Management of stage Ⅳ rectal cancer - World Journal of ...
Management of stage Ⅳ rectal cancer - World Journal of ...
Management of stage Ⅳ rectal cancer - World Journal of ...
Create successful ePaper yourself
Turn your PDF publications into a flip-book with our unique Google optimized e-Paper software.
<strong>World</strong> <strong>Journal</strong> <strong>of</strong><br />
Gastroenterology<br />
<strong>World</strong> J Gastroenterol 2011 February 21; 17(7): 817-952<br />
www.wjgnet.com<br />
ISSN 1007-9327 (print)<br />
ISSN 2219-2840 (online)
Editorial Board<br />
2010-2013<br />
The <strong>World</strong> <strong>Journal</strong> <strong>of</strong> Gastroenterology Editorial Board consists <strong>of</strong> 1144 members, representing a team <strong>of</strong> worldwide<br />
experts in gastroenterology and hepatology. They are from 60 countries, including Albania (1), Argentina (8),<br />
Australia (29), Austria (14), Belgium (12), Brazil (10), Brunei Darussalam (1), Bulgaria (2), Canada (20), Chile (3),<br />
China (69), Colombia (1), Croatia (2), Cuba (1), Czech (4), Denmark (8), Ecuador (1), Egypt (2), Estonia (2), Finland<br />
(8), France (24), Germany (75), Greece (14), Hungary (10), India (26), Iran (6), Ireland (7), Israel (12), Italy (101),<br />
Japan (112), Jordan (1), Kuwait (1), Lebanon (3), Lithuania (2), Malaysia (1), Mexico (10), Moldova (1), Netherlands<br />
(29), New Zealand (2), Norway (11), Pakistan (2), Poland (11), Portugal (4), Romania (3), Russia (1), Saudi Arabia<br />
(3), Serbia (3), Singapore (10), South Africa (2), South Korea (32), Spain (38), Sweden (18), Switzerland (11),<br />
Thailand (1), Trinidad and Tobago (1), Turkey (24), United Arab Emirates (2), United Kingdom (82), United States<br />
(249), and Uruguay (1).<br />
HONORARY EDITORS-IN-CHIEF<br />
James L Boyer, New Haven<br />
Ke-Ji Chen, Beijing<br />
Martin H Floch, New Haven<br />
Emmet B Keeffe, Palo Alto<br />
Geng-Tao Liu, Beijing<br />
Lein-Ray Mo, Tainan<br />
Eamonn M Quigley, Cork<br />
Rafiq A Sheikh, Sacramento<br />
Nicholas J Talley, Rochester<br />
Ming-Lung Yu, Kaohsiung<br />
PRESIDENT AND EDITOR-IN-<br />
CHIEF<br />
Lian-Sheng Ma, Beijing<br />
ACADEMIC EDITOR-IN-CHIEF<br />
Tauseef Ali, Oklahoma City<br />
Mauro Bortolotti, Bologna<br />
Tarkan Karakan, Ankara<br />
Weekitt Kittisupamongkol, Bangkok<br />
Anastasios Koulaouzidis, Edinburgh<br />
Bo-Rong Pan, Xi’an<br />
Sylvia LF Pender, Southampton<br />
Max S Petrov, Auckland<br />
George Y Wu, Farmington<br />
STRATEGY ASSOCIATE<br />
EDITORS-IN-CHIEF<br />
Peter Draganov, Florida<br />
Hugh J Freeman, Vancouver<br />
Maria C Gutiérrez-Ruiz, Mexico<br />
Kazuhiro Hanazaki, Kochi<br />
Akio Inui, Kagoshima<br />
Kalpesh Jani, Baroda<br />
Javier S Martin, Punta del Este<br />
WJG|www.wjgnet.com<br />
Natalia A Osna, Omaha<br />
Wei Tang, Tokyo<br />
Alan BR Thomson, Edmonton<br />
Harry HX Xia, Hanover<br />
Jesus K Yamamoto-Furusho, Mexico<br />
Yoshio Yamaoka, Houston<br />
ASSOCIATE EDITORS-IN-CHIEF<br />
You-Yong Lu, Beijing<br />
John M Luk, Singapore<br />
Hiroshi Shimada, Yokohama<br />
GUEST EDITORIAL BOARD<br />
MEMBERS<br />
Chien-Jen Chen, Taipei<br />
Yang-Yuan Chen, Changhua<br />
Jen-Hwey Chiu, Taipei<br />
Seng-Kee Chuah, Kaohsiung<br />
Wan-Long Chuang, Kaohsiun<br />
Ming-Chih Hou, Taipei<br />
Kevin Cheng-Wen Hsiao, Taipei<br />
Po-Shiuan Hsieh, Taipei<br />
Tsung-Hui Hu, Kaohsiung<br />
Wen-Hsin Huang, Taichung<br />
Chao-Hung Hung, Kaohsiung<br />
I-Rue Lai, Taipei<br />
Teng-Yu Lee, Taichung<br />
Ching Chung Lin, Taipei<br />
Hui-Kang Liu, Taipei<br />
Hon-Yi Shi, Kaohsiung<br />
Chih-Chi Wang, Kaohsiung<br />
Jin-Town Wang, Taipei<br />
Cheng-Shyong Wu, Chia-Yi<br />
Jaw-Ching Wu, Taipei<br />
Jiunn-Jong Wu, Tainan<br />
Ming-Shiang Wu, Taipei<br />
I<br />
Ta-Sen Yeh, Taoyuan<br />
Hsu-Heng Yen, Changhua<br />
Ming-Whei Yu, Taipei<br />
MEMBERS OF THE EDITORIAL<br />
BOARD<br />
Albania<br />
Bashkim Resuli, Tirana<br />
Argentina<br />
Julio H Carri, Córdoba<br />
Eduardo de Santibañes, Buenos Aires<br />
Bernardo Frider, Buenos Aires<br />
Carlos J Pirola, Buenos Aires<br />
Bernabe Matias Quesada, Buenos Aires<br />
Silvia Sookoian, Buenos Aires<br />
Adriana M Torres, Rosario<br />
Maria Ines Vaccaro, Buenos Aires<br />
Australia<br />
Leon Anton Adams, Nedlands<br />
Richard Anderson, Victoria<br />
Minoti V Apte, New South Wales<br />
Andrew V Biankin, Sydney<br />
Filip Braet, Sydney<br />
Christopher Christophi, Melbourne<br />
Philip G Dinning, Koagarah<br />
Guy D Eslick, Sydney<br />
Michael A Fink, Melbourne<br />
January 7, 2011
Robert JL Fraser, Daw Park<br />
Jacob George, Westmead<br />
Mark D Gorrell, Sydney<br />
Alexander G Heriot, Melbourne<br />
Michael Horowitz, Adelaide<br />
John E Kellow, Sydney<br />
William Kemp, Melbourne<br />
Finlay A Macrae, Victoria<br />
Daniel Markovich, Brisbane<br />
Vance Matthews, Melbourne<br />
Phillip S Oates, Perth<br />
Shan Rajendra, Tasmania<br />
Rajvinder Singh, Elizabeth Vale<br />
Ross C Smith, Sydney<br />
Kevin J Spring, Brisbane<br />
Nathan Subramaniam, Brisbane<br />
Phil Sutton, Melbourne<br />
Cuong D Tran, North Adelaide<br />
Debbie Trinder, Fremantle<br />
David Ian Watson, Bedford Park<br />
Austria<br />
Herwig R Cerwenka, Graz<br />
Ashraf Dahaba, Graz<br />
Peter Ferenci, Vienna<br />
Valentin Fuhrmann, Vienna<br />
Alfred Gangl, Vienna<br />
Alexander M Hirschl, Wien<br />
Kurt Lenz, Linz<br />
Dietmar Öfner, Salzburg<br />
Markus Peck-Radosavljevic, Vienna<br />
Markus Raderer, Vienna<br />
Stefan Riss, Vienna<br />
Georg Roth, Vienna<br />
Michael Trauner, Graz<br />
Thomas Wild, Kapellerfeld<br />
Belgium<br />
Rudi Beyaert, Gent<br />
Benedicte Y De Winter, Antwerp<br />
Inge I Depoortere, Leuven<br />
Olivier Detry, Liège<br />
Philip Meuleman, Ghent<br />
Marc Peeters, De Pintelaan<br />
Freddy Penninckx, Leuven<br />
Jean-Yves L Reginster, Liège<br />
Mark De Ridder, Brussels<br />
Etienne M Sokal, Brussels<br />
Kristin Verbeke, Leuven<br />
Eddie Wisse, Keerbergen<br />
Brazil<br />
José LF Caboclo, São José do Rio Preto<br />
Roberto J Carvalho-Filho, São Paulo<br />
Jaime Natan Eisig, São Paulo<br />
Andre Castro Lyra, Salvador<br />
Marcelo Lima Ribeiro, Braganca Paulista<br />
Joao Batista Teixeira Rocha, Santa Maria<br />
Heitor Rosa, Goiania<br />
Damiao C Moraes Santos, Rio de Janeiro<br />
Ana Cristina Simões e Silva, Belo Horizonte<br />
Eduardo Garcia Vilela, Belo Horizonte<br />
WJG|www.wjgnet.com<br />
Brunei Darussalam<br />
Vui Heng Chong, Bandar Seri Begawan<br />
Bulgaria<br />
Zahariy Krastev, S<strong>of</strong>ia<br />
Mihaela Petrova, S<strong>of</strong>ia<br />
Canada<br />
Alain Bitton, Montreal<br />
Michael F Byrne, Vancouver<br />
Kris Chadee, Calgary<br />
Wangxue Chen, Ottawa<br />
Ram Prakash Galwa, Ottawa<br />
Philip H Gordon, Montreal<br />
Waliul Khan, Ontario<br />
Qiang Liu, Saskatoon<br />
John K Marshall, Ontario<br />
Andrew L Mason, Alberta<br />
Kostas Pantopoulos, Quebec<br />
Nathalie Perreault, Sherbrooke<br />
Baljinder Singh Salh, Vancouver<br />
Eldon Shaffer, Calgary<br />
Martin Storr, Calgary<br />
Pingchang Yang, Hamilton<br />
Eric M Yoshida, Vancouver<br />
Claudia Zwingmann, Montreal<br />
Chile<br />
Marcelo A Beltran, La Serena<br />
Xabier De Aretxabala, Santiago<br />
Silvana Zanlungo, Santiago<br />
China<br />
Hui-Jie Bian, Xi’an<br />
San-Jun Cai, Shanghai<br />
Guang-Wen Cao, Shanghai<br />
Xiao-Ping Chen, Wuhan<br />
Chi-Hin Cho, Hong Kong<br />
Zong-Jie Cui, Beijing<br />
Jing-Yuan Fang, Shanghai<br />
De-Liang Fu, Shanghai<br />
Ze-Guang Han, Shanghai<br />
Chun-Yi Hao, Beijing<br />
Ming-Liang He, Hong Kong<br />
Ching-Lung Lai, Hong Kong<br />
Simon Law, Hong Kong<br />
Yuk-Tong Lee, Hong Kong<br />
En-Min Li, Shantou<br />
Fei Li, Beijing<br />
Yu-Yuan Li, Guangzhou<br />
Zhao-Shen Li, Shanghai<br />
Xing-Hua Lu, Beijing<br />
Yi-Min Mao, Shanghai<br />
Qin Su, Beijing<br />
Paul Kwong-Hang Tam, Hong Kong<br />
Yuk Him Tam, Hong Kong<br />
Ren-Xiang Tan, Nanjing<br />
Wei-Dong Tong, Chongqing<br />
Eric WC Tse, Hong Kong<br />
II<br />
Fu-Sheng Wang, Beijing<br />
Xiang-Dong Wang, Shanghai<br />
Nathalie Wong, Hong Kong<br />
Justin CY Wu, Hong Kong<br />
Wen-Rong Xu, Zhenjiang<br />
An-Gang Yang, Xi’an<br />
Wei-Cheng You, Beijing<br />
Chun-Qing Zhang, Jinan<br />
Jian-Zhong Zhang, Beijing<br />
Xiao-Peng Zhang, Beijing<br />
Xuan Zhang, Beijing<br />
Colombia<br />
Germán Campuzano-Maya, Medellín<br />
Croatia<br />
Tamara Cacev, Zagreb<br />
Marko Duvnjak, Zagreb<br />
Cuba<br />
Damian C Rodriguez, Havana<br />
Czech<br />
Jan Bures, Hradec Kralove<br />
Milan Jirsa, Praha<br />
Marcela Kopacova, Hradec Kralove<br />
Pavel Trunečka, Prague<br />
Denmark<br />
Leif Percival Andersen, Copenhagen<br />
Asbjørn M Drewes, Aalborg<br />
Morten Frisch, Copenhagen<br />
Jan Mollenhauer, Odense<br />
Morten Hylander Møller, Holte<br />
Søren Rafaelsen, Vejle<br />
Jorgen Rask-Madsen, Skodsborg<br />
Peer Wille-Jørgensen, Copenhagen<br />
Ecuador<br />
Fernando E Sempértegui, Quito<br />
Egypt<br />
Zeinab Nabil Ahmed, Cairo<br />
Hussein M Atta, El-Minia<br />
Estonia<br />
Riina Salupere, Tartu<br />
Tamara Vorobjova, Tartu<br />
Finland<br />
Saila Kauhanen, Turku<br />
January 7, 2011
Thomas Kietzmann, Oulu<br />
Kaija-Leena Kolho, Helsinki<br />
Jukka-Pekka Mecklin, Jyvaskyla<br />
Minna Nyström, Helsinki<br />
Pauli Antero Puolakkainen, Turku<br />
Juhani Sand, Tampere<br />
Lea Veijola, Helsinki<br />
France<br />
Claire Bonithon-Kopp, Dijon<br />
Lionel Bueno, Toulouse<br />
Sabine Colnot, Paris<br />
Catherine Daniel, Lille Cedex<br />
Alexis Desmoulière, Limoges<br />
Thabut Dominique, Paris<br />
Francoise L Fabiani, Angers<br />
Jean-Luc Faucheron, Grenoble<br />
Jean Paul Galmiche, Nantes cedex<br />
Boris Guiu, Dijon<br />
Paul H<strong>of</strong>man, Nice<br />
Laurent Huwart, Paris<br />
Juan Iovanna, Marseille<br />
Abdel-Majid Khatib, Paris<br />
Philippe Lehours, Bordeaux<br />
Flavio Maina, Marseille<br />
Patrick Marcellin, Paris<br />
Rene Gerolami Santandera, Marseille<br />
Annie Schmid-Alliana, Nice cedex<br />
Alain L Servin, Châtenay-Malabry<br />
Stephane Supiot, Nantes<br />
Baumert F Thomas, Strasbourg<br />
Jean-Jacques Tuech, Rouen<br />
Frank Zerbib, Bordeaux Cedex<br />
Germany<br />
Erwin Biecker, Siegburg<br />
Hubert Blum, Freiburg<br />
Thomas Bock, Tuebingen<br />
Dean Bogoevski, Hamburg<br />
Elfriede Bollschweiler, Köln<br />
Jürgen Borlak, Hannover<br />
Christa Buechler, Regensburg<br />
Jürgen Büning, Lübeck<br />
Elke Cario, Essen<br />
Bruno Christ, Halle/Saale<br />
Christoph F Dietrich, Bad Mergentheim<br />
Ulrich R Fölsch, Kiel<br />
Nikolaus Gassler, Aachen<br />
Markus Gerhard, Munich<br />
Dieter Glebe, Giessen<br />
Ralph Graeser, Freiburg<br />
Axel M Gressner, Aachen<br />
Nils Habbe, Marburg<br />
Thilo Hackert, Heidelberg<br />
Wolfgang Hagmann, Heidelberg<br />
Dirk Haller, Freising<br />
Philip D Hard, Giessen<br />
Claus Hellerbrand, Regensburg<br />
Klaus R Herrlinger, Stuttgart<br />
Eberhard Hildt, Berlin<br />
Andrea Hille, Goettingen<br />
Joerg C H<strong>of</strong>fmann, Berlin<br />
Philipe N Khalil, Munich<br />
Andrej Khandoga, Munich<br />
Jorg Kleeff, Munich<br />
Ingmar Königsrainer, Tübingen<br />
Peter Konturek, Erlangen<br />
WJG|www.wjgnet.com<br />
Stefan Kubicka, Hannover<br />
Joachim Labenz, Siegen<br />
Michael Linnebacher, Rostock<br />
Jutta Elisabeth Lüttges, Riegelsberg<br />
Peter Malfertheiner, Magdeburg<br />
Oliver Mann, Hamburg<br />
Peter N Meier, Hannover<br />
Sabine Mihm, Göttingen<br />
Klaus Mönkemüller, Bottrop<br />
Jonas Mudter, Erlangen<br />
Sebastian Mueller, Heidelberg<br />
Robert Obermaier, Freiburg<br />
Matthias Ocker, Erlangen<br />
Stephan Johannes Ott, Kiel<br />
Gustav Paumgartner, Munich<br />
Christoph Reichel, Bad Brückenau<br />
Markus Reiser, Bochum<br />
Steffen Rickes, Magdeburg<br />
Elke Roeb, Giessen<br />
Christian Rust, Munich<br />
Hans Scherubl, Berlin<br />
Martin K Schilling, Homburg<br />
Joerg F Schlaak, Essen<br />
Rene Schmidt, Freiburg<br />
Andreas G Schreyer, Regensburg<br />
Karsten Schulmann, Bochum<br />
Henning Schulze-Bergkamen, Mainz<br />
Manfred V Singer, Mannheim<br />
Jens Standop, Bonn<br />
Jurgen M Stein, Frankfurt<br />
Ulrike S Stein, Berlin<br />
Wolfgang R Stremmel, Heidelberg<br />
Harald F Teutsch, Ulm<br />
Hans L Tillmann, Leipzig<br />
Christian Trautwein, Aachen<br />
Joerg Trojan, Frankfurt<br />
Arndt Vogel, Hannover<br />
Siegfried Wagner, Deggendorf<br />
Frank Ulrich Weiss, Greifswald<br />
Fritz von Weizsäcker, Berlin<br />
Thomas Wex, Magdeburg<br />
Stefan Wirth, Wuppertal<br />
Marty Zdichavsky, Tübingen<br />
Greece<br />
Helen Christopoulou-Aletra, Thessaloniki<br />
T Choli-Papadopoulou, Thessaloniki<br />
Tsianos Epameinondas, Ioannina<br />
Ioannis Kanellos, Thessaloniki<br />
Elias A Kouroumalis, Heraklion<br />
Ioannis E Koutroubakis, Heraklion<br />
Michael Koutsilieris, Athens<br />
Andreas Larentzakis, Athens<br />
Emanuel K Manesis, Athens<br />
Spilios Manolakopoulos, Athens<br />
Konstantinos Mimidis, Alexandroupolis<br />
George Papatheodoridis, Athens<br />
Spiros Sgouros, Athens<br />
Evangelos Tsiambas, Ag Paraskevi Attiki<br />
Hungary<br />
György M Buzás, Budapest<br />
László Czakó, Szeged<br />
Gyula Farkas, Szeged<br />
Peter Hegyi, Szeged<br />
Peter L Lakatos, Budapest<br />
III<br />
Yvette Mándi, Szeged<br />
Zoltan Rakonczay, Szeged<br />
Ferenc Sipos, Budapest<br />
Zsuzsa Szondy, Debrecen<br />
Gabor Veres, Budapest<br />
India<br />
Philip Abraham, Mumbai<br />
Vineet Ahuja, New Delhi<br />
Giriraj Ratan Chandak, Hyderabad<br />
Devinder Kumar Dhawan, Chandigarh<br />
Radha K Dhiman, Chandigarh<br />
Pankaj Garg, Panchkula<br />
Pramod Kumar Garg, New Delhi<br />
Debidas Ghosh, Midnpore<br />
Uday C Ghoshal, Lucknow<br />
Bhupendra Kumar Jain, Delhi<br />
Ashok Kumar, Lucknow<br />
Bikash Medhi, Chandigarh<br />
Sri P Misra, Allahabad<br />
Gopal Nath, Varanasi<br />
Samiran Nundy, New Delhi<br />
Jagannath Palepu, Mumbai<br />
Vandana Panda, Mumbai<br />
Benjamin Perakath, Tamil Nadu<br />
Ramesh Roop Rai, Jaipur<br />
Nageshwar D Reddy, Hyderabad<br />
Barjesh Chander Sharma, New Delhi<br />
Virendra Singh, Chandigarh<br />
Rupjyoti Talukdar, Guwahati<br />
Rakesh Kumar Tandon, New Delhi<br />
Jai Dev Wig, Chandigarh<br />
Iran<br />
Mohammad Abdollahi, Tehran<br />
Peyman Adibi, Isfahan<br />
Seyed-Moayed Alavian, Tehran<br />
Seyed Mohsen Dehghani, Shiraz<br />
Reza Malekzadeh, Tehran<br />
Alireza Mani, Tehran<br />
Ireland<br />
Billy Bourke, Dublin<br />
Ted Dinan, Cork<br />
Catherine Greene, Dublin<br />
Ross McManus, Dublin<br />
Anthony P Moran, Galway<br />
Marion Rowland, Dublin<br />
Israel<br />
Simon Bar-Meir, Hashomer<br />
Alexander Becker, Afula<br />
Abraham R Eliakim, Haifa<br />
Sigal Fishman, Tel Aviv<br />
Boris Kirshtein, Beer Sheva<br />
Eli Magen, Ashdod<br />
Menachem Moshkowitz, Tel-Aviv<br />
Assy Nimer, Safed<br />
Shmuel Odes, Beer Sheva<br />
Mark Pines, Bet Dagan<br />
Ron Shaoul, Haifa<br />
Ami D Sperber, Beer-Sheva<br />
January 7, 2011
Italy<br />
Donato F Altomare, Bari<br />
Piero Amodio, Padova<br />
Angelo Andriulli, San Giovanni Rotondo<br />
Paolo Angeli, Padova<br />
Bruno Annibale, Rome<br />
Paolo Aurello, Rome<br />
Salvatore Auricchio, Naples<br />
Antonio Basoli, Rome<br />
Claudio Bassi, Verona<br />
Gabrio Bassotti, Perugia<br />
Mauro Bernardi, Bologna<br />
Alberto Biondi, Rome<br />
Luigi Bonavina, Milano<br />
Guglielmo Borgia, Naples<br />
Roberto Berni Canani, Naples<br />
Maria Gabriella Caruso, Bari<br />
Fausto Catena, Bologna<br />
Giuseppe Chiarioni, Valeggio<br />
Michele Cicala, Rome<br />
Dario Conte, Milano<br />
Francesco Costa, Pisa<br />
Antonio Craxì, Palermo<br />
Salvatore Cucchiara, Rome<br />
Giuseppe Currò, Messina<br />
Mario M D’Elios, Florence<br />
Mirko D’On<strong>of</strong>rio, Verona<br />
Silvio Danese, Milano<br />
Roberto de Franchis, Milano<br />
Paola De Nardi, Milan<br />
Giovanni D De Palma, Naples<br />
Giuliana Decorti, Trieste<br />
Gianlorenzo Dionigi, Varese<br />
Massimo Falconi, Verona<br />
Silvia Fargion, Milan<br />
Giammarco Fava, Ancona<br />
Francesco Feo, Sassari<br />
Alessandra Ferlini, Ferrara<br />
Alessandro Ferrero, Torino<br />
Mirella Fraquelli, Milan<br />
Luca Frulloni, Verona<br />
Giovanni B Gaeta, Napoli<br />
Antonio Gasbarrini, Rome<br />
Edoardo G Giannini, Genoa<br />
Alessandro Granito, Bologna<br />
Fabio Grizzi, Milan<br />
Salvatore Gruttadauria, Palermo<br />
Pietro Invernizzi, Milan<br />
Achille Iolascon, Naples<br />
Angelo A Izzo, Naples<br />
Ezio Laconi, Cagliari<br />
Giovanni Latella, L’Aquila<br />
Massimo Levrero, Rome<br />
Francesco Luzza, Catanzaro<br />
Lucia Malaguarnera, Catania<br />
Francesco Manguso, Napoli<br />
Pier Mannuccio Mannucci, Milan<br />
Giancarlo Mansueto, Verona<br />
Giulio Marchesini, Bologna<br />
Mara Massimi, Coppito<br />
Giovanni Milito, Rome<br />
Giuseppe Montalto, Palermo<br />
Giovanni Monteleone, Rome<br />
Luca Morelli, Trento<br />
Giovanni Musso, Torino<br />
Mario Nano, Torino<br />
Gerardo Nardone, Napoli<br />
Riccardo Nascimbeni, Brescia<br />
Valerio Nobili, Rome<br />
Fabio Pace, Milan<br />
Nadia Peparini, Rome<br />
WJG|www.wjgnet.com<br />
Marcello Persico, Naples<br />
Mario Pescatori, Rome<br />
Raffaele Pezzilli, Bologna<br />
Alberto Piperno, Monza<br />
Anna C Piscaglia, Rome<br />
Piero Portincasa, Bari<br />
Michele Reni, Milan<br />
Vittorio Ricci, Pavia<br />
Oliviero Riggio, Rome<br />
Mario Rizzetto, Torino<br />
Ballarin Roberto, Modena<br />
Gerardo Rosati, Potenza<br />
Franco Roviello, Siena<br />
Cesare Ruffolo, Treviso<br />
Massimo Rugge, Padova<br />
Marco Scarpa, Padova<br />
C armelo Scarpignato, Parma<br />
Giuseppe Sica, Rome<br />
Marco Silano, Rome<br />
Pierpaolo Sileri, Rome<br />
Vincenzo Stanghellini, Bologna<br />
Fiorucci Stefano, Perugia<br />
Giovanni Tarantino, Naples<br />
Alberto Tommasini, Trieste<br />
Guido Torzilli, Rozzano Milan<br />
Cesare Tosetti, Porretta Terme<br />
Antonello Trecca, Rome<br />
Vincenzo Villanacci, Brescia<br />
Lucia Ricci Vitiani, Rome<br />
Marco Vivarelli, Bologna<br />
Japan<br />
Kyoichi Adachi, Izumo<br />
Yasushi Adachi, Sapporo<br />
Takafumi Ando, Nagoya<br />
Akira Andoh, Otsu<br />
Masahiro Arai, Tokyo<br />
Hitoshi Asakura, Tokyo<br />
Kazuo Chijiiwa, Miyazaki<br />
Yuichiro Eguchi, Saga<br />
Itaru Endo, Yokohama<br />
Munechika Enjoji, Fukuoka<br />
Yasuhiro Fujino, Akashi<br />
Mitsuhiro Fujishiro, Tokyo<br />
Kouhei Fukushima, Sendai<br />
Masanori Hatakeyama, Tokyo<br />
Keiji Hirata, Kitakyushu<br />
Toru Hiyama, Higashihiroshima<br />
Masahiro Iizuka, Akita<br />
Susumu Ikehara, Osaka<br />
Kenichi Ikejima, Bunkyo-ku<br />
Yutaka Inagaki, Kanagawa<br />
Hiromi Ishibashi, Nagasaki<br />
Shunji Ishihara, Izumo<br />
Toru Ishikawa, Niigata<br />
Toshiyuki Ishiwata, Tokyo<br />
Hajime Isomoto, Nagasaki<br />
Yoshiaki Iwasaki, Okayama<br />
Satoru Kakizaki, Gunma<br />
Terumi Kamisawa, Tokyo<br />
Mototsugu Kato, Sapporo<br />
Naoya Kato, Tokyo<br />
Takumi Kawaguchi, Kurume<br />
Yohei Kida, Kainan<br />
Shogo Kikuchi, Aichi<br />
Tsuneo Kitamura, Chiba<br />
Takashi Kobayashi, Tokyo<br />
Yasuhiro Koga, Isehara<br />
Takashi Kojima, Sapporo<br />
Norihiro Kokudo, Tokyo<br />
Masatoshi Kudo, Osaka<br />
Shin Maeda, Tokyo<br />
IV<br />
Satoshi Mamori, Hyogo<br />
Atsushi Masamune, Sendai<br />
Yasushi Matsuzaki, Tsukuba<br />
Kenji Miki, Tokyo<br />
Toshihiro Mitaka, Sapporo<br />
Hiroto Miwa, Hyogo<br />
Kotaro Miyake, Tokushima<br />
Manabu Morimoto, Yokohama<br />
Yoshiharu Motoo, Kanazawa<br />
Yoshiaki Murakami, Hiroshima<br />
Yoshiki Murakami, Kyoto<br />
Kunihiko Murase, Tusima<br />
Akihito Nagahara, Tokyo<br />
Yuji Naito, Kyoto<br />
Atsushi Nakajima, Yokohama<br />
Hisato Nakajima, Tokyo<br />
Hiroki Nakamura, Yamaguchi<br />
Shotaro Nakamura, Fukuoka<br />
Akimasa Nakao, Nagogya<br />
Shuhei Nishiguchi, Hyogo<br />
Mikio Nishioka, Niihama<br />
Keiji Ogura, Tokyo<br />
Susumu Ohmada, Maebashi<br />
Hirohide Ohnishi, Akita<br />
Kenji Okajima, Nagoya<br />
Kazuichi Okazaki, Osaka<br />
Morikazu Onji, Ehime<br />
Satoshi Osawa, Hamamatsu<br />
Hidetsugu Saito, Tokyo<br />
Yutaka Saito, Tokyo<br />
Naoaki Sakata, Sendai<br />
Yasushi Sano, Chiba<br />
Tokihiko Sawada, Tochigi<br />
Tomohiko Shimatan, Hiroshima<br />
Yukihiro Shimizu, Kyoto<br />
Shinji Shimoda, Fukuoka<br />
Yoshio Shirai, Niigata<br />
Masayuki Sho, Nara<br />
Shoichiro Sumi, Kyoto<br />
Hidekazu Suzuki, Tokyo<br />
Masahiro Tajika, Nagoya<br />
Yoshihisa Takahashi, Tokyo<br />
Toshinari Takamura, Kanazawa<br />
Hiroaki Takeuchi, Kochi<br />
Yoshitaka Takuma, Okayama<br />
Akihiro Tamori, Osaka<br />
Atsushi Tanaka, Tokyo<br />
Shinji Tanaka, Hiroshima<br />
Satoshi Tanno, Hokkaido<br />
Shinji Togo, Yokohama<br />
Hitoshi Tsuda, Tokyo<br />
Hiroyuki Uehara, Osaka<br />
Masahito Uemura, Kashihara<br />
Yoshiyuki Ueno, Sendai<br />
Mitsuyoshi Urashima, Tokyo<br />
Takuya Watanabe, Niigata<br />
Satoshi Yamagiwa, Niigata<br />
Taketo Yamaguchi, Chiba<br />
Mitsunori Yamakawa, Yamagata<br />
Takayuki Yamamoto, Yokkaichi<br />
Yutaka Yata, Maebashi<br />
Hiroshi Yoshida, Tokyo<br />
Norimasa Yoshida, Kyoto<br />
Yuichi Yoshida, Osaka<br />
Kentaro Yoshika, Toyoake<br />
Hitoshi Yoshiji, Nara<br />
Katsutoshi Yoshizato, Higashihiroshima<br />
Tomoharu Yoshizumi, Fukuoka<br />
Jordan<br />
Ismail Matalka, Irbid<br />
January 7, 2011
Islam Khan, Safat<br />
Kuwait<br />
Lebanon<br />
Bassam N Abboud, Beirut<br />
Ala I Sharara, Beirut<br />
Rita Slim, Beirut<br />
Lithuania<br />
Giedrius Barauskas, Kaunas<br />
Limas Kupcinskas, Kaunas<br />
Malaysia<br />
Andrew Seng Boon Chua, Ipoh<br />
Mexico<br />
Richard A Awad, Mexico<br />
Aldo Torre Delgadillo, Mexico<br />
Diego Garcia-Compean, Monterrey<br />
Paulino M Hernández Magro, Celaya<br />
Miguel Angel Mercado, Distrito Federal<br />
Arturo Panduro, Jalisco<br />
Omar Vergara-Fernandez, Tlalpan<br />
Saúl Villa-Trevio, Mexico<br />
Moldova<br />
Igor Mishin, Kishinev<br />
Netherlands<br />
Ulrich Beuers, Amsterdam<br />
Lee Bouwman, Leiden<br />
Albert J Bredenoord, Nieuwegein<br />
Lodewijk AA Brosens, Utrecht<br />
J Bart A Crusius, Amsterdam<br />
Wouter de Herder, Rotterdam<br />
Pieter JF de Jonge, Rotterdam<br />
Robert J de Knegt, Rotterdam<br />
Wendy W Johanna de Leng, Utrecht<br />
Annemarie de Vries, Rotterdam<br />
James CH Hardwick, Leiden<br />
Frank Hoentjen, Haarlem<br />
Misha Luyer, Sittard<br />
Jeroen Maljaars, Maastricht<br />
Gerrit A Meijer, Amsterdam<br />
Servaas Morré, Amsterdam<br />
Chris JJ Mulder, Amsterdam<br />
John Plukker, Groningen<br />
Albert Frederik Pull ter Gunne, Tilburg<br />
Paul E Sijens, Groningen<br />
BW Marcel Spanier, Arnhem<br />
Shiri Sverdlov, Maastricht<br />
Maarten Tushuizen, Amsterdam<br />
Jantine van Baal, Heidelberglaan<br />
Astrid van der Velde, The Hague<br />
Karel van Erpecum, Utrecht<br />
Loes van Keimpema, Nijmegen<br />
WJG|www.wjgnet.com<br />
Robert Christiaan Verdonk, Groningen<br />
Erwin G Zoetendal, Wageningen<br />
New Zealand<br />
Andrew S Day, Christchurch<br />
Norway<br />
Olav Dalgard, Oslo<br />
Trond Peder Flaten, Trondheim<br />
Reidar Fossmark, Trondheim<br />
Rasmus Goll, Tromso<br />
Ole Høie, Arendal<br />
Asle W Medhus, Oslo<br />
Espen Melum, Oslo<br />
Trine Olsen, Tromso<br />
Eyvind J Paulssen, Tromso<br />
Jon Arne Søreide, Stavanger<br />
Kjetil Soreide, Stavanger<br />
Pakistan<br />
Shahab Abid, Karachi<br />
Syed MW Jafri, Karachi<br />
Poland<br />
Marek Bebenek, Wroclaw<br />
Tomasz Brzozowski, Cracow<br />
Halina Cichoż-Lach, Lublin<br />
Andrzej Dabrowski, Bialystok<br />
Hanna Gregorek, Warsaw<br />
Marek Hartleb, Katowice<br />
Beata Jolanta Jablońska, Katowice<br />
Stanislaw J Konturek, Krakow<br />
Jan Kulig, Krakow<br />
Dariusz M Lebensztejn, Bialystok<br />
Julian Swierczynski, Gdansk<br />
Portugal<br />
Raquel Almeida, Porto<br />
Ana Isabel Lopes, Lisboa Codex<br />
Ricardo Marcos, Porto<br />
Guida Portela-Gomes, Estoril<br />
Romania<br />
Dan L Dumitrascu, Cluj<br />
Adrian Saftoiu, Craiova<br />
Andrada Seicean, Cluj-Napoca<br />
Russia<br />
Vasiliy I Reshetnyak, Moscow<br />
Saudi Arabia<br />
Ibrahim A Al M<strong>of</strong>leh, Riyadh<br />
Abdul-Wahed Meshikhes, Qatif<br />
Faisal Sanai, Riyadh<br />
V<br />
Serbia<br />
Tamara M Alempijevic, Belgrade<br />
Dusan M Jovanovic, Sremska Kamenica<br />
Zoran Krivokapic, Belgrade<br />
Singapore<br />
Madhav Bhatia, Singapore<br />
Kong Weng Eu, Singapore<br />
Brian Kim Poh Goh, Singapore<br />
Khek-Yu Ho, Singapore<br />
Kok Sun Ho, Singapore<br />
Fock Kwong Ming, Singapore<br />
London Lucien Ooi, Singapore<br />
Nagarajan Perumal, Singapore<br />
Francis Seow-Choen, Singapore<br />
South Africa<br />
Rosemary Joyce Burnett, Pretoria<br />
Michael Kew, Cape Town<br />
South Korea<br />
Sang Hoon Ahn, Seoul<br />
Sung-Gil Chi, Seoul<br />
Myung-Gyu Choi, Seoul<br />
Hoon Jai Chun, Seoul<br />
Yeun-Jun Chung, Seoul<br />
Young-Hwa Chung, Seoul<br />
Kim Donghee, Seoul<br />
Ki-Baik Hahm, Incheon<br />
Sun Pyo Hong, Geonggi-do<br />
Seong Gyu Hwang, Seongnam<br />
Hong Joo Kim, Seoul<br />
Jae J Kim, Seoul<br />
Jin-Hong Kim, Suwon<br />
Nayoung Kim, Seongnam-si<br />
Sang Geon Kim, Seoul<br />
Seon Hahn Kim, Seoul<br />
Sung Kim, Seoul<br />
Won Ho Kim, Seoul<br />
Jeong Min Lee, Seoul<br />
Kyu Taek Lee, Seoul<br />
Sang Kil Lee, Seoul<br />
Sang Yeoup Lee, Gyeongsangnam-do<br />
Yong Chan Lee, Seoul<br />
Eun-Yi Moon, Seoul<br />
Hyoung-Chul Oh, Seoul<br />
Seung Woon Paik, Seoul<br />
Joong-Won Park, Goyang<br />
Ji Kon Ryu, Seoul<br />
Si Young Song, Seoul<br />
Marie Yeo, Suwon<br />
Byung Chul Yoo, Seoul<br />
Dae-Yeul Yu, Daejeon<br />
Spain<br />
Maria-Angeles Aller, Madrid<br />
Raul J Andrade, Málaga<br />
Luis Aparisi, Valencia<br />
Gloria González Aseguinolaza, Navarra<br />
Matias A Avila, Pamplona<br />
January 7, 2011
Fernando Azpiroz, Barcelona<br />
Ramon Bataller, Barcelona<br />
Belén Beltrán, Valencia<br />
Adolfo Benages, Valencia<br />
Josep M Bordas, Barcelona<br />
Lisardo Boscá, Madrid<br />
Luis Bujanda, San Sebastián<br />
Juli Busquets, Barcelona<br />
Matilde Bustos, Pamplona<br />
José Julián calvo Andrés, Salamanca<br />
Andres Cardenas, Barcelona<br />
Antoni Castells, Barcelona<br />
Fernando J Corrales, Pamplona<br />
J E Domínguez-Muñoz, Santiago de Compostela<br />
Juan Carlos Laguna Egea, Barcelona<br />
Isabel Fabregat, Barcelona<br />
Antoni Farré, Barcelona<br />
Vicente Felipo, Valencia<br />
Laureano Fernández-Cruz, Barcelona<br />
Luis Grande, Barcelona<br />
Angel Lanas, Zaragoza<br />
Juan-Ramón Larrubia, Guadalajara<br />
María IT López, Jaén<br />
Juan Macías, Seville<br />
Javier Martin, Granada<br />
José Manuel Martin-Villa, Madrid<br />
Julio Mayol, Madrid<br />
Mireia Miquel, Sabadell<br />
Albert Parés, Barcelona<br />
Jesús M Prieto, Pamplona<br />
Pedro L Majano Rodriguez, Madrid<br />
Joan Roselló-Catafau, Barcelona<br />
Eva Vaquero, Barcelona<br />
Sweden<br />
Lars Erik Agréus, Stockholm<br />
Mats Andersson, Stockholm<br />
Roland Andersson, Lund<br />
Mauro D’Amato, Huddinge<br />
Evangelos Kalaitzakis, Gothenburg<br />
Greger Lindberg, Stockholm<br />
Annika Lindblom, Stockholm<br />
Sara Lindén, Göteborg<br />
Hanns-Ulrich Marschall, Stockholm<br />
Pär Erik Myrelid, Linköping<br />
Åke Nilsson, Lund<br />
Helena Nordenstedt, Stockholm<br />
Kjell Öberg, Uppsala<br />
Lars A Pahlman, Uppsala<br />
Stefan G Pierzynowski, Lund<br />
Sara Regnér, Malmö<br />
Bobby Tingstedt, Lund<br />
Zongli Zheng, Stockholm<br />
Switzerland<br />
Pascal Bucher, Geneva<br />
Michelangelo Foti, Geneva<br />
Jean L Frossard, Geneva<br />
Andreas Geier, Zürich<br />
Pascal Gervaz, Geneva<br />
Gerd A Kullak-Ublick, Zürich<br />
Fabrizio Montecucco, Geneva<br />
Paul M Schneider, Zürich<br />
Felix Stickel, Berne<br />
Bruno Stieger, Zürich<br />
Inti Zlobec, Basel<br />
WJG|www.wjgnet.com<br />
Trinidad and Tobago<br />
Shivananda Nayak, Mount Hope<br />
Turkey<br />
Sinan Akay, Tekirdag<br />
Metin Basaranoglu, Istanbul<br />
Yusuf Bayraktar, Ankara<br />
A Mithat Bozdayi, Ankara<br />
Hayrullah Derici, Balıkesir<br />
Eren Ersoy, Ankara<br />
Mukaddes Esrefoglu, Malatya<br />
Can Goen, Kutahya<br />
Selin Kapan, Istanbul<br />
Aydin Karabacakoglu, Konya<br />
Cuneyt Kayaalp, Malatya<br />
Kemal Kismet, Ankara<br />
Seyfettin Köklü, Ankara<br />
Mehmet Refik Mas, Etlik-Ankara<br />
Osman C Ozdogan, Istanbul<br />
Bülent Salman, Ankara<br />
Orhan Sezgin, Mersin<br />
Ilker Tasci, Ankara<br />
Müge Tecder-Ünal, Ankara<br />
Ahmet Tekin, Mersin<br />
Mesut Tez, Ankara<br />
Ekmel Tezel, Ankara<br />
Özlem Yilmaz, Izmir<br />
United Arab Emirates<br />
Fikri M Abu-Zidan, Al-Ain<br />
Sherif M Karam, Al-Ain<br />
United Kingdom<br />
Simon Afford, Birmingham<br />
Navneet K Ahluwalia, Stockport<br />
Mohamed H Ahmed, Southampton<br />
Basil Ammori, Salford<br />
Lesley A Anderson, Belfast<br />
Chin Wee Ang, Liverpool<br />
Yeng S Ang, Wigan<br />
Anthony TR Axon, Leeds<br />
Kathleen B Bamford, London<br />
Jim D Bell, London<br />
John Beynon, Swansea<br />
Chris Briggs, Sheffield<br />
Ge<strong>of</strong>frey Burnstock, London<br />
Alastair D Burt, Newcastle<br />
Jeff Butterworth, Shrewsbury<br />
Jeremy FL Cobbold, London<br />
Jean E Crabtree, Leeds<br />
Tatjana Crnogorac-Jurcevic, London<br />
William Dickey, Londonderry<br />
Sunil Dolwani, Cardiff<br />
Emad M El-Omar, Aberdeen<br />
A M El-Tawil, Birmingham<br />
Charles B Ferguson, Belfast<br />
Andrew Fowell, Southampton<br />
Piers Gatenby, London<br />
Daniel R Gaya, Edinburgh<br />
Anil George, London<br />
Rob Glynne-Jones, Northwood<br />
Jason CB Goh, Birmingham<br />
Gianpiero Gravante, Leicester<br />
VI<br />
Brian Green, Belfast<br />
William Greenhalf, Liverpool<br />
Indra N Guha, Nottingham<br />
Stefan G Hübscher, Birmingham<br />
Robin Hughes, London<br />
Pali Hungin, Stockton<br />
Nawfal Hussein, Nottingham<br />
Clement W Imrie, Glasgow<br />
Janusz AZ Jankowski, Oxford<br />
Sharad Karandikar, Birmingham<br />
Peter Karayiannis, London<br />
Shahid A Khan, London<br />
Patricia F Lalor, Birmingham<br />
John S Leeds, Sheffield<br />
Ian Lindsey, Oxford<br />
Hong-Xiang Liu, Cambridge<br />
Dileep N Lobo, Nottingham<br />
Graham MacKay, Glasgow<br />
Mark Edward McAlindon, Sheffield<br />
Anne McCune, Bristol<br />
Donald Campbell McMillan, Glasgow<br />
Giorgina Mieli-Vergani, London<br />
Jamie Murphy, London<br />
Guy Fairbairn Nash, Poole<br />
James Neuberger, Birmingham<br />
Patrick O’Dwyer, Glasgow<br />
Christos Paraskeva, Bristol<br />
Richard Parker, North Staffordshire<br />
Thamara Perera, Birmingham<br />
Kondragunta Rajendra Prasad, Leeds<br />
D Mark Pritchard, Liverpool<br />
Alberto Quaglia, London<br />
Akhilesh B Reddy, Cambridge<br />
Kevin Robertson, Glasgow<br />
Sanchoy Sarkar, Liverpool<br />
John B Sch<strong>of</strong>ield, Kent<br />
Marco Senzolo, Padova<br />
Venkatesh Shanmugam, Derby<br />
Paul Sharp, London<br />
Chew Thean Soon, Manchester<br />
Aravind Suppiah, East Yorkshire<br />
Noriko Suzuki, Middlesex<br />
Simon D Taylor-Robinson, London<br />
Frank I Tovey, London<br />
A McCulloch Veitch, Wolverhampton<br />
Vamsi R Velchuru, Lowest<strong>of</strong>t<br />
Sumita Verma, Brighton<br />
Catherine Walter, Cheltenham<br />
Julian RF Walters, London<br />
Roger Williams, London<br />
United States<br />
Kareem M Abu-Elmagd, Pittsburgh<br />
Sami R Achem, Florida<br />
Golo Ahlenstiel, Bethesda<br />
Bhupinder S Anand, Houston<br />
M Ananthanarayanan, New York<br />
Balamurugan N Appakalal, Minneapolis<br />
Dimitrios V Avgerinos, New York<br />
Shashi Bala, Worcester<br />
Anthony J Bauer, Pittsburgh<br />
Kevin E Behrns, Gainesville<br />
Roberto Bergamaschi, New York<br />
Henry J Binder, New Haven<br />
Edmund J Bini, New York<br />
Wojciech Blonski, Philadelphia<br />
Mark Bloomston, Columbus<br />
Edward L Bradley III, Sarasota<br />
Carla W Brady, Durham<br />
January 7, 2011
David A Brenner, San Diego<br />
Adeel A Butt, Pittsburgh<br />
Shi-Ying Cai, New Haven<br />
Justin MM Cates, Nashville<br />
Eugene P Ceppa, Durham<br />
Jianyuan Chai, Long Beach<br />
Ronald S Chamberlain, Livingston<br />
Fei Chen, Morgantown<br />
Xian-Ming Chen, Omaha<br />
Ramsey Chi-man Cheung, Palo Alto<br />
Denesh Chitkara, East Brunswick<br />
Clifford S Cho, Madison<br />
Parimal Chowdhury, Arkansas<br />
John David Christein, Birmingham<br />
Thomas Clancy, Boston<br />
Ana J Coito, Los Angeles<br />
Ricardo Alberto Cruciani, New York<br />
Joseph J Cullen, Iowa City<br />
Mark J Czaja, New York<br />
Mariana D Dabeva, Bronx<br />
Jessica A Davila, Houston<br />
Conor P Delaney, Cleveland<br />
Laurie DeLeve, Los Angeles<br />
Anthony J Demetris, Pittsburgh<br />
Sharon DeMorrow, Temple<br />
Bijan Eghtesad, Cleveland<br />
Yoram Elitsur, Huntington<br />
Mohamad A Eloubeidi, Alabama<br />
Wael El-Rifai, Nashville<br />
Sukru H Emre, New Haven<br />
Giamila Fantuzzi, Chicago<br />
Ashkan Farhadi, Irvine<br />
Ronnie Fass, Tucson<br />
Martín E Fernández-Zapico, Rochester<br />
Alessandro Fichera, Chicago<br />
Josef E Fischer, Boston<br />
Piero Marco Fisichella, Maywood<br />
Fritz Francois, New York<br />
Glenn T Furuta, Aurora<br />
T Clark Gamblin, Pittsburgh<br />
Henning Gerke, Iowa City<br />
Jean-Francois Geschwind, Baltimore<br />
R Mark Ghobrial, Texas<br />
John F Gibbs, Buffalo<br />
Shannon S Glaser, Temple<br />
Ajay Goel, Dallas<br />
Jon C Gould, Madison<br />
Eileen F Grady, San Francisco<br />
James H Grendell, New York<br />
John R Grider, Richmond<br />
Anna S Gukovskaya, Los Angeles<br />
Chakshu Gupta, St. Joseph<br />
Grigoriy E Gurvits, New York<br />
Hai-Yong Han, Phoenix<br />
Yuan-Ping Han, Los Angeles<br />
Imran Hassan, Springfield<br />
Charles P Heise, Madison<br />
Lisa J Herrinton, Oakland<br />
Oscar Joe Hines, Los Angeles<br />
Samuel B Ho, San Diego<br />
Steven Hochwald, Gainesville<br />
Richard Hu, Los Angeles<br />
Eric S Hungness, Chicago<br />
Jamal A Ibdah, Columbia<br />
Atif Iqbal, Omaha<br />
Hartmut Jaeschke, Tucson<br />
Donald M Jensen, Chicago<br />
Robert Jensen, Bethesda<br />
Leonard R Johnson, Memphis<br />
Andreas M Kaiser, Los Angeles<br />
JingXuan Kang, Charlestown<br />
John Y Kao, Michigan<br />
Randeep Singh Kashyap, New York<br />
Rashmi Kaul, Tulsa<br />
WJG|www.wjgnet.com<br />
Jonathan D Kaunitz, Los Angeles<br />
Stephen M Kavic, Baltimore<br />
Ali Keshavarzian, Chicago<br />
Amir Maqbul Khan, Marshall<br />
Kusum K Kharbanda, Omaha<br />
Chang Kim, West Lafayette<br />
Dean Y Kim, Detroit<br />
Miran Kim, Providence<br />
Burton I Korelitz, New York<br />
Josh Korzenik, Boston<br />
Richard A Kozarek, Seattle<br />
Alyssa M Krasinskas, Pittsburgh<br />
Shiu-Ming Kuo, Buffalo<br />
Michelle Lai, Boston<br />
Michael Leitman, New York<br />
Dong-Hui Li, Houston<br />
Ming Li, New Orleans<br />
Zhiping Li, Baltimore<br />
Gary R Lichtenstein, Philadelphia<br />
Chen Liu, Gainesville<br />
Zhang-Xu Liu, Los Angeles<br />
Craig D Logsdon, Houston<br />
Kaye M Reid Lombardo, Rochester<br />
Michael R Lucey, Madison<br />
Kirk Ludwig, Wisconsin<br />
James D Luketich, Pittsburgh<br />
Patrick M Lynch, Houston<br />
John S Macdonald, New York<br />
Willis C Maddrey, Dallas<br />
Mercedes Susan Mandell, Aurora<br />
Christopher Mantyh, Durham<br />
Wendy M Mars, Pittsburgh<br />
John Marshall, Columbia<br />
Robert CG Martin, Louisville<br />
Laura E Matarese, Pittsburgh<br />
Craig J McClain, Louisville<br />
Lynne V McFarland, Washington<br />
David J McGee, Shreveport<br />
Valentina Medici, Sacramento<br />
Stephan Menne, New York<br />
Didier Merlin, Atlanta<br />
George Michalopoulos, Pittsburgh<br />
James M Millis, Chicago<br />
Pramod K Mistry, New Haven<br />
Emiko Mizoguchi, Boston<br />
Huanbiao Mo, Denton<br />
Robert C Moesinger, Ogden<br />
Smruti R Mohanty, Chicago<br />
John Morton, Stanford<br />
Peter L Moses, Burlington<br />
Sandeep Mukherjee, Omaha<br />
Million Mulugeta, Los Angeles<br />
Michel M Murr, Tampa<br />
Pete Muscarella, Columbus<br />
Ece A Mutlu, Chicago<br />
Masaki Nagaya, Boston<br />
Laura E Nagy, Cleveland<br />
Aejaz Nasir, Tampa<br />
Udayakumar Navaneethan, Cincinnati<br />
Stephen JD O’Keefe, Pittsburgh<br />
Robert D Odze, Boston<br />
Giuseppe Orlando, Winston Salem<br />
Pal Pacher, Rockville<br />
Georgios Papachristou, Pittsburgh<br />
Jong Park, Tampa<br />
William R Parker, Durham<br />
Mansour A Parsi, Cleveland<br />
Marco Giuseppe Patti, Chicago<br />
Zhiheng Pei, New York<br />
CS Pitchumoni, New Brunswiuc<br />
Parviz M Pour, Omaha<br />
Xia<strong>of</strong>a Qin, Newark<br />
Florencia Georgina Que, Rochester<br />
Massimo Raimondo, Jacksonville<br />
VII<br />
Raymund R Razonable, Minnesota<br />
Kevin Michael Reavis, Orange<br />
Robert V Rege, Dallas<br />
Douglas K Rex, Indianapolis<br />
Victor E Reyes, Galveston<br />
Basil Rigas, New York<br />
Richard A Rippe, Chapel Hill<br />
Alexander S Rosemurgy, Tampa<br />
Philip Rosenthal, San Francisco<br />
Raul J Rosenthal, Weston<br />
Joel H Rubenstein, Ann Arbor<br />
Shawn D Safford, Norfolk<br />
Rabih M Salloum, Rochester<br />
Bruce E Sands, Boston<br />
Tor C Savidge, Galveston<br />
Michael L Schilsky, New Haven<br />
Beat Schnüriger, California<br />
Robert E Schoen, Pittsburgh<br />
Matthew James Schuchert, Pittsburgh<br />
Ekihiro Seki, La Jolla<br />
Le Shen, Chicago<br />
Perry Shen, Winston-Salem<br />
Stuart Sherman, Indianapolis<br />
Mitchell L Shiffman, Richmond<br />
Shivendra Shukla, Columbia<br />
Bronislaw L Slomiany, Newark<br />
Scott Steele, Fort Lewis<br />
Branko Stefanovic, Tallahassee<br />
Lygia Stewart, San Francisco<br />
Luca Stocchi, Cleveland<br />
Daniel S Straus, Riverside<br />
Robert Todd Striker, Madison<br />
Jonathan Strosberg, Tampa<br />
Christina Surawicz, Seattle<br />
Patricia Sylla, Boston<br />
Wing-Kin Syn, Durham<br />
Yvette Taché, Los Angeles<br />
Kazuaki Takabe, Richmond<br />
Kam-Meng Tchou-Wong, New York<br />
Klaus Thaler, Columbia<br />
Charles Thomas, Oregon<br />
Natalie J Torok, Sacramento<br />
George Triadafilopoulos, Stanford<br />
Chung-Jyi Tsai, Lexington<br />
Thérèse Tuohy, Salt Lake City<br />
Andrew Ukleja, Florida<br />
Santhi Swaroop Vege, Rochester<br />
Aaron Vinik, Norfolk<br />
Dinesh Vyas, Washington<br />
Arnold Wald, Wisconsin<br />
Scott A Waldman, Philadelphia<br />
Jack R Wands, Providence<br />
Jiping Wang, Boston<br />
Irving Waxman, Chicago<br />
Wilfred M Weinstein, Los Angeles<br />
Steven D Wexner, Weston<br />
John W Wiley, Ann Arbor<br />
Jackie Wood, Ohio<br />
Jian Wu, Sacramento<br />
Wen Xie, Pittsburgh<br />
Guang-Yin Xu, Galveston<br />
Fang Yan, Nashville<br />
Radha Krishna Yellapu, New York<br />
Anthony T Yeung, Philadelphia<br />
Zobair M Younossi, Virginia<br />
Liqing Yu, Winston-Salem<br />
Run Yu, Los Angeles<br />
Ruben Zamora, Pittsburgh<br />
Michael E Zenilman, New York<br />
Mark A Zern, Sacramento<br />
Lin Zhang, Pittsburgh<br />
Martin D Zielinski, Rochester<br />
Michael A Zimmerman, Colorado<br />
January 7, 2011
Contents<br />
BRIEF ARTICLE<br />
WJG|www.wjgnet.com<br />
<strong>World</strong> <strong>Journal</strong> <strong>of</strong> Gastroenterology<br />
Volume 17 Number 7 February 21, 2011<br />
906 Outcome <strong>of</strong> non surgical hepatic decompression procedures in Egyptian<br />
patients with Budd-Chiari<br />
Eldorry A, Barakat E, Abdella H, Abdelhakam S, Shaker M, Hamed A, Sakr M<br />
914 Body mass index is associated with age-at-onset <strong>of</strong> HCV-infected<br />
hepatocellular carcinoma patients<br />
Akiyama T, Mizuta T, Kawazoe S, Eguchi Y, Kawaguchi Y, Takahashi H, Ozaki I, Fujimoto K<br />
922 Vitamin D deficiency in cirrhosis relates to liver dysfunction rather than<br />
aetiology<br />
Malham M, Jørgensen SP, Ott P, Agnholt J, Vilstrup H, Borre M, Dahlerup JF<br />
926 Natural orifice transluminal endoscopic wedge hepatic resection with a water-<br />
jet hybrid knife in a non-survival porcine model<br />
Shi H, Jiang SJ, Li B, Fu DK, Xin P, Wang YG<br />
932 Upregulated CD133 expression in tumorigenesis <strong>of</strong> colon <strong>cancer</strong> cells<br />
Yang ZL, Zheng Q, Yan J, Pan Y, Wang ZG<br />
938 Transplantation <strong>of</strong> microencapsulated umbilical-cord-blood-derived hepatic-<br />
like cells for treatment <strong>of</strong> hepatic failure<br />
Zhang FT, Wan HJ, Li MH, Ye J, Yin MJ, Huang CQ, Yu J<br />
946 Primary clear cell carcinoma in the liver: CT and MRI findings<br />
Liu QY, Li HG, Gao M, Lin XF, Li Y, Chen JY<br />
February 21, 2011|Volume 17| ssue 7|
Contents<br />
APPENDIX<br />
FLYLEAF<br />
EDITORS FOR<br />
THIS ISSUE<br />
NAME OF JOURNAL<br />
<strong>World</strong> <strong>Journal</strong> <strong>of</strong> Gastroenterology<br />
LAUNCH DATE<br />
October 1, 1995<br />
RESPONSIBLE INSTITUTION<br />
Department <strong>of</strong> Science and Technology <strong>of</strong> Shanxi<br />
Province<br />
SPONSOR<br />
Taiyuan Research and Treatment Center for Digestive<br />
Diseases, 77 Shuangta Xijie, Taiyuan 030001, Shanxi<br />
Province, China<br />
EDITING<br />
Editorial Board <strong>of</strong> <strong>World</strong> <strong>Journal</strong> <strong>of</strong> Gastroenterology,<br />
Room 903, Building D, Ocean International Center,<br />
No. 62 Dongsihuan Zhonglu, Chaoyang District,<br />
Beijing 100025, China<br />
Telephone: +86-10-5908-0039<br />
Fax: +86-10-8538-1893<br />
E-mail: wjg@wjgnet.com<br />
http://www.wjgnet.com<br />
PUBLISHING<br />
Baishideng Publishing Group Co., Limited,<br />
Room 1701, 17/F, Henan Building,<br />
No.90 Jaffe Road, Wanchai, Hong Kong, China<br />
Fax: +852-3115-8812<br />
Telephone: +852-5804-2046<br />
E-mail: baishideng@wjgnet.com<br />
http://www.wjgnet.com<br />
SUBSCRIPTION<br />
Beijing Baishideng BioMed Scientific Co., Ltd.,<br />
Room 903, Building D, Ocean International Center,<br />
No. 62 Dongsihuan Zhonglu, Chaoyang District,<br />
Beijing 100025, China<br />
Telephone: +86-10-8538-1892<br />
Fax: +86-10-8538-1893<br />
E-mail: baishideng@wjgnet.com<br />
http://www.wjgnet.com<br />
<strong>World</strong> <strong>Journal</strong> <strong>of</strong> Gastroenterology<br />
Volume 17 Number 7 February 21, 2011<br />
ACKNOWLEDGMENTS I Acknowledgments to reviewers <strong>of</strong> <strong>World</strong> <strong>Journal</strong> <strong>of</strong> Gastroenterology<br />
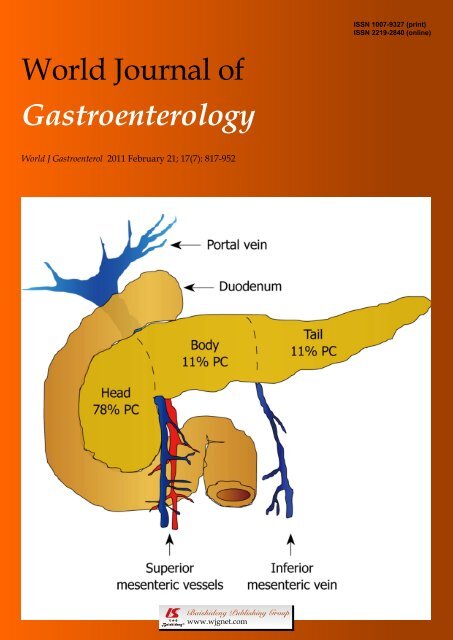
ABOUT COVER<br />
AIM AND SCOPE<br />
WJG|www.wjgnet.com<br />
I Meetings<br />
I-VI Instructions to authors<br />
Sharma C, Eltawil KM, Renfrew PD, Walsh MJ, Molinari M. Advances in diagnosis,<br />
treatment and palliation <strong>of</strong> pancreatic carcinoma: 1990-2010.<br />
<strong>World</strong> J Gastroenterol 2011; 17(7): 867-897<br />
http://www.wjgnet.com/1007-9327/full/v17/i7/867.htm<br />
<strong>World</strong> <strong>Journal</strong> <strong>of</strong> Gastroenterology (<strong>World</strong> J Gastroenterol, WJG, print ISSN 1007-9327, DOI:<br />
10.3748) is a weekly, open-access, peer-reviewed journal supported by an editorial board <strong>of</strong><br />
1144 experts in gastroenterology and hepatology from 60 countries.<br />
The major task <strong>of</strong> WJG is to report rapidly the most recent results in basic and clinical<br />
research on esophageal, gastrointestinal, liver, pancreas and biliary tract diseases, Helicobacter<br />
pylori, endoscopy and gastrointestinal surgery, including: gastroesophageal reflux disease,<br />
gastrointestinal bleeding, infection and tumors; gastric and duodenal disorders; intestinal<br />
inflammation, micr<strong>of</strong>lora and immunity; celiac disease, dyspepsia and nutrition; viral hepatitis,<br />
portal hypertension, liver fibrosis, liver cirrhosis, liver transplantation, and metabolic liver<br />
disease; molecular and cell biology; geriatric and pediatric gastroenterology; diagnosis and<br />
screening, imaging and advanced technology.<br />
I-VII Editorial Board<br />
Responsible Assistant Editor: Xiao-Fang Liu Responsible Science Editor: Zhong-Fang Shi<br />
Responsible Electronic Editor: Wen-Hua Ma Pro<strong>of</strong>ing Editorial Office Director: Jian-Xia Cheng<br />
Pro<strong>of</strong>ing Editor-in-Chief: Lian-Sheng Ma<br />
PRINT SUBSCRIPTION<br />
RMB 245 Yuan for each issue, RMB 11760 Yuan for<br />
one year.<br />
ONLINE SUBSCRIPTION<br />
One-Year Price 864.00 USD<br />
PUBLICATION DATE<br />
February 21, 2011<br />
SERIAL PUBLICATION NUMBER<br />
ISSN 1007-9327 (print)<br />
ISSN 2219-2840 (online)<br />
HONORARY EDITORS-IN-CHIEF<br />
James L Boyer, New Haven<br />
Ke-Ji Chen, Beijing<br />
Martin H Floch, New Haven<br />
Geng-Tao Liu, Beijing<br />
Emmet B Keeffe, Palo Alto<br />
Lein-Ray Mo, Tainan<br />
Eamonn M Quigley, Cork<br />
Rafiq A Sheikh, Sacramento<br />
Nicholas J Talley, Rochester<br />
Ming-Lung Yu, Kaohsiung<br />
PRESIDENT AND EDITOR-IN-CHIEF<br />
Lian-Sheng Ma, Beijing<br />
ACADEMIC EDITOR-IN-CHIEF<br />
Tauseef Ali, Oklahoma<br />
Mauro Bortolotti, Bologna<br />
Tarkan Karakan, Ankara<br />
Weekitt Kittisupamongkol, Bangkok<br />
Anastasios Koulaouzidis, Edinburgh<br />
Gerd A Kullak-Ublick, Zürich<br />
Bo-Rong Pan, Xi’an<br />
Sylvia LF Pender, Southampton<br />
Max S Petrov, Auckland<br />
George Y Wu, Farmington<br />
STRATEGY ASSOCIATE EDITORS-IN-CHIEF<br />
Peter Draganov, Florida<br />
Hugh J Freeman, Vancouver<br />
Maria Concepción Gutiérrez-Ruiz, México<br />
Kazuhiro Hanazaki, Kochi<br />
Akio Inui, Kagoshima<br />
Kalpesh Jani, Baroda<br />
Javier S Martin, Punta del Este<br />
Natalia A Osna, Omaha<br />
Wei Tang, Tokyo<br />
Alan BR Thomson, Edmonton<br />
Harry HX Xia, Hanover<br />
ASSOCIATE EDITORS-IN-CHIEF<br />
You-Yong Lu, Beijing<br />
John M Luk, Pokfulam<br />
Hiroshi Shimada, Yokohama<br />
EDITORIAL OFFICE<br />
Jian-Xia Cheng, Director<br />
<strong>World</strong> <strong>Journal</strong> <strong>of</strong> Gastroenterology<br />
Room 903, Building D, Ocean International Center,<br />
No. 62 Dongsihuan Zhonglu, Chaoyang District,<br />
Beijing 100025, China<br />
Telephone: +86-10-5908-0039<br />
Fax: +86-10-8538-1893<br />
E-mail: wjg@wjgnet.com<br />
http://www.wjgnet.com<br />
COPYRIGHT<br />
© 2011 Baishideng. Articles published by this Open-<br />
Access journal are distributed under the terms <strong>of</strong> the<br />
Creative Commons Attribution Non-commercial<br />
License, which permits use, distribution, and reproduction<br />
in any medium, provided the original work<br />
is properly cited, the use is non commercial and is<br />
otherwise in compliance with the license.<br />
SPECIAL STATEMENT<br />
All articles published in this journal represent the<br />
viewpoints <strong>of</strong> the authors except where indicated<br />
otherwise.<br />
INSTRUCTIONS TO AUTHORS<br />
Full instructions are available online at http://www.<br />
wjgnet.com/1007-9327/g_info_20100315215714.htm.<br />
If you do not have web access please contact the<br />
editorial <strong>of</strong>fice.<br />
ONLINE SUBMISSION<br />
http://www.wjgnet.com/1007-9327<strong>of</strong>fice<br />
February 21, 2011|Volume 17| ssue 7|
Online Submissions: http://www.wjgnet.com/1007-9327<strong>of</strong>fice<br />
wjg@wjgnet.com<br />
doi:10.3748/wjg.v17.i7.817<br />
MicroRNAs in pancreatic ductal adenocarcinoma<br />
Jong Y Park, James Helm, Domenico Coppola, Donghwa Kim, Mokenge Malafa, Seung Joon Kim<br />
Jong Y Park, Division <strong>of</strong> Cancer Prevention and Control, M<strong>of</strong>fitt<br />
Cancer Center, FL 33612, United States<br />
James Helm, Mokenge Malafa, Gastrointestinal Tumor Program,<br />
M<strong>of</strong>fitt Cancer Center, FL 33612, United States<br />
Domenico Coppola, Department <strong>of</strong> Anatomic Pathology, M<strong>of</strong>fitt<br />
Cancer Center, FL 33612, United States<br />
Donghwa Kim, Department <strong>of</strong> Molecular Oncology, M<strong>of</strong>fitt<br />
Cancer Center, FL 33612, United States<br />
Seung Joon Kim, Department <strong>of</strong> Internal Medicine, College<br />
<strong>of</strong> Medicine, the Catholic University <strong>of</strong> Korea, Seoul 137-040,<br />
South Korea<br />
Author contributions: Park JY drafted the initial concept,<br />
wrote, reviewed and finalized the manuscript; Helm J provided<br />
clinical information, participated in writing, and revised the<br />
manuscript; Coppola D provided clinical information, participated<br />
in writing, and revised the manuscript; Kim D provided<br />
valuable advice for study design and drew the figure; Malafa<br />
M provided clinical information, participated in writing, and<br />
revised the manuscript; Kim SJ designed the manuscript format,<br />
collected the references and wrote the manuscript.<br />
Supported by M<strong>of</strong>fitt Faculty Support Fund<br />
Correspondence to: Seung Joon Kim, MD, PhD, Department<br />
<strong>of</strong> Internal Medicine, College <strong>of</strong> Medicine, the Catholic<br />
University <strong>of</strong> Korea, Seoul 137-040,<br />
South Korea. cmcksj@catholic.ac.kr<br />
Telephone: +82-2-22586063 Fax: +82-2-5993589<br />
Received: August 14, 2010 Revised: November 25, 2010<br />
Accepted: December 2, 2010<br />
Published online: February 21, 2011<br />
Abstract<br />
Ductal adenocarcinoma <strong>of</strong> the pancreas is a lethal <strong>cancer</strong><br />
for which the only chance <strong>of</strong> long-term survival<br />
belongs to the patient with localized disease in whom<br />
a potentially curative resection can be done. Therefore,<br />
biomarkers for early detection and new therapeutic strategies<br />
are urgently needed. miRNAs are a recently discovered<br />
class <strong>of</strong> small endogenous non-coding RNAs <strong>of</strong><br />
about 22 nucleotides that have gained attention for their<br />
role in downregulation <strong>of</strong> mRNA expression at the posttranscriptional<br />
level. miRNAs regulate proteins involved<br />
in critical cellular processes such as differentiation, proliferation,<br />
and apoptosis. Evidence suggests that deregu-<br />
WJG|www.wjgnet.com<br />
817<br />
<strong>World</strong> J Gastroenterol 2011 February 21; 17(7): 817-827<br />
ISSN 1007-9327 (print) ISSN 2219-2840 (online)<br />
© 2011 Baishideng. All rights reserved.<br />
EDITORIAL<br />
lated miRNA expression is involved in carcinogenesis at<br />
many sites, including the pancreas. Aberrant expression<br />
<strong>of</strong> miRNAs may upregulate the expression <strong>of</strong> oncogenes<br />
or downregulate the expression <strong>of</strong> tumor suppressor<br />
genes, as well as play a role in other mechanisms <strong>of</strong> carcinogenesis.<br />
The purpose <strong>of</strong> this review is to summarize<br />
our knowledge <strong>of</strong> deregulated miRNA expression in pancreatic<br />
<strong>cancer</strong> and discuss the implication for potential<br />
translation <strong>of</strong> this knowledge into clinical practice.<br />
© 2011 Baishideng. All rights reserved.<br />
Key words: MicroRNAs; Pancreatic <strong>cancer</strong><br />
Peer reviewer: Yoshiharu Motoo, MD, PhD, FACP, FACG,<br />
Pr<strong>of</strong>essor and Chairman, Department <strong>of</strong> Medical Oncology,<br />
Kanazawa Medical University, 1-1 Daigaku, Uchinada,<br />
Ishikawa 920-0293, Japan<br />
Park JY, Helm J, Coppola D, Kim D, Malafa M, Kim SJ. MicroRNAs<br />
in pancreatic ductal adenocarcinoma. <strong>World</strong> J Gastroenterol<br />
2011; 17(7): 817-827 Available from: URL: http://www.<br />
wjgnet.com/1007-9327/full/v17/i7/817.htm DOI: http://dx.doi.<br />
org/10.3748/wjg.v17.i7.817<br />
INTRODUCTION<br />
Pancreatic <strong>cancer</strong> is the fourth leading cause <strong>of</strong> <strong>cancer</strong>-related<br />
mortality in the United States, with 36 800 estimated<br />
deaths in 2010, with the great majority being due to ductal<br />
adenocarcinomas [1] . Due to the asymptomatic onset <strong>of</strong><br />
pancreatic <strong>cancer</strong>, most patients are in advanced or metastatic<br />
condition at the time <strong>of</strong> diagnosis, resulting in poor<br />
prognosis. Most patients found to have pancreatic <strong>cancer</strong><br />
die within 12 mo, and few survive 5 years after diagnosis.<br />
The poor prognosis <strong>of</strong> these patients is due to its late<br />
clinical presentation with symptoms, early and aggressive<br />
local invasion, and high metastatic potential [2] . Advances in<br />
chemo-radiation therapy have been slow over the last few<br />
decades, and the overall prognosis in pancreatic <strong>cancer</strong> has<br />
remained essentially unchanged. The only chance <strong>of</strong> longterm<br />
survival with pancreatic adenocarcinoma belongs to<br />
February 21, 2011|Volume 17|Issue 7|
Park JY et al . MicroRNAs in pancreatic <strong>cancer</strong><br />
Table 1 miRNA deregulation in human pancreatic <strong>cancer</strong><br />
miRNA Lee<br />
et al [49]<br />
Szafranska<br />
et al [50]<br />
Bloomston<br />
et al [51]<br />
Zhang<br />
et al [52]<br />
Other Outcome<br />
let-7 ↓ [53]<br />
let-7d ↑ 1<br />
let-7f-1 ↑<br />
miR-10a ↑ ↑ [54]<br />
miR-10b ↑<br />
miR-15b ↑ ↑<br />
miR-16-1 ↑<br />
miR-18a ↑<br />
miR-21 ↑ ↑<br />
[55, 56]<br />
↑ Poor [55]<br />
miR-23a ↑<br />
miR-23b ↑<br />
miR-24-1,2 ↑<br />
miR-29c ↓<br />
miR-31 ↑<br />
miR-92-1 ↑<br />
miR-93 ↑<br />
miR-95 ↑<br />
miR-96 ↓<br />
miR-99 ↑<br />
miR-100 ↑ ↑<br />
miR-100-1/2 ↑<br />
miR-103-2 ↑<br />
miR-107 ↑ ↑<br />
miR-125a ↑<br />
miR-125b-1 ↑ ↑<br />
miR-130b ↓<br />
miR-139 ↓<br />
miR-141 ↓<br />
miR-142-P ↓<br />
miR-143 ↑ ↑<br />
miR-145 ↑<br />
miR-146 ↑<br />
miR-146a ↑<br />
miR-148a ↓ ↓<br />
miR-148b ↓ ↓<br />
miR-150 ↑<br />
miR-155 ↑ ↑ ↑ Poor [57]<br />
miR-181a ↑ ↑<br />
miR-181b ↑<br />
miR-181b-1 ↑<br />
miR-181b-2 ↑<br />
miR-181c ↑ ↑<br />
miR-181d ↑<br />
miR-186 ↑<br />
miR-190 ↑<br />
miR-196a ↑ ↑ miR-<br />
196a-2;<br />
Poor [51]<br />
miR-196b ↑<br />
miR-199a-1 ↑<br />
miR-199a-2 ↑<br />
miR-200b ↑<br />
miR-203 ↑ Poor [57]<br />
miR-205 ↑ ↑<br />
miR-210 ↑ ↑ Poor [57]<br />
miR-212 ↑<br />
miR-213 ↑<br />
miR-216 ↓<br />
miR-217 ↓<br />
miR-220 ↑<br />
miR-221 ↑ ↑ ↑ ↑<br />
miR-222 ↑ ↑ ↑ Poor [57]<br />
miR-223 ↑ ↑<br />
miR-224 ↑<br />
miR-301 ↑<br />
miR-345 ↓<br />
WJG|www.wjgnet.com<br />
miR-375 ↓ ↓<br />
miR-376a ↑<br />
miR-424 ↑<br />
1 Arrows indicate increased (↑) or decreased (↓) expression <strong>of</strong> the specified<br />
miRNA.<br />
duced at the transcriptional level by transforming growth<br />
factor β/Smad, nuclear factor-κB and activator protein-1<br />
family transcription factors through direct interaction with<br />
the miR-155/BIC promoter [46-48] . Further studies have<br />
shown that miR-155 processing also regulates mature<br />
miR-155 expression levels [36,45] , suggesting that overexpression<br />
<strong>of</strong> miR-155 in <strong>cancer</strong> is due to transcriptional activation<br />
and miRNA processing.<br />
miRNA EXPRESSION PROFILE IN<br />
NORMAL PANCREATIC TISSUE AND<br />
PANCREATIC TUMOR<br />
miRNA expression pr<strong>of</strong>iles in pancreatic tumor tissues<br />
are different from those identified in normal pancreas or<br />
in chronic pancreatitis. Most miRNA expression pr<strong>of</strong>ile<br />
analyses show that miRNAs are deregulated in tumor<br />
tissues as compared to normal pancreas, and that the expression<br />
pattern is tissue specific. Several studies focusing<br />
on miRNA expression pr<strong>of</strong>iles in pancreatic tissues have<br />
identified a number <strong>of</strong> differentially expressed miRNAs.<br />
Table 1 summarizes the aberrantly expressed miRNAs in<br />
human pancreatic <strong>cancer</strong> and their association with patient<br />
survival.<br />
Szafranska et al [50] have performed the first comprehensive<br />
miRNA expression pr<strong>of</strong>ile study in tissues from normal<br />
pancreas (n = 7), chronic pancreatitis (n = 7), PDAC<br />
(n = 10) and 33 human tissues <strong>of</strong> different non-pancreatic<br />
origin, to identify miRNA candidates with a potential for<br />
future clinical application from a pool <strong>of</strong> 377 known and<br />
novel miRNAs. The authors have found that two miR-<br />
NAs, miR-216 and miR-217, are pancreas-specific. These<br />
results were in agreement with those <strong>of</strong> two previous<br />
studies [58,59] . Furthermore, both miR-216 and miR-217 are<br />
absent or only minimally expressed in pancreatic carcinoma<br />
tissues and cell lines. Therefore, miR-216 and miR-217<br />
are potential biomarkers. Based upon clustering analysis,<br />
the three pancreatic tissues types can be classified according<br />
to their respective miRNA expression pr<strong>of</strong>iles. Among<br />
26 miRNAs that have been identified as most prominently<br />
deregulated in PDAC, only miR-217 and miR-196a have<br />
been found to discriminate between normal pancreas,<br />
chronic pancreatitis and tumor tissues. These miRNAs are<br />
also potential biomarkers.<br />
Recently, expression <strong>of</strong> 201 miRNA precursors (representing<br />
222 miRNAs) was pr<strong>of</strong>iled in pancreatic adenocarcinoma,<br />
paired with benign tissue, normal pancreas,<br />
chronic pancreatitis and pancreatic <strong>cancer</strong> cell lines with<br />
the real-time PCR miRNA array [49] . These three cell types<br />
could be classified by the clustering algorithm. One hundred<br />
miRNA precursors have been identified as aberrantly<br />
820 February 21, 2011|Volume 17|Issue 7|
expressed miRNAs including known ones in other <strong>cancer</strong>s<br />
and novel ones in pancreatic tumor. A list <strong>of</strong> the top 20<br />
aberrantly expressed miRNA precursors has been proposed<br />
as a signature for pancreatic adenocarcinoma.<br />
Bloomston et al [51] have identified a large global expression<br />
pattern <strong>of</strong> miRNAs that can differentiate PDAC<br />
from chronic pancreatitis with 93% accuracy. Among several<br />
deregulated miRNAs in the pancreatic <strong>cancer</strong>s, most<br />
notably, miR-21 and miR-155 are uniquely overexpressed<br />
in pancreatic tumor, as compared to tissues from normal<br />
pancreas and chronic pancreatitis. Both miR-21 and<br />
miR-155 have been suggested to play an important role in<br />
functioning as a proto-oncogene and have been shown to<br />
be overexpressed in several <strong>cancer</strong>s. These authors have<br />
performed an miRNA microarray pr<strong>of</strong>iling with about<br />
1100 miRNA probes, which included 326 human miR-<br />
NAs, using microdissected pancreatic tumor tissues.<br />
Zhang et al [52] have evaluated 95 miRNAs, selected<br />
from pancreatic <strong>cancer</strong> pr<strong>of</strong>iling, and correlated them<br />
to their potential biological functions related to <strong>cancer</strong><br />
biology, cell development, and apoptosis. Among them,<br />
eight miRNAs (miR-196a, miR-190, miR-186, miR-221,<br />
miR-222, miR-200b, miR-15b, and miR-95) are differentially<br />
expressed in most pancreatic <strong>cancer</strong> tissues and<br />
cell lines. All <strong>of</strong> these eight genes are significantly unregulated,<br />
from 3- to 2018-fold, in pancreatic tumors as<br />
compared with normal control samples.<br />
In summary, these pr<strong>of</strong>iling data may provide novel<br />
insights into the miRNA-driven mechanisms involved<br />
in pancreatic carcinogenesis, and <strong>of</strong>fer new potential<br />
targets for early detection and therapeutic strategies in<br />
pancreatic <strong>cancer</strong>.<br />
miRNAS AS BIOMARKERS FOR<br />
PANCREATIC CANCER DIAGNOSIS<br />
Development <strong>of</strong> biomarkers for pancreatic <strong>cancer</strong> is<br />
especially critical because most patients with this disease<br />
remain asymptomatic until the disease progresses to become<br />
locally advanced or develops distant metastases.<br />
Therefore, most <strong>of</strong> these patients are surgically inoperable<br />
at the time <strong>of</strong> diagnosis. Sensitive and specific biomarkers<br />
for pancreatic <strong>cancer</strong> are urgently needed to <strong>of</strong>fer better<br />
therapeutic options and survival outcome.<br />
Over the years, a number <strong>of</strong> protein- and DNAbased<br />
biomarkers have been proposed as markers <strong>of</strong> early<br />
detection for pancreatic <strong>cancer</strong>. However, most <strong>of</strong> these<br />
markers fail to have clinical potential, and they have not<br />
influenced patients’ survival. Since the first discovery <strong>of</strong><br />
miRNAs by Lee et al [11] in 1993, many researchers have<br />
investigated expression pr<strong>of</strong>iles, biological functions and<br />
targets <strong>of</strong> miRNAs in carcinogenesis and tumor progression,<br />
with the purpose <strong>of</strong> translating the results to clinical<br />
settings.<br />
Endoscopic ultrasound-guided fine-needle aspiration<br />
(EUS-FNA) <strong>of</strong> the pancreas is not likely to be used routinely<br />
for screening for PDAC because <strong>of</strong> its invasive na-<br />
WJG|www.wjgnet.com<br />
Park JY et al . MicroRNAs in pancreatic <strong>cancer</strong><br />
ture. However, this procedure has recently emerged as a<br />
specific and minimally invasive modality for preoperative<br />
diagnosis and staging <strong>of</strong> pancreatic <strong>cancer</strong>. Furthermore,<br />
EUS-FNA may also be useful for screening high-risk<br />
individuals, as well as for the prognosis and predicting<br />
the response to treatment in cases in which the tumor is<br />
inoperable [60-62] . Szafranska et al [63] have identified potential<br />
miRNA markers in EUS-FNA biopsies <strong>of</strong> pancreatic<br />
tissue. The combination <strong>of</strong> expression pattern <strong>of</strong> miR-<br />
196a and miR-217 can differentiate PDAC cases from<br />
healthy controls and chronic pancreatitis in the FNA<br />
samples. Furthermore, miR-196a expression is likely specific<br />
to PDAC cells and is positively associated with the<br />
progression <strong>of</strong> PDAC.<br />
Carcinogenesis in PDAC develops with a multistep<br />
progression from morphologically distinct non-invasive<br />
precursor lesions within exocrine pancreatic ducts [64] .<br />
These precursors include the intraductal papillary mucinous<br />
neoplasms (IPMNs), the mucinous cystic neoplasms,<br />
and pancreatic intraepithelial neoplasia (PanIN). Two<br />
studies have been carried out to detect expression patterns<br />
<strong>of</strong> miRNA in IPMNs and PanIN. IPMNs are grossly<br />
visible, non-invasive, mucin-producing precursors <strong>of</strong><br />
pancreatic <strong>cancer</strong> within the main pancreatic duct or one<br />
<strong>of</strong> its branches [65,66] . In contrast, PanINs are non-invasive,<br />
microscopic epithelial neoplasms, arising within smaller<br />
pancreatic ducts, < 5 mm in diameter, and characterized<br />
by cytological and architectural atypia [65,67] . Habbe et al [68]<br />
have reported significant overexpression <strong>of</strong> 10 miRNAs<br />
in IPMNs (n = 15). miR-155 and miR-21 show the highest<br />
relative fold-changes in the precursor lesions. These<br />
results have been validated by in situ hybridization analysis.<br />
miR-155 and miR-21 are upregulated in most IPMNs [83%<br />
(53/64) and 81% (52/64)] as compared to normal ducts<br />
[7% (4/54) and 2% (1/54)]. With these promising data,<br />
the potential use <strong>of</strong> these miRNAs as biomarkers has<br />
been evaluated in pancreatic juices. A total <strong>of</strong> 15 pancreatic<br />
juice samples from 10 patients with IPMNs, and five<br />
with other pancreatobiliary disorders obtained at the time<br />
<strong>of</strong> surgical resection were measured for relative levels <strong>of</strong><br />
miR-155 and miR-21 by quantitative real-time RT-PCR.<br />
Upregulation <strong>of</strong> both miR-155 and miR-21 in the subset<br />
<strong>of</strong> IPMN-associated pancreatic juices was observed, as<br />
compared with control samples. These results indicate that<br />
aberrant miRNA expression occurs early in the precursor<br />
lesion during the multiple <strong>stage</strong>s <strong>of</strong> pancreatic <strong>cancer</strong><br />
development, and miRNA pr<strong>of</strong>iles may be assessed with<br />
more accessible clinical samples, such as pancreatic juice,<br />
and could be used as a diagnostic tool.<br />
du Rieu et al [69] have investigated miRNAs in PanIN<br />
tissues from a conditional Kras (G12D) mouse model<br />
(n = 29) and from human origin (n = 38). Expression<br />
<strong>of</strong> miR-21, miR-205 and miR-200 has been found to be<br />
positively associated with PanIN progression in the Kras<br />
(G12D) mouse model. In the human tissues, expression<br />
<strong>of</strong> miR-21, miR-221, miR-222 and let-7a increases with<br />
PanIN grade. The authors, using in situ hybridization<br />
analysis, have observed that miR-21 expression is concen-<br />
821 February 21, 2011|Volume 17|Issue 7|
Park JY et al . MicroRNAs in pancreatic <strong>cancer</strong><br />
Table 2 miRNAs and their targets involved in human pancreatic <strong>cancer</strong><br />
miRNA Function Targets Related cellular events Ref.<br />
let-7 Suppress RAS [71]<br />
Inhibit cell proliferation, KRAS expression, and mitogen-activated protein kinase<br />
activation<br />
let-7, miR-200 Suppress Reverse EMT<br />
Let-7a Suppress RAS Attenuate KRAS expression and radiosensitize tumor cell<br />
miR-10a Oncogenic HOXB1, 3 Promote metastatic behavior<br />
miR-21 Oncogenic Induce cell proliferation, invasion, chemoresistance<br />
miR-21 Oncogenic Potentially associated with cell proliferation<br />
miR-200c Suppress Potentially associated with G0/G1 arrest and increased apoptotic rate<br />
miR-21,<br />
miR-221<br />
trated in the dysplastic ductal epithelial cells. Using PDACderived<br />
cell lines, they also have noted that miR-21 expression<br />
is regulated by Kras (G12D) and epidermal growth<br />
factor receptor (EGFR).<br />
Wang et al [70] have studied plasma samples from patients<br />
with PDAC and have found that four miRNAs<br />
(miR-21, miR-210, miR-155 and miR-196a) are able to differentiate<br />
pancreatic <strong>cancer</strong> patients from healthy controls,<br />
with moderate accuracy (sensitivity: 64%, and specificity:<br />
89%). In summary, these studies suggest a potential value<br />
<strong>of</strong> miRNAs in the clinical setting as a potential diagnostic<br />
tool for PDAC.<br />
miRNAS AS ONCOGENES AND TUMOR<br />
SUPPRESSORS<br />
Oncogenic PTEN, RECK,<br />
CDKN1B<br />
miRNAs are functionally classified into oncogenes or tumor<br />
suppressors based upon their targets, thus binding to<br />
oncogenes or tumor suppressor genes. Therefore, oncogenic<br />
miRNAs are upregulated in tumors, whereas tumor<br />
suppressor miRNAs are downregulated. The functions<br />
and targets <strong>of</strong> a handful <strong>of</strong> miRNAs have been investigated<br />
in pancreatic <strong>cancer</strong> (Table 2).<br />
Torrisani et al [53] have reported that tumor suppressor<br />
let-7 miRNA is expressed in normal acinar pancreatic<br />
cells, but is extensively downregulated in PDAC samples,<br />
as compared with adjacent non-involved tissues. Transfection<br />
<strong>of</strong> pancreatic <strong>cancer</strong> cell lines with let-7 miRNA<br />
inhibits cell proliferation, Kras expression, and mitogenactivated<br />
protein kinase activation. This study has demonstrated<br />
that intracellular restoration <strong>of</strong> let-7 miRNA<br />
reverts neoplastic characteristics <strong>of</strong> PDAC, suggesting<br />
that let-7 miRNA functions as a tumor suppressor in pan-<br />
WJG|www.wjgnet.com<br />
Arrest cell cycle, induce apoptosis, and sensitize the effects <strong>of</strong> gemcitabine with<br />
inhibition <strong>of</strong> miR-21 or -221<br />
miR-22 Suppress SP1, ESR1 Potentially inhibit tumorigenesis<br />
miR-34 Suppress BCL2, NOTCH1/2 Inhibit clonogenic cell growth and invasion, induce apoptosis and G1 and G2/M<br />
arrest in cell cycle, sensitize to chemotherapy and radiation, and potentially inhibit<br />
pancreatic <strong>cancer</strong> stem cells<br />
miR-107 Suppress CDK6 Induce in vitro cell growth downregulation<br />
miR-155 Oncogenic TP53INP1 Inhibit apoptosis<br />
miR-194, miR-200b,<br />
miR-200c, miR-429<br />
Oncogenic EP300 Potentially promote metastatic behavior<br />
miR-224, miR-486 Oncogenic CD40 Potentially associated with invasion and metastasis<br />
BCL2: B-cell CLL/lymphoma 2; CD40: CD40 molecule; CDK6: Cyclin-dependent kinase 6; CDKN1B: Cyclin-dependent kinase inhibitor 1B; EP300: E1A<br />
binding protein p300; ESR1: Estrogen receptor 1; HOXB1, 3: Homeobox B1, 3; KRAS: v-Ki-ras2 Kirsten rat sarcoma viral oncogene homolog; NOTCH1/2:<br />
Notch 1/2; PTEN: Phosphatase and tensin homolog; RECK: Reversion-inducing-cysteine-rich protein with kazal motifs; SP1: Sp1 transcription factor;<br />
TP53INP1: Tumor protein p53 inducible nuclear protein 1; EMT: Epithelial-to-mesenchymal transition.<br />
creatic <strong>cancer</strong>. In addition, the results <strong>of</strong> this study suggest<br />
let-7 miRNA as a replacement therapy for pancreatic<br />
<strong>cancer</strong>.<br />
miRNAS AS THERAPEUTIC TARGETS IN<br />
PANCREATIC CANCER<br />
Most epithelial tumors, including pancreatic <strong>cancer</strong>, are<br />
believed to progress toward loss <strong>of</strong> epithelial differentiation<br />
and acquisition <strong>of</strong> a mesenchymal phenotype that<br />
leads to enhanced <strong>cancer</strong> cell invasion and migration [82,83] .<br />
The aggressiveness <strong>of</strong> pancreatic <strong>cancer</strong> is, in part, due to<br />
its drug resistance characteristics, which are also associated<br />
with the epithelial-to-mesenchymal transition (EMT). Several<br />
studies have shown that the events leading to EMT<br />
are regulated by miRNAs [84-89] . Li et al [72] have investigated<br />
the effects <strong>of</strong> let-7 and miR-200 on the morphological<br />
changes <strong>of</strong> EMT in gemcitabine-resistant pancreatic <strong>cancer</strong><br />
cells (GRPCCs). They have found that: (1) the expression<br />
<strong>of</strong> miR-200 and let-7 is significantly downregulated<br />
in GRPCCs, which have EMT characteristics; and (2)<br />
transfection <strong>of</strong> GRPCCs with miR-200 rescues the epithelial<br />
phenotype by upregulating the epithelial marker<br />
E-cadherin and downregulating the mesenchymal markers<br />
ZEB1 and vimentin. These authors also have demonstrated<br />
that tumor cell sensitivity to gemcitabine is increased<br />
after re-expression <strong>of</strong> miR-200b. These results suggest<br />
that EMT could be regulated by miRNAs, and provide a<br />
potential strategy for treatment.<br />
RAS mutations are frequent in human tumors and are<br />
known to be one <strong>of</strong> the responsible factors for radiationinduced<br />
cell death [90,91] . Using transfection <strong>of</strong> Lin28 siR-<br />
NA into pancreatic <strong>cancer</strong> cells harboring Kras mutation,<br />
822 February 21, 2011|Volume 17|Issue 7|<br />
[53]<br />
[72]<br />
[73]<br />
[54]<br />
[56]<br />
[74]<br />
[75]<br />
[76]<br />
[77]<br />
[78]<br />
[79]<br />
[80]<br />
[81]
Oh et al [73] have shown that upregulation with let-7a results<br />
in attenuated expression <strong>of</strong> Kras and increased radiosensitization<br />
<strong>of</strong> pancreatic <strong>cancer</strong> cells. This suggests that<br />
miRNA could be used as a valuable therapeutic option in<br />
radioresistant tumors that have Kras mutations.<br />
The main reason for poor survival in pancreatic <strong>cancer</strong><br />
is the presence <strong>of</strong> metastasis at the time <strong>of</strong> diagnosis.<br />
Weiss et al [54] have shown that miR-10a expression promoted<br />
metastasis, and repression <strong>of</strong> miR-10a inhibited<br />
invasion and metastasis in xenotransplantation experiments<br />
using zebrafish embryos. They have further identified<br />
tumor suppressors HOXB1 and HOXB3 as targets<br />
<strong>of</strong> miR-10a, and have reported that retinoic acid receptor<br />
antagonists inhibit miR-10a expression and suppress metastasis.<br />
These data suggest new therapeutic applications<br />
for miRNA in patients with metastatic pancreatic <strong>cancer</strong>.<br />
Several studies have reported significant overexpression<br />
<strong>of</strong> miR-21 in pancreatic tumors [49,51] , suggesting the potential<br />
role <strong>of</strong> miR-21 in pancreatic <strong>cancer</strong>. Moriyama et al [56]<br />
have confirmed that miR-21 is overexpressed in pancreatic<br />
<strong>cancer</strong> cells. They also have observed that miR-21 contributes<br />
to cell proliferation, invasion, and chemoresistance.<br />
They also have found that mRNA expression <strong>of</strong> invasionrelated<br />
genes, matrix metalloproteinase (MMP)-2 and<br />
MMP-9, and vascular endothelial growth factor is positively<br />
correlated with miR-21 expression. The above studies<br />
show that miR-21 functions as an oncogene, and that it is<br />
involved in pancreatic <strong>cancer</strong> chemoresistance. Therefore,<br />
miR-21 could be a target for a therapeutic strategy for patients<br />
with chemoresistant pancreatic <strong>cancer</strong>.<br />
Zhang et al [74] have found that pancreatic <strong>cancer</strong> cells<br />
treated with trichostatin A (TSA), one <strong>of</strong> the common<br />
histone deacetylase inhibitors [92,93] , are arrested in G0/G1<br />
phase, and exhibit an increased in apoptotic rate. The<br />
treatment also induces downregulation <strong>of</strong> miR-21 and<br />
upregulation <strong>of</strong> miR-200c. The data support the oncogenic<br />
function <strong>of</strong> miR-21, and the tumor suppressor<br />
function <strong>of</strong> miR-200, suggesting that epigenetic regulation<br />
<strong>of</strong> miRNAs with histone deacetylase inhibitor could<br />
be used as a therapeutic option in pancreatic <strong>cancer</strong>.<br />
It has been shown that antisense oligonucleotides<br />
(ASOs) can inhibit upregulated miRNAs in tumors [94] .<br />
Park et al [75] have investigated miR-21 and miR-221 biological<br />
function using ASOs in pancreatic <strong>cancer</strong>. ASOs for<br />
miR-21 and miR-221 both reduce proliferation <strong>of</strong> pancreatic<br />
<strong>cancer</strong> cell lines, increase apoptosis by 3-6-fold, and<br />
induced G1 arrest. ASOs also increase the levels <strong>of</strong> the<br />
miR-21 targets PTEN and RECK, and the miR-221 target,<br />
CDKN1B, at the protein level. The authors have found<br />
that ASO targeting <strong>of</strong> miR-21 and miR-221 sensitizes<br />
tumor cells to the effects <strong>of</strong> gemcitabine, and that ASOgemcitabine<br />
combination treatments generate synergistic<br />
antiproliferative effects in pancreatic <strong>cancer</strong> cells. These<br />
results imply that targeting miRNAs with ASOs could be a<br />
potential new therapeutic strategy for pancreatic <strong>cancer</strong>.<br />
In vitro and in vivo studies have reported the anti<strong>cancer</strong><br />
activity, with low toxicity, <strong>of</strong> curcumin (diferuloylmethane)<br />
[95,96] , a naturally occurring flavonoid from the rhizome<br />
<strong>of</strong> Curcuma longa [97,98] . Sun et al [76] have investigated whether<br />
WJG|www.wjgnet.com<br />
Park JY et al . MicroRNAs in pancreatic <strong>cancer</strong><br />
curcumin affects the expression pr<strong>of</strong>iles <strong>of</strong> miRNAs in<br />
pancreatic <strong>cancer</strong>, and have reported overexpression <strong>of</strong><br />
miR-22 and downregulation <strong>of</strong> miR-199a* in pancreatic<br />
<strong>cancer</strong> cells treated with curcumin. The predicted target<br />
genes <strong>of</strong> miRNA-22 are Sp1 transcription factor (SP1)<br />
and estrogen receptor 1 (ESR1). The expression <strong>of</strong> these<br />
genes (SP1 and ESR1), which are involved in cell growth,<br />
metastasis and apoptosis, is suppressed by upregulation<br />
<strong>of</strong> miR-22. Thus, Sun et al have suggested that one <strong>of</strong> the<br />
important anti<strong>cancer</strong> mechanisms <strong>of</strong> curcumin is modulation<br />
<strong>of</strong> miRNA expression, such as miR-22.<br />
Some <strong>cancer</strong> stem cells are involved in tumor initiation,<br />
self-renewal and survival [99] , and miRNAs have been<br />
shown to have critical roles in <strong>cancer</strong> stem cell differentiation.<br />
Ji et al [77] , using cell sorting <strong>of</strong> CD44 + /CD133 + , have<br />
examined the roles <strong>of</strong> miR-34 in p53-mutant human pancreatic<br />
<strong>cancer</strong> cell lines, to find a potential link between<br />
stem cells and pancreatic <strong>cancer</strong>. These authors have observed<br />
that miR-34 upregulation results in significant inhibition<br />
<strong>of</strong> clonogenic growth and cell invasion, induction<br />
<strong>of</strong> apoptosis, G1 and G2/M cell cycle arrest, and sensitization<br />
<strong>of</strong> the cells to chemotherapy and radiation. They<br />
also have detected an 87% reduction in tumor initiating<br />
cells (or <strong>cancer</strong> stem cells), which was mediated by downregulation<br />
<strong>of</strong> its downstream targets BCL2 and NOTCH.<br />
This study has shown that restoration <strong>of</strong> miR-34 could<br />
have significant promise as a novel molecular therapy for<br />
human pancreatic <strong>cancer</strong> via inhibiting pancreatic <strong>cancer</strong><br />
stem cell differentiation.<br />
Aberrations in epigenetic regulation are common<br />
in human <strong>cancer</strong>s, and tumor suppressor genes are frequently<br />
silenced by this mechanism in nearly all malignancies<br />
[100,101] . Recent studies have shown that subsets <strong>of</strong><br />
miRNAs are also silenced by the same mechanism [102,103] .<br />
For example, Lee et al [78] have shown that miR-107 is<br />
silenced by promoter DNA methylation in pancreatic tumors.<br />
These authors treated human pancreatic <strong>cancer</strong> cell<br />
lines with the demethylating agent, 5-aza-2’-deoxycytidine<br />
or the histone deacetylase inhibitor, TSA, or with a combination<br />
<strong>of</strong> the two, and identified the upregulation <strong>of</strong><br />
14 miRNAs, including miR-107. Retroviral expression <strong>of</strong><br />
miR-107 in pancreatic <strong>cancer</strong> cells downregulates in vitro<br />
cell growth by repressing cyclin-dependent kinase 6, a<br />
putative miR-107 target. This study shows that epigenetic<br />
mechanisms <strong>of</strong> miRNA may be involved in pancreatic<br />
carcinogenesis.<br />
Tumor protein p53 inducible nuclear protein 1 (TP53-<br />
INP1) is a pro-apoptotic stress-induced gene. TP53 is able<br />
to activate TP53INP1 transcription as a target [104,105] . However,<br />
overexpression <strong>of</strong> TP53INP1 induces cell cycle arrest<br />
and apoptosis in vitro, independently from TP53. Gironella<br />
et al [79] have reported that TP53INP1 is expressed<br />
in normal tissues but is markedly downregulated or lost in<br />
early <strong>stage</strong>s <strong>of</strong> pancreatic <strong>cancer</strong> development. TP53INP1<br />
repression by transfection <strong>of</strong> miR-155 causes loss or significant<br />
decrease in expression <strong>of</strong> TP53INP1. These data<br />
suggest that TP53INP1 is an additional potential target <strong>of</strong><br />
miR-155.<br />
Several studies have suggested that EP300 may func-<br />
823 February 21, 2011|Volume 17|Issue 7|
Park JY et al . MicroRNAs in pancreatic <strong>cancer</strong><br />
tion as a tumor suppressor. This gene is located on chromosome<br />
22q; a region known for its frequent loss <strong>of</strong><br />
heterozygosity in different <strong>cancer</strong>s, including pancreatic<br />
<strong>cancer</strong> [106-109] . Mees et al [80] have classified 16 human PDAC<br />
cell lines into three hierarchical groups according to their<br />
metastatic potential, and have pr<strong>of</strong>iled their mRNA and<br />
miRNA expression. The highly metastatic PDAC cell<br />
lines, when compared to the non-metastatic cell lines,<br />
have shown decreased mRNA and protein expression<br />
<strong>of</strong> EP300, which is related to significant upregulation <strong>of</strong><br />
EP300-targeting miRNAs (miR-194, miR-200b, miR-200c<br />
and miR-429). Using the same 16 human PDAC cell lines,<br />
these authors have found markedly reduced expression<br />
<strong>of</strong> CD40 protein, which is involved in the host antitumor<br />
immune response [110,111] . CD40-targeting miR-224<br />
and miR-486 are upregulated in the highly invasive and<br />
metastatic PDAC [81] . These results show that miRNAs are<br />
involved in regulating the metastatic behavior <strong>of</strong> PDAC,<br />
and in modulating metastasis-specific tumor suppressor<br />
genes. Targeting <strong>of</strong> these miRNAs may have potential<br />
therapeutic value in PDAC.<br />
miRNAS AS CLINICAL ASPECTS IN<br />
PANCREATIC CANCER<br />
Most tumors show deregulation <strong>of</strong> miRNAs for the initiation<br />
and progression <strong>of</strong> human <strong>cancer</strong>, therefore, many<br />
researchers have been trying to exploit these miRNAs for<br />
therapeutic applications, and to develop novel therapies<br />
for human <strong>cancer</strong> [112-115] . Thus, oncogenic miRNAs can<br />
be suppressed with ASOs to their precursor or mature<br />
forms [94,116] , and tumor suppressor miRNAs can be upregulated<br />
[53,72] .<br />
Numerous miRNA studies have demonstrated that<br />
miRNA-directed targeting therapy has therapeutic potential<br />
in human <strong>cancer</strong>. Recent studies have further<br />
demonstrated synergistic effects when miRNA-directed<br />
therapy is used in combination with conventional chemotherapy<br />
or radiotherapy for pancreatic <strong>cancer</strong> [73,75] .<br />
However, currently, there is no miRNA that is used in<br />
the clinical setting for treatment <strong>of</strong> <strong>cancer</strong> patients. Significant<br />
work needs to be done before miRNA-directed<br />
therapeutic strategies can be applied. However, current<br />
data have shown encouraging preliminary results to support<br />
their clinical applications in human <strong>cancer</strong>.<br />
Several investigators have attempted to utilize miR-<br />
NA expression pr<strong>of</strong>iles as a diagnostic tool to differentiate<br />
tumors from normal tissues [43,117,118] , and as predictors<br />
<strong>of</strong> clinical outcome. However, there have not been<br />
sufficient studies that have investigated the correlation<br />
between alterations in miRNA expression and patient<br />
outcome in PDAC.<br />
A few miRNA expression patterns have been investigated<br />
to predict prognostic outcome from specimens <strong>of</strong><br />
patients with pancreatic <strong>cancer</strong> [51,55,57] . Bloomston et al [51]<br />
have analyzed the association between survival <strong>of</strong> patients<br />
and miRNA expression patterns. In the subgroup<br />
analysis <strong>of</strong> patients with lymph-node positive disease, a<br />
WJG|www.wjgnet.com<br />
panel <strong>of</strong> six miRNAs (miR-452, miR-105, miR-127, miR-<br />
518a-2, miR-187 and miR-30a-3p) was able to differentiate<br />
between long-term survivors and short-term survivors<br />
who died within 2 years. Furthermore, high expression<br />
<strong>of</strong> miR-196a-2 is associated with poor outcome; patients<br />
with high miR-196a-2 expression have a shorter median<br />
survival <strong>of</strong> 14.3 mo when compared with patients with<br />
low miR-196a-2 expression, who have a median survival<br />
<strong>of</strong> 26.5 mo.<br />
Dillh<strong>of</strong>f et al [55] have performed in situ hybridization<br />
after microdissection and tissue microarray analysis <strong>of</strong> 80<br />
resected pancreatic <strong>cancer</strong> specimens, and found 79% <strong>of</strong><br />
the pancreatic <strong>cancer</strong> samples, 27% <strong>of</strong> the chronic pancreatitis<br />
samples, and 8% <strong>of</strong> the normal pancreatic samples<br />
had positive miR-21 expression. Among the subset <strong>of</strong><br />
patients with node-negative disease, high miR-21 expression<br />
resulted in poorer survival than in patients with low<br />
miR-21 expression (median: 27.7 mo vs 15.2 mo, P = 0.037),<br />
although miR-21 expression did not correlate with tumor<br />
size, differentiation, nodal status, or T <strong>stage</strong>.<br />
Greither et al [57] have measured the levels <strong>of</strong> miR-155,<br />
miR-203, miR-210, miR-216, miR-217 and miR-222,<br />
which are known to be differentially expressed in pancreatic<br />
tumors. From 56 microdissected PDACs, they found<br />
that elevated levels <strong>of</strong> miR-155, miR-203, miR-210 and<br />
miR-222 were associated with poorer overall survival<br />
rates. They further noted that higher expression <strong>of</strong> all<br />
four miRNAs had a 6.2-fold increased risk <strong>of</strong> tumorrelated<br />
death as compared to cases in which the expression<br />
<strong>of</strong> these miRNAs was low.<br />
CONCLUSION<br />
Since the discovery <strong>of</strong> miRNAs, growing evidence has<br />
confirmed a link between miRNAs and malignant diseases,<br />
and has identified their functions and targets that<br />
affect the complex process <strong>of</strong> carcinogenesis. Like other<br />
malignant tumors, PDAC has its unique miRNA expression<br />
patterns, which are different from those <strong>of</strong> other human<br />
tumors, and are able to differentiate normal pancreas<br />
from benign inflammatory pancreatic tissues and pancreatic<br />
<strong>cancer</strong>. At present, several important oncogenic and<br />
tumor suppressor miRNAs, and their molecular targets,<br />
have been identified in PDAC. More importantly, this<br />
information will lead to new development <strong>of</strong> prognostic,<br />
diagnostic, and treatment strategies. However, additional<br />
studies are required to find ways to utilize miRNAs as a<br />
therapeutic target in the clinical setting.<br />
REFERENCES<br />
1 Jemal A, Siegel R, Xu J, Ward E. Cancer statistics, 2010. CA<br />
Cancer J Clin 2010; 60: 277-300<br />
2 Li D, Xie K, Wolff R, Abbruzzese JL. Pancreatic <strong>cancer</strong>. Lancet<br />
2004; 363: 1049-1057<br />
3 Garcea G, Neal CP, Pattenden CJ, Steward WP, Berry DP.<br />
Molecular prognostic markers in pancreatic <strong>cancer</strong>: a systematic<br />
review. Eur J Cancer 2005; 41: 2213-2236<br />
4 Takaori K. Current understanding <strong>of</strong> precursors to pancreatic<br />
<strong>cancer</strong>. J Hepatobiliary Pancreat Surg 2007; 14: 217-223<br />
824 February 21, 2011|Volume 17|Issue 7|
5 Bardeesy N, DePinho RA. Pancreatic <strong>cancer</strong> biology and<br />
genetics. Nat Rev Cancer 2002; 2: 897-909<br />
6 Goggins M. Molecular markers <strong>of</strong> early pancreatic <strong>cancer</strong>. J<br />
Clin Oncol 2005; 23: 4524-4531<br />
7 Goggins M, Kern SE, Offerhaus JA, Hruban RH. Progress in<br />
<strong>cancer</strong> genetics: lessons from pancreatic <strong>cancer</strong>. Ann Oncol<br />
1999; 10 Suppl 4: 4-8<br />
8 Sakorafas GH, Tsiotou AG. Multi-step pancreatic carcinogenesis<br />
and its clinical implications. Eur J Surg Oncol 1999;<br />
25: 562-565<br />
9 Farh KK, Grimson A, Jan C, Lewis BP, Johnston WK, Lim<br />
LP, Burge CB, Bartel DP. The widespread impact <strong>of</strong> mammalian<br />
MicroRNAs on mRNA repression and evolution.<br />
Science 2005; 310: 1817-1821<br />
10 Ambros V. The functions <strong>of</strong> animal microRNAs. Nature<br />
2004; 431: 350-355<br />
11 Lee RC, Feinbaum RL, Ambros V. The C. elegans heterochronic<br />
gene lin-4 encodes small RNAs with antisense complementarity<br />
to lin-14. Cell 1993; 75: 843-854<br />
12 Pasquinelli AE, Reinhart BJ, Slack F, Martindale MQ, Kuroda<br />
MI, Maller B, Hayward DC, Ball EE, Degnan B, Muller<br />
P, Spring J, Srinivasan A, Fishman M, Finnerty J, Corbo J,<br />
Levine M, Leahy P, Davidson E, Ruvkun G. Conservation <strong>of</strong><br />
the sequence and temporal expression <strong>of</strong> let-7 heterochronic<br />
regulatory RNA. Nature 2000; 408: 86-89<br />
13 Bentwich I, Avniel A, Karov Y, Aharonov R, Gilad S, Barad<br />
O, Barzilai A, Einat P, Einav U, Meiri E, Sharon E, Spector Y,<br />
Bentwich Z. Identification <strong>of</strong> hundreds <strong>of</strong> conserved and nonconserved<br />
human microRNAs. Nat Genet 2005; 37: 766-770<br />
14 Sanger. Sanger miRBase. 2010 [cited April 2010]. Available<br />
from: URL: http://www.mirbase.org/index.shtml<br />
15 Cai X, Hagedorn CH, Cullen BR. Human microRNAs are<br />
processed from capped, polyadenylated transcripts that can<br />
also function as mRNAs. RNA 2004; 10: 1957-1966<br />
16 Lee Y, Ahn C, Han J, Choi H, Kim J, Yim J, Lee J, Provost P,<br />
Radmark O, Kim S, Kim VN. The nuclear RNase III Drosha<br />
initiates microRNA processing. Nature 2003; 425: 415-419<br />
17 Han J, Lee Y, Yeom KH, Kim YK, Jin H, Kim VN. The<br />
Drosha-DGCR8 complex in primary microRNA processing.<br />
Genes Dev 2004; 18: 3016-3027<br />
18 Tang G. siRNA and miRNA: an insight into RISCs. Trends<br />
Biochem Sci 2005; 30: 106-114<br />
19 Lewis BP, Burge CB, Bartel DP. Conserved seed pairing,<br />
<strong>of</strong>ten flanked by adenosines, indicates that thousands <strong>of</strong> human<br />
genes are microRNA targets. Cell 2005; 120: 15-20<br />
20 Muckstein U, Tafer H, Hackermuller J, Bernhart SH, Stadler<br />
PF, H<strong>of</strong>acker IL. Thermodynamics <strong>of</strong> RNA-RNA binding.<br />
Bioinformatics 2006; 22: 1177-1182<br />
21 Negrini M, Ferracin M, Sabbioni S, Croce CM. MicroRNAs<br />
in human <strong>cancer</strong>: from research to therapy. J Cell Sci 2007;<br />
120: 1833-1840<br />
22 Shomron N. MicroRNAs and their antagonists as novel<br />
therapeutics. Eur J Cancer 2009; 45 Suppl 1: 388-390<br />
23 Didiano D, Hobert O. Perfect seed pairing is not a generally<br />
reliable predictor for miRNA-target interactions. Nat Struct<br />
Mol Biol 2006; 13: 849-851<br />
24 Grimson A, Farh KK, Johnston WK, Garrett-Engele P, Lim<br />
LP, Bartel DP. MicroRNA targeting specificity in mammals:<br />
determinants beyond seed pairing. Mol Cell 2007; 27: 91-105<br />
25 Long D, Lee R, Williams P, Chan CY, Ambros V, Ding Y.<br />
Potent effect <strong>of</strong> target structure on microRNA function. Nat<br />
Struct Mol Biol 2007; 14: 287-294<br />
26 Kertesz M, Iovino N, Unnerstall U, Gaul U, Segal E. The<br />
role <strong>of</strong> site accessibility in microRNA target recognition. Nat<br />
Genet 2007; 39: 1278-1284<br />
27 Huang JC, Babak T, Corson TW, Chua G, Khan S, Gallie BL,<br />
Hughes TR, Blencowe BJ, Frey BJ, Morris QD. Using expression<br />
pr<strong>of</strong>iling data to identify human microRNA targets.<br />
Nat Methods 2007; 4: 1045-1049<br />
28 Gottwein E, Mukherjee N, Sachse C, Frenzel C, Majoros<br />
WJG|www.wjgnet.com<br />
Park JY et al . MicroRNAs in pancreatic <strong>cancer</strong><br />
WH, Chi JT, Braich R, Manoharan M, Soutschek J, Ohler U,<br />
Cullen BR. A viral microRNA functions as an orthologue <strong>of</strong><br />
cellular miR-155. Nature 2007; 450: 1096-1099<br />
29 Skalsky RL, Samols MA, Plaisance KB, Boss IW, Riva A,<br />
Lopez MC, Baker HV, Renne R. Kaposi's sarcoma-associated<br />
herpesvirus encodes an ortholog <strong>of</strong> miR-155. J Virol 2007; 81:<br />
12836-12845<br />
30 Tavazoie SF, Alarcón C, Oskarsson T, Padua D, Wang Q, Bos<br />
PD, Gerald WL, Massagué J. Endogenous human microR-<br />
NAs that suppress breast <strong>cancer</strong> metastasis. Nature 2008; 451:<br />
147-152<br />
31 Lu J, Getz G, Miska EA, Alvarez-Saavedra E, Lamb J, Peck D,<br />
Sweet-Cordero A, Ebert BL, Mak RH, Ferrando AA, Downing<br />
JR, Jacks T, Horvitz HR, Golub TR. MicroRNA expression<br />
pr<strong>of</strong>iles classify human <strong>cancer</strong>s. Nature 2005; 435: 834-838<br />
32 Calin GA, Dumitru CD, Shimizu M, Bichi R, Zupo S, Noch<br />
E, Aldler H, Rattan S, Keating M, Rai K, Rassenti L, Kipps<br />
T, Negrini M, Bullrich F, Croce CM. Frequent deletions and<br />
down-regulation <strong>of</strong> micro- RNA genes miR15 and miR16 at<br />
13q14 in chronic lymphocytic leukemia. Proc Natl Acad Sci<br />
USA 2002; 99: 15524-15529<br />
33 Cimmino A, Calin GA, Fabbri M, Iorio MV, Ferracin M, Shimizu<br />
M, Wojcik SE, Aqeilan RI, Zupo S, Dono M, Rassenti L,<br />
Alder H, Volinia S, Liu CG, Kipps TJ, Negrini M, Croce CM.<br />
miR-15 and miR-16 induce apoptosis by targeting BCL2.<br />
Proc Natl Acad Sci USA 2005; 102: 13944-13949<br />
34 Metzler M, Wilda M, Busch K, Viehmann S, Borkhardt A.<br />
High expression <strong>of</strong> precursor microRNA-155/BIC RNA in<br />
children with Burkitt lymphoma. Genes Chromosomes Cancer<br />
2004; 39: 167-169<br />
35 Takamizawa J, Konishi H, Yanagisawa K, Tomida S, Osada H,<br />
Endoh H, Harano T, Yatabe Y, Nagino M, Nimura Y, Mitsudomi<br />
T, Takahashi T. Reduced expression <strong>of</strong> the let-7 microR-<br />
NAs in human lung <strong>cancer</strong>s in association with shortened<br />
postoperative survival. Cancer Res 2004; 64: 3753-3756<br />
36 Eis PS, Tam W, Sun L, Chadburn A, Li Z, Gomez MF, Lund<br />
E, Dahlberg JE. Accumulation <strong>of</strong> miR-155 and BIC RNA in<br />
human B cell lymphomas. Proc Natl Acad Sci USA 2005; 102:<br />
3627-3632<br />
37 He L, Thomson JM, Hemann MT, Hernando-Monge E, Mu D,<br />
Goodson S, Powers S, Cordon-Cardo C, Lowe SW, Hannon<br />
GJ, Hammond SM. A microRNA polycistron as a potential<br />
human oncogene. Nature 2005; 435: 828-833<br />
38 Iorio MV, Ferracin M, Liu CG, Veronese A, Spizzo R, Sabbioni<br />
S, Magri E, Pedriali M, Fabbri M, Campiglio M, Ménard<br />
S, Palazzo JP, Rosenberg A, Musiani P, Volinia S, Nenci I,<br />
Calin GA, Querzoli P, Negrini M, Croce CM. MicroRNA<br />
gene expression deregulation in human breast <strong>cancer</strong>. Cancer<br />
Res 2005; 65: 7065-7070<br />
39 Yanaihara N, Caplen N, Bowman E, Seike M, Kumamoto K,<br />
Yi M, Stephens RM, Okamoto A, Yokota J, Tanaka T, Calin<br />
GA, Liu CG, Croce CM, Harris CC. Unique microRNA molecular<br />
pr<strong>of</strong>iles in lung <strong>cancer</strong> diagnosis and prognosis. Cancer<br />
Cell 2006; 9: 189-198<br />
40 Calin GA, Croce CM. MicroRNA signatures in human <strong>cancer</strong>s.<br />
Nat Rev Cancer 2006; 6: 857-866<br />
41 Cummins JM, Velculescu VE. Implications <strong>of</strong> micro-RNA<br />
pr<strong>of</strong>iling for <strong>cancer</strong> diagnosis. Oncogene 2006; 25: 6220-6227<br />
42 Dalmay T, Edwards DR. MicroRNAs and the hallmarks <strong>of</strong><br />
<strong>cancer</strong>. Oncogene 2006; 25: 6170-6175<br />
43 Tricoli JV, Jacobson JW. MicroRNA: Potential for Cancer<br />
Detection, Diagnosis, and Prognosis. Cancer Res 2007; 67:<br />
4553-4555<br />
44 Deng S, Calin GA, Croce CM, Coukos G, Zhang L. Mechanisms<br />
<strong>of</strong> microRNA deregulation in human <strong>cancer</strong>. Cell Cycle<br />
2008; 7: 2643-2646<br />
45 Kluiver J, van den Berg A, de Jong D, Blokzijl T, Harms<br />
G, Bouwman E, Jacobs S, Poppema S, Kroesen BJ. Regulation<br />
<strong>of</strong> pri-microRNA BIC transcription and processing in<br />
Burkitt lymphoma. Oncogene 2007; 26: 3769-3776<br />
825 February 21, 2011|Volume 17|Issue 7|
Park JY et al . MicroRNAs in pancreatic <strong>cancer</strong><br />
46 O'Connell RM, Taganov KD, Boldin MP, Cheng G, Baltimore<br />
D. MicroRNA-155 is induced during the macrophage<br />
inflammatory response. Proc Natl Acad Sci USA 2007; 104:<br />
1604-1609<br />
47 Kong W, Yang H, He L, Zhao JJ, Coppola D, Dalton WS,<br />
Cheng JQ. MicroRNA-155 is regulated by the transforming<br />
growth factor beta/Smad pathway and contributes to epithelial<br />
cell plasticity by targeting RhoA. Mol Cell Biol 2008;<br />
28: 6773-6784<br />
48 Yin Q, Wang X, McBride J, Fewell C, Flemington E. B-cell<br />
receptor activation induces BIC/miR-155 expression through<br />
a conserved AP-1 element. J Biol Chem 2008; 283: 2654-2662<br />
49 Lee EJ, Gusev Y, Jiang J, Nuovo GJ, Lerner MR, Frankel<br />
WL, Morgan DL, Postier RG, Brackett DJ, Schmittgen TD.<br />
Expression pr<strong>of</strong>iling identifies microRNA signature in pancreatic<br />
<strong>cancer</strong>. Int J Cancer 2007; 120: 1046-1054<br />
50 Szafranska AE, Davison TS, John J, Cannon T, Sipos B,<br />
Maghnouj A, Labourier E, Hahn SA. MicroRNA expression<br />
alterations are linked to tumorigenesis and non-neoplastic<br />
processes in pancreatic ductal adenocarcinoma. Oncogene<br />
2007; 26: 4442-4452<br />
51 Bloomston M, Frankel WL, Petrocca F, Volinia S, Alder H,<br />
Hagan JP, Liu CG, Bhatt D, Taccioli C, Croce CM. MicroR-<br />
NA expression patterns to differentiate pancreatic adenocarcinoma<br />
from normal pancreas and chronic pancreatitis.<br />
JAMA 2007; 297: 1901-1908<br />
52 Zhang Y, Li M, Wang H, Fisher WE, Lin PH, Yao Q, Chen<br />
C. Pr<strong>of</strong>iling <strong>of</strong> 95 microRNAs in pancreatic <strong>cancer</strong> cell lines<br />
and surgical specimens by real-time PCR analysis. <strong>World</strong> J<br />
Surg 2009; 33: 698-709<br />
53 Torrisani J, Bournet B, du Rieu MC, Bouisson M, Souque A,<br />
Escourrou J, Buscail L, Cordelier P. let-7 MicroRNA transfer<br />
in pancreatic <strong>cancer</strong>-derived cells inhibits in vitro cell proliferation<br />
but fails to alter tumor progression. Hum Gene Ther<br />
2009; 20: 831-844<br />
54 Weiss FU, Marques IJ, Woltering JM, Vlecken DH, Aghdassi<br />
A, Partecke LI, Heidecke CD, Lerch MM, Bagowski<br />
CP. Retinoic acid receptor antagonists inhibit miR-10a expression<br />
