may be necessary <strong>to</strong> produce optimal effects. Injection<br />
site reactions can occur and antibodies may<br />
develop <strong>to</strong> specific immunological strains, thus<br />
limiting efficacy. Because the delivery of <strong>to</strong>xin is<br />
not entirely contained, the paralysis of muscles<br />
may not be exact. Excessive weakness, though ultimately<br />
reversible, may result.<br />
3.8 Intrathecal Baclofen<br />
When treatment with oral medication fails in a<br />
patient with persistent severe spasticity, intrathecal<br />
administrationofbaclofenshouldbeconsidered.A<br />
pump with reservoir is surgically implanted in the<br />
© Adis International Limited. All rights reserved. <strong>Drugs</strong> 2000 Mar; 59 (3)
Drug <strong>Treat</strong>ment of <strong>Spasticity</strong> 493<br />
subcutaneous tissue of the abdominal wall. A catheter<br />
is threaded in<strong>to</strong> the subarachnoid space allowing<br />
delivery of baclofen directly in<strong>to</strong> the CSF. This<br />
allows as much as 4 times the concentration of drug<br />
<strong>to</strong> be delivered at only 1% of the oral dosage, without<br />
concomitant elevation of serum concentrations,<br />
and thereby reducing unwanted cerebral adverse<br />
effects. [70] Penn et al. [70] conducted a double-blind,<br />
placebo-controlled, 3-day crossover study in 20<br />
patients (10 with MS and 10 with spinal cord injury).<br />
All patients had decreased muscle <strong>to</strong>ne and frequency<br />
of spasms while treated with baclofen. All<br />
patients were subsequently enrolled in a long term<br />
nonblind trial of continuous infusion, with a mean<br />
follow-up period of 19 months. Using the Ashworth<br />
scale [71,72] (a standardised scale <strong>to</strong> assess muscle<br />
<strong>to</strong>ne), all patients exhibited normal <strong>to</strong>ne and spasm<br />
frequency was diminished <strong>to</strong> the point that there<br />
was no interference with ADLs. Seven of 8 patients<br />
also experienced improvement in bladder function.<br />
[70] Others have found equally dramatic results.<br />
[73-75] Well <strong>to</strong>lerated and effective long term<br />
follow-uphasbeenreportedinpatientsup<strong>to</strong>84<br />
months. [76]<br />
Pump implantation is considered only after a<br />
patient undergoes a trial of intrathecal baclofen <strong>to</strong><br />
establish responsiveness. <strong>Treat</strong>ment is started at a<br />
dosage of 25 µg/day, increasing up <strong>to</strong> an average of<br />
400 <strong>to</strong> 500 µg/day, although dosages as high as<br />
1500 µg/dayhavebeenreported. [77] The half-life<br />
of intrathecal baclofen is approximately 5 hours.<br />
Many patients require increased dosages during<br />
the first 6 months’treatment and <strong>to</strong>lerance has been<br />
reported. [71,78] Most adverse effects tend <strong>to</strong> occur<br />
during the titration phase and include drowsiness,<br />
headache, nausea, weakness, and hypotension. Reversible<br />
coma has been reported in baclofen overdosing.<br />
[79] Other complications may be due <strong>to</strong> mechanical<br />
problems (dislodgment, disconnection,<br />
kinking, blockage), pump failure or infection. Intrathecal<br />
baclofen is a costly treatment and although<br />
useful, should only be considered in patients<br />
with severe functional limitations who have<br />
not responded satisfac<strong>to</strong>rily <strong>to</strong> other treatments.<br />
4. Conclusion<br />
As with any symp<strong>to</strong>matic therapy, the treatment<br />
of spasticity should be individualised. Goals for<br />
therapy and realistic expectations should be established<br />
by both care provider and patient. Conservative<br />
measures should be incorporated in<strong>to</strong> treatment<br />