and block metastatic behavior <strong>of</strong> pancreatic <strong>cancer</strong>.<br />
Gastroenterology 2009; 137: 2136-2145.e1-7<br />
55 Dillh<strong>of</strong>f M, Liu J, Frankel W, Croce C, Bloomston M. MicroR-<br />
NA-21 is overexpressed in pancreatic <strong>cancer</strong> and a potential<br />
predictor <strong>of</strong> survival. J Gastrointest Surg 2008; 12: 2171-2176<br />
56 Moriyama T, Ohuchida K, Mizumoto K, Yu J, Sato N, Nabae<br />
T, Takahata S, Toma H, Nagai E, Tanaka M. MicroR-<br />
NA-21 modulates biological functions <strong>of</strong> pancreatic <strong>cancer</strong><br />
cells including their proliferation, invasion, and chemoresistance.<br />
Mol Cancer Ther 2009; 8: 1067-1074<br />
57 Greither T, Grochola LF, Udelnow A, Lautenschläger C,<br />
Würl P, Taubert H. Elevated expression <strong>of</strong> microRNAs 155,<br />
203, 210 and 222 in pancreatic tumors is associated with<br />
poorer survival. Int J Cancer 2010; 126: 73-80<br />
58 Sood P, Krek A, Zavolan M, Macino G, Rajewsky N. Celltype-specific<br />
signatures <strong>of</strong> microRNAs on target mRNA<br />
expression. Proc Natl Acad Sci USA 2006; 103: 2746-2751<br />
59 Baskerville S, Bartel DP. Microarray pr<strong>of</strong>iling <strong>of</strong> microR-<br />
NAs reveals frequent coexpression with neighboring miR-<br />
NAs and host genes. RNA 2005; 11: 241-247<br />
60 Eloubeidi MA, Jhala D, Chhieng DC, Chen VK, Eltoum I,<br />
Vickers S, Mel Wilcox C, Jhala N. Yield <strong>of</strong> endoscopic ultrasound-guided<br />
fine-needle aspiration biopsy in patients with<br />
suspected pancreatic carcinoma. Cancer 2003; 99: 285-292<br />
61 Jhala NC, Jhala D, Eltoum I, Vickers SM, Wilcox CM,<br />
Chhieng DC, Eloubeidi MA. Endoscopic ultrasound-guided<br />
fine-needle aspiration biopsy: a powerful tool to obtain<br />
samples from small lesions. Cancer 2004; 102: 239-246<br />
62 Chen Y, Zheng B, Robbins DH, Lewin DN, Mikhitarian K,<br />
Graham A, Rumpp L, Glenn T, Gillanders WE, Cole DJ, Lu<br />
X, H<strong>of</strong>fman BJ, Mitas M. Accurate discrimination <strong>of</strong> pancreatic<br />
ductal adenocarcinoma and chronic pancreatitis using<br />
WJG|www.wjgnet.com<br />
multimarker expression data and samples obtained by minimally<br />
invasive fine needle aspiration. Int J Cancer 2007; 120:<br />
1511-1517<br />
63 Szafranska AE, Doleshal M, Edmunds HS, Gordon S, Luttges<br />
J, Munding JB, Barth RJ Jr, Gutmann EJ, Suriawinata AA,<br />
Marc Pipas J, Tannapfel A, Korc M, Hahn SA, Labourier<br />
E, Tsongalis GJ. Analysis <strong>of</strong> microRNAs in pancreatic fineneedle<br />
aspirates can classify benign and malignant tissues.<br />
Clin Chem 2008; 54: 1716-1724<br />
64 Hruban RH, Maitra A, Kern SE, Goggins M. Precursors<br />
to pancreatic <strong>cancer</strong>. Gastroenterol Clin North Am 2007; 36:<br />
831-849, vi<br />
65 Hruban RH, Takaori K, Klimstra DS, Adsay NV, Albores-<br />
Saavedra J, Biankin AV, Biankin SA, Compton C, Fukushima<br />
N, Furukawa T, Goggins M, Kato Y, Klöppel G, Longnecker<br />
DS, Lüttges J, Maitra A, Offerhaus GJ, Shimizu M,<br />
Yonezawa S. An illustrated consensus on the classification<br />
<strong>of</strong> pancreatic intraepithelial neoplasia and intraductal papillary<br />
mucinous neoplasms. Am J Surg Pathol 2004; 28: 977-987<br />
66 Adsay NV. Cystic neoplasia <strong>of</strong> the pancreas: pathology and<br />
biology. J Gastrointest Surg 2008; 12: 401-404<br />
67 Takaori K, Hruban RH, Maitra A, Tanigawa N. Pancreatic<br />
intraepithelial neoplasia. Pancreas 2004; 28: 257-262<br />
68 Habbe N, Koorstra JB, Mendell JT, Offerhaus GJ, Ryu JK,<br />
Feldmann G, Mullendore ME, Goggins MG, Hong SM, Maitra<br />
A. MicroRNA miR-155 is a biomarker <strong>of</strong> early pancreatic<br />
neoplasia. Cancer Biol Ther 2009; 8: 340-346<br />
69 du Rieu MC, Torrisani J, Selves J, Al Saati T, Souque A, Dufresne<br />
M, Tsongalis GJ, Suriawinata AA, Carrère N, Buscail<br />
L, Cordelier P. MicroRNA-21 is induced early in pancreatic<br />
ductal adenocarcinoma precursor lesions. Clin Chem 2010; 56:<br />
603-612<br />
70 Wang J, Chen J, Chang P, LeBlanc A, Li D, Abbruzzesse JL,<br />
Frazier ML, Killary AM, Sen S. MicroRNAs in plasma <strong>of</strong> pancreatic<br />
ductal adenocarcinoma patients as novel blood-based<br />
biomarkers <strong>of</strong> disease. Cancer Prev Res (Phila) 2009; 2: 807-813<br />
71 Johnson SM, Grosshans H, Shingara J, Byrom M, Jarvis R,<br />
Cheng A, Labourier E, Reinert KL, Brown D, Slack FJ. RAS<br />
is regulated by the let-7 microRNA family. Cell 2005; 120:<br />
635-647<br />
72 Li Y, VandenBoom TG 2nd, Kong D, Wang Z, Ali S, Philip<br />
PA, Sarkar FH. Up-regulation <strong>of</strong> miR-200 and let-7 by natural<br />
agents leads to the reversal <strong>of</strong> epithelial-to-mesenchymal<br />
transition in gemcitabine-resistant pancreatic <strong>cancer</strong> cells.<br />
Cancer Res 2009; 69: 6704-6712<br />
73 Oh JS, Kim JJ, Byun JY, Kim IA. Lin28-let7 modulates radiosensitivity<br />
<strong>of</strong> human <strong>cancer</strong> cells with activation <strong>of</strong> K-Ras.<br />
Int J Radiat Oncol Biol Phys 2010; 76: 5-8<br />
74 Zhang S, Cai X, Huang F, Zhong W, Yu Z. Effect <strong>of</strong> trichostatin<br />
a on viability and microRNA expression in human<br />
pancreatic <strong>cancer</strong> cell line BxPC-3. Exp Oncol 2008; 30: 265-268<br />
75 Park JK, Lee EJ, Esau C, Schmittgen TD. Antisense inhibition<br />
<strong>of</strong> microRNA-21 or -221 arrests cell cycle, induces apoptosis,<br />
and sensitizes the effects <strong>of</strong> gemcitabine in pancreatic<br />
adenocarcinoma. Pancreas 2009; 38: e190-e199<br />
76 Sun M, Estrov Z, Ji Y, Coombes KR, Harris DH, Kurzrock R.<br />
Curcumin (diferuloylmethane) alters the expression pr<strong>of</strong>iles<br />
<strong>of</strong> microRNAs in human pancreatic <strong>cancer</strong> cells. Mol Cancer<br />
Ther 2008; 7: 464-473<br />
77 Ji Q, Hao X, Zhang M, Tang W, Yang M, Li L, Xiang D, Desano<br />
JT, Bommer GT, Fan D, Fearon ER, Lawrence TS, Xu L.<br />
MicroRNA miR-34 inhibits human pancreatic <strong>cancer</strong> tumorinitiating<br />
cells. PLoS One 2009; 4: e6816<br />
78 Lee KH, Lotterman C, Karikari C, Omura N, Feldmann G,<br />
Habbe N, Goggins MG, Mendell JT, Maitra A. Epigenetic<br />
silencing <strong>of</strong> MicroRNA miR-107 regulates cyclin-dependent<br />
kinase 6 expression in pancreatic <strong>cancer</strong>. Pancreatology 2009;<br />
9: 293-301<br />
79 Gironella M, Seux M, Xie MJ, Cano C, Tomasini R, Gommeaux<br />
J, Garcia S, Nowak J, Yeung ML, Jeang KT, Chaix A,<br />
826 February 21, 2011|Volume 17|Issue 7|
Fazli L, Motoo Y, Wang Q, Rocchi P, Russo A, Gleave M,<br />
Dagorn JC, Iovanna JL, Carrier A, Pébusque MJ, Dusetti NJ.<br />
Tumor protein 53-induced nuclear protein 1 expression is<br />
repressed by miR-155, and its restoration inhibits pancreatic<br />
tumor development. Proc Natl Acad Sci USA 2007; 104:<br />
16170-16175<br />
80 Mees ST, Mardin WA, Wendel C, Baeumer N, Willscher E,<br />
Senninger N, Schleicher C, Colombo-Benkmann M, Haier J.<br />
EP300--a miRNA-regulated metastasis suppressor gene in<br />
ductal adenocarcinomas <strong>of</strong> the pancreas. Int J Cancer 2010;<br />
126: 114-124<br />
81 Mees ST, Mardin WA, Sielker S, Willscher E, Senninger N,<br />
Schleicher C, Colombo-Benkmann M, Haier J. Involvement<br />
<strong>of</strong> CD40 targeting miR-224 and miR-486 on the progression<br />
<strong>of</strong> pancreatic ductal adenocarcinomas. Ann Surg Oncol 2009;<br />
16: 2339-2350<br />
82 Thiery JP. Epithelial-mesenchymal transitions in tumour<br />
progression. Nat Rev Cancer 2002; 2: 442-454<br />
83 Sabbah M, Emami S, Redeuilh G, Julien S, Prévost G, Zimber<br />
A, Ouelaa R, Bracke M, De Wever O, Gespach C. Molecular<br />
signature and therapeutic perspective <strong>of</strong> the epithelialto-mesenchymal<br />
transitions in epithelial <strong>cancer</strong>s. Drug Resist<br />
Updat 2008; 11: 123-151<br />
84 Korpal M, Kang Y. The emerging role <strong>of</strong> miR-200 family <strong>of</strong><br />
microRNAs in epithelial-mesenchymal transition and <strong>cancer</strong><br />
metastasis. RNA Biol 2008; 5: 115-119<br />
85 Gregory PA, Bracken CP, Bert AG, Goodall GJ. MicroRNAs<br />
as regulators <strong>of</strong> epithelial-mesenchymal transition. Cell<br />
Cycle 2008; 7: 3112-3118<br />
86 Wellner U, Schubert J, Burk UC, Schmalh<strong>of</strong>er O, Zhu F,<br />
Sonntag A, Waldvogel B, Vannier C, Darling D, zur Hausen A,<br />
Brunton VG, Morton J, Sansom O, Schüler J, Stemmler MP,<br />
Herzberger C, Hopt U, Keck T, Brabletz S, Brabletz T. The<br />
EMT-activator ZEB1 promotes tumorigenicity by repressing<br />
stemness-inhibiting microRNAs. Nat Cell Biol 2009; 11:<br />
1487-1495<br />
87 Iliopoulos D, Polytarchou C, Hatziapostolou M, Kottakis F,<br />
Maroulakou IG, Struhl K, Tsichlis PN. MicroRNAs differentially<br />
regulated by Akt is<strong>of</strong>orms control EMT and stem cell<br />
renewal in <strong>cancer</strong> cells. Sci Signal 2009; 2: ra62<br />
88 Wright JA, Richer JK, Goodall GJ. microRNAs and EMT in<br />
mammary cells and breast <strong>cancer</strong>. J Mammary Gland Biol<br />
Neoplasia 2010; 15: 213-223<br />
89 Braun J, Hoang-Vu C, Dralle H, Hüttelmaier S. Downregulation<br />
<strong>of</strong> microRNAs directs the EMT and invasive potential<br />
<strong>of</strong> anaplastic thyroid carcinomas. Oncogene 2010; 29:<br />
4237-4244<br />
90 Downward J. Targeting RAS signalling pathways in <strong>cancer</strong><br />
therapy. Nat Rev Cancer 2003; 3: 11-22<br />
91 Kim IA, Bae SS, Fernandes A, Wu J, Muschel RJ, McKenna<br />
WG, Birnbaum MJ, Bernhard EJ. Selective inhibition <strong>of</strong> Ras,<br />
phosphoinositide 3 kinase, and Akt is<strong>of</strong>orms increases the<br />
radiosensitivity <strong>of</strong> human carcinoma cell lines. Cancer Res<br />
2005; 65: 7902-7910<br />
92 Egger G, Liang G, Aparicio A, Jones PA. Epigenetics in human<br />
disease and prospects for epigenetic therapy. Nature<br />
2004; 429: 457-463<br />
93 Lane AA, Chabner BA. Histone deacetylase inhibitors in<br />
<strong>cancer</strong> therapy. J Clin Oncol 2009; 27: 5459-5468<br />
94 Esau CC. Inhibition <strong>of</strong> microRNA with antisense oligonucleotides.<br />
Methods 2008; 44: 55-60<br />
95 Li L, Aggarwal BB, Shishodia S, Abbruzzese J, Kurzrock R.<br />
Nuclear factor-kappaB and IkappaB kinase are constitutively<br />
active in human pancreatic cells, and their down-regulation<br />
by curcumin (diferuloylmethane) is associated with the suppression<br />
<strong>of</strong> proliferation and the induction <strong>of</strong> apoptosis. Cancer<br />
2004; 101: 2351-2362<br />
WJG|www.wjgnet.com<br />
Park JY et al . MicroRNAs in pancreatic <strong>cancer</strong><br />
96 Li L, Braiteh FS, Kurzrock R. Liposome-encapsulated curcumin:<br />
in vitro and in vivo effects on proliferation, apoptosis,<br />
signaling, and angiogenesis. Cancer 2005; 104: 1322-1331<br />
97 Aggarwal BB, Kumar A, Bharti AC. Anti<strong>cancer</strong> potential<br />
<strong>of</strong> curcumin: preclinical and clinical studies. Anti<strong>cancer</strong> Res<br />
2003; 23: 363-398<br />
98 Dhillon N, Aggarwal BB, Newman RA, Wolff RA, Kunnumakkara<br />
AB, Abbruzzese JL, Ng CS, Badmaev V, Kurzrock<br />
R. Phase II trial <strong>of</strong> curcumin in patients with advanced pancreatic<br />
<strong>cancer</strong>. Clin Cancer Res 2008; 14: 4491-4499<br />
99 Frank NY, Schatton T, Frank MH. The therapeutic promise<br />
<strong>of</strong> the <strong>cancer</strong> stem cell concept. J Clin Invest 2010; 120: 41-50<br />
100 Jones PA, Baylin SB. The epigenomics <strong>of</strong> <strong>cancer</strong>. Cell 2007;<br />
128: 683-692<br />
101 Sharma S, Kelly TK, Jones PA. Epigenetics in <strong>cancer</strong>. Carcinogenesis<br />
2010; 31: 27-36<br />
102 Han L, Witmer PD, Casey E, Valle D, Sukumar S. DNA<br />
methylation regulates MicroRNA expression. Cancer Biol<br />
Ther 2007; 6: 1284-1288<br />
103 Davalos V, Esteller M. MicroRNAs and <strong>cancer</strong> epigenetics:<br />
a macrorevolution. Curr Opin Oncol 2010; 22: 35-45<br />
104 Tomasini R, Samir AA, Vaccaro MI, Pebusque MJ, Dagorn<br />
JC, Iovanna JL, Dusetti NJ. Molecular and functional characterization<br />
<strong>of</strong> the stress-induced protein (SIP) gene and<br />
its two transcripts generated by alternative splicing. SIP<br />
induced by stress and promotes cell death. J Biol Chem 2001;<br />
276: 44185-44192<br />
105 Tomasini R, Samir AA, Pebusque MJ, Calvo EL, Totaro S,<br />
Dagorn JC, Dusetti NJ, Iovanna JL. P53-dependent expression<br />
<strong>of</strong> the stress-induced protein (SIP). Eur J Cell Biol 2002;<br />
81: 294-301<br />
106 Zhou CZ, Peng ZH, Zhang F, Qiu GQ, He L. Loss <strong>of</strong> heterozygosity<br />
on long arm <strong>of</strong> chromosome 22 in sporadic colo<strong>rectal</strong><br />
carcinoma. <strong>World</strong> J Gastroenterol 2002; 8: 668-673<br />
107 Wild A, Langer P, Celik I, Chaloupka B, Bartsch DK. Chromosome<br />
22q in pancreatic endocrine tumors: identification<br />
<strong>of</strong> a homozygous deletion and potential prognostic associations<br />
<strong>of</strong> allelic deletions. Eur J Endocrinol 2002; 147: 507-513<br />
108 Muraoka M, Konishi M, Kikuchi-Yanoshita R, Tanaka K,<br />
Shitara N, Chong JM, Iwama T, Miyaki M. p300 gene alterations<br />
in colo<strong>rectal</strong> and gastric carcinomas. Oncogene 1996;<br />
12: 1565-1569<br />
109 Iyer NG, Ozdag H, Caldas C. p300/CBP and <strong>cancer</strong>. Oncogene<br />
2004; 23: 4225-4231<br />
110 Melief CJ. Cancer immunotherapy by dendritic cells. Immunity<br />
2008; 29: 372-383<br />
111 Loskog AS, Eliopoulos AG. The Janus faces <strong>of</strong> CD40 in <strong>cancer</strong>.<br />
Semin Immunol 2009; 21: 301-307<br />
112 Sassen S, Miska EA, Caldas C. MicroRNA: implications for<br />
<strong>cancer</strong>. Virchows Arch 2008; 452: 1-10<br />
113 Garzon R, Calin GA, Croce CM. MicroRNAs in Cancer.<br />
Annu Rev Med 2009; 60: 167-179<br />
114 Iorio MV, Croce CM. MicroRNAs in <strong>cancer</strong>: small molecules<br />
with a huge impact. J Clin Oncol 2009; 27: 5848-5856<br />
115 Mirnezami AH, Pickard K, Zhang L, Primrose JN, Packham<br />
G. MicroRNAs: key players in carcinogenesis and novel<br />
therapeutic targets. Eur J Surg Oncol 2009; 35: 339-347<br />
116 Davis S, Propp S, Freier SM, Jones LE, Serra MJ, Kinberger<br />
G, Bhat B, Swayze EE, Bennett CF, Esau C. Potent inhibition<br />
<strong>of</strong> microRNA in vivo without degradation. Nucleic Acids Res<br />
2009; 37: 70-77<br />
117 Jay C, Nemunaitis J, Chen P, Fulgham P, Tong AW. miRNA<br />
pr<strong>of</strong>iling for diagnosis and prognosis <strong>of</strong> human <strong>cancer</strong>.<br />
DNA Cell Biol 2007; 26: 293-300<br />
118 Yang N, Coukos G, Zhang L. MicroRNA epigenetic alterations<br />
in human <strong>cancer</strong>: one step forward in diagnosis and<br />
treatment. Int J Cancer 2008; 122: 963-968<br />
S- Editor Sun H L- Editor Kerr C E- Editor Ma WH<br />
827 February 21, 2011|Volume 17|Issue 7|
Online Submissions: http://www.wjgnet.com/1007-9327<strong>of</strong>fice<br />
wjg@wjgnet.com<br />
doi:10.3748/wjg.v17.i7.828<br />
Imran Hassan, MD, Assistant Pr<strong>of</strong>essor, Series Editor<br />
Current trends in staging <strong>rectal</strong> <strong>cancer</strong><br />
Abdus Samee, Chelliah Ramachandran Selvasekar<br />
Abdus Samee, Department <strong>of</strong> Surgery, Princess Royal Hospital,<br />
Telford, Shropshire, United Kingdom<br />
Chelliah Ramachandran Selvasekar, Department <strong>of</strong> Surgery,<br />
Mid Cheshire Hospitals NHS Foundation Trust, Crewe,<br />
United Kingdom<br />
Author contributions: Selvasekar CR designed the study;<br />
Samee A and Selvasekar CR were literature search and drafting<br />
the article; Samee A and Selvasekar CR revised the critically.<br />
Correspondence to: Chelliah Ramachandran Selvasekar,<br />
MD, FRCS, Consultant Colo<strong>rectal</strong> Surgeon, Department <strong>of</strong><br />
Surgery, Mid Cheshire Hospitals NHS Foundation Trust, Crewe,<br />
United Kingdom. crselvasekar@aol.com<br />
Telephone: +44-1270-612046 Fax: +44-1270-612494<br />
Received: August 30, 2010 Revised: November 12, 2010<br />
Accepted: November 19, 2010<br />
Published online: February 21, 2011<br />
Abstract<br />
<strong>Management</strong> <strong>of</strong> <strong>rectal</strong> <strong>cancer</strong> has evolved over the years.<br />
In this condition preoperative investigations assist in deciding<br />
the optimal treatment. The relation <strong>of</strong> the tumor<br />
edge to the circumferential margin (CRM) is an important<br />
factor in deciding the need for neoadjuvant treatment<br />
and determines the prognosis. Those with threatened or<br />
involved margins are <strong>of</strong>fered long course chemoradiation<br />
to enable R0 surgical resection. Endoanal ultrasound<br />
(EUS) is useful for tumor (T) staging; hence EUS is a<br />
useful imaging modality for early <strong>rectal</strong> <strong>cancer</strong>. Magnetic<br />
resonance imaging (MRI) is useful for assessing the<br />
mesorectum and the meso<strong>rectal</strong> fascia which has useful<br />
prognostic significance and for early identification <strong>of</strong> local<br />
recurrence. Computerized tomography (CT) <strong>of</strong> the chest,<br />
abdomen and pelvis is used to rule out distant metastasis.<br />
Identification <strong>of</strong> the malignant nodes using EUS, CT<br />
and MRI is based on the size, morphology and internal<br />
characteristics but has drawbacks. Most <strong>of</strong> the common<br />
imaging techniques are suboptimal for imaging following<br />
chemoradiation as they struggle to differentiate fibrotic<br />
changes and tumor. In this situation, EUS and MRI may<br />
provide complementary information to decide further<br />
treatment. Functional imaging using positron emission<br />
WJG|www.wjgnet.com<br />
828<br />
<strong>World</strong> J Gastroenterol 2011 February 21; 17(7): 828-834<br />
ISSN 1007-9327 (print) ISSN 2219-2840 (online)<br />
© 2011 Baishideng. All rights reserved.<br />
tomography (PET) is useful, particularly PET/CT fusion<br />
scans to identify areas <strong>of</strong> the functionally hot spots. In<br />
the current state, imaging has enabled the multidisciplinary<br />
team <strong>of</strong> surgeons, oncologists, radiologists and<br />
pathologists to decide on the patient centered management<br />
<strong>of</strong> <strong>rectal</strong> <strong>cancer</strong>. In future, functional imaging may<br />
play an active role in identifying patients with lymph<br />
node metastasis and those with residual and recurrent<br />
disease following neoadjuvant chemoradiotherapy.<br />
© 2011 Baishideng. All rights reserved.<br />
Key words: Rectal <strong>cancer</strong>; Staging; Investigations;<br />
Magnetic resonance imaging; Ultrasound; Endoanal ultrasound;<br />
Positron emission tomography; Computerized<br />
tomography<br />
Peer reviewer: Christopher Mantyh, MD, Associate Pr<strong>of</strong>essor,<br />
Department <strong>of</strong> Surgery, Duke University Medical Center, Box<br />
3117, Durham, NC 2771, United States<br />
Samee A, Selvasekar CR. Current trends in staging <strong>rectal</strong> <strong>cancer</strong>.<br />
<strong>World</strong> J Gastroenterol 2011; 17(7): 828-834 Available from:<br />
URL: http://www.wjgnet.com/1007-9327/full/v17/i7/828.htm<br />
DOI: http://dx.doi.org/10.3748/wjg.v17.i7.828<br />
INTRODUCTION<br />
TOPIC HIGHLIGHT<br />
Nearly one million patients are diagnosed with colo<strong>rectal</strong><br />
<strong>cancer</strong>s (CRC) annually in the world [1] . The incidence <strong>of</strong><br />
CRC is highest in the western world where it is the second<br />
commonest cause <strong>of</strong> <strong>cancer</strong> death and fourth commonest<br />
cause <strong>of</strong> death from <strong>cancer</strong> worldwide [2] . In the western<br />
world there is a life time risk <strong>of</strong> CRC <strong>of</strong> 5%. Overall the 5<br />
year survival has improved in the UK (55% in males and<br />
51% in females) but to a lesser extent than in the USA and<br />
Europe [3] .<br />
Around 30%-40% <strong>of</strong> colo<strong>rectal</strong> <strong>cancer</strong> is defined to<br />
arise from the rectum which is defined as the distal margin<br />
<strong>of</strong> tumor within 15 cm <strong>of</strong> the anal verge [4,5] .<br />
Colonoscopy and biopsy is considered as the gold<br />
February 21, 2011|Volume 17|Issue 7|
standard investigation to confirm the diagnosis <strong>of</strong> <strong>rectal</strong><br />
<strong>cancer</strong> and to exclude synchronous lesions. Patients are<br />
then <strong>stage</strong>d to assess the extent <strong>of</strong> local disease and to<br />
identify the distant spread.<br />
Traditional <strong>rectal</strong> <strong>cancer</strong> surgery is associated with high<br />
rates <strong>of</strong> local recurrence <strong>of</strong> 5%-20% [6] . However, with the<br />
combination <strong>of</strong> high quality surgery using total meso<strong>rectal</strong><br />
excision [7] along with use <strong>of</strong> neoadjuvant and adjuvant<br />
treatment there has been a significant reduction in local<br />
recurrence and improved survival [8] . The surgeon aims to<br />
achieve a microscopic tumor free (R0) resection. Despite<br />
this, there is a risk <strong>of</strong> local failure. Careful preoperative<br />
assessment <strong>of</strong> the pelvis identifies high risk patients in<br />
whom the resection margins are either involved or within<br />
1 mm <strong>of</strong> the meso<strong>rectal</strong> fascia. Involvement or threatened<br />
CRM (tumors within 1 mm <strong>of</strong> the meso<strong>rectal</strong> fascia) have<br />
a reduced chance <strong>of</strong> obtaining complete clearance. Thus,<br />
the status <strong>of</strong> the CRM has become more important than<br />
the TNM staging. In Europe and the UK, patients with<br />
involved CRM/threatened CRM are considered for long<br />
course chemoradiation prior to surgery.<br />
IMPORTANCE OF PREOPERATIVE<br />
STAGING IN RECTAL CANCER<br />
Accurate pre-operative staging <strong>of</strong> <strong>rectal</strong> <strong>cancer</strong> is crucial<br />
in planning the surgical treatment and is the strongest predictor<br />
for recurrence [9] . The staging helps us to formulate<br />
a structured multidisciplinary management care plan and<br />
assess the prognosis. It is also used to compare the results<br />
<strong>of</strong> hospitals <strong>of</strong>fering <strong>rectal</strong> <strong>cancer</strong> treatment and to define<br />
the role <strong>of</strong> different treatment modalities.<br />
Preoperative staging <strong>of</strong> <strong>rectal</strong> <strong>cancer</strong> can be divided<br />
into either local or distant staging. Local staging incorporates<br />
the assessment <strong>of</strong> mural wall invasion, circumferential<br />
resection margin involvement, and the nodal status for<br />
metastasis. Distant staging assesses for evidence <strong>of</strong> metastatic<br />
disease.<br />
Rectal <strong>cancer</strong> is palpable in 40%-80% <strong>of</strong> cases [10] . Digital<br />
<strong>rectal</strong> examination helps in documentation <strong>of</strong> the size,<br />
location, distance from the anal verge, and fixity. Lesions<br />
felt by digital <strong>rectal</strong> examination can be visualized using a<br />
rigid proctoscope. The procedure allows an accurate localization<br />
and assessment <strong>of</strong> the tumor including fixity. Biopsies<br />
can be carried out where necessary. Rectal examination<br />
using proctoscopy may be considered as an important<br />
tool for newly diagnosed <strong>rectal</strong> <strong>cancer</strong>s. Painful local perineal<br />
and anal conditions such as fissures or abscesses can<br />
restrict the use <strong>of</strong> this excellent tool. A trial comparing<br />
the use <strong>of</strong> CT virtual proctoscopy with <strong>rectal</strong> ultrasound<br />
examination in determining the <strong>stage</strong> <strong>of</strong> <strong>rectal</strong> <strong>cancer</strong> is<br />
being conducted in the USA and its results are awaited<br />
(http://clinical trials.gov/ct2/show/NCT00585728).<br />
Currently, several modalities exist for the preoperative<br />
staging <strong>of</strong> <strong>rectal</strong> <strong>cancer</strong>. A combination <strong>of</strong> modalities involving<br />
use <strong>of</strong> computed tomography (CT), magnetic resonance<br />
imaging (MRI), and/or endo<strong>rectal</strong> ultrasonography<br />
(EUS) is used to precisely assess the extent <strong>of</strong> spread<br />
<strong>of</strong> <strong>rectal</strong> <strong>cancer</strong>. The choice <strong>of</strong> investigations performed,<br />
WJG|www.wjgnet.com<br />
Samee A et al . Current trends in staging <strong>rectal</strong> <strong>cancer</strong><br />
however, is influenced by local expertise, guidelines and<br />
availability. Imaging in <strong>rectal</strong> <strong>cancer</strong> plays a crucial role in<br />
optimizing radiotherapy target definition to avoid adjacent<br />
vital structures [11] . EUS and MRI <strong>of</strong> the pelvis are used<br />
to assess the local spread while CT is the main modality<br />
to assess systemic spread. PET is indicated when there is<br />
clinical, biochemical or radiological suspicion <strong>of</strong> local recurrence<br />
or systemic disease.<br />
Computerized tomography and computerized<br />
tomography colonography or virtual colonoscopy<br />
CT scan <strong>of</strong> the entire chest, abdomen and pelvis is used<br />
for the detection <strong>of</strong> metastatic disease. CT is widely<br />
available and has faster acquisition times. However, it<br />
is not considered as the investigation <strong>of</strong> choice when it<br />
comes to assessing the layers <strong>of</strong> the <strong>rectal</strong> wall; hence<br />
it is not useful for local staging in <strong>rectal</strong> <strong>cancer</strong> and certainly<br />
is poor at evaluating superficial <strong>rectal</strong> <strong>cancer</strong>s. The<br />
accuracy <strong>of</strong> CT to assess the tumor has been reported<br />
to be between 80%-95% in patients with advanced local<br />
disease [12] . The accuracy, however, decreased to around<br />
63% when a broader spectrum <strong>of</strong> tumor sizes was analyzed.<br />
Sensitivity to pick up nodal disease has been found<br />
to be between 55%-70% [13] . In a meta-analysis involving<br />
5000 patients, CT showed an accuracy for T staging <strong>of</strong><br />
73% and for nodal staging <strong>of</strong> 22%-73% [14] .<br />
The use <strong>of</strong> contrast enhanced multidetector CT colonography<br />
has improved the staging accuracy [15] , by achieving<br />
superior spatial resolution and visualizing pictures in a<br />
variety <strong>of</strong> planes. However, its role in staging remains to<br />
be determined and currently it is used mainly to assess the<br />
distant metastatic disease (Figure 1A and B).<br />
Virtual colonoscopy or CT colonogram (CTC) has<br />
been reported to be safer than colonoscopy [16] while being<br />
more sensitive than barium enema, and appears to<br />
be more acceptable to patients than either <strong>of</strong> the other<br />
tests [17] . The procedure can be performed by technicians<br />
thus saving clinicians time. In principle the data could be<br />
analysed by computer-assistance thus accelerating diagnosis<br />
time [18] . The results <strong>of</strong> the SIGGAR trial evaluating<br />
CTC versus colonoscopy or barium enema in symptomatic<br />
elderly patients are awaited [19] . CTC is the best<br />
radiological imaging for assessing the colon and rectum<br />
and at the same time identifies nodal disease and distant<br />
metastasis. The diagnosis <strong>of</strong> <strong>rectal</strong> <strong>cancer</strong> still needs to<br />
be confirmed by colonoscopy and biopsy.<br />
Magnetic resonance imaging<br />
Magnetic resonance imaging (MRI) is routinely used for<br />
preoperative staging <strong>of</strong> <strong>rectal</strong> <strong>cancer</strong> as it provides an accurate<br />
assessment <strong>of</strong> the tumor and the surrounding meso<strong>rectal</strong><br />
fascia. It identifies patients at risk <strong>of</strong> local recurrence<br />
and those likely to benefit from neoadjuvant therapy.<br />
When compared with CT and ultrasound, MRI is more<br />
reliable for the evaluation <strong>of</strong> the extent <strong>of</strong> locoregional<br />
disease, planning radiation therapy, assessing postoperative<br />
changes and pelvic recurrence. The evaluation <strong>of</strong> nodal<br />
metastases remains a challenge with MRI (Figure 2).<br />
Earlier MRI studies used body coils which lacked the<br />
829 February 21, 2011|Volume 17|Issue 7|
A<br />
B<br />
Samee A et al . Current trends in staging <strong>rectal</strong> <strong>cancer</strong><br />
Figure 1 Computerized tomography. A: Computerized tomography (CT) abdomen<br />
showing a patient with <strong>rectal</strong> <strong>cancer</strong> having liver metastasis and ascites;<br />
B: CT Chest showing a patient with <strong>rectal</strong> <strong>cancer</strong> having lung metastasis.<br />
Figure 2 Coronal magnetic resonance imaging (arrow) showing possible<br />
lymph node or early vascular involvement.<br />
resolution to differentiate the different layers <strong>of</strong> the <strong>rectal</strong><br />
wall and added no advantage to conventional CT [20] .<br />
Subsequent use <strong>of</strong> phased-array coils permitted reliable<br />
identification <strong>of</strong> the meso<strong>rectal</strong> fascia which is crucial in<br />
the management <strong>of</strong> <strong>rectal</strong> <strong>cancer</strong> [21] . Initial studies suggested<br />
a histological clearance <strong>of</strong> at least 10 mm could be<br />
accurately predicted when the radiological clearance from<br />
the meso<strong>rectal</strong> fascia and critical structure was at least<br />
5 mm [22] . Subsequent single centre study showed 92% accuracy<br />
in prediction <strong>of</strong> CRM involvement when the CRM<br />
cut<strong>of</strong>f <strong>of</strong> 1 mm was used and this is now confirmed from<br />
the multicentre European MERCURY study [21,23] . In Europe,<br />
MRI is now routinely used in the preoperative investigation<br />
for <strong>rectal</strong> <strong>cancer</strong>. Techniques for obtaining optimal<br />
WJG|www.wjgnet.com<br />
Figure 3 Magnetic resonance imaging (arrow) showing possible extension<br />
beyond the muscularis propria, radiologically <strong>stage</strong>d as early T3.<br />
Figure 4 Coronal T2 W magnetic resonance imaging (arrow) showing<br />
the intact muscularis propria in a patient with <strong>rectal</strong> <strong>cancer</strong>. Radiologically<br />
<strong>stage</strong>d as T1 or T2.<br />
MRI images are described in the literature [24] . An axial picture<br />
enables identification <strong>of</strong> the distance <strong>of</strong> the CRM to<br />
the tumor. Coronal sections are useful in low <strong>rectal</strong> tumors<br />
to identify the relation to anal sphincter complex, pelvic<br />
floor, and pelvic side wall [25] . High signal intensity <strong>of</strong> the<br />
tumor on T2 w images suggest the presence <strong>of</strong> mucinous<br />
carcinoma which has poor prognosis compared to nonmucinous<br />
carcinoma [26] . The standard phased array MRI<br />
produces good quality images with good contrast resolution<br />
and a relatively large field <strong>of</strong> view. Routine use <strong>of</strong> intravenous<br />
contrast does not appear to improve the accuracy [27] .<br />
MRI cannot differentiate between T2 and early T3 lesions;<br />
a nodular or rounded advancing margin at the interface between<br />
muscularis propria and peri<strong>rectal</strong> fat is suggestive <strong>of</strong><br />
T3 (Figure 3). Sometimes spiculations in the peri<strong>rectal</strong> fat<br />
are considered as T3 when in fact they are T2 with desmoplastic<br />
reaction [22,28] . MRI certainly cannot differentiate between<br />
a T1 and T2 <strong>cancer</strong> (Figure 4). Another area <strong>of</strong> drawback<br />
is restaging following long course chemoradiotherapy.<br />
Studies by Chen and H<strong>of</strong>fmann found T staging accuracy<br />
was 52% and 54% when compared to histology [29] . This is<br />
due to the inability to distinguish fibrosis from tumor with<br />
MRI similar to EUS. In low anterior tumors where the meso<strong>rectal</strong><br />
fascia is close to the muscularis propria early T3 can<br />
still infiltrate the meso<strong>rectal</strong> fascia [24] . Extramural vascular<br />
invasion is known to be an independent predictor <strong>of</strong> local<br />
recurrence [30,31] . The presence <strong>of</strong> a tubular structure in<br />
830 February 21, 2011|Volume 17|Issue 7|
proximity to a T3 tumor or nodules with an irregular margin<br />
probably represents vascular invasion [21,32] . Recently there<br />
has been interest in the use <strong>of</strong> functional imaging such as<br />
diffusion weighted MRI imaging (DWI) and CT/PET to<br />
distinguish fibrosis from tumor [33] .<br />
MRI has been found to be useful in more advanced<br />
disease by providing clearer definition <strong>of</strong> the mesorectum<br />
and meso<strong>rectal</strong> fascia and seems to be a promising tool in<br />
assessing the locally advanced disease. With the advent <strong>of</strong><br />
endo<strong>rectal</strong> coils, the T staging accuracy has been reported<br />
to be between 70%-90% [34] . However, this technique has<br />
its limitations specially when evaluating the surrounding<br />
tissue, owing to signal attenuation at a short distance from<br />
the coil. Patient’s compliance, limited availability and cost<br />
also contribute to its less wide application. Obstructing<br />
or nearly obstructing lesions can be difficult to negotiate<br />
as are high <strong>rectal</strong> <strong>cancer</strong>s leading to failed/improper coil<br />
insertion in approximately 40% <strong>of</strong> patients [34] .<br />
Nodal accuracy has also been found to be variable although<br />
use <strong>of</strong> superparamagnetic iron oxide particles appears<br />
to be promising [35] as evidenced by studies in head,<br />
neck and urological <strong>cancer</strong>s.<br />
Ultrasound<br />
Abdominal ultrasound (USS) is used to evaluate liver for<br />
metastasis, ascites, adenopathy, and for omental cake. The<br />
false negative rate is reported to be around 8% [36] . The<br />
technique, although inexpensive and widely available, is<br />
operator dependent. Intraoperative USS is rarely used<br />
apart from when synchronous <strong>rectal</strong> and liver resections<br />
are planned. Rapid advancement in imaging modalities has<br />
made USS a less favoured imaging modality in <strong>rectal</strong> <strong>cancer</strong><br />
staging [37] .<br />
Endo<strong>rectal</strong> ultrasound<br />
Endo<strong>rectal</strong> ultrasound (EUS) is sensitive for early <strong>rectal</strong> <strong>cancer</strong>s<br />
(T1 and T2 lesions) with an accuracy <strong>of</strong> 69%-97% [38-43]<br />
and is useful in the surveillance following post transanal surgery.<br />
The standard technique involves a transanal probe enclosed<br />
in a water filled balloon introduced into the rectum to<br />
allow radial visualization <strong>of</strong> the rectum. High resolution allows<br />
the assessment <strong>of</strong> the <strong>rectal</strong> wall but the assessment <strong>of</strong><br />
the meso<strong>rectal</strong> fascia is not possible and the assessment <strong>of</strong><br />
the lymph nodes can be an issue and overstating has been a<br />
concern. Peritumor inflammation and artifacts due to faeces<br />
may lead to an ultrasound appearance which can be misinterpreted<br />
as tumor. These drawbacks can be exaggerated between<br />
the muscle layer and the surrounding fat which makes<br />
T2 and T3 lesions difficult to distinguish [44] . The accuracy <strong>of</strong><br />
the T <strong>stage</strong> evaluation varies from 62%-92% [45] . In a metaanalysis<br />
<strong>of</strong> 11 studies it has been shown that sensitivities for<br />
superficial tumors are better than advanced lesions [46] . A 20<br />
year (1984-2004) systematic review looking at studies with<br />
a minimum <strong>of</strong> 50 patients, evaluating the use <strong>of</strong> endo<strong>rectal</strong><br />
ultrasound and magnetic resonance imaging (MRI) in the<br />
local staging <strong>of</strong> <strong>rectal</strong> <strong>cancer</strong>, have found a complementary<br />
role for these imaging modalities in the assessment <strong>of</strong> tumor<br />
depth. Ultrasound was found to be highly accurate in<br />
early lesions (T1, 2, 40%-100%; T3, 4, 25%-100%, overall 82%).<br />
WJG|www.wjgnet.com<br />
Samee A et al . Current trends in staging <strong>rectal</strong> <strong>cancer</strong><br />
The review also found a similar accuracy in the assessment<br />
<strong>of</strong> nodal metastases [47] . Two meta-analyses in literature have<br />
shown that the sensitivity is affected by T <strong>stage</strong> [48] . A metaanalysis<br />
including 84 studies found EUS to be slightly superior<br />
in assessing the local involvement such as lymph nodes,<br />
however, no significant differences were noted when compared<br />
to other imaging modalities such as MRI. The results<br />
suggest that none <strong>of</strong> the current imaging modalities enable<br />
reliable detection <strong>of</strong> metastatic nodal disease [49] .<br />
EUS however, has its limitations as it cannot reliably<br />
distinguish an irregular outer <strong>rectal</strong> wall due to peritumoral<br />
inflammation or transmural tumor extension. Obstructing<br />
lesions may be difficult to scan especially with rigid probes<br />
leading to suboptimal staging. The scanning, although less<br />
expensive and portable, is operator dependent and has a<br />
steep learning curve. Bulky, high, stenotic, advanced (T3)<br />
lesions or post-neoadjuvant therapy down<strong>stage</strong>d tumors<br />
can be a challenge [50-52] .<br />
EUS nodal staging accuracy is around 75% [53] . Morphologic<br />
characteristics suggestive <strong>of</strong> malignant involvement<br />
include hypoechoic appearance, round shape, peritumoral<br />
location, and size > 5 mm [45,46,51-53] . The locoregional<br />
tumor assessment using three-dimensional EUS<br />
consists <strong>of</strong> transverse, coronal and sagital scan and has<br />
been found to be superior to CT and two-dimensional<br />
EUS. The 3D-reconstructed image shows tumor protrusion<br />
infiltrating into adjacent structures, thus, allowing<br />
for improved T and N staging [54] . Further, EUS-guided<br />
fine-needle aspiration can be carried out at the same time<br />
from the lesion or suspiciously looking lymph nodes.<br />
Positron emission tomography<br />
The principle <strong>of</strong> positron emission tomography (PET)<br />
is based on the differential metabolic pr<strong>of</strong>ile <strong>of</strong> tumors<br />
compared to normal tissue. Fluoro-deoxy-glucose (FDG)<br />
is the most common PET tracer used. Due to increased<br />
metabolic activity, and change in the tumor biology,<br />
tumors preferentially show an increased uptake which<br />
results in radiolabelling [55] . Although selective, FDG accumulates<br />
in areas <strong>of</strong> infection, inflammation, in organs <strong>of</strong><br />
increased metabolic activity such as brain, myocardium,<br />
liver or kidneys leading to false positive results [55] . FDG<br />
uptake is also influenced by the presence <strong>of</strong> mucin. PET<br />
is useful in identifying non-mucinous tumors compared to<br />
mucinous tumors. FDG/PET is mainly useful in the assessment<br />
<strong>of</strong> local recurrence and metastatic disease when<br />
conventional imaging is not helpful [56,57] . Currently it is not<br />
used as a primary staging modality in <strong>rectal</strong> <strong>cancer</strong>s. Interpretation<br />
<strong>of</strong> PET without anatomic correlation poses difficulties<br />
hence PET-CT fusion scans where the pictures <strong>of</strong><br />
both investigations are fused using s<strong>of</strong>tware is used. This<br />
<strong>of</strong>fers a detailed anatomical and functional imaging and is<br />
gaining rapid popularity and acceptance. The combination<br />
provides additional value to localize the hot spots. There<br />
are some technical limitations with this combination imaging<br />
and with the false positive rates due to other disease<br />
and physiological processes. The role <strong>of</strong> PET CT fusion<br />
scan has not changed compared to PET scans.<br />
However, a recent study has found preoperative PET<br />
831 February 21, 2011|Volume 17|Issue 7|
Samee A et al . Current trends in staging <strong>rectal</strong> <strong>cancer</strong><br />
changed the management in 17% <strong>of</strong> patients [58] with improved<br />
staging accuracy in combination with CT [56] . Another<br />
study carried by Gearhart in 37 patients reported an<br />
altered management plan for 27% <strong>of</strong> patients using FDG-<br />
PET/CT imaging modality for low <strong>rectal</strong> <strong>cancer</strong> [59] .<br />
Staging accuracy post-neoadjuvant therapy<br />
With the increasing use <strong>of</strong> pre-operative neoadjuvant<br />
therapy, <strong>rectal</strong> tumor re-staging is increasingly performed<br />
prior to curative resection.<br />
A reduction in staging accuracy has been noted which<br />
may be as a result <strong>of</strong> effects <strong>of</strong> neoadjuvant treatment due to<br />
post-radiation edema, inflammation, fibrosis, and necrosis [60] .<br />
A recent study <strong>of</strong> 29 patients undergoing neoadjuvant<br />
therapy and pretreatment and post-treatment staging<br />
with CT, MRI, and PET showed that PET was 100%<br />
sensitive in predicting response to therapy (compared<br />
with 54% for CT and 71% for MRI). Corresponding<br />
specificity for predicting tumor response to treatment<br />
was 60%, 80%, and 67% for PET, CT, and MRI, respectively<br />
[61] , thus suggesting a further possible role <strong>of</strong> PET<br />
in predicting response to neoadjuvant therapy.<br />
Tumor re-staging following post-neoadjuvant therapy<br />
remains problematic and it is hoped that a combination<br />
<strong>of</strong> imaging technique (CT, MRI, and EUS) and functional<br />
(PET) imaging may improve staging accuracy.<br />
Suggested investigations for tumor staging <strong>of</strong> <strong>rectal</strong><br />
<strong>cancer</strong><br />
On review <strong>of</strong> the literature, phased array MRI and EUS<br />
should be considered as the initial modalities to <strong>stage</strong> the<br />
local tumor. A fixed, locally advanced <strong>rectal</strong> <strong>cancer</strong> may be<br />
imaged better by MRI (Figure 5), whereas EUS is more<br />
appropriate for an early mobile <strong>rectal</strong> tumor (T1-T2 lesions).<br />
MRI has been shown to be highly accurate in predicting<br />
a clear circumferential resection margin in patients<br />
undergoing TME. Although both MRI and EUS provide<br />
a comparable overall T- and N-staging, use <strong>of</strong> these modalities<br />
is limited by issues such as availability, costs and<br />
technical expertise. CT scanning, although still the current<br />
standard for distant staging, may not be an effective tool<br />
to <strong>stage</strong> the local disease. A combination <strong>of</strong> CT and PET<br />
<strong>of</strong>fering a detailed anatomical and functional imaging,<br />
however, seem to be promising and gaining popularity<br />
and acceptance for recurrent <strong>rectal</strong> <strong>cancer</strong>s.<br />
Suggested investigation for nodal staging <strong>of</strong> <strong>rectal</strong> <strong>cancer</strong><br />
The accuracy <strong>of</strong> MRI, CT and EUS for identifying malignant<br />
nodes is poor. Current criteria are based on size,<br />
shape and morphology. Any node <strong>of</strong> 1 cm and over is<br />
taken as significant [62] . The enlarged lymph node can be<br />
as a result <strong>of</strong> the inflammatory process but normal size<br />
nodes can have micrometastases. Brown et al [54] found<br />
58% <strong>of</strong> positive malignant nodes were less than 5 mm.<br />
Morphological characteristics such as round shape, irregular<br />
borders and heterogenous signal intensity suggest<br />
nodal involvement [63] .<br />
Nodal accuracy has also been found to be variable,<br />
although use <strong>of</strong> superparamagnetic iron oxide particles<br />
WJG|www.wjgnet.com<br />
A<br />
B<br />
Figure 5 Magnetic resonance imaging. A: Magnetic resonance imaging<br />
(MRI) (arrow) showing the <strong>rectal</strong> <strong>cancer</strong> involving the circumferential resection<br />
margin; B: MRI (arrow) showing the <strong>rectal</strong> <strong>cancer</strong> invading the ischio<strong>rectal</strong> fat<br />
on the right (T4).<br />
(SPIO) seem to be promising as evidenced by studies in<br />
head, neck and urological <strong>cancer</strong>s. The technique involves<br />
use <strong>of</strong> a contrast media containing SPIO which accumulates<br />
in normal lymph nodes, whereas due to defective<br />
phagocytosis, the uptake is poor or absent in malignant<br />
nodes. Hence by using T2 weighted imaging, these nodes<br />
can be identified. Initial studies are promising but further<br />
research is needed [35] .<br />
CHOOSING THE CORRECT<br />
MANAGEMENT BASED ON STAGING IN<br />
THE ELDERLY<br />
Over the age <strong>of</strong> 80, there is 10% mortality with <strong>rectal</strong> <strong>cancer</strong><br />
surgery [64] . Studies from Brazil have shown a complete<br />
pathological response with chemoradiation [65] and it is well<br />
known that the elderly respond better to radiotherapy.<br />
Hence in a selected group <strong>of</strong> patients, imaging with<br />
EUS and MRI can identify patients who can be treated<br />
with neoadjuvant treatment and those with a complete<br />
radiological response can be followed by active surveillance<br />
with an intensive imaging protocol to identify those<br />
who recur to be considered for standard salvage surgical<br />
treatment or for local excision, thereby avoiding the risks<br />
associated with major <strong>rectal</strong> <strong>cancer</strong> surgery and possibly<br />
avoiding the need for permanent stoma and enabling organ<br />
preservation. This is possible only with high quality<br />
imaging techniques to assess the loco-regional disease.<br />
832 February 21, 2011|Volume 17|Issue 7|
CONCLUSION<br />
Imaging in <strong>rectal</strong> <strong>cancer</strong> helps in deciding the treatment and<br />
determining the prognosis. The newer techniques help in<br />
superior image resolution, three-dimensional viewing, with<br />
decreased image acquisition times, minimal bowel preparation,<br />
and sometimes with functional qualities. This may be<br />
important following neo-adjuvant treatment. The most accurate<br />
method <strong>of</strong> <strong>rectal</strong> wall staging <strong>of</strong> <strong>rectal</strong> <strong>cancer</strong> is endo<strong>rectal</strong><br />
ultrasound and MRI but accurate staging <strong>of</strong> meso<strong>rectal</strong><br />
fascia and lymph nodes is by phased array MRI. The<br />
management <strong>of</strong> <strong>rectal</strong> <strong>cancer</strong> is based on the proximity <strong>of</strong><br />
the tumor to the meso<strong>rectal</strong> fascia. Hence the phased array<br />
MRI is the best overall technique for local staging <strong>of</strong> <strong>rectal</strong><br />
<strong>cancer</strong>. Neoadjuvant treatment is not without risks; hence<br />
careful staging is important in obtaining good oncological<br />
and functional results and improving patient experience in<br />
the management <strong>of</strong> <strong>rectal</strong> <strong>cancer</strong>. In symptomatic patients<br />
local excision is beneficial in only 5% and this is the group<br />
which benefits most from EUS. With the introduction <strong>of</strong><br />
colo<strong>rectal</strong> screening it is felt nearly 50% <strong>of</strong> <strong>cancer</strong>s may be<br />
<strong>of</strong> early <strong>stage</strong> disease which can be identified by EUS and<br />
managed by organ preserving intervention. Hence the role<br />
<strong>of</strong> EUS is likely to increase as part <strong>of</strong> the staging investigations<br />
in future and all these investigations are complementary<br />
in the management <strong>of</strong> <strong>rectal</strong> <strong>cancer</strong>.<br />
ACKNOWLEDGMENTS<br />
The authors would like to thank Dr. M Tee, Consultant<br />
Radiologist, Mid Cheshire Hospitals NHS Foundation<br />
Trust for providing the images used in this manuscript.<br />
REFERENCES<br />
1 WHO, Cancer, fact sheet number 297, <strong>World</strong> Health Organization,<br />
Geneva. 2009<br />
2 Jemal A, Siegel R, Ward E, Hao Y, Xu J, Thun MJ. Cancer statistics,<br />
2009. CA Cancer J Clin 2009; 59: 225-249<br />
3 Cancer Research UK, By <strong>stage</strong> at diagnosis, Cancer Research<br />
UK, London. 2009<br />
4 Hayne D, Brown RS, McCormack M, Quinn MJ, Payne HA,<br />
Babb P. Current trends in colo<strong>rectal</strong> <strong>cancer</strong>: site, incidence,<br />
mortality and survival in England and Wales. Clin Oncol (R<br />
Coll Radiol) 2001; 13: 448-452<br />
5 Salerno G, Daniels IR, Moran BJ, Wotherspoon A, Brown G.<br />
Clarifying margins in the multidisciplinary management <strong>of</strong><br />
<strong>rectal</strong> <strong>cancer</strong>: the MERCURY experience. Clin Radiol 2006; 61:<br />
916-923<br />
6 Phillips RK, Hittinger R, Blesovsky L, Fry JS, Fielding LP.<br />
Local recurrence following 'curative' surgery for large bowel<br />
<strong>cancer</strong>: II. The rectum and rectosigmoid. Br J Surg 1984; 71:<br />
17-20<br />
7 Heald RJ. The 'Holy Plane' <strong>of</strong> <strong>rectal</strong> surgery. J R Soc Med<br />
1988; 81: 503-508<br />
8 Hospers GA, Punt CJ, Tesselaar ME, Cats A, Havenga K,<br />
Leer JW, Marijnen CA, Jansen EP, Van Krieken HH, Wiggers<br />
T, Van de Velde CJ, Mulder NH. Preoperative chemoradiotherapy<br />
with capecitabine and oxaliplatin in locally advanced<br />
<strong>rectal</strong> <strong>cancer</strong>. A phase I-II multicenter study <strong>of</strong> the Dutch<br />
Colo<strong>rectal</strong> Cancer Group. Ann Surg Oncol 2007; 14: 2773-2779<br />
9 Smith N, Brown G. Preoperative staging <strong>of</strong> <strong>rectal</strong> <strong>cancer</strong>. Acta<br />
Oncol 2008; 47: 20-31<br />
10 McSherry CK, Cornell GN, Glenn F. Carcinoma <strong>of</strong> the colon<br />
WJG|www.wjgnet.com<br />
Samee A et al . Current trends in staging <strong>rectal</strong> <strong>cancer</strong><br />
and rectum. Ann Surg 1969; 169: 502-509<br />
11 Tho LM, Glegg M, Paterson J, Yap C, MacLeod A, McCabe M,<br />
McDonald AC. Acute small bowel toxicity and preoperative<br />
chemoradiotherapy for <strong>rectal</strong> <strong>cancer</strong>: investigating dose-volume<br />
relationships and role for inverse planning. Int J Radiat<br />
Oncol Biol Phys 2006; 66: 505-513<br />
12 Beets-Tan RG, Beets GL, Borstlap AC, Oei TK, Teune TM,<br />
von Meyenfeldt MF, van Engelshoven JM. Preoperative assessment<br />
<strong>of</strong> local tumor extent in advanced <strong>rectal</strong> <strong>cancer</strong>: CT<br />
or high-resolution MRI? Abdom Imaging 2000; 25: 533-541<br />
13 Rifkin MD, Ehrlich SM, Marks G. Staging <strong>of</strong> <strong>rectal</strong> carcinoma:<br />
prospective comparison <strong>of</strong> endo<strong>rectal</strong> US and CT. Radiology<br />
1989; 170: 319-322<br />
14 Kwok H, Bissett IP, Hill GL. Preoperative staging <strong>of</strong> <strong>rectal</strong><br />
<strong>cancer</strong>. Int J Colo<strong>rectal</strong> Dis 2000; 15: 9-20<br />
15 Maizlin ZV, Brown JA, So G, Brown C, Phang TP, Walker<br />
ML, Kirby JM, Vora P, Tiwari P. Can CT replace MRI in preoperative<br />
assessment <strong>of</strong> the circumferential resection margin<br />
in <strong>rectal</strong> <strong>cancer</strong>? Dis Colon Rectum 2010; 53: 308-314<br />
16 Burling D. CT colonography standards. Clin Radiol 2010; 65:<br />
474-480<br />
17 Rosman AS, Korsten MA. Meta-analysis comparing CT colonography,<br />
air contrast barium enema, and colonoscopy. Am J<br />
Med 2007; 120: 203-210.e4<br />
18 Taylor SA, Robinson C, Boone D, Honeyfield L, Halligan S.<br />
Polyp characteristics correctly annotated by computer-aided<br />
detection s<strong>of</strong>tware but ignored by reporting radiologists during<br />
CT colonography. Radiology 2009; 253: 715-723<br />
19 Halligan S, Lilford RJ, Wardle J, Morton D, Rogers P,<br />
Wooldrage K, Edwards R, Kanani R, Shah U, Atkin W. Design<br />
<strong>of</strong> a multicentre randomized trial to evaluate CT colonography<br />
versus colonoscopy or barium enema for diagnosis<br />
<strong>of</strong> colonic <strong>cancer</strong> in older symptomatic patients: the SIGGAR<br />
study. Trials 2007; 8: 32<br />
20 Guinet C, Buy JN, Ghossain MA, Sézeur A, Mallet A, Bigot<br />
JM, Vadrot D, Ecoiffier J. Comparison <strong>of</strong> magnetic resonance<br />
imaging and computed tomography in the preoperative staging<br />
<strong>of</strong> <strong>rectal</strong> <strong>cancer</strong>. Arch Surg 1990; 125: 385-388<br />
21 Brown G, Radcliffe AG, Newcombe RG, Dallimore NS,<br />
Bourne MW, Williams GT. Preoperative assessment <strong>of</strong> prognostic<br />
factors in <strong>rectal</strong> <strong>cancer</strong> using high-resolution magnetic<br />
resonance imaging. Br J Surg 2003; 90: 355-364<br />
22 Beets-Tan RG, Beets GL, Vliegen RF, Kessels AG, Van Boven<br />
H, De Bruine A, von Meyenfeldt MF, Baeten CG, van Engelshoven<br />
JM. Accuracy <strong>of</strong> magnetic resonance imaging in<br />
prediction <strong>of</strong> tumour-free resection margin in <strong>rectal</strong> <strong>cancer</strong><br />
surgery. Lancet 2001; 357: 497-504<br />
23 Diagnostic accuracy <strong>of</strong> preoperative magnetic resonance<br />
imaging in predicting curative resection <strong>of</strong> <strong>rectal</strong> <strong>cancer</strong>: prospective<br />
observational study. BMJ 2006; 333: 779<br />
24 Brown G. Thin section MRI in multidisciplinary pre-operative<br />
decision making for patients with <strong>rectal</strong> <strong>cancer</strong>. Br J Radiol<br />
2005; 78 Spec No 2: S117-S127<br />
25 Taylor FG, Swift RI, Blomqvist L, Brown G. A systematic approach<br />
to the interpretation <strong>of</strong> preoperative staging MRI for<br />
<strong>rectal</strong> <strong>cancer</strong>. AJR Am J Roentgenol 2008; 191: 1827-1835<br />
26 Hussain SM, Outwater EK, Siegelman ES. Mucinous versus<br />
nonmucinous <strong>rectal</strong> carcinomas: differentiation with MR imaging.<br />
Radiology 1999; 213: 79-85<br />
27 Vliegen RF, Beets GL, von Meyenfeldt MF, Kessels AG, Lemaire<br />
EE, van Engelshoven JM, Beets-Tan RG. Rectal <strong>cancer</strong>:<br />
MR imaging in local staging--is gadolinium-based contrast<br />
material helpful? Radiology 2005; 234: 179-188<br />
28 Brown G, Richards CJ, Newcombe RG, Dallimore NS, Radcliffe<br />
AG, Carey DP, Bourne MW, Williams GT. Rectal carcinoma:<br />
thin-section MR imaging for staging in 28 patients.<br />
Radiology 1999; 211: 215-222<br />
29 Chen CC, Lee RC, Lin JK, Wang LW, Yang SH. How accurate<br />
is magnetic resonance imaging in restaging <strong>rectal</strong> <strong>cancer</strong> in<br />
patients receiving preoperative combined chemoradiotherapy?<br />
Dis Colon Rectum 2005; 48: 722-728<br />
30 Ross A, Rusnak C, Weinerman B, Kuechler P, Hayashi A,<br />
833 February 21, 2011|Volume 17|Issue 7|
Samee A et al . Current trends in staging <strong>rectal</strong> <strong>cancer</strong><br />
MacLachlan G, Frew E, Dunlop W. Recurrence and survival<br />
after surgical management <strong>of</strong> <strong>rectal</strong> <strong>cancer</strong>. Am J Surg 1999;<br />
177: 392-395<br />
31 Talbot IC, Ritchie S, Leighton MH, Hughes AO, Bussey HJ,<br />
Morson BC. The clinical significance <strong>of</strong> invasion <strong>of</strong> veins by<br />
<strong>rectal</strong> <strong>cancer</strong>. Br J Surg 1980; 67: 439-442<br />
32 Smith NJ, Shihab O, Arnaout A, Swift RI, Brown G. MRI for<br />
detection <strong>of</strong> extramural vascular invasion in <strong>rectal</strong> <strong>cancer</strong>.<br />
AJR Am J Roentgenol 2008; 191: 1517-1522<br />
33 Dzik-Jurasz A, Domenig C, George M, Wolber J, Padhani A,<br />
Brown G, Doran S. Diffusion MRI for prediction <strong>of</strong> response<br />
<strong>of</strong> <strong>rectal</strong> <strong>cancer</strong> to chemoradiation. Lancet 2002; 360: 307-308<br />
34 Hünerbein M, Pegios W, Rau B, Vogl TJ, Felix R, Schlag PM.<br />
Prospective comparison <strong>of</strong> endo<strong>rectal</strong> ultrasound, three-dimensional<br />
endo<strong>rectal</strong> ultrasound, and endo<strong>rectal</strong> MRI in the<br />
preoperative evaluation <strong>of</strong> <strong>rectal</strong> tumors. Preliminary results.<br />
Surg Endosc 2000; 14: 1005-1009<br />
35 Koh DM, Brown G, Temple L, Raja A, Toomey P, Bett N,<br />
Norman AR, Husband JE. Rectal <strong>cancer</strong>: meso<strong>rectal</strong> lymph<br />
nodes at MR imaging with USPIO versus histopathologic<br />
findings--initial observations. Radiology 2004; 231: 91-99<br />
36 Grace RH, Hale M, Mackie G, Marks CG, Bloomberg TJ,<br />
Walker WJ. Role <strong>of</strong> ultrasound in the diagnosis <strong>of</strong> liver metastases<br />
before surgery for large bowel <strong>cancer</strong>. Br J Surg 1987;<br />
74: 480-481<br />
37 Rafaelsen SR, Kronborg O, Larsen C, Fenger C. Intraoperative<br />
ultrasonography in detection <strong>of</strong> hepatic metastases from<br />
colo<strong>rectal</strong> <strong>cancer</strong>. Dis Colon Rectum 1995; 38: 355-360<br />
38 Akasu T, Kondo H, Moriya Y, Sugihara K, Gotoda T, Fujita<br />
S, Muto T, Kakizoe T. Endo<strong>rectal</strong> ultrasonography and<br />
treatment <strong>of</strong> early <strong>stage</strong> <strong>rectal</strong> <strong>cancer</strong>. <strong>World</strong> J Surg 2000; 24:<br />
1061-1068<br />
39 Garcia-Aguilar J, Pollack J, Lee SH, Hernandez de Anda E,<br />
Mellgren A, Wong WD, Finne CO, Rothenberger DA, Mad<strong>of</strong>f<br />
RD. Accuracy <strong>of</strong> endo<strong>rectal</strong> ultrasonography in preoperative<br />
staging <strong>of</strong> <strong>rectal</strong> tumors. Dis Colon Rectum 2002; 45: 10-15<br />
40 Gualdi GF, Casciani E, Guadalaxara A, d'Orta C, Polettini E,<br />
Pappalardo G. Local staging <strong>of</strong> <strong>rectal</strong> <strong>cancer</strong> with trans<strong>rectal</strong><br />
ultrasound and endo<strong>rectal</strong> magnetic resonance imaging:<br />
comparison with histologic findings. Dis Colon Rectum 2000;<br />
43: 338-345<br />
41 Hulsmans FJ, Tio TL, Fockens P, Bosma A, Tytgat GN. Assessment<br />
<strong>of</strong> tumor infiltration depth in <strong>rectal</strong> <strong>cancer</strong> with<br />
trans<strong>rectal</strong> sonography: caution is necessary. Radiology 1994;<br />
190: 715-720<br />
42 Rifkin MD, Ehrlich SM, Marks G. Staging <strong>of</strong> <strong>rectal</strong> carcinoma:<br />
prospective comparison <strong>of</strong> endo<strong>rectal</strong> US and CT. Radiology<br />
1989; 170: 319-322<br />
43 Bipat S, Glas AS, Slors FJ, Zwinderman AH, Bossuyt PM,<br />
Stoker J. Rectal <strong>cancer</strong>: local staging and assessment <strong>of</strong> lymph<br />
node involvement with endoluminal US, CT, and MR imaging--a<br />
meta-analysis. Radiology 2004; 232: 773-783<br />
44 Mackay SG, Pager CK, Joseph D, Stewart PJ, Solomon MJ.<br />
Assessment <strong>of</strong> the accuracy <strong>of</strong> trans<strong>rectal</strong> ultrasonography in<br />
ano<strong>rectal</strong> neoplasia. Br J Surg 2003; 90: 346-350<br />
45 Schaffzin DM, Wong WD. Endo<strong>rectal</strong> ultrasound in the<br />
preoperative evaluation <strong>of</strong> <strong>rectal</strong> <strong>cancer</strong>. Clin Colo<strong>rectal</strong> Cancer<br />
2004; 4: 124-132<br />
46 Solomon MJ, McLeod RS. Endoluminal trans<strong>rectal</strong> ultrasonography:<br />
accuracy, reliability, and validity. Dis Colon Rectum<br />
1993; 36: 200-205<br />
47 Skandarajah AR, Tjandra JJ. Preoperative loco-regional imaging<br />
in <strong>rectal</strong> <strong>cancer</strong>. ANZ J Surg 2006; 76: 497-504<br />
48 Bipat S, Glas AS, Slors FJ, Zwinderman AH, Bossuyt PM,<br />
Stoker J. Rectal <strong>cancer</strong>: local staging and assessment <strong>of</strong> lymph<br />
node involvement with endoluminal US, CT, and MR imaging--a<br />
meta-analysis. Radiology 2004; 232: 773-783<br />
WJG|www.wjgnet.com<br />
49 Lahaye MJ, Engelen SM, Nelemans PJ, Beets GL, van de<br />
Velde CJ, van Engelshoven JM, Beets-Tan RG. Imaging for<br />
predicting the risk factors--the circumferential resection margin<br />
and nodal disease--<strong>of</strong> local recurrence in <strong>rectal</strong> <strong>cancer</strong>: a<br />
meta-analysis. Semin Ultrasound CT MR 2005; 26: 259-268<br />
50 Garcia-Aguilar J, Pollack J, Lee SH, Hernandez de Anda E,<br />
Mellgren A, Wong WD, Finne CO, Rothenberger DA, Mad<strong>of</strong>f<br />
RD. Accuracy <strong>of</strong> endo<strong>rectal</strong> ultrasonography in preoperative<br />
staging <strong>of</strong> <strong>rectal</strong> tumors. Dis Colon Rectum 2002; 45: 10-15<br />
51 Rieger N, Tjandra J, Solomon M. Endoanal and endo<strong>rectal</strong> ultrasound:<br />
applications in colo<strong>rectal</strong> surgery. ANZ J Surg 2004;<br />
74: 671-675<br />
52 Zammit M, Jenkins JT, Urie A, O'Dwyer PJ, Molloy RG. A<br />
technically difficult endo<strong>rectal</strong> ultrasound is more likely to be<br />
inaccurate. Colo<strong>rectal</strong> Dis 2005; 7: 486-491<br />
53 Akasu T, Sugihara K, Moriya Y, Fujita S. Limitations and<br />
pitfalls <strong>of</strong> trans<strong>rectal</strong> ultrasonography for staging <strong>of</strong> <strong>rectal</strong><br />
<strong>cancer</strong>. Dis Colon Rectum 1997; 40: S10-S15<br />
54 Saftoiu A, Gheonea DI. Tridimensional (3D) endoscopic ultrasound<br />
- a pictorial review. J Gastrointestin Liver Dis 2009;<br />
18: 501-505<br />
55 Strauss LG. Fluorine-18 deoxyglucose and false-positive<br />
results: a major problem in the diagnostics <strong>of</strong> oncological patients.<br />
Eur J Nucl Med 1996; 23: 1409-1415<br />
56 Cho YB, Chun HK, Kim MJ, Choi JY, Park CM, Kim BT, Lee<br />
SJ, Yun SH, Kim HC, Lee WY. Accuracy <strong>of</strong> MRI and 18F-FDG<br />
PET/CT for restaging after preoperative concurrent chemoradiotherapy<br />
for <strong>rectal</strong> <strong>cancer</strong>. <strong>World</strong> J Surg 2009; 33: 2688-2694<br />
57 Joyce DL, Wahl RL, Patel PV, Schulick RD, Gearhart SL,<br />
Choti MA. Preoperative positron emission tomography to<br />
evaluate potentially resectable hepatic colo<strong>rectal</strong> metastases.<br />
Arch Surg 2006; 141: 1220-1226; discussion 1227<br />
58 Heriot AG, Hicks RJ, Drummond EG, Keck J, Mackay J, Chen<br />
F, Kalff V. Does positron emission tomography change management<br />
in primary <strong>rectal</strong> <strong>cancer</strong>? A prospective assessment.<br />
Dis Colon Rectum 2004; 47: 451-458<br />
59 Gearhart SL, Frassica D, Rosen R, Choti M, Schulick R, Wahl<br />
R. Improved staging with pretreatment positron emission tomography/computed<br />
tomography in low <strong>rectal</strong> <strong>cancer</strong>. Ann<br />
Surg Oncol 2006; 13: 397-404<br />
60 Maor Y, Nadler M, Barshack I, Zmora O, Koller M, Kundel Y,<br />
Fidder H, Bar-Meir S, Avidan B. Endoscopic ultrasound staging<br />
<strong>of</strong> <strong>rectal</strong> <strong>cancer</strong>: diagnostic value before and following<br />
chemoradiation. J Gastroenterol Hepatol 2006; 21: 454-458<br />
61 Denecke T, Rau B, H<strong>of</strong>fmann KT, Hildebrandt B, Ruf J, Gutberlet<br />
M, Hünerbein M, Felix R, Wust P, Amthauer H. Comparison<br />
<strong>of</strong> CT, MRI and FDG-PET in response prediction <strong>of</strong><br />
patients with locally advanced <strong>rectal</strong> <strong>cancer</strong> after multimodal<br />
preoperative therapy: is there a benefit in using functional<br />
imaging? Eur Radiol 2005; 15: 1658-1666<br />
62 Kim JH, Beets GL, Kim MJ, Kessels AG, Beets-Tan RG. Highresolution<br />
MR imaging for nodal staging in <strong>rectal</strong> <strong>cancer</strong>: are<br />
there any criteria in addition to the size? Eur J Radiol 2004; 52:<br />
78-83<br />
63 Brown G, Richards CJ, Bourne MW, Newcombe RG, Radcliffe<br />
AG, Dallimore NS, Williams GT. Morphologic predictors<br />
<strong>of</strong> lymph node status in <strong>rectal</strong> <strong>cancer</strong> with use <strong>of</strong> highspatial-resolution<br />
MR imaging with histopathologic comparison.<br />
Radiology 2003; 227: 371-377<br />
64 O'Neill BD, Brown G, Heald RJ, Cunningham D, Tait DM.<br />
Non-operative treatment after neoadjuvant chemoradiotherapy<br />
for <strong>rectal</strong> <strong>cancer</strong>. Lancet Oncol 2007; 8: 625-633<br />
65 Habr-Gama A, Perez RO, Nadalin W, Sabbaga J, Ribeiro U Jr,<br />
Silva e Sousa AH Jr, Campos FG, Kiss DR, Gama-Rodrigues<br />
J. Operative versus nonoperative treatment for <strong>stage</strong> 0 distal<br />
<strong>rectal</strong> <strong>cancer</strong> following chemoradiation therapy: long-term<br />
results. Ann Surg 2004; 240: 711-717; discussion 717-718<br />
S- Editor Sun H L- Editor O’Neill M E- Editor Ma WH<br />
834 February 21, 2011|Volume 17|Issue 7|
Ronnekleiv-Kelly SM et al . Palliation in <strong>rectal</strong> <strong>cancer</strong><br />
aggressive operative intervention is warranted can ensure<br />
the most appropriate treatment strategy is devised. The<br />
goals in palliation should include the alleviation <strong>of</strong> symptoms,<br />
enhancing quality <strong>of</strong> life and improving comfort [5] .<br />
Herein, we review the current relevant literature on various<br />
treatment strategies as they are related to the palliative<br />
treatment <strong>of</strong> <strong>rectal</strong> <strong>cancer</strong>.<br />
EVALUATION<br />
Rectal <strong>cancer</strong> is defined as a malignant lesion within 15 cm<br />
<strong>of</strong> the anal verge as seen by rigid proctoscopy [6-8] . Subsequent<br />
to histological confirmation <strong>of</strong> diagnosis via tumor<br />
biopsy, initial work-up <strong>of</strong> the extent <strong>of</strong> disease guides<br />
subsequent treatment [4,9] . Proper staging is essential as decisions<br />
regarding neoadjuvant versus adjuvant therapy and<br />
operative versus palliative surgical intent will be based on<br />
clinical <strong>stage</strong>. The patient should undergo proctoscopy to<br />
determine distance from anal verge, as well as colonoscopy<br />
to interrogate the entire colon for synchronous lesions.<br />
Cross-sectional imaging <strong>of</strong> the chest, abdomen and pelvis<br />
in conjunction with endoscopic ultrasound (EUS) can<br />
assess depth <strong>of</strong> tumor penetration or invasion <strong>of</strong> local<br />
structures, lymph node status, and presence <strong>of</strong> metastatic<br />
disease [9,10] . Although EUS has appropriate sensitivity and<br />
specificity for differentiating muscularis propria invasion<br />
(94% and 86%), as well as peri<strong>rectal</strong> tissue invasion (90%<br />
and 75%), magnetic resonance imaging (MRI) has proven<br />
to be an important adjunct for accurate staging <strong>of</strong> <strong>rectal</strong><br />
<strong>cancer</strong> as well [9,11,12] . MRI has been found to have an 85%<br />
diagnostic accuracy for T-<strong>stage</strong> with 57%-85% accuracy for<br />
correctly identifying spread to lymph nodes; furthermore,<br />
the relationship to meso<strong>rectal</strong> fascia in conjunction with detection<br />
<strong>of</strong> adjacent organ invasion is superior utilizing MRI<br />
versus EUS [13-18] . In addition to imaging, a preoperative<br />
carcinoembryonic antigen level combined with basic laboratory<br />
values, comprehensive history and complete physical<br />
examination to assess performance status and comorbidity<br />
play important roles in the preoperative workup, because<br />
these factor significantly for choice <strong>of</strong> intervention [19] .<br />
When the pretreatment evaluation has determined a<br />
patient to no longer be appropriate for curative intent due<br />
to the presence <strong>of</strong> distant metastases or local invasion<br />
precluding a margin-negative resection, quality <strong>of</strong> life and<br />
symptom relief must become the main focus. In general,<br />
findings indicative <strong>of</strong> unresectability are utilized to predict<br />
the ability to achieve resection with negative margins. In<br />
those situations presented in Table 1, negative margins<br />
are obtained in 6%-36% <strong>of</strong> cases and surgical extirpation<br />
can result in significant postoperative disability [20] . However,<br />
resectability <strong>of</strong> the disease should be assessed by an<br />
experienced surgeon. In a study by Mathis et al [21] , patients<br />
who were initially deemed locally unresectable, secondary<br />
to advanced primary colon and <strong>rectal</strong> <strong>cancer</strong>, were<br />
treated with aggressive multimodal therapy and found to<br />
have median survival <strong>of</strong> 3.7 years. Conversely, decision<br />
stratification must be influenced by expected survival in<br />
those patients evaluated properly and determined not to<br />
be candidates for aggressive resection. Consideration <strong>of</strong><br />
WJG|www.wjgnet.com<br />
Table 1 Contraindications to resective operative intervention<br />
Sciatic nerve pain<br />
Bilateral ureteral obstruction<br />
Extensive fixation to lateral pelvic side wall (CT/MRI or trial dissection)<br />
Sacral involvement above S2 (resection produces spinal instability or<br />
post-operative complications)<br />
Bilateral lymphedema or bilateral venous thrombosis (indicating<br />
encasement <strong>of</strong> major vascular structures)<br />
Multiple peritoneal metastasis or metastasis fixed to or invading vital<br />
structures<br />
CT: Computed tomography; MRI: Magnetic resonance imaging.<br />
operative interventions is more appropriately included in<br />
the conversation <strong>of</strong> palliative treatment for patients with<br />
expected outcomes exceeding 6 mo [19,22-25] .<br />
Approximately 50% <strong>of</strong> patients either present with<br />
distant metastases or develop distant metastases after primary<br />
treatment. Those that cannot be treated curatively<br />
should have care guided by patient wishes, functional<br />
status, expected life duration, and extent <strong>of</strong> disease and<br />
debilitating symptoms. In a study by Law et al [26] , the most<br />
common presenting symptoms <strong>of</strong> patients undergoing<br />
palliative intervention for colo<strong>rectal</strong> <strong>cancer</strong> were intestinal<br />
obstruction and <strong>rectal</strong> bleeding. In another study, 42% <strong>of</strong><br />
patients presenting for palliative treatment were obstructed,<br />
37% <strong>of</strong> patients experienced <strong>rectal</strong> bleeding, and 5%<br />
were asymptomatic, with the remainder (16%) experiencing<br />
pain or <strong>rectal</strong> discharge [27] . Taking into consideration<br />
the presenting symptoms and the underlying condition<br />
<strong>of</strong> the patient, palliative management can be divided into<br />
operative versus non-operative treatment.<br />
CLINICAL SCENARIOS AND<br />
MANAGEMENT OPTIONS<br />
Obstruction<br />
Patients with <strong>rectal</strong> <strong>cancer</strong> can present with any number<br />
<strong>of</strong> symptoms that prompt evaluation (e.g. bleeding,<br />
perforation, abdominal pain, anemia, hematochezia,<br />
tenesmus, and malaise) and 10%-25% <strong>of</strong> patients present<br />
with obstructive symptoms [19,22,26,28] . Such a clinical<br />
scenario requires expedient yet thorough evaluation <strong>of</strong><br />
the patient for resectability and potential for cure, because<br />
these patients <strong>of</strong>ten necessitate urgent, if not emergency,<br />
surgical intervention [28] . Rosen retrospectively analyzed<br />
116 patients initially presenting with <strong>stage</strong> IV colo<strong>rectal</strong><br />
<strong>cancer</strong> and found that 26% presented with obstructive<br />
symptoms [22] . In another study, although the most common<br />
symptom precipitating medical evaluation in advanced<br />
colo<strong>rectal</strong> <strong>cancer</strong> was bleeding (24%), Law et al [26]<br />
found that obstruction (23%) in conjunction with change<br />
in bowel habits (15%) comprised a significant proportion<br />
<strong>of</strong> patient presentations. Phang et al [29] found that nearly<br />
10% <strong>of</strong> patients with <strong>rectal</strong> <strong>cancer</strong> presented with a bowel<br />
obstruction and required some emergency intervention.<br />
In that series, patients who underwent primary resection<br />
<strong>of</strong> the tumor at the time <strong>of</strong> emergency surgery had<br />
836 February 21, 2011|Volume 17|Issue 7|
Online Submissions: http://www.wjgnet.com/1007-9327<strong>of</strong>fice<br />
wjg@wjgnet.com<br />
doi:10.3748/wjg.v17.i7.848<br />
Imran Hassan, MD, Assistant Pr<strong>of</strong>essor, Series Editor<br />
Neoadjuvant vs adjuvant pelvic radiotherapy for locally<br />
advanced <strong>rectal</strong> <strong>cancer</strong>: Which is superior?<br />
Sarah Popek, Vassiliki Liana Tsikitis<br />
Sarah Popek, Vassiliki Liana Tsikitis, Department <strong>of</strong> Surgery,<br />
University <strong>of</strong> Arizona, Tucson, AZ 85724, United States<br />
Author contributions: All authors contributed equally to this<br />
work; all authors analyzed the data and wrote the paper.<br />
Correspondence to: Vassiliki Liana Tsikitis, MD, Assistant<br />
Pr<strong>of</strong>essor, Department <strong>of</strong> Surgery, University <strong>of</strong> Arizona, 1515<br />
N Campbell Ave, Tucson, AZ 85724,<br />
United States. ltsikitis@surgery.arizona.edu<br />
Telephone: +1-520-6266788 Fax: +1-520-6262191<br />
Received: August 30, 2010 Revised: September 29, 2010<br />
Accepted: October 6, 2010<br />
Published online: February 21, 2011<br />
Abstract<br />
The treatment <strong>of</strong> locally advanced <strong>rectal</strong> <strong>cancer</strong> including<br />
timing and dosage <strong>of</strong> radiotherapy, degree <strong>of</strong><br />
sphincter preservation with neoadjuvant radiotherapy,<br />
and short and long term effects <strong>of</strong> radiotherapy are controversial<br />
topics. The MEDLINE, Cochrane Library databases,<br />
and meeting proceedings from the American Society<br />
<strong>of</strong> Clinical Oncology, were searched for reports <strong>of</strong><br />
randomized controlled trials and meta-analyses comparing<br />
neoadjuvant and adjuvant radiotherapy with surgery<br />
to surgery alone for <strong>rectal</strong> <strong>cancer</strong>. Neoadjuvant radiotherapy<br />
shows superior results in terms <strong>of</strong> local control<br />
compared to adjuvant radiotherapy. Neither adjuvant<br />
or neoadjuvant radiotherapy impacts overall survival.<br />
Short course versus long course neoadjuvant radiotherapy<br />
remains controversial. There is insufficient data<br />
to conclude that neoadjuvant therapy improves rates<br />
<strong>of</strong> sphincter preserving surgery. Radiation significantly<br />
impacts ano<strong>rectal</strong> and sexual function and includes both<br />
acute and long term toxicity. Data demonstrate that<br />
neoadjuvant radiation causes less toxicity compared<br />
to adjuvant radiotherapy, and specifically short course<br />
neoadjuvant radiation results in less toxicity than long<br />
course neoadjuvant radiation. Neoadjuvant radiotherapy<br />
is the preferred modality for administering radiation in<br />
WJG|www.wjgnet.com<br />
<strong>World</strong> J Gastroenterol 2011 February 21; 17(7): 848-854<br />
ISSN 1007-9327 (print) ISSN 2219-2840 (online)<br />
© 2011 Baishideng. All rights reserved.<br />
locally advanced <strong>rectal</strong> <strong>cancer</strong>. There are significant side<br />
effects from radiation, including ano<strong>rectal</strong> and sexual<br />
dysfunction, which may be less with short course neoadjuvant<br />
radiation.<br />
© 2011 Baishideng. All rights reserved.<br />
Key words: Locally advanced <strong>rectal</strong> <strong>cancer</strong>; Neoadjuvant<br />
radiation; Adjuvant radiation; Rectal neoplasm;<br />
Chemoradiotherapy; Neoadjuvant chemoradiotherapy<br />
Peer reviewer: Paul E Sijens, PhD, Associate Pr<strong>of</strong>essor, Radiology,<br />
UMCG, Hanzeplein 1, 9713GZ Groningen, The Netherlands<br />
Popek S, Tsikitis VL. Neoadjuvant vs adjuvant pelvic radiotherapy<br />
for locally advanced <strong>rectal</strong> <strong>cancer</strong>: Which is superior?<br />
<strong>World</strong> J Gastroenterol 2011; 17(7): 848-854 Available from:<br />
URL: http://www.wjgnet.com/1007-9327/full/v17/i7/848.htm<br />
DOI: http://dx.doi.org/10.3748/wjg.v17.i7.848<br />
INTRODUCTION<br />
TOPIC HIGHLIGHT<br />
Colo<strong>rectal</strong> <strong>cancer</strong> is the third most frequent <strong>cancer</strong> in men<br />
and women. In 2009, in the United States 40 000 new cases<br />
<strong>of</strong> <strong>rectal</strong> <strong>cancer</strong> alone were diagnosed [1] . The past 2 decades<br />
have seen many advances in the treatment <strong>of</strong> patients with<br />
<strong>rectal</strong> <strong>cancer</strong>. Surgery remains the mainstay. The standard <strong>of</strong><br />
surgical care now includes total meso<strong>rectal</strong> excision (TME),<br />
which was shown to significantly decrease local recurrence<br />
rates [2] . Evolution <strong>of</strong> Combined Modality Treatment<br />
(CMT) revolutionized care <strong>of</strong> locally advanced <strong>rectal</strong> <strong>cancer</strong><br />
with the most considerable change the introduction<br />
<strong>of</strong> pelvic radiation. Improvements in preoperative staging<br />
with endo<strong>rectal</strong> ultrasound and magnetic resonance imaging<br />
have allowed experimentation with different regimens<br />
<strong>of</strong> neoadjuvant (preoperative) and adjuvant (postoperative)<br />
radiotherapy (RT).<br />
The goals <strong>of</strong> this review are to provide a critical over-<br />
848 February 21, 2011|Volume 17|Issue 7|
Popek S et al . Neoadjuvant vs adjuvant radiotherapy for <strong>rectal</strong> <strong>cancer</strong><br />
61% <strong>of</strong> patients in the RT arm and 58% in the CMT arm<br />
underwent sphincter-preserving surgery (P = 0.57). In<br />
conclusion, although short-course RT improves local control,<br />
no strong evidence exists that it also improves rates<br />
<strong>of</strong> sphincter-preserving surgery indicating short-course<br />
neoadjuvant RT does not have a significant effect on preoperative<br />
tumor downsizing or downstaging.<br />
A significant benefit <strong>of</strong> neoadjuvant RT is patient compliance<br />
with treatment. Adjuvant RT has been associated<br />
with higher rates <strong>of</strong> treatment interruption. Lebwohl et al [25]<br />
assessed for principle factors associated with treatment interruption<br />
in 113 RT patients. Patients in the adjuvant arm<br />
had a significantly increased chance <strong>of</strong> RT interruption, as<br />
compared with the neoadjuvant RT arm (OR, 14.08, CI:<br />
1.55-127.87). Development <strong>of</strong> an adverse event was also<br />
significantly correlated with RT interruption (OR, 20.66,<br />
CI: 1.76-242).<br />
ANORECTAL FUNCTION OUTCOMES<br />
One <strong>of</strong> the most important variables evaluating quality<br />
<strong>of</strong> life in <strong>rectal</strong> <strong>cancer</strong> is ano<strong>rectal</strong> function, specifically<br />
bowel function and sexual function [26] . This is affected by<br />
both chemoradiation and surgical technique. The Dutch<br />
colo<strong>rectal</strong> group assessed ano<strong>rectal</strong> functional outcomes<br />
after short-course preoperative RT and TME and found<br />
significant differences between patients who did vs did<br />
not undergo RT [27] . RT patients had higher rates <strong>of</strong> fecal<br />
incontinence (62% with RT vs 38% without, P < 0.001),<br />
pad wearing as a result <strong>of</strong> incontinence (56% vs 33%, P<br />
< 0.001), and anal blood loss (11% vs 3%, P = 0.004). RT<br />
patients also reported significantly lower satisfaction with<br />
bowel function.<br />
A second prospective study randomized 316 patients to<br />
(1) short-course neoadjuvant RT or (2) long-course neoadjuvant<br />
chemoradiation [26] . The goal was to evaluate ano<strong>rectal</strong><br />
and sexual dysfunction and quality <strong>of</strong> life. Early complications<br />
were more common in the chemoradiation arm, but<br />
no significant differences were found in the degree <strong>of</strong> ano<strong>rectal</strong><br />
and sexual function or in quality <strong>of</strong> life.<br />
In addition to bowel and sexual dysfunction, RT patients<br />
may experience acute and late RT toxicity, including<br />
nausea/vomiting, postoperative hernia, femoral neck<br />
fracture, skin problems (nonhealing perineal wounds), ileus,<br />
anastomotic stricture, and fistula. The Dutch colo<strong>rectal</strong><br />
group assessed RT toxicity, intraoperative and postoperative<br />
complications, and other variables in patients who<br />
underwent short-course neoadjuvant RT vs TME alone [27] .<br />
No differences were found in operative time, intraoperative<br />
complications, or hospital stay; however, the amount<br />
<strong>of</strong> intraoperative blood loss was higher in the RT arm<br />
(P < 0.001). Rates <strong>of</strong> perineal complications were also<br />
higher (29% with RT vs 18% with TME alone, P = 0.008).<br />
But no significant differences were found in the rate <strong>of</strong><br />
abdominal wound complications (4.0% with RT vs 3.3%<br />
with TME alone) or in the overall postoperative mortality<br />
rate.<br />
Frykholm et al [28] looked at long-term complications<br />
WJG|www.wjgnet.com<br />
(minimum follow-up time, 5 years) after either neoadjuvant<br />
short-course RT (n = 255) or adjuvant long-course<br />
RT (n = 127), as compared with surgery alone (control<br />
group, n = 82). Long-term complications (defined as occurring<br />
at least 6 mo postoperatively) included recurrent<br />
abdominal pain, diarrhea, fecal incontinence, ileus, cystitis,<br />
paresthesias, delayed wound healing, and any neurologic<br />
dysfunction. The percentage <strong>of</strong> patients with small bowel<br />
obstruction did not significantly differ between the neoadjuvant<br />
RT group and control group. In the adjuvant<br />
RT group, the risk <strong>of</strong> developing a small bowel obstruction<br />
was significantly higher (P < 0.01). Overall, the frequency<br />
<strong>of</strong> complications possibly related to RT in the<br />
neoadjuvant group was 20%; in the adjuvant group, 41%.<br />
However, in the control group, the percentage <strong>of</strong> similar<br />
complications was 23%. In addition to finding a significant<br />
decrease in local recurrence after neoadjuvant shortcourse<br />
RT (13% in the neoadjuvant group vs 22% in the<br />
adjuvant group, P = 0.02), the cumulative risk <strong>of</strong> bowel<br />
obstruction was significantly higher in the adjuvant group.<br />
Minsky et al [29] also demonstrated significantly lower<br />
rates <strong>of</strong> adverse events and improved compliance in patients<br />
treated with neoadjuvant CMT compared to patients<br />
treated with adjuvant CMT. Despite receiving higher doses<br />
<strong>of</strong> chemotherapy, the neoadjuvant arm experienced a<br />
13% incidence <strong>of</strong> acute grade 3 or 4 toxicity compared to<br />
a 48% incidence in the adjuvant arm (P = 0.045). A metaanalysis<br />
by Birgisson et al [30] found that the most common<br />
late adverse effects <strong>of</strong> RT were bowel obstruction, bowel<br />
dysfunction (fecal incontinence), and sexual dysfunction.<br />
Several different RT regimens were included in the metaanalysis,<br />
<strong>of</strong>fering some insight into how complications<br />
correlated with dosage. Overall, in the more recent studies<br />
which used lower doses and better techniques, the rates<br />
<strong>of</strong> adverse events were lower. Unfortunately, to date, no<br />
specific markers have been identified that might help predict<br />
which patients have a higher risk <strong>of</strong> acute RT toxicity.<br />
Further work is needed in this important area <strong>of</strong> ongoing<br />
research.<br />
CONCLUSION<br />
Patients with locally advanced <strong>rectal</strong> <strong>cancer</strong> clearly benefit,<br />
in terms <strong>of</strong> locoregional control, from both neoadjuvant<br />
and adjuvant RT; and patient compliance is better with<br />
neoadjuvant RT. No definitive evidence demonstrates the<br />
superiority <strong>of</strong> using short vs long-course RT.<br />
The current standard treatment for patients with locally<br />
advanced <strong>rectal</strong> <strong>cancer</strong> in the United States consists <strong>of</strong><br />
neoadjuvant radiation (45 to 55 Gy administered over 5 to<br />
6 wk), followed by neoadjuvant chemotherapy (5-FU-based<br />
infusion + leucovorin), surgery 6 to 8 wk after completion<br />
<strong>of</strong> chemotherapy, and additional adjuvant chemotherapy<br />
after surgery [31] . In contrast, the standard regimen in most<br />
<strong>of</strong> Europe is now neoadjuvant short-course RT. The<br />
most recent European Rectal Cancer Consensus Conference<br />
concluded that neoadjuvant short-course RT (25 Gy<br />
administered over 1 wk), especially when combined with<br />
852 February 21, 2011|Volume 17|Issue 7|
Popek S et al . Neoadjuvant vs adjuvant radiotherapy for <strong>rectal</strong> <strong>cancer</strong><br />
Oncol 2007; 84: 217-225<br />
27 Peeters KC, van de Velde CJ, Leer JW, Martijn H, Junggeburt<br />
JM, Kranenbarg EK, Steup WH, Wiggers T, Rutten HJ, Marijnen<br />
CA. Late side effects <strong>of</strong> short-course preoperative radiotherapy<br />
combined with total meso<strong>rectal</strong> excision for <strong>rectal</strong><br />
<strong>cancer</strong>: increased bowel dysfunction in irradiated patients-<br />
-a Dutch colo<strong>rectal</strong> <strong>cancer</strong> group study. J Clin Oncol 2005; 23:<br />
6199-6206<br />
28 Frykholm GJ, Glimelius B, Påhlman L. Preoperative or postoperative<br />
irradiation in adenocarcinoma <strong>of</strong> the rectum: final<br />
treatment results <strong>of</strong> a randomized trial and an evaluation <strong>of</strong><br />
late secondary effects. Dis Colon Rectum 1993; 36: 564-572<br />
29 Minsky BD, Cohen AM, Kemeny N, Enker WE, Kelsen DP,<br />
Reichman B, Saltz L, Sigurdson ER, Frankel J. Combined modality<br />
therapy <strong>of</strong> <strong>rectal</strong> <strong>cancer</strong>: decreased acute toxicity with<br />
WJG|www.wjgnet.com<br />
the preoperative approach. J Clin Oncol 1992; 10: 1218-1224<br />
30 Birgisson H, Påhlman L, Gunnarsson U, Glimelius B. Late<br />
adverse effects <strong>of</strong> radiation therapy for <strong>rectal</strong> <strong>cancer</strong> - a systematic<br />
overview. Acta Oncol 2007; 46: 504-516<br />
31 Wong RK, Tandan V, De Silva S, Figueredo A. Pre-operative<br />
radiotherapy and curative surgery for the management <strong>of</strong><br />
localized <strong>rectal</strong> carcinoma. Cochrane Database Syst Rev 2007;<br />
CD002102<br />
32 Valentini V, Aristei C, Glimelius B, Minsky BD, Beets-Tan R,<br />
Borras JM, Haustermans K, Maingon P, Overgaard J, Pahlman<br />
L, Quirke P, Schmoll HJ, Sebag-Montefiore D, Taylor I,<br />
Van Cutsem E, Van de Velde C, Cellini N, Latini P. Multidisciplinary<br />
Rectal Cancer <strong>Management</strong>: 2nd European Rectal<br />
Cancer Consensus Conference (EURECA-CC2). Radiother<br />
Oncol 2009; 92: 148-163<br />
S- Editor Sun H L- Editor O’Neill M E- Editor Zheng XM<br />
854 February 21, 2011|Volume 17|Issue 7|
Online Submissions: http://www.wjgnet.com/1007-9327<strong>of</strong>fice<br />
wjg@wjgnet.com<br />
doi:10.3748/wjg.v17.i7.855<br />
Imran Hassan, MD, Assistant Pr<strong>of</strong>essor, Series Editor<br />
Sphincter preservation for distal <strong>rectal</strong> <strong>cancer</strong> - a goal<br />
worth achieving at all costs?<br />
Jürgen Mulsow, Des C Winter<br />
Jürgen Mulsow, Des C Winter, Institute for Clinical Outcomes<br />
Research and Education, St. Vincent’s University Hospital,<br />
Elm Park, Dublin 4, Ireland<br />
Author contributions: Mulsow J and Winter DC both contributed<br />
to the literature review and drafting <strong>of</strong> manuscript.<br />
Correspondence to: Des C Winter, Pr<strong>of</strong>essor, Institute for<br />
Clinical Outcomes Research and Education, St. Vincent’s University<br />
Hospital, Elm Park, Dublin 4, Ireland. winterd@indigo.ie<br />
Telephone: +353-1-2695033 Fax: +353-1-2609249<br />
Received: August 30, 2010 Revised: January 18, 2011<br />
Accepted: January 25, 2011<br />
Published online: February 21, 2011<br />
Abstract<br />
To assess the merits <strong>of</strong> currently available treatment<br />
options in the management <strong>of</strong> patients with low <strong>rectal</strong><br />
<strong>cancer</strong>, a review <strong>of</strong> the medical literature pertaining to<br />
the operative and non-operative management <strong>of</strong> low<br />
<strong>rectal</strong> <strong>cancer</strong> was performed, with particular emphasis<br />
on sphincter preservation, oncological outcome,<br />
functional outcome, morbidity, quality <strong>of</strong> life, and patient<br />
preference. Low anterior resection (AR) is technically<br />
feasible in an increasing proportion <strong>of</strong> patients with<br />
low <strong>rectal</strong> <strong>cancer</strong>. The cost <strong>of</strong> sphincter preservation<br />
is the risk <strong>of</strong> morbidity and poor functional outcome<br />
in a significant proportion <strong>of</strong> patients. Transanal and<br />
endoscopic surgery are attractive options in selected<br />
patients that can provide satisfactory oncological<br />
outcomes while avoiding the morbidity and functional<br />
sequelae <strong>of</strong> open total meso<strong>rectal</strong> excision. In complete<br />
responders to neo-adjuvant chemoradiotherapy, a<br />
non-operative approach may prove to be an option.<br />
Abdominoperineal excision (APE) imposes a permanent<br />
stoma and is associated with significant incidence <strong>of</strong><br />
perineal morbidity but avoids the risk <strong>of</strong> poor functional<br />
outcome following AR. Quality <strong>of</strong> life following AR and<br />
APE is comparable. Given the choice, most patients will<br />
choose AR over APE, however patients following APE<br />
positively appraise this option. In striving toward sphinc-<br />
WJG|www.wjgnet.com<br />
855<br />
<strong>World</strong> J Gastroenterol 2011 February 21; 17(7): 855-861<br />
ISSN 1007-9327 (print) ISSN 2219-2840 (online)<br />
© 2011 Baishideng. All rights reserved.<br />
ter preservation the challenge is not only to achieve the<br />
best possible oncological outcome, but also to ensure<br />
that patients with low <strong>rectal</strong> <strong>cancer</strong> have realistic and<br />
accurate expectations <strong>of</strong> their treatment choice so that<br />
the best possible overall outcome can be obtained by<br />
each individual.<br />
© 2011 Baishideng. All rights reserved.<br />
Key words: Rectal <strong>cancer</strong>; Survival; Local recurrence;<br />
Morbidity; Ano<strong>rectal</strong> function; Quality <strong>of</strong> life; Patient<br />
preference<br />
Peer reviewer: Hiroki Yamaue, MD, PhD, Department <strong>of</strong> Surgery,<br />
Wakayama Medical University, School <strong>of</strong> Medicine, 811-1<br />
Kimiidera, Wakayama 641-8510, Japan<br />
Mulsow J, Winter DC. Sphincter preservation for distal <strong>rectal</strong><br />
<strong>cancer</strong> - a goal worth achieving at all costs? <strong>World</strong> J Gastroenterol<br />
2011; 17(7): 855-861 Available from: URL: http://www.<br />
wjgnet.com/1007-9327/full/v17/i7/855.htm DOI: http://<br />
dx.doi.org/10.3748/wjg.v17.i7.855<br />
INTRODUCTION<br />
TOPIC HIGHLIGHT<br />
In the management <strong>of</strong> patients with <strong>rectal</strong> <strong>cancer</strong>, sphincter<br />
preservation is a priority and regarded a marker <strong>of</strong><br />
surgical quality. Technical and technological advances have<br />
led to an increase in sphincter preserving surgery and a<br />
fall in the rate <strong>of</strong> abdominoperineal excision (APE) [1] .<br />
Furthermore, the recognition <strong>of</strong> the oncological importance<br />
<strong>of</strong> the circumferential, rather than distal resection<br />
margin, has allowed an increasingly aggressive surgical<br />
approach. The knowledge that a distal margin <strong>of</strong> 1 cm<br />
will safely allow complete tumor removal affords an ever<br />
greater proportion <strong>of</strong> patients the opportunity <strong>of</strong> sphincter<br />
preserving surgery for low <strong>rectal</strong> <strong>cancer</strong> [2] . In addition,<br />
our ever increasing understanding <strong>of</strong> tumor behaviour<br />
gives patients new options in the form <strong>of</strong> non-operative<br />
February 21, 2011|Volume 17|Issue 7|
Mulsow J et al . Treatment options and their outcomes in the management <strong>of</strong> distal <strong>rectal</strong> <strong>cancer</strong><br />
treatment (following complete response to neo-adjuvant<br />
treatment), or transanal excision in selected circumstances.<br />
On the other hand, tumor down-staging following neoadjuvant<br />
chemoradiotherapy has not led to the expected<br />
increase in sphincter preserving surgery.<br />
Thus, for patients with low <strong>rectal</strong> tumors, and for<br />
whom APE would formerly have been the only option,<br />
a number <strong>of</strong> sphincter preserving options are now available.<br />
However, while it may be technically possible to reconstruct<br />
(or avoid radical surgery altogether) an increasing<br />
majority <strong>of</strong> patients with <strong>rectal</strong> <strong>cancer</strong>, we should<br />
pause to consider the overall merits <strong>of</strong> this approach<br />
and consider the patient’s overall outcome (both oncological<br />
and functional), while remembering that there<br />
remain acceptable non-reconstructive alternatives (APE<br />
or low Hartmann’s procedure). In doing so, a number <strong>of</strong><br />
factors must be considered and the ‘costs’ <strong>of</strong> sphincter<br />
preservation evaluated.<br />
ONCOLOGICAL OUTCOME IN THE<br />
TREATMENT OF RECTAL CANCER<br />
The oncological outcome is <strong>of</strong> paramount importance<br />
whether anterior resection (AR), APE, transanal excision,<br />
or a non-operative approach is adopted in the treatment<br />
<strong>of</strong> low <strong>rectal</strong> <strong>cancer</strong>.<br />
High rates <strong>of</strong> circumferential resection margin (CRM)<br />
positivity (up to 40%) following APE in some series<br />
and consequent high local recurrence rates have led to<br />
suggestions that the outcome following APE is inherently<br />
worse than that following AR. It does appear that <strong>rectal</strong><br />
tumors in patients who undergo APE are <strong>of</strong>ten more<br />
locally advanced, more poorly differentiated, and show<br />
a lesser response to neo-adjuvant chemoradiotherapy [3] .<br />
However, with meticulous surgery and the avoidance <strong>of</strong><br />
tumor perforation and margin positivity, results following<br />
APE can be similar to those after AR [4] . Indeed, local<br />
recurrence rates in the order <strong>of</strong> 5% can be achieved<br />
following the application <strong>of</strong> a standardised approach [5,6] .<br />
Undoubtedly the technique <strong>of</strong> APE has drifted<br />
from that originally described by Miles [7] in which a wide<br />
dissection <strong>of</strong> the rectum was performed to produce a<br />
cylindrical specimen. Application <strong>of</strong> TME principles and<br />
evolution in technique have resulted in an APE in which<br />
the specimen tapers (Morson’s waist) at the level <strong>of</strong> the<br />
pelvic floor with a consequent narrow circumferential<br />
resection margin and risk <strong>of</strong> CRM positivity and tumor<br />
perforation. Recourse to originally described principles<br />
via an extra-levator approach avoids “waisting” <strong>of</strong> the<br />
specimen [8] and reduces the rate <strong>of</strong> CRM involvement [9] .<br />
Nonetheless, rates <strong>of</strong> CRM involvement may still lag<br />
behind those seen in AR [10] and there remains a need to<br />
further examine surgical technique in APE and develop a<br />
standardised approach with appropriate training if needed.<br />
Inter-sphincteric resection represents the most extreme<br />
form <strong>of</strong> sphincter preserving surgery in which part, or<br />
all, <strong>of</strong> the internal sphincter is resected. This approach<br />
may be applied to tumors within 2 cm <strong>of</strong> the sphincter<br />
WJG|www.wjgnet.com<br />
complex and is made feasible by the recognition that distal<br />
intramural tumor spread beyond 1 cm is uncommon.<br />
Thus, inter-sphincteric resection becomes an option<br />
for patients with tumors within 2 cm <strong>of</strong> the sphincter<br />
complex, in whom pre-operative continence is intact, and<br />
for whom the tumor, at least in its distal part, is confined<br />
to the <strong>rectal</strong> wall. Follow-up suggests that local (6.6%)<br />
and distant (8.8%) recurrence rates [11] are comparable to<br />
those in published series <strong>of</strong> APE. Patients with locally<br />
advanced (T3-T4) tumors may become candidates for<br />
inter-sphincteric resection if a favourable down-staging<br />
response to neo-adjuvant chemoradiotherapy is<br />
demonstrated [3] . Those who are not suitable for intersphincteric<br />
resection and require APE are likely to selfselect<br />
as they have locally advanced tumors, that are poorly<br />
differentiated and show poor response to neo-adjuvant<br />
treatment [3] .<br />
Laparoscopy is increasingly employed as a less invasive<br />
approach in the management <strong>of</strong> <strong>rectal</strong> <strong>cancer</strong>. While the<br />
initial results from the UK MRC CLASSIC trial highlighted<br />
increased rates <strong>of</strong> margin positivity following laparoscopic<br />
<strong>rectal</strong> <strong>cancer</strong> surgery (when compared to conventional,<br />
open TME) [12] , the long-term oncological outcomes<br />
do not appear to be compromised [13,14] . This study remains<br />
the only randomised controlled trial to assess the role <strong>of</strong><br />
laparoscopy in <strong>rectal</strong> <strong>cancer</strong>, however results from prospective<br />
series <strong>of</strong> laparoscopic resection have also demonstrated<br />
similar oncological outcomes to those reported<br />
following open TME [15] .<br />
Transanal surgery for <strong>rectal</strong> <strong>cancer</strong> represents an attractive<br />
approach that may allow the morbidity and functional<br />
sequelae <strong>of</strong> total meso<strong>rectal</strong> excision (TME) to be<br />
avoided. Better surgical results with lower margin positivity<br />
are achieved following transanal endoscopic microsurgery<br />
(TEMS) than conventional transanal (TA) excision<br />
(2% vs 16%) [16] , however outcomes are generally inferior to<br />
those following radical resection with a 3-5 fold increased<br />
local recurrence risk [17] . TEMS appears to be a reasonable<br />
option (LR < 5%) in selected patients with favourable<br />
pathological features (pT1 Sm1; well or moderately differentiated;<br />
< 3 cm diameter; no lymphovascular invasion) [18] .<br />
For tumors with less favourable features, the oncological<br />
result following TEMS is inferior to that seen after TME.<br />
Difficulty in reliably predicting the T-<strong>stage</strong> pre-operatively<br />
remains an obstacle to patient selection. Likewise, prediction<br />
<strong>of</strong> N-<strong>stage</strong> is problematic as up to 18% <strong>of</strong> T1 tumors<br />
will have associated nodal disease. However, in patients<br />
with adverse pathological features after TEMS, subsequent<br />
conversion to radical surgery does not appear to<br />
be associated with significantly increased LR rates [18] . In<br />
reality, the decision to adopt a transanal approach is frequently<br />
based upon the fitness <strong>of</strong> the patient.<br />
One-fifth to one-quarter <strong>of</strong> patients following neo-adjuvant<br />
chemoradiotherapy will show a complete pathological<br />
response. Predicting those likely to respond and those<br />
who have had a complete pathological response remains<br />
difficult - up to 40% <strong>of</strong> patients who appear to have had a<br />
complete clinical response have residual disease following<br />
856 February 21, 2011|Volume 17|Issue 7|
esection [19] . Conversely, approximately 10% <strong>of</strong> patients<br />
who have an incomplete clinical response will show a<br />
complete pathological response [20] . Observation alone<br />
may be a viable alternative in selected patients who show<br />
a complete clinical response to neo-adjuvant therapy [20] .<br />
Local recurrence has been reported in 11% <strong>of</strong> those who<br />
had a sustained complete clinical response. These patients<br />
appear amenable to salvage therapy without adverse oncological<br />
outcome in the event <strong>of</strong> local recurrence [21] .<br />
There may also be a role for full thickness transanal<br />
excision <strong>of</strong> tumor in selected patients with T3 tumors<br />
who show an excellent response to neo-adjuvant chemoradiotherapy<br />
and who are deemed unfit for or refuse<br />
TME, or who had a perceived complete response to neoadjuvant<br />
treatment. The limited available data point to<br />
local recurrence and survival figures that are comparable<br />
to those achieved with radical surgery [22] . This approach<br />
requires further validation.<br />
Finally, endoscopic submucosal dissection is an evolving<br />
technique that may represent an alternative sphincter<br />
preserving approach in the management <strong>of</strong> <strong>rectal</strong> tumors.<br />
This technique has been reported with low complication<br />
rates and in patients in whom complete resection is<br />
achieved (approximately 70%) recurrence rates at shortterm<br />
follow-up are low [23] . Further studies are required to<br />
establish the role <strong>of</strong> this technique.<br />
FUNCTIONAL OUTCOME AND QUALITY<br />
OF LIFE FOLLOWING SURGERY FOR<br />
RECTAL CANCER<br />
Mulsow J et al . Treatment options and their outcomes in the management <strong>of</strong> distal <strong>rectal</strong> <strong>cancer</strong><br />
Functional outcome<br />
Frequency, urgency, and soiling (anterior resection syndrome)<br />
are common problems after anterior resection<br />
that reflect loss <strong>of</strong> the capacitance and compliance <strong>of</strong> the<br />
<strong>rectal</strong> reservoir. Approximately 60% <strong>of</strong> patients experience<br />
some degree <strong>of</strong> incontinence, while one-third experience<br />
frequent symptoms <strong>of</strong> urgency and frequency. Postoperative<br />
studies suggest that ano<strong>rectal</strong> dysfunction after<br />
low anterior resection is more a factor <strong>of</strong> reduced compliance<br />
and capacity, than diminished sphincter function [24,25] .<br />
Furthermore, reflexes <strong>of</strong> the anal sphincter that help to<br />
maintain continence are preserved after low anterior resection<br />
[26] .<br />
Patients undergoing inter-sphincteric resection have the<br />
additional insult <strong>of</strong> reduced internal sphincter function [24] .<br />
Inter-sphincteric resection is associated with a fall in resting<br />
anal canal pressures [27] and continence when compared<br />
to conventional anastomosis, but not with a worsening <strong>of</strong><br />
stool frequency (typically averaging 2/24 h [28] ) and urgency<br />
[29] . Long-term satisfactory continence rates are achievable<br />
in 75% <strong>of</strong> patients [11] . Outcomes, particularly in the<br />
first post-operative year, can be improved by performing<br />
only a partial or subtotal resection <strong>of</strong> the internal sphincter<br />
and through construction <strong>of</strong> a colonic J-pouch [27,30-32] . Preoperative<br />
radiotherapy significantly worsens the functional<br />
outcome following inter-sphincteric resection [11] .<br />
Following straight anastomosis progressive dilatation<br />
WJG|www.wjgnet.com<br />
<strong>of</strong> the neorectum can allow some improvement in compliance<br />
[33] and function over time. Colonic reservoirs (J-pouch<br />
or coloplasty) may allow early preservation <strong>of</strong> function by<br />
providing a neorectum functionally comparable to the resected<br />
rectum. It is technically possible to create a J-pouch<br />
in the majority <strong>of</strong> patients (95%) [34] . With optimum pouch<br />
size (5 cm) [35,36] and level <strong>of</strong> anastomosis (< 8 cm from the<br />
anal verge) [37] , there appear to be functional advantages<br />
to the creation <strong>of</strong> a colonic J-pouch. Patients undergoing<br />
low anterior resection with J-pouch reconstruction have<br />
less stool frequency and urgency when compared to those<br />
with a straight anastomosis, however this benefit is not<br />
maintained beyond two years [34] . Surprisingly, this functional<br />
gain may not impact positively on quality <strong>of</strong> life<br />
after surgery [38] . Evidence would suggest that there is no<br />
significant advantage to coloplasty over straight anastomosis<br />
[38] . Side-to-end anastomosis using a short side limb may<br />
represent an alternative to colonic pouch with the limited<br />
available data suggesting comparable functional and surgical<br />
outcomes, however further studies are needed [39-41] .<br />
The benefits <strong>of</strong> the colonic pouch may not be attributable<br />
to an increased capacity when compared to straight<br />
anastomosis, but rather due to the interruption <strong>of</strong> normal<br />
propulsive motility [42,43] .<br />
Pre- or post-operative irradiation has a significant negative<br />
impact on function following anterior resection. In the<br />
Dutch TME study, pre-operative radiotherapy was associated<br />
with a significant increase in bowel frequency and incontinence<br />
(62% vs 38% for surgery alone) and this had a<br />
significant negative impact on patient satisfaction and daily<br />
activity [44] . Incontinence was worst in patients with lower<br />
tumors [44] . These findings have been replicated in other<br />
studies with long-term follow-up showing an approximate<br />
doubling <strong>of</strong> symptoms <strong>of</strong> faecal incontinence, soiling and<br />
bowel frequency when compared to patients treated with<br />
surgery alone [45] . Ano<strong>rectal</strong> manometry has shown irradiated<br />
patients to have significantly lower resting and squeeze<br />
pressure, while endoanal ultrasound has shown increased<br />
scarring <strong>of</strong> the anal sphincter when compared to nonirradiated<br />
patients [24,45] . Short course pre-operative radiotherapy<br />
and pre-operative long-course chemoradiotherapy<br />
appear to impact similarly on ano<strong>rectal</strong> function [46] . The<br />
functional outcome following post-operative radiotherapy<br />
is worse than following pre-operative treatment with patients<br />
experiencing increased frequency <strong>of</strong> defecation and<br />
clustering [47] .<br />
While reduced following pre-operative radiotherapy,<br />
the functional result in patients undergoing low anterior<br />
resection with colo-anal anastomosis appears to better<br />
with a colonic J-pouch rather than straight anastomosis<br />
or coloplasty at 24 mo follow-up [48] .<br />
Despite increased tumor down-staging, pre-operative<br />
conventionally fractionated radiotherapy does not appear<br />
to confer an advantage with respect to sphincter preservation<br />
over short-course radiotherapy [49] .<br />
Extended pelvic lymphadenectomy is frequently performed<br />
in Japan as an adjunct to TME, and <strong>of</strong>ten without<br />
neo-adjuvant treatment. This approach does not appear<br />
to confer an oncological advantage when compared to<br />
857 February 21, 2011|Volume 17|Issue 7|
Mulsow J et al . Treatment options and their outcomes in the management <strong>of</strong> distal <strong>rectal</strong> <strong>cancer</strong><br />
TME alone (with neoadjuvant treatment) and is associated<br />
with an increased incidence <strong>of</strong> urinary and sexual<br />
dysfunction [50-52] .<br />
Quality <strong>of</strong> life<br />
There is an absence <strong>of</strong> randomised studies comparing<br />
outcomes following APE and AR for low <strong>rectal</strong> tumors<br />
(due to presumption that AR is superior). As a result, inferences<br />
as to their comparative quality <strong>of</strong> life outcomes<br />
can only be drawn from individual studies. None-theless,<br />
the available data challenges the presumption that<br />
a permanent stoma automatically renders an inferior<br />
quality <strong>of</strong> life outcome when compared to that following<br />
restorative surgery. A meta-analysis <strong>of</strong> over 1400 patients<br />
from 11 studies showed no difference in general quality<br />
<strong>of</strong> life scores between patients who underwent APE and<br />
AR. While APE was associated with better emotional and<br />
cognitive function scores and superior future perspectives<br />
(patients’ understanding <strong>of</strong> disease <strong>stage</strong>), vitality and sexual<br />
function scored better in patients undergoing AR [53] .<br />
These findings were consistent with those <strong>of</strong> an earlier<br />
meta-analysis [54] , however, their interpretation must be<br />
tempered by the poor quality <strong>of</strong> a number <strong>of</strong> individual<br />
studies, and the limited follow-up duration which fails to<br />
allow for the progressive functional improvement patients<br />
<strong>of</strong>ten experience following AR.<br />
MORBIDITY<br />
The argument in favour <strong>of</strong> observation (and/or transanal<br />
excision) in complete responders to neo-adjuvant<br />
treatment is the avoidance <strong>of</strong> the morbidity and functional<br />
loss associated with TME, with or without a<br />
temporary or permanent stoma. Ano<strong>rectal</strong> dysfunction,<br />
sexual dysfunction, difficulty voiding, and urinary incontinence<br />
are seen in up to one-third <strong>of</strong> patients following<br />
TME. Furthermore, these problems are exacerbated by<br />
pre-operative radiotherapy. Post-operative morbidity following<br />
laparoscopic and open <strong>rectal</strong> resection appears<br />
to be similar [12] , while a benefit to the laparoscopic approach<br />
with respect to long-term complications such as<br />
adhesion small bowel obstruction and incisional hernia<br />
remains to be proven [55] . Laparoscopic resection appears<br />
to impact similarly on bladder function when compared<br />
to open TME, but may be associated with a worse outcome<br />
with regard to male sexual function [56] .<br />
For patients undergoing TME, larger studies have<br />
shown overall rates <strong>of</strong> early morbidity <strong>of</strong> approximately<br />
40%. This figure increases to almost 50% following preoperative<br />
radiotherapy. Of patients undergoing APE,<br />
approximately one-fifth develop perineal wound problems<br />
[57] . The incidence <strong>of</strong> perineal wound problems rises<br />
to 30% following radiotherapy [57] and doubles following<br />
extralevator APE (38%) [10] . Eleven percent <strong>of</strong> patients<br />
undergoing AR developed clinical anastomotic leaks in<br />
the Dutch TME trial. The leak rate was not affected by<br />
pre-operative radiotherapy, but was reduced with proximal<br />
defunctioning stoma (8% vs 16%) [57] . The mortality rate<br />
for non-irradiated patients was 3.3% in the same study.<br />
WJG|www.wjgnet.com<br />
Again, from the Dutch study we know that approximately<br />
50% <strong>of</strong> patients undergoing AR will have a defunctioning<br />
stoma. It is worth noting that at long-term<br />
follow-up (median 48 mo) 21% <strong>of</strong> patients in one study<br />
who had undergone sphincter preserving surgery still<br />
had a stoma [58] . Loop ileostomy closure is associated with<br />
17% morbidity, however the majority (80%) <strong>of</strong> patients<br />
can be managed non-operatively [59] .<br />
PATIENT PREFERENCE<br />
The limited available evidence suggests that a majority<br />
(65%) <strong>of</strong> patients with <strong>rectal</strong> <strong>cancer</strong> are willing to defer<br />
decision making about their surgery to their surgeon [60] .<br />
What is not known, unlike for breast <strong>cancer</strong>, is the<br />
role that patients with <strong>rectal</strong> <strong>cancer</strong> would like to adopt<br />
in decision making, and how their given role influences<br />
their satisfaction with decision making and outcomes.<br />
We do know however that the relative importance that<br />
surgeons place on various outcomes such as permanent<br />
stoma and incontinence is <strong>of</strong>ten not matched by their<br />
patients [61] . Surgeons may in particular underestimate<br />
their patients’ concerns. Furthermore, surgeon’s choices<br />
may frequently be at odds with their patient’s inherent<br />
and perhaps unrecognised true preference [62] . Patients,<br />
for example, express a stronger desire to avoid chemotherapy<br />
than to avoid permanent stoma, while doctors<br />
express the opposite view.<br />
Multimedia decision aids (incorporating patient values<br />
into evidence based data) have been used to assess<br />
and quantify the relative importance patients with <strong>rectal</strong><br />
<strong>cancer</strong> place on different quality <strong>of</strong> life outcomes. Patients<br />
who have had surgery place greater emphasis on<br />
the avoidance <strong>of</strong> incontinence post-operatively than the<br />
avoidance <strong>of</strong> a permanent stoma [61] .<br />
Trade-<strong>of</strong>f techniques are another useful means <strong>of</strong><br />
gauging patient’s true preferences and will <strong>of</strong>ten highlight<br />
disparity between patients’ preferences and those<br />
<strong>of</strong> their physicians [62] . Using this technique, the strength<br />
<strong>of</strong> a preference is measured by determining the degree<br />
<strong>of</strong> risk <strong>of</strong> a particular (poor) outcome that the patient<br />
would be willing to accept in order to have the treatment.<br />
When patient preferences are assessed using time-trade<br />
methods, patients strongly express a desire to avoid a<br />
stoma with 65% willing to trade a mean <strong>of</strong> 34% <strong>of</strong> their<br />
life expectancy to avoid this outcome [63] . Furthermore,<br />
patients expressed a stronger desire to avoid the option<br />
<strong>of</strong> APE and thus permanent stoma than their treating<br />
physicians. Again, in patients who have had surgery for<br />
<strong>rectal</strong> <strong>cancer</strong>, the majority <strong>of</strong> those without a stoma<br />
would be willing to trade frequent (monthly) episodes<br />
<strong>of</strong> incontinence in order to avoid a permanent stoma [64] .<br />
APE patients would however hypothetically trade fewer<br />
years <strong>of</strong> remaining life to be without a stoma, than AR<br />
patients would to be without incontinence [65] .<br />
While patients may <strong>of</strong>ten be happy to defer decisions<br />
as to the type <strong>of</strong> surgery to their surgeons, the majority<br />
<strong>of</strong> those patients who do choose, would favour AR over<br />
APE [60] . More patients who have had AR would choose<br />
858 February 21, 2011|Volume 17|Issue 7|
that option again, than patients who have had APE (69%<br />
vs 46%) [60] . Interestingly, at longer term follow-up 80% <strong>of</strong><br />
patients who had APE indicate that they would choose<br />
the same option given the benefit <strong>of</strong> their experience [60] .<br />
CONCLUSION<br />
Sphincter preservation in <strong>rectal</strong> <strong>cancer</strong> - a goal worth<br />
achieving at all costs? The answer must be no. While we<br />
should strive toward sphincter preserving options, we<br />
must recognize the limitations <strong>of</strong> currently available approaches<br />
and accept that sphincter preservation may not<br />
be the best overall option for each individual patient.<br />
Oncological outcomes following AR and APE should<br />
be equivalent, however there remains room to uniformly<br />
improve and standardise approaches and outcomes in<br />
APE. If equivalence for oncological outcome is achieved,<br />
then functional outcome, quality <strong>of</strong> life, and ultimately<br />
patient preference become <strong>of</strong> paramount importance in<br />
decision making for the treatment <strong>of</strong> low <strong>rectal</strong> <strong>cancer</strong>.<br />
Ano<strong>rectal</strong> dysfunction and poor functional outcome are<br />
common following AR. The alternative <strong>of</strong> APE or low<br />
Hartmann’s procedure imposes a permanent stoma. Quality<br />
<strong>of</strong> life following APE appears to be similar to that<br />
following AR. Given the choice, most patients would<br />
choose AR over APE. It is doubtful however that patients<br />
appreciate fully the functional outcome following AR, and<br />
also likely that patients harbour excessively negative misconceptions<br />
about life with a permanent stoma. Patients<br />
must be informed that function may not be as good as<br />
they expect after AR, and also that patients who have undergone<br />
APE positively appraise this option at follow-up.<br />
The morbidity associated with stoma reversal (following<br />
AR), and the significant risk <strong>of</strong> perineal wound problems<br />
following APE must also be considered. Non-radical and<br />
even non-operative approaches are increasingly an option<br />
in the management <strong>of</strong> selected patients with low <strong>rectal</strong><br />
<strong>cancer</strong> that obviate the morbidity and outcomes following<br />
TME. Ultimately we must ensure that patients with low<br />
<strong>rectal</strong> <strong>cancer</strong> have realistic expectations <strong>of</strong> their treatment<br />
options and that their decisions are truly informed.<br />
REFERENCES<br />
Mulsow J et al . Treatment options and their outcomes in the management <strong>of</strong> distal <strong>rectal</strong> <strong>cancer</strong><br />
1 Tilney HS, Heriot AG, Purkayastha S, Antoniou A, Aylin P,<br />
Darzi AW, Tekkis PP. A national perspective on the decline<br />
<strong>of</strong> abdominoperineal resection for <strong>rectal</strong> <strong>cancer</strong>. Ann Surg<br />
2008; 247: 77-84<br />
2 Guillem JG, Chessin DB, Shia J, Suriawinata A, Riedel E,<br />
Moore HG, Minsky BD, Wong WD. A prospective pathologic<br />
analysis using whole-mount sections <strong>of</strong> <strong>rectal</strong> <strong>cancer</strong><br />
following preoperative combined modality therapy: implications<br />
for sphincter preservation. Ann Surg 2007; 245: 88-93<br />
3 Weiser MR, Quah HM, Shia J, Guillem JG, Paty PB, Temple<br />
LK, Goodman KA, Minsky BD, Wong WD. Sphincter preservation<br />
in low <strong>rectal</strong> <strong>cancer</strong> is facilitated by preoperative<br />
chemoradiation and intersphincteric dissection. Ann Surg<br />
2009; 249: 236-242<br />
4 Wibe A, Syse A, Andersen E, Tretli S, Myrvold HE, Søreide<br />
O. Oncological outcomes after total meso<strong>rectal</strong> excision for<br />
cure for <strong>cancer</strong> <strong>of</strong> the lower rectum: anterior vs. abdomino-<br />
WJG|www.wjgnet.com<br />
perineal resection. Dis Colon Rectum 2004; 47: 48-58<br />
5 Chuwa EW, Seow-Choen F. Outcomes for abdominoperineal<br />
resections are not worse than those <strong>of</strong> anterior resections.<br />
Dis Colon Rectum 2006; 49: 41-49<br />
6 Davies M, Harris D, Hirst G, Beynon R, Morgan AR, Carr<br />
ND, Beynon J. Local recurrence after abdomino-perineal<br />
resection. Colo<strong>rectal</strong> Dis 2009; 11: 39-43<br />
7 Miles WE. A method <strong>of</strong> performing abdomino-perineal excision<br />
for carcinoma <strong>of</strong> the rectum and <strong>of</strong> the terminal portion<br />
<strong>of</strong> the pelvic colon (1908). CA Cancer J Clin 1971; 21: 361-364<br />
8 Holm T, Ljung A, Häggmark T, Jurell G, Lagergren J. Extended<br />
abdominoperineal resection with gluteus maximus<br />
flap reconstruction <strong>of</strong> the pelvic floor for <strong>rectal</strong> <strong>cancer</strong>. Br J<br />
Surg 2007; 94: 232-238<br />
9 West NP, Finan PJ, Anderin C, Lindholm J, Holm T, Quirke<br />
P. Evidence <strong>of</strong> the oncologic superiority <strong>of</strong> cylindrical abdominoperineal<br />
excision for low <strong>rectal</strong> <strong>cancer</strong>. J Clin Oncol<br />
2008; 26: 3517-3522<br />
10 West NP, Anderin C, Smith KJ, Holm T, Quirke P. Multicentre<br />
experience with extralevator abdominoperineal excision<br />
for low <strong>rectal</strong> <strong>cancer</strong>. Br J Surg 2010; 97: 588-599<br />
11 Chamlou R, Parc Y, Simon T, Bennis M, Dehni N, Parc R,<br />
Tiret E. Long-term results <strong>of</strong> intersphincteric resection for<br />
low <strong>rectal</strong> <strong>cancer</strong>. Ann Surg 2007; 246: 916-921; discussion<br />
921-922<br />
12 Guillou PJ, Quirke P, Thorpe H, Walker J, Jayne DG, Smith<br />
AM, Heath RM, Brown JM. Short-term endpoints <strong>of</strong> conventional<br />
versus laparoscopic-assisted surgery in patients<br />
with colo<strong>rectal</strong> <strong>cancer</strong> (MRC CLASICC trial): multicentre,<br />
randomised controlled trial. Lancet 2005; 365: 1718-1726<br />
13 Jayne DG, Guillou PJ, Thorpe H, Quirke P, Copeland J,<br />
Smith AM, Heath RM, Brown JM. Randomized trial <strong>of</strong> laparoscopic-assisted<br />
resection <strong>of</strong> colo<strong>rectal</strong> carcinoma: 3-year<br />
results <strong>of</strong> the UK MRC CLASICC Trial Group. J Clin Oncol<br />
2007; 25: 3061-3068<br />
14 Jayne DG, Thorpe HC, Copeland J, Quirke P, Brown JM,<br />
Guillou PJ. Five-year follow-up <strong>of</strong> the Medical Research<br />
Council CLASICC trial <strong>of</strong> laparoscopically assisted versus<br />
open surgery for colo<strong>rectal</strong> <strong>cancer</strong>. Br J Surg 2010; 97:<br />
1638-1645<br />
15 Tsang WW, Chung CC, Kwok SY, Li MK. Laparoscopic<br />
sphincter-preserving total meso<strong>rectal</strong> excision with colonic<br />
J-pouch reconstruction: five-year results. Ann Surg 2006;<br />
243: 353-358<br />
16 Christ<strong>of</strong>oridis D, Cho HM, Dixon MR, Mellgren AF,<br />
Mad<strong>of</strong>f RD, Finne CO. Transanal endoscopic microsurgery<br />
versus conventional transanal excision for patients with<br />
early <strong>rectal</strong> <strong>cancer</strong>. Ann Surg 2009; 249: 776-782<br />
17 Bentrem DJ, Okabe S, Wong WD, Guillem JG, Weiser MR,<br />
Temple LK, Ben-Porat LS, Minsky BD, Cohen AM, Paty PB.<br />
T1 adenocarcinoma <strong>of</strong> the rectum: transanal excision or radical<br />
surgery? Ann Surg 2005; 242: 472-477; discussion 477-479<br />
18 Bach SP, Hill J, Monson JR, Simson JN, Lane L, Merrie A,<br />
Warren B, Mortensen NJ. A predictive model for local recurrence<br />
after transanal endoscopic microsurgery for <strong>rectal</strong><br />
<strong>cancer</strong>. Br J Surg 2009; 96: 280-290<br />
19 Bedrosian I, Rodriguez-Bigas MA, Feig B, Hunt KK, Ellis<br />
L, Curley SA, Vauthey JN, Delclos M, Crane C, Janjan N,<br />
Skibber JM. Predicting the node-negative mesorectum after<br />
preoperative chemoradiation for locally advanced <strong>rectal</strong> carcinoma.<br />
J Gastrointest Surg 2004; 8: 56-62; discussion 62-63<br />
20 Habr-Gama A, Perez RO, Nadalin W, Sabbaga J, Ribeiro U Jr,<br />
Silva e Sousa AH Jr, Campos FG, Kiss DR, Gama-Rodrigues<br />
J. Operative versus nonoperative treatment for <strong>stage</strong> 0 distal<br />
<strong>rectal</strong> <strong>cancer</strong> following chemoradiation therapy: long-term<br />
results. Ann Surg 2004; 240: 711-717; discussion 717-718<br />
21 Habr-Gama A, Perez RO. Non-operative management <strong>of</strong><br />
<strong>rectal</strong> <strong>cancer</strong> after neoadjuvant chemoradiation. Br J Surg<br />
2009; 96: 125-127<br />
22 Callender GG, Das P, Rodriguez-Bigas MA, Skibber JM,<br />
859 February 21, 2011|Volume 17|Issue 7|
Mulsow J et al . Treatment options and their outcomes in the management <strong>of</strong> distal <strong>rectal</strong> <strong>cancer</strong><br />
Crane CH, Krishnan S, Delclos ME, Feig BW. Local excision<br />
after preoperative chemoradiation results in an equivalent<br />
outcome to total meso<strong>rectal</strong> excision in selected patients<br />
with T3 <strong>rectal</strong> <strong>cancer</strong>. Ann Surg Oncol 2010; 17: 441-447<br />
23 Onozato Y, Kakizaki S, Ishihara H, Iizuka H, Sohara N,<br />
Okamura S, Mori M, Itoh H. Endoscopic submucosal dissection<br />
for <strong>rectal</strong> tumors. Endoscopy 2007; 39: 423-427<br />
24 Matzel KE, Bittorf B, Günther K, Stadelmaier U, Hohenberger<br />
W. Rectal resection with low anastomosis: functional<br />
outcome. Colo<strong>rectal</strong> Dis 2003; 5: 458-464<br />
25 Nesbakken A, Nygaard K, Lunde OC. Meso<strong>rectal</strong> excision<br />
for <strong>rectal</strong> <strong>cancer</strong>: functional outcome after low anterior<br />
resection and colo<strong>rectal</strong> anastomosis without a reservoir.<br />
Colo<strong>rectal</strong> Dis 2002; 4: 172-176<br />
26 Lane RH, Parks AG. Function <strong>of</strong> the anal sphincters following<br />
colo-anal anastomosis. Br J Surg 1977; 64: 596-599<br />
27 Yamada K, Ogata S, Saiki Y, Fukunaga M, Tsuji Y, Takano M.<br />
Functional results <strong>of</strong> intersphincteric resection for low <strong>rectal</strong><br />
<strong>cancer</strong>. Br J Surg 2007; 94: 1272-1277<br />
28 Tilney HS, Tekkis PP. Extending the horizons <strong>of</strong> restorative<br />
<strong>rectal</strong> surgery: intersphincteric resection for low <strong>rectal</strong> <strong>cancer</strong>.<br />
Colo<strong>rectal</strong> Dis 2008; 10: 3-15; discussion 15-16<br />
29 Bretagnol F, Rullier E, Laurent C, Zerbib F, Gontier R, Saric J.<br />
Comparison <strong>of</strong> functional results and quality <strong>of</strong> life between<br />
intersphincteric resection and conventional coloanal anastomosis<br />
for low <strong>rectal</strong> <strong>cancer</strong>. Dis Colon Rectum 2004; 47: 832-838<br />
30 Willis S, Kasperk R, Braun J, Schumpelick V. Comparison<br />
<strong>of</strong> colonic J-pouch reconstruction and straight coloanal anastomosis<br />
after intersphincteric <strong>rectal</strong> resection. Langenbecks<br />
Arch Surg 2001; 386: 193-199<br />
31 Park JG, Lee MR, Lim SB, Hong CW, Yoon SN, Kang SB,<br />
Heo SC, Jeong SY, Park KJ. Colonic J-pouch anal anastomosis<br />
after ultralow anterior resection with upper sphincter excision<br />
for low-lying <strong>rectal</strong> <strong>cancer</strong>. <strong>World</strong> J Gastroenterol 2005;<br />
11: 2570-2573<br />
32 Bittorf B, Stadelmaier U, Göhl J, Hohenberger W, Matzel<br />
KE. Functional outcome after intersphincteric resection <strong>of</strong><br />
the rectum with coloanal anastomosis in low <strong>rectal</strong> <strong>cancer</strong>.<br />
Eur J Surg Oncol 2004; 30: 260-265<br />
33 Pedersen IK, Christiansen J, Hint K, Jensen P, Olsen J,<br />
Mortensen PE. Ano<strong>rectal</strong> function after low anterior resection<br />
for carcinoma. Ann Surg 1986; 204: 133-135<br />
34 Heriot AG, Tekkis PP, Constantinides V, Paraskevas P,<br />
Nicholls RJ, Darzi A, Fazio VW. Meta-analysis <strong>of</strong> colonic<br />
reservoirs versus straight coloanal anastomosis after anterior<br />
resection. Br J Surg 2006; 93: 19-32<br />
35 Hida J, Yasutomi M, Fujimoto K, Okuno K, Ieda S, Machidera<br />
N, Kubo R, Shindo K, Koh K. Functional outcome<br />
after low anterior resection with low anastomosis for <strong>rectal</strong><br />
<strong>cancer</strong> using the colonic J-pouch. Prospective randomized<br />
study for determination <strong>of</strong> optimum pouch size. Dis Colon<br />
Rectum 1996; 39: 986-991<br />
36 Lazorthes F, Gamagami R, Chiotasso P, Istvan G, Muhammad<br />
S. Prospective, randomized study comparing clinical<br />
results between small and large colonic J-pouch following<br />
coloanal anastomosis. Dis Colon Rectum 1997; 40: 1409-1413<br />
37 Hida J, Yasutomi M, Maruyama T, Fujimoto K, Nakajima<br />
A, Uchida T, Wakano T, Tokoro T, Kubo R, Shindo K. Indications<br />
for colonic J-pouch reconstruction after anterior<br />
resection for <strong>rectal</strong> <strong>cancer</strong>: determining the optimum level<br />
<strong>of</strong> anastomosis. Dis Colon Rectum 1998; 41: 558-563<br />
38 Fazio VW, Zutshi M, Remzi FH, Parc Y, Ruppert R, Fürst A,<br />
Celebrezze J Jr, Galanduik S, Orangio G, Hyman N, Bokey<br />
L, Tiret E, Kirchdorfer B, Medich D, Tietze M, Hull T, Hammel<br />
J. A randomized multicenter trial to compare long-term<br />
functional outcome, quality <strong>of</strong> life, and complications <strong>of</strong><br />
surgical procedures for low <strong>rectal</strong> <strong>cancer</strong>s. Ann Surg 2007;<br />
246: 481-488; discussion 488-490<br />
39 Huber FT, Herter B, Siewert JR. Colonic pouch vs. side-toend<br />
anastomosis in low anterior resection. Dis Colon Rectum<br />
WJG|www.wjgnet.com<br />
1999; 42: 896-902<br />
40 Machado M, Nygren J, Goldman S, Ljungqvist O. Similar<br />
outcome after colonic pouch and side-to-end anastomosis<br />
in low anterior resection for <strong>rectal</strong> <strong>cancer</strong>: a prospective randomized<br />
trial. Ann Surg 2003; 238: 214-220<br />
41 Tsunoda A, Kamiyama G, Narita K, Watanabe M, Nakao K,<br />
Kusano M. Prospective randomized trial for determination<br />
<strong>of</strong> optimum size <strong>of</strong> side limb in low anterior resection with<br />
side-to-end anastomosis for <strong>rectal</strong> carcinoma. Dis Colon Rectum<br />
2009; 52: 1572-1577<br />
42 Hallböök O, Nystrom PO, Sjödahl R. Physiologic characteristics<br />
<strong>of</strong> straight and colonic J-pouch anastomoses after<br />
<strong>rectal</strong> excision for <strong>cancer</strong>. Dis Colon Rectum 1997; 40: 332-338<br />
43 Fürst A, Burgh<strong>of</strong>er K, Hutzel L, Jauch KW. Neo<strong>rectal</strong> reservoir<br />
is not the functional principle <strong>of</strong> the colonic J-pouch:<br />
the volume <strong>of</strong> a short colonic J-pouch does not differ from<br />
a straight coloanal anastomosis. Dis Colon Rectum 2002; 45:<br />
660-667<br />
44 Peeters KC, van de Velde CJ, Leer JW, Martijn H, Junggeburt<br />
JM, Kranenbarg EK, Steup WH, Wiggers T, Rutten HJ, Marijnen<br />
CA. Late side effects <strong>of</strong> short-course preoperative radiotherapy<br />
combined with total meso<strong>rectal</strong> excision for <strong>rectal</strong><br />
<strong>cancer</strong>: increased bowel dysfunction in irradiated patients-<br />
-a Dutch colo<strong>rectal</strong> <strong>cancer</strong> group study. J Clin Oncol 2005; 23:<br />
6199-6206<br />
45 Pollack J, Holm T, Cedermark B, Holmström B, Mellgren A.<br />
Long-term effect <strong>of</strong> preoperative radiation therapy on ano<strong>rectal</strong><br />
function. Dis Colon Rectum 2006; 49: 345-352<br />
46 Pietrzak L, Bujko K, Nowacki MP, Kepka L, Oledzki J, Rutkowski<br />
A, Szmeja J, Kladny J, Dymecki D, Wieczorek A,<br />
Pawlak M, Lesniak T, Kowalska T, Richter P. Quality <strong>of</strong> life,<br />
ano<strong>rectal</strong> and sexual functions after preoperative radiotherapy<br />
for <strong>rectal</strong> <strong>cancer</strong>: report <strong>of</strong> a randomised trial. Radiother<br />
Oncol 2007; 84: 217-225<br />
47 Nathanson DR, Espat NJ, Nash GM, D’Alessio M, Thaler<br />
H, Minsky BD, Enker W, Wong D, Guillem J, Cohen A, Paty<br />
PB. Evaluation <strong>of</strong> preoperative and postoperative radiotherapy<br />
on long-term functional results <strong>of</strong> straight coloanal<br />
anastomosis. Dis Colon Rectum 2003; 46: 888-894<br />
48 Parc Y, Zutshi M, Zalinski S, Ruppert R, Fürst A, Fazio VW.<br />
Preoperative radiotherapy is associated with worse functional<br />
results after coloanal anastomosis for <strong>rectal</strong> <strong>cancer</strong>.<br />
Dis Colon Rectum 2009; 52: 2004-2014<br />
49 Bujko K, Nowacki MP, Nasierowska-Guttmejer A, Michalski<br />
W, Bebenek M, Pudełko M, Kryj M, Oledzki J, Szmeja J,<br />
Słuszniak J, Serkies K, Kładny J, Pamucka M, Kukołowicz P.<br />
Sphincter preservation following preoperative radiotherapy<br />
for <strong>rectal</strong> <strong>cancer</strong>: report <strong>of</strong> a randomised trial comparing<br />
short-term radiotherapy vs. conventionally fractionated radiochemotherapy.<br />
Radiother Oncol 2004; 72: 15-24<br />
50 Georgiou P, Tan E, Gouvas N, Antoniou A, Brown G, Nicholls<br />
RJ, Tekkis P. Extended lymphadenectomy versus conventional<br />
surgery for <strong>rectal</strong> <strong>cancer</strong>: a meta-analysis. Lancet<br />
Oncol 2009; 10: 1053-1062<br />
51 Akasu T, Sugihara K, Moriya Y. Male urinary and sexual<br />
functions after meso<strong>rectal</strong> excision alone or in combination<br />
with extended lateral pelvic lymph node dissection for <strong>rectal</strong><br />
<strong>cancer</strong>. Ann Surg Oncol 2009; 16: 2779-2786<br />
52 Kusters M, Beets GL, van de Velde CJ, Beets-Tan RG, Marijnen<br />
CA, Rutten HJ, Putter H, Moriya Y. A comparison<br />
between the treatment <strong>of</strong> low <strong>rectal</strong> <strong>cancer</strong> in Japan and the<br />
Netherlands, focusing on the patterns <strong>of</strong> local recurrence.<br />
Ann Surg 2009; 249: 229-235<br />
53 Cornish JA, Tilney HS, Heriot AG, Lavery IC, Fazio VW,<br />
Tekkis PP. A meta-analysis <strong>of</strong> quality <strong>of</strong> life for abdominoperineal<br />
excision <strong>of</strong> rectum versus anterior resection for<br />
<strong>rectal</strong> <strong>cancer</strong>. Ann Surg Oncol 2007; 14: 2056-2068<br />
54 Pachler J, Wille-Jørgensen P. Quality <strong>of</strong> life after <strong>rectal</strong> resection<br />
for <strong>cancer</strong>, with or without permanent colostomy.<br />
Cochrane Database Syst Rev 2005; CD004323<br />
860 February 21, 2011|Volume 17|Issue 7|
Mulsow J et al . Treatment options and their outcomes in the management <strong>of</strong> distal <strong>rectal</strong> <strong>cancer</strong><br />
55 Taylor GW, Jayne DG, Brown SR, Thorpe H, Brown JM,<br />
Dewberry SC, Parker MC, Guillou PJ. Adhesions and incisional<br />
hernias following laparoscopic versus open surgery<br />
for colo<strong>rectal</strong> <strong>cancer</strong> in the CLASICC trial. Br J Surg 2010; 97:<br />
70-78<br />
56 Jayne DG, Brown JM, Thorpe H, Walker J, Quirke P, Guillou<br />
PJ. Bladder and sexual function following resection for<br />
<strong>rectal</strong> <strong>cancer</strong> in a randomized clinical trial <strong>of</strong> laparoscopic<br />
versus open technique. Br J Surg 2005; 92: 1124-1132<br />
57 Marijnen CA, Kapiteijn E, van de Velde CJ, Martijn H,<br />
Steup WH, Wiggers T, Kranenbarg EK, Leer JW. Acute side<br />
effects and complications after short-term preoperative radiotherapy<br />
combined with total meso<strong>rectal</strong> excision in primary<br />
<strong>rectal</strong> <strong>cancer</strong>: report <strong>of</strong> a multicenter randomized trial.<br />
J Clin Oncol 2002; 20: 817-825<br />
58 Bujko K, Nowacki MP, Nasierowska-Guttmejer A, Michalski<br />
W, Bebenek M, Kryj M. Long-term results <strong>of</strong> a randomized<br />
trial comparing preoperative short-course radiotherapy<br />
with preoperative conventionally fractionated chemoradiation<br />
for <strong>rectal</strong> <strong>cancer</strong>. Br J Surg 2006; 93: 1215-1223<br />
59 Perez RO, Habr-Gama A, Seid VE, Proscurshim I, Sousa<br />
AH Jr, Kiss DR, Linhares M, Sapucahy M, Gama-Rodrigues<br />
J. Loop ileostomy morbidity: timing <strong>of</strong> closure matters. Dis<br />
Colon Rectum 2006; 49: 1539-1545<br />
WJG|www.wjgnet.com<br />
60 Zolciak A, Bujko K, Kepka L, Oledzki J, Rutkowski A,<br />
Nowacki MP. Abdominoperineal resection or anterior resection<br />
for <strong>rectal</strong> <strong>cancer</strong>: patient preferences before and after<br />
treatment. Colo<strong>rectal</strong> Dis 2006; 8: 575-580<br />
61 Masya LM, Young JM, Solomon MJ, Harrison JD, Dennis RJ,<br />
Salkeld GP. Preferences for outcomes <strong>of</strong> treatment for <strong>rectal</strong><br />
<strong>cancer</strong>: patient and clinician utilities and their application in<br />
an interactive computer-based decision aid. Dis Colon Rectum<br />
2009; 52: 1994-2002<br />
62 Solomon MJ, Pager CK, Keshava A, Findlay M, Butow P,<br />
Salkeld GP, Roberts R. What do patients want? Patient preferences<br />
and surrogate decision making in the treatment <strong>of</strong><br />
colo<strong>rectal</strong> <strong>cancer</strong>. Dis Colon Rectum 2003; 46: 1351-1357<br />
63 Harrison JD, Solomon MJ, Young JM, Meagher A, Butow P,<br />
Salkeld G, Hruby G, Clarke S. Patient and physician preferences<br />
for surgical and adjuvant treatment options for <strong>rectal</strong><br />
<strong>cancer</strong>. Arch Surg 2008; 143: 389-394<br />
64 Bossema ER, Marijnen CA, Baas-Thijssen MC, van de Velde<br />
CJ, Stiggelbout AM. Evaluation <strong>of</strong> the treatment trade<strong>of</strong>f<br />
method in <strong>rectal</strong> <strong>cancer</strong> patients: is surgery preference related<br />
to outcome utilities? Med Decis Making 2008; 28: 888-898<br />
65 Bossema E, Stiggelbout A, Baas-Thijssen M, van de Velde C,<br />
Marijnen C. Patients’ preferences for low <strong>rectal</strong> <strong>cancer</strong> surgery.<br />
Eur J Surg Oncol 2008; 34: 42-48<br />
S- Editor Sun H L- Editor O’Neill M E- Editor Ma WH<br />
861 February 21, 2011|Volume 17|Issue 7|
Online Submissions: http://www.wjgnet.com/1007-9327<strong>of</strong>fice<br />
wjg@wjgnet.com<br />
doi:10.3748/wjg.v17.i7.862<br />
Imran Hassan, MD, Assistant Pr<strong>of</strong>essor, Series Editor<br />
Minimally invasive surgery for <strong>rectal</strong> <strong>cancer</strong>: Are we there<br />
yet?<br />
Bradley J Champagne, Rohit Makhija<br />
Bradley J Champagne, Division <strong>of</strong> Colo<strong>rectal</strong> Surgery, University<br />
Hospitals Case Medical Center, Cleveland, OH 44106,<br />
United States<br />
Rohit Makhija, Laparoscopic Colo<strong>rectal</strong> Fellow, University Hospitals<br />
Case Medical Center, Cleveland, OH 44106, United States<br />
Author contributions: Champagne BC wrote the paper, performed<br />
a literature search, analyzed data; Makhija R performed<br />
literature search and contributed to writing the paper.<br />
Correspondence to: Bradley J Champagne, MD, FACS, Associate<br />
Pr<strong>of</strong>essor, Division <strong>of</strong> Colo<strong>rectal</strong> Surgery, University<br />
Hospitals Case Medical Center, Cleveland, OH 44106,<br />
United States. brad.champagne@uhhospitals.org<br />
Telephone: +1-216-5267221 Fax: +1-216-8445957<br />
Received: September 26, 2010 Revised: December 16, 2010<br />
Accepted: December 23, 2010<br />
Published online: February 21, 2011<br />
Abstract<br />
Laparoscopic colon surgery for select <strong>cancer</strong>s is slowly<br />
evolving as the standard <strong>of</strong> care but minimally invasive<br />
approaches for <strong>rectal</strong> <strong>cancer</strong> have been viewed with significant<br />
skepticism. This procedure has been performed<br />
by select surgeons at specialized centers and concerns<br />
over local recurrence, sexual dysfunction and appropriate<br />
training measures have further hindered widespread<br />
acceptance. Data for laparoscopic <strong>rectal</strong> resection now<br />
supports its continued implementation and widespread<br />
usage by expeienced surgeons for select patients. The<br />
current controversies regarding technical approaches<br />
have created ambiguity amongst opinion leaders and are<br />
also addressed in this review.<br />
© 2011 Baishideng. All rights reserved.<br />
Key words: Laparoscopic; Rectal <strong>cancer</strong>; Minimally invasive;<br />
Meso<strong>rectal</strong> excision<br />
Peer reviewer: Dr. Stefan Riss, Department <strong>of</strong> Surgery, Medical<br />
University <strong>of</strong> Vienna, Vienna, 1090, Austria<br />
WJG|www.wjgnet.com<br />
862<br />
<strong>World</strong> J Gastroenterol 2011 February 21; 17(7): 862-866<br />
ISSN 1007-9327 (print) ISSN 2219-2840 (online)<br />
© 2011 Baishideng. All rights reserved.<br />
Champagne BJ, Makhija R. Minimally invasive surgery for<br />
<strong>rectal</strong> <strong>cancer</strong>: Are we there yet? <strong>World</strong> J Gastroenterol 2011;<br />
17(7): 862-866 Available from: URL: http://www.wjgnet.<br />
com/1007-9327/full/v17/i7/862.htm DOI: http://dx.doi.<br />
org/10.3748/wjg.v17.i7.862<br />
INTRODUCTION<br />
The benefits <strong>of</strong> laparoscopic colon surgery compared to<br />
the open approach are well established [1-4] . Furthermore,<br />
laparotomy has been associated with an increased morbidity<br />
when compared to minimally invasive techniques<br />
for colo<strong>rectal</strong> disease [5] . More recently, the implementation<br />
<strong>of</strong> enhanced care programs coupled to laparoscopic<br />
resection has also resulted in a significant reduction in<br />
length <strong>of</strong> stay after both colon and <strong>rectal</strong> resection [6,7] .<br />
Laparoscopic colon surgery for select <strong>cancer</strong>s is slowly<br />
evolving as the standard <strong>of</strong> care but minimally invasive<br />
approaches for <strong>rectal</strong> <strong>cancer</strong> have been viewed with significant<br />
skepticism.<br />
Laparoscopic <strong>rectal</strong> resection for <strong>cancer</strong> is performed<br />
by select surgeons at specialized centers. The variability<br />
in anatomic definitions <strong>of</strong> the rectum, technique, selection<br />
criteria, and need for neoadjuvant therapy amongst<br />
this group <strong>of</strong> surgeons have made parallel comparisons<br />
difficult and ambiguous. Concern over local recurrence,<br />
sexual dysfunction and appropriate training measures<br />
have further hindered widespread acceptance <strong>of</strong> this approach.<br />
This opinion addresses short-term and oncological<br />
outcomes for laparoscopic resection <strong>of</strong> <strong>rectal</strong> <strong>cancer</strong>,<br />
the aforementioned obstacles, and current controversies<br />
regarding technical approaches.<br />
ONCOlOgICal OUTCOmes<br />
TOPIC HIGHLIGHT<br />
There are many potential endpoints for determining success<br />
for laparoscopic <strong>rectal</strong> resection. Undoubtedly, the<br />
February 21, 2011|Volume 17|Issue 7|
most significant is ensuring oncologic equivalence when<br />
compared to the open technique. This variable can primarily<br />
be measured by the adequacy <strong>of</strong> circumferential radial<br />
margins, recurrence rates, and both disease free and overall<br />
survival. Furthermore, the incidence <strong>of</strong> sexual dysfunction<br />
and other complications after laparoscopic pelvic dissection<br />
should approximate that with the open approach.<br />
Circumferential radial margin<br />
A positive circumferential resection margin (CRM) is a<br />
known marker for increased risk <strong>of</strong> future recurrence [8] .<br />
Strict adherence to the principles <strong>of</strong> “total meso<strong>rectal</strong> excision”<br />
is essential to preserve the meso<strong>rectal</strong> envelope, obtain<br />
an adequate circumferential margin and therefore reduce<br />
local recurrence rates. The first randomized trial for laparoscopic<br />
<strong>rectal</strong> resection showed a trend towards increased<br />
CRM positivity (6% open vs 12% laparoscopic, P = 0.19)<br />
for anterior resection [3] . Although this was initially alarming,<br />
several surgeons involved were on their learning curve, and<br />
preoperative chemoradiotherapy (CRT) was not standardized.<br />
Fortunately, three year outcomes showed that the difference<br />
in CRM positivity between laparoscopic and open<br />
approaches for anterior resection did not influence local<br />
recurrence rates. More recently, five year outcomes revealed<br />
no difference between groups in survival, disease-free survival,<br />
and local and distant recurrence [9,10] . Wound/port-site<br />
recurrence rates in the laparoscopic arm were 2.4% and also<br />
unchanged [10] . Conversion was associated with significantly<br />
worse outcomes overall but not disease-free survival.<br />
In the largest retrospective review to date, Ng et al [11]<br />
reported 579 laparoscopic <strong>rectal</strong> resections for <strong>cancer</strong><br />
with a CRM positivity <strong>of</strong> 2.14%. These encouraging results<br />
were further substantiated by two recent randomized<br />
controlled trials that reported CRM positivity rates <strong>of</strong> 2.9%<br />
(open) vs 4% (laparoscopic) [12] and 1.4% (open) and 2.6%<br />
(laparoscopic) [13] .<br />
In 2006, the Spanish Association <strong>of</strong> Surgeons started<br />
an audited teaching program to both make known the<br />
results <strong>of</strong> <strong>rectal</strong> <strong>cancer</strong> treatment and improve the outcomes<br />
by the teaching process. The quality <strong>of</strong> the pathologic<br />
specimens for laparoscopic and open <strong>rectal</strong> resection<br />
patients was scored and the circumferential radial margin<br />
was positive if tumor was located 1 mm or less from the<br />
surface <strong>of</strong> the specimen. No differences between groups<br />
for the completeness <strong>of</strong> the mesorectum or distance <strong>of</strong><br />
the tumor from the CRM were observed [14] . Although<br />
laparoscopic TME amongst this experienced group approximates<br />
that for their open resection for select tumors,<br />
the results may not be as favorable for low bulky lesions<br />
or those in an obese male or narrow pelvis.<br />
Local recurrence<br />
As highlighted above, the five year results <strong>of</strong> the MRC<br />
CLASSIC trial reported similar regional recurrence for<br />
laparoscopic vs open resection <strong>of</strong> <strong>rectal</strong> <strong>cancer</strong>. Several<br />
other studies have also shown acceptable regional recurrence<br />
rates. In their retrospective review, Ng and colleagues<br />
reported two port site recurrences and a pelvic recurrence<br />
rate <strong>of</strong> 7.4% [11] . Similarly, ten year outcomes from a pro-<br />
WJG|www.wjgnet.com<br />
Champagne BJ et al . Evidence for laparoscopic <strong>rectal</strong> resection<br />
Table 1 Overall survival for laparoscopic <strong>rectal</strong> resection with<br />
minimal 5 yr follow-up<br />
Authors Survival<br />
(laparoscopic)<br />
Survival<br />
(open)<br />
Follow-up<br />
(yr)<br />
MRC CLASSIC (Jayne et al) 57.9% 58.1% 5<br />
Sartori et al 75.4% NA 5<br />
Ng et al 63.9% 55.0% 10<br />
Lam et al 64.0% 5<br />
Laurent et al 82.0% 79.0% 5<br />
Ng et al 70.0% NA 5<br />
Siami et al 80.2% NA 5<br />
Bianchi et al 81.4% NA 5<br />
Tsang et al 81.3% NA 5<br />
NA: Not applicable.<br />
spective randomized trial for the laparoscopic resection <strong>of</strong><br />
upper <strong>rectal</strong> <strong>cancer</strong>s demonstrated a regional recurrence<br />
rate <strong>of</strong> 7.1% with no port-site recurrences [13] . Laurent and<br />
colleagues aimed to assess long-term oncologic outcomes<br />
after laparoscopic versus open surgery for <strong>rectal</strong> <strong>cancer</strong><br />
from in a retrospective comparative study [15] . 471 patients<br />
had <strong>rectal</strong> excision for invasive <strong>rectal</strong> carcinoma during<br />
the trial period: 238 were treated by laparoscopy and 233<br />
by open procedure. At 5 years, there was no difference <strong>of</strong><br />
local recurrence (3.9% vs 5.5%, P = 0.371) between laparoscopic<br />
and open surgery [15] .<br />
The multi-institutional series from Japan reported 1057<br />
selected patients with <strong>rectal</strong> <strong>cancer</strong> that underwent laparoscopic<br />
surgery [16] . All the data regarding the patient details<br />
and operative and postoperative outcome were collected<br />
retrospectively. At thirty months recurrence was found in<br />
6.6% <strong>of</strong> the 1011 curatively treated patients. Specifically,<br />
local recurrence occurred in 11 patients (1.0%) and there<br />
was no port-site metastasis (Table 1) [15] .<br />
FUNCTIONal OUTCOmes<br />
Laparoscopic <strong>rectal</strong> surgery proponents argue that the view<br />
in the pelvis is superior compared to the open approach.<br />
This magnification theoretically provides better visualization<br />
<strong>of</strong> the pelvic nerves. However, in the first randomized<br />
trial for laparoscopic <strong>rectal</strong> <strong>cancer</strong> male sexual function,<br />
erection and ejaculation were all significantly reduced with<br />
laparoscopic surgery. This should be interpreted with caution<br />
considering the aforementioned learning curve and<br />
that more patients in the laparoscopic group underwent a<br />
full TME, as compared to the open group. Bladder function<br />
remained similar between groups.<br />
In a prospective evaluation <strong>of</strong> sexual function Stamopoulos<br />
and colleagues [17] used the international index <strong>of</strong><br />
erectile function (IIEF) for 56 patients who underwent<br />
<strong>rectal</strong> <strong>cancer</strong> surgery (38 open vs 18 laparoscopic procedures,<br />
38 low anterior vs 18 abdominoperineal resections).<br />
Rectal <strong>cancer</strong> resections were associated with a significant<br />
reduction in IIEF scores and high rates <strong>of</strong> sexual dysfunction<br />
at 3 and 6 mo. The IIEF and domain scores at<br />
different assessment points were comparable between the<br />
laparoscopic and open surgery groups [17] .<br />
863 February 21, 2011|Volume 17|Issue 7|
Champagne BJ et al . Evidence for laparoscopic <strong>rectal</strong> resection<br />
Morino et al [18] also analyzed male sexual and urinary<br />
function after laparoscopic total meso<strong>rectal</strong> excision. They<br />
found that sexual desire was maintained by 55.6%, ability<br />
to engage in intercourse by 57.8%, and ability to achieve<br />
orgasm and ejaculation by 37.8% <strong>of</strong> the patients. The distance<br />
<strong>of</strong> the tumor from the anal verge and adjuvant or<br />
neoadjuvant treatments were the significant predictors <strong>of</strong><br />
poor postoperative sexual function. Seven patients (14%)<br />
presented transitory postoperative urinary dysfunction, all<br />
<strong>of</strong> whom were medically treated. Tumor <strong>stage</strong> and distance<br />
from the anal verge were independently associated with the<br />
postoperative global international prostatic symptom score<br />
(IPSS). No differences were observed in urinary quality <strong>of</strong><br />
life. The authors concluded that laparoscopic resection did<br />
not reproduce or improve on sexual and urinary dysfunction<br />
outcomes obtained in the best open TME series [18] .<br />
In another series with investigators well beyond their<br />
learning curve, urinary dysfunction was reported by 6 (6%)<br />
patients and 6 (6%) patients had sexual dysfunction, manifesting<br />
as retrograde ejaculation in four patients and erectile<br />
dysfunction in a further two patients. The low rates <strong>of</strong><br />
sexual dysfunction in this unit may be attributable to pelvic<br />
dissection only being undertaken by experienced, dedicated<br />
laparoscopic colo<strong>rectal</strong> surgeons. Previous studies reporting<br />
poorer functional outcomes have probably included a significant<br />
number <strong>of</strong> patients on the surgeons’ learning curve.<br />
CONVeRsION<br />
The conversion rate for laparoscopic <strong>rectal</strong> resection is<br />
variable between centers and levels <strong>of</strong> expertise. The MRC<br />
CLASSIC randomized trial had a conversion rate <strong>of</strong> 32%<br />
for <strong>rectal</strong> <strong>cancer</strong> [3] , yet a previous experience <strong>of</strong> only 20<br />
laparoscopic colon and <strong>rectal</strong> cases was sufficient to participate.<br />
A similar conversion rate (30%) was realized by Ng<br />
et al [11] in their ten year experience with laparoscopic <strong>rectal</strong><br />
resection. After the inception <strong>of</strong> this trial significant improvements<br />
in energy devices, ports, cameras, and stapling<br />
devices have occurred that, combined with their experience,<br />
would likely decrease their current conversion rate.<br />
Further analysis has shown that factors associated<br />
with conversion are BMI, male sex, and locally advanced<br />
tumors [19] .<br />
More recently, conversion rates reflect the beneficial<br />
impact <strong>of</strong> extensive experience. Three large retrospective<br />
series (2008-2010) have reported conversion rates as low<br />
as 5.4% [11] , 15% [15] , and 4.9% [20] . The multi-center retrospective<br />
series from Japan also demonstrated a reasonable<br />
conversion rate <strong>of</strong> 7.3% [16] .<br />
Conversion rates are as dependent on a reasonable<br />
inclusion or selection criteria as surgeon experience. Very<br />
low bulky tumors, anterior lesions in men with previous<br />
intervention for prostate <strong>cancer</strong>, T4 lesions, reoperative<br />
pelvic dissections and morbidly obese patients should be<br />
reserved for the open approach in most cases.<br />
DeFININg THe ReCTUm<br />
There has been considerable debate as to the exact length<br />
WJG|www.wjgnet.com<br />
<strong>of</strong> the rectum, the site <strong>of</strong> transition from sigmoid to rectum<br />
and most importantly the point <strong>of</strong> reference from<br />
where measurements are made. Within the surgical literature,<br />
numerous series have reported <strong>rectal</strong> <strong>cancer</strong> as being<br />
within 15, 16 and even 18 cm from the verge, although<br />
several other series use the dentate line as the reference<br />
point. Currently, the variability <strong>of</strong> these definitions not<br />
only impacts surgical decision making between centers but<br />
also the timing and need for neoadjuvant therapy, which<br />
in turn impacts oncologic outcomes and morbidity rates.<br />
There are also significant differences in practice internationally<br />
with respect to the selection criteria used for<br />
CRT. In the United States, most practitioners adhere to<br />
the NCCN guidelines that recommend neoadjuvant CRT<br />
for patients with T3 or N1 disease with tumors within<br />
10 cm <strong>of</strong> the dentate line [21] . The Mercury study group [22]<br />
has provided evidence that pre-operative MRI can accurately<br />
predict surgical resection margins. This report<br />
has led to a paradigm shift in the preoperative investigation<br />
and treatment <strong>of</strong> <strong>rectal</strong> <strong>cancer</strong> in the UK. With this<br />
approach, CRT is predominantly used when the tumor<br />
threatens or involves the meso<strong>rectal</strong> fascia and in all low<br />
<strong>rectal</strong> <strong>cancer</strong> where there is an inherent increased risk <strong>of</strong><br />
involving the CRM.<br />
Despite these apparent discrepancies most surgeons<br />
and oncologists generally agree that <strong>rectal</strong> <strong>cancer</strong> consists<br />
<strong>of</strong> extraperitoneal and intraperitoneal lesions. Tumors at<br />
or below the anterior reflection should be grouped together<br />
in investigations and are the real subject <strong>of</strong> this and<br />
other discussions surrounding laparoscopic <strong>rectal</strong> <strong>cancer</strong>.<br />
TeCHNICal IssUes<br />
The most important variable being assessed with laparoscopic<br />
vs open <strong>rectal</strong> resection for <strong>cancer</strong> is the pelvic<br />
dissection. Surgeons must analyze their own ability to<br />
perform a laparoscopic total meso<strong>rectal</strong> excision with<br />
the same precision achieved by their open technique. Although<br />
this fact seems obvious it cannot be understated.<br />
Several studies continue to populate the literature describing<br />
a “hybrid” technique. With this approach the mobilization<br />
<strong>of</strong> the left colon is performed laparoscopically<br />
and the pelvic dissection and transection <strong>of</strong> the rectum<br />
are performed through a Pfannenstiel or lower midline<br />
incision. Outcomes with this technique have been favorable<br />
and it certainly has inherent advantages but unquestionably<br />
it is not laparoscopic <strong>rectal</strong> surgery. Therefore,<br />
although published results substantiate its role, ideally it<br />
should not be included in trials or case series for laparoscopic<br />
<strong>rectal</strong> resection and should not be billed or coded<br />
as such. If this procedure continues to demonstrate favorable<br />
outcomes and has a shorter learning curve it may<br />
require its own procedure code in the future.<br />
Internationally, the straight laparoscopic approach with<br />
three or four abdominal trocar sites and a left lower quadrant<br />
or periumbilical extraction incision is preferred. Outcomes<br />
with this approach (outlined in previous section)<br />
were initially concerning but have now more consistently<br />
been favorable. As discussed above, the protracted opera-<br />
864 February 21, 2011|Volume 17|Issue 7|
tive times and concerns over both local recurrence and sexual<br />
function have been diminished with increased operative<br />
experience. This may be the most technically demanding<br />
method and surgeons preferring this technique recognize<br />
its limitations. Dividing the lower rectum, providing adequate<br />
traction low in the pelvis, and teaching trainees how<br />
to perform an appropriate total meso<strong>rectal</strong> excision are the<br />
current challenges. This procedure is less daunting for patients<br />
requiring an abdominal perineal resection. They are<br />
left without the morbidity <strong>of</strong> an abdominal wound as the<br />
specimen is routinely removed through the perineum.<br />
Proponents <strong>of</strong> hand-assisted laparoscopy in the United<br />
States continuously have demonstrated equivalent outcomes<br />
for laparoscopic colon resection with reduced operative<br />
times. More recently results with hand-assisted methods<br />
for <strong>rectal</strong> <strong>cancer</strong> have also been reported with success [23,24] .<br />
When the hand-assisted device is left in place and the pelvic<br />
dissection is performed laparoscopically these cases should<br />
be included with other minimally invasive approaches to<br />
<strong>rectal</strong> <strong>cancer</strong>. This approach may be favorable in patients<br />
with a bulky mesorectum or when additional tension is required<br />
to facilitate accurate transection <strong>of</strong> the low rectum.<br />
Dividing the rectum laparoscopically is not always<br />
technically feasible The limited angulation <strong>of</strong> the stapler<br />
and physical limitations <strong>of</strong> working in the bony confines<br />
<strong>of</strong> the pelvis are common deterrents [25] . In this situation,<br />
having an assistant apply perineal pressure may elevate the<br />
pelvic floor enough to allow the first cartridge <strong>of</strong> the stapler<br />
to reach the ano<strong>rectal</strong> junction. Furthermore, utilizing<br />
a suprapubic port or medicalizing the right lower quadrant<br />
port may help. Lastly, if these techniques are unsuccessful<br />
a limited lower midline or Pfannenstiel incision can<br />
be made and a 30 mm open stapler can be introduced. If<br />
an appropriate distal margin is not obtainable with these<br />
methods a mucosectomy with partial inter-sphincteric resection<br />
and hand-sewn coloanal anastomosis is performed.<br />
In addition to the difficulty with transection, very low<br />
anteriorly based and bulky lesions are <strong>of</strong>ten challenging.<br />
Entering the appropriate plane anterior to Denonvillier’s<br />
fascia laparoscopically, respecting the need for an adequate<br />
radial margin, and maintaining meticulous hemostasis is<br />
essential. In this location, tissue planes can be more ambiguous<br />
and any bleeding further obscures the appropriate<br />
anatomy. If there is considerable doubt that the correct<br />
tissue plane is being violated, immediate conversion is<br />
warranted. Ideally these tumors are approached by surgeons<br />
who are well past their learning curve for laparoscopic<br />
pelvic dissection.<br />
The recognition <strong>of</strong> these technical limitations and the<br />
ongoing development <strong>of</strong> advanced technology led to the<br />
introduction <strong>of</strong> robotic applications for low pelvic dissection.<br />
Data for robotic approaches to <strong>rectal</strong> <strong>cancer</strong> have<br />
recently been published and presented in national and<br />
international forums. The advantage <strong>of</strong> operating with<br />
more degrees <strong>of</strong> freedom for low <strong>rectal</strong> <strong>cancer</strong> is apparent<br />
and is <strong>of</strong> particular benefit in a narrow male pelvis. However,<br />
concerns over significantly increased cost, operative<br />
times, and training have limited its widespread adoption.<br />
Furthermore, proponents seem to be employing this<br />
WJG|www.wjgnet.com<br />
Champagne BJ et al . Evidence for laparoscopic <strong>rectal</strong> resection<br />
approach carte blanche and looking for opportunities to<br />
expand its indications rather than using it as a tool. In the<br />
era <strong>of</strong> economic constraints and limited resident exposure<br />
to cases a costly technique with ill defined training methods<br />
should be used for select cases only.<br />
CONClUsION<br />
Technical advances in the field <strong>of</strong> coloproctology have<br />
unquestionably improved patient outcomes. However,<br />
it is essential that we continue to strive to define the appropriate<br />
inclusion criteria for new approaches in regards<br />
to patient, disease, and surgeon experience. Historically,<br />
new technology, such as the PPH stapler, robotics, and<br />
laparoscopy, has become more than an optional approach<br />
or “tool”. Surgeons inherently develop extraordinary<br />
comfort with the technology and tend to expand its indications,<br />
<strong>of</strong>ten illogically. Creativity and “pushing the envelope”<br />
should not be discouraged but when it becomes<br />
apparent that new approaches become simply a “means to<br />
an end” patients outcomes may be less than ideal.<br />
The abundance <strong>of</strong> data for laparoscopic <strong>rectal</strong> resection<br />
for <strong>cancer</strong> supports its continued implantation and<br />
widespread usage by experienced surgeons for select<br />
patients. Until we become more adept at operating in the<br />
low narrow pelvis and transecting the rectum we must<br />
recognize that this approach is complementary to our<br />
open technique. To ensure the best outcomes we must<br />
continue to recognize the difference between the questions,<br />
“can you?” and “should you?” in regards to minimally<br />
invasive surgery.<br />
ReFeReNCes<br />
1 Lacy AM, García-Valdecasas JC, Delgado S, Castells A,<br />
Taurá P, Piqué JM, Visa J. Laparoscopy-assisted colectomy<br />
versus open colectomy for treatment <strong>of</strong> non-metastatic colon<br />
<strong>cancer</strong>: a randomised trial. Lancet 2002; 359: 2224-2229<br />
2 A comparison <strong>of</strong> laparoscopically assisted and open colectomy<br />
for colon <strong>cancer</strong>. N Engl J Med 2004; 350: 2050-2059<br />
3 Guillou PJ, Quirke P, Thorpe H, Walker J, Jayne DG, Smith<br />
AM, Heath RM, Brown JM. Short-term endpoints <strong>of</strong> conventional<br />
versus laparoscopic-assisted surgery in patients<br />
with colo<strong>rectal</strong> <strong>cancer</strong> (MRC CLASICC trial): multicentre,<br />
randomised controlled trial. Lancet 2005; 365: 1718-1726<br />
4 Leung KL, Kwok SP, Lam SC, Lee JF, Yiu RY, Ng SS, Lai PB,<br />
Lau WY. Laparoscopic resection <strong>of</strong> rectosigmoid carcinoma:<br />
prospective randomised trial. Lancet 2004; 363: 1187-1192<br />
5 Kennedy GD, Heise C, Rajamanickam V, Harms B, Foley EF.<br />
Laparoscopy decreases postoperative complication rates after<br />
abdominal colectomy: results from the national surgical quality<br />
improvement program. Ann Surg 2009; 249: 596-601<br />
6 Delaney CP. Outcome <strong>of</strong> discharge within 24 to 72 hours<br />
after laparoscopic colo<strong>rectal</strong> surgery. Dis Colon Rectum 2008;<br />
51: 181-185<br />
7 Lindsetmo RO, Champagne B, Delaney CP. Laparoscopic<br />
<strong>rectal</strong> resections and fast-track surgery: what can be expected?<br />
Am J Surg 2009; 197: 408-412<br />
8 Nagtegaal ID, Quirke P. What is the role for the circumferential<br />
margin in the modern treatment <strong>of</strong> <strong>rectal</strong> <strong>cancer</strong>? J<br />
Clin Oncol 2008; 26: 303-312<br />
9 Jayne DG, Guillou PJ, Thorpe H, Quirke P, Copeland J,<br />
Smith AM, Heath RM, Brown JM. Randomized trial <strong>of</strong> laparoscopic-assisted<br />
resection <strong>of</strong> colo<strong>rectal</strong> carcinoma: 3-year<br />
865 February 21, 2011|Volume 17|Issue 7|
Champagne BJ et al . Evidence for laparoscopic <strong>rectal</strong> resection<br />
results <strong>of</strong> the UK MRC CLASICC Trial Group. J Clin Oncol<br />
2007; 25: 3061-3068<br />
10 Jayne DG, Thorpe HC, Copeland J, Quirke P, Brown JM,<br />
Guillou PJ. Five-year follow-up <strong>of</strong> the Medical Research<br />
Council CLASICC trial <strong>of</strong> laparoscopically assisted versus<br />
open surgery for colo<strong>rectal</strong> <strong>cancer</strong>. Br J Surg 2010; 97:<br />
1638-1645<br />
11 Ng KH, Ng DC, Cheung HY, Wong JC, Yau KK, Chung CC,<br />
Li MK. Laparoscopic resection for <strong>rectal</strong> <strong>cancer</strong>s: lessons<br />
learned from 579 cases. Ann Surg 2009; 249: 82-86<br />
12 Lujan J, Valero G, Hernandez Q, Sanchez A, Frutos MD,<br />
Parrilla P. Randomized clinical trial comparing laparoscopic<br />
and open surgery in patients with <strong>rectal</strong> <strong>cancer</strong>. Br J Surg<br />
2009; 96: 982-989<br />
13 Ng SS, Leung KL, Lee JF, Yiu RY, Li JC, Hon SS. Long-term<br />
morbidity and oncologic outcomes <strong>of</strong> laparoscopic-assisted<br />
anterior resection for upper <strong>rectal</strong> <strong>cancer</strong>: ten-year results <strong>of</strong><br />
a prospective, randomized trial. Dis Colon Rectum 2009; 52:<br />
558-566<br />
14 Biondo S, Ortiz H, Lujan J, Codina-Cazador A, Espin E,<br />
Garcia-Granero E, Kreisler E, de Miguel M, Alos R, Echeverria<br />
A. Quality <strong>of</strong> mesorectum after laparoscopic resection<br />
for <strong>rectal</strong> <strong>cancer</strong> - results <strong>of</strong> an audited teaching programme<br />
in Spain. Colo<strong>rectal</strong> Dis 2010; 12: 24-31<br />
15 Laurent C, Leblanc F, Wütrich P, Scheffler M, Rullier E.<br />
Laparoscopic versus open surgery for <strong>rectal</strong> <strong>cancer</strong>: longterm<br />
oncologic results. Ann Surg 2009; 250: 54-61<br />
16 Miyajima N, Fukunaga M, Hasegawa H, Tanaka J, Okuda<br />
J, Watanabe M. Results <strong>of</strong> a multicenter study <strong>of</strong> 1,057 cases<br />
<strong>of</strong> <strong>rectal</strong> <strong>cancer</strong> treated by laparoscopic surgery. Surg Endosc<br />
2009; 23: 113-118<br />
17 Stamopoulos P, Theodoropoulos GE, Papailiou J, Savidis<br />
D, Golemati C, Bramis K, Panoussopoulos SG, Leandros E.<br />
Prospective evaluation <strong>of</strong> sexual function after open and<br />
laparoscopic surgery for <strong>rectal</strong> <strong>cancer</strong>. Surg Endosc 2009;<br />
Epub ahead <strong>of</strong> print<br />
WJG|www.wjgnet.com<br />
18 Morino M, Allaix ME, Giraudo G, Corno F, Garrone C.<br />
Laparoscopic versus open surgery for extraperitoneal <strong>rectal</strong><br />
<strong>cancer</strong>: a prospective comparative study. Surg Endosc 2005;<br />
19: 1460-1467<br />
19 Thorpe H, Jayne DG, Guillou PJ, Quirke P, Copeland J,<br />
Brown JM. Patient factors influencing conversion from laparoscopically<br />
assisted to open surgery for colo<strong>rectal</strong> <strong>cancer</strong>.<br />
Br J Surg 2008; 95: 199-205<br />
20 Bege T, Lelong B, Esterni B, Turrini O, Guiramand J, Francon<br />
D, Mokart D, Houvenaeghel G, Giovannini M, Delpero JR.<br />
The learning curve for the laparoscopic approach to conservative<br />
meso<strong>rectal</strong> excision for <strong>rectal</strong> <strong>cancer</strong>: lessons drawn from<br />
a single institution’s experience. Ann Surg 2010; 251: 249-253<br />
21 Engstrom PF, Arnoletti JP, Benson AB 3rd, Chen YJ, Choti<br />
MA, Cooper HS, Covey A, Dilawari RA, Early DS, Enzinger<br />
PC, Fakih MG, Fleshman J Jr, Fuchs C, Grem JL, Kiel K, Knol<br />
JA, Leong LA, Lin E, Mulcahy MF, Rao S, Ryan DP, Saltz L,<br />
Shibata D, Skibber JM, S<strong>of</strong>ocleous C, Thomas J, Venook AP,<br />
Willett C. NCCN Clinical Practice Guidelines in Oncology:<br />
<strong>rectal</strong> <strong>cancer</strong>. J Natl Compr Canc Netw 2009; 7: 838-881<br />
22 Salerno G, Daniels IR, Brown G, Heald RJ, Moran BJ. Magnetic<br />
resonance imaging pelvimetry in 186 patients with <strong>rectal</strong><br />
<strong>cancer</strong> confirms an overlap in pelvic size between males<br />
and females. Colo<strong>rectal</strong> Dis 2006; 8: 772-776<br />
23 Milsom JW, de Oliveira O Jr, Trencheva KI, Pandey S, Lee<br />
SW, Sonoda T. Long-term outcomes <strong>of</strong> patients undergoing<br />
curative laparoscopic surgery for mid and low <strong>rectal</strong> <strong>cancer</strong>.<br />
Dis Colon Rectum 2009; 52: 1215-1222<br />
24 Larson DW, Boostrom SY, Cima RR, Pemberton JH, Larson<br />
DR, Dozois EJ. Laparoscopic surgery for <strong>rectal</strong> <strong>cancer</strong>: shortterm<br />
benefits and oncologic outcomes using more than one<br />
technique. Tech Coloproctol 2010; 14: 125-131<br />
25 Brannigan AE, De Buck S, Suetens P, Penninckx F, D’Hoore<br />
A. Intracorporeal <strong>rectal</strong> stapling following laparoscopic total<br />
meso<strong>rectal</strong> excision: overcoming a challenge. Surg Endosc<br />
2006; 20: 952-955<br />
S- Editor Sun H L- Editor O’Neill M E- Editor Ma WH<br />
866 February 21, 2011|Volume 17|Issue 7|
Online Submissions: http://www.wjgnet.com/1007-9327<strong>of</strong>fice<br />
wjg@wjgnet.com<br />
doi:10.3748/wjg.v17.i7.867<br />
Advances in diagnosis, treatment and palliation <strong>of</strong><br />
pancreatic carcinoma: 1990-2010<br />
Chakshu Sharma, Karim M Eltawil, Paul D Renfrew, Mark J Walsh, Michele Molinari<br />
Chakshu Sharma, Karim M Eltawil, Paul D Renfrew, Mark J<br />
Walsh, Michele Molinari, Department <strong>of</strong> Surgery, Queen Elizabeth<br />
ІІ Health Sciences Center, Dalhousie University, Halifax,<br />
Nova Scotia, B3H 2Y9, Canada<br />
Author contributions: Sharma C, Eltawil KM and Molinari<br />
M contributed equally to this work; Sharma C performed the<br />
systematic literature review, contributed to the appraisal <strong>of</strong> the<br />
literature and wrote the paper; Eltawil KM performed the systematic<br />
literature review, contributed to the appraisal <strong>of</strong> the literature<br />
and wrote the paper; Renfrew PD and Walsh MJ contributed<br />
to the design framework <strong>of</strong> the systematic review; Molinari M<br />
performed the systematic literature review, contributed to the appraisal<br />
<strong>of</strong> the literature and wrote the paper.<br />
Correspondence to: Michele Molinari, MD, Department <strong>of</strong><br />
Surgery, Queen Elizabeth ІІ Health Sciences Center, Dalhousie<br />
University, Rm 6-254, Victoria Building, 1276 South Park Street,<br />
Halifax, Nova Scotia, B3H 2Y9,<br />
Canada. michele.molinari@cdha.nshealth.ca<br />
Telephone: +1-902-4737624 Fax: +1-902-4737639<br />
Received: October 25, 2010 Revised: December 8, 2010<br />
Accepted: December 15, 2010<br />
Published online: February 21, 2011<br />
Abstract<br />
Several advances in genetics, diagnosis and palliation<br />
<strong>of</strong> pancreatic <strong>cancer</strong> (PC) have occurred in the last decades.<br />
A multidisciplinary approach to this disease is<br />
therefore recommended. PC is relatively common as it<br />
is the fourth leading cause <strong>of</strong> <strong>cancer</strong> related mortality.<br />
Most patients present with obstructive jaundice, epigastric<br />
or back pain, weight loss and anorexia. Despite<br />
improvements in diagnostic modalities, the majority <strong>of</strong><br />
cases are still detected in advanced <strong>stage</strong>s. The only<br />
curative treatment for PC remains surgical resection. No<br />
more than 20% <strong>of</strong> patients are candidates for surgery<br />
at the time <strong>of</strong> diagnosis and survival remains quite poor<br />
as adjuvant therapies are not very effective. A small<br />
percentage <strong>of</strong> patients with borderline non-resectable<br />
PC might benefit from neo-adjuvant chemoradiation<br />
therapy enabling them to undergo resection; however,<br />
randomized controlled studies are needed to prove the<br />
WJG|www.wjgnet.com<br />
<strong>World</strong> J Gastroenterol 2011 February 21; 17(7): 867-897<br />
ISSN 1007-9327 (print) ISSN 2219-2840 (online)<br />
© 2011 Baishideng. All rights reserved.<br />
benefits <strong>of</strong> this strategy. Patients with unresectable<br />
PC benefit from palliative interventions such as biliary<br />
decompression and celiac plexus block. Further clinical<br />
trials to evaluate new chemo and radiation protocols<br />
as well as identification <strong>of</strong> genetic markers for PC are<br />
needed to improve the overall survival <strong>of</strong> patients affected<br />
by PC, as the current overall 5-year survival rate<br />
<strong>of</strong> patients affected by PC is still less than 5%. The aim<br />
<strong>of</strong> this article is to review the most recent high quality<br />
literature on this topic.<br />
© 2011 Baishideng. All rights reserved.<br />
Key words: Diagnosis; Epidemiology; Palliation; Pancreatic<br />
<strong>cancer</strong>; Therapy<br />
Peer reviewer: Hiroyuki Uehara, MD, PhD, Chief, Division <strong>of</strong><br />
Pancreatology, Department <strong>of</strong> Gastroenterology, Osaka Medical<br />
Center for Cancer and Cardiovascular Diseases, 1-3-3 Nakamichi,<br />
Higashinari, Osaka 537-8511, Japan<br />
Sharma C, Eltawil KM, Renfrew PD, Walsh MJ, Molinari M.<br />
Advances in diagnosis, treatment and palliation <strong>of</strong> pancreatic carcinoma:<br />
1990-2010. <strong>World</strong> J Gastroenterol 2011; 17(7): 867-897<br />
Available from: URL: http://www.wjgnet.com/1007-9327/full/<br />
v17/i7/867.htm DOI: http://dx.doi.org/10.3748/wjg.v17.i7.867<br />
INTRODUCTION<br />
REVIEW<br />
The vast majority (90%) <strong>of</strong> pancreatic <strong>cancer</strong>s (PC) are<br />
malignant tumors originating from pancreatic ductal cells [1] .<br />
Anatomically, 78% <strong>of</strong> PCs are located in the head, and<br />
the remaining 22% are equally distributed in the body and<br />
in the tail [2] . The most common clinical presentations are<br />
progressive weight loss and anorexia, mid abdominal pain<br />
and jaundice [3-5] . Over the past two decades many advances<br />
in the diagnosis, therapy and palliation <strong>of</strong> PC have taken<br />
place although the overall survival <strong>of</strong> affected patients has<br />
not improved significantly. The aim <strong>of</strong> this article is to review<br />
the most recent high quality literature on this topic.<br />
867 February 21, 2011|Volume 17|Issue 7|
Sharma C et al . Clinical advances in pancreatic carcinoma<br />
the risk in comparison to normal individuals [39] . This was<br />
confirmed by another study that estimated a 40% cumulative<br />
risk <strong>of</strong> PC in patients with hereditary pancreatitis<br />
by the age <strong>of</strong> 70. For patients with paternal inheritance,<br />
the cumulative risk <strong>of</strong> PC was even higher with risk up<br />
to 75% [40] . Cytokines, reactive oxygen molecules and proinflammatory<br />
compounds seem to be responsible, as inflammation<br />
is a risk factor for many other solid tumors [38] .<br />
Genetic predisposition for PC<br />
Genetic predisposing factors have been a topic <strong>of</strong> intense<br />
research in the last decades. Case reports <strong>of</strong> families with<br />
multiple affected members suggest that PC might have a<br />
hereditary background [41] . Yet, a large population study on<br />
twins identified hereditary factors for prostatic, breast and<br />
colo<strong>rectal</strong> <strong>cancer</strong>s, but not for PC [42] . A Canadian study<br />
on patients with suspected hereditary <strong>cancer</strong> syndromes<br />
found that the standardized incidence rate <strong>of</strong> PC was 4.5<br />
(CI 0.54-16.) when <strong>cancer</strong> affected one 1st degree relative,<br />
and increased to 6.4 (CI 1.8-16.4) and 32 (CI 10.4-74.7)<br />
when two and three 1st degree relatives were affected, respectively<br />
[43] . This translates to an estimated incidence <strong>of</strong><br />
PC <strong>of</strong> 41, 58 and 288 per 100 000 individuals, respectively,<br />
compared to 9 per 100 000 for the general population [44] .<br />
Brentnall et al [45] and Meckler et al [46] described examples<br />
<strong>of</strong> autosomal dominant PC in individuals presenting at<br />
early age (median age 43 years) and with high genetic penetrance<br />
(more than 80%). A mutation causing a proline<br />
(hydrophobic) to serine (hydrophilic) amino acid change<br />
(P239S) within a highly conserved region <strong>of</strong> the gene<br />
encoding paladin (PALLD) was found in all affected family<br />
members and was absent in non-affected individuals<br />
<strong>of</strong> the same family (family X). Another study has shown<br />
that the P239S mutation was only specific for family X<br />
and was not a common finding in other individuals with<br />
suspected familial PC [47] . Currently, genetic predisposition<br />
is thought to be responsible for 7% to 10% <strong>of</strong> all PC [48] .<br />
Genetic factors including germline mutations in p16/CD-<br />
KN2A [49] , BRCA2 [50-52] and STK 11 [53] genes increase the<br />
risk <strong>of</strong> PC. The combination <strong>of</strong> all these known genetic<br />
factors accounts for less than 20% <strong>of</strong> the familial aggregation<br />
<strong>of</strong> PC, suggesting the role <strong>of</strong> other additional genes.<br />
A systematic review and meta analysis <strong>of</strong> studies that<br />
quantified familial risk <strong>of</strong> PC has shown that individuals<br />
with positive family history have an almost two-fold<br />
increased risk (RR = 1.80, CI 1.48-2.12) [54] . Therefore,<br />
families with two or more cases may benefit from a comprehensive<br />
risk assessment involving collection <strong>of</strong> detailed<br />
family history information and data regarding other risk<br />
factors [55] . A case-control study <strong>of</strong> PC in two Canadian<br />
provinces (Ontario and Quebec) assessed a total <strong>of</strong> 174<br />
PC cases and 136 healthy controls that were compared for<br />
their family histories <strong>of</strong> <strong>cancer</strong>. Information regarding the<br />
ages and sites <strong>of</strong> <strong>cancer</strong> was obtained in 966 first degree<br />
relatives <strong>of</strong> the PC patients and for 903 first degree relatives<br />
<strong>of</strong> the control group. PC was the only malignancy in<br />
excess in relatives <strong>of</strong> patients with PC, compared to the<br />
control group (RR = 5, P = 0.01). The lifetime risk <strong>of</strong> PC<br />
was 4.7% for the first degree relatives and the risk was 7.2%<br />
WJG|www.wjgnet.com<br />
for relatives <strong>of</strong> patients diagnosed before the age <strong>of</strong> 60 [56] .<br />
Besides the isolated aggregation <strong>of</strong> PC in some families,<br />
several other hereditary disorders predispose to PC in<br />
known familial <strong>cancer</strong> conditions [57] . These include hereditary<br />
pancreatitis, Puetz-Jeghers syndrome, familial atypical<br />
multiple mole melanoma, familial breast and ovarian<br />
<strong>cancer</strong>, Li-Fraumeni syndrome, Fanconi anaemia, Ataxiatelangiectasia,<br />
familial adenomatous polyposis, cystic fibrosis<br />
and possible hereditary non-polyposis colon <strong>cancer</strong><br />
or Lynch syndrome [11,55,58-60] .<br />
Familial PC registries<br />
As the prognosis <strong>of</strong> PC is generally poor, there has been<br />
a strong interest in detecting genes or other markers that<br />
could help identify high risk patients at an early <strong>stage</strong>.<br />
Although a precise genetic marker for this scope is not<br />
currently available, geneticists and epidemiologists have<br />
been pr<strong>of</strong>iling traits <strong>of</strong> high risk families enrolled in registries<br />
established in North America and Europe [61] . Even<br />
if there is no standardized definition for familial PC, most<br />
authors apply the term to families with at least two first<br />
degree relatives affected by PC in the absence <strong>of</strong> other<br />
predisposing familial conditions [61] . The creation <strong>of</strong> familial<br />
PC registries has been used not only for identification<br />
<strong>of</strong> genetic mutations, but also for the screening <strong>of</strong> high<br />
risk individuals. In selected centers in North America and<br />
Europe, screening programs for high risk individuals have<br />
been implemented with the use <strong>of</strong> endoscopic ultrasound<br />
(EUS) and computed tomography (CT) scanning or magnetic<br />
resonance imaging (MRI). Such early diagnosis <strong>of</strong><br />
PC within a comprehensive screening program is hoped<br />
to ultimately result in improved survival [62] . The discovery<br />
<strong>of</strong> the genetic bases <strong>of</strong> inherited PC continues to be an<br />
active area <strong>of</strong> research, and in 2001 a multi-center linkage<br />
was formed to conduct studies aimed at the localization<br />
and identification <strong>of</strong> PC susceptibility genes (PAC-<br />
GENE) [63] . The complex nature <strong>of</strong> pedigree data makes<br />
it difficult to accurately assess risk based upon the simple<br />
counting <strong>of</strong> the number <strong>of</strong> affected family members, as<br />
it does not adjust for family size, age <strong>of</strong> onset <strong>of</strong> PC, and<br />
the exact relationship between affected family members.<br />
Therefore, computer programs have been developed to<br />
integrate these complex risk factors and pedigree data. In<br />
April 2007, the 1st risk prediction tool for PC, PanaPro<br />
was released [64] . This model provides accurate risk assessment<br />
for kindreds with familial PC as the receiver operating<br />
characteristic (ROC) curve was 0.75 which is considered<br />
good for predictive models.<br />
Nutritional status<br />
A number <strong>of</strong> studies have explored the relationship<br />
between BMI, lifestyle, diet and the risk <strong>of</strong> PC, but uncertainty<br />
regarding the strength <strong>of</strong> this relationship still<br />
exists. A recent case-control study <strong>of</strong> 841 patients and<br />
754 healthy controls showed that individuals with a BMI<br />
<strong>of</strong> 25-29.9 had an OR <strong>of</strong> 1.67 (95% CI: 1.20-2.34) in<br />
comparison to obese patients (BMI <strong>of</strong> ≥ 30) who had an<br />
OR <strong>of</strong> 2.58 (95% CI: 1.70-3.90) independently <strong>of</strong> their<br />
diabetes status [65] . The duration <strong>of</strong> being overweight was<br />
870 February 21, 2011|Volume 17|Issue 7|
Sharma C et al . Clinical advances in pancreatic carcinoma<br />
Table 3 clinico-pathological features <strong>of</strong> the most frequent classes <strong>of</strong> pancreatic <strong>cancer</strong><br />
Classification Frequency<br />
(%)<br />
DIA (incidence per 100 000 patients at risk = 8.37) [69]<br />
SPPN (incidence per 100 000 patients at risk = NA) [69]<br />
IPMN (incidence per 100 000 patients at risk = 0.03) [69]<br />
IPMN with simultaneous DIA: (incidence per 100 000 patients at risk =<br />
NA) [69]<br />
Pancreatoblastoma (incidence per 100 000 patients at risk = NA) [69]<br />
Undifferentiated (incidence per 100 000 patients at risk = 0.03) [69]<br />
Medullary carcinoma (incidence per 100 000 patients at risk = NA) [69]<br />
Mucinous cystadenocarcinoma (incidence per 100 000 patients at risk =<br />
0.43) [69]<br />
Adenosquamous carcinoma (incidence per 100 000 patients at risk =<br />
0.05) [69]<br />
Acinar cell carcinoma (incidence per 100 000 patients at risk = 0.02) [69]<br />
sible for the metabolism <strong>of</strong> β-catenin protein causing its<br />
accumulation in the cytoplasm and nucleus <strong>of</strong> neoplastic<br />
cells [94] . As a result alteration in β-catenin protein expression<br />
disrupts E-cadherin which is a key regulator <strong>of</strong> cell<br />
junctions causing poor adhesion <strong>of</strong> neoplastic cells [95] . Although<br />
there is some histological overlap between SPNN<br />
and other tumors <strong>of</strong> the pancreas, immunolabeling for<br />
β-catenin protein may help establish the diagnosis.<br />
Intraductal papillary mucinous neoplasm<br />
Intraductal papillary mucinous neoplasms (IPMNs) represent<br />
5% <strong>of</strong> all PCs and are papillary epithelial mucinproducing<br />
neoplasms arising in the main pancreatic duct<br />
or in one <strong>of</strong> its branches. IPMNs are relatively common<br />
with increasing age <strong>of</strong> the population [91] and the mean<br />
age at presentation is 65 years [96] . IPMN is a potential premalignant<br />
condition and the risks <strong>of</strong> developing invasive<br />
adenocarcinoma increase with tumor size and when originating<br />
in the main pancreatic duct.<br />
Adenocarcinoma is present in up to one-third <strong>of</strong><br />
patients with IPMN and current guidelines recommend<br />
surgical resection when IPMNs are greater than 3 cm, in<br />
the presence <strong>of</strong> main pancreatic duct dilatation and when<br />
mural nodules are detected [97] .<br />
Neoplastic cells <strong>of</strong> IPMN are columnar with gene<br />
pr<strong>of</strong>iles similar to infiltrating ductal carcinoma. About<br />
25% <strong>of</strong> patients show loss <strong>of</strong> heterozygosity <strong>of</strong> the<br />
STK11/LKB1 gene [98,99] . Other frequent gene mutations<br />
are TP53, KRAS2, and P16/CDKN2A [100] .<br />
Pancreatic intraepithelial neoplasia<br />
Pancreatic intraepithelial neoplasia (PanIN) represents a<br />
WJG|www.wjgnet.com<br />
85-90 [1]<br />
0.1-3 [73]<br />
0.50 [79]<br />
Author yr Survival (5-yr survival after<br />
surgical resection)<br />
Conlon et al [70]<br />
Winter et al [71]<br />
Poultsides et al [72]<br />
Papavramidis et al [74]<br />
Shin et al [76]<br />
5 [75]<br />
Poultsides et al [72]<br />
Fan et al [77]<br />
Sohn et al [78]<br />
Dhebri et al [80]<br />
Saif et al [79]<br />
Paal et al [82]<br />
Connolly et al [83]<br />
NA Wilentz et al [84]<br />
2-7 [81]<br />
1 Ridder et al [85]<br />
4 Madura et al [86]<br />
Mulkeen et al [87]<br />
2 Holen et al [88]<br />
1996 10%<br />
2006 18%<br />
2010 19%<br />
2005 95%<br />
2010 Benign: 95%<br />
Malignant: 64%<br />
2010 42%<br />
2010 57%<br />
2004 43%<br />
2004 50%<br />
2007 80%<br />
2001 3% (3-yr survival)<br />
1987 5 mo (average survival)<br />
2000 11%<br />
14 mo (average survival)<br />
1996 56%<br />
1999 5-7 mo (median survival)<br />
2006<br />
2002 38 mo after surgical resection<br />
(median survival)<br />
14 mo for unresectable disease<br />
(median survival)<br />
DIA: Ductal infiltrating adenocarcinoma; SPPN: Solid pseudo-papillary neoplasm; IPMN: Intraductal papillary nucinous neoplasm; NA: Not applicable.<br />
neoplastic proliferation <strong>of</strong> mucin producing epithelial cells<br />
confined to the smaller pancreatic ducts and is considered<br />
a precursor to invasive ductal carcinoma [101] .<br />
PanINs are usually characterized by lesions too small<br />
to be symptomatic or to be detected by current imaging<br />
technologies [89] . Microscopically, PanINs are classified into<br />
three grades (PanIN-1, PanIN-2 and PanIN-3) based on<br />
the progressive degree <strong>of</strong> architecture abnormality and<br />
cellular atypia [102] . PanIN-1 shows minimum cellular atypia,<br />
PanIN-2 moderate changes and PanIN-3 is equivalent to<br />
PC-in-situ. The discovery <strong>of</strong> specific molecular changes<br />
present in both PanIN and PC has helped to establish<br />
that these small lesions are the precursors to DIA [103] .<br />
Early abnormalities <strong>of</strong> IPMNs are telomerase shortening<br />
and activating point mutations in the KRAS2 gene while<br />
intermediate mutation is the activation <strong>of</strong> the p16/CD-<br />
KN2A gene and late events are alterations in the TP53,<br />
MADH4/DPC4, and BRCA2 genes [102] . The understanding<br />
that many DIAs arise from PanIN lesions has prompted<br />
screening efforts on the detection <strong>of</strong> these small and<br />
potentially curable lesions [104] .<br />
Pancreatoblastoma<br />
Pancreatoblastoma is a rare malignant tumor (0.5% <strong>of</strong><br />
PC) usually presenting in the pediatric age group. Generally,<br />
it appears as a s<strong>of</strong>t and well demarcated mass with<br />
epithelial or acinar differentiation, but <strong>of</strong>ten it has cells<br />
with endocrine and mesenchymal characteristics [79] . Most<br />
pancreato-blastomas affect children with a mean age <strong>of</strong><br />
5 years and are frequently associated with elevated levels<br />
<strong>of</strong> serum alpha fetoprotein. The median survival <strong>of</strong> patients<br />
with pancreato-blastomas is 48 mo and the 5-year<br />
872 February 21, 2011|Volume 17|Issue 7|
survival rate after successful resection is 50% (95% CI:<br />
37%-62%) [80,105] .<br />
The majority <strong>of</strong> pancreato-blastomas have loss <strong>of</strong><br />
heterozygosity <strong>of</strong> chromosome 11p from the maternal<br />
side [106] . These molecular findings unite pancreatoblastoma<br />
with other primitive neoplasms such as hepatoblastoma<br />
and nephroblastoma [107] . Genetic alterations in the adenomatous<br />
polyposis coli (APC)/β-catenin pathway have also<br />
been detected in most pancreato-blastomas including mutations<br />
in β-catenin (CTNNB1) and APC genes [107] .<br />
Undifferentiated carcinoma<br />
Undifferentiated PC (UPC) lacks differentiation direction<br />
[91] and presents with symptoms similar to patients<br />
with DIA, but has a worse prognosis as it has a more aggressive<br />
behavior and tends to metastasize and infiltrate<br />
surrounding organs in early <strong>stage</strong>s [82] . The average time<br />
from diagnosis to death is about 5 mo and only 3% <strong>of</strong><br />
patients are alive at 5 years after undergoing surgical resection.<br />
UPCs can form large locally aggressive masses and<br />
may present with severe hemorrhage and necrosis. The<br />
majority <strong>of</strong> UPCs have KRAS2 gene mutation suggesting<br />
that they arise from pre-existing ductal adenocarcinomas<br />
that transform into poorly differentiated tumors during<br />
their progression [108] .<br />
Medullary carcinoma<br />
Medullary carcinoma (MC) is a variant <strong>of</strong> PC characterized<br />
by poor differentiation and syncytial growth that has<br />
been described and recognized only in recent years [84] . Patients<br />
with MC have a better prognosis and are more likely<br />
to have a family history <strong>of</strong> any kind <strong>of</strong> <strong>cancer</strong> [109] . MC<br />
does not differ significantly from other classes <strong>of</strong> PC in its<br />
clinical presentation, age and gender. These tumors tend<br />
to form well demarcated s<strong>of</strong>t masses and microscopically<br />
they are usually poorly differentiated with pushing rather<br />
than infiltrating features [110] . Focal necrosis and intratumoral<br />
lymphocytic infiltration can be prominent similar<br />
to MC <strong>of</strong> the colon and other tumors with microsatellite<br />
instability [89] . MCs have been shown to have loss <strong>of</strong><br />
expression <strong>of</strong> one <strong>of</strong> the DNA mismatch repair proteins<br />