regimens for spasticity. Stretching, massage<br />
and passive range of motion exercises are extremely<br />
important in preventing muscle shortening<br />
and the formation of contractures. Guidance on<br />
proper positioning and posture, as well as how <strong>to</strong><br />
avoid specific positions that may elicit clonus or<br />
spasms, can result in increasing functional. Patients<br />
should also be evaluated for adaptive equipment<br />
such as ambula<strong>to</strong>ry aids, reachers and other<br />
devices, and be instructed on the appropriate use<br />
of these <strong>to</strong>ols. Direct effects of muscle relaxation<br />
from physiotherapy are often short-lived and for<br />
many patients, these conservative measures alone<br />
are insufficient <strong>to</strong> treat their symp<strong>to</strong>ms. Most patients<br />
experience symp<strong>to</strong>matic improvement with<br />
physiotherapy in combination with one or more<br />
antispasticity agents. Patients refrac<strong>to</strong>ry <strong>to</strong> these<br />
treatment options may respond <strong>to</strong> intrathecal baclofen.<br />
An understanding of the mechanism of action<br />
of these therapies should aid in developing<br />
individualised regimens for patients.<br />
References<br />
1. Lance JW. Symposium synopsis. In: Feldman RG, Young RR,<br />
Koella WP, edi<strong>to</strong>rs. <strong>Spasticity</strong>: disordered mo<strong>to</strong>r control. Chicago<br />
(IL): Year Book Medical Publishers, 1980: 485-94<br />
2. Young RR. <strong>Spasticity</strong>: a review. Neurology 1994; 44 Suppl. 9:<br />
12S-20S<br />
3. Bormann J. Electrophysiology of Gaba-a and Gaba-b recep<strong>to</strong>r<br />
subtypes. Trends Neurol Sci 1988; 11: 112-6<br />
4. Davidoff RA. Antispasticity drugs: mechanism of action. Ann<br />
Neurol 1985; 17: 107-17<br />
5. Van Hemet JCJ. A double-blind comparison of baclofen and<br />
placebo in patients with spasticity of cerebral origin. In: Feldman<br />
RG, Young RR, Koella WP, edi<strong>to</strong>rs. <strong>Spasticity</strong>: disordered<br />
mo<strong>to</strong>r control. Chigaco (IL): Year Book Medical<br />
Publishers, 1980<br />
6. Jerusalem F. A double-blind study on the antispastic action of<br />
beta-(4-chlorophenyl)-gamma-amino butyric acid in multiple<br />
sclerosis, Nervenarzt 1968; 39: 515<br />
7. Jones RF, Burke D, Morasszeky JE, et al. A new agent for the<br />
control of spasticity. J Neurol Neurosurg Psychiatry 1970; 33:<br />
464-8<br />
8. Hudgson P, Weightman D. Baclofen in the treatment of spasticity.<br />
BMJ 1971; 4: 15-17<br />
© Adis International Limited. All rights reserved. <strong>Drugs</strong> 2000 Mar; 59 (3)
494 Kita & Goodkin<br />
9. Basmajan JV. Lioresal (baclofen) treatment of spasticity in multiple<br />
sclerosis. Am J Phys Med 1975; 54 (4): 175-7<br />
10. Duncan GW, Shahani BT, Young RR. An evaluation of baclofen<br />
treatment for certain symp<strong>to</strong>ms in patients with spinal cord<br />
lesions. Neurology 1976; 441: 446<br />
11. Levine IM, Jossmann PB, DeAngelis V. Lioresal, a new muscle<br />
relaxant in the treatment of spasticity: a double blind quantitative<br />
evaluation. Dis Nerv Sys 1977; 38: 1011-5<br />
12. Sawa GM, Paty DW. The use of baclofen in treatment of spasticity<br />
in multiple sclerosis. Can J Neurol Sci 1979; 6 (3): 351-4<br />
13. Hinderer SR, Lehman JF, Price R, et al. <strong>Spasticity</strong> in spinal cord<br />
injured persons: quantitative effects of baclofen and placebo<br />
treatments. Am J Phys Med Rehabil 1990; 69 (6): 311-7<br />
14. Smith CR, LaRocca NG, Giesser BS, et al. High dose oral baclofen:<br />
experience in patients with multiple sclerosis. Neurology<br />
1991; 41: 1829-31<br />
15. Pedersen E, Arlien-Soborg P, Mai J. The mode of action of the<br />