(M1h1 and Msh2) and mutation in the BRAF gene, which<br />
is a downstream effector <strong>of</strong> the k-ras pathway [111] . Patients<br />
with MC and their families may benefit from genetic<br />
counseling and more frequent screening for early detection<br />
<strong>of</strong> other common <strong>cancer</strong>s. The prognosis <strong>of</strong> MC is<br />
better than adenocarcinoma, although it is not responsive<br />
to adjuvant chemotherapy based on fluorouracil (5-FU),<br />
similar to colon <strong>cancer</strong> with microsatellite instability [112] .<br />
Other rare classes <strong>of</strong> PCs<br />
Mucinous cystadenocarcinoma: Malignant cystic neoplasms<br />
are rare entities that account for only 1% <strong>of</strong> all<br />
pancreatic tumors [113] . Both serous and mucinous cystic<br />
neoplasms are tumors <strong>of</strong> the exocrine pancreas with different<br />
biological behaviors. Serous cystadenomas are considered<br />
benign tumors with almost no malignant potential<br />
<strong>of</strong>ten managed expectantly unless symptomatic. However,<br />
the preoperative differentiation between a benign serous<br />
WJG|www.wjgnet.com<br />
Sharma C et al . Clinical advances in pancreatic carcinoma<br />
cystadenoma and malignant serous cystadenocarcinoma<br />
remains difficult [114] . Histologically, cystadenocarcinomas<br />
appear identical to serous cystadenomas and are distinguished<br />
only by the presence <strong>of</strong> lymphovascular invasion<br />
or metastases [115] . Mucinous cystadenocarcinomas resemble<br />
DIAs although some cell populations can present with<br />
undifferentiated features and other histological characteristics<br />
such as osteoclast-like giant cells, adenosquamous<br />
carcinoma, choriocarcinoma, or high-grade sarcoma [116-119] .<br />
Mucinous cystic neoplasms <strong>of</strong> the pancreas are slowly<br />
growing and only about 20% show invasive features [120,121] .<br />
The prognosis <strong>of</strong> cystadenocarcinoma is favorable<br />
compared to DIA with 5-year survival rates <strong>of</strong> 56% after<br />
radical resection [85] . There is limited evidence on the role<br />
<strong>of</strong> chemotherapy for cystadenocarcinomas <strong>of</strong> the pancreas<br />
as they appear to be unresponsive to current chemotherapy<br />
agents and radiation therapy [122,123] .<br />
Adenosquamous carcinoma: Adenosquamous carcinoma<br />
has previously been referred as adenoachantoma,<br />
mixed squamous and adenocarcinoma, and mucoepidermoid<br />
carcinoma. Histologically, they are characterized by<br />
mixed populations <strong>of</strong> adenomatous cells and cells with<br />
varying amount <strong>of</strong> keratinized squamous features. Usually<br />
this tumor affects patients in their seventh decade <strong>of</strong><br />
life, with symptoms and pancreatic distribution similar to<br />
DIAs. Although it is reported that adenosquamous carcinomas<br />
represents 4% <strong>of</strong> all PCs (range 3%-11%), the<br />
literature on the natural history and survival is limited to<br />
case series only [86] . The prognosis seems to be worse than<br />
DIAs, with a mean survival <strong>of</strong> 5-7 mo even after surgical<br />
resection [86,87] . Lymphovascular and perineural invasion appear<br />
to be common and early features <strong>of</strong> adenosquamous<br />
carcinomas and the role <strong>of</strong> adjuvant chemo and radiation<br />
therapy is still not clear [124] .<br />
Acinar cell carcinoma: Acinar cell carcinomas (ACCs)<br />
represent less than 2% <strong>of</strong> all pancreatic malignancies [87,88] .<br />
ACCs are predominantly constituted by neoplastic cells<br />
with immunohistochemical staining characteristic for exocrine<br />
enzymes such as trypsin, chymotripsin or lipase, and<br />
they present in older patients than DIAs and the prognosis<br />
is slightly better, although the literature is somewhat limited<br />
[125,126] . Symptoms at presentation are aspecific and include<br />
abdominal pain and weight loss that are similar to all<br />
other PCs [125] . Very rarely, patients with ACC can develop<br />
subcutaneous fat necrosis secondary to exceedingly high<br />
concentrations <strong>of</strong> serum lipase and contrary to DIAs, bile<br />
duct obstruction causing jaundice is not as common [125] .<br />
Median survival for ACC confined to the pancreas treated<br />
by surgical resection is 38 mo, whereas it is 14 mo for<br />
individuals with unresectable disease [88] . For the majority<br />
<strong>of</strong> patients, surgical management is not curative as distant<br />
recurrent disease is more frequent than in DIA, suggesting<br />
the presence <strong>of</strong> early micrometastases even when the<br />
tumors are in the early <strong>stage</strong>s [88] . Because ACCs are rare,<br />
there is a lack <strong>of</strong> studies on the role <strong>of</strong> chemotherapy, although<br />
radiation therapy seems to provide good responses<br />
in patients with regional unresectable disease [88] .<br />
873 February 21, 2011|Volume 17|Issue 7|
Sharma C et al . Clinical advances in pancreatic carcinoma<br />
DIAGNOSIS<br />
Clinical presentation<br />
Early symptoms <strong>of</strong> PC are notoriously difficult to measure<br />
as educational and economic factors influence their<br />
perception and reporting [127,128] . Cholestatic symptoms are<br />
more common in early PC <strong>of</strong> the head, while abdominal<br />
and back pain are more common in patients with distal<br />
PC and in patients with tumors infiltrating peripancreatic<br />
nerve tissue [129] . The appearance <strong>of</strong> these symptoms usually<br />
indicates advanced disease (Table 4) [129,130] .<br />
Early symptoms are usually vague such as anorexia,<br />
moderate weight loss, and early satiety [131] . Diabetes might<br />
be a sign <strong>of</strong> PC particularly when presenting during or beyond<br />
the sixth decade <strong>of</strong> life in the absence <strong>of</strong> risk factors<br />
and family history [20] . Diabetes is detected in 60% [132] to<br />
81% [133] <strong>of</strong> PC patients within two years <strong>of</strong> their diagnosis.<br />
Early detection is possible if symptoms raise clinicians’<br />
suspicion, as 25% <strong>of</strong> patients report upper abdominal discomfort<br />
up to 6 mo prior to their diagnosis [134,135] .<br />
In two European studies [128,130] , weight loss was present in<br />
66%-84% <strong>of</strong> patients, jaundice (bilirubin level > 3 mg/dL)<br />
in 56%-61%, recent onset <strong>of</strong> diabetes in 97% and distended<br />
palpable gall bladder in 12%-94%, energy loss in 86%,<br />
abdominal pain in 78%, back pain in 48%, nausea in 50%,<br />
clay-coloured stools in 54%, dark urine in 58%, jaundice in<br />
56% and pruritis in 32% <strong>of</strong> patients.<br />
Serum tumor markers<br />
Several serum tumor markers are associated with PC,<br />
however, to date, no single marker has been found to be<br />
optimal for screening.<br />
Carbohydrate antigen 19-9: Carbohydrate antigens have<br />
been used as markers for several <strong>cancer</strong>s [136,137] . The production<br />
<strong>of</strong> these antigens seems to be caused by the upregulation<br />
<strong>of</strong> glycosyl transferase genes [138] . Among these<br />
carbohydrate antigen epitopes, Sialyl Lewis a (sLe a ) detected<br />
by the 1116NS19-9 monoclonal antibody is commonly<br />
called carbohydrate antigen 19-9 (CA19-9) [139] . The serum<br />
levels <strong>of</strong> CA19-9 at the time <strong>of</strong> diagnosis and during follow-up<br />
<strong>of</strong> PC provide useful diagnostic and prognostic information<br />
[140,141] . Its sensitivity, specificity, positive predictive<br />
value (PPV), and negative predictive value (NPV) are<br />
70%-90%, 43%-91%, 72% and 81%, respectively [142-145] . A<br />
worse survival was observed in patients with pre-operative<br />
CA19-9 levels above 370 U/mL (median survival 4.4 mo<br />
vs 9.5 mo if CA19-9 < 370 U/mL, P value < 0.01) [146] . In<br />
another study, serum levels <strong>of</strong> CA19-9 > 200 U/mL were<br />
associated with a survival rate <strong>of</strong> 8 mo compared to 22 mo<br />
for patients with lower tumor antigen levels (P < 0.001) [147] .<br />
In a prospective study <strong>of</strong> patients undergoing curative<br />
resection for PC, post-operative CA19-9 < 37 U/mL<br />
was associated with a longer median and disease-free survival<br />
compared to the control group [148-150] . One <strong>of</strong> the<br />
limitations <strong>of</strong> CA19-9 is that high serum bilirubin can<br />
falsely increase its level and therefore the risk <strong>of</strong> false positive<br />
results in patients with jaundice. This is not observed<br />
for other markers such as carcinoembryonic antigen (CEA)<br />
and carbohydrate antigen 242 (CA 242) [141] .<br />
WJG|www.wjgnet.com<br />
Table 4 Presenting symptoms <strong>of</strong> advanced pancreatic <strong>cancer</strong><br />
Symptom Percentage<br />
Abdominal pain 78-82<br />
Anorexia 64<br />
Early satiety 62<br />
Jaundice 56-80<br />
Sleep disorders 54<br />
Weight loss 66-84<br />
Diabetes 97<br />
Back pain 48<br />
Nausea and weight loss 50-86<br />
CEA: CEA is part <strong>of</strong> a subgroup <strong>of</strong> glycoproteins functioning<br />
as intracellular adhesion molecules. CEA was first<br />
detected in pancreatic secretions, and several studies have<br />
shown high levels <strong>of</strong> CEA in the pancreatic juice <strong>of</strong> patients<br />
with PC [151-153] . A Japanese study found significantly<br />
higher CEA levels in the pancreatic juice <strong>of</strong> PC patients<br />
compared to those with benign pancreatic diseases. When<br />
the CEA cut <strong>of</strong>f level in pancreatic juice was 50 ng/mL,<br />
the PPV, NPV, and the accuracy for diagnosis <strong>of</strong> carcinoma<br />
were 77%, 95% and 85%, respectively. CEA levels in<br />
pancreatic juice were higher in smaller tumors in comparison<br />
to advanced PC due to the incomplete obstruction <strong>of</strong><br />
the pancreatic duct [154] . A recent study examining single vs<br />
combined efficacy <strong>of</strong> tumor markers showed that CEA (><br />
5 ng/mL) alone had a sensitivity <strong>of</strong> 45% and a specificity<br />
<strong>of</strong> 75% in comparison to CA19-9 which had a sensitivity<br />
<strong>of</strong> 80% but lower specificity (43%) (P = 0.005) [141,155] .<br />
The combination <strong>of</strong> CEA (> 5 ng/mL) and CA 19-9 (><br />
37 U/mL) decreased the sensitivity to 37%, but increased<br />
the specificity to 84%. Similarly, the combination <strong>of</strong> CEA<br />
(> 5 ng/mL) and CA242 (> 20 U/mL) decreased the<br />
sensitivity to 34% and increased the specificity to 92%.<br />
Yet, CEA and CA242 are currently not used as single tumor<br />
markers for PC, and the simultaneous use <strong>of</strong> CEA<br />
and CA19-9 provides the same information as CA19-9<br />
alone [156-158] .<br />
CA 242: CA 242, a sialylated carbohydrate was first defined<br />
by Lindholm et al in 1985 and has been used for<br />
diagnostic and prognostic purposes [159,160] . For PC, its diagnostic<br />
sensitivity and specificity are 60% (P = 0.073) and<br />
76% (P = 0.197), respectively, comparable to CEA. It also<br />
seems to be valuable in differentiating PC from benign<br />
pancreatic tumors as well as other hepatobiliary <strong>cancer</strong>s<br />
and to predict outcomes as survival rates in CA 242 positive<br />
patients are lower than those with negative serum<br />
levels (P = 0.002) [141] .<br />
In a study comparing CA 242 and CA19-9 [161] , CA<br />
242 appeared to be an independent prognostic factor for<br />
patients with resectable disease as serum levels <strong>of</strong> CA 242<br />
< 25 U/mL were associated with a significantly better<br />
survival (P < 0.05). For patients with unresectable disease,<br />
poorer outcomes were observed when CA 242 levels were<br />
> 100 U/mL.<br />
Similar results have been confirmed by Ni et al, who<br />
found that CA 242 is an independent prognostic factor<br />
874 February 21, 2011|Volume 17|Issue 7|
Table 5 Summary <strong>of</strong> the performance characteristics <strong>of</strong> serum tumor markers for the diagnosis <strong>of</strong> pancreatic <strong>cancer</strong><br />
Serum tumor marker Author Yr Sensitivity (%) Specificity (%) PPV (%) NPV (%) Accuracy (%)<br />
CA19-9 Boeck et al [141]<br />
Ni et al [142]<br />
Steinberg et al [143]<br />
Safi et al [144]<br />
Mu et al [162]<br />
CEA in pancreatic juice Ozkan et al [155]<br />
Futakawa et al [154]<br />
Ni et al [142]<br />
CEA in serum Boeck et al [141]<br />
CA19-9 + CEA Ni et al [142]<br />
Ozkan et al [155]<br />
Ma et al [163]<br />
CA 242 Nilsson et al [160]<br />
Röthlin et al [164]<br />
Carpelan-Holmström et al [165]<br />
Pålsson et al [166]<br />
CEA + CA 242 Ni et al [142]<br />
Ozkan et al [155]<br />
Hall et al [167]<br />
CA19-9 + CA 242 Ni et al [142]<br />
Röthlin et al [164]<br />
Jiang et al [158]<br />
CA19-9 + CA 242 + CEA Ni et al [142]<br />
in PC yielding more information than CA 19-9 [142,161] . In<br />
this study the use <strong>of</strong> combined tumor markers resulted in<br />
lower sensitivity, but higher specificity (Table 5). Despite<br />
these findings, CA 242 is not used in clinical practice as<br />
commonly as Ca 19-9 due to the limited number <strong>of</strong> laboratories<br />
equipped to run this test.<br />
Other tumor markers<br />
Recent studies have identified other serum molecules such<br />
as CA494 [168] , CEACAM1 [169] , PTHrP [170] , TuM2-PK [171] ,<br />
CAM 17.1 [172] and serum beta HCG [173] as potential markers<br />
for PC. Although preliminary results appear promising<br />
with sensitivity and specificity comparable and sometimes<br />
superior to CA19-9 and CEA, their clinical use has to<br />
be confirmed in larger studies and their role is currently<br />
confined to a limited number <strong>of</strong> medical centers and for<br />
research purposes.<br />
Imaging modalities<br />
Although PC may be detected with one particular diagnostic<br />
test, proper staging <strong>of</strong>ten requires the use <strong>of</strong> several<br />
imaging modalities [174] .<br />
Abdominal ultrasound: Trans-abdominal ultrasound<br />
(US) is currently used as a screening test for patients with<br />
suspected PC [175] . Its sensitivity ranges between 48% [176]<br />
and 89% [177] , specificity between 40% [178] and 91% [179] and<br />
accuracy between 46% [176] and 64% [180] . PCs measuring less<br />
than 1 cm are detected by US in only 50% <strong>of</strong> cases, while<br />
the sensitivity increases to 95.8% for tumors larger than<br />
3 cm [177] . Other factors affecting the sensitivity <strong>of</strong> US are<br />
the operator’s experience [181] and the technical character-<br />
WJG|www.wjgnet.com<br />
Sharma C et al . Clinical advances in pancreatic carcinoma<br />
2006<br />
2005<br />
1990<br />
1997<br />
2003<br />
70-90 43-91 72 81 67<br />
2003<br />
2000<br />
2005<br />
NA NA 77 95 85<br />
2006 45 75 NA NA NA<br />
2005<br />
2003<br />
2009<br />
37 84 91 90 89<br />
1992<br />
1993<br />
2002<br />
1993<br />
60 76 63 61 71<br />
2005<br />
2003<br />
1994<br />
34 92 67 90 87<br />
2005<br />
1993<br />
2004<br />
59 77 65.3 87.8 65.1<br />
2005 29 96 NA NA NA<br />
PPV: Positive predictive value; NPV: Negative predictive value; CA19-9: Carbohydrate antigen 19-9; CEA: Carcinoembryonic antigen; CA 242: Carbohydrate<br />
antigen 242; NA: Not applicable.<br />
istics <strong>of</strong> the machine. Newer US machines such as tissue<br />
harmonic imaging decrease artefacts and improve tissue<br />
contrast and therefore diagnostic accuracy [182] . US has a<br />
relatively low performance pr<strong>of</strong>ile for the staging <strong>of</strong> PC<br />
as its sensitivity for lymph node involvement only ranges<br />
between 8% [159] and 57% [177] .<br />
Color Doppler US has been used to assess the possible<br />
involvement <strong>of</strong> the portal vein and superior mesenteric<br />
vessels with a sensitivity ranging between 50% [183]<br />
and 94% [184] , specificity between 80% and 100% [183] and<br />
accuracy between 81% and 95% [175] .<br />
The recent introduction <strong>of</strong> intravenous contrast has<br />
been shown to improve evaluation <strong>of</strong> the vascularity <strong>of</strong><br />
pancreatic lesions allowing differentiation between PC and<br />
other conditions with 90% sensitivity, 100% specificity<br />
and 93% accuracy [185] . Currently, US is considered a useful<br />
imaging modality for the initial screening <strong>of</strong> PC based on<br />
its ability to document unresectability (PPV = 94%) [176] .<br />
However, the PPV for resectabiltiy is only 55% [186] , therefore,<br />
other imaging techniques are usually employed for<br />
better staging.<br />
EUS: EUS provides high resolution images <strong>of</strong> the pancreas<br />
without interference by bowel gas [187] . Despite the<br />
advancement <strong>of</strong> CT scans, EUS appears to have a higher<br />
sensitivity in detecting small PCs (98%) in comparison to<br />
CT (86%) [188] . EUS has higher sensitivity compared to CT<br />
for local tumor staging (67% vs 41%), similar sensitivity<br />
for lymph node involvement (44% vs 47%) and potential<br />
tumor resectability (68% vs 64%) [185] . EUS has a NPV<br />
<strong>of</strong> 100% for PC <strong>of</strong> the head [186,189] and an accuracy <strong>of</strong><br />
90% for the assessment <strong>of</strong> portal and splenic vein inva-<br />
875 February 21, 2011|Volume 17|Issue 7|
Sharma C et al . Clinical advances in pancreatic carcinoma<br />
sion [178,190] . On the other hand, EUS does not appear to<br />
be accurate enough in assessing the invasion <strong>of</strong> SMA and<br />
superior mesenteric vein (SMV) with a NPV <strong>of</strong> 82% and<br />
sensitivity <strong>of</strong> only 50% [191,192] .<br />
In order to improve EUS performance in PC staging,<br />
recent studies have assessed the benefits <strong>of</strong> using parenteral<br />
contrast agents. This technique has shown 92% sensitivity,<br />
100% specificity, 100% PPV, 86% NPV and 95%<br />
accuracy [193] . Although EUS is becoming a leading modality<br />
for staging and diagnosis <strong>of</strong> PC, drawbacks <strong>of</strong> this<br />
technique are the fact that it is invasive, highly operator<br />
dependent, costly and associated with a small risk <strong>of</strong> pancreatitis<br />
(0.85%) [194] , bleeding and duodenal perforation.<br />
CT: On contrast CT, PC appears as an ill-defined, hypoattenuating<br />
focal mass with dilatation <strong>of</strong> the upstream<br />
pancreatic and or biliary duct [174] . Optimum visualization<br />
<strong>of</strong> the pancreas requires imaging acquisition obtained<br />
during both arterial and portal phases [195] . Sensitivity and<br />
specificity <strong>of</strong> thin section triple phase helical CT is 77%<br />
and 100%, respectively, for lesions less than 2 cm [196] . In<br />
a multicentric trial, the diagnostic accuracy <strong>of</strong> CT for resectability<br />
was 73% with a PPV for non resectability <strong>of</strong><br />
90% [197] .<br />
With the advent <strong>of</strong> multi detector CT scanners (MDCT),<br />
the pancreas can be imaged at a very high spatial and temporal<br />
resolution [198,199] . The dual phase pancreatic protocol<br />
MDCT using 1 to 3 mm slice collimation is one <strong>of</strong> the<br />
most sensitive techniques for metastatic disease to the liver<br />
and peritoneum [186,200,201] . Recent studies have shown that<br />
MDCT has a NPV <strong>of</strong> 87% for tumor resectability compared<br />
to a NPV <strong>of</strong> 79% for conventional helical CT [202] and<br />
with an accuracy between 85% and 95% [203,204] .<br />
Images from MDCT can be used to visualize the biliary<br />
tree and normal vascular variants such as replaced hepatic<br />
arteries before surgical planning. Gangi et al [198] reported<br />
that pancreatic ductal dilatation in asymptomatic patients<br />
could be identified between 0 to 50 mo before PC diagnosis<br />
was confirmed. The sensitivity, specificity and accuracy <strong>of</strong><br />
CT in the presence <strong>of</strong> hypo-attenuated pancreatic lesions,<br />
pancreatic ductal dilatation with cut-<strong>of</strong>f, distal pancreatic<br />
atrophy, pancreatic contour abnormalities and common bile<br />
duct dilatation are reported in Table 6 [205] .<br />
Despite these improvements, interpretation <strong>of</strong> the CT<br />
scan is quite challenging in the setting <strong>of</strong> pancreatitis forming<br />
mass effects [206] and in the presence <strong>of</strong> loco-regional<br />
lymph node involvement and small hepatic metastasis [207] .<br />
Magnetic resonance imaging-magnetic resonance<br />
cholangiopancreatography: In most institutions, MRI<br />
is performed when other imaging modalities provide<br />
insufficient data for the clinical staging <strong>of</strong> the tumor, or<br />
when treatment planning can not be based on the images<br />
obtained by other techniques. Several studies have<br />
shown that MRI is superior to CT for the detection and<br />
staging <strong>of</strong> PC (100% vs 94%, respectively) [208-211] . However,<br />
recent evidence has challenged this belief. The use<br />
<strong>of</strong> MRI-magnetic resonance cholangiopancreatography<br />
(MRCP) to better characterize PC is supported by a pro-<br />
WJG|www.wjgnet.com<br />
Table 6 Sensitivity, specificity and accuracy <strong>of</strong> computed tomography<br />
findings in pancreatic <strong>cancer</strong> patients<br />
CT finding Sensitivity<br />
(%)<br />
Specificity<br />
(%)<br />
Accuracy<br />
(%)<br />
Hypoattenuation 75 84 81<br />
Ductal dilatation 50 78 70<br />
Ductal interruption 45 82 70<br />
Distal pancreatic atrophy 45 96 81<br />
Pancreatic contour anomalies 15 92 70<br />
CBD dilatation 5 92 67<br />
CT: Computed tomography; CBD: Common bile duct.<br />
spective analysis that compared these two modalities in<br />
patients with periampullary <strong>cancer</strong>s [212] . MRI-MRCP was<br />
superior to CT in differentiating malignant from benign<br />
lesions (ROC = 0.96 vs 0.81, P < 0.05) and MRI-MRCP<br />
had better sensitivity (92% vs 76%), specificity (85% vs<br />
69%), accuracy (90% vs 75%), PPV (95% vs 88%) and<br />
NPV (79% vs 50%) compared to CT. Another study<br />
confirmed the previous results with MRI-MRCP showing<br />
97% sensitivity, 81% specificity and 89% accuracy [213] .<br />
On the other hand, other studies comparing gadolinium-enhanced<br />
MRI with MDCT have shown that MRI<br />
and CT had equivalent sensitivity and specificity (83%-85%<br />
vs 83% and 63% vs 63%-75%, respectively). Both techniques<br />
had good to excellent agreement between radiologists,<br />
although MRI had a superior agreement for the<br />
evaluation <strong>of</strong> distant metastases (inter-observer agreement<br />
between MRI and CT scan; 0.78 vs 0.59 P = 0.1) [214] . On<br />
the other hand, with the improvement in CT scan technology,<br />
recent studies have shown that MRI might have<br />
lower sensitivity in comparison to MDCT (82%-94% vs<br />
100%) [215] . This was confirmed by a recent meta-analysis<br />
comparing the accuracy <strong>of</strong> several imaging modalities<br />
which showed that helical CT had superior sensitivity<br />
compared to MRI (91% vs 84%) and transabdominal US<br />
(91% vs 76%) [216] . Sensitivity for resectability <strong>of</strong> the tumor<br />
was equal for both MRI and helical CT (82% vs 81%, respectively)<br />
[216] .<br />
Positron emission tomography: 18 F-2fluoro-2-deoxy-<br />
D-glucose (FDG) accumulated by tumor cells provides<br />
positron emission tomography (PET) with the advantage<br />
<strong>of</strong> combining metabolic activity and imaging characteristics.<br />
Newly developed PET scanners can detect small<br />
PCs up to 7 mm in diameter and diagnose metastatic<br />
disease in about 40% <strong>of</strong> cases [217,218] . A Japanese study<br />
found that the overall sensitivity <strong>of</strong> PET-CT was superior<br />
to contrast CT (92% vs 88%) and that PET was better<br />
at detecting bone metastases (100% vs 12%). However,<br />
CT scanning was superior for the evaluation <strong>of</strong> vascular<br />
invasion (100% vs 22%), involvement <strong>of</strong> para aortic regional<br />
lymph nodes (78% vs 57%), identification <strong>of</strong> peritoneal<br />
dissemination (57% vs 42%) and hepatic metastases<br />
(73% vs 52%) [219] . Another Japanese study confirmed<br />
that PET had a sensitivity <strong>of</strong> 87%, a specificity <strong>of</strong> 67%<br />
and accuracy <strong>of</strong> 85%, and that tumors with metastatic<br />
876 February 21, 2011|Volume 17|Issue 7|
Table 7 Summary <strong>of</strong> the performance characteristics <strong>of</strong> imaging tests for the diagnosis <strong>of</strong> pancreatic <strong>cancer</strong><br />
Diagnostic modality Author Yr Sensitivity (%) Specificity (%) PPV (%) NPV (%) Accuracy (%)<br />
US Giovannini et al [176]<br />
Böttger et al [177]<br />
Rösch et al [178]<br />
Niederau et al [179]<br />
Palazzo et al [180]<br />
Tanaka et al [231]<br />
Doppler US Candiani et al [232]<br />
Casadei et al [184]<br />
Calculli et al [233]<br />
EUS Akahoshi et al [234]<br />
Legmann et al [235]<br />
Contrast enhanced US Dietrich et al [185]<br />
CT Bronstein et al [196]<br />
Megibow et al [197]<br />
MDCT Park et al [214]<br />
Vargas et al [202]<br />
Diehl et al [203]<br />
Schima et al [208]<br />
MRI-MRCP Andersson et al [212]<br />
PET Maemura et al [217]<br />
Delbeke et al [221]<br />
disease had significantly higher standardized uptake<br />
values [SUV = tissue concentration (millicuries/g)/injection<br />
dose (millicuries)/body weight (g)] than those without<br />
metastases [220] . PET had superior sensitivity (100%<br />
vs 65%), specificity (77% vs 61%), NPV (100% vs 31%),<br />
PPV (94% vs 87%) and accuracy (95% vs 65%) in an<br />
American study comparing PET-CT with a SUV cut <strong>of</strong>f<br />
<strong>of</strong> 2.0 vs contrast CT [221] . A recent study enrolling 59 PC<br />
patients showed similar results, with 91% PPV and 64%<br />
NPV for PET-CT. One <strong>of</strong> the most interesting results<br />
was that the clinical management <strong>of</strong> patients undergoing<br />
PET was changed in 16% <strong>of</strong> cases deemed resectable<br />
after routine staging (P = 0.031) preventing unnecessary<br />
surgery because <strong>of</strong> distant metastases [222] .<br />
Diffuse uptake <strong>of</strong> FDG is frequent in pancreatitis in<br />
comparison to PC (53% vs 3%, P < 0.001), and therefore<br />
PET is extremely useful in distinguishing these two conditions<br />
in controversial cases [218,223] . Animal studies have<br />
shown that 11 C-acetate-PET appears to be superior to<br />
FDG PET for the detection <strong>of</strong> early PC and might be<br />
useful in differentiating inflammatory processes from malignancies<br />
as 11 C-acetate-PET is less affected by the presence<br />
<strong>of</strong> inflammation in human tissues [224] .<br />
Another very important characteristic <strong>of</strong> PET-CT is<br />
its ability to provide useful information on tumor viability,<br />
and this technique also allows monitoring <strong>of</strong> tumor response<br />
to treatment [217] and the metabolic features <strong>of</strong> PET<br />
help predict the prognosis as a SUV less than 3 appears to<br />
be a positive predictive factor [222,225-229] .<br />
Similar results were found by Zimny et al [230] who<br />
showed that better survival trends were noted in patients<br />
with PC and a SUV less than 6.0 in comparison to those<br />
with a higher SUV. Sensitivity and specificity <strong>of</strong> imaging<br />
modalities are summarized in Table 7.<br />
WJG|www.wjgnet.com<br />
Sharma C et al . Clinical advances in pancreatic carcinoma<br />
1994<br />
1998<br />
1991<br />
1992<br />
1993<br />
1996<br />
1998<br />
48-95 40-91 92 100 46-64<br />
1998<br />
2002<br />
50-94 80-100 79 88 81-95<br />
1998<br />
1998<br />
98 97 94 100 90<br />
2008 90 100 100 86 93<br />
2004<br />
1995<br />
2009<br />
77 100 NA NA 73<br />
2004<br />
1998<br />
2002<br />
83-91 63-75 80 87 85-95<br />
2005 83-92 63-85 95 79 89<br />
2006<br />
1999<br />
87-100 67-77 94 100 85-95<br />
PPV: Positive predictive value; NPV: Negative predictive value; US: Ultrasound; EUS: Endoscopic ultrasound; CT: Computed tomography; MDCT: Multi<br />
detector computed tomography; PET: Positron emission tomography; NA: Not applicable; MRI: Magnetic resonance imaging.<br />
STAGING<br />
Pathological staging<br />
In the 7th edition <strong>of</strong> the American Joint Committee on<br />
Cancer the different categories <strong>of</strong> PC are classified according<br />
to only one TNM staging system, even if neuroendocrine<br />
tumors have a different biology and a better<br />
prognosis than ductal carcinomas. Yet, the TNM system<br />
provides a reasonable discrimination and prognostic validity<br />
for these patients [236] .<br />
The TNM system classifies PC into 3 clinically important<br />
categories: (1) patients with Tis-T2 PC have<br />
localized <strong>cancer</strong> within the pancreas; (2) patients with T3<br />
<strong>cancer</strong> have locally invasive disease; and (3) patients with<br />
T4 tumors have unresectable PC [237] (Table 8).<br />
Prognostic features <strong>of</strong> PC include perineural and lymphovascular<br />
invasion, elevated serum CA19-9 levels and<br />
incomplete tumor resection. Therefore, gross and microscopic<br />
assessment <strong>of</strong> the resection margins is <strong>of</strong> major<br />
importance even if it is not included in the TNM staging<br />
system. Patients undergoing resections with grossly or<br />
microscopically positive margins have no survival benefits<br />
compared to individuals undergoing palliative chemo- radiation<br />
therapy alone.<br />
Clinical staging<br />
Surgery is the only chance <strong>of</strong> cure and the presence <strong>of</strong><br />
negative resection margins <strong>of</strong> the primary tumor represent<br />
the strongest prognostic factor. Preoperative staging<br />
modalities include the combination <strong>of</strong> several imaging<br />
techniques such as CT scan, MRI, EUS, staging laparoscopy<br />
and laparoscopic ultrasound which aim to identify<br />
patients with resectable disease. There is consensus that<br />
patients with distant metastases (liver, lungs, peritoneum)<br />
877 February 21, 2011|Volume 17|Issue 7|
Table 10 Published results on laparoscopic pancreaticoduodenectomies<br />
Author Yr Patient No. Morbidity (%) Pancreatic fistula (%) Mean hospital stay Mortality (%)<br />
Kendrick et al [323]<br />
Palanivelu et al [324]<br />
Dulucq et al [325]<br />
Pugliese et al [326]<br />
that the number <strong>of</strong> lymph nodes removed during the minimally<br />
invasive procedure was significantly inferior (mean<br />
number: 5.2) in comparison to the open approach (mean<br />
number: 9.4) [333] . These findings suggest that at this time<br />
there is a lack <strong>of</strong> evidence to support oncological equipoise<br />
between laparoscopic and open resections for PC.<br />
Total pancreatectomy: Total pancreatectomy has been<br />
employed in selected patients with chronic pancreatitis [334] ,<br />
multifocal islet cell tumors or diffuse IPMN [335] . Total<br />
pancreatectomy for PC was initially proposed to avoid the<br />
risk <strong>of</strong> pancreatico-enteric leaks and to remove potential<br />
undetectable synchronous disease in other parts <strong>of</strong> the<br />
gland [336] . However, the indication <strong>of</strong> total pancreatectomy<br />
to avoid the risks <strong>of</strong> pancreatic fistulae is still controversial<br />
[337] . Improvement in operative techniques, advances<br />
in nutritional support, critical care and interventional<br />
radiology have significantly decreased the incidence <strong>of</strong><br />
life-threatening sequels <strong>of</strong> pancreaticoenteric leaks [338] .<br />
In addition, the permanent endocrine insufficiency associated<br />
with total pancreatectomy impacts enormously<br />
on the quality <strong>of</strong> life and long-term outcome <strong>of</strong> these<br />
patients [339] . Some studies have demonstrated a significant<br />
increased risk <strong>of</strong> perioperative morbidity and mortality associated<br />
with total pancreatectomy compared with PD [318] .<br />
A recent study by Reddy et al [335] showed that long-term<br />
survival rates were equivalent after total pancreatectomy<br />
and PD (19.9% vs 18.5%), supporting the fact that there is<br />
no oncological benefit <strong>of</strong> total pancreatectomy vs a more<br />
limited resection in PC. Currently, total pancreatectomy<br />
should be performed in patients with PC if it is the only<br />
oncologically sound treatment option [335] .<br />
Vascular resections and extended lymphadenectomy:<br />
With the advancement in operative techniques and perioperative<br />
management <strong>of</strong> patients with PC, more radical<br />
surgical procedures with vascular resection and extended<br />
lymphadenectomy have been proposed for selected<br />
cases [340] . The results <strong>of</strong> extended vascular and lymphatic<br />
resections remain controversial.<br />
The principal use <strong>of</strong> venous resection and reconstruction<br />
is to allow complete tumor clearance when precluded<br />
by tumor involvement <strong>of</strong> the superior mesenteric or<br />
portal vein, and when the surgeon expects to achieve a<br />
negative resection margin [341] . Post-operative morbidity<br />
and mortality rates following portal or superior mesenteric<br />
vein resections seem to be similar to those <strong>of</strong> patients<br />
with standard PD (42%-48.4% vs 47.1%, 3.2%-5.9% vs<br />
2.5%, respectively) [342,343] . Another study showed that patients<br />
undergoing pancreatic resection with venous recon-<br />
WJG|www.wjgnet.com<br />
Sharma C et al . Clinical advances in pancreatic carcinoma<br />
2010 62 42 18 7 1.6<br />
2007 42 28.6 7.1 10.2 2.4<br />
2006 25 31.8 4.5 16.2 0<br />
2008 19 31.6 15.8 18 0<br />
struction (VR) had a median survival <strong>of</strong> 22 mo compared<br />
to 20 mo for those who had classic PD (P = 0.25) [344] . In<br />
another study, a slight survival benefit was noted in patients<br />
who did not require VR (33.5%) compared to those<br />
with VR (20%, P = 0.18), although this did not reach statistical<br />
significance [345] .<br />
Pancreatectomies with major arterial resections (common<br />
hepatic artery/celiac axis and superior mesenteric<br />
artery) have been reported in recent years with acceptable<br />
outcomes. Nevertheless, arterial reconstruction during<br />
pancreatectomies remains a challenging procedure with<br />
increased risk <strong>of</strong> complications compared to classic PD<br />
and PD with VR. In addition, most PCs with arterial invasion<br />
are for the majority, advanced tumors with distant<br />
lymph node involvement and metastases, and therefore<br />
indicated only in a very select group <strong>of</strong> patients [346] . Recent<br />
data on pancreatectomies requiring arterial resections at<br />
high volume tertiary centers have shown operative mortality<br />
rates <strong>of</strong> 4.3% [346] , peri-operative mortality rates (60 d)<br />
<strong>of</strong> 17% [347] , morbidity rates <strong>of</strong> 48% [348] and 3-year survival<br />
rates <strong>of</strong> 17%-23.1%, which are much higher than for classic<br />
PD [346,347] .<br />
It has been noted that lymph node involvement outside<br />
the standard PD specimens occurs in more than 30%<br />
<strong>of</strong> cases [349] . This has led to the evaluation <strong>of</strong> the need for<br />
a more extended lymph node dissection (ELND) in the<br />
surgical management <strong>of</strong> PC. To date, the definitions <strong>of</strong> a<br />
standard lymphadenectomy as well as ELND are still not<br />
very clear [341] . A number <strong>of</strong> Japanese studies have shown<br />
an increased survival rate in patients who have undergone<br />
ELND compared to conventional PD [350-352] . However,<br />
these studies were not randomized and their data were not<br />
validated by other centers [353] .<br />
The first RCT comparing standard PD and ELND<br />
was reported by Pedrazzoli et al [354] in 1998. In this study,<br />
standard lymph node dissection was defined as the removal<br />
<strong>of</strong> lymph nodes from the anterior and posterior pancreatoduodenal<br />
region, pyloric region, biliary duct, superior<br />
and inferior pancreatic head and body. In addition to the<br />
above, ELND included removal <strong>of</strong> lymph nodes from<br />
the hepatic hilum and along the aorta from the diaphragmatic<br />
hiatus to the inferior mesenteric artery and laterally<br />
to both renal hila, with circumferential clearance <strong>of</strong> the<br />
origin <strong>of</strong> the celiac trunk and SMA. This study showed no<br />
difference in morbidity, mortality or 4-year survival rates<br />
between the two groups.<br />
Recently, a meta-analysis on standard PD and PD +<br />
ELND for PC patients showed comparable morbidity and<br />
mortality rates with a trend towards higher rates <strong>of</strong> delayed<br />
gastric emptying in the ELND group. The weighted<br />
881 February 21, 2011|Volume 17|Issue 7|
controls (P = 0.099). The two- and five-year overall survival<br />
rates were 37% and 20% for the experimental arm<br />
and 23% and 10% for the control arm (P = NS) [379] .<br />
The European Study Group for PC 1 trial (ESPAC-1)<br />
compared four groups <strong>of</strong> patients who underwent pancreatic<br />
resection; (1) surgery alone; (2) 5-FU and Leucovorin<br />
adjuvant chemotherapy; (3) combination <strong>of</strong> adjuvant<br />
radiation therapy and 5-FU chemotherapy; and (4) adjuvant<br />
chemoradiation followed by chemotherapy [380] . In this<br />
study, the five-year survival rate for patients who received<br />
adjuvant chemotherapy was 21% compared to 8% for<br />
patients who did not (P = 0.009). Patients who underwent<br />
chemoradiation therapy had an inferior five-year survival<br />
rate (10% vs 20%) in comparison to patients who did not<br />
receive radiation (P = 0.05).<br />
In 2006, the Radiation Therapy Oncology Group trial<br />
compared patients receiving adjuvant chemoradiation (5040<br />
cGy in combination with continuous 5-FU) followed by<br />
5-FU vs similar chemoradiation therapy followed by Gemcitabine.<br />
For patients affected by PC <strong>of</strong> the head, the arm<br />
treated with Gemcitabine had a superior median (18.8 mo<br />
vs 16.7 mo) and overall survival at 3 years [31% vs 21% (P<br />
= 0.047)], but with a higher incidence <strong>of</strong> toxicity (80% vs<br />
60%) [381] .<br />
In 2007, a RCT conducted in Germany and Austria<br />
(CONKO-1 [Charite Onkologie Clinical Studies in GI Cancer<br />
001]) compared patients undergoing R0 or R1 pancreatic<br />
resection alone vs resection followed by Gemcitabine-based<br />
chemotherapy. The median disease-free survival for patients<br />
treated with Gemcitabine was 13.9 mo vs 6.9 mo in the<br />
observation arm (P < 0.001), although there was no difference<br />
in the overall survival between the two groups (22 mo<br />
vs 20 mo) [382] . From the results <strong>of</strong> these studies, adjuvant<br />
chemotherapy has become the standard <strong>of</strong> care for patients<br />
who can tolerate the treatment after surgical resection.<br />
NEOADJUVANT THERAPY<br />
Neoadjuvant therapy is defined as the preoperative intervention<br />
aiming to convert unresectable PCs to resectable<br />
tumors or to increase the probability <strong>of</strong> complete microscopic<br />
tumor resection [383] . One <strong>of</strong> the limitations <strong>of</strong> the<br />
role <strong>of</strong> neoadjuvant therapy for PC is the fact that there<br />
is no standardized definition for tumor resectability and<br />
there is no data from randomized phase three trials on<br />
the benefit <strong>of</strong> neoadjuvant therapy. In addition, data from<br />
prospective and retrospective studies have several biases<br />
due to heterogeneity <strong>of</strong> inclusion and exclusion criteria,<br />
preoperative quality <strong>of</strong> imaging tests, and surgical pathology<br />
reports on lymph node involvement and resection<br />
margin status.<br />
A recent systematic review [383] evaluating retrospective<br />
and prospective studies on neoadjuvant chemo and radiation<br />
therapy from 1966 to 2009 included a total <strong>of</strong> 111<br />
studies and 4,394 patients. The results <strong>of</strong> this meta-analysis<br />
showed that the majority <strong>of</strong> patients were treated with<br />
Gemcitabine, 5-FU or oral analogue Mitomycin-c, and<br />
Platinum compounds. Patients undergoing neoadjuvant<br />
treatment received radiotherapy in the range <strong>of</strong> 24-63 Gy.<br />
WJG|www.wjgnet.com<br />
Sharma C et al . Clinical advances in pancreatic carcinoma<br />
The analysis showed that neoadjuvant treatment in patients<br />
with unresectable tumor was able to convert 33.2%<br />
<strong>of</strong> patients to resectable candidates, providing a median<br />
survival <strong>of</strong> 20.5 mo which was equivalent to patients undergoing<br />
resection followed by adjuvant therapy who had<br />
median survival <strong>of</strong> 20.1 to 23.6 mo. On the other hand,<br />
neoadjuvant therapy for patients with resectable <strong>cancer</strong><br />
did not seem to improve overall outcome.<br />
RADIATION THERAPY<br />
Persistent loco-regional disease after pancreatic surgery<br />
is a major determinant <strong>of</strong> recurrence [384] . Although there<br />
is supportive evidence for the use <strong>of</strong> adjuvant chemotherapy<br />
[380,385] , the role <strong>of</strong> adjuvant radiation remains<br />
unresolved. Generally it is believed that external-beam<br />
radiotherapy (EBRT) alone is a suboptimal treatment for<br />
locally advanced PC as most patients will die <strong>of</strong> systemic<br />
disease [386] .<br />
In the Mayo clinic clinical trial and the GITSG trial,<br />
patients who were randomized to receive EBRT only had<br />
a median survival <strong>of</strong> 5.3-6.3 mo which was inferior to<br />
EBRT plus 5-FU [387,388] .<br />
Among 210 patients who underwent surgical resection<br />
for PC [PD (73%), total and/or distal pancreatectomy<br />
(25%), Appleby procedure (2%)] followed by intraoperative<br />
electron beam radiotherapy (IOERT), some patients<br />
received a single fraction <strong>of</strong> IOERT alone (25 Gy), whereas<br />
others (30%) received additional EBRT and 54% received<br />
various forms <strong>of</strong> adjuvant chemotherapy. The study<br />
demonstrated excellent local control with the addition <strong>of</strong><br />
IOERT (75%). Despite the benefit in local control, the<br />
overall median survival was similar to other studies with<br />
adjuvant chemotherapy or chemoradiation (19 mo) [389] . A<br />
combined study <strong>of</strong> extended resection and intraoperative<br />
radiation therapy (IORT) concluded that IORT contributed<br />
to local control; however, it provided no overall survival<br />
benefits (14.6% 5-year survival) [390] .<br />
In the United States, chemoradiation with concurrent<br />
5-FU followed by Gemcitabine continues to represent the<br />
standard for adjuvant therapy <strong>of</strong> tumor <strong>of</strong> the pancreatic<br />
head. A direct comparison <strong>of</strong> chemo-radiation therapy<br />
and chemotherapy alone seems to be difficult to achieve<br />
and additive chemotherapy before or after chemo-radiation-therapy<br />
will have to be tested in randomized studies<br />
in order to determine the optimal sequencing [391] .<br />
PALLIATIVE MEASURES<br />
Palliative treatment <strong>of</strong> patients with PC plays a very important<br />
role as 80% to 90% <strong>of</strong> newly diagnosed tumors<br />
are not resectable due to local invasion or presence <strong>of</strong><br />
distal metastatic disease [392] . Median survival for patients<br />
with unresectable PC located in the head and body <strong>of</strong> the<br />
gland is approximately 7 mo, while for PC located in the<br />
tail median survival is significantly less [3 mo (P = 0.0002)],<br />
as they are usually diagnosed in more advanced <strong>stage</strong>s [393] .<br />
For these patients, relief <strong>of</strong> symptoms secondary to gastric<br />
outlet obstruction, jaundice and pain are essential to<br />
883 February 21, 2011|Volume 17|Issue 7|
Sharma C et al . Clinical advances in pancreatic carcinoma<br />
improve their quality <strong>of</strong> life and overall survival. In the<br />
past, surgical palliation was more common as the diagnosis<br />
<strong>of</strong> unresectable disease was frequently done in the<br />
operating room and patients underwent one or more <strong>of</strong><br />
the following procedures: gastric bypass, hepatico-enteric<br />
decompression and celiac plexus neurolysis for pain relief<br />
during the same surgery. With the improvement in<br />
diagnostic imaging tests, the role <strong>of</strong> surgical staging has<br />
decreased as the vast majority <strong>of</strong> patients can be currently<br />
classified as suffering from unresectable disease by noninvasive<br />
modalities such as CT and MRI or by endoscopic<br />
US. Nevertheless, there are still controversies on the best<br />
palliative strategies for these patients as there is a lack <strong>of</strong><br />
randomized controlled trials and abundant contrasting<br />
data from observational studies.<br />
Gastro-duodenal decompression<br />
There is still some controversy on the use <strong>of</strong> routine<br />
gastro-intestinal bypass for PC diagnosed as unresectable<br />
at the time <strong>of</strong> exploratory laparoscopy or laparotomy.<br />
In a large observational study <strong>of</strong> 155 patients with<br />
unresectable PC <strong>stage</strong>d by extended laparoscopy at the<br />
Memorial Sloan Kettering Cancer Center, only 4% <strong>of</strong><br />
patients required surgical intervention for gastric outlet<br />
obstruction before their death: 2 patients required open<br />
gastro-jejunal anastomosis alone and 1 patient underwent<br />
a combined gastro and hepatico-jejunostomy a few days<br />
after laparoscopy [393] . In addition, 1 patient required a<br />
percutaneous endoscopic gastrostomy for palliation <strong>of</strong><br />
gastric outlet obstruction a few weeks before demise. The<br />
authors concluded that the routine use <strong>of</strong> gastric bypass<br />
in patients with unresectable PC is not indicated. On the<br />
other hand, several other retrospective studies [394,395] have<br />
suggested that up to 25% <strong>of</strong> patients with unresectable<br />
PC would develop gastric outlet obstruction requiring surgical<br />
intervention.<br />
A recent prospective randomized trial compared 44<br />
patients who were found unresectable at the time <strong>of</strong> surgery<br />
and who underwent a retrocolic gastro-jejunostomy<br />
to 43 patients who did not [396] . The two groups had similar<br />
morbidity (32% vs 33%), mortality (0%) and hospital stay.<br />
On the other hand, patients who had gastric bypass did<br />
not develop any gastric outlet obstruction, while 19% <strong>of</strong><br />
patients in the control group did (P < 0.01). Although this<br />
study would suggest that gastric bypass should be performed<br />
in all patients found unresectable at the time <strong>of</strong><br />
surgery, the introduction <strong>of</strong> metallic self-expanding intestinal<br />
stents has changed the options for palliation.<br />
A prospective multicenter cohort study <strong>of</strong> 51 patients<br />
with malignant gastric outlet obstruction treated with selfexpandable<br />
metallic stents showed that in 98% <strong>of</strong> cases<br />
the stent was successfully deployed and that the median<br />
duration <strong>of</strong> patency was 10 mo. Only 14% <strong>of</strong> patients had<br />
stent dysfunction, and migration was observed in only 2%<br />
<strong>of</strong> cases [397] . Similar results were reported by another study<br />
from South Korea which showed a median stent patency<br />
<strong>of</strong> 385 d, and only 1% serious complications (gastrointestinal<br />
bleeding or perforation) [398] . Other observational<br />
studies have shown that compared with palliative surgery,<br />
WJG|www.wjgnet.com<br />
stent placement provides a shorter hospital stay, earlier<br />
resumption <strong>of</strong> oral intake, fewer complications and lower<br />
hospital costs [399,400] . The only randomized controlled<br />
study that compared duodenal stent and laparoscopic<br />
gastrojejunostomy favored endoscopic therapy as it was<br />
associated with less discomfort, shorter hospital stay and<br />
improved physical health scores at 1 mo [401] . In this small<br />
study, only a third <strong>of</strong> patients were alive at 1 year and no<br />
cases <strong>of</strong> stent occlusion were observed. The two groups<br />
had similar overall survival supporting equipoise between<br />
endoscopic and surgical palliation. Nevertheless, surgical<br />
palliation can still play an important role when patients<br />
have a long life-expectancy, need biliary and gastric bypass<br />
in combination with celiac neurolysis for pain control.<br />
Biliary decompression<br />
The majority <strong>of</strong> PCs occur in the head <strong>of</strong> the pancreas<br />
and obstructive jaundice is one <strong>of</strong> the early symptoms for<br />
50%-80% <strong>of</strong> patients [396] . In the past, staging laparotomy<br />
and biliary bypass were frequently performed for unresectable<br />
PC <strong>of</strong> the head [402,403] . During the last decades,<br />
the development <strong>of</strong> interventional radiology and endoscopy<br />
has allowed palliation <strong>of</strong> obstructive jaundice by<br />
the insertion <strong>of</strong> percutaneous or endoluminal stents with<br />
minimal morbidity and mortality. Currently, endoscopic<br />
biliary stenting is the treatment <strong>of</strong> choice for unresectable<br />
PC with obstructive jaundice. Percutaneous transhepatic<br />
stenting is reserved only for patients in whom endoscopic<br />
stenting has failed as it is associated with a higher complication<br />
rate than endoscopic palliation (61% vs 35%) [404,405] .<br />
High risk surgical patients are best managed by biliary<br />
stenting, however, it is still unclear whether palliative surgical<br />
biliary decompression is superior to other interventions<br />
for patients who are fit for surgery or who have a<br />
longer life expectancy. A European randomized controlled<br />
study comparing surgical biliary decompression vs endoscopic<br />
plastic stenting showed that both interventions<br />
were equally successful in palliating jaundice (95% vs 94%,<br />
respectively) and provided equal overall survival. Nevertheless,<br />
major complications (29% vs 11%) and procedurerelated<br />
mortality (14% vs 3%) were significantly higher for<br />
surgical patients [406] . In addition, surgical decompression<br />
was more expensive than stenting, although recurrent biliary<br />
obstructions and late gastric bypasses were more common<br />
in patients undergoing endoscopic treatment even<br />
if that did not reach statistical significance. Similar results<br />
were reported in a more recent Brazilian study which<br />
found that endoscopic therapy with self-expandable metallic<br />
stents was more cost-effective than surgical decompression<br />
(US$2832 vs US$3821, P = 0.031) and provided<br />
better quality <strong>of</strong> life at 30 (P = 0.04) and 60 d (P = 0.05) [407] .<br />
The only available meta-analysis <strong>of</strong> randomized controlled<br />
studies comparing surgery with endoscopic stenting included<br />
only 3 studies where none tested the use <strong>of</strong> metallic<br />
self-expanding stents [408] . Although the reintervention<br />
rate was 3% (0%-16%) in surgically treated patients compared<br />
with 36% (28%-43%) in stented patients, because<br />
<strong>of</strong> the limited number <strong>of</strong> studies with a relatively small<br />
group <strong>of</strong> patients and heterogeneous quality, the authors<br />
884 February 21, 2011|Volume 17|Issue 7|
concluded that they could not identify which treatment<br />
was preferable.<br />
The patency <strong>of</strong> biliary stents has greatly improved<br />
with the introduction <strong>of</strong> expandable metallic stents (EMS)<br />
as they <strong>of</strong>fer a larger diameter for drainage and are associated<br />
with a lower occlusion rate than plastic stents [409,410] .<br />
The concurrent use <strong>of</strong> chemotherapeutic agents in patients<br />
palliated with SEMS was thought to increase the<br />
risk for ascending cholangitis. However, a Japanese retrospective<br />
study has demonstrated that the combination<br />
<strong>of</strong> SEMS and palliative chemotherapy for unresectable<br />
PC did not change the incidence <strong>of</strong> biliary infectious<br />
complications [411] . In patients with combined biliary and<br />
duodenal obstructions, concomitant biliary and duodenal<br />
stenting is now feasible and justified as the need to repeat<br />
endoscopic therapies is rarely required even in long-term<br />
survival patients [412] .<br />
Currently, surgical biliary bypass is advocated only for<br />
patients with obstructive jaundice who fail endoscopic or<br />
percutaneous stent placement.<br />
Pain control<br />
About 70% <strong>of</strong> patients with unresectable PC develop<br />
clinically important pain during their lives [413] . Pain is the<br />
main cause <strong>of</strong> the significant drop in quality and quantity<br />
<strong>of</strong> life <strong>of</strong> these patients and good palliation is necessary as<br />
pain incidence and severity increases with disease progression<br />
[414] .<br />
For the majority <strong>of</strong> patients, pain from PC can be<br />
managed with opioid analgesics. However, approximately<br />
one third <strong>of</strong> patients experience inadequate control <strong>of</strong><br />
pain with oral analgesics alone [415] . For these patients, radiation<br />
therapy, chemotherapy and celiac plexus neurolysis<br />
have been used. Percutaneous neurolytic celiac plexus<br />
block with injection <strong>of</strong> 50%-100% ethyl alcohol under<br />
radiological guidance has become the most commonly<br />
recognized method <strong>of</strong> splanchnicectomy with a 70%-96%<br />
success rate [416] . The celiac plexus block has several advantages<br />
as it has been proven to ease pain without the side<br />
effects <strong>of</strong> opioids and can be administered intraoperatively,<br />
percutaneously, or by endoscopic ultrasonography. Recent<br />
studies have shown that endoscopic ultrasonographyguided<br />
neurolysis is effective and has minimal risk <strong>of</strong> the<br />
potentially serious complications associated with surgical<br />
or percutaneous approaches [417,418] .<br />
A recent double-blind randomized controlled study<br />
comparing patients treated with celiac plexus block vs systemic<br />
analgesic therapy showed that splanchnic neurolysis<br />
provided superior pain relief and quality <strong>of</strong> life scores, but<br />
overall opioid consumption, frequency <strong>of</strong> opioid adverse<br />
effects and overall survival did not reach statistical significance<br />
between the two groups [419] . For the majority <strong>of</strong> PC<br />
patients, pain is still controlled pharmacologically even if<br />
other modalities such as surgical thoracoscopic splanchnicectomy,<br />
epidural anesthesia, subcutaneous injection with<br />
octreotide, hyp<strong>of</strong>ractionated-accelerated radiotherapy and<br />
more recently photodynamic therapy have shown some<br />
temporary success [414,420-423] .<br />
WJG|www.wjgnet.com<br />
Sharma C et al . Clinical advances in pancreatic carcinoma<br />
Nutritional supportive care<br />
The median survival <strong>of</strong> patients with unresectable PC<br />
is 33 wk and for advanced metastatic disease is only<br />
10 wk [424] . About 90% <strong>of</strong> patients with PC have significant<br />
weight loss at the time <strong>of</strong> diagnosis and all <strong>of</strong> them<br />
develop progressive cachexia due to neoplastic metabolic<br />
derangements. Secondary events such as pancreatic exocrine<br />
insufficiency due to pancreatic duct obstruction, fat<br />
malabsorption due to biliary obstruction and poor oral caloric<br />
intake caused by nausea or gastric outlet obstruction<br />
are also responsible for the progressive weight loss. Even<br />
if weight loss has been found to have a prognostic effect<br />
on survival, most <strong>of</strong> the palliative care interventions for<br />
PC are directed at correcting biliary obstruction, gastric<br />
outlet obstruction and pain, and relatively little attention<br />
has been paid to interventions that can prevent or reduce<br />
the progressive weight loss <strong>of</strong> these patients [425] . Recently,<br />
a placebo-controlled trial comparing patients receiving<br />
enteric coated pancreatic enzyme supplements vs placebo<br />
showed that after 2 mo, patients receiving pancreatin had<br />
gained 1.2% <strong>of</strong> their body weight in comparison to controls<br />
who lost 3.7% (P = 0.02), and that they had higher<br />
daily total energy intake (8.4 MJ vs 6.6 MJ, P = 0.04) [424] .<br />
Although the Karn<strong>of</strong>sky performance status between the<br />
two groups was not different and survival analysis was not<br />
performed to determine if body weight gain translates into<br />
better prognosis, this study was the first to show an effective<br />
palliative strategy able to increase the intestinal absorptive<br />
function <strong>of</strong> patients who suffer from steatorrhea.<br />
CONCLUSION<br />
In recent decades, diagnostic modalities, and the surgical<br />
and palliative treatments <strong>of</strong> PC have clearly progressed<br />
although the overall prognosis has barely changed. The<br />
management <strong>of</strong> patients affected by PC is complex and<br />
requires expertise in many fields. Multidisciplinary teams<br />
are necessary to optimize the overall care, and palliative<br />
techniques have to be mastered as the majority <strong>of</strong> PCs are<br />
diagnosed in advanced <strong>stage</strong>s. Better outcomes are reached<br />
if PC patients are appropriately referred to tertiary centers<br />
for assessment by surgical, medical and radiation oncologists,<br />
gastroenterologists, palliative care specialists and other<br />
dedicated health care providers. Despite recent progress,<br />
there is still a very limited ability to detect PC at an early<br />
<strong>stage</strong>, and there is a need for more studies to better understand<br />
genetic predisposing factors and to discover new<br />
markers that could assist physicians in this task. Randomized<br />
controlled studies are necessary to explore the role<br />
<strong>of</strong> neo-adjuvant therapies and new protocols for adjuvant<br />
strategies in patients undergoing pancreatic resection.<br />
REFERENCES<br />
1 Cubilla AL, Fitzgerald PJ. Morphological lesions associated<br />
with human primary invasive nonendocrine pancreas <strong>cancer</strong>.<br />
Cancer Res 1976; 36: 2690-2698<br />
2 Sener SF, Fremgen A, Menck HR, Winchester DP. Pancreatic<br />
<strong>cancer</strong>: a report <strong>of</strong> treatment and survival trends for 100,313<br />
885 February 21, 2011|Volume 17|Issue 7|
Sharma C et al . Clinical advances in pancreatic carcinoma<br />
patients diagnosed from 1985-1995, using the National Cancer<br />
Database. J Am Coll Surg 1999; 189: 1-7<br />
3 Porta M, Fabregat X, Malats N, Guarner L, Carrato A, de<br />
Miguel A, Ruiz L, Jariod M, Costafreda S, Coll S, Alguacil J,<br />
Corominas JM, Solà R, Salas A, Real FX. Exocrine pancreatic<br />
<strong>cancer</strong>: symptoms at presentation and their relation to tumour<br />
site and <strong>stage</strong>. Clin Transl Oncol 2005; 7: 189-197<br />
4 Kullavanijaya P, Treeprasertsuk S, Thong-Ngam D, Kladcharoen<br />
N, Mahachai V, Suwanagool P. Adenocarcinoma <strong>of</strong><br />
the pancreas: the clinical experience <strong>of</strong> 45 histopathologically<br />
proven patients, a 6 year study. J Med Assoc Thai 2001; 84:<br />
640-647<br />
5 Elli M, Piazza E, Franzone PC, Isabella L, Poliziani D, Taschieri<br />
AM. Considerations on early diagnosis <strong>of</strong> carcinoma <strong>of</strong><br />
the pancreas. Hepatogastroenterology 2003; 50: 2205-2207<br />
6 Cook DJ, Mulrow CD, Haynes RB. Systematic reviews: synthesis<br />
<strong>of</strong> best evidence for clinical decisions. Ann Intern Med<br />
1997; 126: 376-380<br />
7 Mulrow CD, Oxman AD. Cochrane Collaboration Handbook.<br />
Oxford: Update S<strong>of</strong>tware, 1997: 1<br />
8 Downs SH, Black N. The feasibility <strong>of</strong> creating a checklist<br />
for the assessment <strong>of</strong> the methodological quality both <strong>of</strong><br />
randomised and non-randomised studies <strong>of</strong> health care interventions.<br />
J Epidemiol Community Health 1998; 52: 377-384<br />
9 Jemal A, Siegel R, Ward E, Hao Y, Xu J, Thun MJ. Cancer<br />
statistics, 2009. CA Cancer J Clin 2009; 59: 225-249<br />
10 Shaib YH, Davila JA, El-Serag HB. The epidemiology <strong>of</strong><br />
pancreatic <strong>cancer</strong> in the United States: changes below the<br />
surface. Aliment Pharmacol Ther 2006; 24: 87-94<br />
11 Ghadirian P, Lynch HT, Krewski D. Epidemiology <strong>of</strong> pancreatic<br />
<strong>cancer</strong>: an overview. Cancer Detect Prev 2003; 27: 87-93<br />
12 Lowenfels AB, Maisonneuve P. Epidemiology and risk factors<br />
for pancreatic <strong>cancer</strong>. Best Pract Res Clin Gastroenterol<br />
2006; 20: 197-209<br />
13 Neugut AI, Ahsan H, Robinson E. Pancreas <strong>cancer</strong> as a second<br />
primary malignancy. A population-based study. Cancer<br />
1995; 76: 589-592<br />
14 Lynch SM, Vrieling A, Lubin JH, Kraft P, Mendelsohn JB,<br />
Hartge P, Canzian F, Steplowski E, Arslan AA, Gross M,<br />
Helzlsouer K, Jacobs EJ, LaCroix A, Petersen G, Zheng<br />
W, Albanes D, Amundadottir L, Bingham SA, B<strong>of</strong>fetta P,<br />
Boutron-Ruault MC, Chanock SJ, Clipp S, Hoover RN, Jacobs<br />
K, Johnson KC, Kooperberg C, Luo J, Messina C, Palli D,<br />
Patel AV, Riboli E, Shu XO, Rodriguez Suarez L, Thomas G,<br />
Tjønneland A, Tobias GS, Tong E, Trichopoulos D, Virtamo J,<br />
Ye W, Yu K, Zeleniuch-Jacquette A, Bueno-de-Mesquita HB,<br />
Stolzenberg-Solomon RZ. Cigarette smoking and pancreatic<br />
<strong>cancer</strong>: a pooled analysis from the pancreatic <strong>cancer</strong> cohort<br />
consortium. Am J Epidemiol 2009; 170: 403-413<br />
15 Brand RE, Greer JB, Zolotarevsky E, Brand R, Du H, Simeone<br />
D, Zisman A, Gorchow A, Lee SY, Roy HK, Anderson<br />
MA. Pancreatic <strong>cancer</strong> patients who smoke and drink are<br />
diagnosed at younger ages. Clin Gastroenterol Hepatol 2009; 7:<br />
1007-1012<br />
16 Iodice S, Gandini S, Maisonneuve P, Lowenfels AB. Tobacco<br />
and the risk <strong>of</strong> pancreatic <strong>cancer</strong>: a review and meta-analysis.<br />
Langenbecks Arch Surg 2008; 393: 535-545<br />
17 Hassan MM, Bondy ML, Wolff RA, Abbruzzese JL, Vauthey<br />
JN, Pisters PW, Evans DB, Khan R, Chou TH, Lenzi R, Jiao L,<br />
Li D. Risk factors for pancreatic <strong>cancer</strong>: case-control study.<br />
Am J Gastroenterol 2007; 102: 2696-2707<br />
18 Permert J, Ihse I, Jorfeldt L, von Schenck H, Arnqvist HJ,<br />
Larsson J. Pancreatic <strong>cancer</strong> is associated with impaired glucose<br />
metabolism. Eur J Surg 1993; 159: 101-107<br />
19 Gullo L, Pezzilli R, Morselli-Labate AM. Diabetes and the<br />
risk <strong>of</strong> pancreatic <strong>cancer</strong>. N Engl J Med 1994; 331: 81-84<br />
20 Everhart J, Wright D. Diabetes mellitus as a risk factor for pancreatic<br />
<strong>cancer</strong>. A meta-analysis. JAMA 1995; 273: 1605-1609<br />
21 Wider<strong>of</strong>f L, Gridley G, Mellemkjaer L, Chow WH, Linet<br />
M, Keehn S, Borch-Johnsen K, Olsen JH. Cancer incidence<br />
in a population-based cohort <strong>of</strong> patients hospitalized with<br />
WJG|www.wjgnet.com<br />
diabetes mellitus in Denmark. J Natl Cancer Inst 1997; 89:<br />
1360-1365<br />
22 Gapstur SM, Gann PH, Lowe W, Liu K, Colangelo L, Dyer A.<br />
Abnormal glucose metabolism and pancreatic <strong>cancer</strong> mortality.<br />
JAMA 2000; 283: 2552-2558<br />
23 Chari ST, Leibson CL, Rabe KG, Ransom J, de Andrade M,<br />
Petersen GM. Probability <strong>of</strong> pancreatic <strong>cancer</strong> following diabetes:<br />
a population-based study. Gastroenterology 2005; 129:<br />
504-511<br />
24 Ogawa Y, Tanaka M, Inoue K, Yamaguchi K, Chijiiwa K,<br />
Mizumoto K, Tsutsu N, Nakamura Y. A prospective pancreatographic<br />
study <strong>of</strong> the prevalence <strong>of</strong> pancreatic carcinoma<br />
in patients with diabetes mellitus. Cancer 2002; 94: 2344-2349<br />
25 Huxley R, Ansary-Moghaddam A, Berrington de González<br />
A, Barzi F, Woodward M. Type-II diabetes and pancreatic<br />
<strong>cancer</strong>: a meta-analysis <strong>of</strong> 36 studies. Br J Cancer 2005; 92:<br />
2076-2083<br />
26 Yalniz M, Pour PM. Diabetes mellitus: a risk factor for pancreatic<br />
<strong>cancer</strong>? Langenbecks Arch Surg 2005; 390: 66-72<br />
27 Silverman DT, Schiffman M, Everhart J, Goldstein A, Lillemoe<br />
KD, Swanson GM, Schwartz AG, Brown LM, Greenberg<br />
RS, Schoenberg JB, Pottern LM, Hoover RN, Fraumeni JF Jr.<br />
Diabetes mellitus, other medical conditions and familial history<br />
<strong>of</strong> <strong>cancer</strong> as risk factors for pancreatic <strong>cancer</strong>. Br J Cancer<br />
1999; 80: 1830-1837<br />
28 Perrin MC, Terry MB, Kleinhaus K, Deutsch L, Yanetz R,<br />
Tiram E, Calderon R, Friedlander Y, Paltiel O, Harlap S.<br />
Gestational diabetes as a risk factor for pancreatic <strong>cancer</strong>: a<br />
prospective cohort study. BMC Med 2007; 5: 25<br />
29 Fisher WE, Boros LG, Schirmer WJ. Insulin promotes pancreatic<br />
<strong>cancer</strong>: evidence for endocrine influence on exocrine<br />
pancreatic tumors. J Surg Res 1996; 63: 310-313<br />
30 Lowenfels AB, Maisonneuve P, Cavallini G, Ammann RW,<br />
Lankisch PG, Andersen JR, Dimagno EP, Andrén-Sandberg<br />
A, Domellöf L. Pancreatitis and the risk <strong>of</strong> pancreatic <strong>cancer</strong>.<br />
International Pancreatitis Study Group. N Engl J Med 1993;<br />
328: 1433-1437<br />
31 Jiao L, Silverman DT, Schairer C, Thiébaut AC, Hollenbeck<br />
AR, Leitzmann MF, Schatzkin A, Stolzenberg-Solomon RZ.<br />
Alcohol use and risk <strong>of</strong> pancreatic <strong>cancer</strong>: the NIH-AARP<br />
Diet and Health Study. Am J Epidemiol 2009; 169: 1043-1051<br />
32 Genkinger JM, Spiegelman D, Anderson KE, Bergkvist L,<br />
Bernstein L, van den Brandt PA, English DR, Freudenheim<br />
JL, Fuchs CS, Giles GG, Giovannucci E, Hankinson SE, Horn-<br />
Ross PL, Leitzmann M, Männistö S, Marshall JR, McCullough<br />
ML, Miller AB, Reding DJ, Robien K, Rohan TE, Schatzkin A,<br />
Stevens VL, Stolzenberg-Solomon RZ, Verhage BA, Wolk A,<br />
Ziegler RG, Smith-Warner SA. Alcohol intake and pancreatic<br />
<strong>cancer</strong> risk: a pooled analysis <strong>of</strong> fourteen cohort studies. Cancer<br />
Epidemiol Biomarkers Prev 2009; 18: 765-776<br />
33 Rohrmann S, Linseisen J, Vrieling A, B<strong>of</strong>fetta P, Stolzenberg-<br />
Solomon RZ, Lowenfels AB, Jensen MK, Overvad K, Olsen<br />
A, Tjonneland A, Boutron-Ruault MC, Clavel-Chapelon F,<br />
Fagherazzi G, Misirli G, Lagiou P, Trichopoulou A, Kaaks<br />
R, Bergmann MM, Boeing H, Bingham S, Khaw KT, Allen<br />
N, Roddam A, Palli D, Pala V, Panico S, Tumino R, Vineis<br />
P, Peeters PH, Hjartåker A, Lund E, Redondo Cornejo ML,<br />
Agudo A, Arriola L, Sánchez MJ, Tormo MJ, Barricarte Gurrea<br />
A, Lindkvist B, Manjer J, Johansson I, Ye W, Slimani N,<br />
Duell EJ, Jenab M, Michaud DS, Mouw T, Riboli E, Bueno-de-<br />
Mesquita HB. Ethanol intake and the risk <strong>of</strong> pancreatic <strong>cancer</strong><br />
in the European Prospective Investigation into Cancer and<br />
Nutrition (EPIC). Cancer Causes Control 2009; 20: 785-794<br />
34 Fernandez E, La Vecchia C, Porta M, Negri E, d'Avanzo B,<br />
Boyle P. Pancreatitis and the risk <strong>of</strong> pancreatic <strong>cancer</strong>. Pancreas<br />
1995; 11: 185-189<br />
35 Silverman DT, Brown LM, Hoover RN, Schiffman M, Lillemoe<br />
KD, Schoenberg JB, Swanson GM, Hayes RB, Greenberg<br />
RS, Benichou J. Alcohol and pancreatic <strong>cancer</strong> in blacks and<br />
whites in the United States. Cancer Res 1995; 55: 4899-4905<br />
36 Bansal P, Sonnenberg A. Pancreatitis is a risk factor for pan-<br />
886 February 21, 2011|Volume 17|Issue 7|
creatic <strong>cancer</strong>. Gastroenterology 1995; 109: 247-251<br />
37 Karlson BM, Ekbom A, Josefsson S, McLaughlin JK, Fraumeni<br />
JF Jr, Nyrén O. The risk <strong>of</strong> pancreatic <strong>cancer</strong> following<br />
pancreatitis: an association due to confounding? Gastroenterology<br />
1997; 113: 587-592<br />
38 Farrow B, Evers BM. Inflammation and the development <strong>of</strong><br />
pancreatic <strong>cancer</strong>. Surg Oncol 2002; 10: 153-169<br />
39 Whitcomb DC, Applebaum S, Martin SP. Hereditary pancreatitis<br />
and pancreatic carcinoma. Ann N Y Acad Sci 1999;<br />
880: 201-209<br />
40 Lowenfels AB, Maisonneuve P, DiMagno EP, Elitsur Y,<br />
Gates LK Jr, Perrault J, Whitcomb DC. Hereditary pancreatitis<br />
and the risk <strong>of</strong> pancreatic <strong>cancer</strong>. International Hereditary<br />
Pancreatitis Study Group. J Natl Cancer Inst 1997; 89: 442-446<br />
41 Hruban RH, Petersen GM, Goggins M, Tersmette AC, Offerhaus<br />
GJ, Falatko F, Yeo CJ, Kern SE. Familial pancreatic<br />
<strong>cancer</strong>. Ann Oncol 1999; 10 Suppl 4: 69-73<br />
42 O'Brien JM. Environmental and heritable factors in the causation<br />
<strong>of</strong> <strong>cancer</strong>: analyses <strong>of</strong> cohorts <strong>of</strong> twins from Sweden,<br />
Denmark, and Finland, by P. Lichtenstein, N.V. Holm, P.K.<br />
Verkasalo, A. Iliadou, J. Kaprio, M. Koskenvuo, E. Pukkala,<br />
A. Skytthe, and K. Hemminki. N Engl J Med 343:78-84, 2000.<br />
Surv Ophthalmol 2000; 45: 167-168<br />
43 Lilley M, Gilchrist D. The hereditary spectrum <strong>of</strong> pancreatic<br />
<strong>cancer</strong>: the Edmonton experience. Can J Gastroenterol 2004;<br />
18: 17-21<br />
44 Klein AP, Brune KA, Petersen GM, Goggins M, Tersmette<br />
AC, Offerhaus GJ, Griffin C, Cameron JL, Yeo CJ, Kern S,<br />
Hruban RH. Prospective risk <strong>of</strong> pancreatic <strong>cancer</strong> in familial<br />
pancreatic <strong>cancer</strong> kindreds. Cancer Res 2004; 64: 2634-2638<br />
45 Brentnall TA, Bronner MP, Byrd DR, Haggitt RC, Kimmey<br />
MB. Early diagnosis and treatment <strong>of</strong> pancreatic dysplasia<br />
in patients with a family history <strong>of</strong> pancreatic <strong>cancer</strong>. Ann<br />
Intern Med 1999; 131: 247-255<br />
46 Meckler KA, Brentnall TA, Haggitt RC, Crispin D, Byrd DR,<br />
Kimmey MB, Bronner MP. Familial fibrocystic pancreatic<br />
atrophy with endocrine cell hyperplasia and pancreatic carcinoma.<br />
Am J Surg Pathol 2001; 25: 1047-1053<br />
47 Zogopoulos G, Rothenmund H, Eppel A, Ash C, Akbari MR,<br />
Hedley D, Narod SA, Gallinger S. The P239S palladin variant<br />
does not account for a significant fraction <strong>of</strong> hereditary<br />
or early onset pancreas <strong>cancer</strong>. Hum Genet 2007; 121: 635-637<br />
48 Lynch HT, Fitzsimmons ML, Smyrk TC, Lanspa SJ, Watson<br />
P, McClellan J, Lynch JF. Familial pancreatic <strong>cancer</strong>: clinicopathologic<br />
study <strong>of</strong> 18 nuclear families. Am J Gastroenterol<br />
1990; 85: 54-60<br />
49 Goldstein AM, Fraser MC, Struewing JP, Hussussian CJ,<br />
Ranade K, Zametkin DP, Fontaine LS, Organic SM, Dracopoli<br />
NC, Clark WH Jr. Increased risk <strong>of</strong> pancreatic <strong>cancer</strong> in<br />
melanoma-prone kindreds with p16INK4 mutations. N Engl<br />
J Med 1995; 333: 970-974<br />
50 Goggins M, Schutte M, Lu J, Moskaluk CA, Weinstein CL,<br />
Petersen GM, Yeo CJ, Jackson CE, Lynch HT, Hruban RH,<br />
Kern SE. Germline BRCA2 gene mutations in patients with<br />
apparently sporadic pancreatic carcinomas. Cancer Res 1996;<br />
56: 5360-5364<br />
51 Hahn SA, Greenhalf B, Ellis I, Sina-Frey M, Rieder H, Korte B,<br />
Gerdes B, Kress R, Ziegler A, Raeburn JA, Campra D, Grützmann<br />
R, Rehder H, Rothmund M, Schmiegel W, Neoptolemos<br />
JP, Bartsch DK. BRCA2 germline mutations in familial<br />
pancreatic carcinoma. J Natl Cancer Inst 2003; 95: 214-221<br />
52 Murphy KM, Brune KA, Griffin C, Sollenberger JE, Petersen<br />
GM, Bansal R, Hruban RH, Kern SE. Evaluation <strong>of</strong> candidate<br />
genes MAP2K4, MADH4, ACVR1B, and BRCA2 in familial<br />
pancreatic <strong>cancer</strong>: deleterious BRCA2 mutations in 17%.<br />
Cancer Res 2002; 62: 3789-3793<br />
53 Su GH, Hruban RH, Bansal RK, Bova GS, Tang DJ, Shekher<br />
MC, Westerman AM, Entius MM, Goggins M, Yeo CJ, Kern<br />
SE. Germline and somatic mutations <strong>of</strong> the STK11/LKB1<br />
Peutz-Jeghers gene in pancreatic and biliary <strong>cancer</strong>s. Am J<br />
Pathol 1999; 154: 1835-1840<br />
WJG|www.wjgnet.com<br />
Sharma C et al . Clinical advances in pancreatic carcinoma<br />
54 Permuth-Wey J, Egan KM. Family history is a significant<br />
risk factor for pancreatic <strong>cancer</strong>: results from a systematic<br />
review and meta-analysis. Fam Cancer 2009; 8: 109-117<br />
55 Shi C, Hruban RH, Klein AP. Familial pancreatic <strong>cancer</strong>.<br />
Arch Pathol Lab Med 2009; 133: 365-374<br />
56 Ghadirian P, Liu G, Gallinger S, Schmocker B, Paradis AJ,<br />
Lal G, Brunet JS, Foulkes WD, Narod SA. Risk <strong>of</strong> pancreatic<br />
<strong>cancer</strong> among individuals with a family history <strong>of</strong> <strong>cancer</strong> <strong>of</strong><br />
the pancreas. Int J Cancer 2002; 97: 807-810<br />
57 Bartsch DK, Kress R, Sina-Frey M, Grützmann R, Gerdes<br />
B, Pilarsky C, Heise JW, Schulte KM, Colombo-Benkmann<br />
M, Schleicher C, Witzigmann H, Pridöhl O, Ghadimi MB,<br />
Horstmann O, von Bernstorff W, Jochimsen L, Schmidt J, Eisold<br />
S, Estévéz-Schwarz L, Hahn SA, Schulmann K, Böck W,<br />
Gress TM, Zügel N, Breitschaft K, Prenzel K, Messmann H,<br />
Endlicher E, Schneider M, Ziegler A, Schmiegel W, Schäfer<br />
H, Rothmund M, Rieder H. Prevalence <strong>of</strong> familial pancreatic<br />
<strong>cancer</strong> in Germany. Int J Cancer 2004; 110: 902-906<br />
58 Bartsch DK. Familial pancreatic <strong>cancer</strong>. Br J Surg 2003; 90:<br />
386-387<br />
59 Landi S. Genetic predisposition and environmental risk factors<br />
to pancreatic <strong>cancer</strong>: A review <strong>of</strong> the literature. Mutat<br />
Res 2009; 681: 299-307<br />
60 van der Heijden MS, Yeo CJ, Hruban RH, Kern SE. Fanconi<br />
anemia gene mutations in young-onset pancreatic <strong>cancer</strong>.<br />
Cancer Res 2003; 63: 2585-2588<br />
61 Rieder H, Sina-Frey M, Ziegler A, Hahn SA, Przypadlo E,<br />
Kress R, Gerdes B, Colombo Benkmann M, Eberl T, Grützmann<br />
R, Lörken M, Schmidt J, Bartsch DK. German national<br />
case collection <strong>of</strong> familial pancreatic <strong>cancer</strong> - clinicalgenetic<br />
analysis <strong>of</strong> the first 21 families. Onkologie 2002; 25:<br />
262-266<br />
62 Hruban RH, Canto MI, Yeo CJ. Prevention <strong>of</strong> pancreatic<br />
<strong>cancer</strong> and strategies for management <strong>of</strong> familial pancreatic<br />
<strong>cancer</strong>. Dig Dis 2001; 19: 76-84<br />
63 Petersen GM, de Andrade M, Goggins M, Hruban RH,<br />
Bondy M, Korczak JF, Gallinger S, Lynch HT, Syngal S, Rabe<br />
KG, Seminara D, Klein AP. Pancreatic <strong>cancer</strong> genetic epidemiology<br />
consortium. Cancer Epidemiol Biomarkers Prev 2006;<br />
15: 704-710<br />
64 Wang W, Chen S, Brune KA, Hruban RH, Parmigiani G,<br />
Klein AP. PancPRO: risk assessment for individuals with<br />
a family history <strong>of</strong> pancreatic <strong>cancer</strong>. J Clin Oncol 2007; 25:<br />
1417-1422<br />
65 Li D, Morris JS, Liu J, Hassan MM, Day RS, Bondy ML, Abbruzzese<br />
JL. Body mass index and risk, age <strong>of</strong> onset, and<br />
survival in patients with pancreatic <strong>cancer</strong>. JAMA 2009; 301:<br />
2553-2562<br />
66 Patel AV, Rodriguez C, Bernstein L, Chao A, Thun MJ,<br />
Calle EE. Obesity, recreational physical activity, and risk <strong>of</strong><br />
pancreatic <strong>cancer</strong> in a large U.S. Cohort. Cancer Epidemiol<br />
Biomarkers Prev 2005; 14: 459-466<br />
67 Larsson SC, Permert J, Håkansson N, Näslund I, Bergkvist L,<br />
Wolk A. Overall obesity, abdominal adiposity, diabetes and<br />
cigarette smoking in relation to the risk <strong>of</strong> pancreatic <strong>cancer</strong><br />
in two Swedish population-based cohorts. Br J Cancer 2005;<br />
93: 1310-1315<br />
68 Berrington de González A, Spencer EA, Bueno-de-Mesquita<br />
HB, Roddam A, Stolzenberg-Solomon R, Halkjaer J,<br />
Tjønneland A, Overvad K, Clavel-Chapelon F, Boutron-<br />
Ruault MC, Boeing H, Pischon T, Linseisen J, Rohrmann S,<br />
Trichopoulou A, Benetou V, Papadimitriou A, Pala V, Palli<br />
D, Panico S, Tumino R, Vineis P, Boshuizen HC, Ocke MC,<br />
Peeters PH, Lund E, Gonzalez CA, Larrañaga N, Martinez-<br />
Garcia C, Mendez M, Navarro C, Quirós JR, Tormo MJ,<br />
Hallmans G, Ye W, Bingham SA, Khaw KT, Allen N, Key TJ,<br />
Jenab M, Norat T, Ferrari P, Riboli E. Anthropometry, physical<br />
activity, and the risk <strong>of</strong> pancreatic <strong>cancer</strong> in the European<br />
prospective investigation into <strong>cancer</strong> and nutrition. Cancer<br />
Epidemiol Biomarkers Prev 2006; 15: 879-885<br />
69 Fitzgerald TL, Hickner ZJ, Schmitz M, Kort EJ. Changing<br />
887 February 21, 2011|Volume 17|Issue 7|
Sharma C et al . Clinical advances in pancreatic carcinoma<br />
incidence <strong>of</strong> pancreatic neoplasms: a 16-year review <strong>of</strong> statewide<br />
tumor registry. Pancreas 2008; 37: 134-138<br />
70 Conlon KC, Klimstra DS, Brennan MF. Long-term survival<br />
after curative resection for pancreatic ductal adenocarcinoma.<br />
Clinicopathologic analysis <strong>of</strong> 5-year survivors. Ann Surg<br />
1996; 223: 273-279<br />
71 Winter JM, Cameron JL, Campbell KA, Arnold MA, Chang<br />
DC, Coleman J, Hodgin MB, Sauter PK, Hruban RH, Riall<br />
TS, Schulick RD, Choti MA, Lillemoe KD, Yeo CJ. 1423<br />
pancreaticoduodenectomies for pancreatic <strong>cancer</strong>: A singleinstitution<br />
experience. J Gastrointest Surg 2006; 10: 1199-1210;<br />
discussion 1210-1211<br />
72 Poultsides GA, Reddy S, Cameron JL, Hruban RH, Pawlik<br />
TM, Ahuja N, Jain A, Edil BH, Iacobuzio-Donahue CA,<br />
Schulick RD, Wolfgang CL. Histopathologic basis for the<br />
favorable survival after resection <strong>of</strong> intraductal papillary<br />
mucinous neoplasm-associated invasive adenocarcinoma <strong>of</strong><br />
the pancreas. Ann Surg 2010; 251: 470-476<br />
73 Mortenson MM, Katz MH, Tamm EP, Bhutani MS, Wang H,<br />
Evans DB, Fleming JB. Current diagnosis and management<br />
<strong>of</strong> unusual pancreatic tumors. Am J Surg 2008; 196: 100-113<br />
74 Papavramidis T, Papavramidis S. Solid pseudopapillary<br />
tumors <strong>of</strong> the pancreas: review <strong>of</strong> 718 patients reported in<br />
English literature. J Am Coll Surg 2005; 200: 965-972<br />
75 Chadwick B, Willmore-Payne C, Tripp S, Layfield LJ,<br />
Hirschowitz S, Holden J. Histologic, immunohistochemical,<br />
and molecular classification <strong>of</strong> 52 IPMNs <strong>of</strong> the pancreas.<br />
Appl Immunohistochem Mol Morphol 2009; 17: 31-39<br />
76 Shin SH, Han DJ, Park KT, Kim YH, Park JB, Kim SC. Validating<br />
a simple scoring system to predict malignancy and<br />
invasiveness <strong>of</strong> intraductal papillary mucinous neoplasms <strong>of</strong><br />
the pancreas. <strong>World</strong> J Surg 2010; 34: 776-783<br />
77 Fan F, Lai EC, Xie F, Yang JM, Xu F, Kan T, Shen RX, Yang<br />
XY, Lau Wan Y, Wu MC. Intraductal papillary mucinous<br />
neoplasms <strong>of</strong> the pancreas--predictors <strong>of</strong> malignancy. Hepatogastroenterology<br />
2010; 57: 635-639<br />
78 Sohn TA, Yeo CJ, Cameron JL, Hruban RH, Fukushima N,<br />
Campbell KA, Lillemoe KD. Intraductal papillary mucinous<br />
neoplasms <strong>of</strong> the pancreas: an updated experience. Ann Surg<br />
2004; 239: 788-797; discussion 797-799<br />
79 Saif MW. Pancreatoblastoma. JOP 2007; 8: 55-63<br />
80 Dhebri AR, Connor S, Campbell F, Ghaneh P, Sutton R,<br />
Neoptolemos JP. Diagnosis, treatment and outcome <strong>of</strong> pancreatoblastoma.<br />
Pancreatology 2004; 4: 441-451; discussion<br />
452-453<br />
81 Chen J, Baithun SI. Morphological study <strong>of</strong> 391 cases <strong>of</strong> exocrine<br />
pancreatic tumours with special reference to the classification<br />
<strong>of</strong> exocrine pancreatic carcinoma. J Pathol 1985; 146:<br />
17-29<br />
82 Paal E, Thompson LD, Frommelt RA, Przygodzki RM, Heffess<br />
CS. A clinicopathologic and immunohistochemical<br />
study <strong>of</strong> 35 anaplastic carcinomas <strong>of</strong> the pancreas with a review<br />
<strong>of</strong> the literature. Ann Diagn Pathol 2001; 5: 129-140<br />
83 Connolly MM, Dawson PJ, Michelassi F, Moossa AR, Lowenstein<br />
F. Survival in 1001 patients with carcinoma <strong>of</strong> the<br />
pancreas. Ann Surg 1987; 206: 366-373<br />
84 Wilentz RE, Goggins M, Redston M, Marcus VA, Adsay NV,<br />
Sohn TA, Kadkol SS, Yeo CJ, Choti M, Zahurak M, Johnson<br />
K, Tascilar M, Offerhaus GJ, Hruban RH, Kern SE. Genetic,<br />
immunohistochemical, and clinical features <strong>of</strong> medullary<br />
carcinoma <strong>of</strong> the pancreas: A newly described and characterized<br />
entity. Am J Pathol 2000; 156: 1641-1651<br />
85 Ridder GJ, Maschek H, Klempnauer J. Favourable prognosis<br />
<strong>of</strong> cystadeno- over adenocarcinoma <strong>of</strong> the pancreas after curative<br />
resection. Eur J Surg Oncol 1996; 22: 232-236<br />
86 Madura JA, Jarman BT, Doherty MG, Yum MN, Howard TJ.<br />
Adenosquamous carcinoma <strong>of</strong> the pancreas. Arch Surg 1999;<br />
134: 599-603<br />
87 Mulkeen AL, Yoo PS, Cha C. Less common neoplasms <strong>of</strong><br />
the pancreas. <strong>World</strong> J Gastroenterol 2006; 12: 3180-3185<br />
88 Holen KD, Klimstra DS, Hummer A, Gonen M, Conlon K,<br />
WJG|www.wjgnet.com<br />
Brennan M, Saltz LB. Clinical characteristics and outcomes<br />
from an institutional series <strong>of</strong> acinar cell carcinoma <strong>of</strong> the<br />
pancreas and related tumors. J Clin Oncol 2002; 20: 4673-4678<br />
89 Shi C, Daniels JA, Hruban RH. Molecular characterization <strong>of</strong><br />
pancreatic neoplasms. Adv Anat Pathol 2008; 15: 185-195<br />
90 Liu F. SMAD4/DPC4 and pancreatic <strong>cancer</strong> survival. Commentary<br />
re: M. Tascilar et al., The SMAD4 protein and<br />
prognosis <strong>of</strong> pancreatic ductal adenocarcinoma. Clin. Cancer<br />
Res., 7: 4115-4121, 2001. Clin Cancer Res 2001; 7: 3853-3856<br />
91 Hurban RH, Pitman MB, Klimstra DS. Tumors <strong>of</strong> the pancreas.<br />
Atlas <strong>of</strong> tumor pathology. Washington DC: American<br />
Registry <strong>of</strong> Pathology and Armed forces Institute <strong>of</strong> Patholgy,<br />
2007<br />
92 Klimstra DS, Wenig BM, Heffess CS. Solid-pseudopapillary<br />
tumor <strong>of</strong> the pancreas: a typically cystic carcinoma <strong>of</strong> low<br />
malignant potential. Semin Diagn Pathol 2000; 17: 66-80<br />
93 Abraham SC, Klimstra DS, Wilentz RE, Yeo CJ, Conlon K,<br />
Brennan M, Cameron JL, Wu TT, Hruban RH. Solid-pseudopapillary<br />
tumors <strong>of</strong> the pancreas are genetically distinct from<br />
pancreatic ductal adenocarcinomas and almost always harbor<br />
beta-catenin mutations. Am J Pathol 2002; 160: 1361-1369<br />
94 Tanaka Y, Kato K, Notohara K, Hojo H, Ijiri R, Miyake T,<br />
Nagahara N, Sasaki F, Kitagawa N, Nakatani Y, Kobayashi<br />
Y. Frequent beta-catenin mutation and cytoplasmic/nuclear<br />
accumulation in pancreatic solid-pseudopapillary neoplasm.<br />
Cancer Res 2001; 61: 8401-8404<br />
95 El-Bahrawy MA, Rowan A, Horncastle D, Tomlinson I,<br />
Theis BA, Russell RC, Stamp G. E-cadherin/catenin complex<br />
status in solid pseudopapillary tumor <strong>of</strong> the pancreas. Am J<br />
Surg Pathol 2008; 32: 1-7<br />
96 Laffan TA, Horton KM, Klein AP, Berlanstein B, Siegelman<br />
SS, Kawamoto S, Johnson PT, Fishman EK, Hruban RH.<br />
Prevalence <strong>of</strong> unsuspected pancreatic cysts on MDCT. AJR<br />
Am J Roentgenol 2008; 191: 802-807<br />
97 Tanaka M, Chari S, Adsay V, Fernandez-del Castillo C,<br />
Falconi M, Shimizu M, Yamaguchi K, Yamao K, Matsuno S.<br />
International consensus guidelines for management <strong>of</strong> intraductal<br />
papillary mucinous neoplasms and mucinous cystic<br />
neoplasms <strong>of</strong> the pancreas. Pancreatology 2006; 6: 17-32<br />
98 Schönleben F, Qiu W, Ciau NT, Ho DJ, Li X, Allendorf JD,<br />
Remotti HE, Su GH. PIK3CA mutations in intraductal papillary<br />
mucinous neoplasm/carcinoma <strong>of</strong> the pancreas. Clin<br />
Cancer Res 2006; 12: 3851-3855<br />
99 Sato N, Rosty C, Jansen M, Fukushima N, Ueki T, Yeo CJ,<br />
Cameron JL, Iacobuzio-Donahue CA, Hruban RH, Goggins<br />
M. STK11/LKB1 Peutz-Jeghers gene inactivation in intraductal<br />
papillary-mucinous neoplasms <strong>of</strong> the pancreas. Am J<br />
Pathol 2001; 159: 2017-2022<br />
100 Iacobuzio-Donahue CA, Klimstra DS, Adsay NV, Wilentz<br />
RE, Argani P, Sohn TA, Yeo CJ, Cameron JL, Kern SE, Hruban<br />
RH. Dpc-4 protein is expressed in virtually all human<br />
intraductal papillary mucinous neoplasms <strong>of</strong> the pancreas:<br />
comparison with conventional ductal adenocarcinomas. Am<br />
J Pathol 2000; 157: 755-761<br />
101 Hruban RH, Adsay NV, Albores-Saavedra J, Compton C,<br />
Garrett ES, Goodman SN, Kern SE, Klimstra DS, Klöppel G,<br />
Longnecker DS, Lüttges J, Offerhaus GJ. Pancreatic intraepithelial<br />
neoplasia: a new nomenclature and classification<br />
system for pancreatic duct lesions. Am J Surg Pathol 2001; 25:<br />
579-586<br />
102 Wilentz RE, Iacobuzio-Donahue CA, Argani P, McCarthy<br />
DM, Parsons JL, Yeo CJ, Kern SE, Hruban RH. Loss <strong>of</strong> expression<br />
<strong>of</strong> Dpc4 in pancreatic intraepithelial neoplasia:<br />
evidence that DPC4 inactivation occurs late in neoplastic<br />
progression. Cancer Res 2000; 60: 2002-2006<br />
103 Maitra A, Hruban RH. Pancreatic <strong>cancer</strong>. Annu Rev Pathol<br />
2008; 3: 157-188<br />
104 Canto MI, Goggins M, Hruban RH, Petersen GM, Giardiello<br />
FM, Yeo C, Fishman EK, Brune K, Axilbund J, Griffin C, Ali S,<br />
Richman J, Jagannath S, Kantsevoy SV, Kalloo AN. Screening<br />
for early pancreatic neoplasia in high-risk individuals: a<br />
888 February 21, 2011|Volume 17|Issue 7|
prospective controlled study. Clin Gastroenterol Hepatol 2006;<br />
4: 766-781; quiz 665<br />
105 Klimstra DS, Longnecker DS. Acinar cell carcinoma. In:<br />
Hamilton SR, Aaltonen LA, editors. <strong>World</strong> Health Organization<br />
Classifiaction <strong>of</strong> tumors. Lyon: IARC Press, 2000: 241-243<br />
106 Kerr NJ, Chun YH, Yun K, Heathcott RW, Reeve AE, Sullivan<br />
MJ. Pancreatoblastoma is associated with chromosome<br />
11p loss <strong>of</strong> heterozygosity and IGF2 overexpression. Med<br />
Pediatr Oncol 2002; 39: 52-54<br />
107 Abraham SC, Wu TT, Klimstra DS, Finn LS, Lee JH, Yeo<br />
CJ, Cameron JL, Hruban RH. Distinctive molecular genetic<br />
alterations in sporadic and familial adenomatous polyposisassociated<br />
pancreatoblastomas : frequent alterations in the<br />
APC/beta-catenin pathway and chromosome 11p. Am J<br />
Pathol 2001; 159: 1619-1627<br />
108 Hoorens A, Prenzel K, Lemoine NR, Klöppel G. Undifferentiated<br />
carcinoma <strong>of</strong> the pancreas: analysis <strong>of</strong> intermediate<br />
filament pr<strong>of</strong>ile and Ki-ras mutations provides evidence <strong>of</strong> a<br />
ductal origin. J Pathol 1998; 185: 53-60<br />
109 Goggins M, Offerhaus GJ, Hilgers W, Griffin CA, Shekher M,<br />
Tang D, Sohn TA, Yeo CJ, Kern SE, Hruban RH. Pancreatic<br />
adenocarcinomas with DNA replication errors (RER+) are<br />
associated with wild-type K-ras and characteristic histopathology.<br />
Poor differentiation, a syncytial growth pattern,<br />
and pushing borders suggest RER+. Am J Pathol 1998; 152:<br />
1501-1507<br />
110 Yamamoto H, Itoh F, Nakamura H, Fukushima H, Sasaki S,<br />
Perucho M, Imai K. Genetic and clinical features <strong>of</strong> human<br />
pancreatic ductal adenocarcinomas with widespread microsatellite<br />
instability. Cancer Res 2001; 61: 3139-3144<br />
111 Calhoun ES, Jones JB, Ashfaq R, Adsay V, Baker SJ, Valentine<br />
V, Hempen PM, Hilgers W, Yeo CJ, Hruban RH, Kern<br />
SE. BRAF and FBXW7 (CDC4, FBW7, AGO, SEL10) mutations<br />
in distinct subsets <strong>of</strong> pancreatic <strong>cancer</strong>: potential therapeutic<br />
targets. Am J Pathol 2003; 163: 1255-1260<br />
112 Ribic CM, Sargent DJ, Moore MJ, Thibodeau SN, French<br />
AJ, Goldberg RM, Hamilton SR, Laurent-Puig P, Gryfe<br />
R, Shepherd LE, Tu D, Redston M, Gallinger S. Tumor<br />
microsatellite-instability status as a predictor <strong>of</strong> benefit from<br />
fluorouracil-based adjuvant chemotherapy for colon <strong>cancer</strong>.<br />
N Engl J Med 2003; 349: 247-257<br />
113 Becker WF, Welsh RA, Pratt HS. Cystadenoma and cystadenocarcinoma<br />
<strong>of</strong> the pancreas. Ann Surg 1965; 161: 845-863<br />
114 King JC, Ng TT, White SC, Cortina G, Reber HA, Hines OJ.<br />
Pancreatic serous cystadenocarcinoma: a case report and review<br />
<strong>of</strong> the literature. J Gastrointest Surg 2009; 13: 1864-1868<br />
115 Roggin KK, Chennat J, Oto A, N<strong>of</strong>fsinger A, Briggs A, Matthews<br />
JB. Pancreatic cystic neoplasm. Curr Probl Surg 2010;<br />
47: 459-510<br />
116 Wenig BM, Albores-Saavedra J, Buetow PC, Heffess CS.<br />
Pancreatic mucinous cystic neoplasm with sarcomatous stroma:<br />
a report <strong>of</strong> three cases. Am J Surg Pathol 1997; 21: 70-80<br />
117 Posen JA. Giant cell tumor <strong>of</strong> the pancreas <strong>of</strong> the osteoclastic<br />
type associated with a mucous secreting cystadenocarcinoma.<br />
Hum Pathol 1981; 12: 944-947<br />
118 Sarnaik AA, Saad AG, Mutema GK, Martin SP, Attar A,<br />
Lowy AM. Osteoclast-like giant cell tumor <strong>of</strong> the pancreas<br />
associated with a mucinous cystadenocarcinoma. Surgery<br />
2003; 133: 700-701<br />
119 Campman SC, Fajardo MA, Rippon MB, Kraegel SA, Ruebner<br />
BH. Adenosquamous carcinoma arising in a mucinous<br />
cystadenoma <strong>of</strong> the pancreas. J Surg Oncol 1997; 64: 159-162<br />
120 Fukushima N, Mukai K, Kanai Y, Hasebe T, Shimada K,<br />
Ozaki H, Kinoshita T, Kosuge T. Intraductal papillary tumors<br />
and mucinous cystic tumors <strong>of</strong> the pancreas: clinicopathologic<br />
study <strong>of</strong> 38 cases. Hum Pathol 1997; 28: 1010-1017<br />
121 Crippa S, Salvia R, Warshaw AL, Domínguez I, Bassi C, Falconi<br />
M, Thayer SP, Zamboni G, Lauwers GY, Mino-Kenudson<br />
M, Capelli P, Pederzoli P, Castillo CF. Mucinous cystic<br />
neoplasm <strong>of</strong> the pancreas is not an aggressive entity: lessons<br />
from 163 resected patients. Ann Surg 2008; 247: 571-579<br />
WJG|www.wjgnet.com<br />
Sharma C et al . Clinical advances in pancreatic carcinoma<br />
122 Wood D, Silberman AW, Heifetz L, Memsic L, Shabot MM.<br />
Cystadenocarcinoma <strong>of</strong> the pancreas: neo-adjuvant therapy<br />
and CEA monitoring. J Surg Oncol 1990; 43: 56-60<br />
123 Bradley EL 3rd, Satchidanand SK. Is there a role for chemoradiation<br />
in the management <strong>of</strong> cystadenocarcinoma <strong>of</strong> the<br />
pancreas? Pancreas 2005; 31: 101-103<br />
124 Brown HA, Dotto J, Robert M, Salem RR. Squamous cell carcinoma<br />
<strong>of</strong> the pancreas. J Clin Gastroenterol 2005; 39: 915-919<br />
125 Stelow EB, Shaco-Levy R, Bao F, Garcia J, Klimstra DS. Pancreatic<br />
acinar cell carcinomas with prominent ductal differentiation:<br />
Mixed acinar ductal carcinoma and mixed acinar endocrine<br />
ductal carcinoma. Am J Surg Pathol 2010; 34: 510-518<br />
126 Caruso RA, Inferrera A, Tuccari G, Barresi G. Acinar cell carcinoma<br />
<strong>of</strong> the pancreas. A histologic, immunocytochemical<br />
and ultrastructural study. Histol Histopathol 1994; 9: 53-58<br />
127 Halder SL, McBeth J, Silman AJ, Thompson DG, Macfarlane<br />
GJ. Psychosocial risk factors for the onset <strong>of</strong> abdominal pain.<br />
Results from a large prospective population-based study. Int<br />
J Epidemiol 2002; 31: 1219-1225; discussion 1225-1226<br />
128 Fernandez E, Porta M, Malats N, Belloc J, Gallén M. Symptom-to-diagnosis<br />
interval and survival in <strong>cancer</strong>s <strong>of</strong> the digestive<br />
tract. Dig Dis Sci 2002; 47: 2434-2440<br />
129 Ridder GJ, Klempnauer J. Back pain in patients with ductal<br />
pancreatic <strong>cancer</strong>. Its impact on resectability and prognosis<br />
after resection. Scand J Gastroenterol 1995; 30: 1216-1220<br />
130 La Seta F, Cottone M, Marcenò MP, Maringhini A, Sciarrino<br />
E, Pagliaro L. [Echography in patients with clinically<br />
suspected pancreatic carcinoma. Analysis <strong>of</strong> a prospective<br />
study]. Radiol Med 1983; 69: 538-540<br />
131 Krech RL, Walsh D. Symptoms <strong>of</strong> pancreatic <strong>cancer</strong>. J Pain<br />
Symptom Manage 1991; 6: 360-367<br />
132 Permert J, Larsson J, Westermark GT, Herrington MK,<br />
Christmanson L, Pour PM, Westermark P, Adrian TE. Islet<br />
amyloid polypeptide in patients with pancreatic <strong>cancer</strong> and<br />
diabetes. N Engl J Med 1994; 330: 313-318<br />
133 Schwarts SS, Zeidler A, Moossa AR, Kuku SF, Rubenstein<br />
AH. A prospective study <strong>of</strong> glucose tolerance, insulin,<br />
C-peptide, and glucagon responses in patients with pancreatic<br />
carcinoma. Am J Dig Dis 1978; 23: 1107-1114<br />
134 Tarpila E, Borch K, Kullman E, Liedberg G. Pancreatic <strong>cancer</strong>.<br />
Ann Chir Gynaecol 1986; 75: 146-150<br />
135 Grahm AL, Andrén-Sandberg A. Prospective evaluation <strong>of</strong><br />
pain in exocrine pancreatic <strong>cancer</strong>. Digestion 1997; 58: 542-549<br />
136 Nicolson GL. Cancer metastasis. Organ colonization and<br />
the cell-surface properties <strong>of</strong> malignant cells. Biochim Biophys<br />
Acta 1982; 695: 113-176<br />
137 Hakomori S. Aberrant glycosylation in tumors and tumorassociated<br />
carbohydrate antigens. Adv Cancer Res 1989; 52:<br />
257-331<br />
138 Kleene R, Berger EG. The molecular and cell biology <strong>of</strong> glycosyltransferases.<br />
Biochim Biophys Acta 1993; 1154: 283-325<br />
139 Magnani JL, Nilsson B, Brockhaus M, Zopf D, Steplewski Z,<br />
Koprowski H, Ginsburg V. A monoclonal antibody-defined<br />
antigen associated with gastrointestinal <strong>cancer</strong> is a ganglioside<br />
containing sialylated lacto-N-fucopentaose II. J Biol<br />
Chem 1982; 257: 14365-14369<br />
140 Tanaka N, Okada S, Ueno H, Okusaka T, Ikeda M. The usefulness<br />
<strong>of</strong> serial changes in serum CA19-9 levels in the diagnosis<br />
<strong>of</strong> pancreatic <strong>cancer</strong>. Pancreas 2000; 20: 378-381<br />
141 Boeck S, Stieber P, Holdenrieder S, Wilkowski R, Heinemann<br />
V. Prognostic and therapeutic significance <strong>of</strong> carbohydrate<br />
antigen 19-9 as tumor marker in patients with pancreatic<br />
<strong>cancer</strong>. Oncology 2006; 70: 255-264<br />
142 Ni XG, Bai XF, Mao YL, Shao YF, Wu JX, Shan Y, Wang CF,<br />
Wang J, Tian YT, Liu Q, Xu DK, Zhao P. The clinical value <strong>of</strong><br />
serum CEA, CA19-9, and CA242 in the diagnosis and prognosis<br />
<strong>of</strong> pancreatic <strong>cancer</strong>. Eur J Surg Oncol 2005; 31: 164-169<br />
143 Steinberg W. The clinical utility <strong>of</strong> the CA 19-9 tumor-associated<br />
antigen. Am J Gastroenterol 1990; 85: 350-355<br />
144 Safi F, Schlosser W, Kolb G, Beger HG. Diagnostic value <strong>of</strong><br />
CA 19-9 in patients with pancreatic <strong>cancer</strong> and nonspecific<br />
889 February 21, 2011|Volume 17|Issue 7|
Sharma C et al . Clinical advances in pancreatic carcinoma<br />
gastrointestinal symptoms. J Gastrointest Surg 1997; 1: 106-112<br />
145 Goonetilleke KS, Siriwardena AK. Systematic review <strong>of</strong><br />
carbohydrate antigen (CA 19-9) as a biochemical marker in<br />
the diagnosis <strong>of</strong> pancreatic <strong>cancer</strong>. Eur J Surg Oncol 2007; 33:<br />
266-270<br />
146 Lundin J, Roberts PJ, Kuusela P, Haglund C. The prognostic<br />
value <strong>of</strong> preoperative serum levels <strong>of</strong> CA 19-9 and CEA in<br />
patients with pancreatic <strong>cancer</strong>. Br J Cancer 1994; 69: 515-519<br />
147 Sperti C, Pasquali C, Catalini S, Cappellazzo F, Bonadimani B,<br />
Behboo R, Pedrazzoli S. CA 19-9 as a prognostic index after<br />
resection for pancreatic <strong>cancer</strong>. J Surg Oncol 1993; 52: 137-141<br />
148 Glenn J, Steinberg WM, Kurtzman SH, Steinberg SM, Sindelar<br />
WF. Evaluation <strong>of</strong> the utility <strong>of</strong> a radioimmunoassay for<br />
serum CA 19-9 levels in patients before and after treatment<br />
<strong>of</strong> carcinoma <strong>of</strong> the pancreas. J Clin Oncol 1988; 6: 462-468<br />
149 Safi F, Schlosser W, Falkenreck S, Beger HG. Prognostic<br />
value <strong>of</strong> CA 19-9 serum course in pancreatic <strong>cancer</strong>. Hepatogastroenterology<br />
1998; 45: 253-259<br />
150 Tian F, Appert HE, Myles J, Howard JM. Prognostic value<br />
<strong>of</strong> serum CA 19-9 levels in pancreatic adenocarcinoma. Ann<br />
Surg 1992; 215: 350-355<br />
151 Basso D, Fabris C, Del Favero G, Angonese C, Meggiato T,<br />
Infantino A, Plebani M, Piccoli A, Leandro G, Burlina A. Serum<br />
carcinoembryonic antigen in the differential diagnosis<br />
<strong>of</strong> pancreatic <strong>cancer</strong>: influence <strong>of</strong> tumour spread, liver impairment,<br />
and age. Dis Markers 1988; 6: 203-207<br />
152 Chevinsky AH. CEA in tumors <strong>of</strong> other than colo<strong>rectal</strong> origin.<br />
Semin Surg Oncol 1991; 7: 162-166<br />
153 Ona FV, Zamcheck N, Dhar P, Moore T, Kupchik HZ. Carcinoembryonic<br />
antigen (CEA) in the diagnosis <strong>of</strong> pancreatic<br />
<strong>cancer</strong>. Cancer 1973; 31: 324-327<br />
154 Futakawa N, Kimura W, Yamagata S, Zhao B, Ilsoo H, Inoue<br />
T, Sata N, Kawaguchi Y, Kubota Y, Muto T. Significance <strong>of</strong><br />
K-ras mutation and CEA level in pancreatic juice in the diagnosis<br />
<strong>of</strong> pancreatic <strong>cancer</strong>. J Hepatobiliary Pancreat Surg 2000;<br />
7: 63-71<br />
155 Ozkan H, Kaya M, Cengiz A. Comparison <strong>of</strong> tumor marker<br />
CA 242 with CA 19-9 and carcinoembryonic antigen (CEA) in<br />
pancreatic <strong>cancer</strong>. Hepatogastroenterology 2003; 50: 1669-1674<br />
156 Gattani AM, Mandeli J, Bruckner HW. Tumor markers in<br />
patients with pancreatic carcinoma. Cancer 1996; 78: 57-62<br />
157 Pasanen PA, Eskelinen M, Partanen K, Pikkarainen P, Penttilä<br />
I, Alhava E. A prospective study <strong>of</strong> serum tumour markers<br />
carcinoembryonic antigen, carbohydrate antigens 50<br />
and 242, tissue polypeptide antigen and tissue polypeptide<br />
specific antigen in the diagnosis <strong>of</strong> pancreatic <strong>cancer</strong> with<br />
special reference to multivariate diagnostic score. Br J Cancer<br />
1994; 69: 562-565<br />
158 Jiang XT, Tao HQ, Zou SC. Detection <strong>of</strong> serum tumor markers<br />
in the diagnosis and treatment <strong>of</strong> patients with pancreatic<br />
<strong>cancer</strong>. Hepatobiliary Pancreat Dis Int 2004; 3: 464-468<br />
159 Lindholm L, Johansson C, Jansson EL, Hallberg C, Nilsson O.<br />
An immunoradiometric assay (IRMA) for the CA 50 antigen.<br />
In: Holmgren J, editor. Tumor Maker Antigens. Lund: Studentlitteratur,<br />
1985: 122-133<br />
160 Nilsson O, Johansson C, Glimelius B, Persson B, Nørgaard-<br />
Pedersen B, Andrén-Sandberg A, Lindholm L. Sensitivity and<br />
specificity <strong>of</strong> CA242 in gastro-intestinal <strong>cancer</strong>. A comparison<br />
with CEA, CA50 and CA 19-9. Br J Cancer 1992; 65: 215-221<br />
161 Lundin J, Roberts PJ, Kuusela P, Haglund C. Prognostic significance<br />
<strong>of</strong> serum CA 242 in pancreatic <strong>cancer</strong>. A comparison<br />
with CA 19-9. Anti<strong>cancer</strong> Res 1995; 15: 2181-2186<br />
162 Mu DQ, Wang GF, Peng SY. p53 protein expression and<br />
CA19.9 values in differential cytological diagnosis <strong>of</strong> pancreatic<br />
<strong>cancer</strong> complicated with chronic pancreatitis and chronic<br />
pancreatitis. <strong>World</strong> J Gastroenterol 2003; 9: 1815-1818<br />
163 Ma ZH, Wang Z. An evaluation <strong>of</strong> the diagnostic value <strong>of</strong><br />
CA 19-9 and CEA levels in patients with pancreatic <strong>cancer</strong>.<br />
Nanjing Yike Daxue Xuebao 2009; 23: 199-202<br />
164 Röthlin MA, Joller H, Largiadèr F. CA 242 is a new tumor<br />
marker for pancreatic <strong>cancer</strong>. Cancer 1993; 71: 701-707<br />
WJG|www.wjgnet.com<br />
165 Carpelan-Holmström M, Louhimo J, Stenman UH, Alfthan<br />
H, Haglund C. CEA, CA 19-9 and CA 72-4 improve the diagnostic<br />
accuracy in gastrointestinal <strong>cancer</strong>s. Anti<strong>cancer</strong> Res<br />
2002; 22: 2311-2316<br />
166 Pålsson B, Masson P, Andrén-Sandberg A. The influence <strong>of</strong><br />
cholestasis on CA 50 and CA 242 in pancreatic <strong>cancer</strong> and<br />
benign biliopancreatic diseases. Scand J Gastroenterol 1993; 28:<br />
981-987<br />
167 Hall NR, Finan PJ, Stephenson BM, Purves DA, Cooper EH.<br />
The role <strong>of</strong> CA-242 and CEA in surveillance following curative<br />
resection for colo<strong>rectal</strong> <strong>cancer</strong>. Br J Cancer 1994; 70: 549-553<br />
168 Friess H, Büchler M, Auerbach B, Weber A, Malfertheiner P,<br />
Hammer K, Madry N, Greiner S, Bosslet K, Beger HG. CA<br />
494--a new tumor marker for the diagnosis <strong>of</strong> pancreatic <strong>cancer</strong>.<br />
Int J Cancer 1993; 53: 759-763<br />
169 Simeone DM, Ji B, Banerjee M, Arumugam T, Li D, Anderson<br />
MA, Bamberger AM, Greenson J, Brand RE, Ramachandran<br />
V, Logsdon CD. CEACAM1, a novel serum biomarker<br />
for pancreatic <strong>cancer</strong>. Pancreas 2007; 34: 436-443<br />
170 Bouvet M, Nardin SR, Burton DW, Lee NC, Yang M, Wang X,<br />
Baranov E, Behling C, Moossa AR, H<strong>of</strong>fman RM, Deftos LJ.<br />
Parathyroid hormone-related protein as a novel tumor marker<br />
in pancreatic adenocarcinoma. Pancreas 2002; 24: 284-290<br />
171 Kumar Y, Gurusamy K, Pamecha V, Davidson BR. Tumor<br />
M2-pyruvate kinase as tumor marker in exocrine pancreatic<br />
<strong>cancer</strong> a meta-analysis. Pancreas 2007; 35: 114-119<br />
172 Gansauge F, Gansauge S, Parker N, Beger MI, Poch B, Link<br />
KH, Safi F, Beger HG. CAM 17.1--a new diagnostic marker<br />
in pancreatic <strong>cancer</strong>. Br J Cancer 1996; 74: 1997-2002<br />
173 Louhimo J, Alfthan H, Stenman UH, Haglund C. Serum<br />
HCG beta and CA 72-4 are stronger prognostic factors than<br />
CEA, CA 19-9 and CA 242 in pancreatic <strong>cancer</strong>. Oncology<br />
2004; 66: 126-131<br />
174 Tamm EP, Silverman PM, Charnsangavej C, Evans DB. Diagnosis,<br />
staging, and surveillance <strong>of</strong> pancreatic <strong>cancer</strong>. AJR<br />
Am J Roentgenol 2003; 180: 1311-1323<br />
175 Gandolfi L, Torresan F, Solmi L, Puccetti A. The role <strong>of</strong> ultrasound<br />
in biliary and pancreatic diseases. Eur J Ultrasound<br />
2003; 16: 141-159<br />
176 Giovannini M, Seitz JF. Endoscopic ultrasonography with<br />
a linear-type echoendoscope in the evaluation <strong>of</strong> 94 patients<br />
with pancreatobiliary disease. Endoscopy 1994; 26: 579-585<br />
177 Böttger TC, Boddin J, Düber C, Heintz A, Küchle R, Junginger<br />
T. Diagnosing and staging <strong>of</strong> pancreatic carcinoma-what<br />
is necessary? Oncology 1998; 55: 122-129<br />
178 Rösch T, Lorenz R, Braig C, Feuerbach S, Siewert JR, Schusdziarra<br />
V, Classen M. Endoscopic ultrasound in pancreatic<br />
tumor diagnosis. Gastrointest Endosc 1991; 37: 347-352<br />
179 Niederau C, Grendell JH. Diagnosis <strong>of</strong> pancreatic carcinoma.<br />
Imaging techniques and tumor markers. Pancreas 1992; 7:<br />
66-86<br />
180 Palazzo L, Roseau G, Gayet B, Vilgrain V, Belghiti J, Fékéte<br />
F, Paolaggi JA. Endoscopic ultrasonography in the diagnosis<br />
and staging <strong>of</strong> pancreatic adenocarcinoma. Results <strong>of</strong> a prospective<br />
study with comparison to ultrasonography and CT<br />
scan. Endoscopy 1993; 25: 143-150<br />
181 Karlson BM, Ekbom A, Lindgren PG, Källskog V, Rastad J.<br />
Abdominal US for diagnosis <strong>of</strong> pancreatic tumor: prospective<br />
cohort analysis. Radiology 1999; 213: 107-111<br />
182 Shapiro RS, Wagreich J, Parsons RB, Stancato-Pasik A, Yeh<br />
HC, Lao R. Tissue harmonic imaging sonography: evaluation<br />
<strong>of</strong> image quality compared with conventional sonography.<br />
AJR Am J Roentgenol 1998; 171: 1203-1206<br />
183 Baarir N, Amouyal G, Faintuch JM, Houry S, Huguier M.<br />
[Comparison <strong>of</strong> color Doppler ultrasonography and endoscopic<br />
ultrasonography for preoperative evaluation <strong>of</strong> the<br />
mesenteric-portal axis in pancreatic lesions]. Chirurgie 1998;<br />
123: 445-449<br />
184 Casadei R, Ghigi G, Gullo L, Moretti CC, Greco VM, Salizzoni<br />
E, Canini R, Marrano D. Role <strong>of</strong> color Doppler ultrasonography<br />
in the preoperative staging <strong>of</strong> pancreatic <strong>cancer</strong>.<br />
890 February 21, 2011|Volume 17|Issue 7|
Pancreas 1998; 16: 26-30<br />
185 Dietrich CF, Braden B, Hocke M, Ott M, Ignee A. Improved<br />
characterisation <strong>of</strong> solitary solid pancreatic tumours using<br />
contrast enhanced transabdominal ultrasound. J Cancer Res<br />
Clin Oncol 2008; 134: 635-643<br />
186 Sørensen MB, Weibull AS, Haubek A, Rokkjaer M, Jørgensen<br />
J. [Resectability <strong>of</strong> papillary and pancreatic <strong>cancer</strong><br />
assessed by ultrasonography and computer tomography].<br />
Ugeskr Laeger 1997; 159: 743-747<br />
187 Sahani DV, Shah ZK, Catalano OA, Boland GW, Brugge<br />
WR. Radiology <strong>of</strong> pancreatic adenocarcinoma: current status<br />
<strong>of</strong> imaging. J Gastroenterol Hepatol 2008; 23: 23-33<br />
188 DeWitt J, Devereaux B, Chriswell M, McGreevy K, Howard<br />
T, Imperiale TF, Ciaccia D, Lane KA, Maglinte D, Kopecky K,<br />
LeBlanc J, McHenry L, Madura J, Aisen A, Cramer H, Cummings<br />
O, Sherman S. Comparison <strong>of</strong> endoscopic ultrasonography<br />
and multidetector computed tomography for detecting<br />
and staging pancreatic <strong>cancer</strong>. Ann Intern Med 2004; 141:<br />
753-763<br />
189 Klapman JB, Chang KJ, Lee JG, Nguyen P. Negative predictive<br />
value <strong>of</strong> endoscopic ultrasound in a large series <strong>of</strong><br />
patients with a clinical suspicion <strong>of</strong> pancreatic <strong>cancer</strong>. Am J<br />
Gastroenterol 2005; 100: 2658-2661<br />
190 Brugge WR, Lee MJ, Kelsey PB, Schapiro RH, Warshaw AL.<br />
The use <strong>of</strong> EUS to diagnose malignant portal venous system<br />
invasion by pancreatic <strong>cancer</strong>. Gastrointest Endosc 1996; 43:<br />
561-567<br />
191 Faigel DO, Kochman ML. The role <strong>of</strong> endoscopic ultrasound<br />
in the preoperative staging <strong>of</strong> pancreatic malignancies. Gastrointest<br />
Endosc 1996; 43: 626-628<br />
192 Aslanian H, Salem R, Lee J, Andersen D, Robert M, Topazian<br />
M. EUS diagnosis <strong>of</strong> vascular invasion in pancreatic<br />
<strong>cancer</strong>: surgical and histologic correlates. Am J Gastroenterol<br />
2005; 100: 1381-1385<br />
193 Dietrich CF, Ignee A, Braden B, Barreiros AP, Ott M, Hocke<br />
M. Improved differentiation <strong>of</strong> pancreatic tumors using<br />
contrast-enhanced endoscopic ultrasound. Clin Gastroenterol<br />
Hepatol 2008; 6: 590-597.e1<br />
194 Eloubeidi MA, Tamhane A, Varadarajulu S, Wilcox CM.<br />
Frequency <strong>of</strong> major complications after EUS-guided FNA <strong>of</strong><br />
solid pancreatic masses: a prospective evaluation. Gastrointest<br />
Endosc 2006; 63: 622-629<br />
195 Choi BI, Chung MJ, Han JK, Han MC, Yoon YB. Detection <strong>of</strong><br />
pancreatic adenocarcinoma: relative value <strong>of</strong> arterial and late<br />
phases <strong>of</strong> spiral CT. Abdom Imaging 1997; 22: 199-203<br />
196 Bronstein YL, Loyer EM, Kaur H, Choi H, David C, DuBrow<br />
RA, Broemeling LD, Cleary KR, Charnsangavej C. Detection<br />
<strong>of</strong> small pancreatic tumors with multiphasic helical CT. AJR<br />
Am J Roentgenol 2004; 182: 619-623<br />
197 Megibow AJ, Zhou XH, Rotterdam H, Francis IR, Zerhouni<br />
EA, Balfe DM, Weinreb JC, Aisen A, Kuhlman J, Heiken JP.<br />
Pancreatic adenocarcinoma: CT versus MR imaging in the<br />
evaluation <strong>of</strong> resectability--report <strong>of</strong> the Radiology Diagnostic<br />
Oncology Group. Radiology 1995; 195: 327-332<br />
198 Gangi S, Fletcher JG, Nathan MA, Christensen JA, Harmsen<br />
WS, Crownhart BS, Chari ST. Time interval between abnormalities<br />
seen on CT and the clinical diagnosis <strong>of</strong> pancreatic<br />
<strong>cancer</strong>: retrospective review <strong>of</strong> CT scans obtained before<br />
diagnosis. AJR Am J Roentgenol 2004; 182: 897-903<br />
199 Ohwada S, Ogawa T, Tanahashi Y, Nakamura S, Takeyoshi I,<br />
Ohya T, Ikeya T, Kawashima K, Kawashima Y, Morishita Y.<br />
Fibrin glue sandwich prevents pancreatic fistula following<br />
distal pancreatectomy. <strong>World</strong> J Surg 1998; 22: 494-498<br />
200 Baum U, Lell M, Nömayr A, Wolf H, Brunner T, Greess H,<br />
Bautz W. [Multiplanar spiral CT in the diagnosis <strong>of</strong> pancreatic<br />
tumors]. Radiologe 1999; 39: 958-964<br />
201 Fletcher JG, Wiersema MJ, Farrell MA, Fidler JL, Burgart LJ,<br />
Koyama T, Johnson CD, Stephens DH, Ward EM, Harmsen<br />
WS. Pancreatic malignancy: value <strong>of</strong> arterial, pancreatic, and<br />
hepatic phase imaging with multi-detector row CT. Radiology<br />
2003; 229: 81-90<br />
WJG|www.wjgnet.com<br />
Sharma C et al . Clinical advances in pancreatic carcinoma<br />
202 Vargas R, Nino-Murcia M, Trueblood W, Jeffrey RB Jr.<br />
MDCT in Pancreatic adenocarcinoma: prediction <strong>of</strong> vascular<br />
invasion and resectability using a multiphasic technique<br />
with curved planar reformations. AJR Am J Roentgenol 2004;<br />
182: 419-425<br />
203 Diehl SJ, Lehmann KJ, Sadick M, Lachmann R, Georgi M.<br />
Pancreatic <strong>cancer</strong>: value <strong>of</strong> dual-phase helical CT in assessing<br />
resectability. Radiology 1998; 206: 373-378<br />
204 Lu DS, Reber HA, Krasny RM, Kadell BM, Sayre J. Local<br />
staging <strong>of</strong> pancreatic <strong>cancer</strong>: criteria for unresectability <strong>of</strong><br />
major vessels as revealed by pancreatic-phase, thin-section<br />
helical CT. AJR Am J Roentgenol 1997; 168: 1439-1443<br />
205 Ahn SS, Kim MJ, Choi JY, Hong HS, Chung YE, Lim JS. Indicative<br />
findings <strong>of</strong> pancreatic <strong>cancer</strong> in prediagnostic CT.<br />
Eur Radiol 2009; 19: 2448-2455<br />
206 Johnson PT, Outwater EK. Pancreatic carcinoma versus<br />
chronic pancreatitis: dynamic MR imaging. Radiology 1999;<br />
212: 213-218<br />
207 Bluemke DA, Cameron JL, Hruban RH, Pitt HA, Siegelman<br />
SS, Soyer P, Fishman EK. Potentially resectable pancreatic<br />
adenocarcinoma: spiral CT assessment with surgical and<br />
pathologic correlation. Radiology 1995; 197: 381-385<br />
208 Schima W, Függer R, Schober E, Oettl C, Wamser P, Grabenwöger<br />
F, Ryan JM, Novacek G. Diagnosis and staging <strong>of</strong><br />
pancreatic <strong>cancer</strong>: comparison <strong>of</strong> mangafodipir trisodiumenhanced<br />
MR imaging and contrast-enhanced helical hydro-<br />
CT. AJR Am J Roentgenol 2002; 179: 717-724<br />
209 Ichikawa T, Haradome H, Hachiya J, Nitatori T, Ohtomo<br />
K, Kinoshita T, Araki T. Pancreatic ductal adenocarcinoma:<br />
preoperative assessment with helical CT versus dynamic MR<br />
imaging. Radiology 1997; 202: 655-662<br />
210 Irie H, Honda H, Kaneko K, Kuroiwa T, Yoshimitsu K, Masuda<br />
K. Comparison <strong>of</strong> helical CT and MR imaging in detecting<br />
and staging small pancreatic adenocarcinoma. Abdom<br />
Imaging 1997; 22: 429-433<br />
211 Romijn MG, Stoker J, van Eijck CH, van Muiswinkel JM,<br />
Torres CG, Laméris JS. MRI with mangafodipir trisodium in<br />
the detection and staging <strong>of</strong> pancreatic <strong>cancer</strong>. J Magn Reson<br />
Imaging 2000; 12: 261-268<br />
212 Andersson M, Kostic S, Johansson M, Lundell L, Asztély M,<br />
Hellström M. MRI combined with MR cholangiopancreatography<br />
versus helical CT in the evaluation <strong>of</strong> patients with<br />
suspected periampullary tumors: a prospective comparative<br />
study. Acta Radiol 2005; 46: 16-27<br />
213 Hänninen EL, Ricke J, Amthauer H, Röttgen R, Böhmig M,<br />
Langrehr J, Pech M, Denecke T, Rosewicz S, Felix R. Magnetic<br />
resonance cholangiopancreatography: image quality,<br />
ductal morphology, and value <strong>of</strong> additional T2- and T1weighted<br />
sequences for the assessment <strong>of</strong> suspected pancreatic<br />
<strong>cancer</strong>. Acta Radiol 2005; 46: 117-125<br />
214 Park HS, Lee JM, Choi HK, Hong SH, Han JK, Choi BI. Preoperative<br />
evaluation <strong>of</strong> pancreatic <strong>cancer</strong>: comparison <strong>of</strong><br />
gadolinium-enhanced dynamic MRI with MR cholangiopancreatography<br />
versus MDCT. J Magn Reson Imaging 2009; 30:<br />
586-595<br />
215 Grenacher L, Klauss M, Dukic L, Delorme S, Knaebel HP,<br />
Düx M, Kauczor HU, Büchler MW, Kauffmann GW, Richter<br />
GM. [Diagnosis and staging <strong>of</strong> pancreatic carcinoma: MRI<br />
versus multislice-CT -- a prospective study]. R<strong>of</strong>o 2004; 176:<br />
1624-1633<br />
216 Bipat S, Phoa SS, van Delden OM, Bossuyt PM, Gouma DJ,<br />
Laméris JS, Stoker J. Ultrasonography, computed tomography<br />
and magnetic resonance imaging for diagnosis and<br />
determining resectability <strong>of</strong> pancreatic adenocarcinoma: a<br />
meta-analysis. J Comput Assist Tomogr 2005; 29: 438-445<br />
217 Maemura K, Takao S, Shinchi H, Noma H, Mataki Y, Kurahara<br />
H, Jinnouchi S, Aikou T. Role <strong>of</strong> positron emission tomography<br />
in decisions on treatment strategies for pancreatic<br />
<strong>cancer</strong>. J Hepatobiliary Pancreat Surg 2006; 13: 435-441<br />
218 Higashi T, Saga T, Nakamoto Y, Ishimori T, Fujimoto K, Doi<br />
R, Imamura M, Konishi J. Diagnosis <strong>of</strong> pancreatic <strong>cancer</strong><br />
891 February 21, 2011|Volume 17|Issue 7|
Sharma C et al . Clinical advances in pancreatic carcinoma<br />
using fluorine-18 fluorodeoxyglucose positron emission tomography<br />
(FDG PET) --usefulness and limitations in "clinical<br />
reality". Ann Nucl Med 2003; 17: 261-279<br />
219 Wakabayashi H, Nishiyama Y, Otani T, Sano T, Yachida S,<br />
Okano K, Izuishi K, Suzuki Y. Role <strong>of</strong> 18F-fluorodeoxyglucose<br />
positron emission tomography imaging in surgery for<br />
pancreatic <strong>cancer</strong>. <strong>World</strong> J Gastroenterol 2008; 14: 64-69<br />
220 Schima W, Függer R. Evaluation <strong>of</strong> focal pancreatic masses:<br />
comparison <strong>of</strong> mangafodipir-enhanced MR imaging and<br />
contrast-enhanced helical CT. Eur Radiol 2002; 12: 2998-3008<br />
221 Delbeke D, Rose DM, Chapman WC, Pinson CW, Wright<br />
JK, Beauchamp RD, Shyr Y, Leach SD. Optimal interpretation<br />
<strong>of</strong> FDG PET in the diagnosis, staging and management<br />
<strong>of</strong> pancreatic carcinoma. J Nucl Med 1999; 40: 1784-1791<br />
222 Heinrich S, Goerres GW, Schäfer M, Sagmeister M, Bauerfeind<br />
P, Pestalozzi BC, Hany TF, von Schulthess GK, Clavien<br />
PA. Positron emission tomography/computed tomography<br />
influences on the management <strong>of</strong> resectable pancreatic <strong>cancer</strong><br />
and its cost-effectiveness. Ann Surg 2005; 242: 235-243<br />
223 Lee TY, Kim MH, Park do H, Seo DW, Lee SK, Kim JS, Lee<br />
KT. Utility <strong>of</strong> 18F-FDG PET/CT for differentiation <strong>of</strong> autoimmune<br />
pancreatitis with atypical pancreatic imaging findings<br />
from pancreatic <strong>cancer</strong>. AJR Am J Roentgenol 2009; 193:<br />
343-348<br />
224 Zhao C, Chen Z, Ye X, Zhang Y, Zhan H, Aburano T, Tian M,<br />
Zhang H. Imaging a pancreatic carcinoma xenograft model<br />
with 11C-acetate: a comparison study with 18F-FDG. Nucl<br />
Med Commun 2009; 30: 971-977<br />
225 Nakata B, Nishimura S, Ishikawa T, Ohira M, Nishino H,<br />
Kawabe J, Ochi H, Hirakawa K. Prognostic predictive value<br />
<strong>of</strong> 18F-fluorodeoxyglucose positron emission tomography<br />
for patients with pancreatic <strong>cancer</strong>. Int J Oncol 2001; 19: 53-58<br />
226 Yoshioka M, Sato T, Furuya T, Shibata S, Andoh H, Asanuma<br />
Y, Hatazawa J, Shimosegawa E, Koyama K, Yamamoto<br />
Y. Role <strong>of</strong> positron emission tomography with 2-deoxy-<br />
2-[18F]fluoro-D-glucose in evaluating the effects <strong>of</strong> arterial<br />
infusion chemotherapy and radiotherapy on pancreatic <strong>cancer</strong>.<br />
J Gastroenterol 2004; 39: 50-55<br />
227 Klever P, Bares R, Fass J, Büll U, Schumpelick V. PET with<br />
fluorine-18 deoxyglucose for pancreatic disease. Lancet 1992;<br />
340: 1158-1159<br />
228 Nakamoto Y, Higashi T, Sakahara H, Tamaki N, Kogire M,<br />
Imamura M, Konishi J. Contribution <strong>of</strong> PET in the detection<br />
<strong>of</strong> liver metastases from pancreatic tumours. Clin Radiol<br />
1999; 54: 248-252<br />
229 Berberat P, Friess H, Kashiwagi M, Beger HG, Büchler MW.<br />
Diagnosis and staging <strong>of</strong> pancreatic <strong>cancer</strong> by positron emission<br />
tomography. <strong>World</strong> J Surg 1999; 23: 882-887<br />
230 Zimny M, Fass J, Bares R, Cremerius U, Sabri O, Buechin P,<br />
Schumpelick V, Buell U. Fluorodeoxyglucose positron emission<br />
tomography and the prognosis <strong>of</strong> pancreatic carcinoma.<br />
Scand J Gastroenterol 2000; 35: 883-888<br />
231 Tanaka S, Kitamra T, Yamamoto K, Fujikawa S, Imaoka T,<br />
Nishikawa S, Nakaizumi A, Uehara H, Ishikawa O, Ohigashi<br />
H. Evaluation <strong>of</strong> routine sonography for early detection <strong>of</strong><br />
pancreatic <strong>cancer</strong>. Jpn J Clin Oncol 1996; 26: 422-427<br />
232 Candiani F, Meduri F, Norberto L, Calderone M. [Contrast<br />
media in ultrasonography. Venous involvement in tumors <strong>of</strong><br />
the head <strong>of</strong> the pancreas]. Radiol Med 1998; 95: 29-33<br />
233 Calculli L, Casadei R, Amore B, Albini Riccioli L, Minni F,<br />
Caputo M, Marrano D, Gavelli G. The usefulness <strong>of</strong> spiral<br />
Computed Tomography and colour-Doppler ultrasonography<br />
to predict portal-mesenteric trunk involvement in pancreatic<br />
<strong>cancer</strong>. Radiol Med 2002; 104: 307-315<br />
234 Akahoshi K, Chijiiwa Y, Nakano I, Nawata H, Ogawa Y,<br />
Tanaka M, Nagai E, Tsuneyoshi M. Diagnosis and staging <strong>of</strong><br />
pancreatic <strong>cancer</strong> by endoscopic ultrasound. Br J Radiol 1998;<br />
71: 492-496<br />
235 Legmann P, Vignaux O, Dousset B, Baraza AJ, Palazzo L,<br />
Dumontier I, Coste J, Louvel A, Roseau G, Couturier D, Bonnin<br />
A. Pancreatic tumors: comparison <strong>of</strong> dual-phase helical<br />
WJG|www.wjgnet.com<br />
CT and endoscopic sonography. AJR Am J Roentgenol 1998;<br />
170: 1315-1322<br />
236 Bilimoria KY, Bentrem DJ, Ko CY, Ritchey J, Stewart AK,<br />
Winchester DP, Talamonti MS. Validation <strong>of</strong> the 6th edition<br />
AJCC Pancreatic Cancer Staging System: report from the National<br />
Cancer Database. Cancer 2007; 110: 738-744<br />
237 AJCC Cancer Staging Handbook. 7th edition. New York:<br />
Springer-Verlag, 2010<br />
238 Warshaw AL, Fernández-del Castillo C. Pancreatic carcinoma.<br />
N Engl J Med 1992; 326: 455-465<br />
239 Soriano A, Castells A, Ayuso C, Ayuso JR, de Caralt MT, Ginès<br />
MA, Real MI, Gilabert R, Quintó L, Trilla A, Feu F, Montanyà<br />
X, Fernández-Cruz L, Navarro S. Preoperative staging<br />
and tumor resectability assessment <strong>of</strong> pancreatic <strong>cancer</strong>:<br />
prospective study comparing endoscopic ultrasonography,<br />
helical computed tomography, magnetic resonance imaging,<br />
and angiography. Am J Gastroenterol 2004; 99: 492-501<br />
240 Cuschieri A. Laparoscopy for pancreatic <strong>cancer</strong>: does it benefit<br />
the patient? Eur J Surg Oncol 1988; 14: 41-44<br />
241 Warshaw AL, Tepper JE, Shipley WU. Laparoscopy in the<br />
staging and planning <strong>of</strong> therapy for pancreatic <strong>cancer</strong>. Am J<br />
Surg 1986; 151: 76-80<br />
242 Warshaw AL, Gu ZY, Wittenberg J, Waltman AC. Preoperative<br />
staging and assessment <strong>of</strong> resectability <strong>of</strong> pancreatic<br />
<strong>cancer</strong>. Arch Surg 1990; 125: 230-233<br />
243 Camacho D, Reichenbach D, Duerr GD, Venema TL, Sweeney<br />
JF, Fisher WE. Value <strong>of</strong> laparoscopy in the staging <strong>of</strong><br />
pancreatic <strong>cancer</strong>. JOP 2005; 6: 552-561<br />
244 Ellsmere J, Mortele K, Sahani D, Maher M, Cantisani V,<br />
Wells W, Brooks D, Rattner D. Does multidetector-row CT<br />
eliminate the role <strong>of</strong> diagnostic laparoscopy in assessing the<br />
resectability <strong>of</strong> pancreatic head adenocarcinoma? Surg Endosc<br />
2005; 19: 369-373<br />
245 Morganti AG, Brizi MG, Macchia G, Sallustio G, Costamagna<br />
G, Alfieri S, Mattiucci GC, Valentini V, Natale L, Deodato<br />
F, Mutignani M, Doglietto GB, Cellini N. The prognostic<br />
effect <strong>of</strong> clinical staging in pancreatic adenocarcinoma. Ann<br />
Surg Oncol 2005; 12: 145-151<br />
246 Nieveen van Dijkum EJ, Romijn MG, Terwee CB, de Wit<br />
LT, van der Meulen JH, Lameris HS, Rauws EA, Obertop H,<br />
van Eyck CH, Bossuyt PM, Gouma DJ. Laparoscopic staging<br />
and subsequent palliation in patients with peripancreatic<br />
carcinoma. Ann Surg 2003; 237: 66-73<br />
247 Conlon KC, Dougherty E, Klimstra DS, Coit DG, Turnbull<br />
AD, Brennan MF. The value <strong>of</strong> minimal access surgery in the<br />
staging <strong>of</strong> patients with potentially resectable peripancreatic<br />
malignancy. Ann Surg 1996; 223: 134-140<br />
248 Tilleman EH, Busch OR, Bemelman WA, van Gulik TM,<br />
Obertop H, Gouma DJ. Diagnostic laparoscopy in staging<br />
pancreatic carcinoma: developments during the past decade.<br />
J Hepatobiliary Pancreat Surg 2004; 11: 11-16<br />
249 Pisters PW, Lee JE, Vauthey JN, Charnsangavej C, Evans DB.<br />
Laparoscopy in the staging <strong>of</strong> pancreatic <strong>cancer</strong>. Br J Surg<br />
2001; 88: 325-337<br />
250 Kwon AH, Inui H, Kamiyama Y. Preoperative laparoscopic<br />
examination using surgical manipulation and ultrasonography<br />
for pancreatic lesions. Endoscopy 2002; 34: 464-468<br />
251 Catheline JM, Turner R, Rizk N, Barrat C, Champault G. The<br />
use <strong>of</strong> diagnostic laparoscopy supported by laparoscopic<br />
ultrasonography in the assessment <strong>of</strong> pancreatic <strong>cancer</strong>. Surg<br />
Endosc 1999; 13: 239-245<br />
252 White R, Winston C, Gonen M, D'Angelica M, Jarnagin W,<br />
Fong Y, Conlon K, Brennan M, Allen P. Current utility <strong>of</strong><br />
staging laparoscopy for pancreatic and peripancreatic neoplasms.<br />
J Am Coll Surg 2008; 206: 445-450<br />
253 National Comprehensive Cancer Network. Practice Guidelines<br />
for Pancreatic Cancer. Accessed on October 20, 2010<br />
254 Chang DK, Merrett ND, Biankin AV. Improving outcomes<br />
for operable pancreatic <strong>cancer</strong>: is access to safer surgery the<br />
problem? J Gastroenterol Hepatol 2008; 23: 1036-1045<br />
255 Freelove R, Walling AD. Pancreatic <strong>cancer</strong>: diagnosis and<br />
892 February 21, 2011|Volume 17|Issue 7|
management. Am Fam Physician 2006; 73: 485-492<br />
256 Büchler MW, Wagner M, Schmied BM, Uhl W, Friess H,<br />
Z'graggen K. Changes in morbidity after pancreatic resection:<br />
toward the end <strong>of</strong> completion pancreatectomy. Arch<br />
Surg 2003; 138: 1310-1314; discussion 1315<br />
257 Birkmeyer JD, Siewers AE, Finlayson EV, Stukel TA, Lucas<br />
FL, Batista I, Welch HG, Wennberg DE. Hospital volume and<br />
surgical mortality in the United States. N Engl J Med 2002;<br />
346: 1128-1137<br />
258 Cameron JL, Riall TS, Coleman J, Belcher KA. One thousand<br />
consecutive pancreaticoduodenectomies. Ann Surg 2006; 244:<br />
10-15<br />
259 The US National Cancer Institute. Surveillance Epidemiology<br />
and End Results (SEER) data base. 2007. Available from:<br />
URL: http://seer.<strong>cancer</strong>.gov/<br />
260 Zuckerman DS, Ryan DP. Adjuvant therapy for pancreatic<br />
<strong>cancer</strong>: a review. Cancer 2008; 112: 243-249<br />
261 Takhar AS, Palaniappan P, Dhingsa R, Lobo DN. Recent developments<br />
in diagnosis <strong>of</strong> pancreatic <strong>cancer</strong>. BMJ 2004; 329:<br />
668-673<br />
262 Li D, Xie K, Wolff R, Abbruzzese JL. Pancreatic <strong>cancer</strong>. Lancet<br />
2004; 363: 1049-1057<br />
263 Barugola G, Partelli S, Marcucci S, Sartori N, Capelli P, Bassi<br />
C, Pederzoli P, Falconi M. Resectable pancreatic <strong>cancer</strong>:<br />
who really benefits from resection? Ann Surg Oncol 2009; 16:<br />
3316-3322<br />
264 van der Gaag NA, Kloek JJ, de Castro SM, Busch OR, van<br />
Gulik TM, Gouma DJ. Preoperative biliary drainage in patients<br />
with obstructive jaundice: history and current status. J<br />
Gastrointest Surg 2009; 13: 814-820<br />
265 Klinkenbijl JH, Jeekel J, Schmitz PI, Rombout PA, Nix GA,<br />
Bruining HA, van Blankenstein M. Carcinoma <strong>of</strong> the pancreas<br />
and periampullary region: palliation versus cure. Br J<br />
Surg 1993; 80: 1575-1578<br />
266 Kimmings AN, van Deventer SJ, Obertop H, Rauws EA,<br />
Huibregtse K, Gouma DJ. Endotoxin, cytokines, and endotoxin<br />
binding proteins in obstructive jaundice and after preoperative<br />
biliary drainage. Gut 2000; 46: 725-731<br />
267 Jethwa P, Breuning E, Bhati C, Buckles J, Mirza D, Bramhall<br />
S. The microbiological impact <strong>of</strong> pre-operative biliary drainage<br />
on patients undergoing hepato-biliary-pancreatic (HPB)<br />
surgery. Aliment Pharmacol Ther 2007; 25: 1175-1180<br />
268 Limongelli P, Pai M, Bansi D, Thiallinagram A, Tait P,<br />
Jackson J, Habib NA, Williamson RC, Jiao LR. Correlation<br />
between preoperative biliary drainage, bile duct contamination,<br />
and postoperative outcomes for pancreatic surgery.<br />
Surgery 2007; 142: 313-318<br />
269 Coates JM, Beal SH, Russo JE, Vanderveen KA, Chen SL,<br />
Bold RJ, Canter RJ. Negligible effect <strong>of</strong> selective preoperative<br />
biliary drainage on perioperative resuscitation, morbidity,<br />
and mortality in patients undergoing pancreaticoduodenectomy.<br />
Arch Surg 2009; 144: 841-847<br />
270 Mezhir JJ, Brennan MF, Baser RE, D'Angelica MI, Fong Y,<br />
DeMatteo RP, Jarnagin WR, Allen PJ. A matched case-control<br />
study <strong>of</strong> preoperative biliary drainage in patients with<br />
pancreatic adenocarcinoma: routine drainage is not justified.<br />
J Gastrointest Surg 2009; 13: 2163-2169<br />
271 Wang Q, Gurusamy KS, Lin H, Xie X, Wang C. Preoperative<br />
biliary drainage for obstructive jaundice. Cochrane Database<br />
Syst Rev 2008; CD005444<br />
272 Sewnath ME, Karsten TM, Prins MH, Rauws EJ, Obertop H,<br />
Gouma DJ. A meta-analysis on the efficacy <strong>of</strong> preoperative<br />
biliary drainage for tumors causing obstructive jaundice.<br />
Ann Surg 2002; 236: 17-27<br />
273 van der Gaag NA, Rauws EA, van Eijck CH, Bruno MJ, van<br />
der Harst E, Kubben FJ, Gerritsen JJ, Greve JW, Gerhards<br />
MF, de Hingh IH, Klinkenbijl JH, Nio CY, de Castro SM,<br />
Busch OR, van Gulik TM, Bossuyt PM, Gouma DJ. Preoperative<br />
biliary drainage for <strong>cancer</strong> <strong>of</strong> the head <strong>of</strong> the pancreas. N<br />
Engl J Med 2010; 362: 129-137<br />
274 Landry J, Catalano PJ, Staley C, Harris W, H<strong>of</strong>fman J, Tal-<br />
WJG|www.wjgnet.com<br />
Sharma C et al . Clinical advances in pancreatic carcinoma<br />
amonti M, Xu N, Cooper H, Benson AB 3rd. Randomized<br />
phase II study <strong>of</strong> gemcitabine plus radiotherapy versus gemcitabine,<br />
5-fluorouracil, and cisplatin followed by radiotherapy<br />
and 5-fluorouracil for patients with locally advanced, potentially<br />
resectable pancreatic adenocarcinoma. J Surg Oncol<br />
2010; 101: 587-592<br />
275 Lee S, Oh SY, Kim BG, Kwon HC, Kim SH, Rho MH, Kim<br />
YH, Rho MS, Jeong JS, Kim HJ. Second-line treatment with a<br />
combination <strong>of</strong> continuous 5-fluorouracil, doxorubicin, and<br />
mitomycin-C (conti-FAM) in gemcitabine-pretreated pancreatic<br />
and biliary tract <strong>cancer</strong>. Am J Clin Oncol 2009; 32: 348-352<br />
276 Le Scodan R, Mornex F, Girard N, Mercier C, Valette PJ,<br />
Ychou M, Bibeau F, Roy P, Scoazec JY, Partensky C. Preoperative<br />
chemoradiation in potentially resectable pancreatic<br />
adenocarcinoma: feasibility, treatment effect evaluation and<br />
prognostic factors, analysis <strong>of</strong> the SFRO-FFCD 9704 trial and<br />
literature review. Ann Oncol 2009; 20: 1387-1396<br />
277 Heinrich S, Schäfer M, Weber A, Hany TF, Bhure U,<br />
Pestalozzi BC, Clavien PA. Neoadjuvant chemotherapy generates<br />
a significant tumor response in resectable pancreatic<br />
<strong>cancer</strong> without increasing morbidity: results <strong>of</strong> a prospective<br />
phase II trial. Ann Surg 2008; 248: 1014-1022<br />
278 Marti JL, Hochster HS, Hiotis SP, Donahue B, Ryan T, Newman<br />
E. Phase I/II trial <strong>of</strong> induction chemotherapy followed<br />
by concurrent chemoradiotherapy and surgery for locoregionally<br />
advanced pancreatic <strong>cancer</strong>. Ann Surg Oncol 2008;<br />
15: 3521-3531<br />
279 Le Scodan R, Mornex F, Partensky C, Mercier C, Valette PJ,<br />
Ychou M, Roy P, Scoazec JY. Histopathological response to<br />
preoperative chemoradiation for resectable pancreatic adenocarcinoma:<br />
the French Phase II FFCD 9704-SFRO Trial.<br />
Am J Clin Oncol 2008; 31: 545-552<br />
280 Lind PA, Isaksson B, Almström M, Johnsson A, Albiin N,<br />
Byström P, Permert J. Efficacy <strong>of</strong> preoperative radiochemotherapy<br />
in patients with locally advanced pancreatic carcinoma.<br />
Acta Oncol 2008; 47: 413-420<br />
281 Evans DB, Varadhachary GR, Crane CH, Sun CC, Lee JE,<br />
Pisters PW, Vauthey JN, Wang H, Cleary KR, Staerkel GA,<br />
Charnsangavej C, Lano EA, Ho L, Lenzi R, Abbruzzese JL,<br />
Wolff RA. Preoperative gemcitabine-based chemoradiation<br />
for patients with resectable adenocarcinoma <strong>of</strong> the pancreatic<br />
head. J Clin Oncol 2008; 26: 3496-3502<br />
282 Varadhachary GR, Wolff RA, Crane CH, Sun CC, Lee JE, Pisters<br />
PW, Vauthey JN, Abdalla E, Wang H, Staerkel GA, Lee<br />
JH, Ross WA, Tamm EP, Bhosale PR, Krishnan S, Das P, Ho L,<br />
Xiong H, Abbruzzese JL, Evans DB. Preoperative gemcitabine<br />
and cisplatin followed by gemcitabine-based chemoradiation<br />
for resectable adenocarcinoma <strong>of</strong> the pancreatic head. J<br />
Clin Oncol 2008; 26: 3487-3495<br />
283 Heinrich S, Pestalozzi BC, Schäfer M, Weber A, Bauerfeind<br />
P, Knuth A, Clavien PA. Prospective phase II trial <strong>of</strong> neoadjuvant<br />
chemotherapy with gemcitabine and cisplatin for resectable<br />
adenocarcinoma <strong>of</strong> the pancreatic head. J Clin Oncol<br />
2008; 26: 2526-2531<br />
284 Boulay BR, Gardner TB, Gordon SR. Occlusion rate and<br />
complications <strong>of</strong> plastic biliary stent placement in patients<br />
undergoing neoadjuvant chemoradiotherapy for pancreatic<br />
<strong>cancer</strong> with malignant biliary obstruction. J Clin Gastroenterol<br />
2010; 44: 452-455<br />
285 Wasan SM, Ross WA, Staerkel GA, Lee JH. Use <strong>of</strong> expandable<br />
metallic biliary stents in resectable pancreatic <strong>cancer</strong>.<br />
Am J Gastroenterol 2005; 100: 2056-2061<br />
286 Kausch W. Das carcinom der papilla duodeni und seine radikale<br />
entfernung. Beitr Klin Chir 1912; 78: 439-451<br />
287 Whipple A. Present-day surgery <strong>of</strong> the pancreas. N Engl J<br />
Med 1942; 226: 515-518<br />
288 Trede M. Surgery <strong>of</strong> the pancreas. Edinburgh: Churchill Livingstone,<br />
1993<br />
289 Seiler CA, Wagner M, Sadowski C, Kulli C, Büchler MW.<br />
Randomized prospective trial <strong>of</strong> pylorus-preserving vs. Classic<br />
duodenopancreatectomy (Whipple procedure): initial<br />
893 February 21, 2011|Volume 17|Issue 7|
Sharma C et al . Clinical advances in pancreatic carcinoma<br />
clinical results. J Gastrointest Surg 2000; 4: 443-452<br />
290 Williamson RC, Bliouras N, Cooper MJ, Davies ER. Gastric<br />
emptying and enterogastric reflux after conservative and conventional<br />
pancreatoduodenectomy. Surgery 1993; 114: 82-86<br />
291 Watson K. Carcinoma <strong>of</strong> the ampulla <strong>of</strong> Vater. Successful<br />
radical resection. Br J Surg 1944; 31: 368<br />
292 Traverso LW, Longmire WP Jr. Preservation <strong>of</strong> the pylorus<br />
in pancreaticoduodenectomy. Surg Gynecol Obstet 1978; 146:<br />
959-962<br />
293 Loos M, Kleeff J, Friess H, Buchler MW. Surgical treatment<br />
<strong>of</strong> pancreatic <strong>cancer</strong>. Ann N Y Acad Sci 2008; 1138: 169-180<br />
294 Horstmann O, Markus PM, Ghadimi MB, Becker H. Pylorus<br />
preservation has no impact on delayed gastric emptying after<br />
pancreatic head resection. Pancreas 2004; 28: 69-74<br />
295 Wenger FA, Jacobi CA, Haubold K, Zieren HU, Müller<br />
JM. [Gastrointestinal quality <strong>of</strong> life after duodenopancreatectomy<br />
in pancreatic carcinoma. Preliminary results <strong>of</strong> a<br />
prospective randomized study: pancreatoduodenectomy or<br />
pylorus-preserving pancreatoduodenectomy]. Chirurg 1999;<br />
70: 1454-1459<br />
296 Park YC, Kim SW, Jang JY, Ahn YJ, Park YH. Factors influencing<br />
delayed gastric emptying after pylorus-preserving<br />
pancreatoduodenectomy. J Am Coll Surg 2003; 196: 859-865<br />
297 Roder JD, Stein HJ, Hüttl W, Siewert JR. Pylorus-preserving<br />
versus standard pancreatico-duodenectomy: an analysis <strong>of</strong><br />
110 pancreatic and periampullary carcinomas. Br J Surg 1992;<br />
79: 152-155<br />
298 Diener MK, Knaebel HP, Heukaufer C, Antes G, Büchler<br />
MW, Seiler CM. A systematic review and meta-analysis <strong>of</strong><br />
pylorus-preserving versus classical pancreaticoduodenectomy<br />
for surgical treatment <strong>of</strong> periampullary and pancreatic<br />
carcinoma. Ann Surg 2007; 245: 187-200<br />
299 Seiler CA, Wagner M, Bachmann T, Redaelli CA, Schmied<br />
B, Uhl W, Friess H, Büchler MW. Randomized clinical trial<br />
<strong>of</strong> pylorus-preserving duodenopancreatectomy versus classical<br />
Whipple resection-long term results. Br J Surg 2005; 92:<br />
547-556<br />
300 Lin PW, Shan YS, Lin YJ, Hung CJ. Pancreaticoduodenectomy<br />
for pancreatic head <strong>cancer</strong>: PPPD versus Whipple procedure.<br />
Hepatogastroenterology 2005; 52: 1601-1604<br />
301 Schmidt CM, Powell ES, Yiannoutsos CT, Howard TJ,<br />
Wiebke EA, Wiesenauer CA, Baumgardner JA, Cummings<br />
OW, Jacobson LE, Broadie TA, Canal DF, Goulet RJ Jr, Curie<br />
EA, Cardenes H, Watkins JM, Loehrer PJ, Lillemoe KD, Madura<br />
JA. Pancreaticoduodenectomy: a 20-year experience in<br />
516 patients. Arch Surg 2004; 139: 718-725; discussion 725-727<br />
302 Bassi C, Falconi M, Salvia R, Mascetta G, Molinari E, Pederzoli<br />
P. <strong>Management</strong> <strong>of</strong> complications after pancreaticoduodenectomy<br />
in a high volume centre: results on 150 consecutive<br />
patients. Dig Surg 2001; 18: 453-457; discussion 458<br />
303 Shrikhande SV, D'Souza MA. Pancreatic fistula after pancreatectomy:<br />
evolving definitions, preventive strategies and modern<br />
management. <strong>World</strong> J Gastroenterol 2008; 14: 5789-5796<br />
304 Dixon E, Fingerhut A, Bassi C, Sutherland F, McKay A.<br />
Meta-analysis <strong>of</strong> pancreaticojejunostomy versus pancreaticogastrostomy<br />
reconstruction after pancreaticoduodenectomy:<br />
authors' comment (Br J Surg 2006; 93: 929-936). Br J Surg 2006;<br />
93: 1435<br />
305 Wente MN, Shrikhande SV, Müller MW, Diener MK, Seiler<br />
CM, Friess H, Büchler MW. Pancreaticojejunostomy versus<br />
pancreaticogastrostomy: systematic review and meta-analysis.<br />
Am J Surg 2007; 193: 171-183<br />
306 Andrén-Sandberg A, Wagner M, Tihanyi T, Löfgren P,<br />
Friess H. Technical aspects <strong>of</strong> left-sided pancreatic resection<br />
for <strong>cancer</strong>. Dig Surg 1999; 16: 305-312<br />
307 Shoup M, Brennan MF, McWhite K, Leung DH, Klimstra<br />
D, Conlon KC. The value <strong>of</strong> splenic preservation with distal<br />
pancreatectomy. Arch Surg 2002; 137: 164-168<br />
308 Warshaw AL. Conservation <strong>of</strong> the spleen with distal pancreatectomy.<br />
Arch Surg 1988; 123: 550-553<br />
309 Bilimoria MM, Cormier JN, Mun Y, Lee JE, Evans DB, Pi-<br />
WJG|www.wjgnet.com<br />
sters PW. Pancreatic leak after left pancreatectomy is reduced<br />
following main pancreatic duct ligation. Br J Surg 2003; 90:<br />
190-196<br />
310 Sheehan MK, Beck K, Creech S, Pickleman J, Aranha GV.<br />
Distal pancreatectomy: does the method <strong>of</strong> closure influence<br />
fistula formation? Am Surg 2002; 68: 264-267; discussion<br />
267-268<br />
311 Takeuchi K, Tsuzuki Y, Ando T, Sekihara M, Hara T, Kori<br />
T, Nakajima H, Kuwano H. Distal pancreatectomy: is staple<br />
closure beneficial? ANZ J Surg 2003; 73: 922-925<br />
312 Balzano G, Zerbi A, Cristallo M, Di Carlo V. The unsolved<br />
problem <strong>of</strong> fistula after left pancreatectomy: the benefit <strong>of</strong> cautious<br />
drain management. J Gastrointest Surg 2005; 9: 837-842<br />
313 Suzuki Y, Fujino Y, Tanioka Y, Hori Y, Ueda T, Takeyama Y,<br />
Tominaga M, Ku Y, Yamamoto YM, Kuroda Y. Randomized<br />
clinical trial <strong>of</strong> ultrasonic dissector or conventional division<br />
in distal pancreatectomy for non-fibrotic pancreas. Br J Surg<br />
1999; 86: 608-611<br />
314 Adam U, Makowiec F, Riediger H, Trzeczak S, Benz S, Hopt<br />
UT. [Distal pancreatic resection--indications, techniques and<br />
complications]. Zentralbl Chir 2001; 126: 908-912<br />
315 Moriura S, Kimura A, Ikeda S, Iwatsuka Y, Ikezawa T, Naiki<br />
K. Closure <strong>of</strong> the distal pancreatic stump with a seromuscular<br />
flap. Surg Today 1995; 25: 992-994<br />
316 Kluger Y, Alfici R, Abbley B, S<strong>of</strong>fer D, Aladgem D. Gastric<br />
serosal patch in distal pancreatectomy for injury: a neglected<br />
technique. Injury 1997; 28: 127-129<br />
317 Brennan MF, Moccia RD, Klimstra D. <strong>Management</strong> <strong>of</strong> adenocarcinoma<br />
<strong>of</strong> the body and tail <strong>of</strong> the pancreas. Ann Surg<br />
1996; 223: 506-511; discussion 511-512<br />
318 Sohn TA, Yeo CJ, Cameron JL, Koniaris L, Kaushal S,<br />
Abrams RA, Sauter PK, Coleman J, Hruban RH, Lillemoe<br />
KD. Resected adenocarcinoma <strong>of</strong> the pancreas-616 patients:<br />
results, outcomes, and prognostic indicators. J Gastrointest<br />
Surg 2000; 4: 567-579<br />
319 Mori T, Abe N, Sugiyama M, Atomi Y. Laparoscopic pancreatic<br />
surgery. J Hepatobiliary Pancreat Surg 2005; 12: 451-455<br />
320 Olivié D, Lepanto L, Billiard JS, Audet P, Lavallée JM. Predicting<br />
resectability <strong>of</strong> pancreatic head <strong>cancer</strong> with multidetector<br />
CT. Surgical and pathologic correlation. JOP 2007; 8:<br />
753-758<br />
321 Gagner M, Pomp A. Laparoscopic pylorus-preserving pancreatoduodenectomy.<br />
Surg Endosc 1994; 8: 408-410<br />
322 Gagner M, Palermo M. Laparoscopic Whipple procedure:<br />
review <strong>of</strong> the literature. J Hepatobiliary Pancreat Surg 2009; 16:<br />
726-730<br />
323 Kendrick ML, Cusati D. Total laparoscopic pancreaticoduodenectomy:<br />
feasibility and outcome in an early experience.<br />
Arch Surg 2010; 145: 19-23<br />
324 Palanivelu C, Jani K, Senthilnathan P, Parthasarathi R, Rajapandian<br />
S, Madhankumar MV. Laparoscopic pancreaticoduodenectomy:<br />
technique and outcomes. J Am Coll Surg 2007;<br />
205: 222-230<br />
325 Dulucq JL, Wintringer P, Mahajna A. Laparoscopic pancreaticoduodenectomy<br />
for benign and malignant diseases. Surg<br />
Endosc 2006; 20: 1045-1050<br />
326 Pugliese R, Scandroglio I, Sansonna F, Maggioni D, Costanzi<br />
A, Citterio D, Ferrari GC, Di Lernia S, Magistro C. Laparoscopic<br />
pancreaticoduodenectomy: a retrospective review <strong>of</strong><br />
19 cases. Surg Laparosc Endosc Percutan Tech 2008; 18: 13-18<br />
327 Sahm M, Pross M, Schubert D, Lippert H. Laparoscopic distal<br />
pancreatic resection: our own experience in the treatment<br />
<strong>of</strong> solid tumors. Surg Today 2009; 39: 1103-1108<br />
328 Al-Taan OS, Stephenson JA, Briggs C, Pollard C, Metcalfe<br />
MS, Dennison AR. Laparoscopic pancreatic surgery: a review<br />
<strong>of</strong> present results and future prospects. HPB (Oxford)<br />
2010; 12: 239-243<br />
329 Kooby DA, Gillespie T, Bentrem D, Nakeeb A, Schmidt MC,<br />
Merchant NB, Parikh AA, Martin RC 2nd, Scoggins CR,<br />
Ahmad S, Kim HJ, Park J, Johnston F, Strouch MJ, Menze A,<br />
Rymer J, McClaine R, Strasberg SM, Talamonti MS, Staley<br />
894 February 21, 2011|Volume 17|Issue 7|
CA, McMasters KM, Lowy AM, Byrd-Sellers J, Wood WC,<br />
Hawkins WG. Left-sided pancreatectomy: a multicenter<br />
comparison <strong>of</strong> laparoscopic and open approaches. Ann Surg<br />
2008; 248: 438-446<br />
330 Mabrut JY, Fernandez-Cruz L, Azagra JS, Bassi C, Delvaux<br />
G, Weerts J, Fabre JM, Boulez J, Baulieux J, Peix JL, Gigot JF.<br />
Laparoscopic pancreatic resection: results <strong>of</strong> a multicenter<br />
European study <strong>of</strong> 127 patients. Surgery 2005; 137: 597-605<br />
331 Fernández-Cruz L, Cosa R, Blanco L, Levi S, López-Boado<br />
MA, Navarro S. Curative laparoscopic resection for pancreatic<br />
neoplasms: a critical analysis from a single institution. J<br />
Gastrointest Surg 2007; 11: 1607-1621; discussion 1621-1622<br />
332 Briggs CD, Mann CD, Irving GR, Neal CP, Peterson M, Cameron<br />
IC, Berry DP. Systematic review <strong>of</strong> minimally invasive<br />
pancreatic resection. J Gastrointest Surg 2009; 13: 1129-1137<br />
333 Baker MS, Bentrem DJ, Ujiki MB, Stocker S, Talamonti MS.<br />
A prospective single institution comparison <strong>of</strong> peri-operative<br />
outcomes for laparoscopic and open distal pancreatectomy.<br />
Surgery 2009; 146: 635-643; discussion 643-645<br />
334 Sohn TA, Campbell KA, Pitt HA, Sauter PK, Coleman JA,<br />
Lillemo KD, Yeo CJ, Cameron JL. Quality <strong>of</strong> life and longterm<br />
survival after surgery for chronic pancreatitis. J Gastrointest<br />
Surg 2000; 4: 355-364; discussion 364-365<br />
335 Reddy S, Wolfgang CL, Cameron JL, Eckhauser F, Choti<br />
MA, Schulick RD, Edil BH, Pawlik TM. Total pancreatectomy<br />
for pancreatic adenocarcinoma: evaluation <strong>of</strong> morbidity<br />
and long-term survival. Ann Surg 2009; 250: 282-287<br />
336 Pliam MB, ReMine WH. Further evaluation <strong>of</strong> total pancreatectomy.<br />
Arch Surg 1975; 110: 506-512<br />
337 Bahra M, Neuhaus P. Pancreas: Is there still a role for total<br />
pancreatectomy? Nat Rev Gastroenterol Hepatol 2010; 7: 72-74<br />
338 Yeo CJ, Cameron JL, Sohn TA, Lillemoe KD, Pitt HA, Talamini<br />
MA, Hruban RH, Ord SE, Sauter PK, Coleman J, Zahurak<br />
ML, Grochow LB, Abrams RA. Six hundred fifty consecutive<br />
pancreaticoduodenectomies in the 1990s: pathology, complications,<br />
and outcomes. Ann Surg 1997; 226: 248-257; discussion<br />
257-260<br />
339 Pezzilli R. Diabetic control after total pancreatectomy. Dig<br />
Liver Dis 2006; 38: 420-422<br />
340 Hartwig W, Hackert T, Hinz U, Hassenpflug M, Strobel O,<br />
Büchler MW, Werner J. Multivisceral resection for pancreatic<br />
malignancies: risk-analysis and long-term outcome. Ann<br />
Surg 2009; 250: 81-87<br />
341 Adams RB, Allen PJ. Surgical treatment <strong>of</strong> resectable and<br />
borderline resectable pancreatic <strong>cancer</strong>: expert consensus<br />
statement by Evans et al. Ann Surg Oncol 2009; 16: 1745-1750<br />
342 Bachellier P, Nakano H, Oussoultzoglou PD, Weber JC,<br />
Boudjema K, Wolf PD, Jaeck D. Is pancreaticoduodenectomy<br />
with mesentericoportal venous resection safe and worthwhile?<br />
Am J Surg 2001; 182: 120-129<br />
343 Siriwardana HP, Siriwardena AK. Systematic review <strong>of</strong> outcome<br />
<strong>of</strong> synchronous portal-superior mesenteric vein resection<br />
during pancreatectomy for <strong>cancer</strong>. Br J Surg 2006; 93: 662-673<br />
344 Leach SD, Lee JE, Charnsangavej C, Cleary KR, Lowy AM,<br />
Fenoglio CJ, Pisters PW, Evans DB. Survival following<br />
pancreaticoduodenectomy with resection <strong>of</strong> the superior<br />
mesenteric-portal vein confluence for adenocarcinoma <strong>of</strong> the<br />
pancreatic head. Br J Surg 1998; 85: 611-617<br />
345 Al-Haddad M, Martin JK, Nguyen J, Pungpapong S, Raimondo<br />
M, Woodward T, Kim G, Noh K, Wallace MB. Vascular resection<br />
and reconstruction for pancreatic malignancy: a single<br />
center survival study. J Gastrointest Surg 2007; 11: 1168-1174<br />
346 Amano H, Miura F, Toyota N, Wada K, Katoh K, Hayano<br />
K, Kadowaki S, Shibuya M, Maeno S, Eguchi T, Takada T,<br />
Asano T. Is pancreatectomy with arterial reconstruction a<br />
safe and useful procedure for locally advanced pancreatic<br />
<strong>cancer</strong>? J Hepatobiliary Pancreat Surg 2009; 16: 850-857<br />
347 Stitzenberg KB, Watson JC, Roberts A, Kagan SA, Cohen SJ,<br />
Konski AA, H<strong>of</strong>fman JP. Survival after pancreatectomy with<br />
major arterial resection and reconstruction. Ann Surg Oncol<br />
2008; 15: 1399-1406<br />
WJG|www.wjgnet.com<br />
Sharma C et al . Clinical advances in pancreatic carcinoma<br />
348 Hirano S, Kondo S, Hara T, Ambo Y, Tanaka E, Shichinohe<br />
T, Suzuki O, Hazama K. Distal pancreatectomy with en bloc<br />
celiac axis resection for locally advanced pancreatic body<br />
<strong>cancer</strong>: long-term results. Ann Surg 2007; 246: 46-51<br />
349 Cubilla AL, Fortner J, Fitzgerald PJ. Lymph node involvement<br />
in carcinoma <strong>of</strong> the head <strong>of</strong> the pancreas area. Cancer<br />
1978; 41: 880-887<br />
350 Ishikawa O, Ohhigashi H, Sasaki Y, Kabuto T, Fukuda I,<br />
Furukawa H, Imaoka S, Iwanaga T. Practical usefulness <strong>of</strong><br />
lymphatic and connective tissue clearance for the carcinoma<br />
<strong>of</strong> the pancreas head. Ann Surg 1988; 208: 215-220<br />
351 Manabe T, Ohshio G, Baba N, Miyashita T, Asano N, Tamura<br />
K, Yamaki K, Nonaka A, Tobe T. Radical pancreatectomy<br />
for ductal cell carcinoma <strong>of</strong> the head <strong>of</strong> the pancreas. Cancer<br />
1989; 64: 1132-1137<br />
352 Kawarada Y, Yokoi H, Isaji S, Naganuma T, Tabata M, Machishi<br />
H, Das BC, Takahashi K, Murabayashi K. Modified<br />
standard pancreaticoduodenectomy for the treatment <strong>of</strong><br />
pancreatic head <strong>cancer</strong>. Digestion 1999; 60 Suppl 1: 120-125<br />
353 Samra JS, Gananadha S, Hugh TJ. Surgical management <strong>of</strong><br />
carcinoma <strong>of</strong> the head <strong>of</strong> pancreas: extended lymphadenectomy<br />
or modified en bloc resection? ANZ J Surg 2008; 78:<br />
228-236<br />
354 Pedrazzoli S, DiCarlo V, Dionigi R, Mosca F, Pederzoli P,<br />
Pasquali C, Klöppel G, Dhaene K, Michelassi F. Standard<br />
versus extended lymphadenectomy associated with pancreatoduodenectomy<br />
in the surgical treatment <strong>of</strong> adenocarcinoma<br />
<strong>of</strong> the head <strong>of</strong> the pancreas: a multicenter, prospective,<br />
randomized study. Lymphadenectomy Study Group. Ann<br />
Surg 1998; 228: 508-517<br />
355 Michalski CW, Kleeff J, Wente MN, Diener MK, Büchler<br />
MW, Friess H. Systematic review and meta-analysis <strong>of</strong> standard<br />
and extended lymphadenectomy in pancreaticoduodenectomy<br />
for pancreatic <strong>cancer</strong>. Br J Surg 2007; 94: 265-273<br />
356 Lieberman MD, Kilburn H, Lindsey M, Brennan MF. Relation<br />
<strong>of</strong> perioperative deaths to hospital volume among patients<br />
undergoing pancreatic resection for malignancy. Ann<br />
Surg 1995; 222: 638-645<br />
357 Imperato PJ, Nenner RP, Starr HA, Will TO, Rosenberg CR,<br />
Dearie MB. The effects <strong>of</strong> regionalization on clinical outcomes<br />
for a high risk surgical procedure: a study <strong>of</strong> the Whipple procedure<br />
in New York State. Am J Med Qual 1996; 11: 193-197<br />
358 Rosemurgy AS, Bloomston M, Serafini FM, Coon B, Murr<br />
MM, Carey LC. Frequency with which surgeons undertake<br />
pancreaticoduodenectomy determines length <strong>of</strong> stay, hospital<br />
charges, and in-hospital mortality. J Gastrointest Surg<br />
2001; 5: 21-26<br />
359 Sosa JA, Bowman HM, Gordon TA, Bass EB, Yeo CJ, Lillemoe<br />
KD, Pitt HA, Tielsch JM, Cameron JL. Importance <strong>of</strong><br />
hospital volume in the overall management <strong>of</strong> pancreatic<br />
<strong>cancer</strong>. Ann Surg 1998; 228: 429-438<br />
360 Ho V, Heslin MJ. Effect <strong>of</strong> hospital volume and experience on<br />
in-hospital mortality for pancreaticoduodenectomy. Ann Surg<br />
2003; 237: 509-514<br />
361 Simunovic M, To T, Theriault M, Langer B. Relation between<br />
hospital surgical volume and outcome for pancreatic resection<br />
for neoplasm in a publicly funded health care system.<br />
CMAJ 1999; 160: 643-648<br />
362 Gouma DJ, van Geenen RC, van Gulik TM, de Haan RJ, de<br />
Wit LT, Busch OR, Obertop H. Rates <strong>of</strong> complications and<br />
death after pancreaticoduodenectomy: risk factors and the<br />
impact <strong>of</strong> hospital volume. Ann Surg 2000; 232: 786-795<br />
363 Nienhuijs SW, Rutten HJ, Luiten EJ, van Driel OJ, Reemst<br />
PH, Lemmens VE, de Hingh IH. Reduction <strong>of</strong> in-hospital<br />
mortality following regionalisation <strong>of</strong> pancreatic surgery in<br />
the south-east <strong>of</strong> the Netherlands. Eur J Surg Oncol 2010; 36:<br />
652-656<br />
364 Edge SB, Schmieg RE Jr, Rosenl<strong>of</strong> LK, Wilhelm MC. Pancreas<br />
<strong>cancer</strong> resection outcome in American University centers<br />
in 1989-1990. Cancer 1993; 71: 3502-3508<br />
365 Birkmeyer JD, Finlayson SR, Tosteson AN, Sharp SM, War-<br />
895 February 21, 2011|Volume 17|Issue 7|
Sharma C et al . Clinical advances in pancreatic carcinoma<br />
shaw AL, Fisher ES. Effect <strong>of</strong> hospital volume on in-hospital<br />
mortality with pancreaticoduodenectomy. Surgery 1999; 125:<br />
250-256<br />
366 Bilimoria KY, Bentrem DJ, Ko CY, Tomlinson JS, Stewart<br />
AK, Winchester DP, Talamonti MS. Multimodality therapy<br />
for pancreatic <strong>cancer</strong> in the U.S. : utilization, outcomes, and<br />
the effect <strong>of</strong> hospital volume. Cancer 2007; 110: 1227-1234<br />
367 Bilimoria KY, Bentrem DJ, Ko CY, Stewart AK, Winchester<br />
DP, Talamonti MS. National failure to operate on early <strong>stage</strong><br />
pancreatic <strong>cancer</strong>. Ann Surg 2007; 246: 173-180<br />
368 Sherman WH, Fine RL. Combination gemcitabine and<br />
docetaxel therapy in advanced adenocarcinoma <strong>of</strong> the pancreas.<br />
Oncology 2001; 60: 316-321<br />
369 Moertel CG. Chemotherapy <strong>of</strong> gastrointestinal <strong>cancer</strong>. Clin<br />
Gastroenterol 1976; 5: 777-793<br />
370 Burris HA 3rd, Moore MJ, Andersen J, Green MR, Rothenberg<br />
ML, Modiano MR, Cripps MC, Portenoy RK, Storniolo AM,<br />
Tarass<strong>of</strong>f P, Nelson R, Dorr FA, Stephens CD, Von H<strong>of</strong>f DD.<br />
Improvements in survival and clinical benefit with gemcitabine<br />
as first-line therapy for patients with advanced pancreas<br />
<strong>cancer</strong>: a randomized trial. J Clin Oncol 1997; 15: 2403-2413<br />
371 Fatima J, Schnelldorfer T, Barton J, Wood CM, Wiste HJ,<br />
Smyrk TC, Zhang L, Sarr MG, Nagorney DM, Farnell MB. Pancreatoduodenectomy<br />
for ductal adenocarcinoma: implications<br />
<strong>of</strong> positive margin on survival. Arch Surg 2010; 145: 167-172<br />
372 Shimada K, Sakamoto Y, Sano T, Kosuge T. Prognostic factors<br />
after distal pancreatectomy with extended lymphadenectomy<br />
for invasive pancreatic adenocarcinoma <strong>of</strong> the body<br />
and tail. Surgery 2006; 139: 288-295<br />
373 Raut CP, Tseng JF, Sun CC, Wang H, Wolff RA, Crane CH,<br />
Hwang R, Vauthey JN, Abdalla EK, Lee JE, Pisters PW, Evans<br />
DB. Impact <strong>of</strong> resection status on pattern <strong>of</strong> failure and<br />
survival after pancreaticoduodenectomy for pancreatic adenocarcinoma.<br />
Ann Surg 2007; 246: 52-60<br />
374 Moon HJ, Jang KT, Heo JS, Choi SH, Joh JW, Kim YI. [A result<br />
<strong>of</strong> surgical treatment for ductal adenocarcinoma <strong>of</strong> the<br />
head <strong>of</strong> the pancreas]. Korean J Gastroenterol 2003; 42: 156-163<br />
375 Howard TJ, Krug JE, Yu J, Zyromski NJ, Schmidt CM, Jacobson<br />
LE, Madura JA, Wiebke EA, Lillemoe KD. A marginnegative<br />
R0 resection accomplished with minimal postoperative<br />
complications is the surgeon's contribution to longterm<br />
survival in pancreatic <strong>cancer</strong>. J Gastrointest Surg 2006;<br />
10: 1338-1345; discussion 1345-1346<br />
376 Kato K, Yamada S, Sugimoto H, Kanazumi N, Nomoto S,<br />
Takeda S, Kodera Y, Morita S, Nakao A. Prognostic factors<br />
for survival after extended pancreatectomy for pancreatic<br />
head <strong>cancer</strong>: influence <strong>of</strong> resection margin status on survival.<br />
Pancreas 2009; 38: 605-612<br />
377 Sorg C, Schmidt J, Büchler MW, Edler L, Märten A. Examination<br />
<strong>of</strong> external validity in randomized controlled trials for<br />
adjuvant treatment <strong>of</strong> pancreatic adenocarcinoma. Pancreas<br />
2009; 38: 542-550<br />
378 Further evidence <strong>of</strong> effective adjuvant combined radiation<br />
and chemotherapy following curative resection <strong>of</strong> pancreatic<br />
<strong>cancer</strong>. Gastrointestinal Tumor Study Group. Cancer 1987;<br />
59: 2006-2010<br />
379 Klinkenbijl JH, Jeekel J, Sahmoud T, van Pel R, Couvreur<br />
ML, Veenh<strong>of</strong> CH, Arnaud JP, Gonzalez DG, de Wit LT, Hennipman<br />
A, Wils J. Adjuvant radiotherapy and 5-fluorouracil<br />
after curative resection <strong>of</strong> <strong>cancer</strong> <strong>of</strong> the pancreas and periampullary<br />
region: phase III trial <strong>of</strong> the EORTC gastrointestinal<br />
tract <strong>cancer</strong> cooperative group. Ann Surg 1999; 230: 776-782;<br />
discussion 782-784<br />
380 Neoptolemos JP, Stocken DD, Friess H, Bassi C, Dunn JA,<br />
Hickey H, Beger H, Fernandez-Cruz L, Dervenis C, Lacaine<br />
F, Falconi M, Pederzoli P, Pap A, Spooner D, Kerr DJ, Büchler<br />
MW. A randomized trial <strong>of</strong> chemoradiotherapy and chemotherapy<br />
after resection <strong>of</strong> pancreatic <strong>cancer</strong>. N Engl J Med<br />
2004; 350: 1200-1210<br />
381 Crane CH, Winter K, Regine WF, Safran H, Rich TA, Curran<br />
W, Wolff RA, Willett CG. Phase II study <strong>of</strong> bevacizumab with<br />
WJG|www.wjgnet.com<br />
concurrent capecitabine and radiation followed by maintenance<br />
gemcitabine and bevacizumab for locally advanced<br />
pancreatic <strong>cancer</strong>: Radiation Therapy Oncology Group RTOG<br />
0411. J Clin Oncol 2009; 27: 4096-4102<br />
382 Oettle H, Post S, Neuhaus P, Gellert K, Langrehr J, Ridwelski<br />
K, Schramm H, Fahlke J, Zuelke C, Burkart C, Gutberlet K,<br />
Kettner E, Schmalenberg H, Weigang-Koehler K, Bechstein<br />
WO, Niedergethmann M, Schmidt-Wolf I, Roll L, Doerken B,<br />
Riess H. Adjuvant chemotherapy with gemcitabine vs observation<br />
in patients undergoing curative-intent resection <strong>of</strong> pancreatic<br />
<strong>cancer</strong>: a randomized controlled trial. JAMA 2007; 297:<br />
267-277<br />
383 Gillen S, Schuster T, Meyer Zum Büschenfelde C, Friess H,<br />
Kleeff J. Preoperative/neoadjuvant therapy in pancreatic<br />
<strong>cancer</strong>: a systematic review and meta-analysis <strong>of</strong> response<br />
and resection percentages. PLoS Med 2010; 7: e1000267<br />
384 Shah AP, Strauss JB, Abrams RA. Review and commentary<br />
on the role <strong>of</strong> radiation therapy in the adjuvant management<br />
<strong>of</strong> pancreatic <strong>cancer</strong>. Am J Clin Oncol 2010; 33: 101-106<br />
385 Stocken DD, Büchler MW, Dervenis C, Bassi C, Jeekel H,<br />
Klinkenbijl JH, Bakkevold KE, Takada T, Amano H, Neoptolemos<br />
JP. Meta-analysis <strong>of</strong> randomised adjuvant therapy<br />
trials for pancreatic <strong>cancer</strong>. Br J Cancer 2005; 92: 1372-1381<br />
386 Kim R, Saif MW. Is there an optimal neoadjuvant therapy<br />
for locally advanced pancreatic <strong>cancer</strong>? JOP 2007; 8: 279-288<br />
387 Moertel CG, Childs DS Jr, Reitemeier RJ, Colby MY Jr, Holbrook<br />
MA. Combined 5-fluorouracil and supervoltage radiation<br />
therapy <strong>of</strong> locally unresectable gastrointestinal <strong>cancer</strong>.<br />
Lancet 1969; 2: 865-867<br />
388 Moertel CG, Frytak S, Hahn RG, O'Connell MJ, Reitemeier<br />
RJ, Rubin J, Schutt AJ, Weiland LH, Childs DS, Holbrook<br />
MA, Lavin PT, Livstone E, Spiro H, Knowlton A, Kalser M,<br />
Barkin J, Lessner H, Mann-Kaplan R, Ramming K, Douglas<br />
HO Jr, Thomas P, Nave H, Bateman J, Lokich J, Brooks J,<br />
Chaffey J, Corson JM, Zamcheck N, Novak JW. Therapy <strong>of</strong><br />
locally unresectable pancreatic carcinoma: a randomized<br />
comparison <strong>of</strong> high dose (6000 rads) radiation alone, moderate<br />
dose radiation (4000 rads + 5-fluorouracil), and high dose<br />
radiation + 5-fluorouracil: The Gastrointestinal Tumor Study<br />
Group. Cancer 1981; 48: 1705-1710<br />
389 Ogawa K, Karasawa K, Ito Y, Ogawa Y, Jingu K, Onishi H,<br />
Aoki S, Wada H, Kokubo M, Etoh H, Kazumoto T, Takayama<br />
M, Negoro Y, Nemoto K, Nishimura Y. Intraoperative<br />
radiotherapy for resected pancreatic <strong>cancer</strong>: a multi-institutional<br />
retrospective analysis <strong>of</strong> 210 patients. Int J Radiat Oncol<br />
Biol Phys 2010; 77: 734-742<br />
390 Takamori H, Hiraoka T, Kanemitsu K, Tsuji T, Tanaka H,<br />
Chikamoto A, Horino K, Beppu T, Hirota M, Baba H. Longterm<br />
outcomes <strong>of</strong> extended radical resection combined with<br />
intraoperative radiation therapy for pancreatic <strong>cancer</strong>. J<br />
Hepatobiliary Pancreat Surg 2008; 15: 603-607<br />
391 Klautke G, Brunner TB. Radiotherapy in pancreatic <strong>cancer</strong>.<br />
Strahlenther Onkol 2008; 184: 557-564<br />
392 Carter DC. Cancer <strong>of</strong> the pancreas. Gut 1990; 31: 494-496<br />
393 Espat NJ, Brennan MF, Conlon KC. Patients with laparoscopically<br />
<strong>stage</strong>d unresectable pancreatic adenocarcinoma<br />
do not require subsequent surgical biliary or gastric bypass.<br />
J Am Coll Surg 1999; 188: 649-655; discussion 655-657<br />
394 Warshaw AL, Swanson RS. Pancreatic <strong>cancer</strong> in 1988. Possibilities<br />
and probabilities. Ann Surg 1988; 208: 541-553<br />
395 Singh SM, Longmire WP Jr, Reber HA. Surgical palliation<br />
for pancreatic <strong>cancer</strong>. The UCLA experience. Ann Surg 1990;<br />
212: 132-139<br />
396 Lillemoe KD, Cameron JL, Hardacre JM, Sohn TA, Sauter<br />
PK, Coleman J, Pitt HA, Yeo CJ. Is prophylactic gastrojejunostomy<br />
indicated for unresectable periampullary <strong>cancer</strong>? A<br />
prospective randomized trial. Ann Surg 1999; 230: 322-328;<br />
discussion 328-330<br />
397 van Ho<strong>of</strong>t JE, Uitdehaag MJ, Bruno MJ, Timmer R, Siersema<br />
PD, Dijkgraaf MG, Fockens P. Efficacy and safety <strong>of</strong> the new<br />
WallFlex enteral stent in palliative treatment <strong>of</strong> malignant<br />
896 February 21, 2011|Volume 17|Issue 7|
gastric outlet obstruction (DUOFLEX study): a prospective<br />
multicenter study. Gastrointest Endosc 2009; 69: 1059-1066<br />
398 Kim JH, Song HY, Shin JH, Hu HT, Lee SK, Jung HY, Yook<br />
JH. Metallic stent placement in the palliative treatment <strong>of</strong><br />
malignant gastric outlet obstructions: primary gastric carcinoma<br />
versus pancreatic carcinoma. AJR Am J Roentgenol<br />
2009; 193: 241-247<br />
399 Maetani I, Tada T, Ukita T, Inoue H, Sakai Y, Nagao J. Comparison<br />
<strong>of</strong> duodenal stent placement with surgical gastrojejunostomy<br />
for palliation in patients with duodenal obstructions<br />
caused by pancreaticobiliary malignancies. Endoscopy 2004;<br />
36: 73-78<br />
400 Maetani I, Akatsuka S, Ikeda M, Tada T, Ukita T, Nakamura<br />
Y, Nagao J, Sakai Y. Self-expandable metallic stent placement<br />
for palliation in gastric outlet obstructions caused by gastric<br />
<strong>cancer</strong>: a comparison with surgical gastrojejunostomy. J Gastroenterol<br />
2005; 40: 932-937<br />
401 Mehta S, Hindmarsh A, Cheong E, Cockburn J, Saada J,<br />
Tighe R, Lewis MP, Rhodes M. Prospective randomized trial<br />
<strong>of</strong> laparoscopic gastrojejunostomy versus duodenal stenting<br />
for malignant gastric outflow obstruction. Surg Endosc 2006;<br />
20: 239-242<br />
402 Watanapa P, Williamson RC. Surgical palliation for pancreatic<br />
<strong>cancer</strong>: developments during the past two decades. Br J<br />
Surg 1992; 79: 8-20<br />
403 Neuberger TJ, Wade TP, Swope TJ, Virgo KS, Johnson FE.<br />
Palliative operations for pancreatic <strong>cancer</strong> in the hospitals <strong>of</strong><br />
the U.S. Department <strong>of</strong> Veterans Affairs from 1987 to 1991.<br />
Am J Surg 1993; 166: 632-636; discussion 636-637<br />
404 Piñol V, Castells A, Bordas JM, Real MI, Llach J, Montañà X,<br />
Feu F, Navarro S. Percutaneous self-expanding metal stents<br />
versus endoscopic polyethylene endoprostheses for treating<br />
malignant biliary obstruction: randomized clinical trial. Radiology<br />
2002; 225: 27-34<br />
405 Maosheng D, Ohtsuka T, Ohuchida J, Inoue K, Yokohata K,<br />
Yamaguchi K, Chijiiwa K, Tanaka M. Surgical bypass versus<br />
metallic stent for unresectable pancreatic <strong>cancer</strong>. J Hepatobiliary<br />
Pancreat Surg 2001; 8: 367-373<br />
406 Smith AC, Dowsett JF, Russell RC, Hatfield AR, Cotton PB.<br />
Randomised trial <strong>of</strong> endoscopic stenting versus surgical bypass<br />
in malignant low bileduct obstruction. Lancet 1994; 344:<br />
1655-1660<br />
407 Artifon EL, Sakai P, Cunha JE, Dupont A, Filho FM, Hondo<br />
FY, Ishioka S, Raju GS. Surgery or endoscopy for palliation<br />
<strong>of</strong> biliary obstruction due to metastatic pancreatic <strong>cancer</strong>. Am<br />
J Gastroenterol 2006; 101: 2031-2037<br />
408 Taylor MC, McLeod RS, Langer B. Biliary stenting versus<br />
bypass surgery for the palliation <strong>of</strong> malignant distal bile duct<br />
obstruction: a meta-analysis. Liver Transpl 2000; 6: 302-308<br />
409 Knyrim K, Wagner HJ, Pausch J, Vakil N. A prospective, randomized,<br />
controlled trial <strong>of</strong> metal stents for malignant obstruction<br />
<strong>of</strong> the common bile duct. Endoscopy 1993; 25: 207-212<br />
410 Davids PH, Groen AK, Rauws EA, Tytgat GN, Huibregtse K.<br />
Randomised trial <strong>of</strong> self-expanding metal stents versus polyethylene<br />
stents for distal malignant biliary obstruction. Lancet<br />
1992; 340: 1488-1492<br />
411 Nakai Y, Isayama H, Kawabe T, Tsujino T, Yoshida H, Sasaki<br />
WJG|www.wjgnet.com<br />
Sharma C et al . Clinical advances in pancreatic carcinoma<br />
T, Tada M, Arizumi T, Yagioka H, Kogure H, Togawa O, Ito<br />
Y, Matsubara S, Hirano K, Sasahira N, Omata M. Efficacy and<br />
safety <strong>of</strong> metallic stents in patients with unresectable pancreatic<br />
<strong>cancer</strong> receiving gemcitabine. Pancreas 2008; 37: 405-410<br />
412 Maire F, Hammel P, Ponsot P, Aubert A, O'Toole D, Hentic<br />
O, Levy P, Ruszniewski P. Long-term outcome <strong>of</strong> biliary<br />
and duodenal stents in palliative treatment <strong>of</strong> patients with<br />
unresectable adenocarcinoma <strong>of</strong> the head <strong>of</strong> pancreas. Am J<br />
Gastroenterol 2006; 101: 735-742<br />
413 Wang T, Tian FZ, Cai ZH, Li X, Cheng T, Shi L, Cheng Q.<br />
Ultrasonic interventional analgesia in pancreatic carcinoma<br />
with chemical destruction <strong>of</strong> celiac ganglion. <strong>World</strong> J Gastroenterol<br />
2006; 12: 3288-3291<br />
414 Caraceni A, Portenoy RK. Pain management in patients with<br />
pancreatic carcinoma. Cancer 1996; 78: 639-653<br />
415 Shulman M, Harris JE, Lubenow TR, Nath HA, Ivankovich<br />
AD. Comparison <strong>of</strong> epidural butamben to celiac plexus<br />
neurolytic block for the treatment <strong>of</strong> the pain <strong>of</strong> pancreatic<br />
<strong>cancer</strong>. Clin J Pain 2000; 16: 304-309<br />
416 Eisenberg E, Carr DB, Chalmers TC. Neurolytic celiac plexus<br />
block for treatment <strong>of</strong> <strong>cancer</strong> pain: a meta-analysis. Anesth<br />
Analg 1995; 80: 290-295<br />
417 Gunaratnam NT, Sarma AV, Norton ID, Wiersema MJ. A<br />
prospective study <strong>of</strong> EUS-guided celiac plexus neurolysis for<br />
pancreatic <strong>cancer</strong> pain. Gastrointest Endosc 2001; 54: 316-324<br />
418 Puli SR, Reddy JB, Bechtold ML, Antillon MR, Brugge WR.<br />
EUS-guided celiac plexus neurolysis for pain due to chronic<br />
pancreatitis or pancreatic <strong>cancer</strong> pain: a meta-analysis and<br />
systematic review. Dig Dis Sci 2009; 54: 2330-2337<br />
419 Wong GY, Schroeder DR, Carns PE, Wilson JL, Martin DP,<br />
Kinney MO, Mantilla CB, Warner DO. Effect <strong>of</strong> neurolytic<br />
celiac plexus block on pain relief, quality <strong>of</strong> life, and survival<br />
in patients with unresectable pancreatic <strong>cancer</strong>: a randomized<br />
controlled trial. JAMA 2004; 291: 1092-1099<br />
420 Russell RC. Palliation <strong>of</strong> pain and jaundice: an overview.<br />
Ann Oncol 1999; 10 Suppl 4: 165-169<br />
421 Bown SG, Rogowska AZ, Whitelaw DE, Lees WR, Lovat LB,<br />
Ripley P, Jones L, Wyld P, Gillams A, Hatfield AW. Photodynamic<br />
therapy for <strong>cancer</strong> <strong>of</strong> the pancreas. Gut 2002; 50: 549-557<br />
422 Morganti AG, Trodella L, Valentini V, Barbi S, Macchia G,<br />
Mantini G, Turriziani A, Cellini N. Pain relief with shortterm<br />
irradiation in locally advanced carcinoma <strong>of</strong> the pancreas.<br />
J Palliat Care 2003; 19: 258-262<br />
423 De Conno F, Saita L, Ripamonti C, Ventafridda V. Subcutaneous<br />
octreotide in the treatment <strong>of</strong> pain in advanced <strong>cancer</strong><br />
patients. J Pain Symptom Manage 1994; 9: 34-38<br />
424 Bruno MJ, Haverkort EB, Tijssen GP, Tytgat GN, van Leeuwen<br />
DJ. Placebo controlled trial <strong>of</strong> enteric coated pancreatin<br />
microsphere treatment in patients with unresectable <strong>cancer</strong><br />
<strong>of</strong> the pancreatic head region. Gut 1998; 42: 92-96<br />
425 Dewys WD, Begg C, Lavin PT, Band PR, Bennett JM, Bertino<br />
JR, Cohen MH, Douglass HO Jr, Engstrom PF, Ezdinli<br />
EZ, Horton J, Johnson GJ, Moertel CG, Oken MM, Perlia<br />
C, Rosenbaum C, Silverstein MN, Skeel RT, Sponzo RW,<br />
Tormey DC. Prognostic effect <strong>of</strong> weight loss prior to chemotherapy<br />
in <strong>cancer</strong> patients. Eastern Cooperative Oncology<br />
Group. Am J Med 1980; 69: 491-497<br />
S- Editor Tian L L- Editor Webster JR E- Editor Lin YP<br />
897 February 21, 2011|Volume 17|Issue 7|
Online Submissions: http://www.wjgnet.com/1007-9327<strong>of</strong>fice<br />
wjg@wjgnet.com<br />
doi:10.3748/wjg.v17.i7.898<br />
Neuroprotective action <strong>of</strong> Ginkgo biloba on the enteric<br />
nervous system <strong>of</strong> diabetic rats<br />
Glasiella Gonzalez Perez da Silva, Jacqueline Nelisis Zanoni, Nilza Cristina Buttow<br />
Glasiella Gonzalez Perez da Silva, Jacqueline Nelisis Zanoni,<br />
Nilza Cristina Buttow, Department <strong>of</strong> Morphological Sciences,<br />
Universidade Estadual de Maringá, Av. Colombo, 5790<br />
Bloco H-79, CEP 87020-900, Maringá, PR, Brazil<br />
Author contributions: da Silva GGP performed data collection<br />
and wrote the paper; Buttow NC designed the study, contributed<br />
analytical tools and corrected the paper; Zanoni JN analyzed the<br />
data.<br />
Correspondence to: Nilza Cristina Buttow, PhD, Department<br />
<strong>of</strong> Morphological Sciences, Universidade Estadual de Maringá,<br />
Av. Colombo, 5790 Bloco H-79, CEP 87020-900, Maringá, PR,<br />
Brazil. ncbuttow@uem.br<br />
Telephone: +55-44-30111370 Fax: +55-44-30114340<br />
Received: February 18, 2010 Revised: March 24, 2010<br />
Accepted: March 31, 2010<br />
Published online: February 21, 2011<br />
Abstract<br />
AIM: To investigate the effect <strong>of</strong> Ginkgo biloba extract<br />
on the enteric neurons in the small intestine <strong>of</strong> diabetic<br />
rats.<br />
METHODS: Fifteen Wistar rats were divided into three<br />
groups: control group (C), diabetic group (D) and diabetic-treated<br />
(DT) daily with EGb 761 extract (50 mg/kg<br />
body weight) for 120 d. The enteric neurons were identified<br />
by the myosin-V immunohistochemical technique.<br />
The neuronal density and the cell body area were also<br />
analyzed.<br />
RESULTS: There was a significant decrease in the<br />
neuronal population (myenteric plexus P = 0.0351;<br />
submucous plexus P = 0.0217) in both plexuses <strong>of</strong> the<br />
jejunum in group D when compared to group C. With<br />
regard to the ileum, there was a significant decrease (P<br />
= 0.0117) only in the myenteric plexus. The DT group<br />
showed preservation <strong>of</strong> the neuronal population in the<br />
jejunum submucous plexus and in the myenteric plexus<br />
in the ileum. The cell body area in group D increased<br />
significantly (P = 0.0001) in the myenteric plexus <strong>of</strong><br />
WJG|www.wjgnet.com<br />
<strong>World</strong> J Gastroenterol 2011 February 21; 17(7): 898-905<br />
ISSN 1007-9327 (print) ISSN 2219-2840 (online)<br />
© 2011 Baishideng. All rights reserved.<br />
both segments studied as well as in the ileum submucosal<br />
plexus, when compared to C. The treatment reduced<br />
(P = 0.0001) the cell body area <strong>of</strong> the submucosal neurons<br />
<strong>of</strong> both segments and the jejunum myenteric neurons.<br />
CONCLUSION: The purified Ginkgo biloba extract has<br />
a neuroprotective effect on the jejunum submucous<br />
plexus and the myenteric plexus <strong>of</strong> the ileum <strong>of</strong> diabetic<br />
rats.<br />
© 2011 Baishideng. All rights reserved.<br />
Key words: Diabetes mellitus; Ginkgo biloba; Myenteric<br />
plexus; Submucous plexus; Neuroprotection<br />
Peer reviewer: Claudio Daniel Gonzalez, MD, Pr<strong>of</strong>essor <strong>of</strong><br />
Pharmacology, Department <strong>of</strong> Pharmacology, CEMIC University<br />
Hospital, Buenos Aires, Argentina<br />
da Silva GGP, Zanoni JN, Buttow NC. Neuroprotective action<br />
<strong>of</strong> Ginkgo biloba on the enteric nervous system <strong>of</strong> diabetic rats.<br />
<strong>World</strong> J Gastroenterol 2011; 17(7): 898-905 Available from:<br />
URL: http://www.wjgnet.com/1007-9327/full/v17/i7/898.htm<br />
DOI: http://dx.doi.org/10.3748/wjg.v17.i7.898<br />
INTRODUCTION<br />
ORIGINAL ARTICLE<br />
Diabetes mellitus (DM) is a group <strong>of</strong> metabolic diseases<br />
characterized by high levels <strong>of</strong> glucose due to the lack <strong>of</strong><br />
insulin and/or the inability <strong>of</strong> insulin to properly exercise<br />
its effects [1] . Long-term hyperglycemia induces morbid<br />
states in patients, resulting in macroangiopathy [2] complications,<br />
microangiopathy (retinopathy and nephropathy) [3]<br />
and neuropathies [4] .<br />
Neuropathy is the most common late complication<br />
in diabetic patients [5,6] . It compromises the sympathetic,<br />
parasympathetic and enteric nerves, causing a variety <strong>of</strong><br />
abnormalities such as ulcerations <strong>of</strong> the lower limbs, sud-<br />
898 February 21, 2011|Volume 17|Issue 7|
da Silva GGP et al . Neuroprotection in enteric neurons<br />
mucosa and submucosal tunica were removed from the<br />
myenteric plexus, while the external muscular layer was<br />
kept. The mucosa was removed from the submucosal<br />
plexus with the aid <strong>of</strong> a wooden spatula.<br />
Immunohistochemistry <strong>of</strong> the myenteric and<br />
submucosal plexuses<br />
The myenteric and submucous plexuses were stained by<br />
the anti-myosin-V immunohistochemical technique as<br />
described by Buttow et al [23] . The final concentration <strong>of</strong><br />
antibody was 0.89 mg/mL. The dilution used was 1:1000<br />
(v/v). The membranes were first immersed in a blocking<br />
solution <strong>of</strong> 0.1 mol/L PBS containing 2% bovine serum<br />
albumin (BSA) and 0.5% Triton X-100 and normal goat<br />
serum at a ratio <strong>of</strong> 1:50 (v/v) for 3 h. The material was incubated<br />
with primary antibody for 48 h at room temperature<br />
(RT); this was performed in a solution <strong>of</strong> 0.1 mol/L<br />
PBS containing 1% BSA and 0.1% Triton X-100 and<br />
normal goat serum in the proportion <strong>of</strong> 1:50 (v/v). After<br />
the incubation, the material was washed twice for 15 min<br />
with PBS solution 0.1 mol/L and Triton X-100 0.1% and<br />
then also washed twice in PBS 0.1 mol/L and Tween 20 at<br />
a concentration <strong>of</strong> 0.05% for 15 min. The whole-mounts<br />
were then incubated with anti-rabbit secondary antibody<br />
produced in goat, peroxidase-conjugated [ImmunoPure ®<br />
Goat Anti-Rabbit IgG, (Fc), Peroxidase Conjugated, brand<br />
Pierce] in a blocking solution containing 0.1 mol/LPBS, 1%<br />
BSA and 0.05% Tween 20 for 24 h at RT. Normal goat serum<br />
at 1:50 (v/v) was also added to this blocking solution.<br />
The material was washed 4 times for 15 min in a solution<br />
<strong>of</strong> 0.1 mol/L PBS containing 0.05% Tween 20. The membranes<br />
were developed with the use <strong>of</strong> a diaminobenzidine<br />
solution (Sigma, St. Louis, MO, USA) for approximately<br />
10 min at a concentration <strong>of</strong> 0.14 mg/mL. After developing,<br />
the material was mounted on histological slides<br />
with glycerol-gel (containing 50% glycerol, 0.07 g/mL<br />
gelatin in PBS, and 2 μL/mL phenol). The slides were<br />
then placed in refrigerator (4℃), in order to slowly dry the<br />
whole-mounts.<br />
Density analysis <strong>of</strong> myosin-V immunoreactive neurons<br />
Enteric neurons were counted on a BX 40 Olympus<br />
microscope under a 40 × lens. Forty microscopy fields,<br />
randomly selected, were counted for each preparation.<br />
The area <strong>of</strong> each field was 0.229 mm 2 . The results were<br />
expressed in number <strong>of</strong> neurons per cm 2 .<br />
Morphometric analysis <strong>of</strong> myosin-V immunoreactive<br />
neurons<br />
Images <strong>of</strong> the ganglia were taken and then measured with<br />
the aid <strong>of</strong> the image analysis s<strong>of</strong>tware Image Pro-Plus 3.0.1<br />
(Media Cybernetics, Silver Spring, MD, USA) to study the<br />
area <strong>of</strong> neurons in different groups. The area (μm 2 ) <strong>of</strong><br />
100 cell bodies per animal was measured, for a total <strong>of</strong><br />
500 neurons (5 animals per group). Neurons were classified<br />
into the class interval <strong>of</strong> 10 μm 2 , and the percentage<br />
<strong>of</strong> each group was calculated for each interval.<br />
WJG|www.wjgnet.com<br />
Table 1 Final weight and glycemia in groups: control, diabetic<br />
and EGb 76-treated diabetic (mean ± SE)<br />
Group Final weight (g) Blood glucose (mg/dL)<br />
C 445.6 ± 63.04 78.97 ± 5.12<br />
D 264.6 ± 22.88 253 ± 64.97<br />
DT 308 ± 19.27 322 ± 20.42<br />
n = 5/groups. C: Control; D: Diabetic; DT: EGb 76-treated diabetic.<br />
Statistical analysis<br />
To compare the parameters <strong>of</strong> the studied groups we<br />
used analysis <strong>of</strong> variance (ANOVA). When there was a<br />
significant difference we used Tukey’s test. For this study<br />
we used the Prism s<strong>of</strong>tware version 3.0. Results were considered<br />
significant when P < 0.05. The results were shown<br />
as mean ± SE, n indicating the number <strong>of</strong> samples in each<br />
group.<br />
RESULTS<br />
Streptozotocin caused diabetic syndrome onset in animal<br />
groups D and DT, as evidenced by the significant increase<br />
in blood glucose, as well as a significant reduction in body<br />
weight, when compared to group C (Table 1). Other typical<br />
symptoms <strong>of</strong> the disease (polyuria, polydipsia and<br />
polyphagia) were observed during the experimental period.<br />
Neuronal density<br />
There was a significant reduction (P < 0.05) in the neuronal<br />
density <strong>of</strong> myenteric neurons in the jejunum in group<br />
D when compared to C (Table 2). There was no significant<br />
difference in the DT group when compared to groups C<br />
and D. The neuronal density <strong>of</strong> submucosal neurons decreased<br />
significantly (P < 0.05) in group D when compared<br />
to C. No significant difference in the neuronal density was<br />
observed when group DT was compared to C (Table 2).<br />
The neuronal density <strong>of</strong> myenteric neurons in the ileum<br />
decreased significantly (P < 0.05) in group D when<br />
compared to C (Table 3). No significant difference was<br />
seen when comparing group DT to C. There was no<br />
significant reduction in the neuronal density in the ileum<br />
submucous plexus when the three groups were compared<br />
(Table 3).<br />
Areas <strong>of</strong> neuronal cell bodies<br />
The results obtained with the measurements <strong>of</strong> 500 neurons<br />
per studied group were distributed according to<br />
the relative frequency <strong>of</strong> areas <strong>of</strong> neuronal cell bodies<br />
at intervals <strong>of</strong> 10 μm 2 (Figures 1 and 2). The cell body<br />
area in the jejunum ranged between 81.33 and 538.9 μm 2<br />
for animals in group C; between 119.9 and 588.9 μm 2 in<br />
group D; and between 101.0 and 609.2 μm 2 in group DT.<br />
There were no significant differences in the mean areas <strong>of</strong><br />
the jejunum myenteric neurons when comparing groups<br />
C and D. However, there was a significant reduction in the<br />
mean area (P < 0.05) <strong>of</strong> the DT group when compared to<br />
the other two groups (Table 2). The cell body area in the<br />
900 February 21, 2011|Volume 17|Issue 7|
Table 2 Neuronal density and mean area <strong>of</strong> cell bodies <strong>of</strong> myenteric and submucosal neurons in the jejunum <strong>of</strong> rat<br />
groups: control, diabetic and EGb 761-treated diabetic (mean ± SE)<br />
Group Myenteric plexus Submucous plexus<br />
Neuronal density (cm 2 ) Mean area <strong>of</strong> cell body (μm 2 ) Neuronal density (cm 2 ) Mean area <strong>of</strong> cell body (μm 2 )<br />
C 15 884 ± 712.0 234.2 ± 88.10 12 602 ± 233.8 230.6 ± 62.89<br />
D 13 483 ± 617.9 245.6 ± 77.19 11 383 ± 159.6 235.4 ± 67.99<br />
DT 14 426 ± 301.2 218.2 ± 72.10 12 682 ± 353.4 216.2 ± 62.03<br />
n = 5/myenteric plexus group; n = 3/submucous plexus group. C: Control; D: Diabetic; DT: EGb 76-treated diabetic.<br />
Table 3 Neuronal density and mean area <strong>of</strong> cell bodies <strong>of</strong> myenteric and submucosal neurons in the ileum <strong>of</strong> rat<br />
groups: control, diabetic and EGb 761-treated diabetic (mean ± SE)<br />
Group Myenteric plexus Submucous plexus<br />
Neuronal density (cm²) Mean area <strong>of</strong> cell body (μm²) Neuronal density (cm²) Mean area <strong>of</strong> cell body (μm²)<br />
C 16 522 ± 625.5 232.7 ± 82.97 11 657 ± 403.9 210.0 ± 59.18<br />
D 14 568 ± 424.7 251.4 ± 98.23 11 275 ± 281.9 231.3 ± 74.37<br />
DT 16 884 ± 366.1 239.3 ± 81.19 11 943 ± 299.3 204.5 ± 57.36<br />
n = 5/myenteric plexus group; n = 3/submucous plexus group. C: Control; D: Diabetic; DT: EGb 76-treated diabetic.<br />
A<br />
% Mean <strong>of</strong> neurons<br />
B<br />
% Mean <strong>of</strong> neurons<br />
0.075<br />
0.050<br />
0.025<br />
0.000<br />
0.075<br />
0.050<br />
0.025<br />
0.000<br />
submucosal neurons in the jejunum ranged between 106.1<br />
and 474.4 μm 2 in group C, between 102.3 to 523.4 μm 2 in<br />
group D and between 91.73 to 401.1 μm 2 in group DT.<br />
There were no significant differences between the mean<br />
cell body areas in groups C and D (P > 0.05). However,<br />
there was a significant reduction (P < 0.05) in group DT<br />
when compared to groups C and D (Table 2).<br />
WJG|www.wjgnet.com<br />
C<br />
D<br />
DT<br />
0 150 300 450 600 750 900<br />
Neuronal cell bodies areas in μm 2<br />
C<br />
D<br />
DT<br />
0 150 300 450 600 750 900<br />
Neuronal cell bodies areas in μm 2<br />
Figure 1 Neuronal behavior: area <strong>of</strong> cell body <strong>of</strong> myenteric (A) and submucosal<br />
(B) neurons, myosin-V immunoreactive in the jejunum, <strong>of</strong> control<br />
(C), diabetic (D) and diabetic-treated with EGb 761 (DT).<br />
da Silva GGP et al . Neuroprotection in enteric neurons<br />
A<br />
% Mean <strong>of</strong> neurons<br />
B<br />
% Mean <strong>of</strong> neurons<br />
0.075<br />
0.050<br />
0.025<br />
0.000<br />
0.075<br />
0.050<br />
0.025<br />
0.000<br />
C<br />
D<br />
DT<br />
0 150 300 450 600 750 900<br />
Neuronal cell bodies areas in μm 2<br />
C<br />
D<br />
DT<br />
0 150 300 450 600 750 900<br />
Neuronal cell bodies areas in μm 2<br />
Figure 2 Neuronal behavior: area <strong>of</strong> cell body <strong>of</strong> myenteric (A) and submucosal<br />
(B) neurons, myosin-V immunoreactive in the ileum, <strong>of</strong> control<br />
(C), diabetic (D) and diabetic-treated with EGb 761 (DT).<br />
The cell body area <strong>of</strong> myenteric neurons in the ileum<br />
ranged between 97.70 and 725.7 μm 2 in group C, between<br />
101.5 and 595.5 μm 2 in group D, and between 96.32 and<br />
512.9 μm 2 in group DT. There was a significant increase<br />
(P < 0.05) in group D when compared to C. No significant<br />
difference was observed when comparing group DT<br />
to groups C or D (Table 3). As for the ileum submucous<br />
901 February 21, 2011|Volume 17|Issue 7|
A<br />
da Silva GGP et al . Neuroprotection in enteric neurons<br />
D<br />
plexus, the area ranged between 89.54 and 426.2 μm 2 ,<br />
between 99.52 and 534.0 μm 2 in group D, and between<br />
72.77 and 435.0 μm 2 in group DT. There was a significant<br />
increase in the mean cell body area in group D (P < 0.05)<br />
when compared to C. The DT group showed no significant<br />
difference in mean cell body area when compared to<br />
group C (Table 3). In the submucous plexus, reduction<br />
in neuronal pr<strong>of</strong>ile area was greater than in the myenteric<br />
plexus; the values in the submucous plexus just below<br />
those <strong>of</strong> the control group.<br />
The distribution <strong>of</strong> the relative frequency <strong>of</strong> areas<br />
<strong>of</strong> cell bodies in the jejunum showed a displacement<br />
curve to the right in the myenteric plexus; thus showing<br />
a higher relative frequency <strong>of</strong> neurons at about 160 μm 2<br />
in both plexuses (Figure 1). There was a similarity in the<br />
curves <strong>of</strong> groups C and DT in both plexuses in the ileum<br />
(Figure 2). Group D showed a displacement to the right<br />
in both plexuses.<br />
DISCUSSION<br />
Streptozotocin (STZ) is widely used in experimental animal<br />
models to induce DM. Its cellular action includes<br />
irreversible changes in genetic material causing lethal<br />
alterations in the metabolism <strong>of</strong> β cells [24] . There is a reduction<br />
in overall myenteric plexus neuron population in<br />
animal models with chronic STZ-diabetes [11,12,25,26] . There<br />
are no studies <strong>of</strong> changes caused by diabetes in the overall<br />
neuronal population <strong>of</strong> the submucous plexus. Our study<br />
showed that the 120-d treatment with purified Ginkgo biloba<br />
extract (EGb 761) has a neuroprotective effect on the<br />
ileum myenteric plexus and on the jejunum submucous<br />
plexus <strong>of</strong> STZ-diabetic rats.<br />
Characteristic diabetic symptoms (polydipsia, polyuria<br />
WJG|www.wjgnet.com<br />
B<br />
20 μm 20 μm<br />
20 μm<br />
20 μm<br />
E<br />
Figure 3 Myosin-V immunoreactive myenteric neurons in the jejunum (A-C) and myosin-V immunoreactive submucosal neurons in the jejunum (D-F).<br />
There is a significant reduction in the neuronal density in the myenteric (B) and submucous (E) plexus in group diabetic. The neuronal density in the submucous<br />
plexus (F) was preserved in group EGb 76-treated (DT) (F). There was a significant reduction in the neuronal cell body area in group DT <strong>of</strong> both plexuses (C and F).<br />
20 μm<br />
C<br />
F<br />
20 μm<br />
and polyphagia) were observed in animals <strong>of</strong> D and DT<br />
groups. These data support the experimental model <strong>of</strong><br />
streptozotocin-induced diabetes [27-29] . The immunohistochemical<br />
technique, anti-myosin-V (Figures 3 and 4), was<br />
used to assess the effect <strong>of</strong> Ginkgo biloba extract (EGb<br />
761) on the enteric neuronal population. The protein myosin-V<br />
is present in cell bodies and projections <strong>of</strong> enteric<br />
neurons [30] and is being used as a pan-neuronal marker.<br />
The reduction <strong>of</strong> the myenteric neuron density in the<br />
jejunum was 15.12% in group D when compared to C (P<br />
< 0.05). The submucosal neuron density was 9.61% lower<br />
in group D when compared to C (P < 0.05). A reduction<br />
<strong>of</strong> 11.83% in myenteric neuron density was observed in<br />
the ileum in group D when compared to C (P < 0.05).<br />
The submucosal neuron density in the ileum was similar<br />
among the three groups. Several authors report the reduction<br />
<strong>of</strong> myenteric neuron density in rats with STZdiabetes<br />
in different regions <strong>of</strong> the gastrointestinal tract,<br />
including the cecum [31] , ileum [11,26] , jejunum [25] and proximal<br />
colon [12] . There are no studies in the submucosal plexus<br />
<strong>of</strong> the total neuronal population in STZ-diabetes models.<br />
Pereira et al [26] reported a 24% reduction in the number<br />
<strong>of</strong> myosin-V myenteric neurons in the ileum (after<br />
120 d) <strong>of</strong> diabetic rats when compared to non-diabetic<br />
ones. De Freitas et al [25] observed a 37.9% neuronal loss <strong>of</strong><br />
myosin-V myenteric neurons in the jejunum <strong>of</strong> diabetic rats<br />
when compared to non-diabetic animals, also after 120 d.<br />
These studies used 90-d-old animals at the beginning <strong>of</strong><br />
the experiment and our study was carried out with 150-dold<br />
rats, which may have contributed to the neuronal loss<br />
variation due to age.<br />
The degenerative changes that affect the enteric nervous<br />
system seen in DM are due to metabolic disorders.<br />
High oxidative stress, resulting from the imbalance be-<br />
902 February 21, 2011|Volume 17|Issue 7|
A<br />
D<br />
tween ROS production and neutralization, is a well established<br />
mechanism <strong>of</strong> diabetic neuropathy pathogenesis<br />
and other complications [32,33] . The levels <strong>of</strong> endogenous<br />
and exogenous antioxidants are reduced in this condition.<br />
New studies have confirmed the destruction <strong>of</strong> endogenous<br />
antioxidants in peripheral nerves and the increased<br />
production <strong>of</strong> free radicals in the vasa nervorum [4] .<br />
Ginkgo biloba extract is widely used for its neuroprotective<br />
and antioxidant activity in several cardiovascular and<br />
neurologic disorders [34,35] . The Ginkgo biloba extract (EGb<br />
761) was given at a daily dose <strong>of</strong> 50 mg/kg body weight<br />
for 120 d in this experiment. This standardized extract<br />
contains 24% flavonoid glycosides (quercetin, kaempferol,<br />
isorhamnetin) and 6% terpene lactones (ginkgolides, bilobalides).<br />
The EGb 761 extract components eliminate<br />
free radicals such as the hydroxyl radical and the superoxide<br />
anion [36] . Quercetin is a powerful antioxidant within<br />
the flavonoid family due to its molecular configuration<br />
which is capable <strong>of</strong> eliminating free radicals [37] .<br />
The myenteric neuronal density in the jejunum in the<br />
DT group was 9.17% lower when compared to C, though<br />
this reduction is not significant. On the other hand, the<br />
submucosal neuronal density in DT had very similar values<br />
to those <strong>of</strong> group C. The treatment with EGb 671<br />
resulted in the preservation <strong>of</strong> the neuronal population<br />
in the ileum, represented by very similar values to those<br />
<strong>of</strong> the control group (Table 2), thus demonstrating a<br />
neuroprotective effect on this complex. The submucosal<br />
neuronal density in this segment was similar in all three<br />
groups. The Ginkgo biloba extract reduces the oxidative<br />
stress in diabetic rats by increasing the activity <strong>of</strong> antioxidant<br />
enzymes [38] . Wu et al [39] reported that this extract may<br />
be vital to postpone diabetic cataract, since their studies<br />
showed that, besides inhibiting aldose reductase activity,<br />
Ginkgo biloba also inhibits apoptosis induced by high glu-<br />
WJG|www.wjgnet.com<br />
B<br />
20 μm 20 μm<br />
20 μm<br />
20 μm<br />
E<br />
da Silva GGP et al . Neuroprotection in enteric neurons<br />
Figure 4 Myosin-V immunoreactive myenteric neurons in the ileum (A-C) and myosin-V immunoreactive submucosal neurons in the jejunum (D-F). There<br />
is a significant reduction in the neuronal density in the myenteric plexus (B), but the neuronal density was preserved in this plexus in group EGb 76-treated (DT) (C).<br />
There is a significant increase in the neuronal cell body area in group diabetic in the myenteric (B) and submucous (E) plexuses. There was a significant reduction in<br />
the neuronal cell body area in group DT in the submucous plexus (F).<br />
20 μm<br />
C<br />
F<br />
20 μm<br />
cose levels by reducing the Bax/Bcl2 ratio. This high ratio<br />
harms the mitochondria which release apoptosis-inducing<br />
proteins, such as the apoptosis-inducing factor, leading to<br />
the activation <strong>of</strong> caspase-3 via caspase 9. The myenteric<br />
plexus neuroprotection, seen only in the ileum, is similar<br />
to results in aging models [40] where 120-d treatment <strong>of</strong> rats<br />
with the same dose <strong>of</strong> Ginkgo biloba extract was more efficient<br />
in the ileum myenteric plexus than in the jejunum.<br />
Few studies have been carried out in the submucous<br />
plexus due to the difficulty <strong>of</strong> dissection. Some authors<br />
have reported changes in neuronal subpopulations through<br />
the neurotransmitter immunoreactivity. Belai et al [41] observed<br />
an increase in VIP and neuropeptide Y immunoreactivity<br />
when analyzing the submucous plexus in the<br />
ileum <strong>of</strong> STZ-diabetic rats aged 8 and 16 wk. They also<br />
observed a reduction in calcitonin gene-related peptide<br />
(CGRP) immunoreactivity. However, no change in substance<br />
P immunoreactivity or dopamine beta hydroxylase<br />
was seen. VIP-ergic neurons <strong>of</strong> diabetic rats show increased<br />
immunoreactivity in the jejunum [42] and ileum [43]<br />
submucous plexus.<br />
The mean cell body areas <strong>of</strong> myenteric neurons in the<br />
jejunum were similar in groups C and D. These results are<br />
similar to those observed by De Freitas et al [25] , who did<br />
not observe an increase in the mean area <strong>of</strong> the cell body<br />
<strong>of</strong> immunoreactive myosin-V neurons in the jejunum <strong>of</strong><br />
diabetic rats when compared to non-diabetic rats. The<br />
mean areas <strong>of</strong> cell bodies <strong>of</strong> submucosal neurons in the<br />
jejunum were similar in groups C and D. Studies on morphometric<br />
changes in the submucosal plexus caused by<br />
diabetic syndrome report an increase in the mean area <strong>of</strong><br />
the cell body <strong>of</strong> neuronal subpopulations. Defani et al [42]<br />