BAGA derivative baclofen in human spasticity. Acta Neurol<br />
Scand 1974; 50: 665-80<br />
16. Milanov IG. Mechanisms of baclofen action on spasticity. Acta<br />
Neurol Scand 1992; 85: 305-10<br />
17. Costa E, Guidotti A. Molecular mechanisms in the recep<strong>to</strong>r action<br />
of the benzodiazepines. Ann Rev Toxicol 1979; 19: 531-45<br />
18. Schwarz M, Turski L, Janiszewski W, et al. Is the muscle relaxant<br />
effect of diazepam in spastic mutant rats mediated through<br />
GABA-independent benzodiazepine recep<strong>to</strong>rs Neurosci Lett<br />
1983; 36: 175-80<br />
19. Pedersen E. Clinical assessment and pharmacologic therapy of<br />
spasticity. Arch Phys Med Rehabil 1974; 55: 344-54<br />
20. Kendall PH. The use of diazepam in hemiplegia. Ann Phys Med<br />
1964; 7: 225-8<br />
21. Neill RW. Diazepam in the relief of muscle spasm resulting<br />
from spinal-cord lesions. Ann Phys Med 1964; Suppl.: 33-8<br />
22. Nathan PW. The action of diazepam in neurological disorders<br />
with excessive mo<strong>to</strong>r activity. J Neurol Sci 1970; 10: 33-50<br />
23. Corbett M, Frankel HL, Michaelis L. A double-blind cross-over<br />
trial of valium in the treatment of spasticity. Paraplegia 1972;<br />
10: 19-22<br />
24. From A, Heltberg A. A double-blind trial with baclofen and<br />
diazepam in spasticity due <strong>to</strong> multiple sclerosis. Acta Neurol<br />
Scand 1975; 51: 158-66<br />
25. Roussan M, Terrence C, Fromm G. Baclofen versus diazepam<br />
for the treatment of spasticity and long term follow-up of<br />
baclofen therapy. Pharmatherapeutica 1987; 4 (5): 278-84<br />
26. Cartlidge NE, Hudgson P, Weightman D. A comparison of baclofen<br />
and diazepam in the treatment of spasticity. J Neurol Sci<br />
1974; 23: 17-24<br />
27. Mitchell G. Update on multiple sclerosis therapy. Med Clin<br />
North Am 1993; 77: 231-49<br />
28. Coward DM. Selective muscle relaxant properties of tizanidine<br />
and an examination of its mode of action. Triangle 1981; 20:<br />
151-58<br />
29. Davies J. Selective depression of synaptic transmission of spinal<br />
neurones in the cat by a new centrally acting muscle relaxant,<br />
5-chloro-4-(2-imidazolin-2-yl-amino)-2,1,3-benzothiadazole<br />
(DS 103 282). Br J Pharmacol 1982; 76: 473-81<br />
30. Newman PM, Nogues M, Newman PK, et al. Tizanidine in the<br />
treatment of spasticity. Eur J. Clin Pharmacol 1982; 23: 31-5<br />
31. Delwaide PJ. Electrophysiological testing of spastic patients:<br />
it’s potential usefulness and limitations. In: Delwaide PJ,<br />
Young RR edi<strong>to</strong>rs. Clinical neurophysiology in spasticity.<br />
Amsterdam: Elsevier, 1985: 185-203<br />
32. United Kingdom Tizanidine Study Group. A double-blind placebo-controlled<br />
trial of tizanidine in the treatment of spasticity<br />
caused my multiple sclerosis. Neurology 1994; 44 Suppl.<br />
9: 70-9<br />
33. Lapierre Y, Bouchard S, Tansey C, et al. <strong>Treat</strong>ment of spasticity<br />
with tizanidine in multiple sclerosis. Can J Neurol Sci 1987;<br />
14: 513-7<br />
34. Nance PW, Bugaresti J, Shellenberger K, et al. Efficacy and<br />
safety of tizanidine in the treatment of spasticity in patients<br />
with spinal cord injury. Neurology 1994; Suppl. 9: 44S-52S<br />
35. Milanov I, Georgiev D. Mechanisms of tizanidine action on<br />
spasticity. Acta Neurol Scand 1994; 89: 274-9<br />
36. Bass B, Weinshenker B, Rice GPA, et al. Tizanidine versus<br />
baclofen in the treatment of spasticity in patients with multiple<br />
sclerosis. Can J Sci 1988; 15 (1): 15-9<br />
37. Stein R, Nordal HJ, Oftendal SI, et al. The treatment of spasticity<br />
in multiple sclerosis: a double-blind clinical trial of a new<br />
anti-spasticity drug tizanidine compared with baclofen. Acta<br />
Neurol Scand 1987; 75: 190-4<br />
38. Smolenski C, Muff S, Smolenski-Kauts S. A double-blind comparative<br />