observed an increase in the mean area <strong>of</strong> the cell body <strong>of</strong><br />
submucous VIP-ergic neurons in the jejunum. The technique<br />
used to stain the total population showed no change<br />
903 February 21, 2011|Volume 17|Issue 7|
da Silva GGP et al . Neuroprotection in enteric neurons<br />
in the mean area <strong>of</strong> submucosal neurons in the jejunum.<br />
The mean area <strong>of</strong> the cell body <strong>of</strong> myenteric neurons in<br />
the ileum was 7.44% (P < 0.05) higher in group D than<br />
in group C in our study. This increase was also observed<br />
by Zanoni et al [11] and Pereira et al [26] in Wistar rats after a<br />
120-d experimental period. The mean area <strong>of</strong> the body<br />
cell <strong>of</strong> submucosal neurons in the ileum showed a statistically<br />
significant increase <strong>of</strong> 9.2% (P < 0.05) in group D<br />
when compared to C. Zanoni et al [43] reported an increase<br />
in the mean area <strong>of</strong> the body cell <strong>of</strong> submucous VIP-ergic<br />
neurons in the ileum.<br />
The increase in the neuronal cell body area in rats with<br />
chronic diabetes may be the result <strong>of</strong> neuronal edema [11] .<br />
The aldose reductase hyperactivity observed in diabetes<br />
is associated with increased levels <strong>of</strong> sorbitol [44] which increases<br />
the intracellular osmolarity, resulting in edema and<br />
neuronal lesions [43] .<br />
The EGb 761 treatment induced a reduction <strong>of</strong> 6.8%<br />
in the mean area <strong>of</strong> the cell body in the jejunum myenteric<br />
neurons in DT when compared to C (P < 0.05).<br />
The mean area <strong>of</strong> the cell body <strong>of</strong> submucosal neurons<br />
decreased 6.2% in group DT when compared to C (P <<br />
0.05). The mean area <strong>of</strong> the cell body <strong>of</strong> myenteric and<br />
submucosal neurons in the ileum in DT was reduced to<br />
values similar to group C. Schneider et al [40] observed that<br />
the EGb 761 treatment reduced the mean area <strong>of</strong> myenteric<br />
neuronal cell bodies in the jejunum and ileum <strong>of</strong><br />
aging rats. However, studies by Perez et al [45] in the large<br />
intestine treated with EGb 761 at a dose <strong>of</strong> 50 mg/kg <strong>of</strong><br />
body weight observed that the EGb 761 extract promotes<br />
an increase in the mean area <strong>of</strong> myenteric neurons in rats<br />
in the aging process. These results show that the response<br />
to the use <strong>of</strong> antioxidants such as the Gingko biloba extract<br />
may be different according to the segment evaluated.<br />
This study showed that treatment with Ginkgo biloba<br />
extract reduced the area <strong>of</strong> the cell body <strong>of</strong> myenteric and<br />
submucosal neurons in the jejunum and ileum <strong>of</strong> diabetictreated<br />
rats (group DT) when compared to non-treated diabetic<br />
rats (group D). However, the reduction in the mean<br />
area <strong>of</strong> the cell body <strong>of</strong> myenteric neurons in the ileum<br />
was not significant. The inhibitory action <strong>of</strong> Ginkgo biloba<br />
on aldose redutase [19] enzyme activity may be responsible<br />
for the reduction in the mean area <strong>of</strong> neuronal cell bodies<br />
observed in rats treated with EGb 761 (DT group).<br />
In conclusion, our results show that the 50 mg/kg <strong>of</strong><br />
body weight dose <strong>of</strong> standardized Ginkgo biloba extract<br />
(EGb761) has a neuroprotective effect on the ileum myenteric<br />
plexus and on the jejunum submucous plexus <strong>of</strong><br />
STZ-diabetic rats.<br />
ACKNOWLEDGMENTS<br />
The authors wish to thank Dr. Enilza Maria Espreafico<br />
(USP-Ribeirão Preto, Brazil) for her invaluable assistance<br />
and support in the production <strong>of</strong> the anti-myosin-V antibody,<br />
Maria Eurides do Carmo Cancino, Maria dos Anjos<br />
Fortunato, Valdir Trombeli and José Antônio de Souza<br />
(UEM, Brazil) for their excellent technical support, and<br />
WJG|www.wjgnet.com<br />
Ali Suleiman Mahmoud for translating the text. We gratefully<br />
acknowledge Altana Pharma for supplying the Ginkgo<br />
biloba extract (EGb 761).<br />
COMMENTS<br />
Background<br />
Gingko biloba extract possesses various biological activities and has been<br />
shown to be useful in diabetes treatment. Oxidative stress has been known to<br />
play an important role in the development and progression <strong>of</strong> diabetes mellitus<br />
(DM), and reactive oxygen species (ROS) production is a direct consequence <strong>of</strong><br />
hyperglycemia. Chronic hyperglycemia in diabetes is involved in direct neuronal<br />
damage caused by intracellular glucose which leads to altered neurotransmitter<br />
functions and reduced motor activity. Oxygen free radicals are also thought to<br />
play an important role in the diabetic and hypoxic condition <strong>of</strong> cells. Success <strong>of</strong><br />
Ginkgo biloba application is determined by its main active substances, flavonoids<br />
(flavone glycosides, primarily composed <strong>of</strong> quercetin) and terpenoids (ginkgolides<br />
and bilobalides). Ginkgo biloba can improve hemodynamics, scavenge ROS,<br />
suppress platelet-activating factor (PAF) and relax vascular smooth muscle.<br />
Research frontiers<br />
Gastrointestinal (GI) afflictions are not normally life threatening but do pr<strong>of</strong>oundly<br />
affect quality <strong>of</strong> life. Diabetic patients experience a wide range <strong>of</strong> GI discomforts including<br />
nausea, vomiting, heartburn, diarrhea, constipation, abdominal pain and fecal<br />
incontinence. The high morbidity, high socioeconomic costs and lack <strong>of</strong> specific<br />
treatments are key factors that define the relevance <strong>of</strong> DM for human health and<br />
the importance <strong>of</strong> research on neuronal protective agents. Some studies provide a<br />
strong case for the application <strong>of</strong> Ginkgo biloba in diabetic nephropathy therapy.<br />
Innovations and breakthroughs<br />
Ginkgo biloba has been ascertained to be protective against DM. However,<br />
there has been little in the literature reporting on the protective effects <strong>of</strong> Ginkgo<br />
biloba on the enteric nervous system <strong>of</strong> the small intestine <strong>of</strong> streptozotocininduced<br />
diabetic rats in vivo.<br />
Applications<br />
This study indicated that standardized extract <strong>of</strong> Ginkgo biloba (EGb 761) could<br />
improve antioxidant ability and protect the enteric nervous system <strong>of</strong> the small<br />
intestine <strong>of</strong> streptozotocin-induced diabetic rats in vivo. These biological activities<br />
have considerable potential in diabetes mellitus treatment.<br />
Peer review<br />
The authors investigated the effect <strong>of</strong> Ginkgo biloba extract on the enteric neurons<br />
on the small intestine <strong>of</strong> diabetic rats. They found purified Ginkgo biloba<br />
extract has a neuroprotective effect on the jejunum submucous plexus and the<br />
myenteric plexus <strong>of</strong> the ileum <strong>of</strong> diabetic rats. This is a well written paper.<br />
REFERENCES<br />
1 American Diabetes Association. Diagnosis and classification<br />
<strong>of</strong> diabetes mellitus. Diabetes Care 2008; 31 Suppl 1: S55-S60<br />
2 Bortolotto LA. [Modifications <strong>of</strong> structural and functional<br />
properties <strong>of</strong> large arteries in diabetes mellitus]. Arq Bras Endocrinol<br />
Metabol 2007; 51: 176-184<br />
3 Aguiar LG, Villela NR, Bouskela E. [Microcirculation in diabetes:<br />
implications for chronic complications and treatment<br />
<strong>of</strong> the disease]. Arq Bras Endocrinol Metabol 2007; 51: 204-211<br />
4 Obrosova IG. Diabetes and the peripheral nerve. Biochim Biophys<br />
Acta 2009; 1792: 931-940<br />
5 Rang HP, Dali MM, Ritter JM. O pâncreas endócrino e o<br />
controle da glicemia In: Farmacologia. 4th ed. Rio de Janeiro:<br />
Guanabara Koogan, 2000: 318-329<br />
6 Boucek P. Advanced Diabetic Neuropathy: A Point <strong>of</strong> no Return?<br />
Rev Diabet Stud 2006; 3: 143-150<br />
7 Vinik AI, Mehrabyan A. Diabetic neuropathies. Med Clin<br />
North Am 2004; 88: 947-999, xi<br />
8 Chandrasekharan B, Srinivasan S. Diabetes and the enteric<br />
nervous system. Neurogastroenterol Motil 2007; 19: 951-960<br />
9 Pasricha PJ, Pehlivanov ND, Gomez G, Vittal H, Lurken MS,<br />
Farrugia G. Changes in the gastric enteric nervous system<br />
and muscle: a case report on two patients with diabetic gas-<br />
904 February 21, 2011|Volume 17|Issue 7|
troparesis. BMC Gastroenterol 2008; 8: 21<br />
10 Belai A, Lincoln J, Milner P, Burnstock G. Progressive<br />
changes in adrenergic, serotonergic, and peptidergic nerves<br />
in proximal colon <strong>of</strong> streptozotocin-diabetic rats. Gastroenterology<br />
1988; 95: 1234-1241<br />
11 Zanoni JN, Buttow NC, Bazotte RB, Miranda Neto MH.<br />
Evaluation <strong>of</strong> the population <strong>of</strong> NADPH-diaphorase-stained<br />
and myosin-V myenteric neurons in the ileum <strong>of</strong> chronically<br />
streptozotocin-diabetic rats treated with ascorbic acid. Auton<br />
Neurosci 2003; 104: 32-38<br />
12 Tashima CM, Tronchini EA, Pereira RV, Bazotte RB, Zanoni<br />
JN. Diabetic rats supplemented with L-glutamine: a study <strong>of</strong><br />
immunoreactive myosin-V myenteric neurons and the proximal<br />
colonic mucosa. Dig Dis Sci 2007; 52: 1233-1241<br />
13 Figueroa-Romero C, Sadidi M, Feldman EL. Mechanisms <strong>of</strong><br />
disease: the oxidative stress theory <strong>of</strong> diabetic neuropathy.<br />
Rev Endocr Metab Disord 2008; 9: 301-314<br />
14 Ramakrishna V, Jailkhani R. Evaluation <strong>of</strong> oxidative stress in<br />
Insulin Dependent Diabetes Mellitus (IDDM) patients. Diagn<br />
Pathol 2007; 2: 22<br />
15 Bonnefont-Rousselot D. Glucose and reactive oxygen species.<br />
Curr Opin Clin Nutr Metab Care 2002; 5: 561-568<br />
16 Vincent AM, Russell JW, Low P, Feldman EL. Oxidative<br />
stress in the pathogenesis <strong>of</strong> diabetic neuropathy. Endocr Rev<br />
2004; 25: 612-628<br />
17 Shirpoor A, Ansari MH, Salami S, Pakdel FG, Rasmi Y. Effect<br />
<strong>of</strong> vitamin E on oxidative stress status in small intestine <strong>of</strong><br />
diabetic rat. <strong>World</strong> J Gastroenterol 2007; 13: 4340-4344<br />
18 Aksoy N, Vural H, Sabuncu T, Arslan O, Aksoy S. Beneficial<br />
effects <strong>of</strong> vitamins C and E against oxidative stress in diabetic<br />
rats. Nutr Res 2005; 25: 625-630<br />
19 Head KA. Natural therapies for ocular disorders, part two:<br />
cataracts and glaucoma. Altern Med Rev 2001; 6: 141-166<br />
20 Calapai G, Crupi A, Firenzuoli F, Marciano MC, Squadrito<br />
F, Inferrera G, Parisi A, Rizzo A, Crisafulli C, Fiore A, Caputi<br />
AP. Neuroprotective effects <strong>of</strong> Ginkgo biloba extract in brain<br />
ischemia are mediated by inhibition <strong>of</strong> nitric oxide synthesis.<br />
Life Sci 2000; 67: 2673-2683<br />
21 Maclennan KM, Darlington CL, Smith PF. The CNS effects <strong>of</strong><br />
Ginkgo biloba extracts and ginkgolide B. Prog Neurobiol 2002;<br />
67: 235-257<br />
22 Husstedt IW, Grotemeyer KH, Evers S, Staschewski F, Wertelewski<br />
R. Progression <strong>of</strong> distal symmetric polyneuropathy<br />
during diabetes mellitus: clinical, neurophysiological,<br />
haemorheological changes and self-rating scales <strong>of</strong> patients.<br />
Eur Neurol 1997; 37: 90-94<br />
23 Buttow NC, Santin M, Macedo LC, Neres Teixeira AC, Novakowski<br />
GC, Bolonheis Armelin TR, Assmann K. Study <strong>of</strong> the<br />
myenteric and submucous plexuses after BAC treatment in<br />
the intestine <strong>of</strong> rats. Biocell 2004; 28: 135-142<br />
24 Delfino VDA, Figueiredo JF, Matsuo T, Favero ME, Matni<br />
AM, Mocelin AJ. Streptozotocin-induced diabetes mellitus:<br />
long-term comparison <strong>of</strong> two drug administration routes. J<br />
Bras Nefrol 2002; 24: 31-36<br />
25 De Freitas P, Natali MR, Pereira RV, Miranda Neto MH, Zanoni<br />
JN. Myenteric neurons and intestinal mucosa <strong>of</strong> diabetic<br />
rats after ascorbic acid supplementation. <strong>World</strong> J Gastroenterol<br />
2008; 14: 6518-6524<br />
26 Pereira RV, de Miranda-Neto MH, da Silva Souza ID, Zanoni<br />
JN. Vitamin E supplementation in rats with experimental diabetes<br />
mellitus: analysis <strong>of</strong> myosin-V and nNOS immunoreactive<br />
myenteric neurons from terminal ileum. J Mol Histol 2008;<br />
39: 595-603<br />
27 Romano EB, Miranda-Neto MH, Cardoso RCS. Preliminary<br />
investigation about the effects <strong>of</strong> streptozotocin-induced<br />
WJG|www.wjgnet.com<br />
da Silva GGP et al . Neuroprotection in enteric neurons<br />
chronic diabetes on the nerve cell number and size <strong>of</strong> myenteric<br />
ganglia in rat colon. Rev Chil Anat 1996; 14: 139-145<br />
28 Büttow NC, Miranda Neto MH, Bazotte RB. Morphological<br />
and quantitative study <strong>of</strong> the myenteric plexus <strong>of</strong> the duodenum<br />
<strong>of</strong> streptozotocin-induced diabetic rats. Arq Gastroenterol<br />
1997; 34: 34-42<br />
29 Hernandes L, Bazotte RB, Gama P, Miranda-Neto MH.<br />
Streptozotocin-induced diabetes duration is important to<br />
determine changes in the number and basophily <strong>of</strong> myenteric<br />
neurons. Arq Neuropsiquiatr 2000; 58: 1035-1039<br />
30 Drengk AC, Kajiwara JK, Garcia SB, Carmo VS, Larson RE,<br />
Zucoloto S, Espreafico EM. Immunolocalisation <strong>of</strong> myosin-V<br />
in the enteric nervous system <strong>of</strong> the rat. J Auton Nerv Syst<br />
2000; 78: 109-112<br />
31 Zanoni JN, de Miranda Neto MH, Bazotte RB, de Souza RR.<br />
Morphological and quantitative analysis <strong>of</strong> the neurons <strong>of</strong><br />
the myenteric plexus <strong>of</strong> the cecum <strong>of</strong> streptozotocin-induced<br />
diabetic rats. Arq Neuropsiquiatr 1997; 55: 696-702<br />
32 Van Dam PS, Van Asbeck BS, Erkelens DW, Marx JJ, Gispen<br />
WH, Bravenboer B. The role <strong>of</strong> oxidative stress in neuropathy<br />
and other diabetic complications. Diabetes Metab Rev 1995; 11:<br />
181-192<br />
33 Figueroa-Romero C, Sadidi M, Feldman EL. Mechanisms <strong>of</strong><br />
disease: the oxidative stress theory <strong>of</strong> diabetic neuropathy.<br />
Rev Endocr Metab Disord 2008; 9: 301-314<br />
34 Diamond BJ, Shiflett SC, Feiwel N, Matheis RJ, Noskin O,<br />
Richards JA, Schoenberger NE. Ginkgo biloba extract: mechanisms<br />
and clinical indications. Arch Phys Med Rehabil 2000; 81:<br />
668-678<br />
35 Defeudis FV. Bilobalide and neuroprotection. Pharmacol Res<br />
2002; 46: 565-568<br />
36 Ni Y, Zhao B, Hou J, Xin W. Preventive effect <strong>of</strong> Ginkgo<br />
biloba extract on apoptosis in rat cerebellar neuronal cells induced<br />
by hydroxyl radicals. Neurosci Lett 1996; 214: 115-118<br />
37 Boots AW, Haenen GR, Bast A. Health effects <strong>of</strong> quercetin:<br />
from antioxidant to nutraceutical. Eur J Pharmacol 2008; 585:<br />
325-337<br />
38 Lu Q, Yin XX, Wang JY, Gao YY, Pan YM. Effects <strong>of</strong> Ginkgo<br />
biloba on prevention <strong>of</strong> development <strong>of</strong> experimental diabetic<br />
nephropathy in rats. Acta Pharmacol Sin 2007; 28: 818-828<br />
39 Wu ZM, Yin XX, Ji L, Gao YY, Pan YM, Lu Q, Wang JY.<br />
Ginkgo biloba extract prevents against apoptosis induced by<br />
high glucose in human lens epithelial cells. Acta Pharmacol Sin<br />
2008; 29: 1042-1050<br />
40 Schneider LC, Perez GG, Banzi SR, Zanoni JN, Natali MR,<br />
Buttow NC. Evaluation <strong>of</strong> the effect <strong>of</strong> Ginkgo biloba extract<br />
(EGb 761) on the myenteric plexus <strong>of</strong> the small intestine <strong>of</strong><br />
Wistar rats. J Gastroenterol 2007; 42: 624-630<br />
41 Belai A, Burnstock G. Changes in adrenergic and peptidergic<br />
nerves in the submucous plexus <strong>of</strong> streptozocin-diabetic rat<br />
ileum. Gastroenterology 1990; 98: 1427-1436<br />
42 Defani MA, Zanoni JN, Natali MR, Bazotte RB, de Miranda-<br />
Neto MH. Effect <strong>of</strong> acetyl-L-carnitine on VIP-ergic neurons in<br />
the jejunum submucous plexus <strong>of</strong> diabetic rats. Arq Neuropsiquiatr<br />
2003; 61: 962-967<br />
43 Zanoni JN, Hernandes L, Bazotte RB, Miranda Neto MH.<br />
Terminal ileum submucous plexus: Study <strong>of</strong> the VIP-ergic<br />
neurons <strong>of</strong> diabetic rats treated with ascorbic acid. Arq Neuropsiquiatr<br />
2002; 60: 32-37<br />
44 Obrosova IG. Increased sorbitol pathway activity generates<br />
oxidative stress in tissue sites for diabetic complications. Antioxid<br />
Redox Signal 2005; 7: 1543-1552<br />
45 Perez GG, Schneider LC, Buttow NC. Ginkgo biloba (EGb<br />
761) extract: effects on the myenteric plexus <strong>of</strong> the large intestine<br />
in Wistar rats. Dig Dis Sci 2009; 54: 232-237<br />
S- Editor Tian L L- Editor Logan S E- Editor Zheng XM<br />
905 February 21, 2011|Volume 17|Issue 7|
Online Submissions: http://www.wjgnet.com/1007-9327<strong>of</strong>fice<br />
wjg@wjgnet.com<br />
doi:10.3748/wjg.v17.i7.906<br />
ORIGINAL ARTICLE<br />
Outcome <strong>of</strong> non surgical hepatic decompression procedures<br />
in Egyptian patients with Budd-Chiari<br />
Ahmed Eldorry, Eman Barakat, Heba Abdella, Sara Abdelhakam, Mohamed Shaker, Amr Hamed,<br />
Mohammad Sakr<br />
Ahmed Eldorry, Mohamed Shaker, Department <strong>of</strong> Radiodiagnosis<br />
and Interventional Radiology, Faculty <strong>of</strong> Medicine, Ain<br />
Shams University, Cairo 11341, Egypt<br />
Eman Barakat, Heba Abdella, Sara Abdelhakam, Amr<br />
Hamed, Mohammad Sakr, Department <strong>of</strong> Tropical Medicine,<br />
Faculty <strong>of</strong> Medicine, Ain Shams University, Cairo 11341, Egypt<br />
Author contributions: Eldorry A and Sakr M contributed<br />
equally to this work; Sakr M, Eldorry A, Barakat E, Abdella<br />
H, Abdelhakam S and Hamed A designed the research; Abdelhakam<br />
S, Hamed A and Shaker M performed the research;<br />
Eldorry A, Sakr M, Barakat E, Abdella H, Abdelhakam S and<br />
Shaker M contributed analytic tools; Sakr M, Eldorry A, Barakat<br />
E, Abdella H, Abdelhakam S and Hamed A analyzed the<br />
data; Barakat E, Abdella H and Abdelhakam S wrote the paper.<br />
Correspondence to: Sara Abdelhakam, MD, Department <strong>of</strong><br />
Tropical Medicine, Faculty <strong>of</strong> Medicine, Ain Shams University,<br />
Cairo 11341, Egypt. saratropical@yahoo.com<br />
Telephone: +20-101601548 Fax: +20-2-22598751<br />
Received: August 4, 2010 Revised: September 29, 2010<br />
Accepted: October 6, 2010<br />
Published online: February 21, 2011<br />
Abstract<br />
AIM: To evaluate outcome <strong>of</strong> patients with Budd-<br />
Chiari syndrome after balloon angioplasty ± stenting<br />
or transjugular intrahepatic portosystemic shunt (TIPS).<br />
METHODS: Twenty five patients with Budd-Chiari<br />
syndrome admitted to Ain Shams University Hospitals,<br />
Tropical Medicine Department were included. Twelve<br />
patients (48%) with short segment occlusion were<br />
candidates for angioplasty; with stenting in ten cases<br />
and without stenting in two. Thirteen patients (52%)<br />
had Transjugular Intrahepatic Portosystemic Shunt. Patients<br />
were followed up for 12-32 mo.<br />
RESULTS: Patency rate in patients who underwent<br />
angioplasty ± stenting was 83.3% at one year and at<br />
end <strong>of</strong> follow up. The need <strong>of</strong> revision was 41.6% with<br />
one year survival <strong>of</strong> 100%, dropped to 91.6% at end<br />
WJG|www.wjgnet.com<br />
906<br />
<strong>World</strong> J Gastroenterol 2011 February 21; 17(7): 906-913<br />
ISSN 1007-9327 (print) ISSN 2219-2840 (online)<br />
© 2011 Baishideng. All rights reserved.<br />
<strong>of</strong> follow up. In patients who had Transjugular Intrahepatic<br />
Portosystemic Shunt, patency rate was 92.3% at<br />
one year, dropped to 84.6% at end <strong>of</strong> follow up. The<br />
need <strong>of</strong> revision was 38.4% with one year and end <strong>of</strong><br />
follow up survival <strong>of</strong> 100%. Patients with patent shunts<br />
showed marked improvement compared to those with<br />
occluded shunts.<br />
CONCLUSION: Morbidity and mortality following angioplasty<br />
± stenting and TIPS are low with satisfactory<br />
outcome. Proper patient selection and management <strong>of</strong><br />
shunt dysfunction are crucial in improvement.<br />
© 2011 Baishideng. All rights reserved.<br />
Key words: Angioplasty; Stenting; Transjugular Intrahepatic<br />
portosystemic shunt; Patency rate<br />
Peer reviewer: Bijan Eghtesad, Dr, Associate Pr<strong>of</strong>essor, Department<br />
<strong>of</strong> General Surgery, Cleveland Clinic Foundation,<br />
9500 Euclid Avenue, Cleveland, OH 44195, United States<br />
Eldorry A, Barakat E, Abdella H, Abdelhakam S, Shaker M,<br />
Hamed A, Sakr M. Outcome <strong>of</strong> non surgical hepatic decompression<br />
procedures in Egyptian patients with Budd-Chiari. <strong>World</strong><br />
J Gastroenterol 2011; 17(7): 906-913 Available from: URL:<br />
http://www.wjgnet.com/1007-9327/full/v17/i7/906.htm DOI:<br />
http://dx.doi.org/10.3748/wjg.v17.i7.906<br />
INTRODUCTION<br />
Budd-Chiari syndrome (BCS) results from hepatic venous<br />
outflow obstruction at any level, from hepatic<br />
venules to the right atrium [1] . If obstruction is due to endoluminal<br />
venous lesion like thrombosis, primary BCS is<br />
considered. In secondary BCS, the cause originates from<br />
neighboring structures like extrinsic compression or tumor<br />
invasion [2] .<br />
Imaging studies combined with clinical information<br />
February 21, 2011|Volume 17|Issue 7|
Table 2 Details <strong>of</strong> patients who needed revisions and their follow up (n = 10)<br />
Patient Intervention Time <strong>of</strong> dysfunction Action taken No <strong>of</strong> revisions 1 yr patency End <strong>of</strong> FUP patency<br />
23 yr F Angioplasty without<br />
stenting<br />
Table 3 Patient survival n (%)<br />
Figure 1 shows frequency <strong>of</strong> all complications in total<br />
procedures done [Twenty six angioplasty ± stenting procedures<br />
(12 as primary intervention and 14 as a trial for<br />
maintenance <strong>of</strong> previously occluded angioplasty or TIPS)<br />
and 16 TIPS procedures (13 as primary intervention and<br />
3 in patients with occluded stents following angioplasty in<br />
whom redilatation was not possible)].<br />
In total procedures done (whether primary or revision<br />
procedures), the frequency <strong>of</strong> angioplasty dysfunction<br />
was 53.85% (14 out <strong>of</strong> 26 procedures) and the<br />
frequency <strong>of</strong> TIPS dysfunction was 43.75% (7 out <strong>of</strong> 16<br />
procedures).<br />
Statistical analysis<br />
The mean duration <strong>of</strong> follow up was 20.04 ± 7.817 mo<br />
(ranging from 12-32 mo). One year survival rate was<br />
100% for all patients and at the end <strong>of</strong> follow up survival<br />
rate was 96% due to death <strong>of</strong> one patient at the 17th<br />
mo <strong>of</strong> follow up as shown in Table 3.<br />
Figure 2A shows patency rate in patients who underwent<br />
angioplasty ± stenting procedures; it was 11/12<br />
(91.7%) at 9 mo (due to persistent shunt occlusion in one<br />
WJG|www.wjgnet.com<br />
Day 7 and Day 10 TIPS was done, occluded at<br />
day 10; then re-angioplasty was<br />
done 1<br />
2 Patent Patent at 20th mo<br />
27 yr M Angioplasty and stenting Day 7 and 2nd yr Angioplasty was done-then<br />
angioplasty + thrombectomy<br />
2 Patent Patent at 24th mo<br />
28 yr F Angioplasty and stenting 4th mo Angioplasty + local<br />
thrombolytic therapy<br />
1 Patent Patent at 12th mo<br />
30 yr F Angioplasty and stenting 1st, 4th, 6th and 9th mo TIPS was done-then angioplasty<br />
(3 times)<br />
4 Occluded at 9th mo Occluded at 24th mo<br />
28 yr M Angioplasty and stenting 3rd mo and 14th mo Angioplasty + stent was donethen<br />
mesoatrial shunt<br />
1 Occluded at 1 yr Dead 2 at 17th mo<br />
27 yr F TIPS Day 1 (stent occlusion and migration<br />
to portal vein) - Re (TIPS)<br />
1 Patent Patent at 20th m<br />
33 yr F TIPS Day 3 Angioplasty + thrombectomy +<br />
systemic thrombolytic therapy<br />
1 Patent Patent at 32nd mo<br />
37 yr F TIPS Day 7 and 1st mo Angioplasty (2 times) 2 Patent Patent at 12th mo<br />
27 yr M TIPS Day 7, 3rd and 8th mo Angioplasty (3 times) 3 Patent Occluded at 20th mo<br />
17 yr M TIPS 1st mo Patient refused intervention 0 Occluded Occluded at 12th mo<br />
1 Patient had angioplasty dysfunction at Day 7, so transjugular intrahepatic portosystemic shunt (TIPS) was done but was occluded at Day 10, so angioplasty<br />
<strong>of</strong> TIPS stent was done; 2 Cause <strong>of</strong> death: Intraperitoneal bleeding. Follow up period: Minimum (12 mo), Maximum (32 mo). F: Female; M: Male; yr: Years<br />
old; FUP: Follow up.<br />
Angioplasty TIPS Total<br />
One year<br />
Alive 12 (100) 13 (100) 25 (100)<br />
Dead 0 (0) 0 (0) 0 (0)<br />
End <strong>of</strong> follow up<br />
Alive 11 (91.6) 13 (100) 24 (96)<br />
Dead 1 (8.4) 0 (0) 1 (4)<br />
Because <strong>of</strong> death <strong>of</strong> one patient only out <strong>of</strong> 25; Kaplan–Meier curve couldn’t<br />
be drawn for patient survival. TIPS: Transjugular intrahepatic portosystemic<br />
shunt.<br />
Eldorry A et al . Non surgical hepatic decompression in Budd-Chiari<br />
%<br />
60<br />
50<br />
40<br />
30<br />
20<br />
10<br />
0<br />
11.53%<br />
Angioplasty<br />
TIPS<br />
18.75%<br />
0%<br />
12.50% 11.53%<br />
25%<br />
3.84% 6.25%<br />
53.85%<br />
Sepsis Transient HE Bleeding Stent Shunt<br />
43.75%<br />
migration dysfunction<br />
Figure 1 Procedure complications. Transient hepatic encephalopathy (HE):<br />
HE lasting 2-3 d after procedure with rapid response to treatment. Bleeding was<br />
either intra-peritoneal or hemobilia. TIPS: Transjugular intrahepatic portosystemic<br />
shunt.<br />
patient). Patency rate dropped to 10/12 (83.3%) at one<br />
year and continued till the end <strong>of</strong> follow up at 32 mo. (There<br />
was persistent shunt occlusion in 2 patients in spite <strong>of</strong> repeated<br />
revisions and optimal anticoagulation therapy).<br />
Figure 2B shows patency rate in patients who had TIPS<br />
procedures; it was 12/13 (92.3%) at one year (due to persistent<br />
shunt occlusion in one patient despite repeated revisions).<br />
Patency rate dropped to 11/13 (84.6%) at 20 mo<br />
and this continued till the end <strong>of</strong> follow up at 32 mo (due<br />
to persistent shunt occlusion in another patient).<br />
At one year <strong>of</strong> follow up, only three patients <strong>of</strong><br />
25 (12%) had occluded shunts. Patients with occluded<br />
shunts showed no improvement regarding their clinical<br />
manifestations, laboratory pr<strong>of</strong>ile and performance<br />
status. On the contrary, patients with patent shunts (22<br />
<strong>of</strong> 25; 88%) showed marked improvement as shown in<br />
Tables 4 and 5.<br />
909 February 21, 2011|Volume 17|Issue 7|
A 1.0<br />
Survival function Survival function<br />
0<br />
B 1.0<br />
Cum survival<br />
Eldorry A et al . Non surgical hepatic decompression in Budd-Chiari<br />
0.8<br />
0.6<br />
0.4<br />
0.2<br />
0.0<br />
DISCUSSION<br />
0 10 20 30 40<br />
Occlusion time or end <strong>of</strong> followup<br />
This is the first study that addresses the short term outcome<br />
<strong>of</strong> interventional radiology procedures in management<br />
<strong>of</strong> Egyptian patients with BCS. In this study, 12<br />
patients (48%) had short segment occlusion that enabled<br />
us to perform angioplasty with stenting in ten cases and<br />
without stenting in two cases. Thirteen patients (52%)<br />
were not suited for angioplasty and had TIPS.<br />
According to Xu et al [13] , short-term results <strong>of</strong> balloon<br />
angioplasty alone without stenting were excellent but the<br />
sustained patency rate was only 50% at two years after the<br />
procedure. In this study, one <strong>of</strong> the cases that had angioplasty<br />
alone was still having patent shunt at 24 mo after<br />
the procedure without any need for shunt revision; the<br />
other one had occluded shunt on the seventh day that necessitated<br />
re-intervention in the form <strong>of</strong> TIPS which was<br />
still patent at 20 mo after procedure.<br />
Patency rate in patients who underwent angioplasty ±<br />
stenting procedures was 10/12 (83.3%) at one year and<br />
at the end <strong>of</strong> follow up due to persistent shunt occlusion<br />
in 2 patients in spite <strong>of</strong> repeated revisions and optimal<br />
WJG|www.wjgnet.com<br />
Cum survival<br />
0.8<br />
0.6<br />
0.4<br />
0.2<br />
0.0<br />
Survival function Survival function<br />
0 10 20 30 40<br />
Occlusion time or end <strong>of</strong> followup<br />
Censored<br />
Figure 2 Patency rate in patients who underwent angioplasty ± stenting (A) and transjugular intrahepatic portosystemic shunt (B). A: Type <strong>of</strong> intervention: angioplasty<br />
± stenting <strong>of</strong> hepatic veins, it was 91.7% at 9 mo and dropped to 83.3% at one year till the end <strong>of</strong> follow up at 32 mo; B: Type <strong>of</strong> intervention: transjugular intrahepatic<br />
portosystemic shunt, it was 92.3% at one year and dropped to 84.6% at 20 mo till the end <strong>of</strong> follow up at 32 mo.<br />
Table 4 Clinical data <strong>of</strong> patients before and after intervention<br />
Before intervention One year after intervention P value Sig<br />
+VE -VE +VE -VE<br />
Patients with occluded shunts (n = 3)<br />
Abdominal pain 3 0 2 1 > 0.05 NS<br />
Jaundice 1 2 0 3 > 0.05 NS<br />
Lower limb edema 2 1 1 2 > 0.05 NS<br />
Dilated veins 1 2 0 3 > 0.05 NS<br />
Ascites 3 0 3 0 > 0.05 NS<br />
Patients with patent shunts (n = 22)<br />
Abdominal pain 20 2 1 21 < 0.001 VHS<br />
Jaundice 8 14 0 22 < 0.01 HS<br />
Lower limb edema 8 14 1 21 < 0.05 S<br />
Dilated veins 4 18 0 22 > 0.05 NS<br />
Ascites 21 1 1 21 < 0.001 VHS<br />
Sig: Significance; NS: Non significant; S: Significant; HS: Highly significant; VHS: Very highly significant; -VE: Negative; +VE: Positive.<br />
anticoagulation therapy. This is a more or less satisfactory<br />
outcome; however it might have been influenced by<br />
the relatively short follow up period (ranging from 12 to<br />
32 mo) as well as most <strong>of</strong> the patients having good or<br />
intermediate prognosis according to Rotterdam score.<br />
The need <strong>of</strong> revision in cases with angioplasty ± stenting<br />
was 41.6% (5 out <strong>of</strong> 12 cases). One year survival was<br />
100% and at the end <strong>of</strong> follow up, survival dropped to<br />
91.6% due to death <strong>of</strong> one patient who had occluded<br />
shunt after one year and was also referred for mesoatrial<br />
shunt due to occlusion <strong>of</strong> IVC.<br />
Although angioplasty is considered a simple procedure;<br />
some complications were reported in the current study.<br />
Twenty six angioplasty ± stenting procedures have been<br />
done (12 procedures as primary intervention and 14 procedures<br />
as a trial for maintenance <strong>of</strong> previously occluded<br />
angioplasty or TIPS); <strong>of</strong> these procedures, angioplasty dysfunction<br />
was reported in 53.85%. This is consistent with<br />
Senzolo et al [14] who stated that although long-term patency<br />
rates can reach 80%-90% in angioplasty ± stenting procedures;<br />
angioplasty may later be required in 50% <strong>of</strong> these<br />
cases to overcome angioplasty dysfunction.<br />
910 February 21, 2011|Volume 17|Issue 7|
Table 5 Lab data and performance status <strong>of</strong> patients before and after intervention<br />
Stent migration, which is very rare, occurred in one<br />
angioplasty procedure (3.84%) where stent migrated to<br />
the heart just after insertion. However, no serious complications<br />
occurred and stent was embedded in the wall<br />
<strong>of</strong> right atrium and the patient was quite well.<br />
Post procedure (angioplasty ± stenting) bleeding was<br />
encountered in 3 procedures (11.53%), 2 <strong>of</strong> which were<br />
intraperitoneal and one <strong>of</strong> which was hemobilia. All 3 cases<br />
were managed conservatively by temporary stoppage<br />
<strong>of</strong> anticoagulation and blood transfusion when indicated.<br />
This complication could be attributed to the application<br />
<strong>of</strong> a transhepatic approach in these procedures. Beckett<br />
and Olliff [5] stated that this approach has the merit <strong>of</strong><br />
simplicity over a transjugular or transfemoral approach, as<br />
well as feasibility with major superior vena caval obstruction<br />
but with a potentially greater risk <strong>of</strong> bleeding.<br />
Post procedure sepsis occurred in 3 procedures (11.53%)<br />
in spite <strong>of</strong> antibiotic prophylaxis with cefotaxime in combination<br />
with ampicillin-sulbactam. This could be due to infection<br />
from resistant organisms. According to McDermott<br />
et al [15] , pathogens that precipitated infection after angio-<br />
WJG|www.wjgnet.com<br />
Before intervention One year after intervention P value Sig<br />
mean SD mean SD<br />
Patients with occluded shunts (n = 3)<br />
ALT (N = 7-40 IU/L) 70.33 75.070 29.66 24.66 > 0.05 NS<br />
AST (N = 7-37 IU/L) 42 24.240 42.33 32.51 > 0.05 NS<br />
Total bilirubin (N = 0.2-1.2 mg/dL) 2.9 2.940 1.26 0.832 > 0.05 NS<br />
Direct bilirubin (N = 0-0.3 mg/dL) 1.53 1.560 0.53 0.577 > 0.05 NS<br />
Albumin (N = 3.5-5.3 g/dL) 3.7 0.800 3.56 0.901 > 0.05 NS<br />
Performance status 3.33 0.577 2.00 1.730 > 0.05 NS<br />
Patients with patent shunts (n = 22)<br />
ALT (N = 7-40 IU/L) 66.95 117.265 26.45 8.528 < 0.05 S<br />
AST (N = 7-37 IU/L) 53.95 33.832 32.22 9.586 < 0.01 HS<br />
Total bilirubin (N = 0.2-1.2 mg/dL) 2.818 3.198 1.21 0.414 < 0.01 HS<br />
Direct bilirubin (N = 0-0.3 mg/dL) 1.29 2.022 0.51 0.296 < 0.01 HS<br />
Albumin (N = 3.5-5.3 g/dL) 3.5 0.475 3.93 0.576 < 0.01 HS<br />
Performance status 2.59 1.007 0.18 0.664 < 0.001 VHS<br />
N: Normal range; ALT: Alanine aminotransferase; AST: Aspartate aminotransferase; Sig: Significance; NS: Non significant; S: Significant; HS: Highly significant;<br />
VHS: Very highly significant.<br />
Table 6 Comparison <strong>of</strong> different transjugular intrahepatic portosystemic shunt studies in Budd-Chiari syndrome with the current study<br />
Points <strong>of</strong> comparison Mancuso et al [18]<br />
Perelló et al [19]<br />
Rössle et al [20]<br />
Hernández-Guerra et al [21] Current study<br />
No. <strong>of</strong> patients 15 13 35 25 (9 covered stents) 13<br />
Mean age in years (range) 40 (20-73) 36 (17-67) 43 (12-74) 40 (17-54) 29 (14-57)<br />
Median child score 11 9 9 9 8<br />
Acute, fulminant/chronic presentation 8/6 4/6 11/13 ND 2/11<br />
Mean follow-up (mo) 24 48 37 20 18<br />
Stent stenosis (%) 36 72 47 67 (19% covered stents) 38.4<br />
Anticoagulation (%) 100 95 100 ND 100<br />
Patients with acute presentation who died 4 ND 2 ND 0<br />
Patients with chronic presentation who died 0 ND 1 ND 0<br />
Death total (%) 30 10 9 0 0<br />
Liver transplantation 0 1 2 0 0<br />
Surgical portocaval shunt 0 2 0 0 0<br />
ND: Not determined; Anticoagulation: Percent <strong>of</strong> patients who were adherent to anticoagulation therapy.<br />
Eldorry A et al . Non surgical hepatic decompression in Budd-Chiari<br />
plasty and stent were Staphylococcus aureus and S. epidermidis,<br />
which were sensitive to cefazolin.<br />
In this study, the results <strong>of</strong> angioplasty ± stenting<br />
agreed with Fisher et al [16] who stated that, with appropriate<br />
case selection, many patients with BCS caused by short<br />
length HV stenosis or occlusion may be managed successfully<br />
by angioplasty ± stenting with a good outcome<br />
following the procedure, provided that anticoagulation is<br />
maintained. According to the authors’ comparative study<br />
between percutaneous angioplasty and operative shunt<br />
surgery; both groups had the same re-occlusion rate and<br />
both were related to suboptimal dose <strong>of</strong> anticoagulation.<br />
In the current study, 13 patients (52%) were not candidates<br />
for angioplasty and underwent TIPS. The need<br />
for revision was 38.4% (compared to 41.6% in angioplasty<br />
± stenting). One year and end <strong>of</strong> follow up survival<br />
rates following TIPS were 100%. This could be attributed<br />
to the relatively short follow up duration (ranging<br />
from 12 to 32 mo) and good selection <strong>of</strong> cases, as most<br />
<strong>of</strong> our patients had good or intermediate predictable<br />
prognosis according to Rotterdam score.<br />
911 February 21, 2011|Volume 17|Issue 7|
Eldorry A et al . Non surgical hepatic decompression in Budd-Chiari<br />
Patency rate in patients who had TIPS procedures was<br />
12/13 (92.3%) at one year due to persistent shunt occlusion<br />
in one patient despite repeated revisions. At the end<br />
<strong>of</strong> follow up; patency rate dropped to 11/13 (84.6%) due<br />
to persistent shunt occlusion in another patient.<br />
The results <strong>of</strong> the current study are much better than<br />
what had been reported by Valla [17] , namely that secondary<br />
thrombosis or shunt dysfunction requiring revision<br />
occurs in about 70% <strong>of</strong> cases by 6 mo. However, the results<br />
<strong>of</strong> this study are more or less comparable to those<br />
reported by Senzolo et al [14] who stated that 36%-72% <strong>of</strong><br />
patients needed reintervention after TIPS. The authors<br />
also reported a long-term patency rate <strong>of</strong> about 50% despite<br />
<strong>of</strong> routine anticoagulation therapy.<br />
Comparison between the results <strong>of</strong> the current study,<br />
regarding TIPS, with other studies is shown in Table 6.<br />
Sixteen TIPS procedures have been done throughout<br />
the current study (13 as primary intervention and 3 in<br />
patients with occluded stents following angioplasty in<br />
which predilatation was not possible).<br />
Post TIPS sepsis occurred in 3 procedures (18.75%),<br />
in spite <strong>of</strong> prophylactic antibiotics. According to Dravid<br />
et al [22] ; an infection rate <strong>of</strong> 13% following TIPS was reported.<br />
According to Ryan et al [11] , acute infection related to<br />
TIPS placement appears to be uncommon. Whether or<br />
not prophylactic antibiotics are <strong>of</strong> value remains undetermined.<br />
Options for prophylactic antibiotics for TIPS<br />
are: (1) no prophylaxis; (2) 1 g ceftriaxone single dose intravenously<br />
before procedure; and (3) 1.5-3 g ampicillin/<br />
sulbactam single dose intravenously before procedure.<br />
We adopted the third strategy successfully in combination<br />
with cefotaxime 1 gm IV and completed the course<br />
<strong>of</strong> antibiotics for five days after intervention.<br />
Hepatic encephalopathy after TIPS occurred in 2 patients<br />
(12.5%) and was transient, lasting only for 2-3 d and<br />
responded well to anti hepatic encephalopathy measures.<br />
Post procedure bleeding was encountered in 4 procedures<br />
(25%), 2 intraperitoneal and 2 hemobilia; all were<br />
managed conservatively with temporary stoppage <strong>of</strong><br />
anticoagulation and blood transfusion if indicated.<br />
In the current study, the overall 1 year shunt patency<br />
<strong>of</strong> all procedures (angioplasty ± stenting and TIPS) was<br />
22/25 (88%) as 3 patients had occluded shunts in spite <strong>of</strong><br />
repeated trials <strong>of</strong> dilatation and adherence to anticoagulation<br />
therapy. We compared clinical and laboratory characteristics<br />
before and after intervention in patients with patent<br />
shunts (22 patients) and in those with occluded shunts<br />
(3 patients) irrespective <strong>of</strong> the type <strong>of</strong> procedure performed.<br />
We observed that patients with occluded shunts<br />
showed no improvement compared to those with patent<br />
shunts even after multiple revisions in terms <strong>of</strong> clinical<br />
manifestations, laboratory pr<strong>of</strong>ile and performance status.<br />
These observations are consistent with Bachet et al [23]<br />
who concluded that, in patients with BCS treated with<br />
portosystemic shunting, shunt dysfunction has a major<br />
impact on morbidity and mortality and maintenance <strong>of</strong><br />
shunt patency is <strong>of</strong> major importance for better long-term<br />
outcome.<br />
WJG|www.wjgnet.com<br />
In conclusion; Budd Chiari syndrome is a potentially<br />
life-threatening disorder that requires a multidisciplinary<br />
approach with hepatologist, hematologist, interventional<br />
radiologist and vascular surgeon. Morbidity and mortality<br />
following both angioplasty ± stenting and TIPS are<br />
low with satisfactory stent and patient survival. Proper<br />
selection <strong>of</strong> procedure candidates and maintenance <strong>of</strong><br />
shunt patency by strict adherence to anticoagulation<br />
and early management <strong>of</strong> shunt dysfunction are crucial<br />
in clinical, laboratory and radiological improvement <strong>of</strong><br />
BCS patients.<br />
COMMENTS<br />
Background<br />
Budd-Chiari syndrome (BCS) results from hepatic venous outflow obstruction<br />
at any level from hepatic venules to the right atrium. Few patients respond to<br />
medical treatment (anticoagulation ± thrombolytic therapy, diuretics). However,<br />
most patients need intervention to restore the hepatic blood flow. Restoring<br />
outflow in one <strong>of</strong> the major hepatic veins by balloon dilatation ± stenting is the<br />
management <strong>of</strong> choice. When not possible or failed, Transjugular Intrahepatic<br />
Portosystemic Shunt is used.<br />
Research frontiers<br />
Follow up <strong>of</strong> patients after radiological intervention is crucial in order to assess<br />
patient improvement, shunt patency and function and to manage any procedure<br />
related complications. In this study, the authors demonstrate that morbidity and<br />
mortality following angioplasty ± stenting and transjugular intrahepatic portosystemic<br />
shunt (TIPS) are low with satisfactory outcome.<br />
Innovations and breakthroughs<br />
This is the first Egyptian study that addresses the short term outcome <strong>of</strong> interventional<br />
radiology procedures in management <strong>of</strong> BCS.<br />
Applications<br />
This study may represent a future strategy for good selection <strong>of</strong> procedure<br />
candidates, maintenance <strong>of</strong> shunt patency by strict adherence to anticoagulation<br />
and early management <strong>of</strong> shunt dysfunction which are all crucial in clinical,<br />
laboratory and radiological improvement <strong>of</strong> BCS patients.<br />
Terminology<br />
Angioplasty means balloon dilatation <strong>of</strong> hepatic vein; it may be with or without<br />
stent insertion. This procedure is performed in BCS patients with short segment<br />
stenosis or occlusion <strong>of</strong> the hepatic veins with significant patent segments. This<br />
approach will re-establish hepatic venous outflow via the physiological route. In<br />
cases where blood flow cannot be restored or where the approach fails (usually<br />
because the remaining patent veins are too small or have insufficient flow),<br />
Transjugular Intrahepatic Portosystemic Shunt is used; in which the shunt connects<br />
the hepatic vein to the portal vein to bypass the obstruction.<br />
Peer review<br />
The authors evaluated the outcome <strong>of</strong> patients with BCS after non surgical<br />
hepatic decompression procedures (either balloon angioplasty ± stenting or<br />
TIPS). It revealed that morbidity and mortality following both procedures are low<br />
with satisfactory stent and patient survival. Thus, proper selection <strong>of</strong> procedure<br />
candidates and maintenance <strong>of</strong> shunt patency by strict adherence to anticoagulation<br />
and early management <strong>of</strong> shunt dysfunction are crucial in clinical, laboratory<br />
and radiological improvement <strong>of</strong> those patients. Their results are excellent<br />
on managing a very challenging group <strong>of</strong> patients and their program should be<br />
commended for this outcome.<br />
REFERENCES<br />
1 Zimmerman MA, Cameron AM, Ghobrial RM. Budd-Chiari<br />
syndrome. Clin Liver Dis 2006; 10: 259-273, viii<br />
2 Aydinli M, Bayraktar Y. Budd-Chiari syndrome: etiology,<br />
pathogenesis and diagnosis. <strong>World</strong> J Gastroenterol 2007; 13:<br />
2693-2696<br />
3 Brancatelli G, Vilgrain V, Federle MP, Hakime A, Lagalla<br />
R, Iannaccone R, Valla D. Budd-Chiari syndrome: spectrum<br />
<strong>of</strong> imaging findings. AJR Am J Roentgenol 2007; 188:<br />
912 February 21, 2011|Volume 17|Issue 7|
W168-W176<br />
4 Slakey DP, Klein AS, Venbrux AC, Cameron JL. Budd-<br />
Chiari syndrome: current management options. Ann Surg<br />
2001; 233: 522-527<br />
5 Beckett D, Olliff S. Interventional radiology in the management<br />
<strong>of</strong> Budd Chiari syndrome. Cardiovasc Intervent Radiol<br />
2008; 31: 839-847<br />
6 Boyer TD, Haskal ZJ. The role <strong>of</strong> transjugular intrahepatic<br />
portosystemic shunt in the management <strong>of</strong> portal hypertension.<br />
Hepatology 2005; 41: 386-400<br />
7 Oken MM, Creech RH, Tormey DC, Horton J, Davis TE,<br />
McFadden ET, Carbone PP. Toxicity and response criteria <strong>of</strong><br />
the Eastern Cooperative Oncology Group. Am J Clin Oncol<br />
1982; 5: 649-655<br />
8 Darwish Murad S, Valla DC, de Groen PC, Zeitoun G, Hopmans<br />
JA, Haagsma EB, van Hoek B, Hansen BE, Rosendaal<br />
FR, Janssen HL. Determinants <strong>of</strong> survival and the effect <strong>of</strong><br />
portosystemic shunting in patients with Budd-Chiari syndrome.<br />
Hepatology 2004; 39: 500-508<br />
9 Pugh RN, Murray-Lyon IM, Dawson JL, Pietroni MC, Williams<br />
R. Transection <strong>of</strong> the oesophagus for bleeding oesophageal<br />
varices. Br J Surg 1973; 60: 646-649<br />
10 Madura JA, Rookstool M, Wease G. The management <strong>of</strong> patients<br />
on chronic Coumadin therapy undergoing subsequent<br />
surgical procedures. Am Surg 1994; 60: 542-546; discussion<br />
546-547<br />
11 Ryan JM, Ryan BM, Smith TP. Antibiotic prophylaxis in interventional<br />
radiology. J Vasc Interv Radiol 2004; 15: 547-556<br />
12 Kraai EP, Lopes RD, Alexander JH, Garcia D. Perioperative<br />
management <strong>of</strong> anticoagulation: guidelines translated for<br />
the clinician. J Thromb Thrombolysis 2009; 28: 16-22<br />
13 Xu K, He FX, Zhang HG, Zhang XT, Han MJ, Wang CR,<br />
Kaneko M, Takahashi M, Okawada T. Budd-Chiari syndrome<br />
caused by obstruction <strong>of</strong> the hepatic inferior vena<br />
cava: immediate and 2-year treatment results <strong>of</strong> transluminal<br />
angioplasty and metallic stent placement. Cardiovasc<br />
Intervent Radiol 1996; 19: 32-36<br />
14 Senzolo M, Cholongitas EC, Patch D, Burroughs AK. Up-<br />
WJG|www.wjgnet.com<br />
Eldorry A et al . Non surgical hepatic decompression in Budd-Chiari<br />
date on the classification, assessment <strong>of</strong> prognosis and therapy<br />
<strong>of</strong> Budd-Chiari syndrome. Nat Clin Pract Gastroenterol<br />
Hepatol 2005; 2: 182-190<br />
15 McDermott VG, Schuster MG, Smith TP. Antibiotic prophylaxis<br />
in vascular and interventional radiology. AJR Am J<br />
Roentgenol 1997; 169: 31-38<br />
16 Fisher NC, McCafferty I, Dolapci M, Wali M, Buckels JA,<br />
Olliff SP, Elias E. Managing Budd-Chiari syndrome: a retrospective<br />
review <strong>of</strong> percutaneous hepatic vein angioplasty<br />
and surgical shunting. Gut 1999; 44: 568-574<br />
17 Valla DC. The diagnosis and management <strong>of</strong> the Budd-<br />
Chiari syndrome: consensus and controversies. Hepatology<br />
2003; 38: 793-803<br />
18 Mancuso A, Fung K, Mela M, Tibballs J, Watkinson A,<br />
Burroughs AK, Patch D. TIPS for acute and chronic Budd-<br />
Chiari syndrome: a single-centre experience. J Hepatol 2003;<br />
38: 751-754<br />
19 Perelló A, García-Pagán JC, Gilabert R, Suárez Y, Moitinho E,<br />
Cervantes F, Reverter JC, Escorsell A, Bosch J, Rodés J. TIPS<br />
is a useful long-term derivative therapy for patients with<br />
Budd-Chiari syndrome uncontrolled by medical therapy.<br />
Hepatology 2002; 35: 132-139<br />
20 Rössle M, Olschewski M, Siegerstetter V, Berger E, Kurz<br />
K, Grandt D. The Budd-Chiari syndrome: outcome after<br />
treatment with the transjugular intrahepatic portosystemic<br />
shunt. Surgery 2004; 135: 394-403<br />
21 Hernández-Guerra M, Turnes J, Rubinstein P, Olliff S, Elias<br />
E, Bosch J, García-Pagán JC. PTFE-covered stents improve<br />
TIPS patency in Budd-Chiari syndrome. Hepatology 2004; 40:<br />
1197-1202<br />
22 Dravid VS, Gupta A, Zegel HG, Morales AV, Rabinowitz B,<br />
Freiman DB. Investigation <strong>of</strong> antibiotic prophylaxis usage<br />
for vascular and nonvascular interventional procedures. J<br />
Vasc Interv Radiol 1998; 9: 401-406<br />
23 Bachet JB, Condat B, Hagège H, Plessier A, Consigny Y,<br />
Belghiti J, Valla D. Long-term portosystemic shunt patency<br />
as a determinant <strong>of</strong> outcome in Budd-Chiari syndrome. J<br />
Hepatol 2007; 46: 60-68<br />
S- Editor Cheng JX L- Editor Rutheford A E- Editor Ma WH<br />
913 February 21, 2011|Volume 17|Issue 7|
Online Submissions: http://www.wjgnet.com/1007-9327<strong>of</strong>fice<br />
wjg@wjgnet.com<br />
doi:10.3748/wjg.v17.i7.914<br />
ORIGINAL ARTICLE<br />
Body mass index is associated with age-at-onset <strong>of</strong> HCVinfected<br />
hepatocellular carcinoma patients<br />
Takumi Akiyama, Toshihiko Mizuta, Seiji Kawazoe, Yuichiro Eguchi, Yasunori Kawaguchi, Hirokazu Takahashi,<br />
Iwata Ozaki, Kazuma Fujimoto<br />
Takumi Akiyama, Toshihiko Mizuta, Yuichiro Eguchi, Yasunori<br />
Kawaguchi, Hirokazu Takahashi, Iwata Ozaki, Kazuma<br />
Fujimoto, Department <strong>of</strong> Internal Medicine, Saga Medical<br />
School, Saga 8498501, Japan<br />
Takumi Akiyama, Seiji Kawazoe, Department <strong>of</strong> Hepatology,<br />
Saga Prefectural Hospital, Saga 8408571, Japan<br />
Author contributions: Akiyama T and Mizuta T designed research<br />
and analyzed data; Kawazoe S, Eguchi Y, Kawaguchi Y,<br />
Takahashi H and Ozaki I provided the patient data; Fujimoto K<br />
reviewed the manuscript; Akiyama T wrote the paper; Mizuta T<br />
reviewed and edited the manuscript.<br />
Correspondence to: Toshihiko Mizuta, MD, PhD, Department<br />
<strong>of</strong> Internal Medicine, Saga Medical School, 5-1-1<br />
Nabeshima, Saga 8498501, Japan. mizutat@med.saga-u.ac.jp<br />
Telephone: +81-952-342362 Fax: +81-952-342017<br />
Received: August 10, 2010 Revised: September 29, 2010<br />
Accepted: October 6, 2010<br />
Published online: February 21, 2011<br />
Abstract<br />
AIM: To identify factors associated with the age at<br />
onset <strong>of</strong> hepatitis C virus (HCV)-related hepatocellular<br />
carcinoma (HCC).<br />
METHODS: Five hundred and fifty-six consecutive<br />
patients positive for HCV antibody and treatmentnaïve<br />
HCC diagnosed between 1995 and 2004 were<br />
analyzed. Patients were classified into three groups<br />
according to age at HCC onset: < 60 years (n = 79),<br />
60-79 years (n = 439), or ≥ 80 years (n = 38). Differences<br />
among groups in terms <strong>of</strong> sex, body mass<br />
index (BMI), lifestyle characteristics, and liver function<br />
were assessed. Factors associated with HCC onset in<br />
patients < 60 or ≥ 80 years were analyzed by logistic<br />
regression analysis.<br />
RESULTS: Significant differences emerged for sex, BMI,<br />
degree <strong>of</strong> smoking and alcohol consumption, mean bilirubin,<br />
alanine aminotransferase (ALT), and γ-glutamyl<br />
transpeptidase (GGT) levels, prothrombin activity, and<br />
WJG|www.wjgnet.com<br />
914<br />
<strong>World</strong> J Gastroenterol 2011 February 21; 17(7): 914-921<br />
ISSN 1007-9327 (print) ISSN 2219-2840 (online)<br />
© 2011 Baishideng. All rights reserved.<br />
platelet counts. The mean BMI values <strong>of</strong> male patients<br />
> 60 years old were lower and mean BMI values <strong>of</strong><br />
female patients < 60 years old were higher than those<br />
<strong>of</strong> the general Japanese population. BMI > 25 kg/m 2<br />
[hazard ratio (HR), 1.8, P = 0.045], excessive alcohol<br />
consumption (HR, 2.5, P = 0.024), male sex (HR, 3.6, P<br />
= 0.002), and GGT levels > 50 IU/L (HR, 2.4, P = 0.014)<br />
were independently associated with HCC onset in patients<br />
< 60 years. Low ALT level was the only factor associated<br />
with HCC onset in patients aged ≥ 80 years.<br />
CONCLUSION: Increased BMI is associated with increased<br />
risk for early HCC development in HCV-infected<br />
patients. Achieving recommended BMI and reducing alcohol<br />
intake could help prevent hepatic carcinogenesis.<br />
© 2011 Baishideng. All rights reserved.<br />
Key words: Age-at-onset; Hepatocellular carcinoma;<br />
Hepatitis C virus; Body mass index; Alcohol consumption;<br />
Sex difference<br />
Peer reviewers: Heitor Rosa, Pr<strong>of</strong>essor, Department <strong>of</strong> Gastroenterology<br />
and Hepatology, Federal University School <strong>of</strong><br />
Medicine, Rua 126 n.21, Goiania - GO 74093-080, Brazil; Jian<br />
Wu, Associate Pr<strong>of</strong>essor <strong>of</strong> Medicine, Internal Medicine/Transplant<br />
Research Program, University <strong>of</strong> California, Davis Medical<br />
Center, 4635 2nd Ave. Suite 1001, Sacramento, CA 95817,<br />
United States<br />
Akiyama T, Mizuta T, Kawazoe S, Eguchi Y, Kawaguchi Y,<br />
Takahashi H, Ozaki I, Fujimoto K. Body mass index is associated<br />
with age-at-onset <strong>of</strong> HCV-infected hepatocellular carcinoma<br />
patients. <strong>World</strong> J Gastroenterol 2011; 17(7): 914-921 Available<br />
from: URL: http://www.wjgnet.com/1007-9327/full/v17/i7/<br />
914.htm DOI: http://dx.doi.org/10.3748/wjg.v17.i7.914<br />
INTRODUCTION<br />
Hepatocellular carcinoma (HCC) is the fifth most com-<br />
February 21, 2011|Volume 17|Issue 7|
A<br />
BMI<br />
28<br />
26<br />
24<br />
22<br />
20<br />
18<br />
40-49 50-59 60-69 70-79 80 <<br />
Age <strong>of</strong> HCC occurrence<br />
Figure 2 Mean body mass index in each age group at onset <strong>of</strong> hepatocellular carcinoma (A: Men; B: Women). The bars show the mean body mass index (BMI)<br />
± SD in patients with hepatocellular carcinoma (HCC). The dashed lines show the mean BMI for the general Japanese population in 2005 and 2006, which was surveyed<br />
by the Ministry <strong>of</strong> Health, Labour and Welfare, Japan.<br />
P = 0.033), habitual smoking (HR, 2.7; 95% CI, 1.67-4.39;<br />
P < 0.0001), heavy drinking (HR, 3.9; 95% CI, 1.93-7.87;<br />
P = 0.0002), total bilirubin > 2.0 mg/dL (HR, 2.2; 95%<br />
CI, 1.00-4.96; P = 0.049), prothrombin activity > 70%<br />
(HR, 1.9; 95% CI, 1.11-3.26; P = 0.019), and GGT level<br />
> 50 IU/L (HR, 3.2; 95% CI, 1.73-6.05; P = 0.0002). In<br />
multivariate analysis, independent risk factors for earlier<br />
age at onset <strong>of</strong> HCC were male sex (HR, 3.6; 95% CI,<br />
WJG|www.wjgnet.com<br />
BMI<br />
28<br />
26<br />
24<br />
22<br />
20<br />
18<br />
50-59 60-69 70-79 80 <<br />
Age <strong>of</strong> HCC occurrence<br />
Table 2 Analysis <strong>of</strong> factors affecting development <strong>of</strong> hepatocellular carcinoma at younger age (under 60 yr old)<br />
Variables Univariate analysis Multivariate analysis<br />
B<br />
HR 95% CI P HR 95% CI P<br />
Sex<br />
Female 1 1<br />
Male 5.43 2.647-11.120 < 0.0001 3.58 1.580-8.133 0.002<br />
BMI<br />
< 25 1 1<br />
≥ 25 1.73 1.044-2.851 0.033 1.82 1.015-3.270 0.045<br />
Diabetes mellitus<br />
Without 1 1<br />
With 1.12 0.619-2.037 0.703 1.00 0.516-1.952 0.991<br />
Smoking (packs year)<br />
< 20 1 1<br />
≥ 20 2.71 1.669-4.393 < 0.0001 1.64 1.904-2.991 0.104<br />
Alcohol (g/d)<br />
< 60 1 1<br />
≥ 60 3.89 1.926-7.874 0.0002 2.51 1.130-5.563 0.024<br />
Total bilirubin (mg/dL)<br />
< 2.0 1 1<br />
≥ 2.0 2.23 1.003-4.958 0.049 2.33 0.898-6.033 0.082<br />
Prothrombin activity (%)<br />
≥ 70 1 1<br />
< 70 1.91 1.111-3.262 0.019 1.60 0.859-2.987 0.139<br />
Platelet (× 10 4 /μL)<br />
≥ 10 1 1<br />
< 10 1.34 0.829-2.166 0.232 1.60 0.877-2.886 0.118<br />
ALT (IU/L)<br />
< 80 1 1<br />
≥ 80 1.44 0.884-2.350 0.142 1.17 0.656-2.090 0.542<br />
GGT (IU/L)<br />
< 50 1 1<br />
≥ 50 3.24 1.731-6.053 0.0002 2.38 1.194-4.727 0.014<br />
HR: Hazard ratio; BMI: Body mass index; ALT: Alanine aminotransferase; GGT: γ-glutamyl transpeptidase.<br />
Akiyama T et al . BMI and age at HCC onset<br />
1.58-8.13; P = 0.002), BMI > 25 kg/m 2 (HR, 1.8; 95%<br />
CI, 1.015-3.270; P = 0.045), heavy drinking (HR, 2.5; 95%<br />
CI, 1.13-5.56; P = 0.024), and GGT > 50 IU/L (HR, 2.4;<br />
95% CI, 1.19-4.73; P = 0.014).<br />
Factors associated with the development <strong>of</strong> HCC at ≥<br />
80 years <strong>of</strong> age<br />
We also investigated factors associated with the develop-<br />
917 February 21, 2011|Volume 17|Issue 7|
Akiyama T et al . BMI and age at HCC onset<br />
Table 3 Analysis <strong>of</strong> factors affecting development <strong>of</strong> hepatocellular carcinoma at older age (over 80 yr old)<br />
Variables Univariate analysis Multivariate analysis<br />
ment <strong>of</strong> HCC at an older age (i.e. ≥ 80 years <strong>of</strong> age) (Table<br />
3). In univariate analysis, the following were significantly<br />
and negatively associated with age at onset <strong>of</strong> HCC ≥ 80<br />
years: male sex (HR, 0.45; 95% CI, 0.23-0.87; P = 0.017),<br />
diabetes mellitus (HR, 0.23; 95% CI, 0.05-0.96; P = 0.043),<br />
prothrombin activity < 70% (HR, 0.1; 95% CI, 0.01-0.76;<br />
P = 0.025), ALT > 80 IU/L (HR, 0.1; 95% CI, 0.02-0.43;<br />
P = 0.002), and GGT > 50 IU/L (HR, 0.51; 95% CI,<br />
0.26-0.98; P = 0.045). In multivariate analysis, ALT > 80<br />
IU/L was the only independent factor associated with age<br />
at onset <strong>of</strong> HCC ≥ 80 years (HR, 0.13; 95% CI, 0.03-0.57;<br />
P = 0.007).<br />
Age at onset <strong>of</strong> HCC stratified by BMI in relation to sex<br />
or alcohol consumption<br />
Differences in age at onset <strong>of</strong> HCC stratified by BMI<br />
were assessed in relation to sex or alcohol consumption.<br />
In men, age at onset decreased significantly with increasing<br />
BMI (mean age ± SD; underweight, 71.1 ± 7.4 years;<br />
normal weight, 67.0 ± 8.5 years; overweight, 63.6 ± 8.1<br />
years; obese, 57.0 ± 7.0 years) (Figure 3A). Although a<br />
similar trend was noted in women, this was not significant<br />
(underweight, 73.6 ± 7.8 years; normal weight, 70.4<br />
± 7.0 years; overweight, 68.9 ± 6.4 years; obese, 67.0 ± 7.5<br />
years) (Figure 3B).<br />
WJG|www.wjgnet.com<br />
HR 95% CI P HR 95% CI P<br />
Sex<br />
Female 1 1<br />
Male 0.45 0.229-0.867 0.017 0.47 0.200-1.119 0.089<br />
BMI<br />
A<br />
Age (yr)<br />
90<br />
80<br />
70<br />
60<br />
50<br />
40<br />
P < 0.05<br />
NS P < 0.05 NS<br />
as the core protein, cause oxidative damage by exposing<br />
the endoplasmic reticulum to oxidative stress [19-21] . Hepatic<br />
oxidative stress is strongly associated with increased risk<br />
for HCC in patients with chronic HCV [22] . Because oxidative<br />
stress is also caused by various host-related factors, it<br />
is expected to be influenced more strongly by host-related<br />
factors in HCV-infected patients than in those with HCVnegative<br />
liver disease. Indeed, we have previously reported<br />
that visceral fat accumulation was associated with greater<br />
insulin resistance in chronic HCV patients than in those<br />
with non-alcoholic fatty liver disease [23] . Therefore, it is<br />
plausible that the association between earlier onset <strong>of</strong><br />
HCC and increased BMI is due to the generation <strong>of</strong> hepatic<br />
oxidative stress.<br />
An interesting aspect <strong>of</strong> our results is that underweight<br />
patients, defined as those with a BMI <strong>of</strong> < 18.5 kg/m 2 ,<br />
tended to be older at HCC onset than patients within the<br />
WJG|www.wjgnet.com<br />
P < 0.05<br />
NS<br />
< 18.5 18.5-25 25-30 30 <<br />
BMI<br />
Figure 3 Differences in age at onset <strong>of</strong> hepatocellular carcinoma stratified by body mass index according to sex (A: Men; B: Women). Statistical analysis<br />
was performed using the Tukey-Kramer method. NS: Not significant; BMI: Body mass index.<br />
A<br />
Age (yr)<br />
90<br />
80<br />
70<br />
60<br />
50<br />
40<br />
P < 0.05<br />
P < 0.05<br />
< 18.5 18.5-25 25-30 30 <<br />
BMI<br />
NS<br />
P < 0.05 P < 0.05 NS<br />
B<br />
Age (yr)<br />
90<br />
80<br />
70<br />
60<br />
50<br />
40<br />
NS<br />
NS NS NS<br />
< 18.5 18.5-25 25-30 30 <<br />
Figure 4 Differences in age at onset <strong>of</strong> hepatocellular carcinoma stratified by body mass index according to degree <strong>of</strong> alcohol consumption (A: Non-heavy<br />
drinkers < 60 g/d; B: Heavy drinkers ≥ 60 g/d). Statistical analysis was performed using the Tukey-Kramer method. NS: Not significant; BMI: Body mass index.<br />
B<br />
Age (yr)<br />
90<br />
80<br />
70<br />
60<br />
50<br />
40<br />
Akiyama T et al . BMI and age at HCC onset<br />
NS<br />
normal weight range (BMI 18.5-25 kg/m 2 ). Recently, Ohki<br />
et al [11] reported that patients with a BMI < 18.5 kg/m 2<br />
had the lowest risk <strong>of</strong> developing HCC due to chronic<br />
HCV infection among all BMI groups. In general, the<br />
mortality rate associated with cardiovascular disease or<br />
<strong>cancer</strong> is higher in underweight patients than in normal<br />
weight patients [24,25] . Clearly, a larger cohort study is needed<br />
to investigate whether leanness confers a protective effect<br />
against hepatocarcinogenesis in HCV-infected patients.<br />
Excessive alcohol consumption is also known to exacerbate<br />
hepatic oxidative stress and evoke liver fibrosis<br />
or HCC [20,26] . In this study, there was no association between<br />
BMI and age at onset <strong>of</strong> HCC in heavy drinkers.<br />
We speculate that this group may include some patients<br />
who are malnourished and possibly losing weight.<br />
Sex modulates the natural history <strong>of</strong> chronic liver disease.<br />
Previous studies have suggested that chronic HCV<br />
919 February 21, 2011|Volume 17|Issue 7|<br />
NS<br />
BMI<br />
NS<br />
NS<br />
NS NS NS<br />
< 18.5 18.5-25 25-30 30 <<br />
BMI<br />
NS
Akiyama T et al . BMI and age at HCC onset<br />
infection progresses more rapidly in men than women,<br />
and that cirrhosis is predominately a disease <strong>of</strong> men and<br />
postmenopausal women [27] . Shimizu et al suggested that<br />
estrogens protect against oxidative stress in liver injury<br />
and hepatic fibrosis [28] . In this study, the effect <strong>of</strong> BMI<br />
on age at onset <strong>of</strong> HCC was more remarkable in men<br />
than women. We speculate two mechanisms to account<br />
for this difference: (1) estrogens mitigate oxidative stress<br />
or insulin resistance associated with obesity; and (2) subcutaneous<br />
fat accumulation is more dominant in obese<br />
women than visceral fat, which is known to produce several<br />
adipokines that cause insulin resistance [29] .<br />
In addition, we examined factors associated with onset<br />
<strong>of</strong> HCC at an older age (≥ 80 years). In this analysis,<br />
ALT level was the only independent factor associated with<br />
hepatocarcinogenesis in HCV-infected patients at an age<br />
≥ 80 years. It is well known that ALT levels are associated<br />
with liver inflammation and fibrosis progression, and<br />
Ishiguro et al recently reported that elevated ALT levels<br />
were strongly associated with the incidence <strong>of</strong> HCC, regardless<br />
<strong>of</strong> hepatitis virus positivity, in a large populationbased<br />
cohort study [30] . Therefore, lower ALT levels might<br />
indicate a slow course <strong>of</strong> progression <strong>of</strong> hepatic fibrosis<br />
or carcinogenesis.<br />
A limitation <strong>of</strong> this study is that it was a cross-sectional<br />
observation, rather than a cohort follow-up study.<br />
Further studies are needed to confirm our results.<br />
In conclusion, the results <strong>of</strong> the present study indicate<br />
that higher BMI, excessive alcohol consumption, and male<br />
sex are independent risk factors for onset <strong>of</strong> HCV-related<br />
HCC at an age <strong>of</strong> < 60 years. These results suggest that<br />
interventions to promote changes in the lifestyle <strong>of</strong> patients<br />
with chronic HCV may slow the progression <strong>of</strong><br />
HCV infection to HCC.<br />
ACKNOWLEDGMENTS<br />
The authors would like to thank Yukie Watanabe and<br />
Chieko Ogawa for their assistance.<br />
COMMENTS<br />
Background<br />
The incidence and mortality associated with hepatocellular carcinoma (HCC)<br />
have been increasing worldwide, and hepatitis C virus (HCV) infection plays an<br />
important role in the pathogenesis <strong>of</strong> HCC. However, the factors that influence<br />
the development <strong>of</strong> HCC in HCV-infected patients remain largely unknown. Previous<br />
studies have suggested that host factors, such as sex, alcohol consumption,<br />
smoking, diabetes mellitus, and obesity, are important risk factors for HCC.<br />
Meanwhile, it has been reported that HCV infection causes insulin resistance<br />
and leads to oxidative stress, potentiating fibrosis and hepatic carcinogenesis.<br />
Therefore, we hypothesized that body mass index (BMI) influences the onset<br />
age <strong>of</strong> HCC related to HCV infection.<br />
Research frontiers<br />
Many studies have indicated that obesity is an independent and a significant<br />
risk factor for HCC occurrence. Recently, several metabolic markers have been<br />
implicated in the development and progression <strong>of</strong> HCC.<br />
Innovations and breakthroughs<br />
This study indicated that higher BMI, heavy alcohol consumption, male sex, and<br />
high γ-glutamyl transpeptidase levels are independent risk factors for younger<br />
age at onset <strong>of</strong> HCV-related HCC. Interestingly, the underweight patients (BMI<br />
WJG|www.wjgnet.com<br />
< 18.5 kg/m 2 ), tended to be older at HCC onset than patients within the normal<br />
weight range (BMI 18.5-25 kg/m 2 ).<br />
Applications<br />
The results <strong>of</strong> this study suggest that achieving an adequate body weight along<br />
with a reduction <strong>of</strong> alcohol intake in patients with chronic hepatitis C could help<br />
prevent hepatic carcinogenesis.<br />
Peer review<br />
The study was reasonably designed and well conducted, and the data support<br />
their conclusions.<br />
REFERENCES<br />
1 El-Serag HB. Epidemiology <strong>of</strong> hepatocellular carcinoma in<br />
USA. Hepatol Res 2007; 37 Suppl 2: S88-S94<br />
2 El-Serag HB, Rudolph KL. Hepatocellular carcinoma: epidemiology<br />
and molecular carcinogenesis. Gastroenterology<br />
2007; 132: 2557-2576<br />
3 Umemura T, Ichijo T, Yoshizawa K, Tanaka E, Kiyosawa K.<br />
Epidemiology <strong>of</strong> hepatocellular carcinoma in Japan. J Gastroenterol<br />
2009; 44 Suppl 19: 102-107<br />
4 El-Serag HB. Hepatocellular carcinoma and hepatitis C in<br />
the United States. Hepatology 2002; 36: S74-S83<br />
5 Fattovich G, Str<strong>of</strong>folini T, Zagni I, Donato F. Hepatocellular<br />
carcinoma in cirrhosis: incidence and risk factors. Gastroenterology<br />
2004; 127: S35-S50<br />
6 Sinn DH, Paik SW, Kang P, Kil JS, Park SU, Lee SY, Song<br />
SM, Gwak GY, Choi MS, Lee JH, Koh KC, Yoo BC. Disease<br />
progression and the risk factor analysis for chronic hepatitis<br />
C. Liver Int 2008; 28: 1363-1369<br />
7 Marrero JA, Fontana RJ, Fu S, Conjeevaram HS, Su GL, Lok<br />
AS. Alcohol, tobacco and obesity are synergistic risk factors<br />
for hepatocellular carcinoma. J Hepatol 2005; 42: 218-224<br />
8 Hara M, Tanaka K, Sakamoto T, Higaki Y, Mizuta T, Eguchi<br />
Y, Yasutake T, Ozaki I, Yamamoto K, Onohara S, Kawazoe<br />
S, Shigematsu H, Koizumi S. Case-control study on cigarette<br />
smoking and the risk <strong>of</strong> hepatocellular carcinoma among<br />
Japanese. Cancer Sci 2008; 99: 93-97<br />
9 Polesel J, Zucchetto A, Montella M, Dal Maso L, Crispo<br />
A, La Vecchia C, Serraino D, Franceschi S, Talamini R. The<br />
impact <strong>of</strong> obesity and diabetes mellitus on the risk <strong>of</strong> hepatocellular<br />
carcinoma. Ann Oncol 2009; 20: 353-357<br />
10 Aizawa Y, Shibamoto Y, Takagi I, Zeniya M, Toda G. Analysis<br />
<strong>of</strong> factors affecting the appearance <strong>of</strong> hepatocellular carcinoma<br />
in patients with chronic hepatitis C. A long term followup<br />
study after histologic diagnosis. Cancer 2000; 89: 53-59<br />
11 Ohki T, Tateishi R, Sato T, Masuzaki R, Imamura J, Goto T,<br />
Yamashiki N, Yoshida H, Kanai F, Kato N, Shiina S, Yoshida<br />
H, Kawabe T, Omata M. Obesity is an independent risk factor<br />
for hepatocellular carcinoma development in chronic hepatitis<br />
C patients. Clin Gastroenterol Hepatol 2008; 6: 459-464<br />
12 Vidali M, Tripodi MF, Ivaldi A, Zampino R, Occhino G, Restivo<br />
L, Sutti S, Marrone A, Ruggiero G, Albano E, Adinolfi<br />
LE. Interplay between oxidative stress and hepatic steatosis<br />
in the progression <strong>of</strong> chronic hepatitis C. J Hepatol 2008; 48:<br />
399-406<br />
13 Koike K. Steatosis, liver injury, and hepatocarcinogenesis in<br />
hepatitis C viral infection. J Gastroenterol 2009; 44 Suppl 19:<br />
82-88<br />
14 Sheikh MY, Choi J, Qadri I, Friedman JE, Sanyal AJ. Hepatitis<br />
C virus infection: molecular pathways to metabolic syndrome.<br />
Hepatology 2008; 47: 2127-2133<br />
15 Liver Cancer Study Group. The General Rules for the Clinical<br />
and Pathological Study <strong>of</strong> Primary Liver Cancer. 5th ed.<br />
Japan, 2008: 24-28<br />
16 <strong>World</strong> Health Organization. Obesity: Preventing and managing<br />
the global epidemic; Report <strong>of</strong> a WHO Consultation<br />
on Obesity, Geneva, 3-5, June 1997. Geneva: WHO, 1998<br />
17 Report <strong>of</strong> a WHO Consultation. Definition, diagnosis and<br />
classification <strong>of</strong> diabetes mellitus and its complication:<br />
920 February 21, 2011|Volume 17|Issue 7|
Part1. Diagnosis and classification <strong>of</strong> diabetes mellitus.<br />
<strong>World</strong> Health Organization, Department <strong>of</strong> Noncommunicable<br />
Disease Surveillance, Geneva, 1999<br />
18 Hamada H, Yatsuhashi H, Yano K, Daikoku M, Arisawa<br />
K, Inoue O, Koga M, Nakata K, Eguchi K, Yano M. Impact<br />
<strong>of</strong> aging on the development <strong>of</strong> hepatocellular carcinoma<br />
in patients with posttransfusion chronic hepatitis C. Cancer<br />
2002; 95: 331-339<br />
19 Tardif KD, Waris G, Siddiqui A. Hepatitis C virus, ER stress,<br />
and oxidative stress. Trends Microbiol 2005; 13: 159-163<br />
20 Ji C, Kaplowitz N. ER stress: can the liver cope? J Hepatol<br />
2006; 45: 321-333<br />
21 Ciccaglione AR, Costantino A, Tritarelli E, Marcantonio<br />
C, Equestre M, Marziliano N, Rapicetta M. Activation <strong>of</strong><br />
endoplasmic reticulum stress response by hepatitis C virus<br />
proteins. Arch Virol 2005; 150: 1339-1356<br />
22 Tanaka H, Fujita N, Sugimoto R, Urawa N, Horiike S, Kobayashi<br />
Y, Iwasa M, Ma N, Kawanishi S, Watanabe S, Kaito<br />
M, Takei Y. Hepatic oxidative DNA damage is associated<br />
with increased risk for hepatocellular carcinoma in chronic<br />
hepatitis C. Br J Cancer 2008; 98: 580-586<br />
23 Eguchi Y, Mizuta T, Ishibashi E, Kitajima Y, Oza N, Nakashita<br />
S, Hara M, Iwane S, Takahashi H, Akiyama T, Ario<br />
K, Kawaguchi Y, Yasutake T, Iwakiri R, Ozaki I, Hisatomi<br />
A, Eguchi T, Ono N, Fujimoto K. Hepatitis C virus infection<br />
enhances insulin resistance induced by visceral fat accumu-<br />
WJG|www.wjgnet.com<br />
Akiyama T et al . BMI and age at HCC onset<br />
lation. Liver Int 2009; 29: 213-220<br />
24 Whitlock G, Lewington S, Sherliker P, Clarke R, Emberson<br />
J, Halsey J, Qizilbash N, Collins R, Peto R. Body-mass index<br />
and cause-specific mortality in 900 000 adults: collaborative<br />
analyses <strong>of</strong> 57 prospective studies. Lancet 2009; 373: 1083-1096<br />
25 Calle EE, Thun MJ, Petrelli JM, Rodriguez C, Heath CW Jr.<br />
Body-mass index and mortality in a prospective cohort <strong>of</strong><br />
U.S. adults. N Engl J Med 1999; 341: 1097-1105<br />
26 de la Monte SM, Yeon JE, Tong M, Longato L, Chaudhry R,<br />
Pang MY, Duan K, Wands JR. Insulin resistance in experimental<br />
alcohol-induced liver disease. J Gastroenterol Hepatol<br />
2008; 23: e477-e486<br />
27 Farinati F, Sergio A, Giacomin A, Di Nolfo MA, Del Poggio<br />
P, Benvegnù L, Rapaccini G, Zoli M, Borzio F, Giannini EG,<br />
Caturelli E, Trevisani F. Is female sex a significant favorable<br />
prognostic factor in hepatocellular carcinoma? Eur J Gastroenterol<br />
Hepatol 2009; 21: 1212-1218<br />
28 Shimizu I, Ito S. Protection <strong>of</strong> estrogens against the progression<br />
<strong>of</strong> chronic liver disease. Hepatol Res 2007; 37: 239-247<br />
29 Geer EB, Shen W. Gender differences in insulin resistance,<br />
body composition, and energy balance. Gend Med 2009; 6<br />
Suppl 1: 60-75<br />
30 Ishiguro S, Inoue M, Tanaka Y, Mizokami M, Iwasaki M,<br />
Tsugane S. Serum aminotransferase level and the risk <strong>of</strong> hepatocellular<br />
carcinoma: a population-based cohort study in<br />
Japan. Eur J Cancer Prev 2009; 18: 26-32<br />
S- Editor Sun H L- Editor O’Neill M E- Editor Ma WH<br />
921 February 21, 2011|Volume 17|Issue 7|
Online Submissions: http://www.wjgnet.com/1007-9327<strong>of</strong>fice<br />
wjg@wjgnet.com<br />
doi:10.3748/wjg.v17.i7.922<br />
Vitamin D deficiency in cirrhosis relates to liver dysfunction<br />
rather than aetiology<br />
Mikkel Malham, Søren Peter Jørgensen, Peter Ott, Jørgen Agnholt, Hendrik Vilstrup, Mette Borre,<br />
Jens F Dahlerup<br />
Mikkel Malham, Søren Peter Jørgensen, Peter Ott, Jørgen<br />
Agnholt, Hendrik Vilstrup, Mette Borre, Jens F Dahlerup,<br />
Department <strong>of</strong> Medicine V (Hepatology and Gastroenterology),<br />
Aarhus University Hospital, DK-8000, Aarhus C, Denmark<br />
Author contributions: Malham M wrote the protocol, carried<br />
out the study and wrote the first draft <strong>of</strong> the manuscript; All<br />
authors contributed to the study design, data interpretation and<br />
analysis, preparation <strong>of</strong> the manuscript, and critical review; All<br />
authors read and approved the final manuscript.<br />
Correspondence to: Mikkel Malham, MD, Department <strong>of</strong><br />
Medicine V (Hepatology and Gastroenterology), Aarhus University<br />
Hospital, 44 Noerrebrogade, Building 1C, DK-8000,<br />
Aarhus C, Denmark. mikkel.malham@gmail.com<br />
Telephone: +45-31121035 Fax: +45-89492740<br />
Received: August 26, 2010 Revised: October 16, 2010<br />
Accepted: October 23, 2010<br />
Published online: February 21, 2011<br />
Abstract<br />
AIM: To examine the vitamin D status in patients with<br />
alcoholic cirrhosis compared to those with primary biliary<br />
cirrhosis.<br />
METHODS: Our retrospective case series comprised 89<br />
patients with alcoholic cirrhosis and 34 patients with primary<br />
biliary cirrhosis who visited our outpatient clinic in<br />
2005 and underwent a serum vitamin D status assessment.<br />
RESULTS: Among the patients with alcoholic cirrhosis,<br />
85% had serum vitamin D levels below 50 nmol/L and<br />
55% had levels below 25 nmol/L, as compared to 60%<br />
and 16% <strong>of</strong> the patients with primary biliary cirrhosis,<br />
respectively (P < 0.001). In both groups, serum vitamin<br />
D levels decreased with increasing liver disease severity,<br />
as determined by the Child-Pugh score.<br />
CONCLUSION: Vitamin D deficiency in cirrhosis relates<br />
WJG|www.wjgnet.com<br />
<strong>World</strong> J Gastroenterol 2011 February 21; 17(7): 922-925<br />
ISSN 1007-9327 (print) ISSN 2219-2840 (online)<br />
© 2011 Baishideng. All rights reserved.<br />
to liver dysfunction rather than aetiology, with lower<br />
levels <strong>of</strong> vitamin D in alcoholic cirrhosis than in primary<br />
biliary cirrhosis.<br />
© 2011 Baishideng. All rights reserved.<br />
Key words: Alcoholic liver cirrhosis; Child-Pugh score;<br />
Primary biliary cirrhosis; Vitamin D deficiency<br />
Peer reviewer: Lixin Zhu, MD, State University <strong>of</strong> New York,<br />
3435 Main Street, 422 BRB, Buffalo, 14214 New York,<br />
United States<br />
Malham M, Jørgensen SP, Ott P, Agnholt J, Vilstrup H, Borre<br />
M, Dahlerup JF. Vitamin D deficiency in cirrhosis relates to<br />
liver dysfunction rather than aetiology. <strong>World</strong> J Gastroenterol<br />
2011; 17(7): 922-925 Available from: URL: http://www.wjgnet.com/1007-9327/full/v17/i7/922.htm<br />
DOI: http://dx.doi.<br />
org/10.3748/wjg.v17.i7.922<br />
INTRODUCTION<br />
BRIEF ARTICLE<br />
Patients with chronic liver disease have an increased<br />
risk for the development <strong>of</strong> osteoporosis and fractures,<br />
reduced muscle strength, an impaired inflammatory response,<br />
and malignancy [1-3] . These conditions have also<br />
been associated with vitamin D deficiency [4-6] . Vitamin D<br />
deficiency and osteomalacia have been described in chronic<br />
cholestatic liver disease, such as primary biliary cirrhosis<br />
(PBC) [7] . However, the frequency <strong>of</strong> vitamin D deficiency,<br />
specifically in alcoholic liver cirrhosis (ALC), has not been<br />
well described. The limited available data suggest that<br />
there is a high frequency <strong>of</strong> vitamin D deficiency in patients<br />
with chronic liver disease [8,9] .<br />
The main source <strong>of</strong> vitamin D in humans is the exposure<br />
<strong>of</strong> skin to sunlight. For further activation, vitamin<br />
D is hydroxylated in the liver to form 25-(OH) vitamin D<br />
922 February 21, 2011|Volume 17|Issue 7|
(25-OHD) and in the kidneys to form the active metabolite<br />
1,25(OH)2 vitamin D. The body stores <strong>of</strong> vitamin D<br />
are best reflected by the serum levels <strong>of</strong> 25-(OH)D [10] .<br />
The aim <strong>of</strong> the present study was to describe the<br />
serum vitamin D status in a retrospective case series <strong>of</strong><br />
patients with ALC compared to those with PBC. Patients<br />
with PBC were considered a priori to demonstrate a high<br />
incidence <strong>of</strong> vitamin D deficiency.<br />
MATERIALS AND METHODS<br />
We collected data from the medical records <strong>of</strong> all patients<br />
with a diagnosis <strong>of</strong> PBC or ALC who visited our outpatient<br />
clinic in 2005. A total <strong>of</strong> 205 patients were identified:<br />
58 had PBC, and 147 had ALC. The study population<br />
comprised patients for whom vitamin D measurements<br />
had been completed and for whom the Child-Pugh status<br />
could be assessed (34 and 89 patients, respectively). In patients<br />
who had undergone serial vitamin D measurements,<br />
the first blood sample collected in 2005 was used. The<br />
vitamin D status was defined according to the following<br />
levels <strong>of</strong> 25-(OH)D: severe deficiency: 0-12.5 nmol/L,<br />
deficiency: 12.5-25 nmol/L, insufficiency: 25-50 nmol/L,<br />
and vitamin D replete: > 50 nmol/L [11] . Data concerning<br />
previous and ongoing vitamin D supplementation were<br />
collected from the patients’ medical records. To assess the<br />
severity <strong>of</strong> liver disease, the patients were scored according<br />
to the Child-Pugh classification. This score is based<br />
on the degree <strong>of</strong> encephalopathy, the presence <strong>of</strong> ascites,<br />
prothrombin time, and the serum levels <strong>of</strong> bilirubin, and<br />
albumin. The score ranges from 5 to 15 with increasing<br />
severity. Accordingly, the patients had either compensated<br />
liver disease (Class A, 5-6 points), moderate liver disease<br />
(Class B, 7-9 points), or severe liver disease (Class C, 10-15<br />
points).<br />
Techniques<br />
Plasma 25(OH)D2 and 25(OH)D3 were analysed by<br />
isotope-dilution liquid chromatography-tandem mass spectrometry<br />
using an API3000 TM mass spectrometer (Applied<br />
Biosystems, Foster City, CA, USA) and a method adapted<br />
from Maunsell et al [12] . The interassay variation coefficients<br />
for plasma 25(OH)D2 were 8.5% at 23.4 nmol/L and 8.0%<br />
at 64.4 nmol/L, and for plasma 25(OH)D3 these values<br />
were 9.6% at 24.8 nmol/L and 8.1% at 47.7 nmol/L.<br />
Statistics<br />
Non-parametric statistics were used for the descriptions,<br />
and the Mann-Whitney U test was employed for comparisons<br />
between groups. The association between two variables<br />
was assessed by the contingency coefficient C, and<br />
statistical significance was determined using the χ 2 test.<br />
RESULTS<br />
In the patients with ALC, 18% had a severe vitamin D<br />
deficiency. In comparison, none <strong>of</strong> the patients with PBC<br />
had such a deficiency. Similarly, in a comparison <strong>of</strong> patients<br />
WJG|www.wjgnet.com<br />
25-OH vitamin D (nmol/L)<br />
Malham M et al . Vitamin D deficiency in liver cirrhosis<br />
160<br />
140<br />
120<br />
100<br />
80<br />
60<br />
40<br />
20<br />
0<br />
Table 1 Study group stratified according to the Child-Pugh<br />
class and the degree <strong>of</strong> vitamin D deficiency<br />
Vitamin D (nmol/L) Child-Pugh group<br />
with ALC and PBC, vitamin D deficiency was identified in<br />
37% vs 16% and vitamin D insufficiency was identified in<br />
30% vs 41% <strong>of</strong> patients, respectively. Only 15% <strong>of</strong> patients<br />
with ALC were vitamin D replete in comparison to 40%<br />
<strong>of</strong> patients with PBC. The median 25-OHD blood concentration<br />
in ALC patients was 24 nmol/L, or 53% <strong>of</strong> the<br />
median serum level <strong>of</strong> 45 nmol/L in PBC patients (P <<br />
0.001, Mann-Whitney U test) (Figure 1).<br />
Four patients with ALC and 13 patients with PBC<br />
were receiving vitamin D supplementation at the time<br />
<strong>of</strong> blood sampling. Their vitamin D levels did not differ<br />
from those determined in patients who did not receive<br />
supplementation.<br />
The distribution <strong>of</strong> Child-Pugh groups A, B, and C differed<br />
between ALC and PBC patients. Patients with ALC<br />
demonstrated more advanced disease (16 A, 36 B, and 37 C)<br />
compared to those with PBC (33 A, 1 B, and no C). In all<br />
the cirrhotic patients, there was an association between the<br />
Child-Pugh score and vitamin D status (contingency coefficient<br />
C = 0.29, P < 0.05, χ 2 test) (Table 1).<br />
DISCUSSION<br />
P < 0.0001<br />
PBC ALC<br />
50 nmol/L<br />
25 nmol/L<br />
12.5 nmol/L<br />
Figure 1 Vitamin D levels in the study group. Vitamin D levels in 37 patients<br />
with primary biliary cirrhosis and 89 patients with alcoholic liver cirrhosis. Patients<br />
with alcoholic liver cirrhosis demonstrated significantly lower overall vitamin D<br />
levels in comparison to patients with primary biliary cirrhosis (P < 0.0001, Mann-<br />
Whitney U test). PBC: Primary biliary cirrhosis; ALC: Alcoholic liver cirrhosis.<br />
A B C<br />
< 25 17 15 21<br />
25-50 14 16 12<br />
> 50 18 6 4<br />
The vast majority (85%) <strong>of</strong> patients with ALC presented<br />
a compromised vitamin D status. The same was found<br />
in fewer than half <strong>of</strong> the patients with PBC (47%). This<br />
finding is in contrast to the standard clinical knowledge<br />
that vitamin D deficiency is expected in PBC. Further-<br />
923 February 21, 2011|Volume 17|Issue 7|
Malham M et al . Vitamin D deficiency in liver cirrhosis<br />
more, this marked vitamin D deficiency has never been<br />
demonstrated in a study population <strong>of</strong> this size.<br />
Our study group included 60% <strong>of</strong> the cirrhotic patients<br />
who were seen at our clinic during 2005. This distribution<br />
does not introduce a selection bias because the<br />
vitamin D measurements were ordered without physician<br />
knowledge <strong>of</strong> the study purpose. Because the intensity<br />
<strong>of</strong> sunlight changes throughout the year, there might<br />
have been a seasonal difference in the vitamin D levels<br />
according to when the blood samples were drawn. However,<br />
patients were recruited throughout the year in both<br />
groups, and therefore, seasonal changes should not affect<br />
comparisons between the two groups.<br />
The observed deficiency in vitamin D might be related<br />
to several causes: an impaired hepatic hydroxylation <strong>of</strong><br />
vitamin D, dietary insufficiency, malabsorption, reduced<br />
hepatic production <strong>of</strong> vitamin D binding protein, and<br />
an impaired cutaneous production due to either reduced<br />
exposure to sunlight or jaundice [9,13] . The observation that<br />
the deficiency was less pronounced in PBC patients suggests<br />
that bile acid-related lipid malabsorption is not the<br />
only mechanism involved in vitamin D deficiency. It seems<br />
plausible that the mechanism <strong>of</strong> vitamin D deficiency is<br />
multifactorial and differs between the two groups <strong>of</strong> cirrhotic<br />
patients. When the results were stratified according<br />
to the Child-Pugh class, an association was observed<br />
between vitamin D deficiency and the severity <strong>of</strong> liver<br />
disease. This association has never been demonstrated in<br />
such a large study population. Thus, the better preservation<br />
<strong>of</strong> vitamin D status in patients with PBC might be<br />
ascribed to the diminished severity <strong>of</strong> their liver disease, as<br />
assessed by their Child-Pugh scores. Based on this finding,<br />
one could hypothesise that the risk for vitamin D deficiency<br />
or insufficiency might be influenced more by the degree<br />
<strong>of</strong> liver dysfunction than by the aetiology <strong>of</strong> the liver disease.<br />
However, our study was not designed to elucidate the<br />
exact mechanism underlying the vitamin D deficiency. The<br />
purpose <strong>of</strong> the study was to emphasise the importance <strong>of</strong><br />
monitoring the vitamin D status in all patients with cirrhosis,<br />
especially those with ALC for whom nutritional status<br />
has been a relatively neglected area <strong>of</strong> study.<br />
Our results imply that vitamin D deficiency is highly<br />
prevalent in patients with ALC. Because this was a retrospective<br />
study, we cannot extrapolate the results to the<br />
general population <strong>of</strong> cirrhotic patients. However, these<br />
results indicate that the frequency and severity <strong>of</strong> vitamin<br />
D deficiency in ALC patients warrant greater attention,<br />
similar to the usual clinical practice in patients with PBC.<br />
Although 17 <strong>of</strong> the study patients received vitamin D<br />
supplementation, this supplementation was clearly insufficient,<br />
as their vitamin D concentrations remained low.<br />
Thus, it appears that the vitamin D deficiency in these<br />
patients should be treated with higher doses <strong>of</strong> vitamin D<br />
than that used in standard clinical practice for repletion.<br />
The risk for bone disease in cirrhotic patients justifies<br />
the use <strong>of</strong> routine vitamin D therapy. Furthermore,<br />
the patients might also benefit from correction <strong>of</strong> their<br />
WJG|www.wjgnet.com<br />
vitamin D status with respect to reduced muscle function,<br />
<strong>cancer</strong> risk, and immune impairment.<br />
COMMENTS<br />
Background<br />
Patients with liver cirrhosis have an increased incidence <strong>of</strong> <strong>cancer</strong>, infections,<br />
osteoporosis, and decreased muscle strength. Vitamin D deficiency is associated<br />
with these complications in other patient groups and could be partially<br />
involved in the clinical complications related to cirrhosis.<br />
Research frontiers<br />
Vitamin D deficiency is a well reported complication in chronic cholestatic liver<br />
disease such as primary biliary cirrhosis. While the prevalence and treatment <strong>of</strong><br />
this deficiency has been addressed in many articles over the last decades, little<br />
is known <strong>of</strong> the vitamin D status in alcoholic liver cirrhosis.<br />
Innovations and breakthroughs<br />
Recent studies imply that vitamin D deficiency is frequent in all patients with<br />
cirrhosis. The current study shows that vitamin D deficiency is more frequent<br />
and severe in patients with alcoholic liver cirrhosis than in patients with primary<br />
biliary cirrhosis. Furthermore, it indicates that the degree <strong>of</strong> liver dysfunction,<br />
rather than the aetiology <strong>of</strong> cirrhosis, dictates the risk <strong>of</strong> vitamin D deficiency.<br />
Applications<br />
This study emphasizes the importance <strong>of</strong> monitoring vitamin D levels in all<br />
patients with cirrhosis. However, further studies are needed to find the most<br />
favourable form <strong>of</strong> vitamin D supplementation for these patients.<br />
Terminology<br />
Primary biliary cirrhosis and alcoholic cirrhosis are two different diseases that<br />
cause cirrhosis <strong>of</strong> the liver. While primary biliary cirrhosis is a cholestatic, autoimmune<br />
disease, alcoholic liver cirrhosis is an alcohol-induced liver disease usually<br />
without cholestatic features. The Child-Pugh score assesses the prognosis in patients<br />
with cirrhosis and is also used to quantitate the degree <strong>of</strong> liver dysfunction.<br />
Peer review<br />
This brief article nicely demonstrated the association <strong>of</strong> the liver damage severity<br />
with the level <strong>of</strong> 25-hydroxy vitamin D. This is a very important report, as many<br />
doctors do not realize that liver damage could cause significant vitamin D deficiency.<br />
REFERENCES<br />
1 Ormarsdóttir S, Ljunggren O, Mallmin H, Michaëlsson K,<br />
Lööf L. Increased rate <strong>of</strong> bone loss at the femoral neck in<br />
patients with chronic liver disease. Eur J Gastroenterol Hepatol<br />
2002; 14: 43-48<br />
2 Sorensen HT, Friis S, Olsen JH, Thulstrup AM, Mellemkjaer<br />
L, Linet M, Trichopoulos D, Vilstrup H, Olsen J. Risk <strong>of</strong> liver<br />
and other types <strong>of</strong> <strong>cancer</strong> in patients with cirrhosis: a nationwide<br />
cohort study in Denmark. Hepatology 1998; 28: 921-925<br />
3 Wasmuth HE, Kunz D, Yagmur E, Timmer-Stranghöner<br />
A, Vidacek D, Siewert E, Bach J, Geier A, Purucker EA,<br />
Gressner AM, Matern S, Lammert F. Patients with acute on<br />
chronic liver failure display "sepsis-like" immune paralysis. J<br />
Hepatol 2005; 42: 195-201<br />
4 Glerup H, Mikkelsen K, Poulsen L, Hass E, Overbeck S,<br />
Andersen H, Charles P, Eriksen EF. Hypovitaminosis D<br />
myopathy without biochemical signs <strong>of</strong> osteomalacic bone<br />
involvement. Calcif Tissue Int 2000; 66: 419-424<br />
5 Holick MF. Sunlight and vitamin D for bone health and<br />
prevention <strong>of</strong> autoimmune diseases, <strong>cancer</strong>s, and cardiovascular<br />
disease. Am J Clin Nutr 2004; 80: 1678S-1688S<br />
6 Lappe JM, Travers-Gustafson D, Davies KM, Recker RR, Heaney<br />
RP. Vitamin D and calcium supplementation reduces<br />
<strong>cancer</strong> risk: results <strong>of</strong> a randomized trial. Am J Clin Nutr<br />
2007; 85: 1586-1591<br />
7 Reed JS, Meredith SC, Nemchausky BA, Rosenberg IH,<br />
Boyer JL. Bone disease in primary biliary cirrhosis: reversal<br />
924 February 21, 2011|Volume 17|Issue 7|
<strong>of</strong> osteomalacia with oral 25-hydroxyvitamin D. Gastroenterology<br />
1980; 78: 512-517<br />
8 Crawford BA, Kam C, Donaghy AJ, McCaughan GW. The<br />
heterogeneity <strong>of</strong> bone disease in cirrhosis: a multivariate<br />
analysis. Osteoporos Int 2003; 14: 987-994<br />
9 Fisher L, Fisher A. Vitamin D and parathyroid hormone in<br />
outpatients with noncholestatic chronic liver disease. Clin<br />
Gastroenterol Hepatol 2007; 5: 513-520<br />
10 Crawford BA, Labio ED, Strasser SI, McCaughan GW. Vitamin<br />
D replacement for cirrhosis-related bone disease. Nat<br />
WJG|www.wjgnet.com<br />
Malham M et al . Vitamin D deficiency in liver cirrhosis<br />
Clin Pract Gastroenterol Hepatol 2006; 3: 689-699<br />
11 Lips P. Which circulating level <strong>of</strong> 25-hydroxyvitamin D is<br />
appropriate? J Steroid Biochem Mol Biol 2004; 89-90: 611-614<br />
12 Maunsell Z, Wright DJ, Rainbow SJ. Routine isotope-dilution<br />
liquid chromatography-tandem mass spectrometry assay for<br />
simultaneous measurement <strong>of</strong> the 25-hydroxy metabolites <strong>of</strong><br />
vitamins D2 and D3. Clin Chem 2005; 51: 1683-1690<br />
13 Pappa HM, Bern E, Kamin D, Grand RJ. Vitamin D status<br />
in gastrointestinal and liver disease. Curr Opin Gastroenterol<br />
2008; 24: 176-183<br />
S- Editor Sun H L- Editor Webster JR E- Editor Lin YP<br />
925 February 21, 2011|Volume 17|Issue 7|
Online Submissions: http://www.wjgnet.com/1007-9327<strong>of</strong>fice<br />
wjg@wjgnet.com<br />
doi:10.3748/wjg.v17.i7.926<br />
BRIEF ARTICLE<br />
Natural orifice transluminal endoscopic wedge hepatic<br />
resection with a water-jet hybrid knife in a non-survival<br />
porcine model<br />
Hong Shi, Sheng-Jun Jiang, Bin Li, Deng-Ke Fu, Pei Xin, Yong-Guang Wang<br />
Hong Shi, Bin Li, Pei Xin, Yong-Guang Wang, Institute <strong>of</strong><br />
Minimally Invasive Medicine, Tongji University, Shanghai<br />
200092, China<br />
Hong Shi, Sheng-Jun Jiang, Bin Li, Deng-Ke Fu, Pei Xin,<br />
Yong-Guang Wang, Department <strong>of</strong> Minimally Invasive Surgery,<br />
Beijing Chuiyangliu Hospital, Beijing 100022, China<br />
Author contributions: Shi H, Jiang SJ and Wang YG designed<br />
the study; Shi H wrote the first draft <strong>of</strong> the paper; all the authors<br />
contributed to the design and interpretation <strong>of</strong> the study and to<br />
the final manuscript.<br />
Correspondence to: Yong-Guang Wang, MD, PhD, Department<br />
<strong>of</strong> Minimally Invasive Surgery, Beijing Chuiyangliu Hospital,<br />
No. 2, Chuiyangliu South Street, Chaoyang District, Beijing<br />
100022, China. endowang@vip.sina.com<br />
Telephone: +86-10-67718822 Fax: +86-10-67711960<br />
Received: October 6, 2010 Revised: November 17, 2010<br />
Accepted: November 24, 2010<br />
Published online: February 21, 2011<br />
Abstract<br />
AIM: To explore the feasibility <strong>of</strong> a water-jet hybrid<br />
knife to facilitate wedge hepatic resection using a<br />
natural orifice transluminal endoscopic surgery (NOTES)<br />
approach in a non-survival porcine model.<br />
METHODS: The Erbe Jet2 water-jet system allows a<br />
needleless, tissue-selective hydro-dissection with a preselected<br />
pressure. Using this system, wedge hepatic<br />
resection was performed through three natural routes<br />
(trans-anal, trans-vaginal and trans-umbilical) in three female<br />
pigs weighing 35 kg under general anesthesia. Entry<br />
into the peritoneal cavity was via a 15-mm incision using<br />
a hook knife. The targeted liver segment was marked<br />
by an APC probe, followed by wedge hepatic resection<br />
performed using a water-jet hybrid knife with the aid <strong>of</strong><br />
a 4-mm transparent distance s<strong>of</strong>t cap mounted onto the<br />
tip <strong>of</strong> the endoscope for holding up the desired plane.<br />
The exposed vascular and ductal structures were clipped<br />
with Endoclips. Hemostasis was applied to the bleeding<br />
WJG|www.wjgnet.com<br />
926<br />
<strong>World</strong> J Gastroenterol 2011 February 21; 17(7): 926-931<br />
ISSN 1007-9327 (print) ISSN 2219-2840 (online)<br />
© 2011 Baishideng. All rights reserved.<br />
cut edges <strong>of</strong> the liver parenchyma by electrocautery. After<br />
the procedure, the incision site was left open, and the<br />
animal was euthanized followed by necropsy.<br />
RESULTS: Using the Erbe Jet2 water-jet system, transanal<br />
and trans-vaginal wedge hepatic resection was successfully<br />
performed in two pigs without laparoscopic assistance.<br />
Trans-umbilical attempt failed due to an unstable<br />
operating platform. The incision for peritoneal entry took<br />
1 min, and about 2 h was spent on excision <strong>of</strong> the liver<br />
tissue. The intra-operative blood loss ranged from 100 to<br />
250 mL. Microscopically, the hydro-dissections were relatively<br />
precise and gentle, preserving most vessels.<br />
CONCLUSION: The Erbe Jet2 water-jet system can<br />
safely accomplish non-anatomic wedge hepatic resection<br />
in NOTES, which deserves further studies to shorten<br />
the dissection time.<br />
© 2011 Baishideng. All rights reserved.<br />
Key words: Natural orifice transluminal endoscopic surgery;<br />
Hepatic resection; Water-jet; Hybrid knife; Triangulation<br />
Peer reviewer: Chih-Chi Wang, MD, Department <strong>of</strong> Surgery,<br />
Chang Gung Memorial Hospital-Kaohsiung Medical Center,<br />
123 Ta-Pei Road, Niao-Sung, Kaohsiung 833, Taiwan, China<br />
Shi H, Jiang SJ, Li B, Fu DK, Xin P, Wang YG. Natural orifice<br />
transluminal endoscopic wedge hepatic resection with a water-jet<br />
hybrid knife in a non-survival porcine model. <strong>World</strong> J Gastroenterol<br />
2011; 17(7): 926-931 Available from: URL: http://www.<br />
wjgnet.com/1007-9327/full/v17/i7/926.htm DOI: http://dx.doi.<br />
org/10.3748/wjg.v17.i7.926<br />
INTRODUCTION<br />
Liver resection, a surgical procedure consisting <strong>of</strong> he-<br />
February 21, 2011|Volume 17|Issue 7|
patic parenchymal dissection as well as precise identification<br />
followed by control <strong>of</strong> intra/extra-hepatic vascular<br />
and biliary anatomy, is technically challenging due to the<br />
risk <strong>of</strong> massive bleeding during operation. Since excessive<br />
hemorrhage and subsequent blood transfusion are<br />
strongly associated with increased peri-operative morbidity<br />
and mortality, technical innovations have mainly focused<br />
on minimizing blood loss [1] . Besides inflow occlusion<br />
and low central pressure used to prevent bleeding<br />
from inflow vessels and hepatic veins in the transaction<br />
surface since the early 20th century, the development <strong>of</strong><br />
specific devices for separating hepatic parenchyma, such<br />
as the ultrasonic dissector, water jet, Harmonic scalpel,<br />
Ligasure, and Tissue-Link dissecting sealer, has also<br />
contributed to bloodless transection. A meta-analysis [2]<br />
assessing the benefits and risks <strong>of</strong> current techniques <strong>of</strong><br />
parenchymal transection showed that there were no significant<br />
differences in terms <strong>of</strong> the mortality, morbidity,<br />
markers <strong>of</strong> liver parenchymal injury or liver dysfunction<br />
in pairwise comparisons including cavitron ultrasound<br />
surgical aspirator, radi<strong>of</strong>requency dissecting sealer, sharp<br />
dissection and hydro-jet. Among them, the water-jet dissector<br />
employs a pressurized jet <strong>of</strong> water to fragment the<br />
liver parenchyma tissue, with intact vascular and ductal<br />
structures, which can be ligated with staplers or clipped<br />
with titanium hemoclips, resulting in reduced blood loss,<br />
transfusion requirement, and biliary leak [3] .<br />
High-pressure water-jet dissection technology was<br />
originally developed in the steel and glass industries,<br />
where ultra-precise cutting and engraving were considered<br />
as pr<strong>of</strong>essional demands [4] . Since introduced to<br />
medical application in 1982 [5] , this technology (Hydro-<br />
Jet ® ; ERBE, Tuebingen, Germany) has been successfully<br />
employed in open and laparoscopic operations, achieving<br />
favorable results in precise, controllable tissue-selective<br />
(indicating water-rich tissue such as liver parenchyma)<br />
dissection with excellent visualization and minimal injury<br />
to the surrounding fibrous structures (such as ductal and<br />
vessel systems with a high content <strong>of</strong> collagen and elastin)<br />
[6] . The above-mentioned Helix Hydro-Jet device with<br />
a rigid hand-held applicator is not designed with sufficient<br />
flexibility for natural orifice transluminal endoscopic<br />
surgery (NOTES) procedures, and can not be passed<br />
through a standard working channel <strong>of</strong> the current flexible<br />
endoscope because its outer-diameter is larger than<br />
the endoscopic operative channel. Now a new water-jet<br />
hybrid knife [7] incorporating with high-pressure water-jet<br />
and radi<strong>of</strong>requency may overcome this drawback. It has<br />
a smaller size, being easy to handle, and showing more<br />
preciseness, with almost linear correlation <strong>of</strong> pressure<br />
and dissection depth, and less foaming compared with<br />
the precursor model Helix Hydro-Jet [5] .<br />
As is known, trans-luminal liver resection is technically<br />
demanding and its expansion has been lagged behind<br />
other NOTES procedures. Phee et al [8] demonstrated for<br />
the first time how a dexterous master and slave transluminal<br />
endoscopic robot could efficiently perform the<br />
wedge hepatic resection without laparoscopic assistance.<br />
Unfortunately, this technology is still an unexplored field<br />
WJG|www.wjgnet.com<br />
Shi H et al . Water-jet system in NOTES liver resection<br />
in China. The aim <strong>of</strong> our study was to explore the safety<br />
and efficacy <strong>of</strong> a water-jet hybrid knife to facilitate wedge<br />
hepatic resection using a NOTES approach in a nonsurvival<br />
porcine model.<br />
MATERIALS AND METHODS<br />
Experimental design<br />
This non-survival study evaluated the performance <strong>of</strong><br />
the water-jet hybrid knife during NOTES procedure in<br />
a live porcine model. A pilot experiment in an isolated<br />
liver was conducted first, and followed by an open procedure<br />
in a 35-kg female porcine model. The formal<br />
study included three operations <strong>of</strong> wedge hepatic resection<br />
using NOTES and water-jet technology through<br />
three respective natural routes (trans-anal, trans-vaginal<br />
and trans-umbilical). The outcome measures were the<br />
time spent in performing a trans-visceral incision, the<br />
time spent in excising the liver segment, and the blood<br />
loss including oozing and brisk vascular hemorrhage, determined<br />
as blood accumulation in the suction device.<br />
This study was conducted with prior approval by the<br />
Institutional Animal Care and Use Committee <strong>of</strong> Tongji<br />
University <strong>of</strong> China.<br />
Experimental animal and instrument<br />
Transluminal hepatic wedge hydro-dissection was performed<br />
in three 35-kg female pigs. The pigs were food<br />
deprived but allowed liquids for 24 h before the procedure.<br />
Urethral catheterization and warm saline enema<br />
were conducted immediately before surgery. The animals<br />
were then transferred to an operating table, and placed<br />
in supine position.<br />
The water-jet hybrid knife (Erbe Elektromedizin) used<br />
in this study is a stainless-steel tube that incorporates a<br />
microcapillary with a diameter <strong>of</strong> 150 mm [7] . The flexible<br />
instrument has an outer diameter <strong>of</strong> 2.1 mm and a length<br />
<strong>of</strong> 2.20 mm so that it can pass through the operating<br />
channels (diameter, 2.8 and 3.7 mm) <strong>of</strong> a forward-viewing<br />
dual-channel therapeutic endoscope (GIF-2T160; Olympus<br />
Medical Systems Corporation, Tokyo, Japan). The hybrid<br />
knife can be used for hydro-dissection, rinsing blood<br />
clot and rinsing for a better endoscopic view by waterjet<br />
application, as well as coagulation by radi<strong>of</strong>requency<br />
application. The foaming with the use <strong>of</strong> the hybridknife<br />
can be scavenged by the suction mechanism <strong>of</strong> the<br />
endoscope. In NOTES procedure, a 4-mm transparent<br />
distance s<strong>of</strong>t cap was mounted onto the tip <strong>of</strong> the endoscope<br />
for holding up the desired surface, subsequently<br />
avoiding the deviation in the direction <strong>of</strong> the water-jet.<br />
However, it was not used in the previous open procedure,<br />
because distraction (with surgical retractors) could allow<br />
the water-jet hybrid knife to effectively dissect the tissue<br />
by exposing the base <strong>of</strong> the cutting plane.<br />
Rau et al [6] found that a pressure <strong>of</strong> 30-40 bar was very<br />
effective to dissect normal human liver tissues, and the<br />
long-distance transmission attenuation was about 10%.<br />
Therefore, we set the pressure at 45 bar, which was proved<br />
to be effective in our pilot experiment and open operation.<br />
927 February 21, 2011|Volume 17|Issue 7|
Shi H et al . Water-jet system in NOTES liver resection<br />
Figure 1 Colostomy on anterior wall <strong>of</strong> <strong>rectal</strong> junction and sigmoid colon.<br />
At the beginning <strong>of</strong> trans-annual natural orifice transluminal endoscopic surgery<br />
procedure, entry into the peritoneal cavity was via a 15-mm linear incision using<br />
the hook knife (cutting width set at 6 units and cutting interval set at 1 unit). The<br />
ideal access point was the junction <strong>of</strong> rectum and sigmoid colon at a distance <strong>of</strong><br />
15-20 cm away from the anus.<br />
Figure 2 Hydro-dissection <strong>of</strong> liver segment in natural orifice transluminal<br />
endoscopic surgery procedure. Hepatic parenchyma dissection was performed<br />
using the water-jet hybrid knife kept away from the tissue in a no-touch<br />
fashion and perpendicular to but not tangentially against the predetermined<br />
surface, keeping in a smooth, reproducible, back-and-forth waving motion. A<br />
4-mm transparent distance s<strong>of</strong>t cap was mounted onto the tip <strong>of</strong> the endoscope<br />
for holding up the desired surface, subsequently avoiding the deviation in the<br />
direction <strong>of</strong> the water-jet.<br />
Other instruments used were as follows: a flexible sterile<br />
overtube (MD48618, Sumitomo Bakelite, Tokyo, Japan),<br />
a transparent distance flat s<strong>of</strong>t cap (D-201-13404, Olympus),<br />
a hook knife (KD-620LR, Olympus), endoscopic hemostatic<br />
forceps (FD-410LR, Olympus), endoclips (HX-<br />
610-135L OLYMPUS, Olympus), a foreign forcep (FQ-<br />
46L-1, Olympus), APC probe (argon plasma coagulation,<br />
APC) (ERBE Elektromedizin), and the modular VIO<br />
generator (VIO 300D; Erbe Elektromedizin, Tubingen,<br />
Germany).<br />
Experimental procedure<br />
Anesthesia was induced with 5% is<strong>of</strong>lurane administered<br />
intravenously. The animal was then intubated with endoendotracheal<br />
tube, followed by general anesthesia with<br />
1%-2% is<strong>of</strong>lurane. Throughout the operation, oxygen<br />
was administered to the animal at a flow rate according<br />
to oxygen saturation, and both pulse rate and oxygen<br />
WJG|www.wjgnet.com<br />
Figure 3 Hydro-dissection <strong>of</strong> liver segment in open procedure. Hepatic parenchyma<br />
dissection was performed using the water-jet hybrid knife in a similar<br />
natural orifice transluminal endoscopic surgery procedure, except that the 4-mm<br />
transparent distance s<strong>of</strong>t cap was not used.<br />
saturation were monitored continuously using the pulse<br />
oximeter clamped to the animal tougue. Then normal<br />
saline enema was administered to each animal. Residual<br />
stool would be removed with aggressive washing, and<br />
suctioning during endoscopic inspection.<br />
At the beginning <strong>of</strong> the procedure, entry into the peritoneal<br />
cavity was via a 15-mm linear incision made by the<br />
hook knife (a cutting width was set at 6 units and cutting<br />
interval was set at 1 unit). The ideal access point was the<br />
abdominal site 1 cm away from the umbilicus in transumbilical<br />
route, the bottom <strong>of</strong> the vagina in trans-vaginal<br />
route, the junction <strong>of</strong> rectum and sigmoid colon at a distance<br />
<strong>of</strong> 15-20 cm away from the anus in trans-anal route<br />
(Figure 1). Then the endoscope with a 4-mm transparent<br />
distance s<strong>of</strong>t cap mounted onto the tip <strong>of</strong> the endoscope<br />
beforehand was passed through the access to reach the<br />
peritoneum using the air inflation mechanism <strong>of</strong> the endoscope.<br />
After the target liver segment was identified, hepatic<br />
parenchymal dissection with the water-jet hybrid knife was<br />
performed in the following steps (Figure 2), which were<br />
generally similar to those in the previous open operation<br />
except the assistance <strong>of</strong> manual retraction (Figure 3). The<br />
range to be separated was marked by an APC probe. The<br />
Glisson’s capsule was scored 2-3 mm deep along the demarcated<br />
plane <strong>of</strong> transaction with the hook knife. Then<br />
hepatic parenchyma dissection was performed using the<br />
water-jet hybrid knife kept away from the tissue in a notouch<br />
fashion. The tip <strong>of</strong> the knife was perpendicular to<br />
but not tangentially against the predetermined surface (this<br />
was achieved with a 4-mm transparent distance s<strong>of</strong>t cap<br />
mounted onto the tip <strong>of</strong> the endoscope for holding up<br />
the desired surface, subsequently avoiding the deviation<br />
in the direction <strong>of</strong> the water-jet). A smooth, reproducible,<br />
back-and-forth waving motion was used. Minor slow<br />
oozing from the cutting surface was controlled using the<br />
same knife, the hook knife or APC probe to initiate bursts<br />
<strong>of</strong> coagulation. Visible intra-hepatic vascular and ductal<br />
structures were clipped with endoscopic hemoclips. Once<br />
the liver segment was completely free and after checking<br />
for hemostasis, the incision was slightly enlarged, then an<br />
928 February 21, 2011|Volume 17|Issue 7|
Table 1 Comparisons <strong>of</strong> three routes for natural orifice transluminal endoscopic surgery procedure<br />
Items Trans-umbilical route Trans-anal route Trans-vaginal route<br />
Access position Visually inspected at para-umbilical region Verified by finger<br />
pressing<br />
endoscopic retrieval net was inserted through the endoscopic<br />
working channel and the specimen was introduced<br />
into the net and was retrieved intactly. After the procedure,<br />
the incision site was left open, and the animal was<br />
euthanized followed by necropsy.<br />
Histopathological examination<br />
Histologic examination was performed for all dissected<br />
specimens. The results were observed under microscope<br />
after hematoxylin and eosin staining based on the characteristics<br />
<strong>of</strong> the dissection margins, vessel preservation and<br />
dissection impact on the surrounding tissues. Thermal<br />
alterations such as edema and structural changes <strong>of</strong> different<br />
layers <strong>of</strong> the specimen were also microscopically<br />
analyzed.<br />
RESULTS<br />
It took 20 min to complete the excision <strong>of</strong> a liver segment<br />
50 mm × 30 mm × 10 mm in size during the pilot<br />
experiment, and 45 min to complete the excision <strong>of</strong> a<br />
liver segment 45 mm × 25 mm × 10 mm in size during<br />
the open procedure. The blood loss was 100 mL in the<br />
open operation.<br />
As for the NOTES procedure, using the Erbe Jet2 water-jet<br />
system, trans-anal and trans-vaginal wedge hepatic<br />
resections were successfully performed in two pigs without<br />
WJG|www.wjgnet.com<br />
laparoscopic assistance. Trans-umbilical attempt failed due<br />
to an unstable operating platform. Each incision for peritoneal<br />
entry took 1 min, and 2 h was spent on excision <strong>of</strong><br />
the liver tissue, indicating a hugely time-consuming part <strong>of</strong><br />
the entire procedure. There was neither hemodynamic nor<br />
pulmonary instability throughout the NOTES procedure,<br />
and target visualization within the peritoneum was always<br />
kept clear. No untoward incident such as injury to surrounding<br />
organs occurred, and the whole intra-operative<br />
blood loss ranged from 100 to 250 mL. Parenchymal<br />
bleeding from resection could be adequately controlled by<br />
electrocautery with the hybrid knife itself, the hook knife<br />
or the APC probe (Table 1, Figure 4). Since all the exposed<br />
ductal structures were successfully clipped with Endoclips,<br />
no bile leak from the remnant liver occurred.<br />
There were relatively smooth and precise cutting margins<br />
in all histological preparations. The cutting width at<br />
the bottom <strong>of</strong> the cut was similar to the dissection width<br />
at tissue surface, with little vessel damage (Figure 5). Some<br />
thermal alterations were obtained due to intra-operative<br />
electrocautery (Figure 6).<br />
DISCUSSION<br />
Located by surrounding anatomic<br />
landmarks<br />
Time to complete a trans-visceral incision About 1 min<br />
Time to reach peritoneum About 2 min<br />
Liver exposure Antero-lateral segments could be easily detected, while posterosuperior segments were hard to be explored<br />
Working platform Unstable Relatively stable<br />
Time to hydro-dissection Abandoned 1 h later 2 h 2 h and 40 min<br />
Size <strong>of</strong> resected liver segment No resected specimen was obtained due to<br />
failure in trans-umbilical hepatic resection<br />
50 mm × 25 mm ×<br />
5 mm<br />
45 mm × 30 mm × 7 mm<br />
Bile leak Not found<br />
Blood loss 100 mL 200 mL 250 mL<br />
Injury to surrounding organs Not occurred<br />
Figure 4 A resected liver segment compared with the reserved part. A<br />
resected liver segment was picked out with white gauze.<br />
Shi H et al . Water-jet system in NOTES liver resection<br />
Figure 5 Microscopic findings <strong>of</strong> water-jet dissection in liver tissues (HE<br />
stain, × 40). A smooth and gentle cutting margin was presented. The cutting<br />
width at the bottom <strong>of</strong> the cut was similar to the dissection width at tissue surface,<br />
with little vessel damage.<br />
To the best <strong>of</strong> our knowledge, this is the first study in<br />
929 February 21, 2011|Volume 17|Issue 7|
Shi H et al . Water-jet system in NOTES liver resection<br />
Figure 6 Thermal alterations due to intra-operative coagulation (HE stain,<br />
× 100). Removal <strong>of</strong> the liver capsule could be seen in an example <strong>of</strong> thermal<br />
damage.<br />
a non-survival porcine model evaluating the feasibility<br />
and safety <strong>of</strong> wedge hepatic resection merely using a<br />
NOTES approach, Erbe Jet2 water-jet technology and<br />
endoscopic instrument.<br />
Since first described by Kalloo et al [9] , natural orifice<br />
transluminal endoscopic surgery (NOTES) has become<br />
the newest minimally invasive surgical procedure in contrast<br />
to open and laparoscopic technology. It involves<br />
passing flexible endoscopic systems through natural orifices<br />
(per-oral, trans-vaginal, trans-anal, trans-umbilical or<br />
trans-vesical routes), approaching target organs and performing<br />
intra-abdominal procedures. For the entry into<br />
the peritoneal cavity, a trans-luminal incision is mostly created<br />
by endoscopic needle knife followed by balloon dilation.<br />
However, in our study, it was achieved just in about<br />
1 min via a hook knife, with the same desirable effect. The<br />
air-inflation mechanism <strong>of</strong> the endoscope was used to<br />
induce and maintain peritoneum, and the suction mechanism<br />
<strong>of</strong> the endoscope was used intermittently to avoid a<br />
high intra-abdominal pressure. Overall, there was neither<br />
hemodynamic nor pulmonary instability during NOTES,<br />
as described elsewhere [10] .<br />
Similar to laparoscopic liver resection, NOTES hepatic<br />
procedures must confront one and the same Achilles’<br />
heel, difficulty in obtaining hemostasis. Given the facts<br />
that protection <strong>of</strong> blood vessels is essential to minimize<br />
hemorrhage and blood transfusion, and smooth dissection<br />
margins might minimize adhesion formation [11] , the waterjet<br />
hybrid knife was taken into consideration. Hydro-dissection<br />
was accomplished with the hybrid knife kept away<br />
from the tissue in a no-touch fashion and perpendicular<br />
to but not tangentially against the predetermined surface.<br />
Minor slow oozing from the cutting surface was controlled<br />
using the same knife, the hook knife or APC probe<br />
to initiate bursts <strong>of</strong> coagulation. Visible intra-hepatic vascular<br />
and ductal structures were clipped with endoscopic<br />
hemoclip. Certainly, the need for coagulation or clipping<br />
<strong>of</strong> individual vessels led to a prolonged operative time.<br />
Current flexible endoscopes have significant limitations<br />
when used for complex therapeutic procedures. Stable<br />
platform and <strong>of</strong>f-axis operation are <strong>of</strong>ten necessary for<br />
the NOTES. However, standard endoscopic shafts are too<br />
WJG|www.wjgnet.com<br />
flexible and prone to looping, if these unfavorable factors<br />
caused the failure in transumbilical endoscopic hepatic<br />
resection. As for triangulation <strong>of</strong> endoscopically deployed<br />
instruments to approach the same target, internal double<br />
channels are small and in close proximity, producing parallelism<br />
and limiting possible triangulating interactions [12] .<br />
The operator interface parallelism does not allow satisfactory<br />
traction/countertraction for effective dissection <strong>of</strong><br />
tissue and organs. To counteract the negative impact on<br />
dissection efficiency, a 4-mm transparent distance s<strong>of</strong>t cap<br />
was mounted onto the tip <strong>of</strong> the endoscope for holding<br />
up the desired plane, subsequently avoiding the deviation<br />
in the direction <strong>of</strong> the water-jet. Unfortunately, its<br />
effect was limited due to the heavy weight <strong>of</strong> the porcine<br />
liver and the restricted field <strong>of</strong> view. As a result, excision<br />
<strong>of</strong> one piece <strong>of</strong> the same size from the porcine liver was<br />
more difficult in NOTES than in open procedure (more<br />
than 2 h was spent in NOTES, but only 45 min spent in<br />
open procedure).<br />
Notably, non-anatomic wedge hepatic resection by a<br />
NOTES approach in either our or Phee’s [8] study is still at<br />
a primary <strong>stage</strong>. As NOTES using current endoscopic instruments<br />
is technically difficult to realize pedicle control<br />
with an intrahepatic Glissonian approach [13] , it is suitable<br />
only for superficial lesions <strong>of</strong> the liver mostly with the fine<br />
trabecular infrastructures and medium caliber structures.<br />
In order to achieve the same level <strong>of</strong> segment-based laparoscopic<br />
liver resection [14] , advance in NOTES technology<br />
still has a long way to go.<br />
In conclusion, the water-jet hybrid knife with the capacity<br />
<strong>of</strong> selective vessel-sparing tissue dissection can<br />
safely accomplish non-anatomic wedge hepatic resection<br />
through a NOTES approach. At the same time, its efficiency<br />
may be discounted by endoscopic deficiencies: lack<br />
<strong>of</strong> surgical triangulation, unstable operating platform as<br />
well as transmission attenuation caused by long distance<br />
and endoscopic looping. Although this technology is only<br />
at its beginning <strong>stage</strong>, as the old saying goes: well begun is<br />
half done.<br />
ACKNOWLEDGMENTS<br />
We thank Dr. Jiang-Fan Zhu for his editorial assistance.<br />
COMMENTS<br />
Background<br />
Liver resection is technically challenging due to the risk <strong>of</strong> massive bleeding<br />
during operation. Since the early 20th century, the development <strong>of</strong> specific<br />
devices for separating hepatic parenchyma has contributed to bloodless transection.<br />
Furthermore, trans-luminal liver resection is technically demanding and<br />
its expansion has been lagged behind other natural orifice transluminal endoscopic<br />
surgery (NOTES) procedures.<br />
Research frontiers<br />
Phee described for the first time how a dexterous master and slave transluminal<br />
endoscopic robot could efficiently perform the wedge hepatic resection without<br />
laparoscopic assistance. This technology is still an unexplored field in China.<br />
Innovations and breakthroughs<br />
This is the first study to evaluate the feasibility and safety <strong>of</strong> non-anatomic<br />
wedge hepatic resection in a non-survival porcine model using a NOTES<br />
approach, Erbe Jet2 water-jet technology and endoscopic instruments. The<br />
930 February 21, 2011|Volume 17|Issue 7|
study demonstrated that the water-jet hybrid knife with the capacity <strong>of</strong> selective<br />
vessel-sparing tissue dissection can safely accomplish non-anatomic wedge<br />
hepatic resection through a NOTES approach.<br />
Applications<br />
Currently, non-anatomic wedge hepatic resection using NOTES approach and<br />
water-jet technology is suitable only for superficial lesions <strong>of</strong> the liver mostly<br />
with the fine trabecular infrastructures and medium caliber structures.<br />
Terminology<br />
High-pressure water-jet dissection technology was originally developed in the<br />
steel and glass industries, where ultra-precise cutting and engraving were<br />
considered as pr<strong>of</strong>essional demands [4] . Since introduced to medical application<br />
in 1982 [5] , this technology has been successfully employed in open and<br />
laparoscopic operations, achieving favorable results in precise, controllable<br />
tissue-selective dissection with excellent visualization and minimal injury to the<br />
surrounding fibrous structures (such as ductal and vessel systems with a high<br />
content <strong>of</strong> collagen and elastin).<br />
Peer review<br />
This is the study in a non-survival porcine model evaluating the feasibility and<br />
safety <strong>of</strong> wedge hepatic resection by using pure NOTES approach.<br />
REFERENCES<br />
1 Lesurtel M, Belghiti J. Open hepatic parenchymal transection<br />
using ultrasonic dissection and bipolar coagulation.<br />
HPB (Oxford) 2008; 10: 265-270<br />
2 Gurusamy KS, Pamecha V, Sharma D, Davidson BR. Techniques<br />
for liver parenchymal transection in liver resection.<br />
Cochrane Database Syst Rev 2009; CD006880<br />
3 Rau HG, Wichmann MW, Schinkel S, Buttler E, Pickelmann S,<br />
Schauer R, Schildberg FW. [Surgical techniques in hepatic resections:<br />
Ultrasonic aspirator versus Jet-Cutter. A prospective<br />
randomized clinical trial]. Zentralbl Chir 2001; 126: 586-590<br />
4 Vollmer CM, Dixon E, Sahajpal A, Cattral MS, Grant DR,<br />
Gallinger S, Taylor BR, Greig PD. Water-jet dissection for<br />
parenchymal division during hepatectomy. HPB (Oxford)<br />
2006; 8: 377-385<br />
5 Tschan CA, Tschan K, Krauss JK, Oertel J. First experimental<br />
results with a new waterjet dissector: Erbejet 2. Acta Neurochir<br />
(Wien) 2009; 151: 1473-1482<br />
WJG|www.wjgnet.com<br />
Shi H et al . Water-jet system in NOTES liver resection<br />
6 Rau HG, Duessel AP, Wurzbacher S. The use <strong>of</strong> water-jet<br />
dissection in open and laparoscopic liver resection. HPB<br />
(Oxford) 2008; 10: 275-280<br />
7 Neuhaus H, Wirths K, Schenk M, Enderle MD, Schumacher<br />
B. Randomized controlled study <strong>of</strong> EMR versus endoscopic<br />
submucosal dissection with a water-jet hybrid-knife <strong>of</strong><br />
esophageal lesions in a porcine model. Gastrointest Endosc<br />
2009; 70: 112-120<br />
8 Phee SJ, Ho KY, Lomanto D, Low SC, Huynh VA, Kencana<br />
AP, Yang K, Sun ZL, Chung SC. Natural orifice transgastric<br />
endoscopic wedge hepatic resection in an experimental model<br />
using an intuitively controlled master and slave transluminal<br />
endoscopic robot (MASTER). Surg Endosc 2010; 24: 2293-2298<br />
9 Kalloo AN, Singh VK, Jagannath SB, Niiyama H, Hill SL,<br />
Vaughn CA, Magee CA, Kantsevoy SV. Flexible transgastric<br />
peritoneoscopy: a novel approach to diagnostic and therapeutic<br />
interventions in the peritoneal cavity. Gastrointest<br />
Endosc 2004; 60: 114-117<br />
10 von Delius S, Sager J, Feussner H, Wilhelm D, Thies P,<br />
Huber W, Schuster T, Schneider A, Schmid RM, Meining A.<br />
Carbon dioxide versus room air for natural orifice transluminal<br />
endoscopic surgery (NOTES) and comparison with<br />
standard laparoscopic pneumoperitoneum. Gastrointest Endosc<br />
2010; 72: 161-169, 169.e1-2<br />
11 Dubcenco E, Grantcharov T, Streutker C. A pilot study in a<br />
survival Porcine model evaluating the feasibility and safety<br />
<strong>of</strong> adhesiolysis by using transgastric NOTES® approach,<br />
waterjet technology and endoscopic instruments. Gastrointest<br />
Endosc 2010; 71: AB198<br />
12 Thompson CC, Ryou M, Soper NJ, Hungess ES, Rothstein<br />
RI, Swanstrom LL. Evaluation <strong>of</strong> a manually driven, multitasking<br />
platform for complex endoluminal and natural<br />
orifice transluminal endoscopic surgery applications (with<br />
video). Gastrointest Endosc 2009; 70: 121-125<br />
13 Machado MA, Makdissi FF, Galvão FH, Machado MC.<br />
Intrahepatic Glissonian approach for laparoscopic right segmental<br />
liver resections. Am J Surg 2008; 196: e38-e42<br />
14 Yoon YS, Han HS, Cho JY, Ahn KS. Total laparoscopic liver<br />
resection for hepatocellular carcinoma located in all segments<br />
<strong>of</strong> the liver. Surg Endosc 2010; 24: 1630-1637<br />
S- Editor Tian L L- Editor Ma JY E- Editor Ma WH<br />
931 February 21, 2011|Volume 17|Issue 7|
Online Submissions: http://www.wjgnet.com/1007-9327<strong>of</strong>fice<br />
wjg@wjgnet.com<br />
doi:10.3748/wjg.v17.i7.932<br />
BRIEF ARTICLE<br />
Upregulated CD133 expression in tumorigenesis <strong>of</strong> colon<br />
<strong>cancer</strong> cells<br />
Zhi-Li Yang, Qi Zheng, Jun Yan, Ye Pan, Zhi-Gang Wang<br />
Zhi-Li Yang, Qi Zheng, Jun Yan, Ye Pan, Zhi-Gang Wang,<br />
Department <strong>of</strong> Surgery, Affiliated Sixth People’s Hospital <strong>of</strong><br />
Shanghai Jiao Tong University, Shanghai 200233, China<br />
Author contributions: Yang ZL analyzed the CD133 expression<br />
in a panel <strong>of</strong> colon <strong>cancer</strong> cell lines and spheroid culture<br />
and drafted the manuscript; Zheng Q, Yan J and Pan Y participated<br />
in the study design and performed the RT-qPCR analysis;<br />
Wang ZG conceived the study and revised the manuscript.<br />
Correspondence to: Zhi-Gang Wang, MD, Assistant Pr<strong>of</strong>essor,<br />
Department <strong>of</strong> Surgery, Affiliated Sixth People’s Hospital<br />
<strong>of</strong> Shanghai Jiao Tong University, Shanghai 200233,<br />
China. surlab@hotmail.com<br />
Telephone: +86-21-64369181 Fax: +86-21-64701361<br />
Received: August 7, 2010 Revised: November 12, 2010<br />
Accepted: November 19, 2010<br />
Published online: February 21, 2011<br />
Abstract<br />
AIM: To analyze the upregulated CD133 expression in<br />
tumorigenesis <strong>of</strong> primary colon <strong>cancer</strong> cells.<br />
METHODS: Upregulated CD133 expression in tumorigenesis<br />
<strong>of</strong> colo<strong>rectal</strong> <strong>cancer</strong> cell lines (Lovo, Colo205,<br />
Caco-2, HCT116 and SW620) was analyzed by flow<br />
cytometry. Human colon <strong>cancer</strong> tissue samples were<br />
stained with anti-human CD133. SW620 cells were<br />
sorted according to the CD133 expression level measured<br />
by fluorescence-activated cell sorting. Spheroids<br />
<strong>of</strong> colo<strong>rectal</strong> <strong>cancer</strong> cells were cultured with the hanging<br />
drop. Expression <strong>of</strong> CD133 and Lgr5 in spheroids<br />
<strong>of</strong> colo<strong>rectal</strong> <strong>cancer</strong> cells and monolayer culture was<br />
detected by RT-qPCR. Spheroids <strong>of</strong> colo<strong>rectal</strong> <strong>cancer</strong><br />
cells were analyzed using anti-human CD133 with immunohistochemical<br />
staining.<br />
RESULTS: CD133 antigen was expressed in colo<strong>rectal</strong><br />
<strong>cancer</strong> cell lines (Lovo, Colo205, Caco-2, HCT116 and<br />
SW620) as well as in primary and metastatic human<br />
colon <strong>cancer</strong> tissues. However, the CD133 was differently<br />
expressed in these cell lines and tissues. The<br />
expression levels <strong>of</strong> CD133 and Lgr5 were significantly<br />
WJG|www.wjgnet.com<br />
932<br />
<strong>World</strong> J Gastroenterol 2011 February 21; 17(7): 932-937<br />
ISSN 1007-9327 (print) ISSN 2219-2840 (online)<br />
© 2011 Baishideng. All rights reserved.<br />
higher in spheroids <strong>of</strong> parental, CD133 hi and CD133 -<br />
cells than in their monolayer culture at the mRNA level<br />
(P < 0.05). Immunohistochemical staining <strong>of</strong> spheroids<br />
<strong>of</strong> CD133 - cells showed that CD133 was highly expressed<br />
in colo<strong>rectal</strong> <strong>cancer</strong> cell lines.<br />
CONCLUSION: Upregulated CD133 expression plays<br />
a role in tumorigenesis colo<strong>rectal</strong> <strong>cancer</strong> cells, which<br />
may promote the expression <strong>of</strong> other critical genes<br />
that can drive tumorigenesis.<br />
© 2011 Baishideng. All rights reserved.<br />
Key words: CD133; Colon <strong>cancer</strong> cells; Tumorigenesis;<br />
Cancer stem cells<br />
Peer reviewer: Ioannis Kanellos, Pr<strong>of</strong>essor, 4th Surgical Department,<br />
Aristotle University <strong>of</strong> Thessaloniki, Antheon 1, Panorama,<br />
Thessaloniki 55236, Greece<br />
Yang ZL, Zheng Q, Yan J, Pan Y, Wang ZG. Upregulated CD133<br />
expression in tumorigenesis <strong>of</strong> colon <strong>cancer</strong> cells. <strong>World</strong> J Gastroenterol<br />
2011; 17(7): 932-937 Available from: URL: http://<br />
www.wjgnet.com/1007-9327/full/v17/i7/932.htm DOI: http://<br />
dx.doi.org/10.3748/wjg.v17.i7.932<br />
INTRODUCTION<br />
CD133, also known as prominin-1, a transmembrane pentaspan<br />
protein, is originally described as a surface antigen<br />
specific for human hematopoietic stem and progenitor<br />
cells [1,2] . Later, CD133 is recognized as a stem cell marker<br />
for other normal tissues <strong>of</strong> brain [3] , kidney [4] , prostate [5] ,<br />
liver [6] , pancreas [7] , and skin [8] . It has been increasingly reported<br />
that CD133 is a marker <strong>of</strong> putative <strong>cancer</strong> stem<br />
cells (CSC) in brain tumor [9,10] , prostate <strong>cancer</strong> [11] , colon<br />
<strong>cancer</strong> [12-14] , lung <strong>cancer</strong> [15] , hepatocellular carcinoma [16] ,<br />
melanoma [17] , ovarian <strong>cancer</strong> [18] , and pancreatic <strong>cancer</strong> [19] .<br />
Accordingly, CD133 has been referred to as “the molecule<br />
<strong>of</strong> the moment” [20] .<br />
February 21, 2011|Volume 17|Issue 7|
It has been recently shown that CD133 expression is<br />
broadly distributed in primary colon <strong>cancer</strong> cells including<br />
<strong>cancer</strong> stem cells, both CD133 + and CD133 - metastatic<br />
colon <strong>cancer</strong> cells initiate tumors [21-23] . However,<br />
whether CD133 expression plays a role in tumorigenesis<br />
<strong>of</strong> colo<strong>rectal</strong> <strong>cancer</strong> cells is unknown.<br />
In the present study, upregulated CD133 expression in<br />
several colo<strong>rectal</strong> <strong>cancer</strong> cell lines as well as in human primary<br />
and metastatic colon <strong>cancer</strong> tissue samples was analyzed.<br />
SW620 cell line was sorted using CD133 antigen.<br />
Spheroids <strong>of</strong> parental, CD133 - and CD133 hi cells were cultured<br />
with the hanging drop. Expressions <strong>of</strong> CD133 and<br />
Lgr5 were detected in spheroids <strong>of</strong> colo<strong>rectal</strong> <strong>cancer</strong> cells.<br />
CD133 was widely expressed in human colo<strong>rectal</strong> <strong>cancer</strong><br />
cell lines as well as in primary and metastatic colon <strong>cancer</strong><br />
tissues and upregulated CD133 expression was detected<br />
in spheroids <strong>of</strong> colo<strong>rectal</strong> <strong>cancer</strong> cells, indicating that upregulated<br />
CD133 expression may promote the expression<br />
<strong>of</strong> other critical genes that can drive tumorigenesis.<br />
MATERIALS AND METHODS<br />
Cell lines and cell culture and tissue samples<br />
Human colo<strong>rectal</strong> <strong>cancer</strong> cell lines (Lovo, Colo205, Caco-2,<br />
HCT116 and SW620) were cultured in RPMI1640 medium<br />
containing 10% fetal bovine serum (FBS), 2 mmol/L<br />
L-glutamine, 10 μmol/L thioglycerol, 12.5 U insulin,<br />
0.5 mg hydrocostisone, and 30mg penicillin G/0.05 g<br />
streptomycin. Colo<strong>rectal</strong> <strong>cancer</strong> cells were cultured at<br />
37℃ in a humidified atmosphere containing 10% CO2.<br />
CD133 expression was detected in formalin-fixed, paraffinembedded<br />
primary and metastatic colo<strong>rectal</strong> <strong>cancer</strong> tissue<br />
samples from Affiliated Sixth People’s Hospital <strong>of</strong> Shanghai<br />
Jiaotong University. The study was approved by the<br />
Ethics Committee <strong>of</strong> Affiliated Sixth People’s Hospital <strong>of</strong><br />
Shanghai Jiaotong University.<br />
Fluorescence-activated cell sorting<br />
Single-cell suspensions were stained with antibodies against<br />
human CD133 (AC133, 1:40) and human CD133/1 and<br />
CD133/2(1:10, APC conjugated, Miltenyi Biotech, Germany).<br />
Dead cells, cell debris, doublets and aggregates were<br />
excluded by forward and side scattering and pulse-width<br />
gating. Colo<strong>rectal</strong> <strong>cancer</strong> ells (1 × 10 5 ) were stained in an eppendorf<br />
tube. Primary antibody was incubated for 45 min<br />
on ice and second antibody (anti-mouse Alexa488, 1:400)<br />
was incubated for 30 min on ice in the dark. Flow cytometry<br />
analysis was carried out on a fluorescence-activated cell<br />
sorting (FACS) caliber (BD). Colo<strong>rectal</strong> <strong>cancer</strong> ells (1 × 10 6 )<br />
were prepared for sorting, stained with human CD133/1<br />
(1:10, APC conjugated, Miltenyi Biotech) and 1 μg/mL<br />
propidium iodide (PI) to exclude dead cells during sorting.<br />
The cells were sorted using FACSAria (BD). Matched isotype<br />
antibodies were applied in parallel as controls.<br />
Colon spheroids were culture with hanging drop<br />
SW620 colo<strong>rectal</strong> <strong>cancer</strong> cells and their sorted CD133 -<br />
and CD133 hi cells were prepared as a single cell suspension.<br />
The cells were counted and diluted in RPMI1640<br />
WJG|www.wjgnet.com<br />
Yang ZL et al . Upregulated CD133 expression in tumorigenesis <strong>of</strong> colon <strong>cancer</strong> cells<br />
containing 20% FBS and antibiotics to a concentration <strong>of</strong><br />
500 cells per 20 μL/drop in a sterile basin. The lid was lifted,<br />
inverted and placed on top <strong>of</strong> the dish containing 10<br />
mL PBS. An 8-channel pipette was used to make rows <strong>of</strong><br />
20 μL drops on the up-turned inner surface <strong>of</strong> the tissue<br />
culture dish lid. The drops were incubated at 37℃ in an<br />
atmosphere containing 10% CO2 for 10 d.<br />
Immunohistochemistry<br />
Frozen sections <strong>of</strong> the spheroids <strong>of</strong> colo<strong>rectal</strong> <strong>cancer</strong> cells<br />
were fixed in acetone at -20℃ for 10 min and rehydrated<br />
in PBS. Endogenous peroxidase was inactivated by immersing<br />
the sections in 0.3% hydrogen peroxide for 20<br />
min. The primary antibody for frozen sections <strong>of</strong> the<br />
spheroids <strong>of</strong> colo<strong>rectal</strong> <strong>cancer</strong> cells and paraffin-embedded<br />
sections <strong>of</strong> colo<strong>rectal</strong> <strong>cancer</strong> tissue samples was a mouse<br />
anti-human monoclonal CD133/2 (1:40, Miltenyi Biotech,<br />
Germany) and a rabbit anti-human polyclonal CD133<br />
(1:100, Abcam, England), respectively. The sections were<br />
incubated overnight at 4℃ in a humidified chamber, then<br />
with biotinylated secondary antibody (VECTASTAIN<br />
ABC kit, Vector Laboratories) for 30 min at room temperature.<br />
Each section was incubated with the VECTASTAIN<br />
ABC reagent for 30 min at room temperature. The sections<br />
were developed using the DAB (Vector Laboratories)<br />
as the substrate and then counterstained with hematoxylin.<br />
The negative control was performed by incubating samples<br />
with PBS.<br />
Quantification <strong>of</strong> CD133 expression by quantitative<br />
polymerase chain reaction<br />
Total RNA was isolated from cultured colo<strong>rectal</strong> <strong>cancer</strong><br />
cells and their spheroids using the RNeasy extraction<br />
kit (GE Healthcare) and reverse transcribed using<br />
high-capacity cDNA reverse transcription kit (Applied<br />
Biosystems) according to their manufacturer’s instructions,<br />
respectively. Relative quantitative polymerase chain<br />
reaction (PCR) was performed on a 7300 fast real-time<br />
PCR system (Applied Biosystems) using SYBR green<br />
PCR master mix (Applied Biosystems). The humanspecific<br />
intron spanning primer pairs for CD133 were<br />
provided by QIAGEN (Catalog number: QT00075586).<br />
The sequences <strong>of</strong> primer pairs used for GAPDH and<br />
Lgr5 are CAATGACCCCTTCATTGACC (forward) and<br />
TGATGACAAGCTTCCCGTTC (reverse), and CTTC-<br />
CAACCTCAGCGTCTTC (forward) and TTTCCCG-<br />
CAAGACGTAACTC (reverse), respectively. PCR was<br />
performed for 1 cycle at 50℃ for 2 min and 1 cycle at<br />
95℃ for 10 min, followed by 40 cycles at 95℃ for 15 s<br />
and 60℃ for 1 min. Specificity <strong>of</strong> PCR products was<br />
tested according to the dissociation curves. Relative values<br />
<strong>of</strong> transcripts were calculated using the equation: 2 -ΔΔCt ,<br />
where ΔCt is equal to the difference in threshold cycles<br />
for target and reference.<br />
Statistical analysis<br />
Results were expressed as mean ± SD for three repeated<br />
individual experiments in each group. Statistical analyses<br />
were conducted using the SPSS s<strong>of</strong>tware (version 10.0).<br />
933 February 21, 2011|Volume 17|Issue 7|
A<br />
Count<br />
Yang ZL et al . Upregulated CD133 expression in tumorigenesis <strong>of</strong> colon <strong>cancer</strong> cells<br />
200<br />
160<br />
120<br />
80<br />
40<br />
0<br />
10 0 10 1 10 2 10 3 10 4<br />
Figure 1 Fluorescence-activated cell sorting showing CD133 expression in different colo<strong>rectal</strong> <strong>cancer</strong> cell lines (A), CD133 staining <strong>of</strong> human primary<br />
colo<strong>rectal</strong> <strong>cancer</strong> tissue (B) and metastatic colo<strong>rectal</strong> <strong>cancer</strong> tissue (C) (Original magnification × 100). Brown indicates positive staining.<br />
Correlation between sample groups and molecular variables<br />
was assayed with paired t test. P < 0.05 was considered<br />
statistically significant.<br />
RESULTS<br />
200<br />
200<br />
200<br />
200<br />
Lovo Colo 205 SW 620 Caco-2 HCT116<br />
FL4-H<br />
Count<br />
160<br />
120<br />
80<br />
40<br />
CD133 expression in colon <strong>cancer</strong> cell lines and human<br />
colon <strong>cancer</strong> tissues<br />
CD133 antigen was expressed in all colo<strong>rectal</strong> <strong>cancer</strong> cell<br />
lines with a difference <strong>of</strong> 30%-95% (Figure 1A). CD133<br />
in human colo<strong>rectal</strong> <strong>cancer</strong> tissue samples was stained<br />
with polyclonal antibody. CD133 expression was detected<br />
in 18 <strong>of</strong> the 20 primary <strong>cancer</strong> tissue samples, exclusively<br />
on the membrane <strong>of</strong> the vast majority <strong>of</strong> colo<strong>rectal</strong> <strong>cancer</strong><br />
gland cells (Figure 1B), and in 9 <strong>of</strong> the 10 metastatic<br />
colo<strong>rectal</strong> <strong>cancer</strong> tissue samples with positive staining in<br />
cytoplasm <strong>of</strong> <strong>cancer</strong> cells (Figure 1C).<br />
CD133 expression in spheroids <strong>of</strong> sorted colo<strong>rectal</strong><br />
<strong>cancer</strong> cell subpopulations<br />
To minimize the contamination between the sorted<br />
CD133 + and CD133 - cells, a high CD133 expression cell<br />
subpopulation (CD133 hi ) and a CD133 - cell subpopulation<br />
sorted from the SW620 cells could be persistently<br />
passed. CD133 antigen was stably expressed in the monolayer<br />
culture (Figure 2A). To mimic the tumorigenesis <strong>of</strong><br />
colo<strong>rectal</strong> <strong>cancer</strong> cells in vivo, spheroids <strong>of</strong> the sorted cells<br />
were cultured with hanging drop. The parental, CD133 hi<br />
and CD133 - cells could grow into spheroids. CD133 expression<br />
was upregulated in spheroids <strong>of</strong> CD133 - cells.<br />
Although the CD133 expression rate was not changed,<br />
WJG|www.wjgnet.com<br />
0<br />
10 0 10 1 10 2 10 3 10 4<br />
FL4-H<br />
B C<br />
M1<br />
M2<br />
Count<br />
160<br />
120<br />
80<br />
40<br />
M1<br />
0<br />
10 0 10 1 10 2 10 3 10 4<br />
FL4-H<br />
M2<br />
Count<br />
160<br />
120<br />
80<br />
40<br />
the mean fluorescence intensity (MFI) was significantly<br />
increased in spheroids <strong>of</strong> CD133 hi cells, and the CD133<br />
expression rate and MFI were significantly increased in<br />
spheroids <strong>of</strong> parental cells detected by FACS assay (Figure<br />
2B). Immunohistochemical staining <strong>of</strong> CD133 antigen<br />
was observed in spheroids <strong>of</strong> CD133 - cells (Figure 2C).<br />
The CD133 gene expression level was significantly higher<br />
in spheroids <strong>of</strong> SW620, CD133 hi and CD133 - cells than in<br />
their monolayer culture at the mRNA level (4.224 ± 0.063<br />
vs 2.680 ± 0.117, 3.653 ± 0.061 vs 1.325 ± 0.044, 8.746 ±<br />
0.029 vs 3.761 ± 0.065, P < 0.05) (Figure 2D).<br />
Lgr5 expression in spheroids <strong>of</strong> sorted colo<strong>rectal</strong><br />
<strong>cancer</strong> cell subpopulations<br />
Lgr5 expression was analyzed by RT-qPCR in order to<br />
observe the role <strong>of</strong> the expression <strong>of</strong> other colon stem<br />
cell genes in tumorigenesis <strong>of</strong> colo<strong>rectal</strong> <strong>cancer</strong> cells.<br />
The results showed that the Lgr5 expression level was<br />
significantly higher in spheroids <strong>of</strong> parental, CD133 hi<br />
and CD133 - cells than in their monolayer cells (5.942 ±<br />
0.091 vs 4.003 ± 0.039, 6.611 ± 0.214 vs 3.645 ± 0.046,<br />
5.910 ± 0.035 vs 3.903 ± 0.083, P < 0.05) (Figure 3).<br />
DISCUSSION<br />
0<br />
10 0 10 1 10 2 10 3 10 4<br />
FL4-H<br />
Whether CD133 antigen can be used as a marker <strong>of</strong><br />
colo<strong>rectal</strong> <strong>cancer</strong> stem cells is still controversial. The focus<br />
is that CD133 expression is not restricted to just a<br />
small number <strong>of</strong> colo<strong>rectal</strong> <strong>cancer</strong> cells. In this study, the<br />
CD133 expression was upregulated in colo<strong>rectal</strong> <strong>cancer</strong><br />
cell lines and primary or metastatic colo<strong>rectal</strong> <strong>cancer</strong> tissue<br />
934 February 21, 2011|Volume 17|Issue 7|<br />
Count<br />
160<br />
120<br />
80<br />
40<br />
0<br />
10 0 10 1 10 2 10 3 10 4<br />
FL4-H
A<br />
B<br />
C<br />
Count<br />
Count<br />
200<br />
160<br />
120<br />
80<br />
40<br />
200<br />
200<br />
SW 620 cells CD133 hi cells CD133 - cells<br />
0<br />
10 0 10 1 10 2 10 3 10 4<br />
200<br />
160<br />
120<br />
80<br />
40<br />
D 2.40<br />
log10 (relative quantitation)<br />
M1<br />
FL4-H<br />
M2<br />
0<br />
10 0 10 1 10 2 10 3 10 4<br />
2.00<br />
1.60<br />
1.20<br />
0.80<br />
0.40<br />
0.00<br />
FL4-H<br />
Count<br />
160<br />
120<br />
Figure 2 Fluorescence-activated cell sorting showing CD133 expression in SW620, CD133 - and CD133 hi cells (A) and in their spheroids (B), CD133 staining in<br />
spheroids <strong>of</strong> SW620, CD133 - and CD133 hi cells (original magnification × 100, brown indicates positive staining) (C), and reverse transcription-polymerase chain<br />
reaction showing CD133 expression in SW620, CD133 - and CD133 hi cells and their spheroids. a P < 0.05 vs monolayer cells. SP: Spheroid.<br />
samples, showing that CD133 antigen can be expressed in<br />
colo<strong>rectal</strong> <strong>cancer</strong> cell lines with a difference <strong>of</strong> 30%-95%.<br />
CD133 expression was detected in 18 <strong>of</strong> the 20 primary<br />
colo<strong>rectal</strong> <strong>cancer</strong> tissue samples, exclusively on the membrane<br />
<strong>of</strong> a large number <strong>of</strong> colo<strong>rectal</strong> <strong>cancer</strong> gland cells,<br />
and in 9 <strong>of</strong> the 10 metastatic colo<strong>rectal</strong> <strong>cancer</strong> tissue<br />
samples with a positive staining in cytoplasm <strong>of</strong> colorec-<br />
80<br />
40<br />
WJG|www.wjgnet.com<br />
0<br />
10 0 10 1 10 2 10 3 10 4<br />
FL4-H<br />
Count<br />
160<br />
120<br />
80<br />
40<br />
M1<br />
0<br />
10 0 10 1 10 2 10 3 10 4<br />
FL4-H<br />
200<br />
200<br />
SW620-spheroids CD133 hi -spheroids CD133 - -spheroids<br />
Count<br />
160<br />
120<br />
80<br />
40<br />
0<br />
10 0 10 1 10 2 10 3 10 4<br />
FL4-H<br />
Count<br />
160<br />
120<br />
80<br />
40<br />
M2<br />
0<br />
10 0 10 1 10 2 10 3 10 4<br />
FL4-H<br />
Control SW620-spheroids CD133 hi -spheroids CD133 - -spheroids<br />
1.290<br />
1.447<br />
Yang ZL et al . Upregulated CD133 expression in tumorigenesis <strong>of</strong> colon <strong>cancer</strong> cells<br />
a<br />
2.115<br />
Gene expression<br />
0.000<br />
SW620 CD133 hi CD133 hi _SP CD133- CD133 - _SP SW620_SP H2O<br />
CD133<br />
a<br />
1.404<br />
a<br />
1.711<br />
a<br />
tal <strong>cancer</strong> cells, which is consistent with the reported<br />
findings [21-23] . The different CD133 expression levels in<br />
colo<strong>rectal</strong> caner cell lines may be related to the different<br />
glycosylation to the mask specific epitopes <strong>of</strong> CD133 antigen<br />
in colo<strong>rectal</strong> <strong>cancer</strong> cell differentiation [24] . Therefore,<br />
our data indicate that CD133 is commonly expressed in<br />
colo<strong>rectal</strong> <strong>cancer</strong> cells.<br />
935 February 21, 2011|Volume 17|Issue 7|
Yang ZL et al . Upregulated CD133 expression in tumorigenesis <strong>of</strong> colon <strong>cancer</strong> cells<br />
log10 (relative quantitation)<br />
1.00<br />
0.80<br />
0.60<br />
0.40<br />
0.20<br />
0.00<br />
-0.20<br />
0.210<br />
0.000<br />
Figure 3 Quantitative reverse transcription-polymerase chain reaction showing Lgr5 expression in SW620, CD133 - and CD133 hi cells and their spheroids.<br />
a P < 0.05 vs monolayer cells. SP: Spheroid.<br />
To investigate whether the upregulated CD133 expression<br />
plays a role in tumorigenesis <strong>of</strong> colo<strong>rectal</strong> <strong>cancer</strong> cells,<br />
SW620 cell line containing two cell subpopulations (CD-<br />
133 hi , CD133 - ) was selected and sorted using CD133 antigen,<br />
the spheroids <strong>of</strong> parental, CD133 hi and CD133 - cells<br />
were cultured with the hanging drop in vitro, which is based<br />
on the natural disposition <strong>of</strong> cells to aggregate without the<br />
need for polymer scaffolds such as matrigel, polyglycolic<br />
acid or microporous supports to achieve homogeneous<br />
multicellular tumor spheroids [25] . The spheroids represent<br />
a popular in vitro 3D tissue structure that mimics in vivo tumor<br />
tissue organization and microenvironment [26,27] . In the<br />
present study, CD133 hi and CD133 - cells could be cultured<br />
into their spheroids, CD133 expression was upregulated in<br />
spheroids <strong>of</strong> CD133 - cells. Although the CD133 expression<br />
was not changed, the mean fluorescence intensity<br />
(MFI) was significantly increased in spheroids <strong>of</strong> CD133 hi<br />
cells as detected by FACS assay. Immunohistochemical<br />
staining <strong>of</strong> CD133 antigen was observed in spheroids <strong>of</strong><br />
CD133 - cells, indicating that CD133 antigen expression<br />
is upregulated in spheroids <strong>of</strong> CD133 - and CD133 hi cells.<br />
Further analysis revealed that the CD133 gene expression<br />
level was significantly higher in spheroids <strong>of</strong> SW620,<br />
CD133 hi and CD133 - cells than in their monolayer culture<br />
at the mRNA level, suggesting that the upregulated expression<br />
<strong>of</strong> CD133 including protein and gene plays a role in<br />
tumorigenesis <strong>of</strong> colo<strong>rectal</strong> <strong>cancer</strong> cells.<br />
Since the upregulated CD133 expression plays a role in<br />
tumorigenesis <strong>of</strong> colo<strong>rectal</strong> <strong>cancer</strong> cells, whether CD133<br />
protein supports the growth <strong>of</strong> colo<strong>rectal</strong> <strong>cancer</strong> is a subject<br />
that should be actively studied. As CD133 by itself<br />
may lack <strong>of</strong> a functional role in initiation <strong>of</strong> tumors and<br />
metastasis <strong>of</strong> human colo<strong>rectal</strong> <strong>cancer</strong> [28,29] , it has an impact<br />
on the survival <strong>of</strong> colo<strong>rectal</strong> <strong>cancer</strong> patients [22,29] . It has<br />
been recently demonstrated that prominin 1 (also called<br />
CD133)-marked mouse intestinal stem cells are susceptible<br />
to neoplastic transformation [30] , possibly due to the fact that<br />
upregulated CD133 expression may promote the expression<br />
<strong>of</strong> other critical genes that can drive tumorigenesis <strong>of</strong><br />
colo<strong>rectal</strong> <strong>cancer</strong> cells. In this study, the expression level<br />
<strong>of</strong> Lgr5 (leucine-rich-repeat-containing G-protein-coupled<br />
receptor 5), also known as Gpr49, a colon stem cell marker<br />
WJG|www.wjgnet.com<br />
a<br />
0.842<br />
Gene expression<br />
0.213<br />
SW620 CD133 hi CD133 hi _SP CD133- CD133 - _SP SW620_SP H2O<br />
Lgr5<br />
a<br />
0.779<br />
a<br />
0.736<br />
0.000<br />
gene [31] , was significantly higher in spheroids <strong>of</strong> parental,<br />
CD133 hi and CD133 - cells than in their monolayer cells.<br />
In conclusion, the upregulated CD133 expression plays<br />
a role in tumorigenesis <strong>of</strong> colo<strong>rectal</strong> <strong>cancer</strong> cells, which<br />
may be related to the expression <strong>of</strong> other critical genes that<br />
can drive tumorigenesis <strong>of</strong> colo<strong>rectal</strong> <strong>cancer</strong> cells. Further<br />
study is needed to confirm the present results in vivo.<br />
ACKNOWLEDGMENTS<br />
The authors thank Francesca Walker and Hui-Hua Zhang<br />
(Ludwig Institute, Melbourne) for their assistance to cell<br />
experiments and FACS studies, and You-Fang Zhang<br />
(Ludwig Institute, Melbourne) for his support in immunohistochemical<br />
studies.<br />
COMMENTS<br />
Background<br />
It has been recently shown that CD133 expression is broadly distributed in<br />
primary colo<strong>rectal</strong> <strong>cancer</strong> cells, and not restricted to <strong>cancer</strong> stem cells. Whether<br />
the upregulated CD133 expression plays a role in tumorigenesis <strong>of</strong> colo<strong>rectal</strong><br />
<strong>cancer</strong> cells is unknown.<br />
Research frontiers<br />
It has been increasingly reported that CD133 is a marker <strong>of</strong> putative <strong>cancer</strong> stem<br />
cells (CSC) in some <strong>cancer</strong>s. However, it has been recently shown that CD133<br />
expression is broadly distributed in primary colon <strong>cancer</strong> cells and not restricted to<br />
<strong>cancer</strong> stem cells, and both CD133 + and CD133 - metastatic colo<strong>rectal</strong> <strong>cancer</strong> cells<br />
initiate tumors. Whether the upregulated CD133 expression plays a role in tumorigenesis<br />
<strong>of</strong> colo<strong>rectal</strong> <strong>cancer</strong> cells is unknown. In this study, the upregulated CD133<br />
expression was found to play a role in tumorigenesis <strong>of</strong> colo<strong>rectal</strong> <strong>cancer</strong> cells.<br />
Innovations and breakthroughs<br />
Recent reports have shown that whether CD133 antigen can be used as a<br />
marker <strong>of</strong> colo<strong>rectal</strong> <strong>cancer</strong> stem cells is controversial. This is the first study to<br />
report the role <strong>of</strong> upregulated CD133 expression in tumorigenesis <strong>of</strong> colo<strong>rectal</strong><br />
<strong>cancer</strong> cells. Furthermore, our in vitro studies suggested that the upregulated<br />
CD133 expression may promote the expression <strong>of</strong> other critical genes that can<br />
drive tumorigenesis <strong>of</strong> colo<strong>rectal</strong> <strong>cancer</strong> cells.<br />
Applications<br />
Whether the upregulated CD133 expression plays a role in tumorigenesis <strong>of</strong><br />
colo<strong>rectal</strong> <strong>cancer</strong> cells was studied, the results may help to solve the controversy<br />
on CD133 antigen as a marker <strong>of</strong> colo<strong>rectal</strong> <strong>cancer</strong> stem cells.<br />
Terminology<br />
CD133, also known as prominin-1, a transmembrane pentaspan protein, is<br />
originally described as a surface antigen specific for human hematopoietic stem<br />
936 February 21, 2011|Volume 17|Issue 7|
and progenitor cells. Lgr5 (leucine-rich-repeat-containing G-protein-coupled<br />
receptor 5), also known as Gpr49, is a colon stem cell marker gene.<br />
Peer review<br />
The authors detected the expression <strong>of</strong> CD133 in a panel <strong>of</strong> colo<strong>rectal</strong> <strong>cancer</strong><br />
cell lines and human colo<strong>rectal</strong> <strong>cancer</strong> tissue samples. The expression <strong>of</strong><br />
CD133 and Lgr5 in spheroids <strong>of</strong> the sorted colo<strong>rectal</strong> <strong>cancer</strong> cell subpopulations<br />
suggests that the upregulated expression plays a role in tumorigenesis<br />
<strong>of</strong> colo<strong>rectal</strong> <strong>cancer</strong> cells, which may promote the expression <strong>of</strong> other critical<br />
genes that can drive tumorigenesis. The results are interesting.<br />
REFERENCES<br />
1 Yin AH, Miraglia S, Zanjani ED, Almeida-Porada G, Ogawa<br />
M, Leary AG, Olweus J, Kearney J, Buck DW. AC133, a novel<br />
marker for human hematopoietic stem and progenitor cells.<br />
Blood 1997; 90: 5002-5012<br />
2 Miraglia S, Godfrey W, Yin AH, Atkins K, Warnke R, Holden<br />
JT, Bray RA, Waller EK, Buck DW. A novel five-transmembrane<br />
hematopoietic stem cell antigen: isolation, characterization,<br />
and molecular cloning. Blood 1997; 90: 5013-5021<br />
3 Uchida N, Buck DW, He D, Reitsma MJ, Masek M, Phan TV,<br />
Tsukamoto AS, Gage FH, Weissman IL. Direct isolation <strong>of</strong><br />
human central nervous system stem cells. Proc Natl Acad Sci<br />
USA 2000; 97: 14720-14725<br />
4 Sagrinati C, Netti GS, Mazzinghi B, Lazzeri E, Liotta F, Frosali<br />
F, Ronconi E, Meini C, Gacci M, Squecco R, Carini M, Gesualdo<br />
L, Francini F, Maggi E, Annunziato F, Lasagni L, Serio<br />
M, Romagnani S, Romagnani P. Isolation and characterization<br />
<strong>of</strong> multipotent progenitor cells from the Bowman’s capsule <strong>of</strong><br />
adult human kidneys. J Am Soc Nephrol 2006; 17: 2443-2456<br />
5 Richardson GD, Robson CN, Lang SH, Neal DE, Maitland<br />
NJ, Collins AT. CD133, a novel marker for human prostatic<br />
epithelial stem cells. J Cell Sci 2004; 117: 3539-3545<br />
6 Kordes C, Sawitza I, Müller-Marbach A, Ale-Agha N, Keitel V,<br />
Klonowski-Stumpe H, Häussinger D. CD133+ hepatic stellate<br />
cells are progenitor cells. Biochem Biophys Res Commun 2007;<br />
352: 410-417<br />
7 Sugiyama T, Rodriguez RT, McLean GW, Kim SK. Conserved<br />
markers <strong>of</strong> fetal pancreatic epithelium permit prospective<br />
isolation <strong>of</strong> islet progenitor cells by FACS. Proc Natl Acad<br />
Sci USA 2007; 104: 175-180<br />
8 Ito Y, Hamazaki TS, Ohnuma K, Tamaki K, Asashima M,<br />
Okochi H. Isolation <strong>of</strong> murine hair-inducing cells using the<br />
cell surface marker prominin-1/CD133. J Invest Dermatol<br />
2007; 127: 1052-1060<br />
9 Singh SK, Clarke ID, Terasaki M, Bonn VE, Hawkins C,<br />
Squire J, Dirks PB. Identification <strong>of</strong> a <strong>cancer</strong> stem cell in human<br />
brain tumors. Cancer Res 2003; 63: 5821-5828<br />
10 Taylor MD, Poppleton H, Fuller C, Su X, Liu Y, Jensen P,<br />
Magdaleno S, Dalton J, Calabrese C, Board J, Macdonald T,<br />
Rutka J, Guha A, Gajjar A, Curran T, Gilbertson RJ. Radial<br />
glia cells are candidate stem cells <strong>of</strong> ependymoma. Cancer Cell<br />
2005; 8: 323-335<br />
11 Collins AT, Berry PA, Hyde C, Stower MJ, Maitland NJ. Prospective<br />
identification <strong>of</strong> tumorigenic prostate <strong>cancer</strong> stem<br />
cells. Cancer Res 2005; 65: 10946-10951<br />
12 O’Brien CA, Pollett A, Gallinger S, Dick JE. A human colon<br />
<strong>cancer</strong> cell capable <strong>of</strong> initiating tumour growth in immunodeficient<br />
mice. Nature 2007; 445: 106-110<br />
13 Ricci-Vitiani L, Lombardi DG, Pilozzi E, Biffoni M, Todaro M,<br />
Peschle C, De Maria R. Identification and expansion <strong>of</strong> human<br />
colon-<strong>cancer</strong>-initiating cells. Nature 2007; 445: 111-115<br />
14 Todaro M, Alea MP, Di Stefano AB, Cammareri P, Vermeulen<br />
L, Iovino F, Tripodo C, Russo A, Gulotta G, Medema JP,<br />
Stassi G. Colon <strong>cancer</strong> stem cells dictate tumor growth and<br />
resist cell death by production <strong>of</strong> interleukin-4. Cell Stem Cell<br />
2007; 1: 389-402<br />
15 Eramo A, Lotti F, Sette G, Pilozzi E, Biffoni M, Di Virgilio<br />
A, Conticello C, Ruco L, Peschle C, De Maria R. Identifica-<br />
WJG|www.wjgnet.com<br />
Yang ZL et al . Upregulated CD133 expression in tumorigenesis <strong>of</strong> colon <strong>cancer</strong> cells<br />
tion and expansion <strong>of</strong> the tumorigenic lung <strong>cancer</strong> stem cell<br />
population. Cell Death Differ 2008; 15: 504-514<br />
16 Ma S, Chan KW, Hu L, Lee TK, Wo JY, Ng IO, Zheng BJ,<br />
Guan XY. Identification and characterization <strong>of</strong> tumorigenic<br />
liver <strong>cancer</strong> stem/progenitor cells. Gastroenterology 2007; 132:<br />
2542-2556<br />
17 Monzani E, Facchetti F, Galmozzi E, Corsini E, Benetti A,<br />
Cavazzin C, Gritti A, Piccinini A, Porro D, Santinami M,<br />
Invernici G, Parati E, Alessandri G, La Porta CA. Melanoma<br />
contains CD133 and ABCG2 positive cells with enhanced tumourigenic<br />
potential. Eur J Cancer 2007; 43: 935-946<br />
18 Curley MD, Therrien VA, Cummings CL, Sergent PA, Koulouris<br />
CR, Friel AM, Roberts DJ, Seiden MV, Scadden DT,<br />
Rueda BR, Foster R. CD133 expression defines a tumor initiating<br />
cell population in primary human ovarian <strong>cancer</strong>. Stem<br />
Cells 2009; 27: 2875-2883<br />
19 Hermann PC, Huber SL, Herrler T, Aicher A, Ellwart JW,<br />
Guba M, Bruns CJ, Heeschen C. Distinct populations <strong>of</strong> <strong>cancer</strong><br />
stem cells determine tumor growth and metastatic activity<br />
in human pancreatic <strong>cancer</strong>. Cell Stem Cell 2007; 1: 313-323<br />
20 Mizrak D, Brittan M, Alison MR. CD133: molecule <strong>of</strong> the moment.<br />
J Pathol 2008; 214: 3-9<br />
21 Shmelkov SV, Butler JM, Hooper AT, Hormigo A, Kushner<br />
J, Milde T, St Clair R, Baljevic M, White I, Jin DK, Chadburn<br />
A, Murphy AJ, Valenzuela DM, Gale NW, Thurston G, Yancopoulos<br />
GD, D’Angelica M, Kemeny N, Lyden D, Rafii S.<br />
CD133 expression is not restricted to stem cells, and both<br />
CD133+ and CD133- metastatic colon <strong>cancer</strong> cells initiate tumors.<br />
J Clin Invest 2008; 118: 2111-2120<br />
22 Horst D, Kriegl L, Engel J, Kirchner T, Jung A. CD133 expression<br />
is an independent prognostic marker for low survival in<br />
colo<strong>rectal</strong> <strong>cancer</strong>. Br J Cancer 2008; 99: 1285-1289<br />
23 Kojima M, Ishii G, Atsumi N, Fujii S, Saito N, Ochiai A. Immunohistochemical<br />
detection <strong>of</strong> CD133 expression in colo<strong>rectal</strong><br />
<strong>cancer</strong>: a clinicopathological study. Cancer Sci 2008; 99:<br />
1578-1583<br />
24 Kemper K, Sprick MR, de Bree M, Scopelliti A, Vermeulen L,<br />
Hoek M, Zeilstra J, Pals ST, Mehmet H, Stassi G, Medema JP.<br />
The AC133 epitope, but not the CD133 protein, is lost upon<br />
<strong>cancer</strong> stem cell differentiation. Cancer Res 2010; 70: 719-729<br />
25 Kelm JM, Timmins NE, Brown CJ, Fussenegger M, Nielsen<br />
LK. Method for generation <strong>of</strong> homogeneous multicellular<br />
tumor spheroids applicable to a wide variety <strong>of</strong> cell types.<br />
Biotechnol Bioeng 2003; 83: 173-180<br />
26 Weiswald LB, Richon S, Validire P, Briffod M, Lai-Kuen R,<br />
Cordelières FP, Bertrand F, Dargere D, Massonnet G, Marangoni<br />
E, Gayet B, Pocard M, Bieche I, Poupon MF, Bellet D,<br />
Dangles-Marie V. Newly characterised ex vivo colospheres<br />
as a three-dimensional colon <strong>cancer</strong> cell model <strong>of</strong> tumour aggressiveness.<br />
Br J Cancer 2009; 101: 473-482<br />
27 Friedrich J, Seidel C, Ebner R, Kunz-Schughart LA. Spheroidbased<br />
drug screen: considerations and practical approach.<br />
Nat Protoc 2009; 4: 309-324<br />
28 Du L, Wang H, He L, Zhang J, Ni B, Wang X, Jin H, Cahuzac<br />
N, Mehrpour M, Lu Y, Chen Q. CD44 is <strong>of</strong> functional importance<br />
for colo<strong>rectal</strong> <strong>cancer</strong> stem cells. Clin Cancer Res 2008; 14:<br />
6751-6760<br />
29 Horst D, Scheel SK, Liebmann S, Neumann J, Maatz S, Kirchner<br />
T, Jung A. The <strong>cancer</strong> stem cell marker CD133 has high<br />
prognostic impact but unknown functional relevance for the<br />
metastasis <strong>of</strong> human colon <strong>cancer</strong>. J Pathol 2009; 219: 427-434<br />
30 Zhu L, Gibson P, Currle DS, Tong Y, Richardson RJ, Bayazitov<br />
IT, Poppleton H, Zakharenko S, Ellison DW, Gilbertson<br />
RJ. Prominin 1 marks intestinal stem cells that are susceptible<br />
to neoplastic transformation. Nature 2009; 457: 603-607<br />
31 Barker N, van Es JH, Kuipers J, Kujala P, van den Born M,<br />
Cozijnsen M, Haegebarth A, Korving J, Begthel H, Peters PJ,<br />
Clevers H. Identification <strong>of</strong> stem cells in small intestine and<br />
colon by marker gene Lgr5. Nature 2007; 449: 1003-1007<br />
S- Editor Sun H L- Editor Wang XL E- Editor Ma WH<br />
937 February 21, 2011|Volume 17|Issue 7|
Online Submissions: http://www.wjgnet.com/1007-9327<strong>of</strong>fice<br />
wjg@wjgnet.com<br />
doi:10.3748/wjg.v17.i7.938<br />
BRIEF ARTICLE<br />
Transplantation <strong>of</strong> microencapsulated umbilical-cord-bloodderived<br />
hepatic-like cells for treatment <strong>of</strong> hepatic failure<br />
Fang-Ting Zhang, Hui-Juan Wan, Ming-Hua Li, Jing Ye, Mei-Jun Yin, Chun-Qiao Huang, Jie Yu<br />
Fang-Ting Zhang, Hui-Juan Wan, Ming-Hua Li, Jing Ye,<br />
Mei-Jun Yin, Chun-Qiao Huang, Jie Yu, Central Laboratory,<br />
Peking University Shenzhen Hospital, Shenzhen 518036, China<br />
Author contributions: Zhang FT and Yu J designed the research;<br />
Zhang FT, Wan HJ, Li MH, Yin MJ, Ye J and Huang<br />
CQ performed the research; Zhang FT analyzed data; Zhang FT<br />
wrote the paper; Yu J edited the paper.<br />
Supported by Guangdong Natural Science Foundation (9151<br />
030002000008) and Shenzhen Science and Technology Planning<br />
Priority Program (JH200205270412B, 200808001, 2008<br />
01012)<br />
Correspondence to: Jie Yu, PhD, Central Laboratory, Peking<br />
University Shenzhen Hospital, 1120 Lian Hua Road, Shenzhen<br />
518036, China. yujie007@hotmail.com<br />
Telephone: +86-755-83923333 Fax: +86-755-83923333<br />
Received: July 19, 2010 Revised: October 20, 2010<br />
Accepted: October 27, 2010<br />
Published online: February 21, 2011<br />
Abstract<br />
AIM: To investigate intraperitoneal transplantation <strong>of</strong><br />
microencapsulated hepatic-like cells from human umbilical<br />
cord blood for treatment <strong>of</strong> hepatic failure in rats.<br />
METHODS: CD34 + cells in umbilical cord blood cells<br />
were isolated by magnetic cell sorting. In the in vitro<br />
experiment, sorted CD34 + cells were amplified and<br />
induced into hepatic-like cells by culturing with a combination<br />
<strong>of</strong> fibroblast growth factor 4 and hepatocyte<br />
growth factor. Cultures without growth factor addition<br />
served as controls. mRNA and protein levels for hepatic-like<br />
cells were analyzed by reverse transcriptionpolymerase<br />
chain reaction, immunohistochemistry and<br />
immun<strong>of</strong>luorescence. In the in vivo experiment, the<br />
hepatic-like cells were encapsulated and transplanted<br />
into the abdominal cavity <strong>of</strong> acute hepatic failure (AHF)<br />
rats at 48 h after D-galactosamine induction <strong>of</strong> acute<br />
hepatic failure. Transplantation with PBS and unencapsulated<br />
hepatic-like cells served as controls. The<br />
mortality rate, hepatic pathological changes and serum<br />
WJG|www.wjgnet.com<br />
938<br />
<strong>World</strong> J Gastroenterol 2011 February 21; 17(7): 938-945<br />
ISSN 1007-9327 (print) ISSN 2219-2840 (online)<br />
© 2011 Baishideng. All rights reserved.<br />
biochemical indexes were determined. The morphology<br />
and structure <strong>of</strong> microcapsules in the greater omentum<br />
were observed.<br />
RESULTS: Human albumin, alpha-fetoprotein and<br />
GATA-4 mRNA and albumin protein positive cells were<br />
found among cultured cells after 16 d. Albumin level in<br />
culture medium was significantly increased after culturing<br />
with growth factors in comparison with culturing<br />
without growth factor addition (P < 0.01). Compared<br />
with the unencapsulated group, the mortality rate <strong>of</strong> the<br />
encapsulated hepatic-like cell-transplanted group was<br />
significantly lower (P < 0.05). Serum biochemical parameters,<br />
alanine aminotransferase, aspartate aminotransferase<br />
and total bilirubin in the encapsulated group were<br />
significantly improvement compared with the PBS control<br />
group (P < 0.01). Pathological staining further supported<br />
these findings. At 1-2 wk post-transplantation, free microcapsules<br />
with a round clear structure and a smooth<br />
surface were observed in peritoneal lavage fluid, surviving<br />
cells inside microcapsules were found by trypan blue<br />
staining, but some fibrous tissue around microcapsules<br />
was also detected in the greater omentum <strong>of</strong> encapsulated<br />
group by hematoxylin and eosin staining.<br />
CONCLUSION: Transplantation <strong>of</strong> microencapsulated<br />
hepatic-like cells derived from umbilical cord blood cells<br />
could preliminarily alleviate the symptoms <strong>of</strong> AHF rats.<br />
© 2011 Baishideng. All rights reserved.<br />
Key words: Microencapsulation; Hepatic-like cells; Umbilical<br />
cord blood cells; CD34 antigen; Alginate; Acute<br />
hepatic failure<br />
Peer reviewer: Toshihiro Mitaka, MD, Pr<strong>of</strong>essor, Department<br />
<strong>of</strong> Pathophysiology, Cancer Research Institute, Sapporo Medical<br />
University, 060-85567 Sapporo, Japan<br />
Zhang FT, Wan HJ, Li MH, Ye J, Yin MJ, Huang CQ, Yu J.<br />
Transplantation <strong>of</strong> microencapsulated umbilical-cord-bloodderived<br />
hepatic-like cells for treatment <strong>of</strong> hepatic failure. <strong>World</strong><br />
February 21, 2011|Volume 17|Issue 7|
J Gastroenterol 2011; 17(7): 938-945 Available from: URL:<br />
http://www.wjgnet.com/1007-9327/full/v17/i7/938.htm DOI:<br />
http://dx.doi.org/10.3748/wjg.v17.i7.938<br />
INTRODUCTION<br />
Substantial efforts have been made with regard to cell<br />
transplantation as an effective supporting system for hepatic<br />
failure and assisted therapies. However, immunological<br />
rejection has always been an important problem for<br />
cell transplantation. Alginate-poly-l-lysine-alginate (APA)<br />
microcapsules have proven to be effective in protecting<br />
enclosed target cells from immune rejection following<br />
transplantation into experimental animals, thereby eliminating<br />
the problems <strong>of</strong> immunosuppressive therapy [1-3] .<br />
Extensive studies have also been conducted on the<br />
core <strong>of</strong> this therapy, namely the cell sources. The investigated<br />
cells have included liver stem cells, embryonic stem<br />
cells, human umbilical cord blood (UCB) cells and bone<br />
marrow stem cells. Human UCB cells have some advantages<br />
that other cells do not have. The frequencies <strong>of</strong><br />
UCB hematopoietic stem/progenitor cells exceed those<br />
from bone marrow and peripheral blood. In our previous<br />
study, we confirmed the differentiation <strong>of</strong> mononuclear<br />
cells (MNCs) from human UCB into hepatocytes in three<br />
different ways, namely co-culture with injured liver cells,<br />
growth factor-assisted culture, and MNC transplantation<br />
in animal models <strong>of</strong> liver injury [4] . In the present study, we<br />
found that CD34 + cells derived from human UCB could<br />
be converted into hepatic-like cells that generate hepatocyte<br />
lineage cells. Furthermore, we encapsulated the hepatic-like<br />
cells using an alginate method and transplanted<br />
them into acute hepatic failure (AHF) rats to evaluate the<br />
effects <strong>of</strong> encapsulated hepatic-like cell transplantation.<br />
MATERIALS AND METHODS<br />
Isolation and identification <strong>of</strong> CD34 + cells<br />
UCB (more than 80 samples) from full-term deliveries<br />
were obtained from the Obstetrics Department <strong>of</strong> Peking<br />
University Shenzhen Hospital. UCB cells were harvested<br />
after written inform consent was obtained. The study<br />
protocol was approved by the Ethics Committee <strong>of</strong> Peking<br />
University Shenzhen Hospital. MNCs were isolated<br />
from the UCB samples by density-gradient centrifugation<br />
at 2000 r/min for 35 min using Ficoll-Hypaque (Huajing,<br />
Shanghai, China). CD34 + subpopulations were isolated<br />
using a Miltenyi Direct CD34 Progenitor Cell Isolation<br />
Kit (Miltenyi Biotec, Bergisch Gladbach, Germany). The<br />
specific steps were as follows: (1) isolated MNCs were resuspended<br />
in a final volume <strong>of</strong> 300 μL <strong>of</strong> PBS that contained<br />
5 g/L bovine serum albumin (BSA); (2) 100 μL <strong>of</strong><br />
FcR Blocking Reagent and 100 μL <strong>of</strong> CD34 Micro Beads<br />
per 1 × 10 8 total cells were sequentially added, mixed well<br />
and incubated for 30 min in a refrigerator at 4℃; (3) cells<br />
were passed through a magnetic column twice and purified;<br />
and (4) CD34 + cells were collected, resuspended in<br />
WJG|www.wjgnet.com<br />
Zhang FT et al . Transplantation <strong>of</strong> microencapsulated hepatic-like cells<br />
Table 1 Primers used for reverse transcription-polymerase<br />
chain reaction<br />
Gene Primer (5’-3’) Amplicon<br />
(bp)<br />
Forward primer Reverse primer<br />
ALB CTTTCAAAGCAT-<br />
GGGCAGTAG<br />
GATA-4 ACCTGGGACTTG-<br />
GAGGATAG<br />
AFP TGAGCACTGTTG-<br />
CAGAGGAG<br />
ALB: Albumin; AFP: α-fetoprotein.<br />
GCAGCAGCACGA-<br />
CAGAGTAA<br />
GACAAGGACATCTT-<br />
GGGAAA<br />
CTGAGACAG-<br />
CAAGCTGAGGA<br />
100 μL PBS, incubated with 10 μL CD34-phycoerythrin<br />
for 10 min at 4℃ and identified by flow cytometry.<br />
Differentiation in vitro<br />
Freshly isolated CD34 + cells were primarily cultured<br />
in Dulbecco’s modified Eagle’s medium - low glucose<br />
(DMEM-LG, Gibco, Carlsbad, CA, USA), amplified for<br />
3-5 d with a combination <strong>of</strong> 12.5 μg/mL thrombopoietin<br />
(TPO) (R&D Systems, Minneapolis, MN, USA),<br />
50 ng/mL stem cell factor (SCF) (R&D Systems) and<br />
50 ng/mL Flt-3 (R&D Systems); then induced into hepatic-like<br />
cells by culturing in DMEM-LG that contained<br />
50 mL/L fetal bovine serum (Gibco), 100 U/mL penicillin,<br />
100 μg/mL streptomycin, 4.7 μg/mL linoleic acid, 1 ×<br />
insulin-transferrin-selenium and 1 × 10 -4 mol/L L-ascorbic<br />
acid 2-P supplemented with 100 ng/mL fibroblast growth<br />
factor (FGF)4 (R&D Systems) and 20 ng/mL hepatocyte<br />
growth factor (HGF; Sigma, St. Louis, MO, USA). CD34 +<br />
cells were incubated in 24-well plates at 37℃ in a 5% CO2<br />
atmosphere. Culture medium was replaced every 3 d. Cultured<br />
cells were collected after 8 and 16 d. Cultures without<br />
growth factors served as controls.<br />
Total mRNA isolation and reverse transcriptionpolymerase<br />
chain reaction<br />
Total mRNA was extracted from collected cells using<br />
Trizol (Mrcgene, Cincinnati, OH, USA). mRNA was<br />
reverse-transcribed and the resulting cDNA was amplified<br />
using the primer sets shown in Table 1 and a RobusT I<br />
reverse transcription-polymerase chain reaction (RT-PCR)<br />
Kit (Finnzymes, Espoo, Finland). Reverse transcriptase<br />
reaction was run at 48℃ for 45 min and PCR was initiated<br />
with pre-denaturation at 94℃ for 2 min, followed by<br />
35 cycles <strong>of</strong> 30 s at 94℃, annealing at 58℃ for 30 s and<br />
extension at 72℃ for 30 s, with 72℃ for 7 min for final<br />
extension. The PCR products were separated on a 1.2%<br />
agarose gel.<br />
Immunocytochemistry for CD34 + cells<br />
Cytospins prepared from cells were fixed with 4% paraformaldehyde<br />
and 0.15% picric acid in PBS at room temperature<br />
for 20 min, then permeabilized and blocked with<br />
10% goat serum and 0.1% Triton X-100 in PBS at room<br />
temperature for 10 min. The cells were sequentially incu-<br />
939 February 21, 2011|Volume 17|Issue 7|<br />
411<br />
250<br />
308
Zhang FT et al . Transplantation <strong>of</strong> microencapsulated hepatic-like cells<br />
bated with a mouse anti-human albumin antibody (R&D<br />
Systems) for 30 min, a biotinylated peroxidase-conjugated<br />
secondary antibody (Zymed, South San Francisco, CA,<br />
USA) for 10 min, and diaminobenzidine for 10 min. Between<br />
the above steps, cells were washed with 0.1 mol/L<br />
PBS that contained 1 g/L BSA.<br />
Albumin determination<br />
Culture media were collected for the quantitative determination<br />
<strong>of</strong> human albumin by ELISA using a Human<br />
Albumin ELISA Kit (Alpha Diagnostics International,<br />
San Antonio, TX, USA) according to the manufacturer’s<br />
instructions.<br />
Cell encapsulation<br />
Cells collected after 16 d induction were washed with PBS<br />
and resuspended in the alginate. The alginate-cell mixture<br />
was passed though a microcapsule generator and extruded<br />
into 40 mL 1.1% CaCl2 solution. The airflow rate was<br />
adjusted for the regulation <strong>of</strong> the microcapsule diameter<br />
between 300 and 800 μm. The capsules and CaCl2 solution<br />
were then transferred to 50-mL conical tubes. After<br />
removal <strong>of</strong> the supernatant, the capsules were gently<br />
mixed with the wash solution and allowed to settle for<br />
2 min. Before transplantation, a few drops <strong>of</strong> encapsulated<br />
cells were placed on a slide, stained with 0.4% Trypan<br />
blue, covered with a cover glass and lightly pressed to<br />
force cells out <strong>of</strong> the microcapsules. Numbers <strong>of</strong> living<br />
cells were counted and expressed as percentages.<br />
Induction <strong>of</strong> AHF and cell transplantation<br />
Sprague-Dawley rats were purchased from the Experimental<br />
Animal Center <strong>of</strong> Southern Medical University<br />
(Guangzhou, China). The Scientific Committee at Peking<br />
University Shenzhen Hospital approved the use <strong>of</strong><br />
animals for experimental purposes. Forty-eight hours<br />
before transplantation, the Sprague-Dawley rats (weight:<br />
180-250 g) were intraperitoneally injected at 1.4 g/kg<br />
with a 10% D-galactosamine solution in normal saline.<br />
On the day <strong>of</strong> the experiment, microencapsulated cells at<br />
a density <strong>of</strong> 2 × 10 6 cells/mL were prepared and transplanted<br />
into the abdominal cavity <strong>of</strong> rats. Transplantation<br />
with PBS only or unencapsulated hepatocyte-like<br />
cells were performed for the establishment <strong>of</strong> control<br />
groups. As UCB samples are not delivered on the same<br />
day, animal experiments were carried out by batch and<br />
the transplantation <strong>of</strong> cells performed also on different<br />
days. The mortality rate, hepatic pathological changes<br />
and serum biochemical indexes were determined.<br />
AHF rats grouping<br />
We obtained total 135 AHF rats 48 h after injection <strong>of</strong><br />
D-galactosamine. They were divided into three groups<br />
on the day <strong>of</strong> the transplantation. Namely, encapsulated<br />
group (transplantation with encapsulated hepatic-like<br />
cells, n = 55), unencapsulated group (transplantation with<br />
unencapsulated hepatic-like cells, n = 40), PBS group<br />
(transplantation with PBS, n = 40). Among these, 76 AHF<br />
rats were determined for hepatic pathological changes and<br />
WJG|www.wjgnet.com<br />
serum biochemical indexes (encapsulated group, n = 36;<br />
unencapsulated group, n = 20; PBS group, n = 20). The<br />
remaining 59 rats were determined for mortality rate (encapsulated<br />
group, n = 19; unencapsulated group, n = 20;<br />
PBS group, n = 20).<br />
Histology<br />
The liver and greater omentum from all three groups<br />
were fixed in 4% buffered formaldehyde overnight. After<br />
paraffin embedding, 4-5-μm thick serial sections were<br />
stained with hematoxylin and eosin (HE) and observed<br />
under the light microscope.<br />
Statistical analysis<br />
Data were expressed as the mean ± SD. Mortality rate<br />
analysis was determined by Fisher’s exact test. Serum<br />
biochemical index statistical analysis was performed by<br />
ANOVA using SPSS version 13.0 (SPSS Inc., Chicago,<br />
IL, USA). Differences with P values < 0.05 were considered<br />
statistically significant.<br />
RESULTS<br />
Differentiation <strong>of</strong> CD34 + cells into hepatic-like cells<br />
Approximately 3 × 10 5 -9 × 10 5 /mL sorted cells were obtained<br />
using the CD34 immunomagnetic bead method, and<br />
91% <strong>of</strong> them expressed CD34 by flow cytometry analysis<br />
(Figure 1). CD34 + cells were firstly amplified 20-fold by a<br />
combination <strong>of</strong> TPO, SCF and Flt-3, and then they were<br />
cultured with HGF and FGF4. At 16 d, they developed<br />
larger volumes, richer cytoplasts, and binucleated structures,<br />
as observed under a H<strong>of</strong>fman microscope (Figure 2).<br />
The RT-PCR showed no human albumin, α-fetoprotein<br />
(AFP) and GATA-4 mRNA expression in CD34 + cells<br />
before the induction procedure. The expression <strong>of</strong> albumin<br />
and GATA-4 mRNA increased with the culture time<br />
after the addition <strong>of</strong> growth factors, whereas the amount<br />
<strong>of</strong> AFP mRNA expression peaked after 8 d and reduced<br />
at 16 d (Figure 3). Cells that expressed albumin and AFP<br />
were verified by immunocytochemical staining and ELISA<br />
(Figures 2 and 4). The percentage <strong>of</strong> albumin- and AFPpositive<br />
cells at 16 d was 30% and 24%, respectively. The<br />
albumin product in culture medium was significantly<br />
increased after culturing with HGF and FGF4 in comparison<br />
with control groups (P < 0.01).<br />
Cell encapsulation and transplantation<br />
The APA microencapsulation technique was used to encapsulate<br />
hepatic-like cells. The percentage <strong>of</strong> living cells<br />
was > 80%, as determined by trypan blue staining. The<br />
AHF animal model was successfully established using<br />
Sprague-Dawley rats by the injection <strong>of</strong> D-galactosamine.<br />
Pathological section <strong>of</strong> the AHF liver revealed that the<br />
structure <strong>of</strong> the hepatic lobules was destroyed and the<br />
hepatic cord was disordered, with large areas <strong>of</strong> denatured<br />
and necrotic hepatocytes, and infiltrating lymphocytes<br />
were found on the portal area at 48 h after injection. On<br />
the day <strong>of</strong> the experiment, microencapsulated cells at a<br />
density <strong>of</strong> 2 × 10 6 cells/mL were prepared and transplant-<br />
940 February 21, 2011|Volume 17|Issue 7|
A<br />
SS<br />
0 1023<br />
ed into the abdominal cavity <strong>of</strong> AHF rats. The mortality<br />
rate and hepatic pathological changes were determined.<br />
At 48 h after transplantation, HE staining <strong>of</strong> the encapsulated<br />
group revealed that the hepatic lobules were still<br />
intact; denaturation was the major change in hepatocytes<br />
and the area <strong>of</strong> necrosis nidus was small, and congestion<br />
and hemorrhage were almost undetectable (Figure 5). The<br />
mortality rate at 48 h after transplantation in three groups<br />
was 42.1% (encapsulated group), 65% (unencapsulated<br />
group) and 75% (PBS group), respectively. Compared<br />
with the unencapsulated group, the mortality rate <strong>of</strong> the<br />
encapsulated group was significantly lower (P < 0.05). In<br />
addition, the serum biochemical indexes <strong>of</strong> ALT, AST<br />
and total bilirubin in the microencapsulated group differed<br />
significantly from those in the PBS group (P < 0.01)<br />
WJG|www.wjgnet.com<br />
C<br />
91.2%<br />
10 0 10 1<br />
CD34-PE<br />
10 2<br />
10 3<br />
FS<br />
10 0 10 1<br />
Figure 1 FACS determination <strong>of</strong> CD34 + cells. A: Purity <strong>of</strong> CD34 + cells; B: Homotypic control cells.<br />
A B<br />
C D<br />
Zhang FT et al . Transplantation <strong>of</strong> microencapsulated hepatic-like cells<br />
B<br />
0 1023<br />
H<br />
0.2%<br />
CD34-PE<br />
50 μm 100 μm<br />
50 μm 50 μm<br />
Figure 2 Cell culture and analyses. A: After 16 d; B: A binucleated cell; C, D: Positive staining for albumin (C) and α-fetoprotein (D) after 16 d <strong>of</strong> indction.<br />
at 48 h after transplantation, but there were no differences<br />
between the encapsulated and the unencapsulated group<br />
(Table 2). At 1-2 wk post-transplantation, free microcapsules<br />
with a round clear structure and a smooth surface<br />
were observed in peritoneal lavage fluid, surviving cells<br />
in microcapsules were found by trypan blue staining, but<br />
some fibrous tissues around microcapsules were also detected<br />
in the greater omentum <strong>of</strong> encapsulated group by<br />
HE staining (Figure 6).<br />
DISCUSSION<br />
10 2<br />
With the continued increase in people with hepatic failure<br />
from cirrhosis and hepatocarcinoma, cell transplantation<br />
as an effective therapy is becoming a matter <strong>of</strong> concern<br />
941 February 21, 2011|Volume 17|Issue 7|<br />
10 3
Zhang FT et al . Transplantation <strong>of</strong> microencapsulated hepatic-like cells<br />
Table 2 Changes in serum biochemical indexes at different times<br />
48 h after<br />
injection D-GalN<br />
All 3 groups Encapsulated group Unencapsulated<br />
group<br />
ALT (U/L) 3242.3 ± 2403.24 93.93 ± 63.45 b<br />
AST (U/L) 4237.20 ± 1372.07 168.87 ± 89.33 b<br />
TBIL (μmol/L) 5.57 ± 1.86 1.73 ± 1.01 a<br />
WJG|www.wjgnet.com<br />
48 h after transplantation 7 d after transplantation<br />
PBS group Encapsulated group Unencapsulated<br />
group<br />
PBS group<br />
126.1 ± 54.35 245.9 ± 67.87 42.25 ± 11.86 45.07 ± 10.56 47.27 ± 11.08<br />
275.7 ± 52.74 439.7 ± 133.01 162.6 ± 54.29 124.52 ± 24.61 114.83 ± 16.50<br />
2.23 ± 1.98 3.50 ± 1.23 1.90 ± 0.52 2.72 ± 0.96 3.72 ± 1.18<br />
Data are shown as means ± SD. a P < 0.05; b P < 0.01, in comparison with PBS group. TBIL: total bilirubin; AST: Aspartate aminotransferase; ALT: Alanine aminotransferase.<br />
ALB<br />
GATA-4<br />
AFP<br />
GAPDH<br />
d 0 d 8 d 16<br />
Figure 3 Reverse transcription-polymerase chain reaction analysis <strong>of</strong><br />
umbilical cord blood CD34 + cells cultured in vitro d 0, d 8 and d 16. ALB:<br />
Albumin; AFP: α-fetoprotein.<br />
A B<br />
C D<br />
ALB (μg/mL) 48 h<br />
100<br />
80<br />
60<br />
40<br />
20<br />
0<br />
With growth factors<br />
Without growth factors<br />
0 8 16<br />
Figure 4 Determination <strong>of</strong> albumin expression by Enzyme-Linked Immunosorbent<br />
Assay. ALB: Albumin.<br />
100 μm 100 μm<br />
Figure 5 Pathological changes in the livers <strong>of</strong> acute hepatic failure rats. A: Liver at 48 h after injection <strong>of</strong> D-galactosamine; B: Liver at 48 h after microcapsule<br />
transplantation; C: HE staining <strong>of</strong> the liver shown in section (A); D: HE staining <strong>of</strong> the liver shown in section (B).<br />
942 February 21, 2011|Volume 17|Issue 7|<br />
t/d
A B<br />
C D<br />
for more scientists. Cell transplantation could <strong>of</strong>fer metabolic<br />
support when liver function is damaged, and extend<br />
the waiting time for a liver donor [5,6] . Hepatic cell transplantation<br />
via the peritoneum or spleen has shown good<br />
prospects in clinical and animal experiments. However,<br />
the cell sources for transplantation and the requirement<br />
for long-term immunosuppression have caused stagnation<br />
in this field.<br />
There have been some intriguing studies that have described<br />
adult stem cells displaying plasticity in recent years.<br />
These studies have led us to consider that using adult<br />
stem cells might cure diseases such as AHF [7,8] . Human<br />
UCB cells are enriched in hematopoietic stem/progenitor<br />
cells that exceed those in the bone marrow and peripheral<br />
blood. In comparison with bone marrow stem cells, UCB<br />
stem cells are even more immature and with lower immunogenicity.<br />
In our previous study, we confirmed that<br />
the conversion <strong>of</strong> UCB MNCs into hepatocytes by three<br />
different ways, namely co-culture with injured liver cells,<br />
growth-factor-assisted culture, and MNC transplantation<br />
in AHF animal models [4] . In the present study, we explored<br />
the possibility that CD34 + cells derived from human UCB<br />
could be converted into hepatic-like cells. At present, the<br />
curative effect <strong>of</strong> hepatic-like cells derived from CD34 +<br />
cells in the bone marrow has already been confirmed by<br />
in vivo animal experiments [9-12] . This showed that an AHF<br />
model was initially set up using immunodeficient mice,<br />
and CD34 + cells enriched by immunobeads were injected<br />
through the tail vein or portal vein into the model animals.<br />
Expression <strong>of</strong> differentiation markers <strong>of</strong> donor cells in<br />
WJG|www.wjgnet.com<br />
Zhang FT et al . Transplantation <strong>of</strong> microencapsulated hepatic-like cells<br />
500 μm 200 μm<br />
200 μm 100 μm<br />
Figure 6 Encapsules observation. A: Microcapsules created by the Alginate-poly-l-lysine-alginate microencapsulation method; B: Microcapsule masses in the peritoneal<br />
lavage fluid; C: Free microcapsules in the peritoneal lavage fluid; D: HE staining shows microcapsules in the greater omentum.<br />
recipient livers at different times after transplantation was<br />
determined by fluorescence in situ hybridization, immunohistochemistry<br />
and molecular biological techniques. It<br />
was found that stress-induced signals, such as increased<br />
expression <strong>of</strong> stromal-cell-derived factor 1, matrix metalloproteinase-9<br />
and HGF, recruits human CD34 + progenitors<br />
with hematopoietic and/or hepatic-like potential to<br />
the liver <strong>of</strong> NOD/SCID mice [13] . Furthermore, another<br />
study has confirmed that FGF, leukemia inhibitory factor,<br />
SCF, HGF, FGF4 and oncostatin M contribute to<br />
the proliferation and/or differentiation <strong>of</strong> hepatic cells<br />
in different ways, and that combinations <strong>of</strong> these factors,<br />
especially HGF and FGF4, are necessary for human UCB<br />
cells to convert into albumin-producing cells [14] .<br />
With a combination <strong>of</strong> HGF and FGF4, we have<br />
established a 16-d culture system to induce CD34 + cell<br />
differentiation. The culture system with HGF and FGF4<br />
displays the capability to convert the CD34 + cells from human<br />
UCB into cells with hepatocyte phenotypes, as confirmed<br />
by RT-PCR, immunohistochemical staining, and<br />
ELISA. Moreover, the positive ratio <strong>of</strong> albumin-containing<br />
cells by immunocytochemical staining was about 30%,<br />
which is consistent with the study <strong>of</strong> Kakinuma et al [14] . All<br />
these indicate that after proliferation and differentiation,<br />
we could obtain many transplantable hepatic-like cells.<br />
Although the lower immunogenicity <strong>of</strong> UCB stem<br />
cells has advantages in heterogenic transplantation, untreated<br />
UCB cells can sometimes cause serious immune<br />
rejection. How to resolve this problem is therefore a key<br />
point for further studies. Microencapsulation <strong>of</strong>fers a<br />
943 February 21, 2011|Volume 17|Issue 7|
Zhang FT et al . Transplantation <strong>of</strong> microencapsulated hepatic-like cells<br />
possibility to overcome the difficulty. This technique uses<br />
microcapsules such as APA microcapsules to coat target<br />
cells or organs, and is beneficial for heterogenic transplantation<br />
because its biocompatible and semi-permeable<br />
membranes are capable <strong>of</strong> intercepting substances with<br />
molecular weights above 11 × 10 4 . Since Lim et al [15] first<br />
presented the concept <strong>of</strong> bio-microcapsules in 1980,<br />
artificial cell microcapsules as an effective barrier system<br />
for immunoprotection have been successfully applied in<br />
diabetes, parkinsonism, spinal cord injury, and peripheral<br />
nerve regeneration [15,16] .<br />
Our study examined coated hepatic-like cells derived<br />
from UCB by the APA microencapsulation technique. The<br />
obtained microcapsules exhibited a good smooth surface<br />
and integrated appearance. Furthermore, living cells inside<br />
the microcapsules were > 80% as determined by trypan<br />
blue staining. The mortality rate <strong>of</strong> AHF rats transplanted<br />
with microencapsulated hepatic-like cells significantly decreased<br />
in comparison with AHF rats transplanted with<br />
unencapsulated cells. In addition, there were significantly<br />
better outcomes in serum biochemical indexes such as<br />
ALT, AST and total bilirubin in the encapsulated group<br />
than in the PBS group, but no differences were observed<br />
between the encapsulated and the unencapsulated groups.<br />
Liver pathological staining supported these findings. The<br />
reason why the latter two groups showed no difference requires<br />
further exploration, although it is possibly related to<br />
the lower number <strong>of</strong> encapsulated cells. There have been<br />
some studies to support the notion that microcapsules<br />
provide the encapsulated cells with a good living space,<br />
and can significantly increase their survival time, therefore,<br />
we could theoretically reduce the number <strong>of</strong> transplanted<br />
cells [17] . Our data suggest that the transplantation <strong>of</strong> microencapsulated<br />
hepatic-like cells could <strong>of</strong>fer a metabolic<br />
support to AHF rats in the short term, but it is not sufficient<br />
to interrupt or repair the damage <strong>of</strong> the recipient<br />
hepatocytes.<br />
In our study, the pathological staining clearly showed<br />
liver recovery at 7 d after induction <strong>of</strong> AHF with D-galactosamine.<br />
At 2 wk post-transplantation, the morphological<br />
form <strong>of</strong> free microcapsules could be observed in the<br />
peritoneal lavage fluid, and showed round clear structures<br />
and smooth surfaces, and some microcapsule fragments<br />
were observed as well. HE staining revealed that some<br />
microcapsules attached to the greater omentum exhibited<br />
lymphocyte invasion surrounded with fibrous tissues.<br />
Although transplantation <strong>of</strong> microencapsulated hepaticlike<br />
cells could preliminarily alleviate the symptoms <strong>of</strong><br />
AHF rats, their short lifespan and varying stability are<br />
still problems for the further use <strong>of</strong> the technique. The<br />
improvement in the airflow encapsulation system might<br />