trial of a new muscle-relaxant, tizanidine (DS102-<br />
282) and baclofen in the treatment of chronic spasticity in<br />
multiple sclerosis. Curr Med Res Opin 1981; 7 (6): 374-83<br />
39. Hoorgstraten MC, van der Ploeg RJO, Van der Burg W, et al.<br />
Tizanidine versus baclofen in the treatment of multiple sclerosis<br />
patients. Acta Neurol Scand 1988; 77: 224-30<br />
40. Eyssette M, Rohmer F, Serratrice G, et al. Multi-centre, doubleblind<br />
trial of a novel antispastic agent, tizanidine, in spasticity<br />
associated with multiple sclerosis. Curr Med Res Opin 1988;<br />
10 (10): 699-708<br />
41. Pagano MA, Ferreiro ME, Herskovits E. Comparative study of<br />
tizanidine and baclofen in patients with chronic spasticity.<br />
Rev Neurol Argent 1988; 14 (4): 268-76<br />
42. Rinne UK. Tizanidine treatment of spasticity in multiple sclerosis<br />
and chronic myelopathy. Curr Ther Res 1980 Dec 1; 28<br />
(6): 827-36<br />
43. Bes A, Eyssette M, Pierrot-Deseilligny E, et al. A multi-centre,<br />
double-blind trial of tizanidine, a new anti-spastic agent, in<br />
spasticity associated with hemiplegia. Curr Med Res Opin<br />
1988; 10: 709-18<br />
44. Nance PW, Shears AH, Nance DM. Reflex changes induced by<br />
clonidine in spinal cord injured patients. Paraplegia 1989; 4:<br />
296-301<br />
45. Dall JT, Harmon RL, Quinn CM. Use of clonidine for treatment<br />
of spasticity arising from various forms of brain injury: a case<br />
series. Brain Injury 1996; 10 (6): 453-8<br />
46. Donovan WH, Carter RE, Rossi CD, et al. Clonidine effect on<br />
spasticity: a clinical trial. Arch Phys Med Rehabil 1988; 69 (3<br />
Pt 1): 193-4<br />
47. Herman R, Mayer N, Mecomber SA. Clinical pharmaco-physiology<br />
of dantrolene sodium. Am J Physical Med 1972; 51:<br />
296-311<br />
48. Ellis KO, Carpenter JF. Mechanisms of control of skeletal muscle<br />
contraction by dantrolene sodium. Arch Phys Med Rehabil<br />
1974; 55: 362-9<br />
49. Pinder RM, Brodgen RN, Speight TM, et al. Dantrolene sodium:<br />
a review of its pharmacological properties and therapeutic<br />
efficacy in spasticity. <strong>Drugs</strong> 1977; 13: 3-23<br />
50. Whyte J, Robinson KM. Pharmacologic management. In: Glenn<br />
M, Whyte J, edi<strong>to</strong>rs. The practical management of spasticity<br />
in children and adults. Philadelphia (PA): Lea & Febiger,<br />
1990: 201-26<br />
51. Monster AW, Tamai Y, McHenry J. Dantrolene sodium in spasticity.<br />
Acta Neurol Scand 1979; 59: 309-16<br />
52. Gelenberg AJ, Poskanzer DC. The effect of dantrolene sodium<br />
on spasticity in multiple sclerosis. Neurology 1973; 23: 1313-5<br />
© Adis International Limited. All rights reserved. <strong>Drugs</strong> 2000 Mar; 59 (3)
Drug <strong>Treat</strong>ment of <strong>Spasticity</strong> 495<br />
53. Tolosa ES, Soll RW, Loewenson R. <strong>Treat</strong>ment of spasticity in<br />
multiple sclerosis with dantrolene. JAMA 1975; 233 (10): 1046<br />
54. Katrak PH, Cole A, Poulos CJ, et al. Objective assessment of<br />
spasticity, strength and function with early exhibition of dantrolene<br />
sodium after cerebrovascular accident: a randomized<br />
double-blind study. Arch Phys Med Rehabil 1992; 73: 4-9<br />
55. Schmidt RT, Lee RH, Spehlman R. Comparison of dantrolene<br />
sodium and diazepam in the treatment of spasticity. J Neurol<br />
Neurosurg Psychiatry 1976; 39: 350-6<br />
56. Nogen AG. Medical treatment for spasticity in children with<br />
cerebral palsy. Child’s Brain 1976; 2: 304-8<br />
57. Glass A, Hannah A. A comparison of dantrolene sodium and<br />
diazepam in the treatment of spasticity. Paraplegia 1974; 12:<br />
170-4<br />
58. US Gabapentin Study Group. The long-term safety and efficacy<br />
of gabapentin (Neurontin) as add-on therapy in drug-resistant<br />
partial epilepsy. Epilep Res, 1994 May, 18 (1): 67-73<br />
59. Fromm GH. Gabapentin. Epilepsia 1994; 35 Suppl. 5: 77-80S<br />
60. McLean MJ. Gabapentin. Epilepsia 1995; 36 Suppl. 2: 73S-86S<br />
61. Priebe MM, Sherwood AM, Graves DE, et al. Effectiveness of<br />
gabapentin in controlling spasticity: a quantitative study. Spinal<br />
Cord 1997; 35: 171-5<br />
62. Dunevsky A, Perel A. Gabapentin for relief of spasticity associated<br />
with multiple sclerosis. Am J Phys Med Rehabil 1998;<br />
77: 451-4<br />
63. Yablon SA, Agana BT, Ivanhoe CB, et al. Botulinum <strong>to</strong>xin in<br />
severe upper extremity spasticity among patients with traumatic<br />
brain injury: an open label trial. Neurology 1996; 47:<br />
939-44<br />
64. Simpson DM, Alexander DN, O’Brien CF, et al. Botulinum<br />
<strong>to</strong>xin type A in the treatment of upper extremity spasticity: a<br />
randomized, double-blind, placebo-controlled trial. Neurology<br />
1996; 46: 1306-10<br />
65. Burbaud P, Wiart L, Dubos JL, et al. Arandomized, double blind<br />
placebo controlled trial of botulinum <strong>to</strong>xin in the treatment of<br />
spastic foot in hemiparetic patients. J Neurol Neurosurg Psychiatry<br />
1996; 61: 265-9<br />
66. Das TK, Park DM. Effect of treatment with botulinum <strong>to</strong>xin on<br />
spasticity. Postgrad Med J 1989; 65: 208-10<br />
67. Snow BJ, Tsui JKC, Bhatt MH, et al. <strong>Treat</strong>ment of spasticity<br />
with botulinum <strong>to</strong>xin: a double-blind study. Ann Neurol 1990;<br />
28: 512-5<br />
68. Cosgrove AP, Corry IS, Graham HK. Botulinium <strong>to</strong>xin in the<br />
management of the lower limb in cerebral palsy. Dev Med<br />
Child Neurol 1994; 36 (5): 386-96<br />
69. Koman LA, Mooney III JF, Smith BP, et al. Management of<br />
spasticity in cerebral palsy with botulinum-A <strong>to</strong>xin: report of<br />
a preliminary, randomized, double-blind trial. J Pediatr Orthop<br />
1994; 14 (3): 299-303<br />
70. Penn RD, Savoy SM, Corcos D, et al. Intrathecal baclofen for<br />
severe spinal spasticity. N Engl J Med 1989; 320: 1517-21<br />
71. Ashworth B. Preliminary trial of carisprodol in multiple sclerosis.<br />
Practitioner 1964; 192: 540-2<br />
72.LeeKC,CarsonL,KinninE,etal.TheAshworthScale:a<br />
reliable and reproducible method of measuring spasticity. J<br />
Neuro Rehab 1989; 3: 205-9<br />
73. Ochs G, Struppler A, Meyerson BA, et al. Intrathecal baclofen<br />
for long-term treatment of spasticity: a multi-centre study. J<br />
Neurol Neurosurg Psychiatry 1989; 52: 933-9<br />
74. Albright AL, Barron WB, Fasick MP, et al. Continuous intrathecal<br />
baclofen infusion for spasticity of cerebral origin. JAMA<br />
1993; 270: 2475-7<br />
75. Dralle D, Muller H, Zierski J, et al. Intrathecal baclofen for<br />
spasticity [letter]. Lancet 1985; II 8462: 1003<br />
76. Penn RD. Intrathecal baclofen for spasticity of spinal origin:<br />
seven years experience. J Neurosurg 1992; 77: 236-40<br />
77. Nance PW, Schryvers OI, Schmidt BJ, et al. Intrathecal baclofen<br />
therapy for adults with spinal spasticity: therapeutic efficacy<br />
and effect on hospital admission. Can J Neurol Sci<br />
1995; 22: 122-9<br />
78. Nanninga JB, Frost F, Penn R. Effect of intrathecal baclofen on<br />
bladder and sphincter function. J Urol 1989; 142: 101-5<br />
79. Siegfried J, Rea GL. Intrathecal application of drugs for muscle<br />
hyper<strong>to</strong>nus. Scand J Rehab Med 1988; 17 Suppl.: 145-8<br />
Correspondence and offprints: Dr Mariko Kita, Department<br />
of Neurology, University of California at San Francisco,<br />
School of Medicine UCSF/Mt Zion Multiple Sclerosis Center,<br />
1701 Divisadero Suite 480, San Francisco, CA 94115-<br />
1642, USA.<br />
E-mail: kita@itsa.ucsf.edu<br />
© Adis International Limited. All rights reserved. <strong>Drugs</strong> 2000 Mar; 59 (3)