be considered to yield sufficient uniformity in the size <strong>of</strong><br />
microcapsules [18] .<br />
Transplantation <strong>of</strong> microencapsulated cells could<br />
provide a temporary metabolic support to AHF patients<br />
and/or be a transitional treatment, because its mechanism<br />
is not only related to the immunosuppressive and substitution<br />
effects <strong>of</strong> the transplanted cells, but is also associated<br />
WJG|www.wjgnet.com<br />
with liver repair promoted by the transplanted cells. This<br />
new approach could provide a potential alternative for severe<br />
liver diseases.<br />
COMMENTS<br />
Background<br />
With the continued increase in people with hepatic failure from cirrhosis and<br />
hepatocarcinoma, cell transplantation could <strong>of</strong>fer metabolic support when liver<br />
function is damaged, and extend the waiting time for a liver donor. However, the<br />
cell sources for transplantation and the requirement for long-term immunosuppression<br />
have caused stagnation in this field.<br />
Research frontiers<br />
Alginate-poly-l-lysine-alginate (APA) microcapsules have been proved effective<br />
in protecting enclosed target cells from immune rejection following transplantation<br />
into experimental animals. Many studies have been conducted on the cell<br />
sources such as liver stem cells, embryonic stem cells, umbilical cord blood<br />
(UCB) cells and bone marrow stem cells.<br />
Innovations and breakthroughs<br />
The research team led by Pr<strong>of</strong>essor Yu has established an artificial cell microcapsules<br />
platform, which is based on APA microcapsule technology and stem cell<br />
differentiation, to study the therapeutic effects <strong>of</strong> intraperitoneal transplantation <strong>of</strong><br />
microencapsulated hepatic-like cells derived from UCB cells on AHF in rats. The<br />
effective immunoprotectivity <strong>of</strong> artificial cell microcapsules has been observed in<br />
this study, which suggests that the transplantation <strong>of</strong> microencapsulated hepaticlike<br />
cells could <strong>of</strong>fer a metabolic support to AHF rats in the short term, but it is not<br />
yet sufficient to interrupt or repair the damage <strong>of</strong> the recipient hepatocytes.<br />
Applications<br />
Transplantation <strong>of</strong> microencapsulated cells could provide a temporary metabolic<br />
support to AHF patients and/or be used as a transitional treatment. This new<br />
approach could provide a potential alternative for severe liver diseases.<br />
Terminology<br />
UCB was obtained from full-term deliveries at the Obstetrics Department <strong>of</strong> Peking<br />
University Shenzhen Hospital. Hepatic-like cells were induced from UCB<br />
CD34 + cells by culturing with FGF4 and HGF. Alginate-poly-l-lysine-alginate<br />
microcapsules have biocompatibility and semi-permeable membranes, and can<br />
intercept substances with molecular weights > 1.1 × 10 5 .<br />
Peer review<br />
Zhang et al reported that CD34 + cells sorted from human UCB cells were<br />
cultured for 16 d in a specific medium and could differentiate into hepatocytelike<br />
cells. When the hepatocyte-like cells were encapsulated by alginate and<br />
intraperitoneally transplanted into rats with galactosamine-induced AHF, the<br />
number <strong>of</strong> surviving rats increased compared to that <strong>of</strong> control rats at 2 d after<br />
transplantation. Although the differentiation <strong>of</strong> CD34 + cells derived from UCB<br />
to hepatocyte-like cells has been reported, it is interesting to use the peritoneal<br />
injection <strong>of</strong> alginate-encapsulated hepatocyte-like cells for the alleviation <strong>of</strong><br />
AHF. If the preserved UCB cells are used for the treatment <strong>of</strong> AHF and related<br />
diseases, it will be beneficial to the patients.<br />
REFERENCES<br />
1 Sun Y, Ma X, Zhou D, Vacek I, Sun AM. Normalization <strong>of</strong><br />
diabetes in spontaneously diabetic cynomologus monkeys<br />
by xenografts <strong>of</strong> microencapsulated porcine islets without<br />
immunosuppression. J Clin Invest 1996; 98: 1417-1422<br />
2 Chang TM. Therapeutic applications <strong>of</strong> polymeric artificial<br />
cells. Nat Rev Drug Discov 2005; 4: 221-235<br />
3 Orive G, Hernández RM, Gascón AR, Calafiore R, Chang<br />
TM, De Vos P, Hortelano G, Hunkeler D, Lacík I, Shapiro<br />
AM, Pedraz JL. Cell encapsulation: promise and progress.<br />
Nat Med 2003; 9: 104-107<br />
4 Zhang FT, Fang JZ, Yu J, Wan HJ, Ye J, Long X, Yin MJ,<br />
Huang CQ. Conversion <strong>of</strong> mononuclear cells from human<br />
umbilical cord blood into hepatocyte-like cells. Junyi Daxue<br />
Xuebao 2006; 21: 358-364<br />
5 Petersen BE, Bowen WC, Patrene KD, Mars WM, Sullivan<br />
AK, Murase N, Boggs SS, Greenberger JS, G<strong>of</strong>f JP. Bone<br />
944 February 21, 2011|Volume 17|Issue 7|
marrow as a potential source <strong>of</strong> hepatic oval cells. Science<br />
1999; 284: 1168-1170<br />
6 Theise ND, Badve S, Saxena R, Henegariu O, Sell S, Crawford<br />
JM, Krause DS. Derivation <strong>of</strong> hepatocytes from bone<br />
marrow cells in mice after radiation-induced myeloablation.<br />
Hepatology 2000; 31: 235-240<br />
7 Teratani T, Yamamoto H, Aoyagi K, Sasaki H, Asari A,<br />
Quinn G, Sasaki H, Terada M, Ochiya T. Direct hepatic fate<br />
specification from mouse embryonic stem cells. Hepatology<br />
2005; 41: 836-846<br />
8 Sakaida I, Terai S, Nishina H, Okita K. Development <strong>of</strong> cell<br />
therapy using autologous bone marrow cells for liver cirrhosis.<br />
Med Mol Morphol 2005; 38: 197-202<br />
9 Wang X, Ge S, McNamara G, Hao QL, Crooks GM, Nolta<br />
JA. Albumin-expressing hepatocyte-like cells develop in the<br />
livers <strong>of</strong> immune-deficient mice that received transplants <strong>of</strong><br />
highly purified human hematopoietic stem cells. Blood 2003;<br />
101: 4201-4208<br />
10 Newsome PN, Johannessen I, Boyle S, Dalakas E, McAulay<br />
KA, Samuel K, Rae F, Forrester L, Turner ML, Hayes PC,<br />
Harrison DJ, Bickmore WA, Plevris JN. Human cord bloodderived<br />
cells can differentiate into hepatocytes in the mouse<br />
liver with no evidence <strong>of</strong> cellular fusion. Gastroenterology<br />
2003; 124: 1891-1900<br />
11 Ishikawa F, Drake CJ, Yang S, Fleming P, Minamiguchi H,<br />
Visconti RP, Crosby CV, Argraves WS, Harada M, Key LL<br />
Jr, Livingston AG, Wingard JR, Ogawa M. Transplanted human<br />
cord blood cells give rise to hepatocytes in engrafted<br />
mice. Ann N Y Acad Sci 2003; 996: 174-185<br />
WJG|www.wjgnet.com<br />
Zhang FT et al . Transplantation <strong>of</strong> microencapsulated hepatic-like cells<br />
12 Danet GH, Luongo JL, Butler G, Lu MM, Tenner AJ, Simon<br />
MC, Bonnet DA. C1qRp defines a new human stem cell<br />
population with hematopoietic and hepatic potential. Proc<br />
Natl Acad Sci USA 2002; 99: 10441-10445<br />
13 Kollet O, Shivtiel S, Chen YQ, Suriawinata J, Thung SN,<br />
Dabeva MD, Kahn J, Spiegel A, Dar A, Samira S, Goichberg<br />
P, Kalinkovich A, Arenzana-Seisdedos F, Nagler A, Hardan I,<br />
Revel M, Shafritz DA, Lapidot T. HGF, SDF-1, and MMP-9<br />
are involved in stress-induced human CD34+ stem cell recruitment<br />
to the liver. J Clin Invest 2003; 112: 160-169<br />
14 Kakinuma S, Tanaka Y, Chinzei R, Watanabe M, Shimizu-<br />
Saito K, Hara Y, Teramoto K, Arii S, Sato C, Takase K,<br />
Yasumizu T, Teraoka H. Human umbilical cord blood as a<br />
source <strong>of</strong> transplantable hepatic progenitor cells. Stem Cells<br />
2003; 21: 217-227<br />
15 Lim F, Sun AM. Microencapsulated islets as bioartificial endocrine<br />
pancreas. Science 1980; 210: 908-910<br />
16 Kim YT, Hitchcock R, Broadhead KW, Messina DJ, Tresco<br />
PA. A cell encapsulation device for studying soluble factor<br />
release from cells transplanted in the rat brain. J Control Release<br />
2005; 102: 101-111<br />
17 Wang YF, Xue YL, Nan X, Liang F, Luo Y, Li YL, Gao YH,<br />
Yue W, Pei XT. [Sustainment <strong>of</strong> hepatocyte function with<br />
mixed cellular co-encapsulation]. Zhonghua Yixue Zazhi<br />
2005; 85: 2481-2486<br />
18 Shito M, Balis UJ, Tompkins RG, Yarmush ML, Toner M. A<br />
fulminant hepatic failure model in the rat: involvement <strong>of</strong><br />
interleukin-1beta and tumor necrosis factor-alpha. Dig Dis<br />
Sci 2001; 46: 1700-1708<br />
S- Editor Sun H L- Editor Kerr C E- Editor Ma WH<br />
945 February 21, 2011|Volume 17|Issue 7|
Online Submissions: http://www.wjgnet.com/1007-9327<strong>of</strong>fice<br />
wjg@wjgnet.com<br />
doi:10.3748/wjg.v17.i7.946<br />
Primary clear cell carcinoma in the liver: CT and MRI<br />
findings<br />
Qing-Yu Liu, Hai-Gang Li, Ming Gao, Xiao-Feng Lin, Yong Li, Jian-Yu Chen<br />
Qing-Yu Liu, Ming Gao, Xiao-Feng Lin, Yong Li, Jian-Yu<br />
Chen, Department <strong>of</strong> Radiology, The Second Affiliated Hospital<br />
<strong>of</strong> Sun Yat-sen University, Guangzhou 510120, Guangdong Province,<br />
China<br />
Hai-Gang Li, Department <strong>of</strong> Pathology, The Second Affiliated<br />
Hospital <strong>of</strong> Sun Yat-sen University, Guangzhou 510120,<br />
Guangdong Province, China<br />
Author contributions: Liu QY designed the study and wrote the<br />
manuscript; Gao M, Li Y and Chen JY contributed to the analysis<br />
and interpretation <strong>of</strong> data; Li HG performed the pathological<br />
analysis; Lin XF contributed to the statistical analysis.<br />
Correspondence to: Qing-Yu Liu, PhD, Department <strong>of</strong> Radiology,<br />
The Second Affiliated Hospital <strong>of</strong> Sun Yat-sen University,<br />
107 Yan Jiang Xi Road, Guangzhou 510120, Guangdong Province,<br />
China. liu.qingyu@163.com<br />
Telephone: +86-20-81332243 Fax: +86-20-81332702<br />
Received: August 29, 2010 Revised: December 1, 2010<br />
Accepted: December 8, 2010<br />
Published online: February 21, 2011<br />
Abstract<br />
AIM: To retrospectively analyze the computed tomography<br />
(CT) and magnetic resonance imaging (MRI) appearances<br />
<strong>of</strong> primary clear cell carcinoma <strong>of</strong> the liver (PCCCL)<br />
and compare the imaging appearances <strong>of</strong> PCCCL and common<br />
type hepatocellular carcinoma (CHCC) to determine<br />
whether any differences exist between the two groups.<br />
METHODS: Twenty cases with pathologically proven<br />
PCCCL and 127 cases with CHCC in the Second Affiliated<br />
Hospital <strong>of</strong> Sun Yat-sen University were included in<br />
this study. CT or MRI images from these patients were<br />
retrospectively analyzed. The following imaging findings<br />
were reviewed: the presence <strong>of</strong> liver cirrhosis, tumor<br />
size, the enhancement pattern on dynamic contrast<br />
scanning, the presence <strong>of</strong> pseudo capsules, tumor rupture,<br />
portal vein thrombosis and lymph node metastasis.<br />
RESULTS: Both PCCCL and CHCC were prone to occur<br />
in patients with liver cirrhosis, the association rate <strong>of</strong><br />
liver cirrhosis was 80.0% and 78.7%, respectively (P ><br />
WJG|www.wjgnet.com<br />
<strong>World</strong> J Gastroenterol 2011 February 21; 17(7): 946-952<br />
ISSN 1007-9327 (print) ISSN 2219-2840 (online)<br />
© 2011 Baishideng. All rights reserved.<br />
0.05). The mean sizes <strong>of</strong> PCCCL and CHCC tumors were<br />
(7.28 ± 4.25) cm and (6.96 ± 3.98) cm, respectively.<br />
Small HCCs were found in 25.0% (5/20) <strong>of</strong> PCCCL and<br />
19.7% (25/127) <strong>of</strong> CHCC cases. No significant differences<br />
in mean size and ratio <strong>of</strong> small HCCs were found<br />
between the two groups (P = 0.658 and 0.803, respectively).<br />
Compared with CHCC patients, PCCCL patients<br />
were more prone to form pseudo capsules (49.6% vs<br />
75.0%, P = 0.034). Tumor rupture, typical HCC enhancement<br />
patterns and portal vein tumor thrombosis<br />
were detected in 15.0% (3/20), 72.2% (13/18) and<br />
20.0% (4/20) <strong>of</strong> patients with PCCCL and 3.1% (4/127),<br />
83.6% (97/116) and 17.3% (22/127) <strong>of</strong> patients with<br />
CHCC, respectively. There were no significant differences<br />
between the two groups (all P > 0.05). No patients<br />
with PCCCL and 2.4% (3/127) <strong>of</strong> patients with CHCC<br />
showed signs <strong>of</strong> lymph node metastasis (P > 0.05).<br />
CONCLUSION: The imaging characteristics <strong>of</strong> PCCCL<br />
are similar to those <strong>of</strong> CHCC and could be useful for differentiating<br />
these from other liver tumors (such as hemangioma<br />
and hepatic metastases). PCCCLs are more<br />
prone than CHCCs to form pseudo capsules.<br />
© 2011 Baishideng. All rights reserved.<br />
BRIEF ARTICLE<br />
Key words: Clear cell carcinoma; Hepatocellular carcinoma;<br />
Pathology; Magnetic resonance imaging; Computed<br />
Tomography; X-ray<br />
Peer reviewers: C Triantopoulou, MD, PhD, Head <strong>of</strong> Radiology<br />
Department, Konstantopouleio general Hospital, 3-5, Agias Olgas<br />
street, 14233 N. Ionia, Athens, Greece; Hiroshi Yoshida, Associate<br />
Pr<strong>of</strong>essor, Department <strong>of</strong> Surgery, Nippon Medical School<br />
Tama Nagayama Hospital, 1-7-1 Nagayama, Tama-city, Tokyo,<br />
206-8512, Japan<br />
Liu QY, Li HG, Gao M, Lin XF, Li Y, Chen JY. Primary clear<br />
cell carcinoma in the liver: CT and MRI findings. <strong>World</strong> J<br />
Gastroenterol 2011; 17(7): 946-952 Available from: URL:<br />
http://www.wjgnet.com/1007-9327/full/v17/i7/946.htm DOI:<br />
http://dx.doi.org/10.3748/wjg.v17.i7.946<br />
946 February 21, 2011|Volume 17|Issue 7|
INTRODUCTION<br />
Hepatocellular carcinoma (HCC) is the most common<br />
primary malignant tumor <strong>of</strong> the liver. It can be classified<br />
according to its histological architecture or cytological<br />
features. HCC includes various cytological types; the less<br />
common ones are clear cell type, spindle cell type, giant<br />
cell type, small cell type and squamous cell type [1,2] . Primary<br />
clear cell carcinoma <strong>of</strong> the liver (PCCCL) is rare, with a<br />
frequency varying between 2.2% and 6.7% among HCCs<br />
reported in the published literatures [3,4] . Due to the accumulation<br />
<strong>of</strong> glycogens and/or fats, the PCCCL cell cytoplasm<br />
is clear to hematoxylin-eosin staining. PCCCL may<br />
pose a diagnostic dilemma even with histological evaluation<br />
because the morphology <strong>of</strong> PCCCL cells is similar<br />
to that <strong>of</strong> extrahepatic clear cell tumors, such as clear cell<br />
<strong>cancer</strong>s <strong>of</strong> the kidneys, adrenal glands, ovaries, thyroid, endometrium,<br />
uterine cervix, and vagina [5,6] . PCCCLs should<br />
be differentiated from metastatic clear cell <strong>cancer</strong> because<br />
their treatment strategies and prognoses are quite different.<br />
The prognosis <strong>of</strong> PCCCL is generally considered better<br />
than that <strong>of</strong> the common type <strong>of</strong> HCC (CHCC) [3,7,8] .<br />
Computed tomography (CT) and magnetic resonance<br />
imaging (MRI) are important examinations for the detection<br />
and characterization <strong>of</strong> liver tumors [9,10] . To our<br />
knowledge, the imaging features <strong>of</strong> PCCCL have rarely<br />
been reported in the English literature [11] . The purpose<br />
<strong>of</strong> this study was to describe the CT and MRI findings<br />
<strong>of</strong> PCCCL and compare them to CHCC to determine<br />
whether any differences exist between the two groups.<br />
MATERIALS AND METHODS<br />
Patients<br />
Between January 2005 and August 2009, a total <strong>of</strong> 570<br />
patients with primary HCC underwent hepatectomy at<br />
the Second Affiliated Hospital <strong>of</strong> Sun Yat-sen University.<br />
Twenty (3.5%) <strong>of</strong> these patients had pathologically confirmed<br />
PCCCL. The participants <strong>of</strong> this study included<br />
20 patients with PCCCL and 127 patients with CHCC<br />
(randomly selected from the other 550 cases <strong>of</strong> primary<br />
HCC). No patient had received preoperative treatment,<br />
such as interventional therapy or chemotherapy.<br />
Of the 20 patients with PCCCL, 14 had right upper<br />
abdominal pain, two complained <strong>of</strong> fatigue and four were<br />
asymptomatic. All patients with PCCCL were positive for<br />
HBsAg, and two were positive for anti-hepatitis C virus-<br />
IgG. The serum concentration <strong>of</strong> α-fetoprotein (AFP)<br />
was 5.8-68 787.0 μg/L for PCCCL patients, with a median<br />
<strong>of</strong> 149.9 μg/L. Of the 20 patients with PCCCL, 17 were<br />
AFP-positive (> 25 μg/L).<br />
Pathologic examinations were retrospectively reviewed<br />
by an experienced pathologist. According to diagnostic<br />
criteria generally accepted by pathologists in China,<br />
PCCCL was diagnosed when clear cells accounted for<br />
more than 50% <strong>of</strong> the tumor [1,3,4,12] .<br />
Imaging protocols<br />
CT or MRI examinations were performed no more than 5<br />
WJG|www.wjgnet.com<br />
Liu QY et al . Primary clear cell carcinoma in the liver<br />
days before hepatectomy. Thirteen patients with PCCCL<br />
and 73 patients with CHCC underwent dynamic CT examination<br />
using a spiral CT scanner (HiSpeed NX/I; GE<br />
Medical Systems, Milwaukee, WI) or a multi-detector CT<br />
scanner (Sensation 64; Siemens Medical Solutions, Erlangen,<br />
Germany). The scan parameters were as follows: 5-<br />
7 mm slice thickness reconstructions, 120-kV, 220-400<br />
mA current, 25 cm field <strong>of</strong> view, and 256 × 256 matrix.<br />
Scans began at the dome <strong>of</strong> the diaphragm and proceeded<br />
in a caudal direction. After pre-contrast CT scans, the patients<br />
underwent dynamic contrast-enhanced scans. A bolus<br />
injection <strong>of</strong> 80-100 mL <strong>of</strong> non-ionic contrast medium<br />
(Iopamidol, Bracco, Milano, Italy) with a concentration <strong>of</strong><br />
350 mg I/mL was given via the antecubital vein at a rate<br />
<strong>of</strong> 3.5 mL/s. Images <strong>of</strong> the hepatic arterial phase (HAP),<br />
portal venous phase (PVP) and equilibrium phase (EP)<br />
were obtained at 25 s, 70 s and 120 s, respectively, after the<br />
injection <strong>of</strong> contrast agent.<br />
Seven patients with PCCCL and 54 patients with<br />
CHCC underwent MRI studies with a 1.5-T MR unit<br />
(Gyroscan Intera, Philips Medical System, Best, the Netherlands).<br />
Unenhanced MR images included T1-weighted<br />
images with a water-selective excitation technique (FFE,<br />
TR 218ms, TE 4.9 ms, flip angle <strong>of</strong> 80, one acquisition)<br />
and turbo spin-echo T2-weighted images with fat saturation<br />
(TR 1600 ms, TE 70 ms, TSE Factor 24, three acquisitions).<br />
Five patients with PCCCL and 43 patients with<br />
CHCC underwent dynamic contrast-enhanced MR scans<br />
using a high-resolution turbo spin-echo sequence (TR<br />
5.3 ms, TE 1.4 ms, flip angle <strong>of</strong> 40, 3.0-mm slice thickness,<br />
no gap, one acquisition) via a power injector; contrast<br />
agent was administrated at a rate <strong>of</strong> 2.5 mL/sec.<br />
HAP, PVP and EP scans were obtained at 20, 60, and 110 s,<br />
respectively. The other 13 patients (2 with PCCCL and 11<br />
with CHCC) received manual injections <strong>of</strong> gadopentetate<br />
dimeglumine (Magnevist, Bayer Schering, Berlin, Germany)<br />
at a dose <strong>of</strong> 0.1 mmol/kg; post-contrast T1-weighted<br />
images were obtained at PVP (60-80 s after injection) with<br />
the same scanning parameters as the pre-contrast T1W<br />
scan. Regardless <strong>of</strong> the technique employed, axial and<br />
coronal images were acquired with 5.0-mm slice thickness.<br />
Image interpretation<br />
The CT and MRI images were retrospectively analyzed by<br />
two radiologists who have 10 and 15 years <strong>of</strong> experience<br />
in diagnosing abdominal diseases. Neither radiologist was<br />
aware <strong>of</strong> the patients’ clinicopathological data. Reviews<br />
were performed jointly and by consensus. The presence<br />
<strong>of</strong> liver cirrhosis, tumor size, the enhancement pattern<br />
on dynamic contrast scanning, the presence <strong>of</strong> pseudocapsule,<br />
tumor rupture, portal vein thrombus, and lymph<br />
node metastasis were recorded. A typical HCC enhancement<br />
pattern was defined as early enhancement at HAP<br />
and rapid contrast medium washout at PVP or EP with<br />
hypo-attenuation/intense signal or iso-attenuation/intense<br />
signal [9,10] .<br />
Statistical analysis<br />
Differences in mean age and tumor size were assessed<br />
947 February 21, 2011|Volume 17|Issue 7|
Liu QY et al . Primary clear cell carcinoma in the liver<br />
with an independent-samples t test. Differences in the<br />
frequencies <strong>of</strong> liver cirrhosis, tumor capsule formation,<br />
tumor rupture, typical enhancement pattern, portal vein<br />
tumor thrombus and lymph node metastases between the<br />
two groups were compared using the Chi-squared test or<br />
Fischer’s exact test. A P value <strong>of</strong> 0.05 or less was considered<br />
significant. Statistical analysis was performed using the<br />
SPSS 13.0 s<strong>of</strong>tware package (SPSS Inc., Chicago, IL, USA).<br />
RESULTS<br />
The male-to-female ratio was 4.0:1 in the PCCCL group<br />
and 6.1:1 in the CHCC group. The mean age was 52.00<br />
± 10.09 years (range, 29-66 years) in the PCCCL group<br />
and 51.82 ± 13.20 years (range, 19-83 years) in the CHCC<br />
group. There were no statistical differences between the<br />
two groups regarding sex or age (P = 0.733 and P = 0.953,<br />
respectively).<br />
Table 1 summarizes the imaging features observed in patients<br />
with PCCCL and patients with CHCC. Both PCCCL<br />
and CHCC were prone to occur in patients with liver cirrhosis,<br />
with a rate <strong>of</strong> 80.0% and 78.7%, respectively. The mean<br />
sizes <strong>of</strong> PCCCLs and CHCCs were 7.28 ± 4.25 cm (range,<br />
2.0-15.9 cm), and 6.96 ± 3.98 cm (range, 1.0-17.0 cm),<br />
respectively. Small HCCs with diameters ≤ 3.0 cm were<br />
found in 25.0% (5/20) <strong>of</strong> PCCCL cases and 19.7% (25/127)<br />
<strong>of</strong> CHCC cases. No statistically significant differences in<br />
mean size or ratio <strong>of</strong> small HCC were found between the<br />
two groups (P = 0.658 and 0.803, respectively). Compared<br />
with CHCCs, PCCCLs were more prone to form pseudo<br />
capsules, with a rate <strong>of</strong> 49.6% and 75.0%, respectively (P =<br />
0.034). Pseudo capsules showed hypo-attenuation/intensity<br />
haloes on pre-contrast scans and rim enhancement after<br />
contrast administration (Figures 1 and 2).<br />
A higher percentage <strong>of</strong> tumor rupture was found<br />
in patients with PCCCL (15.0%, 3/20) than in patients<br />
with CHCC (3.1%, 4/127); however, there was no significant<br />
difference between the two groups (P > 0.05).<br />
Of the 20 PCCCL cases, three showed tumor ruptures.<br />
The ruptured tumors were 15.9 cm, 10.9 cm and 9.3cm<br />
in diameter and were located at the periphery <strong>of</strong> the liver<br />
with protruding contours. Two cases presented as discontinuities<br />
<strong>of</strong> the liver surface on CT scan (Figure 1). The<br />
remaining case presented a local hematoma at the rupture<br />
site on MRI, which appeared as mixed iso-/hypo-intense<br />
signals on T1WI and hypo-intense signals on T2WI with<br />
no enhancement after injection <strong>of</strong> contrast agent.<br />
Typical HCC enhancement patterns were noted in<br />
72.2% (13/18) <strong>of</strong> PCCCLs and 83.6% (97/116) <strong>of</strong><br />
CHCCs; however, no significant difference was found<br />
between the two groups (P > 0.05) (Figures 1 and 3). The<br />
other five PCCCL cases showed atypical CT features on<br />
dynamic scan: two cases showed minimal enhancement<br />
and remained hypo-attenuated at HAP and PVP, while the<br />
other three cases showed gradual contrast enhancement<br />
during the portal phase.<br />
Four patients (20.0%) with PCCCL had portal vein<br />
tumor thrombosis: one located at the left branch <strong>of</strong> the<br />
portal vein, one at the right branch, and one at the right<br />
WJG|www.wjgnet.com<br />
Table 1 Characteristics <strong>of</strong> clear cell hepatocellular carcinoma<br />
in the liver<br />
Parameters PCCCL<br />
(n = 20)<br />
anterior branch and main portal vein. Compared with<br />
CHCC patients, PCCCL patients showed a slightly higher<br />
incidence <strong>of</strong> portal vein tumor thrombosis (17.3% and<br />
20.0%, respectively); however, there was no significant difference<br />
between the two groups (P > 0.05). No PCCCL<br />
patients and 2.4% (3/127) CHCC patients showed sign <strong>of</strong><br />
lymph node metastasis (P > 0.05).<br />
DISCUSSION<br />
CHCC<br />
(n = 127)<br />
P value<br />
Sex 0.733<br />
Male 16 109<br />
Female 4 18<br />
Liver cirrhosis 1.000<br />
Positive 16 100<br />
Negative 4 27<br />
Tumor diameter (cm) 0.803<br />
≤ 3.0 5 25<br />
> 3.0 15 102<br />
Capsule formation 0.034<br />
Positive 15 63<br />
Negative 5 64<br />
Rupture 0.053<br />
Positive 3 4<br />
Negative 17 123<br />
Typical enhancement pattern 0.399<br />
Positive 13 97<br />
Negative 5 19<br />
Portal vein tumor thrombus 1.000<br />
Positive 4 22<br />
Negative 16 105<br />
Lymph node metastases 1.000<br />
Positive 0 3<br />
Negative 20 124<br />
PCCCL: Primary clear cell carcinoma <strong>of</strong> the liver; CHCC: Common type <strong>of</strong><br />
hepatocellular carcinoma.<br />
PCCCL is a specific and rare subtype <strong>of</strong> primary HCC.<br />
The reported incidence <strong>of</strong> PCCCL is 0.4%-37%; inconsistent<br />
diagnostic criteria may be responsible for the variable<br />
reports [1,3,4,7,8,12,13] . Lai et al [7] suggested that the diagnosis<br />
<strong>of</strong> PCCCL could be made even when the proportion <strong>of</strong><br />
clear cells was < 30%, while Buchanan et al [8] suggested<br />
that PCCCL should be diagnosed when the proportion<br />
<strong>of</strong> clear cells was > 30%. Most studies diagnosed PCCCL<br />
when the proportion <strong>of</strong> clear cells was > 50% [1,3,4,12] . Using<br />
this criteria, PCCCL only accounts for 2.2%-6.7% <strong>of</strong><br />
all resectable HCCs in most reports [3,4] . Among the 570<br />
cases <strong>of</strong> primary HCC resected in our hospital, only 3.5%<br />
patients had PCCCL. The clear cell development is presumed<br />
to involve metabolic disorders and abnormalities<br />
<strong>of</strong> sugar metabolism [14,15] .<br />
The clinicopathological presentations <strong>of</strong> PCCCL were<br />
different from those <strong>of</strong> CHCC. The rates <strong>of</strong> hepatitis C<br />
infection and capsule formation were higher in PCCCL<br />
patients than in those with CHCC; however, no remarkable<br />
differences in patients’ age, sex, AFP-positive rate or<br />
948 February 21, 2011|Volume 17|Issue 7|
A<br />
C<br />
Liu QY et al . Primary clear cell carcinoma in the liver<br />
the location, number, size and grade <strong>of</strong> tumors were observed<br />
between the two groups [3] . Both tumor types were<br />
prone to occur in patients with hepatitis B, mostly on the<br />
basis <strong>of</strong> liver cirrhosis [3] . PCCCL had a better prognosis<br />
than CHCC, mainly related to capsule formation, vascular<br />
invasion, preoperative liver function and clear cell proportion<br />
[3,4,12] . Surgical resection is an effective treatment for<br />
patients with PCCCL [3,4,7] .<br />
The presence <strong>of</strong> clear cells and fatty changes characterizes<br />
well-differentiated HCC in the early <strong>stage</strong>, and their<br />
ratio is presumed to decrease as the tumor enlarges [15] . In<br />
1999, Monzawa et al [16] analyzed the pathologic and imaging<br />
changes <strong>of</strong> well-differentiated HCC; and found that<br />
some well-differentiated HCCs showed clear cell formation<br />
and/or fatty changes, which presented as high echo<br />
on ultrasound and hyper-intense signals on T1WI. However,<br />
in their study, the proportion <strong>of</strong> clear cells in the recruited<br />
HCC was less than 10%, or only 10%-50%, which<br />
did not meet the diagnosis criteria for PCCCL. In 2008,<br />
Takahashi et al [11] described CT, MR and angiographic<br />
findings <strong>of</strong> PCCCL in a woman with a normal liver. To<br />
our knowledge, no further research on the imaging manifestations<br />
<strong>of</strong> PCCCL has been conducted.<br />
Pseudocapsule formation (consisting mainly <strong>of</strong> peritumoral<br />
hepatic sinusoids and/or fibrosis) is an important<br />
gross pathologic feature <strong>of</strong> HCC. Pseudocapsule indicates<br />
a relatively positive prognosis after tumor resection [17] . Liu<br />
et al [3] found a higher ratio <strong>of</strong> pseudocapsule formation in<br />
PCCCL than in CHCC microscopically (88.4% vs 68.0%,<br />
P < 0.05); and pseudocapsule formation might be related<br />
WJG|www.wjgnet.com<br />
B<br />
D<br />
Figure 3 Primary clear cell carcinoma <strong>of</strong> the liver in a 62-year-old man. A: On pre-contrast computed tomography scan, the mass shows hypo-attenuation (arrows);<br />
B: At hepatic arterial phase, the mass shows early enhancement; C: At portal venous phase, the mass shows hypo-attenuation and thin rim enhancement (pseudocapsule);<br />
D: Microscopically, the mass is mainly composed <strong>of</strong> clear cells (HE, × 200).<br />
to a relatively lower degree <strong>of</strong> malignancy and a better<br />
prognosis for PCCCL. CT and MRI are reliable imaging<br />
examinations for the detection <strong>of</strong> HCC pseudo capsules.<br />
The pseudocapsule presents as rim enhancement on dynamic<br />
contrast scanning, and MRI is more sensitive than<br />
CT in identifying pseudocapsule [17-19] . Among the 20 cases<br />
<strong>of</strong> PCCCL in our study, 15 (75.0%) had pseudocapsule,<br />
all <strong>of</strong> which were confirmed pathologically. The percentage<br />
<strong>of</strong> pseudocapsule formation was higher in PCCCL<br />
patients than in CHCC patients (P < 0.05).<br />
Because <strong>of</strong> hypervascular blood supply, typical HCC<br />
showed early enhancement at HAP, and rapid contrast<br />
medium washout at PVP or EP with hypo-attenuation/intense<br />
signal or iso-attenuation/intense signal [9,10] . Among<br />
the 18 PCCCL cases in our study that underwent dynamic<br />
contrast CT or MRI examination, 13 presented a typical<br />
HCC enhancement pattern, indicating that the tumor is<br />
rich <strong>of</strong> blood supply. The enhancement pattern <strong>of</strong> PCCCL<br />
is not different from that <strong>of</strong> CHCC (P > 0.05). This imaging<br />
characteristic may be useful in differentiating PCCCL<br />
from other liver tumors, such as hemangioma and hepatic<br />
metastases. The other five PCCCL cases presented atypical<br />
enhancement on dynamic CT scans: two cases showed<br />
minimal enhancement with hypo-attenuation at HAP and<br />
PVP, indicating hypovascularity, and three cases showed<br />
gradual contrast enhancement during the portal phase,<br />
which may be attributable to the difference in blood supply<br />
(such as existence <strong>of</strong> small arterioportal shunts), tumor<br />
differentiation or liver cirrhosis background [20,21] .<br />
Spontaneous rupture <strong>of</strong> HCC is usually life-threaten-<br />
950 February 21, 2011|Volume 17|Issue 7|
ing but relatively uncommon, with a reported incidence<br />
<strong>of</strong> 3%-15% [22] . CT is a valuable imaging technique for<br />
diagnosing HCC ruptures. The imaging findings include:<br />
discontinuity or disruption <strong>of</strong> the liver capsule adjacent<br />
to the liver mass and hematoma with hyper-attenuation<br />
at the rupture site. The enucleation sign is a specific sign<br />
for diagnosing HCC rupture [23,24] . To our knowledge, no<br />
report on PCCCL rupture is available for review. Among<br />
the 20 PCCCL cases in our study, only three had tumor<br />
rupture: two showed discontinuity <strong>of</strong> the liver capsule on<br />
CT scans, and the other showed a hematoma at the rupture<br />
site on MRI, with iso-/hypo-intense signals on T1WI<br />
and hypo-intense signals on T2WI.<br />
Portal vein thrombosis, the characteristic growth pattern<br />
<strong>of</strong> HCC, occurs in 12.5%-39.7% <strong>of</strong> HCC patients [25] .<br />
Liu et al [3] reported that the microscopic vascular invasion<br />
rates are similar between PCCCL and CHCC (53.4% vs<br />
65.0%, P > 0.05). In our study, the incidence <strong>of</strong> macroscopic<br />
portal vein tumor thrombus in PCCCL and CHCC<br />
detected on imaging examination was not significantly different<br />
(P > 0.05). Portal vein invasion was an independent<br />
risk factor for the prognosis <strong>of</strong> patients with PCCCL [12] .<br />
Chemical shift imaging is valuable for characterizing<br />
lesions with a mixture <strong>of</strong> water and fat [26] . Renal clear<br />
cell carcinomas usually contain fat, and present focal and<br />
diffused signal loss on chemical shift imaging. This imaging<br />
technique is helpful for differentiating renal clear cell<br />
carcinoma from other types <strong>of</strong> renal <strong>cancer</strong> [27,28] . The cell<br />
morphology <strong>of</strong> PCCCL is similar to that <strong>of</strong> renal clear<br />
cell carcinoma, with cytoplasmic accumulation <strong>of</strong> glycogens<br />
and/or fat. The signal reduction <strong>of</strong> HCC during<br />
chemical shift imaging may help identify intratumoral fatty<br />
components and confirm a diagnosis <strong>of</strong> PCCCL [2] .<br />
In summary, the imaging characteristics <strong>of</strong> PCCCL are<br />
similar to those <strong>of</strong> CHCC, including early enhancement<br />
and rapid washout <strong>of</strong> contrast agent on dynamic contrast<br />
scans, and presence <strong>of</strong> portal vein thrombus or tumor rupture.<br />
These imaging features may help differentiate PCCCL<br />
from other liver tumors, such as hemangioma and hepatic<br />
metastases. Pseudocapsule formation is more likely to occur<br />
in PCCCL than in CHCC and may be related to PCCCL’s<br />
relatively lower degree <strong>of</strong> malignancy and better prognosis.<br />
COMMENTS<br />
Background<br />
Primary clear cell carcinoma <strong>of</strong> the liver (PCCCL) is a specific and rare subtype<br />
<strong>of</strong> primary hepatocellular carcinoma (HCC), with a frequency varying between<br />
2.2% and 6.7% among HCCs in the published literatures. PCCCL may pose a<br />
diagnostic dilemma even with histological sections because the morphology <strong>of</strong><br />
PCCCL cells is similar to that <strong>of</strong> metastatic clear cell tumors. As a result <strong>of</strong> the<br />
paucity <strong>of</strong> cases, available data about its imaging findings are limited.<br />
Research frontiers<br />
Imaging modalities [computed tomography (CT) and magnetic resonance imaging<br />
(MRI)] are important for the detection and characterization <strong>of</strong> liver tumors.<br />
The imaging characteristics <strong>of</strong> common type hepatocellular carcinoma (CHCC)<br />
are well documented; for example, CHCC is usually associated with liver cirrhosis,<br />
typical enhancement pattern on dynamic contrast scanning (early enhancement<br />
at hepatic arterial phase and rapid contrast medium washout at portal<br />
venous phase or equilibrium phase) and the presence <strong>of</strong> pseudocapsule. However,<br />
the imaging features <strong>of</strong> PCCCL have not been unequivocally addressed.<br />
This study clarifies the CT or MRI findings <strong>of</strong> PCCCL.<br />
WJG|www.wjgnet.com<br />
Liu QY et al . Primary clear cell carcinoma in the liver<br />
Innovations and breakthroughs<br />
The authors presented 20 surgically confirmed PCCCL cases and retrospectively<br />
analyzed their imaging findings. This study revealed that the imaging<br />
characteristics <strong>of</strong> PCCCL are similar to those <strong>of</strong> CHCC. PCCCLs are more<br />
likely to form pseudo capsules than CHCCs.<br />
Applications<br />
With a better understanding <strong>of</strong> the imaging features <strong>of</strong> PCCCL, further investigations<br />
should determine how to use imaging modalities, especially MRI, to differentiate<br />
PCCCL from CHCC or metastatic clear cell <strong>cancer</strong>. Chemical shift imaging<br />
with an MR scanner may help detect lipid component in the cytoplasm <strong>of</strong> clear<br />
cells in PCCCL.<br />
Terminology<br />
PCCCL is a rare variant <strong>of</strong> HCC. Due to the accumulation <strong>of</strong> large amounts <strong>of</strong> glycogen<br />
and/or lipids that are dissolved by routine histological processing (hematoxylineosin<br />
staining), the cytoplasm <strong>of</strong> PCCCL cells is clear. PCCCL can be diagnosed<br />
when the tumor cells are predominantly or wholly composed <strong>of</strong> clear cell cytoplasm<br />
(a proportion <strong>of</strong> clear cells > 50%). The prognosis <strong>of</strong> PCCCL is generally considered<br />
better than that <strong>of</strong> the CHCC.<br />
Peer review<br />
It is a well written paper, with interesting results.<br />
REFERENCES<br />
1 Cong WM, Zhang SH. Introduction <strong>of</strong> the rare types <strong>of</strong><br />
HCC. Chin J Pathol 2002; 31: 457-460<br />
2 Chung YE, Park MS, Park YN, Lee HJ, Seok JY, Yu JS, Kim<br />
MJ. Hepatocellular carcinoma variants: radiologic-pathologic<br />
correlation. AJR Am J Roentgenol 2009; 193: W7-W13<br />
3 Liu Z, Ma W, Li H, Li Q. Clinicopathological and prognostic<br />
features <strong>of</strong> primary clear cell carcinoma <strong>of</strong> the liver. Hepatol<br />
Res 2008; 38: 291-299<br />
4 Lao XM, Zhang YQ, Jin X, Lin XJ, Guo RP, Li GH, Li JQ. Primary<br />
clear cell carcinoma <strong>of</strong> liver--clinicopathologic features<br />
and surgical results <strong>of</strong> 18 cases. Hepatogastroenterology 2006;<br />
53: 128-132<br />
5 Murakata LA, Ishak KG, Nzeako UC. Clear cell carcinoma<br />
<strong>of</strong> the liver: a comparative immunohistochemical study with<br />
renal clear cell carcinoma. Mod Pathol 2000; 13: 874-881<br />
6 Oliveira AM, Erickson LA, Burgart LJ, Lloyd RV. Differentiation<br />
<strong>of</strong> primary and metastatic clear cell tumors in the liver<br />
by in situ hybridization for albumin messenger RNA. Am J<br />
Surg Pathol 2000; 24: 177-182<br />
7 Lai CL, Wu PC, Lam KC, Todd D. Histologic prognostic indicators<br />
in hepatocellular carcinoma. Cancer 1979; 44: 1677-1683<br />
8 Buchanan TF Jr, Huvos AG. Clear-cell carcinoma <strong>of</strong> the liver.<br />
A clinicopathologic study <strong>of</strong> 13 patients. Am J Clin Pathol<br />
1974; 61: 529-539<br />
9 Willatt JM, Hussain HK, Adusumilli S, Marrero JA. MR Imaging<br />
<strong>of</strong> hepatocellular carcinoma in the cirrhotic liver: challenges<br />
and controversies. Radiology 2008; 247: 311-330<br />
10 Jeong YY, Yim NY, Kang HK. Hepatocellular carcinoma in<br />
the cirrhotic liver with helical CT and MRI: imaging spectrum<br />
and pitfalls <strong>of</strong> cirrhosis-related nodules. AJR Am J<br />
Roentgenol 2005; 185: 1024-1032<br />
11 Takahashi A, Saito H, Kanno Y, Abe K, Yokokawa J, Irisawa<br />
A, Kenjo A, Saito T, Gotoh M, Ohira H. Case <strong>of</strong> clear-cell hepatocellular<br />
carcinoma that developed in the normal liver <strong>of</strong><br />
a middle-aged woman. <strong>World</strong> J Gastroenterol 2008; 14: 129-131<br />
12 Ji SP, Li Q, Dong H. Therapy and prognostic features <strong>of</strong> primary<br />
clear cell carcinoma <strong>of</strong> the liver. <strong>World</strong> J Gastroenterol<br />
2010; 16: 764-769<br />
13 Kashala LO, Conne B, Kalengayi MM, Kapanci Y, Frei PC,<br />
Lambert PH. Histopathologic features <strong>of</strong> hepatocellular carcinoma<br />
in Zaire. Cancer 1990; 65: 130-134<br />
14 Yang SH, Watanabe J, Nakashima O, Kojiro M. Clinicopathologic<br />
study on clear cell hepatocellular carcinoma. Pathol Int<br />
1996; 46: 503-509<br />
15 Kojiro M. Pathology <strong>of</strong> early liver <strong>cancer</strong> and similar lesions.<br />
1st ed. Tokyo: Igaku-Shoin Ltd., 1996: 35-37<br />
16 Monzawa S, Omata K, Shimazu N, Yagawa A, Hosoda K,<br />
951 February 21, 2011|Volume 17|Issue 7|
Liu QY et al . Primary clear cell carcinoma in the liver<br />
Araki T. Well-differentiated hepatocellular carcinoma: findings<br />
<strong>of</strong> US, CT, and MR imaging. Abdom Imaging 1999; 24: 392-397<br />
17 Ishigami K, Yoshimitsu K, Nishihara Y, Irie H, Asayama<br />
Y, Tajima T, Nishie A, Hirakawa M, Ushijima Y, Okamoto<br />
D, Taketomi A, Honda H. Hepatocellular carcinoma with a<br />
pseudocapsule on gadolinium-enhanced MR images: correlation<br />
with histopathologic findings. Radiology 2009; 250:<br />
435-443<br />
18 Grazioli L, Olivetti L, Fugazzola C, Benetti A, Stanga C,<br />
Dettori E, Gallo C, Matricardi L, Giacobbe A, Chiesa A. The<br />
pseudocapsule in hepatocellular carcinoma: correlation between<br />
dynamic MR imaging and pathology. Eur Radiol 1999; 9:<br />
62-67<br />
19 Ebara M, Ohto M, Watanabe Y, Kimura K, Saisho H, Tsuchiya<br />
Y, Okuda K, Arimizu N, Kondo F, Ikehira H. Diagnosis <strong>of</strong><br />
small hepatocellular carcinoma: correlation <strong>of</strong> MR imaging<br />
and tumor histologic studies. Radiology 1986; 159: 371-377<br />
20 Efremidis SC, Hytiroglou P, Matsui O. Enhancement patterns<br />
and signal-intensity characteristics <strong>of</strong> small hepatocellular<br />
carcinoma in cirrhosis: pathologic basis and diagnostic<br />
challenges. Eur Radiol 2007; 17: 2969-2982<br />
21 Hayashida M, Ito K, Fujita T, Shimizu A, Sasaki K, Tanabe M,<br />
Matsunaga N. Small hepatocellular carcinomas in cirrhosis:<br />
differences in contrast enhancement effects between helical<br />
WJG|www.wjgnet.com<br />
CT and MR imaging during multiphasic dynamic imaging.<br />
Magn Reson Imaging 2008; 26: 65-71<br />
22 Lai EC, Lau WY. Spontaneous rupture <strong>of</strong> hepatocellular carcinoma:<br />
a systematic review. Arch Surg 2006; 141: 191-198<br />
23 Choi BG, Park SH, Byun JY, Jung SE, Choi KH, Han JY. The<br />
findings <strong>of</strong> ruptured hepatocellular carcinoma on helical CT.<br />
Br J Radiol 2001; 74: 142-146<br />
24 Kim HC, Yang DM, Jin W, Park SJ. The various manifestations<br />
<strong>of</strong> ruptured hepatocellular carcinoma: CT imaging<br />
findings. Abdom Imaging 2008; 33: 633-642<br />
25 Minagawa M, Makuuchi M. Treatment <strong>of</strong> hepatocellular<br />
carcinoma accompanied by portal vein tumor thrombus.<br />
<strong>World</strong> J Gastroenterol 2006; 12: 7561-7567<br />
26 Valls C, Iannacconne R, Alba E, Murakami T, Hori M, Passariello<br />
R, Vilgrain V. Fat in the liver: diagnosis and characterization.<br />
Eur Radiol 2006; 16: 2292-2308<br />
27 Outwater EK, Bhatia M, Siegelman ES, Burke MA, Mitchell<br />
DG. Lipid in renal clear cell carcinoma: detection on opposed-phase<br />
gradient-echo MR images. Radiology 1997; 205:<br />
103-107<br />
28 Yoshimitsu K, Honda H, Kuroiwa T, Irie H, Tajima T, Jimi M,<br />
Kuroiwa K, Naito S, Masuda K. MR detection <strong>of</strong> cytoplasmic<br />
fat in clear cell renal cell carcinoma utilizing chemical shift<br />
gradient-echo imaging. J Magn Reson Imaging 1999; 9: 579-585<br />
S- Editor Tian L L- Editor Ma JY E- Editor Lin YP<br />
952 February 21, 2011|Volume 17|Issue 7|
Online Submissions: http://www.wjgnet.com/1007-9327<strong>of</strong>fice<br />
wjg@wjgnet.com<br />
www.wjgnet.com<br />
<strong>World</strong> J Gastroenterol 2011 February 21; 17(7): I<br />
ISSN 1007-9327 (print) ISSN 2219-2840 (online)<br />
© 2011 Baishideng. All rights reserved.<br />
ACKNOWLEDGMENTS<br />
Acknowledgments to reviewers <strong>of</strong> <strong>World</strong> <strong>Journal</strong> <strong>of</strong><br />
Gastroenterology<br />
Many reviewers have contributed their expertise and<br />
time to the peer review, a critical process to ensure the<br />
quality <strong>of</strong> <strong>World</strong> <strong>Journal</strong> <strong>of</strong> Gastroenterology. The editors<br />
and authors <strong>of</strong> the articles submitted to the journal are<br />
grateful to the following reviewers for evaluating the<br />
articles (including those published in this issue and<br />
those rejected for this issue) during the last editing<br />
time period.<br />
Shahab Abid, Dr., Associate Pr<strong>of</strong>essor, Department <strong>of</strong> Medicine, Aga<br />
Khan University, Stadium Road, PO Box 3500, Karachi 74800, Pakistan<br />
Hussein M Atta, MD, PhD, Department <strong>of</strong> Surgery, Faculty <strong>of</strong> Medicine,<br />
Minia University, Mir-Aswan Road, El-Minia 61519, Egypt<br />
Huijie Bian, Pr<strong>of</strong>essor, Vice-Director ,Department <strong>of</strong> Cell Biololy/Cell<br />
Engineering Research Center, Fourth Military Medical University, Xi'an<br />
710032, Shaanxi Province, China<br />
Alberto Biondi, Dr., PhD, Department <strong>of</strong> Surgery, 1st Surgical Division,<br />
Catholic University <strong>of</strong> Rome, Largo A. Gemelli 8, Rome 00168, Italy<br />
Hoon Jai Chun, MD, PhD, AGAF, Pr<strong>of</strong>essor, Department <strong>of</strong> Internal<br />
Medicine, Institute <strong>of</strong> Digestive Disease and Nutrition, Korea University<br />
College <strong>of</strong> Medicine, 126-1, Anam-dong 5-ga, Seongbuk-gu, Seoul<br />
136-705, South Korea<br />
Laurie DeLeve, Dr., University <strong>of</strong> Southern California Keck School <strong>of</strong><br />
Medicine, 2011 Zonal Avenue-HMR603, LA 90033, United States<br />
AM El-Tawil, MSc, MRCS, PhD, Department <strong>of</strong> Surgery, University<br />
Hospital <strong>of</strong> Birmingham, East Corridor, Ground Floor, Birmingham, B15<br />
2TH, United Kingdom<br />
Giammarco Fava, MD, Department <strong>of</strong> Gastroenterology, Università<br />
Politecnica delle Marche, Ancona, via Gervasoni 12, 60129 Ancona, Italy<br />
Fritz Francois, Dr., Assistant Dean for Academic Affairs and Diversity,<br />
Assistant Pr<strong>of</strong>essor <strong>of</strong> Medicine, New York University School <strong>of</strong> Medicine,<br />
423 E. 23rd St. Room 1132N, New York, NY 10010, United States<br />
Beata Jolanta Jablońska, MD, PhD, Department <strong>of</strong> Digestive Tract<br />
Surgery, University Hospital <strong>of</strong> Medical University <strong>of</strong> Silesia, Medyków 14<br />
St. 40-752 Katowice, Poland<br />
Waliul Khan, MBBs, PhD, Assistant Pr<strong>of</strong>essor, Department <strong>of</strong> Medicine,<br />
McMaster University, Room 3N5D, Health Science Center, 1200<br />
Main Street West, Hamilton, Ontario L8N 3Z5, Canada<br />
Hong Joo Kim, MD, Pr<strong>of</strong>essor, Department <strong>of</strong> Internal Medicine,<br />
WJG|www.wjgnet.com<br />
Sungkyunkwan University Kangbuk Samsung Hospital, 108, Pyung-Dong,<br />
Jongro-Ku, Seoul, 110-746, South Korea<br />
Kirk Ludwig, M.D., Associate Pr<strong>of</strong>essor <strong>of</strong> Surgery, Chief <strong>of</strong> Colo<strong>rectal</strong><br />
Surgery, Department <strong>of</strong> Surgery, Medical College <strong>of</strong> Wisconsin, 9200<br />
West Wisconsin Avenue, Milwaukee, Wisconsin, WI 53226, United States<br />
Eli Magen, Allergy and Clinical Immunology, Medicine B, Barzilai Medical<br />
Center, Ashdod 77456, Israel<br />
Ricardo Marcos, Ph.D, Lab Histology and Embryology, Institute <strong>of</strong><br />
Biomedical Sciences Abel Salazar, ICBAS, Lg Pr<strong>of</strong> Abel Salazar, 2, Porto,<br />
4099-003, Portugal<br />
Luca Morelli, MD, UO, Dr., Anatomy and Histology, Ospedale S. Chiara,<br />
Largo Medaglie d’Oro 9, Trento, 38100, Italy<br />
Tor C Savidge, PhD, Associate Pr<strong>of</strong>essor, Department <strong>of</strong> Gastroenterology<br />
& Hepatology, Galveston, TX 77555, United States<br />
Giovanni Tarantino, MD, Pr<strong>of</strong>essor, Department <strong>of</strong> Clinical and Experimental<br />
Medicine, Federico II University Medical School, VIA S. PAN-<br />
SINI, 5, Naples 80131, Italy<br />
Cesare Tosetti, MD, Department <strong>of</strong> Primary Care, Health Care Agency<br />
<strong>of</strong> Bologna Via Rosselli 21, 40046 Porretta Terme (BO), Italy<br />
Evangelos Tsiambas, MD, PhD, Cytopathologist, Lecturer in Molecular<br />
Cytopathology, Department <strong>of</strong> Pathology, Medical School, University<br />
<strong>of</strong> Athens, Ag Paraskevi Attiki, 15341, Greece<br />
Masahito Uemura, MD, Associate Pr<strong>of</strong>essor, Third Department <strong>of</strong> Internal<br />
Medicine, Nara Medical University, Shijo-cho, 840, Kashihara, Nara<br />
634-8522, Japan<br />
Lea Veijola, Consultant Gastroenterologist, Herttoniemi Hospital,<br />
Health Care <strong>of</strong> City <strong>of</strong> Helsinki, Kettutie 8, Helsinki, 00800, Finland<br />
Steven D Wexner, MD, Pr<strong>of</strong>essor <strong>of</strong> Surgery, The Cleveland Clinic Foundation<br />
Health Sciences Center <strong>of</strong> the Ohio State University, and Clinical<br />
Pr<strong>of</strong>essor, Department <strong>of</strong> Surgery, Division <strong>of</strong> General Surgery, University<br />
<strong>of</strong> South Florida College <strong>of</strong> Medicine, 21st Century Oncology Chair in<br />
Colo<strong>rectal</strong> Surgery, Chairman Department <strong>of</strong> Colo<strong>rectal</strong> Surgery, Chief <strong>of</strong><br />
Staff, Cleveland Clinic Florida, 2950 Cleveland Clinic Boulevard, Weston, FL<br />
33331, United States<br />
George Y Wu, Pr<strong>of</strong>essor, Department <strong>of</strong> Medicine, Division <strong>of</strong> Gastroenterology-Hepatology,<br />
University <strong>of</strong> Connecticut Health Center, 263<br />
Farmington Ave, Farmington, CT 06030, United States<br />
Satoshi Yamagiwa, MD, PhD, Division <strong>of</strong> Gastroenterology and Hepatology,<br />
Niigata University Graduate School <strong>of</strong> Medical and Dental Sciences,<br />
757 Asahimachi-dori, Chuo-ku, Niigata, 951-8510, Japan<br />
I February 21, 2011|Volume 17|Issue 7|
Online Submissions: http://www.wjgnet.com/1007-9327<strong>of</strong>fice<br />
wjg@wjgnet.com<br />
www.wjgnet.com<br />
Meetings<br />
Events Calendar 2011<br />
January 14-15, 2011<br />
AGA Clinical Congress <strong>of</strong><br />
Gastroenterology and Hepatology:<br />
Best Practices in 2011 Miami, FL<br />
33101, United States<br />
January 20-22, 2011<br />
Gastrointestinal Cancers Symposium<br />
2011, San Francisco, CA 94143,<br />
United States<br />
January 27-28, 2011<br />
Falk Workshop, Liver and<br />
Immunology, Medical University,<br />
Franz-Josef-Strauss-Allee 11, 93053<br />
Regensburg, Germany<br />
January 28-29, 2011<br />
9. Gastro Forum München, Munich,<br />
Germany<br />
February 4-5, 2011<br />
13th Duesseldorf International<br />
Endoscopy Symposium,<br />
Duesseldorf, Germany<br />
February 13-27, 2011<br />
Gastroenterology: New Zealand<br />
CME Cruise Conference, Sydney,<br />
NSW, Australia<br />
February 17-20, 2011<br />
APASL 2011-The 21st Conference <strong>of</strong><br />
the Asian Pacific Association for the<br />
Study <strong>of</strong> the Liver<br />
Bangkok, Thailand<br />
February 22, 2011-March 04, 2011<br />
Canadian Digestive Diseases Week<br />
2011, Vancouver, BC, Canada<br />
February 24-26, 2011<br />
Inflammatory Bowel Diseases<br />
2011-6th Congress <strong>of</strong> the European<br />
Crohn's and Colitis Organisation,<br />
Dublin, Ireland<br />
February 24-26, 2011<br />
2nd International Congress on<br />
Abdominal Obesity, Buenos Aires,<br />
Brazil<br />
February 24-26, 2011<br />
International Colo<strong>rectal</strong> Disease<br />
Symposium 2011, Hong Kong, China<br />
February 26-March 1, 2011<br />
Canadian Digestive Diseases Week,<br />
WJG|www.wjgnet.com<br />
Westin Bayshore, Vancouver, British<br />
Columbia, Canada<br />
February 28-March 1, 2011<br />
Childhood & Adolescent Obesity:<br />
A whole-system strategic approach,<br />
Abu Dhabi, United Arab Emirates<br />
March 3-5, 2011<br />
42nd Annual Topics in Internal<br />
Medicine, Gainesville, FL 32614,<br />
United States<br />
March 7-11, 2011<br />
Infectious Diseases: Adult Issues<br />
in the Outpatient and Inpatient<br />
Settings, Sarasota, FL 34234,<br />
United States<br />
March 14-17, 2011<br />
British Society <strong>of</strong> Gastroenterology<br />
Annual Meeting 2011, Birmingham,<br />
England, United Kingdom<br />
March 17-19, 2011<br />
41. Kongress der Deutschen<br />
Gesellschaft für Endoskopie und<br />
Bildgebende Verfahren e.V., Munich,<br />
Germany<br />
March 17-20, 2011<br />
Mayo Clinic Gastroenterology &<br />
Hepatology 2011, Jacksonville, FL<br />
34234, United States<br />
March 18, 2011<br />
UC Davis Health Informatics:<br />
Change <strong>Management</strong> and Health<br />
Informatics, The Keys to Health<br />
Reform, Sacramento, CA 94143,<br />
United States<br />
March 25-27, 2011<br />
MedicReS IC 2011 Good Medical<br />
Research, Istanbul, Turkey<br />
March 26-27, 2011<br />
26th Annual New Treatments in<br />
Chronic Liver Disease, San Diego,<br />
CA 94143, United States<br />
April 6-7, 2011<br />
IBS-A Global Perspective, Pfister<br />
Hotel, 424 East Wisconsin Avenue,<br />
Milwaukee, WI 53202, United States<br />
April 7-9, 2011<br />
International and Interdisciplinary<br />
Conference Excellence in Female<br />
Surgery, Florence, Italy<br />
April 15-16, 2011<br />
Falk Symposium 177, Endoscopy<br />
Live Berlin 2011 Intestinal Disease<br />
Meeting, Stauffenbergstr. 26, 10785<br />
Berlin, Germany<br />
April 18-22, 2011<br />
Pediatric Emergency Medicine:<br />
Detection, Diagnosis and Developing<br />
Treatment Plans, Sarasota, FL 34234,<br />
United States<br />
April 20-23, 2011<br />
9th International Gastric Cancer<br />
Congress, COEX, <strong>World</strong> Trade<br />
Center, Samseong-dong, Gangnamgu,<br />
Seoul 135-731, South Korea<br />
April 25-27, 2011<br />
The Second International Conference<br />
<strong>of</strong> the Saudi Society <strong>of</strong> Pediatric<br />
Gastroenterology, Hepatology &<br />
Nutrition, Riyadh, Saudi Arabia<br />
April 25-29, 2011<br />
Neurology Updates for Primary<br />
Care, Sarasota, FL 34230-6947,<br />
United States<br />
April 28-30, 2011<br />
4th Central European Congress <strong>of</strong><br />
Surgery, Budapest, Hungary<br />
May 7-10, 2011<br />
Digestive Disease Week, Chicago, IL<br />
60446, United States<br />
May 12-13, 2011<br />
2nd National Conference Clinical<br />
Advances in Cystic Fibrosis, London,<br />
England, United Kingdom<br />
May 19-22, 2011<br />
1st <strong>World</strong> Congress on Controversies<br />
in the <strong>Management</strong> <strong>of</strong> Viral Hepatitis<br />
(C-Hep), Palau de Congressos de<br />
Catalunya, Av. Diagonal, 661-671<br />
Barcelona 08028, Spain<br />
May 21-24, 2011<br />
22nd European Society <strong>of</strong><br />
Gastrointestinal and Abdominal<br />
Radiology Annual Meeting and<br />
Postgraduate Course, Venise, Italy<br />
May 25-28, 2011<br />
4th Congress <strong>of</strong> the Gastroenterology<br />
Association <strong>of</strong> Bosnia and<br />
Herzegovina with international<br />
participation, Hotel Holiday Inn,<br />
Sarajevo, Bosnia and Herzegovina<br />
June 11-12, 2011<br />
The International Digestive Disease<br />
Forum 2011, Hong Kong, China<br />
June 13-16, 2011<br />
Surgery and Disillusion XXIV<br />
SPIGC, II ESYS, Napoli, Italy<br />
June 14-16, 2011<br />
International Scientific Conference<br />
<strong>World</strong> J Gastroenterol 2011 February 21; 17(7): I<br />
ISSN 1007-9327 (print) ISSN 2219-2840 (online)<br />
© 2011 Baishideng. All rights reserved.<br />
on Probiotics and Prebiotics-<br />
IPC2011, Kosice, Slovakia<br />
June 22-25, 2011<br />
ESMO Conference: 13th <strong>World</strong><br />
Congress on Gastrointestinal Cancer,<br />
Barcelona, Spain<br />
June 29-2, 2011<br />
XI Congreso Interamericano<br />
de Pediatria "Monterrey 2011",<br />
Monterrey, Mexico<br />
September 2-3, 2011 Falk Symposium<br />
178, Diverticular Disease, A Fresh<br />
Approach to a Neglected Disease,<br />
Gürzenich Cologne, Martinstr. 29-37,<br />
50667 Cologne, Germany<br />
September 10-11, 2011<br />
New Advances in Inflammatory<br />
Bowel Disease, La Jolla, CA 92093,<br />
United States<br />
September 10-14, 2011<br />
ICE 2011-International Congress <strong>of</strong><br />
Endoscopy, Los Angeles Convention<br />
Center, 1201 South Figueroa Street<br />
Los Angeles, CA 90015,<br />
United States<br />
September 30-October 1, 2011<br />
Falk Symposium 179, Revisiting<br />
IBD <strong>Management</strong>: Dogmas to be<br />
Challenged, Sheraton Brussels<br />
Hotel, Place Rogier 3, 1210 Brussels,<br />
Belgium<br />
October 19-29, 2011<br />
Cardiology & Gastroenterology |<br />
Tahiti 10 night CME Cruise, Papeete,<br />
French Polynesia<br />
October 22-26, 2011<br />
19th United European<br />
Gastroenterology Week, Stockholm,<br />
Sweden<br />
October 28-November 2, 2011<br />
ACG Annual Scientific Meeting &<br />
Postgraduate Course, Washington,<br />
DC 20001, United States<br />
November 11-12, 2011<br />
Falk Symposium 180, IBD 2011:<br />
Progress and Future for Lifelong<br />
<strong>Management</strong>, ANA Interconti Hotel,<br />
1-12-33 Akasaka, Minato-ku, Tokyo<br />
107-0052, Japan<br />
December 1-4, 2011<br />
2011 Advances in Inflammatory<br />
Bowel Diseases/Crohn's & Colitis<br />
Foundation's Clinical & Research<br />
Conference, Hollywood, FL 34234,<br />
United States<br />
I February 21, 2011|Volume 17|Issue 7|
Online Submissions: http://www.wjgnet.com/1007-9327<strong>of</strong>fice<br />
wjg@wjgnet.com<br />
www.wjgnet.com<br />
Instructions to authors<br />
GENERAL INFORMATION<br />
<strong>World</strong> <strong>Journal</strong> <strong>of</strong> Gastroenterology (<strong>World</strong> J Gastroenterol, WJG, print<br />
ISSN 1007-9327, online ISSN 2219-2840, DOI: 10.3748) is a<br />
weekly, open-access (OA), peer-reviewed journal supported by an<br />
editorial board <strong>of</strong> 1144 experts in gastroenterology and hepatology<br />
from 60 countries.<br />
The biggest advantage <strong>of</strong> the OA model is that it provides<br />
free, full-text articles in PDF and other formats for experts and<br />
the public without registration, which eliminates the obstacle<br />
that traditional journals possess and usually delays the speed<br />
<strong>of</strong> the propagation and communication <strong>of</strong> scientific research<br />
results. The open access model has been proven to be a true approach<br />
that may achieve the ultimate goal <strong>of</strong> the journals, i.e. the<br />
maximization <strong>of</strong> the value to the readers, authors and society.<br />
Maximization <strong>of</strong> personal benefits<br />
The role <strong>of</strong> academic journals is to exhibit the scientific levels <strong>of</strong><br />
a country, a university, a center, a department, and even a scientist,<br />
and build an important bridge for communication between scientists<br />
and the public. As we all know, the significance <strong>of</strong> the publication<br />
<strong>of</strong> scientific articles lies not only in disseminating and communicating<br />
innovative scientific achievements and academic views,<br />
as well as promoting the application <strong>of</strong> scientific achievements, but<br />
also in formally recognizing the “priority” and “copyright” <strong>of</strong> innovative<br />
achievements published, as well as evaluating research performance<br />
and academic levels. So, to realize these desired attributes<br />
<strong>of</strong> WJG and create a well-recognized journal, the following four<br />
types <strong>of</strong> personal benefits should be maximized. The maximization<br />
<strong>of</strong> personal benefits refers to the pursuit <strong>of</strong> the maximum personal<br />
benefits in a well-considered optimal manner without violation <strong>of</strong><br />
the laws, ethical rules and the benefits <strong>of</strong> others. (1) Maximization<br />
<strong>of</strong> the benefits <strong>of</strong> editorial board members: The primary task <strong>of</strong><br />
editorial board members is to give a peer review <strong>of</strong> an unpublished<br />
scientific article via online <strong>of</strong>fice system to evaluate its innovativeness,<br />
scientific and practical values and determine whether it should<br />
be published or not. During peer review, editorial board members<br />
can also obtain cutting-edge information in that field at first hand.<br />
As leaders in their field, they have priority to be invited to write<br />
articles and publish commentary articles. We will put peer reviewers’<br />
names and affiliations along with the article they reviewed in<br />
the journal to acknowledge their contribution; (2) Maximization<br />
<strong>of</strong> the benefits <strong>of</strong> authors: Since WJG is an open-access journal,<br />
readers around the world can immediately download and read, free<br />
<strong>of</strong> charge, high-quality, peer-reviewed articles from WJG <strong>of</strong>ficial<br />
website, thereby realizing the goals and significance <strong>of</strong> the communication<br />
between authors and peers as well as public reading; (3)<br />
Maximization <strong>of</strong> the benefits <strong>of</strong> readers: Readers can read or use,<br />
free <strong>of</strong> charge, high-quality peer-reviewed articles without any limits,<br />
and cite the arguments, viewpoints, concepts, theories, methods,<br />
results, conclusion or facts and data <strong>of</strong> pertinent literature so as to<br />
validate the innovativeness, scientific and practical values <strong>of</strong> their<br />
own research achievements, thus ensuring that their articles have<br />
novel arguments or viewpoints, solid evidence and correct conclu-<br />
WJG|www.wjgnet.com<br />
<strong>World</strong> J Gastroenterol 2011 February 21; 17(7): I-VI<br />
ISSN 1007-9327 (print) ISSN 2219-2840 (online)<br />
© 2011 Baishideng. All rights reserved.<br />
sion; and (4) Maximization <strong>of</strong> the benefits <strong>of</strong> employees: It is an<br />
iron law that a first-class journal is unable to exist without first-class<br />
editors, and only first-class editors can create a first-class academic<br />
journal. We insist on strengthening our team cultivation and construction<br />
so that every employee, in an open, fair and transparent<br />
environment, could contribute their wisdom to edit and publish<br />
high-quality articles, thereby realizing the maximization <strong>of</strong> the<br />
personal benefits <strong>of</strong> editorial board members, authors and readers,<br />
and yielding the greatest social and economic benefits.<br />
Aims and scope<br />
The major task <strong>of</strong> WJG is to report rapidly the most recent results<br />
in basic and clinical research on esophageal, gastrointestinal,<br />
liver, pancreas and biliary tract diseases, Helicobacter pylori, endoscopy<br />
and gastrointestinal surgery, including: gastroesophageal<br />
reflux disease, gastrointestinal bleeding, infection and tumors;<br />
gastric and duodenal disorders; intestinal inflammation, micr<strong>of</strong>lora<br />
and immunity; celiac disease, dyspepsia and nutrition; viral<br />
hepatitis, portal hypertension, liver fibrosis, liver cirrhosis, liver<br />
transplantation, and metabolic liver disease; molecular and cell<br />
biology; geriatric and pediatric gastroenterology; diagnosis and<br />
screening, imaging and advanced technology.<br />
Columns<br />
The columns in the issues <strong>of</strong> WJG will include: (1) Editorial: To<br />
introduce and comment on major advances and developments in<br />
the field; (2) Frontier: To review representative achievements, comment<br />
on the state <strong>of</strong> current research, and propose directions for<br />
future research; (3) Topic Highlight: This column consists <strong>of</strong> three<br />
formats, including (A) 10 invited review articles on a hot topic, (B)<br />
a commentary on common issues <strong>of</strong> this hot topic, and (C) a commentary<br />
on the 10 individual articles; (4) Observation: To update<br />
the development <strong>of</strong> old and new questions, highlight unsolved<br />
problems, and provide strategies on how to solve the questions;<br />
(5) Guidelines for Basic Research: To provide guidelines for basic<br />
research; (6) Guidelines for Clinical Practice: To provide guidelines<br />
for clinical diagnosis and treatment; (7) Review: To review systemically<br />
progress and unresolved problems in the field, comment<br />
on the state <strong>of</strong> current research, and make suggestions for future<br />
work; (8) Original Article: To report innovative and original findings<br />
in gastroenterology; (9) Brief Article: To briefly report the<br />
novel and innovative findings in gastroenterology and hepatology;<br />
(10) Case Report: To report a rare or typical case; (11) Letters to the<br />
Editor: To discuss and make reply to the contributions published<br />
in WJG, or to introduce and comment on a controversial issue <strong>of</strong><br />
general interest; (12) Book Reviews: To introduce and comment on<br />
quality monographs <strong>of</strong> gastroenterology and hepatology; and (13)<br />
Guidelines: To introduce consensuses and guidelines reached by<br />
international and national academic authorities worldwide on basic<br />
research and clinical practice gastroenterology and hepatology.<br />
Name <strong>of</strong> journal<br />
<strong>World</strong> <strong>Journal</strong> <strong>of</strong> Gastroenterology<br />
Serial publication number<br />
ISSN 1007-9327 (print)<br />
ISSN 2219-2840 (online)<br />
I February 21, 2011|Volume 17|Issue 7|
Instructions to authors<br />
Indexed and Abstracted in<br />
Current Contents ® /Clinical Medicine, Science Citation Index<br />
Expanded (also known as SciSearch ® ), <strong>Journal</strong> Citation Reports ® ,<br />
Index Medicus, MEDLINE, PubMed, PubMed Central, and<br />
Digital Object Identifer. ISI, Thomson Reuters, 2009 Impact<br />
Factor: 2.092 (33/65 Gastroenterology and Hepatology).<br />
Published by<br />
Baishideng Publishing Group Co., Limited<br />
SPECIAL STATEMENT<br />
All articles published in this journal represent the viewpoints<br />
<strong>of</strong> the authors except where indicated otherwise.<br />
Biostatistical editing<br />
Statisital review is performed after peer review. We invite an<br />
expert in Biomedical Statistics from to evaluate the statistical<br />
method used in the paper, including t-test (group or paired comparisons),<br />
chi-squared test, Ridit, probit, logit, regression (linear,<br />
curvilinear, or stepwise), correlation, analysis <strong>of</strong> variance, analysis<br />
<strong>of</strong> covariance, etc. The reviewing points include: (1) Statistical<br />
methods should be described when they are used to verify the results;<br />
(2) Whether the statistical techniques are suitable or correct;<br />
(3) Only homogeneous data can be averaged. Standard deviations<br />
are preferred to standard errors. Give the number <strong>of</strong> observations<br />
and subjects (n). Losses in observations, such as drop-outs<br />
from the study should be reported; (4) Values such as ED50,<br />
LD50, IC50 should have their 95% confidence limits calculated<br />
and compared by weighted probit analysis (Bliss and Finney); and<br />
(5) The word ‘significantly’ should be replaced by its synonyms (if<br />
it indicates extent) or the P value (if it indicates statistical significance).<br />
Conflict-<strong>of</strong>-interest statement<br />
In the interests <strong>of</strong> transparency and to help reviewers assess<br />
any potential bias, WJG requires authors <strong>of</strong> all papers to declare<br />
any competing commercial, personal, political, intellectual, or<br />
religious interests in relation to the submitted work. Referees<br />
are also asked to indicate any potential conflict they might have<br />
reviewing a particular paper. Before submitting, authors are suggested<br />
to read “Uniform Requirements for Manuscripts Submitted<br />
to Biomedical <strong>Journal</strong>s: Ethical Considerations in the Conduct<br />
and Reporting <strong>of</strong> Research: Conflicts <strong>of</strong> Interest” from<br />
International Committee <strong>of</strong> Medical <strong>Journal</strong> Editors (ICMJE),<br />
which is available at: http://www.icmje.org/ethical_4conflicts.<br />
html.<br />
Sample wording: [Name <strong>of</strong> individual] has received fees for<br />
serving as a speaker, a consultant and an advisory board member<br />
for [names <strong>of</strong> organizations], and has received research funding<br />
from [names <strong>of</strong> organization]. [Name <strong>of</strong> individual] is an employee<br />
<strong>of</strong> [name <strong>of</strong> organization]. [Name <strong>of</strong> individual] owns stocks<br />
and shares in [name <strong>of</strong> organization]. [Name <strong>of</strong> individual] owns<br />
patent [patent identification and brief description].<br />
Statement <strong>of</strong> informed consent<br />
Manuscripts should contain a statement to the effect that all human<br />
studies have been reviewed by the appropriate ethics committee<br />
or it should be stated clearly in the text that all persons<br />
gave their informed consent prior to their inclusion in the study.<br />
Details that might disclose the identity <strong>of</strong> the subjects under<br />
study should be omitted. Authors should also draw attention to<br />
the Code <strong>of</strong> Ethics <strong>of</strong> the <strong>World</strong> Medical Association (Declaration<br />
<strong>of</strong> Helsinki, 1964, as revised in 2004).<br />
WJG|www.wjgnet.com<br />
Statement <strong>of</strong> human and animal rights<br />
When reporting the results from experiments, authors should<br />
follow the highest standards and the trial should conform to<br />
Good Clinical Practice (for example, US Food and Drug Administration<br />
Good Clinical Practice in FDA-Regulated Clinical Trials;<br />
UK Medicines Research Council Guidelines for Good Clinical<br />
Practice in Clinical Trials) and/or the <strong>World</strong> Medical Association<br />
Declaration <strong>of</strong> Helsinki. Generally, we suggest authors follow<br />
the lead investigator’s national standard. If doubt exists whether<br />
the research was conducted in accordance with the above standards,<br />
the authors must explain the rationale for their approach<br />
and demonstrate that the institutional review body explicitly approved<br />
the doubtful aspects <strong>of</strong> the study.<br />
Before submitting, authors should make their study approved<br />
by the relevant research ethics committee or institutional<br />
review board. If human participants were involved, manuscripts<br />
must be accompanied by a statement that the experiments were<br />
undertaken with the understanding and appropriate informed<br />
consent <strong>of</strong> each. Any personal item or information will not be<br />
published without explicit consents from the involved patients.<br />
If experimental animals were used, the materials and methods<br />
(experimental procedures) section must clearly indicate that appropriate<br />
measures were taken to minimize pain or discomfort,<br />
and details <strong>of</strong> animal care should be provided.<br />
SUBMISSION OF MANUSCRIPTS<br />
Manuscripts should be typed in 1.5 line spacing and 12 pt. Book<br />
Antiqua with ample margins. Number all pages consecutively,<br />
and start each <strong>of</strong> the following sections on a new page: Title<br />
Page, Abstract, Introduction, Materials and Methods, Results,<br />
Discussion, Acknowledgements, References, Tables, Figures,<br />
and Figure Legends. Neither the editors nor the publisher are<br />
responsible for the opinions expressed by contributors. Manuscripts<br />
formally accepted for publication become the permanent<br />
property <strong>of</strong> Baishideng Publishing Group Co., Limited, and may<br />
not be reproduced by any means, in whole or in part, without the<br />
written permission <strong>of</strong> both the authors and the publisher. We<br />
reserve the right to copy-edit and put onto our website accepted<br />
manuscripts. Authors should follow the relevant guidelines for<br />
the care and use <strong>of</strong> laboratory animals <strong>of</strong> their institution or<br />
national animal welfare committee. For the sake <strong>of</strong> transparency<br />
in regard to the performance and reporting <strong>of</strong> clinical trials, we<br />
endorse the policy <strong>of</strong> the ICMJE to refuse to publish papers<br />
on clinical trial results if the trial was not recorded in a publiclyaccessible<br />
registry at its outset. The only register now available, to<br />
our knowledge, is http://www.clinicaltrials.gov sponsored by the<br />
United States National Library <strong>of</strong> Medicine and we encourage<br />
all potential contributors to register with it. However, in the case<br />
that other registers become available you will be duly notified.<br />
A letter <strong>of</strong> recommendation from each author’s organization<br />
should be provided with the contributed article to ensure the privacy<br />
and secrecy <strong>of</strong> research is protected.<br />
Authors should retain one copy <strong>of</strong> the text, tables, photographs<br />
and illustrations because rejected manuscripts will not be<br />
returned to the author(s) and the editors will not be responsible<br />
for loss or damage to photographs and illustrations sustained<br />
during mailing.<br />
Online submissions<br />
Manuscripts should be submitted through the Online Submission<br />
System at: http://www.wjgnet.com/1007-9327<strong>of</strong>fice. Authors<br />
are highly recommended to consult the ONLINE INSTRUC-<br />
TIONS TO AUTHORS (http://www.wjgnet.com/1007-9327/<br />
g_info_20100315215714.htm) before attempting to submit on-<br />
II February 21, 2011|Volume 17|Issue 7|
line. For assistance, authors encountering problems with the Online<br />
Submission System may send an email describing the problem<br />
to wjg@wjgnet.com, or by telephone: +86-10-5908-0039. If<br />
you submit your manuscript online, do not make a postal contribution.<br />
Repeated online submission for the same manuscript is<br />
strictly prohibited.<br />
MANUSCRIPT PREPARATION<br />
All contributions should be written in English. All articles must be<br />
submitted using word-processing s<strong>of</strong>tware. All submissions must<br />
be typed in 1.5 line spacing and 12 pt. Book Antiqua with ample<br />
margins. Style should conform to our house format. Required information<br />
for each <strong>of</strong> the manuscript sections is as follows:<br />
Title page<br />
Title: Title should be less than 12 words.<br />
Running title: A short running title <strong>of</strong> less than 6 words should<br />
be provided.<br />
Authorship: Authorship credit should be in accordance with the<br />
standard proposed by ICMJE, based on (1) substantial contributions<br />
to conception and design, acquisition <strong>of</strong> data, or analysis and<br />
interpretation <strong>of</strong> data; (2) drafting the article or revising it critically<br />
for important intellectual content; and (3) final approval <strong>of</strong> the<br />
version to be published. Authors should meet conditions 1, 2, and 3.<br />
Institution: Author names should be given first, then the complete<br />
name <strong>of</strong> institution, city, province and postcode. For example,<br />
Xu-Chen Zhang, Li-Xin Mei, Department <strong>of</strong> Pathology,<br />
Chengde Medical College, Chengde 067000, Hebei Province,<br />
China. One author may be represented from two institutions,<br />
for example, George Sgourakis, Department <strong>of</strong> General, Visceral,<br />
and Transplantation Surgery, Essen 45122, Germany; George<br />
Sgourakis, 2nd Surgical Department, Korgialenio-Benakio Red<br />
Cross Hospital, Athens 15451, Greece.<br />
Author contributions: The format <strong>of</strong> this section should be:<br />
Author contributions: Wang CL and Liang L contributed equally<br />
to this work; Wang CL, Liang L, Fu JF, Zou CC, Hong F and Wu<br />
XM designed the research; Wang CL, Zou CC, Hong F and Wu<br />
XM performed the research; Xue JZ and Lu JR contributed new<br />
reagents/analytic tools; Wang CL, Liang L and Fu JF analyzed the<br />
data; and Wang CL, Liang L and Fu JF wrote the paper.<br />
Supportive foundations: The complete name and number <strong>of</strong><br />
supportive foundations should be provided, e.g. Supported by<br />
National Natural Science Foundation <strong>of</strong> China, No. 30224801<br />
Correspondence to: Only one corresponding address should be<br />
provided. Author names should be given first, then author title,<br />
affiliation, the complete name <strong>of</strong> institution, city, postcode, province,<br />
country, and email. All the letters in the email should be in<br />
lower case. A space interval should be inserted between country<br />
name and email address. For example, Montgomery Bissell, MD,<br />
Pr<strong>of</strong>essor <strong>of</strong> Medicine, Chief, Liver Center, Gastroenterology<br />
Division, University <strong>of</strong> California, Box 0538, San Francisco, CA<br />
94143, United States. montgomery.bissell@ucsf.edu<br />
Telephone and fax: Telephone and fax should consist <strong>of</strong> +,<br />
country number, district number and telephone or fax number,<br />
e.g. Telephone: +86-10-59080039 Fax: +86-10-85381893<br />
Peer reviewers: All articles received are subject to peer review.<br />
WJG|www.wjgnet.com<br />
Instructions to authors<br />
Normally, three experts are invited for each article. Decision for<br />
acceptance is made only when at least two experts recommend<br />
an article for publication. Reviewers for accepted manuscripts<br />
are acknowledged in each manuscript, and reviewers <strong>of</strong> articles<br />
which were not accepted will be acknowledged at the end <strong>of</strong><br />
each issue. To ensure the quality <strong>of</strong> the articles published in WJG,<br />
reviewers <strong>of</strong> accepted manuscripts will be announced by publishing<br />
the name, title/position and institution <strong>of</strong> the reviewer in the<br />
footnote accompanying the printed article. For example, reviewers:<br />
Pr<strong>of</strong>essor Jing-Yuan Fang, Shanghai Institute <strong>of</strong> Digestive<br />
Disease, Shanghai, Affiliated Renji Hospital, Medical Faculty,<br />
Shanghai Jiaotong University, Shanghai, China; Pr<strong>of</strong>essor Xin-<br />
Wei Han, Department <strong>of</strong> Radiology, The First Affiliated Hospital,<br />
Zhengzhou University, Zhengzhou, Henan Province, China; and<br />
Pr<strong>of</strong>essor Anren Kuang, Department <strong>of</strong> Nuclear Medicine, Huaxi<br />
Hospital, Sichuan University, Chengdu, Sichuan Province, China.<br />
Abstract<br />
There are unstructured abstracts (no more than 256 words)<br />
and structured abstracts (no more than 480). The specific requirements<br />
for structured abstracts are as follows:<br />
An informative, structured abstracts <strong>of</strong> no more than 480<br />
words should accompany each manuscript. Abstracts for original<br />
contributions should be structured into the following sections.<br />
AIM (no more than 20 words): Only the purpose should be<br />
included. Please write the aim as the form <strong>of</strong> “To investigate/<br />
study/…”; MATERIALS AND METHODS (no more than<br />
140 words); RESULTS (no more than 294 words): You should<br />
present P values where appropriate and must provide relevant<br />
data to illustrate how they were obtained, e.g. 6.92 ± 3.86 vs 3.61<br />
± 1.67, P < 0.001; CONCLUSION (no more than 26 words).<br />
Key words<br />
Please list 5-10 key words, selected mainly from Index Medicus,<br />
which reflect the content <strong>of</strong> the study.<br />
Text<br />
For articles <strong>of</strong> these sections, original articles and brief articles,<br />
the main text should be structured into the following sections:<br />
INTRODUCTION, MATERIALS AND METHODS,<br />
RESULTS and DISCUSSION, and should include appropriate<br />
Figures and Tables. Data should be presented in the main<br />
text or in Figures and Tables, but not in both. The main text<br />
format <strong>of</strong> these sections, editorial, topic highlight, case report,<br />
letters to the editors, can be found at: http://www.wjgnet.<br />
com/1007-9327/g_info_20100315215714.htm.<br />
Illustrations<br />
Figures should be numbered as 1, 2, 3, etc., and mentioned clearly<br />
in the main text. Provide a brief title for each figure on a separate<br />
page. Detailed legends should not be provided under the<br />
figures. This part should be added into the text where the figures<br />
are applicable. Figures should be either Photoshop or Illustrator<br />
files (in tiff, eps, jpeg formats) at high-resolution. Examples<br />
can be found at: http://www.wjgnet.com/1007-9327/13/4520.<br />
pdf; http://www.wjgnet.com/1007-9327/13/4554.pdf;<br />
http://www.wjgnet.com/1007-9327/13/4891.pdf; http://<br />
www.wjgnet.com/1007-9327/13/4986.pdf; http://www.<br />
wjgnet.com/1007-9327/13/4498.pdf. Keeping all elements<br />
compiled is necessary in line-art image. Scale bars should be<br />
used rather than magnification factors, with the length <strong>of</strong><br />
the bar defined in the legend rather than on the bar itself.<br />
File names should identify the figure and panel. Avoid layering<br />
type directly over shaded or textured areas. Please use<br />
III February 21, 2011|Volume 17|Issue 7|
Instructions to authors<br />
uniform legends for the same subjects. For example: Figure 1<br />
Pathological changes in atrophic gastritis after treatment. A:...;<br />
B:...; C:...; D:...; E:...; F:...; G: …etc. It is our principle to publish<br />
high resolution-figures for the printed and E-versions.<br />
Tables<br />
Three-line tables should be numbered 1, 2, 3, etc., and mentioned<br />
clearly in the main text. Provide a brief title for each<br />
table. Detailed legends should not be included under tables,<br />
but rather added into the text where applicable. The information<br />
should complement, but not duplicate the text. Use one<br />
horizontal line under the title, a second under column heads,<br />
and a third below the Table, above any footnotes. Vertical and<br />
italic lines should be omitted.<br />
Notes in tables and illustrations<br />
Data that are not statistically significant should not be noted.<br />
a P < 0.05, b P < 0.01 should be noted (P > 0.05 should not be<br />
noted). If there are other series <strong>of</strong> P values, c P < 0.05 and d P<br />
< 0.01 are used. A third series <strong>of</strong> P values can be expressed as<br />
e P < 0.05 and f P < 0.01. Other notes in tables or under illustrations<br />
should be expressed as 1 F, 2 F, 3 F; or sometimes as other<br />
symbols with a superscript (Arabic numerals) in the upper left<br />
corner. In a multi-curve illustration, each curve should be labeled<br />
with ●, ○, ■, □, ▲, △, etc., in a certain sequence.<br />
Acknowledgments<br />
Brief acknowledgments <strong>of</strong> persons who have made genuine<br />
contributions to the manuscript and who endorse the data and<br />
conclusions should be included. Authors are responsible for<br />
obtaining written permission to use any copyrighted text and/or<br />
illustrations.<br />
REFERENCES<br />
Coding system<br />
The author should number the references in Arabic numerals according<br />
to the citation order in the text. Put reference numbers<br />
in square brackets in superscript at the end <strong>of</strong> citation content or<br />
after the cited author’s name. For citation content which is part <strong>of</strong><br />
the narration, the coding number and square brackets should be<br />
typeset normally. For example, “Crohn’s disease (CD) is associated<br />
with increased intestinal permeability [1,2] ”. If references are cited<br />
directly in the text, they should be put together within the text, for<br />
example, “From references [19,22-24] , we know that...”.<br />
When the authors write the references, please ensure that<br />
the order in text is the same as in the references section, and also<br />
ensure the spelling accuracy <strong>of</strong> the first author’s name. Do not list<br />
the same citation twice.<br />
PMID and DOI<br />
Pleased provide PubMed citation numbers to the reference list,<br />
e.g. PMID and DOI, which can be found at http://www.ncbi.<br />
nlm.nih.gov/sites/entrez?db=pubmed and http://www.crossref.org/SimpleTextQuery/,<br />
respectively. The numbers will be<br />
used in E-version <strong>of</strong> this journal.<br />
Style for journal references<br />
Authors: the name <strong>of</strong> the first author should be typed in boldfaced<br />
letters. The family name <strong>of</strong> all authors should be typed<br />
with the initial letter capitalized, followed by their abbreviated<br />
first and middle initials. (For example, Lian-Sheng Ma is abbreviated<br />
as Ma LS, Bo-Rong Pan as Pan BR). The title <strong>of</strong> the<br />
cited article and italicized journal title (journal title should be<br />
in its abbreviated form as shown in PubMed), publication date,<br />
WJG|www.wjgnet.com<br />
volume number (in black), start page, and end page [PMID:<br />
11819634 DOI: 10.3748/wjg.13.5396].<br />
Style for book references<br />
Authors: the name <strong>of</strong> the first author should be typed in boldfaced<br />
letters. The surname <strong>of</strong> all authors should be typed with the<br />
initial letter capitalized, followed by their abbreviated middle and<br />
first initials. (For example, Lian-Sheng Ma is abbreviated as Ma LS,<br />
Bo-Rong Pan as Pan BR) Book title. Publication number. Publication<br />
place: Publication press, Year: start page and end page.<br />
Format<br />
<strong>Journal</strong>s<br />
English journal article (list all authors and include the PMID where applicable)<br />
1 Jung EM, Clevert DA, Schreyer AG, Schmitt S, Rennert J,<br />
Kubale R, Feuerbach S, Jung F. Evaluation <strong>of</strong> quantitative<br />
contrast harmonic imaging to assess malignancy <strong>of</strong> liver<br />
tumors: A prospective controlled two-center study. <strong>World</strong> J<br />
Gastroenterol 2007; 13: 6356-6364 [PMID: 18081224 DOI:<br />
10.3748/wjg.13.6356]<br />
Chinese journal article (list all authors and include the PMID where applicable)<br />
2 Lin GZ, Wang XZ, Wang P, Lin J, Yang FD. Immunologic<br />
effect <strong>of</strong> Jianpi Yishen decoction in treatment <strong>of</strong> Pixudiarrhoea.<br />
Shijie Huaren Xiaohua Zazhi 1999; 7: 285-287<br />
In press<br />
3 Tian D, Araki H, Stahl E, Bergelson J, Kreitman M.<br />
Signature <strong>of</strong> balancing selection in Arabidopsis. Proc Natl<br />
Acad Sci USA 2006; In press<br />
Organization as author<br />
4 Diabetes Prevention Program Research Group. Hypertension,<br />
insulin, and proinsulin in participants with impaired<br />
glucose tolerance. Hypertension 2002; 40: 679-686 [PMID:<br />
12411462 PMCID:2516377 DOI:10.1161/01.HYP.00000<br />
35706.28494.09]<br />
Both personal authors and an organization as author<br />
5 Vallancien G, Emberton M, Harving N, van Moorselaar<br />
RJ; Alf-One Study Group. Sexual dysfunction in 1,<br />
274 European men suffering from lower urinary tract<br />
symptoms. J Urol 2003; 169: 2257-2261 [PMID: 12771764<br />
DOI:10.1097/01.ju.0000067940.76090.73]<br />
No author given<br />
6 21st century heart solution may have a sting in the tail. BMJ<br />
2002; 325: 184 [PMID: 12142303 DOI:10.1136/bmj.325.<br />
7357.184]<br />
Volume with supplement<br />
7 Geraud G, Spierings EL, Keywood C. Tolerability and<br />
safety <strong>of</strong> frovatriptan with short- and long-term use for<br />
treatment <strong>of</strong> migraine and in comparison with sumatriptan.<br />
Headache 2002; 42 Suppl 2: S93-99 [PMID: 12028325<br />
DOI:10.1046/j.1526-4610.42.s2.7.x]<br />
Issue with no volume<br />
8 Banit DM, Kaufer H, Hartford JM. Intraoperative frozen<br />
section analysis in revision total joint arthroplasty. Clin<br />
Orthop Relat Res 2002; (401): 230-238 [PMID: 12151900<br />
DOI:10.1097/00003086-200208000-00026]<br />
No volume or issue<br />
9 Outreach: Bringing HIV-positive individuals into care.<br />
HRSA Careaction 2002; 1-6 [PMID: 12154804]<br />
Books<br />
Personal author(s)<br />
10 Sherlock S, Dooley J. Diseases <strong>of</strong> the liver and billiary<br />
system. 9th ed. Oxford: Blackwell Sci Pub, 1993: 258-296<br />
IV February 21, 2011|Volume 17|Issue 7|
Chapter in a book (list all authors)<br />
11 Lam SK. Academic investigator’s perspectives <strong>of</strong> medical<br />
treatment for peptic ulcer. In: Swabb EA, Azabo S. Ulcer<br />
disease: investigation and basis for therapy. New York:<br />
Marcel Dekker, 1991: 431-450<br />
Author(s) and editor(s)<br />
12 Breedlove GK, Schorfheide AM. Adolescent pregnancy.<br />
2nd ed. Wieczorek RR, editor. White Plains (NY): March<br />
<strong>of</strong> Dimes Education Services, 2001: 20-34<br />
Conference proceedings<br />
13 Harnden P, J<strong>of</strong>fe JK, Jones WG, editors. Germ cell tumours<br />
V. Proceedings <strong>of</strong> the 5th Germ cell tumours Conference;<br />
2001 Sep 13-15; Leeds, UK. New York: Springer,<br />
2002: 30-56<br />
Conference paper<br />
14 Christensen S, Oppacher F. An analysis <strong>of</strong> Koza’s computational<br />
effort statistic for genetic programming. In: Foster<br />
JA, Lutton E, Miller J, Ryan C, Tettamanzi AG, editors. Genetic<br />
programming. EuroGP 2002: Proceedings <strong>of</strong> the 5th<br />
European Conference on Genetic Programming; 2002 Apr<br />
3-5; Kinsdale, Ireland. Berlin: Springer, 2002: 182-191<br />
Electronic journal (list all authors)<br />
15 Morse SS. Factors in the emergence <strong>of</strong> infectious diseases.<br />
Emerg Infect Dis serial online, 1995-01-03, cited<br />
1996-06-05; 1(1): 24 screens. Available from: URL: http://<br />
www.cdc.gov/ncidod/eid/index.htm<br />
Patent (list all authors)<br />
16 Pagedas AC, inventor; Ancel Surgical R&D Inc., assignee.<br />
Flexible endoscopic grasping and cutting device<br />
and positioning tool assembly. United States patent US<br />
20020103498. 2002 Aug 1<br />
Statistical data<br />
Write as mean ± SD or mean ± SE.<br />
Statistical expression<br />
Express t test as t (in italics), F test as F (in italics), chi square test<br />
as χ 2 (in Greek), related coefficient as r (in italics), degree <strong>of</strong> freedom<br />
as υ (in Greek), sample number as n (in italics), and probability<br />
as P (in italics).<br />
Units<br />
Use SI units. For example: body mass, m (B) = 78 kg; blood pressure,<br />
p (B) = 16.2/12.3 kPa; incubation time, t (incubation) = 96 h,<br />
blood glucose concentration, c (glucose) 6.4 ± 2.1 mmol/L; blood<br />
CEA mass concentration, p (CEA) = 8.6 24.5 mg/L; CO 2 volume<br />
fraction, 50 mL/L CO 2, not 5% CO 2; likewise for 40 g/L formaldehyde,<br />
not 10% formalin; and mass fraction, 8 ng/g, etc. Arabic<br />
numerals such as 23, 243, 641 should be read 23 243 641.<br />
The format for how to accurately write common units and<br />
quantums can be found at: http://www.wjgnet.com/1007-9327/<br />
g_info_20100315223018.htm.<br />
Abbreviations<br />
Standard abbreviations should be defined in the abstract and<br />
on first mention in the text. In general, terms should not be abbreviated<br />
unless they are used repeatedly and the abbreviation<br />
is helpful to the reader. Permissible abbreviations are listed in<br />
Units, Symbols and Abbreviations: A Guide for Biological and<br />
Medical Editors and Authors (Ed. Baron DN, 1988) published<br />
by The Royal Society <strong>of</strong> Medicine, London. Certain commonly<br />
used abbreviations, such as DNA, RNA, HIV, LD50, PCR,<br />
HBV, ECG, WBC, RBC, CT, ESR, CSF, IgG, ELISA, PBS, ATP,<br />
EDTA, mAb, can be used directly without further explanation.<br />
WJG|www.wjgnet.com<br />
Italics<br />
Quantities: t time or temperature, c concentration, A area, l length,<br />
m mass, V volume.<br />
Genotypes: gyrA, arg 1, c myc, c fos, etc.<br />
Restriction enzymes: EcoRI, HindI, BamHI, Kbo I, Kpn I, etc.<br />
Biology: H. pylori, E coli, etc.<br />
Examples for paper writing<br />
Editorial: http://www.wjgnet.com/1007-9327/g_info_20100315<br />
220036.htm<br />
Frontier: http://www.wjgnet.com/1007-9327/g_info_20100315<br />
220305.htm<br />
Topic highlight: http://www.wjgnet.com/1007-9327/g_info_20<br />
100315220601.htm<br />
Observation: http://www.wjgnet.com/1007-9327/g_info_201003<br />
12232427.htm<br />
Guidelines for basic research: http://www.wjgnet.com/1007-93<br />
27/g_info_20100315220730.htm<br />
Guidelines for clinical practice: http://www.wjgnet.com/1007-<br />
9327/g_info_20100315221301.htm<br />
Review: http://www.wjgnet.com/1007-9327/g_info_20100315<br />
221554.htm<br />
Original articles: http://www.wjgnet.com/1007-9327/g_info_20<br />
100315221814.htm<br />
Brief articles: http://www.wjgnet.com/1007-9327/g_info_2010<br />
0312231400.htm<br />
Case report: http://www.wjgnet.com/1007-9327/g_info_2010<br />
0315221946.htm<br />
Letters to the editor: http://www.wjgnet.com/1007-9327/g_info_<br />
20100315222254.htm<br />
Book reviews: http://www.wjgnet.com/1007-9327/g_info_2010<br />
0312231947.htm<br />
Guidelines: http://www.wjgnet.com/1007-9327/g_info_2010<br />
0312232134.htm<br />
RESUBMISSION OF THE REVISED<br />
MANUSCRIPTS<br />
Please revise your article according to the revision policies <strong>of</strong><br />
WJG. The revised version includes manuscript and high-resolution<br />
image figures. The author should re-submit the revised<br />
manuscript online, along with printed high-resolution color or<br />
black and white photos; Copyright transfer letter, and responses<br />
to the reviewers, and science news are sent to us via email.<br />
Editorial Office<br />
<strong>World</strong> <strong>Journal</strong> <strong>of</strong> Gastroenterology<br />
Editorial Department: Room 903, Building D,<br />
Ocean International Center,<br />
No. 62 Dongsihuan Zhonglu,<br />
Chaoyang District, Beijing 100025, China<br />
E-mail: wjg@wjgnet.com<br />
http://www.wjgnet.com<br />
Telephone: +86-10-5908-0039<br />
Fax: +86-10-85381893<br />
Instructions to authors<br />
V February 21, 2011|Volume 17|Issue 7|
Instructions to authors<br />
Language evaluation<br />
The language <strong>of</strong> a manuscript will be graded before it is sent for<br />
revision. (1) Grade A: priority publishing; (2) Grade B: minor<br />
language polishing; (3) Grade C: a great deal <strong>of</strong> language polishing<br />
needed; and (4) Grade D: rejected. Revised articles should<br />
reach Grade A or B.<br />
Copyright assignment form<br />
Please download a Copyright assignment form from http://<br />
www.wjgnet.com/1007-9327/g_info_20100315222818.htm.<br />
Responses to reviewers<br />
Please revise your article according to the comments/suggestions<br />
provided by the reviewers. The format for responses to<br />
the reviewers’ comments can be found at: http://www.wjgnet.<br />
com/1007-9327/g_info_20100315222607.htm.<br />
Pro<strong>of</strong> <strong>of</strong> financial support<br />
For paper supported by a foundation, authors should provide<br />
a copy <strong>of</strong> the document and serial number <strong>of</strong> the foundation.<br />
Links to documents related to the manuscript<br />
WJG will be initiating a platform to promote dynamic interac-<br />
WJG|www.wjgnet.com<br />
tions between the editors, peer reviewers, readers and authors.<br />
After a manuscript is published online, links to the PDF version<br />
<strong>of</strong> the submitted manuscript, the peer-reviewers’ report and the<br />
revised manuscript will be put on-line. Readers can make comments<br />
on the peer reviewer’s report, authors’ responses to peer<br />
reviewers, and the revised manuscript. We hope that authors will<br />
benefit from this feedback and be able to revise the manuscript<br />
accordingly in a timely manner.<br />
Science news releases<br />
Authors <strong>of</strong> accepted manuscripts are suggested to write a science<br />
news item to promote their articles. The news will be<br />
released rapidly at EurekAlert/AAAS (http://www.eurekalert.<br />
org). The title for news items should be less than 90 characters;<br />
the summary should be less than 75 words; and main body less<br />
than 500 words. Science news items should be lawful, ethical,<br />
and strictly based on your original content with an attractive title<br />
and interesting pictures.<br />
Publication fee<br />
Authors <strong>of</strong> accepted articles must pay a publication fee.<br />
EDITORIAL, TOPIC HIGHLIGHTS, BOOK REVIEWS and<br />
LETTERS TO THE EDITOR are published free <strong>of</strong> charge.<br />
VI February 21, 2011|Volume 17|Issue 7|